User login
Psoriasis Patients Still Going Unscreened for Heart Disease
BOSTON – Despite the growing body of literature linking psoriasis to poor cardiovascular outcomes, most psoriasis patients are not being regularly screened for the major CV risk factors, according to the results of a new analysis.
"Screening for high blood pressure, diabetes, hypercholesterolemia, and obesity are not performed at most outpatient visits for psoriasis," wrote clinical research fellow Amir Al-Dabagh and colleagues at the center for dermatology research at Wake Forest University, Winston-Salem, N.C.
To determine whether and to what degree CV screening is taking place during outpatient psoriasis visits in the ambulatory care setting, the investigators reviewed data from the NAMCS (National Ambulatory Medical Care Survey) from 2005 to 2009. They calculated the probability of a patient’s being screened for at least one of four CV risk factors (blood pressure, glucose, cholesterol, and body mass index). They also compared screening rates by physician specialty, patient demographics, and clinical practice characteristics.
Approximately 11.4 million psoriasis patient visits were recorded during the study period. Age was found to be the only demographic factor that was significantly associated with all CV risk screens, Mr. Al-Dabagh reported in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting. "Psoriasis had a statistically significant negative association on overall screening rates for blood pressure and BMI screening, but not for glucose or cholesterol."
A comparison of screening rates among patients with and without psoriasis showed that only 41.2% of the psoriasis patients were screened for at least one of the four risk factors, compared with 66.3% of patients without psoriasis. When looking at psoriasis patients only, the researchers found that screening for each of the risk factors occurred more frequently during nondermatology vs. dermatology visits, regardless of disease severity.
Specifically, among patients with severe and nonsevere psoriasis, respectively, 100% and 89.9% of psoriasis visits to nondermatology offices included screening for at least one risk factor, compared with 28.9% and 12.3% of psoriasis visits to dermatology offices, according to the analysis. In both settings, screening rates were higher among male patients, as well as among black and non-Hispanic patients, Mr. Al-Dabagh noted.
The majority of nondermatologist visits for patients with severe and nonsevere psoriasis included screening for blood pressure (100% for severe; 87.9% for not severe) and BMI (88.3% for severe; 54.4% for not severe). By comparison, during dermatology visits, 3.8% of patients with severe disease and 2.4% of those with mild to moderate disease had blood pressure screens, and 14.8% and 8.5%, respectively, had BMI recorded. Relatively few visits in either setting included glucose or cholesterol measurement, regardless of disease severity.
In 2008, the National Psoriasis Foundation issued a clinical consensus report recommending that screening psoriasis patients for cardiovascular risk factors begin as early as 20 years of age. The recommendation was based on mounting evidence from population-based studies that found psoriasis to be a risk factor for developing atherosclerosis and myocardial infarction (J. Amer. Acad. Derm. 2008;58:1031-42).
In addition to early, routine screening, psoriasis patients should be counseled to modify cholesterol levels when necessary, to take measures to control depression, to quit smoking, to moderate their alcohol intake, to eat a healthy diet, and to exercise at least three times a week, according to the consensus report.
The center for dermatology research at Wake Forest University is supported by an educational grant from Galderma. The study investigators reported financial relationships with multiple pharmaceutical companies, including Galderma.
BOSTON – Despite the growing body of literature linking psoriasis to poor cardiovascular outcomes, most psoriasis patients are not being regularly screened for the major CV risk factors, according to the results of a new analysis.
"Screening for high blood pressure, diabetes, hypercholesterolemia, and obesity are not performed at most outpatient visits for psoriasis," wrote clinical research fellow Amir Al-Dabagh and colleagues at the center for dermatology research at Wake Forest University, Winston-Salem, N.C.
To determine whether and to what degree CV screening is taking place during outpatient psoriasis visits in the ambulatory care setting, the investigators reviewed data from the NAMCS (National Ambulatory Medical Care Survey) from 2005 to 2009. They calculated the probability of a patient’s being screened for at least one of four CV risk factors (blood pressure, glucose, cholesterol, and body mass index). They also compared screening rates by physician specialty, patient demographics, and clinical practice characteristics.
Approximately 11.4 million psoriasis patient visits were recorded during the study period. Age was found to be the only demographic factor that was significantly associated with all CV risk screens, Mr. Al-Dabagh reported in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting. "Psoriasis had a statistically significant negative association on overall screening rates for blood pressure and BMI screening, but not for glucose or cholesterol."
A comparison of screening rates among patients with and without psoriasis showed that only 41.2% of the psoriasis patients were screened for at least one of the four risk factors, compared with 66.3% of patients without psoriasis. When looking at psoriasis patients only, the researchers found that screening for each of the risk factors occurred more frequently during nondermatology vs. dermatology visits, regardless of disease severity.
Specifically, among patients with severe and nonsevere psoriasis, respectively, 100% and 89.9% of psoriasis visits to nondermatology offices included screening for at least one risk factor, compared with 28.9% and 12.3% of psoriasis visits to dermatology offices, according to the analysis. In both settings, screening rates were higher among male patients, as well as among black and non-Hispanic patients, Mr. Al-Dabagh noted.
The majority of nondermatologist visits for patients with severe and nonsevere psoriasis included screening for blood pressure (100% for severe; 87.9% for not severe) and BMI (88.3% for severe; 54.4% for not severe). By comparison, during dermatology visits, 3.8% of patients with severe disease and 2.4% of those with mild to moderate disease had blood pressure screens, and 14.8% and 8.5%, respectively, had BMI recorded. Relatively few visits in either setting included glucose or cholesterol measurement, regardless of disease severity.
In 2008, the National Psoriasis Foundation issued a clinical consensus report recommending that screening psoriasis patients for cardiovascular risk factors begin as early as 20 years of age. The recommendation was based on mounting evidence from population-based studies that found psoriasis to be a risk factor for developing atherosclerosis and myocardial infarction (J. Amer. Acad. Derm. 2008;58:1031-42).
In addition to early, routine screening, psoriasis patients should be counseled to modify cholesterol levels when necessary, to take measures to control depression, to quit smoking, to moderate their alcohol intake, to eat a healthy diet, and to exercise at least three times a week, according to the consensus report.
The center for dermatology research at Wake Forest University is supported by an educational grant from Galderma. The study investigators reported financial relationships with multiple pharmaceutical companies, including Galderma.
BOSTON – Despite the growing body of literature linking psoriasis to poor cardiovascular outcomes, most psoriasis patients are not being regularly screened for the major CV risk factors, according to the results of a new analysis.
"Screening for high blood pressure, diabetes, hypercholesterolemia, and obesity are not performed at most outpatient visits for psoriasis," wrote clinical research fellow Amir Al-Dabagh and colleagues at the center for dermatology research at Wake Forest University, Winston-Salem, N.C.
To determine whether and to what degree CV screening is taking place during outpatient psoriasis visits in the ambulatory care setting, the investigators reviewed data from the NAMCS (National Ambulatory Medical Care Survey) from 2005 to 2009. They calculated the probability of a patient’s being screened for at least one of four CV risk factors (blood pressure, glucose, cholesterol, and body mass index). They also compared screening rates by physician specialty, patient demographics, and clinical practice characteristics.
Approximately 11.4 million psoriasis patient visits were recorded during the study period. Age was found to be the only demographic factor that was significantly associated with all CV risk screens, Mr. Al-Dabagh reported in a poster presented at the American Academy of Dermatology’s Summer Academy Meeting. "Psoriasis had a statistically significant negative association on overall screening rates for blood pressure and BMI screening, but not for glucose or cholesterol."
A comparison of screening rates among patients with and without psoriasis showed that only 41.2% of the psoriasis patients were screened for at least one of the four risk factors, compared with 66.3% of patients without psoriasis. When looking at psoriasis patients only, the researchers found that screening for each of the risk factors occurred more frequently during nondermatology vs. dermatology visits, regardless of disease severity.
Specifically, among patients with severe and nonsevere psoriasis, respectively, 100% and 89.9% of psoriasis visits to nondermatology offices included screening for at least one risk factor, compared with 28.9% and 12.3% of psoriasis visits to dermatology offices, according to the analysis. In both settings, screening rates were higher among male patients, as well as among black and non-Hispanic patients, Mr. Al-Dabagh noted.
The majority of nondermatologist visits for patients with severe and nonsevere psoriasis included screening for blood pressure (100% for severe; 87.9% for not severe) and BMI (88.3% for severe; 54.4% for not severe). By comparison, during dermatology visits, 3.8% of patients with severe disease and 2.4% of those with mild to moderate disease had blood pressure screens, and 14.8% and 8.5%, respectively, had BMI recorded. Relatively few visits in either setting included glucose or cholesterol measurement, regardless of disease severity.
In 2008, the National Psoriasis Foundation issued a clinical consensus report recommending that screening psoriasis patients for cardiovascular risk factors begin as early as 20 years of age. The recommendation was based on mounting evidence from population-based studies that found psoriasis to be a risk factor for developing atherosclerosis and myocardial infarction (J. Amer. Acad. Derm. 2008;58:1031-42).
In addition to early, routine screening, psoriasis patients should be counseled to modify cholesterol levels when necessary, to take measures to control depression, to quit smoking, to moderate their alcohol intake, to eat a healthy diet, and to exercise at least three times a week, according to the consensus report.
The center for dermatology research at Wake Forest University is supported by an educational grant from Galderma. The study investigators reported financial relationships with multiple pharmaceutical companies, including Galderma.
AT THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
Major Finding: Approximately 41% of psoriasis patients were screened for at least one of four risk factors for cardiovascular disease during outpatient visits, compared with 66.3% of patients without the chronic inflammatory disease.
Data Source: Analysis of data from the National Ambulatory Medical Care Survey on outpatient psoriasis visits from 2005-2009.
Disclosures: The Center for Dermatology Research at Wake Forest University is supported by an educational grant from Galderma. The study investigators reported financial relationships with multiple pharmaceutical companies, including Galderma.
Intermittent Androgen Suppression 'Noninferior' to Continuous in Prostate Cancer
Intermittent androgen deprivation was not associated with inferior survival for men with a rising prostate-specific antigen level after definitive radiotherapy in a study reported in the Sept. 6 issue of the New England Journal of Medicine.
The findings from the phase III National Cancer Institute of Canada (NCIC) Clinical Trials Group study appear to conflict with those of another international phase III clinical trial reported in June at the annual meeting of the American Society of Clinical Oncology, and as such may fuel rather than extinguish the longstanding debate regarding the proper use and timing of endocrine therapy with androgen antagonists.
In the NCIC trial, 696 of 1,386 men with a PSA level greater than 3 ng/mL more than 1 year after primary or salvage radiotherapy for localized prostate cancer were randomized to continuous androgen suppression therapy consisting of a luteinizing hormone–releasing hormone agonist (LHRHa), combined with a minimum of 4 weeks of a nonsteroidal antiandrogen, or orchiectomy.
Another 690 men were randomized to intermittent androgen deprivation in 8-month cycles, with periods of nontreatment determined by PSA level. Each treatment cycle for the latter group began with the administration of LHRHa injections combined with a nonsteroidal antiandrogen for a minimum of 4 weeks and ended after 8 months if there was no evidence of clinical disease progression and if the patient’s PSA level was less than 4 ng/mL and not more than 1 ng/mL above the previous recorded value.
"During the treatment interval, the PSA level was monitored every 2 months until it reached 10 ng/mL, provided there was no intervening evidence of disease progression," stated lead investigator Dr. Juanita M. Crook of the British Columbia Cancer Agency, Kelowna, and her colleagues. (N. Engl. J. Med. 2012;367:895-903).
Overall survival was the primary end point of the study, and time to castration-resistant disease and quality of life were secondary end points, the authors wrote. Duration of off-treatment intervals, time to testosterone recovery, and time to potency recovery were additional end points for patients randomized to intermittent therapy.
At a median follow-up of 6.9 years, 524 patients had died, including 268 in the intermittent group and 256 in the continuous group, the authors reported. Median overall survival in both arms was statistically similar, at 8.8 years in the intermittent group and 9.1 years in the continuous therapy group.
"The hazard ratio for death with intermittent therapy versus continuous therapy was 1.02," the authors wrote, and the P value for noninferiority, at.009, supported the investigators’ initial hypothesis that intermittent therapy was not inferior to continuous therapy. A nonsignificant increase in deaths from other causes was observed in the continuous therapy group.
Because most of the deaths (59%) were unrelated to prostate cancer, the investigators retrospectively analyzed disease-specific survival "to determine whether a significant difference in treatment effect was obscured by the data on deaths from causes other than prostate cancer," they said. The estimated disease-specific hazard ratio after adjustment for stratification and confounding factors was 1.23, and the estimated 7-year cumulative disease-related death rates were 18% and 15%, respectively, for the intermittent and continuous groups.
With respect to time to castration-resistant disease, based on a Cox regression analysis adjusted for stratification and prognostic factors, the estimated hazard ratio for intermittent versus continuous therapy was 0.81, the authors reported, noting, however, that the study design contributed to a bias "by an unknown magnitude" against continuous androgen-deprivation therapy.
"For patients in the intermittent-therapy group, there was an inherent delay in the identification of castration-resistant disease, because treatment had to be restarted in these patients and they had to have a ‘castrate-range’ testosterone level and an additional three increases in the PSA level before being classified as having castration-resistant disease," the investigators wrote.
In quality of life measures, the intermittent therapy group had nonsignificantly better scores for functional domains (physical, role, and global health) and significantly better scores for symptoms, including hot flashes, desire for sexual activity, and urinary symptoms, the authors reported. Full testosterone recovery in the intermittent group occurred in 35% of the patients, while recovery to the trial entry threshold occurred in 79%, they said.
The authors concluded that their trial "raises provocative questions" and cautioned that their results "cannot be extrapolated to other intermittent-treatment schedules or disease characteristics."
The article did not address the apparent contradiction between the NCIC trial results and the findings of the Southwest Oncology Group (SWOG) 9346 trial reported earlier in the year at the ASCO annual meeting.
The latter trial randomized 3,040 patients with newly diagnosed hormone-sensitive metastatic prostate cancer with a PSA level of at least 5 ng/mL before androgen deprivation and a SWOG performance status of 0-2 to intermittent or continuous therapy. The investigators reported a 9% increase in the relative risk of death associated with intermittent therapy, which did not meet the prespecified criteria for noninferiority.
A secondary analysis of the SWOG 9346 data suggested that intermittent therapy was noninferior to continuous in patients with extensive disease but not minimal disease.
"The two studies targeted different populations," Dr. Crook said in an interview. "There are also some important differences in the way the results were handled in the statistical analysis. The results of the SWOG study are equivocal regarding survival."
"Our study has shown that men with only PSA evidence of recurrent prostate cancer and no evidence of metastatic disease can safely be treated with this intermittent program of androgen suppression to gain quality of life benefits without sacrificing length of life," she added.
"Our study did not address the optimal time to begin androgen ablation, or specifically how long intervention can be safely postponed."
The NCIC trial was supported by grants from the Canadian Cancer Society, the U.S. National Cancer Institute, and Hoeschst Marion Roussel Canada Research. Dr. Crook disclosed no relevant financial conflicts. Study coinvestigators disclosed financial relationships with numerous companies.
*This story was updated 9/6/2012.
In an accompanying editorial, Dr Oliver Sartor called the study by Dr. Crook and her colleagues "the most definitive study to date comparing intermittent versus continuous androgen-deprivation therapy in patients with nonmetastatic cancer."
He noted, however, that an important question remains unanswered: "It is still unclear which men with rising PSA levels needed treatment. This is a heterogeneous patient group, and only a minority of men might be expected to have clinical consequences from their rise in PSA level."
Considering the slow progression of prostate cancer in men, "which of these asymptomatic patients actually benefited from androgen-deprivation therapy?" he asked (N. Engl. J. Med. 2012;367:945-6).
Dr. Sartor is medical director of the Tulane Cancer Center and the C.E. and Bernadine Laborde Professor of Cancer Research at Tulane University, New Orleans He disclosed a financial relationship with Tolmar.
In an accompanying editorial, Dr Oliver Sartor called the study by Dr. Crook and her colleagues "the most definitive study to date comparing intermittent versus continuous androgen-deprivation therapy in patients with nonmetastatic cancer."
He noted, however, that an important question remains unanswered: "It is still unclear which men with rising PSA levels needed treatment. This is a heterogeneous patient group, and only a minority of men might be expected to have clinical consequences from their rise in PSA level."
Considering the slow progression of prostate cancer in men, "which of these asymptomatic patients actually benefited from androgen-deprivation therapy?" he asked (N. Engl. J. Med. 2012;367:945-6).
Dr. Sartor is medical director of the Tulane Cancer Center and the C.E. and Bernadine Laborde Professor of Cancer Research at Tulane University, New Orleans He disclosed a financial relationship with Tolmar.
In an accompanying editorial, Dr Oliver Sartor called the study by Dr. Crook and her colleagues "the most definitive study to date comparing intermittent versus continuous androgen-deprivation therapy in patients with nonmetastatic cancer."
He noted, however, that an important question remains unanswered: "It is still unclear which men with rising PSA levels needed treatment. This is a heterogeneous patient group, and only a minority of men might be expected to have clinical consequences from their rise in PSA level."
Considering the slow progression of prostate cancer in men, "which of these asymptomatic patients actually benefited from androgen-deprivation therapy?" he asked (N. Engl. J. Med. 2012;367:945-6).
Dr. Sartor is medical director of the Tulane Cancer Center and the C.E. and Bernadine Laborde Professor of Cancer Research at Tulane University, New Orleans He disclosed a financial relationship with Tolmar.
Intermittent androgen deprivation was not associated with inferior survival for men with a rising prostate-specific antigen level after definitive radiotherapy in a study reported in the Sept. 6 issue of the New England Journal of Medicine.
The findings from the phase III National Cancer Institute of Canada (NCIC) Clinical Trials Group study appear to conflict with those of another international phase III clinical trial reported in June at the annual meeting of the American Society of Clinical Oncology, and as such may fuel rather than extinguish the longstanding debate regarding the proper use and timing of endocrine therapy with androgen antagonists.
In the NCIC trial, 696 of 1,386 men with a PSA level greater than 3 ng/mL more than 1 year after primary or salvage radiotherapy for localized prostate cancer were randomized to continuous androgen suppression therapy consisting of a luteinizing hormone–releasing hormone agonist (LHRHa), combined with a minimum of 4 weeks of a nonsteroidal antiandrogen, or orchiectomy.
Another 690 men were randomized to intermittent androgen deprivation in 8-month cycles, with periods of nontreatment determined by PSA level. Each treatment cycle for the latter group began with the administration of LHRHa injections combined with a nonsteroidal antiandrogen for a minimum of 4 weeks and ended after 8 months if there was no evidence of clinical disease progression and if the patient’s PSA level was less than 4 ng/mL and not more than 1 ng/mL above the previous recorded value.
"During the treatment interval, the PSA level was monitored every 2 months until it reached 10 ng/mL, provided there was no intervening evidence of disease progression," stated lead investigator Dr. Juanita M. Crook of the British Columbia Cancer Agency, Kelowna, and her colleagues. (N. Engl. J. Med. 2012;367:895-903).
Overall survival was the primary end point of the study, and time to castration-resistant disease and quality of life were secondary end points, the authors wrote. Duration of off-treatment intervals, time to testosterone recovery, and time to potency recovery were additional end points for patients randomized to intermittent therapy.
At a median follow-up of 6.9 years, 524 patients had died, including 268 in the intermittent group and 256 in the continuous group, the authors reported. Median overall survival in both arms was statistically similar, at 8.8 years in the intermittent group and 9.1 years in the continuous therapy group.
"The hazard ratio for death with intermittent therapy versus continuous therapy was 1.02," the authors wrote, and the P value for noninferiority, at.009, supported the investigators’ initial hypothesis that intermittent therapy was not inferior to continuous therapy. A nonsignificant increase in deaths from other causes was observed in the continuous therapy group.
Because most of the deaths (59%) were unrelated to prostate cancer, the investigators retrospectively analyzed disease-specific survival "to determine whether a significant difference in treatment effect was obscured by the data on deaths from causes other than prostate cancer," they said. The estimated disease-specific hazard ratio after adjustment for stratification and confounding factors was 1.23, and the estimated 7-year cumulative disease-related death rates were 18% and 15%, respectively, for the intermittent and continuous groups.
With respect to time to castration-resistant disease, based on a Cox regression analysis adjusted for stratification and prognostic factors, the estimated hazard ratio for intermittent versus continuous therapy was 0.81, the authors reported, noting, however, that the study design contributed to a bias "by an unknown magnitude" against continuous androgen-deprivation therapy.
"For patients in the intermittent-therapy group, there was an inherent delay in the identification of castration-resistant disease, because treatment had to be restarted in these patients and they had to have a ‘castrate-range’ testosterone level and an additional three increases in the PSA level before being classified as having castration-resistant disease," the investigators wrote.
In quality of life measures, the intermittent therapy group had nonsignificantly better scores for functional domains (physical, role, and global health) and significantly better scores for symptoms, including hot flashes, desire for sexual activity, and urinary symptoms, the authors reported. Full testosterone recovery in the intermittent group occurred in 35% of the patients, while recovery to the trial entry threshold occurred in 79%, they said.
The authors concluded that their trial "raises provocative questions" and cautioned that their results "cannot be extrapolated to other intermittent-treatment schedules or disease characteristics."
The article did not address the apparent contradiction between the NCIC trial results and the findings of the Southwest Oncology Group (SWOG) 9346 trial reported earlier in the year at the ASCO annual meeting.
The latter trial randomized 3,040 patients with newly diagnosed hormone-sensitive metastatic prostate cancer with a PSA level of at least 5 ng/mL before androgen deprivation and a SWOG performance status of 0-2 to intermittent or continuous therapy. The investigators reported a 9% increase in the relative risk of death associated with intermittent therapy, which did not meet the prespecified criteria for noninferiority.
A secondary analysis of the SWOG 9346 data suggested that intermittent therapy was noninferior to continuous in patients with extensive disease but not minimal disease.
"The two studies targeted different populations," Dr. Crook said in an interview. "There are also some important differences in the way the results were handled in the statistical analysis. The results of the SWOG study are equivocal regarding survival."
"Our study has shown that men with only PSA evidence of recurrent prostate cancer and no evidence of metastatic disease can safely be treated with this intermittent program of androgen suppression to gain quality of life benefits without sacrificing length of life," she added.
"Our study did not address the optimal time to begin androgen ablation, or specifically how long intervention can be safely postponed."
The NCIC trial was supported by grants from the Canadian Cancer Society, the U.S. National Cancer Institute, and Hoeschst Marion Roussel Canada Research. Dr. Crook disclosed no relevant financial conflicts. Study coinvestigators disclosed financial relationships with numerous companies.
*This story was updated 9/6/2012.
Intermittent androgen deprivation was not associated with inferior survival for men with a rising prostate-specific antigen level after definitive radiotherapy in a study reported in the Sept. 6 issue of the New England Journal of Medicine.
The findings from the phase III National Cancer Institute of Canada (NCIC) Clinical Trials Group study appear to conflict with those of another international phase III clinical trial reported in June at the annual meeting of the American Society of Clinical Oncology, and as such may fuel rather than extinguish the longstanding debate regarding the proper use and timing of endocrine therapy with androgen antagonists.
In the NCIC trial, 696 of 1,386 men with a PSA level greater than 3 ng/mL more than 1 year after primary or salvage radiotherapy for localized prostate cancer were randomized to continuous androgen suppression therapy consisting of a luteinizing hormone–releasing hormone agonist (LHRHa), combined with a minimum of 4 weeks of a nonsteroidal antiandrogen, or orchiectomy.
Another 690 men were randomized to intermittent androgen deprivation in 8-month cycles, with periods of nontreatment determined by PSA level. Each treatment cycle for the latter group began with the administration of LHRHa injections combined with a nonsteroidal antiandrogen for a minimum of 4 weeks and ended after 8 months if there was no evidence of clinical disease progression and if the patient’s PSA level was less than 4 ng/mL and not more than 1 ng/mL above the previous recorded value.
"During the treatment interval, the PSA level was monitored every 2 months until it reached 10 ng/mL, provided there was no intervening evidence of disease progression," stated lead investigator Dr. Juanita M. Crook of the British Columbia Cancer Agency, Kelowna, and her colleagues. (N. Engl. J. Med. 2012;367:895-903).
Overall survival was the primary end point of the study, and time to castration-resistant disease and quality of life were secondary end points, the authors wrote. Duration of off-treatment intervals, time to testosterone recovery, and time to potency recovery were additional end points for patients randomized to intermittent therapy.
At a median follow-up of 6.9 years, 524 patients had died, including 268 in the intermittent group and 256 in the continuous group, the authors reported. Median overall survival in both arms was statistically similar, at 8.8 years in the intermittent group and 9.1 years in the continuous therapy group.
"The hazard ratio for death with intermittent therapy versus continuous therapy was 1.02," the authors wrote, and the P value for noninferiority, at.009, supported the investigators’ initial hypothesis that intermittent therapy was not inferior to continuous therapy. A nonsignificant increase in deaths from other causes was observed in the continuous therapy group.
Because most of the deaths (59%) were unrelated to prostate cancer, the investigators retrospectively analyzed disease-specific survival "to determine whether a significant difference in treatment effect was obscured by the data on deaths from causes other than prostate cancer," they said. The estimated disease-specific hazard ratio after adjustment for stratification and confounding factors was 1.23, and the estimated 7-year cumulative disease-related death rates were 18% and 15%, respectively, for the intermittent and continuous groups.
With respect to time to castration-resistant disease, based on a Cox regression analysis adjusted for stratification and prognostic factors, the estimated hazard ratio for intermittent versus continuous therapy was 0.81, the authors reported, noting, however, that the study design contributed to a bias "by an unknown magnitude" against continuous androgen-deprivation therapy.
"For patients in the intermittent-therapy group, there was an inherent delay in the identification of castration-resistant disease, because treatment had to be restarted in these patients and they had to have a ‘castrate-range’ testosterone level and an additional three increases in the PSA level before being classified as having castration-resistant disease," the investigators wrote.
In quality of life measures, the intermittent therapy group had nonsignificantly better scores for functional domains (physical, role, and global health) and significantly better scores for symptoms, including hot flashes, desire for sexual activity, and urinary symptoms, the authors reported. Full testosterone recovery in the intermittent group occurred in 35% of the patients, while recovery to the trial entry threshold occurred in 79%, they said.
The authors concluded that their trial "raises provocative questions" and cautioned that their results "cannot be extrapolated to other intermittent-treatment schedules or disease characteristics."
The article did not address the apparent contradiction between the NCIC trial results and the findings of the Southwest Oncology Group (SWOG) 9346 trial reported earlier in the year at the ASCO annual meeting.
The latter trial randomized 3,040 patients with newly diagnosed hormone-sensitive metastatic prostate cancer with a PSA level of at least 5 ng/mL before androgen deprivation and a SWOG performance status of 0-2 to intermittent or continuous therapy. The investigators reported a 9% increase in the relative risk of death associated with intermittent therapy, which did not meet the prespecified criteria for noninferiority.
A secondary analysis of the SWOG 9346 data suggested that intermittent therapy was noninferior to continuous in patients with extensive disease but not minimal disease.
"The two studies targeted different populations," Dr. Crook said in an interview. "There are also some important differences in the way the results were handled in the statistical analysis. The results of the SWOG study are equivocal regarding survival."
"Our study has shown that men with only PSA evidence of recurrent prostate cancer and no evidence of metastatic disease can safely be treated with this intermittent program of androgen suppression to gain quality of life benefits without sacrificing length of life," she added.
"Our study did not address the optimal time to begin androgen ablation, or specifically how long intervention can be safely postponed."
The NCIC trial was supported by grants from the Canadian Cancer Society, the U.S. National Cancer Institute, and Hoeschst Marion Roussel Canada Research. Dr. Crook disclosed no relevant financial conflicts. Study coinvestigators disclosed financial relationships with numerous companies.
*This story was updated 9/6/2012.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: Median overall survival associated with intermittent androgen suppression therapy for rising PSA level after radiotherapy was 8.8 years compared with 9.1 years among men treated continuously.
Data Source: A noninferiority trial was done comparing intermittent to continuous androgen deprivation therapy in 1,386 men randomized 1:1 with localized prostate cancer after primary or salvage radiotherapy
Disclosures: The NCIC trial was supported by grants from the Canadian Cancer Society, the U.S. National Cancer Institute, and Hoeschst Marion Roussel Canada Research. Dr. Crook disclosed no relevant financial conflicts. Study coinvestigators disclosed financial relationships with numerous companies.
Lipid Abnormalities Common in Granuloma Annulare
BOSTON – A diagnosis of granuloma annulare "should trigger a high index of suspicion for dyslipidemia, especially among patients with generalized and annular disease," said Dr. George Kroumpouzos.
He and his colleagues found that adults with granuloma annulare are four times more likely to develop dyslipidemia than those without the inflammatory dermatosis.
Therefore, it is incumbent upon physicians treating granuloma annulare patients to communicate with primary care physicians regarding the need for simultaneous dyslipidemia management, said Dr. Kroumpouzos of the dermatology department at Brown University in Providence, R.I.
To estimate the prevalence of dyslipidemia in granuloma annulare patients, the investigators reviewed the medical records of 140 adult patients with idiopathic granuloma annulare and 420 controls matched for age, gender, race, type 2 diabetes, hypertension, and hypothyroidism, according to data presented in a poster at the American Academy of Dermatology’s Summer Academy Meeting.
The individuals included in the analysis were seen at a university hospital or a regional health care center from 2002 to 2010. To examine associations between disease characteristics and comorbidities, the granuloma annulare patients were divided into subgroups based on disease extent (localized, disseminated, generalized), morphology (annular, nonannular), and histopathology (interstitial, palisaded, mixed, deep).
Dyslipidemia was defined as the presence of one or more of the following lipid abnormalities: hypercholesterolemia (value greater than 200 mg/dL), hypertriglyceridemia (greater than 150 mg/dL), elevated LDL cholesterol (greater than 130 mg/dL), or low HDL cholesterol (less than 40 mg/dL).
According to the analysis, the prevalence of dyslipidemia in granuloma annulare patients was 79.3%, compared with 51.9% among the matched controls. After adjusting for confounding variables, the odds ratio for dyslipidemia in granuloma annulare was 4.04.
The investigators found that the association with dyslipidemia, which is independent of cardiovascular comorbidities, was more prevalent among individuals with the generalized form of the skin condition than among those with localized or disseminated disease.
"The data also demonstrates a statistically significant association between the extent of disease and dyslipidemia," said Dr. Kroumpouzos in an interview. Dyslipidemia was more common in the generalized disease subgroup than in the localized or disseminated subgroups, he explained. Further, annular lesion morphology was associated with hypercholesterolemia and dyslipidemia, which was an unexpected finding.
Although the findings are limited by the lack of account for other potential confounders, including smoking history, exercise, alcohol use, and use of other medications, and additional studies are needed to confirm the results and validate granuloma annulare as a new marker for dyslipidemia – physicians should be aware of the association, Dr. Kroumpouzos said.
The study was also published in Archives of Dermatology (2012 June 18 [doi: 10.1001/archdermatol.2012.1381]).
The investigators disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
BOSTON – A diagnosis of granuloma annulare "should trigger a high index of suspicion for dyslipidemia, especially among patients with generalized and annular disease," said Dr. George Kroumpouzos.
He and his colleagues found that adults with granuloma annulare are four times more likely to develop dyslipidemia than those without the inflammatory dermatosis.
Therefore, it is incumbent upon physicians treating granuloma annulare patients to communicate with primary care physicians regarding the need for simultaneous dyslipidemia management, said Dr. Kroumpouzos of the dermatology department at Brown University in Providence, R.I.
To estimate the prevalence of dyslipidemia in granuloma annulare patients, the investigators reviewed the medical records of 140 adult patients with idiopathic granuloma annulare and 420 controls matched for age, gender, race, type 2 diabetes, hypertension, and hypothyroidism, according to data presented in a poster at the American Academy of Dermatology’s Summer Academy Meeting.
The individuals included in the analysis were seen at a university hospital or a regional health care center from 2002 to 2010. To examine associations between disease characteristics and comorbidities, the granuloma annulare patients were divided into subgroups based on disease extent (localized, disseminated, generalized), morphology (annular, nonannular), and histopathology (interstitial, palisaded, mixed, deep).
Dyslipidemia was defined as the presence of one or more of the following lipid abnormalities: hypercholesterolemia (value greater than 200 mg/dL), hypertriglyceridemia (greater than 150 mg/dL), elevated LDL cholesterol (greater than 130 mg/dL), or low HDL cholesterol (less than 40 mg/dL).
According to the analysis, the prevalence of dyslipidemia in granuloma annulare patients was 79.3%, compared with 51.9% among the matched controls. After adjusting for confounding variables, the odds ratio for dyslipidemia in granuloma annulare was 4.04.
The investigators found that the association with dyslipidemia, which is independent of cardiovascular comorbidities, was more prevalent among individuals with the generalized form of the skin condition than among those with localized or disseminated disease.
"The data also demonstrates a statistically significant association between the extent of disease and dyslipidemia," said Dr. Kroumpouzos in an interview. Dyslipidemia was more common in the generalized disease subgroup than in the localized or disseminated subgroups, he explained. Further, annular lesion morphology was associated with hypercholesterolemia and dyslipidemia, which was an unexpected finding.
Although the findings are limited by the lack of account for other potential confounders, including smoking history, exercise, alcohol use, and use of other medications, and additional studies are needed to confirm the results and validate granuloma annulare as a new marker for dyslipidemia – physicians should be aware of the association, Dr. Kroumpouzos said.
The study was also published in Archives of Dermatology (2012 June 18 [doi: 10.1001/archdermatol.2012.1381]).
The investigators disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
BOSTON – A diagnosis of granuloma annulare "should trigger a high index of suspicion for dyslipidemia, especially among patients with generalized and annular disease," said Dr. George Kroumpouzos.
He and his colleagues found that adults with granuloma annulare are four times more likely to develop dyslipidemia than those without the inflammatory dermatosis.
Therefore, it is incumbent upon physicians treating granuloma annulare patients to communicate with primary care physicians regarding the need for simultaneous dyslipidemia management, said Dr. Kroumpouzos of the dermatology department at Brown University in Providence, R.I.
To estimate the prevalence of dyslipidemia in granuloma annulare patients, the investigators reviewed the medical records of 140 adult patients with idiopathic granuloma annulare and 420 controls matched for age, gender, race, type 2 diabetes, hypertension, and hypothyroidism, according to data presented in a poster at the American Academy of Dermatology’s Summer Academy Meeting.
The individuals included in the analysis were seen at a university hospital or a regional health care center from 2002 to 2010. To examine associations between disease characteristics and comorbidities, the granuloma annulare patients were divided into subgroups based on disease extent (localized, disseminated, generalized), morphology (annular, nonannular), and histopathology (interstitial, palisaded, mixed, deep).
Dyslipidemia was defined as the presence of one or more of the following lipid abnormalities: hypercholesterolemia (value greater than 200 mg/dL), hypertriglyceridemia (greater than 150 mg/dL), elevated LDL cholesterol (greater than 130 mg/dL), or low HDL cholesterol (less than 40 mg/dL).
According to the analysis, the prevalence of dyslipidemia in granuloma annulare patients was 79.3%, compared with 51.9% among the matched controls. After adjusting for confounding variables, the odds ratio for dyslipidemia in granuloma annulare was 4.04.
The investigators found that the association with dyslipidemia, which is independent of cardiovascular comorbidities, was more prevalent among individuals with the generalized form of the skin condition than among those with localized or disseminated disease.
"The data also demonstrates a statistically significant association between the extent of disease and dyslipidemia," said Dr. Kroumpouzos in an interview. Dyslipidemia was more common in the generalized disease subgroup than in the localized or disseminated subgroups, he explained. Further, annular lesion morphology was associated with hypercholesterolemia and dyslipidemia, which was an unexpected finding.
Although the findings are limited by the lack of account for other potential confounders, including smoking history, exercise, alcohol use, and use of other medications, and additional studies are needed to confirm the results and validate granuloma annulare as a new marker for dyslipidemia – physicians should be aware of the association, Dr. Kroumpouzos said.
The study was also published in Archives of Dermatology (2012 June 18 [doi: 10.1001/archdermatol.2012.1381]).
The investigators disclosed no financial conflicts of interest.
In a commentary accompanying the online publication of the study, Dr. Mark V. Dahl wrote that the finding of dyslipidemia among so many granuloma annulare patients "comes as a surprise." The cause of granuloma annulare is unknown, and until now, "only vague hints suggested a possible association with a lipid abnormality," he wrote, noting, however, that patients with generalized granuloma annulare "occasionally have an abnormality of glucose metabolism, microangiopathy, and microdroplet lipid deposits inside histiocytes" (Arch. Dermatol. 2012 June 18 [doi: 10.1001/archdermatol.2012.1503]).
Dr. Dahl is a senior consultant for the department of dermatology at the Mayo Clinic in Scottsdale, Ariz. He disclosed no financial conflicts of interest.
AT THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
Major Finding: The prevalence of dyslipidemia among granuloma annulare patients was 79.3%, compared with 51.9% among matched controls.
Data Source: This was a two-center study of 140 adult patients with idiopathic granuloma annulare and 420 matched controls.
Disclosures: The investigators disclosed no financial conflicts of interest.
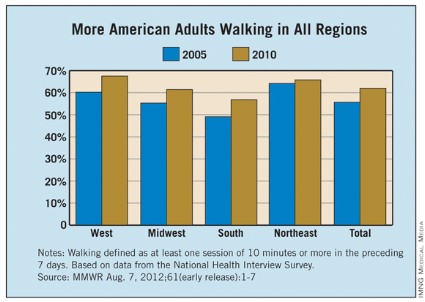
Uncontrolled Hypertension Deemed Pervasive in U.S. Adults
More than half of American adults with hypertension in the United States do not have their blood pressure under control, including many of those being treated for the condition, according to the Centers for Disease Control and Prevention.
Referring to uncontrolled blood pressure as "public health enemy No. 2" – second only to tobacco in the number of potentially preventable deaths associated with it annually – CDC director Thomas R. Frieden said that an estimated 66.9 million American adults had hypertension, defined as an average systolic blood pressure of 140 mm Hg or higher and an average diastolic blood pressure of 90 mm Hg or higher. The condition is deemed uncontrolled in approximately 35.8 million of them. Further, while an estimated 14.1 million of these adults were not aware of their hypertension, roughly 16 million were aware and receiving treatment for it; another 5.7 million were aware, but were not being treated, according to an analysis of data from the National Health and Nutrition Examination Survey 2003-2010.
"We’re talking about $131 billion in health care costs annually and 1,000 deaths/day, today and every day this year" that can be attributed to uncontrolled hypertension, which is a major risk factor for heart disease and stroke, Dr. Frieden stated in a media telebriefing.
"Nearly one quarter of the adults with uncontrolled hypertension in the survey had stage 2 disease [systolic blood pressure of 160 mm Hg or higher; diastolic of 100 mm Hg or higher], putting them at increased risk for both heart disease and stroke," he said.
According to the analysis of the data, reported in the Sept. 4 Morbidity and Mortality Weekly Report, the majority of adults with uncontrolled hypertension had a usual source of health care (89%), had received medical care in the previous year (88%), and had health insurance (85%). That said, the prevalence rates of uncontrolled hypertension were highest (93% and 87%, respectively) among those who reported receiving no medical care in the previous year and those without a usual source of health care. Additionally, of an estimated 14.1 million Medicare beneficiaries with hypertension, more than half (52%) did not have their blood pressure under control (MMWR 2012 Sept. 4 [61]:1-7).
"There are obviously a lot of missed opportunities for getting blood pressure under control. We [clinicians] know what to do, there are great medications that work well when taken as prescribed. We have to roll up our sleeves and make blood pressure control a priority at every visit," Dr. Frieden said. "We have to engage the entire health care team, including pharmacists, nurses, nutritionists, office staff to optimize patient support and follow-up care." He suggested tapping into electronic health records to track outcomes, streamlining prescription refills, and, most important, measuring and recording blood pressure at every visit and being aware of the numbers.
"We know that as many as one-third of the patients or more with multiple high blood pressure readings are not being diagnosed or treated," he said. "We have to increase provider and patient awareness."
In addition to improving recognition and diagnosis of hypertension through the use of team-based delivery models, other strategies for improving hypertension control in the clinical setting include increasing knowledge of and adherence to management guidelines, optimizing dosing and the use of effective combinations of antihypertensive medications, monitoring patients’ progress, encouraging patient self-monitoring of blood pressure, and educating and counseling patients about healthy lifestyle choices, Dr. Frieden explained, noting that such efforts can lead to dramatic and rapid improvements at the patient level as well as substantial public health improvements.
No conflicts of interest were disclosed.
More than half of American adults with hypertension in the United States do not have their blood pressure under control, including many of those being treated for the condition, according to the Centers for Disease Control and Prevention.
Referring to uncontrolled blood pressure as "public health enemy No. 2" – second only to tobacco in the number of potentially preventable deaths associated with it annually – CDC director Thomas R. Frieden said that an estimated 66.9 million American adults had hypertension, defined as an average systolic blood pressure of 140 mm Hg or higher and an average diastolic blood pressure of 90 mm Hg or higher. The condition is deemed uncontrolled in approximately 35.8 million of them. Further, while an estimated 14.1 million of these adults were not aware of their hypertension, roughly 16 million were aware and receiving treatment for it; another 5.7 million were aware, but were not being treated, according to an analysis of data from the National Health and Nutrition Examination Survey 2003-2010.
"We’re talking about $131 billion in health care costs annually and 1,000 deaths/day, today and every day this year" that can be attributed to uncontrolled hypertension, which is a major risk factor for heart disease and stroke, Dr. Frieden stated in a media telebriefing.
"Nearly one quarter of the adults with uncontrolled hypertension in the survey had stage 2 disease [systolic blood pressure of 160 mm Hg or higher; diastolic of 100 mm Hg or higher], putting them at increased risk for both heart disease and stroke," he said.
According to the analysis of the data, reported in the Sept. 4 Morbidity and Mortality Weekly Report, the majority of adults with uncontrolled hypertension had a usual source of health care (89%), had received medical care in the previous year (88%), and had health insurance (85%). That said, the prevalence rates of uncontrolled hypertension were highest (93% and 87%, respectively) among those who reported receiving no medical care in the previous year and those without a usual source of health care. Additionally, of an estimated 14.1 million Medicare beneficiaries with hypertension, more than half (52%) did not have their blood pressure under control (MMWR 2012 Sept. 4 [61]:1-7).
"There are obviously a lot of missed opportunities for getting blood pressure under control. We [clinicians] know what to do, there are great medications that work well when taken as prescribed. We have to roll up our sleeves and make blood pressure control a priority at every visit," Dr. Frieden said. "We have to engage the entire health care team, including pharmacists, nurses, nutritionists, office staff to optimize patient support and follow-up care." He suggested tapping into electronic health records to track outcomes, streamlining prescription refills, and, most important, measuring and recording blood pressure at every visit and being aware of the numbers.
"We know that as many as one-third of the patients or more with multiple high blood pressure readings are not being diagnosed or treated," he said. "We have to increase provider and patient awareness."
In addition to improving recognition and diagnosis of hypertension through the use of team-based delivery models, other strategies for improving hypertension control in the clinical setting include increasing knowledge of and adherence to management guidelines, optimizing dosing and the use of effective combinations of antihypertensive medications, monitoring patients’ progress, encouraging patient self-monitoring of blood pressure, and educating and counseling patients about healthy lifestyle choices, Dr. Frieden explained, noting that such efforts can lead to dramatic and rapid improvements at the patient level as well as substantial public health improvements.
No conflicts of interest were disclosed.
More than half of American adults with hypertension in the United States do not have their blood pressure under control, including many of those being treated for the condition, according to the Centers for Disease Control and Prevention.
Referring to uncontrolled blood pressure as "public health enemy No. 2" – second only to tobacco in the number of potentially preventable deaths associated with it annually – CDC director Thomas R. Frieden said that an estimated 66.9 million American adults had hypertension, defined as an average systolic blood pressure of 140 mm Hg or higher and an average diastolic blood pressure of 90 mm Hg or higher. The condition is deemed uncontrolled in approximately 35.8 million of them. Further, while an estimated 14.1 million of these adults were not aware of their hypertension, roughly 16 million were aware and receiving treatment for it; another 5.7 million were aware, but were not being treated, according to an analysis of data from the National Health and Nutrition Examination Survey 2003-2010.
"We’re talking about $131 billion in health care costs annually and 1,000 deaths/day, today and every day this year" that can be attributed to uncontrolled hypertension, which is a major risk factor for heart disease and stroke, Dr. Frieden stated in a media telebriefing.
"Nearly one quarter of the adults with uncontrolled hypertension in the survey had stage 2 disease [systolic blood pressure of 160 mm Hg or higher; diastolic of 100 mm Hg or higher], putting them at increased risk for both heart disease and stroke," he said.
According to the analysis of the data, reported in the Sept. 4 Morbidity and Mortality Weekly Report, the majority of adults with uncontrolled hypertension had a usual source of health care (89%), had received medical care in the previous year (88%), and had health insurance (85%). That said, the prevalence rates of uncontrolled hypertension were highest (93% and 87%, respectively) among those who reported receiving no medical care in the previous year and those without a usual source of health care. Additionally, of an estimated 14.1 million Medicare beneficiaries with hypertension, more than half (52%) did not have their blood pressure under control (MMWR 2012 Sept. 4 [61]:1-7).
"There are obviously a lot of missed opportunities for getting blood pressure under control. We [clinicians] know what to do, there are great medications that work well when taken as prescribed. We have to roll up our sleeves and make blood pressure control a priority at every visit," Dr. Frieden said. "We have to engage the entire health care team, including pharmacists, nurses, nutritionists, office staff to optimize patient support and follow-up care." He suggested tapping into electronic health records to track outcomes, streamlining prescription refills, and, most important, measuring and recording blood pressure at every visit and being aware of the numbers.
"We know that as many as one-third of the patients or more with multiple high blood pressure readings are not being diagnosed or treated," he said. "We have to increase provider and patient awareness."
In addition to improving recognition and diagnosis of hypertension through the use of team-based delivery models, other strategies for improving hypertension control in the clinical setting include increasing knowledge of and adherence to management guidelines, optimizing dosing and the use of effective combinations of antihypertensive medications, monitoring patients’ progress, encouraging patient self-monitoring of blood pressure, and educating and counseling patients about healthy lifestyle choices, Dr. Frieden explained, noting that such efforts can lead to dramatic and rapid improvements at the patient level as well as substantial public health improvements.
No conflicts of interest were disclosed.
FROM THE MORBIDITY AND MORTALITY WEEKLY REPORT
Major Finding: The prevalence of hypertension among U.S. adults in 2003-2010 was 30%. More than half (54%) of the estimated 66.9 million with high blood pressure did not have the condition under control.
Data Source: Data were from an analysis of the National Health and Nutrition Examination Survey 2003-2010 examining awareness and treatment of uncontrolled hypertension among U.S. adults with the condition.
Disclosures: No conflicts of interest were reported.
Acne Prescriptions for Topical Combination Therapy Rising
BOSTON – Although there are proven clinical advantages to prescribing topical combination therapies for acne, the benefits must be weighed against the higher cost and loss of flexibility of the products, according to Dr. Laura F. Sandoval.
The use of "combination products allows physicians to adhere to current acne treatment guidelines," which can be complex, as they direct the use of multiple agents for optimal treatment, noted Dr. Sandoval and her colleagues. Combination products with benzoyl peroxide (BPO), however, help decrease the incidence of antibiotic resistance, which is a growing concern in the treatment of acne.
On the heels of a recent meta-analysis of studies comparing combination topical therapy to retinoid monotherapy for acne vulgaris, in which combination treatment was more effective than monotherapy in eight of the nine studies evaluated (J. Drugs Dermatol. 2011;10:636-44), Dr. Sandoval and her colleagues at the Center for Dermatology Research at Wake Forest University, Winston-Salem, N.C., sought to assess practice trends regarding the use of topical combination products in specialty and general practices.
The investigators used the National Ambulatory Medical Care Survey (NAMCS) database to identify acne visits from 1989 to 2009 and to compare prescribing practices between dermatologists and primary care physicians.
From 1989 to 2009, dermatologists and primary care physicians prescribed combination products to 11.5% and 12.6% of their acne patients, respectively, representing frequency increases during the same time period of 0.66% and 1.26%, Dr. Sandoval and her colleagues reported at the American Academy of Dermatology’s Summer Academy Meeting.
From 2007 to 2009, the respective prescription rates of combination products were 20% (dermatology) and 33.8% (primary care). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the top 10 products used by both dermatologists (4.7% and 6.3% of prescriptions, respectively) and primary care physicians (3.4% and 7.9%, respectively).
From 2007 to 2009, dermatologists prescribed clindamycin/BPO for 16.4% of acne visits and clindamycin/tretinoin for 3.9%, while primary care physicians prescribed clindamycin/BPO for 15.6% of acne visits, erythromycin/BPO for 14.6% of acne visits, and the oral contraceptive combination norgestimate/ethinyl estradiol for 8.6%, according to the analysis.
The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. The principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the
BOSTON – Although there are proven clinical advantages to prescribing topical combination therapies for acne, the benefits must be weighed against the higher cost and loss of flexibility of the products, according to Dr. Laura F. Sandoval.
The use of "combination products allows physicians to adhere to current acne treatment guidelines," which can be complex, as they direct the use of multiple agents for optimal treatment, noted Dr. Sandoval and her colleagues. Combination products with benzoyl peroxide (BPO), however, help decrease the incidence of antibiotic resistance, which is a growing concern in the treatment of acne.
On the heels of a recent meta-analysis of studies comparing combination topical therapy to retinoid monotherapy for acne vulgaris, in which combination treatment was more effective than monotherapy in eight of the nine studies evaluated (J. Drugs Dermatol. 2011;10:636-44), Dr. Sandoval and her colleagues at the Center for Dermatology Research at Wake Forest University, Winston-Salem, N.C., sought to assess practice trends regarding the use of topical combination products in specialty and general practices.
The investigators used the National Ambulatory Medical Care Survey (NAMCS) database to identify acne visits from 1989 to 2009 and to compare prescribing practices between dermatologists and primary care physicians.
From 1989 to 2009, dermatologists and primary care physicians prescribed combination products to 11.5% and 12.6% of their acne patients, respectively, representing frequency increases during the same time period of 0.66% and 1.26%, Dr. Sandoval and her colleagues reported at the American Academy of Dermatology’s Summer Academy Meeting.
From 2007 to 2009, the respective prescription rates of combination products were 20% (dermatology) and 33.8% (primary care). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the top 10 products used by both dermatologists (4.7% and 6.3% of prescriptions, respectively) and primary care physicians (3.4% and 7.9%, respectively).
From 2007 to 2009, dermatologists prescribed clindamycin/BPO for 16.4% of acne visits and clindamycin/tretinoin for 3.9%, while primary care physicians prescribed clindamycin/BPO for 15.6% of acne visits, erythromycin/BPO for 14.6% of acne visits, and the oral contraceptive combination norgestimate/ethinyl estradiol for 8.6%, according to the analysis.
The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. The principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
BOSTON – Although there are proven clinical advantages to prescribing topical combination therapies for acne, the benefits must be weighed against the higher cost and loss of flexibility of the products, according to Dr. Laura F. Sandoval.
The use of "combination products allows physicians to adhere to current acne treatment guidelines," which can be complex, as they direct the use of multiple agents for optimal treatment, noted Dr. Sandoval and her colleagues. Combination products with benzoyl peroxide (BPO), however, help decrease the incidence of antibiotic resistance, which is a growing concern in the treatment of acne.
On the heels of a recent meta-analysis of studies comparing combination topical therapy to retinoid monotherapy for acne vulgaris, in which combination treatment was more effective than monotherapy in eight of the nine studies evaluated (J. Drugs Dermatol. 2011;10:636-44), Dr. Sandoval and her colleagues at the Center for Dermatology Research at Wake Forest University, Winston-Salem, N.C., sought to assess practice trends regarding the use of topical combination products in specialty and general practices.
The investigators used the National Ambulatory Medical Care Survey (NAMCS) database to identify acne visits from 1989 to 2009 and to compare prescribing practices between dermatologists and primary care physicians.
From 1989 to 2009, dermatologists and primary care physicians prescribed combination products to 11.5% and 12.6% of their acne patients, respectively, representing frequency increases during the same time period of 0.66% and 1.26%, Dr. Sandoval and her colleagues reported at the American Academy of Dermatology’s Summer Academy Meeting.
From 2007 to 2009, the respective prescription rates of combination products were 20% (dermatology) and 33.8% (primary care). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the top 10 products used by both dermatologists (4.7% and 6.3% of prescriptions, respectively) and primary care physicians (3.4% and 7.9%, respectively).
From 2007 to 2009, dermatologists prescribed clindamycin/BPO for 16.4% of acne visits and clindamycin/tretinoin for 3.9%, while primary care physicians prescribed clindamycin/BPO for 15.6% of acne visits, erythromycin/BPO for 14.6% of acne visits, and the oral contraceptive combination norgestimate/ethinyl estradiol for 8.6%, according to the analysis.
The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. The principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the
). The findings may be a reflection of clinicians’ desire to streamline patient management and improve treatment adherence – both of which can be compromised by the complexity of juggling topical drugs from multiple classes, Dr. Sandoval said in an interview.
During the 20-year period, topical retinoids were the most common treatment for acne and tretinoin was the top retinoid, accounting for 19.2% of prescriptions for acne from dermatologists and 17.9% from primary care physicians, Dr. Sandoval reported in a poster at the meeting. Two combination products – clindamycin/BPO and erythromycin/BPO – were among the
AT THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
Major Finding: From 2007 to 2009, dermatologists and primary care physicians prescribed topical fixed combination treatment for 20% and 33.8% of their acne vulgaris patients, respectively.
Data Source: Analysis of data from the National Ambulatory Medical Care Survey on prescribing trends for the treatment of acne vulgaris for 1989-2009.
Disclosures: The Center for Dermatology Research at Wake Forest is supported by an educational grant from Galderma. The principal investigator, Dr. Steven R. Feldman, reported significant financial relationships with several pharmaceutical companies, including Galderma. Dr. Sandoval and her other coauthors reported no conflicts of interest.
The Pain of Rheumatology
Pain is the elephant in the middle of every rheumatology clinic, and it’s taking up a disproportionate amount of space. It is ever present and ever stubborn, and although everybody wants it gone, nobody is really certain about how to get rid of it. Thus, by default if not design, pain management is becoming an area of increasing research and clinical effort in rheumatology, according to Dr. Ronald Rapoport, director of the osteoporosis and research Center at Charlton Memorial Hospital in Fall River, Mass.
"Pain is the most common complaint of patients presenting to the rheumatology clinic, and it plays a central role in the clinical spectrum of rheumatologic conditions," Dr. Rapoport said. The challenge that time-crunched clinicians face, however, is that musculoskeletal pain across the range of rheumatologic conditions is typically not a consequence of the disease process alone, but rather is the result of a range of biologic, psychological, and social factors that, taken together, preclude easy assessment and treatment. If the pain of rheumatoid arthritis, for example, were simply secondary to inflammation, "then our jobs might be much easier: By treating the underlying manifestations of the disease, we would have a positive impact on the pain," he said. "The reality is that there’s much more to it than that."
In this month’s column, Dr. Rapoport discusses the challenge of rheumatologic pain and the integration of pain management into clinical practice.
Question: Why is rheumatologic pain so difficult to manage?
Dr. Rapoport: The reason is that we’re not just dealing with pain by itself. Halting disease progression is our main concern when we treat the majority of rheumatologic illnesses. If we are not able to control a patient’s pain, the odds of that patient’s returning are diminished, as is our plan of decreasing disease activity. The things we can do to help control pain may have no impact upon progression of the disease. We commonly use steroids as a bridge while we wait for disease-modifying antirheumatic drugs and biologics to have their effect. However, although these agents address pain quickly and effectively, they don’t really have a major impact on disease progression. Patients report feeling better on steroids, but the treatment does not slow or stop radiographic disease progression, which correlates better with future patient disability than does pain. Easing pain and stopping joint destruction often may not be achieved by the same therapeutic pathway.
Another obvious challenge is that ours is an aging population, and a patient’s complaint of pain may be associated with a number of conditions, rather than just the primary rheumatologic condition. A patient with rheumatoid arthritis may also have osteoarthritis or fibromyalgia, for example, and at times the pain associated with each condition may not be easily separable, so there are a lot of variables in the management equation.
Question: Are rheumatologists well equipped to deal with the complexity of chronic pain?
Dr. Rapoport: We are equipped to deal very specifically with pain that is aligned to the disease process, but in our training, there is no separate section on treating pain that is associated with the myriad other influences I mentioned. To treat pain optimally, rheumatologists have to learn about the pain pathways; how and where the various pain medications work; if, when, and in whom to start opioid therapy; whether to prescribe sustained-release or rapid-onset opioids; when and how to combine pharmacologic agents; and when and how to taper pain meds in the presence of improvements in disease progression.
On top of all of this, we must not be naive about the potential for abuse or misuse of pain medications. We need to determine which patients really need these pain meds and which might be abusing or diverting them. Frankly, even the most highly skilled rheumatologists may not always know the difference. This can be a major obstacle to pain management, because even though we all know that there are patients who do not have adequate pain control, there are also many patients who are abusing the potent pain medications. Differentiating between them is especially challenging among patients with significant arthritis.
Question: In recent years, novel pharmacologic agents have emerged that target various pain mediators as well as those that target nonpain symptoms that may inhibit pain secondarily. In your opinion, what have been some of the more important developments or breakthroughs in this regard?
Dr. Rapoport: The most significant advances have really been in the differentiation between pain states and the pathways associated with the different states. Researchers are working on uncovering and understanding the various pain pathways, with an eye toward interrupting the pain signals, in addition to focusing on the receptors and various channels.
Acute pain and persistent peripheral, articular pain tend to respond to NSAIDs and classic opioids, whereas it appears that the central pain conditions may respond best to the central nervous system neuromodulating agents, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) and anticonvulsants.
The key is finding out the source of the patient’s pain and whether there is more than one condition to be addressed. In most cases, polypharmacy for pain control is the rule rather than the exception. Rheumatoid arthritis is a prime example. When we control disease activity and inflammation, sometimes the pain diminishes in a fashion that you would expect, but sometimes it doesn’t. In the latter case, searching for the etiology of the pain and considering an alternative agent is imperative.
Question: The prescription of long-term opioids for chronic, nonmalignant pain is increasingly common, but rheumatologists still grapple with fears of regulatory pressure and the possibility of abuse or diversion. What are some practical measures that can be easily implemented in the clinic to optimize the benefits of these drugs while minimizing the risks?
Dr. Rapoport: Before prescribing these drugs, take the time to explain how they work, the possible side effects, and details of the clinic protocol, such as the need for periodic urine testing. I also tell patients that there is only one health care professional who can write their pain medication prescription, and that no one will write a prescription at 5:00 pm on Fridays. It is also a good idea to have a written agreement – not a "contract," which implies legality – to be signed by the patient and the prescribing clinician that outlines the expectations. It can be time consuming, but it’s very important.
Question: Where, if anywhere, does medical marijuana fit into the mix?
Dr. Rapoport: Most of us – even those of us who were in college in the 1960s and 1970s – are not sure what to do with this yet. Many patients say it works. They are very convincing and very demanding, and they may be very right. But the legality of this is still murky, and the evidence is not totally clear. Most of what we have to go on is anecdotal, and in science that’s not enough. The majority of the patients using cannabis and seeking it do not have inflammatory arthritis. They are chronic pain patients who have exhausted most options. Even so, most of us are on the fence, neither rejecting nor embracing it until there are more data.
Question: Given the complexity of chronic pain, are rheumatologists the best specialists to manage it, or would patients be better served by referral to pain specialists?
Dr. Rapoport: This is a difficult question. I think rheumatologists are not necessarily the best clinicians for this aspect of care, for a number of reasons. First, most of us have an interest in the science associated with rheumatologic disease, and to the degree that pain is an outgrowth of this, it falls under our umbrella. Certain extra-articular pain states – such as neuropathic pain or pain associated with psychosocial factors related to disability – are outside of our domain and often would be best addressed by a pain specialist or primary care physician.
The problem is that these distinctions are not always clear. For example, a patient might present with lower back pain. It could be muscular, it could be discogenic, or it could be arthritis. I’m not sure a rheumatologist’s time, which is already at a premium, is best spent trying to figure this out and how to manage it, especially considering the prevalence of patients with lower back pain. We need to share the burden of these patients.
Question: Are there currently any guidelines or accepted algorithms or hierarchies for pain management in rheumatology, or are rheumatologists in practice flying solo?
Dr. Rapoport: I am unaware of any official guidelines for the treatment of pain in rheumatologic diseases in general or diseases such as rheumatoid arthritis in particular. A number of published articles suggest certain approaches, but beyond that, it’s up to clinicians to get an overall feel for their patients’ pain and its causes, and to proceed accordingly. This is where the art of being a doctor trumps most everything else.
Dr. Rapoport is medical director of phase III clinical research at the Truesdale Clinic Inc., in Fall River, Mass. Dr. Rapoport disclosed financial relationships with Abbott Laboratories, Amgen, Covidien, Forest Laboratories, Lilly, and Pfizer.
Pain is the elephant in the middle of every rheumatology clinic, and it’s taking up a disproportionate amount of space. It is ever present and ever stubborn, and although everybody wants it gone, nobody is really certain about how to get rid of it. Thus, by default if not design, pain management is becoming an area of increasing research and clinical effort in rheumatology, according to Dr. Ronald Rapoport, director of the osteoporosis and research Center at Charlton Memorial Hospital in Fall River, Mass.
"Pain is the most common complaint of patients presenting to the rheumatology clinic, and it plays a central role in the clinical spectrum of rheumatologic conditions," Dr. Rapoport said. The challenge that time-crunched clinicians face, however, is that musculoskeletal pain across the range of rheumatologic conditions is typically not a consequence of the disease process alone, but rather is the result of a range of biologic, psychological, and social factors that, taken together, preclude easy assessment and treatment. If the pain of rheumatoid arthritis, for example, were simply secondary to inflammation, "then our jobs might be much easier: By treating the underlying manifestations of the disease, we would have a positive impact on the pain," he said. "The reality is that there’s much more to it than that."
In this month’s column, Dr. Rapoport discusses the challenge of rheumatologic pain and the integration of pain management into clinical practice.
Question: Why is rheumatologic pain so difficult to manage?
Dr. Rapoport: The reason is that we’re not just dealing with pain by itself. Halting disease progression is our main concern when we treat the majority of rheumatologic illnesses. If we are not able to control a patient’s pain, the odds of that patient’s returning are diminished, as is our plan of decreasing disease activity. The things we can do to help control pain may have no impact upon progression of the disease. We commonly use steroids as a bridge while we wait for disease-modifying antirheumatic drugs and biologics to have their effect. However, although these agents address pain quickly and effectively, they don’t really have a major impact on disease progression. Patients report feeling better on steroids, but the treatment does not slow or stop radiographic disease progression, which correlates better with future patient disability than does pain. Easing pain and stopping joint destruction often may not be achieved by the same therapeutic pathway.
Another obvious challenge is that ours is an aging population, and a patient’s complaint of pain may be associated with a number of conditions, rather than just the primary rheumatologic condition. A patient with rheumatoid arthritis may also have osteoarthritis or fibromyalgia, for example, and at times the pain associated with each condition may not be easily separable, so there are a lot of variables in the management equation.
Question: Are rheumatologists well equipped to deal with the complexity of chronic pain?
Dr. Rapoport: We are equipped to deal very specifically with pain that is aligned to the disease process, but in our training, there is no separate section on treating pain that is associated with the myriad other influences I mentioned. To treat pain optimally, rheumatologists have to learn about the pain pathways; how and where the various pain medications work; if, when, and in whom to start opioid therapy; whether to prescribe sustained-release or rapid-onset opioids; when and how to combine pharmacologic agents; and when and how to taper pain meds in the presence of improvements in disease progression.
On top of all of this, we must not be naive about the potential for abuse or misuse of pain medications. We need to determine which patients really need these pain meds and which might be abusing or diverting them. Frankly, even the most highly skilled rheumatologists may not always know the difference. This can be a major obstacle to pain management, because even though we all know that there are patients who do not have adequate pain control, there are also many patients who are abusing the potent pain medications. Differentiating between them is especially challenging among patients with significant arthritis.
Question: In recent years, novel pharmacologic agents have emerged that target various pain mediators as well as those that target nonpain symptoms that may inhibit pain secondarily. In your opinion, what have been some of the more important developments or breakthroughs in this regard?
Dr. Rapoport: The most significant advances have really been in the differentiation between pain states and the pathways associated with the different states. Researchers are working on uncovering and understanding the various pain pathways, with an eye toward interrupting the pain signals, in addition to focusing on the receptors and various channels.
Acute pain and persistent peripheral, articular pain tend to respond to NSAIDs and classic opioids, whereas it appears that the central pain conditions may respond best to the central nervous system neuromodulating agents, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) and anticonvulsants.
The key is finding out the source of the patient’s pain and whether there is more than one condition to be addressed. In most cases, polypharmacy for pain control is the rule rather than the exception. Rheumatoid arthritis is a prime example. When we control disease activity and inflammation, sometimes the pain diminishes in a fashion that you would expect, but sometimes it doesn’t. In the latter case, searching for the etiology of the pain and considering an alternative agent is imperative.
Question: The prescription of long-term opioids for chronic, nonmalignant pain is increasingly common, but rheumatologists still grapple with fears of regulatory pressure and the possibility of abuse or diversion. What are some practical measures that can be easily implemented in the clinic to optimize the benefits of these drugs while minimizing the risks?
Dr. Rapoport: Before prescribing these drugs, take the time to explain how they work, the possible side effects, and details of the clinic protocol, such as the need for periodic urine testing. I also tell patients that there is only one health care professional who can write their pain medication prescription, and that no one will write a prescription at 5:00 pm on Fridays. It is also a good idea to have a written agreement – not a "contract," which implies legality – to be signed by the patient and the prescribing clinician that outlines the expectations. It can be time consuming, but it’s very important.
Question: Where, if anywhere, does medical marijuana fit into the mix?
Dr. Rapoport: Most of us – even those of us who were in college in the 1960s and 1970s – are not sure what to do with this yet. Many patients say it works. They are very convincing and very demanding, and they may be very right. But the legality of this is still murky, and the evidence is not totally clear. Most of what we have to go on is anecdotal, and in science that’s not enough. The majority of the patients using cannabis and seeking it do not have inflammatory arthritis. They are chronic pain patients who have exhausted most options. Even so, most of us are on the fence, neither rejecting nor embracing it until there are more data.
Question: Given the complexity of chronic pain, are rheumatologists the best specialists to manage it, or would patients be better served by referral to pain specialists?
Dr. Rapoport: This is a difficult question. I think rheumatologists are not necessarily the best clinicians for this aspect of care, for a number of reasons. First, most of us have an interest in the science associated with rheumatologic disease, and to the degree that pain is an outgrowth of this, it falls under our umbrella. Certain extra-articular pain states – such as neuropathic pain or pain associated with psychosocial factors related to disability – are outside of our domain and often would be best addressed by a pain specialist or primary care physician.
The problem is that these distinctions are not always clear. For example, a patient might present with lower back pain. It could be muscular, it could be discogenic, or it could be arthritis. I’m not sure a rheumatologist’s time, which is already at a premium, is best spent trying to figure this out and how to manage it, especially considering the prevalence of patients with lower back pain. We need to share the burden of these patients.
Question: Are there currently any guidelines or accepted algorithms or hierarchies for pain management in rheumatology, or are rheumatologists in practice flying solo?
Dr. Rapoport: I am unaware of any official guidelines for the treatment of pain in rheumatologic diseases in general or diseases such as rheumatoid arthritis in particular. A number of published articles suggest certain approaches, but beyond that, it’s up to clinicians to get an overall feel for their patients’ pain and its causes, and to proceed accordingly. This is where the art of being a doctor trumps most everything else.
Dr. Rapoport is medical director of phase III clinical research at the Truesdale Clinic Inc., in Fall River, Mass. Dr. Rapoport disclosed financial relationships with Abbott Laboratories, Amgen, Covidien, Forest Laboratories, Lilly, and Pfizer.
Pain is the elephant in the middle of every rheumatology clinic, and it’s taking up a disproportionate amount of space. It is ever present and ever stubborn, and although everybody wants it gone, nobody is really certain about how to get rid of it. Thus, by default if not design, pain management is becoming an area of increasing research and clinical effort in rheumatology, according to Dr. Ronald Rapoport, director of the osteoporosis and research Center at Charlton Memorial Hospital in Fall River, Mass.
"Pain is the most common complaint of patients presenting to the rheumatology clinic, and it plays a central role in the clinical spectrum of rheumatologic conditions," Dr. Rapoport said. The challenge that time-crunched clinicians face, however, is that musculoskeletal pain across the range of rheumatologic conditions is typically not a consequence of the disease process alone, but rather is the result of a range of biologic, psychological, and social factors that, taken together, preclude easy assessment and treatment. If the pain of rheumatoid arthritis, for example, were simply secondary to inflammation, "then our jobs might be much easier: By treating the underlying manifestations of the disease, we would have a positive impact on the pain," he said. "The reality is that there’s much more to it than that."
In this month’s column, Dr. Rapoport discusses the challenge of rheumatologic pain and the integration of pain management into clinical practice.
Question: Why is rheumatologic pain so difficult to manage?
Dr. Rapoport: The reason is that we’re not just dealing with pain by itself. Halting disease progression is our main concern when we treat the majority of rheumatologic illnesses. If we are not able to control a patient’s pain, the odds of that patient’s returning are diminished, as is our plan of decreasing disease activity. The things we can do to help control pain may have no impact upon progression of the disease. We commonly use steroids as a bridge while we wait for disease-modifying antirheumatic drugs and biologics to have their effect. However, although these agents address pain quickly and effectively, they don’t really have a major impact on disease progression. Patients report feeling better on steroids, but the treatment does not slow or stop radiographic disease progression, which correlates better with future patient disability than does pain. Easing pain and stopping joint destruction often may not be achieved by the same therapeutic pathway.
Another obvious challenge is that ours is an aging population, and a patient’s complaint of pain may be associated with a number of conditions, rather than just the primary rheumatologic condition. A patient with rheumatoid arthritis may also have osteoarthritis or fibromyalgia, for example, and at times the pain associated with each condition may not be easily separable, so there are a lot of variables in the management equation.
Question: Are rheumatologists well equipped to deal with the complexity of chronic pain?
Dr. Rapoport: We are equipped to deal very specifically with pain that is aligned to the disease process, but in our training, there is no separate section on treating pain that is associated with the myriad other influences I mentioned. To treat pain optimally, rheumatologists have to learn about the pain pathways; how and where the various pain medications work; if, when, and in whom to start opioid therapy; whether to prescribe sustained-release or rapid-onset opioids; when and how to combine pharmacologic agents; and when and how to taper pain meds in the presence of improvements in disease progression.
On top of all of this, we must not be naive about the potential for abuse or misuse of pain medications. We need to determine which patients really need these pain meds and which might be abusing or diverting them. Frankly, even the most highly skilled rheumatologists may not always know the difference. This can be a major obstacle to pain management, because even though we all know that there are patients who do not have adequate pain control, there are also many patients who are abusing the potent pain medications. Differentiating between them is especially challenging among patients with significant arthritis.
Question: In recent years, novel pharmacologic agents have emerged that target various pain mediators as well as those that target nonpain symptoms that may inhibit pain secondarily. In your opinion, what have been some of the more important developments or breakthroughs in this regard?
Dr. Rapoport: The most significant advances have really been in the differentiation between pain states and the pathways associated with the different states. Researchers are working on uncovering and understanding the various pain pathways, with an eye toward interrupting the pain signals, in addition to focusing on the receptors and various channels.
Acute pain and persistent peripheral, articular pain tend to respond to NSAIDs and classic opioids, whereas it appears that the central pain conditions may respond best to the central nervous system neuromodulating agents, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) and anticonvulsants.
The key is finding out the source of the patient’s pain and whether there is more than one condition to be addressed. In most cases, polypharmacy for pain control is the rule rather than the exception. Rheumatoid arthritis is a prime example. When we control disease activity and inflammation, sometimes the pain diminishes in a fashion that you would expect, but sometimes it doesn’t. In the latter case, searching for the etiology of the pain and considering an alternative agent is imperative.
Question: The prescription of long-term opioids for chronic, nonmalignant pain is increasingly common, but rheumatologists still grapple with fears of regulatory pressure and the possibility of abuse or diversion. What are some practical measures that can be easily implemented in the clinic to optimize the benefits of these drugs while minimizing the risks?
Dr. Rapoport: Before prescribing these drugs, take the time to explain how they work, the possible side effects, and details of the clinic protocol, such as the need for periodic urine testing. I also tell patients that there is only one health care professional who can write their pain medication prescription, and that no one will write a prescription at 5:00 pm on Fridays. It is also a good idea to have a written agreement – not a "contract," which implies legality – to be signed by the patient and the prescribing clinician that outlines the expectations. It can be time consuming, but it’s very important.
Question: Where, if anywhere, does medical marijuana fit into the mix?
Dr. Rapoport: Most of us – even those of us who were in college in the 1960s and 1970s – are not sure what to do with this yet. Many patients say it works. They are very convincing and very demanding, and they may be very right. But the legality of this is still murky, and the evidence is not totally clear. Most of what we have to go on is anecdotal, and in science that’s not enough. The majority of the patients using cannabis and seeking it do not have inflammatory arthritis. They are chronic pain patients who have exhausted most options. Even so, most of us are on the fence, neither rejecting nor embracing it until there are more data.
Question: Given the complexity of chronic pain, are rheumatologists the best specialists to manage it, or would patients be better served by referral to pain specialists?
Dr. Rapoport: This is a difficult question. I think rheumatologists are not necessarily the best clinicians for this aspect of care, for a number of reasons. First, most of us have an interest in the science associated with rheumatologic disease, and to the degree that pain is an outgrowth of this, it falls under our umbrella. Certain extra-articular pain states – such as neuropathic pain or pain associated with psychosocial factors related to disability – are outside of our domain and often would be best addressed by a pain specialist or primary care physician.
The problem is that these distinctions are not always clear. For example, a patient might present with lower back pain. It could be muscular, it could be discogenic, or it could be arthritis. I’m not sure a rheumatologist’s time, which is already at a premium, is best spent trying to figure this out and how to manage it, especially considering the prevalence of patients with lower back pain. We need to share the burden of these patients.
Question: Are there currently any guidelines or accepted algorithms or hierarchies for pain management in rheumatology, or are rheumatologists in practice flying solo?
Dr. Rapoport: I am unaware of any official guidelines for the treatment of pain in rheumatologic diseases in general or diseases such as rheumatoid arthritis in particular. A number of published articles suggest certain approaches, but beyond that, it’s up to clinicians to get an overall feel for their patients’ pain and its causes, and to proceed accordingly. This is where the art of being a doctor trumps most everything else.
Dr. Rapoport is medical director of phase III clinical research at the Truesdale Clinic Inc., in Fall River, Mass. Dr. Rapoport disclosed financial relationships with Abbott Laboratories, Amgen, Covidien, Forest Laboratories, Lilly, and Pfizer.
Infantile Hemangioma Growth Peaks in Second Month of Life
BOSTON – Approximately half of all central facial hemangiomas in infants result in significant scarring – an outcome that could potentially be prevented with earlier recognition and treatment, according to Dr. Ilona Frieden.
The challenge, however, lies in determining which infantile lesions are a high risk, and which are unlikely to pose a problem, she explained at the American Academy of Dermatology’s Summer Academy Meeting.
In a recent study of early infantile hemangioma growth based on a review of parental photographs, Dr. Frieden, a clinical professor of dermatology and pediatrics at the University of California, San Francisco, and colleagues found that lesion growth peaked between 5.5 and 7.5 weeks of age (Pediatrics 2012;130:e314-20).
This is "much earlier than we had previously believed," she said. "Unfortunately, referral to a specialist for evaluation and the initiation of treatment typically occurs later than this."
Because most hemangiomas eventually shrink, "pediatricians often recommend waiting for them to go away," Dr. Frieden said. "There is a historic dogma that because hemangiomas are benign, we don’t have to be too worried about them. Unfortunately pediatricians don’t always understand enough about hemangiomas to be able to pick out the bad actors from the ones that are benign." And while dermatologists do have the necessary understanding, it is estimated that 4%-10% of infants develop a hemangioma in the first weeks after birth. "Obviously we are never going to be able to see all of them," she said.
To bridge the divide, Dr. Frieden said that a paradigm shift in the timing of referral and management of high-risk infantile hemangiomas – "ideally by 4 weeks of age to prevent permanent skin changes or growth complications" – is warranted.
Clinical dermatology practices should have mechanisms in place to accommodate urgent evaluations of infants with high-risk hemangiomas, she said. Some of the larger, integrated practices, such as Kaiser Permanente in Northern California, are beginning to do this by establishing photo triage capabilities, where an expert reviews photos of hemangiomas.
Dr. Frieden disclosed having no financial conflicts of interest.
BOSTON – Approximately half of all central facial hemangiomas in infants result in significant scarring – an outcome that could potentially be prevented with earlier recognition and treatment, according to Dr. Ilona Frieden.
The challenge, however, lies in determining which infantile lesions are a high risk, and which are unlikely to pose a problem, she explained at the American Academy of Dermatology’s Summer Academy Meeting.
In a recent study of early infantile hemangioma growth based on a review of parental photographs, Dr. Frieden, a clinical professor of dermatology and pediatrics at the University of California, San Francisco, and colleagues found that lesion growth peaked between 5.5 and 7.5 weeks of age (Pediatrics 2012;130:e314-20).
This is "much earlier than we had previously believed," she said. "Unfortunately, referral to a specialist for evaluation and the initiation of treatment typically occurs later than this."
Because most hemangiomas eventually shrink, "pediatricians often recommend waiting for them to go away," Dr. Frieden said. "There is a historic dogma that because hemangiomas are benign, we don’t have to be too worried about them. Unfortunately pediatricians don’t always understand enough about hemangiomas to be able to pick out the bad actors from the ones that are benign." And while dermatologists do have the necessary understanding, it is estimated that 4%-10% of infants develop a hemangioma in the first weeks after birth. "Obviously we are never going to be able to see all of them," she said.
To bridge the divide, Dr. Frieden said that a paradigm shift in the timing of referral and management of high-risk infantile hemangiomas – "ideally by 4 weeks of age to prevent permanent skin changes or growth complications" – is warranted.
Clinical dermatology practices should have mechanisms in place to accommodate urgent evaluations of infants with high-risk hemangiomas, she said. Some of the larger, integrated practices, such as Kaiser Permanente in Northern California, are beginning to do this by establishing photo triage capabilities, where an expert reviews photos of hemangiomas.
Dr. Frieden disclosed having no financial conflicts of interest.
BOSTON – Approximately half of all central facial hemangiomas in infants result in significant scarring – an outcome that could potentially be prevented with earlier recognition and treatment, according to Dr. Ilona Frieden.
The challenge, however, lies in determining which infantile lesions are a high risk, and which are unlikely to pose a problem, she explained at the American Academy of Dermatology’s Summer Academy Meeting.
In a recent study of early infantile hemangioma growth based on a review of parental photographs, Dr. Frieden, a clinical professor of dermatology and pediatrics at the University of California, San Francisco, and colleagues found that lesion growth peaked between 5.5 and 7.5 weeks of age (Pediatrics 2012;130:e314-20).
This is "much earlier than we had previously believed," she said. "Unfortunately, referral to a specialist for evaluation and the initiation of treatment typically occurs later than this."
Because most hemangiomas eventually shrink, "pediatricians often recommend waiting for them to go away," Dr. Frieden said. "There is a historic dogma that because hemangiomas are benign, we don’t have to be too worried about them. Unfortunately pediatricians don’t always understand enough about hemangiomas to be able to pick out the bad actors from the ones that are benign." And while dermatologists do have the necessary understanding, it is estimated that 4%-10% of infants develop a hemangioma in the first weeks after birth. "Obviously we are never going to be able to see all of them," she said.
To bridge the divide, Dr. Frieden said that a paradigm shift in the timing of referral and management of high-risk infantile hemangiomas – "ideally by 4 weeks of age to prevent permanent skin changes or growth complications" – is warranted.
Clinical dermatology practices should have mechanisms in place to accommodate urgent evaluations of infants with high-risk hemangiomas, she said. Some of the larger, integrated practices, such as Kaiser Permanente in Northern California, are beginning to do this by establishing photo triage capabilities, where an expert reviews photos of hemangiomas.
Dr. Frieden disclosed having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE AMERICAN ACADEMY OF DERMATOLOGY'S SUMMER ACADEMY MEETING
JUPITER: Cardiovascular Benefits of Statins Outweigh Diabetes Risk
The cardiovascular benefits of statin treatment outweigh the risk of developing diabetes, even among individuals with multiple diabetes risk factors, according to a new analysis of data from the JUPITER (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin) trial reported online ahead of print in the Lancet on Aug. 9.
In light of recent evidence suggesting a small increased risk of incident type 2 diabetes associated with all statins, Dr. Paul Ridker of Brigham and Women’s Hospital in Boston and his colleagues sought to evaluate the balance of vascular benefits and the diabetes hazard of statin use in JUPITER trial participants.
Toward this end, they divided 17,603 individuals who took part in the randomized, double-blind, placebo-controlled JUPITER trial into two groups based on diabetes risk factors at study entry, and assessed the impact of rosuvastatin (Crestor) allocation (20 mg/day for up to 5 years) on cardiovascular and mortality risk and the risk of developing incident diabetes.
Of the study cohort, 6,095 individuals had no major risk factors for diabetes at study entry, and 11,508 had one or more major risk factors, defined as metabolic syndrome, impaired fasting glucose, body mass index of 30 kg/m2 or higher, and hemoglobin A1c greater than 6%. Subjects in the latter category were more likely to be female; have higher baseline blood pressure, HbA1c, glucose, and triglyceride values; and have lower baseline HDL cholesterol levels, the authors wrote.
Predictably, those patients with one or more diabetes risk factors had an increased risk of developing diabetes during trial follow-up, with an incidence rate of 1.88 per 100 person-years, compared with 0.18 per 100 person-years in those with no diabetes risk factors, the authors reported (Lancet 2012;380:565-71).
Incident diabetes occurred more frequently in the rosuvastatin group than in the placebo group, with a hazard ratio of 1.25 (270 vs. 216 cases, respectively). Among those who developed diabetes, the average time from randomization to diagnosis was shorter in the statin group, at 84.3 weeks vs. 89.7 weeks. "Almost all the excess risk of diabetes associated with rosuvastatin occurred in participants with baseline evidence of impaired fasting glucose," the authors noted.
In participants with and without diabetes risk factors, random allocation to rosuvastatin was associated with 39% and 52% reductions, respectively, in the study’s primary end point (myocardial infarction, stroke, hospital admission for unstable angina, arterial revascularization, or cardiovascular death), the authors wrote. Further, among those with diabetes risk factors, statin use was associated with a 36% reduction in thromboembolism, a 17% reduction in total mortality, and a 28% increase in diabetes, while statin use in the risk-free group led to a 53% reduction in venous thromboembolism, a 22% reduction in total mortality, and no increase in diabetes risk.
In absolute terms, among those with one or more diabetes risks, a total of 134 cardiovascular events or deaths were avoided in the statin users for every 54 new cases of diabetes, and among those with no diabetes risks, 86 total cardiovascular events or deaths were avoided with no excess new cases of diabetes diagnosed.
With respect to the primary cardiovascular end point, "the relative treatment benefits attributable to rosuvastatin were similar in participants with and without diabetes risk factors," the authors wrote. They also noted that the relative benefits and risks of rosuvastatin were generally consistent for all components of the primary and secondary end points and in all subgroups evaluated, and the risks of diabetes associated with rosuvastatin use did not change substantially as the number of diabetes risk factors increased.
The investigators also looked specifically at participants who developed diabetes during the trial and observed that, of the 486 total, 18 primary cardiovascular end points occurred, including 8 among rosuvastatin patients (1.10 per 100 person-years) and 10 in placebo patients (1.73 per 100 person-years). Thus, the authors reported, "the cardiovascular risk reduction associated with rosuvastatin was consistent with that for the trial as a whole."
The findings suggest that the cardiovascular and mortality benefits of statin therapy exceed the diabetes hazard in individuals with and without major diabetes risk, the authors stated.
They acknowledged, however, that the findings are limited by the fact that all of the study participants had elevated serum C-reactive protein (hsCRP) levels, which is a risk marker for both incident type 2 diabetes and incident cardiovascular events. "Thus, care should be used when considering these primary prevention data for those with hsCRP less than 2 mg/L," they cautioned. Other limitations of the findings include the fact that data from this analysis were limited to rosuvastatin at one dose, even though all statins increase diabetes risk, and the fact that the median JUPITER follow-up was 2 years, so "long-term data for benefits and risks cannot be gleaned from this study," they said.
In an accompanying commentary, Dr. Gerald F. Watts and Dr. Esther M. Ooi of the University of Western Australia, Perth, noted that although the findings reaffirm the net value of statins in the primary prevention of cardiovascular disease, "the diabetogenic effect of these drugs is highest in individuals with risk factors for diabetes, including raised C-reactive protein," while the risk of diabetes is negligible in the absence of statins. As such, they wrote, "a major take-home message for the clinician involved in either primary or secondary prevention of cardiovascular disease is that all individuals on a statin who have major risk factors for diabetes, particularly impaired fasting glucose, need to be informed about the risk, monitored regularly for hyperglycemia, and advised to lose weight and take regular physical exercise to mitigate the emergence of diabetes" (Lancet 2012;380:541-3).
This analysis and the JUPITER trial were funded by AstraZeneca. Dr. Ridker and some of his coinvestigators disclosed financial relationships with AstraZeneca, Merck, Isis, and other companies. Dr. Watts disclosed receiving honoraria or lecture fees from AstraZeneca, Pfizer, Merck Sharp & Dohme, and other companies. Dr. Ooi declared that she had no financial conflicts of interest.
The cardiovascular benefits of statin treatment outweigh the risk of developing diabetes, even among individuals with multiple diabetes risk factors, according to a new analysis of data from the JUPITER (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin) trial reported online ahead of print in the Lancet on Aug. 9.
In light of recent evidence suggesting a small increased risk of incident type 2 diabetes associated with all statins, Dr. Paul Ridker of Brigham and Women’s Hospital in Boston and his colleagues sought to evaluate the balance of vascular benefits and the diabetes hazard of statin use in JUPITER trial participants.
Toward this end, they divided 17,603 individuals who took part in the randomized, double-blind, placebo-controlled JUPITER trial into two groups based on diabetes risk factors at study entry, and assessed the impact of rosuvastatin (Crestor) allocation (20 mg/day for up to 5 years) on cardiovascular and mortality risk and the risk of developing incident diabetes.
Of the study cohort, 6,095 individuals had no major risk factors for diabetes at study entry, and 11,508 had one or more major risk factors, defined as metabolic syndrome, impaired fasting glucose, body mass index of 30 kg/m2 or higher, and hemoglobin A1c greater than 6%. Subjects in the latter category were more likely to be female; have higher baseline blood pressure, HbA1c, glucose, and triglyceride values; and have lower baseline HDL cholesterol levels, the authors wrote.
Predictably, those patients with one or more diabetes risk factors had an increased risk of developing diabetes during trial follow-up, with an incidence rate of 1.88 per 100 person-years, compared with 0.18 per 100 person-years in those with no diabetes risk factors, the authors reported (Lancet 2012;380:565-71).
Incident diabetes occurred more frequently in the rosuvastatin group than in the placebo group, with a hazard ratio of 1.25 (270 vs. 216 cases, respectively). Among those who developed diabetes, the average time from randomization to diagnosis was shorter in the statin group, at 84.3 weeks vs. 89.7 weeks. "Almost all the excess risk of diabetes associated with rosuvastatin occurred in participants with baseline evidence of impaired fasting glucose," the authors noted.
In participants with and without diabetes risk factors, random allocation to rosuvastatin was associated with 39% and 52% reductions, respectively, in the study’s primary end point (myocardial infarction, stroke, hospital admission for unstable angina, arterial revascularization, or cardiovascular death), the authors wrote. Further, among those with diabetes risk factors, statin use was associated with a 36% reduction in thromboembolism, a 17% reduction in total mortality, and a 28% increase in diabetes, while statin use in the risk-free group led to a 53% reduction in venous thromboembolism, a 22% reduction in total mortality, and no increase in diabetes risk.
In absolute terms, among those with one or more diabetes risks, a total of 134 cardiovascular events or deaths were avoided in the statin users for every 54 new cases of diabetes, and among those with no diabetes risks, 86 total cardiovascular events or deaths were avoided with no excess new cases of diabetes diagnosed.
With respect to the primary cardiovascular end point, "the relative treatment benefits attributable to rosuvastatin were similar in participants with and without diabetes risk factors," the authors wrote. They also noted that the relative benefits and risks of rosuvastatin were generally consistent for all components of the primary and secondary end points and in all subgroups evaluated, and the risks of diabetes associated with rosuvastatin use did not change substantially as the number of diabetes risk factors increased.
The investigators also looked specifically at participants who developed diabetes during the trial and observed that, of the 486 total, 18 primary cardiovascular end points occurred, including 8 among rosuvastatin patients (1.10 per 100 person-years) and 10 in placebo patients (1.73 per 100 person-years). Thus, the authors reported, "the cardiovascular risk reduction associated with rosuvastatin was consistent with that for the trial as a whole."
The findings suggest that the cardiovascular and mortality benefits of statin therapy exceed the diabetes hazard in individuals with and without major diabetes risk, the authors stated.
They acknowledged, however, that the findings are limited by the fact that all of the study participants had elevated serum C-reactive protein (hsCRP) levels, which is a risk marker for both incident type 2 diabetes and incident cardiovascular events. "Thus, care should be used when considering these primary prevention data for those with hsCRP less than 2 mg/L," they cautioned. Other limitations of the findings include the fact that data from this analysis were limited to rosuvastatin at one dose, even though all statins increase diabetes risk, and the fact that the median JUPITER follow-up was 2 years, so "long-term data for benefits and risks cannot be gleaned from this study," they said.
In an accompanying commentary, Dr. Gerald F. Watts and Dr. Esther M. Ooi of the University of Western Australia, Perth, noted that although the findings reaffirm the net value of statins in the primary prevention of cardiovascular disease, "the diabetogenic effect of these drugs is highest in individuals with risk factors for diabetes, including raised C-reactive protein," while the risk of diabetes is negligible in the absence of statins. As such, they wrote, "a major take-home message for the clinician involved in either primary or secondary prevention of cardiovascular disease is that all individuals on a statin who have major risk factors for diabetes, particularly impaired fasting glucose, need to be informed about the risk, monitored regularly for hyperglycemia, and advised to lose weight and take regular physical exercise to mitigate the emergence of diabetes" (Lancet 2012;380:541-3).
This analysis and the JUPITER trial were funded by AstraZeneca. Dr. Ridker and some of his coinvestigators disclosed financial relationships with AstraZeneca, Merck, Isis, and other companies. Dr. Watts disclosed receiving honoraria or lecture fees from AstraZeneca, Pfizer, Merck Sharp & Dohme, and other companies. Dr. Ooi declared that she had no financial conflicts of interest.
The cardiovascular benefits of statin treatment outweigh the risk of developing diabetes, even among individuals with multiple diabetes risk factors, according to a new analysis of data from the JUPITER (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin) trial reported online ahead of print in the Lancet on Aug. 9.
In light of recent evidence suggesting a small increased risk of incident type 2 diabetes associated with all statins, Dr. Paul Ridker of Brigham and Women’s Hospital in Boston and his colleagues sought to evaluate the balance of vascular benefits and the diabetes hazard of statin use in JUPITER trial participants.
Toward this end, they divided 17,603 individuals who took part in the randomized, double-blind, placebo-controlled JUPITER trial into two groups based on diabetes risk factors at study entry, and assessed the impact of rosuvastatin (Crestor) allocation (20 mg/day for up to 5 years) on cardiovascular and mortality risk and the risk of developing incident diabetes.
Of the study cohort, 6,095 individuals had no major risk factors for diabetes at study entry, and 11,508 had one or more major risk factors, defined as metabolic syndrome, impaired fasting glucose, body mass index of 30 kg/m2 or higher, and hemoglobin A1c greater than 6%. Subjects in the latter category were more likely to be female; have higher baseline blood pressure, HbA1c, glucose, and triglyceride values; and have lower baseline HDL cholesterol levels, the authors wrote.
Predictably, those patients with one or more diabetes risk factors had an increased risk of developing diabetes during trial follow-up, with an incidence rate of 1.88 per 100 person-years, compared with 0.18 per 100 person-years in those with no diabetes risk factors, the authors reported (Lancet 2012;380:565-71).
Incident diabetes occurred more frequently in the rosuvastatin group than in the placebo group, with a hazard ratio of 1.25 (270 vs. 216 cases, respectively). Among those who developed diabetes, the average time from randomization to diagnosis was shorter in the statin group, at 84.3 weeks vs. 89.7 weeks. "Almost all the excess risk of diabetes associated with rosuvastatin occurred in participants with baseline evidence of impaired fasting glucose," the authors noted.
In participants with and without diabetes risk factors, random allocation to rosuvastatin was associated with 39% and 52% reductions, respectively, in the study’s primary end point (myocardial infarction, stroke, hospital admission for unstable angina, arterial revascularization, or cardiovascular death), the authors wrote. Further, among those with diabetes risk factors, statin use was associated with a 36% reduction in thromboembolism, a 17% reduction in total mortality, and a 28% increase in diabetes, while statin use in the risk-free group led to a 53% reduction in venous thromboembolism, a 22% reduction in total mortality, and no increase in diabetes risk.
In absolute terms, among those with one or more diabetes risks, a total of 134 cardiovascular events or deaths were avoided in the statin users for every 54 new cases of diabetes, and among those with no diabetes risks, 86 total cardiovascular events or deaths were avoided with no excess new cases of diabetes diagnosed.
With respect to the primary cardiovascular end point, "the relative treatment benefits attributable to rosuvastatin were similar in participants with and without diabetes risk factors," the authors wrote. They also noted that the relative benefits and risks of rosuvastatin were generally consistent for all components of the primary and secondary end points and in all subgroups evaluated, and the risks of diabetes associated with rosuvastatin use did not change substantially as the number of diabetes risk factors increased.
The investigators also looked specifically at participants who developed diabetes during the trial and observed that, of the 486 total, 18 primary cardiovascular end points occurred, including 8 among rosuvastatin patients (1.10 per 100 person-years) and 10 in placebo patients (1.73 per 100 person-years). Thus, the authors reported, "the cardiovascular risk reduction associated with rosuvastatin was consistent with that for the trial as a whole."
The findings suggest that the cardiovascular and mortality benefits of statin therapy exceed the diabetes hazard in individuals with and without major diabetes risk, the authors stated.
They acknowledged, however, that the findings are limited by the fact that all of the study participants had elevated serum C-reactive protein (hsCRP) levels, which is a risk marker for both incident type 2 diabetes and incident cardiovascular events. "Thus, care should be used when considering these primary prevention data for those with hsCRP less than 2 mg/L," they cautioned. Other limitations of the findings include the fact that data from this analysis were limited to rosuvastatin at one dose, even though all statins increase diabetes risk, and the fact that the median JUPITER follow-up was 2 years, so "long-term data for benefits and risks cannot be gleaned from this study," they said.
In an accompanying commentary, Dr. Gerald F. Watts and Dr. Esther M. Ooi of the University of Western Australia, Perth, noted that although the findings reaffirm the net value of statins in the primary prevention of cardiovascular disease, "the diabetogenic effect of these drugs is highest in individuals with risk factors for diabetes, including raised C-reactive protein," while the risk of diabetes is negligible in the absence of statins. As such, they wrote, "a major take-home message for the clinician involved in either primary or secondary prevention of cardiovascular disease is that all individuals on a statin who have major risk factors for diabetes, particularly impaired fasting glucose, need to be informed about the risk, monitored regularly for hyperglycemia, and advised to lose weight and take regular physical exercise to mitigate the emergence of diabetes" (Lancet 2012;380:541-3).
This analysis and the JUPITER trial were funded by AstraZeneca. Dr. Ridker and some of his coinvestigators disclosed financial relationships with AstraZeneca, Merck, Isis, and other companies. Dr. Watts disclosed receiving honoraria or lecture fees from AstraZeneca, Pfizer, Merck Sharp & Dohme, and other companies. Dr. Ooi declared that she had no financial conflicts of interest.
FROM THE LANCET
More Americans Walking but Still Far From Fit
More adults are walking these days, but many are still not walking long enough, far enough, or frequently enough to improve their health, according to a new government report.
In 2010, 62% of American adults who responded to the National Health Interview Survey (NHIS) reported at least one 10-minute walk in the previous week, compared with 56% of those surveyed in 2005. Despite the relative improvement, reported in the Centers for Disease Control and Prevention’s Aug. 7 issue of the Morbidity and Mortality Weekly Report, fewer than half of the adults surveyed meet the minimum recommended amount of physical activity, Dr. Thomas R. Frieden, CDC director, said in a press telebriefing announcing the findings.
Specifically, to attain the health benefits associated with physical fitness, adults require a minimum of 150 minutes per week of moderate aerobic physical activity, achieved no less than 10 minutes at a time, according to the 2008 Physical Activity Guidelines for Americans. So, while the jump in the number of adults who report walking for fun, transportation, or exercise is "encouraging," according to Joan M. Dorn, Ph.D., of the CDC’s Division of Nutrition, Physical Activity, and Obesity, "there is still much room for improvement."
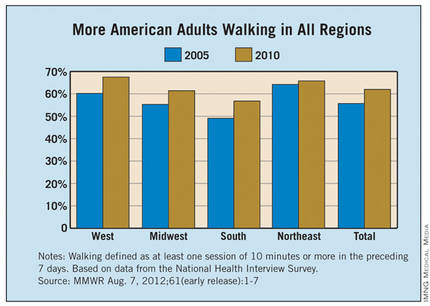
The report noted an increase in walking in nearly all of the groups surveyed, with the greatest increase – from 49% in 2005 to 57% in 2010 – among adults in the South. The smallest increase – 1.6% – was observed in the Northeast, but 66% of adults in that region are walkers, which is the second highest regional rate. The respective rate increases in the Midwest and West regions of the country were 6.1% and 7.3%, with approximately 61% and 68% of adults living in those regions reporting at least 10 minutes of walking per week (MMWR 2012 Aug. 7 [61]:1-7).
Approximately 62% of both men and women reported being walkers in 2010, compared with approximately 54% and 57%, respectively, in 2005. When evaluated by age and body mass index, respectively, the greatest rate increases were seen among 25- to 34-year-olds (9.3%) and overweight adults (7.2%), while the smallest increases were observed in adults aged 65 years or older (3.6%) and those classified as obese (5.8%). Curiously, although the percentage of adult walkers increased, even among subgroups at risk for inactivity, such as those with lower educational attainment (the percentage point change among non–high school graduates was 4.2%), according to the authors, "average walking time among those who walked at least 10 minutes in the preceding 7 days decreased by about 2 minutes per day." The reason for the decrease is unknown, they wrote.
Although only 48% of adults surveyed in 2010 met the aerobic activity recommendation, that rate is nearly six percentage points higher than in 2005, according to the report. Not surprisingly, according to Dr. Dorn, "the percentage of adults who meet the physical activity requirements is higher among walkers than nonwalkers." Specifically, in 2010, 59.5% of those who walked met the guideline, compared with 29.5% of those who did not, and walkers were significantly more likely to meet the guideline than were nonwalkers across every subgroup examined, even among adults requiring walking assistance and those with chronic diseases such as arthritis, hypertension, and diabetes.
The public health implications of the findings are substantial, Dr. Frieden stressed, referring to the association between physical activity and heart disease, stroke, type 2 diabetes, depression, and some cancers. They also point to the need for environmental and policy efforts aimed at getting people walking – an easily achievable physical activity for most people that doesn’t require special skills or facilities, he said.
Specific strategies from the Guide to Community Preventive Services that can be used to promote walking include increasing access to places for physical activity, informational outreach, and urban design and land-use policies developed with an eye toward walker friendliness. "People need more safe and convenient places to walk," Dr. Dorn said in a press statement. "People walk more where they feel protected from traffic and safe from crime. Communities can be designed or improved to make it easier for people to walk to the places the need and want to go."
More adults are walking these days, but many are still not walking long enough, far enough, or frequently enough to improve their health, according to a new government report.
In 2010, 62% of American adults who responded to the National Health Interview Survey (NHIS) reported at least one 10-minute walk in the previous week, compared with 56% of those surveyed in 2005. Despite the relative improvement, reported in the Centers for Disease Control and Prevention’s Aug. 7 issue of the Morbidity and Mortality Weekly Report, fewer than half of the adults surveyed meet the minimum recommended amount of physical activity, Dr. Thomas R. Frieden, CDC director, said in a press telebriefing announcing the findings.
Specifically, to attain the health benefits associated with physical fitness, adults require a minimum of 150 minutes per week of moderate aerobic physical activity, achieved no less than 10 minutes at a time, according to the 2008 Physical Activity Guidelines for Americans. So, while the jump in the number of adults who report walking for fun, transportation, or exercise is "encouraging," according to Joan M. Dorn, Ph.D., of the CDC’s Division of Nutrition, Physical Activity, and Obesity, "there is still much room for improvement."
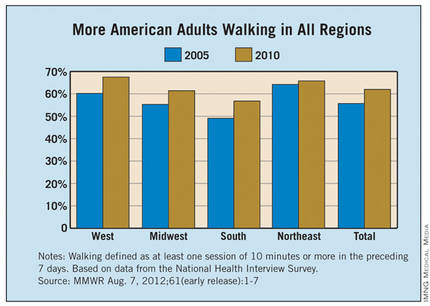
The report noted an increase in walking in nearly all of the groups surveyed, with the greatest increase – from 49% in 2005 to 57% in 2010 – among adults in the South. The smallest increase – 1.6% – was observed in the Northeast, but 66% of adults in that region are walkers, which is the second highest regional rate. The respective rate increases in the Midwest and West regions of the country were 6.1% and 7.3%, with approximately 61% and 68% of adults living in those regions reporting at least 10 minutes of walking per week (MMWR 2012 Aug. 7 [61]:1-7).
Approximately 62% of both men and women reported being walkers in 2010, compared with approximately 54% and 57%, respectively, in 2005. When evaluated by age and body mass index, respectively, the greatest rate increases were seen among 25- to 34-year-olds (9.3%) and overweight adults (7.2%), while the smallest increases were observed in adults aged 65 years or older (3.6%) and those classified as obese (5.8%). Curiously, although the percentage of adult walkers increased, even among subgroups at risk for inactivity, such as those with lower educational attainment (the percentage point change among non–high school graduates was 4.2%), according to the authors, "average walking time among those who walked at least 10 minutes in the preceding 7 days decreased by about 2 minutes per day." The reason for the decrease is unknown, they wrote.
Although only 48% of adults surveyed in 2010 met the aerobic activity recommendation, that rate is nearly six percentage points higher than in 2005, according to the report. Not surprisingly, according to Dr. Dorn, "the percentage of adults who meet the physical activity requirements is higher among walkers than nonwalkers." Specifically, in 2010, 59.5% of those who walked met the guideline, compared with 29.5% of those who did not, and walkers were significantly more likely to meet the guideline than were nonwalkers across every subgroup examined, even among adults requiring walking assistance and those with chronic diseases such as arthritis, hypertension, and diabetes.
The public health implications of the findings are substantial, Dr. Frieden stressed, referring to the association between physical activity and heart disease, stroke, type 2 diabetes, depression, and some cancers. They also point to the need for environmental and policy efforts aimed at getting people walking – an easily achievable physical activity for most people that doesn’t require special skills or facilities, he said.
Specific strategies from the Guide to Community Preventive Services that can be used to promote walking include increasing access to places for physical activity, informational outreach, and urban design and land-use policies developed with an eye toward walker friendliness. "People need more safe and convenient places to walk," Dr. Dorn said in a press statement. "People walk more where they feel protected from traffic and safe from crime. Communities can be designed or improved to make it easier for people to walk to the places the need and want to go."
More adults are walking these days, but many are still not walking long enough, far enough, or frequently enough to improve their health, according to a new government report.
In 2010, 62% of American adults who responded to the National Health Interview Survey (NHIS) reported at least one 10-minute walk in the previous week, compared with 56% of those surveyed in 2005. Despite the relative improvement, reported in the Centers for Disease Control and Prevention’s Aug. 7 issue of the Morbidity and Mortality Weekly Report, fewer than half of the adults surveyed meet the minimum recommended amount of physical activity, Dr. Thomas R. Frieden, CDC director, said in a press telebriefing announcing the findings.
Specifically, to attain the health benefits associated with physical fitness, adults require a minimum of 150 minutes per week of moderate aerobic physical activity, achieved no less than 10 minutes at a time, according to the 2008 Physical Activity Guidelines for Americans. So, while the jump in the number of adults who report walking for fun, transportation, or exercise is "encouraging," according to Joan M. Dorn, Ph.D., of the CDC’s Division of Nutrition, Physical Activity, and Obesity, "there is still much room for improvement."
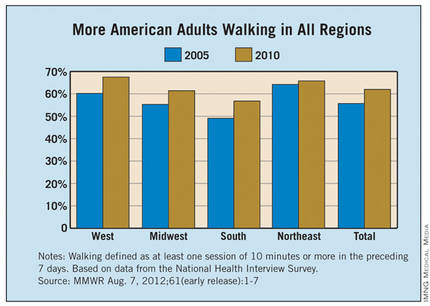
The report noted an increase in walking in nearly all of the groups surveyed, with the greatest increase – from 49% in 2005 to 57% in 2010 – among adults in the South. The smallest increase – 1.6% – was observed in the Northeast, but 66% of adults in that region are walkers, which is the second highest regional rate. The respective rate increases in the Midwest and West regions of the country were 6.1% and 7.3%, with approximately 61% and 68% of adults living in those regions reporting at least 10 minutes of walking per week (MMWR 2012 Aug. 7 [61]:1-7).
Approximately 62% of both men and women reported being walkers in 2010, compared with approximately 54% and 57%, respectively, in 2005. When evaluated by age and body mass index, respectively, the greatest rate increases were seen among 25- to 34-year-olds (9.3%) and overweight adults (7.2%), while the smallest increases were observed in adults aged 65 years or older (3.6%) and those classified as obese (5.8%). Curiously, although the percentage of adult walkers increased, even among subgroups at risk for inactivity, such as those with lower educational attainment (the percentage point change among non–high school graduates was 4.2%), according to the authors, "average walking time among those who walked at least 10 minutes in the preceding 7 days decreased by about 2 minutes per day." The reason for the decrease is unknown, they wrote.
Although only 48% of adults surveyed in 2010 met the aerobic activity recommendation, that rate is nearly six percentage points higher than in 2005, according to the report. Not surprisingly, according to Dr. Dorn, "the percentage of adults who meet the physical activity requirements is higher among walkers than nonwalkers." Specifically, in 2010, 59.5% of those who walked met the guideline, compared with 29.5% of those who did not, and walkers were significantly more likely to meet the guideline than were nonwalkers across every subgroup examined, even among adults requiring walking assistance and those with chronic diseases such as arthritis, hypertension, and diabetes.
The public health implications of the findings are substantial, Dr. Frieden stressed, referring to the association between physical activity and heart disease, stroke, type 2 diabetes, depression, and some cancers. They also point to the need for environmental and policy efforts aimed at getting people walking – an easily achievable physical activity for most people that doesn’t require special skills or facilities, he said.
Specific strategies from the Guide to Community Preventive Services that can be used to promote walking include increasing access to places for physical activity, informational outreach, and urban design and land-use policies developed with an eye toward walker friendliness. "People need more safe and convenient places to walk," Dr. Dorn said in a press statement. "People walk more where they feel protected from traffic and safe from crime. Communities can be designed or improved to make it easier for people to walk to the places the need and want to go."
FROM THE CDC'S MORBIDITY AND MORTALITY WEEKLY REPORT
Major Finding: Approximately 62% of both men and women reported being walkers in 2010, compared with approximately 54% and 57%, respectively, in 2005. When evaluated by region, age, and body mass index, respectively, the greatest rate increases were seen among Midwesterners (6.2%), 25- to 34-year-olds (9.3%) and overweight adults (7.2%).
Data Source: Data are from a comparison of the results of the 2005 and 2010 National Health Interview Surveys reported in the Centers for Disease Control and Prevention’s Mortality and Morbidity Weekly Report.
Disclosures: No conflicts of interest were reported.
Not All Long QT Athletes Have to Be Benched
Tailored therapy and close supervision may help keep competitive athletes with long QT syndrome, such as Olympic hopeful Dana Vollmer, in the game, a study has shown.
A thorough diagnostic evaluation, appropriate medication, risk counseling, education, and a defibrillator device at the ready kept rates of potentially fatal arrhythmias low among a cohort of athletes who chose to remain in competitive sports despite a diagnosis of the cardiac electrical disorder, Dr. Jonathan N. Johnson and Dr. Michael J. Ackerman of the Mayo Clinic in Rochester, Minn., wrote in the July 21 issue of JAMA.
Their research letter was published online concurrently with a pre-Olympics medical conference in Glasgow, Scotland.
"The issue of long QT syndrome [LQTS] and sports participation has received significant publicity due to reports of sudden death in young, competitive athletes," Dr. Ackerman said in an interview. Additionally, medical eligibility criteria established by two sets of guidelines – those of the 36th Bethesda Conference and the European Society of Cardiology – effectively sideline many athletes, but for those who ignore the recommendations.
To determine the outcomes of patients with LQTS who remain in competitive sports contrary to guideline recommendations, the Mayo investigators reviewed the records of patients who were evaluated at Mayo’s LQTS clinic between July 2000 and November 2010 for athletic participation after LQTS diagnosis and syndrome-related events during a mean follow-up of 5.1 years. Of the 353 LQTS patients aged 6-40 years who were identified, 157 were involved in competitive sports at the Little League, middle school, high school, college, or professional level at the time of diagnosis, and 130 remained in competitive athletics following their diagnosis, including 20 with an implantable cardioverter-defibrillator (ICD), they wrote (JAMA 2012 July 21 [doi:10.1001/jama.2012.9334]).
Of the 130 continuing athletes, 60 were competing contrary to both the Bethesda guidelines and the more-restrictive European guidelines, whereas 70 were continuing in sports contrary to the European guidelines but within the Bethesda recommendations, the authors wrote. The only significant difference between the total cohort and the athletes was age, they reported. The mean age at diagnosis for the continuing athletes was 11 years vs. 17 years for the group overall.
Only one of the continuing athletes – a 9-year-old boy with extreme QT prolongation and a history of aborted cardiac arrest – experienced LQTS-triggered cardiac events during sporting activities. "He received 2 appropriate ventricular fibrillation–terminating ICD shocks, both while warming up before games," the authors wrote. "Each episode occurred in the setting of admitted beta-blocker nonadherence."
All of the LQTS athletes seen during the period of study were managed via the same protocol, which, at the Mayo Clinic, includes providing the patient and his or her family with information to enable them to make an informed decision regarding continued sports participation.
Specifically, according to the authors, this includes a comprehensive clinical and genetic evaluation; a consultation with LQTS experts as needed; extensive counseling regarding individual risks and athletic guidelines; tailored therapy (beta-blockers, left cardiac sympathetic denervation, and/or an ICD); education regarding appropriate hydration and electrolyte replenishment; minimizing elevations of core body temperature; and avoidance of QT drugs. Furthermore, all athletes received an automatic external defibrillator to be kept with their sports gear at all sporting events and practices, and relevant school and athletic officials and coaches were informed of the athlete’s condition, they wrote.
Despite the study’s small sample size and limited follow-up, the low rate of cardiac events per athlete year studied (0.003, or 1 event in 331 athlete years) suggests that exercise and sports participation are "manageable risks" in well-counseled, well-managed LQTS patients, Dr. Ackerman said. "We don’t think it’s necessary to control these risks by telling patients they can’t participate in their sport or get too excited," he said.
However, he noted that limiting sports participation may ultimately be in the best interest of certain patients, depending on their individual situation. In all cases, "patients have to be evaluated, risk-stratified, treated, and counseled carefully. The decision to continue has to be an informed one," he said.
Dr. Ackerman is a consultant for Biotronik, Boston Scientific, Medtronic, St. Jude Medical, and Transgenomic. Dr. Johnson reported having no financial disclosures.
Tailored therapy and close supervision may help keep competitive athletes with long QT syndrome, such as Olympic hopeful Dana Vollmer, in the game, a study has shown.
A thorough diagnostic evaluation, appropriate medication, risk counseling, education, and a defibrillator device at the ready kept rates of potentially fatal arrhythmias low among a cohort of athletes who chose to remain in competitive sports despite a diagnosis of the cardiac electrical disorder, Dr. Jonathan N. Johnson and Dr. Michael J. Ackerman of the Mayo Clinic in Rochester, Minn., wrote in the July 21 issue of JAMA.
Their research letter was published online concurrently with a pre-Olympics medical conference in Glasgow, Scotland.
"The issue of long QT syndrome [LQTS] and sports participation has received significant publicity due to reports of sudden death in young, competitive athletes," Dr. Ackerman said in an interview. Additionally, medical eligibility criteria established by two sets of guidelines – those of the 36th Bethesda Conference and the European Society of Cardiology – effectively sideline many athletes, but for those who ignore the recommendations.
To determine the outcomes of patients with LQTS who remain in competitive sports contrary to guideline recommendations, the Mayo investigators reviewed the records of patients who were evaluated at Mayo’s LQTS clinic between July 2000 and November 2010 for athletic participation after LQTS diagnosis and syndrome-related events during a mean follow-up of 5.1 years. Of the 353 LQTS patients aged 6-40 years who were identified, 157 were involved in competitive sports at the Little League, middle school, high school, college, or professional level at the time of diagnosis, and 130 remained in competitive athletics following their diagnosis, including 20 with an implantable cardioverter-defibrillator (ICD), they wrote (JAMA 2012 July 21 [doi:10.1001/jama.2012.9334]).
Of the 130 continuing athletes, 60 were competing contrary to both the Bethesda guidelines and the more-restrictive European guidelines, whereas 70 were continuing in sports contrary to the European guidelines but within the Bethesda recommendations, the authors wrote. The only significant difference between the total cohort and the athletes was age, they reported. The mean age at diagnosis for the continuing athletes was 11 years vs. 17 years for the group overall.
Only one of the continuing athletes – a 9-year-old boy with extreme QT prolongation and a history of aborted cardiac arrest – experienced LQTS-triggered cardiac events during sporting activities. "He received 2 appropriate ventricular fibrillation–terminating ICD shocks, both while warming up before games," the authors wrote. "Each episode occurred in the setting of admitted beta-blocker nonadherence."
All of the LQTS athletes seen during the period of study were managed via the same protocol, which, at the Mayo Clinic, includes providing the patient and his or her family with information to enable them to make an informed decision regarding continued sports participation.
Specifically, according to the authors, this includes a comprehensive clinical and genetic evaluation; a consultation with LQTS experts as needed; extensive counseling regarding individual risks and athletic guidelines; tailored therapy (beta-blockers, left cardiac sympathetic denervation, and/or an ICD); education regarding appropriate hydration and electrolyte replenishment; minimizing elevations of core body temperature; and avoidance of QT drugs. Furthermore, all athletes received an automatic external defibrillator to be kept with their sports gear at all sporting events and practices, and relevant school and athletic officials and coaches were informed of the athlete’s condition, they wrote.
Despite the study’s small sample size and limited follow-up, the low rate of cardiac events per athlete year studied (0.003, or 1 event in 331 athlete years) suggests that exercise and sports participation are "manageable risks" in well-counseled, well-managed LQTS patients, Dr. Ackerman said. "We don’t think it’s necessary to control these risks by telling patients they can’t participate in their sport or get too excited," he said.
However, he noted that limiting sports participation may ultimately be in the best interest of certain patients, depending on their individual situation. In all cases, "patients have to be evaluated, risk-stratified, treated, and counseled carefully. The decision to continue has to be an informed one," he said.
Dr. Ackerman is a consultant for Biotronik, Boston Scientific, Medtronic, St. Jude Medical, and Transgenomic. Dr. Johnson reported having no financial disclosures.
Tailored therapy and close supervision may help keep competitive athletes with long QT syndrome, such as Olympic hopeful Dana Vollmer, in the game, a study has shown.
A thorough diagnostic evaluation, appropriate medication, risk counseling, education, and a defibrillator device at the ready kept rates of potentially fatal arrhythmias low among a cohort of athletes who chose to remain in competitive sports despite a diagnosis of the cardiac electrical disorder, Dr. Jonathan N. Johnson and Dr. Michael J. Ackerman of the Mayo Clinic in Rochester, Minn., wrote in the July 21 issue of JAMA.
Their research letter was published online concurrently with a pre-Olympics medical conference in Glasgow, Scotland.
"The issue of long QT syndrome [LQTS] and sports participation has received significant publicity due to reports of sudden death in young, competitive athletes," Dr. Ackerman said in an interview. Additionally, medical eligibility criteria established by two sets of guidelines – those of the 36th Bethesda Conference and the European Society of Cardiology – effectively sideline many athletes, but for those who ignore the recommendations.
To determine the outcomes of patients with LQTS who remain in competitive sports contrary to guideline recommendations, the Mayo investigators reviewed the records of patients who were evaluated at Mayo’s LQTS clinic between July 2000 and November 2010 for athletic participation after LQTS diagnosis and syndrome-related events during a mean follow-up of 5.1 years. Of the 353 LQTS patients aged 6-40 years who were identified, 157 were involved in competitive sports at the Little League, middle school, high school, college, or professional level at the time of diagnosis, and 130 remained in competitive athletics following their diagnosis, including 20 with an implantable cardioverter-defibrillator (ICD), they wrote (JAMA 2012 July 21 [doi:10.1001/jama.2012.9334]).
Of the 130 continuing athletes, 60 were competing contrary to both the Bethesda guidelines and the more-restrictive European guidelines, whereas 70 were continuing in sports contrary to the European guidelines but within the Bethesda recommendations, the authors wrote. The only significant difference between the total cohort and the athletes was age, they reported. The mean age at diagnosis for the continuing athletes was 11 years vs. 17 years for the group overall.
Only one of the continuing athletes – a 9-year-old boy with extreme QT prolongation and a history of aborted cardiac arrest – experienced LQTS-triggered cardiac events during sporting activities. "He received 2 appropriate ventricular fibrillation–terminating ICD shocks, both while warming up before games," the authors wrote. "Each episode occurred in the setting of admitted beta-blocker nonadherence."
All of the LQTS athletes seen during the period of study were managed via the same protocol, which, at the Mayo Clinic, includes providing the patient and his or her family with information to enable them to make an informed decision regarding continued sports participation.
Specifically, according to the authors, this includes a comprehensive clinical and genetic evaluation; a consultation with LQTS experts as needed; extensive counseling regarding individual risks and athletic guidelines; tailored therapy (beta-blockers, left cardiac sympathetic denervation, and/or an ICD); education regarding appropriate hydration and electrolyte replenishment; minimizing elevations of core body temperature; and avoidance of QT drugs. Furthermore, all athletes received an automatic external defibrillator to be kept with their sports gear at all sporting events and practices, and relevant school and athletic officials and coaches were informed of the athlete’s condition, they wrote.
Despite the study’s small sample size and limited follow-up, the low rate of cardiac events per athlete year studied (0.003, or 1 event in 331 athlete years) suggests that exercise and sports participation are "manageable risks" in well-counseled, well-managed LQTS patients, Dr. Ackerman said. "We don’t think it’s necessary to control these risks by telling patients they can’t participate in their sport or get too excited," he said.
However, he noted that limiting sports participation may ultimately be in the best interest of certain patients, depending on their individual situation. In all cases, "patients have to be evaluated, risk-stratified, treated, and counseled carefully. The decision to continue has to be an informed one," he said.
Dr. Ackerman is a consultant for Biotronik, Boston Scientific, Medtronic, St. Jude Medical, and Transgenomic. Dr. Johnson reported having no financial disclosures.
FROM JAMA
Major Finding: Among 130 athletes with LQTS who chose to continue participating in competitive sports, only one experienced a syndrome-triggered, potentially fatal arrhythmia over a mean 5.1 years of follow-up.
Data Source: Findings are based on a retrospective study of 353 patients who were evaluated in the Mayo LQTS clinic between July 2000 and November 2010, including 130 LQTS patients (mean age, 11 years) who chose to continue athletic participation.
Disclosures: Dr. Ackerman is a consultant for Biotronik, Boston Scientific, Medtronic, St. Jude Medical, and Transgenomic. Dr. Johnson had no financial disclosures.