User login
Shrink Rap News: Brandon Marshall, the NFL, and borderline personality disorder
I am what you’d call an unwilling sports fan – and then just barely – in that I reside in a family where everyone else is riveted by sports, and by football in particular. The National Football League is the backdrop to my home life on Sundays, Mondays, and Thursdays, with Saturday reserved for college football, all the more so since both of my children have attended Big 10 universities. With that as a background, I was delighted when the Sept. 19 episode of the NFL’s “A Football Life,” focused on Brandon Marshall, the Chicago Bears wide receiver who has talked publicly about his personal struggles with borderline personality disorder.
While many psychiatric disorders are stigmatized by people who are unfamiliar with them, borderline personality disorder is likely the illness that gets most stigmatized within our profession. “Borderline” or “Cluster B” are sometimes uttered as code, to mean that a patient is difficult to work with, unlikeable, or perhaps even manipulative. We often blame patients for their behaviors in ways that we don’t when a patient is ill with an Axis I disorder, and few psychiatrists relish the opportunity to work with patients who have borderline personality disorder.
The television episode focused on Marshall’s football career, his legal struggles, and his interpersonal relationships both on and off the playing field. There were spotlights on many of the people who were affected by his troubling behavior. Marshall described his relationship with his best friend and quarterback, Jay Cutler, as, “We’re the couple that really love each other but shouldn’t be together.”
Cutler was interviewed. He described Marshall as an emotional man who loved media attention and who would lose his temper and hang on to grudges. They first played together for the Denver Broncos, and now both men play for the Chicago Bears.
Marshall’s agent was interviewed and made the point that Marshall had “…personally destroyed maybe five of my vacations.” Marshall’s former coach; his wife; his mother; and his psychiatrist, Dr. John Gunderson of McLean Hospital in Belmont, Mass., were all interviewed on the show.
The narrator for “A Football Life” described Marshall’s behavior as erratic, both on and off the field. Film clips were shown of Marshall losing his temper, kicking the ball off the field during a penalty, and celebrating excessively. His mother referred to his outbursts as “hissy fits,” and she noted, “We were all under the impression Brandon could control this.”
Despite his talent as a wide receiver – while playing for the Broncos, Marshall caught more than 100 passes in each of three consecutive seasons – the Broncos traded him to the Miami Dolphins. His career with the Broncos had been marked by a brief suspension for charges of drunk driving and domestic violence, and Marshall had had numerous arrests over the years. He finally was required to have a psychiatric assessment, and Marshall flew to Massachusetts for a day-long evaluation with Dr. Gunderson. Dr. Gunderson described Marshall at that meeting as “hostile and nondisclosing.”
In Miami, Marshall’s behavior continued to be a source of contention. His girlfriend, Michi, described him as remote and withdrawn. After a domestic dispute in which she was charged with stabbing him – charges that both denied and were later dropped – Marshall returned to see Dr. Gunderson and dedicated 3 months of his off-season to getting treatment.
Dr. Gunderson noted that on his return visit, “He was troubled enough by his behaviors and the difficulties they were causing for him.”
With a diagnosis of borderline personality disorder, Marshall became invested in learning about the disorder and devoted his days to intensive treatment, which included group therapy. He discussed the difficulties he has regulating his emotions and noted that he now had strategies to help him maintain control. Cutler noted that Marshall still loses his cool, but he quickly regains his composure, while in the past he could stay angry for days.
The rest of the show went on to document Marshall’s successes. He gained better control of his temper and became less difficult to work with. Coach Tony Sparano was interviewed, and both he and Marshall talked of Sparano’s role in providing emotional support to the football player. He was offered a $30 million contract extension with the Bears. He and Michi married, started the Brandon Marshall Foundation to support mental health education and treatment, and the couple announced in September that they are expecting twins.
Dr. Gunderson noted that Brandon Marshall’s openness about his disorder does a great deal to alleviate the stigma associated with borderline personality disorder.
“He’s an articulate and charismatic male football player,” he said. “This takes it out of the realm of something that’s about weak people.”
The special did not talk about whether Marshall was taking medications – it was implied that he wasn’t – or if he has continued in treatment. We think of borderline personality disorder as being resistant to treatments, and certainly not as a disorder that can be fixed with 3 months of treatment. It was noted that Marshall has some unusual assets in addition to his charismatic personality: He has a vocation he loves and is good at, and he has supportive relationships. A clip was shown of an appearance he and Michi had made on “The View,” where he credited her support as being key to his success.
As psychiatrists, there is a delicate balance when treating patients with personality disorders. On the one hand, we want them to take ownership for their behaviors in the hopes that they will be able to gain some control over them. To balance this, however, personality disorders can be as crippling as any illness we treat in psychiatry, and the prognosis for some people is dismal. While it may be helpful to have a diagnosis and an explanation, it’s not beneficial if the patient sees himself as the victim of an untreatable condition. The television special on Brandon Marshall did a wonderful job of presenting this disorder with a balance – as a problem that happens to people, perhaps because of their difficult childhoods – but one that the individual can learn to take control of in an empowering way.
We might imagine this remains an ongoing struggle for Marshall, not one that was treated and fixed. I, however, enjoyed watching an NFL production with a positive spin on what we think of as being such a devastating psychiatric disorder.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
I am what you’d call an unwilling sports fan – and then just barely – in that I reside in a family where everyone else is riveted by sports, and by football in particular. The National Football League is the backdrop to my home life on Sundays, Mondays, and Thursdays, with Saturday reserved for college football, all the more so since both of my children have attended Big 10 universities. With that as a background, I was delighted when the Sept. 19 episode of the NFL’s “A Football Life,” focused on Brandon Marshall, the Chicago Bears wide receiver who has talked publicly about his personal struggles with borderline personality disorder.
While many psychiatric disorders are stigmatized by people who are unfamiliar with them, borderline personality disorder is likely the illness that gets most stigmatized within our profession. “Borderline” or “Cluster B” are sometimes uttered as code, to mean that a patient is difficult to work with, unlikeable, or perhaps even manipulative. We often blame patients for their behaviors in ways that we don’t when a patient is ill with an Axis I disorder, and few psychiatrists relish the opportunity to work with patients who have borderline personality disorder.
The television episode focused on Marshall’s football career, his legal struggles, and his interpersonal relationships both on and off the playing field. There were spotlights on many of the people who were affected by his troubling behavior. Marshall described his relationship with his best friend and quarterback, Jay Cutler, as, “We’re the couple that really love each other but shouldn’t be together.”
Cutler was interviewed. He described Marshall as an emotional man who loved media attention and who would lose his temper and hang on to grudges. They first played together for the Denver Broncos, and now both men play for the Chicago Bears.
Marshall’s agent was interviewed and made the point that Marshall had “…personally destroyed maybe five of my vacations.” Marshall’s former coach; his wife; his mother; and his psychiatrist, Dr. John Gunderson of McLean Hospital in Belmont, Mass., were all interviewed on the show.
The narrator for “A Football Life” described Marshall’s behavior as erratic, both on and off the field. Film clips were shown of Marshall losing his temper, kicking the ball off the field during a penalty, and celebrating excessively. His mother referred to his outbursts as “hissy fits,” and she noted, “We were all under the impression Brandon could control this.”
Despite his talent as a wide receiver – while playing for the Broncos, Marshall caught more than 100 passes in each of three consecutive seasons – the Broncos traded him to the Miami Dolphins. His career with the Broncos had been marked by a brief suspension for charges of drunk driving and domestic violence, and Marshall had had numerous arrests over the years. He finally was required to have a psychiatric assessment, and Marshall flew to Massachusetts for a day-long evaluation with Dr. Gunderson. Dr. Gunderson described Marshall at that meeting as “hostile and nondisclosing.”
In Miami, Marshall’s behavior continued to be a source of contention. His girlfriend, Michi, described him as remote and withdrawn. After a domestic dispute in which she was charged with stabbing him – charges that both denied and were later dropped – Marshall returned to see Dr. Gunderson and dedicated 3 months of his off-season to getting treatment.
Dr. Gunderson noted that on his return visit, “He was troubled enough by his behaviors and the difficulties they were causing for him.”
With a diagnosis of borderline personality disorder, Marshall became invested in learning about the disorder and devoted his days to intensive treatment, which included group therapy. He discussed the difficulties he has regulating his emotions and noted that he now had strategies to help him maintain control. Cutler noted that Marshall still loses his cool, but he quickly regains his composure, while in the past he could stay angry for days.
The rest of the show went on to document Marshall’s successes. He gained better control of his temper and became less difficult to work with. Coach Tony Sparano was interviewed, and both he and Marshall talked of Sparano’s role in providing emotional support to the football player. He was offered a $30 million contract extension with the Bears. He and Michi married, started the Brandon Marshall Foundation to support mental health education and treatment, and the couple announced in September that they are expecting twins.
Dr. Gunderson noted that Brandon Marshall’s openness about his disorder does a great deal to alleviate the stigma associated with borderline personality disorder.
“He’s an articulate and charismatic male football player,” he said. “This takes it out of the realm of something that’s about weak people.”
The special did not talk about whether Marshall was taking medications – it was implied that he wasn’t – or if he has continued in treatment. We think of borderline personality disorder as being resistant to treatments, and certainly not as a disorder that can be fixed with 3 months of treatment. It was noted that Marshall has some unusual assets in addition to his charismatic personality: He has a vocation he loves and is good at, and he has supportive relationships. A clip was shown of an appearance he and Michi had made on “The View,” where he credited her support as being key to his success.
As psychiatrists, there is a delicate balance when treating patients with personality disorders. On the one hand, we want them to take ownership for their behaviors in the hopes that they will be able to gain some control over them. To balance this, however, personality disorders can be as crippling as any illness we treat in psychiatry, and the prognosis for some people is dismal. While it may be helpful to have a diagnosis and an explanation, it’s not beneficial if the patient sees himself as the victim of an untreatable condition. The television special on Brandon Marshall did a wonderful job of presenting this disorder with a balance – as a problem that happens to people, perhaps because of their difficult childhoods – but one that the individual can learn to take control of in an empowering way.
We might imagine this remains an ongoing struggle for Marshall, not one that was treated and fixed. I, however, enjoyed watching an NFL production with a positive spin on what we think of as being such a devastating psychiatric disorder.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
I am what you’d call an unwilling sports fan – and then just barely – in that I reside in a family where everyone else is riveted by sports, and by football in particular. The National Football League is the backdrop to my home life on Sundays, Mondays, and Thursdays, with Saturday reserved for college football, all the more so since both of my children have attended Big 10 universities. With that as a background, I was delighted when the Sept. 19 episode of the NFL’s “A Football Life,” focused on Brandon Marshall, the Chicago Bears wide receiver who has talked publicly about his personal struggles with borderline personality disorder.
While many psychiatric disorders are stigmatized by people who are unfamiliar with them, borderline personality disorder is likely the illness that gets most stigmatized within our profession. “Borderline” or “Cluster B” are sometimes uttered as code, to mean that a patient is difficult to work with, unlikeable, or perhaps even manipulative. We often blame patients for their behaviors in ways that we don’t when a patient is ill with an Axis I disorder, and few psychiatrists relish the opportunity to work with patients who have borderline personality disorder.
The television episode focused on Marshall’s football career, his legal struggles, and his interpersonal relationships both on and off the playing field. There were spotlights on many of the people who were affected by his troubling behavior. Marshall described his relationship with his best friend and quarterback, Jay Cutler, as, “We’re the couple that really love each other but shouldn’t be together.”
Cutler was interviewed. He described Marshall as an emotional man who loved media attention and who would lose his temper and hang on to grudges. They first played together for the Denver Broncos, and now both men play for the Chicago Bears.
Marshall’s agent was interviewed and made the point that Marshall had “…personally destroyed maybe five of my vacations.” Marshall’s former coach; his wife; his mother; and his psychiatrist, Dr. John Gunderson of McLean Hospital in Belmont, Mass., were all interviewed on the show.
The narrator for “A Football Life” described Marshall’s behavior as erratic, both on and off the field. Film clips were shown of Marshall losing his temper, kicking the ball off the field during a penalty, and celebrating excessively. His mother referred to his outbursts as “hissy fits,” and she noted, “We were all under the impression Brandon could control this.”
Despite his talent as a wide receiver – while playing for the Broncos, Marshall caught more than 100 passes in each of three consecutive seasons – the Broncos traded him to the Miami Dolphins. His career with the Broncos had been marked by a brief suspension for charges of drunk driving and domestic violence, and Marshall had had numerous arrests over the years. He finally was required to have a psychiatric assessment, and Marshall flew to Massachusetts for a day-long evaluation with Dr. Gunderson. Dr. Gunderson described Marshall at that meeting as “hostile and nondisclosing.”
In Miami, Marshall’s behavior continued to be a source of contention. His girlfriend, Michi, described him as remote and withdrawn. After a domestic dispute in which she was charged with stabbing him – charges that both denied and were later dropped – Marshall returned to see Dr. Gunderson and dedicated 3 months of his off-season to getting treatment.
Dr. Gunderson noted that on his return visit, “He was troubled enough by his behaviors and the difficulties they were causing for him.”
With a diagnosis of borderline personality disorder, Marshall became invested in learning about the disorder and devoted his days to intensive treatment, which included group therapy. He discussed the difficulties he has regulating his emotions and noted that he now had strategies to help him maintain control. Cutler noted that Marshall still loses his cool, but he quickly regains his composure, while in the past he could stay angry for days.
The rest of the show went on to document Marshall’s successes. He gained better control of his temper and became less difficult to work with. Coach Tony Sparano was interviewed, and both he and Marshall talked of Sparano’s role in providing emotional support to the football player. He was offered a $30 million contract extension with the Bears. He and Michi married, started the Brandon Marshall Foundation to support mental health education and treatment, and the couple announced in September that they are expecting twins.
Dr. Gunderson noted that Brandon Marshall’s openness about his disorder does a great deal to alleviate the stigma associated with borderline personality disorder.
“He’s an articulate and charismatic male football player,” he said. “This takes it out of the realm of something that’s about weak people.”
The special did not talk about whether Marshall was taking medications – it was implied that he wasn’t – or if he has continued in treatment. We think of borderline personality disorder as being resistant to treatments, and certainly not as a disorder that can be fixed with 3 months of treatment. It was noted that Marshall has some unusual assets in addition to his charismatic personality: He has a vocation he loves and is good at, and he has supportive relationships. A clip was shown of an appearance he and Michi had made on “The View,” where he credited her support as being key to his success.
As psychiatrists, there is a delicate balance when treating patients with personality disorders. On the one hand, we want them to take ownership for their behaviors in the hopes that they will be able to gain some control over them. To balance this, however, personality disorders can be as crippling as any illness we treat in psychiatry, and the prognosis for some people is dismal. While it may be helpful to have a diagnosis and an explanation, it’s not beneficial if the patient sees himself as the victim of an untreatable condition. The television special on Brandon Marshall did a wonderful job of presenting this disorder with a balance – as a problem that happens to people, perhaps because of their difficult childhoods – but one that the individual can learn to take control of in an empowering way.
We might imagine this remains an ongoing struggle for Marshall, not one that was treated and fixed. I, however, enjoyed watching an NFL production with a positive spin on what we think of as being such a devastating psychiatric disorder.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
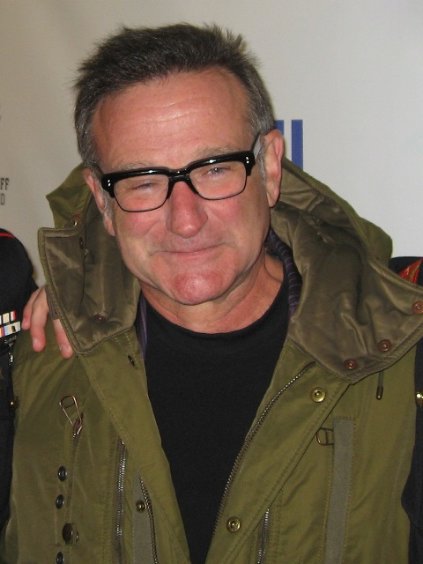
Shrink Rap News: Suicide hotline calls increase after Robin Williams’ death
National Suicide Prevention Day fell on Sept. 10 this year, surrounded by National Suicide Prevention Week Sept. 8-14. The conversation, as I’m sure everyone noticed, was focused on the suicide of actor Robin Williams. As we move out a few weeks, my patients – especially those who have contemplated ending their own lives – continue to talk about this tragic loss.
The fear is that the suicide of a celebrity will lead to an increase in the suicide rate in the general public – copycat suicides, if you will. In the month after Marilyn Monroe died of an overdose in 1962, the suicide rate rose by more than 10%. On the other hand, the death of a celebrity may lead to a decrease in the suicide rate, as happened after Kurt Cobain’s death from a self-inflicted gunshot wound in 1994. In the period after Cobain’s death, an effort was made to publicize resources for those who need help. The suicide rate dropped, while calls to hotlines rose.
After Robin Williams’ death, my own social media feeds were full of ads for the National Suicide Prevention Lifeline (NSPL), a hotline with the number 1-800-273-TALK. There are other hotlines, but this was the one I saw most. I wanted to learn about suicide hotlines, so I did a few things: I asked readers of our Shrink Rap blog to tell me about their experiences, and I called the hotline myself to see if I could learn about the structure of the organization, what resources they had to offer a distraught caller, and whether there had been a change in the number of calls they’d received in the time following Mr. Williams’ death.
I called from my cell phone, which is registered in Maryland, while sitting in my home in Baltimore City. The call was routed to Grassroots Crisis Intervention Center in Columbia, Md. Google Maps tells me the center is 25 miles from my house, and it would take me 32 minutes to drive there. In addition to being part of a network of 160 hotline centers across the country, Grassroots has a walk-in crisis center and a mobile treatment center, and is adjacent to a homeless shelter.
“Most of the people who call the National Suicide Prevention Lifeline are suicidal,” said Nicole DeChirico, director of crisis intervention services for Grassroots. “There is a gradation in suicidal thinking, but about 90% of our callers are considering it.”
“We first form rapport, and then we try to quickly assess if an attempt has already been made, and if they are in any danger. We use the assessment of suicidality that is put out by the NSPL. It’s a structured template that is used as a guideline.”
Ms. DeChirico noted that the people who man the hotlines have bachelor’s or master’s degrees – often in psychology, social work, counseling, or education. If feasible, a Safety Planning Intervention is implemented, based on the work of Barbara Stanley, Ph.D., at Columbia University in New York.
“We talk to people about what they need to do to feel safe. If they allow it, we set up a follow-up call. Of the total number of people who have attempted suicide once in the past and lived, 90%-96% never go on to attempt suicide again,” Ms. DeChirico noted. Suicide is a time-limited acute crisis.”
The Grassroots team can see patients on site while they wait for appointments with an outpatient clinician, and can send a mobile crisis team to those who need it if they are in the county served by the organization. I wondered if all 160 agencies that received calls from the NSPL could also provide crisis services.
Marcia Epstein, LMSW, was director of the Headquarters Counseling Center in Lawrence, Kan., from 1979 to 2013. The center became part of the first national suicide prevention hotline network, the National Hopeline Network, 1-800-SUICIDE, in 2001, and then became part of the National Suicide Prevention Lifeline, 1-800-274-TALK (8255), when that network began in January 2005.
“The types of programs and agencies which are part of NSPL vary greatly. The accreditation that allows them to be part of the NSPL network also varies. Some centers are staffed totally by licensed mental health therapists, while others might include trained volunteers and paid counselors who have no professional degree or licensure. Service may be delivered by phone, as well as in person, by text, and by live chat. In person might be on site or through mobile crisis outreach. Some centers are part of other organizations, while others are free-standing, and some serve entire states, while others serve geographically smaller regions,” Ms. Epstein explained in a series of e-mails. She noted that some centers assess and refer, while others, like Grassroots, are able to provide more counseling.
“So if it sounds like I’m saying there is little consistency between centers, yes, that is my experience. But the centers all bring strong commitment to preventing suicide.”
Ms. Epstein continued to discuss the power of the work done with hotline callers.
“The really helpful counseling comes from the heart, from connecting to people with caring and respect and patience, and using our skills in helping them stay safer through the crisis and then, when needed, to stay safer in the long run. It takes a lot of bravery from the people letting us help. And it takes a lot of creativity and flexibility in coming up together with realistic plans to support safety.”
I was curious about the patient response, and I found that was mixed. It was also notable that different patients found different forms of communication to be helpful.
A woman who identified herself only as “Virginia Woolf” wrote, “I have contacted the Samaritans on the jo@samaritans.org line because I could write to them via e-mail. I don’t like phones and I also know too many of the counselors on the local crisis line. Each time I was definitely close to suicide. I was in despair and I had the means at hand. I think what stopped me was knowing they would reply. They always did, within a few hours, but waiting for their reply kept me safe.”
Not every response was as positive.
One writer noted, “It was not a productive, supportive, or empathetic person. I felt like she was arrogant, judgmental, and didn’t really care about why I was calling.” The same writer, however, was able to find solace elsewhere. “I have texted CrisisChat and it was an excellent chat and I did feel better.”
Finally, Ms. DeChirico sent me information about the call volume from our local NPSL center in Columbia. From July 1, 2013, to July 31, 2014, the Lifeline received an average of 134 calls per month. December had the highest number of calls, with 163, while August had the lowest with 118. September, February, and April all had 120 calls or fewer.
Robin Williams died on Aug. 11, 2014, and the center received 200 calls in August – a 49% increase over the average volume. Hopefully, we’ll end up seeing a decline in suicide in the months following Mr. Williams’ tragic death.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
National Suicide Prevention Day fell on Sept. 10 this year, surrounded by National Suicide Prevention Week Sept. 8-14. The conversation, as I’m sure everyone noticed, was focused on the suicide of actor Robin Williams. As we move out a few weeks, my patients – especially those who have contemplated ending their own lives – continue to talk about this tragic loss.
The fear is that the suicide of a celebrity will lead to an increase in the suicide rate in the general public – copycat suicides, if you will. In the month after Marilyn Monroe died of an overdose in 1962, the suicide rate rose by more than 10%. On the other hand, the death of a celebrity may lead to a decrease in the suicide rate, as happened after Kurt Cobain’s death from a self-inflicted gunshot wound in 1994. In the period after Cobain’s death, an effort was made to publicize resources for those who need help. The suicide rate dropped, while calls to hotlines rose.
After Robin Williams’ death, my own social media feeds were full of ads for the National Suicide Prevention Lifeline (NSPL), a hotline with the number 1-800-273-TALK. There are other hotlines, but this was the one I saw most. I wanted to learn about suicide hotlines, so I did a few things: I asked readers of our Shrink Rap blog to tell me about their experiences, and I called the hotline myself to see if I could learn about the structure of the organization, what resources they had to offer a distraught caller, and whether there had been a change in the number of calls they’d received in the time following Mr. Williams’ death.
I called from my cell phone, which is registered in Maryland, while sitting in my home in Baltimore City. The call was routed to Grassroots Crisis Intervention Center in Columbia, Md. Google Maps tells me the center is 25 miles from my house, and it would take me 32 minutes to drive there. In addition to being part of a network of 160 hotline centers across the country, Grassroots has a walk-in crisis center and a mobile treatment center, and is adjacent to a homeless shelter.
“Most of the people who call the National Suicide Prevention Lifeline are suicidal,” said Nicole DeChirico, director of crisis intervention services for Grassroots. “There is a gradation in suicidal thinking, but about 90% of our callers are considering it.”
“We first form rapport, and then we try to quickly assess if an attempt has already been made, and if they are in any danger. We use the assessment of suicidality that is put out by the NSPL. It’s a structured template that is used as a guideline.”
Ms. DeChirico noted that the people who man the hotlines have bachelor’s or master’s degrees – often in psychology, social work, counseling, or education. If feasible, a Safety Planning Intervention is implemented, based on the work of Barbara Stanley, Ph.D., at Columbia University in New York.
“We talk to people about what they need to do to feel safe. If they allow it, we set up a follow-up call. Of the total number of people who have attempted suicide once in the past and lived, 90%-96% never go on to attempt suicide again,” Ms. DeChirico noted. Suicide is a time-limited acute crisis.”
The Grassroots team can see patients on site while they wait for appointments with an outpatient clinician, and can send a mobile crisis team to those who need it if they are in the county served by the organization. I wondered if all 160 agencies that received calls from the NSPL could also provide crisis services.
Marcia Epstein, LMSW, was director of the Headquarters Counseling Center in Lawrence, Kan., from 1979 to 2013. The center became part of the first national suicide prevention hotline network, the National Hopeline Network, 1-800-SUICIDE, in 2001, and then became part of the National Suicide Prevention Lifeline, 1-800-274-TALK (8255), when that network began in January 2005.
“The types of programs and agencies which are part of NSPL vary greatly. The accreditation that allows them to be part of the NSPL network also varies. Some centers are staffed totally by licensed mental health therapists, while others might include trained volunteers and paid counselors who have no professional degree or licensure. Service may be delivered by phone, as well as in person, by text, and by live chat. In person might be on site or through mobile crisis outreach. Some centers are part of other organizations, while others are free-standing, and some serve entire states, while others serve geographically smaller regions,” Ms. Epstein explained in a series of e-mails. She noted that some centers assess and refer, while others, like Grassroots, are able to provide more counseling.
“So if it sounds like I’m saying there is little consistency between centers, yes, that is my experience. But the centers all bring strong commitment to preventing suicide.”
Ms. Epstein continued to discuss the power of the work done with hotline callers.
“The really helpful counseling comes from the heart, from connecting to people with caring and respect and patience, and using our skills in helping them stay safer through the crisis and then, when needed, to stay safer in the long run. It takes a lot of bravery from the people letting us help. And it takes a lot of creativity and flexibility in coming up together with realistic plans to support safety.”
I was curious about the patient response, and I found that was mixed. It was also notable that different patients found different forms of communication to be helpful.
A woman who identified herself only as “Virginia Woolf” wrote, “I have contacted the Samaritans on the jo@samaritans.org line because I could write to them via e-mail. I don’t like phones and I also know too many of the counselors on the local crisis line. Each time I was definitely close to suicide. I was in despair and I had the means at hand. I think what stopped me was knowing they would reply. They always did, within a few hours, but waiting for their reply kept me safe.”
Not every response was as positive.
One writer noted, “It was not a productive, supportive, or empathetic person. I felt like she was arrogant, judgmental, and didn’t really care about why I was calling.” The same writer, however, was able to find solace elsewhere. “I have texted CrisisChat and it was an excellent chat and I did feel better.”
Finally, Ms. DeChirico sent me information about the call volume from our local NPSL center in Columbia. From July 1, 2013, to July 31, 2014, the Lifeline received an average of 134 calls per month. December had the highest number of calls, with 163, while August had the lowest with 118. September, February, and April all had 120 calls or fewer.
Robin Williams died on Aug. 11, 2014, and the center received 200 calls in August – a 49% increase over the average volume. Hopefully, we’ll end up seeing a decline in suicide in the months following Mr. Williams’ tragic death.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
National Suicide Prevention Day fell on Sept. 10 this year, surrounded by National Suicide Prevention Week Sept. 8-14. The conversation, as I’m sure everyone noticed, was focused on the suicide of actor Robin Williams. As we move out a few weeks, my patients – especially those who have contemplated ending their own lives – continue to talk about this tragic loss.
The fear is that the suicide of a celebrity will lead to an increase in the suicide rate in the general public – copycat suicides, if you will. In the month after Marilyn Monroe died of an overdose in 1962, the suicide rate rose by more than 10%. On the other hand, the death of a celebrity may lead to a decrease in the suicide rate, as happened after Kurt Cobain’s death from a self-inflicted gunshot wound in 1994. In the period after Cobain’s death, an effort was made to publicize resources for those who need help. The suicide rate dropped, while calls to hotlines rose.
After Robin Williams’ death, my own social media feeds were full of ads for the National Suicide Prevention Lifeline (NSPL), a hotline with the number 1-800-273-TALK. There are other hotlines, but this was the one I saw most. I wanted to learn about suicide hotlines, so I did a few things: I asked readers of our Shrink Rap blog to tell me about their experiences, and I called the hotline myself to see if I could learn about the structure of the organization, what resources they had to offer a distraught caller, and whether there had been a change in the number of calls they’d received in the time following Mr. Williams’ death.
I called from my cell phone, which is registered in Maryland, while sitting in my home in Baltimore City. The call was routed to Grassroots Crisis Intervention Center in Columbia, Md. Google Maps tells me the center is 25 miles from my house, and it would take me 32 minutes to drive there. In addition to being part of a network of 160 hotline centers across the country, Grassroots has a walk-in crisis center and a mobile treatment center, and is adjacent to a homeless shelter.
“Most of the people who call the National Suicide Prevention Lifeline are suicidal,” said Nicole DeChirico, director of crisis intervention services for Grassroots. “There is a gradation in suicidal thinking, but about 90% of our callers are considering it.”
“We first form rapport, and then we try to quickly assess if an attempt has already been made, and if they are in any danger. We use the assessment of suicidality that is put out by the NSPL. It’s a structured template that is used as a guideline.”
Ms. DeChirico noted that the people who man the hotlines have bachelor’s or master’s degrees – often in psychology, social work, counseling, or education. If feasible, a Safety Planning Intervention is implemented, based on the work of Barbara Stanley, Ph.D., at Columbia University in New York.
“We talk to people about what they need to do to feel safe. If they allow it, we set up a follow-up call. Of the total number of people who have attempted suicide once in the past and lived, 90%-96% never go on to attempt suicide again,” Ms. DeChirico noted. Suicide is a time-limited acute crisis.”
The Grassroots team can see patients on site while they wait for appointments with an outpatient clinician, and can send a mobile crisis team to those who need it if they are in the county served by the organization. I wondered if all 160 agencies that received calls from the NSPL could also provide crisis services.
Marcia Epstein, LMSW, was director of the Headquarters Counseling Center in Lawrence, Kan., from 1979 to 2013. The center became part of the first national suicide prevention hotline network, the National Hopeline Network, 1-800-SUICIDE, in 2001, and then became part of the National Suicide Prevention Lifeline, 1-800-274-TALK (8255), when that network began in January 2005.
“The types of programs and agencies which are part of NSPL vary greatly. The accreditation that allows them to be part of the NSPL network also varies. Some centers are staffed totally by licensed mental health therapists, while others might include trained volunteers and paid counselors who have no professional degree or licensure. Service may be delivered by phone, as well as in person, by text, and by live chat. In person might be on site or through mobile crisis outreach. Some centers are part of other organizations, while others are free-standing, and some serve entire states, while others serve geographically smaller regions,” Ms. Epstein explained in a series of e-mails. She noted that some centers assess and refer, while others, like Grassroots, are able to provide more counseling.
“So if it sounds like I’m saying there is little consistency between centers, yes, that is my experience. But the centers all bring strong commitment to preventing suicide.”
Ms. Epstein continued to discuss the power of the work done with hotline callers.
“The really helpful counseling comes from the heart, from connecting to people with caring and respect and patience, and using our skills in helping them stay safer through the crisis and then, when needed, to stay safer in the long run. It takes a lot of bravery from the people letting us help. And it takes a lot of creativity and flexibility in coming up together with realistic plans to support safety.”
I was curious about the patient response, and I found that was mixed. It was also notable that different patients found different forms of communication to be helpful.
A woman who identified herself only as “Virginia Woolf” wrote, “I have contacted the Samaritans on the jo@samaritans.org line because I could write to them via e-mail. I don’t like phones and I also know too many of the counselors on the local crisis line. Each time I was definitely close to suicide. I was in despair and I had the means at hand. I think what stopped me was knowing they would reply. They always did, within a few hours, but waiting for their reply kept me safe.”
Not every response was as positive.
One writer noted, “It was not a productive, supportive, or empathetic person. I felt like she was arrogant, judgmental, and didn’t really care about why I was calling.” The same writer, however, was able to find solace elsewhere. “I have texted CrisisChat and it was an excellent chat and I did feel better.”
Finally, Ms. DeChirico sent me information about the call volume from our local NPSL center in Columbia. From July 1, 2013, to July 31, 2014, the Lifeline received an average of 134 calls per month. December had the highest number of calls, with 163, while August had the lowest with 118. September, February, and April all had 120 calls or fewer.
Robin Williams died on Aug. 11, 2014, and the center received 200 calls in August – a 49% increase over the average volume. Hopefully, we’ll end up seeing a decline in suicide in the months following Mr. Williams’ tragic death.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Psychiatry, free speech, school safety, and cannibalism
Over the past few days, an article has circulated about a 23-year-old middle school teacher in Cambridge, Md., who was suspended from his job because of two futuristic novels he wrote, including one about a school massacre 900 years in the future. The story was reported in The Atlantic under the headline, "In Maryland, a Soviet-Style Punishment for a Novelist."
The article, by Jeffrey Goldberg, said the young teacher had self-published his novels some time ago under a pseudonym. In addition to his being suspended, an "emergency medical evaluation" was ordered, his house was searched, and the school was swept for bombs by K-9 dogs. No charges have been filed as of this writing.
This response was deemed an "overreaction," and certainly has been good for book sales but probably not so much for the young man’s teaching career. The idea that artistic expression must conform to a specific standard or jeopardize one’s job leaves those with creative pursuits to worry and civil rights advocates to protest.
Soon after, the Los Angeles Times published an article stating that the issue was not the novels – the school knew about those in 2012 – but rather the content of a four-page letter the teacher had written to the school board suggesting that the teacher was suffering from some type of psychiatric condition and might have included indications that he was suicidal or dangerous. With this information, it was not as clear if the police response was an overreaction, and such determinations are generally made in hindsight: If a bomb is found, the decision was heroic, if not, it was an overreaction and a civil rights violation.
The case reminded me of the story about a New York City police officer who had Internet discussions about his desire to cook and eat women, including his ex-wife. While the officer never ate anyone, he was part of an online community called the Dark Fetish Network, which has of tens of thousands of registered users who discuss violent sexual fantasies. The officer, known in the media frenzy as Cannibal Cop, lost his job and was convicted of plotting to kidnap, a crime that could carry a life sentence. He reportedly had graphic discussions of plans to kill, roast, and eat specified victims, and he claimed that he had the means to do so. An investigation revealed that he did not own the implements that would enable him to carry out such a plan. His lawyer insisted that he was engaged in a role-playing fantasy, but he was convicted by a jury in 2012. In July, his conviction was overturned and he was released on bond. By that time, Cannibal Cop had served a year and a half in prison, with several months of it in solitary confinement.
Situations in which a person has done nothing illegal but has spoken or written words that indicate he or she might be a threat to public safety are fraught with concerns. While violent fantasies might be seen as "creepy" at a minimum, the criminal justice system is left to decide where the line is between fantasy and plan, and when a real threat exists. A person has the right to his dark fantasies, and the First Amendment right to free speech allows for discussion of those fantasies, while artistic endeavors allow for their expression. At the same time, if there are named or presumed victims, those individuals should not have to live with the terror of wondering if the fantasizer is going to act on the fantasies.
Invariably, psychiatrists end up being involved, even if the individual in question has no psychiatric history or obvious diagnosis. In a New York magazine article about the police officer titled, "A Dangerous Mind," Robert Kolker noted: "Pre-crime and psychiatry often go hand in hand. Legal instruments like institutionalization and sex-offender registration all share the goal of preventing crime from taking place, and for better or worse, they’re based on a psychiatric rationale."
As we all know, it can be difficult – if not impossible – to distinguish those who are having fantasies from those who are planning to commit a dangerous act. As psychiatrists, we deal with this uncertainty for patients who have suicidal thoughts on a regular basis. Often, even the patients don’t know for sure if they will act on their impulses. Fantasies that involve harming others are more unusual in clinical practice, and our risk assessment often begins with the stated intent of the individual. Our strongest predictor of future behavior continues to be past behavior, and neither the teacher nor the police officer in the stories above had criminal records.
To make it even more confusing, the Internet has added to the uncertainty; people have always had dangerous and fetishistic fantasies, but now there are ways others can learn the content of what was once very private. The risk, of course, is that fantasies and artistic endeavors become subject to both psychiatric scrutiny and criminal prosecution in a way that threatens civil rights and squelches creativity.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore:The Johns Hopkins University Press, 2011).
Over the past few days, an article has circulated about a 23-year-old middle school teacher in Cambridge, Md., who was suspended from his job because of two futuristic novels he wrote, including one about a school massacre 900 years in the future. The story was reported in The Atlantic under the headline, "In Maryland, a Soviet-Style Punishment for a Novelist."
The article, by Jeffrey Goldberg, said the young teacher had self-published his novels some time ago under a pseudonym. In addition to his being suspended, an "emergency medical evaluation" was ordered, his house was searched, and the school was swept for bombs by K-9 dogs. No charges have been filed as of this writing.
This response was deemed an "overreaction," and certainly has been good for book sales but probably not so much for the young man’s teaching career. The idea that artistic expression must conform to a specific standard or jeopardize one’s job leaves those with creative pursuits to worry and civil rights advocates to protest.
Soon after, the Los Angeles Times published an article stating that the issue was not the novels – the school knew about those in 2012 – but rather the content of a four-page letter the teacher had written to the school board suggesting that the teacher was suffering from some type of psychiatric condition and might have included indications that he was suicidal or dangerous. With this information, it was not as clear if the police response was an overreaction, and such determinations are generally made in hindsight: If a bomb is found, the decision was heroic, if not, it was an overreaction and a civil rights violation.
The case reminded me of the story about a New York City police officer who had Internet discussions about his desire to cook and eat women, including his ex-wife. While the officer never ate anyone, he was part of an online community called the Dark Fetish Network, which has of tens of thousands of registered users who discuss violent sexual fantasies. The officer, known in the media frenzy as Cannibal Cop, lost his job and was convicted of plotting to kidnap, a crime that could carry a life sentence. He reportedly had graphic discussions of plans to kill, roast, and eat specified victims, and he claimed that he had the means to do so. An investigation revealed that he did not own the implements that would enable him to carry out such a plan. His lawyer insisted that he was engaged in a role-playing fantasy, but he was convicted by a jury in 2012. In July, his conviction was overturned and he was released on bond. By that time, Cannibal Cop had served a year and a half in prison, with several months of it in solitary confinement.
Situations in which a person has done nothing illegal but has spoken or written words that indicate he or she might be a threat to public safety are fraught with concerns. While violent fantasies might be seen as "creepy" at a minimum, the criminal justice system is left to decide where the line is between fantasy and plan, and when a real threat exists. A person has the right to his dark fantasies, and the First Amendment right to free speech allows for discussion of those fantasies, while artistic endeavors allow for their expression. At the same time, if there are named or presumed victims, those individuals should not have to live with the terror of wondering if the fantasizer is going to act on the fantasies.
Invariably, psychiatrists end up being involved, even if the individual in question has no psychiatric history or obvious diagnosis. In a New York magazine article about the police officer titled, "A Dangerous Mind," Robert Kolker noted: "Pre-crime and psychiatry often go hand in hand. Legal instruments like institutionalization and sex-offender registration all share the goal of preventing crime from taking place, and for better or worse, they’re based on a psychiatric rationale."
As we all know, it can be difficult – if not impossible – to distinguish those who are having fantasies from those who are planning to commit a dangerous act. As psychiatrists, we deal with this uncertainty for patients who have suicidal thoughts on a regular basis. Often, even the patients don’t know for sure if they will act on their impulses. Fantasies that involve harming others are more unusual in clinical practice, and our risk assessment often begins with the stated intent of the individual. Our strongest predictor of future behavior continues to be past behavior, and neither the teacher nor the police officer in the stories above had criminal records.
To make it even more confusing, the Internet has added to the uncertainty; people have always had dangerous and fetishistic fantasies, but now there are ways others can learn the content of what was once very private. The risk, of course, is that fantasies and artistic endeavors become subject to both psychiatric scrutiny and criminal prosecution in a way that threatens civil rights and squelches creativity.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore:The Johns Hopkins University Press, 2011).
Over the past few days, an article has circulated about a 23-year-old middle school teacher in Cambridge, Md., who was suspended from his job because of two futuristic novels he wrote, including one about a school massacre 900 years in the future. The story was reported in The Atlantic under the headline, "In Maryland, a Soviet-Style Punishment for a Novelist."
The article, by Jeffrey Goldberg, said the young teacher had self-published his novels some time ago under a pseudonym. In addition to his being suspended, an "emergency medical evaluation" was ordered, his house was searched, and the school was swept for bombs by K-9 dogs. No charges have been filed as of this writing.
This response was deemed an "overreaction," and certainly has been good for book sales but probably not so much for the young man’s teaching career. The idea that artistic expression must conform to a specific standard or jeopardize one’s job leaves those with creative pursuits to worry and civil rights advocates to protest.
Soon after, the Los Angeles Times published an article stating that the issue was not the novels – the school knew about those in 2012 – but rather the content of a four-page letter the teacher had written to the school board suggesting that the teacher was suffering from some type of psychiatric condition and might have included indications that he was suicidal or dangerous. With this information, it was not as clear if the police response was an overreaction, and such determinations are generally made in hindsight: If a bomb is found, the decision was heroic, if not, it was an overreaction and a civil rights violation.
The case reminded me of the story about a New York City police officer who had Internet discussions about his desire to cook and eat women, including his ex-wife. While the officer never ate anyone, he was part of an online community called the Dark Fetish Network, which has of tens of thousands of registered users who discuss violent sexual fantasies. The officer, known in the media frenzy as Cannibal Cop, lost his job and was convicted of plotting to kidnap, a crime that could carry a life sentence. He reportedly had graphic discussions of plans to kill, roast, and eat specified victims, and he claimed that he had the means to do so. An investigation revealed that he did not own the implements that would enable him to carry out such a plan. His lawyer insisted that he was engaged in a role-playing fantasy, but he was convicted by a jury in 2012. In July, his conviction was overturned and he was released on bond. By that time, Cannibal Cop had served a year and a half in prison, with several months of it in solitary confinement.
Situations in which a person has done nothing illegal but has spoken or written words that indicate he or she might be a threat to public safety are fraught with concerns. While violent fantasies might be seen as "creepy" at a minimum, the criminal justice system is left to decide where the line is between fantasy and plan, and when a real threat exists. A person has the right to his dark fantasies, and the First Amendment right to free speech allows for discussion of those fantasies, while artistic endeavors allow for their expression. At the same time, if there are named or presumed victims, those individuals should not have to live with the terror of wondering if the fantasizer is going to act on the fantasies.
Invariably, psychiatrists end up being involved, even if the individual in question has no psychiatric history or obvious diagnosis. In a New York magazine article about the police officer titled, "A Dangerous Mind," Robert Kolker noted: "Pre-crime and psychiatry often go hand in hand. Legal instruments like institutionalization and sex-offender registration all share the goal of preventing crime from taking place, and for better or worse, they’re based on a psychiatric rationale."
As we all know, it can be difficult – if not impossible – to distinguish those who are having fantasies from those who are planning to commit a dangerous act. As psychiatrists, we deal with this uncertainty for patients who have suicidal thoughts on a regular basis. Often, even the patients don’t know for sure if they will act on their impulses. Fantasies that involve harming others are more unusual in clinical practice, and our risk assessment often begins with the stated intent of the individual. Our strongest predictor of future behavior continues to be past behavior, and neither the teacher nor the police officer in the stories above had criminal records.
To make it even more confusing, the Internet has added to the uncertainty; people have always had dangerous and fetishistic fantasies, but now there are ways others can learn the content of what was once very private. The risk, of course, is that fantasies and artistic endeavors become subject to both psychiatric scrutiny and criminal prosecution in a way that threatens civil rights and squelches creativity.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore:The Johns Hopkins University Press, 2011).
Robin Williams’s suspected suicide could encourage others to get help
The news last night was tragic: Robin Williams has died of an apparent suicide at the early age of 63. I saw the news and felt overwhelmingly sad. Really? He was a tremendous actor, a creative genius by any account, a man who I imagined had everything – talent, wealth, fame, the wonderful ability to make people laugh and to brighten lives. Such people also get draped with love and admiration, though certainly at a price. For what it’s worth, Robin Williams has been open about the fact that he’s struggled with both depression and addiction, but the complete story is never the one that gets told by the media.
Twitter started with 140-character links to suicide hotlines and suicide awareness, to statements about how depression is a treatable illness – Is it always? – and I hit retweet on a comment stating:" We’re never going to get anywhere till we take seriously that depression is an illness, not a weakness" and several people retweeted my retweet. I’m not sure why I did this; I don’t think that most people still think of mood disorders as a "weakness," or that those who do might change their minds because of a tweet. And I don’t think that suicide does anything to reduce stigma.
One psychiatrist friend tweeted a comment about how one should never ask someone why they are depressed, I guess because the "why?" implies something other than because biology dictated it, but if you’ve ever spoken to a person suffering from depression, you know that it comes in all shades of severity and that people often write a story to explain it. Sometimes that story is right: I’m depressed because of a breakup, or because I don’t have a job now, or because of ongoing work stress – and indeed, the person suffering often feels better after talking about the situation, after getting a new boyfriend or a new job, or after their boss moves to Zimbabwe.
I’m convinced that treatment works best when psychotherapy is combined with medication (if indicated), and while medicines are a miracle for some, they aren’t for others. As psychiatrists, we certainly see a good deal of treatment-resistant depression. And yes, the antipsychiatry faction may postulate that it is the treatment – the medications, specifically – that cause people to kill themselves and others, but I will leave you with the idea that the science just doesn’t support that. Certainly, they aren’t for everyone, but clinically, I have seen medications do more good than harm in clinical practice overall.
I know nothing about Robin Williams beyond what I’ve read in the media, and I know that the media reports are often incomplete and distorted. I do imagine that Mr. Williams had the resources to get good care and that he may well have had treatment for depression since he was open about his struggle. His story will be used to say: "Get help," and if you’re feeling suicidal and aren’t getting help, please do so. If you’re feeling suicidal and "help" isn’t making you feel better, please consider getting a second opinion or a different kind of help.
The tragic thing about suicide is that it’s a permanent answer to what is often a temporary problem.
Sometimes, I imagine that there are people who have tried and tried to get help and that their pain remains so unbearable for so long that suicide offers them the only possible relief – if such a thing is even to be had given that we don’t what comes next and some religions will say that suicide leads to nowhere good. Even if it provides relief to the person involved, it comes with the cost of leaving those who remain in horrible pain. Sadly, depressed people sometimes imagine that the world will be better off without them, and often that idea is just not true.
I hope that Robin Williams is in a better place, for his sake. I hope that before he ended his life, he tried every possible treatment option, and that this wasn’t an impulsive decision, or one based on an episodic relapse of either depression or substance abuse – a relapse that may have resolved and let him live for decades more. I hope his wife and children and all the people who knew and loved him will eventually find some peace. His death, however, is not simply a personal one because he touched us all with his talent and his charisma. What a tragic loss.
Dr. Miller also posted a version http://bit.ly/1kyO1a7 of this piece on the Shrink Rap News website. She is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
The news last night was tragic: Robin Williams has died of an apparent suicide at the early age of 63. I saw the news and felt overwhelmingly sad. Really? He was a tremendous actor, a creative genius by any account, a man who I imagined had everything – talent, wealth, fame, the wonderful ability to make people laugh and to brighten lives. Such people also get draped with love and admiration, though certainly at a price. For what it’s worth, Robin Williams has been open about the fact that he’s struggled with both depression and addiction, but the complete story is never the one that gets told by the media.
Twitter started with 140-character links to suicide hotlines and suicide awareness, to statements about how depression is a treatable illness – Is it always? – and I hit retweet on a comment stating:" We’re never going to get anywhere till we take seriously that depression is an illness, not a weakness" and several people retweeted my retweet. I’m not sure why I did this; I don’t think that most people still think of mood disorders as a "weakness," or that those who do might change their minds because of a tweet. And I don’t think that suicide does anything to reduce stigma.
One psychiatrist friend tweeted a comment about how one should never ask someone why they are depressed, I guess because the "why?" implies something other than because biology dictated it, but if you’ve ever spoken to a person suffering from depression, you know that it comes in all shades of severity and that people often write a story to explain it. Sometimes that story is right: I’m depressed because of a breakup, or because I don’t have a job now, or because of ongoing work stress – and indeed, the person suffering often feels better after talking about the situation, after getting a new boyfriend or a new job, or after their boss moves to Zimbabwe.
I’m convinced that treatment works best when psychotherapy is combined with medication (if indicated), and while medicines are a miracle for some, they aren’t for others. As psychiatrists, we certainly see a good deal of treatment-resistant depression. And yes, the antipsychiatry faction may postulate that it is the treatment – the medications, specifically – that cause people to kill themselves and others, but I will leave you with the idea that the science just doesn’t support that. Certainly, they aren’t for everyone, but clinically, I have seen medications do more good than harm in clinical practice overall.
I know nothing about Robin Williams beyond what I’ve read in the media, and I know that the media reports are often incomplete and distorted. I do imagine that Mr. Williams had the resources to get good care and that he may well have had treatment for depression since he was open about his struggle. His story will be used to say: "Get help," and if you’re feeling suicidal and aren’t getting help, please do so. If you’re feeling suicidal and "help" isn’t making you feel better, please consider getting a second opinion or a different kind of help.
The tragic thing about suicide is that it’s a permanent answer to what is often a temporary problem.
Sometimes, I imagine that there are people who have tried and tried to get help and that their pain remains so unbearable for so long that suicide offers them the only possible relief – if such a thing is even to be had given that we don’t what comes next and some religions will say that suicide leads to nowhere good. Even if it provides relief to the person involved, it comes with the cost of leaving those who remain in horrible pain. Sadly, depressed people sometimes imagine that the world will be better off without them, and often that idea is just not true.
I hope that Robin Williams is in a better place, for his sake. I hope that before he ended his life, he tried every possible treatment option, and that this wasn’t an impulsive decision, or one based on an episodic relapse of either depression or substance abuse – a relapse that may have resolved and let him live for decades more. I hope his wife and children and all the people who knew and loved him will eventually find some peace. His death, however, is not simply a personal one because he touched us all with his talent and his charisma. What a tragic loss.
Dr. Miller also posted a version http://bit.ly/1kyO1a7 of this piece on the Shrink Rap News website. She is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
The news last night was tragic: Robin Williams has died of an apparent suicide at the early age of 63. I saw the news and felt overwhelmingly sad. Really? He was a tremendous actor, a creative genius by any account, a man who I imagined had everything – talent, wealth, fame, the wonderful ability to make people laugh and to brighten lives. Such people also get draped with love and admiration, though certainly at a price. For what it’s worth, Robin Williams has been open about the fact that he’s struggled with both depression and addiction, but the complete story is never the one that gets told by the media.
Twitter started with 140-character links to suicide hotlines and suicide awareness, to statements about how depression is a treatable illness – Is it always? – and I hit retweet on a comment stating:" We’re never going to get anywhere till we take seriously that depression is an illness, not a weakness" and several people retweeted my retweet. I’m not sure why I did this; I don’t think that most people still think of mood disorders as a "weakness," or that those who do might change their minds because of a tweet. And I don’t think that suicide does anything to reduce stigma.
One psychiatrist friend tweeted a comment about how one should never ask someone why they are depressed, I guess because the "why?" implies something other than because biology dictated it, but if you’ve ever spoken to a person suffering from depression, you know that it comes in all shades of severity and that people often write a story to explain it. Sometimes that story is right: I’m depressed because of a breakup, or because I don’t have a job now, or because of ongoing work stress – and indeed, the person suffering often feels better after talking about the situation, after getting a new boyfriend or a new job, or after their boss moves to Zimbabwe.
I’m convinced that treatment works best when psychotherapy is combined with medication (if indicated), and while medicines are a miracle for some, they aren’t for others. As psychiatrists, we certainly see a good deal of treatment-resistant depression. And yes, the antipsychiatry faction may postulate that it is the treatment – the medications, specifically – that cause people to kill themselves and others, but I will leave you with the idea that the science just doesn’t support that. Certainly, they aren’t for everyone, but clinically, I have seen medications do more good than harm in clinical practice overall.
I know nothing about Robin Williams beyond what I’ve read in the media, and I know that the media reports are often incomplete and distorted. I do imagine that Mr. Williams had the resources to get good care and that he may well have had treatment for depression since he was open about his struggle. His story will be used to say: "Get help," and if you’re feeling suicidal and aren’t getting help, please do so. If you’re feeling suicidal and "help" isn’t making you feel better, please consider getting a second opinion or a different kind of help.
The tragic thing about suicide is that it’s a permanent answer to what is often a temporary problem.
Sometimes, I imagine that there are people who have tried and tried to get help and that their pain remains so unbearable for so long that suicide offers them the only possible relief – if such a thing is even to be had given that we don’t what comes next and some religions will say that suicide leads to nowhere good. Even if it provides relief to the person involved, it comes with the cost of leaving those who remain in horrible pain. Sadly, depressed people sometimes imagine that the world will be better off without them, and often that idea is just not true.
I hope that Robin Williams is in a better place, for his sake. I hope that before he ended his life, he tried every possible treatment option, and that this wasn’t an impulsive decision, or one based on an episodic relapse of either depression or substance abuse – a relapse that may have resolved and let him live for decades more. I hope his wife and children and all the people who knew and loved him will eventually find some peace. His death, however, is not simply a personal one because he touched us all with his talent and his charisma. What a tragic loss.
Dr. Miller also posted a version http://bit.ly/1kyO1a7 of this piece on the Shrink Rap News website. She is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
The stigma of being a shrink
A Clinical Psychiatry News reader wrote in recently to object to the use of the term "shrink" in our column name. The writer noted, "We spend a lot of time trying to destigmatize the field, then use terms like this among ourselves. It’s odd and offensive." The feedback made me pause and wonder to myself if the term "shrink" is, in fact, stigmatizing.
Let me first give a little history of the decision to name our column "Shrink Rap News." In 2006, I was sitting at the kitchen table and decided I wanted a blog. I didn’t know what a blog actually was, but I wanted one. I went to blogger.com to set up a free website and was asked what I’d like to call my blog. On an impulse, I titled it "Shrink Rap." There was no debate or consideration, and no consultation. I liked the play on words with "shrink wrap," which is used for food storage, and I liked the connotation of psychiatrists talking, or "rapping." In a matter of hours, my impulsive thought was turned into the Shrink Rap blog.
Over the next few days, I invited Dr. Steve Daviss and Dr. Annette Hanson to join me in this venture, and Shrink Rap has continued to publish regular blog posts for 8.5 years now. Steve initially balked at the use of "shrink," but when he went to start our podcast, he titled it "My Three Shrinks" and modified the logo from an old television show, "My Three Sons." When we went to title our book, I wanted to call it "Off the Couch," but I was told that there was no room for couches anywhere. After many months of lively debate, we ended up in a restaurant with our editor and a whiteboard, and by the end of the evening we were back at Shrink Rap for a title for the book.
When Clinical Psychiatry News and Psychology Today approached us to write for their sites, we decided to remain with an image that was working for us, and used Shrink Rap News and Shrink Rap Today for column titles. Because the term may imply something less than a serious look at psychiatric issues, the umbrella name for all our endeavors is The Accessible Psychiatry Project.
So, is the term "shrink" actually stigmatizing? When I think of words as being part of stigma, I think of racial and religious slurs, and those induce a visceral response of disgust in me. For whatever reason, I personally don’t have a clear negative association to the term "shrink" or even "headshrinker." To me, it evokes something lighthearted and includes having a sense of humor about the field. I imagine if psychiatrists ever had actually shrunken heads, I might feel differently. Others may well have another response to the term, but the emotional link to something negative is just not there for me.
From a site called World Wide Words – Investigating the English Language Across the Globe, which is devoted to linguistics and run by a British etymologist, I found the following history of the term "headshrinker":
The original meaning of the term head-shrinker was in reference to a member of a group in Amazonia, the Jivaro, who preserved the heads of their enemies by stripping the skin from the skull, which resulted in a shrunken mummified remnant the size of a fist. The term isn’t that old – it’s first recorded from 1926.
All the early evidence suggests that the person who invented the psychiatrist sense worked in the movies (no jokes please). We have to assume that the term came about because people regarded the process of psychiatry as being like head-shrinking because it reduced the size of the swollen egos so common in show business. Or perhaps they were suspicious about what psychiatrists actually did to their heads and how they did it and so made a joke to relieve the tension.
The earliest example we have is from an article in Time in November 1950 to which an editor has helpfully added a footnote to say that head-shrinker was Hollywood jargon for a psychiatrist. The term afterward became moderately popular, in part because it was used in the film Rebel Without a Cause in 1955. Robert Heinlein felt his readers needed it to be explained when he introduced it in "Time for the Stars" in 1956: " ‘Dr. Devereaux is the boss head-shrinker.’ I looked puzzled and Uncle Steve went on, ‘You don’t savvy? Psychiatrist.’ " By the time it turns up in West Side Story on Broadway in 1957, it was becoming established.
Shrink, the abbreviation, became popular in the United States in the 1970s, though it had first appeared in one of Thomas Pynchon’s books, "The Crying of Lot 49," in 1965, and there is anecdotal evidence that it was around earlier, which is only to be expected of a slang term that would have been mainly transmitted through the spoken word in its earliest days.
The issue of stigma in mental health has gotten a lot of attention as being one reason that people who have difficulties may not seek help. Certainly, words can be powerful, but I wonder if the term "shrink" might actually be easier for patients to use? "I’m going to see my shrink," might imply a visit with any number of mental health professionals and might disassociate it from the implication that the patient is going to see a psychiatrist for treatment of a mental illness, a condition that the media is all too happy to tell us causes people to commit mass murders.
"Shrink" may have a disparaging tone to it, or it may have a ring of affection, depending on the context. Certainly, there are many negative associations and jokes related to being an attorney, and one friend told me that his son was "going to the dark side" when the son applied to law school. Still, there is no stigma associated with having an appointment with one’s lawyer, leading me to believe that a profession can be stigmatized without stigmatizing the clientele.
Some words have taken on a pervasively negative meaning; others are harder to capture. After 8 years, Shrink Rap is now a platform for our writing, invested with its own meanings to us and our readers. The psychiatrist who wrote in to say it is offensive, odd, and stigmatizing certainly has a different set of associations to the word then we do, or we would never have let this be a title for our work.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011).
A Clinical Psychiatry News reader wrote in recently to object to the use of the term "shrink" in our column name. The writer noted, "We spend a lot of time trying to destigmatize the field, then use terms like this among ourselves. It’s odd and offensive." The feedback made me pause and wonder to myself if the term "shrink" is, in fact, stigmatizing.
Let me first give a little history of the decision to name our column "Shrink Rap News." In 2006, I was sitting at the kitchen table and decided I wanted a blog. I didn’t know what a blog actually was, but I wanted one. I went to blogger.com to set up a free website and was asked what I’d like to call my blog. On an impulse, I titled it "Shrink Rap." There was no debate or consideration, and no consultation. I liked the play on words with "shrink wrap," which is used for food storage, and I liked the connotation of psychiatrists talking, or "rapping." In a matter of hours, my impulsive thought was turned into the Shrink Rap blog.
Over the next few days, I invited Dr. Steve Daviss and Dr. Annette Hanson to join me in this venture, and Shrink Rap has continued to publish regular blog posts for 8.5 years now. Steve initially balked at the use of "shrink," but when he went to start our podcast, he titled it "My Three Shrinks" and modified the logo from an old television show, "My Three Sons." When we went to title our book, I wanted to call it "Off the Couch," but I was told that there was no room for couches anywhere. After many months of lively debate, we ended up in a restaurant with our editor and a whiteboard, and by the end of the evening we were back at Shrink Rap for a title for the book.
When Clinical Psychiatry News and Psychology Today approached us to write for their sites, we decided to remain with an image that was working for us, and used Shrink Rap News and Shrink Rap Today for column titles. Because the term may imply something less than a serious look at psychiatric issues, the umbrella name for all our endeavors is The Accessible Psychiatry Project.
So, is the term "shrink" actually stigmatizing? When I think of words as being part of stigma, I think of racial and religious slurs, and those induce a visceral response of disgust in me. For whatever reason, I personally don’t have a clear negative association to the term "shrink" or even "headshrinker." To me, it evokes something lighthearted and includes having a sense of humor about the field. I imagine if psychiatrists ever had actually shrunken heads, I might feel differently. Others may well have another response to the term, but the emotional link to something negative is just not there for me.
From a site called World Wide Words – Investigating the English Language Across the Globe, which is devoted to linguistics and run by a British etymologist, I found the following history of the term "headshrinker":
The original meaning of the term head-shrinker was in reference to a member of a group in Amazonia, the Jivaro, who preserved the heads of their enemies by stripping the skin from the skull, which resulted in a shrunken mummified remnant the size of a fist. The term isn’t that old – it’s first recorded from 1926.
All the early evidence suggests that the person who invented the psychiatrist sense worked in the movies (no jokes please). We have to assume that the term came about because people regarded the process of psychiatry as being like head-shrinking because it reduced the size of the swollen egos so common in show business. Or perhaps they were suspicious about what psychiatrists actually did to their heads and how they did it and so made a joke to relieve the tension.
The earliest example we have is from an article in Time in November 1950 to which an editor has helpfully added a footnote to say that head-shrinker was Hollywood jargon for a psychiatrist. The term afterward became moderately popular, in part because it was used in the film Rebel Without a Cause in 1955. Robert Heinlein felt his readers needed it to be explained when he introduced it in "Time for the Stars" in 1956: " ‘Dr. Devereaux is the boss head-shrinker.’ I looked puzzled and Uncle Steve went on, ‘You don’t savvy? Psychiatrist.’ " By the time it turns up in West Side Story on Broadway in 1957, it was becoming established.
Shrink, the abbreviation, became popular in the United States in the 1970s, though it had first appeared in one of Thomas Pynchon’s books, "The Crying of Lot 49," in 1965, and there is anecdotal evidence that it was around earlier, which is only to be expected of a slang term that would have been mainly transmitted through the spoken word in its earliest days.
The issue of stigma in mental health has gotten a lot of attention as being one reason that people who have difficulties may not seek help. Certainly, words can be powerful, but I wonder if the term "shrink" might actually be easier for patients to use? "I’m going to see my shrink," might imply a visit with any number of mental health professionals and might disassociate it from the implication that the patient is going to see a psychiatrist for treatment of a mental illness, a condition that the media is all too happy to tell us causes people to commit mass murders.
"Shrink" may have a disparaging tone to it, or it may have a ring of affection, depending on the context. Certainly, there are many negative associations and jokes related to being an attorney, and one friend told me that his son was "going to the dark side" when the son applied to law school. Still, there is no stigma associated with having an appointment with one’s lawyer, leading me to believe that a profession can be stigmatized without stigmatizing the clientele.
Some words have taken on a pervasively negative meaning; others are harder to capture. After 8 years, Shrink Rap is now a platform for our writing, invested with its own meanings to us and our readers. The psychiatrist who wrote in to say it is offensive, odd, and stigmatizing certainly has a different set of associations to the word then we do, or we would never have let this be a title for our work.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011).
A Clinical Psychiatry News reader wrote in recently to object to the use of the term "shrink" in our column name. The writer noted, "We spend a lot of time trying to destigmatize the field, then use terms like this among ourselves. It’s odd and offensive." The feedback made me pause and wonder to myself if the term "shrink" is, in fact, stigmatizing.
Let me first give a little history of the decision to name our column "Shrink Rap News." In 2006, I was sitting at the kitchen table and decided I wanted a blog. I didn’t know what a blog actually was, but I wanted one. I went to blogger.com to set up a free website and was asked what I’d like to call my blog. On an impulse, I titled it "Shrink Rap." There was no debate or consideration, and no consultation. I liked the play on words with "shrink wrap," which is used for food storage, and I liked the connotation of psychiatrists talking, or "rapping." In a matter of hours, my impulsive thought was turned into the Shrink Rap blog.
Over the next few days, I invited Dr. Steve Daviss and Dr. Annette Hanson to join me in this venture, and Shrink Rap has continued to publish regular blog posts for 8.5 years now. Steve initially balked at the use of "shrink," but when he went to start our podcast, he titled it "My Three Shrinks" and modified the logo from an old television show, "My Three Sons." When we went to title our book, I wanted to call it "Off the Couch," but I was told that there was no room for couches anywhere. After many months of lively debate, we ended up in a restaurant with our editor and a whiteboard, and by the end of the evening we were back at Shrink Rap for a title for the book.
When Clinical Psychiatry News and Psychology Today approached us to write for their sites, we decided to remain with an image that was working for us, and used Shrink Rap News and Shrink Rap Today for column titles. Because the term may imply something less than a serious look at psychiatric issues, the umbrella name for all our endeavors is The Accessible Psychiatry Project.
So, is the term "shrink" actually stigmatizing? When I think of words as being part of stigma, I think of racial and religious slurs, and those induce a visceral response of disgust in me. For whatever reason, I personally don’t have a clear negative association to the term "shrink" or even "headshrinker." To me, it evokes something lighthearted and includes having a sense of humor about the field. I imagine if psychiatrists ever had actually shrunken heads, I might feel differently. Others may well have another response to the term, but the emotional link to something negative is just not there for me.
From a site called World Wide Words – Investigating the English Language Across the Globe, which is devoted to linguistics and run by a British etymologist, I found the following history of the term "headshrinker":
The original meaning of the term head-shrinker was in reference to a member of a group in Amazonia, the Jivaro, who preserved the heads of their enemies by stripping the skin from the skull, which resulted in a shrunken mummified remnant the size of a fist. The term isn’t that old – it’s first recorded from 1926.
All the early evidence suggests that the person who invented the psychiatrist sense worked in the movies (no jokes please). We have to assume that the term came about because people regarded the process of psychiatry as being like head-shrinking because it reduced the size of the swollen egos so common in show business. Or perhaps they were suspicious about what psychiatrists actually did to their heads and how they did it and so made a joke to relieve the tension.
The earliest example we have is from an article in Time in November 1950 to which an editor has helpfully added a footnote to say that head-shrinker was Hollywood jargon for a psychiatrist. The term afterward became moderately popular, in part because it was used in the film Rebel Without a Cause in 1955. Robert Heinlein felt his readers needed it to be explained when he introduced it in "Time for the Stars" in 1956: " ‘Dr. Devereaux is the boss head-shrinker.’ I looked puzzled and Uncle Steve went on, ‘You don’t savvy? Psychiatrist.’ " By the time it turns up in West Side Story on Broadway in 1957, it was becoming established.
Shrink, the abbreviation, became popular in the United States in the 1970s, though it had first appeared in one of Thomas Pynchon’s books, "The Crying of Lot 49," in 1965, and there is anecdotal evidence that it was around earlier, which is only to be expected of a slang term that would have been mainly transmitted through the spoken word in its earliest days.
The issue of stigma in mental health has gotten a lot of attention as being one reason that people who have difficulties may not seek help. Certainly, words can be powerful, but I wonder if the term "shrink" might actually be easier for patients to use? "I’m going to see my shrink," might imply a visit with any number of mental health professionals and might disassociate it from the implication that the patient is going to see a psychiatrist for treatment of a mental illness, a condition that the media is all too happy to tell us causes people to commit mass murders.
"Shrink" may have a disparaging tone to it, or it may have a ring of affection, depending on the context. Certainly, there are many negative associations and jokes related to being an attorney, and one friend told me that his son was "going to the dark side" when the son applied to law school. Still, there is no stigma associated with having an appointment with one’s lawyer, leading me to believe that a profession can be stigmatized without stigmatizing the clientele.
Some words have taken on a pervasively negative meaning; others are harder to capture. After 8 years, Shrink Rap is now a platform for our writing, invested with its own meanings to us and our readers. The psychiatrist who wrote in to say it is offensive, odd, and stigmatizing certainly has a different set of associations to the word then we do, or we would never have let this be a title for our work.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011).
Prescribing psychotropics to family members
Recently, I put up a post on our main Shrink Rap blog titled, "Is it okay to shrink your sister in an emergency?" Given how difficult it can be to get an appointment with a psychiatrist, I wondered about the ethics of prescribing psychotropics to a distressed family member when other options are limited.
First, I created a fictional scenario. Sister Lucy was treated for panic disorder 5 years ago. She took a benzodiazepine for a few weeks, an SSRI for a year, and went to psychotherapy. Her symptoms resolved, and she was able to terminate treatment with the blessing of her psychiatrist. Last year, Lucy moved to a new state and, being generally healthy, she has not yet established relationships with primary care providers. So with no physician, in a new state, Lucy had a recurrence of her panic disorder. She was initially seen in an emergency department, given a small supply of Ativan (lorazepam), and instructions to see a psychiatrist.
Lucy called around, and the earliest appointment she could get was 6 weeks away. She tried a handful of psychiatrists, but she did not call every psychiatrist in town. Most of the ones she tried were not taking new patients, and the voice mail systems of each mental health group were time consuming and frustrating, some cut her off, and no one had any more immediate response than to go to the ED if it were an emergency, and Lucy had already done that. Her brother, a psychiatrist in another state, came to visit for the weekend, and he witnessed several of her panic attacks. He had no more luck finding a psychiatrist for her. Lucy visited an urgent care center, where she was restarted on the SSRI and given more of the Ativan. But at the drugstore, she noticed she was given a 2-week supply and this would not last until the scheduled appointment.
So I asked our blog readers if it was okay for the brother to write prescriptions to hold his sister over until her scheduled appointment. The other options would have been for her to continue to suffer, to see if she could find another form of treatment more quickly, to return to the urgent care center on a continual basis and hope they would provide more medication, or to find a new primary care doctor who could prescribe in the meantime. Lucy didn’t know if this would be any easier. The psychiatrist who saw her 5 years ago before she moved would not be comfortable resuming medications without seeing her, but just in case there was any doubt, he retired, moved to North Korea, and died in a freak accident where he was swept up by a street cleaner so that option was not on the table (fictional characters can lead interesting and tragic lives).
Readers wrote in with a variety of thoughts. One psychiatrist empathized; she had a very depressed relative, and she debated providing medication samples in the interim while the relative waited to get in with a mental health professional. Another psychiatrist had seen too many patients become addicted to prescription benzodiazepines and suggested that this might start a cycle where Sister Lucy would pester brother psychiatrist for more medication in the future. Most of the psychiatrists felt that if a reasonable effort were made to obtain care and the barriers were valid, then it was a tough situation, but ultimately they felt it was okay to resume medications that previously had worked and been tolerated, for a limited period of time, since Lucy was symptomatic and this constituted an emergency.
The patients who wrote in were less forgiving, overall. Several insisted it was easy enough to find a primary care doctor within days, and a primary care doctor would certainly prescribe the medications. I was told that all one has to do is call one’s insurance company, so, curious, I called mine and got two names. The first one had a message saying staff was not in on Wednesday and the caller should try back tomorrow. I didn’t. The second one instructed me to leave a message that would be returned within 24 hours. It wasn’t. I e-mailed my own primary care doctor to ask when the next new patient appointment was – this physician charges a practice fee (too low to be considered "concierge," but high enough to enable a lower caseload). The response I received is that the practice is full. I e-mailed a friend who is a wonderful primary care doctor but takes no health insurance and has opted out of Medicare, and he had an opening the following week. I, however, had insider knowledge that a random newcomer to town might not have, and the insurance companies would certainly not be referring urgent cases to this out-of-network doctor. And all this assumes that any doc will do; there is no allowance here for the idea of waiting for a psychiatrist or internist who might come highly recommended or have subspecialty training.
I was left to say that it wasn’t easy to find a psychiatrist or a primary care doctor on demand when one is new in town and in a state of emotional distress. Again, I was told otherwise! I learned about a service called ZocDoc.com where you can make a next day appointment with a physician, simply by giving your Zip code, insurance, and specialty desired. Interesting, as I do this all the time with an App called OpenTable to schedule reservations at restaurants. Why not doctors’ appointments?
So it was late, and I tried to schedule a next day appointment with a primary care doc. It worked! Only I didn’t really want the appointment; what I wanted was information to write my article for Clinical Psychiatry News this week. I dialed the doctor to cancel the appointment, and instead of getting an office machine, I got the actual doctor – and he even sounded like a nice guy. He couldn’t cancel my appointment, but I then realized that, like OpenTable, there was a button to push to cancel the appointment, and I did that. I looked for psychiatrists, and there weren’t many with next day appointments – perhaps one – nearby, but if I would drive 30 miles or so to the next major city, I could get an appointment very soon, and certainly within a couple of weeks. Interesting. I learned something new!
So I wondered about Sister Lucy, and I decided she lives in Boise, Idaho, a place I’ve never been to and whose availability of medical care I know nothing about. The ZocDoc site there is not active, and so poor Lucy is back to her original problem, and I am left to the original question: Should her brother prescribe her medications?
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
Recently, I put up a post on our main Shrink Rap blog titled, "Is it okay to shrink your sister in an emergency?" Given how difficult it can be to get an appointment with a psychiatrist, I wondered about the ethics of prescribing psychotropics to a distressed family member when other options are limited.
First, I created a fictional scenario. Sister Lucy was treated for panic disorder 5 years ago. She took a benzodiazepine for a few weeks, an SSRI for a year, and went to psychotherapy. Her symptoms resolved, and she was able to terminate treatment with the blessing of her psychiatrist. Last year, Lucy moved to a new state and, being generally healthy, she has not yet established relationships with primary care providers. So with no physician, in a new state, Lucy had a recurrence of her panic disorder. She was initially seen in an emergency department, given a small supply of Ativan (lorazepam), and instructions to see a psychiatrist.
Lucy called around, and the earliest appointment she could get was 6 weeks away. She tried a handful of psychiatrists, but she did not call every psychiatrist in town. Most of the ones she tried were not taking new patients, and the voice mail systems of each mental health group were time consuming and frustrating, some cut her off, and no one had any more immediate response than to go to the ED if it were an emergency, and Lucy had already done that. Her brother, a psychiatrist in another state, came to visit for the weekend, and he witnessed several of her panic attacks. He had no more luck finding a psychiatrist for her. Lucy visited an urgent care center, where she was restarted on the SSRI and given more of the Ativan. But at the drugstore, she noticed she was given a 2-week supply and this would not last until the scheduled appointment.
So I asked our blog readers if it was okay for the brother to write prescriptions to hold his sister over until her scheduled appointment. The other options would have been for her to continue to suffer, to see if she could find another form of treatment more quickly, to return to the urgent care center on a continual basis and hope they would provide more medication, or to find a new primary care doctor who could prescribe in the meantime. Lucy didn’t know if this would be any easier. The psychiatrist who saw her 5 years ago before she moved would not be comfortable resuming medications without seeing her, but just in case there was any doubt, he retired, moved to North Korea, and died in a freak accident where he was swept up by a street cleaner so that option was not on the table (fictional characters can lead interesting and tragic lives).
Readers wrote in with a variety of thoughts. One psychiatrist empathized; she had a very depressed relative, and she debated providing medication samples in the interim while the relative waited to get in with a mental health professional. Another psychiatrist had seen too many patients become addicted to prescription benzodiazepines and suggested that this might start a cycle where Sister Lucy would pester brother psychiatrist for more medication in the future. Most of the psychiatrists felt that if a reasonable effort were made to obtain care and the barriers were valid, then it was a tough situation, but ultimately they felt it was okay to resume medications that previously had worked and been tolerated, for a limited period of time, since Lucy was symptomatic and this constituted an emergency.
The patients who wrote in were less forgiving, overall. Several insisted it was easy enough to find a primary care doctor within days, and a primary care doctor would certainly prescribe the medications. I was told that all one has to do is call one’s insurance company, so, curious, I called mine and got two names. The first one had a message saying staff was not in on Wednesday and the caller should try back tomorrow. I didn’t. The second one instructed me to leave a message that would be returned within 24 hours. It wasn’t. I e-mailed my own primary care doctor to ask when the next new patient appointment was – this physician charges a practice fee (too low to be considered "concierge," but high enough to enable a lower caseload). The response I received is that the practice is full. I e-mailed a friend who is a wonderful primary care doctor but takes no health insurance and has opted out of Medicare, and he had an opening the following week. I, however, had insider knowledge that a random newcomer to town might not have, and the insurance companies would certainly not be referring urgent cases to this out-of-network doctor. And all this assumes that any doc will do; there is no allowance here for the idea of waiting for a psychiatrist or internist who might come highly recommended or have subspecialty training.
I was left to say that it wasn’t easy to find a psychiatrist or a primary care doctor on demand when one is new in town and in a state of emotional distress. Again, I was told otherwise! I learned about a service called ZocDoc.com where you can make a next day appointment with a physician, simply by giving your Zip code, insurance, and specialty desired. Interesting, as I do this all the time with an App called OpenTable to schedule reservations at restaurants. Why not doctors’ appointments?
So it was late, and I tried to schedule a next day appointment with a primary care doc. It worked! Only I didn’t really want the appointment; what I wanted was information to write my article for Clinical Psychiatry News this week. I dialed the doctor to cancel the appointment, and instead of getting an office machine, I got the actual doctor – and he even sounded like a nice guy. He couldn’t cancel my appointment, but I then realized that, like OpenTable, there was a button to push to cancel the appointment, and I did that. I looked for psychiatrists, and there weren’t many with next day appointments – perhaps one – nearby, but if I would drive 30 miles or so to the next major city, I could get an appointment very soon, and certainly within a couple of weeks. Interesting. I learned something new!
So I wondered about Sister Lucy, and I decided she lives in Boise, Idaho, a place I’ve never been to and whose availability of medical care I know nothing about. The ZocDoc site there is not active, and so poor Lucy is back to her original problem, and I am left to the original question: Should her brother prescribe her medications?
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
Recently, I put up a post on our main Shrink Rap blog titled, "Is it okay to shrink your sister in an emergency?" Given how difficult it can be to get an appointment with a psychiatrist, I wondered about the ethics of prescribing psychotropics to a distressed family member when other options are limited.
First, I created a fictional scenario. Sister Lucy was treated for panic disorder 5 years ago. She took a benzodiazepine for a few weeks, an SSRI for a year, and went to psychotherapy. Her symptoms resolved, and she was able to terminate treatment with the blessing of her psychiatrist. Last year, Lucy moved to a new state and, being generally healthy, she has not yet established relationships with primary care providers. So with no physician, in a new state, Lucy had a recurrence of her panic disorder. She was initially seen in an emergency department, given a small supply of Ativan (lorazepam), and instructions to see a psychiatrist.
Lucy called around, and the earliest appointment she could get was 6 weeks away. She tried a handful of psychiatrists, but she did not call every psychiatrist in town. Most of the ones she tried were not taking new patients, and the voice mail systems of each mental health group were time consuming and frustrating, some cut her off, and no one had any more immediate response than to go to the ED if it were an emergency, and Lucy had already done that. Her brother, a psychiatrist in another state, came to visit for the weekend, and he witnessed several of her panic attacks. He had no more luck finding a psychiatrist for her. Lucy visited an urgent care center, where she was restarted on the SSRI and given more of the Ativan. But at the drugstore, she noticed she was given a 2-week supply and this would not last until the scheduled appointment.
So I asked our blog readers if it was okay for the brother to write prescriptions to hold his sister over until her scheduled appointment. The other options would have been for her to continue to suffer, to see if she could find another form of treatment more quickly, to return to the urgent care center on a continual basis and hope they would provide more medication, or to find a new primary care doctor who could prescribe in the meantime. Lucy didn’t know if this would be any easier. The psychiatrist who saw her 5 years ago before she moved would not be comfortable resuming medications without seeing her, but just in case there was any doubt, he retired, moved to North Korea, and died in a freak accident where he was swept up by a street cleaner so that option was not on the table (fictional characters can lead interesting and tragic lives).
Readers wrote in with a variety of thoughts. One psychiatrist empathized; she had a very depressed relative, and she debated providing medication samples in the interim while the relative waited to get in with a mental health professional. Another psychiatrist had seen too many patients become addicted to prescription benzodiazepines and suggested that this might start a cycle where Sister Lucy would pester brother psychiatrist for more medication in the future. Most of the psychiatrists felt that if a reasonable effort were made to obtain care and the barriers were valid, then it was a tough situation, but ultimately they felt it was okay to resume medications that previously had worked and been tolerated, for a limited period of time, since Lucy was symptomatic and this constituted an emergency.
The patients who wrote in were less forgiving, overall. Several insisted it was easy enough to find a primary care doctor within days, and a primary care doctor would certainly prescribe the medications. I was told that all one has to do is call one’s insurance company, so, curious, I called mine and got two names. The first one had a message saying staff was not in on Wednesday and the caller should try back tomorrow. I didn’t. The second one instructed me to leave a message that would be returned within 24 hours. It wasn’t. I e-mailed my own primary care doctor to ask when the next new patient appointment was – this physician charges a practice fee (too low to be considered "concierge," but high enough to enable a lower caseload). The response I received is that the practice is full. I e-mailed a friend who is a wonderful primary care doctor but takes no health insurance and has opted out of Medicare, and he had an opening the following week. I, however, had insider knowledge that a random newcomer to town might not have, and the insurance companies would certainly not be referring urgent cases to this out-of-network doctor. And all this assumes that any doc will do; there is no allowance here for the idea of waiting for a psychiatrist or internist who might come highly recommended or have subspecialty training.
I was left to say that it wasn’t easy to find a psychiatrist or a primary care doctor on demand when one is new in town and in a state of emotional distress. Again, I was told otherwise! I learned about a service called ZocDoc.com where you can make a next day appointment with a physician, simply by giving your Zip code, insurance, and specialty desired. Interesting, as I do this all the time with an App called OpenTable to schedule reservations at restaurants. Why not doctors’ appointments?
So it was late, and I tried to schedule a next day appointment with a primary care doc. It worked! Only I didn’t really want the appointment; what I wanted was information to write my article for Clinical Psychiatry News this week. I dialed the doctor to cancel the appointment, and instead of getting an office machine, I got the actual doctor – and he even sounded like a nice guy. He couldn’t cancel my appointment, but I then realized that, like OpenTable, there was a button to push to cancel the appointment, and I did that. I looked for psychiatrists, and there weren’t many with next day appointments – perhaps one – nearby, but if I would drive 30 miles or so to the next major city, I could get an appointment very soon, and certainly within a couple of weeks. Interesting. I learned something new!
So I wondered about Sister Lucy, and I decided she lives in Boise, Idaho, a place I’ve never been to and whose availability of medical care I know nothing about. The ZocDoc site there is not active, and so poor Lucy is back to her original problem, and I am left to the original question: Should her brother prescribe her medications?
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
Distinguishing the killers among us
When I was in high school, one of my friends told me he intended to kill another one of my friends. It was a different day and age back then, and with more than 4,000 students, my high school was rather large and impersonal – it was easy to get lost in the crowd.
"Juan" (not his real name) confided in me that he wanted to kill "Joe" (also not his real name), which I found a bit odd. Joe was well liked but not did really stand out. Juan was perhaps quieter and more studious, but he also did not stand out. Both boys had friends, did well in school, and were not obviously troubled. When I asked Juan why he wanted to kill Joe, he responded, "Because he’s the all-American boy."
I worried about this. I told my mother, and I told a teacher I trusted. No one knew what to do, and Juan’s plan did not sound feasible. He was going to bring a knife to school in a folder, and when Joe was walking in a crowded hallway, Juan would walk behind him and thrust out the folder to sent the knife flying. The physics of this just didn’t make sense to me, and I didn’t see how the knife would gain enough momentum to travel very far, much less penetrate a person through their clothes. Feasible, or not, however, the equation changed on a day that Juan and I were sitting together in the back row of Latin class. Juan opened his calculus book and showed me the butcher knife.
I excused myself from class, went to a pay phone, and called my mother. She called the school, the principal called the police, and Juan was quietly removed from school when the period ended. It would be hard to imagine that a teenager who plotted the murder of another student, by illogical means for an illogical reason, wasn’t emotionally disturbed. I don’t know what happens to someone like Juan in 2014 – I’m thinking nothing good – but let me tell you what happened to Juan in the late 1970s.
Juan was out of high school for 6 weeks. I heard he had psychological testing, but aside from that, I have no idea what transpired. One of his friends told me it was a joke. He returned to high school, never said another word to me, graduated, and attended an Ivy League university – one of several prestigious schools to which he gained admission. A Google search reveals that Juan later earned a graduate degree and works as an executive making a six-figure salary. (Isn’t Google great?) He’s an adjunct professor at a college where he gets glowing reviews on RateMyProfessors.com. He was elected to serve on a local government committee. He’s married and has children. Compliments of Facebook, I know that he continues to have contact with high school friends.
From what I can tell, Juan’s brief period of being a disturbed adolescent did not progress to a life defined by chronic mental illness, and he did not go on to become a violent felon. I have no idea if I did Juan a favor, prevented a murder, got him much-needed treatment, or simply added an embarrassing diversion to his life. I don’t know if he ever really would have harmed Joe, or if it was in fact a joke designed to yank my chain.
Apparently, my threshold is on the low side, and not long ago I called a friend late one night and insisted she check on her teenager when a Facebook post struck me as alarming and a bit too final. The response I got was, "They were lyrics from a song and you’re overreacting." So be it. I called the mother and not the National Guard, and if the teen had become a statistic, I would have regretted not reacting.
I did wonder, while writing this article, how it would be received if I were to contact Juan and ask his thoughts on those events decades ago. Somehow, it seemed best not to uncover old wounds.
The media talk about the dangerously mentally ill as though they are a separate breed of humans, ones who can be easily distinguished by simply assessing who stands on which side of a well-marked "us-versus-them" line. Human beings, especially young human beings, may go through phases, and they may struggle with controlling their emotions, behaviors, and impulses and with finding their identity at a time in life when fitting in has undue importance. Some of them, no doubt, have these crises in the throes of an acute episode of mental distress – illness, if you’d prefer – and others do so at the genesis of what will prove to be a chronic and persistent psychiatric disorder. It may not be clear at any given moment who is going through a phase, who is suffering from an acute episode of mental illness, and who is beginning their course of a severe and persistent disorder.
Still, there are those who want to neatly categorize those with "serious" mental illness so that we can focus more of our resources on their needs and not on those who they deem to be the "worried well." Juan, it appears, did not fall into that category of chronically or persistently mentally ill. Similarly, all of us know chaotic, misbehaving, and even suicidal teenagers who go on to live productive lives. Does that designation matter if those not-so-seriously (or not-so-obviously) mentally ill individuals kill someone or die during their brief moments of emotional turbulence?
It seems to me that the goal is to keep people safe and help usher them through difficult periods in their lives, regardless of any diagnostic certainty or severity. I would contend that the mentally healthy among us also are subject to impulsive, distressed, and dangerous moments and that the world does not always neatly divide people into proper categorical entities.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011).
When I was in high school, one of my friends told me he intended to kill another one of my friends. It was a different day and age back then, and with more than 4,000 students, my high school was rather large and impersonal – it was easy to get lost in the crowd.
"Juan" (not his real name) confided in me that he wanted to kill "Joe" (also not his real name), which I found a bit odd. Joe was well liked but not did really stand out. Juan was perhaps quieter and more studious, but he also did not stand out. Both boys had friends, did well in school, and were not obviously troubled. When I asked Juan why he wanted to kill Joe, he responded, "Because he’s the all-American boy."
I worried about this. I told my mother, and I told a teacher I trusted. No one knew what to do, and Juan’s plan did not sound feasible. He was going to bring a knife to school in a folder, and when Joe was walking in a crowded hallway, Juan would walk behind him and thrust out the folder to sent the knife flying. The physics of this just didn’t make sense to me, and I didn’t see how the knife would gain enough momentum to travel very far, much less penetrate a person through their clothes. Feasible, or not, however, the equation changed on a day that Juan and I were sitting together in the back row of Latin class. Juan opened his calculus book and showed me the butcher knife.
I excused myself from class, went to a pay phone, and called my mother. She called the school, the principal called the police, and Juan was quietly removed from school when the period ended. It would be hard to imagine that a teenager who plotted the murder of another student, by illogical means for an illogical reason, wasn’t emotionally disturbed. I don’t know what happens to someone like Juan in 2014 – I’m thinking nothing good – but let me tell you what happened to Juan in the late 1970s.
Juan was out of high school for 6 weeks. I heard he had psychological testing, but aside from that, I have no idea what transpired. One of his friends told me it was a joke. He returned to high school, never said another word to me, graduated, and attended an Ivy League university – one of several prestigious schools to which he gained admission. A Google search reveals that Juan later earned a graduate degree and works as an executive making a six-figure salary. (Isn’t Google great?) He’s an adjunct professor at a college where he gets glowing reviews on RateMyProfessors.com. He was elected to serve on a local government committee. He’s married and has children. Compliments of Facebook, I know that he continues to have contact with high school friends.
From what I can tell, Juan’s brief period of being a disturbed adolescent did not progress to a life defined by chronic mental illness, and he did not go on to become a violent felon. I have no idea if I did Juan a favor, prevented a murder, got him much-needed treatment, or simply added an embarrassing diversion to his life. I don’t know if he ever really would have harmed Joe, or if it was in fact a joke designed to yank my chain.
Apparently, my threshold is on the low side, and not long ago I called a friend late one night and insisted she check on her teenager when a Facebook post struck me as alarming and a bit too final. The response I got was, "They were lyrics from a song and you’re overreacting." So be it. I called the mother and not the National Guard, and if the teen had become a statistic, I would have regretted not reacting.
I did wonder, while writing this article, how it would be received if I were to contact Juan and ask his thoughts on those events decades ago. Somehow, it seemed best not to uncover old wounds.
The media talk about the dangerously mentally ill as though they are a separate breed of humans, ones who can be easily distinguished by simply assessing who stands on which side of a well-marked "us-versus-them" line. Human beings, especially young human beings, may go through phases, and they may struggle with controlling their emotions, behaviors, and impulses and with finding their identity at a time in life when fitting in has undue importance. Some of them, no doubt, have these crises in the throes of an acute episode of mental distress – illness, if you’d prefer – and others do so at the genesis of what will prove to be a chronic and persistent psychiatric disorder. It may not be clear at any given moment who is going through a phase, who is suffering from an acute episode of mental illness, and who is beginning their course of a severe and persistent disorder.
Still, there are those who want to neatly categorize those with "serious" mental illness so that we can focus more of our resources on their needs and not on those who they deem to be the "worried well." Juan, it appears, did not fall into that category of chronically or persistently mentally ill. Similarly, all of us know chaotic, misbehaving, and even suicidal teenagers who go on to live productive lives. Does that designation matter if those not-so-seriously (or not-so-obviously) mentally ill individuals kill someone or die during their brief moments of emotional turbulence?
It seems to me that the goal is to keep people safe and help usher them through difficult periods in their lives, regardless of any diagnostic certainty or severity. I would contend that the mentally healthy among us also are subject to impulsive, distressed, and dangerous moments and that the world does not always neatly divide people into proper categorical entities.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011).
When I was in high school, one of my friends told me he intended to kill another one of my friends. It was a different day and age back then, and with more than 4,000 students, my high school was rather large and impersonal – it was easy to get lost in the crowd.
"Juan" (not his real name) confided in me that he wanted to kill "Joe" (also not his real name), which I found a bit odd. Joe was well liked but not did really stand out. Juan was perhaps quieter and more studious, but he also did not stand out. Both boys had friends, did well in school, and were not obviously troubled. When I asked Juan why he wanted to kill Joe, he responded, "Because he’s the all-American boy."
I worried about this. I told my mother, and I told a teacher I trusted. No one knew what to do, and Juan’s plan did not sound feasible. He was going to bring a knife to school in a folder, and when Joe was walking in a crowded hallway, Juan would walk behind him and thrust out the folder to sent the knife flying. The physics of this just didn’t make sense to me, and I didn’t see how the knife would gain enough momentum to travel very far, much less penetrate a person through their clothes. Feasible, or not, however, the equation changed on a day that Juan and I were sitting together in the back row of Latin class. Juan opened his calculus book and showed me the butcher knife.
I excused myself from class, went to a pay phone, and called my mother. She called the school, the principal called the police, and Juan was quietly removed from school when the period ended. It would be hard to imagine that a teenager who plotted the murder of another student, by illogical means for an illogical reason, wasn’t emotionally disturbed. I don’t know what happens to someone like Juan in 2014 – I’m thinking nothing good – but let me tell you what happened to Juan in the late 1970s.
Juan was out of high school for 6 weeks. I heard he had psychological testing, but aside from that, I have no idea what transpired. One of his friends told me it was a joke. He returned to high school, never said another word to me, graduated, and attended an Ivy League university – one of several prestigious schools to which he gained admission. A Google search reveals that Juan later earned a graduate degree and works as an executive making a six-figure salary. (Isn’t Google great?) He’s an adjunct professor at a college where he gets glowing reviews on RateMyProfessors.com. He was elected to serve on a local government committee. He’s married and has children. Compliments of Facebook, I know that he continues to have contact with high school friends.
From what I can tell, Juan’s brief period of being a disturbed adolescent did not progress to a life defined by chronic mental illness, and he did not go on to become a violent felon. I have no idea if I did Juan a favor, prevented a murder, got him much-needed treatment, or simply added an embarrassing diversion to his life. I don’t know if he ever really would have harmed Joe, or if it was in fact a joke designed to yank my chain.
Apparently, my threshold is on the low side, and not long ago I called a friend late one night and insisted she check on her teenager when a Facebook post struck me as alarming and a bit too final. The response I got was, "They were lyrics from a song and you’re overreacting." So be it. I called the mother and not the National Guard, and if the teen had become a statistic, I would have regretted not reacting.
I did wonder, while writing this article, how it would be received if I were to contact Juan and ask his thoughts on those events decades ago. Somehow, it seemed best not to uncover old wounds.
The media talk about the dangerously mentally ill as though they are a separate breed of humans, ones who can be easily distinguished by simply assessing who stands on which side of a well-marked "us-versus-them" line. Human beings, especially young human beings, may go through phases, and they may struggle with controlling their emotions, behaviors, and impulses and with finding their identity at a time in life when fitting in has undue importance. Some of them, no doubt, have these crises in the throes of an acute episode of mental distress – illness, if you’d prefer – and others do so at the genesis of what will prove to be a chronic and persistent psychiatric disorder. It may not be clear at any given moment who is going through a phase, who is suffering from an acute episode of mental illness, and who is beginning their course of a severe and persistent disorder.
Still, there are those who want to neatly categorize those with "serious" mental illness so that we can focus more of our resources on their needs and not on those who they deem to be the "worried well." Juan, it appears, did not fall into that category of chronically or persistently mentally ill. Similarly, all of us know chaotic, misbehaving, and even suicidal teenagers who go on to live productive lives. Does that designation matter if those not-so-seriously (or not-so-obviously) mentally ill individuals kill someone or die during their brief moments of emotional turbulence?
It seems to me that the goal is to keep people safe and help usher them through difficult periods in their lives, regardless of any diagnostic certainty or severity. I would contend that the mentally healthy among us also are subject to impulsive, distressed, and dangerous moments and that the world does not always neatly divide people into proper categorical entities.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011).
Legislation’s privacy exceptions for psychiatric patients are concerning
Like many of you, I’m currently in New York City for 5 days of psychiatry and psychiatrists, 24/7. I’m hoping there will be a bagel with lox in there somewhere as well.
I wanted to talk about one section of Rep. Tim Murphy’s (R-Pa.) proposed legislation, H.R. 3717, the Helping Families in Mental Health Crisis Act. If you’re not familiar with it, the legislation intends to overhaul a broken mental health system in the United States. One component of the bill, Section 301 located on page 44, deals with modifying HIPAA such that mental health providers can speak with caregivers and family members. Rep. Murphy – who is also a psychologist – has noted in his television appearance and in public testimony that HIPAA is misinterpreted such that families are sometimes told they may not provide historical information about the patient. HIPAA does not actually prevent a mental health professional from listening to anyone’s free speech, but there seem to be times when the involved parties believe this is the case.
In addition, Rep. Murphy noted that HIPAA prevents clinicians from releasing information to caretakers that might help in providing for outpatient care – specifically for releasing medication information and follow-up appointments to those who may be responsible for helping patients negotiate these crucial items.
The proposed legislation reads:
"Caregiver Access to Information: ...to an individual with a serious mental illness who does not provide consent for the disclosure of protected health information to a caregiver of such individual, the caregiver shall be treated by a covered entity as a personal representative ... when the provider furnishing services to the individual reasonably believes it is necessary for protected health information of the individual to be made available to the caregiver in order to protect the health, safety, or welfare of such individuals or the safety of one or more other individuals."
The bill goes on to define "caregiver" as an immediate family member, an individual who assumes primary responsibility for providing for the patient’s basic needs, or a personal representative as determined by law. I think we all agree that collaboration and communication are essential to the care of our patients, and so I applaud these efforts. I worry, however, about the unintended consequences and what roads this might lead us down.
Long before we had HIPAA, we had requirements for patient confidentiality. I, like Rep. Murphy, believe that HIPAA gets distorted. "We need to let your family know your discharge medications and follow-up appointments," is not often met with resistance, but if it is, shouldn’t that be respected? What if patients have valid reasons for not wanting family to know their medications? What if they feel their family is too intrusive, or is part of the problem? Such legislation might suggest that the family is always right and the patient is always wrong.
While the intent (as I’ve understood it from Rep. Murphy’s speeches) is to allow hospitals to tell families, "Yes, your loved [one] has been admitted to our inpatient unit," or to allow well-negotiated follow-up to prevent relapse, might such legislation lead patients to believe that the content of their discussions with mental health professionals can be relayed to others against their will? Might it serve as one more reason for a troubled individual to avoid care?
From a psychiatrist’s point of view, I might be concerned that I would agree with a patient that information should not be released to family, and nothing about this law would then force me to release it. But would family members feel the law says otherwise? Will they contend, "My family member is mentally ill so HIPAA does not apply, and you must release information to me?" While any given psychiatrist might choose not to release information on any given patient, I wonder if this might be setting us up to be at odds with families, and that would not be a good thing. Much as I’m no fan of HIPAA for many reasons, people do understand the concept that confidentiality is required by law. Perhaps I’m reading too much into this?
Finally, we all agree that eliminating stigma is a good thing when it comes to facilitating voluntary care for those who might need it. But I wonder if we can say that people with mental illnesses are just like everyone else, that this is a medical condition just like other conditions, but for this select group of people they lose their right to privacy, much as children have no right to medical privacy. Might that add to the stigma of mental illness?
I don’t have an answer. I believe the intentions of the Helping Families in Mental Health Crisis Act are good, and I believe they target weaknesses in our system. But I also worry that the legislation might create as many problems as it might fix.
The comments feature of the Clinical Psychiatry News website is turned off for the moment, and I would love to hear your thoughts. Please do e-mail with your comments; I can be reached at ShrinkRapBlog@gmail.com, or you may comment on a similar post here.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
Like many of you, I’m currently in New York City for 5 days of psychiatry and psychiatrists, 24/7. I’m hoping there will be a bagel with lox in there somewhere as well.
I wanted to talk about one section of Rep. Tim Murphy’s (R-Pa.) proposed legislation, H.R. 3717, the Helping Families in Mental Health Crisis Act. If you’re not familiar with it, the legislation intends to overhaul a broken mental health system in the United States. One component of the bill, Section 301 located on page 44, deals with modifying HIPAA such that mental health providers can speak with caregivers and family members. Rep. Murphy – who is also a psychologist – has noted in his television appearance and in public testimony that HIPAA is misinterpreted such that families are sometimes told they may not provide historical information about the patient. HIPAA does not actually prevent a mental health professional from listening to anyone’s free speech, but there seem to be times when the involved parties believe this is the case.
In addition, Rep. Murphy noted that HIPAA prevents clinicians from releasing information to caretakers that might help in providing for outpatient care – specifically for releasing medication information and follow-up appointments to those who may be responsible for helping patients negotiate these crucial items.
The proposed legislation reads:
"Caregiver Access to Information: ...to an individual with a serious mental illness who does not provide consent for the disclosure of protected health information to a caregiver of such individual, the caregiver shall be treated by a covered entity as a personal representative ... when the provider furnishing services to the individual reasonably believes it is necessary for protected health information of the individual to be made available to the caregiver in order to protect the health, safety, or welfare of such individuals or the safety of one or more other individuals."
The bill goes on to define "caregiver" as an immediate family member, an individual who assumes primary responsibility for providing for the patient’s basic needs, or a personal representative as determined by law. I think we all agree that collaboration and communication are essential to the care of our patients, and so I applaud these efforts. I worry, however, about the unintended consequences and what roads this might lead us down.
Long before we had HIPAA, we had requirements for patient confidentiality. I, like Rep. Murphy, believe that HIPAA gets distorted. "We need to let your family know your discharge medications and follow-up appointments," is not often met with resistance, but if it is, shouldn’t that be respected? What if patients have valid reasons for not wanting family to know their medications? What if they feel their family is too intrusive, or is part of the problem? Such legislation might suggest that the family is always right and the patient is always wrong.
While the intent (as I’ve understood it from Rep. Murphy’s speeches) is to allow hospitals to tell families, "Yes, your loved [one] has been admitted to our inpatient unit," or to allow well-negotiated follow-up to prevent relapse, might such legislation lead patients to believe that the content of their discussions with mental health professionals can be relayed to others against their will? Might it serve as one more reason for a troubled individual to avoid care?
From a psychiatrist’s point of view, I might be concerned that I would agree with a patient that information should not be released to family, and nothing about this law would then force me to release it. But would family members feel the law says otherwise? Will they contend, "My family member is mentally ill so HIPAA does not apply, and you must release information to me?" While any given psychiatrist might choose not to release information on any given patient, I wonder if this might be setting us up to be at odds with families, and that would not be a good thing. Much as I’m no fan of HIPAA for many reasons, people do understand the concept that confidentiality is required by law. Perhaps I’m reading too much into this?
Finally, we all agree that eliminating stigma is a good thing when it comes to facilitating voluntary care for those who might need it. But I wonder if we can say that people with mental illnesses are just like everyone else, that this is a medical condition just like other conditions, but for this select group of people they lose their right to privacy, much as children have no right to medical privacy. Might that add to the stigma of mental illness?
I don’t have an answer. I believe the intentions of the Helping Families in Mental Health Crisis Act are good, and I believe they target weaknesses in our system. But I also worry that the legislation might create as many problems as it might fix.
The comments feature of the Clinical Psychiatry News website is turned off for the moment, and I would love to hear your thoughts. Please do e-mail with your comments; I can be reached at ShrinkRapBlog@gmail.com, or you may comment on a similar post here.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
Like many of you, I’m currently in New York City for 5 days of psychiatry and psychiatrists, 24/7. I’m hoping there will be a bagel with lox in there somewhere as well.
I wanted to talk about one section of Rep. Tim Murphy’s (R-Pa.) proposed legislation, H.R. 3717, the Helping Families in Mental Health Crisis Act. If you’re not familiar with it, the legislation intends to overhaul a broken mental health system in the United States. One component of the bill, Section 301 located on page 44, deals with modifying HIPAA such that mental health providers can speak with caregivers and family members. Rep. Murphy – who is also a psychologist – has noted in his television appearance and in public testimony that HIPAA is misinterpreted such that families are sometimes told they may not provide historical information about the patient. HIPAA does not actually prevent a mental health professional from listening to anyone’s free speech, but there seem to be times when the involved parties believe this is the case.
In addition, Rep. Murphy noted that HIPAA prevents clinicians from releasing information to caretakers that might help in providing for outpatient care – specifically for releasing medication information and follow-up appointments to those who may be responsible for helping patients negotiate these crucial items.
The proposed legislation reads:
"Caregiver Access to Information: ...to an individual with a serious mental illness who does not provide consent for the disclosure of protected health information to a caregiver of such individual, the caregiver shall be treated by a covered entity as a personal representative ... when the provider furnishing services to the individual reasonably believes it is necessary for protected health information of the individual to be made available to the caregiver in order to protect the health, safety, or welfare of such individuals or the safety of one or more other individuals."
The bill goes on to define "caregiver" as an immediate family member, an individual who assumes primary responsibility for providing for the patient’s basic needs, or a personal representative as determined by law. I think we all agree that collaboration and communication are essential to the care of our patients, and so I applaud these efforts. I worry, however, about the unintended consequences and what roads this might lead us down.
Long before we had HIPAA, we had requirements for patient confidentiality. I, like Rep. Murphy, believe that HIPAA gets distorted. "We need to let your family know your discharge medications and follow-up appointments," is not often met with resistance, but if it is, shouldn’t that be respected? What if patients have valid reasons for not wanting family to know their medications? What if they feel their family is too intrusive, or is part of the problem? Such legislation might suggest that the family is always right and the patient is always wrong.
While the intent (as I’ve understood it from Rep. Murphy’s speeches) is to allow hospitals to tell families, "Yes, your loved [one] has been admitted to our inpatient unit," or to allow well-negotiated follow-up to prevent relapse, might such legislation lead patients to believe that the content of their discussions with mental health professionals can be relayed to others against their will? Might it serve as one more reason for a troubled individual to avoid care?
From a psychiatrist’s point of view, I might be concerned that I would agree with a patient that information should not be released to family, and nothing about this law would then force me to release it. But would family members feel the law says otherwise? Will they contend, "My family member is mentally ill so HIPAA does not apply, and you must release information to me?" While any given psychiatrist might choose not to release information on any given patient, I wonder if this might be setting us up to be at odds with families, and that would not be a good thing. Much as I’m no fan of HIPAA for many reasons, people do understand the concept that confidentiality is required by law. Perhaps I’m reading too much into this?
Finally, we all agree that eliminating stigma is a good thing when it comes to facilitating voluntary care for those who might need it. But I wonder if we can say that people with mental illnesses are just like everyone else, that this is a medical condition just like other conditions, but for this select group of people they lose their right to privacy, much as children have no right to medical privacy. Might that add to the stigma of mental illness?
I don’t have an answer. I believe the intentions of the Helping Families in Mental Health Crisis Act are good, and I believe they target weaknesses in our system. But I also worry that the legislation might create as many problems as it might fix.
The comments feature of the Clinical Psychiatry News website is turned off for the moment, and I would love to hear your thoughts. Please do e-mail with your comments; I can be reached at ShrinkRapBlog@gmail.com, or you may comment on a similar post here.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
Privacy or transparency: Maryland psychiatrists speculate on Medicare payments and their accessibility to the public
Despite protests from the American Medical Association, on Wednesday, April 9, the Obama administration made public payments to 880,000 Medicare providers. The data, released by the Centers for Medicare & Medicaid Services, include the clinician's name; specialty; address; and a breakdown of the number of patients who received each itemized service, the number of services rendered, the average amount billed per CPT code, and the average amount paid; along with the physician's total Medicare reimbursement for 2012. The data are easily accessible, and major newspapers have included look-up tools on their websites to allow for easy access to the data.
Through a discussion on the Maryland Psychiatric Society listserv, the opinions of several psychiatrists were solicited. From this, I learned that psychiatrists in my metro area have had mixed responses to the release of this information. Jesse Hellman, a psychiatrist in private practice in Towson, Md., notes: "This was a major privacy violation. Publishing the payments to individual physicians was a blunder. It should never have happened. Relevant data might have been released in another form."
Brian Crowley, a psychiatrist in practice in Washington, feels otherwise. "Personally, I'm in favor of the publication. It is of interest that most of the money goes to a few doctors, I believe, and may help planning. I believe the transparency is likely a good thing."
Roger Peele, a psychiatrist in Rockville, Md., agreed. "Even though misleading in some ways, and even though it might decrease the willingness of a few to be part of Medicare, it adds weight to the argument for a more rational payment system for physicians."
Robert Roca, vice president and medical director of Sheppard Pratt Health Systems added that he’d heard a journalist with expertise about this issue speaking on National Public Radio. "They don’t see this as a privacy issue. Their argument is that these are public dollars and that the public is entitled to know how and where they are spent. Unfortunately, the question of whether detailed information about payment of public dollars for other goods or services should be readily available to the public did not come up."
Steve Daviss, president of FUSE Health Strategies, had a lot to say about making the data public: "Put me in the 'transparency is good' camp. I see this less from a privacy of the doctor viewpoint, but rather from the perspectives of open government, and that this sort of data feedback mechanism is needed for proper homeostasis of our health care system.
"The U.S. spends twice as much per person on health care as any other country – double! – yet, we are not getting twice the health outcomes. When the CMS [Centers for Medicare & Medicaid Services] released this sort of data for hospitals, only then could we see the huge disparity in billing practices across the country. This sort of data about physicians will help demonstrate similar discrepancies, not just the 0.1% of physicians making millions on senior cataract surgery or whatever, but the shortages. There are many explanations for the odd data bits, which provide us a great opportunity to educate our patients and our policy makers.
"I don’t really see the danger," Dr. Daviss continued. "Where I do see the danger is in preventing people from understanding how much health care costs, where the money goes, and how to comparison shop. The next step (maybe it should have been the first) is to also share aggregate quality data, patient experience data, and comorbidity data. Then people will begin to connect the dots and have the information needed to make better health care decisions."
Laurie Orgel, a psychiatrist in private practice in Towson, countered, "I suppose we can look at this as a privacy issue, but there is the issue of relevance. What does it get anyone? Yes, there will be those of us who note the minority who get huge reimbursements, but I suspect that will just tarnish the rest of us rather than be understood as ‘a few outliers.’ Does this information really help planning?"
Kery Hummel, executive director of the Maryland Psychiatric Society, said, "I also wonder why some people have such considerable amounts and others such small amounts." He was quick to point out that the list included income earned for a psychiatrist, still listed at a Maryland address, who had moved out of state several years before.
Whether it's a violation of a doctor’s privacy to have the details of his practice and incomes easily accessible to the public, and whether this degree of transparency adds value when it comes to making health care more efficient with better outcomes, will be seen over time. In terms of capturing fraud, one might think that the CMS always had access to this data, and if it's an outlier for a physician to receive $21 million in Medicare dollars, then that should have been known without the need to make that information public. Notably, the data, even if completely correct, don’t tell the full picture of American health care dollars, as it doesn’t capture the practice habits of those who have opted out, or any transactions that are not provided through the Medicare program. The statistics, by definition, are skewed to reflect the practice habits of participating physicians who treat senior citizens and the disabled.
Finally, and as a bit of a humorous aside, having the data available does enable some interesting statistical analysis. One day after the data went public, Brian Reid published an article on the widely read medical blog KevinMD. In "Doctors who tweet aren’t ones who bill Medicare for millions," Mr. Reid said,"First, we created a list of doctors who appeared both in the dataset of Medicare providers and our MDigitalLife database of verified doctors in the United States with Twitter handles: 8,000 doctors who both used Twitter and received Medicare payments. We compared that group to the top 14,000 or so providers in the Medicare dataset (every single person who received $500,000 or more from the Medicare). There wasn't a lot of overlap. Only 230 docs made both the top-tweeter and the top-biller list. And among the real outliers – the top 1,000 recipients of Medicare dollars – only 13 were on Twitter, with a measly median follower count of 112. What’s more, there was an inverse association between Twitter followers and money received from Medicare."
Typically, I might end an article by asking readers to follow me on Twitter, but today I think I'll opt for a shot at higher reimbursement.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
Despite protests from the American Medical Association, on Wednesday, April 9, the Obama administration made public payments to 880,000 Medicare providers. The data, released by the Centers for Medicare & Medicaid Services, include the clinician's name; specialty; address; and a breakdown of the number of patients who received each itemized service, the number of services rendered, the average amount billed per CPT code, and the average amount paid; along with the physician's total Medicare reimbursement for 2012. The data are easily accessible, and major newspapers have included look-up tools on their websites to allow for easy access to the data.
Through a discussion on the Maryland Psychiatric Society listserv, the opinions of several psychiatrists were solicited. From this, I learned that psychiatrists in my metro area have had mixed responses to the release of this information. Jesse Hellman, a psychiatrist in private practice in Towson, Md., notes: "This was a major privacy violation. Publishing the payments to individual physicians was a blunder. It should never have happened. Relevant data might have been released in another form."
Brian Crowley, a psychiatrist in practice in Washington, feels otherwise. "Personally, I'm in favor of the publication. It is of interest that most of the money goes to a few doctors, I believe, and may help planning. I believe the transparency is likely a good thing."
Roger Peele, a psychiatrist in Rockville, Md., agreed. "Even though misleading in some ways, and even though it might decrease the willingness of a few to be part of Medicare, it adds weight to the argument for a more rational payment system for physicians."
Robert Roca, vice president and medical director of Sheppard Pratt Health Systems added that he’d heard a journalist with expertise about this issue speaking on National Public Radio. "They don’t see this as a privacy issue. Their argument is that these are public dollars and that the public is entitled to know how and where they are spent. Unfortunately, the question of whether detailed information about payment of public dollars for other goods or services should be readily available to the public did not come up."
Steve Daviss, president of FUSE Health Strategies, had a lot to say about making the data public: "Put me in the 'transparency is good' camp. I see this less from a privacy of the doctor viewpoint, but rather from the perspectives of open government, and that this sort of data feedback mechanism is needed for proper homeostasis of our health care system.
"The U.S. spends twice as much per person on health care as any other country – double! – yet, we are not getting twice the health outcomes. When the CMS [Centers for Medicare & Medicaid Services] released this sort of data for hospitals, only then could we see the huge disparity in billing practices across the country. This sort of data about physicians will help demonstrate similar discrepancies, not just the 0.1% of physicians making millions on senior cataract surgery or whatever, but the shortages. There are many explanations for the odd data bits, which provide us a great opportunity to educate our patients and our policy makers.
"I don’t really see the danger," Dr. Daviss continued. "Where I do see the danger is in preventing people from understanding how much health care costs, where the money goes, and how to comparison shop. The next step (maybe it should have been the first) is to also share aggregate quality data, patient experience data, and comorbidity data. Then people will begin to connect the dots and have the information needed to make better health care decisions."
Laurie Orgel, a psychiatrist in private practice in Towson, countered, "I suppose we can look at this as a privacy issue, but there is the issue of relevance. What does it get anyone? Yes, there will be those of us who note the minority who get huge reimbursements, but I suspect that will just tarnish the rest of us rather than be understood as ‘a few outliers.’ Does this information really help planning?"
Kery Hummel, executive director of the Maryland Psychiatric Society, said, "I also wonder why some people have such considerable amounts and others such small amounts." He was quick to point out that the list included income earned for a psychiatrist, still listed at a Maryland address, who had moved out of state several years before.
Whether it's a violation of a doctor’s privacy to have the details of his practice and incomes easily accessible to the public, and whether this degree of transparency adds value when it comes to making health care more efficient with better outcomes, will be seen over time. In terms of capturing fraud, one might think that the CMS always had access to this data, and if it's an outlier for a physician to receive $21 million in Medicare dollars, then that should have been known without the need to make that information public. Notably, the data, even if completely correct, don’t tell the full picture of American health care dollars, as it doesn’t capture the practice habits of those who have opted out, or any transactions that are not provided through the Medicare program. The statistics, by definition, are skewed to reflect the practice habits of participating physicians who treat senior citizens and the disabled.
Finally, and as a bit of a humorous aside, having the data available does enable some interesting statistical analysis. One day after the data went public, Brian Reid published an article on the widely read medical blog KevinMD. In "Doctors who tweet aren’t ones who bill Medicare for millions," Mr. Reid said,"First, we created a list of doctors who appeared both in the dataset of Medicare providers and our MDigitalLife database of verified doctors in the United States with Twitter handles: 8,000 doctors who both used Twitter and received Medicare payments. We compared that group to the top 14,000 or so providers in the Medicare dataset (every single person who received $500,000 or more from the Medicare). There wasn't a lot of overlap. Only 230 docs made both the top-tweeter and the top-biller list. And among the real outliers – the top 1,000 recipients of Medicare dollars – only 13 were on Twitter, with a measly median follower count of 112. What’s more, there was an inverse association between Twitter followers and money received from Medicare."
Typically, I might end an article by asking readers to follow me on Twitter, but today I think I'll opt for a shot at higher reimbursement.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
Despite protests from the American Medical Association, on Wednesday, April 9, the Obama administration made public payments to 880,000 Medicare providers. The data, released by the Centers for Medicare & Medicaid Services, include the clinician's name; specialty; address; and a breakdown of the number of patients who received each itemized service, the number of services rendered, the average amount billed per CPT code, and the average amount paid; along with the physician's total Medicare reimbursement for 2012. The data are easily accessible, and major newspapers have included look-up tools on their websites to allow for easy access to the data.
Through a discussion on the Maryland Psychiatric Society listserv, the opinions of several psychiatrists were solicited. From this, I learned that psychiatrists in my metro area have had mixed responses to the release of this information. Jesse Hellman, a psychiatrist in private practice in Towson, Md., notes: "This was a major privacy violation. Publishing the payments to individual physicians was a blunder. It should never have happened. Relevant data might have been released in another form."
Brian Crowley, a psychiatrist in practice in Washington, feels otherwise. "Personally, I'm in favor of the publication. It is of interest that most of the money goes to a few doctors, I believe, and may help planning. I believe the transparency is likely a good thing."
Roger Peele, a psychiatrist in Rockville, Md., agreed. "Even though misleading in some ways, and even though it might decrease the willingness of a few to be part of Medicare, it adds weight to the argument for a more rational payment system for physicians."
Robert Roca, vice president and medical director of Sheppard Pratt Health Systems added that he’d heard a journalist with expertise about this issue speaking on National Public Radio. "They don’t see this as a privacy issue. Their argument is that these are public dollars and that the public is entitled to know how and where they are spent. Unfortunately, the question of whether detailed information about payment of public dollars for other goods or services should be readily available to the public did not come up."
Steve Daviss, president of FUSE Health Strategies, had a lot to say about making the data public: "Put me in the 'transparency is good' camp. I see this less from a privacy of the doctor viewpoint, but rather from the perspectives of open government, and that this sort of data feedback mechanism is needed for proper homeostasis of our health care system.
"The U.S. spends twice as much per person on health care as any other country – double! – yet, we are not getting twice the health outcomes. When the CMS [Centers for Medicare & Medicaid Services] released this sort of data for hospitals, only then could we see the huge disparity in billing practices across the country. This sort of data about physicians will help demonstrate similar discrepancies, not just the 0.1% of physicians making millions on senior cataract surgery or whatever, but the shortages. There are many explanations for the odd data bits, which provide us a great opportunity to educate our patients and our policy makers.
"I don’t really see the danger," Dr. Daviss continued. "Where I do see the danger is in preventing people from understanding how much health care costs, where the money goes, and how to comparison shop. The next step (maybe it should have been the first) is to also share aggregate quality data, patient experience data, and comorbidity data. Then people will begin to connect the dots and have the information needed to make better health care decisions."
Laurie Orgel, a psychiatrist in private practice in Towson, countered, "I suppose we can look at this as a privacy issue, but there is the issue of relevance. What does it get anyone? Yes, there will be those of us who note the minority who get huge reimbursements, but I suspect that will just tarnish the rest of us rather than be understood as ‘a few outliers.’ Does this information really help planning?"
Kery Hummel, executive director of the Maryland Psychiatric Society, said, "I also wonder why some people have such considerable amounts and others such small amounts." He was quick to point out that the list included income earned for a psychiatrist, still listed at a Maryland address, who had moved out of state several years before.
Whether it's a violation of a doctor’s privacy to have the details of his practice and incomes easily accessible to the public, and whether this degree of transparency adds value when it comes to making health care more efficient with better outcomes, will be seen over time. In terms of capturing fraud, one might think that the CMS always had access to this data, and if it's an outlier for a physician to receive $21 million in Medicare dollars, then that should have been known without the need to make that information public. Notably, the data, even if completely correct, don’t tell the full picture of American health care dollars, as it doesn’t capture the practice habits of those who have opted out, or any transactions that are not provided through the Medicare program. The statistics, by definition, are skewed to reflect the practice habits of participating physicians who treat senior citizens and the disabled.
Finally, and as a bit of a humorous aside, having the data available does enable some interesting statistical analysis. One day after the data went public, Brian Reid published an article on the widely read medical blog KevinMD. In "Doctors who tweet aren’t ones who bill Medicare for millions," Mr. Reid said,"First, we created a list of doctors who appeared both in the dataset of Medicare providers and our MDigitalLife database of verified doctors in the United States with Twitter handles: 8,000 doctors who both used Twitter and received Medicare payments. We compared that group to the top 14,000 or so providers in the Medicare dataset (every single person who received $500,000 or more from the Medicare). There wasn't a lot of overlap. Only 230 docs made both the top-tweeter and the top-biller list. And among the real outliers – the top 1,000 recipients of Medicare dollars – only 13 were on Twitter, with a measly median follower count of 112. What’s more, there was an inverse association between Twitter followers and money received from Medicare."
Typically, I might end an article by asking readers to follow me on Twitter, but today I think I'll opt for a shot at higher reimbursement.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
Legislating kindness
Late in February, I drove to Annapolis, Md., to listen to testimony being given to our state’s Senate Finance Committee on a number of proposed bills relating to involuntary treatments. But this article is not going to be about those bills or the fuss that played out around them, but rather about what happened when I arrived a bit early and heard testimony on another piece of legislation that had nothing to do with psychiatry and everything to do with being human.
Ten bills were scheduled for public testimony that afternoon, and I arrived shortly after 1 p.m. to a hearing room in which there was standing room only. There are 11 members of the Senate Finance Committee; 10 were present, and I’m going to guess there were more than100 people in the room waiting to testify. The only other time I had gone to listen to public testimony was last year for Gov. Martin O’Malley’s Firearm Safety Act, and for that piece of legislation, 1,300 people were there to testify, the large majority of them being Second Amendment activists who were there to oppose the bill.
The legislation in question (the one I did not come to hear about) was Senate Bill 654. The description of that bill reads:
"This bill requires the Department of Health and Mental Hygiene to identify up-to-date, evidence-based, written information about Down syndrome. This information must be provided to health care facilities and providers, who must provide the information to expectant parents who receive a prenatal test result for Down syndrome and parents of a child diagnosed with Down syndrome."
My first thought was this is a standard of care issue, something to be addressed by the specialties involved, not something that should be the subject of legislation. We don’t really want to have condition-specific laws mandating what physicians must tell their patients, do we? Where would it stop: Would legislation be written for every disorder? Shouldn’t the clinician who knows the family determine what information is best for each individual and with what timing? Never mind the nuance of figuring out exactly what is "up to date" and what is not. And it’s not as though the parents couldn’t search for the information themselves – certainly there must be resources online.
Then the testimony began. There were women whose children had been diagnosed, generally in utero, before the time when one could Google the condition and search for available resources. They told stories of asking for resources, only to be told that their clinicians didn’t know of any. And they told stories of being counseled to abort after they wanted to continue with the pregnancy. They discussed how shocked and alone they felt, and how insensitive the care they received was. In addition, they talked about the value their children added to the world. And then the adult children with Down syndrome also testified. In a way, I felt like it was testimony for the rights of these people to be here, more so perhaps than testimony to require clinicians to give out the appropriate pamphlets.
Representatives from MedChi (the Maryland State Medical Society) and the Department of Health and Mental Hygiene also testified. While neither was opposed to the creation of lists and websites of resources and educational information, they did object to the mandate that the clinician must give the information at a specific time. What if the clinician felt it was not in that patient’s best interest to distribute the information to a specific patient or at a specific time? Perhaps it wasn’t there, but I heard the unspoken concern that the clinician might be subject to sanctions or accusations of malpractice if they neglected to distribute the information as required by law if the legislation passed. The Down syndrome information supporters said they had already gone office to office to provide pamphlets and information to clinicians, which were then placed in a drawer and not distributed. They objected to language that would change "must" to "may" with the idea that it wasn’t strong enough to move clinicians to action.
Another bill also caught my attention this year, although I was not present for any public testimony. Delegate Robert A. Costa proposed House Bill 279, legislation that would forbid a physician from charging or filing an insurance claim for any appointment that began more than 30 minutes from the scheduled time. The legislation did allow for an exclusion for emergencies, if the doctor presented an "emergency services verification number" to the patient, but it did not take into account that an appointment might start late because the patient was late!
Regardless of whether the legislation proposed by these two bills makes sense as something for lawmakers to address, and regardless of how practical they are in terms of both their intended and unintended consequences, the message of such legislation is clear: They represent distress at insensitive care and an attempt to legislate kindness. The message comes through that clinicians can’t be trusted to do what’s right, and laws must be passed to make sure they practice in a thoughtful and considerate manner. It would be nice to have some reasonable conclusion about how to rectify these situations without having legislators tell medical professionals how to practice. I don’t have an answer here, but I believe that passing more laws will create its own negative fallout, and we need to find a better route to kindness.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
Late in February, I drove to Annapolis, Md., to listen to testimony being given to our state’s Senate Finance Committee on a number of proposed bills relating to involuntary treatments. But this article is not going to be about those bills or the fuss that played out around them, but rather about what happened when I arrived a bit early and heard testimony on another piece of legislation that had nothing to do with psychiatry and everything to do with being human.
Ten bills were scheduled for public testimony that afternoon, and I arrived shortly after 1 p.m. to a hearing room in which there was standing room only. There are 11 members of the Senate Finance Committee; 10 were present, and I’m going to guess there were more than100 people in the room waiting to testify. The only other time I had gone to listen to public testimony was last year for Gov. Martin O’Malley’s Firearm Safety Act, and for that piece of legislation, 1,300 people were there to testify, the large majority of them being Second Amendment activists who were there to oppose the bill.
The legislation in question (the one I did not come to hear about) was Senate Bill 654. The description of that bill reads:
"This bill requires the Department of Health and Mental Hygiene to identify up-to-date, evidence-based, written information about Down syndrome. This information must be provided to health care facilities and providers, who must provide the information to expectant parents who receive a prenatal test result for Down syndrome and parents of a child diagnosed with Down syndrome."
My first thought was this is a standard of care issue, something to be addressed by the specialties involved, not something that should be the subject of legislation. We don’t really want to have condition-specific laws mandating what physicians must tell their patients, do we? Where would it stop: Would legislation be written for every disorder? Shouldn’t the clinician who knows the family determine what information is best for each individual and with what timing? Never mind the nuance of figuring out exactly what is "up to date" and what is not. And it’s not as though the parents couldn’t search for the information themselves – certainly there must be resources online.
Then the testimony began. There were women whose children had been diagnosed, generally in utero, before the time when one could Google the condition and search for available resources. They told stories of asking for resources, only to be told that their clinicians didn’t know of any. And they told stories of being counseled to abort after they wanted to continue with the pregnancy. They discussed how shocked and alone they felt, and how insensitive the care they received was. In addition, they talked about the value their children added to the world. And then the adult children with Down syndrome also testified. In a way, I felt like it was testimony for the rights of these people to be here, more so perhaps than testimony to require clinicians to give out the appropriate pamphlets.
Representatives from MedChi (the Maryland State Medical Society) and the Department of Health and Mental Hygiene also testified. While neither was opposed to the creation of lists and websites of resources and educational information, they did object to the mandate that the clinician must give the information at a specific time. What if the clinician felt it was not in that patient’s best interest to distribute the information to a specific patient or at a specific time? Perhaps it wasn’t there, but I heard the unspoken concern that the clinician might be subject to sanctions or accusations of malpractice if they neglected to distribute the information as required by law if the legislation passed. The Down syndrome information supporters said they had already gone office to office to provide pamphlets and information to clinicians, which were then placed in a drawer and not distributed. They objected to language that would change "must" to "may" with the idea that it wasn’t strong enough to move clinicians to action.
Another bill also caught my attention this year, although I was not present for any public testimony. Delegate Robert A. Costa proposed House Bill 279, legislation that would forbid a physician from charging or filing an insurance claim for any appointment that began more than 30 minutes from the scheduled time. The legislation did allow for an exclusion for emergencies, if the doctor presented an "emergency services verification number" to the patient, but it did not take into account that an appointment might start late because the patient was late!
Regardless of whether the legislation proposed by these two bills makes sense as something for lawmakers to address, and regardless of how practical they are in terms of both their intended and unintended consequences, the message of such legislation is clear: They represent distress at insensitive care and an attempt to legislate kindness. The message comes through that clinicians can’t be trusted to do what’s right, and laws must be passed to make sure they practice in a thoughtful and considerate manner. It would be nice to have some reasonable conclusion about how to rectify these situations without having legislators tell medical professionals how to practice. I don’t have an answer here, but I believe that passing more laws will create its own negative fallout, and we need to find a better route to kindness.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).
Late in February, I drove to Annapolis, Md., to listen to testimony being given to our state’s Senate Finance Committee on a number of proposed bills relating to involuntary treatments. But this article is not going to be about those bills or the fuss that played out around them, but rather about what happened when I arrived a bit early and heard testimony on another piece of legislation that had nothing to do with psychiatry and everything to do with being human.
Ten bills were scheduled for public testimony that afternoon, and I arrived shortly after 1 p.m. to a hearing room in which there was standing room only. There are 11 members of the Senate Finance Committee; 10 were present, and I’m going to guess there were more than100 people in the room waiting to testify. The only other time I had gone to listen to public testimony was last year for Gov. Martin O’Malley’s Firearm Safety Act, and for that piece of legislation, 1,300 people were there to testify, the large majority of them being Second Amendment activists who were there to oppose the bill.
The legislation in question (the one I did not come to hear about) was Senate Bill 654. The description of that bill reads:
"This bill requires the Department of Health and Mental Hygiene to identify up-to-date, evidence-based, written information about Down syndrome. This information must be provided to health care facilities and providers, who must provide the information to expectant parents who receive a prenatal test result for Down syndrome and parents of a child diagnosed with Down syndrome."
My first thought was this is a standard of care issue, something to be addressed by the specialties involved, not something that should be the subject of legislation. We don’t really want to have condition-specific laws mandating what physicians must tell their patients, do we? Where would it stop: Would legislation be written for every disorder? Shouldn’t the clinician who knows the family determine what information is best for each individual and with what timing? Never mind the nuance of figuring out exactly what is "up to date" and what is not. And it’s not as though the parents couldn’t search for the information themselves – certainly there must be resources online.
Then the testimony began. There were women whose children had been diagnosed, generally in utero, before the time when one could Google the condition and search for available resources. They told stories of asking for resources, only to be told that their clinicians didn’t know of any. And they told stories of being counseled to abort after they wanted to continue with the pregnancy. They discussed how shocked and alone they felt, and how insensitive the care they received was. In addition, they talked about the value their children added to the world. And then the adult children with Down syndrome also testified. In a way, I felt like it was testimony for the rights of these people to be here, more so perhaps than testimony to require clinicians to give out the appropriate pamphlets.
Representatives from MedChi (the Maryland State Medical Society) and the Department of Health and Mental Hygiene also testified. While neither was opposed to the creation of lists and websites of resources and educational information, they did object to the mandate that the clinician must give the information at a specific time. What if the clinician felt it was not in that patient’s best interest to distribute the information to a specific patient or at a specific time? Perhaps it wasn’t there, but I heard the unspoken concern that the clinician might be subject to sanctions or accusations of malpractice if they neglected to distribute the information as required by law if the legislation passed. The Down syndrome information supporters said they had already gone office to office to provide pamphlets and information to clinicians, which were then placed in a drawer and not distributed. They objected to language that would change "must" to "may" with the idea that it wasn’t strong enough to move clinicians to action.
Another bill also caught my attention this year, although I was not present for any public testimony. Delegate Robert A. Costa proposed House Bill 279, legislation that would forbid a physician from charging or filing an insurance claim for any appointment that began more than 30 minutes from the scheduled time. The legislation did allow for an exclusion for emergencies, if the doctor presented an "emergency services verification number" to the patient, but it did not take into account that an appointment might start late because the patient was late!
Regardless of whether the legislation proposed by these two bills makes sense as something for lawmakers to address, and regardless of how practical they are in terms of both their intended and unintended consequences, the message of such legislation is clear: They represent distress at insensitive care and an attempt to legislate kindness. The message comes through that clinicians can’t be trusted to do what’s right, and laws must be passed to make sure they practice in a thoughtful and considerate manner. It would be nice to have some reasonable conclusion about how to rectify these situations without having legislators tell medical professionals how to practice. I don’t have an answer here, but I believe that passing more laws will create its own negative fallout, and we need to find a better route to kindness.
Dr. Miller is a coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: the Johns Hopkins University Press, 2011).