User login
H. pylori antibiotic resistance reaches ‘alarming levels’
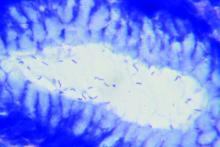
Over the past decade, Helicobacter pylori strains have reached “alarming levels” of antimicrobial resistance worldwide, investigators reported in the November issue of Gastroenterology.
In a large meta-analysis spanning 2007-2017, H. pylori isolates showed a 15% or higher pooled prevalence of primary and secondary resistance to clarithromycin, metronidazole, and levofloxacin in almost all World Health Organization (WHO) regions. “Local surveillance networks are required to select appropriate eradication regimens for each region,” concluded Alessia Savoldi, MD, of the University of Tübingen (Germany) and her associates.
Typically, the threshold of antimicrobial resistance for choosing empiric regimens is 15%, Dr. Savoldi and her associates noted. Their systematic review and meta-analysis included 178 studies comprising 66,142 isolates from 65 countries. They defined H. pylori infection as a positive histology, serology, stool antigen, urea breath test, or rapid urease test. They excluded studies of fewer than 50 isolates, studies that only reported resistance as a percentage with no denominator, studies that failed to specify time frames or clustered data over more than 3 years, and data reported in guidelines, conference presentations, or letters without formal publication.
The prevalence of primary clarithromycin resistance exceeded 15% in the WHO European Region (18%; 95% confidence interval, 16%-20%), the Eastern Mediterranean Region (33%), and the Western Pacific Region (34%) and reached 10% in the Americas and the South East Asia region. Furthermore, primary resistance to metronidazole exceeded 15% in all WHO regions, ranging from 56% in the Eastern Mediterranean Region to 23% in the Americas. Resistance to levofloxacin was at least 15% in all WHO regions except the European region (11%).
In most regions, H. pylori also accrued substantially more antimicrobial resistance over time, the investigators said. Clarithromycin resistance rose from 13% during 2006 through 2008 to 21% during 2012 through 2016 (P less than .001). Levofloxacin resistance in the Western Pacific region increased from 12% to 31% during the same two time periods (P less than .001). Several other WHO regions showed less significant trends toward increasing resistance. Multidrug resistance also rose. Resistance to both clarithromycin and metronidazole increased markedly in all WHO areas with available data, reaching 14% in the Eastern Mediterranean and Western Pacific regions and 23% in the European region.
Secondary analyses linked resistance with dramatic increases in the odds of treatment failure. For example, clarithromycin resistance conferred a sevenfold increase in the odds of treatment failure for regimens containing clarithromycin (odds ratio, 7.0; 95% CI, 5.2 to 9.3; P less than .001). Corresponding ORs were 8.2 for levofloxacin resistance, 2.5 for metronidazole resistance, and 9.4 for dual clarithromycin-metronidazole resistance.
The investigators acknowledged several limitations. Of publications in this meta-analysis, 85% represented single-center studies with limited sample sizes, they wrote. Studies often excluded demographic and endoscopic details. Furthermore, only three studies provided prevalence data for the WHO Africa Region and these only provided overall estimates without stratifying by resistance type.
The German Center for Infection Research, Clinical Research Unit, and the WHO Priority List Pathogens project helped fund the work. One coinvestigator disclosed ties to RedHill Biopharma, BioGaia, and Takeda related to novel H. pylori therapies.
SOURCE: Savoldi A et al. Gastroenterology. 2018 Nov. doi: 10.1053/j.gastro.2018.07.007.
The first-line treatment of individuals with Helicobacter pylori infection using clarithromycin-based triple therapies or, if penicillin allergic, bismuth-based quadruple therapies is generally effective. However, reports of declining therapeutic efficacy have led to published guidelines to recommend confirmation of H. pylori eradication after completing a course of antibiotics. It is believed that increasing antibiotic use in agriculture and medicine around the globe have contributed to the increasing H. pylori antibiotic resistance and declining efficacy of standard H. pylori regimens.
Indeed, most H. pylori guidelines recommend antibiotic sensitivity testing after failing two courses of treatment; however, performing such testing successfully may require sending fresh gastric biopsy samples to an in-house H. pylori culture lab within 1 hour, which is generally not available to most clinicians. Clearly, the gap in knowledge of local antibiotic resistance could be addressed by having a readily accessible culture facility and the testing should be reimbursed by health insurance.
Single-center experiences with antibiotic sensitivity–guided salvage therapy in the United States, however, registered a lower efficacy rate of approximately 50%, which indicates that other host factors (such as gastric acidity pH less than 5.5 or body mass index greater than 30 kg/m2) may affect the minimum inhibitory concentration (MIC) of the antibiotics against H. pylori.
In order to better study the effects of these host factors relative to the effect of antibiotic resistance on therapeutic efficacy, it is critical that we practice precision medicine by determining the antibiotic sensitivity of the H. pylori strain prior to initiating the antibiotic treatment. It may be possible to achieve more than 90% therapeutic efficacy given known antibiotic sensitivities of the bacteria and optimized host factors to lower the MIC. In addition, with the increasing awareness of the importance of gut microbiota in health and disease, clinicians should strive to narrow the antibiotic coverage that will be possible if antibiotic sensitivity is known (for example, use high-dose amoxicillin and proton-pump inhibitor dual therapy).
John Y. Kao, MD, AGAF, is the current chair of the AGA Institute Council Esophageal, Gastric and Duodenal Disorders Section, a physician investigator in the University of Michigan Center for Gastrointestinal Research, and an associate professor in the department of medicine in the division of gastroenterology & hepatology and an associate program director of the GI Fellowship Program at Michigan Medicine at the University of Michigan, Ann Arbor. He has no conflicts.
The first-line treatment of individuals with Helicobacter pylori infection using clarithromycin-based triple therapies or, if penicillin allergic, bismuth-based quadruple therapies is generally effective. However, reports of declining therapeutic efficacy have led to published guidelines to recommend confirmation of H. pylori eradication after completing a course of antibiotics. It is believed that increasing antibiotic use in agriculture and medicine around the globe have contributed to the increasing H. pylori antibiotic resistance and declining efficacy of standard H. pylori regimens.
Indeed, most H. pylori guidelines recommend antibiotic sensitivity testing after failing two courses of treatment; however, performing such testing successfully may require sending fresh gastric biopsy samples to an in-house H. pylori culture lab within 1 hour, which is generally not available to most clinicians. Clearly, the gap in knowledge of local antibiotic resistance could be addressed by having a readily accessible culture facility and the testing should be reimbursed by health insurance.
Single-center experiences with antibiotic sensitivity–guided salvage therapy in the United States, however, registered a lower efficacy rate of approximately 50%, which indicates that other host factors (such as gastric acidity pH less than 5.5 or body mass index greater than 30 kg/m2) may affect the minimum inhibitory concentration (MIC) of the antibiotics against H. pylori.
In order to better study the effects of these host factors relative to the effect of antibiotic resistance on therapeutic efficacy, it is critical that we practice precision medicine by determining the antibiotic sensitivity of the H. pylori strain prior to initiating the antibiotic treatment. It may be possible to achieve more than 90% therapeutic efficacy given known antibiotic sensitivities of the bacteria and optimized host factors to lower the MIC. In addition, with the increasing awareness of the importance of gut microbiota in health and disease, clinicians should strive to narrow the antibiotic coverage that will be possible if antibiotic sensitivity is known (for example, use high-dose amoxicillin and proton-pump inhibitor dual therapy).
John Y. Kao, MD, AGAF, is the current chair of the AGA Institute Council Esophageal, Gastric and Duodenal Disorders Section, a physician investigator in the University of Michigan Center for Gastrointestinal Research, and an associate professor in the department of medicine in the division of gastroenterology & hepatology and an associate program director of the GI Fellowship Program at Michigan Medicine at the University of Michigan, Ann Arbor. He has no conflicts.
The first-line treatment of individuals with Helicobacter pylori infection using clarithromycin-based triple therapies or, if penicillin allergic, bismuth-based quadruple therapies is generally effective. However, reports of declining therapeutic efficacy have led to published guidelines to recommend confirmation of H. pylori eradication after completing a course of antibiotics. It is believed that increasing antibiotic use in agriculture and medicine around the globe have contributed to the increasing H. pylori antibiotic resistance and declining efficacy of standard H. pylori regimens.
Indeed, most H. pylori guidelines recommend antibiotic sensitivity testing after failing two courses of treatment; however, performing such testing successfully may require sending fresh gastric biopsy samples to an in-house H. pylori culture lab within 1 hour, which is generally not available to most clinicians. Clearly, the gap in knowledge of local antibiotic resistance could be addressed by having a readily accessible culture facility and the testing should be reimbursed by health insurance.
Single-center experiences with antibiotic sensitivity–guided salvage therapy in the United States, however, registered a lower efficacy rate of approximately 50%, which indicates that other host factors (such as gastric acidity pH less than 5.5 or body mass index greater than 30 kg/m2) may affect the minimum inhibitory concentration (MIC) of the antibiotics against H. pylori.
In order to better study the effects of these host factors relative to the effect of antibiotic resistance on therapeutic efficacy, it is critical that we practice precision medicine by determining the antibiotic sensitivity of the H. pylori strain prior to initiating the antibiotic treatment. It may be possible to achieve more than 90% therapeutic efficacy given known antibiotic sensitivities of the bacteria and optimized host factors to lower the MIC. In addition, with the increasing awareness of the importance of gut microbiota in health and disease, clinicians should strive to narrow the antibiotic coverage that will be possible if antibiotic sensitivity is known (for example, use high-dose amoxicillin and proton-pump inhibitor dual therapy).
John Y. Kao, MD, AGAF, is the current chair of the AGA Institute Council Esophageal, Gastric and Duodenal Disorders Section, a physician investigator in the University of Michigan Center for Gastrointestinal Research, and an associate professor in the department of medicine in the division of gastroenterology & hepatology and an associate program director of the GI Fellowship Program at Michigan Medicine at the University of Michigan, Ann Arbor. He has no conflicts.
Over the past decade, Helicobacter pylori strains have reached “alarming levels” of antimicrobial resistance worldwide, investigators reported in the November issue of Gastroenterology.
In a large meta-analysis spanning 2007-2017, H. pylori isolates showed a 15% or higher pooled prevalence of primary and secondary resistance to clarithromycin, metronidazole, and levofloxacin in almost all World Health Organization (WHO) regions. “Local surveillance networks are required to select appropriate eradication regimens for each region,” concluded Alessia Savoldi, MD, of the University of Tübingen (Germany) and her associates.
Typically, the threshold of antimicrobial resistance for choosing empiric regimens is 15%, Dr. Savoldi and her associates noted. Their systematic review and meta-analysis included 178 studies comprising 66,142 isolates from 65 countries. They defined H. pylori infection as a positive histology, serology, stool antigen, urea breath test, or rapid urease test. They excluded studies of fewer than 50 isolates, studies that only reported resistance as a percentage with no denominator, studies that failed to specify time frames or clustered data over more than 3 years, and data reported in guidelines, conference presentations, or letters without formal publication.
The prevalence of primary clarithromycin resistance exceeded 15% in the WHO European Region (18%; 95% confidence interval, 16%-20%), the Eastern Mediterranean Region (33%), and the Western Pacific Region (34%) and reached 10% in the Americas and the South East Asia region. Furthermore, primary resistance to metronidazole exceeded 15% in all WHO regions, ranging from 56% in the Eastern Mediterranean Region to 23% in the Americas. Resistance to levofloxacin was at least 15% in all WHO regions except the European region (11%).
In most regions, H. pylori also accrued substantially more antimicrobial resistance over time, the investigators said. Clarithromycin resistance rose from 13% during 2006 through 2008 to 21% during 2012 through 2016 (P less than .001). Levofloxacin resistance in the Western Pacific region increased from 12% to 31% during the same two time periods (P less than .001). Several other WHO regions showed less significant trends toward increasing resistance. Multidrug resistance also rose. Resistance to both clarithromycin and metronidazole increased markedly in all WHO areas with available data, reaching 14% in the Eastern Mediterranean and Western Pacific regions and 23% in the European region.
Secondary analyses linked resistance with dramatic increases in the odds of treatment failure. For example, clarithromycin resistance conferred a sevenfold increase in the odds of treatment failure for regimens containing clarithromycin (odds ratio, 7.0; 95% CI, 5.2 to 9.3; P less than .001). Corresponding ORs were 8.2 for levofloxacin resistance, 2.5 for metronidazole resistance, and 9.4 for dual clarithromycin-metronidazole resistance.
The investigators acknowledged several limitations. Of publications in this meta-analysis, 85% represented single-center studies with limited sample sizes, they wrote. Studies often excluded demographic and endoscopic details. Furthermore, only three studies provided prevalence data for the WHO Africa Region and these only provided overall estimates without stratifying by resistance type.
The German Center for Infection Research, Clinical Research Unit, and the WHO Priority List Pathogens project helped fund the work. One coinvestigator disclosed ties to RedHill Biopharma, BioGaia, and Takeda related to novel H. pylori therapies.
SOURCE: Savoldi A et al. Gastroenterology. 2018 Nov. doi: 10.1053/j.gastro.2018.07.007.
Over the past decade, Helicobacter pylori strains have reached “alarming levels” of antimicrobial resistance worldwide, investigators reported in the November issue of Gastroenterology.
In a large meta-analysis spanning 2007-2017, H. pylori isolates showed a 15% or higher pooled prevalence of primary and secondary resistance to clarithromycin, metronidazole, and levofloxacin in almost all World Health Organization (WHO) regions. “Local surveillance networks are required to select appropriate eradication regimens for each region,” concluded Alessia Savoldi, MD, of the University of Tübingen (Germany) and her associates.
Typically, the threshold of antimicrobial resistance for choosing empiric regimens is 15%, Dr. Savoldi and her associates noted. Their systematic review and meta-analysis included 178 studies comprising 66,142 isolates from 65 countries. They defined H. pylori infection as a positive histology, serology, stool antigen, urea breath test, or rapid urease test. They excluded studies of fewer than 50 isolates, studies that only reported resistance as a percentage with no denominator, studies that failed to specify time frames or clustered data over more than 3 years, and data reported in guidelines, conference presentations, or letters without formal publication.
The prevalence of primary clarithromycin resistance exceeded 15% in the WHO European Region (18%; 95% confidence interval, 16%-20%), the Eastern Mediterranean Region (33%), and the Western Pacific Region (34%) and reached 10% in the Americas and the South East Asia region. Furthermore, primary resistance to metronidazole exceeded 15% in all WHO regions, ranging from 56% in the Eastern Mediterranean Region to 23% in the Americas. Resistance to levofloxacin was at least 15% in all WHO regions except the European region (11%).
In most regions, H. pylori also accrued substantially more antimicrobial resistance over time, the investigators said. Clarithromycin resistance rose from 13% during 2006 through 2008 to 21% during 2012 through 2016 (P less than .001). Levofloxacin resistance in the Western Pacific region increased from 12% to 31% during the same two time periods (P less than .001). Several other WHO regions showed less significant trends toward increasing resistance. Multidrug resistance also rose. Resistance to both clarithromycin and metronidazole increased markedly in all WHO areas with available data, reaching 14% in the Eastern Mediterranean and Western Pacific regions and 23% in the European region.
Secondary analyses linked resistance with dramatic increases in the odds of treatment failure. For example, clarithromycin resistance conferred a sevenfold increase in the odds of treatment failure for regimens containing clarithromycin (odds ratio, 7.0; 95% CI, 5.2 to 9.3; P less than .001). Corresponding ORs were 8.2 for levofloxacin resistance, 2.5 for metronidazole resistance, and 9.4 for dual clarithromycin-metronidazole resistance.
The investigators acknowledged several limitations. Of publications in this meta-analysis, 85% represented single-center studies with limited sample sizes, they wrote. Studies often excluded demographic and endoscopic details. Furthermore, only three studies provided prevalence data for the WHO Africa Region and these only provided overall estimates without stratifying by resistance type.
The German Center for Infection Research, Clinical Research Unit, and the WHO Priority List Pathogens project helped fund the work. One coinvestigator disclosed ties to RedHill Biopharma, BioGaia, and Takeda related to novel H. pylori therapies.
SOURCE: Savoldi A et al. Gastroenterology. 2018 Nov. doi: 10.1053/j.gastro.2018.07.007.
FROM GASTROENTEROLOGY
Key clinical point: Helicobacter pylori now shows significant levels of antibiotic resistance worldwide, complicating choices of empiric therapy.
Major finding: Primary and secondary resistance to clarithromycin, metronidazole, and levofloxacin was 15% or more in all WHO regions except for primary clarithromycin resistance in the Americas (10%) and South East Asia (10%) and primary levofloxacin resistance in Europe (11%).
Study details: Meta-analysis of 178 studies comprising 66,142 isolates from 65 countries.
Disclosures: The German Center for Infection Research, Clinical Research Unit, and the WHO Priority List Pathogens project helped fund the work. One coinvestigator disclosed ties to RedHill Biopharma, BioGaia, and Takeda related to novel H. pylori therapies.
Source: Savoldi A et al. Gastroenterology. 2018 Nov. doi: 10.1053/j.gastro.2018.07.007
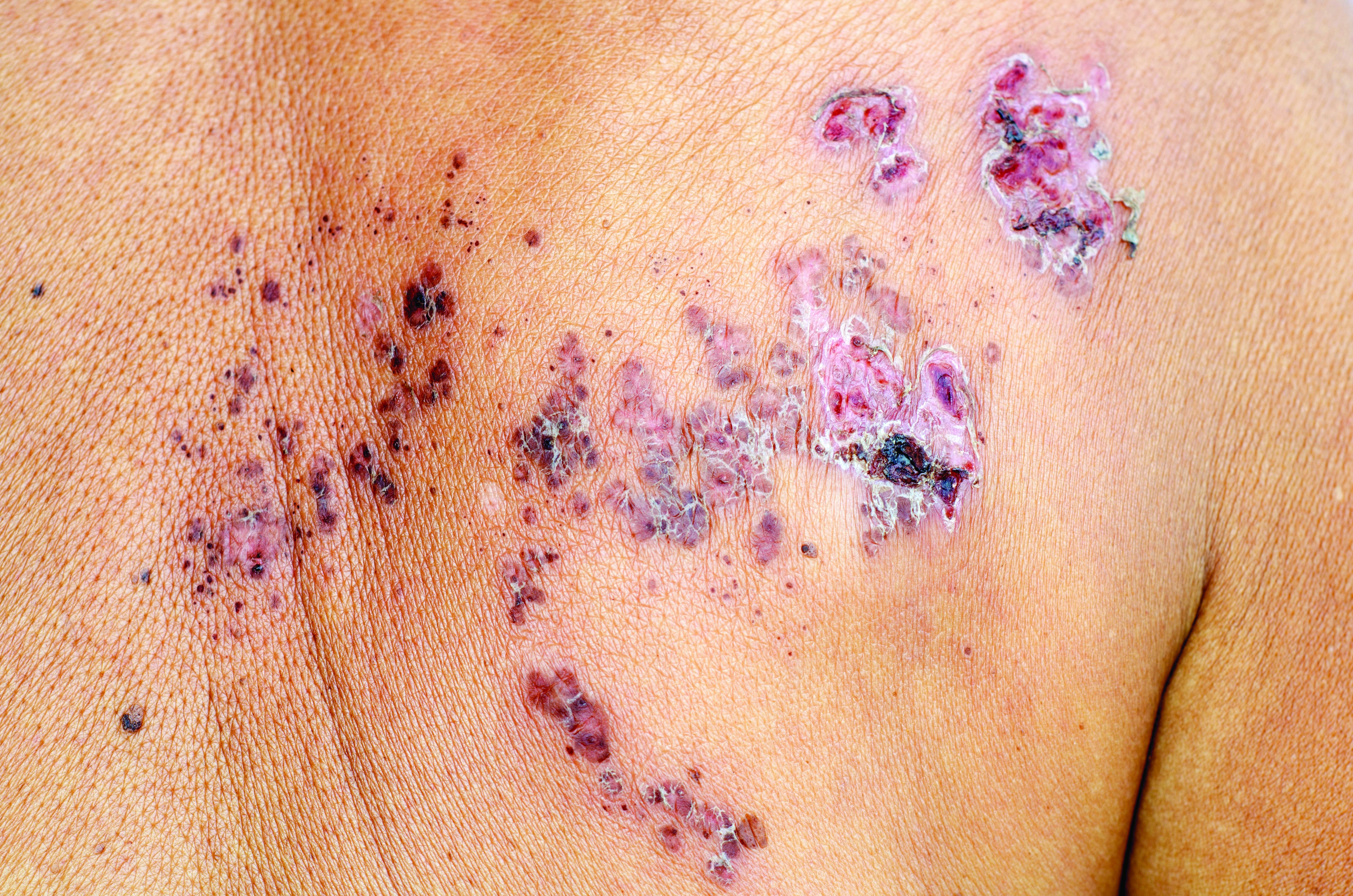
Thiopurines linked to zoster in IBD patients
For patients with inflammatory bowel disease (IBD), thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid (5-ASA) monotherapy, according to the results of two large retrospective cohort studies.
In the multivariable analysis, thiopurine monotherapy was linked to about a 47% increase in the risk of herpes zoster, compared with 5-ASA monotherapy (adjusted hazard ratio, 1.47; 95% confidence interval, 1.31-1.65; P less than .001). Combination therapy with thiopurines and tumor necrosis factor antagonists conferred about a 65% increase in zoster risk (aHR, 1.65; 95% CI, 1.22-2.23; P = .001). However, tumor necrosis factor–antagonist monotherapy did not appear to significantly increase the risk of zoster when compared with 5-ASA monotherapy, reported Nabeel Khan, MD, of the University of Pennsylvania in Philadelphia, and his associates.
“Compared to [patients without] IBD, ulcerative colitis (UC) and Crohn’s disease (CD) each were associated with significantly increased risk of herpes zoster infection,” the researchers wrote online in Clinical Gastroenterology and Hepatology. “With the approval of a new and potentially safer vaccine for herpes zoster, the effects of immunization of patients with IBD should be investigated.”
Past studies have linked IBD with a 1.2- to 1.8-fold increase in the risk of zoster, but these studies date to the prebiologic era or excluded patients who were in their midsixties or older, the researchers wrote. “Additionally, these prior studies have not assessed the validity of the codes used to identify herpes zoster and also did not account for the impact of vaccination,” they added. “They also did not take into consideration the severity of the disease or degree of steroid exposure.”
Therefore, the researchers conducted two retrospective cohort studies of patients in the United States Department of Veterans Affairs between 2000 and 2016. The first cohort study compared the incidence of herpes zoster among patients with IBD who received 5-ASA alone with matched patients without IBD. The second cohort study measured the incidence of herpes zoster in patients with IBD who received various medications and combination regimen. “The VA has a predominantly older population, which makes it an ideal cohort to study herpes zoster incidence in a high-risk population,” the investigators noted. “Unlike insurance databases, the VA database can be validated internally and vaccination records are documented.”
After adjusting for age, race, sex, geographic region, disease flare, corticosteroid use, and baseline comorbidities, the estimated hazard of developing herpes zoster was 1.81 (95% confidence interval, 1.56-2.11) among patients with ulcerative colitis and 1.56 (95% CI, 1.28-1.91) among patients with Crohn’s disease, as compared with patients without IBD. Regardless of their age or the medications they were receiving, patients with IBD had a higher incidence of zoster than the oldest group of patients without IBD (older than 60 years), regardless of age or medication. “The highest risk of herpes zoster was observed in patients with IBD who were less than 60 years of age and on combination therapy,” the investigators wrote. “Patients with IBD younger than 50 years who were on combination therapy had higher risk of herpes zoster, compared with patients with IBD older than 60 years of age who were not on immunosuppressive therapy.” Based on the findings, they recommended studying the efficacy of widespread use of the new herpes zoster vaccine in patients with IBD.
Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
SOURCE: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
Patients with inflammatory bowel disease are thought to have altered immune regulation, which may increase the risk of systemic complications including infections like herpes zoster. Many of the prior studies assessing the risk of herpes zoster in IBD patients were done before the advent of biologics and excluded older patients, thereby limiting their utility. This study by Khan et al. aimed to better estimate the incidence and risk factors for development of herpes zoster and to determine the effect of immunosuppressant use on this risk. In two large, retrospective cohort studies they found that, compared with patients without IBD, patients with IBD had a significantly increased risk of developing herpes zoster. Furthermore, this risk was higher in those with recent or cumulative steroid use and in those treated with thiopurines (as monotherapy or in combination with anti-TNF agents). Interestingly, exposure to TNF antagonists alone was not associated with an increased risk of herpes zoster infection.
Richa Shukla, MD, assistant professor, section of gastroenterology and hepatology, Baylor College of Medicine, Houston.
Patients with inflammatory bowel disease are thought to have altered immune regulation, which may increase the risk of systemic complications including infections like herpes zoster. Many of the prior studies assessing the risk of herpes zoster in IBD patients were done before the advent of biologics and excluded older patients, thereby limiting their utility. This study by Khan et al. aimed to better estimate the incidence and risk factors for development of herpes zoster and to determine the effect of immunosuppressant use on this risk. In two large, retrospective cohort studies they found that, compared with patients without IBD, patients with IBD had a significantly increased risk of developing herpes zoster. Furthermore, this risk was higher in those with recent or cumulative steroid use and in those treated with thiopurines (as monotherapy or in combination with anti-TNF agents). Interestingly, exposure to TNF antagonists alone was not associated with an increased risk of herpes zoster infection.
Richa Shukla, MD, assistant professor, section of gastroenterology and hepatology, Baylor College of Medicine, Houston.
Patients with inflammatory bowel disease are thought to have altered immune regulation, which may increase the risk of systemic complications including infections like herpes zoster. Many of the prior studies assessing the risk of herpes zoster in IBD patients were done before the advent of biologics and excluded older patients, thereby limiting their utility. This study by Khan et al. aimed to better estimate the incidence and risk factors for development of herpes zoster and to determine the effect of immunosuppressant use on this risk. In two large, retrospective cohort studies they found that, compared with patients without IBD, patients with IBD had a significantly increased risk of developing herpes zoster. Furthermore, this risk was higher in those with recent or cumulative steroid use and in those treated with thiopurines (as monotherapy or in combination with anti-TNF agents). Interestingly, exposure to TNF antagonists alone was not associated with an increased risk of herpes zoster infection.
Richa Shukla, MD, assistant professor, section of gastroenterology and hepatology, Baylor College of Medicine, Houston.
For patients with inflammatory bowel disease (IBD), thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid (5-ASA) monotherapy, according to the results of two large retrospective cohort studies.
In the multivariable analysis, thiopurine monotherapy was linked to about a 47% increase in the risk of herpes zoster, compared with 5-ASA monotherapy (adjusted hazard ratio, 1.47; 95% confidence interval, 1.31-1.65; P less than .001). Combination therapy with thiopurines and tumor necrosis factor antagonists conferred about a 65% increase in zoster risk (aHR, 1.65; 95% CI, 1.22-2.23; P = .001). However, tumor necrosis factor–antagonist monotherapy did not appear to significantly increase the risk of zoster when compared with 5-ASA monotherapy, reported Nabeel Khan, MD, of the University of Pennsylvania in Philadelphia, and his associates.
“Compared to [patients without] IBD, ulcerative colitis (UC) and Crohn’s disease (CD) each were associated with significantly increased risk of herpes zoster infection,” the researchers wrote online in Clinical Gastroenterology and Hepatology. “With the approval of a new and potentially safer vaccine for herpes zoster, the effects of immunization of patients with IBD should be investigated.”
Past studies have linked IBD with a 1.2- to 1.8-fold increase in the risk of zoster, but these studies date to the prebiologic era or excluded patients who were in their midsixties or older, the researchers wrote. “Additionally, these prior studies have not assessed the validity of the codes used to identify herpes zoster and also did not account for the impact of vaccination,” they added. “They also did not take into consideration the severity of the disease or degree of steroid exposure.”
Therefore, the researchers conducted two retrospective cohort studies of patients in the United States Department of Veterans Affairs between 2000 and 2016. The first cohort study compared the incidence of herpes zoster among patients with IBD who received 5-ASA alone with matched patients without IBD. The second cohort study measured the incidence of herpes zoster in patients with IBD who received various medications and combination regimen. “The VA has a predominantly older population, which makes it an ideal cohort to study herpes zoster incidence in a high-risk population,” the investigators noted. “Unlike insurance databases, the VA database can be validated internally and vaccination records are documented.”
After adjusting for age, race, sex, geographic region, disease flare, corticosteroid use, and baseline comorbidities, the estimated hazard of developing herpes zoster was 1.81 (95% confidence interval, 1.56-2.11) among patients with ulcerative colitis and 1.56 (95% CI, 1.28-1.91) among patients with Crohn’s disease, as compared with patients without IBD. Regardless of their age or the medications they were receiving, patients with IBD had a higher incidence of zoster than the oldest group of patients without IBD (older than 60 years), regardless of age or medication. “The highest risk of herpes zoster was observed in patients with IBD who were less than 60 years of age and on combination therapy,” the investigators wrote. “Patients with IBD younger than 50 years who were on combination therapy had higher risk of herpes zoster, compared with patients with IBD older than 60 years of age who were not on immunosuppressive therapy.” Based on the findings, they recommended studying the efficacy of widespread use of the new herpes zoster vaccine in patients with IBD.
Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
SOURCE: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
For patients with inflammatory bowel disease (IBD), thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid (5-ASA) monotherapy, according to the results of two large retrospective cohort studies.
In the multivariable analysis, thiopurine monotherapy was linked to about a 47% increase in the risk of herpes zoster, compared with 5-ASA monotherapy (adjusted hazard ratio, 1.47; 95% confidence interval, 1.31-1.65; P less than .001). Combination therapy with thiopurines and tumor necrosis factor antagonists conferred about a 65% increase in zoster risk (aHR, 1.65; 95% CI, 1.22-2.23; P = .001). However, tumor necrosis factor–antagonist monotherapy did not appear to significantly increase the risk of zoster when compared with 5-ASA monotherapy, reported Nabeel Khan, MD, of the University of Pennsylvania in Philadelphia, and his associates.
“Compared to [patients without] IBD, ulcerative colitis (UC) and Crohn’s disease (CD) each were associated with significantly increased risk of herpes zoster infection,” the researchers wrote online in Clinical Gastroenterology and Hepatology. “With the approval of a new and potentially safer vaccine for herpes zoster, the effects of immunization of patients with IBD should be investigated.”
Past studies have linked IBD with a 1.2- to 1.8-fold increase in the risk of zoster, but these studies date to the prebiologic era or excluded patients who were in their midsixties or older, the researchers wrote. “Additionally, these prior studies have not assessed the validity of the codes used to identify herpes zoster and also did not account for the impact of vaccination,” they added. “They also did not take into consideration the severity of the disease or degree of steroid exposure.”
Therefore, the researchers conducted two retrospective cohort studies of patients in the United States Department of Veterans Affairs between 2000 and 2016. The first cohort study compared the incidence of herpes zoster among patients with IBD who received 5-ASA alone with matched patients without IBD. The second cohort study measured the incidence of herpes zoster in patients with IBD who received various medications and combination regimen. “The VA has a predominantly older population, which makes it an ideal cohort to study herpes zoster incidence in a high-risk population,” the investigators noted. “Unlike insurance databases, the VA database can be validated internally and vaccination records are documented.”
After adjusting for age, race, sex, geographic region, disease flare, corticosteroid use, and baseline comorbidities, the estimated hazard of developing herpes zoster was 1.81 (95% confidence interval, 1.56-2.11) among patients with ulcerative colitis and 1.56 (95% CI, 1.28-1.91) among patients with Crohn’s disease, as compared with patients without IBD. Regardless of their age or the medications they were receiving, patients with IBD had a higher incidence of zoster than the oldest group of patients without IBD (older than 60 years), regardless of age or medication. “The highest risk of herpes zoster was observed in patients with IBD who were less than 60 years of age and on combination therapy,” the investigators wrote. “Patients with IBD younger than 50 years who were on combination therapy had higher risk of herpes zoster, compared with patients with IBD older than 60 years of age who were not on immunosuppressive therapy.” Based on the findings, they recommended studying the efficacy of widespread use of the new herpes zoster vaccine in patients with IBD.
Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
SOURCE: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: For patients with inflammatory bowel disease, thiopurine exposure was associated with a significantly increased risk of herpes zoster, compared with 5-aminosalicylic acid monotherapy.
Major finding: The adjusted hazard ratio was 1.47 (95% confidence interval, 1.31-1.65; P less than .001).
Study details: Two large retrospective cohort studies of veterans with and without inflammatory bowel disease.
Disclosures: Pfizer provided unrestricted research funding but was not otherwise involved in the study. One coinvestigator disclosed ties to Pfizer and several other pharmaceutical companies. The remaining investigators reported having no conflicts of interest.
Source: Khan N et al. Clin Gastroenterol Hepatol. 2018 Jan 5. doi: 10.1016/j.cgh.2017.12.052.
MELD sodium score tied to better transplant outcomes
Factoring hyponatremic status into liver graft allocations led to significant reductions in wait-list mortality, researchers reported in the November issue of Gastroenterology.
Hyponatremic patients with low MELD scores benefited significantly from allocation based on the end-stage liver disease–sodium (MELD-Na) score, while its survival benefit was less evident among patients with higher scores, said Shunji Nagai, MD, PhD, of Henry Ford Hospital, Detroit, and his associates. “Therefore, liver allocation rules such as Share 15 and Share 35 need to be revised to fulfill the Final Rule under the MELD-Na based allocation,” they wrote.
The Share 35 rule offers liver grafts locally and regionally to wait-listed patients with MELD-Na scores of at least 35. Under the Share 15 rule, livers are offered regionally or nationally before considering local candidates with MELD scores under 15. The traditional MELD scoring system excluded hyponatremia, which has since been found to independently predict death from cirrhosis. Therefore, in January 2016, a modified MELD-Na score was implemented for patients with traditional MELD scores of at least 12. The MELD-Na score assigns patients between 1 and 11 additional points, and patients with low MELD scores and severe hyponatremia receive the most points. To assess the impact of this change, Dr. Nagai and his associates compared wait-list and posttransplantation outcomes during the pre and post–MELD-Na eras and the survival benefit of liver transplantation during the MELD-Na period. The study included all adults wait-listed for livers from June 2013, when Share 35 was implemented, through September 2017.
Mortality within 90 days on the wait list fell significantly during the MELD-Na era (hazard ratio, 0.74; P less than .001). Transplantation conferred a “definitive” survival benefit when MELD-Na scores were 21-23 (HR versus wait list, 0.34; P less than .001). During the traditional MELD period, the equivalent cutoff was 15-17 (HR, 0.36; P less than .001). “As such, the current rules for liver allocation may be suboptimal under the MELD-Na–based allocation and the criteria for Share 15 may need to be revisited,” the researchers wrote. They recommended raising the cutoff to 21.
The study also confirmed mild hyponatremia (130-134 mmol/L), moderate hyponatremia (125-129 mmol/L), and severe hyponatremia (less than 125 mmol/L) as independent predictors of wait-list mortality during the traditional MELD era. Hazard ratios were 1.4, 1.8, and 1.7, respectively (all P less than .001). The implementation of MELD-Na significantly weakened these associations, with HRs of 1.1 (P = .3), 1.3 (P = .02), and 1.4 (P = .04), respectively).
The probability of transplantation also rose significantly during the MELD-Na era (HR, 1.2; P less than .001), possibly because of the opioid epidemic, the researchers said. Although greater availability of liver grafts might have improved wait-list outcomes, all score categories would have shown a positive impact if this was the only reason, they added. Instead, MELD-Na most benefited patients with lower scores.
Finally, posttransplantation outcomes worsened during the MELD-Na era, perhaps because of transplant population aging. However, the survival benefit of transplant shifted to higher score ranges during the MELD-Na era even after the researchers controlled for this effect. “According to this analysis,” they wrote, “the survival benefit of liver transplant was definitive in patients with score category of 21-23, which could further validate our proposal to revise Share 15 rule to ‘Share 21.’ ”
The investigators reported having no external funding sources or conflicts of interest.
SOURCE: Nagai S et al. Gastroenterology. 2018 Jul 26. doi: 10.1053/j.gastro.2018.07.025.
Factoring hyponatremic status into liver graft allocations led to significant reductions in wait-list mortality, researchers reported in the November issue of Gastroenterology.
Hyponatremic patients with low MELD scores benefited significantly from allocation based on the end-stage liver disease–sodium (MELD-Na) score, while its survival benefit was less evident among patients with higher scores, said Shunji Nagai, MD, PhD, of Henry Ford Hospital, Detroit, and his associates. “Therefore, liver allocation rules such as Share 15 and Share 35 need to be revised to fulfill the Final Rule under the MELD-Na based allocation,” they wrote.
The Share 35 rule offers liver grafts locally and regionally to wait-listed patients with MELD-Na scores of at least 35. Under the Share 15 rule, livers are offered regionally or nationally before considering local candidates with MELD scores under 15. The traditional MELD scoring system excluded hyponatremia, which has since been found to independently predict death from cirrhosis. Therefore, in January 2016, a modified MELD-Na score was implemented for patients with traditional MELD scores of at least 12. The MELD-Na score assigns patients between 1 and 11 additional points, and patients with low MELD scores and severe hyponatremia receive the most points. To assess the impact of this change, Dr. Nagai and his associates compared wait-list and posttransplantation outcomes during the pre and post–MELD-Na eras and the survival benefit of liver transplantation during the MELD-Na period. The study included all adults wait-listed for livers from June 2013, when Share 35 was implemented, through September 2017.
Mortality within 90 days on the wait list fell significantly during the MELD-Na era (hazard ratio, 0.74; P less than .001). Transplantation conferred a “definitive” survival benefit when MELD-Na scores were 21-23 (HR versus wait list, 0.34; P less than .001). During the traditional MELD period, the equivalent cutoff was 15-17 (HR, 0.36; P less than .001). “As such, the current rules for liver allocation may be suboptimal under the MELD-Na–based allocation and the criteria for Share 15 may need to be revisited,” the researchers wrote. They recommended raising the cutoff to 21.
The study also confirmed mild hyponatremia (130-134 mmol/L), moderate hyponatremia (125-129 mmol/L), and severe hyponatremia (less than 125 mmol/L) as independent predictors of wait-list mortality during the traditional MELD era. Hazard ratios were 1.4, 1.8, and 1.7, respectively (all P less than .001). The implementation of MELD-Na significantly weakened these associations, with HRs of 1.1 (P = .3), 1.3 (P = .02), and 1.4 (P = .04), respectively).
The probability of transplantation also rose significantly during the MELD-Na era (HR, 1.2; P less than .001), possibly because of the opioid epidemic, the researchers said. Although greater availability of liver grafts might have improved wait-list outcomes, all score categories would have shown a positive impact if this was the only reason, they added. Instead, MELD-Na most benefited patients with lower scores.
Finally, posttransplantation outcomes worsened during the MELD-Na era, perhaps because of transplant population aging. However, the survival benefit of transplant shifted to higher score ranges during the MELD-Na era even after the researchers controlled for this effect. “According to this analysis,” they wrote, “the survival benefit of liver transplant was definitive in patients with score category of 21-23, which could further validate our proposal to revise Share 15 rule to ‘Share 21.’ ”
The investigators reported having no external funding sources or conflicts of interest.
SOURCE: Nagai S et al. Gastroenterology. 2018 Jul 26. doi: 10.1053/j.gastro.2018.07.025.
Factoring hyponatremic status into liver graft allocations led to significant reductions in wait-list mortality, researchers reported in the November issue of Gastroenterology.
Hyponatremic patients with low MELD scores benefited significantly from allocation based on the end-stage liver disease–sodium (MELD-Na) score, while its survival benefit was less evident among patients with higher scores, said Shunji Nagai, MD, PhD, of Henry Ford Hospital, Detroit, and his associates. “Therefore, liver allocation rules such as Share 15 and Share 35 need to be revised to fulfill the Final Rule under the MELD-Na based allocation,” they wrote.
The Share 35 rule offers liver grafts locally and regionally to wait-listed patients with MELD-Na scores of at least 35. Under the Share 15 rule, livers are offered regionally or nationally before considering local candidates with MELD scores under 15. The traditional MELD scoring system excluded hyponatremia, which has since been found to independently predict death from cirrhosis. Therefore, in January 2016, a modified MELD-Na score was implemented for patients with traditional MELD scores of at least 12. The MELD-Na score assigns patients between 1 and 11 additional points, and patients with low MELD scores and severe hyponatremia receive the most points. To assess the impact of this change, Dr. Nagai and his associates compared wait-list and posttransplantation outcomes during the pre and post–MELD-Na eras and the survival benefit of liver transplantation during the MELD-Na period. The study included all adults wait-listed for livers from June 2013, when Share 35 was implemented, through September 2017.
Mortality within 90 days on the wait list fell significantly during the MELD-Na era (hazard ratio, 0.74; P less than .001). Transplantation conferred a “definitive” survival benefit when MELD-Na scores were 21-23 (HR versus wait list, 0.34; P less than .001). During the traditional MELD period, the equivalent cutoff was 15-17 (HR, 0.36; P less than .001). “As such, the current rules for liver allocation may be suboptimal under the MELD-Na–based allocation and the criteria for Share 15 may need to be revisited,” the researchers wrote. They recommended raising the cutoff to 21.
The study also confirmed mild hyponatremia (130-134 mmol/L), moderate hyponatremia (125-129 mmol/L), and severe hyponatremia (less than 125 mmol/L) as independent predictors of wait-list mortality during the traditional MELD era. Hazard ratios were 1.4, 1.8, and 1.7, respectively (all P less than .001). The implementation of MELD-Na significantly weakened these associations, with HRs of 1.1 (P = .3), 1.3 (P = .02), and 1.4 (P = .04), respectively).
The probability of transplantation also rose significantly during the MELD-Na era (HR, 1.2; P less than .001), possibly because of the opioid epidemic, the researchers said. Although greater availability of liver grafts might have improved wait-list outcomes, all score categories would have shown a positive impact if this was the only reason, they added. Instead, MELD-Na most benefited patients with lower scores.
Finally, posttransplantation outcomes worsened during the MELD-Na era, perhaps because of transplant population aging. However, the survival benefit of transplant shifted to higher score ranges during the MELD-Na era even after the researchers controlled for this effect. “According to this analysis,” they wrote, “the survival benefit of liver transplant was definitive in patients with score category of 21-23, which could further validate our proposal to revise Share 15 rule to ‘Share 21.’ ”
The investigators reported having no external funding sources or conflicts of interest.
SOURCE: Nagai S et al. Gastroenterology. 2018 Jul 26. doi: 10.1053/j.gastro.2018.07.025.
FROM GASTROENTEROLOGY
Key clinical point: The implementation of the MELD sodium (MELD-Na) score for liver allocation was associated with significantly improved outcomes for wait-listed patients.
Major finding: During the MELD-Na era, mortality within 90 days on the liver wait list dropped significantly (HR, 0.74; P less than .001) while the probability of transplant rose significantly (HR, 1.2; P less than .001).
Study details: Comparison of 18,850 adult transplant candidates during the traditional MELD era versus 14,512 candidates during the MELD-Na era.
Disclosures: The investigators had no external funding sources or conflicts of interest.
Source: Nagai S et al. Gastroenterology. 2018 Jul 26. doi: 10.1053/j.gastro.2018.07.025.
Proximal adenoma location does not predict high-grade dysplasia
Proximal adenoma location did not predict high-grade dysplasia in a large registry study.
In fact, the odds of high-grade dysplasia were about 25% lower for proximal versus distal adenomas (odds ratio, 0.75), reported Thomas Rösch, MD, of University Hospital Hamburg-Eppendorf, Hamburg, Germany, and his associates. A third of adenomas in the study lacked location data, but in sensitivity analyses, the odds of high-grade dysplasia fell to 0.72 when these lesions were assumed to be proximal and rose to 0.96 when they were assumed to be distal.
Interval colorectal cancers probably are more likely to be proximal than distal because of a “combination of endoscopy-related factors and biology,” not because of histologic differences alone, the researchers wrote. The report was published in Clinical Gastroenterology and Hepatology.
Interval cancers are more common in the right colon, as several studies have noted. However, it was unclear whether this phenomenon represented a higher miss rate, a lower rate of successful polypectomy, or an increased risk of malignant histology in the proximal colon, the researchers wrote. Accordingly, they analyzed data on 594,614 index adenomas detected during more than 2.5 million screening colonoscopies performed between 2007 and 2012 and entered into the German National Screening Colonoscopy Registry.
A total of 3.5% of index adenomas showed high-grade dysplasia, which correlated most strongly with larger size, said the researchers. In fact, the odds of high-grade dysplasia were 10-fold higher when index adenomas measured at least 1 cm than when they were smaller. High-grade dysplasia also was significantly more frequent when patients were older than 64 years, were male, and when they had pedunculated versus flat lesions. Given the large size of the dataset, all these associations were statistically significant.
Sessile lesions were slightly more likely to be high-grade compared with flat lesions, the investigators noted. Many proximal interval cancers arise from sessile serrated polyps, which may be subtle and difficult to detect or to resect completely, they continued. At the same time, colonoscopy also might be more likely to miss flat, serrated lesions when they are located proximally, and these lesions can become more aggressive over time. Thus, “[e]ndoscopist factors, such as missed lesions or incompletely removed lesions, may account for the predominance of proximal interval colorectal cancers.”
Like other registry studies, this study lacked uniform histopathologic definitions or central histopathology review. The dataset also covered only the largest or most histologically remarkable adenoma for each patient. However, the study findings did not change substantially after the researchers controlled for patients with missing location data, which presumably included patients with multiple polyps in both proximal and distal locations.
The researchers did not disclose external funding sources. They reported having no conflicts of interest.
SOURCE: Rösch T et al. Clin Gastroenterol Hepatol. 2018 Jun 11. doi: 10.1016/j.cgh.2018.05.043.
Colorectal cancers detected in a short interval after a complete and clearing colonoscopy are referred to as postcolonoscopy colon cancers or interval cancers, and are approximately three times more likely to occur in the proximal colon compared with the distal colon. Reasons for this difference are not known and possible explanations include alternate and accelerated tumor biology and rapid cancer progression, such as through the CpG island methylation phenotype pathway, missed cancers or precursor lesions in the proximal colon, or incomplete polyp resection. In the current study, the authors address whether the biology of polyps removed in the proximal colon is different, i.e., are these adenomas more likely to exhibit high-grade dysplasia compared to adenomas in the distal colon in approximately 2.5 million screening colonoscopies performed between 2007 and 2012, obtained from a screening colonoscopy registry in Germany. The authors did not find a difference in frequency of high-grade dysplasia between proximal and distal polyps. As expected, adenoma size, male sex, and older age were associated with finding of high-grade dysplasia, but contrary to current literature, the authors found that distal location and pedunculated (versus sessile) form were associated with high-grade dysplasia. A major limitation of the study is that sessile serrated polyps were not included, and the authors did not have information on villous histology. The study reinforces the hypothesis that missed and incompletely resected adenomas play a bigger role in missed proximal cancers, and that the goal of high-quality colonoscopy should be to detect and completely resect adenomas with equal vigilance in both the proximal and distal colon.
Aasma Shaukat, MD, MPH, AGAF, is professor of medicine in the division of gastroenterology and hepatology at the University of Minnesota, Minneapolis, and the GI Section Chief at the Minneapolis VA Medical Center. She has no conflicts of interest.
Colorectal cancers detected in a short interval after a complete and clearing colonoscopy are referred to as postcolonoscopy colon cancers or interval cancers, and are approximately three times more likely to occur in the proximal colon compared with the distal colon. Reasons for this difference are not known and possible explanations include alternate and accelerated tumor biology and rapid cancer progression, such as through the CpG island methylation phenotype pathway, missed cancers or precursor lesions in the proximal colon, or incomplete polyp resection. In the current study, the authors address whether the biology of polyps removed in the proximal colon is different, i.e., are these adenomas more likely to exhibit high-grade dysplasia compared to adenomas in the distal colon in approximately 2.5 million screening colonoscopies performed between 2007 and 2012, obtained from a screening colonoscopy registry in Germany. The authors did not find a difference in frequency of high-grade dysplasia between proximal and distal polyps. As expected, adenoma size, male sex, and older age were associated with finding of high-grade dysplasia, but contrary to current literature, the authors found that distal location and pedunculated (versus sessile) form were associated with high-grade dysplasia. A major limitation of the study is that sessile serrated polyps were not included, and the authors did not have information on villous histology. The study reinforces the hypothesis that missed and incompletely resected adenomas play a bigger role in missed proximal cancers, and that the goal of high-quality colonoscopy should be to detect and completely resect adenomas with equal vigilance in both the proximal and distal colon.
Aasma Shaukat, MD, MPH, AGAF, is professor of medicine in the division of gastroenterology and hepatology at the University of Minnesota, Minneapolis, and the GI Section Chief at the Minneapolis VA Medical Center. She has no conflicts of interest.
Colorectal cancers detected in a short interval after a complete and clearing colonoscopy are referred to as postcolonoscopy colon cancers or interval cancers, and are approximately three times more likely to occur in the proximal colon compared with the distal colon. Reasons for this difference are not known and possible explanations include alternate and accelerated tumor biology and rapid cancer progression, such as through the CpG island methylation phenotype pathway, missed cancers or precursor lesions in the proximal colon, or incomplete polyp resection. In the current study, the authors address whether the biology of polyps removed in the proximal colon is different, i.e., are these adenomas more likely to exhibit high-grade dysplasia compared to adenomas in the distal colon in approximately 2.5 million screening colonoscopies performed between 2007 and 2012, obtained from a screening colonoscopy registry in Germany. The authors did not find a difference in frequency of high-grade dysplasia between proximal and distal polyps. As expected, adenoma size, male sex, and older age were associated with finding of high-grade dysplasia, but contrary to current literature, the authors found that distal location and pedunculated (versus sessile) form were associated with high-grade dysplasia. A major limitation of the study is that sessile serrated polyps were not included, and the authors did not have information on villous histology. The study reinforces the hypothesis that missed and incompletely resected adenomas play a bigger role in missed proximal cancers, and that the goal of high-quality colonoscopy should be to detect and completely resect adenomas with equal vigilance in both the proximal and distal colon.
Aasma Shaukat, MD, MPH, AGAF, is professor of medicine in the division of gastroenterology and hepatology at the University of Minnesota, Minneapolis, and the GI Section Chief at the Minneapolis VA Medical Center. She has no conflicts of interest.
Proximal adenoma location did not predict high-grade dysplasia in a large registry study.
In fact, the odds of high-grade dysplasia were about 25% lower for proximal versus distal adenomas (odds ratio, 0.75), reported Thomas Rösch, MD, of University Hospital Hamburg-Eppendorf, Hamburg, Germany, and his associates. A third of adenomas in the study lacked location data, but in sensitivity analyses, the odds of high-grade dysplasia fell to 0.72 when these lesions were assumed to be proximal and rose to 0.96 when they were assumed to be distal.
Interval colorectal cancers probably are more likely to be proximal than distal because of a “combination of endoscopy-related factors and biology,” not because of histologic differences alone, the researchers wrote. The report was published in Clinical Gastroenterology and Hepatology.
Interval cancers are more common in the right colon, as several studies have noted. However, it was unclear whether this phenomenon represented a higher miss rate, a lower rate of successful polypectomy, or an increased risk of malignant histology in the proximal colon, the researchers wrote. Accordingly, they analyzed data on 594,614 index adenomas detected during more than 2.5 million screening colonoscopies performed between 2007 and 2012 and entered into the German National Screening Colonoscopy Registry.
A total of 3.5% of index adenomas showed high-grade dysplasia, which correlated most strongly with larger size, said the researchers. In fact, the odds of high-grade dysplasia were 10-fold higher when index adenomas measured at least 1 cm than when they were smaller. High-grade dysplasia also was significantly more frequent when patients were older than 64 years, were male, and when they had pedunculated versus flat lesions. Given the large size of the dataset, all these associations were statistically significant.
Sessile lesions were slightly more likely to be high-grade compared with flat lesions, the investigators noted. Many proximal interval cancers arise from sessile serrated polyps, which may be subtle and difficult to detect or to resect completely, they continued. At the same time, colonoscopy also might be more likely to miss flat, serrated lesions when they are located proximally, and these lesions can become more aggressive over time. Thus, “[e]ndoscopist factors, such as missed lesions or incompletely removed lesions, may account for the predominance of proximal interval colorectal cancers.”
Like other registry studies, this study lacked uniform histopathologic definitions or central histopathology review. The dataset also covered only the largest or most histologically remarkable adenoma for each patient. However, the study findings did not change substantially after the researchers controlled for patients with missing location data, which presumably included patients with multiple polyps in both proximal and distal locations.
The researchers did not disclose external funding sources. They reported having no conflicts of interest.
SOURCE: Rösch T et al. Clin Gastroenterol Hepatol. 2018 Jun 11. doi: 10.1016/j.cgh.2018.05.043.
Proximal adenoma location did not predict high-grade dysplasia in a large registry study.
In fact, the odds of high-grade dysplasia were about 25% lower for proximal versus distal adenomas (odds ratio, 0.75), reported Thomas Rösch, MD, of University Hospital Hamburg-Eppendorf, Hamburg, Germany, and his associates. A third of adenomas in the study lacked location data, but in sensitivity analyses, the odds of high-grade dysplasia fell to 0.72 when these lesions were assumed to be proximal and rose to 0.96 when they were assumed to be distal.
Interval colorectal cancers probably are more likely to be proximal than distal because of a “combination of endoscopy-related factors and biology,” not because of histologic differences alone, the researchers wrote. The report was published in Clinical Gastroenterology and Hepatology.
Interval cancers are more common in the right colon, as several studies have noted. However, it was unclear whether this phenomenon represented a higher miss rate, a lower rate of successful polypectomy, or an increased risk of malignant histology in the proximal colon, the researchers wrote. Accordingly, they analyzed data on 594,614 index adenomas detected during more than 2.5 million screening colonoscopies performed between 2007 and 2012 and entered into the German National Screening Colonoscopy Registry.
A total of 3.5% of index adenomas showed high-grade dysplasia, which correlated most strongly with larger size, said the researchers. In fact, the odds of high-grade dysplasia were 10-fold higher when index adenomas measured at least 1 cm than when they were smaller. High-grade dysplasia also was significantly more frequent when patients were older than 64 years, were male, and when they had pedunculated versus flat lesions. Given the large size of the dataset, all these associations were statistically significant.
Sessile lesions were slightly more likely to be high-grade compared with flat lesions, the investigators noted. Many proximal interval cancers arise from sessile serrated polyps, which may be subtle and difficult to detect or to resect completely, they continued. At the same time, colonoscopy also might be more likely to miss flat, serrated lesions when they are located proximally, and these lesions can become more aggressive over time. Thus, “[e]ndoscopist factors, such as missed lesions or incompletely removed lesions, may account for the predominance of proximal interval colorectal cancers.”
Like other registry studies, this study lacked uniform histopathologic definitions or central histopathology review. The dataset also covered only the largest or most histologically remarkable adenoma for each patient. However, the study findings did not change substantially after the researchers controlled for patients with missing location data, which presumably included patients with multiple polyps in both proximal and distal locations.
The researchers did not disclose external funding sources. They reported having no conflicts of interest.
SOURCE: Rösch T et al. Clin Gastroenterol Hepatol. 2018 Jun 11. doi: 10.1016/j.cgh.2018.05.043.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Proximal adenoma location did not predict high-grade dysplasia.
Major finding: The odds of high-grade dysplasia were about 25% lower for proximal versus distal adenomas (odds ratio, 0.75).
Study details: Registry study of 594,614 adenomas identified during more than 2.5 million screening colonoscopies between 2007 and 2012.
Disclosures: The researchers did not disclose external funding sources. They reported having no conflicts of interest.
Source: Rösch T et al. Clin Gastroenterol Hepatol. 2018 Jun 11. doi: 10.1016/j.cgh.2018.05.043.
ALEX: Alectinib showed superior CNS efficacy in ALK+ NSCLC
For patients with treatment-naive anaplastic lymphoma kinase–positive (ALK+) non–small cell lung cancer (NSCLC), twice-daily oral treatment with alectinib (600 mg) was associated with significantly greater activity in the CNS and significantly delayed CNS progression, compared with crizotinib (200 mg), based on secondary analyses from the pivotal phase 3 ALEX trial.
Time to CNS progression was significantly longer with alectinib versus crizotinib (hazard ratio, 0.18; 95% confidence interval, 0.09-0.36) regardless of whether patients had asymptomatic baseline CNS metastases or a prior history of radiotherapy. For patients with baseline asymptomatic CNS metastases, the 12-month cumulative incidence of CNS progression was 16% with alectinib versus 58.3% with crizotinib. Among patients without asymptomatic CNS metastases at baseline, these rates were 4.6% versus 31.5%, respectively.
The findings “consolidate alectinib as the standard of care for untreated, advanced ALK+ NSCLC, irrespective of the presence or absence of baseline CNS metastases,” Shirish M. Gadgeel, MD, of the University of Michigan, Ann Arbor, and his associates wrote in Annals of Oncology.
ALEX was the first study of an ALK inhibitor to include a prospective, standardized intention-to-treat analysis of CNS lesions, regardless of whether patients had these lesions at baseline. All patients underwent brain imaging at baseline and every 8 weeks thereafter. In the primary analysis of 303 patients, alectinib significantly improved progression-free survival in patients with and without baseline CNS disease and showed a significantly higher intracranial overall response rate, irrespective of whether patients had previously received radiotherapy.
Based on these results, National Comprehensive Cancer Network guidelines were updated to include a category 1 recommendation for the first-line use of alectinib in patients with ALK+ NSCLC.
The current analysis focused on CNS efficacy. In all, 122 patients had CNS metastases at baseline. Progression-free survival was similar regardless of whether patients had these lesions (HR, 0.40; 95% CI, 0.25-0.64) or not (HR, 0.51; 95% CI, 0.33-0.80; P = .36). History of radiotherapy also did not significantly affect overall CNS response or progression-free survival.
“Our data are in agreement with a pooled analysis of alectinib phase 2 trials, which demonstrated that central nervous system efficacy of alectinib is maintained regardless of radiotherapy history in crizotinib-pretreated patients,” the investigators wrote.
Because ALEX excluded patients with symptomatic CNS disease, its effects in this population remain unclear, they noted. “ALEX data strongly suggest that in asymptomatic patients, treating CNS metastases with alectinib alone may result in a reduced or delayed need for local CNS treatment.”
F. Hoffman-La Roche funded the study. Dr. Gadgeel reported honoraria and consultancy fees from Roche/Genentech, ARIAD Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, and Pfizer.
SOURCE: Gadgeel SM et al. Ann Oncol. 2018 Sep 12. doi: 10.1093/annonc/mdy405.
The results of the phase 3 ALEX trial provide strong rationale for the first-line use of alectinib in patients with non–small cell lung cancer (NSCLC) harboring anaplastic lymphoma kinase (ALK) gene rearrangements.
Alectinib showed robust evidence of intracranial and extracranial efficacy, not only eliciting responses in existing brain metastases but also helping prevent new ones. These results likely translate into significant improvements in quality of life, function, and survival for patients, and reduce the well-documented health economic burden associated with the development of CNS metastases.
Newer-generation ALK inhibitors, such as brigatinib and lorlatinib, also show CNS activity and are currently in phase 3 trials. It will be important to assess their effects on brain metastases to help determine their role in managing patients with ALK-positive NSCLC.
Alesha A. Thai, MD, is with the Peter MacCallum Cancer Centre in Melbourne and Benjamin J. Solomon, MD, is with the University of Melbourne. Dr. Thai disclosed no conflicts of interest. Dr. Solomon disclosed advisory board relationships with Roche-Genentech, Pfizer, Novartis, AstraZeneca, Merck, and Bristol-Myers Squibb. These comments are from their editorial (Ann Oncol. 2018 Sep 18. doi: 10.1093/annonc/mdy415).
The results of the phase 3 ALEX trial provide strong rationale for the first-line use of alectinib in patients with non–small cell lung cancer (NSCLC) harboring anaplastic lymphoma kinase (ALK) gene rearrangements.
Alectinib showed robust evidence of intracranial and extracranial efficacy, not only eliciting responses in existing brain metastases but also helping prevent new ones. These results likely translate into significant improvements in quality of life, function, and survival for patients, and reduce the well-documented health economic burden associated with the development of CNS metastases.
Newer-generation ALK inhibitors, such as brigatinib and lorlatinib, also show CNS activity and are currently in phase 3 trials. It will be important to assess their effects on brain metastases to help determine their role in managing patients with ALK-positive NSCLC.
Alesha A. Thai, MD, is with the Peter MacCallum Cancer Centre in Melbourne and Benjamin J. Solomon, MD, is with the University of Melbourne. Dr. Thai disclosed no conflicts of interest. Dr. Solomon disclosed advisory board relationships with Roche-Genentech, Pfizer, Novartis, AstraZeneca, Merck, and Bristol-Myers Squibb. These comments are from their editorial (Ann Oncol. 2018 Sep 18. doi: 10.1093/annonc/mdy415).
The results of the phase 3 ALEX trial provide strong rationale for the first-line use of alectinib in patients with non–small cell lung cancer (NSCLC) harboring anaplastic lymphoma kinase (ALK) gene rearrangements.
Alectinib showed robust evidence of intracranial and extracranial efficacy, not only eliciting responses in existing brain metastases but also helping prevent new ones. These results likely translate into significant improvements in quality of life, function, and survival for patients, and reduce the well-documented health economic burden associated with the development of CNS metastases.
Newer-generation ALK inhibitors, such as brigatinib and lorlatinib, also show CNS activity and are currently in phase 3 trials. It will be important to assess their effects on brain metastases to help determine their role in managing patients with ALK-positive NSCLC.
Alesha A. Thai, MD, is with the Peter MacCallum Cancer Centre in Melbourne and Benjamin J. Solomon, MD, is with the University of Melbourne. Dr. Thai disclosed no conflicts of interest. Dr. Solomon disclosed advisory board relationships with Roche-Genentech, Pfizer, Novartis, AstraZeneca, Merck, and Bristol-Myers Squibb. These comments are from their editorial (Ann Oncol. 2018 Sep 18. doi: 10.1093/annonc/mdy415).
For patients with treatment-naive anaplastic lymphoma kinase–positive (ALK+) non–small cell lung cancer (NSCLC), twice-daily oral treatment with alectinib (600 mg) was associated with significantly greater activity in the CNS and significantly delayed CNS progression, compared with crizotinib (200 mg), based on secondary analyses from the pivotal phase 3 ALEX trial.
Time to CNS progression was significantly longer with alectinib versus crizotinib (hazard ratio, 0.18; 95% confidence interval, 0.09-0.36) regardless of whether patients had asymptomatic baseline CNS metastases or a prior history of radiotherapy. For patients with baseline asymptomatic CNS metastases, the 12-month cumulative incidence of CNS progression was 16% with alectinib versus 58.3% with crizotinib. Among patients without asymptomatic CNS metastases at baseline, these rates were 4.6% versus 31.5%, respectively.
The findings “consolidate alectinib as the standard of care for untreated, advanced ALK+ NSCLC, irrespective of the presence or absence of baseline CNS metastases,” Shirish M. Gadgeel, MD, of the University of Michigan, Ann Arbor, and his associates wrote in Annals of Oncology.
ALEX was the first study of an ALK inhibitor to include a prospective, standardized intention-to-treat analysis of CNS lesions, regardless of whether patients had these lesions at baseline. All patients underwent brain imaging at baseline and every 8 weeks thereafter. In the primary analysis of 303 patients, alectinib significantly improved progression-free survival in patients with and without baseline CNS disease and showed a significantly higher intracranial overall response rate, irrespective of whether patients had previously received radiotherapy.
Based on these results, National Comprehensive Cancer Network guidelines were updated to include a category 1 recommendation for the first-line use of alectinib in patients with ALK+ NSCLC.
The current analysis focused on CNS efficacy. In all, 122 patients had CNS metastases at baseline. Progression-free survival was similar regardless of whether patients had these lesions (HR, 0.40; 95% CI, 0.25-0.64) or not (HR, 0.51; 95% CI, 0.33-0.80; P = .36). History of radiotherapy also did not significantly affect overall CNS response or progression-free survival.
“Our data are in agreement with a pooled analysis of alectinib phase 2 trials, which demonstrated that central nervous system efficacy of alectinib is maintained regardless of radiotherapy history in crizotinib-pretreated patients,” the investigators wrote.
Because ALEX excluded patients with symptomatic CNS disease, its effects in this population remain unclear, they noted. “ALEX data strongly suggest that in asymptomatic patients, treating CNS metastases with alectinib alone may result in a reduced or delayed need for local CNS treatment.”
F. Hoffman-La Roche funded the study. Dr. Gadgeel reported honoraria and consultancy fees from Roche/Genentech, ARIAD Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, and Pfizer.
SOURCE: Gadgeel SM et al. Ann Oncol. 2018 Sep 12. doi: 10.1093/annonc/mdy405.
For patients with treatment-naive anaplastic lymphoma kinase–positive (ALK+) non–small cell lung cancer (NSCLC), twice-daily oral treatment with alectinib (600 mg) was associated with significantly greater activity in the CNS and significantly delayed CNS progression, compared with crizotinib (200 mg), based on secondary analyses from the pivotal phase 3 ALEX trial.
Time to CNS progression was significantly longer with alectinib versus crizotinib (hazard ratio, 0.18; 95% confidence interval, 0.09-0.36) regardless of whether patients had asymptomatic baseline CNS metastases or a prior history of radiotherapy. For patients with baseline asymptomatic CNS metastases, the 12-month cumulative incidence of CNS progression was 16% with alectinib versus 58.3% with crizotinib. Among patients without asymptomatic CNS metastases at baseline, these rates were 4.6% versus 31.5%, respectively.
The findings “consolidate alectinib as the standard of care for untreated, advanced ALK+ NSCLC, irrespective of the presence or absence of baseline CNS metastases,” Shirish M. Gadgeel, MD, of the University of Michigan, Ann Arbor, and his associates wrote in Annals of Oncology.
ALEX was the first study of an ALK inhibitor to include a prospective, standardized intention-to-treat analysis of CNS lesions, regardless of whether patients had these lesions at baseline. All patients underwent brain imaging at baseline and every 8 weeks thereafter. In the primary analysis of 303 patients, alectinib significantly improved progression-free survival in patients with and without baseline CNS disease and showed a significantly higher intracranial overall response rate, irrespective of whether patients had previously received radiotherapy.
Based on these results, National Comprehensive Cancer Network guidelines were updated to include a category 1 recommendation for the first-line use of alectinib in patients with ALK+ NSCLC.
The current analysis focused on CNS efficacy. In all, 122 patients had CNS metastases at baseline. Progression-free survival was similar regardless of whether patients had these lesions (HR, 0.40; 95% CI, 0.25-0.64) or not (HR, 0.51; 95% CI, 0.33-0.80; P = .36). History of radiotherapy also did not significantly affect overall CNS response or progression-free survival.
“Our data are in agreement with a pooled analysis of alectinib phase 2 trials, which demonstrated that central nervous system efficacy of alectinib is maintained regardless of radiotherapy history in crizotinib-pretreated patients,” the investigators wrote.
Because ALEX excluded patients with symptomatic CNS disease, its effects in this population remain unclear, they noted. “ALEX data strongly suggest that in asymptomatic patients, treating CNS metastases with alectinib alone may result in a reduced or delayed need for local CNS treatment.”
F. Hoffman-La Roche funded the study. Dr. Gadgeel reported honoraria and consultancy fees from Roche/Genentech, ARIAD Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, and Pfizer.
SOURCE: Gadgeel SM et al. Ann Oncol. 2018 Sep 12. doi: 10.1093/annonc/mdy405.
FROM ANNALS OF ONCOLOGY
Key clinical point: Alectinib showed superior CNS activity and significantly delayed CNS progression over crizotinib in patients with treatment-naive anaplastic lymphoma kinase–positive non–small cell lung cancer.
Major finding: Time to CNS progression was significantly longer with alectinib versus crizotinib (hazard ratio, 0.18; 95% confidence interval, 0.09-0.36) and was comparable among patients with and without baseline CNS metastases or prior radiotherapy.
Study details: A phase 3 trial of 303 patients receiving alectinib (600 mg) or crizotinib (250 mg) twice daily.
Disclosures: F. Hoffman-La Roche funded the study. Dr. Gadgeel disclosed honoraria and consultancy fees from Roche/Genentech, ARIAD Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, and Pfizer.
Source: Gadgeel SM et al. Ann Oncol. 2018 Sep 12. doi: 10.1093/annonc/mdy405.
Guideline: Early screening warranted if family history of nonhereditary colorectal cancer
New consensus guidelines strongly recommend screening colonoscopy for individuals who have at least one first-degree relative with nonhereditary colorectal cancer or advanced adenoma.
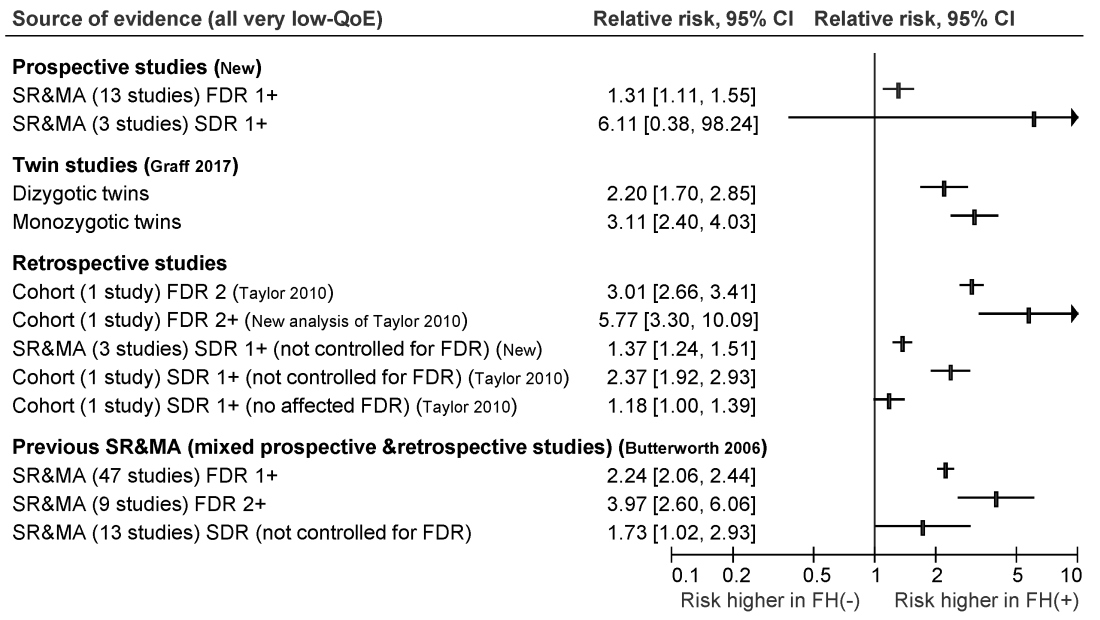
Published in the November issue of Gastroenterology, the guideline cites moderate-quality evidence for this recommendation and reserves fecal immunochemical testing for individuals who refuse colonoscopy, are at increased risk for complications, or face barriers accessing the procedure.
Most colorectal cancer screening guidelines have focused on average-risk individuals or those at highest risk because of heritable germline mutations. However, hereditary syndromes comprise only about 5% of colorectal cancers, noted Desmond Leddin, MB, MSc, FRCPC, FRCPI, of the University of Limerick, Ireland, and David A. Lieberman, MD, AGAF, FACG, of Oregon Health and Science University, Portland, with their associates from the Canadian Association of Gastroenterology Banff Consensus.
To develop the guideline, they searched the literature for studies of family history and colorectal cancer risk apart from hereditary Lynch syndrome, familial adenomatous polyposis, attenuated familial adenomatous polyposis, MUTYH-associated polyposis, Peutz-Jeghers syndrome, juvenile polyposis syndrome, Cowden syndrome, serrated (hyperplastic) polyposis syndrome, hereditary pancreatic cancer, and hereditary gastric cancer.
The ensuant guideline cites two new systematic reviews and meta-analyses of 16 prospective studies, as well as one twin study, four retrospective cohort studies, one new systematic review of retrospective studies, and three prior systematic reviews and meta-analyses. The authors note that this is the first guideline to use the GRADE (Grading of Recommendation Assessment, Development and Evaluation) approach to make screening recommendations for individuals who have a family history of nonhereditary colorectal cancer or advanced adenoma.
For those with one first-degree relative with colorectal cancer, the guideline recommends screening colonoscopy or fecal immunochemical testing beginning at age 40-50 years, or 10 years before the age of diagnosis of the first-degree relative, whichever is earlier. The authors recommend spacing subsequent screening colonoscopies by 5-10 years and spacing fecal immunochemical testing by 1-2 years. They offer the same recommendation for individuals with one or more first-degree relatives with confirmed advanced adenoma.
For individuals whose family history includes at least two first-degree relatives with colorectal cancer, the guideline recommends an initial screening colonoscopy at age 40, or 10 years earlier than the age of earliest-diagnosed first-degree relative, whichever is earlier. Screenings should occur every 5 years.
For persons with at least one second-degree relative with colorectal cancer, the guideline authors strongly recommend screening starting at age 50 with tests and intervals based on guidelines for average-risk individuals. Their recommendation is the same for individuals with at least one first-degree relative with nonadvanced adenoma or a polyp of unknown histology.
Given the low-quality evidence supporting most of these recommendations, the guideline calls for well designed observational studies to better quantify the risk of colorectal cancer among individuals with a family history of nonheritable disease. Studies should especially focus on the optimal age of first screening and appropriate screening intervals, the guideline authors wrote. Also, they call for randomized controlled trials to assess whether colonoscopy, fecal immunochemical testing, or fecal occult blood screening might significantly reduce long-term risk for colorectal cancer and improve survival in this population.
Merck provided unrestricted funding for the work. Dr. Leddin reported having no conflicts of interest. Dr. Lieberman and several coauthors disclosed financial relationships with companies other than Merck. One coauthor disclosed advisory and consulting relationships with Merck.
SOURCE: Leddin D et al. Gastroenterology. 2018 Aug 16. doi: 10.1053/j.gastro.2018.08.017.
New consensus guidelines strongly recommend screening colonoscopy for individuals who have at least one first-degree relative with nonhereditary colorectal cancer or advanced adenoma.
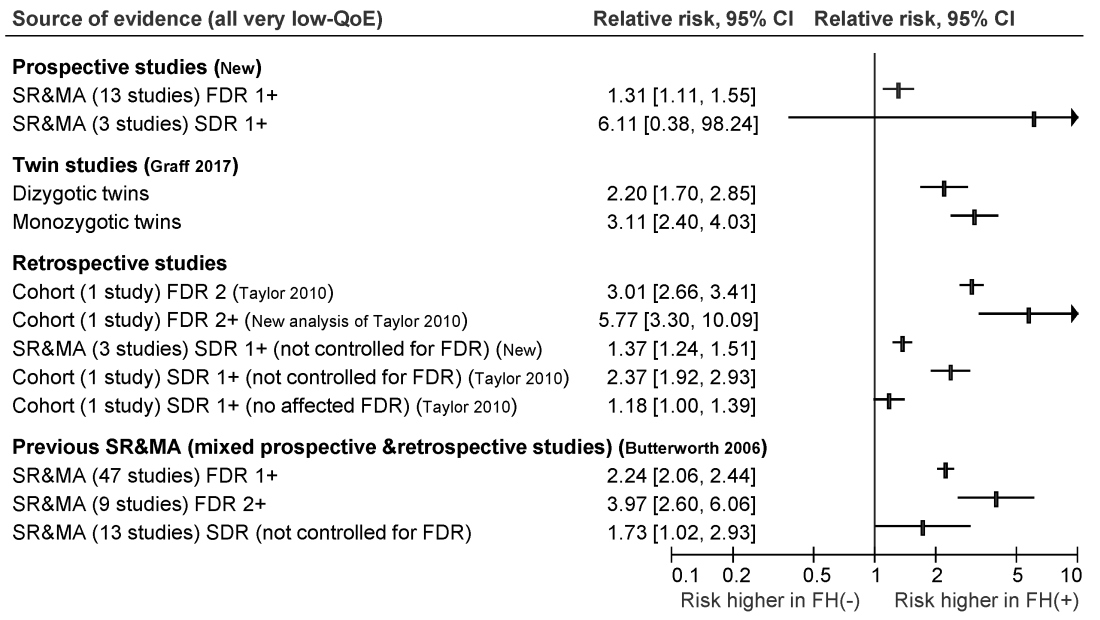
Published in the November issue of Gastroenterology, the guideline cites moderate-quality evidence for this recommendation and reserves fecal immunochemical testing for individuals who refuse colonoscopy, are at increased risk for complications, or face barriers accessing the procedure.
Most colorectal cancer screening guidelines have focused on average-risk individuals or those at highest risk because of heritable germline mutations. However, hereditary syndromes comprise only about 5% of colorectal cancers, noted Desmond Leddin, MB, MSc, FRCPC, FRCPI, of the University of Limerick, Ireland, and David A. Lieberman, MD, AGAF, FACG, of Oregon Health and Science University, Portland, with their associates from the Canadian Association of Gastroenterology Banff Consensus.
To develop the guideline, they searched the literature for studies of family history and colorectal cancer risk apart from hereditary Lynch syndrome, familial adenomatous polyposis, attenuated familial adenomatous polyposis, MUTYH-associated polyposis, Peutz-Jeghers syndrome, juvenile polyposis syndrome, Cowden syndrome, serrated (hyperplastic) polyposis syndrome, hereditary pancreatic cancer, and hereditary gastric cancer.
The ensuant guideline cites two new systematic reviews and meta-analyses of 16 prospective studies, as well as one twin study, four retrospective cohort studies, one new systematic review of retrospective studies, and three prior systematic reviews and meta-analyses. The authors note that this is the first guideline to use the GRADE (Grading of Recommendation Assessment, Development and Evaluation) approach to make screening recommendations for individuals who have a family history of nonhereditary colorectal cancer or advanced adenoma.
For those with one first-degree relative with colorectal cancer, the guideline recommends screening colonoscopy or fecal immunochemical testing beginning at age 40-50 years, or 10 years before the age of diagnosis of the first-degree relative, whichever is earlier. The authors recommend spacing subsequent screening colonoscopies by 5-10 years and spacing fecal immunochemical testing by 1-2 years. They offer the same recommendation for individuals with one or more first-degree relatives with confirmed advanced adenoma.
For individuals whose family history includes at least two first-degree relatives with colorectal cancer, the guideline recommends an initial screening colonoscopy at age 40, or 10 years earlier than the age of earliest-diagnosed first-degree relative, whichever is earlier. Screenings should occur every 5 years.
For persons with at least one second-degree relative with colorectal cancer, the guideline authors strongly recommend screening starting at age 50 with tests and intervals based on guidelines for average-risk individuals. Their recommendation is the same for individuals with at least one first-degree relative with nonadvanced adenoma or a polyp of unknown histology.
Given the low-quality evidence supporting most of these recommendations, the guideline calls for well designed observational studies to better quantify the risk of colorectal cancer among individuals with a family history of nonheritable disease. Studies should especially focus on the optimal age of first screening and appropriate screening intervals, the guideline authors wrote. Also, they call for randomized controlled trials to assess whether colonoscopy, fecal immunochemical testing, or fecal occult blood screening might significantly reduce long-term risk for colorectal cancer and improve survival in this population.
Merck provided unrestricted funding for the work. Dr. Leddin reported having no conflicts of interest. Dr. Lieberman and several coauthors disclosed financial relationships with companies other than Merck. One coauthor disclosed advisory and consulting relationships with Merck.
SOURCE: Leddin D et al. Gastroenterology. 2018 Aug 16. doi: 10.1053/j.gastro.2018.08.017.
New consensus guidelines strongly recommend screening colonoscopy for individuals who have at least one first-degree relative with nonhereditary colorectal cancer or advanced adenoma.
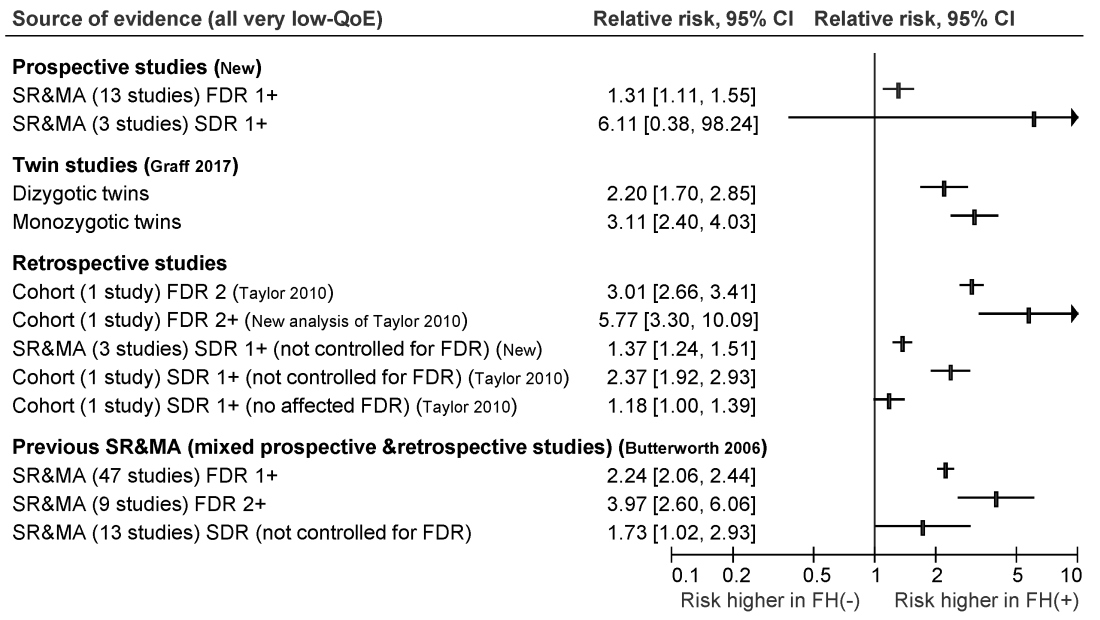
Published in the November issue of Gastroenterology, the guideline cites moderate-quality evidence for this recommendation and reserves fecal immunochemical testing for individuals who refuse colonoscopy, are at increased risk for complications, or face barriers accessing the procedure.
Most colorectal cancer screening guidelines have focused on average-risk individuals or those at highest risk because of heritable germline mutations. However, hereditary syndromes comprise only about 5% of colorectal cancers, noted Desmond Leddin, MB, MSc, FRCPC, FRCPI, of the University of Limerick, Ireland, and David A. Lieberman, MD, AGAF, FACG, of Oregon Health and Science University, Portland, with their associates from the Canadian Association of Gastroenterology Banff Consensus.
To develop the guideline, they searched the literature for studies of family history and colorectal cancer risk apart from hereditary Lynch syndrome, familial adenomatous polyposis, attenuated familial adenomatous polyposis, MUTYH-associated polyposis, Peutz-Jeghers syndrome, juvenile polyposis syndrome, Cowden syndrome, serrated (hyperplastic) polyposis syndrome, hereditary pancreatic cancer, and hereditary gastric cancer.
The ensuant guideline cites two new systematic reviews and meta-analyses of 16 prospective studies, as well as one twin study, four retrospective cohort studies, one new systematic review of retrospective studies, and three prior systematic reviews and meta-analyses. The authors note that this is the first guideline to use the GRADE (Grading of Recommendation Assessment, Development and Evaluation) approach to make screening recommendations for individuals who have a family history of nonhereditary colorectal cancer or advanced adenoma.
For those with one first-degree relative with colorectal cancer, the guideline recommends screening colonoscopy or fecal immunochemical testing beginning at age 40-50 years, or 10 years before the age of diagnosis of the first-degree relative, whichever is earlier. The authors recommend spacing subsequent screening colonoscopies by 5-10 years and spacing fecal immunochemical testing by 1-2 years. They offer the same recommendation for individuals with one or more first-degree relatives with confirmed advanced adenoma.
For individuals whose family history includes at least two first-degree relatives with colorectal cancer, the guideline recommends an initial screening colonoscopy at age 40, or 10 years earlier than the age of earliest-diagnosed first-degree relative, whichever is earlier. Screenings should occur every 5 years.
For persons with at least one second-degree relative with colorectal cancer, the guideline authors strongly recommend screening starting at age 50 with tests and intervals based on guidelines for average-risk individuals. Their recommendation is the same for individuals with at least one first-degree relative with nonadvanced adenoma or a polyp of unknown histology.
Given the low-quality evidence supporting most of these recommendations, the guideline calls for well designed observational studies to better quantify the risk of colorectal cancer among individuals with a family history of nonheritable disease. Studies should especially focus on the optimal age of first screening and appropriate screening intervals, the guideline authors wrote. Also, they call for randomized controlled trials to assess whether colonoscopy, fecal immunochemical testing, or fecal occult blood screening might significantly reduce long-term risk for colorectal cancer and improve survival in this population.
Merck provided unrestricted funding for the work. Dr. Leddin reported having no conflicts of interest. Dr. Lieberman and several coauthors disclosed financial relationships with companies other than Merck. One coauthor disclosed advisory and consulting relationships with Merck.
SOURCE: Leddin D et al. Gastroenterology. 2018 Aug 16. doi: 10.1053/j.gastro.2018.08.017.
FROM GASTROENTEROLOGY
Admission eosinopenia predicted severe CDI outcomes
For patients with even in the absence of hypotension and tachycardia, researchers wrote in JAMA Surgery.
“In animal models, peripheral eosinopenia is a biologically plausible predictive factor for adverse outcomes, and human data from this study indicate that this frequent addition to an admission complete blood cell count is an inexpensive, widely available risk index in the treatment of C. difficile infection,” wrote Audrey S. Kulaylat, MD, of Penn State University, Hershey, and her associates.
In their cohort study of 2,065 patients admitted to two tertiary referral centers with C. difficile infection, undetectable eosinophil counts at hospital admission were associated with significantly increased odds of in-hospital mortality in both a training dataset (odds ratio, 2.01; 95% confidence interval, 1.08-3.73; P = .03) and a validation dataset (OR, 2.26; 95% CI, 1.33-3.83; P = .002). Undetectable eosinophil counts also were associated with elevated odds of severe disease requiring intensive care, vasopressor use, and emergency total colectomy. Besides eosinopenia, significant predictors of mortality included having more comorbidities and lower systolic blood pressure at admission. Strikingly, when patients had no initial hypotension or tachycardia, an undetectable eosinophil count was the only identifiable predictor of in-hospital death (OR, 5.76; 95% CI, 1.99-16.64). An elevated white blood cell count was not a significant predictor of mortality in this subgroup.
Dr. Kulaylat and her associates are studying the microbiome in C. difficile infection. Their work has identified a host immune reaction marked by an “exaggerated inflammasome response” and peripheral eosinopenia, they explained. Two recent murine models have produced similar results.
Admission eosinophil counts “allow for an immediate assessment of mortality risk at admission that is inexpensive and part of a differential for a standard complete blood count available at any hospital,” they concluded. They are now prospectively evaluating a prognostic score for C. difficile infection that includes eosinopenia and other easily discernible admission factors. The National Institutes of Health supported the work. The researchers reported having no conflicts of interest.
SOURCE: Kulaylat AS et al. JAMA Surg. 2018 Sep 12. doi: 10.1001/jamasurg.2018.3174.
For patients with even in the absence of hypotension and tachycardia, researchers wrote in JAMA Surgery.
“In animal models, peripheral eosinopenia is a biologically plausible predictive factor for adverse outcomes, and human data from this study indicate that this frequent addition to an admission complete blood cell count is an inexpensive, widely available risk index in the treatment of C. difficile infection,” wrote Audrey S. Kulaylat, MD, of Penn State University, Hershey, and her associates.
In their cohort study of 2,065 patients admitted to two tertiary referral centers with C. difficile infection, undetectable eosinophil counts at hospital admission were associated with significantly increased odds of in-hospital mortality in both a training dataset (odds ratio, 2.01; 95% confidence interval, 1.08-3.73; P = .03) and a validation dataset (OR, 2.26; 95% CI, 1.33-3.83; P = .002). Undetectable eosinophil counts also were associated with elevated odds of severe disease requiring intensive care, vasopressor use, and emergency total colectomy. Besides eosinopenia, significant predictors of mortality included having more comorbidities and lower systolic blood pressure at admission. Strikingly, when patients had no initial hypotension or tachycardia, an undetectable eosinophil count was the only identifiable predictor of in-hospital death (OR, 5.76; 95% CI, 1.99-16.64). An elevated white blood cell count was not a significant predictor of mortality in this subgroup.
Dr. Kulaylat and her associates are studying the microbiome in C. difficile infection. Their work has identified a host immune reaction marked by an “exaggerated inflammasome response” and peripheral eosinopenia, they explained. Two recent murine models have produced similar results.
Admission eosinophil counts “allow for an immediate assessment of mortality risk at admission that is inexpensive and part of a differential for a standard complete blood count available at any hospital,” they concluded. They are now prospectively evaluating a prognostic score for C. difficile infection that includes eosinopenia and other easily discernible admission factors. The National Institutes of Health supported the work. The researchers reported having no conflicts of interest.
SOURCE: Kulaylat AS et al. JAMA Surg. 2018 Sep 12. doi: 10.1001/jamasurg.2018.3174.
For patients with even in the absence of hypotension and tachycardia, researchers wrote in JAMA Surgery.
“In animal models, peripheral eosinopenia is a biologically plausible predictive factor for adverse outcomes, and human data from this study indicate that this frequent addition to an admission complete blood cell count is an inexpensive, widely available risk index in the treatment of C. difficile infection,” wrote Audrey S. Kulaylat, MD, of Penn State University, Hershey, and her associates.
In their cohort study of 2,065 patients admitted to two tertiary referral centers with C. difficile infection, undetectable eosinophil counts at hospital admission were associated with significantly increased odds of in-hospital mortality in both a training dataset (odds ratio, 2.01; 95% confidence interval, 1.08-3.73; P = .03) and a validation dataset (OR, 2.26; 95% CI, 1.33-3.83; P = .002). Undetectable eosinophil counts also were associated with elevated odds of severe disease requiring intensive care, vasopressor use, and emergency total colectomy. Besides eosinopenia, significant predictors of mortality included having more comorbidities and lower systolic blood pressure at admission. Strikingly, when patients had no initial hypotension or tachycardia, an undetectable eosinophil count was the only identifiable predictor of in-hospital death (OR, 5.76; 95% CI, 1.99-16.64). An elevated white blood cell count was not a significant predictor of mortality in this subgroup.
Dr. Kulaylat and her associates are studying the microbiome in C. difficile infection. Their work has identified a host immune reaction marked by an “exaggerated inflammasome response” and peripheral eosinopenia, they explained. Two recent murine models have produced similar results.
Admission eosinophil counts “allow for an immediate assessment of mortality risk at admission that is inexpensive and part of a differential for a standard complete blood count available at any hospital,” they concluded. They are now prospectively evaluating a prognostic score for C. difficile infection that includes eosinopenia and other easily discernible admission factors. The National Institutes of Health supported the work. The researchers reported having no conflicts of interest.
SOURCE: Kulaylat AS et al. JAMA Surg. 2018 Sep 12. doi: 10.1001/jamasurg.2018.3174.
FROM JAMA SURGERY
Key clinical point: Undetectable peripheral eosinophils predicted severe outcomes in patients admitted with Clostridium difficile infection.
Major finding: In the training and validation datasets, odds of in-hospital mortality were 2.01 (95% CI, 1.08-3.73) and 2.26 (95% CI, 1.33-3.83), respectively.
Study details: Two-hospital cohort study of 2,065 patients admitted with C. difficile infection.
Disclosures: The National Institutes of Health supported the work. The researchers reported having no conflicts of interest.
Source: Kulaylat A et al. JAMA Surg. 2018 Sep 12. doi: 10.1001/jamasurg.2018.3174.
JACOB: Dual HER2 blockade falls short in metastatic gastric cancer
Dual HER2 blockade did not significantly improve overall survival, compared with standard treatment of metastatic HER2-positive gastric cancer, according to final readouts from the international, double-blind JACOB trial.
After a median of 24.4 months of follow-up, median overall survival times were 17.5 months among patients who received pertuzumab in addition to standard trastuzumab therapy plus chemotherapy versus 14.2 months in the control arm (hazard ratio, 0.84; 95% confidence interval, 0.71-1.00; P = .057). The pertuzumab arm also had a higher incidence of moderate to severe diarrhea and more interruptions and dose modifications of chemotherapy, perhaps because of overlapping toxicities, wrote Josep Tabernero, MD. of Vall d’Hebron University Hospital and Centro de Investigación Biomedica en Red Cancer, Barcelona, and his colleagues. The report is in Lancet Oncology.
Gastric cancer remains the fifth most common cancer globally and the third most common cause of cancer-related death. For patients whose metastatic gastric tumors express high levels of HER2, targeted trastuzumab therapy can significantly improve overall survival when added to standard chemotherapy with capecitabine or fluorouracil plus a platinum-based drug. Pertuzumab binds to a HER2 receptor protein epitope different from trastuzumab, and combination treatment with trastuzumab plus pertuzumab has been found to significantly increase overall survival for patients with HER2-positive breast cancer. Although gastric cancer displays more HER2 heterogeneity than does breast cancer, Dr. Tabernero and his associates hypothesized that dual HER2 blockade might show a similar result.
Accordingly, in the phase 3 JACOB trial, 780 patients with HER2-positive metastatic gastric or gastroesophageal junction cancer were randomly assigned to receive treatment every 3 weeks with intravenous pertuzumab (840 mg) or placebo in addition to intravenous trastuzumab (8 mg/kg loading dose, then 6 mg/kg) plus either oral capecitabine (1,000 mg/m2 twice daily), intravenous cisplatin (80 mg/m2), or intravenous 5-fluorouracil (800 mg/m2; 120-hour continuous infusion).
The two groups had similar rates of serious adverse events, most commonly diarrhea. Grade 3 or worse diarrhea affected 13% of pertuzumab patients versus 6% of control patients. There were no treatment-related deaths in the pertuzumab group and seven (2%) in the control group. “The study was not powered to assess efficacy endpoints in clinical and biomarker subgroups and there was no multiplicity control for subgroup analyses, so we cannot assess which patients might be more likely to benefit from pertuzumab treatment,” the investigators wrote. They recommended further evaluating other first-line treatments for advanced HER2-positive gastric cancer, predictors of benefit from dual HER2 blockade, and the best chemotherapy backbone for anti-HER2 regimens.
F. Hoffman-La Roche Ltd. sponsored the work. Dr. Tabernero disclosed advisory board relationships with Genentech/Roche, Roche, Sanofi, Symphogen, and other pharmaceutical companies outside the submitted work. Three coinvestigators also disclosed ties to Roche and several other pharmaceutical companies and one reported owning stock in F. Hoffmann-La Roche. The remaining two investigators reported having no conflicts of interest.
SOURCE: Taberno J, et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30481-9.
The negative results of this trial might reflect intratumoral heterogeneity of HER2-overexpressing gastric tumors or the demographic or clinical effects of variables such as ethnicity, tumor site, histology, or chemotherapy backbone, said Giandomenico Roviello, MD and Daniele Generali, MD.
HER2-positive metastatic breast cancer is a heterogeneous disease, the experts emphasized. They noted prior studies in which approximately 40% of HER2-amplified gastric tumors showed heterogeneity ranging from 10% to nearly 100% of tested cells.
HER2 signaling pathways also might differ between gastric and breast cancer, the experts continued. They called for studies of predictive biomarkers for clinically efficacious HER2 blockade in these patient populations.
Dr. Giandomenico Roviello is with Referral Cancer Center of Basilicata, Rionero in Vulture, Potenza, Italy. Dr. Daniele Generali is with Azienda Socio-Sanitaria Territoriale in Cremona, Italy, and the University of Trieste, Italy. They reported having no conflicts of interest. These comments are from their editorial (Lancet Oncol. 2018 Sep 11. doi: 10.1016/ S1470-2045[18]30481-9).
The negative results of this trial might reflect intratumoral heterogeneity of HER2-overexpressing gastric tumors or the demographic or clinical effects of variables such as ethnicity, tumor site, histology, or chemotherapy backbone, said Giandomenico Roviello, MD and Daniele Generali, MD.
HER2-positive metastatic breast cancer is a heterogeneous disease, the experts emphasized. They noted prior studies in which approximately 40% of HER2-amplified gastric tumors showed heterogeneity ranging from 10% to nearly 100% of tested cells.
HER2 signaling pathways also might differ between gastric and breast cancer, the experts continued. They called for studies of predictive biomarkers for clinically efficacious HER2 blockade in these patient populations.
Dr. Giandomenico Roviello is with Referral Cancer Center of Basilicata, Rionero in Vulture, Potenza, Italy. Dr. Daniele Generali is with Azienda Socio-Sanitaria Territoriale in Cremona, Italy, and the University of Trieste, Italy. They reported having no conflicts of interest. These comments are from their editorial (Lancet Oncol. 2018 Sep 11. doi: 10.1016/ S1470-2045[18]30481-9).
The negative results of this trial might reflect intratumoral heterogeneity of HER2-overexpressing gastric tumors or the demographic or clinical effects of variables such as ethnicity, tumor site, histology, or chemotherapy backbone, said Giandomenico Roviello, MD and Daniele Generali, MD.
HER2-positive metastatic breast cancer is a heterogeneous disease, the experts emphasized. They noted prior studies in which approximately 40% of HER2-amplified gastric tumors showed heterogeneity ranging from 10% to nearly 100% of tested cells.
HER2 signaling pathways also might differ between gastric and breast cancer, the experts continued. They called for studies of predictive biomarkers for clinically efficacious HER2 blockade in these patient populations.
Dr. Giandomenico Roviello is with Referral Cancer Center of Basilicata, Rionero in Vulture, Potenza, Italy. Dr. Daniele Generali is with Azienda Socio-Sanitaria Territoriale in Cremona, Italy, and the University of Trieste, Italy. They reported having no conflicts of interest. These comments are from their editorial (Lancet Oncol. 2018 Sep 11. doi: 10.1016/ S1470-2045[18]30481-9).
Dual HER2 blockade did not significantly improve overall survival, compared with standard treatment of metastatic HER2-positive gastric cancer, according to final readouts from the international, double-blind JACOB trial.
After a median of 24.4 months of follow-up, median overall survival times were 17.5 months among patients who received pertuzumab in addition to standard trastuzumab therapy plus chemotherapy versus 14.2 months in the control arm (hazard ratio, 0.84; 95% confidence interval, 0.71-1.00; P = .057). The pertuzumab arm also had a higher incidence of moderate to severe diarrhea and more interruptions and dose modifications of chemotherapy, perhaps because of overlapping toxicities, wrote Josep Tabernero, MD. of Vall d’Hebron University Hospital and Centro de Investigación Biomedica en Red Cancer, Barcelona, and his colleagues. The report is in Lancet Oncology.
Gastric cancer remains the fifth most common cancer globally and the third most common cause of cancer-related death. For patients whose metastatic gastric tumors express high levels of HER2, targeted trastuzumab therapy can significantly improve overall survival when added to standard chemotherapy with capecitabine or fluorouracil plus a platinum-based drug. Pertuzumab binds to a HER2 receptor protein epitope different from trastuzumab, and combination treatment with trastuzumab plus pertuzumab has been found to significantly increase overall survival for patients with HER2-positive breast cancer. Although gastric cancer displays more HER2 heterogeneity than does breast cancer, Dr. Tabernero and his associates hypothesized that dual HER2 blockade might show a similar result.
Accordingly, in the phase 3 JACOB trial, 780 patients with HER2-positive metastatic gastric or gastroesophageal junction cancer were randomly assigned to receive treatment every 3 weeks with intravenous pertuzumab (840 mg) or placebo in addition to intravenous trastuzumab (8 mg/kg loading dose, then 6 mg/kg) plus either oral capecitabine (1,000 mg/m2 twice daily), intravenous cisplatin (80 mg/m2), or intravenous 5-fluorouracil (800 mg/m2; 120-hour continuous infusion).
The two groups had similar rates of serious adverse events, most commonly diarrhea. Grade 3 or worse diarrhea affected 13% of pertuzumab patients versus 6% of control patients. There were no treatment-related deaths in the pertuzumab group and seven (2%) in the control group. “The study was not powered to assess efficacy endpoints in clinical and biomarker subgroups and there was no multiplicity control for subgroup analyses, so we cannot assess which patients might be more likely to benefit from pertuzumab treatment,” the investigators wrote. They recommended further evaluating other first-line treatments for advanced HER2-positive gastric cancer, predictors of benefit from dual HER2 blockade, and the best chemotherapy backbone for anti-HER2 regimens.
F. Hoffman-La Roche Ltd. sponsored the work. Dr. Tabernero disclosed advisory board relationships with Genentech/Roche, Roche, Sanofi, Symphogen, and other pharmaceutical companies outside the submitted work. Three coinvestigators also disclosed ties to Roche and several other pharmaceutical companies and one reported owning stock in F. Hoffmann-La Roche. The remaining two investigators reported having no conflicts of interest.
SOURCE: Taberno J, et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30481-9.
Dual HER2 blockade did not significantly improve overall survival, compared with standard treatment of metastatic HER2-positive gastric cancer, according to final readouts from the international, double-blind JACOB trial.
After a median of 24.4 months of follow-up, median overall survival times were 17.5 months among patients who received pertuzumab in addition to standard trastuzumab therapy plus chemotherapy versus 14.2 months in the control arm (hazard ratio, 0.84; 95% confidence interval, 0.71-1.00; P = .057). The pertuzumab arm also had a higher incidence of moderate to severe diarrhea and more interruptions and dose modifications of chemotherapy, perhaps because of overlapping toxicities, wrote Josep Tabernero, MD. of Vall d’Hebron University Hospital and Centro de Investigación Biomedica en Red Cancer, Barcelona, and his colleagues. The report is in Lancet Oncology.
Gastric cancer remains the fifth most common cancer globally and the third most common cause of cancer-related death. For patients whose metastatic gastric tumors express high levels of HER2, targeted trastuzumab therapy can significantly improve overall survival when added to standard chemotherapy with capecitabine or fluorouracil plus a platinum-based drug. Pertuzumab binds to a HER2 receptor protein epitope different from trastuzumab, and combination treatment with trastuzumab plus pertuzumab has been found to significantly increase overall survival for patients with HER2-positive breast cancer. Although gastric cancer displays more HER2 heterogeneity than does breast cancer, Dr. Tabernero and his associates hypothesized that dual HER2 blockade might show a similar result.
Accordingly, in the phase 3 JACOB trial, 780 patients with HER2-positive metastatic gastric or gastroesophageal junction cancer were randomly assigned to receive treatment every 3 weeks with intravenous pertuzumab (840 mg) or placebo in addition to intravenous trastuzumab (8 mg/kg loading dose, then 6 mg/kg) plus either oral capecitabine (1,000 mg/m2 twice daily), intravenous cisplatin (80 mg/m2), or intravenous 5-fluorouracil (800 mg/m2; 120-hour continuous infusion).
The two groups had similar rates of serious adverse events, most commonly diarrhea. Grade 3 or worse diarrhea affected 13% of pertuzumab patients versus 6% of control patients. There were no treatment-related deaths in the pertuzumab group and seven (2%) in the control group. “The study was not powered to assess efficacy endpoints in clinical and biomarker subgroups and there was no multiplicity control for subgroup analyses, so we cannot assess which patients might be more likely to benefit from pertuzumab treatment,” the investigators wrote. They recommended further evaluating other first-line treatments for advanced HER2-positive gastric cancer, predictors of benefit from dual HER2 blockade, and the best chemotherapy backbone for anti-HER2 regimens.
F. Hoffman-La Roche Ltd. sponsored the work. Dr. Tabernero disclosed advisory board relationships with Genentech/Roche, Roche, Sanofi, Symphogen, and other pharmaceutical companies outside the submitted work. Three coinvestigators also disclosed ties to Roche and several other pharmaceutical companies and one reported owning stock in F. Hoffmann-La Roche. The remaining two investigators reported having no conflicts of interest.
SOURCE: Taberno J, et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30481-9.
FROM LANCET ONCOLOGY
Key clinical point: Dual HER2 blockade did not significantly improve overall survival in patients with metastatic gastric cancer.
Major finding: Over a median follow-up of 24.4 months, median overall survival was 17.5 months in the intervention arm (pertuzumab in addition to standard trastuzumab therapy plus chemotherapy) versus 14.2 months in the control arm (hazard ratio, 0.84; 95% CI, 0.71 to 1.00; P = .057).
Study details: Double-blind, placebo-controlled, randomized, multicenter trial of 780 adults with HER2-positive metastatic gastric or gastro-esophageal junction cancer.
Disclosures: F. Hoffmann-La Roche Ltd. sponsored the work. Dr. Tabernero disclosed advisory board relationships with Genentech/Roche, Roche, Sanofi, Symphogen, and other pharmaceutical companies outside the submitted work. Three coinvestigators also disclosed ties to Roche and several other pharmaceutical companies and one reported owning stock in F. Hoffmann-La Roche. The remaining two investigators reported having no conflicts of interest.
Source: Taberno J et al. Lancet Oncol. 2018 Sep 11. doi: 10.1016/S1470-2045(18)30481-9.
Commentary: Composite risk, not age, is key for timing first colorectal cancer screening
The American Cancer Society’s recent recommendation to lower the age of first screening for colorectal cancer to 45 years does not reflect clear knowledge of risks versus benefits, experts wrote in a recent commentary.
“In the big picture, [the question of whether to start screening at 45 versus 50 years] seems relatively unimportant compared with using individual patient risk for advanced neoplasia in practical, feasible models” that are geared toward adherence, efficiency, and cost-efficacy, wrote Thomas F. Imperiale, MD, of Indiana University, Indianapolis, and his associates. The commentary is in the October issue of Clinical Gastroenterology and Hepatology.
Tailoring age of first screening on an individual level, based on other risk factors and patient preferences, might improve uptake and benefit-risk ratios, balance, they argued.
Rates of colorectal cancer in persons under age 50 years rose by about 22% between 2000 and 2013. However, estimates for the most recent birth cohorts have wide confidence intervals, “indicating imprecision and uncertainty that this trend will continue,” the experts wrote. Furthermore, the absolute risk of colorectal cancer among individuals younger than 50 years has risen only slightly, from 5.9 cases per 100,000 population to 7.2 cases per 100,000 population. “[This] small increase in incidence may represent a true increase or could be due to increased use of colonoscopy in general, and specifically, for diagnosis or high-risk screening of first-degree relatives of persons with colorectal cancer,” the experts wrote.
Implementing the new recommendation could detect earlier-stage (curable) colorectal cancer “in a youthful and productive age group that may be sandwiched between raising children and caring for aging parents,” they continued. Earlier detection could reduce mortality and reduce the costs of treating a disease that often exceeds $100,000 per person annually.
However, the recommendation was based on a modeling study that assumed 100% adherence. In reality, uptake among 45- to 49-year-olds might be 15%-20%, and “who actually shows up for screening could make or break this recommendation,” the experts said. If younger individuals who underwent screening tended to have few risk factors for colorectal cancer, then the new recommendation would lead to many false positives and unnecessary colonoscopies, with the associated fallout of emotional harm and wasted health care resources, they added.
Population-level studies have identified age as the strongest predictor of colorectal cancer, but age “does not perform as well” at patient level, the experts said. They emphasized the role of other risk factors, such as male sex, having a first-degree relative with colorectal cancer, high body mass index, metabolic syndrome, cigarette smoking, diet, adherence to screening, and use of aspirin, nonsteroidal anti-inflammatory drugs, and hormone therapy. “The goal for providers and health systems is to determine whether and how to change screening practice and policy, and how to incorporate this new recommendation into practice, a necessarily complex process that requires knowing patient risk, patient preferences, and the long-term balance of benefits and burdens,” they concluded (Clin Gastroenterol Hepatol. 2018 Aug 13. doi: 10.1016/j.cgh.2018.08.023).
Dr. Imperiale and coauthor Charles J. Kahi, MD, MS, had no disclosures. Coauthor Douglas K. Rex, MD, disclosed ties to Aries Pharmaceutical, Cosmo Pharmaceuticals, Boston Scientific, Sebela, Medtronic, EndoAid Ltd, Olympus, Paion, Braintree, and Medivators. He also chairs the U.S. Multi-Society Task Force on Colorectal Cancer.
* This story was updated on 10/16/2018.
The American Cancer Society’s recent recommendation to lower the age of first screening for colorectal cancer to 45 years does not reflect clear knowledge of risks versus benefits, experts wrote in a recent commentary.
“In the big picture, [the question of whether to start screening at 45 versus 50 years] seems relatively unimportant compared with using individual patient risk for advanced neoplasia in practical, feasible models” that are geared toward adherence, efficiency, and cost-efficacy, wrote Thomas F. Imperiale, MD, of Indiana University, Indianapolis, and his associates. The commentary is in the October issue of Clinical Gastroenterology and Hepatology.
Tailoring age of first screening on an individual level, based on other risk factors and patient preferences, might improve uptake and benefit-risk ratios, balance, they argued.
Rates of colorectal cancer in persons under age 50 years rose by about 22% between 2000 and 2013. However, estimates for the most recent birth cohorts have wide confidence intervals, “indicating imprecision and uncertainty that this trend will continue,” the experts wrote. Furthermore, the absolute risk of colorectal cancer among individuals younger than 50 years has risen only slightly, from 5.9 cases per 100,000 population to 7.2 cases per 100,000 population. “[This] small increase in incidence may represent a true increase or could be due to increased use of colonoscopy in general, and specifically, for diagnosis or high-risk screening of first-degree relatives of persons with colorectal cancer,” the experts wrote.
Implementing the new recommendation could detect earlier-stage (curable) colorectal cancer “in a youthful and productive age group that may be sandwiched between raising children and caring for aging parents,” they continued. Earlier detection could reduce mortality and reduce the costs of treating a disease that often exceeds $100,000 per person annually.
However, the recommendation was based on a modeling study that assumed 100% adherence. In reality, uptake among 45- to 49-year-olds might be 15%-20%, and “who actually shows up for screening could make or break this recommendation,” the experts said. If younger individuals who underwent screening tended to have few risk factors for colorectal cancer, then the new recommendation would lead to many false positives and unnecessary colonoscopies, with the associated fallout of emotional harm and wasted health care resources, they added.
Population-level studies have identified age as the strongest predictor of colorectal cancer, but age “does not perform as well” at patient level, the experts said. They emphasized the role of other risk factors, such as male sex, having a first-degree relative with colorectal cancer, high body mass index, metabolic syndrome, cigarette smoking, diet, adherence to screening, and use of aspirin, nonsteroidal anti-inflammatory drugs, and hormone therapy. “The goal for providers and health systems is to determine whether and how to change screening practice and policy, and how to incorporate this new recommendation into practice, a necessarily complex process that requires knowing patient risk, patient preferences, and the long-term balance of benefits and burdens,” they concluded (Clin Gastroenterol Hepatol. 2018 Aug 13. doi: 10.1016/j.cgh.2018.08.023).
Dr. Imperiale and coauthor Charles J. Kahi, MD, MS, had no disclosures. Coauthor Douglas K. Rex, MD, disclosed ties to Aries Pharmaceutical, Cosmo Pharmaceuticals, Boston Scientific, Sebela, Medtronic, EndoAid Ltd, Olympus, Paion, Braintree, and Medivators. He also chairs the U.S. Multi-Society Task Force on Colorectal Cancer.
* This story was updated on 10/16/2018.
The American Cancer Society’s recent recommendation to lower the age of first screening for colorectal cancer to 45 years does not reflect clear knowledge of risks versus benefits, experts wrote in a recent commentary.
“In the big picture, [the question of whether to start screening at 45 versus 50 years] seems relatively unimportant compared with using individual patient risk for advanced neoplasia in practical, feasible models” that are geared toward adherence, efficiency, and cost-efficacy, wrote Thomas F. Imperiale, MD, of Indiana University, Indianapolis, and his associates. The commentary is in the October issue of Clinical Gastroenterology and Hepatology.
Tailoring age of first screening on an individual level, based on other risk factors and patient preferences, might improve uptake and benefit-risk ratios, balance, they argued.
Rates of colorectal cancer in persons under age 50 years rose by about 22% between 2000 and 2013. However, estimates for the most recent birth cohorts have wide confidence intervals, “indicating imprecision and uncertainty that this trend will continue,” the experts wrote. Furthermore, the absolute risk of colorectal cancer among individuals younger than 50 years has risen only slightly, from 5.9 cases per 100,000 population to 7.2 cases per 100,000 population. “[This] small increase in incidence may represent a true increase or could be due to increased use of colonoscopy in general, and specifically, for diagnosis or high-risk screening of first-degree relatives of persons with colorectal cancer,” the experts wrote.
Implementing the new recommendation could detect earlier-stage (curable) colorectal cancer “in a youthful and productive age group that may be sandwiched between raising children and caring for aging parents,” they continued. Earlier detection could reduce mortality and reduce the costs of treating a disease that often exceeds $100,000 per person annually.
However, the recommendation was based on a modeling study that assumed 100% adherence. In reality, uptake among 45- to 49-year-olds might be 15%-20%, and “who actually shows up for screening could make or break this recommendation,” the experts said. If younger individuals who underwent screening tended to have few risk factors for colorectal cancer, then the new recommendation would lead to many false positives and unnecessary colonoscopies, with the associated fallout of emotional harm and wasted health care resources, they added.
Population-level studies have identified age as the strongest predictor of colorectal cancer, but age “does not perform as well” at patient level, the experts said. They emphasized the role of other risk factors, such as male sex, having a first-degree relative with colorectal cancer, high body mass index, metabolic syndrome, cigarette smoking, diet, adherence to screening, and use of aspirin, nonsteroidal anti-inflammatory drugs, and hormone therapy. “The goal for providers and health systems is to determine whether and how to change screening practice and policy, and how to incorporate this new recommendation into practice, a necessarily complex process that requires knowing patient risk, patient preferences, and the long-term balance of benefits and burdens,” they concluded (Clin Gastroenterol Hepatol. 2018 Aug 13. doi: 10.1016/j.cgh.2018.08.023).
Dr. Imperiale and coauthor Charles J. Kahi, MD, MS, had no disclosures. Coauthor Douglas K. Rex, MD, disclosed ties to Aries Pharmaceutical, Cosmo Pharmaceuticals, Boston Scientific, Sebela, Medtronic, EndoAid Ltd, Olympus, Paion, Braintree, and Medivators. He also chairs the U.S. Multi-Society Task Force on Colorectal Cancer.
* This story was updated on 10/16/2018.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Proinflammatory diet linked to colorectal cancer testing positive for Fusobacterium nucleatum
Diets promoting colonic inflammation were associated with a greater risk of colorectal carcinomas containing Fusobacterium nucleatum bacteria, according to a report in the October issue of Clinical Gastroenterology and Hepatology.
Courtesy American Gastroenterological Association
Proinflammatory diets were not linked to heightened risk for colon cancers without these bacteria, reported Li Liu, MD, PhD, of Dana-Farber Cancer Institute and Harvard Medical School, Boston. “These findings indicate that diet-induced intestinal inflammation alters the gut microbiome to contribute to colorectal carcinogenesis,” they wrote. “Nutritional interventions might be used in precision medicine and cancer prevention.”
Intestinal inflammation, a risk factor for colorectal cancer, is associated with high levels of circulating interleukin 6, C-reactive protein, and tumor necrosis factor–receptor superfamily member 1B. Colonic inflammation impairs the mucosal barrier and alters immune cell responses, which affects the composition of colonic microbiota. Among these, F. nucleatum is known to potentiate colorectal tumors and is associated with proximal tumor location, other tumor features, and cancer progression and chemoresistance.
For the study, the investigators examined self-reported data from more than 124,000 individuals followed for 28 years as part of the Nurses’ Health Study and the Health Professionals Follow-Up Study. They calculated average dietary patterns based on the empiric dietary inflammatory pattern (EDIP) score, which sums weighted intake scores for 18 foods (such as red and processed meat, coffee, tea, and leafy green or dark yellow vegetables) that are known to affect plasma levels of interleukin 6, C-reactive protein, tumor necrosis factor–receptor superfamily member 1B, and tumor necrosis factor alpha–receptor 2. A higher EDIP score denotes a more inflammatory diet.
During the 28-year follow-up period, 951 individuals developed colorectal carcinomas that were tested with a polymerase chain reaction assay for F. nucleatum DNA. A total of 115 tumors tested positive for F. nucleatum. After the researchers controlled for potential confounders, individuals whose EDIP scores were in the highest tertile were significantly more likely to develop F. nucleatum–positive colorectal cancer than were those who scored in the lowest tertile (adjusted hazard ratio, 1.63; 95% confidence interval, 1.03 to 2.58; P = .03). This differential association “appeared to be stronger in proximal colon cancer than in distal colon and rectal cancer,” the researchers said.
More than 90% of individuals in this study were non-Hispanic white, the researchers noted. Tumor tissue was not available from all cases of colorectal cancer and a fairly small number of cases tested positive for tumor F. nucleatum. Nonetheless, the findings suggest that an inflammatory diet could help amplify gut microbiota involved in tumorigenesis, they said. Pending confirmatory studies, they recommended an anti-inflammatory diet with high intake of green leafy vegetables, dark yellow vegetables, coffee, and tea, and with low intake of red meat, processed meat, refined grain, and sugary beverages. They also recommended studying whether F. nucleatum tumor or stool tests could help personalize dietary interventions.
Funders included the National Institutes of Health, Dana Farber Harvard Cancer, Project P. Fund for Colorectal Cancer Research, Friends of the Dana-Farber Cancer Institute, Bennett Family Fund, the Entertainment Industry Foundation, and American Association for Cancer Research, National Natural Science Foundation of China, Chinese Scholarship Council, Huazhong University of Science and Technology, and others. Dr. Liu had no disclosures. One coinvestigator disclosed ties to Genentech/Roche, Lilly, Sanofi, Bayer, and several other biomedical companies.
SOURCE: Liu L et al. Clin Gastroenterol Hepatol. 2018 Apr 24. doi: 10.1016/j.cgh.2018.04.030.
The underlying reasons colorectal cancer (CRC) develops are unknown, but they likely include a complex interaction between genetics and environmental exposures. Recent studies have highlighted important links between diet, the intestinal microbiota, and CRC development and progression.
Liu et al. used the Nurses’ Health Study and Health Professionals Follow-Up Study cohorts to extend our understanding of the relationship between diet, the intestinal microbiota, and CRC. They utilized validated food frequency questionnaires obtained every 4 years and formalin-fixed paraffin embedded CRC tissue samples collected from 951 individuals. They calculated an empiric dietary inflammatory pattern (EDIP) score, which correlates components of the diet with plasma inflammatory markers. After adjusting for confounders, they found high EDIP scores were significantly associated with Fusobacterium nucleatum–positive CRC, but not with F. nucleatum–negative CRC. In addition, they demonstrated this association was stronger for proximal compared with distal CRC. Their findings suggest an inflammatory diet may interact with the intestinal microbiota to promote the development of CRC and they provide a preliminary recommendation to minimize intake of potentially harmful foods (i.e., red meat, processed meat, refined grains, etc.). Despite the intriguing results, the authors do recognize limitations including the small number of cases with F. nucleatum present (n = 115) and the homogeneous cohort (90% non-Hispanic whites), which may limit generalizability.
As clinicians, we should continue strongly advocating for CRC screening and, based on these findings, may consider dietary recommendations to reduce intake of potentially harmful foods. Further research will be needed to confirm these findings in additional cohorts and to clarify the molecular interactions between dietary components, intestinal microbiota, and development of CRC.
Rajesh R. Shah, MD, is assistant professor of gastroenterology, department of internal medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
The underlying reasons colorectal cancer (CRC) develops are unknown, but they likely include a complex interaction between genetics and environmental exposures. Recent studies have highlighted important links between diet, the intestinal microbiota, and CRC development and progression.
Liu et al. used the Nurses’ Health Study and Health Professionals Follow-Up Study cohorts to extend our understanding of the relationship between diet, the intestinal microbiota, and CRC. They utilized validated food frequency questionnaires obtained every 4 years and formalin-fixed paraffin embedded CRC tissue samples collected from 951 individuals. They calculated an empiric dietary inflammatory pattern (EDIP) score, which correlates components of the diet with plasma inflammatory markers. After adjusting for confounders, they found high EDIP scores were significantly associated with Fusobacterium nucleatum–positive CRC, but not with F. nucleatum–negative CRC. In addition, they demonstrated this association was stronger for proximal compared with distal CRC. Their findings suggest an inflammatory diet may interact with the intestinal microbiota to promote the development of CRC and they provide a preliminary recommendation to minimize intake of potentially harmful foods (i.e., red meat, processed meat, refined grains, etc.). Despite the intriguing results, the authors do recognize limitations including the small number of cases with F. nucleatum present (n = 115) and the homogeneous cohort (90% non-Hispanic whites), which may limit generalizability.
As clinicians, we should continue strongly advocating for CRC screening and, based on these findings, may consider dietary recommendations to reduce intake of potentially harmful foods. Further research will be needed to confirm these findings in additional cohorts and to clarify the molecular interactions between dietary components, intestinal microbiota, and development of CRC.
Rajesh R. Shah, MD, is assistant professor of gastroenterology, department of internal medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
The underlying reasons colorectal cancer (CRC) develops are unknown, but they likely include a complex interaction between genetics and environmental exposures. Recent studies have highlighted important links between diet, the intestinal microbiota, and CRC development and progression.
Liu et al. used the Nurses’ Health Study and Health Professionals Follow-Up Study cohorts to extend our understanding of the relationship between diet, the intestinal microbiota, and CRC. They utilized validated food frequency questionnaires obtained every 4 years and formalin-fixed paraffin embedded CRC tissue samples collected from 951 individuals. They calculated an empiric dietary inflammatory pattern (EDIP) score, which correlates components of the diet with plasma inflammatory markers. After adjusting for confounders, they found high EDIP scores were significantly associated with Fusobacterium nucleatum–positive CRC, but not with F. nucleatum–negative CRC. In addition, they demonstrated this association was stronger for proximal compared with distal CRC. Their findings suggest an inflammatory diet may interact with the intestinal microbiota to promote the development of CRC and they provide a preliminary recommendation to minimize intake of potentially harmful foods (i.e., red meat, processed meat, refined grains, etc.). Despite the intriguing results, the authors do recognize limitations including the small number of cases with F. nucleatum present (n = 115) and the homogeneous cohort (90% non-Hispanic whites), which may limit generalizability.
As clinicians, we should continue strongly advocating for CRC screening and, based on these findings, may consider dietary recommendations to reduce intake of potentially harmful foods. Further research will be needed to confirm these findings in additional cohorts and to clarify the molecular interactions between dietary components, intestinal microbiota, and development of CRC.
Rajesh R. Shah, MD, is assistant professor of gastroenterology, department of internal medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Diets promoting colonic inflammation were associated with a greater risk of colorectal carcinomas containing Fusobacterium nucleatum bacteria, according to a report in the October issue of Clinical Gastroenterology and Hepatology.
Courtesy American Gastroenterological Association
Proinflammatory diets were not linked to heightened risk for colon cancers without these bacteria, reported Li Liu, MD, PhD, of Dana-Farber Cancer Institute and Harvard Medical School, Boston. “These findings indicate that diet-induced intestinal inflammation alters the gut microbiome to contribute to colorectal carcinogenesis,” they wrote. “Nutritional interventions might be used in precision medicine and cancer prevention.”
Intestinal inflammation, a risk factor for colorectal cancer, is associated with high levels of circulating interleukin 6, C-reactive protein, and tumor necrosis factor–receptor superfamily member 1B. Colonic inflammation impairs the mucosal barrier and alters immune cell responses, which affects the composition of colonic microbiota. Among these, F. nucleatum is known to potentiate colorectal tumors and is associated with proximal tumor location, other tumor features, and cancer progression and chemoresistance.
For the study, the investigators examined self-reported data from more than 124,000 individuals followed for 28 years as part of the Nurses’ Health Study and the Health Professionals Follow-Up Study. They calculated average dietary patterns based on the empiric dietary inflammatory pattern (EDIP) score, which sums weighted intake scores for 18 foods (such as red and processed meat, coffee, tea, and leafy green or dark yellow vegetables) that are known to affect plasma levels of interleukin 6, C-reactive protein, tumor necrosis factor–receptor superfamily member 1B, and tumor necrosis factor alpha–receptor 2. A higher EDIP score denotes a more inflammatory diet.
During the 28-year follow-up period, 951 individuals developed colorectal carcinomas that were tested with a polymerase chain reaction assay for F. nucleatum DNA. A total of 115 tumors tested positive for F. nucleatum. After the researchers controlled for potential confounders, individuals whose EDIP scores were in the highest tertile were significantly more likely to develop F. nucleatum–positive colorectal cancer than were those who scored in the lowest tertile (adjusted hazard ratio, 1.63; 95% confidence interval, 1.03 to 2.58; P = .03). This differential association “appeared to be stronger in proximal colon cancer than in distal colon and rectal cancer,” the researchers said.
More than 90% of individuals in this study were non-Hispanic white, the researchers noted. Tumor tissue was not available from all cases of colorectal cancer and a fairly small number of cases tested positive for tumor F. nucleatum. Nonetheless, the findings suggest that an inflammatory diet could help amplify gut microbiota involved in tumorigenesis, they said. Pending confirmatory studies, they recommended an anti-inflammatory diet with high intake of green leafy vegetables, dark yellow vegetables, coffee, and tea, and with low intake of red meat, processed meat, refined grain, and sugary beverages. They also recommended studying whether F. nucleatum tumor or stool tests could help personalize dietary interventions.
Funders included the National Institutes of Health, Dana Farber Harvard Cancer, Project P. Fund for Colorectal Cancer Research, Friends of the Dana-Farber Cancer Institute, Bennett Family Fund, the Entertainment Industry Foundation, and American Association for Cancer Research, National Natural Science Foundation of China, Chinese Scholarship Council, Huazhong University of Science and Technology, and others. Dr. Liu had no disclosures. One coinvestigator disclosed ties to Genentech/Roche, Lilly, Sanofi, Bayer, and several other biomedical companies.
SOURCE: Liu L et al. Clin Gastroenterol Hepatol. 2018 Apr 24. doi: 10.1016/j.cgh.2018.04.030.
Diets promoting colonic inflammation were associated with a greater risk of colorectal carcinomas containing Fusobacterium nucleatum bacteria, according to a report in the October issue of Clinical Gastroenterology and Hepatology.
Courtesy American Gastroenterological Association
Proinflammatory diets were not linked to heightened risk for colon cancers without these bacteria, reported Li Liu, MD, PhD, of Dana-Farber Cancer Institute and Harvard Medical School, Boston. “These findings indicate that diet-induced intestinal inflammation alters the gut microbiome to contribute to colorectal carcinogenesis,” they wrote. “Nutritional interventions might be used in precision medicine and cancer prevention.”
Intestinal inflammation, a risk factor for colorectal cancer, is associated with high levels of circulating interleukin 6, C-reactive protein, and tumor necrosis factor–receptor superfamily member 1B. Colonic inflammation impairs the mucosal barrier and alters immune cell responses, which affects the composition of colonic microbiota. Among these, F. nucleatum is known to potentiate colorectal tumors and is associated with proximal tumor location, other tumor features, and cancer progression and chemoresistance.
For the study, the investigators examined self-reported data from more than 124,000 individuals followed for 28 years as part of the Nurses’ Health Study and the Health Professionals Follow-Up Study. They calculated average dietary patterns based on the empiric dietary inflammatory pattern (EDIP) score, which sums weighted intake scores for 18 foods (such as red and processed meat, coffee, tea, and leafy green or dark yellow vegetables) that are known to affect plasma levels of interleukin 6, C-reactive protein, tumor necrosis factor–receptor superfamily member 1B, and tumor necrosis factor alpha–receptor 2. A higher EDIP score denotes a more inflammatory diet.
During the 28-year follow-up period, 951 individuals developed colorectal carcinomas that were tested with a polymerase chain reaction assay for F. nucleatum DNA. A total of 115 tumors tested positive for F. nucleatum. After the researchers controlled for potential confounders, individuals whose EDIP scores were in the highest tertile were significantly more likely to develop F. nucleatum–positive colorectal cancer than were those who scored in the lowest tertile (adjusted hazard ratio, 1.63; 95% confidence interval, 1.03 to 2.58; P = .03). This differential association “appeared to be stronger in proximal colon cancer than in distal colon and rectal cancer,” the researchers said.
More than 90% of individuals in this study were non-Hispanic white, the researchers noted. Tumor tissue was not available from all cases of colorectal cancer and a fairly small number of cases tested positive for tumor F. nucleatum. Nonetheless, the findings suggest that an inflammatory diet could help amplify gut microbiota involved in tumorigenesis, they said. Pending confirmatory studies, they recommended an anti-inflammatory diet with high intake of green leafy vegetables, dark yellow vegetables, coffee, and tea, and with low intake of red meat, processed meat, refined grain, and sugary beverages. They also recommended studying whether F. nucleatum tumor or stool tests could help personalize dietary interventions.
Funders included the National Institutes of Health, Dana Farber Harvard Cancer, Project P. Fund for Colorectal Cancer Research, Friends of the Dana-Farber Cancer Institute, Bennett Family Fund, the Entertainment Industry Foundation, and American Association for Cancer Research, National Natural Science Foundation of China, Chinese Scholarship Council, Huazhong University of Science and Technology, and others. Dr. Liu had no disclosures. One coinvestigator disclosed ties to Genentech/Roche, Lilly, Sanofi, Bayer, and several other biomedical companies.
SOURCE: Liu L et al. Clin Gastroenterol Hepatol. 2018 Apr 24. doi: 10.1016/j.cgh.2018.04.030.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A proinflammatory diet was associated with a significantly increased risk for colorectal cancer testing positive for Fusobacterium nucleatum.
Major finding: Dietary scores in the highest inflammatory tertile correlated with significantly increased risk (HR, 1.63; P = .03).
Study details: Longitudinal study of self-reported dietary patterns and cancers among 124,433 individuals with 28 years of follow-up.
Disclosures: Funders included the National Institutes of Health, Dana Farber Harvard Cancer, Project P. Fund for Colorectal Cancer Research, Friends of the Dana-Farber Cancer Institute, Bennett Family Fund, the Entertainment Industry Foundation, and American Association for Cancer Research, National Natural Science Foundation of China, Chinese Scholarship Council, Huazhong University of Science and Technology, and others. Dr. Liu had no disclosures. One coinvestigator disclosed ties to Genentech/Roche, Lilly, Sanofi, Bayer, and several other biomedical companies.
Source: Liu L et al. Clin Gastroenterol Hepatol. 2018 Apr 24. doi: 10.1016/j.cgh.2018.04.030.