User login
“Just Getting a Cup of Coffee”—Considering Best Practices for Patients’ Movement off the Hospital Floor
A 58-year-old man with a remote history of endocarditis and no prior injection drug use was admitted to the inpatient medicine service with fever and concern for recurrent endocarditis. A transthoracic echocardiogram was unremarkable and the patient remained clinically stable. A transesophageal echocardiogram (TEE) was scheduled for the following morning, but during nursing rounds, the patient was missing from his room. Multiple staff members searched for the patient and eventually located him in the hospital lobby drinking a cup of coffee purchased from the cafeteria. Despite his opposition, he was escorted back to his room and advised to not leave the floor again. Later that day, the patient became frustrated and left the hospital before his scheduled TEE. He was subsequently lost to follow-up.
INTRODUCTION
Patients are admitted to the hospital based upon a medical determination that the patient requires acute observation, evaluation, or treatment. Once admitted, healthcare providers may impose restrictions on the patient’s movement in the hospital, such as restrictions on leaving their assigned floor. Managing the movement of hospitalized patients poses significant challenges for the clinical staff because of the difficulty of providing a treatment environment that ensures safe and efficient delivery of care while promoting patients’ preferences for an unrestrictive environment that respects their independence.1,2 Broad limits may make it easier for staff to care for patients and reduce concerns about liability, but they may also frustrate patients who may be medically, psychiatrically, and physically stable and do not require stringent monitoring (eg, completing a course of intravenous antibiotics or awaiting placement at outside facilities).
Although this issue has broad implications for patient safety and hospital liability, authoritative guidance and evidence-based literature are lacking. Without clear guidelines, healthcare staff members are likely to spend more time in managing each individual request to leave the floor because they do not have a systematic strategy for making fair and consistent decisions. Here, we describe the patient and institutional considerations when managing patient movement in the hospital. We refer to “patient movement” specifically as a patient’s choice to move to different locations within the hospital, but outside of their assigned room and/or floor. This does not include scheduled, supervised ambulation activities, such as physical therapy.
POTENTIAL CONSEQUENCES OF LIBERALIZING AND RESTRICTING INPATIENT MOVEMENT
Practices that promote patient movement offer significant benefits and risks. Enhancing movement is likely to reduce the “physiologic disruption”3 of hospitalization while improving patients’ overall satisfaction and alignment with patient-centered care. Liberalized movement also promotes independence and ambulation that reduces the rate of physical deconditioning.4
Despite theoretical benefits, hospitals may be more concerned about adverse events related to patient movement, such as falls, the use of illicit substances, or elopement. Given that hospitals may be legally5 and financially responsible6 for adverse events associated with patient movement, allowances for off-floor movement should be carefully considered with input from risk management, physicians, nursing leadership, patient advocates, and hospital administration.
Additionally, unannounced movement off the floor may interfere with timely and efficient care by causing lapses in monitoring, such as cardiac telemetry,7 medication administration, and scheduled diagnostic tests. In these situations, the risks of patient absence from the floor are significant and may ultimately negate the benefits of continued hospitalization by compromising the central elements of patient care.
CLINICAL CONSIDERATIONS
Patients’ requests to leave the hospital floor should be evaluated systemically and transparently to promote fair, high-value care. First, a request for liberalized movement should prompt physicians that the patient may no longer require hospitalization and may be ready for the transition to outpatient care.8 If the patient still requires inpatient care, then the medical practitioner should make a clinical determination if the patient is medically stable enough to leave their hospital floor. The provider should first identify when the liberalization of movement would be universally inappropriate, such as in patients who are physically unable to ambulate without posing significant harm to themselves. This includes an accidental fall (usually while walking5), which is one of the most commonly reported adverse events in an inpatient setting.9 Additionally, patients with significant cognitive impairments or those lacking in decision-making capacity may be restricted from leaving their floors unescorted, as they are at a higher risk of disorientation, falls, and death.10
In determining movement restrictions for patients in isolation, hospitals should refer to the existing guidelines on isolation precautions for the transmission of communicable infections11,12 and neutropenic precautions.13 Additionally, movement restriction for patients who are isolated after screening positive for certain drug-resistant organisms (eg, methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci) is controversial and should be evaluated based on the available medical evidence and standards.14-16
When making a risk-benefit determination about movement, providers should also assess the intent and the potentially unmet needs behind the patient’s request. Patient-centered reasons for enhanced freedom of movement within the hospital include a desire for exercise, greater food choice, and visiting with loved ones, all of which can enable patients to manage the well-known inconveniences and stresses of hospitalization. In contrast, there may be concerns for other intentions behind leaving assigned floors based on the patient’s clinical history, such as the surreptitious use of illicit substances or attempts to elope from the hospital. Advising restriction of movement is justifiable if there is a significant concern for behavior that undermines the safe delivery of care. In patients with active substance use disorders, the appropriate treatment of pain or withdrawal symptoms may better address the patients’ unmet needs, but a lower threshold to restrict movement may be reasonable given the significant risks involved. However, given the widespread stigmatization of patients with substance use disorders,17 institutional policy and clinicians should adhere to systematic, transparent, and consistent risk assessments for all patients in order to minimize the potential for introducing or exacerbating disparities in care.
ETHICAL CONSIDERATIONS
In order to work productively with admitted patients, strong practices honor patients’ autonomy by specifying
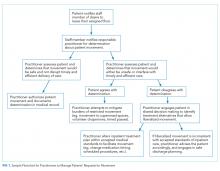
Patients may request or even demand to leave the floor after a healthcare provider has determined that doing so would be unsafe and/or undermine the timely and efficient delivery of care. In these cases, shared decision-making (SDM) can help identify acceptable solutions within the identified constraints. SDM combines the physicians’ experience, expertise, and knowledge of medical evidence with patients’ values, needs, and preferences for care.19 If patients continue to request to leave the floor after the restriction has been communicated, physicians should discuss whether the current treatment plan should be renegotiated to include a relatively minor modification (eg, a change in the timing or route of administration of medication). If inpatient care cannot be provided safely within the patient’s preferences for movement and attempts to accommodate the patient’s preferences are unsuccessful, then a shift to discharge planning may be appropriate. A summary of this decision process is outlined in the Figure.
Of note, physicians’ decisions about the appropriateness of patient movement could conflict with the existing institutional procedures or policies (eg, a physician deems increased patient movement to carry minimal risks, while the institution seeks to restrict movement due to concerns about liability). For this reason, it is important for clinicians to participate in the development of institutional policy to ensure that it reflects the clinical and ethical considerations that clinicians apply to patient care. A policy designed with input from relevant stakeholders across the institution including legal, nursing, physicians, administration, ethics, risk management, and patient advocates can provide expert guidance that is based on and consistent with the institution’s mission, values, and priorities.20
ENHANCING SAFE MOVEMENT
In mitigating the burdens of restriction on movement, hospitals may implement a range of options that address patients’ preferences while maintaining safety. Given the potential consequences of liberalized patient movement, it may be prudent to implement these safeguards as a compromise that addresses both the patients’ needs and the hospital’s concerns. These could include an escort for off-floor supervision, timed passes to leave the floor, or volunteers purchasing food for patients from the cafeteria. Creating open, supervised spaces within the hospital (eg, lounges) may also help provide the respite patients need, but in a safe and medically structured environment.
CONCLUSION
Returning to the introductory case example, we now present an alternative outcome in the context of the practices described above. On the morning of the scheduled TEE, a nurse noted that the patient was missing from his room. Before the staff began searching for the patient, they consulted the medical record which included the admission discussion and agreement to expectations for inpatient movement. The record also included an informed consent discussion indicating the minimal risks of leaving the floor, as the patient could ambulate independently and had no need for continuous monitoring. Finally, a physician’s order authorized the patient to be off the floor until 10
The above scenario highlights the benefits of a comprehensive framework for patient movement practices that are transparent, fair, and systematic. Explicitly recognizing competing institutional and patient perspectives can prevent conflict and promote high-quality, safe, efficient, patient-centered care that only restricts the patient’s movement under specified and justifiable conditions. In developing strong hospital practices, institutions should refer to the relevant clinical and ethical standards and draw upon their institutional resources in risk management, clinical staff, and patient advocates.
Acknowledgments
The authors thank Dr. Neil Shapiro and Dr. David Chuquin for their constructive reviews of prior versions of this manuscript.
Disclosures
The authors have no financial conflicts of interest to disclose.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs, the US Government, or the VA National Center for Ethics in Health Care.
1. Smith T. Wandering off the floors: safety and security risks of patient wandering. PSNet Patient Safety Network. Web M&M 2014. Accessed December 4, 2017.
2. Douglas CH, Douglas MR. Patient-friendly hospital environments: exploring the patients’ perspective. Health Expect. 2004;7(1):61-73. https://doi.org/10.1046/j.1369-6513.2003.00251.x.
3. Detsky AS, Krumholz HM. Reducing the trauma of hospitalization. JAMA. 2014;311(21):2169-2170. https://doi.org/10.1001/jama.2014.3695
4. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure.” JAMA. 2011;306(16):1782-1793. https://doi.org/10.1001/jama.2011.1556.
5. Oliver D, Killick S, Even T, Willmott M. Do falls and falls-injuries in hospital indicate negligent care-and how big is the risk? A retrospective analysis of the NHS Litigation Authority Database of clinical negligence claims, resulting from falls in hospitals in England 1995 to 2006. Qual Saf Health Care. 2008;17(6):431-436. https://doi.org/10.1136/qshc.2007.024703.
6. Mello MM, Chandra A, Gawande AA, Studdert DM. National costs of the medical liability system. Health Aff (Millwood). 2010;29(9):1569-1577. https://doi.org/10.1377/hlthaff.2009.0807.
7. Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med. 2014;174(11):1852-1854. https://doi.org/10.1001/jamainternmed.2014.4491.
8. Conley J, O’Brien CW, Leff BA, Bolen S, Zulman D. Alternative strategies to inpatient hospitalization for acute medical conditions: a systematic review. JAMA Intern Med. 2016;176(11):1693-1702. https://doi.org/10.1001/jamainternmed.2016.5974.
9. Halfon P, Eggli Y, Van Melle G, Vagnair A. Risk of falls for hospitalized patients: a predictive model based on routinely available data. J Clin Epidemiol. 2001;54(12):1258-1266. https://doi.org/10.1016/S0895-4356(01)00406-1
10. Rowe M. Wandering in hospitalized older adults: identifying risk is the first step in this approach to preventing wandering in patients with dementia. Am J Nurs. 2008;108(10):62-70. https://doi.org/10.1097/01.NAJ.0000336968.32462.c9.
11. Siegel JD, Rhinehart E, Jackson M, Chiarello L. Health care infection control practices advisory C. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35(10 Suppl 2):S65-S164. https://doi.org/10.1016/j.ajic.2007.10.007
12. Ito Y, Nagao M, Iinuma Y, et al. Risk factors for nosocomial tuberculosis transmission among health care workers. Am J Infect Control. 2016;44(5):596-598. https://doi.org/10.1016/j.ajic.2015.11.022.
13. Freifeld AG, Bow EJ, Sepkowitz KA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2011;52(4):e56-e93. https://doi.org/10.1093/cid/ciq147
14. Martin EM, Russell D, Rubin Z, et al. Elimination of routine contact precautions for endemic methicillin-resistant staphylococcus aureus and vancomycin-resistant enterococcus: a retrospective quasi-experimental study. Infect Control Hosp Epidemiol. 2016;37(11):1323-1330. https://doi.org/10.1017/ice.2016.156
15. Morgan DJ, Murthy R, Munoz-Price LS, et al. Reconsidering contact precautions for endemic methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus. Infect Control Hosp Epidemiol. 2015;36(10):1163-1172. https://doi.org/10.1017/ice.2015.156.
16. Fatkenheuer G, Hirschel B, Harbarth S. Screening and isolation to control meticillin-resistant Staphylococcus aureus: sense, nonsense, and evidence. Lancet. 2015;385(9973):1146-1149. https://doi.org/10.1016/S0140-6736(14)60660-7.
17. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. https://doi.org/10.1016/j.drugalcdep.2013.02.018.
18. Handel DA, Fu R, Daya M, York J, Larson E, John McConnell K. The use of scripting at triage and its impact on elopements. Acad Emerg Med. 2010;17(5):495-500. https://doi.org/10.1111/j.1553-2712.2010.00721.x.
19. Barry MJ, Edgman-Levitan S. Shared decision making-pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780-781. https://doi.org/10.1056/NEJMp1109283.
20. Donn SM. Medical liability, risk management, and the quality of health care. Semin Fetal Neonatal Med. 2005;10(1):3-9. https://doi.org/10.1016/j.siny.2004.09.004.
A 58-year-old man with a remote history of endocarditis and no prior injection drug use was admitted to the inpatient medicine service with fever and concern for recurrent endocarditis. A transthoracic echocardiogram was unremarkable and the patient remained clinically stable. A transesophageal echocardiogram (TEE) was scheduled for the following morning, but during nursing rounds, the patient was missing from his room. Multiple staff members searched for the patient and eventually located him in the hospital lobby drinking a cup of coffee purchased from the cafeteria. Despite his opposition, he was escorted back to his room and advised to not leave the floor again. Later that day, the patient became frustrated and left the hospital before his scheduled TEE. He was subsequently lost to follow-up.
INTRODUCTION
Patients are admitted to the hospital based upon a medical determination that the patient requires acute observation, evaluation, or treatment. Once admitted, healthcare providers may impose restrictions on the patient’s movement in the hospital, such as restrictions on leaving their assigned floor. Managing the movement of hospitalized patients poses significant challenges for the clinical staff because of the difficulty of providing a treatment environment that ensures safe and efficient delivery of care while promoting patients’ preferences for an unrestrictive environment that respects their independence.1,2 Broad limits may make it easier for staff to care for patients and reduce concerns about liability, but they may also frustrate patients who may be medically, psychiatrically, and physically stable and do not require stringent monitoring (eg, completing a course of intravenous antibiotics or awaiting placement at outside facilities).
Although this issue has broad implications for patient safety and hospital liability, authoritative guidance and evidence-based literature are lacking. Without clear guidelines, healthcare staff members are likely to spend more time in managing each individual request to leave the floor because they do not have a systematic strategy for making fair and consistent decisions. Here, we describe the patient and institutional considerations when managing patient movement in the hospital. We refer to “patient movement” specifically as a patient’s choice to move to different locations within the hospital, but outside of their assigned room and/or floor. This does not include scheduled, supervised ambulation activities, such as physical therapy.
POTENTIAL CONSEQUENCES OF LIBERALIZING AND RESTRICTING INPATIENT MOVEMENT
Practices that promote patient movement offer significant benefits and risks. Enhancing movement is likely to reduce the “physiologic disruption”3 of hospitalization while improving patients’ overall satisfaction and alignment with patient-centered care. Liberalized movement also promotes independence and ambulation that reduces the rate of physical deconditioning.4
Despite theoretical benefits, hospitals may be more concerned about adverse events related to patient movement, such as falls, the use of illicit substances, or elopement. Given that hospitals may be legally5 and financially responsible6 for adverse events associated with patient movement, allowances for off-floor movement should be carefully considered with input from risk management, physicians, nursing leadership, patient advocates, and hospital administration.
Additionally, unannounced movement off the floor may interfere with timely and efficient care by causing lapses in monitoring, such as cardiac telemetry,7 medication administration, and scheduled diagnostic tests. In these situations, the risks of patient absence from the floor are significant and may ultimately negate the benefits of continued hospitalization by compromising the central elements of patient care.
CLINICAL CONSIDERATIONS
Patients’ requests to leave the hospital floor should be evaluated systemically and transparently to promote fair, high-value care. First, a request for liberalized movement should prompt physicians that the patient may no longer require hospitalization and may be ready for the transition to outpatient care.8 If the patient still requires inpatient care, then the medical practitioner should make a clinical determination if the patient is medically stable enough to leave their hospital floor. The provider should first identify when the liberalization of movement would be universally inappropriate, such as in patients who are physically unable to ambulate without posing significant harm to themselves. This includes an accidental fall (usually while walking5), which is one of the most commonly reported adverse events in an inpatient setting.9 Additionally, patients with significant cognitive impairments or those lacking in decision-making capacity may be restricted from leaving their floors unescorted, as they are at a higher risk of disorientation, falls, and death.10
In determining movement restrictions for patients in isolation, hospitals should refer to the existing guidelines on isolation precautions for the transmission of communicable infections11,12 and neutropenic precautions.13 Additionally, movement restriction for patients who are isolated after screening positive for certain drug-resistant organisms (eg, methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci) is controversial and should be evaluated based on the available medical evidence and standards.14-16
When making a risk-benefit determination about movement, providers should also assess the intent and the potentially unmet needs behind the patient’s request. Patient-centered reasons for enhanced freedom of movement within the hospital include a desire for exercise, greater food choice, and visiting with loved ones, all of which can enable patients to manage the well-known inconveniences and stresses of hospitalization. In contrast, there may be concerns for other intentions behind leaving assigned floors based on the patient’s clinical history, such as the surreptitious use of illicit substances or attempts to elope from the hospital. Advising restriction of movement is justifiable if there is a significant concern for behavior that undermines the safe delivery of care. In patients with active substance use disorders, the appropriate treatment of pain or withdrawal symptoms may better address the patients’ unmet needs, but a lower threshold to restrict movement may be reasonable given the significant risks involved. However, given the widespread stigmatization of patients with substance use disorders,17 institutional policy and clinicians should adhere to systematic, transparent, and consistent risk assessments for all patients in order to minimize the potential for introducing or exacerbating disparities in care.
ETHICAL CONSIDERATIONS
In order to work productively with admitted patients, strong practices honor patients’ autonomy by specifying
Patients may request or even demand to leave the floor after a healthcare provider has determined that doing so would be unsafe and/or undermine the timely and efficient delivery of care. In these cases, shared decision-making (SDM) can help identify acceptable solutions within the identified constraints. SDM combines the physicians’ experience, expertise, and knowledge of medical evidence with patients’ values, needs, and preferences for care.19 If patients continue to request to leave the floor after the restriction has been communicated, physicians should discuss whether the current treatment plan should be renegotiated to include a relatively minor modification (eg, a change in the timing or route of administration of medication). If inpatient care cannot be provided safely within the patient’s preferences for movement and attempts to accommodate the patient’s preferences are unsuccessful, then a shift to discharge planning may be appropriate. A summary of this decision process is outlined in the Figure.
Of note, physicians’ decisions about the appropriateness of patient movement could conflict with the existing institutional procedures or policies (eg, a physician deems increased patient movement to carry minimal risks, while the institution seeks to restrict movement due to concerns about liability). For this reason, it is important for clinicians to participate in the development of institutional policy to ensure that it reflects the clinical and ethical considerations that clinicians apply to patient care. A policy designed with input from relevant stakeholders across the institution including legal, nursing, physicians, administration, ethics, risk management, and patient advocates can provide expert guidance that is based on and consistent with the institution’s mission, values, and priorities.20
ENHANCING SAFE MOVEMENT
In mitigating the burdens of restriction on movement, hospitals may implement a range of options that address patients’ preferences while maintaining safety. Given the potential consequences of liberalized patient movement, it may be prudent to implement these safeguards as a compromise that addresses both the patients’ needs and the hospital’s concerns. These could include an escort for off-floor supervision, timed passes to leave the floor, or volunteers purchasing food for patients from the cafeteria. Creating open, supervised spaces within the hospital (eg, lounges) may also help provide the respite patients need, but in a safe and medically structured environment.
CONCLUSION
Returning to the introductory case example, we now present an alternative outcome in the context of the practices described above. On the morning of the scheduled TEE, a nurse noted that the patient was missing from his room. Before the staff began searching for the patient, they consulted the medical record which included the admission discussion and agreement to expectations for inpatient movement. The record also included an informed consent discussion indicating the minimal risks of leaving the floor, as the patient could ambulate independently and had no need for continuous monitoring. Finally, a physician’s order authorized the patient to be off the floor until 10
The above scenario highlights the benefits of a comprehensive framework for patient movement practices that are transparent, fair, and systematic. Explicitly recognizing competing institutional and patient perspectives can prevent conflict and promote high-quality, safe, efficient, patient-centered care that only restricts the patient’s movement under specified and justifiable conditions. In developing strong hospital practices, institutions should refer to the relevant clinical and ethical standards and draw upon their institutional resources in risk management, clinical staff, and patient advocates.
Acknowledgments
The authors thank Dr. Neil Shapiro and Dr. David Chuquin for their constructive reviews of prior versions of this manuscript.
Disclosures
The authors have no financial conflicts of interest to disclose.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs, the US Government, or the VA National Center for Ethics in Health Care.
A 58-year-old man with a remote history of endocarditis and no prior injection drug use was admitted to the inpatient medicine service with fever and concern for recurrent endocarditis. A transthoracic echocardiogram was unremarkable and the patient remained clinically stable. A transesophageal echocardiogram (TEE) was scheduled for the following morning, but during nursing rounds, the patient was missing from his room. Multiple staff members searched for the patient and eventually located him in the hospital lobby drinking a cup of coffee purchased from the cafeteria. Despite his opposition, he was escorted back to his room and advised to not leave the floor again. Later that day, the patient became frustrated and left the hospital before his scheduled TEE. He was subsequently lost to follow-up.
INTRODUCTION
Patients are admitted to the hospital based upon a medical determination that the patient requires acute observation, evaluation, or treatment. Once admitted, healthcare providers may impose restrictions on the patient’s movement in the hospital, such as restrictions on leaving their assigned floor. Managing the movement of hospitalized patients poses significant challenges for the clinical staff because of the difficulty of providing a treatment environment that ensures safe and efficient delivery of care while promoting patients’ preferences for an unrestrictive environment that respects their independence.1,2 Broad limits may make it easier for staff to care for patients and reduce concerns about liability, but they may also frustrate patients who may be medically, psychiatrically, and physically stable and do not require stringent monitoring (eg, completing a course of intravenous antibiotics or awaiting placement at outside facilities).
Although this issue has broad implications for patient safety and hospital liability, authoritative guidance and evidence-based literature are lacking. Without clear guidelines, healthcare staff members are likely to spend more time in managing each individual request to leave the floor because they do not have a systematic strategy for making fair and consistent decisions. Here, we describe the patient and institutional considerations when managing patient movement in the hospital. We refer to “patient movement” specifically as a patient’s choice to move to different locations within the hospital, but outside of their assigned room and/or floor. This does not include scheduled, supervised ambulation activities, such as physical therapy.
POTENTIAL CONSEQUENCES OF LIBERALIZING AND RESTRICTING INPATIENT MOVEMENT
Practices that promote patient movement offer significant benefits and risks. Enhancing movement is likely to reduce the “physiologic disruption”3 of hospitalization while improving patients’ overall satisfaction and alignment with patient-centered care. Liberalized movement also promotes independence and ambulation that reduces the rate of physical deconditioning.4
Despite theoretical benefits, hospitals may be more concerned about adverse events related to patient movement, such as falls, the use of illicit substances, or elopement. Given that hospitals may be legally5 and financially responsible6 for adverse events associated with patient movement, allowances for off-floor movement should be carefully considered with input from risk management, physicians, nursing leadership, patient advocates, and hospital administration.
Additionally, unannounced movement off the floor may interfere with timely and efficient care by causing lapses in monitoring, such as cardiac telemetry,7 medication administration, and scheduled diagnostic tests. In these situations, the risks of patient absence from the floor are significant and may ultimately negate the benefits of continued hospitalization by compromising the central elements of patient care.
CLINICAL CONSIDERATIONS
Patients’ requests to leave the hospital floor should be evaluated systemically and transparently to promote fair, high-value care. First, a request for liberalized movement should prompt physicians that the patient may no longer require hospitalization and may be ready for the transition to outpatient care.8 If the patient still requires inpatient care, then the medical practitioner should make a clinical determination if the patient is medically stable enough to leave their hospital floor. The provider should first identify when the liberalization of movement would be universally inappropriate, such as in patients who are physically unable to ambulate without posing significant harm to themselves. This includes an accidental fall (usually while walking5), which is one of the most commonly reported adverse events in an inpatient setting.9 Additionally, patients with significant cognitive impairments or those lacking in decision-making capacity may be restricted from leaving their floors unescorted, as they are at a higher risk of disorientation, falls, and death.10
In determining movement restrictions for patients in isolation, hospitals should refer to the existing guidelines on isolation precautions for the transmission of communicable infections11,12 and neutropenic precautions.13 Additionally, movement restriction for patients who are isolated after screening positive for certain drug-resistant organisms (eg, methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci) is controversial and should be evaluated based on the available medical evidence and standards.14-16
When making a risk-benefit determination about movement, providers should also assess the intent and the potentially unmet needs behind the patient’s request. Patient-centered reasons for enhanced freedom of movement within the hospital include a desire for exercise, greater food choice, and visiting with loved ones, all of which can enable patients to manage the well-known inconveniences and stresses of hospitalization. In contrast, there may be concerns for other intentions behind leaving assigned floors based on the patient’s clinical history, such as the surreptitious use of illicit substances or attempts to elope from the hospital. Advising restriction of movement is justifiable if there is a significant concern for behavior that undermines the safe delivery of care. In patients with active substance use disorders, the appropriate treatment of pain or withdrawal symptoms may better address the patients’ unmet needs, but a lower threshold to restrict movement may be reasonable given the significant risks involved. However, given the widespread stigmatization of patients with substance use disorders,17 institutional policy and clinicians should adhere to systematic, transparent, and consistent risk assessments for all patients in order to minimize the potential for introducing or exacerbating disparities in care.
ETHICAL CONSIDERATIONS
In order to work productively with admitted patients, strong practices honor patients’ autonomy by specifying
Patients may request or even demand to leave the floor after a healthcare provider has determined that doing so would be unsafe and/or undermine the timely and efficient delivery of care. In these cases, shared decision-making (SDM) can help identify acceptable solutions within the identified constraints. SDM combines the physicians’ experience, expertise, and knowledge of medical evidence with patients’ values, needs, and preferences for care.19 If patients continue to request to leave the floor after the restriction has been communicated, physicians should discuss whether the current treatment plan should be renegotiated to include a relatively minor modification (eg, a change in the timing or route of administration of medication). If inpatient care cannot be provided safely within the patient’s preferences for movement and attempts to accommodate the patient’s preferences are unsuccessful, then a shift to discharge planning may be appropriate. A summary of this decision process is outlined in the Figure.
Of note, physicians’ decisions about the appropriateness of patient movement could conflict with the existing institutional procedures or policies (eg, a physician deems increased patient movement to carry minimal risks, while the institution seeks to restrict movement due to concerns about liability). For this reason, it is important for clinicians to participate in the development of institutional policy to ensure that it reflects the clinical and ethical considerations that clinicians apply to patient care. A policy designed with input from relevant stakeholders across the institution including legal, nursing, physicians, administration, ethics, risk management, and patient advocates can provide expert guidance that is based on and consistent with the institution’s mission, values, and priorities.20
ENHANCING SAFE MOVEMENT
In mitigating the burdens of restriction on movement, hospitals may implement a range of options that address patients’ preferences while maintaining safety. Given the potential consequences of liberalized patient movement, it may be prudent to implement these safeguards as a compromise that addresses both the patients’ needs and the hospital’s concerns. These could include an escort for off-floor supervision, timed passes to leave the floor, or volunteers purchasing food for patients from the cafeteria. Creating open, supervised spaces within the hospital (eg, lounges) may also help provide the respite patients need, but in a safe and medically structured environment.
CONCLUSION
Returning to the introductory case example, we now present an alternative outcome in the context of the practices described above. On the morning of the scheduled TEE, a nurse noted that the patient was missing from his room. Before the staff began searching for the patient, they consulted the medical record which included the admission discussion and agreement to expectations for inpatient movement. The record also included an informed consent discussion indicating the minimal risks of leaving the floor, as the patient could ambulate independently and had no need for continuous monitoring. Finally, a physician’s order authorized the patient to be off the floor until 10
The above scenario highlights the benefits of a comprehensive framework for patient movement practices that are transparent, fair, and systematic. Explicitly recognizing competing institutional and patient perspectives can prevent conflict and promote high-quality, safe, efficient, patient-centered care that only restricts the patient’s movement under specified and justifiable conditions. In developing strong hospital practices, institutions should refer to the relevant clinical and ethical standards and draw upon their institutional resources in risk management, clinical staff, and patient advocates.
Acknowledgments
The authors thank Dr. Neil Shapiro and Dr. David Chuquin for their constructive reviews of prior versions of this manuscript.
Disclosures
The authors have no financial conflicts of interest to disclose.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs, the US Government, or the VA National Center for Ethics in Health Care.
1. Smith T. Wandering off the floors: safety and security risks of patient wandering. PSNet Patient Safety Network. Web M&M 2014. Accessed December 4, 2017.
2. Douglas CH, Douglas MR. Patient-friendly hospital environments: exploring the patients’ perspective. Health Expect. 2004;7(1):61-73. https://doi.org/10.1046/j.1369-6513.2003.00251.x.
3. Detsky AS, Krumholz HM. Reducing the trauma of hospitalization. JAMA. 2014;311(21):2169-2170. https://doi.org/10.1001/jama.2014.3695
4. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure.” JAMA. 2011;306(16):1782-1793. https://doi.org/10.1001/jama.2011.1556.
5. Oliver D, Killick S, Even T, Willmott M. Do falls and falls-injuries in hospital indicate negligent care-and how big is the risk? A retrospective analysis of the NHS Litigation Authority Database of clinical negligence claims, resulting from falls in hospitals in England 1995 to 2006. Qual Saf Health Care. 2008;17(6):431-436. https://doi.org/10.1136/qshc.2007.024703.
6. Mello MM, Chandra A, Gawande AA, Studdert DM. National costs of the medical liability system. Health Aff (Millwood). 2010;29(9):1569-1577. https://doi.org/10.1377/hlthaff.2009.0807.
7. Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med. 2014;174(11):1852-1854. https://doi.org/10.1001/jamainternmed.2014.4491.
8. Conley J, O’Brien CW, Leff BA, Bolen S, Zulman D. Alternative strategies to inpatient hospitalization for acute medical conditions: a systematic review. JAMA Intern Med. 2016;176(11):1693-1702. https://doi.org/10.1001/jamainternmed.2016.5974.
9. Halfon P, Eggli Y, Van Melle G, Vagnair A. Risk of falls for hospitalized patients: a predictive model based on routinely available data. J Clin Epidemiol. 2001;54(12):1258-1266. https://doi.org/10.1016/S0895-4356(01)00406-1
10. Rowe M. Wandering in hospitalized older adults: identifying risk is the first step in this approach to preventing wandering in patients with dementia. Am J Nurs. 2008;108(10):62-70. https://doi.org/10.1097/01.NAJ.0000336968.32462.c9.
11. Siegel JD, Rhinehart E, Jackson M, Chiarello L. Health care infection control practices advisory C. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35(10 Suppl 2):S65-S164. https://doi.org/10.1016/j.ajic.2007.10.007
12. Ito Y, Nagao M, Iinuma Y, et al. Risk factors for nosocomial tuberculosis transmission among health care workers. Am J Infect Control. 2016;44(5):596-598. https://doi.org/10.1016/j.ajic.2015.11.022.
13. Freifeld AG, Bow EJ, Sepkowitz KA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2011;52(4):e56-e93. https://doi.org/10.1093/cid/ciq147
14. Martin EM, Russell D, Rubin Z, et al. Elimination of routine contact precautions for endemic methicillin-resistant staphylococcus aureus and vancomycin-resistant enterococcus: a retrospective quasi-experimental study. Infect Control Hosp Epidemiol. 2016;37(11):1323-1330. https://doi.org/10.1017/ice.2016.156
15. Morgan DJ, Murthy R, Munoz-Price LS, et al. Reconsidering contact precautions for endemic methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus. Infect Control Hosp Epidemiol. 2015;36(10):1163-1172. https://doi.org/10.1017/ice.2015.156.
16. Fatkenheuer G, Hirschel B, Harbarth S. Screening and isolation to control meticillin-resistant Staphylococcus aureus: sense, nonsense, and evidence. Lancet. 2015;385(9973):1146-1149. https://doi.org/10.1016/S0140-6736(14)60660-7.
17. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. https://doi.org/10.1016/j.drugalcdep.2013.02.018.
18. Handel DA, Fu R, Daya M, York J, Larson E, John McConnell K. The use of scripting at triage and its impact on elopements. Acad Emerg Med. 2010;17(5):495-500. https://doi.org/10.1111/j.1553-2712.2010.00721.x.
19. Barry MJ, Edgman-Levitan S. Shared decision making-pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780-781. https://doi.org/10.1056/NEJMp1109283.
20. Donn SM. Medical liability, risk management, and the quality of health care. Semin Fetal Neonatal Med. 2005;10(1):3-9. https://doi.org/10.1016/j.siny.2004.09.004.
1. Smith T. Wandering off the floors: safety and security risks of patient wandering. PSNet Patient Safety Network. Web M&M 2014. Accessed December 4, 2017.
2. Douglas CH, Douglas MR. Patient-friendly hospital environments: exploring the patients’ perspective. Health Expect. 2004;7(1):61-73. https://doi.org/10.1046/j.1369-6513.2003.00251.x.
3. Detsky AS, Krumholz HM. Reducing the trauma of hospitalization. JAMA. 2014;311(21):2169-2170. https://doi.org/10.1001/jama.2014.3695
4. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure.” JAMA. 2011;306(16):1782-1793. https://doi.org/10.1001/jama.2011.1556.
5. Oliver D, Killick S, Even T, Willmott M. Do falls and falls-injuries in hospital indicate negligent care-and how big is the risk? A retrospective analysis of the NHS Litigation Authority Database of clinical negligence claims, resulting from falls in hospitals in England 1995 to 2006. Qual Saf Health Care. 2008;17(6):431-436. https://doi.org/10.1136/qshc.2007.024703.
6. Mello MM, Chandra A, Gawande AA, Studdert DM. National costs of the medical liability system. Health Aff (Millwood). 2010;29(9):1569-1577. https://doi.org/10.1377/hlthaff.2009.0807.
7. Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med. 2014;174(11):1852-1854. https://doi.org/10.1001/jamainternmed.2014.4491.
8. Conley J, O’Brien CW, Leff BA, Bolen S, Zulman D. Alternative strategies to inpatient hospitalization for acute medical conditions: a systematic review. JAMA Intern Med. 2016;176(11):1693-1702. https://doi.org/10.1001/jamainternmed.2016.5974.
9. Halfon P, Eggli Y, Van Melle G, Vagnair A. Risk of falls for hospitalized patients: a predictive model based on routinely available data. J Clin Epidemiol. 2001;54(12):1258-1266. https://doi.org/10.1016/S0895-4356(01)00406-1
10. Rowe M. Wandering in hospitalized older adults: identifying risk is the first step in this approach to preventing wandering in patients with dementia. Am J Nurs. 2008;108(10):62-70. https://doi.org/10.1097/01.NAJ.0000336968.32462.c9.
11. Siegel JD, Rhinehart E, Jackson M, Chiarello L. Health care infection control practices advisory C. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35(10 Suppl 2):S65-S164. https://doi.org/10.1016/j.ajic.2007.10.007
12. Ito Y, Nagao M, Iinuma Y, et al. Risk factors for nosocomial tuberculosis transmission among health care workers. Am J Infect Control. 2016;44(5):596-598. https://doi.org/10.1016/j.ajic.2015.11.022.
13. Freifeld AG, Bow EJ, Sepkowitz KA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2011;52(4):e56-e93. https://doi.org/10.1093/cid/ciq147
14. Martin EM, Russell D, Rubin Z, et al. Elimination of routine contact precautions for endemic methicillin-resistant staphylococcus aureus and vancomycin-resistant enterococcus: a retrospective quasi-experimental study. Infect Control Hosp Epidemiol. 2016;37(11):1323-1330. https://doi.org/10.1017/ice.2016.156
15. Morgan DJ, Murthy R, Munoz-Price LS, et al. Reconsidering contact precautions for endemic methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus. Infect Control Hosp Epidemiol. 2015;36(10):1163-1172. https://doi.org/10.1017/ice.2015.156.
16. Fatkenheuer G, Hirschel B, Harbarth S. Screening and isolation to control meticillin-resistant Staphylococcus aureus: sense, nonsense, and evidence. Lancet. 2015;385(9973):1146-1149. https://doi.org/10.1016/S0140-6736(14)60660-7.
17. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. https://doi.org/10.1016/j.drugalcdep.2013.02.018.
18. Handel DA, Fu R, Daya M, York J, Larson E, John McConnell K. The use of scripting at triage and its impact on elopements. Acad Emerg Med. 2010;17(5):495-500. https://doi.org/10.1111/j.1553-2712.2010.00721.x.
19. Barry MJ, Edgman-Levitan S. Shared decision making-pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780-781. https://doi.org/10.1056/NEJMp1109283.
20. Donn SM. Medical liability, risk management, and the quality of health care. Semin Fetal Neonatal Med. 2005;10(1):3-9. https://doi.org/10.1016/j.siny.2004.09.004.
© 2019 Society of Hospital Medicine
Ethical Considerations in the Care of Hospitalized Patients with Opioid Use and Injection Drug Use Disorders
“Lord have mercy on me, was the kneeling drunkard’s plea.”
—Johnny Cash
The Diagnostic and Statistical Manual of the American Psychiatric Association defines opioid-use disorder (OUD) as a problematic pattern of prescription and/or illicit opioid medication use leading to clinically significant impairment or distress.1 Compared with their non-OUD counterparts, patients with OUD have poorer overall health and worse health service outcomes, including higher rates of morbidity, mortality, HIV and HCV transmission, and 30-day readmissions.2 With the rate of fatal overdoses from opioids at crisis levels, leading scientific and professional organizations have declared OUD to be a public health emergency in the United States.3
The opioid epidemic affects hospitalists through the rising incidence of hospitalization, not only as a result of OUD’s indirect complications, but also its direct effects of intoxication and withdrawal.4 In caring for patients with OUD, hospitalists are often presented with many ethical dilemmas. Whether the dilemma involves timing and circumstances of discharge or the permission to leave the hospital floor, they often involve elements of mutual mistrust. In qualitative ethnographic studies, patients with OUD report not trusting that the medical staff will take their concerns of inadequately treated pain and other needs seriously. Providers may mistrust the patient’s report of pain and withhold treatment for OUD for nonclinical reasons.5 Here, we examine two ethical dilemmas specific to OUD in hospitalized patients. Our aim in describing these dilemmas is to help hospitalists recognize that targeting issues of mistrust may assist them to deliver better care to hospitalized patients with OUD.
DISCHARGING HOSPITALIZED PATIENTS WITH OUD
In the inpatient setting, ethical dilemmas surrounding discharge are common among people who inject drugs (PWID). These patients have disproportionately high rates of soft tissue and systemic infections, such as endocarditis and osteomyelitis, and subsequently often require long-term, outpatient parenteral antibiotic therapy (OPAT).6 From both the clinical and ethical perspectives, discharging PWID requiring OPAT to an unsupervised setting or continuing inpatient hospitalization to prevent a potential adverse event are equally imperfect solutions.
These patients may be clinically stable, suitable for discharge, and prefer to be discharged, but the practitioner’s concerns regarding untoward complications frequently override the patient’s wishes. Valid reasons for this exercise of what could be considered soft-paternalism are considered when physicians unilaterally decide what is best for patients, including refusal of community agencies to provide OPAT to PWID, inadequate social support and/or health literacy to administer the therapy, or varying degrees of homelessness that can affect timely follow-up. However, surveys of both hospitalists and infectious disease specialists also indicate that they may avoid discharge because of concerns the PWID will tamper with the intravenous (IV) catheter to inject drugs.7 This reluctance to discharge otherwise socially and medically suitable patients increases length of stay,7 decreases patient satisfaction, and could lead to misuse of limited hospital resources.
Both patient mistrust and stigmatization may contribute to this dilemma. Healthcare professionals have been shown to share and reflect a long-standing bias in their attitudes toward patients with substance-use disorders and OUD, in particular.8 Studies of providers’ attitudes are limited but suggest that legal concerns over liability and professional sanctions,9 reluctance to contribute to the development or relapse of addiction,10 and a strong psychological investment in not being deceived by the patient11 may influence physicians’ decisions about care.
Closely supervising IV antibiotic therapy for all PWID may not reflect current medical knowledge and may imply a moral assessment of patients’ culpability and lack of will power to resist using drugs.12 No evidence is available to suggest that inpatient parenteral antibiotic treatment offers superior adherence, and emerging evidence showing that carefully selected patients with an injection drug-use history can be safely and effectively treated as outpatients has been obtained.13,14 Ho et al. found high rates of treatment success in patients with adequate housing, a reliable guardian, and willingness to comply with appropriate IV catheter use.13 Although the study by Buehrle et al. found higher rates of OPAT failure among PWIDs, 25% of these failures were due to adverse drug reactions and only 2% were due to documented line manipulations.14 This research suggests that disposition to alternative settings for OPAT in PWID may be feasible, reasonable, and deserving of further study. Rather than treating PWIDs as a homogenous group of increased risk, contextualizing care based on individual risk stratification promotes more patient-centered care that is medically appropriate and potentially more cost efficient. A
Patient-centered approaches that respond to the individual needs of patients have altered the care delivery model in order to improve health services outcomes. In developing an alternative care model to inpatient treatment in PWID who required OPAT, Jafari et al.15 evaluated a community model of care that provided a home-like residence as an alternative to hospitalization where patients could receive OPAT in a medically and socially supportive environment. This environment, which included RN and mental health staff for substance-use counseling, wound care, medication management, and IV therapy, demonstrated lower rates of against medical advice (AMA) discharge and higher patient satisfaction compared with hospitalization.15
MOBILITY OFF OF THE HOSPITAL FLOOR FOR HOSPITALIZED PATIENTS WITH OUD
Ethical dilemmas may also arise when patients with OUD desire greater mobility in the hospital. Although some inpatients may be permitted to leave the floor, some treatment teams may believe that patients with OUD leave the floor to use drugs and that the patient’s IV will facilitate such behavior. Nursing and medical staff may also believe that, if they agree to a request to leave the floor, they are complicit in any potential drug use or harmful consequences resulting from this use. For their part, patients may have a desire for more mobility because of the sometimes unpleasant constraints of hospitalization, which are not unique to these patients16 or to distract them from their cravings. Patients, unable to tolerate the restriction emotionally or believing they are being treated unfairly, even punitively, may leave AMA rather than complete needed medical care. Once more, distrust of the patient and fear of liability may lead hospital staff to respond in counterproductive ways.
Addressing this dilemma depends, in part on creating an environment where PWID and patients with OUD are treated fairly and appropriately for their underlying illness. Such treatment includes ensuring withdrawal symptoms and pain are adequately treated, building trust by empathically addressing patients’ needs and preferences,17 and having a systematic (ie, policy-based) approach for requests to leave the floor. Th
Efforts to adequately treat withdrawal symptoms in the hospital setting have shown promise in maintaining patient engagement, reducing the rate of AMA discharges, and improving follow up with outpatient medical and substance-use treatment.18 Because physicians consistently cite the lack of advanced training in addiction medicine as a treatment limitation,12 training may go a long way in closing this knowledge and skill gap. Furthermore, systematic efforts to better educate and train hospitalists in the care of patients with addiction can improve both knowledge and attitudes about caring for this vulnerable population,19 thereby enhancing therapeutic relationships and patient centeredness. Finally, institutional policies promoting fair, systematic, and transparent guidance are needed for front-line practitioners to manage the legal, clinical, and ethical ambiguities involved when PWID wish to leave the hospital floor.
ENHANCING CARE DELIVERY TO PATIENTS WITH OUD
In addressing the mistrust some staff may have toward the patients described in the preceding ethical dilemmas, the use of universal precautions is an ethical and efficacious approach that balances reliance on patients’ veracity with due diligence in objective clinical assessments.20 These universal precautions, which are grounded in mutual respect and responsibility between physician and patient, include a set of strategies originally established in infectious disease practice and adapted to the management of chronic pain particularly when opioids are used.21 They are based on the recognition that identifying which patients prescribed opioids will develop an OUD or misuse opioids is difficult. Hence, the safest and least-stigmatizing approach is to treat all patients as individuals who could potentially be at risk. This is an ethically strong approach that seeks to balance the competing values of patent safety and patient centeredness, and involves taking a substance-use history from all patients admitted to the hospital and routinely checking state prescription-drug monitoring programs among other steps. Although self-reporting, at least of prescription-drug misuse, is fairly reliable,22 establishing expectations for mutual respect when working with patients with OUD and other addictive disorders is more likely to garner valid reports and a positive alliance. Once this relationship is established, the practitioner can respond to problematic behaviors with clear, compassionate limit setting.
From a broader perspective, a hospital system and culture that is unable to promote trust and adequately treat pain and withdrawal can create a “risk environment” for PWID.23 When providers are inadequately trained in the management of pain and addiction, or there is a shortage of addiction specialists, or inadequate policy guidance for managing the care of these patients, this can result in AMA discharges and reduced willingness to seek future care. Viewing this problem more expansively may persuade healthcare professionals that patients alone are not entirely responsible for the outcomes related to their illness but that modifying practices and structure at the hospital level has the potential to mitigate harm to this vulnerable population.
As inpatient team leaders, hospitalists have the unique opportunity to address the opioid crisis by enhancing the quality of care provided to hospitalized patients with OUD. This enhancement can be accomplished by destigmatizing substance-use disorders, establishing relationships of trust, and promoting remedies to structural deficiencies in the healthcare system that contribute to the problem. These approaches have the potential to enhance not only the care of patients with OUD but also the satisfaction of the treatment team caring for these patients.24 Su
Disclosures
The authors have no conflicts of interest to disclose, financial or otherwise. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs, the U.S. Government, or the VA National Center for Ethics in Health Care.
1. Hasin DS, O’Brien CP, Auriacombe M, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013;170(8):834-851. doi:10.1176/appi.ajp.2013.12060782. PubMed
2. Donroe JH, Holt SR, Tetrault JM. Caring for patients with opioid use disorder in the hospital. CMAJ. 2016;188(17-18):1232-1239. doi:10.1503/cmaj.160290. PubMed
3. National Institute on Drug Abuse. Opioid Overdose Crisis 2018. https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis. Last updated March 2018. Accessed July 1, 2018.
4. Kerr T, Wood E, Grafstein E, et al. High rates of primary care and emergency department use among injection drug users in Vancouver. J Public Health. (Oxf). 2005;27(1):62-66. doi:10.1093/pubmed/fdh189. PubMed
5. Merrill JO, Rhodes LA, Deyo RA, Marlatt GA, Bradley KA. Mutual mistrust in the medical care of drug users: the keys to the “narc” cabinet. J Gen Intern Med. 2002;17(5):327-333. doi:10.1007/s11606-002-0034-5. PubMed
6. DP Levine PB. Infections in Injection Drug Users. In: Mandell GL BJ, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 6th ed. Philadelphia: Churchill Livingstone; 2005.
7. Fanucchi L, Leedy N, Li J, Thornton AC. Perceptions and practices of physicians regarding outpatient parenteral antibiotic therapy in persons who inject drugs. J Hosp Med. 2016;11(8):581-582. doi:10.1002/jhm.2582. PubMed
8. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. doi:10.1016/j.drugalcdep.2013.02.018. PubMed
9. Fishman SM. Risk of the view through the keyhole: there is much more to physician reactions to the DEA than the number of formal actions. Pain Med. 2006;7(4):360-362; discussion 365-366. doi:10.1111/j.1526-4637.2006.00194.x. PubMed
10. Jamison RN, Sheehan KA, Scanlan E, Matthews M, Ross EL. Beliefs and attitudes about opioid prescribing and chronic pain management: survey of primary care providers. J Opioid Manag. 2014;10(6):375-382. doi:10.5055/jom.2014.0234. PubMed
11. Beach SR, Taylor JB, Kontos N. Teaching psychiatric trainees to “think dirty”: uncovering hidden motivations and deception. Psychosomatics. 2017;58(5):474-482. doi:10.1016/j.psym.2017.04.005. PubMed
12. Wakeman SE, Pham-Kanter G, Donelan K. Attitudes, practices, and preparedness to care for patients with substance use disorder: results from a survey of general internists. Subst Abus. 2016;37(4):635-641. doi:10.1080/08897077.2016.1187240. PubMed
13. Ho J, Archuleta S, Sulaiman Z, Fisher D. Safe and successful treatment of intravenous drug users with a peripherally inserted central catheter in an outpatient parenteral antibiotic treatment service. J Antimicrob Chemother. 2010;65(12):2641-2644. doi:10.1093/jac/dkq355. PubMed
14. Buehrle DJ, Shields RK, Shah N, Shoff C, Sheridan K. Risk factors associated with outpatient parenteral antibiotic therapy program failure among intravenous drug users. Open Forum Infect Dis. 2017;4(3):ofx102. doi:10.1093/ofid/ofx102. PubMed
15. Jafari S, Joe R, Elliot D, Nagji A, Hayden S, Marsh DC. A community care model of intravenous antibiotic therapy for injection drug users with deep tissue infection for “reduce leaving against medical advice.” Int J Ment Health Addict. 2015;13:49-58. doi:10.1007/s11469-014-9511-4. PubMed
16. Detsky AS, Krumholz HM. Reducing the trauma of hospitalization. JAMA. 2014;311(21):2169-2170. doi:10.1001/jama.2014.3695. PubMed
17. Joosten EA, De Jong CA, de Weert-van Oene GH, Sensky T, van der Staak CP. Shared decision-making: increases autonomy in substance-dependent patients. Subst Use Misuse. 2011;46(8):1037-1038. doi:10.3109/10826084.2011.552931. PubMed
18. Chan AC, Palepu A, Guh DP, et al. HIV-positive injection drug users who leave the hospital against medical advice: the mitigating role of methadone and social support. J Acquir Immune Defic Syndr. 2004;35(1):56-59. doi:10.1097/00126334-200401010-00008. PubMed
19. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11) 752-758. doi:10.12788/jhm.2993. PubMed
20. Kaye AD, Jones MR, Kaye AM, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse (part 2). Pain Physician. 2017;20(2S):S111-S133. PubMed
21. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107-112. doi: 10.1111/j.1526-4637.2005.05031.x. PubMed
22. Smith M, Rosenblum A, Parrino M, Fong C, Colucci S. Validity of self-reported misuse of prescription opioid analgesics. Subst Use Misuse. 2010;45(10):1509-1524. doi:10.3109/10826081003682107. PubMed
23. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. doi:10.1016/j.socscimed.2014.01.010. PubMed
24. Sullivan MD, Leigh J, Gaster B. Brief report: Training internists in shared decision making about chronic opioid treatment for noncancer pain. J Gen Intern Med. 2006;21(4):360-362. doi:10.1111/j.1525-1497.2006.00352.x. PubMed
“Lord have mercy on me, was the kneeling drunkard’s plea.”
—Johnny Cash
The Diagnostic and Statistical Manual of the American Psychiatric Association defines opioid-use disorder (OUD) as a problematic pattern of prescription and/or illicit opioid medication use leading to clinically significant impairment or distress.1 Compared with their non-OUD counterparts, patients with OUD have poorer overall health and worse health service outcomes, including higher rates of morbidity, mortality, HIV and HCV transmission, and 30-day readmissions.2 With the rate of fatal overdoses from opioids at crisis levels, leading scientific and professional organizations have declared OUD to be a public health emergency in the United States.3
The opioid epidemic affects hospitalists through the rising incidence of hospitalization, not only as a result of OUD’s indirect complications, but also its direct effects of intoxication and withdrawal.4 In caring for patients with OUD, hospitalists are often presented with many ethical dilemmas. Whether the dilemma involves timing and circumstances of discharge or the permission to leave the hospital floor, they often involve elements of mutual mistrust. In qualitative ethnographic studies, patients with OUD report not trusting that the medical staff will take their concerns of inadequately treated pain and other needs seriously. Providers may mistrust the patient’s report of pain and withhold treatment for OUD for nonclinical reasons.5 Here, we examine two ethical dilemmas specific to OUD in hospitalized patients. Our aim in describing these dilemmas is to help hospitalists recognize that targeting issues of mistrust may assist them to deliver better care to hospitalized patients with OUD.
DISCHARGING HOSPITALIZED PATIENTS WITH OUD
In the inpatient setting, ethical dilemmas surrounding discharge are common among people who inject drugs (PWID). These patients have disproportionately high rates of soft tissue and systemic infections, such as endocarditis and osteomyelitis, and subsequently often require long-term, outpatient parenteral antibiotic therapy (OPAT).6 From both the clinical and ethical perspectives, discharging PWID requiring OPAT to an unsupervised setting or continuing inpatient hospitalization to prevent a potential adverse event are equally imperfect solutions.
These patients may be clinically stable, suitable for discharge, and prefer to be discharged, but the practitioner’s concerns regarding untoward complications frequently override the patient’s wishes. Valid reasons for this exercise of what could be considered soft-paternalism are considered when physicians unilaterally decide what is best for patients, including refusal of community agencies to provide OPAT to PWID, inadequate social support and/or health literacy to administer the therapy, or varying degrees of homelessness that can affect timely follow-up. However, surveys of both hospitalists and infectious disease specialists also indicate that they may avoid discharge because of concerns the PWID will tamper with the intravenous (IV) catheter to inject drugs.7 This reluctance to discharge otherwise socially and medically suitable patients increases length of stay,7 decreases patient satisfaction, and could lead to misuse of limited hospital resources.
Both patient mistrust and stigmatization may contribute to this dilemma. Healthcare professionals have been shown to share and reflect a long-standing bias in their attitudes toward patients with substance-use disorders and OUD, in particular.8 Studies of providers’ attitudes are limited but suggest that legal concerns over liability and professional sanctions,9 reluctance to contribute to the development or relapse of addiction,10 and a strong psychological investment in not being deceived by the patient11 may influence physicians’ decisions about care.
Closely supervising IV antibiotic therapy for all PWID may not reflect current medical knowledge and may imply a moral assessment of patients’ culpability and lack of will power to resist using drugs.12 No evidence is available to suggest that inpatient parenteral antibiotic treatment offers superior adherence, and emerging evidence showing that carefully selected patients with an injection drug-use history can be safely and effectively treated as outpatients has been obtained.13,14 Ho et al. found high rates of treatment success in patients with adequate housing, a reliable guardian, and willingness to comply with appropriate IV catheter use.13 Although the study by Buehrle et al. found higher rates of OPAT failure among PWIDs, 25% of these failures were due to adverse drug reactions and only 2% were due to documented line manipulations.14 This research suggests that disposition to alternative settings for OPAT in PWID may be feasible, reasonable, and deserving of further study. Rather than treating PWIDs as a homogenous group of increased risk, contextualizing care based on individual risk stratification promotes more patient-centered care that is medically appropriate and potentially more cost efficient. A
Patient-centered approaches that respond to the individual needs of patients have altered the care delivery model in order to improve health services outcomes. In developing an alternative care model to inpatient treatment in PWID who required OPAT, Jafari et al.15 evaluated a community model of care that provided a home-like residence as an alternative to hospitalization where patients could receive OPAT in a medically and socially supportive environment. This environment, which included RN and mental health staff for substance-use counseling, wound care, medication management, and IV therapy, demonstrated lower rates of against medical advice (AMA) discharge and higher patient satisfaction compared with hospitalization.15
MOBILITY OFF OF THE HOSPITAL FLOOR FOR HOSPITALIZED PATIENTS WITH OUD
Ethical dilemmas may also arise when patients with OUD desire greater mobility in the hospital. Although some inpatients may be permitted to leave the floor, some treatment teams may believe that patients with OUD leave the floor to use drugs and that the patient’s IV will facilitate such behavior. Nursing and medical staff may also believe that, if they agree to a request to leave the floor, they are complicit in any potential drug use or harmful consequences resulting from this use. For their part, patients may have a desire for more mobility because of the sometimes unpleasant constraints of hospitalization, which are not unique to these patients16 or to distract them from their cravings. Patients, unable to tolerate the restriction emotionally or believing they are being treated unfairly, even punitively, may leave AMA rather than complete needed medical care. Once more, distrust of the patient and fear of liability may lead hospital staff to respond in counterproductive ways.
Addressing this dilemma depends, in part on creating an environment where PWID and patients with OUD are treated fairly and appropriately for their underlying illness. Such treatment includes ensuring withdrawal symptoms and pain are adequately treated, building trust by empathically addressing patients’ needs and preferences,17 and having a systematic (ie, policy-based) approach for requests to leave the floor. Th
Efforts to adequately treat withdrawal symptoms in the hospital setting have shown promise in maintaining patient engagement, reducing the rate of AMA discharges, and improving follow up with outpatient medical and substance-use treatment.18 Because physicians consistently cite the lack of advanced training in addiction medicine as a treatment limitation,12 training may go a long way in closing this knowledge and skill gap. Furthermore, systematic efforts to better educate and train hospitalists in the care of patients with addiction can improve both knowledge and attitudes about caring for this vulnerable population,19 thereby enhancing therapeutic relationships and patient centeredness. Finally, institutional policies promoting fair, systematic, and transparent guidance are needed for front-line practitioners to manage the legal, clinical, and ethical ambiguities involved when PWID wish to leave the hospital floor.
ENHANCING CARE DELIVERY TO PATIENTS WITH OUD
In addressing the mistrust some staff may have toward the patients described in the preceding ethical dilemmas, the use of universal precautions is an ethical and efficacious approach that balances reliance on patients’ veracity with due diligence in objective clinical assessments.20 These universal precautions, which are grounded in mutual respect and responsibility between physician and patient, include a set of strategies originally established in infectious disease practice and adapted to the management of chronic pain particularly when opioids are used.21 They are based on the recognition that identifying which patients prescribed opioids will develop an OUD or misuse opioids is difficult. Hence, the safest and least-stigmatizing approach is to treat all patients as individuals who could potentially be at risk. This is an ethically strong approach that seeks to balance the competing values of patent safety and patient centeredness, and involves taking a substance-use history from all patients admitted to the hospital and routinely checking state prescription-drug monitoring programs among other steps. Although self-reporting, at least of prescription-drug misuse, is fairly reliable,22 establishing expectations for mutual respect when working with patients with OUD and other addictive disorders is more likely to garner valid reports and a positive alliance. Once this relationship is established, the practitioner can respond to problematic behaviors with clear, compassionate limit setting.
From a broader perspective, a hospital system and culture that is unable to promote trust and adequately treat pain and withdrawal can create a “risk environment” for PWID.23 When providers are inadequately trained in the management of pain and addiction, or there is a shortage of addiction specialists, or inadequate policy guidance for managing the care of these patients, this can result in AMA discharges and reduced willingness to seek future care. Viewing this problem more expansively may persuade healthcare professionals that patients alone are not entirely responsible for the outcomes related to their illness but that modifying practices and structure at the hospital level has the potential to mitigate harm to this vulnerable population.
As inpatient team leaders, hospitalists have the unique opportunity to address the opioid crisis by enhancing the quality of care provided to hospitalized patients with OUD. This enhancement can be accomplished by destigmatizing substance-use disorders, establishing relationships of trust, and promoting remedies to structural deficiencies in the healthcare system that contribute to the problem. These approaches have the potential to enhance not only the care of patients with OUD but also the satisfaction of the treatment team caring for these patients.24 Su
Disclosures
The authors have no conflicts of interest to disclose, financial or otherwise. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs, the U.S. Government, or the VA National Center for Ethics in Health Care.
“Lord have mercy on me, was the kneeling drunkard’s plea.”
—Johnny Cash
The Diagnostic and Statistical Manual of the American Psychiatric Association defines opioid-use disorder (OUD) as a problematic pattern of prescription and/or illicit opioid medication use leading to clinically significant impairment or distress.1 Compared with their non-OUD counterparts, patients with OUD have poorer overall health and worse health service outcomes, including higher rates of morbidity, mortality, HIV and HCV transmission, and 30-day readmissions.2 With the rate of fatal overdoses from opioids at crisis levels, leading scientific and professional organizations have declared OUD to be a public health emergency in the United States.3
The opioid epidemic affects hospitalists through the rising incidence of hospitalization, not only as a result of OUD’s indirect complications, but also its direct effects of intoxication and withdrawal.4 In caring for patients with OUD, hospitalists are often presented with many ethical dilemmas. Whether the dilemma involves timing and circumstances of discharge or the permission to leave the hospital floor, they often involve elements of mutual mistrust. In qualitative ethnographic studies, patients with OUD report not trusting that the medical staff will take their concerns of inadequately treated pain and other needs seriously. Providers may mistrust the patient’s report of pain and withhold treatment for OUD for nonclinical reasons.5 Here, we examine two ethical dilemmas specific to OUD in hospitalized patients. Our aim in describing these dilemmas is to help hospitalists recognize that targeting issues of mistrust may assist them to deliver better care to hospitalized patients with OUD.
DISCHARGING HOSPITALIZED PATIENTS WITH OUD
In the inpatient setting, ethical dilemmas surrounding discharge are common among people who inject drugs (PWID). These patients have disproportionately high rates of soft tissue and systemic infections, such as endocarditis and osteomyelitis, and subsequently often require long-term, outpatient parenteral antibiotic therapy (OPAT).6 From both the clinical and ethical perspectives, discharging PWID requiring OPAT to an unsupervised setting or continuing inpatient hospitalization to prevent a potential adverse event are equally imperfect solutions.
These patients may be clinically stable, suitable for discharge, and prefer to be discharged, but the practitioner’s concerns regarding untoward complications frequently override the patient’s wishes. Valid reasons for this exercise of what could be considered soft-paternalism are considered when physicians unilaterally decide what is best for patients, including refusal of community agencies to provide OPAT to PWID, inadequate social support and/or health literacy to administer the therapy, or varying degrees of homelessness that can affect timely follow-up. However, surveys of both hospitalists and infectious disease specialists also indicate that they may avoid discharge because of concerns the PWID will tamper with the intravenous (IV) catheter to inject drugs.7 This reluctance to discharge otherwise socially and medically suitable patients increases length of stay,7 decreases patient satisfaction, and could lead to misuse of limited hospital resources.
Both patient mistrust and stigmatization may contribute to this dilemma. Healthcare professionals have been shown to share and reflect a long-standing bias in their attitudes toward patients with substance-use disorders and OUD, in particular.8 Studies of providers’ attitudes are limited but suggest that legal concerns over liability and professional sanctions,9 reluctance to contribute to the development or relapse of addiction,10 and a strong psychological investment in not being deceived by the patient11 may influence physicians’ decisions about care.
Closely supervising IV antibiotic therapy for all PWID may not reflect current medical knowledge and may imply a moral assessment of patients’ culpability and lack of will power to resist using drugs.12 No evidence is available to suggest that inpatient parenteral antibiotic treatment offers superior adherence, and emerging evidence showing that carefully selected patients with an injection drug-use history can be safely and effectively treated as outpatients has been obtained.13,14 Ho et al. found high rates of treatment success in patients with adequate housing, a reliable guardian, and willingness to comply with appropriate IV catheter use.13 Although the study by Buehrle et al. found higher rates of OPAT failure among PWIDs, 25% of these failures were due to adverse drug reactions and only 2% were due to documented line manipulations.14 This research suggests that disposition to alternative settings for OPAT in PWID may be feasible, reasonable, and deserving of further study. Rather than treating PWIDs as a homogenous group of increased risk, contextualizing care based on individual risk stratification promotes more patient-centered care that is medically appropriate and potentially more cost efficient. A
Patient-centered approaches that respond to the individual needs of patients have altered the care delivery model in order to improve health services outcomes. In developing an alternative care model to inpatient treatment in PWID who required OPAT, Jafari et al.15 evaluated a community model of care that provided a home-like residence as an alternative to hospitalization where patients could receive OPAT in a medically and socially supportive environment. This environment, which included RN and mental health staff for substance-use counseling, wound care, medication management, and IV therapy, demonstrated lower rates of against medical advice (AMA) discharge and higher patient satisfaction compared with hospitalization.15
MOBILITY OFF OF THE HOSPITAL FLOOR FOR HOSPITALIZED PATIENTS WITH OUD
Ethical dilemmas may also arise when patients with OUD desire greater mobility in the hospital. Although some inpatients may be permitted to leave the floor, some treatment teams may believe that patients with OUD leave the floor to use drugs and that the patient’s IV will facilitate such behavior. Nursing and medical staff may also believe that, if they agree to a request to leave the floor, they are complicit in any potential drug use or harmful consequences resulting from this use. For their part, patients may have a desire for more mobility because of the sometimes unpleasant constraints of hospitalization, which are not unique to these patients16 or to distract them from their cravings. Patients, unable to tolerate the restriction emotionally or believing they are being treated unfairly, even punitively, may leave AMA rather than complete needed medical care. Once more, distrust of the patient and fear of liability may lead hospital staff to respond in counterproductive ways.
Addressing this dilemma depends, in part on creating an environment where PWID and patients with OUD are treated fairly and appropriately for their underlying illness. Such treatment includes ensuring withdrawal symptoms and pain are adequately treated, building trust by empathically addressing patients’ needs and preferences,17 and having a systematic (ie, policy-based) approach for requests to leave the floor. Th
Efforts to adequately treat withdrawal symptoms in the hospital setting have shown promise in maintaining patient engagement, reducing the rate of AMA discharges, and improving follow up with outpatient medical and substance-use treatment.18 Because physicians consistently cite the lack of advanced training in addiction medicine as a treatment limitation,12 training may go a long way in closing this knowledge and skill gap. Furthermore, systematic efforts to better educate and train hospitalists in the care of patients with addiction can improve both knowledge and attitudes about caring for this vulnerable population,19 thereby enhancing therapeutic relationships and patient centeredness. Finally, institutional policies promoting fair, systematic, and transparent guidance are needed for front-line practitioners to manage the legal, clinical, and ethical ambiguities involved when PWID wish to leave the hospital floor.
ENHANCING CARE DELIVERY TO PATIENTS WITH OUD
In addressing the mistrust some staff may have toward the patients described in the preceding ethical dilemmas, the use of universal precautions is an ethical and efficacious approach that balances reliance on patients’ veracity with due diligence in objective clinical assessments.20 These universal precautions, which are grounded in mutual respect and responsibility between physician and patient, include a set of strategies originally established in infectious disease practice and adapted to the management of chronic pain particularly when opioids are used.21 They are based on the recognition that identifying which patients prescribed opioids will develop an OUD or misuse opioids is difficult. Hence, the safest and least-stigmatizing approach is to treat all patients as individuals who could potentially be at risk. This is an ethically strong approach that seeks to balance the competing values of patent safety and patient centeredness, and involves taking a substance-use history from all patients admitted to the hospital and routinely checking state prescription-drug monitoring programs among other steps. Although self-reporting, at least of prescription-drug misuse, is fairly reliable,22 establishing expectations for mutual respect when working with patients with OUD and other addictive disorders is more likely to garner valid reports and a positive alliance. Once this relationship is established, the practitioner can respond to problematic behaviors with clear, compassionate limit setting.
From a broader perspective, a hospital system and culture that is unable to promote trust and adequately treat pain and withdrawal can create a “risk environment” for PWID.23 When providers are inadequately trained in the management of pain and addiction, or there is a shortage of addiction specialists, or inadequate policy guidance for managing the care of these patients, this can result in AMA discharges and reduced willingness to seek future care. Viewing this problem more expansively may persuade healthcare professionals that patients alone are not entirely responsible for the outcomes related to their illness but that modifying practices and structure at the hospital level has the potential to mitigate harm to this vulnerable population.
As inpatient team leaders, hospitalists have the unique opportunity to address the opioid crisis by enhancing the quality of care provided to hospitalized patients with OUD. This enhancement can be accomplished by destigmatizing substance-use disorders, establishing relationships of trust, and promoting remedies to structural deficiencies in the healthcare system that contribute to the problem. These approaches have the potential to enhance not only the care of patients with OUD but also the satisfaction of the treatment team caring for these patients.24 Su
Disclosures
The authors have no conflicts of interest to disclose, financial or otherwise. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs, the U.S. Government, or the VA National Center for Ethics in Health Care.
1. Hasin DS, O’Brien CP, Auriacombe M, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013;170(8):834-851. doi:10.1176/appi.ajp.2013.12060782. PubMed
2. Donroe JH, Holt SR, Tetrault JM. Caring for patients with opioid use disorder in the hospital. CMAJ. 2016;188(17-18):1232-1239. doi:10.1503/cmaj.160290. PubMed
3. National Institute on Drug Abuse. Opioid Overdose Crisis 2018. https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis. Last updated March 2018. Accessed July 1, 2018.
4. Kerr T, Wood E, Grafstein E, et al. High rates of primary care and emergency department use among injection drug users in Vancouver. J Public Health. (Oxf). 2005;27(1):62-66. doi:10.1093/pubmed/fdh189. PubMed
5. Merrill JO, Rhodes LA, Deyo RA, Marlatt GA, Bradley KA. Mutual mistrust in the medical care of drug users: the keys to the “narc” cabinet. J Gen Intern Med. 2002;17(5):327-333. doi:10.1007/s11606-002-0034-5. PubMed
6. DP Levine PB. Infections in Injection Drug Users. In: Mandell GL BJ, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 6th ed. Philadelphia: Churchill Livingstone; 2005.
7. Fanucchi L, Leedy N, Li J, Thornton AC. Perceptions and practices of physicians regarding outpatient parenteral antibiotic therapy in persons who inject drugs. J Hosp Med. 2016;11(8):581-582. doi:10.1002/jhm.2582. PubMed
8. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. doi:10.1016/j.drugalcdep.2013.02.018. PubMed
9. Fishman SM. Risk of the view through the keyhole: there is much more to physician reactions to the DEA than the number of formal actions. Pain Med. 2006;7(4):360-362; discussion 365-366. doi:10.1111/j.1526-4637.2006.00194.x. PubMed
10. Jamison RN, Sheehan KA, Scanlan E, Matthews M, Ross EL. Beliefs and attitudes about opioid prescribing and chronic pain management: survey of primary care providers. J Opioid Manag. 2014;10(6):375-382. doi:10.5055/jom.2014.0234. PubMed
11. Beach SR, Taylor JB, Kontos N. Teaching psychiatric trainees to “think dirty”: uncovering hidden motivations and deception. Psychosomatics. 2017;58(5):474-482. doi:10.1016/j.psym.2017.04.005. PubMed
12. Wakeman SE, Pham-Kanter G, Donelan K. Attitudes, practices, and preparedness to care for patients with substance use disorder: results from a survey of general internists. Subst Abus. 2016;37(4):635-641. doi:10.1080/08897077.2016.1187240. PubMed
13. Ho J, Archuleta S, Sulaiman Z, Fisher D. Safe and successful treatment of intravenous drug users with a peripherally inserted central catheter in an outpatient parenteral antibiotic treatment service. J Antimicrob Chemother. 2010;65(12):2641-2644. doi:10.1093/jac/dkq355. PubMed
14. Buehrle DJ, Shields RK, Shah N, Shoff C, Sheridan K. Risk factors associated with outpatient parenteral antibiotic therapy program failure among intravenous drug users. Open Forum Infect Dis. 2017;4(3):ofx102. doi:10.1093/ofid/ofx102. PubMed
15. Jafari S, Joe R, Elliot D, Nagji A, Hayden S, Marsh DC. A community care model of intravenous antibiotic therapy for injection drug users with deep tissue infection for “reduce leaving against medical advice.” Int J Ment Health Addict. 2015;13:49-58. doi:10.1007/s11469-014-9511-4. PubMed
16. Detsky AS, Krumholz HM. Reducing the trauma of hospitalization. JAMA. 2014;311(21):2169-2170. doi:10.1001/jama.2014.3695. PubMed
17. Joosten EA, De Jong CA, de Weert-van Oene GH, Sensky T, van der Staak CP. Shared decision-making: increases autonomy in substance-dependent patients. Subst Use Misuse. 2011;46(8):1037-1038. doi:10.3109/10826084.2011.552931. PubMed
18. Chan AC, Palepu A, Guh DP, et al. HIV-positive injection drug users who leave the hospital against medical advice: the mitigating role of methadone and social support. J Acquir Immune Defic Syndr. 2004;35(1):56-59. doi:10.1097/00126334-200401010-00008. PubMed
19. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11) 752-758. doi:10.12788/jhm.2993. PubMed
20. Kaye AD, Jones MR, Kaye AM, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse (part 2). Pain Physician. 2017;20(2S):S111-S133. PubMed
21. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107-112. doi: 10.1111/j.1526-4637.2005.05031.x. PubMed
22. Smith M, Rosenblum A, Parrino M, Fong C, Colucci S. Validity of self-reported misuse of prescription opioid analgesics. Subst Use Misuse. 2010;45(10):1509-1524. doi:10.3109/10826081003682107. PubMed
23. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. doi:10.1016/j.socscimed.2014.01.010. PubMed
24. Sullivan MD, Leigh J, Gaster B. Brief report: Training internists in shared decision making about chronic opioid treatment for noncancer pain. J Gen Intern Med. 2006;21(4):360-362. doi:10.1111/j.1525-1497.2006.00352.x. PubMed
1. Hasin DS, O’Brien CP, Auriacombe M, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013;170(8):834-851. doi:10.1176/appi.ajp.2013.12060782. PubMed
2. Donroe JH, Holt SR, Tetrault JM. Caring for patients with opioid use disorder in the hospital. CMAJ. 2016;188(17-18):1232-1239. doi:10.1503/cmaj.160290. PubMed
3. National Institute on Drug Abuse. Opioid Overdose Crisis 2018. https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis. Last updated March 2018. Accessed July 1, 2018.
4. Kerr T, Wood E, Grafstein E, et al. High rates of primary care and emergency department use among injection drug users in Vancouver. J Public Health. (Oxf). 2005;27(1):62-66. doi:10.1093/pubmed/fdh189. PubMed
5. Merrill JO, Rhodes LA, Deyo RA, Marlatt GA, Bradley KA. Mutual mistrust in the medical care of drug users: the keys to the “narc” cabinet. J Gen Intern Med. 2002;17(5):327-333. doi:10.1007/s11606-002-0034-5. PubMed
6. DP Levine PB. Infections in Injection Drug Users. In: Mandell GL BJ, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 6th ed. Philadelphia: Churchill Livingstone; 2005.
7. Fanucchi L, Leedy N, Li J, Thornton AC. Perceptions and practices of physicians regarding outpatient parenteral antibiotic therapy in persons who inject drugs. J Hosp Med. 2016;11(8):581-582. doi:10.1002/jhm.2582. PubMed
8. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. doi:10.1016/j.drugalcdep.2013.02.018. PubMed
9. Fishman SM. Risk of the view through the keyhole: there is much more to physician reactions to the DEA than the number of formal actions. Pain Med. 2006;7(4):360-362; discussion 365-366. doi:10.1111/j.1526-4637.2006.00194.x. PubMed
10. Jamison RN, Sheehan KA, Scanlan E, Matthews M, Ross EL. Beliefs and attitudes about opioid prescribing and chronic pain management: survey of primary care providers. J Opioid Manag. 2014;10(6):375-382. doi:10.5055/jom.2014.0234. PubMed
11. Beach SR, Taylor JB, Kontos N. Teaching psychiatric trainees to “think dirty”: uncovering hidden motivations and deception. Psychosomatics. 2017;58(5):474-482. doi:10.1016/j.psym.2017.04.005. PubMed
12. Wakeman SE, Pham-Kanter G, Donelan K. Attitudes, practices, and preparedness to care for patients with substance use disorder: results from a survey of general internists. Subst Abus. 2016;37(4):635-641. doi:10.1080/08897077.2016.1187240. PubMed
13. Ho J, Archuleta S, Sulaiman Z, Fisher D. Safe and successful treatment of intravenous drug users with a peripherally inserted central catheter in an outpatient parenteral antibiotic treatment service. J Antimicrob Chemother. 2010;65(12):2641-2644. doi:10.1093/jac/dkq355. PubMed
14. Buehrle DJ, Shields RK, Shah N, Shoff C, Sheridan K. Risk factors associated with outpatient parenteral antibiotic therapy program failure among intravenous drug users. Open Forum Infect Dis. 2017;4(3):ofx102. doi:10.1093/ofid/ofx102. PubMed
15. Jafari S, Joe R, Elliot D, Nagji A, Hayden S, Marsh DC. A community care model of intravenous antibiotic therapy for injection drug users with deep tissue infection for “reduce leaving against medical advice.” Int J Ment Health Addict. 2015;13:49-58. doi:10.1007/s11469-014-9511-4. PubMed
16. Detsky AS, Krumholz HM. Reducing the trauma of hospitalization. JAMA. 2014;311(21):2169-2170. doi:10.1001/jama.2014.3695. PubMed
17. Joosten EA, De Jong CA, de Weert-van Oene GH, Sensky T, van der Staak CP. Shared decision-making: increases autonomy in substance-dependent patients. Subst Use Misuse. 2011;46(8):1037-1038. doi:10.3109/10826084.2011.552931. PubMed
18. Chan AC, Palepu A, Guh DP, et al. HIV-positive injection drug users who leave the hospital against medical advice: the mitigating role of methadone and social support. J Acquir Immune Defic Syndr. 2004;35(1):56-59. doi:10.1097/00126334-200401010-00008. PubMed
19. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11) 752-758. doi:10.12788/jhm.2993. PubMed
20. Kaye AD, Jones MR, Kaye AM, et al. Prescription opioid abuse in chronic pain: an updated review of opioid abuse predictors and strategies to curb opioid abuse (part 2). Pain Physician. 2017;20(2S):S111-S133. PubMed
21. Gourlay DL, Heit HA, Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107-112. doi: 10.1111/j.1526-4637.2005.05031.x. PubMed
22. Smith M, Rosenblum A, Parrino M, Fong C, Colucci S. Validity of self-reported misuse of prescription opioid analgesics. Subst Use Misuse. 2010;45(10):1509-1524. doi:10.3109/10826081003682107. PubMed
23. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. doi:10.1016/j.socscimed.2014.01.010. PubMed
24. Sullivan MD, Leigh J, Gaster B. Brief report: Training internists in shared decision making about chronic opioid treatment for noncancer pain. J Gen Intern Med. 2006;21(4):360-362. doi:10.1111/j.1525-1497.2006.00352.x. PubMed
© 2019 Society of Hospital Medicine
Things We Do For No Reason: Against Medical Advice Discharges
The “Things We Do for No Reason” (TWDFNR) series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent “black and white” conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
Against medical advice (AMA) discharges, which account for up to 2% of all inpatient discharges, are associated with worse health and health services outcomes and disproportionately affect vulnerable patient populations. This paper will review the background data on AMA discharges as well as the reasons physicians may choose to discharge patients AMA. From a healthcare quality perspective, the designation of a discharge as AMA is low-value care in that it is a routine hospital practice without demonstrated benefit and is not supported by a strong evidence base. We argue that designating discharges as AMA has never been shown to advance patient care and that it has the potential to harm patients by reducing access to care and promoting stigma. We believe that greater attention to both shared decision-making as well as harm reduction principles in discharge planning can serve as effective, patient-centered alternatives when patients choose not to follow a healthcare professional’s recommended advice.
CASE PRESENTATION
A 54-year-old man with active intravenous (IV) drug use and hepatitis C was admitted with lower extremity cellulitis. On hospital day 2, the patient insisted that he wanted to go home. The treatment team informed the patient that an additional 2-3 days of IV antibiotics would produce a more reliable cure and reduce the risk of readmission. Should the team inform the patient that he will be discharged against medical advice (AMA) if he chooses to leave the hospital prematurely?
BACKGROUND
In the United States, patients are discharged AMA approximately 500,000 times per year (1%-2% of all discharges).1 These discharges represent a wide array of clinical scenarios that all culminate in the formal recognition and documentation of a competent patient’s choice to decline further inpatient medical care and leave the hospital prior to a recommended clinical endpoint. Compared with standard discharges, AMA discharges are associated with an increased adjusted relative risk of 30-day mortality as high as 10% and 30-day readmission rates that are 20%-40% higher than readmission rates following standard discharges.2 AMA discharges are more likely among patients with substance use disorders, psychiatric illness, and HIV.3
WHY YOU MIGHT THINK AMA DISCHARGES ARE HELPFUL
Although there are little empirical data to inform how and why physicians choose to designate a discharge as AMA when patients decline recommended care, the existing evidence suggests that fears of legal liability are strongly driving the practice.4 Physicians may believe that they must discharge patients AMA in order to fulfill their legal and ethical responsibilities, or to demonstrate in writing the physician’s concern and the significant risk of leaving.5,6 Clinicians may have been acculturated during training to believe that an AMA discharge may also be seen as a way of formally distancing themselves from the patient’s request for a nonstandard or unsafe discharge plan, thus deflecting any potential blame for worse patient outcomes.
Finally, clinicians and administrators may also believe that an AMA discharge is the appropriate designation for a hospital stay that ended because the patient chose to prematurely discontinue the treatment relationship or to decline the postdischarge placement recommendations. This reasoning may explain why the hospital penalties authorized by Medicare’s Hospital Readmission Reduction Program generally exclude initial admissions ending in an AMA discharge7 and may provide the rationale (and perhaps a financial incentive) to discharge patients AMA in order to limit CMS readmission penalties.
WHY AMA DISCHARGES ADD NO VALUE TO A PATIENT’S FULLY INFORMED DECLINATION OF CARE
The AMA discharge is a routine hospital practice without demonstrated patient benefit and which disproportionately affects vulnerable populations. There is also a growing literature that demonstrates that AMA discharges stigmatize patients, reduce their access to care, and can reduce the quality of informed consent discussions in discharge planning.8-10 Although there are no conclusive data that AMA discharges are more likely among underrepresented racial minorities, the disproportionate burden of AMA discharges and their worse health outcomes are borne by the homeless, those with substance use disorders, and the uninsured.3,11
Compared to patients discharged conventionally from an emergency department, 25% of patients discharged AMA reported not wanting to return for follow-up care.8 This reluctance to return for care is in part mediated by provider-generated stigma and blame9,12 and may be exacerbated when patients believe that their decision to leave AMA was based upon extenuating circumstance or competing necessity (eg, limited care options for their dependents, poor quality hospital care, etc.).
To persuade patients to remain hospitalized, 85% of trainees and 67% of attending physicians in one study incorrectly informed their patients that insurance will not reimburse a hospitalization if they leave AMA.13 Because this study demonstrated that there is no empirical evidence that payment after AMA discharges is denied by private or government payers, physicians sharing this misinformation can breed distrust and coercively undermine patients’ ability to make a voluntary choice.
When clinicians assert they are bound by duty to discharge a patient AMA, they may be conflating a presumed legal obligation to formally designate the discharge as AMA in the medical record with their actual obligation to obtain the patient’s informed consent for the discharge. In other words, there is no identifiable medico-legal requirement to specifically designate a discharge as AMA.
Although clinicians may presume that the AMA designation provides protection from liability, the claim is not supported by the available literature.14,15 In these studies, which reviewed relevant case law, defendants prevailed not because of the physician’s AMA designation, but because the plaintiff was not able to prove negligence. The proper execution of the discharge process, not the specific designation of AMA, is what conferred liability protection.5 Indeed, malpractice claims, which are associated with patient perceptions of feeling deserted or devalued,16 might be more likely with AMA discharges when they result from flawed and stigmatizing communication processes.17
Finally, there are no clinical, regulatory, or professional standards that specify the designation of an AMA discharge. Neither the Joint Commission nor any other professional organization specify under what conditions a clinician should discharge a patient AMA, thus promoting wide variability in its use and further limiting it as a valid and reliable healthcare metric.
WHAT SHOULD PHYSICIANS DO INSTEAD: AVOID THE AMA DESIGNATION AND PROMOTE SHARED DECISION-MAKING AND HARM REDUCTION
Because all competent patients have the right to decline recommended inpatient treatment, the ethical and legal standard is that the physician obtain the patient’s informed consent to leave by communicating the risks, benefits, and alternatives to leaving and fully documenting the conversation in the medical record.2 The additional steps of formalizing the discharge as AMA and providing AMA forms for the patient to sign have never been demonstrated to improve quality (and add needless clerical work). When declining any treatment, even life-sustaining treatment, the request for a patient signature to decline such treatment has not been demonstrated to improve risk communication and is not considered a best practice for informed consent.18 When the physician’s motives for this behavior are punitive or directed primarily at reducing liability, it may distract the physician from their fiduciary duty to put patients first.
The solution to improve quality is straightforward—avoid designating discharges as AMA. Instead, clinicians should maintain a single discharge process with clear, objective documentation including providing appropriate prescriptions and follow-up appointments regardless of whether the patient’s choice is consistent with a physician’s recommendation. In its place, the physician should use shared decision-making (SDM) and harm reduction principles to enhance the patient’s well-being within the identified constraints. SDM involves physicians and patients making healthcare decisions together by combining the patients’ values and preferences for care with the physicians’ expertise and knowledge of medical evidence. Harm reduction practices seek to reduce the adverse health consequences that may come from unhealthy behaviors while assuming that patients will likely continue such behaviors. Evidence-based and widely accepted examples of harm reduction strategies include nicotine replacement therapy and needle exchange programs.19
SDM in discharge planning provides a range of discharge and transitional care options that are within prevailing medical standards, not simply a single recommendation that prioritizes health promotion to the exclusion of other identified patient goals. Quality discharge planning should provide the “right care for the right patient at the right time”20 that moves beyond the false choice of either remaining in the hospital under the conditions specified by the physician or leaving AMA. Although physicians are understandably concerned about patients making choices that do not prioritize their health, physicians can consider the evidence for harm reduction programs’ effectiveness in improving health outcomes21 and accommodate patients by providing harm-reducing discharge options that, while suboptimal, may not be substandard.22
Physicians who wish to promote stronger patient-centered discharge practices may find that avoiding or limiting AMA discharges may conflict with their institution’s policy. In those cases, physicians should work closely with their leadership and legal counsel to ensure that any proposed practice changes are legally compliant but also improve SDM and reduce stigma for this population.
Although ending the clinical practice of designating discharges as AMA is unlikely to completely ameliorate the morbidity and costs associated with patients declining episodes of inpatient care, there is reasonable face validity to conclude that replacing the AMA practice with greater attention to harm reduction and SDM can reduce some of the preventable harms like stigmatization and reduced access to care. Together, these practices demonstrate the profession’s continued commitment to the public to practice patient-centered care.
RECOMMENDATIONS
- Treat all discharges similarly. Avoid designating an inpatient discharge as AMA.
- Ensure there is objective documentation of the patient’s informed choice to leave the hospital.
- When patients wish to leave the hospital prior to a physician-recommended clinical endpoint, engage in SDM with a focus on providing all medically reasonable treatment options that promote harm reduction.
- If you choose to designate a discharge as AMA, approach the discharge planning process consistently and with patient-centered principles by optimizing SDM and harm reduction.
CONCLUSION
The physician informed the patient of the risks, benefits, and alternatives to leaving the hospital prior to the completion of IV antibiotics and confirmed the patient’s decision-making capacity. Next, the physician elicited the patient’s preferences for care and identified competing priorities. The patient wanted treatment for his cellulitis, but he was experiencing pain and opioid withdrawal. The physician then expanded the range of potential treatment options, including evaluation for medication-assisted treatment for the patient’s opioid use disorder (OUD) and harm reduction measures such as safer injection practices, needle exchange, housing assistance, and overdose prevention and treatment education.23 An alternative harm-reducing option included discharge with oral antibiotics and follow-up with his primary physician in 48-72 hours. After the patient indicated that he wanted to leave because he was not yet ready for OUD treatment, he was discharged with the standard discharge paperwork and antibiotics, and the physician documented the informed consent discussion.
Disclosure
The authors report no conflicts of interest, financial or otherwise. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs, the VA National Center for Ethics in Health Care or the US Government.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing TWDFNR@hospitalmedicine.org
1. Ibrahim SA, Kwoh CK, Krishnan E. Factors associated with patients who leave acute-care hospitals against medical advice. Am J Public Health. 2007;97(12):2204-2208. PubMed
2. Alfandre DJ. “I’m going home”: discharges against medical advice. Mayo Clin Proc. 2009;84(3):255-260. PubMed
3. Kraut A, Fransoo R, Olafson K, Ramsey CD, Yogendran M, Garland A. A population-based analysis of leaving the hospital against medical advice: incidence and associated variables. BMC Health Serv Res. 2013;13:415. PubMed
4. Green P, Watts D, Poole S, Dhopesh V. Why patients sign out against medical advice (AMA): factors motivating patients to sign out AMA. Am J Drug Alcohol Abuse. 2004;30(2):489-493. PubMed
5. Levy F, Mareiniss DP, Iacovelli C. The Importance of a Proper Against-Medical-Advice (AMA) Discharge: How Signing Out AMA May Create Significant Liability Protection for Providers. J Emerg Med. 2012;43(3):516-520. PubMed
6. Brenner J, Joslin J, Goulette A, Grant WD, Wojcik SM. Against Medical Advice: A Survey of ED Clinicians’ Rationale for Use. J Emerg Nurs. 2016;42(5):408-411. PubMed
7. Hospital-Wide (All-Condition) 30-Day Risk-Standardized Readmission Measure. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/downloads/MMSHospital-WideAll-ConditionReadmissionRate.pdf. Accessed on July 22, 2016.
8. Jerrard DA, Chasm RM. Patients leaving against medical advice (AMA) from the emergency department--disease prevalence and willingness to return. J Emerg Med. 2011;41(4):412-417. PubMed
9. Haywood C, Jr, Lanzkron S, Hughes MT, et al. A video-intervention to improve clinician attitudes toward patients with sickle cell disease: the results of a randomized experiment. J Gen Intern Med. 2011;26(5):518-523. PubMed
10. Wigder HN, Propp DA, Leslie K, Mathew A. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010;55(4):393. PubMed
11. Saab D, Nisenbaum R, Dhalla I, Hwang SW. Hospital Readmissions in a Community-based Sample of Homeless Adults: a Matched-cohort Study. J Gen Intern Med. 2016;31(9):1011-1018. PubMed
12. Lekas HM, Alfandre D, Gordon P, Harwood K, Yin MT. The role of patient-provider interactions: Using an accounts framework to explain hospital discharges against medical advice. Soc Sci Med. 2016;156:106-113. PubMed
13. Schaefer GR, Matus H, Schumann JH, et al. Financial Responsibility of Hospitalized Patients Who Left Against Medical Advice: Medical Urban Legend? J Gen Intern Med. 2012;27(7):825-830. PubMed
14. Devitt PJ, Devitt AC, Dewan M. Does identifying a discharge as “against medical advice” confer legal protection? J Fam Pract. 2000;49(3):224-227. PubMed
15. Devitt PJ, Devitt AC, Dewan M. An examination of whether discharging patients against medical advice protects physicians from malpractice charges. Psychiatr Serv. 2000;51(7):899-902. PubMed
16. Beckman HB, Markakis KM, Suchman AL, Frankel RM. The doctor-patient relationship and malpractice. Lessons from plaintiff depositions. Arch Intern Med. 1994;154(12):1365-1370. PubMed
17. Windish DM, Ratanawongsa N. Providers’ perceptions of relationships and professional roles when caring for patients who leave the hospital against medical advice. J Gen Intern Med. 2008;23(10):1698-1707. PubMed
18. Sulmasy DP, Sood JR, Texiera K, McAuley RL, McGugins J, Ury WA. A prospective trial of a new policy eliminating signed consent for do not resuscitate orders. J Gen Intern Med. 2006;21(12):1261-1268. PubMed
19. Stratton K, Shetty P, Wallace R, Bondurant S. Clearing the smoke: the science base for tobacco harm reduction--executive summary. Tob Control. 2001;10(2):189-195. PubMed
20. What is Health Care Quality and Who Decides?. March 2009. Agency for Healthcare Research and Quality, Rockville, MD. https://archive.ahrq.gov/news/speech/test031809.html
21. Hobden KL, Cunningham JA. Barriers to the dissemination of four harm reduction strategies: a survey of addiction treatment providers in Ontario. Harm Reduct J. 2006;3:35. PubMed
22. Alfandre D. Clinical Recommendations in Medical Practice: A Proposed Framework to Reduce Bias and Improve the Quality of Medical Decisions. J Clin Ethics. 2016;27(1):21-27. PubMed
23. Fanucchi L, Lofwall MR. Putting Parity into Practice - Integrating Opioid-Use Disorder Treatment into the Hospital Setting. N Engl J Med. 2016;375(9):811-813. PubMed
The “Things We Do for No Reason” (TWDFNR) series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent “black and white” conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
Against medical advice (AMA) discharges, which account for up to 2% of all inpatient discharges, are associated with worse health and health services outcomes and disproportionately affect vulnerable patient populations. This paper will review the background data on AMA discharges as well as the reasons physicians may choose to discharge patients AMA. From a healthcare quality perspective, the designation of a discharge as AMA is low-value care in that it is a routine hospital practice without demonstrated benefit and is not supported by a strong evidence base. We argue that designating discharges as AMA has never been shown to advance patient care and that it has the potential to harm patients by reducing access to care and promoting stigma. We believe that greater attention to both shared decision-making as well as harm reduction principles in discharge planning can serve as effective, patient-centered alternatives when patients choose not to follow a healthcare professional’s recommended advice.
CASE PRESENTATION
A 54-year-old man with active intravenous (IV) drug use and hepatitis C was admitted with lower extremity cellulitis. On hospital day 2, the patient insisted that he wanted to go home. The treatment team informed the patient that an additional 2-3 days of IV antibiotics would produce a more reliable cure and reduce the risk of readmission. Should the team inform the patient that he will be discharged against medical advice (AMA) if he chooses to leave the hospital prematurely?
BACKGROUND
In the United States, patients are discharged AMA approximately 500,000 times per year (1%-2% of all discharges).1 These discharges represent a wide array of clinical scenarios that all culminate in the formal recognition and documentation of a competent patient’s choice to decline further inpatient medical care and leave the hospital prior to a recommended clinical endpoint. Compared with standard discharges, AMA discharges are associated with an increased adjusted relative risk of 30-day mortality as high as 10% and 30-day readmission rates that are 20%-40% higher than readmission rates following standard discharges.2 AMA discharges are more likely among patients with substance use disorders, psychiatric illness, and HIV.3
WHY YOU MIGHT THINK AMA DISCHARGES ARE HELPFUL
Although there are little empirical data to inform how and why physicians choose to designate a discharge as AMA when patients decline recommended care, the existing evidence suggests that fears of legal liability are strongly driving the practice.4 Physicians may believe that they must discharge patients AMA in order to fulfill their legal and ethical responsibilities, or to demonstrate in writing the physician’s concern and the significant risk of leaving.5,6 Clinicians may have been acculturated during training to believe that an AMA discharge may also be seen as a way of formally distancing themselves from the patient’s request for a nonstandard or unsafe discharge plan, thus deflecting any potential blame for worse patient outcomes.
Finally, clinicians and administrators may also believe that an AMA discharge is the appropriate designation for a hospital stay that ended because the patient chose to prematurely discontinue the treatment relationship or to decline the postdischarge placement recommendations. This reasoning may explain why the hospital penalties authorized by Medicare’s Hospital Readmission Reduction Program generally exclude initial admissions ending in an AMA discharge7 and may provide the rationale (and perhaps a financial incentive) to discharge patients AMA in order to limit CMS readmission penalties.
WHY AMA DISCHARGES ADD NO VALUE TO A PATIENT’S FULLY INFORMED DECLINATION OF CARE
The AMA discharge is a routine hospital practice without demonstrated patient benefit and which disproportionately affects vulnerable populations. There is also a growing literature that demonstrates that AMA discharges stigmatize patients, reduce their access to care, and can reduce the quality of informed consent discussions in discharge planning.8-10 Although there are no conclusive data that AMA discharges are more likely among underrepresented racial minorities, the disproportionate burden of AMA discharges and their worse health outcomes are borne by the homeless, those with substance use disorders, and the uninsured.3,11
Compared to patients discharged conventionally from an emergency department, 25% of patients discharged AMA reported not wanting to return for follow-up care.8 This reluctance to return for care is in part mediated by provider-generated stigma and blame9,12 and may be exacerbated when patients believe that their decision to leave AMA was based upon extenuating circumstance or competing necessity (eg, limited care options for their dependents, poor quality hospital care, etc.).
To persuade patients to remain hospitalized, 85% of trainees and 67% of attending physicians in one study incorrectly informed their patients that insurance will not reimburse a hospitalization if they leave AMA.13 Because this study demonstrated that there is no empirical evidence that payment after AMA discharges is denied by private or government payers, physicians sharing this misinformation can breed distrust and coercively undermine patients’ ability to make a voluntary choice.
When clinicians assert they are bound by duty to discharge a patient AMA, they may be conflating a presumed legal obligation to formally designate the discharge as AMA in the medical record with their actual obligation to obtain the patient’s informed consent for the discharge. In other words, there is no identifiable medico-legal requirement to specifically designate a discharge as AMA.
Although clinicians may presume that the AMA designation provides protection from liability, the claim is not supported by the available literature.14,15 In these studies, which reviewed relevant case law, defendants prevailed not because of the physician’s AMA designation, but because the plaintiff was not able to prove negligence. The proper execution of the discharge process, not the specific designation of AMA, is what conferred liability protection.5 Indeed, malpractice claims, which are associated with patient perceptions of feeling deserted or devalued,16 might be more likely with AMA discharges when they result from flawed and stigmatizing communication processes.17
Finally, there are no clinical, regulatory, or professional standards that specify the designation of an AMA discharge. Neither the Joint Commission nor any other professional organization specify under what conditions a clinician should discharge a patient AMA, thus promoting wide variability in its use and further limiting it as a valid and reliable healthcare metric.
WHAT SHOULD PHYSICIANS DO INSTEAD: AVOID THE AMA DESIGNATION AND PROMOTE SHARED DECISION-MAKING AND HARM REDUCTION
Because all competent patients have the right to decline recommended inpatient treatment, the ethical and legal standard is that the physician obtain the patient’s informed consent to leave by communicating the risks, benefits, and alternatives to leaving and fully documenting the conversation in the medical record.2 The additional steps of formalizing the discharge as AMA and providing AMA forms for the patient to sign have never been demonstrated to improve quality (and add needless clerical work). When declining any treatment, even life-sustaining treatment, the request for a patient signature to decline such treatment has not been demonstrated to improve risk communication and is not considered a best practice for informed consent.18 When the physician’s motives for this behavior are punitive or directed primarily at reducing liability, it may distract the physician from their fiduciary duty to put patients first.
The solution to improve quality is straightforward—avoid designating discharges as AMA. Instead, clinicians should maintain a single discharge process with clear, objective documentation including providing appropriate prescriptions and follow-up appointments regardless of whether the patient’s choice is consistent with a physician’s recommendation. In its place, the physician should use shared decision-making (SDM) and harm reduction principles to enhance the patient’s well-being within the identified constraints. SDM involves physicians and patients making healthcare decisions together by combining the patients’ values and preferences for care with the physicians’ expertise and knowledge of medical evidence. Harm reduction practices seek to reduce the adverse health consequences that may come from unhealthy behaviors while assuming that patients will likely continue such behaviors. Evidence-based and widely accepted examples of harm reduction strategies include nicotine replacement therapy and needle exchange programs.19
SDM in discharge planning provides a range of discharge and transitional care options that are within prevailing medical standards, not simply a single recommendation that prioritizes health promotion to the exclusion of other identified patient goals. Quality discharge planning should provide the “right care for the right patient at the right time”20 that moves beyond the false choice of either remaining in the hospital under the conditions specified by the physician or leaving AMA. Although physicians are understandably concerned about patients making choices that do not prioritize their health, physicians can consider the evidence for harm reduction programs’ effectiveness in improving health outcomes21 and accommodate patients by providing harm-reducing discharge options that, while suboptimal, may not be substandard.22
Physicians who wish to promote stronger patient-centered discharge practices may find that avoiding or limiting AMA discharges may conflict with their institution’s policy. In those cases, physicians should work closely with their leadership and legal counsel to ensure that any proposed practice changes are legally compliant but also improve SDM and reduce stigma for this population.
Although ending the clinical practice of designating discharges as AMA is unlikely to completely ameliorate the morbidity and costs associated with patients declining episodes of inpatient care, there is reasonable face validity to conclude that replacing the AMA practice with greater attention to harm reduction and SDM can reduce some of the preventable harms like stigmatization and reduced access to care. Together, these practices demonstrate the profession’s continued commitment to the public to practice patient-centered care.
RECOMMENDATIONS
- Treat all discharges similarly. Avoid designating an inpatient discharge as AMA.
- Ensure there is objective documentation of the patient’s informed choice to leave the hospital.
- When patients wish to leave the hospital prior to a physician-recommended clinical endpoint, engage in SDM with a focus on providing all medically reasonable treatment options that promote harm reduction.
- If you choose to designate a discharge as AMA, approach the discharge planning process consistently and with patient-centered principles by optimizing SDM and harm reduction.
CONCLUSION
The physician informed the patient of the risks, benefits, and alternatives to leaving the hospital prior to the completion of IV antibiotics and confirmed the patient’s decision-making capacity. Next, the physician elicited the patient’s preferences for care and identified competing priorities. The patient wanted treatment for his cellulitis, but he was experiencing pain and opioid withdrawal. The physician then expanded the range of potential treatment options, including evaluation for medication-assisted treatment for the patient’s opioid use disorder (OUD) and harm reduction measures such as safer injection practices, needle exchange, housing assistance, and overdose prevention and treatment education.23 An alternative harm-reducing option included discharge with oral antibiotics and follow-up with his primary physician in 48-72 hours. After the patient indicated that he wanted to leave because he was not yet ready for OUD treatment, he was discharged with the standard discharge paperwork and antibiotics, and the physician documented the informed consent discussion.
Disclosure
The authors report no conflicts of interest, financial or otherwise. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs, the VA National Center for Ethics in Health Care or the US Government.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing TWDFNR@hospitalmedicine.org
The “Things We Do for No Reason” (TWDFNR) series reviews practices which have become common parts of hospital care but which may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent “black and white” conclusions or clinical practice standards, but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion. https://www.choosingwisely.org/
Against medical advice (AMA) discharges, which account for up to 2% of all inpatient discharges, are associated with worse health and health services outcomes and disproportionately affect vulnerable patient populations. This paper will review the background data on AMA discharges as well as the reasons physicians may choose to discharge patients AMA. From a healthcare quality perspective, the designation of a discharge as AMA is low-value care in that it is a routine hospital practice without demonstrated benefit and is not supported by a strong evidence base. We argue that designating discharges as AMA has never been shown to advance patient care and that it has the potential to harm patients by reducing access to care and promoting stigma. We believe that greater attention to both shared decision-making as well as harm reduction principles in discharge planning can serve as effective, patient-centered alternatives when patients choose not to follow a healthcare professional’s recommended advice.
CASE PRESENTATION
A 54-year-old man with active intravenous (IV) drug use and hepatitis C was admitted with lower extremity cellulitis. On hospital day 2, the patient insisted that he wanted to go home. The treatment team informed the patient that an additional 2-3 days of IV antibiotics would produce a more reliable cure and reduce the risk of readmission. Should the team inform the patient that he will be discharged against medical advice (AMA) if he chooses to leave the hospital prematurely?
BACKGROUND
In the United States, patients are discharged AMA approximately 500,000 times per year (1%-2% of all discharges).1 These discharges represent a wide array of clinical scenarios that all culminate in the formal recognition and documentation of a competent patient’s choice to decline further inpatient medical care and leave the hospital prior to a recommended clinical endpoint. Compared with standard discharges, AMA discharges are associated with an increased adjusted relative risk of 30-day mortality as high as 10% and 30-day readmission rates that are 20%-40% higher than readmission rates following standard discharges.2 AMA discharges are more likely among patients with substance use disorders, psychiatric illness, and HIV.3
WHY YOU MIGHT THINK AMA DISCHARGES ARE HELPFUL
Although there are little empirical data to inform how and why physicians choose to designate a discharge as AMA when patients decline recommended care, the existing evidence suggests that fears of legal liability are strongly driving the practice.4 Physicians may believe that they must discharge patients AMA in order to fulfill their legal and ethical responsibilities, or to demonstrate in writing the physician’s concern and the significant risk of leaving.5,6 Clinicians may have been acculturated during training to believe that an AMA discharge may also be seen as a way of formally distancing themselves from the patient’s request for a nonstandard or unsafe discharge plan, thus deflecting any potential blame for worse patient outcomes.
Finally, clinicians and administrators may also believe that an AMA discharge is the appropriate designation for a hospital stay that ended because the patient chose to prematurely discontinue the treatment relationship or to decline the postdischarge placement recommendations. This reasoning may explain why the hospital penalties authorized by Medicare’s Hospital Readmission Reduction Program generally exclude initial admissions ending in an AMA discharge7 and may provide the rationale (and perhaps a financial incentive) to discharge patients AMA in order to limit CMS readmission penalties.
WHY AMA DISCHARGES ADD NO VALUE TO A PATIENT’S FULLY INFORMED DECLINATION OF CARE
The AMA discharge is a routine hospital practice without demonstrated patient benefit and which disproportionately affects vulnerable populations. There is also a growing literature that demonstrates that AMA discharges stigmatize patients, reduce their access to care, and can reduce the quality of informed consent discussions in discharge planning.8-10 Although there are no conclusive data that AMA discharges are more likely among underrepresented racial minorities, the disproportionate burden of AMA discharges and their worse health outcomes are borne by the homeless, those with substance use disorders, and the uninsured.3,11
Compared to patients discharged conventionally from an emergency department, 25% of patients discharged AMA reported not wanting to return for follow-up care.8 This reluctance to return for care is in part mediated by provider-generated stigma and blame9,12 and may be exacerbated when patients believe that their decision to leave AMA was based upon extenuating circumstance or competing necessity (eg, limited care options for their dependents, poor quality hospital care, etc.).
To persuade patients to remain hospitalized, 85% of trainees and 67% of attending physicians in one study incorrectly informed their patients that insurance will not reimburse a hospitalization if they leave AMA.13 Because this study demonstrated that there is no empirical evidence that payment after AMA discharges is denied by private or government payers, physicians sharing this misinformation can breed distrust and coercively undermine patients’ ability to make a voluntary choice.
When clinicians assert they are bound by duty to discharge a patient AMA, they may be conflating a presumed legal obligation to formally designate the discharge as AMA in the medical record with their actual obligation to obtain the patient’s informed consent for the discharge. In other words, there is no identifiable medico-legal requirement to specifically designate a discharge as AMA.
Although clinicians may presume that the AMA designation provides protection from liability, the claim is not supported by the available literature.14,15 In these studies, which reviewed relevant case law, defendants prevailed not because of the physician’s AMA designation, but because the plaintiff was not able to prove negligence. The proper execution of the discharge process, not the specific designation of AMA, is what conferred liability protection.5 Indeed, malpractice claims, which are associated with patient perceptions of feeling deserted or devalued,16 might be more likely with AMA discharges when they result from flawed and stigmatizing communication processes.17
Finally, there are no clinical, regulatory, or professional standards that specify the designation of an AMA discharge. Neither the Joint Commission nor any other professional organization specify under what conditions a clinician should discharge a patient AMA, thus promoting wide variability in its use and further limiting it as a valid and reliable healthcare metric.
WHAT SHOULD PHYSICIANS DO INSTEAD: AVOID THE AMA DESIGNATION AND PROMOTE SHARED DECISION-MAKING AND HARM REDUCTION
Because all competent patients have the right to decline recommended inpatient treatment, the ethical and legal standard is that the physician obtain the patient’s informed consent to leave by communicating the risks, benefits, and alternatives to leaving and fully documenting the conversation in the medical record.2 The additional steps of formalizing the discharge as AMA and providing AMA forms for the patient to sign have never been demonstrated to improve quality (and add needless clerical work). When declining any treatment, even life-sustaining treatment, the request for a patient signature to decline such treatment has not been demonstrated to improve risk communication and is not considered a best practice for informed consent.18 When the physician’s motives for this behavior are punitive or directed primarily at reducing liability, it may distract the physician from their fiduciary duty to put patients first.
The solution to improve quality is straightforward—avoid designating discharges as AMA. Instead, clinicians should maintain a single discharge process with clear, objective documentation including providing appropriate prescriptions and follow-up appointments regardless of whether the patient’s choice is consistent with a physician’s recommendation. In its place, the physician should use shared decision-making (SDM) and harm reduction principles to enhance the patient’s well-being within the identified constraints. SDM involves physicians and patients making healthcare decisions together by combining the patients’ values and preferences for care with the physicians’ expertise and knowledge of medical evidence. Harm reduction practices seek to reduce the adverse health consequences that may come from unhealthy behaviors while assuming that patients will likely continue such behaviors. Evidence-based and widely accepted examples of harm reduction strategies include nicotine replacement therapy and needle exchange programs.19
SDM in discharge planning provides a range of discharge and transitional care options that are within prevailing medical standards, not simply a single recommendation that prioritizes health promotion to the exclusion of other identified patient goals. Quality discharge planning should provide the “right care for the right patient at the right time”20 that moves beyond the false choice of either remaining in the hospital under the conditions specified by the physician or leaving AMA. Although physicians are understandably concerned about patients making choices that do not prioritize their health, physicians can consider the evidence for harm reduction programs’ effectiveness in improving health outcomes21 and accommodate patients by providing harm-reducing discharge options that, while suboptimal, may not be substandard.22
Physicians who wish to promote stronger patient-centered discharge practices may find that avoiding or limiting AMA discharges may conflict with their institution’s policy. In those cases, physicians should work closely with their leadership and legal counsel to ensure that any proposed practice changes are legally compliant but also improve SDM and reduce stigma for this population.
Although ending the clinical practice of designating discharges as AMA is unlikely to completely ameliorate the morbidity and costs associated with patients declining episodes of inpatient care, there is reasonable face validity to conclude that replacing the AMA practice with greater attention to harm reduction and SDM can reduce some of the preventable harms like stigmatization and reduced access to care. Together, these practices demonstrate the profession’s continued commitment to the public to practice patient-centered care.
RECOMMENDATIONS
- Treat all discharges similarly. Avoid designating an inpatient discharge as AMA.
- Ensure there is objective documentation of the patient’s informed choice to leave the hospital.
- When patients wish to leave the hospital prior to a physician-recommended clinical endpoint, engage in SDM with a focus on providing all medically reasonable treatment options that promote harm reduction.
- If you choose to designate a discharge as AMA, approach the discharge planning process consistently and with patient-centered principles by optimizing SDM and harm reduction.
CONCLUSION
The physician informed the patient of the risks, benefits, and alternatives to leaving the hospital prior to the completion of IV antibiotics and confirmed the patient’s decision-making capacity. Next, the physician elicited the patient’s preferences for care and identified competing priorities. The patient wanted treatment for his cellulitis, but he was experiencing pain and opioid withdrawal. The physician then expanded the range of potential treatment options, including evaluation for medication-assisted treatment for the patient’s opioid use disorder (OUD) and harm reduction measures such as safer injection practices, needle exchange, housing assistance, and overdose prevention and treatment education.23 An alternative harm-reducing option included discharge with oral antibiotics and follow-up with his primary physician in 48-72 hours. After the patient indicated that he wanted to leave because he was not yet ready for OUD treatment, he was discharged with the standard discharge paperwork and antibiotics, and the physician documented the informed consent discussion.
Disclosure
The authors report no conflicts of interest, financial or otherwise. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs, the VA National Center for Ethics in Health Care or the US Government.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason” topics by emailing TWDFNR@hospitalmedicine.org
1. Ibrahim SA, Kwoh CK, Krishnan E. Factors associated with patients who leave acute-care hospitals against medical advice. Am J Public Health. 2007;97(12):2204-2208. PubMed
2. Alfandre DJ. “I’m going home”: discharges against medical advice. Mayo Clin Proc. 2009;84(3):255-260. PubMed
3. Kraut A, Fransoo R, Olafson K, Ramsey CD, Yogendran M, Garland A. A population-based analysis of leaving the hospital against medical advice: incidence and associated variables. BMC Health Serv Res. 2013;13:415. PubMed
4. Green P, Watts D, Poole S, Dhopesh V. Why patients sign out against medical advice (AMA): factors motivating patients to sign out AMA. Am J Drug Alcohol Abuse. 2004;30(2):489-493. PubMed
5. Levy F, Mareiniss DP, Iacovelli C. The Importance of a Proper Against-Medical-Advice (AMA) Discharge: How Signing Out AMA May Create Significant Liability Protection for Providers. J Emerg Med. 2012;43(3):516-520. PubMed
6. Brenner J, Joslin J, Goulette A, Grant WD, Wojcik SM. Against Medical Advice: A Survey of ED Clinicians’ Rationale for Use. J Emerg Nurs. 2016;42(5):408-411. PubMed
7. Hospital-Wide (All-Condition) 30-Day Risk-Standardized Readmission Measure. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/downloads/MMSHospital-WideAll-ConditionReadmissionRate.pdf. Accessed on July 22, 2016.
8. Jerrard DA, Chasm RM. Patients leaving against medical advice (AMA) from the emergency department--disease prevalence and willingness to return. J Emerg Med. 2011;41(4):412-417. PubMed
9. Haywood C, Jr, Lanzkron S, Hughes MT, et al. A video-intervention to improve clinician attitudes toward patients with sickle cell disease: the results of a randomized experiment. J Gen Intern Med. 2011;26(5):518-523. PubMed
10. Wigder HN, Propp DA, Leslie K, Mathew A. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010;55(4):393. PubMed
11. Saab D, Nisenbaum R, Dhalla I, Hwang SW. Hospital Readmissions in a Community-based Sample of Homeless Adults: a Matched-cohort Study. J Gen Intern Med. 2016;31(9):1011-1018. PubMed
12. Lekas HM, Alfandre D, Gordon P, Harwood K, Yin MT. The role of patient-provider interactions: Using an accounts framework to explain hospital discharges against medical advice. Soc Sci Med. 2016;156:106-113. PubMed
13. Schaefer GR, Matus H, Schumann JH, et al. Financial Responsibility of Hospitalized Patients Who Left Against Medical Advice: Medical Urban Legend? J Gen Intern Med. 2012;27(7):825-830. PubMed
14. Devitt PJ, Devitt AC, Dewan M. Does identifying a discharge as “against medical advice” confer legal protection? J Fam Pract. 2000;49(3):224-227. PubMed
15. Devitt PJ, Devitt AC, Dewan M. An examination of whether discharging patients against medical advice protects physicians from malpractice charges. Psychiatr Serv. 2000;51(7):899-902. PubMed
16. Beckman HB, Markakis KM, Suchman AL, Frankel RM. The doctor-patient relationship and malpractice. Lessons from plaintiff depositions. Arch Intern Med. 1994;154(12):1365-1370. PubMed
17. Windish DM, Ratanawongsa N. Providers’ perceptions of relationships and professional roles when caring for patients who leave the hospital against medical advice. J Gen Intern Med. 2008;23(10):1698-1707. PubMed
18. Sulmasy DP, Sood JR, Texiera K, McAuley RL, McGugins J, Ury WA. A prospective trial of a new policy eliminating signed consent for do not resuscitate orders. J Gen Intern Med. 2006;21(12):1261-1268. PubMed
19. Stratton K, Shetty P, Wallace R, Bondurant S. Clearing the smoke: the science base for tobacco harm reduction--executive summary. Tob Control. 2001;10(2):189-195. PubMed
20. What is Health Care Quality and Who Decides?. March 2009. Agency for Healthcare Research and Quality, Rockville, MD. https://archive.ahrq.gov/news/speech/test031809.html
21. Hobden KL, Cunningham JA. Barriers to the dissemination of four harm reduction strategies: a survey of addiction treatment providers in Ontario. Harm Reduct J. 2006;3:35. PubMed
22. Alfandre D. Clinical Recommendations in Medical Practice: A Proposed Framework to Reduce Bias and Improve the Quality of Medical Decisions. J Clin Ethics. 2016;27(1):21-27. PubMed
23. Fanucchi L, Lofwall MR. Putting Parity into Practice - Integrating Opioid-Use Disorder Treatment into the Hospital Setting. N Engl J Med. 2016;375(9):811-813. PubMed
1. Ibrahim SA, Kwoh CK, Krishnan E. Factors associated with patients who leave acute-care hospitals against medical advice. Am J Public Health. 2007;97(12):2204-2208. PubMed
2. Alfandre DJ. “I’m going home”: discharges against medical advice. Mayo Clin Proc. 2009;84(3):255-260. PubMed
3. Kraut A, Fransoo R, Olafson K, Ramsey CD, Yogendran M, Garland A. A population-based analysis of leaving the hospital against medical advice: incidence and associated variables. BMC Health Serv Res. 2013;13:415. PubMed
4. Green P, Watts D, Poole S, Dhopesh V. Why patients sign out against medical advice (AMA): factors motivating patients to sign out AMA. Am J Drug Alcohol Abuse. 2004;30(2):489-493. PubMed
5. Levy F, Mareiniss DP, Iacovelli C. The Importance of a Proper Against-Medical-Advice (AMA) Discharge: How Signing Out AMA May Create Significant Liability Protection for Providers. J Emerg Med. 2012;43(3):516-520. PubMed
6. Brenner J, Joslin J, Goulette A, Grant WD, Wojcik SM. Against Medical Advice: A Survey of ED Clinicians’ Rationale for Use. J Emerg Nurs. 2016;42(5):408-411. PubMed
7. Hospital-Wide (All-Condition) 30-Day Risk-Standardized Readmission Measure. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/downloads/MMSHospital-WideAll-ConditionReadmissionRate.pdf. Accessed on July 22, 2016.
8. Jerrard DA, Chasm RM. Patients leaving against medical advice (AMA) from the emergency department--disease prevalence and willingness to return. J Emerg Med. 2011;41(4):412-417. PubMed
9. Haywood C, Jr, Lanzkron S, Hughes MT, et al. A video-intervention to improve clinician attitudes toward patients with sickle cell disease: the results of a randomized experiment. J Gen Intern Med. 2011;26(5):518-523. PubMed
10. Wigder HN, Propp DA, Leslie K, Mathew A. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010;55(4):393. PubMed
11. Saab D, Nisenbaum R, Dhalla I, Hwang SW. Hospital Readmissions in a Community-based Sample of Homeless Adults: a Matched-cohort Study. J Gen Intern Med. 2016;31(9):1011-1018. PubMed
12. Lekas HM, Alfandre D, Gordon P, Harwood K, Yin MT. The role of patient-provider interactions: Using an accounts framework to explain hospital discharges against medical advice. Soc Sci Med. 2016;156:106-113. PubMed
13. Schaefer GR, Matus H, Schumann JH, et al. Financial Responsibility of Hospitalized Patients Who Left Against Medical Advice: Medical Urban Legend? J Gen Intern Med. 2012;27(7):825-830. PubMed
14. Devitt PJ, Devitt AC, Dewan M. Does identifying a discharge as “against medical advice” confer legal protection? J Fam Pract. 2000;49(3):224-227. PubMed
15. Devitt PJ, Devitt AC, Dewan M. An examination of whether discharging patients against medical advice protects physicians from malpractice charges. Psychiatr Serv. 2000;51(7):899-902. PubMed
16. Beckman HB, Markakis KM, Suchman AL, Frankel RM. The doctor-patient relationship and malpractice. Lessons from plaintiff depositions. Arch Intern Med. 1994;154(12):1365-1370. PubMed
17. Windish DM, Ratanawongsa N. Providers’ perceptions of relationships and professional roles when caring for patients who leave the hospital against medical advice. J Gen Intern Med. 2008;23(10):1698-1707. PubMed
18. Sulmasy DP, Sood JR, Texiera K, McAuley RL, McGugins J, Ury WA. A prospective trial of a new policy eliminating signed consent for do not resuscitate orders. J Gen Intern Med. 2006;21(12):1261-1268. PubMed
19. Stratton K, Shetty P, Wallace R, Bondurant S. Clearing the smoke: the science base for tobacco harm reduction--executive summary. Tob Control. 2001;10(2):189-195. PubMed
20. What is Health Care Quality and Who Decides?. March 2009. Agency for Healthcare Research and Quality, Rockville, MD. https://archive.ahrq.gov/news/speech/test031809.html
21. Hobden KL, Cunningham JA. Barriers to the dissemination of four harm reduction strategies: a survey of addiction treatment providers in Ontario. Harm Reduct J. 2006;3:35. PubMed
22. Alfandre D. Clinical Recommendations in Medical Practice: A Proposed Framework to Reduce Bias and Improve the Quality of Medical Decisions. J Clin Ethics. 2016;27(1):21-27. PubMed
23. Fanucchi L, Lofwall MR. Putting Parity into Practice - Integrating Opioid-Use Disorder Treatment into the Hospital Setting. N Engl J Med. 2016;375(9):811-813. PubMed
©2017 Society of Hospital Medicine
Improving Quality in Against Medical Advice Discharges
Against Medical Advice (AMA) discharges, when a patient chooses to leave the hospital prior to a clinically specified and physician recommended endpoint, remain a healthcare quality problem. Patients who leave the hospital AMA challenge the healthcare professionals entrusted to care for them as well as the institutions that work to promote continuity and improved quality. AMA discharges account for up to 2% of all hospital discharges and, compared with conventional discharges, are associated with worse health and health services outcomes. Patients discharged AMA have higher rates of 30-day readmission, morbidity, and 30-day mortality.1,2 Additionally, the burden of worse health outcomes is disproportionate among disadvantaged patient populations. Patients with human immunodeficiency virus,3 substance use disorders,4 and psychiatric illness5 are more likely to be discharged AMA, as are patients with low socioeconomic status, without insurance, or with Medicaid insurance.
In this issue of the Journal of Hospital Medicine, Stearns and colleagues6 provide an important contribution to this area of medicine in need of more high quality empiric studies. The study reviewed all AMA discharges from a single year in an urban community hospital in order to assess provider perceptions and knowledge about AMA discharges. The study reconfirmed both the patient-level predictors of AMA discharges that have been demonstrated consistently (ie, male gender, younger age, Medicare or no insurance, and injection drug use) as well as the low rates of documentation of patient capacity, medication prescribed, and follow-up plans in AMA discharges.7
The authors’ investigation has also advanced the study of AMA discharges in two important directions. First, by characterizing patients with multiple AMA discharges, the authors focus on a more vulnerable population. These patients, who may have particular difficulty in consistently engaging in care, could help provide insight into the general phenomenon of AMA discharges. Second, the authors broadened their attention to include the study of nurses, a group of healthcare professionals who may play an important but not well recognized role in the AMA discharge process. In further characterizing nurses’ attitudes toward AMA discharges, medication prescriptions, and outpatient follow-up, the authors highlight nurses’ role in gathering critical patient information and promoting ethical practices in discharge planning. To better understand this dynamic and its potential role in mediating adverse health outcomes, further studies should also examine the attitudes of other central members of the treatment team (eg, pharmacists, social workers, etc.) who participate in discharge planning.
Inadequate documentation of AMA discharges remains a problem. In an attempt to address this, some institutions use AMA discharge forms to facilitate documentation of the informed consent process, the patient’s signed declination of care, medico-legal considerations, and the resulting treatment plan. Although systematic efforts to improve documentation should be encouraged, significant uncertainty about the optimal use of AMA discharge forms remains. Specifically, the use of a patient-signed AMA discharge form has not been demonstrated to advance patient care and may promote harm by stigmatizing patients8 and reducing the likelihood that they will pursue follow-up care.9 Furthermore, given that these forms may be written using institution-centered legalistic language or at an inappropriate reading level, this common hospital practice should be evaluated to assess whether patients comprehend and benefit from the forms, and how the forms influence healthcare decision making.10
Finally, the authors’ finding that 38% of nurses, 22% of physician trainees, and 6% of attendings believe patients discharged AMA lose the “right” to follow-up is noteworthy. The practice would suggest a significant lapse in understanding the professional obligation to acknowledge and communicate that the informed consent process is voluntary and patients have the right to decline recommended treatment without forfeiting future access to care. Harm reduction principles indicate that simply choosing to decline an episode of inpatient care does not make a patient ineligible for other medically indicated treatments and services. Previous studies have demonstrated that physicians may incorrectly inform patients that insurance will not pay for their care if they leave AMA, in order to persuade them to remain hospitalized.11 The current study suggests similar and potentially well-meaning but coercive attitudes about AMA discharge that can undermine a patient’s voluntary choice to accept medical care.
Stearns and colleagues6 rightly point to educational and policy interventions to improve the quality of care for patients discharged AMA. Additionally, setting patients’ expectations early in the hospitalization,12 empathically addressing their concerns,13 and sharing clinical decisions with patients by providing a medically reasonable range of clinical options rather than a single choice14 are practical bedside interventions that all clinicians can implement. System changes like developing clear policies and electronic medical records templates are particularly important, as they are more likely to lead to durable institutional change that is systematic, transparent, and fair. Moreover, research that expands the object of study beyond the physician-patient relationship could significantly improve outcomes in this vulnerable population of patients. Recent studies have begun to elucidate the deficiencies that may underlie communication failures with patients before they choose to leave AMA,15 how providers decide to designate a discharge as AMA,16 and how changing the structure and environment of care for patients who use injection drugs can reduce AMA discharges and improve health outcomes.17
AMA discharges are a persistent, complicated healthcare quality problem that defies an easy solution. Improving the quality of care for these patients will require building upon the empirical research base, providing enhanced education and guidance to healthcare professionals in the ethical and clinical management of AMA discharges, and making systems changes that promote enduring institutional change. We are moving in the right direction, but we have further to go.
Disclosures
The views expressed in this article are those of the author and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the National Center for Ethics in Health Care. The author has no conflicts of interest to disclose.
References
1. Alfandre DJ. “I’m going home”: discharges against medical advice. Mayo Clin Proc. 2009;84(3):255-260. PubMed
2. Southern WN, Nahvi S, Arnsten JH. Increased risk of mortality and readmission among patients discharged against medical advice. Am J Med. 2012;125(6):
594-602. PubMed
3. Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, O’Shaughnessy MV. Leaving hospital against medical advice among HIV-positive patients. CMAJ. 2002;167(6):633-637. PubMed
4. Chan AC, Palepu A, Guh DP, et al. HIV-positive injection drug users who leave the hospital against medical advice: the mitigating role of methadone and social support. J Acquir Immune Defic Syndr. 2004;35(1):56-59. PubMed
5. Kuo CJ, Tsai SY, Liao YT, Lee WC, Sung XW, Chen CC. Psychiatric discharge against medical advice is a risk factor for suicide but not for other causes of death. J Clin Psychiatry. 2010;71(6):808-809. PubMed
6. Edwards J, Markert R, Bricker D. Discharge against medical advice: how often do we intervene? J Hosp Med. 2013;8(10):574-577. PubMed
7. Stearns CR, Bakamjian A, Sattar S, Ritterman Weintraub M. Discharges against medical advice at a county hospital: provider perceptions and practice. J Hosp Med. 2017;12(1):11-17. PubMed
8. Windish DM, Ratanawongsa N. Providers’ perceptions of relationships and professional roles when caring for patients who leave the hospital against medical advice. J Gen Intern Med. 2008;23(10):1698-1707. PubMed
9. Jerrard DA, Chasm RM. Patients leaving against medical advice (AMA) from the emergency department—disease prevalence and willingness to return. J Emerg Med. 2011;41(4):412-417. PubMed
10. Alfandre D. Reconsidering against medical advice discharges: embracing patient-centeredness to promote high quality care and a renewed research agenda.
J Gen Intern Med. 2013;28(12):1657-1662. PubMed
11. Schaefer GR, Matus H, Schumann JH, et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012;27(7):825-830. PubMed
12. Steinglass P, Grantham CE, Hertzman M. Predicting which patients will be discharged against medical advice: a pilot study. Am J Psychiatry. 1980;137(11):
1385-1389. PubMed
13. Clark MA, Abbott JT, Adyanthaya T. Ethics seminars: a best-practice approach to navigating the against-medical-advice discharge. Acad Emerg Med. 2014;21(9):1050-1057. PubMed
14. Alfandre D. Clinical recommendations in medical practice: a proposed framework to reduce bias and improve the quality of medical decisions. J Clin Ethics. 2016;27(1):21-27. PubMed
15. Lekas HM, Alfandre D, Gordon P, Harwood K, Yin MT. The role of patient-provider interactions: Using an accounts framework to explain hospital discharges against medical advice. Soc Sci Med. 2016;156:106-113. PubMed
16. Brenner J, Joslin J, Goulette A, Grant WD, Wojcik SM. Against medical advice: A survey of ED clinicians’ rationale for use. J Emerg Nurs. 2016;42(5):408-411. PubMed
17. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. PubMed
Against Medical Advice (AMA) discharges, when a patient chooses to leave the hospital prior to a clinically specified and physician recommended endpoint, remain a healthcare quality problem. Patients who leave the hospital AMA challenge the healthcare professionals entrusted to care for them as well as the institutions that work to promote continuity and improved quality. AMA discharges account for up to 2% of all hospital discharges and, compared with conventional discharges, are associated with worse health and health services outcomes. Patients discharged AMA have higher rates of 30-day readmission, morbidity, and 30-day mortality.1,2 Additionally, the burden of worse health outcomes is disproportionate among disadvantaged patient populations. Patients with human immunodeficiency virus,3 substance use disorders,4 and psychiatric illness5 are more likely to be discharged AMA, as are patients with low socioeconomic status, without insurance, or with Medicaid insurance.
In this issue of the Journal of Hospital Medicine, Stearns and colleagues6 provide an important contribution to this area of medicine in need of more high quality empiric studies. The study reviewed all AMA discharges from a single year in an urban community hospital in order to assess provider perceptions and knowledge about AMA discharges. The study reconfirmed both the patient-level predictors of AMA discharges that have been demonstrated consistently (ie, male gender, younger age, Medicare or no insurance, and injection drug use) as well as the low rates of documentation of patient capacity, medication prescribed, and follow-up plans in AMA discharges.7
The authors’ investigation has also advanced the study of AMA discharges in two important directions. First, by characterizing patients with multiple AMA discharges, the authors focus on a more vulnerable population. These patients, who may have particular difficulty in consistently engaging in care, could help provide insight into the general phenomenon of AMA discharges. Second, the authors broadened their attention to include the study of nurses, a group of healthcare professionals who may play an important but not well recognized role in the AMA discharge process. In further characterizing nurses’ attitudes toward AMA discharges, medication prescriptions, and outpatient follow-up, the authors highlight nurses’ role in gathering critical patient information and promoting ethical practices in discharge planning. To better understand this dynamic and its potential role in mediating adverse health outcomes, further studies should also examine the attitudes of other central members of the treatment team (eg, pharmacists, social workers, etc.) who participate in discharge planning.
Inadequate documentation of AMA discharges remains a problem. In an attempt to address this, some institutions use AMA discharge forms to facilitate documentation of the informed consent process, the patient’s signed declination of care, medico-legal considerations, and the resulting treatment plan. Although systematic efforts to improve documentation should be encouraged, significant uncertainty about the optimal use of AMA discharge forms remains. Specifically, the use of a patient-signed AMA discharge form has not been demonstrated to advance patient care and may promote harm by stigmatizing patients8 and reducing the likelihood that they will pursue follow-up care.9 Furthermore, given that these forms may be written using institution-centered legalistic language or at an inappropriate reading level, this common hospital practice should be evaluated to assess whether patients comprehend and benefit from the forms, and how the forms influence healthcare decision making.10
Finally, the authors’ finding that 38% of nurses, 22% of physician trainees, and 6% of attendings believe patients discharged AMA lose the “right” to follow-up is noteworthy. The practice would suggest a significant lapse in understanding the professional obligation to acknowledge and communicate that the informed consent process is voluntary and patients have the right to decline recommended treatment without forfeiting future access to care. Harm reduction principles indicate that simply choosing to decline an episode of inpatient care does not make a patient ineligible for other medically indicated treatments and services. Previous studies have demonstrated that physicians may incorrectly inform patients that insurance will not pay for their care if they leave AMA, in order to persuade them to remain hospitalized.11 The current study suggests similar and potentially well-meaning but coercive attitudes about AMA discharge that can undermine a patient’s voluntary choice to accept medical care.
Stearns and colleagues6 rightly point to educational and policy interventions to improve the quality of care for patients discharged AMA. Additionally, setting patients’ expectations early in the hospitalization,12 empathically addressing their concerns,13 and sharing clinical decisions with patients by providing a medically reasonable range of clinical options rather than a single choice14 are practical bedside interventions that all clinicians can implement. System changes like developing clear policies and electronic medical records templates are particularly important, as they are more likely to lead to durable institutional change that is systematic, transparent, and fair. Moreover, research that expands the object of study beyond the physician-patient relationship could significantly improve outcomes in this vulnerable population of patients. Recent studies have begun to elucidate the deficiencies that may underlie communication failures with patients before they choose to leave AMA,15 how providers decide to designate a discharge as AMA,16 and how changing the structure and environment of care for patients who use injection drugs can reduce AMA discharges and improve health outcomes.17
AMA discharges are a persistent, complicated healthcare quality problem that defies an easy solution. Improving the quality of care for these patients will require building upon the empirical research base, providing enhanced education and guidance to healthcare professionals in the ethical and clinical management of AMA discharges, and making systems changes that promote enduring institutional change. We are moving in the right direction, but we have further to go.
Disclosures
The views expressed in this article are those of the author and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the National Center for Ethics in Health Care. The author has no conflicts of interest to disclose.
Against Medical Advice (AMA) discharges, when a patient chooses to leave the hospital prior to a clinically specified and physician recommended endpoint, remain a healthcare quality problem. Patients who leave the hospital AMA challenge the healthcare professionals entrusted to care for them as well as the institutions that work to promote continuity and improved quality. AMA discharges account for up to 2% of all hospital discharges and, compared with conventional discharges, are associated with worse health and health services outcomes. Patients discharged AMA have higher rates of 30-day readmission, morbidity, and 30-day mortality.1,2 Additionally, the burden of worse health outcomes is disproportionate among disadvantaged patient populations. Patients with human immunodeficiency virus,3 substance use disorders,4 and psychiatric illness5 are more likely to be discharged AMA, as are patients with low socioeconomic status, without insurance, or with Medicaid insurance.
In this issue of the Journal of Hospital Medicine, Stearns and colleagues6 provide an important contribution to this area of medicine in need of more high quality empiric studies. The study reviewed all AMA discharges from a single year in an urban community hospital in order to assess provider perceptions and knowledge about AMA discharges. The study reconfirmed both the patient-level predictors of AMA discharges that have been demonstrated consistently (ie, male gender, younger age, Medicare or no insurance, and injection drug use) as well as the low rates of documentation of patient capacity, medication prescribed, and follow-up plans in AMA discharges.7
The authors’ investigation has also advanced the study of AMA discharges in two important directions. First, by characterizing patients with multiple AMA discharges, the authors focus on a more vulnerable population. These patients, who may have particular difficulty in consistently engaging in care, could help provide insight into the general phenomenon of AMA discharges. Second, the authors broadened their attention to include the study of nurses, a group of healthcare professionals who may play an important but not well recognized role in the AMA discharge process. In further characterizing nurses’ attitudes toward AMA discharges, medication prescriptions, and outpatient follow-up, the authors highlight nurses’ role in gathering critical patient information and promoting ethical practices in discharge planning. To better understand this dynamic and its potential role in mediating adverse health outcomes, further studies should also examine the attitudes of other central members of the treatment team (eg, pharmacists, social workers, etc.) who participate in discharge planning.
Inadequate documentation of AMA discharges remains a problem. In an attempt to address this, some institutions use AMA discharge forms to facilitate documentation of the informed consent process, the patient’s signed declination of care, medico-legal considerations, and the resulting treatment plan. Although systematic efforts to improve documentation should be encouraged, significant uncertainty about the optimal use of AMA discharge forms remains. Specifically, the use of a patient-signed AMA discharge form has not been demonstrated to advance patient care and may promote harm by stigmatizing patients8 and reducing the likelihood that they will pursue follow-up care.9 Furthermore, given that these forms may be written using institution-centered legalistic language or at an inappropriate reading level, this common hospital practice should be evaluated to assess whether patients comprehend and benefit from the forms, and how the forms influence healthcare decision making.10
Finally, the authors’ finding that 38% of nurses, 22% of physician trainees, and 6% of attendings believe patients discharged AMA lose the “right” to follow-up is noteworthy. The practice would suggest a significant lapse in understanding the professional obligation to acknowledge and communicate that the informed consent process is voluntary and patients have the right to decline recommended treatment without forfeiting future access to care. Harm reduction principles indicate that simply choosing to decline an episode of inpatient care does not make a patient ineligible for other medically indicated treatments and services. Previous studies have demonstrated that physicians may incorrectly inform patients that insurance will not pay for their care if they leave AMA, in order to persuade them to remain hospitalized.11 The current study suggests similar and potentially well-meaning but coercive attitudes about AMA discharge that can undermine a patient’s voluntary choice to accept medical care.
Stearns and colleagues6 rightly point to educational and policy interventions to improve the quality of care for patients discharged AMA. Additionally, setting patients’ expectations early in the hospitalization,12 empathically addressing their concerns,13 and sharing clinical decisions with patients by providing a medically reasonable range of clinical options rather than a single choice14 are practical bedside interventions that all clinicians can implement. System changes like developing clear policies and electronic medical records templates are particularly important, as they are more likely to lead to durable institutional change that is systematic, transparent, and fair. Moreover, research that expands the object of study beyond the physician-patient relationship could significantly improve outcomes in this vulnerable population of patients. Recent studies have begun to elucidate the deficiencies that may underlie communication failures with patients before they choose to leave AMA,15 how providers decide to designate a discharge as AMA,16 and how changing the structure and environment of care for patients who use injection drugs can reduce AMA discharges and improve health outcomes.17
AMA discharges are a persistent, complicated healthcare quality problem that defies an easy solution. Improving the quality of care for these patients will require building upon the empirical research base, providing enhanced education and guidance to healthcare professionals in the ethical and clinical management of AMA discharges, and making systems changes that promote enduring institutional change. We are moving in the right direction, but we have further to go.
Disclosures
The views expressed in this article are those of the author and do not necessarily reflect the position or policy of the US Department of Veterans Affairs or the National Center for Ethics in Health Care. The author has no conflicts of interest to disclose.
References
1. Alfandre DJ. “I’m going home”: discharges against medical advice. Mayo Clin Proc. 2009;84(3):255-260. PubMed
2. Southern WN, Nahvi S, Arnsten JH. Increased risk of mortality and readmission among patients discharged against medical advice. Am J Med. 2012;125(6):
594-602. PubMed
3. Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, O’Shaughnessy MV. Leaving hospital against medical advice among HIV-positive patients. CMAJ. 2002;167(6):633-637. PubMed
4. Chan AC, Palepu A, Guh DP, et al. HIV-positive injection drug users who leave the hospital against medical advice: the mitigating role of methadone and social support. J Acquir Immune Defic Syndr. 2004;35(1):56-59. PubMed
5. Kuo CJ, Tsai SY, Liao YT, Lee WC, Sung XW, Chen CC. Psychiatric discharge against medical advice is a risk factor for suicide but not for other causes of death. J Clin Psychiatry. 2010;71(6):808-809. PubMed
6. Edwards J, Markert R, Bricker D. Discharge against medical advice: how often do we intervene? J Hosp Med. 2013;8(10):574-577. PubMed
7. Stearns CR, Bakamjian A, Sattar S, Ritterman Weintraub M. Discharges against medical advice at a county hospital: provider perceptions and practice. J Hosp Med. 2017;12(1):11-17. PubMed
8. Windish DM, Ratanawongsa N. Providers’ perceptions of relationships and professional roles when caring for patients who leave the hospital against medical advice. J Gen Intern Med. 2008;23(10):1698-1707. PubMed
9. Jerrard DA, Chasm RM. Patients leaving against medical advice (AMA) from the emergency department—disease prevalence and willingness to return. J Emerg Med. 2011;41(4):412-417. PubMed
10. Alfandre D. Reconsidering against medical advice discharges: embracing patient-centeredness to promote high quality care and a renewed research agenda.
J Gen Intern Med. 2013;28(12):1657-1662. PubMed
11. Schaefer GR, Matus H, Schumann JH, et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012;27(7):825-830. PubMed
12. Steinglass P, Grantham CE, Hertzman M. Predicting which patients will be discharged against medical advice: a pilot study. Am J Psychiatry. 1980;137(11):
1385-1389. PubMed
13. Clark MA, Abbott JT, Adyanthaya T. Ethics seminars: a best-practice approach to navigating the against-medical-advice discharge. Acad Emerg Med. 2014;21(9):1050-1057. PubMed
14. Alfandre D. Clinical recommendations in medical practice: a proposed framework to reduce bias and improve the quality of medical decisions. J Clin Ethics. 2016;27(1):21-27. PubMed
15. Lekas HM, Alfandre D, Gordon P, Harwood K, Yin MT. The role of patient-provider interactions: Using an accounts framework to explain hospital discharges against medical advice. Soc Sci Med. 2016;156:106-113. PubMed
16. Brenner J, Joslin J, Goulette A, Grant WD, Wojcik SM. Against medical advice: A survey of ED clinicians’ rationale for use. J Emerg Nurs. 2016;42(5):408-411. PubMed
17. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. PubMed
References
1. Alfandre DJ. “I’m going home”: discharges against medical advice. Mayo Clin Proc. 2009;84(3):255-260. PubMed
2. Southern WN, Nahvi S, Arnsten JH. Increased risk of mortality and readmission among patients discharged against medical advice. Am J Med. 2012;125(6):
594-602. PubMed
3. Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, O’Shaughnessy MV. Leaving hospital against medical advice among HIV-positive patients. CMAJ. 2002;167(6):633-637. PubMed
4. Chan AC, Palepu A, Guh DP, et al. HIV-positive injection drug users who leave the hospital against medical advice: the mitigating role of methadone and social support. J Acquir Immune Defic Syndr. 2004;35(1):56-59. PubMed
5. Kuo CJ, Tsai SY, Liao YT, Lee WC, Sung XW, Chen CC. Psychiatric discharge against medical advice is a risk factor for suicide but not for other causes of death. J Clin Psychiatry. 2010;71(6):808-809. PubMed
6. Edwards J, Markert R, Bricker D. Discharge against medical advice: how often do we intervene? J Hosp Med. 2013;8(10):574-577. PubMed
7. Stearns CR, Bakamjian A, Sattar S, Ritterman Weintraub M. Discharges against medical advice at a county hospital: provider perceptions and practice. J Hosp Med. 2017;12(1):11-17. PubMed
8. Windish DM, Ratanawongsa N. Providers’ perceptions of relationships and professional roles when caring for patients who leave the hospital against medical advice. J Gen Intern Med. 2008;23(10):1698-1707. PubMed
9. Jerrard DA, Chasm RM. Patients leaving against medical advice (AMA) from the emergency department—disease prevalence and willingness to return. J Emerg Med. 2011;41(4):412-417. PubMed
10. Alfandre D. Reconsidering against medical advice discharges: embracing patient-centeredness to promote high quality care and a renewed research agenda.
J Gen Intern Med. 2013;28(12):1657-1662. PubMed
11. Schaefer GR, Matus H, Schumann JH, et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012;27(7):825-830. PubMed
12. Steinglass P, Grantham CE, Hertzman M. Predicting which patients will be discharged against medical advice: a pilot study. Am J Psychiatry. 1980;137(11):
1385-1389. PubMed
13. Clark MA, Abbott JT, Adyanthaya T. Ethics seminars: a best-practice approach to navigating the against-medical-advice discharge. Acad Emerg Med. 2014;21(9):1050-1057. PubMed
14. Alfandre D. Clinical recommendations in medical practice: a proposed framework to reduce bias and improve the quality of medical decisions. J Clin Ethics. 2016;27(1):21-27. PubMed
15. Lekas HM, Alfandre D, Gordon P, Harwood K, Yin MT. The role of patient-provider interactions: Using an accounts framework to explain hospital discharges against medical advice. Soc Sci Med. 2016;156:106-113. PubMed
16. Brenner J, Joslin J, Goulette A, Grant WD, Wojcik SM. Against medical advice: A survey of ED clinicians’ rationale for use. J Emerg Nurs. 2016;42(5):408-411. PubMed
17. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. PubMed
© 2017 Society of Hospital Medicine