User login
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Observation Care
Many conditions once treated during an “inpatient” hospital stay are currently treated during an “observation” stay (OBS). Although the care remains the same, physician billing is different and requires close attention to admission details for effective charge capture.
Let’s take a look at a typical OBS scenario. A 65-year-old female with longstanding diabetes presents to the ED at 10 p.m. with palpitations, lightheadedness, mild disorientation, and elevated blood sugar. The hospitalist admits the patient to observation, treats her for dehydration, and discharges her the next day. Before billing, the hospitalist should consider the following factors.
Physician of Record
The attending of record writes the orders to admit the patient to observation; indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. The attending reports the initial patient encounter with the most appropriate initial observation-care code, as reflected by the documentation:1
- 99218: Initial observation care, requiring both a detailed or comprehensive history and exam, and straightforward/low-complexity medical decision-making. Usually, the problem(s) is of low severity.
- 99219: Initial observation care, requiring both a comprehensive history and exam, and moderate-complexity medical decision-making. Usually, the problem(s) is of moderate severity.
- 99220: Initial observation care, requiring both a comprehensive history and exam, and high-complexity medical decision-making. Usually, the problem(s) is of high severity.
While other physicians (e.g., specialists) might be involved in the patient’s care, only the attending physician reports codes 99218-99220. Specialists typically are called to an OBS case for their opinion or advice but do not function as the attending of record. Billing for the specialist (consultation) service depends upon the payor.
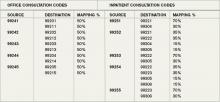
For a non-Medicare patient who pays for consultation codes, the specialist reports an outpatient consultation code (99241-99245) for the appropriately documented service. Conversely, Medicare no longer recognizes consultation codes, and specialists must report either a new patient visit code (99201-99205) or established patient visit code (99212-99215) for Medicare beneficiaries.
Selection of the new or established patient codes follows the “three-year rule”: A “new patient” has not received any face-to-face services (e.g., visit or procedure) in any location from any physician within the same group and same specialty within the past three years.2 There could be occasion when a hospitalist is not the attending of record but is asked to provide their opinion, and must report one of the “non-OBS” codes.
The attending of record is permitted to report a discharge service as long as this service occurs on a calendar day different from the admission service (as in the listed scenario). The attending documents the face-to-face discharge service and any pertinent clinical details, and reports 99217 (observation-care discharge-day management).
Length of Stay
Observation-care services typically do not exceed 24 hours and two calendar days. Observation care for more than 48 hours without inpatient admission is not considered medically necessary but might be payable after medical review. Should the OBS stay span more than two calendar days (as might be the case with “downgraded” hospitalizations), hospitalists should report established patient visit codes (99212-99215) for the calendar day(s) between the admission service (99218-99220) and the discharge service (99217).3 The physician must provide and document a face-to-face encounter on each date of service for which a claim was submitted.
A more likely occurrence is the admission and discharge from OBS on the same calendar date. The attending of record reports the code that corresponds to the patient’s length of stay (LOS). If the total LOS is less than eight hours, the attending only reports standard OBS codes (99218-99220). The hospitalist does not separately report the OBS discharge service (99217), even though the documentation must reflect the attending discharge order and corresponding discharge plan. If the total duration of the patient’s stay lasts more than eight hours and does not overlap two calendar days, the attending reports the same-day admit/discharge codes:1
- 99234: Observation or inpatient care, same date admission and discharge, requiring both a detailed or comprehensive history and exam, and straightforward or low-complexity medical decision-making. Usually the presenting problem(s) is of low severity.
- 99235: Observation or inpatient care, same date admission and discharge, requiring a comprehensive history and exam, and moderate-complexity medical decision-making. Usually the presenting problem(s) is of moderate severity.
- 99236: Observation or inpatient care, same date admission and discharge, requiring a comprehensive history and exam, and high-complexity medical decision-making. Usually the presenting problem(s) is of high severity.
OBS discharge service (99217) is not separately reported with 99234-99236 because these codes are valued to include the discharge component (e.g., the comprehensive service, 99236 [4.26 wRVU, $211], is equivalent to its components, 99220 [2.99 wRVU, $148] and 99217 [1.28 wRVU, $68]). The attending must document the total duration of the stay, as well as the face-to-face service and the corresponding details of each service component (i.e., both an admission and discharge note).3TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:11-16.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.7A. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 11, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8C. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 11, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8D. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 11, 2010.
- Medicare Claims Processing Manual: Chapter 1, Section 50.3. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c01.pdf. Accessed May 12, 2010.
Many conditions once treated during an “inpatient” hospital stay are currently treated during an “observation” stay (OBS). Although the care remains the same, physician billing is different and requires close attention to admission details for effective charge capture.
Let’s take a look at a typical OBS scenario. A 65-year-old female with longstanding diabetes presents to the ED at 10 p.m. with palpitations, lightheadedness, mild disorientation, and elevated blood sugar. The hospitalist admits the patient to observation, treats her for dehydration, and discharges her the next day. Before billing, the hospitalist should consider the following factors.
Physician of Record
The attending of record writes the orders to admit the patient to observation; indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. The attending reports the initial patient encounter with the most appropriate initial observation-care code, as reflected by the documentation:1
- 99218: Initial observation care, requiring both a detailed or comprehensive history and exam, and straightforward/low-complexity medical decision-making. Usually, the problem(s) is of low severity.
- 99219: Initial observation care, requiring both a comprehensive history and exam, and moderate-complexity medical decision-making. Usually, the problem(s) is of moderate severity.
- 99220: Initial observation care, requiring both a comprehensive history and exam, and high-complexity medical decision-making. Usually, the problem(s) is of high severity.
While other physicians (e.g., specialists) might be involved in the patient’s care, only the attending physician reports codes 99218-99220. Specialists typically are called to an OBS case for their opinion or advice but do not function as the attending of record. Billing for the specialist (consultation) service depends upon the payor.
For a non-Medicare patient who pays for consultation codes, the specialist reports an outpatient consultation code (99241-99245) for the appropriately documented service. Conversely, Medicare no longer recognizes consultation codes, and specialists must report either a new patient visit code (99201-99205) or established patient visit code (99212-99215) for Medicare beneficiaries.
Selection of the new or established patient codes follows the “three-year rule”: A “new patient” has not received any face-to-face services (e.g., visit or procedure) in any location from any physician within the same group and same specialty within the past three years.2 There could be occasion when a hospitalist is not the attending of record but is asked to provide their opinion, and must report one of the “non-OBS” codes.
The attending of record is permitted to report a discharge service as long as this service occurs on a calendar day different from the admission service (as in the listed scenario). The attending documents the face-to-face discharge service and any pertinent clinical details, and reports 99217 (observation-care discharge-day management).
Length of Stay
Observation-care services typically do not exceed 24 hours and two calendar days. Observation care for more than 48 hours without inpatient admission is not considered medically necessary but might be payable after medical review. Should the OBS stay span more than two calendar days (as might be the case with “downgraded” hospitalizations), hospitalists should report established patient visit codes (99212-99215) for the calendar day(s) between the admission service (99218-99220) and the discharge service (99217).3 The physician must provide and document a face-to-face encounter on each date of service for which a claim was submitted.
A more likely occurrence is the admission and discharge from OBS on the same calendar date. The attending of record reports the code that corresponds to the patient’s length of stay (LOS). If the total LOS is less than eight hours, the attending only reports standard OBS codes (99218-99220). The hospitalist does not separately report the OBS discharge service (99217), even though the documentation must reflect the attending discharge order and corresponding discharge plan. If the total duration of the patient’s stay lasts more than eight hours and does not overlap two calendar days, the attending reports the same-day admit/discharge codes:1
- 99234: Observation or inpatient care, same date admission and discharge, requiring both a detailed or comprehensive history and exam, and straightforward or low-complexity medical decision-making. Usually the presenting problem(s) is of low severity.
- 99235: Observation or inpatient care, same date admission and discharge, requiring a comprehensive history and exam, and moderate-complexity medical decision-making. Usually the presenting problem(s) is of moderate severity.
- 99236: Observation or inpatient care, same date admission and discharge, requiring a comprehensive history and exam, and high-complexity medical decision-making. Usually the presenting problem(s) is of high severity.
OBS discharge service (99217) is not separately reported with 99234-99236 because these codes are valued to include the discharge component (e.g., the comprehensive service, 99236 [4.26 wRVU, $211], is equivalent to its components, 99220 [2.99 wRVU, $148] and 99217 [1.28 wRVU, $68]). The attending must document the total duration of the stay, as well as the face-to-face service and the corresponding details of each service component (i.e., both an admission and discharge note).3TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:11-16.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.7A. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 11, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8C. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 11, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8D. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 11, 2010.
- Medicare Claims Processing Manual: Chapter 1, Section 50.3. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c01.pdf. Accessed May 12, 2010.
Many conditions once treated during an “inpatient” hospital stay are currently treated during an “observation” stay (OBS). Although the care remains the same, physician billing is different and requires close attention to admission details for effective charge capture.
Let’s take a look at a typical OBS scenario. A 65-year-old female with longstanding diabetes presents to the ED at 10 p.m. with palpitations, lightheadedness, mild disorientation, and elevated blood sugar. The hospitalist admits the patient to observation, treats her for dehydration, and discharges her the next day. Before billing, the hospitalist should consider the following factors.
Physician of Record
The attending of record writes the orders to admit the patient to observation; indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. The attending reports the initial patient encounter with the most appropriate initial observation-care code, as reflected by the documentation:1
- 99218: Initial observation care, requiring both a detailed or comprehensive history and exam, and straightforward/low-complexity medical decision-making. Usually, the problem(s) is of low severity.
- 99219: Initial observation care, requiring both a comprehensive history and exam, and moderate-complexity medical decision-making. Usually, the problem(s) is of moderate severity.
- 99220: Initial observation care, requiring both a comprehensive history and exam, and high-complexity medical decision-making. Usually, the problem(s) is of high severity.
While other physicians (e.g., specialists) might be involved in the patient’s care, only the attending physician reports codes 99218-99220. Specialists typically are called to an OBS case for their opinion or advice but do not function as the attending of record. Billing for the specialist (consultation) service depends upon the payor.
For a non-Medicare patient who pays for consultation codes, the specialist reports an outpatient consultation code (99241-99245) for the appropriately documented service. Conversely, Medicare no longer recognizes consultation codes, and specialists must report either a new patient visit code (99201-99205) or established patient visit code (99212-99215) for Medicare beneficiaries.
Selection of the new or established patient codes follows the “three-year rule”: A “new patient” has not received any face-to-face services (e.g., visit or procedure) in any location from any physician within the same group and same specialty within the past three years.2 There could be occasion when a hospitalist is not the attending of record but is asked to provide their opinion, and must report one of the “non-OBS” codes.
The attending of record is permitted to report a discharge service as long as this service occurs on a calendar day different from the admission service (as in the listed scenario). The attending documents the face-to-face discharge service and any pertinent clinical details, and reports 99217 (observation-care discharge-day management).
Length of Stay
Observation-care services typically do not exceed 24 hours and two calendar days. Observation care for more than 48 hours without inpatient admission is not considered medically necessary but might be payable after medical review. Should the OBS stay span more than two calendar days (as might be the case with “downgraded” hospitalizations), hospitalists should report established patient visit codes (99212-99215) for the calendar day(s) between the admission service (99218-99220) and the discharge service (99217).3 The physician must provide and document a face-to-face encounter on each date of service for which a claim was submitted.
A more likely occurrence is the admission and discharge from OBS on the same calendar date. The attending of record reports the code that corresponds to the patient’s length of stay (LOS). If the total LOS is less than eight hours, the attending only reports standard OBS codes (99218-99220). The hospitalist does not separately report the OBS discharge service (99217), even though the documentation must reflect the attending discharge order and corresponding discharge plan. If the total duration of the patient’s stay lasts more than eight hours and does not overlap two calendar days, the attending reports the same-day admit/discharge codes:1
- 99234: Observation or inpatient care, same date admission and discharge, requiring both a detailed or comprehensive history and exam, and straightforward or low-complexity medical decision-making. Usually the presenting problem(s) is of low severity.
- 99235: Observation or inpatient care, same date admission and discharge, requiring a comprehensive history and exam, and moderate-complexity medical decision-making. Usually the presenting problem(s) is of moderate severity.
- 99236: Observation or inpatient care, same date admission and discharge, requiring a comprehensive history and exam, and high-complexity medical decision-making. Usually the presenting problem(s) is of high severity.
OBS discharge service (99217) is not separately reported with 99234-99236 because these codes are valued to include the discharge component (e.g., the comprehensive service, 99236 [4.26 wRVU, $211], is equivalent to its components, 99220 [2.99 wRVU, $148] and 99217 [1.28 wRVU, $68]). The attending must document the total duration of the stay, as well as the face-to-face service and the corresponding details of each service component (i.e., both an admission and discharge note).3TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:11-16.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.7A. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 11, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8C. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 11, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8D. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 11, 2010.
- Medicare Claims Processing Manual: Chapter 1, Section 50.3. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c01.pdf. Accessed May 12, 2010.
Discharge Services
Discharge day management services (99238-99239) seem unlikely to cause confusion in the physician community; however, continued requests for documentation involving these CPT codes prove the opposite.
Here’s an example of how a billing error might be made for discharge day management services. A patient with diabetes mellitus, hypertension, and chronic kidney disease is stable for discharge. The patient is being transferred to a skilled nursing facility (SNF). Dr. Aardsma prepares the patient for hospital discharge, and Dr. Broxton admits the patient to the SNF later that day. Dr. Aardsma and Dr. Broxton are members of the same group practice, with the same specialty designation. Can both physicians report their services?
Key Elements
Consider the basic billing principles of discharge services: what, who, and when.
Hospital discharge day management codes are used to report the physician’s total duration of time spent preparing the patient for discharge. These codes include, as appropriate:
- Final examination of the patient;
- Discussion of the hospital stay, even if the time spent by the physician on that date is not continuous;
- Instructions for continuing care to all relevant caregivers; and
- Preparation of discharge records, prescriptions, and referral forms.1
Hospitalists should report one discharge code per hospitalization, but only when the service occurs after the initial date of admission: 99238, hospital discharge day management, 30 minutes or less; or 99239, hospital discharge day management, more than 30 minutes.1,2 Select one of the two codes, depending upon the cumulative discharge service time provided on the patient’s hospital unit/floor during a single calendar day. Do not count time for services performed outside of the patient’s unit or floor (i.e., calls to the receiving physician/facility made from the physician’s private office) or services performed after the patient physically leaves the hospital.
Physician documentation must refer to the discharge status, as well as other clinically relevant information. Don’t be misled into believing that the presence of a discharge summary alone satisfies documentation requirements. In addition to the discharge groundwork, hospitalists must physically see the patient on the day he or she reports discharge management. Discharge summaries are not always useful in noting the physician’s required face-to-face encounter with the patient. Simply state, “Patient seen and examined by me on discharge day.”
Alternatively, hospitalists can elect to include details of a discharge day exam. Although a final exam isn’t mandatory for billing 99238-99239, it is the best justification of a face-to-face encounter on discharge day. Documentation of the time is required when reporting 99239 (e.g., discharge time >30 minutes). Time isn’t typically included in a discharge summary, and upon post-payment payor review, a claim involving 99239 without documented time in the patient’s medical record might result in either a service reduction to the lower level of care (99238) or a request for payment refund.3 Physicians can document all necessary details in the formal summary or a progress note.
Transfers of Care
The admitting physician or group is responsible for performing discharge services unless a formal transfer of care occurs, such as the patient’s transfer from the ICU to the standard medical floor as the patient’s condition improves. Without this transfer of care, comanaging physicians should merely report subsequent hospital-care codes (99231-99233) for the final patient encounter. An example of this is surgical comanagement: If a surgeon is identified as the attending of record, they are responsible for postoperative management of the patient, including discharge services.4,5 Providers in a different group or specialty report 99231-99233 for their medically necessary care.
As with all other time-based services, only the billing provider’s time counts. Discharge-related services performed by residents, students, or ancillary staff (i.e., RNs) do not count toward the physician’s discharge service time. Report the date of the physician’s actual discharge visit even if the patient leaves the facility on a different calendar date—for example, if a patient leaves the next day due to availability of the receiving facility.
Pronouncement of Death
Physicians might not realize that they can report discharge day management codes for pronouncement of death.7 Only the hospitalist who performs the pronouncement is allowed to report this service on the date pronouncement occurred, even if the paperwork is delayed to a subsequent date. Completion of the death certificate alone is not sufficient for billing. Hospitalists must “examine” the patient, thus satisfying the “face to face” visit requirement.
Additional services (e.g., speaking with family members, speaking with healthcare providers, filling out the necessary documentation) count toward the cumulative discharge service time, if performed on the patient’s unit or floor. Document the cumulative time when reporting 99239.
Back to the Case
Typical billing and payment rules mandate the reporting of only one E/M service per specialty, per patient, per day. One of the few exceptions involves reporting a hospital discharge code (99238-99239) with initial nursing facility care (99304-99306). Either the same physician or different physicians from the same group and specialty can report the hospital discharge and the nursing facility admission on the same day. When the same physician or group discharges the patient from any other location (e.g., observation unit) on the same day, report only one service: either the observation discharge (99217) or the initial nursing facility care (99304-99306).
When the same physician or group discharges a patient from the hospital and admits the patient to a facility other than a nursing facility on the same day, report only one service: either the hospital discharge (99228-99239) or the admission care (e.g., long-term acute-care hospital: 99221-99223). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1C. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 3, 2010.
- Highmark Medicare Services Provider Bulletins: Hospital Discharge Day Management Codes 99238 and 99239. Highmark Medicare Services Web site. Available at: www.highmarkmedicareservices.com/bulletins/partb/news02212008a.html. Accessed March 4, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.1A. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.3B. Centers for Medicare & Medicaid Services Web site, Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.2E. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1d. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Reporting inpatient hospital evaluation and management (E/M) services that could be described by current procedural terminology (CPT) consultation codes. Cigna Government Services Web site. Available at: www.cignagovernmentservices.com/partb/pubs/news/2010/0210/cope11694.html. Accessed March 5, 2010.
Discharge day management services (99238-99239) seem unlikely to cause confusion in the physician community; however, continued requests for documentation involving these CPT codes prove the opposite.
Here’s an example of how a billing error might be made for discharge day management services. A patient with diabetes mellitus, hypertension, and chronic kidney disease is stable for discharge. The patient is being transferred to a skilled nursing facility (SNF). Dr. Aardsma prepares the patient for hospital discharge, and Dr. Broxton admits the patient to the SNF later that day. Dr. Aardsma and Dr. Broxton are members of the same group practice, with the same specialty designation. Can both physicians report their services?
Key Elements
Consider the basic billing principles of discharge services: what, who, and when.
Hospital discharge day management codes are used to report the physician’s total duration of time spent preparing the patient for discharge. These codes include, as appropriate:
- Final examination of the patient;
- Discussion of the hospital stay, even if the time spent by the physician on that date is not continuous;
- Instructions for continuing care to all relevant caregivers; and
- Preparation of discharge records, prescriptions, and referral forms.1
Hospitalists should report one discharge code per hospitalization, but only when the service occurs after the initial date of admission: 99238, hospital discharge day management, 30 minutes or less; or 99239, hospital discharge day management, more than 30 minutes.1,2 Select one of the two codes, depending upon the cumulative discharge service time provided on the patient’s hospital unit/floor during a single calendar day. Do not count time for services performed outside of the patient’s unit or floor (i.e., calls to the receiving physician/facility made from the physician’s private office) or services performed after the patient physically leaves the hospital.
Physician documentation must refer to the discharge status, as well as other clinically relevant information. Don’t be misled into believing that the presence of a discharge summary alone satisfies documentation requirements. In addition to the discharge groundwork, hospitalists must physically see the patient on the day he or she reports discharge management. Discharge summaries are not always useful in noting the physician’s required face-to-face encounter with the patient. Simply state, “Patient seen and examined by me on discharge day.”
Alternatively, hospitalists can elect to include details of a discharge day exam. Although a final exam isn’t mandatory for billing 99238-99239, it is the best justification of a face-to-face encounter on discharge day. Documentation of the time is required when reporting 99239 (e.g., discharge time >30 minutes). Time isn’t typically included in a discharge summary, and upon post-payment payor review, a claim involving 99239 without documented time in the patient’s medical record might result in either a service reduction to the lower level of care (99238) or a request for payment refund.3 Physicians can document all necessary details in the formal summary or a progress note.
Transfers of Care
The admitting physician or group is responsible for performing discharge services unless a formal transfer of care occurs, such as the patient’s transfer from the ICU to the standard medical floor as the patient’s condition improves. Without this transfer of care, comanaging physicians should merely report subsequent hospital-care codes (99231-99233) for the final patient encounter. An example of this is surgical comanagement: If a surgeon is identified as the attending of record, they are responsible for postoperative management of the patient, including discharge services.4,5 Providers in a different group or specialty report 99231-99233 for their medically necessary care.
As with all other time-based services, only the billing provider’s time counts. Discharge-related services performed by residents, students, or ancillary staff (i.e., RNs) do not count toward the physician’s discharge service time. Report the date of the physician’s actual discharge visit even if the patient leaves the facility on a different calendar date—for example, if a patient leaves the next day due to availability of the receiving facility.
Pronouncement of Death
Physicians might not realize that they can report discharge day management codes for pronouncement of death.7 Only the hospitalist who performs the pronouncement is allowed to report this service on the date pronouncement occurred, even if the paperwork is delayed to a subsequent date. Completion of the death certificate alone is not sufficient for billing. Hospitalists must “examine” the patient, thus satisfying the “face to face” visit requirement.
Additional services (e.g., speaking with family members, speaking with healthcare providers, filling out the necessary documentation) count toward the cumulative discharge service time, if performed on the patient’s unit or floor. Document the cumulative time when reporting 99239.
Back to the Case
Typical billing and payment rules mandate the reporting of only one E/M service per specialty, per patient, per day. One of the few exceptions involves reporting a hospital discharge code (99238-99239) with initial nursing facility care (99304-99306). Either the same physician or different physicians from the same group and specialty can report the hospital discharge and the nursing facility admission on the same day. When the same physician or group discharges the patient from any other location (e.g., observation unit) on the same day, report only one service: either the observation discharge (99217) or the initial nursing facility care (99304-99306).
When the same physician or group discharges a patient from the hospital and admits the patient to a facility other than a nursing facility on the same day, report only one service: either the hospital discharge (99228-99239) or the admission care (e.g., long-term acute-care hospital: 99221-99223). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1C. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 3, 2010.
- Highmark Medicare Services Provider Bulletins: Hospital Discharge Day Management Codes 99238 and 99239. Highmark Medicare Services Web site. Available at: www.highmarkmedicareservices.com/bulletins/partb/news02212008a.html. Accessed March 4, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.1A. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.3B. Centers for Medicare & Medicaid Services Web site, Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.2E. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1d. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Reporting inpatient hospital evaluation and management (E/M) services that could be described by current procedural terminology (CPT) consultation codes. Cigna Government Services Web site. Available at: www.cignagovernmentservices.com/partb/pubs/news/2010/0210/cope11694.html. Accessed March 5, 2010.
Discharge day management services (99238-99239) seem unlikely to cause confusion in the physician community; however, continued requests for documentation involving these CPT codes prove the opposite.
Here’s an example of how a billing error might be made for discharge day management services. A patient with diabetes mellitus, hypertension, and chronic kidney disease is stable for discharge. The patient is being transferred to a skilled nursing facility (SNF). Dr. Aardsma prepares the patient for hospital discharge, and Dr. Broxton admits the patient to the SNF later that day. Dr. Aardsma and Dr. Broxton are members of the same group practice, with the same specialty designation. Can both physicians report their services?
Key Elements
Consider the basic billing principles of discharge services: what, who, and when.
Hospital discharge day management codes are used to report the physician’s total duration of time spent preparing the patient for discharge. These codes include, as appropriate:
- Final examination of the patient;
- Discussion of the hospital stay, even if the time spent by the physician on that date is not continuous;
- Instructions for continuing care to all relevant caregivers; and
- Preparation of discharge records, prescriptions, and referral forms.1
Hospitalists should report one discharge code per hospitalization, but only when the service occurs after the initial date of admission: 99238, hospital discharge day management, 30 minutes or less; or 99239, hospital discharge day management, more than 30 minutes.1,2 Select one of the two codes, depending upon the cumulative discharge service time provided on the patient’s hospital unit/floor during a single calendar day. Do not count time for services performed outside of the patient’s unit or floor (i.e., calls to the receiving physician/facility made from the physician’s private office) or services performed after the patient physically leaves the hospital.
Physician documentation must refer to the discharge status, as well as other clinically relevant information. Don’t be misled into believing that the presence of a discharge summary alone satisfies documentation requirements. In addition to the discharge groundwork, hospitalists must physically see the patient on the day he or she reports discharge management. Discharge summaries are not always useful in noting the physician’s required face-to-face encounter with the patient. Simply state, “Patient seen and examined by me on discharge day.”
Alternatively, hospitalists can elect to include details of a discharge day exam. Although a final exam isn’t mandatory for billing 99238-99239, it is the best justification of a face-to-face encounter on discharge day. Documentation of the time is required when reporting 99239 (e.g., discharge time >30 minutes). Time isn’t typically included in a discharge summary, and upon post-payment payor review, a claim involving 99239 without documented time in the patient’s medical record might result in either a service reduction to the lower level of care (99238) or a request for payment refund.3 Physicians can document all necessary details in the formal summary or a progress note.
Transfers of Care
The admitting physician or group is responsible for performing discharge services unless a formal transfer of care occurs, such as the patient’s transfer from the ICU to the standard medical floor as the patient’s condition improves. Without this transfer of care, comanaging physicians should merely report subsequent hospital-care codes (99231-99233) for the final patient encounter. An example of this is surgical comanagement: If a surgeon is identified as the attending of record, they are responsible for postoperative management of the patient, including discharge services.4,5 Providers in a different group or specialty report 99231-99233 for their medically necessary care.
As with all other time-based services, only the billing provider’s time counts. Discharge-related services performed by residents, students, or ancillary staff (i.e., RNs) do not count toward the physician’s discharge service time. Report the date of the physician’s actual discharge visit even if the patient leaves the facility on a different calendar date—for example, if a patient leaves the next day due to availability of the receiving facility.
Pronouncement of Death
Physicians might not realize that they can report discharge day management codes for pronouncement of death.7 Only the hospitalist who performs the pronouncement is allowed to report this service on the date pronouncement occurred, even if the paperwork is delayed to a subsequent date. Completion of the death certificate alone is not sufficient for billing. Hospitalists must “examine” the patient, thus satisfying the “face to face” visit requirement.
Additional services (e.g., speaking with family members, speaking with healthcare providers, filling out the necessary documentation) count toward the cumulative discharge service time, if performed on the patient’s unit or floor. Document the cumulative time when reporting 99239.
Back to the Case
Typical billing and payment rules mandate the reporting of only one E/M service per specialty, per patient, per day. One of the few exceptions involves reporting a hospital discharge code (99238-99239) with initial nursing facility care (99304-99306). Either the same physician or different physicians from the same group and specialty can report the hospital discharge and the nursing facility admission on the same day. When the same physician or group discharges the patient from any other location (e.g., observation unit) on the same day, report only one service: either the observation discharge (99217) or the initial nursing facility care (99304-99306).
When the same physician or group discharges a patient from the hospital and admits the patient to a facility other than a nursing facility on the same day, report only one service: either the hospital discharge (99228-99239) or the admission care (e.g., long-term acute-care hospital: 99221-99223). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1C. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 3, 2010.
- Highmark Medicare Services Provider Bulletins: Hospital Discharge Day Management Codes 99238 and 99239. Highmark Medicare Services Web site. Available at: www.highmarkmedicareservices.com/bulletins/partb/news02212008a.html. Accessed March 4, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.1A. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 40.3B. Centers for Medicare & Medicaid Services Web site, Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.2E. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1d. Centers for Medicare & Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 5, 2010.
- Reporting inpatient hospital evaluation and management (E/M) services that could be described by current procedural terminology (CPT) consultation codes. Cigna Government Services Web site. Available at: www.cignagovernmentservices.com/partb/pubs/news/2010/0210/cope11694.html. Accessed March 5, 2010.
Admit Documentation
In light of the recent elimination of consultation codes from the Medicare Physician Fee Schedule, physicians of all specialties are being asked to report initial hospital care services (99221-99223) for their first encounter with a patient.1 This leaves hospitalists with questions about the billing and financial implications of reporting admissions services.
Here’s a typical scenario: Dr. A admits a Medicare patient to the hospital from the ED for hyperglycemia and dehydration in the setting of uncontrolled diabetes. He performs and documents an initial hospital-care service on day one of the admission. On day two, another hospitalist, Dr. B, who works in the same HM group, sees the patient for the first time. What should each of the physicians report for their first encounter with the patient?
Each hospitalist should select the CPT code that best fits the service and their role in the case. Remember, only one physician is named “attending of record” or “admitting physician.”
When billing during the course of the hospitalization, consider all physicians of the same specialty in the same provider group as the “admitting physician/group.”
Admissions Service
On day one, Dr. A admits the patient. He performs and documents a comprehensive history, a comprehensive exam, and medical decision-making of high complexity. The documentation corresponds to the highest initial admission service, 99223. Given the recent Medicare billing changes, the attending of record is required to append modifier “AI” (principal physician of record) to the admission service (e.g., 99223-AI).
The purpose of this modifier is “to identify the physician who oversees the patient’s care from all other physicians who may be furnishing specialty care.”2 This modifier has no financial implications. It does not increase or decrease the payment associated with the reported visit level (i.e., 99223 is reimbursed at a national rate of approximately $190, with or without modifier AI).
Initial Encounter by Team Members
As previously stated, the elimination of consultation services requires physicians to report their initial hospital encounter with an initial hospital-care code (i.e., 99221-99223). However, Medicare states that “physicians in the same group practice who are in the same specialty must bill and be paid as though they were a single physician.”3 This means followup services performed on days subsequent to a group member’s initial admission service must be reported with subsequent hospital-care codes (99231-99233). Therefore, in the scenario above, Dr. B is obligated to report the appropriate subsequent hospital-care code for his patient encounter on day two.
Incomplete Documentation
Initial hospital-care services (99221-99223) require the physician to obtain, perform, and document the necessary elements of history, physical exam, and medical decision-making in support of the code reported on the claim. There are occasions when the physician’s documentation does not support the lowest code (i.e., 99221). A reasonable approach is to report the service with an unlisted E&M code (99499). “Unlisted” codes do not have a payor-recognized code description or fee. When reporting an unlisted code, the biller must manually enter a charge description (e.g., expanded problem-focused admissions service) and a fee. A payor-prompted request for documentation is likely before payment is made.
Some payors have more specific references to the situation and allow for options. Two options exist for coding services that do not meet the work and/or medical necessity requirements of 99221-99223: report an unlisted E&M service (99499); or report a subsequent hospital care code (99231-99233) that appropriately reflects physician work and medical necessity for the service, and avoids mandatory medical record submission and manual medical review.4
In fact, Medicare Administrator Contractor TrailBlazer Health’s Web site (www.trailblazerhealth.com) offers guidance to physicians who are unsure if subsequent hospital care is an appropriate choice for this dilemma: “TrailBlazer recognizes provider reluctance to miscode initial hospital care as subsequent hospital care. However, doing so is preferable in that it allows Medicare to process and pay the claims much more efficiently. For those concerned about miscoding these services, please understand that TrailBlazer will not find fault with providers who choose this option when records appropriately demonstrate the work and medical necessity of the subsequent code chosen.”4 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- CMS announces payment, policy changes for physicians services to Medicare beneficiaries in 2010. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/apps/media/ press/release.asp?Counter=3539&intNumPerPage=10&checkDate=&checkKey=&srchType=1&numDays=3500&srchOpt=0&srchData=&keywordType=All&chkNewsType=1%2C+2%2C+3%2C+4%2C+5&intPage=&showAll=&pYear=&year=&desc=&cboOrder=date. Accessed Nov. 12, 2009.
- Revisions to Consultation Services Payment Policy. Medicare Learning Network Web site. Available at: www.cms.hhs.gov/MLNMattersArticles/downloads/ MM6740.pdf. Accessed Jan. 16, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2010.
- Update-evaluation and management services formerly coded as consultations. Trailblazer Health Enterprises Web site. Available at: www.trailblazerhealth.com/Tools/Notices.aspx?DomainID=1. Accessed Jan. 17, 2010.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2009;14-15.
In light of the recent elimination of consultation codes from the Medicare Physician Fee Schedule, physicians of all specialties are being asked to report initial hospital care services (99221-99223) for their first encounter with a patient.1 This leaves hospitalists with questions about the billing and financial implications of reporting admissions services.
Here’s a typical scenario: Dr. A admits a Medicare patient to the hospital from the ED for hyperglycemia and dehydration in the setting of uncontrolled diabetes. He performs and documents an initial hospital-care service on day one of the admission. On day two, another hospitalist, Dr. B, who works in the same HM group, sees the patient for the first time. What should each of the physicians report for their first encounter with the patient?
Each hospitalist should select the CPT code that best fits the service and their role in the case. Remember, only one physician is named “attending of record” or “admitting physician.”
When billing during the course of the hospitalization, consider all physicians of the same specialty in the same provider group as the “admitting physician/group.”
Admissions Service
On day one, Dr. A admits the patient. He performs and documents a comprehensive history, a comprehensive exam, and medical decision-making of high complexity. The documentation corresponds to the highest initial admission service, 99223. Given the recent Medicare billing changes, the attending of record is required to append modifier “AI” (principal physician of record) to the admission service (e.g., 99223-AI).
The purpose of this modifier is “to identify the physician who oversees the patient’s care from all other physicians who may be furnishing specialty care.”2 This modifier has no financial implications. It does not increase or decrease the payment associated with the reported visit level (i.e., 99223 is reimbursed at a national rate of approximately $190, with or without modifier AI).
Initial Encounter by Team Members
As previously stated, the elimination of consultation services requires physicians to report their initial hospital encounter with an initial hospital-care code (i.e., 99221-99223). However, Medicare states that “physicians in the same group practice who are in the same specialty must bill and be paid as though they were a single physician.”3 This means followup services performed on days subsequent to a group member’s initial admission service must be reported with subsequent hospital-care codes (99231-99233). Therefore, in the scenario above, Dr. B is obligated to report the appropriate subsequent hospital-care code for his patient encounter on day two.
Incomplete Documentation
Initial hospital-care services (99221-99223) require the physician to obtain, perform, and document the necessary elements of history, physical exam, and medical decision-making in support of the code reported on the claim. There are occasions when the physician’s documentation does not support the lowest code (i.e., 99221). A reasonable approach is to report the service with an unlisted E&M code (99499). “Unlisted” codes do not have a payor-recognized code description or fee. When reporting an unlisted code, the biller must manually enter a charge description (e.g., expanded problem-focused admissions service) and a fee. A payor-prompted request for documentation is likely before payment is made.
Some payors have more specific references to the situation and allow for options. Two options exist for coding services that do not meet the work and/or medical necessity requirements of 99221-99223: report an unlisted E&M service (99499); or report a subsequent hospital care code (99231-99233) that appropriately reflects physician work and medical necessity for the service, and avoids mandatory medical record submission and manual medical review.4
In fact, Medicare Administrator Contractor TrailBlazer Health’s Web site (www.trailblazerhealth.com) offers guidance to physicians who are unsure if subsequent hospital care is an appropriate choice for this dilemma: “TrailBlazer recognizes provider reluctance to miscode initial hospital care as subsequent hospital care. However, doing so is preferable in that it allows Medicare to process and pay the claims much more efficiently. For those concerned about miscoding these services, please understand that TrailBlazer will not find fault with providers who choose this option when records appropriately demonstrate the work and medical necessity of the subsequent code chosen.”4 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- CMS announces payment, policy changes for physicians services to Medicare beneficiaries in 2010. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/apps/media/ press/release.asp?Counter=3539&intNumPerPage=10&checkDate=&checkKey=&srchType=1&numDays=3500&srchOpt=0&srchData=&keywordType=All&chkNewsType=1%2C+2%2C+3%2C+4%2C+5&intPage=&showAll=&pYear=&year=&desc=&cboOrder=date. Accessed Nov. 12, 2009.
- Revisions to Consultation Services Payment Policy. Medicare Learning Network Web site. Available at: www.cms.hhs.gov/MLNMattersArticles/downloads/ MM6740.pdf. Accessed Jan. 16, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2010.
- Update-evaluation and management services formerly coded as consultations. Trailblazer Health Enterprises Web site. Available at: www.trailblazerhealth.com/Tools/Notices.aspx?DomainID=1. Accessed Jan. 17, 2010.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2009;14-15.
In light of the recent elimination of consultation codes from the Medicare Physician Fee Schedule, physicians of all specialties are being asked to report initial hospital care services (99221-99223) for their first encounter with a patient.1 This leaves hospitalists with questions about the billing and financial implications of reporting admissions services.
Here’s a typical scenario: Dr. A admits a Medicare patient to the hospital from the ED for hyperglycemia and dehydration in the setting of uncontrolled diabetes. He performs and documents an initial hospital-care service on day one of the admission. On day two, another hospitalist, Dr. B, who works in the same HM group, sees the patient for the first time. What should each of the physicians report for their first encounter with the patient?
Each hospitalist should select the CPT code that best fits the service and their role in the case. Remember, only one physician is named “attending of record” or “admitting physician.”
When billing during the course of the hospitalization, consider all physicians of the same specialty in the same provider group as the “admitting physician/group.”
Admissions Service
On day one, Dr. A admits the patient. He performs and documents a comprehensive history, a comprehensive exam, and medical decision-making of high complexity. The documentation corresponds to the highest initial admission service, 99223. Given the recent Medicare billing changes, the attending of record is required to append modifier “AI” (principal physician of record) to the admission service (e.g., 99223-AI).
The purpose of this modifier is “to identify the physician who oversees the patient’s care from all other physicians who may be furnishing specialty care.”2 This modifier has no financial implications. It does not increase or decrease the payment associated with the reported visit level (i.e., 99223 is reimbursed at a national rate of approximately $190, with or without modifier AI).
Initial Encounter by Team Members
As previously stated, the elimination of consultation services requires physicians to report their initial hospital encounter with an initial hospital-care code (i.e., 99221-99223). However, Medicare states that “physicians in the same group practice who are in the same specialty must bill and be paid as though they were a single physician.”3 This means followup services performed on days subsequent to a group member’s initial admission service must be reported with subsequent hospital-care codes (99231-99233). Therefore, in the scenario above, Dr. B is obligated to report the appropriate subsequent hospital-care code for his patient encounter on day two.
Incomplete Documentation
Initial hospital-care services (99221-99223) require the physician to obtain, perform, and document the necessary elements of history, physical exam, and medical decision-making in support of the code reported on the claim. There are occasions when the physician’s documentation does not support the lowest code (i.e., 99221). A reasonable approach is to report the service with an unlisted E&M code (99499). “Unlisted” codes do not have a payor-recognized code description or fee. When reporting an unlisted code, the biller must manually enter a charge description (e.g., expanded problem-focused admissions service) and a fee. A payor-prompted request for documentation is likely before payment is made.
Some payors have more specific references to the situation and allow for options. Two options exist for coding services that do not meet the work and/or medical necessity requirements of 99221-99223: report an unlisted E&M service (99499); or report a subsequent hospital care code (99231-99233) that appropriately reflects physician work and medical necessity for the service, and avoids mandatory medical record submission and manual medical review.4
In fact, Medicare Administrator Contractor TrailBlazer Health’s Web site (www.trailblazerhealth.com) offers guidance to physicians who are unsure if subsequent hospital care is an appropriate choice for this dilemma: “TrailBlazer recognizes provider reluctance to miscode initial hospital care as subsequent hospital care. However, doing so is preferable in that it allows Medicare to process and pay the claims much more efficiently. For those concerned about miscoding these services, please understand that TrailBlazer will not find fault with providers who choose this option when records appropriately demonstrate the work and medical necessity of the subsequent code chosen.”4 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- CMS announces payment, policy changes for physicians services to Medicare beneficiaries in 2010. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/apps/media/ press/release.asp?Counter=3539&intNumPerPage=10&checkDate=&checkKey=&srchType=1&numDays=3500&srchOpt=0&srchData=&keywordType=All&chkNewsType=1%2C+2%2C+3%2C+4%2C+5&intPage=&showAll=&pYear=&year=&desc=&cboOrder=date. Accessed Nov. 12, 2009.
- Revisions to Consultation Services Payment Policy. Medicare Learning Network Web site. Available at: www.cms.hhs.gov/MLNMattersArticles/downloads/ MM6740.pdf. Accessed Jan. 16, 2010.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2010.
- Update-evaluation and management services formerly coded as consultations. Trailblazer Health Enterprises Web site. Available at: www.trailblazerhealth.com/Tools/Notices.aspx?DomainID=1. Accessed Jan. 17, 2010.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2009;14-15.
Consultation Elimination
As of Jan. 1, the Centers for Medicare and Medicaid Services (CMS) ceased physician payment for consultations. The elimination of consult codes will affect physician group payments as well as relative-value-unit (RVU)-based incentive payments to individual physicians.
The Medicare-designated status of outpatient consultation (99241-99245) and inpatient consultation (99251-99255) codes has changed from “A” (separately payable under the physician fee schedule, when covered) to “I” (not valid for Medicare purposes; Medicare uses another code for the reporting of and the payment for these services). So if you submit consultation codes for Medicare beneficiaries, the result will be nonpayment.
While many physicians fear the negative impact of this ruling, hospitalists should consider its potential. Let’s take a look at a scenario hospitalists encounter on a routine basis.
Typical HM Scenario
A surgeon admits a 76-year-old man for aortic valve replacement. The patient’s history also includes well-controlled hypertension and chronic obstructive pulmonary disease (COPD). Postoperatively, the patient experiences an exacerbation of COPD related to anesthesia, elevated blood pressure, and hyperglycemia. The surgeon requests the hospitalist’s advice on appropriate medical interventions of these conditions. How should the hospitalist report the initial encounter with this Medicare beneficiary?
The hospitalist should select the CPT code that best fits the service and the payor. While most physicians regard this requested service as an inpatient consultation (99251-99255), Medicare no longer recognizes those codes. Instead, the hospitalist should report this encounter as an initial hospital care service (99221-99223).
Comanagement Issues
CMS and Medicare administrative contractors regularly uncover reporting errors for co-management requests. CMS decided the nature of these services were not consultative because the surgeon is not asking the physician or qualified nonphysician provider’s (NPP’s) opinion or advice for the surgeon’s use in treating the patient. Instead, these services constituted concurrent care and should have been billed using subsequent hospital care codes (99231-99233) in the hospital inpatient setting, subsequent NF care codes (99307-99310) in the SNF/NF setting, or office or other outpatient visit codes (99201-99215) in the office or outpatient settings.1
The new ruling simplifies coding and reduces reporting errors. The initial encounter with the patient is reported as such. Regardless of who is the attending of record or the consultant, the first physician from a particular provider group reports initial hospital care codes (i.e., 99221-99223) to represent the first patient encounter, even when this encounter does not occur on the admission date. Other physicians of the same specialty within the same provider group will not be permitted to report initial hospital care codes for their own initial encounter if someone from the group and specialty has already seen the patient during that hospitalization. In other words, the first hospitalist in the provider group reports 9922x, while the remaining hospitalists use subsequent hospital care codes (9923x).
In order to differentiate “consultant” services from “attending” services, CMS will be creating a modifier. The anticipated “AI” modifier must be appended to the attending physician’s initial encounter. Other initial hospital care codes reported throughout the hospital stay, as appropriate, are presumed to be that of “consultants” (i.e., physicians with a different specialty designation than the attending physician) participating in the case. Therefore, the hospitalist now can rightfully recover the increased work effort of the initial patient encounter (99223: 3.79 relative value units, ~$147 vs. 99233: 2.0 relative value units, ~$78, based on 2010 Medicare rates). Physicians will be required to meet the minimum documentation required for the selected visit code.
Other and Undefined Service Locations
Consultations in nursing facilities are handled much like inpatient hospital care. Physicians should report initial nursing facility services (99203-99306) for the first patient encounter, and subsequent nursing facility care codes (99307-99310) for each encounter thereafter. The attending physician of record appends the assigned modifier (presumed to be “AI”) when submitting their initial care service. All other initial care codes are presumed to be those of “consulting” physicians.
Initial information from CMS does not address observation services. Logically, these hospital-based services would follow the same methodology as inpatient care: report initial observation care (99218-99220) for the first “consulting” encounter. However, this might not be appropriate given Medicare’s existing rules for observation services, which guide physicians other than the admitting physician/group to “bill the office and other outpatient service codes or outpatient consultation codes as appropriate when they provide services to the patient.”2 With Medicare’s elimination of consultation codes, the consultant reports “office and other outpatient service codes” (i.e., new patient, 99201-99205, or established patient codes, 99212-99215) by default.
Without further clarification on observation services, hospitalists should report new or established patient service codes, depending on whether the patient has been seen by a group member within the last three years.
Medicare also has existing guidelines for the ED, which suggest that any physician not meeting the consultation criteria report ED service codes (99281-99285). Without further clarification, hospitalists should continue to follow this instruction for Medicare beneficiaries.
Nonphysician Providers
Medicare’s split/shared billing guidelines apply to most hospital inpatient, hospital outpatient, and ED evaluation and management (E/M) services, with consultations as one exception. Now, in accordance with the new ruling, hospitalists should select the appropriate initial service codes that correspond to patient’s location (e.g., 99223 for inpatients). NPPs can participate in the initial service provided to patients in these locations without the hospitalist having to replicate the entire service. The hospitalist can submit the claim in their name after selecting the visit level based upon the cumulative service personally provided on the same calendar day by both the NPP and the physician. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.10I. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/ manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8A. CMS Web site. Available at: www. cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- PFS Federal Regulation Notices: Proposed Revisions to Payment Policies Under the Physician Fee Schedule and Part B for CY 2010. CMS Web site. Available at: www.cms.hhs.gov/PhysicianFeeSched/PFSFRN/itemdetail.asp?filterType=none&filterByDID=99&sortByDID=4&sortOrder=descending&itemID=CMS1223902&intNumPerPage=10. Accessed Nov. 12, 2009.
- Payment Policies Under the Physician Fee Schedule and Other Revisions to Part B (for CY 2010). CMS Web site. Available at: www.federalregister.gov/OFR Upload/OFRData/2009-26502_PI.pdf. Accessed Nov. 10, 2009.
As of Jan. 1, the Centers for Medicare and Medicaid Services (CMS) ceased physician payment for consultations. The elimination of consult codes will affect physician group payments as well as relative-value-unit (RVU)-based incentive payments to individual physicians.
The Medicare-designated status of outpatient consultation (99241-99245) and inpatient consultation (99251-99255) codes has changed from “A” (separately payable under the physician fee schedule, when covered) to “I” (not valid for Medicare purposes; Medicare uses another code for the reporting of and the payment for these services). So if you submit consultation codes for Medicare beneficiaries, the result will be nonpayment.
While many physicians fear the negative impact of this ruling, hospitalists should consider its potential. Let’s take a look at a scenario hospitalists encounter on a routine basis.
Typical HM Scenario
A surgeon admits a 76-year-old man for aortic valve replacement. The patient’s history also includes well-controlled hypertension and chronic obstructive pulmonary disease (COPD). Postoperatively, the patient experiences an exacerbation of COPD related to anesthesia, elevated blood pressure, and hyperglycemia. The surgeon requests the hospitalist’s advice on appropriate medical interventions of these conditions. How should the hospitalist report the initial encounter with this Medicare beneficiary?
The hospitalist should select the CPT code that best fits the service and the payor. While most physicians regard this requested service as an inpatient consultation (99251-99255), Medicare no longer recognizes those codes. Instead, the hospitalist should report this encounter as an initial hospital care service (99221-99223).
Comanagement Issues
CMS and Medicare administrative contractors regularly uncover reporting errors for co-management requests. CMS decided the nature of these services were not consultative because the surgeon is not asking the physician or qualified nonphysician provider’s (NPP’s) opinion or advice for the surgeon’s use in treating the patient. Instead, these services constituted concurrent care and should have been billed using subsequent hospital care codes (99231-99233) in the hospital inpatient setting, subsequent NF care codes (99307-99310) in the SNF/NF setting, or office or other outpatient visit codes (99201-99215) in the office or outpatient settings.1
The new ruling simplifies coding and reduces reporting errors. The initial encounter with the patient is reported as such. Regardless of who is the attending of record or the consultant, the first physician from a particular provider group reports initial hospital care codes (i.e., 99221-99223) to represent the first patient encounter, even when this encounter does not occur on the admission date. Other physicians of the same specialty within the same provider group will not be permitted to report initial hospital care codes for their own initial encounter if someone from the group and specialty has already seen the patient during that hospitalization. In other words, the first hospitalist in the provider group reports 9922x, while the remaining hospitalists use subsequent hospital care codes (9923x).
In order to differentiate “consultant” services from “attending” services, CMS will be creating a modifier. The anticipated “AI” modifier must be appended to the attending physician’s initial encounter. Other initial hospital care codes reported throughout the hospital stay, as appropriate, are presumed to be that of “consultants” (i.e., physicians with a different specialty designation than the attending physician) participating in the case. Therefore, the hospitalist now can rightfully recover the increased work effort of the initial patient encounter (99223: 3.79 relative value units, ~$147 vs. 99233: 2.0 relative value units, ~$78, based on 2010 Medicare rates). Physicians will be required to meet the minimum documentation required for the selected visit code.
Other and Undefined Service Locations
Consultations in nursing facilities are handled much like inpatient hospital care. Physicians should report initial nursing facility services (99203-99306) for the first patient encounter, and subsequent nursing facility care codes (99307-99310) for each encounter thereafter. The attending physician of record appends the assigned modifier (presumed to be “AI”) when submitting their initial care service. All other initial care codes are presumed to be those of “consulting” physicians.
Initial information from CMS does not address observation services. Logically, these hospital-based services would follow the same methodology as inpatient care: report initial observation care (99218-99220) for the first “consulting” encounter. However, this might not be appropriate given Medicare’s existing rules for observation services, which guide physicians other than the admitting physician/group to “bill the office and other outpatient service codes or outpatient consultation codes as appropriate when they provide services to the patient.”2 With Medicare’s elimination of consultation codes, the consultant reports “office and other outpatient service codes” (i.e., new patient, 99201-99205, or established patient codes, 99212-99215) by default.
Without further clarification on observation services, hospitalists should report new or established patient service codes, depending on whether the patient has been seen by a group member within the last three years.
Medicare also has existing guidelines for the ED, which suggest that any physician not meeting the consultation criteria report ED service codes (99281-99285). Without further clarification, hospitalists should continue to follow this instruction for Medicare beneficiaries.
Nonphysician Providers
Medicare’s split/shared billing guidelines apply to most hospital inpatient, hospital outpatient, and ED evaluation and management (E/M) services, with consultations as one exception. Now, in accordance with the new ruling, hospitalists should select the appropriate initial service codes that correspond to patient’s location (e.g., 99223 for inpatients). NPPs can participate in the initial service provided to patients in these locations without the hospitalist having to replicate the entire service. The hospitalist can submit the claim in their name after selecting the visit level based upon the cumulative service personally provided on the same calendar day by both the NPP and the physician. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.10I. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/ manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8A. CMS Web site. Available at: www. cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- PFS Federal Regulation Notices: Proposed Revisions to Payment Policies Under the Physician Fee Schedule and Part B for CY 2010. CMS Web site. Available at: www.cms.hhs.gov/PhysicianFeeSched/PFSFRN/itemdetail.asp?filterType=none&filterByDID=99&sortByDID=4&sortOrder=descending&itemID=CMS1223902&intNumPerPage=10. Accessed Nov. 12, 2009.
- Payment Policies Under the Physician Fee Schedule and Other Revisions to Part B (for CY 2010). CMS Web site. Available at: www.federalregister.gov/OFR Upload/OFRData/2009-26502_PI.pdf. Accessed Nov. 10, 2009.
As of Jan. 1, the Centers for Medicare and Medicaid Services (CMS) ceased physician payment for consultations. The elimination of consult codes will affect physician group payments as well as relative-value-unit (RVU)-based incentive payments to individual physicians.
The Medicare-designated status of outpatient consultation (99241-99245) and inpatient consultation (99251-99255) codes has changed from “A” (separately payable under the physician fee schedule, when covered) to “I” (not valid for Medicare purposes; Medicare uses another code for the reporting of and the payment for these services). So if you submit consultation codes for Medicare beneficiaries, the result will be nonpayment.
While many physicians fear the negative impact of this ruling, hospitalists should consider its potential. Let’s take a look at a scenario hospitalists encounter on a routine basis.
Typical HM Scenario
A surgeon admits a 76-year-old man for aortic valve replacement. The patient’s history also includes well-controlled hypertension and chronic obstructive pulmonary disease (COPD). Postoperatively, the patient experiences an exacerbation of COPD related to anesthesia, elevated blood pressure, and hyperglycemia. The surgeon requests the hospitalist’s advice on appropriate medical interventions of these conditions. How should the hospitalist report the initial encounter with this Medicare beneficiary?
The hospitalist should select the CPT code that best fits the service and the payor. While most physicians regard this requested service as an inpatient consultation (99251-99255), Medicare no longer recognizes those codes. Instead, the hospitalist should report this encounter as an initial hospital care service (99221-99223).
Comanagement Issues
CMS and Medicare administrative contractors regularly uncover reporting errors for co-management requests. CMS decided the nature of these services were not consultative because the surgeon is not asking the physician or qualified nonphysician provider’s (NPP’s) opinion or advice for the surgeon’s use in treating the patient. Instead, these services constituted concurrent care and should have been billed using subsequent hospital care codes (99231-99233) in the hospital inpatient setting, subsequent NF care codes (99307-99310) in the SNF/NF setting, or office or other outpatient visit codes (99201-99215) in the office or outpatient settings.1
The new ruling simplifies coding and reduces reporting errors. The initial encounter with the patient is reported as such. Regardless of who is the attending of record or the consultant, the first physician from a particular provider group reports initial hospital care codes (i.e., 99221-99223) to represent the first patient encounter, even when this encounter does not occur on the admission date. Other physicians of the same specialty within the same provider group will not be permitted to report initial hospital care codes for their own initial encounter if someone from the group and specialty has already seen the patient during that hospitalization. In other words, the first hospitalist in the provider group reports 9922x, while the remaining hospitalists use subsequent hospital care codes (9923x).
In order to differentiate “consultant” services from “attending” services, CMS will be creating a modifier. The anticipated “AI” modifier must be appended to the attending physician’s initial encounter. Other initial hospital care codes reported throughout the hospital stay, as appropriate, are presumed to be that of “consultants” (i.e., physicians with a different specialty designation than the attending physician) participating in the case. Therefore, the hospitalist now can rightfully recover the increased work effort of the initial patient encounter (99223: 3.79 relative value units, ~$147 vs. 99233: 2.0 relative value units, ~$78, based on 2010 Medicare rates). Physicians will be required to meet the minimum documentation required for the selected visit code.
Other and Undefined Service Locations
Consultations in nursing facilities are handled much like inpatient hospital care. Physicians should report initial nursing facility services (99203-99306) for the first patient encounter, and subsequent nursing facility care codes (99307-99310) for each encounter thereafter. The attending physician of record appends the assigned modifier (presumed to be “AI”) when submitting their initial care service. All other initial care codes are presumed to be those of “consulting” physicians.
Initial information from CMS does not address observation services. Logically, these hospital-based services would follow the same methodology as inpatient care: report initial observation care (99218-99220) for the first “consulting” encounter. However, this might not be appropriate given Medicare’s existing rules for observation services, which guide physicians other than the admitting physician/group to “bill the office and other outpatient service codes or outpatient consultation codes as appropriate when they provide services to the patient.”2 With Medicare’s elimination of consultation codes, the consultant reports “office and other outpatient service codes” (i.e., new patient, 99201-99205, or established patient codes, 99212-99215) by default.
Without further clarification on observation services, hospitalists should report new or established patient service codes, depending on whether the patient has been seen by a group member within the last three years.
Medicare also has existing guidelines for the ED, which suggest that any physician not meeting the consultation criteria report ED service codes (99281-99285). Without further clarification, hospitalists should continue to follow this instruction for Medicare beneficiaries.
Nonphysician Providers
Medicare’s split/shared billing guidelines apply to most hospital inpatient, hospital outpatient, and ED evaluation and management (E/M) services, with consultations as one exception. Now, in accordance with the new ruling, hospitalists should select the appropriate initial service codes that correspond to patient’s location (e.g., 99223 for inpatients). NPPs can participate in the initial service provided to patients in these locations without the hospitalist having to replicate the entire service. The hospitalist can submit the claim in their name after selecting the visit level based upon the cumulative service personally provided on the same calendar day by both the NPP and the physician. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.10I. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/ manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.8A. CMS Web site. Available at: www. cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2009.
- PFS Federal Regulation Notices: Proposed Revisions to Payment Policies Under the Physician Fee Schedule and Part B for CY 2010. CMS Web site. Available at: www.cms.hhs.gov/PhysicianFeeSched/PFSFRN/itemdetail.asp?filterType=none&filterByDID=99&sortByDID=4&sortOrder=descending&itemID=CMS1223902&intNumPerPage=10. Accessed Nov. 12, 2009.
- Payment Policies Under the Physician Fee Schedule and Other Revisions to Part B (for CY 2010). CMS Web site. Available at: www.federalregister.gov/OFR Upload/OFRData/2009-26502_PI.pdf. Accessed Nov. 10, 2009.
Submission Support
Physicians receive requests for documentation on a daily basis. Insurer requests need particular attention, as they can be directly related to reimbursement. If the documentation supports the service, payment is rendered (pre-payment request) or maintained (post-payment request). If the documentation is not supportive, payment is denied (pre-payment request) or refunded (post-payment request).
The two most common reasons submitted documentation is not supportive: It lacks information or only a portion of the documentation was submitted.
Not Enough Documentation
“Insufficient documentation” can take many forms. Each visit category (e.g., initial hospital care or subsequent hospital care) and level of service (e.g., 99221-99233) has corresponding documentation requirements. A full list of requirements is available on the Centers for Medicare and Medicaid Services Web site (www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf). Selecting an evaluation and management (E/M) level is focused on either upon the content of three key components: history, exam, and decision-making; time can also be a consideration but only when counseling or coordination of care dominate more than 50% of the physician’s total visit time.1 Failure to document any essential element in a given visit level (e.g., family history required but missing for 99222 and 99223) might result in a reviewer down-coding or denying the service.
Dates and signatures are vital to each encounter. The reviewer must be able to identify each individual who performs, documents, and bills for a service, as well as when the service occurred. Notes that lack dates or signatures are not considered in support of a billed service. Notes that contain an illegible signature are equally problematic. If the legibility of a signature prevents the reviewer from correctly identifying the rendering physician, the service can be denied.
It is advisable for the physician to print their name alongside the signature on the encounter note, or include a separate signature sheet with the requested documentation to assist the reviewer in deciphering the physician’s scrawl. Keep in mind that stamped signatures are not acceptable. Medicare accepts handwritten signatures, electronic signatures, or facsimiles of original written or electronic signatures.2
A service is questioned when two different sets of handwriting appear on a note and only one signature is provided. Because the reviewer cannot confirm the credentials of the unidentified individual and cannot be sure which portion belongs to the identified individual, the entire note is disregarded.
Incomplete Submission
Many times, an encounter note does not contain the cumulative information representing the reported service. For example, other pieces of pertinent information might be included in the data section or order section of the chart. If the individual responsible for gathering the requested documentation does not review the information before submitting it, those other important entries could be missed, and the complexity of the billed service might not be justified.
To avoid this, have the designated individual review the note for specific references to information housed in different areas of the chart. The provider should submit any entry with the same date as the requested documentation: labs, diagnostic testing, physician orders, patient instructions, nursing notes, resident notes, notes by other physicians in the same group, discharge summaries, etc.
Legibility is crucial when the documentation is sent for review. Note that the reviewer will not contact the provider if the information is not readable. Most reviewers seek another reviewer’s assistance in translating the handwriting, but they are not obligated to do this. If the note is deemed incomprehensible, the service is denied.
Electronic health records (EHR) are assisting physicians and other providers with legibility issues, and can help take the guesswork out of the note’s content. If a physician is still writing notes by hand, a transcription could be sent along with the documentation to prevent unnecessary denials. It is not advisable to do this for all requests, but only for requests involving providers who have particularly problematic handwriting.
Timeliness of Response
Once the documentation request is received, the physician has a small window of opportunity to review the request, collect the information, and issue a response. A lack of physician response always results in a service denial or a refund request. Once denied, the physician must go through the proper channels of appeal (with a different insurer reviewing department). Requests for refunds are more difficult to overturn. It is difficult to “open” a case that has been “closed.” Denials resulting from a failure to respond to a pre-payment request are a bit easier to resolve because the resulting denial is typically the payor’s initial determination of the claim. The physician usually is allowed an appeal of the payor’s initial determination. However, it is not a cost-effective process to handle prepayment requests in this manner. Always attempt to respond to the initial request within the designated time frame. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians, 2008;79-109.
- Centers for Medicare and Medicaid Services: CR 5971 Clarification-Signature Requirements. Medicare Learning Network Web site. Available at: www.cms.hhs.gov/MLNMattersArticles/downloads/SE0829.pdf. Accessed Sept. 1, 2009.
- Pohlig C. Evaluation and Management Services: An Overview. In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians, 2008; 65-78.
Physicians receive requests for documentation on a daily basis. Insurer requests need particular attention, as they can be directly related to reimbursement. If the documentation supports the service, payment is rendered (pre-payment request) or maintained (post-payment request). If the documentation is not supportive, payment is denied (pre-payment request) or refunded (post-payment request).
The two most common reasons submitted documentation is not supportive: It lacks information or only a portion of the documentation was submitted.
Not Enough Documentation
“Insufficient documentation” can take many forms. Each visit category (e.g., initial hospital care or subsequent hospital care) and level of service (e.g., 99221-99233) has corresponding documentation requirements. A full list of requirements is available on the Centers for Medicare and Medicaid Services Web site (www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf). Selecting an evaluation and management (E/M) level is focused on either upon the content of three key components: history, exam, and decision-making; time can also be a consideration but only when counseling or coordination of care dominate more than 50% of the physician’s total visit time.1 Failure to document any essential element in a given visit level (e.g., family history required but missing for 99222 and 99223) might result in a reviewer down-coding or denying the service.
Dates and signatures are vital to each encounter. The reviewer must be able to identify each individual who performs, documents, and bills for a service, as well as when the service occurred. Notes that lack dates or signatures are not considered in support of a billed service. Notes that contain an illegible signature are equally problematic. If the legibility of a signature prevents the reviewer from correctly identifying the rendering physician, the service can be denied.
It is advisable for the physician to print their name alongside the signature on the encounter note, or include a separate signature sheet with the requested documentation to assist the reviewer in deciphering the physician’s scrawl. Keep in mind that stamped signatures are not acceptable. Medicare accepts handwritten signatures, electronic signatures, or facsimiles of original written or electronic signatures.2
A service is questioned when two different sets of handwriting appear on a note and only one signature is provided. Because the reviewer cannot confirm the credentials of the unidentified individual and cannot be sure which portion belongs to the identified individual, the entire note is disregarded.
Incomplete Submission
Many times, an encounter note does not contain the cumulative information representing the reported service. For example, other pieces of pertinent information might be included in the data section or order section of the chart. If the individual responsible for gathering the requested documentation does not review the information before submitting it, those other important entries could be missed, and the complexity of the billed service might not be justified.
To avoid this, have the designated individual review the note for specific references to information housed in different areas of the chart. The provider should submit any entry with the same date as the requested documentation: labs, diagnostic testing, physician orders, patient instructions, nursing notes, resident notes, notes by other physicians in the same group, discharge summaries, etc.
Legibility is crucial when the documentation is sent for review. Note that the reviewer will not contact the provider if the information is not readable. Most reviewers seek another reviewer’s assistance in translating the handwriting, but they are not obligated to do this. If the note is deemed incomprehensible, the service is denied.
Electronic health records (EHR) are assisting physicians and other providers with legibility issues, and can help take the guesswork out of the note’s content. If a physician is still writing notes by hand, a transcription could be sent along with the documentation to prevent unnecessary denials. It is not advisable to do this for all requests, but only for requests involving providers who have particularly problematic handwriting.
Timeliness of Response
Once the documentation request is received, the physician has a small window of opportunity to review the request, collect the information, and issue a response. A lack of physician response always results in a service denial or a refund request. Once denied, the physician must go through the proper channels of appeal (with a different insurer reviewing department). Requests for refunds are more difficult to overturn. It is difficult to “open” a case that has been “closed.” Denials resulting from a failure to respond to a pre-payment request are a bit easier to resolve because the resulting denial is typically the payor’s initial determination of the claim. The physician usually is allowed an appeal of the payor’s initial determination. However, it is not a cost-effective process to handle prepayment requests in this manner. Always attempt to respond to the initial request within the designated time frame. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians, 2008;79-109.
- Centers for Medicare and Medicaid Services: CR 5971 Clarification-Signature Requirements. Medicare Learning Network Web site. Available at: www.cms.hhs.gov/MLNMattersArticles/downloads/SE0829.pdf. Accessed Sept. 1, 2009.
- Pohlig C. Evaluation and Management Services: An Overview. In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians, 2008; 65-78.
Physicians receive requests for documentation on a daily basis. Insurer requests need particular attention, as they can be directly related to reimbursement. If the documentation supports the service, payment is rendered (pre-payment request) or maintained (post-payment request). If the documentation is not supportive, payment is denied (pre-payment request) or refunded (post-payment request).
The two most common reasons submitted documentation is not supportive: It lacks information or only a portion of the documentation was submitted.
Not Enough Documentation
“Insufficient documentation” can take many forms. Each visit category (e.g., initial hospital care or subsequent hospital care) and level of service (e.g., 99221-99233) has corresponding documentation requirements. A full list of requirements is available on the Centers for Medicare and Medicaid Services Web site (www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf). Selecting an evaluation and management (E/M) level is focused on either upon the content of three key components: history, exam, and decision-making; time can also be a consideration but only when counseling or coordination of care dominate more than 50% of the physician’s total visit time.1 Failure to document any essential element in a given visit level (e.g., family history required but missing for 99222 and 99223) might result in a reviewer down-coding or denying the service.
Dates and signatures are vital to each encounter. The reviewer must be able to identify each individual who performs, documents, and bills for a service, as well as when the service occurred. Notes that lack dates or signatures are not considered in support of a billed service. Notes that contain an illegible signature are equally problematic. If the legibility of a signature prevents the reviewer from correctly identifying the rendering physician, the service can be denied.
It is advisable for the physician to print their name alongside the signature on the encounter note, or include a separate signature sheet with the requested documentation to assist the reviewer in deciphering the physician’s scrawl. Keep in mind that stamped signatures are not acceptable. Medicare accepts handwritten signatures, electronic signatures, or facsimiles of original written or electronic signatures.2
A service is questioned when two different sets of handwriting appear on a note and only one signature is provided. Because the reviewer cannot confirm the credentials of the unidentified individual and cannot be sure which portion belongs to the identified individual, the entire note is disregarded.
Incomplete Submission
Many times, an encounter note does not contain the cumulative information representing the reported service. For example, other pieces of pertinent information might be included in the data section or order section of the chart. If the individual responsible for gathering the requested documentation does not review the information before submitting it, those other important entries could be missed, and the complexity of the billed service might not be justified.
To avoid this, have the designated individual review the note for specific references to information housed in different areas of the chart. The provider should submit any entry with the same date as the requested documentation: labs, diagnostic testing, physician orders, patient instructions, nursing notes, resident notes, notes by other physicians in the same group, discharge summaries, etc.
Legibility is crucial when the documentation is sent for review. Note that the reviewer will not contact the provider if the information is not readable. Most reviewers seek another reviewer’s assistance in translating the handwriting, but they are not obligated to do this. If the note is deemed incomprehensible, the service is denied.
Electronic health records (EHR) are assisting physicians and other providers with legibility issues, and can help take the guesswork out of the note’s content. If a physician is still writing notes by hand, a transcription could be sent along with the documentation to prevent unnecessary denials. It is not advisable to do this for all requests, but only for requests involving providers who have particularly problematic handwriting.
Timeliness of Response
Once the documentation request is received, the physician has a small window of opportunity to review the request, collect the information, and issue a response. A lack of physician response always results in a service denial or a refund request. Once denied, the physician must go through the proper channels of appeal (with a different insurer reviewing department). Requests for refunds are more difficult to overturn. It is difficult to “open” a case that has been “closed.” Denials resulting from a failure to respond to a pre-payment request are a bit easier to resolve because the resulting denial is typically the payor’s initial determination of the claim. The physician usually is allowed an appeal of the payor’s initial determination. However, it is not a cost-effective process to handle prepayment requests in this manner. Always attempt to respond to the initial request within the designated time frame. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians, 2008;79-109.
- Centers for Medicare and Medicaid Services: CR 5971 Clarification-Signature Requirements. Medicare Learning Network Web site. Available at: www.cms.hhs.gov/MLNMattersArticles/downloads/SE0829.pdf. Accessed Sept. 1, 2009.
- Pohlig C. Evaluation and Management Services: An Overview. In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians, 2008; 65-78.
Document Inspection
One constant in all the modifications to billing and reimbursement guidelines for evaluation and management (E/M) services provided by hospitalists is that a face-to-face patient encounter by the billing provider is required. Exceptions do occur (e.g., telehealth services, care plan oversight, home health certification) but are infrequently reported by hospitalist teams. Do not get caught misreporting the following services due to the absence of a physician presence.
Discharge Day Management
Hospital discharge day management (CPT 99238-99239) is a face-to-face E/M service between the attending physician and the patient. Document the date of the actual physician visit even if the patient is discharged from the facility on a different date.1 Documentation must substantiate this personal patient encounter.
A hospitalist can choose to record the face-to-face encounter in a handwritten progress note or make note of it in the formal discharge summary. When relying solely upon the dictated summary, physicians often fail to identify personal contact with the patient. Although an examination need only be performed “as appropriate” on the day of discharge, it is the best indicator of a face-to-face encounter. Such statements as “Upon discharge, the patient appeared well, vital signs stable, lungs clear” or “Patient seen and examined by me on discharge day” clearly illustrate this service.
It is important to note that only the attending physician of record reports the discharge day management service. Physicians or qualified non-physician practitioners (NPPs), other than the attending physician, who have been managing concurrent healthcare problems not primarily managed by the attending physician and who are not acting on behalf of the attending physician should use subsequent hospital care codes (99231-99233) for a final visit.2
Death pronouncement can be reported with discharge day management codes (99238-99239), but only when this service involves a physician-patient encounter. Physicians should report the most appropriate discharge code on the actual day of pronouncement.
Shared/Split Services
Shared/split Medicare services occur when two providers from the same specialty and group practice perform a portion of a facility-based (outpatient hospital, inpatient hospital, or ED) patient encounter on the same day. One provider must be a physician; the other must be a qualified and certified NPP (e.g., nurse practitioner, physician assistant, clinical nurse specialist, certified nurse midwife).
The culmination of the two portions of service must fulfill the requirements of a single E/M service (consultations, critical care, and other time-based services excluded). The physician has the option to report the shared/split service to Medicare under their name for 100% of the allowable reimbursement rate, or under the NPP’s name for 85% of the allowable reimbursement rate.
In order to utilize this billing model, the physician and the NPP must provide a face-to-face encounter on the same day. If there is no face-to-face encounter between the patient and the physician, then the service can only be billed under the NPP’s name at 85% of the allowable reimbursement rate.3
Documentation must clearly identify each provider involved in the shared/split service, along with the presence and the portion of each individual’s service. The NPP and the physician should each indicate the extent of their involvement (e.g., “Patient seen and examined by me … ”) in the patient’s care and sign their portion of the note. If the NPP and physician each write a separate note, each note should refer to the other provider. That way, the supporting documentation for the service rendered encompasses the summation of both notes.4
Teaching Physician Services
A different type of shared service can occur under the teaching physician rules, whereby an attending physician and a “resident” are involved in the same patient encounter. The term “resident” also includes interns and fellows in recognized graduate medical education (GME) programs, as approved for purposes of direct GME payments made by the fiscal intermediary.5 As with services shared with NPPs, the attending physician must provide a face-to-face encounter and participate in a key portion of the service.
The attending physician can perform their portion of the service concurrently or independent of the resident but is allowed to discuss the case (teaching service) with the resident, as appropriate. If the attending physician does not physically see the patient, the service cannot be reported. Payment is made only for the teaching physician’s involvement in the patient’s care.
Instead of detailing the entire encounter, the teaching physician should write a short, legible linking or tethering statement specifically referencing the resident’s note. Physicians must demonstrate their physical presence (e.g., “Patient seen and examined by me. Agree with note by Dr. Jones”) and comment on the patient’s evaluation and their active involvement in the care plan.6 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare and Medicaid Services (CMS) Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.2B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians, 2008;265-271.
- Medicare Claims Processing Manual: Chapter 12, Section 100. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Manaker, S. Teaching Physician Regulations. In: Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians, 2008;299-305.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1D. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
One constant in all the modifications to billing and reimbursement guidelines for evaluation and management (E/M) services provided by hospitalists is that a face-to-face patient encounter by the billing provider is required. Exceptions do occur (e.g., telehealth services, care plan oversight, home health certification) but are infrequently reported by hospitalist teams. Do not get caught misreporting the following services due to the absence of a physician presence.
Discharge Day Management
Hospital discharge day management (CPT 99238-99239) is a face-to-face E/M service between the attending physician and the patient. Document the date of the actual physician visit even if the patient is discharged from the facility on a different date.1 Documentation must substantiate this personal patient encounter.
A hospitalist can choose to record the face-to-face encounter in a handwritten progress note or make note of it in the formal discharge summary. When relying solely upon the dictated summary, physicians often fail to identify personal contact with the patient. Although an examination need only be performed “as appropriate” on the day of discharge, it is the best indicator of a face-to-face encounter. Such statements as “Upon discharge, the patient appeared well, vital signs stable, lungs clear” or “Patient seen and examined by me on discharge day” clearly illustrate this service.
It is important to note that only the attending physician of record reports the discharge day management service. Physicians or qualified non-physician practitioners (NPPs), other than the attending physician, who have been managing concurrent healthcare problems not primarily managed by the attending physician and who are not acting on behalf of the attending physician should use subsequent hospital care codes (99231-99233) for a final visit.2
Death pronouncement can be reported with discharge day management codes (99238-99239), but only when this service involves a physician-patient encounter. Physicians should report the most appropriate discharge code on the actual day of pronouncement.
Shared/Split Services
Shared/split Medicare services occur when two providers from the same specialty and group practice perform a portion of a facility-based (outpatient hospital, inpatient hospital, or ED) patient encounter on the same day. One provider must be a physician; the other must be a qualified and certified NPP (e.g., nurse practitioner, physician assistant, clinical nurse specialist, certified nurse midwife).
The culmination of the two portions of service must fulfill the requirements of a single E/M service (consultations, critical care, and other time-based services excluded). The physician has the option to report the shared/split service to Medicare under their name for 100% of the allowable reimbursement rate, or under the NPP’s name for 85% of the allowable reimbursement rate.
In order to utilize this billing model, the physician and the NPP must provide a face-to-face encounter on the same day. If there is no face-to-face encounter between the patient and the physician, then the service can only be billed under the NPP’s name at 85% of the allowable reimbursement rate.3
Documentation must clearly identify each provider involved in the shared/split service, along with the presence and the portion of each individual’s service. The NPP and the physician should each indicate the extent of their involvement (e.g., “Patient seen and examined by me … ”) in the patient’s care and sign their portion of the note. If the NPP and physician each write a separate note, each note should refer to the other provider. That way, the supporting documentation for the service rendered encompasses the summation of both notes.4
Teaching Physician Services
A different type of shared service can occur under the teaching physician rules, whereby an attending physician and a “resident” are involved in the same patient encounter. The term “resident” also includes interns and fellows in recognized graduate medical education (GME) programs, as approved for purposes of direct GME payments made by the fiscal intermediary.5 As with services shared with NPPs, the attending physician must provide a face-to-face encounter and participate in a key portion of the service.
The attending physician can perform their portion of the service concurrently or independent of the resident but is allowed to discuss the case (teaching service) with the resident, as appropriate. If the attending physician does not physically see the patient, the service cannot be reported. Payment is made only for the teaching physician’s involvement in the patient’s care.
Instead of detailing the entire encounter, the teaching physician should write a short, legible linking or tethering statement specifically referencing the resident’s note. Physicians must demonstrate their physical presence (e.g., “Patient seen and examined by me. Agree with note by Dr. Jones”) and comment on the patient’s evaluation and their active involvement in the care plan.6 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare and Medicaid Services (CMS) Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.2B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians, 2008;265-271.
- Medicare Claims Processing Manual: Chapter 12, Section 100. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Manaker, S. Teaching Physician Regulations. In: Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians, 2008;299-305.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1D. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
One constant in all the modifications to billing and reimbursement guidelines for evaluation and management (E/M) services provided by hospitalists is that a face-to-face patient encounter by the billing provider is required. Exceptions do occur (e.g., telehealth services, care plan oversight, home health certification) but are infrequently reported by hospitalist teams. Do not get caught misreporting the following services due to the absence of a physician presence.
Discharge Day Management
Hospital discharge day management (CPT 99238-99239) is a face-to-face E/M service between the attending physician and the patient. Document the date of the actual physician visit even if the patient is discharged from the facility on a different date.1 Documentation must substantiate this personal patient encounter.
A hospitalist can choose to record the face-to-face encounter in a handwritten progress note or make note of it in the formal discharge summary. When relying solely upon the dictated summary, physicians often fail to identify personal contact with the patient. Although an examination need only be performed “as appropriate” on the day of discharge, it is the best indicator of a face-to-face encounter. Such statements as “Upon discharge, the patient appeared well, vital signs stable, lungs clear” or “Patient seen and examined by me on discharge day” clearly illustrate this service.
It is important to note that only the attending physician of record reports the discharge day management service. Physicians or qualified non-physician practitioners (NPPs), other than the attending physician, who have been managing concurrent healthcare problems not primarily managed by the attending physician and who are not acting on behalf of the attending physician should use subsequent hospital care codes (99231-99233) for a final visit.2
Death pronouncement can be reported with discharge day management codes (99238-99239), but only when this service involves a physician-patient encounter. Physicians should report the most appropriate discharge code on the actual day of pronouncement.
Shared/Split Services
Shared/split Medicare services occur when two providers from the same specialty and group practice perform a portion of a facility-based (outpatient hospital, inpatient hospital, or ED) patient encounter on the same day. One provider must be a physician; the other must be a qualified and certified NPP (e.g., nurse practitioner, physician assistant, clinical nurse specialist, certified nurse midwife).
The culmination of the two portions of service must fulfill the requirements of a single E/M service (consultations, critical care, and other time-based services excluded). The physician has the option to report the shared/split service to Medicare under their name for 100% of the allowable reimbursement rate, or under the NPP’s name for 85% of the allowable reimbursement rate.
In order to utilize this billing model, the physician and the NPP must provide a face-to-face encounter on the same day. If there is no face-to-face encounter between the patient and the physician, then the service can only be billed under the NPP’s name at 85% of the allowable reimbursement rate.3
Documentation must clearly identify each provider involved in the shared/split service, along with the presence and the portion of each individual’s service. The NPP and the physician should each indicate the extent of their involvement (e.g., “Patient seen and examined by me … ”) in the patient’s care and sign their portion of the note. If the NPP and physician each write a separate note, each note should refer to the other provider. That way, the supporting documentation for the service rendered encompasses the summation of both notes.4
Teaching Physician Services
A different type of shared service can occur under the teaching physician rules, whereby an attending physician and a “resident” are involved in the same patient encounter. The term “resident” also includes interns and fellows in recognized graduate medical education (GME) programs, as approved for purposes of direct GME payments made by the fiscal intermediary.5 As with services shared with NPPs, the attending physician must provide a face-to-face encounter and participate in a key portion of the service.
The attending physician can perform their portion of the service concurrently or independent of the resident but is allowed to discuss the case (teaching service) with the resident, as appropriate. If the attending physician does not physically see the patient, the service cannot be reported. Payment is made only for the teaching physician’s involvement in the patient’s care.
Instead of detailing the entire encounter, the teaching physician should write a short, legible linking or tethering statement specifically referencing the resident’s note. Physicians must demonstrate their physical presence (e.g., “Patient seen and examined by me. Agree with note by Dr. Jones”) and comment on the patient’s evaluation and their active involvement in the care plan.6 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare and Medicaid Services (CMS) Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.2B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians, 2008;265-271.
- Medicare Claims Processing Manual: Chapter 12, Section 100. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Manaker, S. Teaching Physician Regulations. In: Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians, 2008;299-305.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1D. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12. pdf. Accessed July 5, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
Revenue Essentials
As physicians take on more extensive roles outside of patient care (e.g., administrative, academic, and billing compliance), involvement in the revenue cycle might diminish or even fail to commence. It is crucial for physicians to keep abreast of revenue cycle issues, but more often than not, they go unnoticed until a physician’s bottom line is affected.
The risk of inappropriately billed claims and corresponding reimbursement is increased until the problem is identified and resolved. In an effort to prevent this from occurring, physicians should get involved with or oversee their billing service or staff. Some of the revenue cycle essentials that require physician attention are:1
- Periodic reports of claims billed on the physician’s behalf and data regarding payments;
- Changes in procedure codes, diagnosis codes, or other information furnished by the physician without the physician’s knowledge and consent; and
- Information received from Medicare and other payors.
Feedback
One of the most common billing-related physician complaints involves the lack of feedback. Most physicians want to receive information regarding their quarterly billings: the volume and frequency of specific reported services, and corresponding payments or denials. Physicians prefer to know how they rank as individuals and as a group. Although they might not be experts in coding and documentation, this information offers physicians a feeling of security, as it permits them to identify typical billing patterns or highlight outlier patterns.
Establish communication with the manager/coder/biller to better assist with feedback. Appoint a physician leader to spearhead this effort; ensure feedback is provided quarterly, at a minimum. If the coders/billers feel that they have an approachable contact, they’re more likely to offer feedback before formal reports are generated. A quick resolution of potential problems lessens the financial burden on the HM group, as well as the resource-intensive education process that ensues.
Discrepancy Notation
Physicians should be notified whenever coding changes take place. Discrepancies occur when the physician employs coders to select the service or diagnosis codes, and the selected codes differ from the physician-intended codes. Discrepancies also occur when billers change the original physician-selected codes to codes that are considered covered or medically necessary by the pay0r. Physicians need to instruct coders to only report codes that are supported by the documentation.
Physicians must be aware that delegating any portion of the billing to an employee or a billing company does not alleviate physicians’ personal responsibility for erroneously submitted claims or receipt of overpayments. Physicians should regularly review information submitted by the designated employee or billing service to ensure consistency with their own records, and also keep complete administrative records for the claims a billing service files on their behalf.1 Physicians also should meet with staff to resolve discrepancies and reinforce the billing education process. If biller/coder performance becomes a recurring problem, the physician should question the competency of the employee or company with whom the billing is entrusted.
Accounts Receivable
Physicians do not necessarily recognize the need for involvement in the accounts receivable (A/R) component of the revenue cycle. Physicians should be aware of denials, and the reasons for the denials. Some services are denied because of issues that can be easily corrected (e.g., truncated diagnoses, two physicians of the same specialty billing on the same date, missing modifiers). These denial types might require physician assistance in changing the codes originally submitted. If the denied services can be corrected with the appropriate information and resubmitted electronically, payment might be recovered quickly. Other types of denials require submission of the documentation to support the service billed.
Billers should know the difference between the types of denials and the required action for each denial type. Physicians should feel confident that such denials will be handled in the correct manner. Be mindful of billing staff that accepts denials and surrenders the reimbursement efforts without hesitation. As a physician, do not default to the idea that “no news is good news.” Do not assume the billing manager (physician employee or outsourced firm) will let the group know if there is a problem. Develop a standard that requires monthly feedback of denials.
Only a short window of time exists for the appeals process to occur. Do not lose the potential to recover monies because the information was not provided to the physician in a timely manner. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Protecting Your Practice. CMS Web site. Available at: www.cms.hhs.gov/MLNProducts/downloads/Protectingpracbroch508-09.pdf. Accessed Aug. 2, 2009.
- Office of Inspector General. Work Plan Health Care Financing Administration Projects Fiscal Year 1999. Physicians: Billing Service Companies. Available at: http://oig.hhs.gov/publications/docs/workplan/1999/99hcfawp.pdf. Accessed Aug. 2, 2009.
- Office of Inspector General. OIG Compliance Program Guidance for Third-Party Medical Billing Companies in Federal Register, December 1998, Vol. 63; pages 70138-70152. Available at: http://oig.hhs.gov/fraud/docs/complianceguidance/thirdparty.pdf. Accessed Aug. 2, 2009.
As physicians take on more extensive roles outside of patient care (e.g., administrative, academic, and billing compliance), involvement in the revenue cycle might diminish or even fail to commence. It is crucial for physicians to keep abreast of revenue cycle issues, but more often than not, they go unnoticed until a physician’s bottom line is affected.
The risk of inappropriately billed claims and corresponding reimbursement is increased until the problem is identified and resolved. In an effort to prevent this from occurring, physicians should get involved with or oversee their billing service or staff. Some of the revenue cycle essentials that require physician attention are:1
- Periodic reports of claims billed on the physician’s behalf and data regarding payments;
- Changes in procedure codes, diagnosis codes, or other information furnished by the physician without the physician’s knowledge and consent; and
- Information received from Medicare and other payors.
Feedback
One of the most common billing-related physician complaints involves the lack of feedback. Most physicians want to receive information regarding their quarterly billings: the volume and frequency of specific reported services, and corresponding payments or denials. Physicians prefer to know how they rank as individuals and as a group. Although they might not be experts in coding and documentation, this information offers physicians a feeling of security, as it permits them to identify typical billing patterns or highlight outlier patterns.
Establish communication with the manager/coder/biller to better assist with feedback. Appoint a physician leader to spearhead this effort; ensure feedback is provided quarterly, at a minimum. If the coders/billers feel that they have an approachable contact, they’re more likely to offer feedback before formal reports are generated. A quick resolution of potential problems lessens the financial burden on the HM group, as well as the resource-intensive education process that ensues.
Discrepancy Notation
Physicians should be notified whenever coding changes take place. Discrepancies occur when the physician employs coders to select the service or diagnosis codes, and the selected codes differ from the physician-intended codes. Discrepancies also occur when billers change the original physician-selected codes to codes that are considered covered or medically necessary by the pay0r. Physicians need to instruct coders to only report codes that are supported by the documentation.
Physicians must be aware that delegating any portion of the billing to an employee or a billing company does not alleviate physicians’ personal responsibility for erroneously submitted claims or receipt of overpayments. Physicians should regularly review information submitted by the designated employee or billing service to ensure consistency with their own records, and also keep complete administrative records for the claims a billing service files on their behalf.1 Physicians also should meet with staff to resolve discrepancies and reinforce the billing education process. If biller/coder performance becomes a recurring problem, the physician should question the competency of the employee or company with whom the billing is entrusted.
Accounts Receivable
Physicians do not necessarily recognize the need for involvement in the accounts receivable (A/R) component of the revenue cycle. Physicians should be aware of denials, and the reasons for the denials. Some services are denied because of issues that can be easily corrected (e.g., truncated diagnoses, two physicians of the same specialty billing on the same date, missing modifiers). These denial types might require physician assistance in changing the codes originally submitted. If the denied services can be corrected with the appropriate information and resubmitted electronically, payment might be recovered quickly. Other types of denials require submission of the documentation to support the service billed.
Billers should know the difference between the types of denials and the required action for each denial type. Physicians should feel confident that such denials will be handled in the correct manner. Be mindful of billing staff that accepts denials and surrenders the reimbursement efforts without hesitation. As a physician, do not default to the idea that “no news is good news.” Do not assume the billing manager (physician employee or outsourced firm) will let the group know if there is a problem. Develop a standard that requires monthly feedback of denials.
Only a short window of time exists for the appeals process to occur. Do not lose the potential to recover monies because the information was not provided to the physician in a timely manner. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Protecting Your Practice. CMS Web site. Available at: www.cms.hhs.gov/MLNProducts/downloads/Protectingpracbroch508-09.pdf. Accessed Aug. 2, 2009.
- Office of Inspector General. Work Plan Health Care Financing Administration Projects Fiscal Year 1999. Physicians: Billing Service Companies. Available at: http://oig.hhs.gov/publications/docs/workplan/1999/99hcfawp.pdf. Accessed Aug. 2, 2009.
- Office of Inspector General. OIG Compliance Program Guidance for Third-Party Medical Billing Companies in Federal Register, December 1998, Vol. 63; pages 70138-70152. Available at: http://oig.hhs.gov/fraud/docs/complianceguidance/thirdparty.pdf. Accessed Aug. 2, 2009.
As physicians take on more extensive roles outside of patient care (e.g., administrative, academic, and billing compliance), involvement in the revenue cycle might diminish or even fail to commence. It is crucial for physicians to keep abreast of revenue cycle issues, but more often than not, they go unnoticed until a physician’s bottom line is affected.
The risk of inappropriately billed claims and corresponding reimbursement is increased until the problem is identified and resolved. In an effort to prevent this from occurring, physicians should get involved with or oversee their billing service or staff. Some of the revenue cycle essentials that require physician attention are:1
- Periodic reports of claims billed on the physician’s behalf and data regarding payments;
- Changes in procedure codes, diagnosis codes, or other information furnished by the physician without the physician’s knowledge and consent; and
- Information received from Medicare and other payors.
Feedback
One of the most common billing-related physician complaints involves the lack of feedback. Most physicians want to receive information regarding their quarterly billings: the volume and frequency of specific reported services, and corresponding payments or denials. Physicians prefer to know how they rank as individuals and as a group. Although they might not be experts in coding and documentation, this information offers physicians a feeling of security, as it permits them to identify typical billing patterns or highlight outlier patterns.
Establish communication with the manager/coder/biller to better assist with feedback. Appoint a physician leader to spearhead this effort; ensure feedback is provided quarterly, at a minimum. If the coders/billers feel that they have an approachable contact, they’re more likely to offer feedback before formal reports are generated. A quick resolution of potential problems lessens the financial burden on the HM group, as well as the resource-intensive education process that ensues.
Discrepancy Notation
Physicians should be notified whenever coding changes take place. Discrepancies occur when the physician employs coders to select the service or diagnosis codes, and the selected codes differ from the physician-intended codes. Discrepancies also occur when billers change the original physician-selected codes to codes that are considered covered or medically necessary by the pay0r. Physicians need to instruct coders to only report codes that are supported by the documentation.
Physicians must be aware that delegating any portion of the billing to an employee or a billing company does not alleviate physicians’ personal responsibility for erroneously submitted claims or receipt of overpayments. Physicians should regularly review information submitted by the designated employee or billing service to ensure consistency with their own records, and also keep complete administrative records for the claims a billing service files on their behalf.1 Physicians also should meet with staff to resolve discrepancies and reinforce the billing education process. If biller/coder performance becomes a recurring problem, the physician should question the competency of the employee or company with whom the billing is entrusted.
Accounts Receivable
Physicians do not necessarily recognize the need for involvement in the accounts receivable (A/R) component of the revenue cycle. Physicians should be aware of denials, and the reasons for the denials. Some services are denied because of issues that can be easily corrected (e.g., truncated diagnoses, two physicians of the same specialty billing on the same date, missing modifiers). These denial types might require physician assistance in changing the codes originally submitted. If the denied services can be corrected with the appropriate information and resubmitted electronically, payment might be recovered quickly. Other types of denials require submission of the documentation to support the service billed.
Billers should know the difference between the types of denials and the required action for each denial type. Physicians should feel confident that such denials will be handled in the correct manner. Be mindful of billing staff that accepts denials and surrenders the reimbursement efforts without hesitation. As a physician, do not default to the idea that “no news is good news.” Do not assume the billing manager (physician employee or outsourced firm) will let the group know if there is a problem. Develop a standard that requires monthly feedback of denials.
Only a short window of time exists for the appeals process to occur. Do not lose the potential to recover monies because the information was not provided to the physician in a timely manner. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Protecting Your Practice. CMS Web site. Available at: www.cms.hhs.gov/MLNProducts/downloads/Protectingpracbroch508-09.pdf. Accessed Aug. 2, 2009.
- Office of Inspector General. Work Plan Health Care Financing Administration Projects Fiscal Year 1999. Physicians: Billing Service Companies. Available at: http://oig.hhs.gov/publications/docs/workplan/1999/99hcfawp.pdf. Accessed Aug. 2, 2009.
- Office of Inspector General. OIG Compliance Program Guidance for Third-Party Medical Billing Companies in Federal Register, December 1998, Vol. 63; pages 70138-70152. Available at: http://oig.hhs.gov/fraud/docs/complianceguidance/thirdparty.pdf. Accessed Aug. 2, 2009.
Facility Transfers
Patient care provided in the acute setting might not always end with discharge to the patient’s home. Frequently, a hospitalist will transfer the patient to a different unit in the hospital or an off-site facility to receive additional services before returning to their home. When the patient’s condition requires a transfer to a physical medicine and rehabilitation (PM&R) unit, a psychiatric unit, a long-term acute-care facility, or a skilled nursing facility, it is important for the hospitalist to identify their role, if any, in the new area of care. Physician billing will depend on several factors:
- A shared medical record;
- The attending of record in each setting; and
- The care rendered by the hospitalist in each setting.
Intrafacility
A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for a 68-year-old male with hypertension and diabetes who sustained a hip fracture. The care plan includes post-discharge therapy and rehabilitation. When the hospitalist transfers care to a PM&R unit within the same facility for which the hospitalist is no longer the attending of record, they might be asked to provide ongoing care for the patient’s medical conditions (e.g., diabetes and hypertension). The hospitalist’s knee-jerk reaction is to bill for an inpatient consultation for the initial service provided in the transferred setting. This would only be appropriate if the request for opinion or advice involved an unrelated, new condition, and the requesting physician’s intent is for opinion or advice on how to manage the patient and not the a priori intent for the hospitalist to assume the patient’s medical care.
If consultation requirements are met (see “Consulataion Reminder,” p. 20), the hospitalist can report an inpatient consultation code (99251-99255). However, when circumstances do not fully represent the intent or need for consultative services but rather a continuity of the medical care provided during the acute phase of the hospitalization, report the most appropriate subsequent hospital care code (99231-99233) for the initial rehab visit and all follow-up services.
On occasion, the hospitalist will be asked to perform and provide the history and physical (H&P) for the patient’s “sub-acute” phase of care, even though the hospitalist is not the attending of record. This usually happens when the attending of record cannot complete the medical requirements of the H&P, either at all or as comprehensively as the hospitalist. When this occurs, the hospitalist should not report an initial hospital care code (99221-99223) because they are not the attending of record—the physician who admits the patient and is responsible for the patient’s stay in the transferred location.
Additionally, a consultation service (99251-99255) should not be reported, because the request involves the completion of a facility-mandated form and not an opinion or advice on caring for the patient. If medical issues require the hospitalist’s evaluation and management, there is medical necessity for capturing the hospitalist’s participation as subsequent hospital care (99231-99233). If no medical conditions present for the hospitalist to manage, the service will not be considered “medically necessary” by the payor.
Interfacility
Hospitalist groups provide patient care and coverage in a variety of facilities. Confusion often arises when the attending of record during acute care and the sub-acute setting are different hospitalists from the same HM group. The hospitalist who receives the patient in the transfer facility may err on the side of caution and report subsequent hospital care (99231-99233) because the group has provided ongoing patient care. In this scenario, the hospitalist group might lose revenue if an admission service (99221-99223) was not reported.
Day of Transfer Billing
A single hospitalist or two hospitalists from the same group might bill both the hospital discharge management code (99238-99239) and an initial hospital care code (99221-99223) when the discharge and admission do not occur on the same day if the transfer is between:
- Different hospitals;
- Different facilities under common ownership that do not have merged records;* or
- Between the acute-care hospital and a prospective payment system (PPS)-exempt unit within the same hospital when there are no merged records.
In all other transfer circumstances that do not meet the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Of note, Medicare Part A covers inpatient care in psychiatric, rehabilitation, critical access, and long-term-care hospitals. Each of these specialty hospitals is exempt from the PPS established for acute-care hospitals in 1983.2 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
*Editor’s note: “Merged record” is not equivalent to commonly accessible charts via an electronic health record system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1E. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
- Department of Health and Human Services. Office of Inspector General: Oversight of Medicare PPS-Exempt Hospital Services. HHS Web site. Available at: www.oig.hhs.gov/oei/reports/oei-12-02-00170.pdf. Accessed June 1, 2009.
- CMS. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1H. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
Patient care provided in the acute setting might not always end with discharge to the patient’s home. Frequently, a hospitalist will transfer the patient to a different unit in the hospital or an off-site facility to receive additional services before returning to their home. When the patient’s condition requires a transfer to a physical medicine and rehabilitation (PM&R) unit, a psychiatric unit, a long-term acute-care facility, or a skilled nursing facility, it is important for the hospitalist to identify their role, if any, in the new area of care. Physician billing will depend on several factors:
- A shared medical record;
- The attending of record in each setting; and
- The care rendered by the hospitalist in each setting.
Intrafacility
A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for a 68-year-old male with hypertension and diabetes who sustained a hip fracture. The care plan includes post-discharge therapy and rehabilitation. When the hospitalist transfers care to a PM&R unit within the same facility for which the hospitalist is no longer the attending of record, they might be asked to provide ongoing care for the patient’s medical conditions (e.g., diabetes and hypertension). The hospitalist’s knee-jerk reaction is to bill for an inpatient consultation for the initial service provided in the transferred setting. This would only be appropriate if the request for opinion or advice involved an unrelated, new condition, and the requesting physician’s intent is for opinion or advice on how to manage the patient and not the a priori intent for the hospitalist to assume the patient’s medical care.
If consultation requirements are met (see “Consulataion Reminder,” p. 20), the hospitalist can report an inpatient consultation code (99251-99255). However, when circumstances do not fully represent the intent or need for consultative services but rather a continuity of the medical care provided during the acute phase of the hospitalization, report the most appropriate subsequent hospital care code (99231-99233) for the initial rehab visit and all follow-up services.
On occasion, the hospitalist will be asked to perform and provide the history and physical (H&P) for the patient’s “sub-acute” phase of care, even though the hospitalist is not the attending of record. This usually happens when the attending of record cannot complete the medical requirements of the H&P, either at all or as comprehensively as the hospitalist. When this occurs, the hospitalist should not report an initial hospital care code (99221-99223) because they are not the attending of record—the physician who admits the patient and is responsible for the patient’s stay in the transferred location.
Additionally, a consultation service (99251-99255) should not be reported, because the request involves the completion of a facility-mandated form and not an opinion or advice on caring for the patient. If medical issues require the hospitalist’s evaluation and management, there is medical necessity for capturing the hospitalist’s participation as subsequent hospital care (99231-99233). If no medical conditions present for the hospitalist to manage, the service will not be considered “medically necessary” by the payor.
Interfacility
Hospitalist groups provide patient care and coverage in a variety of facilities. Confusion often arises when the attending of record during acute care and the sub-acute setting are different hospitalists from the same HM group. The hospitalist who receives the patient in the transfer facility may err on the side of caution and report subsequent hospital care (99231-99233) because the group has provided ongoing patient care. In this scenario, the hospitalist group might lose revenue if an admission service (99221-99223) was not reported.
Day of Transfer Billing
A single hospitalist or two hospitalists from the same group might bill both the hospital discharge management code (99238-99239) and an initial hospital care code (99221-99223) when the discharge and admission do not occur on the same day if the transfer is between:
- Different hospitals;
- Different facilities under common ownership that do not have merged records;* or
- Between the acute-care hospital and a prospective payment system (PPS)-exempt unit within the same hospital when there are no merged records.
In all other transfer circumstances that do not meet the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Of note, Medicare Part A covers inpatient care in psychiatric, rehabilitation, critical access, and long-term-care hospitals. Each of these specialty hospitals is exempt from the PPS established for acute-care hospitals in 1983.2 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
*Editor’s note: “Merged record” is not equivalent to commonly accessible charts via an electronic health record system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1E. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
- Department of Health and Human Services. Office of Inspector General: Oversight of Medicare PPS-Exempt Hospital Services. HHS Web site. Available at: www.oig.hhs.gov/oei/reports/oei-12-02-00170.pdf. Accessed June 1, 2009.
- CMS. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1H. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
Patient care provided in the acute setting might not always end with discharge to the patient’s home. Frequently, a hospitalist will transfer the patient to a different unit in the hospital or an off-site facility to receive additional services before returning to their home. When the patient’s condition requires a transfer to a physical medicine and rehabilitation (PM&R) unit, a psychiatric unit, a long-term acute-care facility, or a skilled nursing facility, it is important for the hospitalist to identify their role, if any, in the new area of care. Physician billing will depend on several factors:
- A shared medical record;
- The attending of record in each setting; and
- The care rendered by the hospitalist in each setting.
Intrafacility
A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for a 68-year-old male with hypertension and diabetes who sustained a hip fracture. The care plan includes post-discharge therapy and rehabilitation. When the hospitalist transfers care to a PM&R unit within the same facility for which the hospitalist is no longer the attending of record, they might be asked to provide ongoing care for the patient’s medical conditions (e.g., diabetes and hypertension). The hospitalist’s knee-jerk reaction is to bill for an inpatient consultation for the initial service provided in the transferred setting. This would only be appropriate if the request for opinion or advice involved an unrelated, new condition, and the requesting physician’s intent is for opinion or advice on how to manage the patient and not the a priori intent for the hospitalist to assume the patient’s medical care.
If consultation requirements are met (see “Consulataion Reminder,” p. 20), the hospitalist can report an inpatient consultation code (99251-99255). However, when circumstances do not fully represent the intent or need for consultative services but rather a continuity of the medical care provided during the acute phase of the hospitalization, report the most appropriate subsequent hospital care code (99231-99233) for the initial rehab visit and all follow-up services.
On occasion, the hospitalist will be asked to perform and provide the history and physical (H&P) for the patient’s “sub-acute” phase of care, even though the hospitalist is not the attending of record. This usually happens when the attending of record cannot complete the medical requirements of the H&P, either at all or as comprehensively as the hospitalist. When this occurs, the hospitalist should not report an initial hospital care code (99221-99223) because they are not the attending of record—the physician who admits the patient and is responsible for the patient’s stay in the transferred location.
Additionally, a consultation service (99251-99255) should not be reported, because the request involves the completion of a facility-mandated form and not an opinion or advice on caring for the patient. If medical issues require the hospitalist’s evaluation and management, there is medical necessity for capturing the hospitalist’s participation as subsequent hospital care (99231-99233). If no medical conditions present for the hospitalist to manage, the service will not be considered “medically necessary” by the payor.
Interfacility
Hospitalist groups provide patient care and coverage in a variety of facilities. Confusion often arises when the attending of record during acute care and the sub-acute setting are different hospitalists from the same HM group. The hospitalist who receives the patient in the transfer facility may err on the side of caution and report subsequent hospital care (99231-99233) because the group has provided ongoing patient care. In this scenario, the hospitalist group might lose revenue if an admission service (99221-99223) was not reported.
Day of Transfer Billing
A single hospitalist or two hospitalists from the same group might bill both the hospital discharge management code (99238-99239) and an initial hospital care code (99221-99223) when the discharge and admission do not occur on the same day if the transfer is between:
- Different hospitals;
- Different facilities under common ownership that do not have merged records;* or
- Between the acute-care hospital and a prospective payment system (PPS)-exempt unit within the same hospital when there are no merged records.
In all other transfer circumstances that do not meet the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Of note, Medicare Part A covers inpatient care in psychiatric, rehabilitation, critical access, and long-term-care hospitals. Each of these specialty hospitals is exempt from the PPS established for acute-care hospitals in 1983.2 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
*Editor’s note: “Merged record” is not equivalent to commonly accessible charts via an electronic health record system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1E. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
- Department of Health and Human Services. Office of Inspector General: Oversight of Medicare PPS-Exempt Hospital Services. HHS Web site. Available at: www.oig.hhs.gov/oei/reports/oei-12-02-00170.pdf. Accessed June 1, 2009.
- CMS. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1H. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
Investigate Claim Denials
In order to recover the appropriate payment for services provided by hospitalists, the following must occur:
- The billing provider renders service fully, or jointly with a resident under the teaching physician guidelines or nonphysician provider under the shared/split billing rules;
- The service is completely and accurately documented in the medical record;
- The correct information is entered on the claim form that is submitted to the payor; and
- The service is determined to be a covered benefit and eligible for payment.
Claims frequently are rejected or denied. Even more frequently, the physician or billing staff does not understand the reason for the denial. The typical reaction to claim denial is twofold: “appeal with paper” and “write off.” In other words, send a copy of the physician notes to the payor and consider the claim unsuccessful and payment unable to be obtained.
Examining and understanding the payor’s initial claim determination might prompt a more successful response. Presuming the patient demographics are entered without error, the insurance information is correct, the patient is eligible for coverage, and all precertifications and authorizations were obtained, check for these other common errors.
Medical Necessity
Denials for “medical necessity” are not always what they seem. Individuals often assume that the physician reported an incorrect diagnosis code. Consider the service/procedure code when trying to formulate a response to the denial. When dealing with procedure codes, it is likely the denial is received for a mismatched diagnosis.
For example, a payor might deny a claim for cardiopulmonary resuscitation (92950) that is associated with a diagnosis code of congestive heart failure (428.0), despite this being the underlying condition that prompted the decline in the patient’s condition. The payor might only accept “cardiac arrest” (427.5) as the diagnosis for cardiopulmonary resuscitation because it was the direct reason for the procedure. After you ensure that the documentation supports the diagnosis, the claim should be resubmitted with the corrected diagnosis code.
If the “medical necessity” denial involves a covered evaluation and management (E/M) visit, it is less likely that the diagnosis code is the issue. When dealing with Medicare in particular, this type of denial likely is the result of a failure to respond to a prepayment request for documentation. Medicare issues prepayment requests for documentation for the following inpatient CPT codes: 99255, 99254, 99233, 99232, 99223, 99239, and 99292. If the documentation isn’t provided to the Medicare review department within the designated time frame, the claim is automatically denied. The reason for denial is cited as “not deemed a medical necessity.” Some providers misunderstand this remittance remark and assume that the physician assigned an incorrect diagnosis code. Although that might be true, it probably is due to a failure to respond to the prepayment documentation request. Appealing these claims requires the submission of documentation to the Medicare appeals department. Once the supporting documentation is reviewed, reimbursement is granted.
Bundling
The National Correct Coding Initiative (NCCI) identifies edits that ultimately affect claims submission and payment. The Column One/Column Two Correct Coding Edits and the Mutually Exclusive Edits list code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group. Under some well-documented circumstances, the physician is allowed to “unbundle” the services by appending the appropriate modifier.
When services are denied as being “incidental/integral” to another reimbursed service (e.g., bundled), the claim should not automatically be resubmitted with a modifier appended to the “bundled” procedure code.
Documentation should be reviewed to determine if the denied service is separately reportable from the paid service. Only when supported by documentation can the physician append the appropriate modifier and resubmit the claim. For example, a hospitalist evaluated a patient with congestive heart failure and pleural effusions. The hospitalist determined that the patient requires placement of a central venous catheter (36556). Because the patient’s underlying condition was evaluated and resulted in the decision to place a central venous catheter, both the visit (99233) and the procedure (36556) can be reported. If submitted without modifiers, some payors may deny payment for the visit because it was not “integral” to the catheter placement. You should resubmit those claims with modifier 25.
Place of Service
Ensure that the place of service (POS) matches the service/procedure code. For example, say a hospitalist performs a consultation in the ED and determines that the patient does not need to be treated as an inpatient but provides recommendations for ED care and outpatient followup. Avoid a mismatch of the service code and the location. Consults performed in the ED should be reported with outpatient consultation codes (99241-99245) as appropriate. The correct POS should be the ED, not the inpatient hospital. Reporting outpatient codes with an inpatient POS (e.g., 21: inpatient hospital, 31: skilled nursing facility) will result in claim denial.
The same is true when trying to report inpatient consultation codes (99251-99255) in an outpatient location (e.g., 23-ED). The appropriate response for this type of denial is to resubmit the claim with the correct the POS and service/procedure code. A complete list of POS codes and corresponding definitions can be found in Chapter 26, Section 10.5 of the Medicare Claims Processing Manual, available at www.cms.hhs.gov/manuals/downloads/clm104c26.pdf.
Provider Enrollment
Provider enrollment issues occur when a physician’s national provider identifier (NPI) is not properly linked to the group practice. More often than not, the group practice receives claim rejections for enrollment issues when services involve nurse practitioners or physician assistants who have not enrolled with Medicare or cannot enroll with non-Medicare payors.
For example, a nurse practitioner independently provides a subsequent hospital-care service (e.g., 99232). The claim is submitted and Medicare reimburses the service at the correct amount as a primary insurer. The remaining balance is submitted to the secondary insurer. Because the submitted claim identifies the service provider as a nonphysician provider, who likely is not enrolled with the non-Medicare payor, the claim is rejected.
If the physician group has a contractual agreement to recognize nonphysician provider services by reporting them under the collaborating physician’s name, the claim can be resubmitted in the physician’s name. In absence of such an agreement, the claim should be written off. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
Reference
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
In order to recover the appropriate payment for services provided by hospitalists, the following must occur:
- The billing provider renders service fully, or jointly with a resident under the teaching physician guidelines or nonphysician provider under the shared/split billing rules;
- The service is completely and accurately documented in the medical record;
- The correct information is entered on the claim form that is submitted to the payor; and
- The service is determined to be a covered benefit and eligible for payment.
Claims frequently are rejected or denied. Even more frequently, the physician or billing staff does not understand the reason for the denial. The typical reaction to claim denial is twofold: “appeal with paper” and “write off.” In other words, send a copy of the physician notes to the payor and consider the claim unsuccessful and payment unable to be obtained.
Examining and understanding the payor’s initial claim determination might prompt a more successful response. Presuming the patient demographics are entered without error, the insurance information is correct, the patient is eligible for coverage, and all precertifications and authorizations were obtained, check for these other common errors.
Medical Necessity
Denials for “medical necessity” are not always what they seem. Individuals often assume that the physician reported an incorrect diagnosis code. Consider the service/procedure code when trying to formulate a response to the denial. When dealing with procedure codes, it is likely the denial is received for a mismatched diagnosis.
For example, a payor might deny a claim for cardiopulmonary resuscitation (92950) that is associated with a diagnosis code of congestive heart failure (428.0), despite this being the underlying condition that prompted the decline in the patient’s condition. The payor might only accept “cardiac arrest” (427.5) as the diagnosis for cardiopulmonary resuscitation because it was the direct reason for the procedure. After you ensure that the documentation supports the diagnosis, the claim should be resubmitted with the corrected diagnosis code.
If the “medical necessity” denial involves a covered evaluation and management (E/M) visit, it is less likely that the diagnosis code is the issue. When dealing with Medicare in particular, this type of denial likely is the result of a failure to respond to a prepayment request for documentation. Medicare issues prepayment requests for documentation for the following inpatient CPT codes: 99255, 99254, 99233, 99232, 99223, 99239, and 99292. If the documentation isn’t provided to the Medicare review department within the designated time frame, the claim is automatically denied. The reason for denial is cited as “not deemed a medical necessity.” Some providers misunderstand this remittance remark and assume that the physician assigned an incorrect diagnosis code. Although that might be true, it probably is due to a failure to respond to the prepayment documentation request. Appealing these claims requires the submission of documentation to the Medicare appeals department. Once the supporting documentation is reviewed, reimbursement is granted.
Bundling
The National Correct Coding Initiative (NCCI) identifies edits that ultimately affect claims submission and payment. The Column One/Column Two Correct Coding Edits and the Mutually Exclusive Edits list code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group. Under some well-documented circumstances, the physician is allowed to “unbundle” the services by appending the appropriate modifier.
When services are denied as being “incidental/integral” to another reimbursed service (e.g., bundled), the claim should not automatically be resubmitted with a modifier appended to the “bundled” procedure code.
Documentation should be reviewed to determine if the denied service is separately reportable from the paid service. Only when supported by documentation can the physician append the appropriate modifier and resubmit the claim. For example, a hospitalist evaluated a patient with congestive heart failure and pleural effusions. The hospitalist determined that the patient requires placement of a central venous catheter (36556). Because the patient’s underlying condition was evaluated and resulted in the decision to place a central venous catheter, both the visit (99233) and the procedure (36556) can be reported. If submitted without modifiers, some payors may deny payment for the visit because it was not “integral” to the catheter placement. You should resubmit those claims with modifier 25.
Place of Service
Ensure that the place of service (POS) matches the service/procedure code. For example, say a hospitalist performs a consultation in the ED and determines that the patient does not need to be treated as an inpatient but provides recommendations for ED care and outpatient followup. Avoid a mismatch of the service code and the location. Consults performed in the ED should be reported with outpatient consultation codes (99241-99245) as appropriate. The correct POS should be the ED, not the inpatient hospital. Reporting outpatient codes with an inpatient POS (e.g., 21: inpatient hospital, 31: skilled nursing facility) will result in claim denial.
The same is true when trying to report inpatient consultation codes (99251-99255) in an outpatient location (e.g., 23-ED). The appropriate response for this type of denial is to resubmit the claim with the correct the POS and service/procedure code. A complete list of POS codes and corresponding definitions can be found in Chapter 26, Section 10.5 of the Medicare Claims Processing Manual, available at www.cms.hhs.gov/manuals/downloads/clm104c26.pdf.
Provider Enrollment
Provider enrollment issues occur when a physician’s national provider identifier (NPI) is not properly linked to the group practice. More often than not, the group practice receives claim rejections for enrollment issues when services involve nurse practitioners or physician assistants who have not enrolled with Medicare or cannot enroll with non-Medicare payors.
For example, a nurse practitioner independently provides a subsequent hospital-care service (e.g., 99232). The claim is submitted and Medicare reimburses the service at the correct amount as a primary insurer. The remaining balance is submitted to the secondary insurer. Because the submitted claim identifies the service provider as a nonphysician provider, who likely is not enrolled with the non-Medicare payor, the claim is rejected.
If the physician group has a contractual agreement to recognize nonphysician provider services by reporting them under the collaborating physician’s name, the claim can be resubmitted in the physician’s name. In absence of such an agreement, the claim should be written off. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
Reference
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
In order to recover the appropriate payment for services provided by hospitalists, the following must occur:
- The billing provider renders service fully, or jointly with a resident under the teaching physician guidelines or nonphysician provider under the shared/split billing rules;
- The service is completely and accurately documented in the medical record;
- The correct information is entered on the claim form that is submitted to the payor; and
- The service is determined to be a covered benefit and eligible for payment.
Claims frequently are rejected or denied. Even more frequently, the physician or billing staff does not understand the reason for the denial. The typical reaction to claim denial is twofold: “appeal with paper” and “write off.” In other words, send a copy of the physician notes to the payor and consider the claim unsuccessful and payment unable to be obtained.
Examining and understanding the payor’s initial claim determination might prompt a more successful response. Presuming the patient demographics are entered without error, the insurance information is correct, the patient is eligible for coverage, and all precertifications and authorizations were obtained, check for these other common errors.
Medical Necessity
Denials for “medical necessity” are not always what they seem. Individuals often assume that the physician reported an incorrect diagnosis code. Consider the service/procedure code when trying to formulate a response to the denial. When dealing with procedure codes, it is likely the denial is received for a mismatched diagnosis.
For example, a payor might deny a claim for cardiopulmonary resuscitation (92950) that is associated with a diagnosis code of congestive heart failure (428.0), despite this being the underlying condition that prompted the decline in the patient’s condition. The payor might only accept “cardiac arrest” (427.5) as the diagnosis for cardiopulmonary resuscitation because it was the direct reason for the procedure. After you ensure that the documentation supports the diagnosis, the claim should be resubmitted with the corrected diagnosis code.
If the “medical necessity” denial involves a covered evaluation and management (E/M) visit, it is less likely that the diagnosis code is the issue. When dealing with Medicare in particular, this type of denial likely is the result of a failure to respond to a prepayment request for documentation. Medicare issues prepayment requests for documentation for the following inpatient CPT codes: 99255, 99254, 99233, 99232, 99223, 99239, and 99292. If the documentation isn’t provided to the Medicare review department within the designated time frame, the claim is automatically denied. The reason for denial is cited as “not deemed a medical necessity.” Some providers misunderstand this remittance remark and assume that the physician assigned an incorrect diagnosis code. Although that might be true, it probably is due to a failure to respond to the prepayment documentation request. Appealing these claims requires the submission of documentation to the Medicare appeals department. Once the supporting documentation is reviewed, reimbursement is granted.
Bundling
The National Correct Coding Initiative (NCCI) identifies edits that ultimately affect claims submission and payment. The Column One/Column Two Correct Coding Edits and the Mutually Exclusive Edits list code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group. Under some well-documented circumstances, the physician is allowed to “unbundle” the services by appending the appropriate modifier.
When services are denied as being “incidental/integral” to another reimbursed service (e.g., bundled), the claim should not automatically be resubmitted with a modifier appended to the “bundled” procedure code.
Documentation should be reviewed to determine if the denied service is separately reportable from the paid service. Only when supported by documentation can the physician append the appropriate modifier and resubmit the claim. For example, a hospitalist evaluated a patient with congestive heart failure and pleural effusions. The hospitalist determined that the patient requires placement of a central venous catheter (36556). Because the patient’s underlying condition was evaluated and resulted in the decision to place a central venous catheter, both the visit (99233) and the procedure (36556) can be reported. If submitted without modifiers, some payors may deny payment for the visit because it was not “integral” to the catheter placement. You should resubmit those claims with modifier 25.
Place of Service
Ensure that the place of service (POS) matches the service/procedure code. For example, say a hospitalist performs a consultation in the ED and determines that the patient does not need to be treated as an inpatient but provides recommendations for ED care and outpatient followup. Avoid a mismatch of the service code and the location. Consults performed in the ED should be reported with outpatient consultation codes (99241-99245) as appropriate. The correct POS should be the ED, not the inpatient hospital. Reporting outpatient codes with an inpatient POS (e.g., 21: inpatient hospital, 31: skilled nursing facility) will result in claim denial.
The same is true when trying to report inpatient consultation codes (99251-99255) in an outpatient location (e.g., 23-ED). The appropriate response for this type of denial is to resubmit the claim with the correct the POS and service/procedure code. A complete list of POS codes and corresponding definitions can be found in Chapter 26, Section 10.5 of the Medicare Claims Processing Manual, available at www.cms.hhs.gov/manuals/downloads/clm104c26.pdf.
Provider Enrollment
Provider enrollment issues occur when a physician’s national provider identifier (NPI) is not properly linked to the group practice. More often than not, the group practice receives claim rejections for enrollment issues when services involve nurse practitioners or physician assistants who have not enrolled with Medicare or cannot enroll with non-Medicare payors.
For example, a nurse practitioner independently provides a subsequent hospital-care service (e.g., 99232). The claim is submitted and Medicare reimburses the service at the correct amount as a primary insurer. The remaining balance is submitted to the secondary insurer. Because the submitted claim identifies the service provider as a nonphysician provider, who likely is not enrolled with the non-Medicare payor, the claim is rejected.
If the physician group has a contractual agreement to recognize nonphysician provider services by reporting them under the collaborating physician’s name, the claim can be resubmitted in the physician’s name. In absence of such an agreement, the claim should be written off. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
Reference
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2008.
Code Correctly
A hospitalist who scrutinizes claims might notice a payment denial related to “unbundling” issues. Line-item rejections might state the service is “mutually exclusive,” “incidental to another procedure,” or “payment was received as part of another service/procedure.” Unbundling refers to the practice of reporting each component of a service or procedure instead of reporting the single, comprehensive code. Two types of practices lead to unbundling: unintentional reporting resulting from a basic misunderstanding of correct coding, and intentional reporting to improperly maximize payment of otherwise bundled Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) codes.1
The Centers for Medicare and Medicaid Services (CMS) developed the National Correct Coding Initiative (NCCI) for implementation and application to physician claims (e.g., Medicare Part B) with dates of service on or after Jan. 1, 1996. The rationale for these edits is a culmination of:
- Coding standards identified in the American Medical Association’s (AMA) CPT manual;
- National and local coverage determinations developed by CMS and local Medicare contractors;
- Coding standards set forth by national medical organizations and specialty societies;
- Appropriate standards of medical and surgical care; and
- Current coding practices identified through claim analysis, pre- and post-payment documentation reviews, and other forms of payor-initiated audit.
The initial NCCI goal was to promote correct coding methodologies and to control improper coding, which led to inappropriate payment in Part B claims.2 It later expanded to include corresponding NCCI edits in the outpatient code editor (OCE) for both outpatient hospital providers and therapy providers. Therapy providers encompass skilled nursing facilities (SNFs), comprehensive outpatient rehabilitation facilities (CORFs), outpatient physical therapy (OPTs) and speech-language pathology providers, and home health agencies (HHAs).
Fact-Check
The NCCI recognizes two edit types: Column One/Column Two Correct Coding edits and Mutually Exclusive edits. Each of these edit categories lists code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When applying Column One/Column Two editing logic to physician claims, the Column One code represents the more comprehensive code of the pair being reported. The Column Two code (the component service that is bundled into the comprehensive service) will be denied. This is not to say a code that appears in Column Two of the NCCI cannot be paid when reported by itself on any given date. The denial occurs only when the component service is reported on the same date as the more comprehensive service.
For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) is considered comprehensive to codes 36000 (introduction of needle or intracatheter, vein) and 36410 (venipuncture, age 3 years or older, necessitating physician’s skill [separate procedure], for diagnostic or therapeutic purposes). These code combinations should not be reported together on the same date when performed as part of the same procedure by the same physician or physicians of the same practice group. If this occurs, the payor will reimburse the initial service and deny the subsequent service. As a result, the first code received by the payor, on the same or separate claims, is reimbursed, even if that code represents the lesser of the two services.
Mutually Exclusive edits occur with less frequency than Column One/Column Two edits. Mutually Exclusive edits prevent reporting of two services or procedures that are highly unlikely to be performed together on the same patient, at the same session or encounter, by the same physician or physicians of the same specialty in a provider group. For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) would not be reported on the same day as 36555 (insertion of nontunneled centrally inserted central venous catheter, younger than 5 years of age).
CMS publishes the National Correct Coding Initiative Coding Policy Manual for Medicare Services (www.cms.hhs.gov/NationalCorrectCodInitEd) and encourages local Medicare contractors and fiscal intermediaries to use it as a reference for claims-processing edits. The manual is updated annually, and the NCCI edits are updated quarterly. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
References
- National correct coding initiative edits. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd. Accessed March 10, 2009.
- Medicare claims processing manual. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 10, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press, 2008;477-481.
- Modifier 59 article. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd/Downloads/modifier59.pdf. Accessed March 10, 2009.
- French K. Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians. 2008;283-287.
A hospitalist who scrutinizes claims might notice a payment denial related to “unbundling” issues. Line-item rejections might state the service is “mutually exclusive,” “incidental to another procedure,” or “payment was received as part of another service/procedure.” Unbundling refers to the practice of reporting each component of a service or procedure instead of reporting the single, comprehensive code. Two types of practices lead to unbundling: unintentional reporting resulting from a basic misunderstanding of correct coding, and intentional reporting to improperly maximize payment of otherwise bundled Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) codes.1
The Centers for Medicare and Medicaid Services (CMS) developed the National Correct Coding Initiative (NCCI) for implementation and application to physician claims (e.g., Medicare Part B) with dates of service on or after Jan. 1, 1996. The rationale for these edits is a culmination of:
- Coding standards identified in the American Medical Association’s (AMA) CPT manual;
- National and local coverage determinations developed by CMS and local Medicare contractors;
- Coding standards set forth by national medical organizations and specialty societies;
- Appropriate standards of medical and surgical care; and
- Current coding practices identified through claim analysis, pre- and post-payment documentation reviews, and other forms of payor-initiated audit.
The initial NCCI goal was to promote correct coding methodologies and to control improper coding, which led to inappropriate payment in Part B claims.2 It later expanded to include corresponding NCCI edits in the outpatient code editor (OCE) for both outpatient hospital providers and therapy providers. Therapy providers encompass skilled nursing facilities (SNFs), comprehensive outpatient rehabilitation facilities (CORFs), outpatient physical therapy (OPTs) and speech-language pathology providers, and home health agencies (HHAs).
Fact-Check
The NCCI recognizes two edit types: Column One/Column Two Correct Coding edits and Mutually Exclusive edits. Each of these edit categories lists code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When applying Column One/Column Two editing logic to physician claims, the Column One code represents the more comprehensive code of the pair being reported. The Column Two code (the component service that is bundled into the comprehensive service) will be denied. This is not to say a code that appears in Column Two of the NCCI cannot be paid when reported by itself on any given date. The denial occurs only when the component service is reported on the same date as the more comprehensive service.
For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) is considered comprehensive to codes 36000 (introduction of needle or intracatheter, vein) and 36410 (venipuncture, age 3 years or older, necessitating physician’s skill [separate procedure], for diagnostic or therapeutic purposes). These code combinations should not be reported together on the same date when performed as part of the same procedure by the same physician or physicians of the same practice group. If this occurs, the payor will reimburse the initial service and deny the subsequent service. As a result, the first code received by the payor, on the same or separate claims, is reimbursed, even if that code represents the lesser of the two services.
Mutually Exclusive edits occur with less frequency than Column One/Column Two edits. Mutually Exclusive edits prevent reporting of two services or procedures that are highly unlikely to be performed together on the same patient, at the same session or encounter, by the same physician or physicians of the same specialty in a provider group. For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) would not be reported on the same day as 36555 (insertion of nontunneled centrally inserted central venous catheter, younger than 5 years of age).
CMS publishes the National Correct Coding Initiative Coding Policy Manual for Medicare Services (www.cms.hhs.gov/NationalCorrectCodInitEd) and encourages local Medicare contractors and fiscal intermediaries to use it as a reference for claims-processing edits. The manual is updated annually, and the NCCI edits are updated quarterly. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
References
- National correct coding initiative edits. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd. Accessed March 10, 2009.
- Medicare claims processing manual. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 10, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press, 2008;477-481.
- Modifier 59 article. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd/Downloads/modifier59.pdf. Accessed March 10, 2009.
- French K. Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians. 2008;283-287.
A hospitalist who scrutinizes claims might notice a payment denial related to “unbundling” issues. Line-item rejections might state the service is “mutually exclusive,” “incidental to another procedure,” or “payment was received as part of another service/procedure.” Unbundling refers to the practice of reporting each component of a service or procedure instead of reporting the single, comprehensive code. Two types of practices lead to unbundling: unintentional reporting resulting from a basic misunderstanding of correct coding, and intentional reporting to improperly maximize payment of otherwise bundled Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) codes.1
The Centers for Medicare and Medicaid Services (CMS) developed the National Correct Coding Initiative (NCCI) for implementation and application to physician claims (e.g., Medicare Part B) with dates of service on or after Jan. 1, 1996. The rationale for these edits is a culmination of:
- Coding standards identified in the American Medical Association’s (AMA) CPT manual;
- National and local coverage determinations developed by CMS and local Medicare contractors;
- Coding standards set forth by national medical organizations and specialty societies;
- Appropriate standards of medical and surgical care; and
- Current coding practices identified through claim analysis, pre- and post-payment documentation reviews, and other forms of payor-initiated audit.
The initial NCCI goal was to promote correct coding methodologies and to control improper coding, which led to inappropriate payment in Part B claims.2 It later expanded to include corresponding NCCI edits in the outpatient code editor (OCE) for both outpatient hospital providers and therapy providers. Therapy providers encompass skilled nursing facilities (SNFs), comprehensive outpatient rehabilitation facilities (CORFs), outpatient physical therapy (OPTs) and speech-language pathology providers, and home health agencies (HHAs).
Fact-Check
The NCCI recognizes two edit types: Column One/Column Two Correct Coding edits and Mutually Exclusive edits. Each of these edit categories lists code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When applying Column One/Column Two editing logic to physician claims, the Column One code represents the more comprehensive code of the pair being reported. The Column Two code (the component service that is bundled into the comprehensive service) will be denied. This is not to say a code that appears in Column Two of the NCCI cannot be paid when reported by itself on any given date. The denial occurs only when the component service is reported on the same date as the more comprehensive service.
For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) is considered comprehensive to codes 36000 (introduction of needle or intracatheter, vein) and 36410 (venipuncture, age 3 years or older, necessitating physician’s skill [separate procedure], for diagnostic or therapeutic purposes). These code combinations should not be reported together on the same date when performed as part of the same procedure by the same physician or physicians of the same practice group. If this occurs, the payor will reimburse the initial service and deny the subsequent service. As a result, the first code received by the payor, on the same or separate claims, is reimbursed, even if that code represents the lesser of the two services.
Mutually Exclusive edits occur with less frequency than Column One/Column Two edits. Mutually Exclusive edits prevent reporting of two services or procedures that are highly unlikely to be performed together on the same patient, at the same session or encounter, by the same physician or physicians of the same specialty in a provider group. For example, CPT code 36556 (insertion of nontunneled centrally inserted central venous catheter, age 5 years or older) would not be reported on the same day as 36555 (insertion of nontunneled centrally inserted central venous catheter, younger than 5 years of age).
CMS publishes the National Correct Coding Initiative Coding Policy Manual for Medicare Services (www.cms.hhs.gov/NationalCorrectCodInitEd) and encourages local Medicare contractors and fiscal intermediaries to use it as a reference for claims-processing edits. The manual is updated annually, and the NCCI edits are updated quarterly. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
References
- National correct coding initiative edits. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd. Accessed March 10, 2009.
- Medicare claims processing manual. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed March 10, 2009.
- Beebe M, Dalton J, Espronceda M, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press, 2008;477-481.
- Modifier 59 article. Centers for Medicare and Medicaid Services Web site. Available at: www.cms.hhs.gov/NationalCorrectCodInitEd/Downloads/modifier59.pdf. Accessed March 10, 2009.
- French K. Coding for Chest Medicine 2009. Northbrook, IL: American College of Chest Physicians. 2008;283-287.