User login
Anticoagulation Hub contains news and clinical review articles for physicians seeking the most up-to-date information on the rapidly evolving treatment options for preventing stroke, acute coronary events, deep vein thrombosis, and pulmonary embolism in at-risk patients. The Anticoagulation Hub is powered by Frontline Medical Communications.
New trials address unresolved issues in endovascular therapy for acute ischemic stroke
BALTIMORE – Endovascular therapy is a bedrock of acute ischemic stroke treatment, but some vexing issues remain unresolved, according to Joseph Broderick, MD, of the University of Cincinnati.
“We have learned a tremendous amount the last few years. We know that thrombectomy can work if initiated in patients within 6 hours of stroke onset with or without TPA [tissue plasminogen activator]. The question is what we don’t know,” Dr. Broderick said.
The good news is that clinical trials are underway or planned to address several of these issues, he said at the annual meeting of the American Neurological Association.
Mechanical thrombectomy beyond 6 hours
Whether the treatment window for thrombectomy can be safely extended in appropriately selected patients beyond 6 hours from onset is “one of the most important issues we face,” Dr. Broderick said.
Along with DEFUSE 3, the DWI or CTP Assessment With Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention (DAWN) trial will examine whether medical management that includes thrombectomy delivered up to 24 hours after AIS symptoms first appear will yield better clinical outcomes than medical management alone in appropriate patients.
The use of mechanical thrombectomy up to 12 hours after symptom development in AIS patients for whom intravenous TPA can’t be used or doesn’t work will be assessed in the Perfusion Imaging Selection of Ischemic Stroke Patients for Endovascular Therapy (POSITIVE) trial. The primary objective is to show less stroke-related disability and improved good functional outcomes, compared with those who receive best medical therapy.
The first Multicenter Randomized Clinical Trial of Endovascular Treatment in the Netherlands (MR CLEAN) trial, which used stent retrievers in almost all cases, demonstrated the benefit of endovascular therapy up to 6 hours after stroke onset in the proximal anterior circulation when used along with best medical therapy (N Engl J Med. 2015;372:11-20). The MR CLEAN LATE trial involving 500 patients will expand the time window up to 12 hours.
Triage of acute stroke patients
The triage of AIS patients before their arrival at the hospital also is an evolving emergency medical service issue. While the classic triage involving CT takes time, the use of scoring systems like the National Institutes of Health Stroke Scale and the Cincinnati Stroke Triage Assessment Tool, or telemedicine-based consultation, can be done faster and with less training.
Where the patient is taken first could be important. The RACECAT trial being conducted in the Catalan territory will compare transfer of acute stroke patients with suspected large-vessel occlusion to the closest local stroke center versus direct transfer to an endovascular stroke center.
Conscious sedation or general anesthesia
Some patients undergoing thrombectomy may be able to tolerate conscious sedation in place of general anesthesia. For these patients, cost-effectiveness becomes a dominant consideration. Several anesthesia trials are addressing the issue. The Sedation Versus Intubation for Endovascular Stroke Treatment (SIESTA) trial involving 150 German patients has been completed, but the findings have not been reported. The General or Local Anaesthesia in Intra-arterial Therapy (GOLIATH) trial is recruiting patients in the Netherlands, with a target enrollment of 128. Other trials are planned in China and Sweden, but recruitment has not started.
Thrombectomy alone
For patients with AIS caused by basilar artery occlusion, stroke specialists have wondered whether intra-arterial treatment, including thrombolysis and potentially thrombectomy, could be more effective than best medical therapy, including intravenous thrombolysis. The Basilar Artery International Cooperation Study (BASICS) in Europe and the BEST trial in China are two trials in the early stages of assessing this question.
A related issue is whether thrombectomy alone is better than intravenous TPA followed by thrombectomy. This issue is being addressed in another MR CLEAN trial that is designed to compare the two approaches in 500 patients randomized to one or the other treatment.
Other intravenous antithrombotic drugs
Another unresolved issue relates to the use of other antithrombotic medications delivered intravenously in combination with TPA. This could be the sole treatment strategy, or could be used in patients who also undergo endovascular thrombectomy. The Multi-Arm Optimization of Stroke Thrombolysis (MOST) trial will randomize patients to receive argatroban or eptifibatide along with TPA, or TPA alone, within 3 hours of stroke symptom onset. Endovascular therapy will be done as indicated.
Heparin use in endovascular therapy
The proper use of antithrombotics like heparin in patients treated with endovascular therapy is unclear. The MR CLEAN MED trial will assess the benefits of two doses of unfractionated heparin and aspirin alone or in combination in 1,500 patients with AIS who receive intra-arterial treatment for confirmed anterior circulation occlusion.
On the horizon
Whether neuroprotection can improve the outcome in patients who undergo embolectomy is unclear, and will be the subject of a trial in Canada that is not yet recruiting patients. Finally, the best way to manage blood pressure following embolectomy and reperfusion is also unclear.
Dr. Broderick had no relevant financial disclosures.
BALTIMORE – Endovascular therapy is a bedrock of acute ischemic stroke treatment, but some vexing issues remain unresolved, according to Joseph Broderick, MD, of the University of Cincinnati.
“We have learned a tremendous amount the last few years. We know that thrombectomy can work if initiated in patients within 6 hours of stroke onset with or without TPA [tissue plasminogen activator]. The question is what we don’t know,” Dr. Broderick said.
The good news is that clinical trials are underway or planned to address several of these issues, he said at the annual meeting of the American Neurological Association.
Mechanical thrombectomy beyond 6 hours
Whether the treatment window for thrombectomy can be safely extended in appropriately selected patients beyond 6 hours from onset is “one of the most important issues we face,” Dr. Broderick said.
Along with DEFUSE 3, the DWI or CTP Assessment With Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention (DAWN) trial will examine whether medical management that includes thrombectomy delivered up to 24 hours after AIS symptoms first appear will yield better clinical outcomes than medical management alone in appropriate patients.
The use of mechanical thrombectomy up to 12 hours after symptom development in AIS patients for whom intravenous TPA can’t be used or doesn’t work will be assessed in the Perfusion Imaging Selection of Ischemic Stroke Patients for Endovascular Therapy (POSITIVE) trial. The primary objective is to show less stroke-related disability and improved good functional outcomes, compared with those who receive best medical therapy.
The first Multicenter Randomized Clinical Trial of Endovascular Treatment in the Netherlands (MR CLEAN) trial, which used stent retrievers in almost all cases, demonstrated the benefit of endovascular therapy up to 6 hours after stroke onset in the proximal anterior circulation when used along with best medical therapy (N Engl J Med. 2015;372:11-20). The MR CLEAN LATE trial involving 500 patients will expand the time window up to 12 hours.
Triage of acute stroke patients
The triage of AIS patients before their arrival at the hospital also is an evolving emergency medical service issue. While the classic triage involving CT takes time, the use of scoring systems like the National Institutes of Health Stroke Scale and the Cincinnati Stroke Triage Assessment Tool, or telemedicine-based consultation, can be done faster and with less training.
Where the patient is taken first could be important. The RACECAT trial being conducted in the Catalan territory will compare transfer of acute stroke patients with suspected large-vessel occlusion to the closest local stroke center versus direct transfer to an endovascular stroke center.
Conscious sedation or general anesthesia
Some patients undergoing thrombectomy may be able to tolerate conscious sedation in place of general anesthesia. For these patients, cost-effectiveness becomes a dominant consideration. Several anesthesia trials are addressing the issue. The Sedation Versus Intubation for Endovascular Stroke Treatment (SIESTA) trial involving 150 German patients has been completed, but the findings have not been reported. The General or Local Anaesthesia in Intra-arterial Therapy (GOLIATH) trial is recruiting patients in the Netherlands, with a target enrollment of 128. Other trials are planned in China and Sweden, but recruitment has not started.
Thrombectomy alone
For patients with AIS caused by basilar artery occlusion, stroke specialists have wondered whether intra-arterial treatment, including thrombolysis and potentially thrombectomy, could be more effective than best medical therapy, including intravenous thrombolysis. The Basilar Artery International Cooperation Study (BASICS) in Europe and the BEST trial in China are two trials in the early stages of assessing this question.
A related issue is whether thrombectomy alone is better than intravenous TPA followed by thrombectomy. This issue is being addressed in another MR CLEAN trial that is designed to compare the two approaches in 500 patients randomized to one or the other treatment.
Other intravenous antithrombotic drugs
Another unresolved issue relates to the use of other antithrombotic medications delivered intravenously in combination with TPA. This could be the sole treatment strategy, or could be used in patients who also undergo endovascular thrombectomy. The Multi-Arm Optimization of Stroke Thrombolysis (MOST) trial will randomize patients to receive argatroban or eptifibatide along with TPA, or TPA alone, within 3 hours of stroke symptom onset. Endovascular therapy will be done as indicated.
Heparin use in endovascular therapy
The proper use of antithrombotics like heparin in patients treated with endovascular therapy is unclear. The MR CLEAN MED trial will assess the benefits of two doses of unfractionated heparin and aspirin alone or in combination in 1,500 patients with AIS who receive intra-arterial treatment for confirmed anterior circulation occlusion.
On the horizon
Whether neuroprotection can improve the outcome in patients who undergo embolectomy is unclear, and will be the subject of a trial in Canada that is not yet recruiting patients. Finally, the best way to manage blood pressure following embolectomy and reperfusion is also unclear.
Dr. Broderick had no relevant financial disclosures.
BALTIMORE – Endovascular therapy is a bedrock of acute ischemic stroke treatment, but some vexing issues remain unresolved, according to Joseph Broderick, MD, of the University of Cincinnati.
“We have learned a tremendous amount the last few years. We know that thrombectomy can work if initiated in patients within 6 hours of stroke onset with or without TPA [tissue plasminogen activator]. The question is what we don’t know,” Dr. Broderick said.
The good news is that clinical trials are underway or planned to address several of these issues, he said at the annual meeting of the American Neurological Association.
Mechanical thrombectomy beyond 6 hours
Whether the treatment window for thrombectomy can be safely extended in appropriately selected patients beyond 6 hours from onset is “one of the most important issues we face,” Dr. Broderick said.
Along with DEFUSE 3, the DWI or CTP Assessment With Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention (DAWN) trial will examine whether medical management that includes thrombectomy delivered up to 24 hours after AIS symptoms first appear will yield better clinical outcomes than medical management alone in appropriate patients.
The use of mechanical thrombectomy up to 12 hours after symptom development in AIS patients for whom intravenous TPA can’t be used or doesn’t work will be assessed in the Perfusion Imaging Selection of Ischemic Stroke Patients for Endovascular Therapy (POSITIVE) trial. The primary objective is to show less stroke-related disability and improved good functional outcomes, compared with those who receive best medical therapy.
The first Multicenter Randomized Clinical Trial of Endovascular Treatment in the Netherlands (MR CLEAN) trial, which used stent retrievers in almost all cases, demonstrated the benefit of endovascular therapy up to 6 hours after stroke onset in the proximal anterior circulation when used along with best medical therapy (N Engl J Med. 2015;372:11-20). The MR CLEAN LATE trial involving 500 patients will expand the time window up to 12 hours.
Triage of acute stroke patients
The triage of AIS patients before their arrival at the hospital also is an evolving emergency medical service issue. While the classic triage involving CT takes time, the use of scoring systems like the National Institutes of Health Stroke Scale and the Cincinnati Stroke Triage Assessment Tool, or telemedicine-based consultation, can be done faster and with less training.
Where the patient is taken first could be important. The RACECAT trial being conducted in the Catalan territory will compare transfer of acute stroke patients with suspected large-vessel occlusion to the closest local stroke center versus direct transfer to an endovascular stroke center.
Conscious sedation or general anesthesia
Some patients undergoing thrombectomy may be able to tolerate conscious sedation in place of general anesthesia. For these patients, cost-effectiveness becomes a dominant consideration. Several anesthesia trials are addressing the issue. The Sedation Versus Intubation for Endovascular Stroke Treatment (SIESTA) trial involving 150 German patients has been completed, but the findings have not been reported. The General or Local Anaesthesia in Intra-arterial Therapy (GOLIATH) trial is recruiting patients in the Netherlands, with a target enrollment of 128. Other trials are planned in China and Sweden, but recruitment has not started.
Thrombectomy alone
For patients with AIS caused by basilar artery occlusion, stroke specialists have wondered whether intra-arterial treatment, including thrombolysis and potentially thrombectomy, could be more effective than best medical therapy, including intravenous thrombolysis. The Basilar Artery International Cooperation Study (BASICS) in Europe and the BEST trial in China are two trials in the early stages of assessing this question.
A related issue is whether thrombectomy alone is better than intravenous TPA followed by thrombectomy. This issue is being addressed in another MR CLEAN trial that is designed to compare the two approaches in 500 patients randomized to one or the other treatment.
Other intravenous antithrombotic drugs
Another unresolved issue relates to the use of other antithrombotic medications delivered intravenously in combination with TPA. This could be the sole treatment strategy, or could be used in patients who also undergo endovascular thrombectomy. The Multi-Arm Optimization of Stroke Thrombolysis (MOST) trial will randomize patients to receive argatroban or eptifibatide along with TPA, or TPA alone, within 3 hours of stroke symptom onset. Endovascular therapy will be done as indicated.
Heparin use in endovascular therapy
The proper use of antithrombotics like heparin in patients treated with endovascular therapy is unclear. The MR CLEAN MED trial will assess the benefits of two doses of unfractionated heparin and aspirin alone or in combination in 1,500 patients with AIS who receive intra-arterial treatment for confirmed anterior circulation occlusion.
On the horizon
Whether neuroprotection can improve the outcome in patients who undergo embolectomy is unclear, and will be the subject of a trial in Canada that is not yet recruiting patients. Finally, the best way to manage blood pressure following embolectomy and reperfusion is also unclear.
Dr. Broderick had no relevant financial disclosures.
Ezetimibe’s ACS benefit centers on high-risk, post-CABG patients
ROME – Patients who have undergone coronary artery bypass surgery and who later have an acute coronary syndrome event gain the most from an aggressive lipid-lowering regimen, according to an exploratory analysis of data from more than 18,000 patients enrolled in the IMPROVE-IT trial that tested the incremental benefit from ezetimibe treatment when added to a statin.
Additional exploratory analyses further showed that high-risk acute coronary syndrome (ACS) patients without a history of coronary artery bypass grafting (CABG) also benefited from adding ezetimibe to a background regimen of simvastatin, but the benefit from adding ezetimibe completely disappeared in low-risk ACS patients, Alon Eisen, MD, said at the annual congress of the European Society of Cardiology.
‘The benefit of adding ezetimibe to a statin was enhanced in patients with prior CABG and in other high-risk patients with no prior CABG, supporting the use of more intensive lipid-lowering therapy in these high-risk patients,” said Dr. Eisen, a cardiologist at Brigham and Women’s Hospital in Boston. He also highlighted that ezetimibe is “a safe drug that is coming off patent.” Adding ezetimibe had a moderate effect on LDL cholesterol levels, cutting them from a median of 70 mg/dL in patients in the placebo arm to a median of 54 mg/dL in the group who received ezetimibe.
These results “show that if we pick the right patients, a very benign drug can have a great benefit,” said Eugene Braunwald, MD, a coinvestigator on the IMPROVE-IT trial and a collaborator with Dr. Eisen on the new analysis. The new findings “emphasize that the higher a patient’s risk, the more effect they get from cholesterol-lowering treatment,” said Dr. Braunwald, professor of medicine at Harvard University and a cardiologist at Brigham and Women’s Hospital, both in Boston.
The second exploratory analysis reported by Dr. Eisen looked at the more than 16,000 patients in IMPROVE-IT without history of CABG. The analysis applied a newly developed, nine-item formula for stratifying atherothrombotic risk (Circulation. 2016 July 26;134[4];304-13) to divide these patients into low-, intermediate- and high-risk subgroups. Patients in the high-risk subgroup (20% of the IMPROVE-IT subgroup) had a 6–percentage point reduction in their primary endpoint event rate with added ezetimibe treatment, while those at intermediate risk (31%) got a 2–percentage point decrease in endpoint events, and low-risk patients (49%) actually showed a small, less than 1–percentage point increase in endpoint events with added ezetimibe, Dr. Eisen reported.
IMPROVE-IT was funded by MERCK, the company that markets ezetimibe (Zetia). Dr. Eisen had no disclosures. Dr. Braunwald has been a consultant to Merck as well as to Bayer, Daiichi Sankyo, The Medicines Company, Novartis, and Sanofi.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
I suspect that the patients in IMPROVE-IT with a history of coronary artery bypass graft surgery were more likely than the other enrolled acute coronary syndrome patients to have more extensive and systemic atherosclerotic disease. Although coronary artery bypass addresses the most acute obstructions to coronary flow that exist at the time of surgery, the procedure does not cure the patient’s underlying vascular disease. We know that a substantial majority of coronary events occur in arteries that are not heavily stenosed.
Another important limitation to keep in mind about the IMPROVE-IT trial was that the background statin treatment all patients received was modest – 40 mg of simvastatin daily. In real-world practice, high-risk patients should go on the most potent statin regimen they can tolerate – ideally, 40 mg daily of rosuvastatin. The need for additional lipid-lowering interventions, with ezetimibe or other drugs, can then be considered as an add-on to aggressive statin therapy.
Richard A. Chazal, MD, is an invasive cardiologist and medical director of the Heart and Vascular Institute of Lee Memorial Health System in Fort Myers, Fla. He is also the current president of the American College of Cardiology. He had no disclosures. He made these comments in an interview.
I suspect that the patients in IMPROVE-IT with a history of coronary artery bypass graft surgery were more likely than the other enrolled acute coronary syndrome patients to have more extensive and systemic atherosclerotic disease. Although coronary artery bypass addresses the most acute obstructions to coronary flow that exist at the time of surgery, the procedure does not cure the patient’s underlying vascular disease. We know that a substantial majority of coronary events occur in arteries that are not heavily stenosed.
Another important limitation to keep in mind about the IMPROVE-IT trial was that the background statin treatment all patients received was modest – 40 mg of simvastatin daily. In real-world practice, high-risk patients should go on the most potent statin regimen they can tolerate – ideally, 40 mg daily of rosuvastatin. The need for additional lipid-lowering interventions, with ezetimibe or other drugs, can then be considered as an add-on to aggressive statin therapy.
Richard A. Chazal, MD, is an invasive cardiologist and medical director of the Heart and Vascular Institute of Lee Memorial Health System in Fort Myers, Fla. He is also the current president of the American College of Cardiology. He had no disclosures. He made these comments in an interview.
I suspect that the patients in IMPROVE-IT with a history of coronary artery bypass graft surgery were more likely than the other enrolled acute coronary syndrome patients to have more extensive and systemic atherosclerotic disease. Although coronary artery bypass addresses the most acute obstructions to coronary flow that exist at the time of surgery, the procedure does not cure the patient’s underlying vascular disease. We know that a substantial majority of coronary events occur in arteries that are not heavily stenosed.
Another important limitation to keep in mind about the IMPROVE-IT trial was that the background statin treatment all patients received was modest – 40 mg of simvastatin daily. In real-world practice, high-risk patients should go on the most potent statin regimen they can tolerate – ideally, 40 mg daily of rosuvastatin. The need for additional lipid-lowering interventions, with ezetimibe or other drugs, can then be considered as an add-on to aggressive statin therapy.
Richard A. Chazal, MD, is an invasive cardiologist and medical director of the Heart and Vascular Institute of Lee Memorial Health System in Fort Myers, Fla. He is also the current president of the American College of Cardiology. He had no disclosures. He made these comments in an interview.
ROME – Patients who have undergone coronary artery bypass surgery and who later have an acute coronary syndrome event gain the most from an aggressive lipid-lowering regimen, according to an exploratory analysis of data from more than 18,000 patients enrolled in the IMPROVE-IT trial that tested the incremental benefit from ezetimibe treatment when added to a statin.
Additional exploratory analyses further showed that high-risk acute coronary syndrome (ACS) patients without a history of coronary artery bypass grafting (CABG) also benefited from adding ezetimibe to a background regimen of simvastatin, but the benefit from adding ezetimibe completely disappeared in low-risk ACS patients, Alon Eisen, MD, said at the annual congress of the European Society of Cardiology.
‘The benefit of adding ezetimibe to a statin was enhanced in patients with prior CABG and in other high-risk patients with no prior CABG, supporting the use of more intensive lipid-lowering therapy in these high-risk patients,” said Dr. Eisen, a cardiologist at Brigham and Women’s Hospital in Boston. He also highlighted that ezetimibe is “a safe drug that is coming off patent.” Adding ezetimibe had a moderate effect on LDL cholesterol levels, cutting them from a median of 70 mg/dL in patients in the placebo arm to a median of 54 mg/dL in the group who received ezetimibe.
These results “show that if we pick the right patients, a very benign drug can have a great benefit,” said Eugene Braunwald, MD, a coinvestigator on the IMPROVE-IT trial and a collaborator with Dr. Eisen on the new analysis. The new findings “emphasize that the higher a patient’s risk, the more effect they get from cholesterol-lowering treatment,” said Dr. Braunwald, professor of medicine at Harvard University and a cardiologist at Brigham and Women’s Hospital, both in Boston.
The second exploratory analysis reported by Dr. Eisen looked at the more than 16,000 patients in IMPROVE-IT without history of CABG. The analysis applied a newly developed, nine-item formula for stratifying atherothrombotic risk (Circulation. 2016 July 26;134[4];304-13) to divide these patients into low-, intermediate- and high-risk subgroups. Patients in the high-risk subgroup (20% of the IMPROVE-IT subgroup) had a 6–percentage point reduction in their primary endpoint event rate with added ezetimibe treatment, while those at intermediate risk (31%) got a 2–percentage point decrease in endpoint events, and low-risk patients (49%) actually showed a small, less than 1–percentage point increase in endpoint events with added ezetimibe, Dr. Eisen reported.
IMPROVE-IT was funded by MERCK, the company that markets ezetimibe (Zetia). Dr. Eisen had no disclosures. Dr. Braunwald has been a consultant to Merck as well as to Bayer, Daiichi Sankyo, The Medicines Company, Novartis, and Sanofi.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
ROME – Patients who have undergone coronary artery bypass surgery and who later have an acute coronary syndrome event gain the most from an aggressive lipid-lowering regimen, according to an exploratory analysis of data from more than 18,000 patients enrolled in the IMPROVE-IT trial that tested the incremental benefit from ezetimibe treatment when added to a statin.
Additional exploratory analyses further showed that high-risk acute coronary syndrome (ACS) patients without a history of coronary artery bypass grafting (CABG) also benefited from adding ezetimibe to a background regimen of simvastatin, but the benefit from adding ezetimibe completely disappeared in low-risk ACS patients, Alon Eisen, MD, said at the annual congress of the European Society of Cardiology.
‘The benefit of adding ezetimibe to a statin was enhanced in patients with prior CABG and in other high-risk patients with no prior CABG, supporting the use of more intensive lipid-lowering therapy in these high-risk patients,” said Dr. Eisen, a cardiologist at Brigham and Women’s Hospital in Boston. He also highlighted that ezetimibe is “a safe drug that is coming off patent.” Adding ezetimibe had a moderate effect on LDL cholesterol levels, cutting them from a median of 70 mg/dL in patients in the placebo arm to a median of 54 mg/dL in the group who received ezetimibe.
These results “show that if we pick the right patients, a very benign drug can have a great benefit,” said Eugene Braunwald, MD, a coinvestigator on the IMPROVE-IT trial and a collaborator with Dr. Eisen on the new analysis. The new findings “emphasize that the higher a patient’s risk, the more effect they get from cholesterol-lowering treatment,” said Dr. Braunwald, professor of medicine at Harvard University and a cardiologist at Brigham and Women’s Hospital, both in Boston.
The second exploratory analysis reported by Dr. Eisen looked at the more than 16,000 patients in IMPROVE-IT without history of CABG. The analysis applied a newly developed, nine-item formula for stratifying atherothrombotic risk (Circulation. 2016 July 26;134[4];304-13) to divide these patients into low-, intermediate- and high-risk subgroups. Patients in the high-risk subgroup (20% of the IMPROVE-IT subgroup) had a 6–percentage point reduction in their primary endpoint event rate with added ezetimibe treatment, while those at intermediate risk (31%) got a 2–percentage point decrease in endpoint events, and low-risk patients (49%) actually showed a small, less than 1–percentage point increase in endpoint events with added ezetimibe, Dr. Eisen reported.
IMPROVE-IT was funded by MERCK, the company that markets ezetimibe (Zetia). Dr. Eisen had no disclosures. Dr. Braunwald has been a consultant to Merck as well as to Bayer, Daiichi Sankyo, The Medicines Company, Novartis, and Sanofi.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE ESC CONGRESS 2016
Key clinical point:
Major finding: The absolute primary-event risk reduction was 9% in post-CABG patients and 1% in all other patients.
Data source: An exploratory, post-hoc analysis of data collected in IMPROVE-IT, a multicenter trial with 18,144 patients.
Disclosures: IMPROVE-IT was funded by MERCK, the company that markets ezetimibe (Zetia). Dr. Eisen had no disclosures. Dr. Braunwald has been a consultant to Merck as well as to Bayer, Daiichi Sankyo, The Medicines Company, Novartis, and Sanofi.
Joint European atrial fibrillation guidelines break new ground
ROME – The 2016 joint European guidelines on management of atrial fibrillation break new ground by declaring as a strong Class IA recommendation that the novel oral anticoagulants are now the drugs of choice – preferred over warfarin – for stroke prevention.
The joint guidelines from the European Society of Cardiology and the European Association for Cardio-Thoracic Surgery recommend that warfarin’s use be reserved for the relatively small proportion of atrial fibrillation (AF) patients who are ineligible for the four commercially available novel oral anticoagulants (NOACs). That’s mainly patients with mechanical heart valves, moderate to severe mitral stenosis, or severe chronic kidney disease.
The ESC/EACTS guidelines, taken together with the American College of Chest Physicians guidelines on antithrombotic therapy for venous thromboembolic disease released earlier in the year, suggest that the old war horse warfarin is being eased out to pasture. The ACCP guidelines recommend any of the four NOACS – apixaban, dabigatran, edoxaban, or rivaroxaban – be used preferentially over warfarin in the treatment of venous thromboembolism (Chest 2016 Feb;149[2]:315-52). Both sets of guidelines cite compelling evidence that the NOACs are significantly safer than warfarin yet equally effective.
The ESC/EACTS guidelines are a full rewrite containing numerous departures from the previous 2012 AF management guidelines as well as from current ACC/AHA guidelines. The report includes more than 1,000 references. Eighty percent of the 154 recommendations provide Class I or IIa guidance. Two-thirds of the recommendations are Level of Evidence A or B, task force chairperson Paulus Kirchhof, MD, said at the annual congress of the European Society of Cardiology.
He and co-chairperson Stefano Benussi, MD, presented some of the highlights.
The guidelines issue a strong call for greater use of targeted ECG screening in populations at risk for silent AF, including stroke survivors and the elderly. And AF should always be documented before starting treatment, given that all of the treatments carry risk, said Dr. Kirchhof, professor of cardiovascular medicine at the University of Birmingham (England).
Once the diagnosis is established, it’s essential to address in a structured way five domains of management: acute rate and rhythm control; management of precipitating factors, including underlying cardiovascular conditions such as hypertension or valvular heart disease; assessment of stroke risk using the CHA2DS2-VASc scoring system; assessment of heart rate; and evaluation of the impact of AF symptoms on the patient’s life, including fatigue and breathlessness, using a structured instrument such as the modified European Heart Rhythm Association symptom scale.
Men with a CHA2DS2-VASc score of 1 and women with a score of 2 should be considered for anticoagulation. And the treatment should be recommended – not merely considered – for men with a score of 2 or more and women with a score of 3; that’s a Class Ia recommendation, Dr. Kirchhof continued.
The use of a specific bleeding risk score is no longer recommended in AF patients on oral anticoagulation. The emphasis has shifted to reduction of modifiable bleeding risk factors, including limiting alcohol intake to fewer than 8 drinks per week, control of hypertension, and discontinuing antiplatelet and anti-inflammatory agents.
Consideration of left atrial appendage occlusion devices should be reserved for the small percentage of patients who have clear contraindications to all forms of oral anticoagulation.
The task force concluded that patients who have bleeding on oral anticoagulation can often be managed with local therapy and discontinuation of anticoagulation therapy for a day or two before resumption. However, decisions regarding resumption of a NOAC or warfarin after an intracranial bleed should be handled by an interdisciplinary panel composed of a stroke neurologist, a cardiologist, a neuroradiologist, and a neurosurgeon.
Evidence-based treatment options in patients with symptomatic AF after failed catheter ablation include minimally invasive surgery with epicardial pulmonary vein isolation, more extensive catheter ablation, and hybrid procedures, according to Dr. Benussi, who is codirector of clinical cardiovascular surgery at University Hospital in Zurich.
The guidelines state that the data supporting catheter ablation to achieve long-term rhythm control are now sufficiently strong that this intervention should be considered as a first-line option alongside antiarrhythmic drugs as a matter of patient preference in the setting of symptomatic paroxysmal AF regardless of whether the patient has CAD, heart failure, valvular heart disease, or no structural heart disease.
Catheter ablation using radiofrequency energy or cryoablation should target complete isolation of the pulmonary veins.
“Additional ablation lines do not provide demonstrable clinical benefit and increase the risk of postablation left atrial arrhythmias,” the surgeon said.
Maze surgery, preferably biatrial, received a favorable Class IIa, Level of Evidence A recommendation as worthy of consideration in patients with symptomatic AF who are already undergoing cardiac surgery. This recommendation was based upon an external review by the Cochrane group which was commissioned by the guidelines task force. The Cochrane review of eight published studies concluded that Maze surgery under such circumstances was associated with a twofold increased freedom from AF, atrial flutter, and atrial tachycardia (Cochrane Database of Systematic Reviews 2016;8: CD012088. doi: 10.1002/14651858.CD012088.pub2).
The AF management guidelines are supported by the ESC Pocket Guidelines app, which includes an overall AF treatment manager developed by the European Union–funded CATCH ME (Characterizing Atrial Fibrillation by Translating its Causes Into Health Modifiers in the Elderly) project.
The multidisciplinary 17-member AF management task force was drawn from cardiology, stroke neurology, cardiac surgery, and specialist nursing. Dr. Kirchhof stressed that only recommendations supported by at least 75% of task force members made it into the guidelines (Eur Heart J. 2016 Aug 27. pii: ehw210. [Epub ahead of print] doi: 10.1093/eurheartj/ehw210).
ROME – The 2016 joint European guidelines on management of atrial fibrillation break new ground by declaring as a strong Class IA recommendation that the novel oral anticoagulants are now the drugs of choice – preferred over warfarin – for stroke prevention.
The joint guidelines from the European Society of Cardiology and the European Association for Cardio-Thoracic Surgery recommend that warfarin’s use be reserved for the relatively small proportion of atrial fibrillation (AF) patients who are ineligible for the four commercially available novel oral anticoagulants (NOACs). That’s mainly patients with mechanical heart valves, moderate to severe mitral stenosis, or severe chronic kidney disease.
The ESC/EACTS guidelines, taken together with the American College of Chest Physicians guidelines on antithrombotic therapy for venous thromboembolic disease released earlier in the year, suggest that the old war horse warfarin is being eased out to pasture. The ACCP guidelines recommend any of the four NOACS – apixaban, dabigatran, edoxaban, or rivaroxaban – be used preferentially over warfarin in the treatment of venous thromboembolism (Chest 2016 Feb;149[2]:315-52). Both sets of guidelines cite compelling evidence that the NOACs are significantly safer than warfarin yet equally effective.
The ESC/EACTS guidelines are a full rewrite containing numerous departures from the previous 2012 AF management guidelines as well as from current ACC/AHA guidelines. The report includes more than 1,000 references. Eighty percent of the 154 recommendations provide Class I or IIa guidance. Two-thirds of the recommendations are Level of Evidence A or B, task force chairperson Paulus Kirchhof, MD, said at the annual congress of the European Society of Cardiology.
He and co-chairperson Stefano Benussi, MD, presented some of the highlights.
The guidelines issue a strong call for greater use of targeted ECG screening in populations at risk for silent AF, including stroke survivors and the elderly. And AF should always be documented before starting treatment, given that all of the treatments carry risk, said Dr. Kirchhof, professor of cardiovascular medicine at the University of Birmingham (England).
Once the diagnosis is established, it’s essential to address in a structured way five domains of management: acute rate and rhythm control; management of precipitating factors, including underlying cardiovascular conditions such as hypertension or valvular heart disease; assessment of stroke risk using the CHA2DS2-VASc scoring system; assessment of heart rate; and evaluation of the impact of AF symptoms on the patient’s life, including fatigue and breathlessness, using a structured instrument such as the modified European Heart Rhythm Association symptom scale.
Men with a CHA2DS2-VASc score of 1 and women with a score of 2 should be considered for anticoagulation. And the treatment should be recommended – not merely considered – for men with a score of 2 or more and women with a score of 3; that’s a Class Ia recommendation, Dr. Kirchhof continued.
The use of a specific bleeding risk score is no longer recommended in AF patients on oral anticoagulation. The emphasis has shifted to reduction of modifiable bleeding risk factors, including limiting alcohol intake to fewer than 8 drinks per week, control of hypertension, and discontinuing antiplatelet and anti-inflammatory agents.
Consideration of left atrial appendage occlusion devices should be reserved for the small percentage of patients who have clear contraindications to all forms of oral anticoagulation.
The task force concluded that patients who have bleeding on oral anticoagulation can often be managed with local therapy and discontinuation of anticoagulation therapy for a day or two before resumption. However, decisions regarding resumption of a NOAC or warfarin after an intracranial bleed should be handled by an interdisciplinary panel composed of a stroke neurologist, a cardiologist, a neuroradiologist, and a neurosurgeon.
Evidence-based treatment options in patients with symptomatic AF after failed catheter ablation include minimally invasive surgery with epicardial pulmonary vein isolation, more extensive catheter ablation, and hybrid procedures, according to Dr. Benussi, who is codirector of clinical cardiovascular surgery at University Hospital in Zurich.
The guidelines state that the data supporting catheter ablation to achieve long-term rhythm control are now sufficiently strong that this intervention should be considered as a first-line option alongside antiarrhythmic drugs as a matter of patient preference in the setting of symptomatic paroxysmal AF regardless of whether the patient has CAD, heart failure, valvular heart disease, or no structural heart disease.
Catheter ablation using radiofrequency energy or cryoablation should target complete isolation of the pulmonary veins.
“Additional ablation lines do not provide demonstrable clinical benefit and increase the risk of postablation left atrial arrhythmias,” the surgeon said.
Maze surgery, preferably biatrial, received a favorable Class IIa, Level of Evidence A recommendation as worthy of consideration in patients with symptomatic AF who are already undergoing cardiac surgery. This recommendation was based upon an external review by the Cochrane group which was commissioned by the guidelines task force. The Cochrane review of eight published studies concluded that Maze surgery under such circumstances was associated with a twofold increased freedom from AF, atrial flutter, and atrial tachycardia (Cochrane Database of Systematic Reviews 2016;8: CD012088. doi: 10.1002/14651858.CD012088.pub2).
The AF management guidelines are supported by the ESC Pocket Guidelines app, which includes an overall AF treatment manager developed by the European Union–funded CATCH ME (Characterizing Atrial Fibrillation by Translating its Causes Into Health Modifiers in the Elderly) project.
The multidisciplinary 17-member AF management task force was drawn from cardiology, stroke neurology, cardiac surgery, and specialist nursing. Dr. Kirchhof stressed that only recommendations supported by at least 75% of task force members made it into the guidelines (Eur Heart J. 2016 Aug 27. pii: ehw210. [Epub ahead of print] doi: 10.1093/eurheartj/ehw210).
ROME – The 2016 joint European guidelines on management of atrial fibrillation break new ground by declaring as a strong Class IA recommendation that the novel oral anticoagulants are now the drugs of choice – preferred over warfarin – for stroke prevention.
The joint guidelines from the European Society of Cardiology and the European Association for Cardio-Thoracic Surgery recommend that warfarin’s use be reserved for the relatively small proportion of atrial fibrillation (AF) patients who are ineligible for the four commercially available novel oral anticoagulants (NOACs). That’s mainly patients with mechanical heart valves, moderate to severe mitral stenosis, or severe chronic kidney disease.
The ESC/EACTS guidelines, taken together with the American College of Chest Physicians guidelines on antithrombotic therapy for venous thromboembolic disease released earlier in the year, suggest that the old war horse warfarin is being eased out to pasture. The ACCP guidelines recommend any of the four NOACS – apixaban, dabigatran, edoxaban, or rivaroxaban – be used preferentially over warfarin in the treatment of venous thromboembolism (Chest 2016 Feb;149[2]:315-52). Both sets of guidelines cite compelling evidence that the NOACs are significantly safer than warfarin yet equally effective.
The ESC/EACTS guidelines are a full rewrite containing numerous departures from the previous 2012 AF management guidelines as well as from current ACC/AHA guidelines. The report includes more than 1,000 references. Eighty percent of the 154 recommendations provide Class I or IIa guidance. Two-thirds of the recommendations are Level of Evidence A or B, task force chairperson Paulus Kirchhof, MD, said at the annual congress of the European Society of Cardiology.
He and co-chairperson Stefano Benussi, MD, presented some of the highlights.
The guidelines issue a strong call for greater use of targeted ECG screening in populations at risk for silent AF, including stroke survivors and the elderly. And AF should always be documented before starting treatment, given that all of the treatments carry risk, said Dr. Kirchhof, professor of cardiovascular medicine at the University of Birmingham (England).
Once the diagnosis is established, it’s essential to address in a structured way five domains of management: acute rate and rhythm control; management of precipitating factors, including underlying cardiovascular conditions such as hypertension or valvular heart disease; assessment of stroke risk using the CHA2DS2-VASc scoring system; assessment of heart rate; and evaluation of the impact of AF symptoms on the patient’s life, including fatigue and breathlessness, using a structured instrument such as the modified European Heart Rhythm Association symptom scale.
Men with a CHA2DS2-VASc score of 1 and women with a score of 2 should be considered for anticoagulation. And the treatment should be recommended – not merely considered – for men with a score of 2 or more and women with a score of 3; that’s a Class Ia recommendation, Dr. Kirchhof continued.
The use of a specific bleeding risk score is no longer recommended in AF patients on oral anticoagulation. The emphasis has shifted to reduction of modifiable bleeding risk factors, including limiting alcohol intake to fewer than 8 drinks per week, control of hypertension, and discontinuing antiplatelet and anti-inflammatory agents.
Consideration of left atrial appendage occlusion devices should be reserved for the small percentage of patients who have clear contraindications to all forms of oral anticoagulation.
The task force concluded that patients who have bleeding on oral anticoagulation can often be managed with local therapy and discontinuation of anticoagulation therapy for a day or two before resumption. However, decisions regarding resumption of a NOAC or warfarin after an intracranial bleed should be handled by an interdisciplinary panel composed of a stroke neurologist, a cardiologist, a neuroradiologist, and a neurosurgeon.
Evidence-based treatment options in patients with symptomatic AF after failed catheter ablation include minimally invasive surgery with epicardial pulmonary vein isolation, more extensive catheter ablation, and hybrid procedures, according to Dr. Benussi, who is codirector of clinical cardiovascular surgery at University Hospital in Zurich.
The guidelines state that the data supporting catheter ablation to achieve long-term rhythm control are now sufficiently strong that this intervention should be considered as a first-line option alongside antiarrhythmic drugs as a matter of patient preference in the setting of symptomatic paroxysmal AF regardless of whether the patient has CAD, heart failure, valvular heart disease, or no structural heart disease.
Catheter ablation using radiofrequency energy or cryoablation should target complete isolation of the pulmonary veins.
“Additional ablation lines do not provide demonstrable clinical benefit and increase the risk of postablation left atrial arrhythmias,” the surgeon said.
Maze surgery, preferably biatrial, received a favorable Class IIa, Level of Evidence A recommendation as worthy of consideration in patients with symptomatic AF who are already undergoing cardiac surgery. This recommendation was based upon an external review by the Cochrane group which was commissioned by the guidelines task force. The Cochrane review of eight published studies concluded that Maze surgery under such circumstances was associated with a twofold increased freedom from AF, atrial flutter, and atrial tachycardia (Cochrane Database of Systematic Reviews 2016;8: CD012088. doi: 10.1002/14651858.CD012088.pub2).
The AF management guidelines are supported by the ESC Pocket Guidelines app, which includes an overall AF treatment manager developed by the European Union–funded CATCH ME (Characterizing Atrial Fibrillation by Translating its Causes Into Health Modifiers in the Elderly) project.
The multidisciplinary 17-member AF management task force was drawn from cardiology, stroke neurology, cardiac surgery, and specialist nursing. Dr. Kirchhof stressed that only recommendations supported by at least 75% of task force members made it into the guidelines (Eur Heart J. 2016 Aug 27. pii: ehw210. [Epub ahead of print] doi: 10.1093/eurheartj/ehw210).
LMWH best for preventing PE in patients with major trauma
WAIKOLOA, HAWAII – Venous thromboembolism prophylaxis with low molecular weight heparin (LMWH), instead of unfractionated heparin (UH), is associated with lower risk of pulmonary embolism (PE) in patients with major trauma, results from a large study have shown.
The results of the study, based on data from the American College of Surgeons (ACS) Trauma Quality Improvement Program, suggest that LMWH-based strategies for thromboprophylaxis should be preferred after major trauma.
Dr. Byrne, a general surgery resident at Sunnybrook Health Science Center, Toronto, Ontario, Canada, went on to note that LMWH is often favored because of a randomized controlled trial which showed that LMWH was associated with fewer deep vein thromboses (N Engl. J. Med. 1996;335[10]:701-7). However, significant practice variability continues to exist.
“Practitioners might favor the shorter half-life of unfractionated heparin in patients where they perceive the risk for hemorrhagic complications is high,” he said. “There’s also recent evidence to suggest that dosing may be all important and that unfractionated heparin dosed three times daily may be equivalent to low molecular weight heparin. If this is true, it might suggest that the historically higher cost of low molecular weight heparin could favor the use of unfractionated heparin.”
Furthermore, there is a is a lack of evidence comparing either agent to prevent PE, he added. “This is an important gap in our knowledge, because PE frequently occurs in the absence of an identified DVT and carries a significant risk of death. At present, it is not known how practice patterns with respect to choice of prophylaxis type influence risk of PE at the patient or hospital levels.”
Due to a lack of evidence comparing agents to prevent PE, the researchers set out to compare the effectiveness of LMWH versus UH to prevent PE in patients with major trauma who were treated at trauma centers participating in the ACS Trauma Quality Improvement Program from 2012 to 2015. They included all adults with severe injury who received LMWH or UH and excluded those who died or were discharged within five days, and those with a bleeding disorder or chronic anticoagulation. The exposure was defined as thromboprophylaxis with LMWH versus UH, and the primary outcome was PE confirmed on radiologic imaging. Potential confounders were considered, including patient baseline characteristics, anatomic and global injury severity, presenting characteristics in the emergency department, acute intracranial injuries, orthopedic injuries, early surgical interventions, and timing of prophylaxis initiation.
Dr. Byrne and his associates then used three analytic approaches in the study: a propensity score matching methodology, a multivariable logistic regression model for PE, and a center-level analysis examining the influence of LMWH utilization on hospital rates of PE.
They identified 153,474 trauma patients from 217 trauma centers. Their median age was 50 years and 67% were male. Blunt trauma was most common (89%), with a mean Injury Severity Score score of 20. LMWH was the most common type of thromboprophylaxis used (74%), and PE was diagnosed in 2,722 patients (1.8%).
Compared with patients who received LMWH, those who received UH were older and were significantly more likely to have been injured by falling (42% vs. 28%), with higher rates of severe head injuries (43% vs. 24%) and intracranial hemorrhage (38% vs. 19%). Conversely, LMWH was most favored in patients with orthopedic injuries.
After propensity score matching, patients on LMWH suffered significantly fewer PEs (1.4% vs. 2.4%; odds ratio, 0.56). This result was consistent within propensity-matched subgroups, including for patients with blunt multisystem injuries (OR, 0.60), penetrating truncal injuries (OR, 0.65), shock in the ED (OR, 0.68), isolated severe traumatic brain injury (OR, 0.49), and isolated orthopedic injuries (OR, 0.28).
Results of a sensitivity analysis in which each propensity-matched pair was matched within the same trauma center yielded similar results. Specifically, patients who received LMWH were at significantly lower risk for developing PE (OR, 0.64). “Importantly, this analysis minimized residual confounding due to differences in hospital-level processes of care, such as prophylaxis dosing or frequency, mechanical prophylaxis use, and thromboembolism screening practices,” Dr. Byrne noted.
Multivariable logistic regression also showed that patients who received LMWH had lower odds of PE (OR, 0.59). Other significant predictors of PE included obesity (OR, 1.54), severe chest injury (OR, 1.31), femoral shaft fracture (OR, 1.60), and spinal cord injury (OR, 1.60). Delays in prophylaxis initiation beyond the first day in the hospital were associated with significantly higher rates of PE, with an 80% increased risk of PE for patients who had their prophylaxis initiated after the fourth day.
The researchers conducted a center-level analysis in an effort to answer the question whether practice patterns with respect to choice of prophylaxis type influence hospital rates of PE. Across all 217 trauma centers in the study, the median rate of LMWH use was 80%, while the mean rate of PE was 1.6%. When trauma centers were grouped into quartiles based on their unique rate of LMWH use, trauma centers in the highest quartile (median LMWH use: 95%) were 50 times more likely to use LMWH, compared to those in the lowest quartile (median LMWH use: 39%) after adjusting for patient case mix. Compared with the lowest quartile, trauma centers that used the greatest proportion of LMWH had significantly lower rates of PE (1.2% vs. 2.0%). After adjusting for patient baseline and injury characteristics, patients who were treated at trauma centers in the highest quartile had significantly lower odds of PE (OR, 0.59).
Dr. Byrne acknowledged certain limitations of the study, including the potential for residual confounding and the inability to account for the dosing and frequency of prophylaxis that was given. “We were only able to measure the type and timing of prophylaxis initiation. We don’t know what doses of prophylaxis were used, and it is possible that the trauma centers included in this study favored use of UH twice daily,” he said.
Therefore, it is possible that the results might have been different if they had been able to directly compare LMWH to UH administered three times a day. “We also couldn’t measure interruptions in dosing due to surgery or patient refusal,” he said. “However, if it the case that UH is more likely to be refused based on the need for more frequent dosing, perhaps that is another feather in the cap of low molecular weight heparin-based thromboprophylaxis strategies. Larger prospective studies are needed, that take into account prophylaxis type and dosing, and are powered to detect a difference with respect to PE.”
Dr. Byrne reported having no financial disclosures.
WAIKOLOA, HAWAII – Venous thromboembolism prophylaxis with low molecular weight heparin (LMWH), instead of unfractionated heparin (UH), is associated with lower risk of pulmonary embolism (PE) in patients with major trauma, results from a large study have shown.
The results of the study, based on data from the American College of Surgeons (ACS) Trauma Quality Improvement Program, suggest that LMWH-based strategies for thromboprophylaxis should be preferred after major trauma.
Dr. Byrne, a general surgery resident at Sunnybrook Health Science Center, Toronto, Ontario, Canada, went on to note that LMWH is often favored because of a randomized controlled trial which showed that LMWH was associated with fewer deep vein thromboses (N Engl. J. Med. 1996;335[10]:701-7). However, significant practice variability continues to exist.
“Practitioners might favor the shorter half-life of unfractionated heparin in patients where they perceive the risk for hemorrhagic complications is high,” he said. “There’s also recent evidence to suggest that dosing may be all important and that unfractionated heparin dosed three times daily may be equivalent to low molecular weight heparin. If this is true, it might suggest that the historically higher cost of low molecular weight heparin could favor the use of unfractionated heparin.”
Furthermore, there is a is a lack of evidence comparing either agent to prevent PE, he added. “This is an important gap in our knowledge, because PE frequently occurs in the absence of an identified DVT and carries a significant risk of death. At present, it is not known how practice patterns with respect to choice of prophylaxis type influence risk of PE at the patient or hospital levels.”
Due to a lack of evidence comparing agents to prevent PE, the researchers set out to compare the effectiveness of LMWH versus UH to prevent PE in patients with major trauma who were treated at trauma centers participating in the ACS Trauma Quality Improvement Program from 2012 to 2015. They included all adults with severe injury who received LMWH or UH and excluded those who died or were discharged within five days, and those with a bleeding disorder or chronic anticoagulation. The exposure was defined as thromboprophylaxis with LMWH versus UH, and the primary outcome was PE confirmed on radiologic imaging. Potential confounders were considered, including patient baseline characteristics, anatomic and global injury severity, presenting characteristics in the emergency department, acute intracranial injuries, orthopedic injuries, early surgical interventions, and timing of prophylaxis initiation.
Dr. Byrne and his associates then used three analytic approaches in the study: a propensity score matching methodology, a multivariable logistic regression model for PE, and a center-level analysis examining the influence of LMWH utilization on hospital rates of PE.
They identified 153,474 trauma patients from 217 trauma centers. Their median age was 50 years and 67% were male. Blunt trauma was most common (89%), with a mean Injury Severity Score score of 20. LMWH was the most common type of thromboprophylaxis used (74%), and PE was diagnosed in 2,722 patients (1.8%).
Compared with patients who received LMWH, those who received UH were older and were significantly more likely to have been injured by falling (42% vs. 28%), with higher rates of severe head injuries (43% vs. 24%) and intracranial hemorrhage (38% vs. 19%). Conversely, LMWH was most favored in patients with orthopedic injuries.
After propensity score matching, patients on LMWH suffered significantly fewer PEs (1.4% vs. 2.4%; odds ratio, 0.56). This result was consistent within propensity-matched subgroups, including for patients with blunt multisystem injuries (OR, 0.60), penetrating truncal injuries (OR, 0.65), shock in the ED (OR, 0.68), isolated severe traumatic brain injury (OR, 0.49), and isolated orthopedic injuries (OR, 0.28).
Results of a sensitivity analysis in which each propensity-matched pair was matched within the same trauma center yielded similar results. Specifically, patients who received LMWH were at significantly lower risk for developing PE (OR, 0.64). “Importantly, this analysis minimized residual confounding due to differences in hospital-level processes of care, such as prophylaxis dosing or frequency, mechanical prophylaxis use, and thromboembolism screening practices,” Dr. Byrne noted.
Multivariable logistic regression also showed that patients who received LMWH had lower odds of PE (OR, 0.59). Other significant predictors of PE included obesity (OR, 1.54), severe chest injury (OR, 1.31), femoral shaft fracture (OR, 1.60), and spinal cord injury (OR, 1.60). Delays in prophylaxis initiation beyond the first day in the hospital were associated with significantly higher rates of PE, with an 80% increased risk of PE for patients who had their prophylaxis initiated after the fourth day.
The researchers conducted a center-level analysis in an effort to answer the question whether practice patterns with respect to choice of prophylaxis type influence hospital rates of PE. Across all 217 trauma centers in the study, the median rate of LMWH use was 80%, while the mean rate of PE was 1.6%. When trauma centers were grouped into quartiles based on their unique rate of LMWH use, trauma centers in the highest quartile (median LMWH use: 95%) were 50 times more likely to use LMWH, compared to those in the lowest quartile (median LMWH use: 39%) after adjusting for patient case mix. Compared with the lowest quartile, trauma centers that used the greatest proportion of LMWH had significantly lower rates of PE (1.2% vs. 2.0%). After adjusting for patient baseline and injury characteristics, patients who were treated at trauma centers in the highest quartile had significantly lower odds of PE (OR, 0.59).
Dr. Byrne acknowledged certain limitations of the study, including the potential for residual confounding and the inability to account for the dosing and frequency of prophylaxis that was given. “We were only able to measure the type and timing of prophylaxis initiation. We don’t know what doses of prophylaxis were used, and it is possible that the trauma centers included in this study favored use of UH twice daily,” he said.
Therefore, it is possible that the results might have been different if they had been able to directly compare LMWH to UH administered three times a day. “We also couldn’t measure interruptions in dosing due to surgery or patient refusal,” he said. “However, if it the case that UH is more likely to be refused based on the need for more frequent dosing, perhaps that is another feather in the cap of low molecular weight heparin-based thromboprophylaxis strategies. Larger prospective studies are needed, that take into account prophylaxis type and dosing, and are powered to detect a difference with respect to PE.”
Dr. Byrne reported having no financial disclosures.
WAIKOLOA, HAWAII – Venous thromboembolism prophylaxis with low molecular weight heparin (LMWH), instead of unfractionated heparin (UH), is associated with lower risk of pulmonary embolism (PE) in patients with major trauma, results from a large study have shown.
The results of the study, based on data from the American College of Surgeons (ACS) Trauma Quality Improvement Program, suggest that LMWH-based strategies for thromboprophylaxis should be preferred after major trauma.
Dr. Byrne, a general surgery resident at Sunnybrook Health Science Center, Toronto, Ontario, Canada, went on to note that LMWH is often favored because of a randomized controlled trial which showed that LMWH was associated with fewer deep vein thromboses (N Engl. J. Med. 1996;335[10]:701-7). However, significant practice variability continues to exist.
“Practitioners might favor the shorter half-life of unfractionated heparin in patients where they perceive the risk for hemorrhagic complications is high,” he said. “There’s also recent evidence to suggest that dosing may be all important and that unfractionated heparin dosed three times daily may be equivalent to low molecular weight heparin. If this is true, it might suggest that the historically higher cost of low molecular weight heparin could favor the use of unfractionated heparin.”
Furthermore, there is a is a lack of evidence comparing either agent to prevent PE, he added. “This is an important gap in our knowledge, because PE frequently occurs in the absence of an identified DVT and carries a significant risk of death. At present, it is not known how practice patterns with respect to choice of prophylaxis type influence risk of PE at the patient or hospital levels.”
Due to a lack of evidence comparing agents to prevent PE, the researchers set out to compare the effectiveness of LMWH versus UH to prevent PE in patients with major trauma who were treated at trauma centers participating in the ACS Trauma Quality Improvement Program from 2012 to 2015. They included all adults with severe injury who received LMWH or UH and excluded those who died or were discharged within five days, and those with a bleeding disorder or chronic anticoagulation. The exposure was defined as thromboprophylaxis with LMWH versus UH, and the primary outcome was PE confirmed on radiologic imaging. Potential confounders were considered, including patient baseline characteristics, anatomic and global injury severity, presenting characteristics in the emergency department, acute intracranial injuries, orthopedic injuries, early surgical interventions, and timing of prophylaxis initiation.
Dr. Byrne and his associates then used three analytic approaches in the study: a propensity score matching methodology, a multivariable logistic regression model for PE, and a center-level analysis examining the influence of LMWH utilization on hospital rates of PE.
They identified 153,474 trauma patients from 217 trauma centers. Their median age was 50 years and 67% were male. Blunt trauma was most common (89%), with a mean Injury Severity Score score of 20. LMWH was the most common type of thromboprophylaxis used (74%), and PE was diagnosed in 2,722 patients (1.8%).
Compared with patients who received LMWH, those who received UH were older and were significantly more likely to have been injured by falling (42% vs. 28%), with higher rates of severe head injuries (43% vs. 24%) and intracranial hemorrhage (38% vs. 19%). Conversely, LMWH was most favored in patients with orthopedic injuries.
After propensity score matching, patients on LMWH suffered significantly fewer PEs (1.4% vs. 2.4%; odds ratio, 0.56). This result was consistent within propensity-matched subgroups, including for patients with blunt multisystem injuries (OR, 0.60), penetrating truncal injuries (OR, 0.65), shock in the ED (OR, 0.68), isolated severe traumatic brain injury (OR, 0.49), and isolated orthopedic injuries (OR, 0.28).
Results of a sensitivity analysis in which each propensity-matched pair was matched within the same trauma center yielded similar results. Specifically, patients who received LMWH were at significantly lower risk for developing PE (OR, 0.64). “Importantly, this analysis minimized residual confounding due to differences in hospital-level processes of care, such as prophylaxis dosing or frequency, mechanical prophylaxis use, and thromboembolism screening practices,” Dr. Byrne noted.
Multivariable logistic regression also showed that patients who received LMWH had lower odds of PE (OR, 0.59). Other significant predictors of PE included obesity (OR, 1.54), severe chest injury (OR, 1.31), femoral shaft fracture (OR, 1.60), and spinal cord injury (OR, 1.60). Delays in prophylaxis initiation beyond the first day in the hospital were associated with significantly higher rates of PE, with an 80% increased risk of PE for patients who had their prophylaxis initiated after the fourth day.
The researchers conducted a center-level analysis in an effort to answer the question whether practice patterns with respect to choice of prophylaxis type influence hospital rates of PE. Across all 217 trauma centers in the study, the median rate of LMWH use was 80%, while the mean rate of PE was 1.6%. When trauma centers were grouped into quartiles based on their unique rate of LMWH use, trauma centers in the highest quartile (median LMWH use: 95%) were 50 times more likely to use LMWH, compared to those in the lowest quartile (median LMWH use: 39%) after adjusting for patient case mix. Compared with the lowest quartile, trauma centers that used the greatest proportion of LMWH had significantly lower rates of PE (1.2% vs. 2.0%). After adjusting for patient baseline and injury characteristics, patients who were treated at trauma centers in the highest quartile had significantly lower odds of PE (OR, 0.59).
Dr. Byrne acknowledged certain limitations of the study, including the potential for residual confounding and the inability to account for the dosing and frequency of prophylaxis that was given. “We were only able to measure the type and timing of prophylaxis initiation. We don’t know what doses of prophylaxis were used, and it is possible that the trauma centers included in this study favored use of UH twice daily,” he said.
Therefore, it is possible that the results might have been different if they had been able to directly compare LMWH to UH administered three times a day. “We also couldn’t measure interruptions in dosing due to surgery or patient refusal,” he said. “However, if it the case that UH is more likely to be refused based on the need for more frequent dosing, perhaps that is another feather in the cap of low molecular weight heparin-based thromboprophylaxis strategies. Larger prospective studies are needed, that take into account prophylaxis type and dosing, and are powered to detect a difference with respect to PE.”
Dr. Byrne reported having no financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point:
Major finding: After propensity score matching, patients on LMWH had significantly fewer PEs, compared with those on unfractionated heparin (1.4% vs. 2.4%; odds ratio, 0.56). Data source: A multicenter analysis of 2,722 trauma patients who were diagnosed with pulmonary embolism.
Disclosures: Dr. Byrne reported having no financial disclosures.
Pulmonary embolism common in patients hospitalized for syncope
When specifically looked for, pulmonary embolism was identified in approximately 17% of adults hospitalized for a first episode of syncope, according to a report published in the New England Journal of Medicine.
Most medical textbooks include pulmonary embolism (PE) in the differential diagnosis of syncope, but “current international guidelines, including those from the European Society of Cardiology and the American Heart Association, pay little attention to establishing a diagnostic workup for PE in these patients. Hence, when a patient is admitted to a hospital for an episode of syncope, PE – a potentially fatal disease that can be effectively treated – is rarely considered as a possible cause,” said Paolo Prandoni, MD, PhD, of the vascular medicine unit, University of Padua (Italy), and his associates in the PESY (Prevalence of Pulmonary Embolism in Patients With Syncope) trial.
The investigators used a systematic diagnostic work-up to determine the prevalence of PE in a cross-sectional study involving 560 adults hospitalized for syncope at 11 medical centers across Italy during a 2.5-year period. Most of these patients were elderly (mean age, 76 years), and most had clinical evidence indicating that a factor other than PE had caused their fainting. For this study, syncope was defined as a transient loss of consciousness with rapid onset, short duration (less than 1 minute), and spontaneous resolution, with obvious causes ruled out (such as epileptic seizure, stroke, or head trauma).
The “unexpectedly high” prevalence of PE was 17.3% overall, and it was consistent, ranging from 15% to 20%, across all 11 hospitals. The prevalence was even higher, at 25.4%, in the subgroup of 205 patients who had syncope of undetermined origin, as well as in 12.7% of the subgroup of 355 patients considered to have an alternative explanation for the disorder, Dr. Prandoni and his associates wrote (N Engl J Med. 2016 Oct 20. doi: 10.1056/NEJMoa1602172).
The researchers noted that this study likely underestimates the actual prevalence of PE among patients with syncope because it did not include patients who were not hospitalized, such as those who received only ambulatory care and those who presented to an emergency department but were not admitted.
The study was supported by the University of Padua. Dr. Prandoni and his associates reported having no relevant financial disclosures.
When specifically looked for, pulmonary embolism was identified in approximately 17% of adults hospitalized for a first episode of syncope, according to a report published in the New England Journal of Medicine.
Most medical textbooks include pulmonary embolism (PE) in the differential diagnosis of syncope, but “current international guidelines, including those from the European Society of Cardiology and the American Heart Association, pay little attention to establishing a diagnostic workup for PE in these patients. Hence, when a patient is admitted to a hospital for an episode of syncope, PE – a potentially fatal disease that can be effectively treated – is rarely considered as a possible cause,” said Paolo Prandoni, MD, PhD, of the vascular medicine unit, University of Padua (Italy), and his associates in the PESY (Prevalence of Pulmonary Embolism in Patients With Syncope) trial.
The investigators used a systematic diagnostic work-up to determine the prevalence of PE in a cross-sectional study involving 560 adults hospitalized for syncope at 11 medical centers across Italy during a 2.5-year period. Most of these patients were elderly (mean age, 76 years), and most had clinical evidence indicating that a factor other than PE had caused their fainting. For this study, syncope was defined as a transient loss of consciousness with rapid onset, short duration (less than 1 minute), and spontaneous resolution, with obvious causes ruled out (such as epileptic seizure, stroke, or head trauma).
The “unexpectedly high” prevalence of PE was 17.3% overall, and it was consistent, ranging from 15% to 20%, across all 11 hospitals. The prevalence was even higher, at 25.4%, in the subgroup of 205 patients who had syncope of undetermined origin, as well as in 12.7% of the subgroup of 355 patients considered to have an alternative explanation for the disorder, Dr. Prandoni and his associates wrote (N Engl J Med. 2016 Oct 20. doi: 10.1056/NEJMoa1602172).
The researchers noted that this study likely underestimates the actual prevalence of PE among patients with syncope because it did not include patients who were not hospitalized, such as those who received only ambulatory care and those who presented to an emergency department but were not admitted.
The study was supported by the University of Padua. Dr. Prandoni and his associates reported having no relevant financial disclosures.
When specifically looked for, pulmonary embolism was identified in approximately 17% of adults hospitalized for a first episode of syncope, according to a report published in the New England Journal of Medicine.
Most medical textbooks include pulmonary embolism (PE) in the differential diagnosis of syncope, but “current international guidelines, including those from the European Society of Cardiology and the American Heart Association, pay little attention to establishing a diagnostic workup for PE in these patients. Hence, when a patient is admitted to a hospital for an episode of syncope, PE – a potentially fatal disease that can be effectively treated – is rarely considered as a possible cause,” said Paolo Prandoni, MD, PhD, of the vascular medicine unit, University of Padua (Italy), and his associates in the PESY (Prevalence of Pulmonary Embolism in Patients With Syncope) trial.
The investigators used a systematic diagnostic work-up to determine the prevalence of PE in a cross-sectional study involving 560 adults hospitalized for syncope at 11 medical centers across Italy during a 2.5-year period. Most of these patients were elderly (mean age, 76 years), and most had clinical evidence indicating that a factor other than PE had caused their fainting. For this study, syncope was defined as a transient loss of consciousness with rapid onset, short duration (less than 1 minute), and spontaneous resolution, with obvious causes ruled out (such as epileptic seizure, stroke, or head trauma).
The “unexpectedly high” prevalence of PE was 17.3% overall, and it was consistent, ranging from 15% to 20%, across all 11 hospitals. The prevalence was even higher, at 25.4%, in the subgroup of 205 patients who had syncope of undetermined origin, as well as in 12.7% of the subgroup of 355 patients considered to have an alternative explanation for the disorder, Dr. Prandoni and his associates wrote (N Engl J Med. 2016 Oct 20. doi: 10.1056/NEJMoa1602172).
The researchers noted that this study likely underestimates the actual prevalence of PE among patients with syncope because it did not include patients who were not hospitalized, such as those who received only ambulatory care and those who presented to an emergency department but were not admitted.
The study was supported by the University of Padua. Dr. Prandoni and his associates reported having no relevant financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: When specifically looked for, pulmonary embolism was identified in approximately 17% of adults hospitalized for a first episode of syncope.
Major finding: The “unexpectedly high” prevalence of PE was 17.3% overall, and it was consistent, ranging from 15% to 20%, across all 11 hospitals in the study.
Data source: A cross-sectional study involving 560 adults hospitalized for syncope at 11 Italian medical centers during a 2.5 year period.
Disclosures: This study was supported by the University of Padua (Italy). Dr. Prandoni and his associates reported having no relevant financial disclosures.
Earlier ischemic stroke presentation may sometimes mean delayed tPA
BALTIMORE – Going to the hospital soon after the development of symptoms of acute ischemic stroke may not guarantee quick treatment.
A study of 1,865 patients treated within the past decade at a large urban comprehensive stroke center has revealed delayed treatment with tissue plasminogen activator, compared with patients who came to the emergency room hours after symptom development, Dr. Kyle C. Rossi said at the annual meeting of the American Neurological Association.
Treatment with tissue plasminogen activator (tPA) within 3 hours after the first symptoms of acute ischemic stroke definitely improves long-term outcomes, but meeting this target time remains a challenge. Patients who present to the emergency room soon after symptom development would seemingly have an advantage, yet Dr. Rossi’s preliminary scrutiny of patient records at Mount Sinai raised doubts about this and prompted the present study.
The hypothesis was that cases with a shorter time between symptom development and diagnosis of stroke (last known well-to-stroke code time, or LKW-to-code) will have a longer time between diagnosis and tPA administration (code-to-tPA), “possibly due to the perception on the part of evaluating physicians of sufficient remaining time before the end of the tPA window.”
The researchers examined patient records from the American Heart Association/American Stroke Association’s “Get with the Guidelines” stroke program, a voluntary observational registry for patients with acute stroke. Of the 1,865 ischemic stroke patients treated during 2009-2015, 122 who received intravenous tPA were allocated to three LKW-to-code groups: within an hour (38 patients), within the next hour (49 patients), or 2 hours or more (35 patients).
The patients tended to be in their late 60s. Just over half were female, and about 40% were white.
Overall, the average LKW-to-code time was 91 ± 48 minutes and the average code-to-tPA time was 67 ± 26 minutes.
Average code-to-tPA times were 80, 67, and 52 minutes, respectively, for the three groups (P less than .0001). On average, it took 28 minutes longer to give tPA to patients who presented within an hour than to patients presenting 2 hours or longer after their first stroke symptom. There was an increase in code-to-tPA time of 1 minute for every decrease in LKW-to-code time of 4 minutes (P less than .0001).
The delay in the time to treat patients who arrive sooner after development of stroke symptoms may result from a decision made by the evaluating neurologist to conduct additional testing prior to administering tPA. Sometimes other staff may be unaware of the decision to delay treatment, according to Dr. Rossi and his colleagues.
“Absolutely, folks coming in soon after symptoms develop should be treated early. But treatment needs to balance rapid delivery with adequate testing. Sometimes, when there is some time to spare before the optimum treatment window closes we can do a more thorough examination and address lingering questions,” Dr. Rossi said.
The decision to get more information about the patient’s condition reflects the goal to give tPA as soon as safely possible to the right patients. While laudable, the study highlights that the timing of treatment can be improved.
Dr. Rossi reported having no financial disclosures.
BALTIMORE – Going to the hospital soon after the development of symptoms of acute ischemic stroke may not guarantee quick treatment.
A study of 1,865 patients treated within the past decade at a large urban comprehensive stroke center has revealed delayed treatment with tissue plasminogen activator, compared with patients who came to the emergency room hours after symptom development, Dr. Kyle C. Rossi said at the annual meeting of the American Neurological Association.
Treatment with tissue plasminogen activator (tPA) within 3 hours after the first symptoms of acute ischemic stroke definitely improves long-term outcomes, but meeting this target time remains a challenge. Patients who present to the emergency room soon after symptom development would seemingly have an advantage, yet Dr. Rossi’s preliminary scrutiny of patient records at Mount Sinai raised doubts about this and prompted the present study.
The hypothesis was that cases with a shorter time between symptom development and diagnosis of stroke (last known well-to-stroke code time, or LKW-to-code) will have a longer time between diagnosis and tPA administration (code-to-tPA), “possibly due to the perception on the part of evaluating physicians of sufficient remaining time before the end of the tPA window.”
The researchers examined patient records from the American Heart Association/American Stroke Association’s “Get with the Guidelines” stroke program, a voluntary observational registry for patients with acute stroke. Of the 1,865 ischemic stroke patients treated during 2009-2015, 122 who received intravenous tPA were allocated to three LKW-to-code groups: within an hour (38 patients), within the next hour (49 patients), or 2 hours or more (35 patients).
The patients tended to be in their late 60s. Just over half were female, and about 40% were white.
Overall, the average LKW-to-code time was 91 ± 48 minutes and the average code-to-tPA time was 67 ± 26 minutes.
Average code-to-tPA times were 80, 67, and 52 minutes, respectively, for the three groups (P less than .0001). On average, it took 28 minutes longer to give tPA to patients who presented within an hour than to patients presenting 2 hours or longer after their first stroke symptom. There was an increase in code-to-tPA time of 1 minute for every decrease in LKW-to-code time of 4 minutes (P less than .0001).
The delay in the time to treat patients who arrive sooner after development of stroke symptoms may result from a decision made by the evaluating neurologist to conduct additional testing prior to administering tPA. Sometimes other staff may be unaware of the decision to delay treatment, according to Dr. Rossi and his colleagues.
“Absolutely, folks coming in soon after symptoms develop should be treated early. But treatment needs to balance rapid delivery with adequate testing. Sometimes, when there is some time to spare before the optimum treatment window closes we can do a more thorough examination and address lingering questions,” Dr. Rossi said.
The decision to get more information about the patient’s condition reflects the goal to give tPA as soon as safely possible to the right patients. While laudable, the study highlights that the timing of treatment can be improved.
Dr. Rossi reported having no financial disclosures.
BALTIMORE – Going to the hospital soon after the development of symptoms of acute ischemic stroke may not guarantee quick treatment.
A study of 1,865 patients treated within the past decade at a large urban comprehensive stroke center has revealed delayed treatment with tissue plasminogen activator, compared with patients who came to the emergency room hours after symptom development, Dr. Kyle C. Rossi said at the annual meeting of the American Neurological Association.
Treatment with tissue plasminogen activator (tPA) within 3 hours after the first symptoms of acute ischemic stroke definitely improves long-term outcomes, but meeting this target time remains a challenge. Patients who present to the emergency room soon after symptom development would seemingly have an advantage, yet Dr. Rossi’s preliminary scrutiny of patient records at Mount Sinai raised doubts about this and prompted the present study.
The hypothesis was that cases with a shorter time between symptom development and diagnosis of stroke (last known well-to-stroke code time, or LKW-to-code) will have a longer time between diagnosis and tPA administration (code-to-tPA), “possibly due to the perception on the part of evaluating physicians of sufficient remaining time before the end of the tPA window.”
The researchers examined patient records from the American Heart Association/American Stroke Association’s “Get with the Guidelines” stroke program, a voluntary observational registry for patients with acute stroke. Of the 1,865 ischemic stroke patients treated during 2009-2015, 122 who received intravenous tPA were allocated to three LKW-to-code groups: within an hour (38 patients), within the next hour (49 patients), or 2 hours or more (35 patients).
The patients tended to be in their late 60s. Just over half were female, and about 40% were white.
Overall, the average LKW-to-code time was 91 ± 48 minutes and the average code-to-tPA time was 67 ± 26 minutes.
Average code-to-tPA times were 80, 67, and 52 minutes, respectively, for the three groups (P less than .0001). On average, it took 28 minutes longer to give tPA to patients who presented within an hour than to patients presenting 2 hours or longer after their first stroke symptom. There was an increase in code-to-tPA time of 1 minute for every decrease in LKW-to-code time of 4 minutes (P less than .0001).
The delay in the time to treat patients who arrive sooner after development of stroke symptoms may result from a decision made by the evaluating neurologist to conduct additional testing prior to administering tPA. Sometimes other staff may be unaware of the decision to delay treatment, according to Dr. Rossi and his colleagues.
“Absolutely, folks coming in soon after symptoms develop should be treated early. But treatment needs to balance rapid delivery with adequate testing. Sometimes, when there is some time to spare before the optimum treatment window closes we can do a more thorough examination and address lingering questions,” Dr. Rossi said.
The decision to get more information about the patient’s condition reflects the goal to give tPA as soon as safely possible to the right patients. While laudable, the study highlights that the timing of treatment can be improved.
Dr. Rossi reported having no financial disclosures.
AT ANA 2016
Key clinical point:
Major finding: TPA was delivered 28 minutes longer on average for patients presenting less than 1 hour after stroke symptoms, compared with patients presenting more than 2 hours after.
Data source: Analysis of 1,865 patients with acute ischemic stroke in the American Heart Association/American Stroke Association’s “Get with the Guidelines” stroke program who were diagnosed at Mount Sinai Hospital in New York.
Disclosures: Dr. Rossi reported having no financial disclosures.
FDA reaffirms rivaroxaban’s atrial fib efficacy in ROCKET AF
The Food and Drug Administration reaffirmed its confidence in the data supporting the claim that rivaroxaban (Xarelto) is a safe and effective alternative to warfarin for preventing strokes and blood clots in patients with nonvalvular atrial fibrillation.
“The FDA concludes that Xarelto is a safe and effective alternative to warfarin in patients with atrial fibrillation,” the agency said in a statement released on Oct. 11.
In response to these events the FDA “completed a variety of analyses to assess the impact that this faulty monitoring device had on the ROCKET AF study results. The agency has determined that effects on strokes or bleeding, including bleeding in the head, were minimal,” the agency said in its statement.
Researchers associated with ROCKET AF published their own analysis of the impact of the faulty device on bleeding rates among patients treated with warfarin in the trial and concluded that device malfunction did not appear to influence the results (N Engl J Med. 2016 Feb 25;374[8]:785-8).
Rivaroxaban is one of four new oral anticoagulants (NOACs) on the U.S. market that are alternatives to warfarin for stroke and clot prevention in patients with nonvalvular atrial fibrillation. An analysis of 2014 data on U.S. office-based prescriptions for NOACs in atrial fibrillation patients showed that rivaroxaban was by far the most commonly prescribed drug in the class, prescribed for patients during 48% of physician office visits that led to a NOAC prescription (Am J Med. 2015 Dec;128[12]:1300-5).
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
The Food and Drug Administration reaffirmed its confidence in the data supporting the claim that rivaroxaban (Xarelto) is a safe and effective alternative to warfarin for preventing strokes and blood clots in patients with nonvalvular atrial fibrillation.
“The FDA concludes that Xarelto is a safe and effective alternative to warfarin in patients with atrial fibrillation,” the agency said in a statement released on Oct. 11.
In response to these events the FDA “completed a variety of analyses to assess the impact that this faulty monitoring device had on the ROCKET AF study results. The agency has determined that effects on strokes or bleeding, including bleeding in the head, were minimal,” the agency said in its statement.
Researchers associated with ROCKET AF published their own analysis of the impact of the faulty device on bleeding rates among patients treated with warfarin in the trial and concluded that device malfunction did not appear to influence the results (N Engl J Med. 2016 Feb 25;374[8]:785-8).
Rivaroxaban is one of four new oral anticoagulants (NOACs) on the U.S. market that are alternatives to warfarin for stroke and clot prevention in patients with nonvalvular atrial fibrillation. An analysis of 2014 data on U.S. office-based prescriptions for NOACs in atrial fibrillation patients showed that rivaroxaban was by far the most commonly prescribed drug in the class, prescribed for patients during 48% of physician office visits that led to a NOAC prescription (Am J Med. 2015 Dec;128[12]:1300-5).
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
The Food and Drug Administration reaffirmed its confidence in the data supporting the claim that rivaroxaban (Xarelto) is a safe and effective alternative to warfarin for preventing strokes and blood clots in patients with nonvalvular atrial fibrillation.
“The FDA concludes that Xarelto is a safe and effective alternative to warfarin in patients with atrial fibrillation,” the agency said in a statement released on Oct. 11.
In response to these events the FDA “completed a variety of analyses to assess the impact that this faulty monitoring device had on the ROCKET AF study results. The agency has determined that effects on strokes or bleeding, including bleeding in the head, were minimal,” the agency said in its statement.
Researchers associated with ROCKET AF published their own analysis of the impact of the faulty device on bleeding rates among patients treated with warfarin in the trial and concluded that device malfunction did not appear to influence the results (N Engl J Med. 2016 Feb 25;374[8]:785-8).
Rivaroxaban is one of four new oral anticoagulants (NOACs) on the U.S. market that are alternatives to warfarin for stroke and clot prevention in patients with nonvalvular atrial fibrillation. An analysis of 2014 data on U.S. office-based prescriptions for NOACs in atrial fibrillation patients showed that rivaroxaban was by far the most commonly prescribed drug in the class, prescribed for patients during 48% of physician office visits that led to a NOAC prescription (Am J Med. 2015 Dec;128[12]:1300-5).
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
Rivaroxaban linked to more bleeding compared with dabigatran in elderly patients with nonvalvular AF
Rivaroxaban is associated with significantly more intra- and extracranial bleeding than is dabigatran in older patients who have nonvalvular atrial fibrillation, according to a report published online Oct. 3 in JAMA Internal Medicine.
This is the principal finding of a retrospective cohort study – the only study to directly compare the two oral non–vitamin-K-antagonists – that involved more than 118,000 patients who initiated anticoagulation treatment during a 2.5-year period. The Centers for Medicare & Medicaid Services and the Food and Drug Administration jointly conducted the study.
During the study period, rivaroxaban was used 2-3 times more often than was dabigatran in AF patients in the United States, “perhaps partly because of prescriber misperceptions about bleeding risks with dabigatran, arising from FDA receipt of a large number of postmarketing case reports following its approval. Ironically, we [now find] substantially higher bleeding risks with use of rivaroxaban than dabigatran,” said David J. Graham, MD, of the Office of Surveillance and Epidemiology, Center for Drug Evaluation and Research, FDA, Silver Spring, Md., and his associates.
The researchers assessed Medicare beneficiaries who initiated standard oral doses of rivaroxaban (66,651 patients) or dabigatran (52,240 patients) and were followed for a mean of 110 days.
The primary outcome measure – a composite of thromboembolic stroke, intracranial hemorrhage, major extracranial bleeding events including GI bleeding, and mortality – occurred in significantly more patients taking rivaroxaban than in those taking dabigatran. When the individual components of this composite outcome were considered, rivaroxaban was associated with significant increases in intracranial hemorrhage (HR, 1.65), major extracranial bleeding (HR, 1.48), and major GI bleeding (HR, 1.40); a nonsignificant decrease in thromboembolic stroke (HR, 0.81); and a nonsignificant increase in mortality (HR, 1.15).
In a further analysis of the data, rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment. In addition, rivaroxaban was associated with a significantly increased risk of death in two subgroups of patients: those aged 75 and older and those whose CHADS-2 scores indicated higher bleeding risk, Dr. Graham and his associates said (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.5954).
Of note, “the net increase in intracranial hemorrhage, the outcome with the highest case fatality rate, exceeded the net reduction in thromboembolic stroke” with rivaroxaban treatment, they added.
This “milestone” study offers real-world data for a large number of older patients with multiple comorbidities who constitute the rising tide of the AF population.
The findings should lead physicians to prescribe dabigatran over rivaroxaban in most patients with AF. Even though this was a retrospective cohort study, there are no prospective randomized trials directly comparing the two non–vitamin-K oral anticoagulants, and the few indirect comparisons derived from clinical trial data are very limited.
Anna L. Parks, MD, is at the University of California, San Francisco. Rita F. Redberg, M.D., is the editor of JAMA Internal Medicine and professor of cardiology at UCSF. Dr. Parks and Dr. Redberg made these remarks in an Editor’s Note accompanying Dr. Graham’s report (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.6429).
This “milestone” study offers real-world data for a large number of older patients with multiple comorbidities who constitute the rising tide of the AF population.
The findings should lead physicians to prescribe dabigatran over rivaroxaban in most patients with AF. Even though this was a retrospective cohort study, there are no prospective randomized trials directly comparing the two non–vitamin-K oral anticoagulants, and the few indirect comparisons derived from clinical trial data are very limited.
Anna L. Parks, MD, is at the University of California, San Francisco. Rita F. Redberg, M.D., is the editor of JAMA Internal Medicine and professor of cardiology at UCSF. Dr. Parks and Dr. Redberg made these remarks in an Editor’s Note accompanying Dr. Graham’s report (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.6429).
This “milestone” study offers real-world data for a large number of older patients with multiple comorbidities who constitute the rising tide of the AF population.
The findings should lead physicians to prescribe dabigatran over rivaroxaban in most patients with AF. Even though this was a retrospective cohort study, there are no prospective randomized trials directly comparing the two non–vitamin-K oral anticoagulants, and the few indirect comparisons derived from clinical trial data are very limited.
Anna L. Parks, MD, is at the University of California, San Francisco. Rita F. Redberg, M.D., is the editor of JAMA Internal Medicine and professor of cardiology at UCSF. Dr. Parks and Dr. Redberg made these remarks in an Editor’s Note accompanying Dr. Graham’s report (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.6429).
Rivaroxaban is associated with significantly more intra- and extracranial bleeding than is dabigatran in older patients who have nonvalvular atrial fibrillation, according to a report published online Oct. 3 in JAMA Internal Medicine.
This is the principal finding of a retrospective cohort study – the only study to directly compare the two oral non–vitamin-K-antagonists – that involved more than 118,000 patients who initiated anticoagulation treatment during a 2.5-year period. The Centers for Medicare & Medicaid Services and the Food and Drug Administration jointly conducted the study.
During the study period, rivaroxaban was used 2-3 times more often than was dabigatran in AF patients in the United States, “perhaps partly because of prescriber misperceptions about bleeding risks with dabigatran, arising from FDA receipt of a large number of postmarketing case reports following its approval. Ironically, we [now find] substantially higher bleeding risks with use of rivaroxaban than dabigatran,” said David J. Graham, MD, of the Office of Surveillance and Epidemiology, Center for Drug Evaluation and Research, FDA, Silver Spring, Md., and his associates.
The researchers assessed Medicare beneficiaries who initiated standard oral doses of rivaroxaban (66,651 patients) or dabigatran (52,240 patients) and were followed for a mean of 110 days.
The primary outcome measure – a composite of thromboembolic stroke, intracranial hemorrhage, major extracranial bleeding events including GI bleeding, and mortality – occurred in significantly more patients taking rivaroxaban than in those taking dabigatran. When the individual components of this composite outcome were considered, rivaroxaban was associated with significant increases in intracranial hemorrhage (HR, 1.65), major extracranial bleeding (HR, 1.48), and major GI bleeding (HR, 1.40); a nonsignificant decrease in thromboembolic stroke (HR, 0.81); and a nonsignificant increase in mortality (HR, 1.15).
In a further analysis of the data, rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment. In addition, rivaroxaban was associated with a significantly increased risk of death in two subgroups of patients: those aged 75 and older and those whose CHADS-2 scores indicated higher bleeding risk, Dr. Graham and his associates said (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.5954).
Of note, “the net increase in intracranial hemorrhage, the outcome with the highest case fatality rate, exceeded the net reduction in thromboembolic stroke” with rivaroxaban treatment, they added.
Rivaroxaban is associated with significantly more intra- and extracranial bleeding than is dabigatran in older patients who have nonvalvular atrial fibrillation, according to a report published online Oct. 3 in JAMA Internal Medicine.
This is the principal finding of a retrospective cohort study – the only study to directly compare the two oral non–vitamin-K-antagonists – that involved more than 118,000 patients who initiated anticoagulation treatment during a 2.5-year period. The Centers for Medicare & Medicaid Services and the Food and Drug Administration jointly conducted the study.
During the study period, rivaroxaban was used 2-3 times more often than was dabigatran in AF patients in the United States, “perhaps partly because of prescriber misperceptions about bleeding risks with dabigatran, arising from FDA receipt of a large number of postmarketing case reports following its approval. Ironically, we [now find] substantially higher bleeding risks with use of rivaroxaban than dabigatran,” said David J. Graham, MD, of the Office of Surveillance and Epidemiology, Center for Drug Evaluation and Research, FDA, Silver Spring, Md., and his associates.
The researchers assessed Medicare beneficiaries who initiated standard oral doses of rivaroxaban (66,651 patients) or dabigatran (52,240 patients) and were followed for a mean of 110 days.
The primary outcome measure – a composite of thromboembolic stroke, intracranial hemorrhage, major extracranial bleeding events including GI bleeding, and mortality – occurred in significantly more patients taking rivaroxaban than in those taking dabigatran. When the individual components of this composite outcome were considered, rivaroxaban was associated with significant increases in intracranial hemorrhage (HR, 1.65), major extracranial bleeding (HR, 1.48), and major GI bleeding (HR, 1.40); a nonsignificant decrease in thromboembolic stroke (HR, 0.81); and a nonsignificant increase in mortality (HR, 1.15).
In a further analysis of the data, rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment. In addition, rivaroxaban was associated with a significantly increased risk of death in two subgroups of patients: those aged 75 and older and those whose CHADS-2 scores indicated higher bleeding risk, Dr. Graham and his associates said (JAMA Intern. Med. 2016 Oct 3. doi: 10.1001/jamainternmed.2016.5954).
Of note, “the net increase in intracranial hemorrhage, the outcome with the highest case fatality rate, exceeded the net reduction in thromboembolic stroke” with rivaroxaban treatment, they added.
Key clinical point: Rivaroxaban is associated with significantly more intra- and extracranial bleeding than dabigatran in patients aged 75 and older with nonvalvular atrial fibrillation.
Major finding: Rivaroxaban was linked to 2.3 excess cases of intracranial hemorrhage, 13 excess cases of major extracranial bleeding, 9.4 excess cases of major GI bleeding, and 3.1 excess deaths per 1,000 person-years of treatment.
Data source: A retrospective cohort study of 118,891 patients aged 65 and older who initiated anticoagulation therapy for AF during a 2.5-year period.
Disclosures: This study was conducted by employees or contractors of the Centers for Medicare & Medicaid Services and the Food and Drug Administration. Dr. Graham and his associates reported having no relevant financial disclosures.
Algorithm for suspected pulmonary embolism safely cut CT rate
ROME – A newly validated, simplified algorithm for the management of patients with suspected acute pulmonary embolism enables physicians to safely exclude the disorder in roughly half of patients without resorting to CT pulmonary angiography, Tom van der Hulle, MD, reported at the annual congress of the European Society of Cardiology.
“This is the largest study ever performed in the diagnostic management of suspected pulmonary embolism. Based on our results, I think the YEARS algorithm is ready to be used in daily clinical practice,” declared Dr. van der Hulle of the department of thrombosis and hemostasis at Leiden (the Netherlands) University Medical Center.
Using the YEARS algorithm, PE was reliably ruled out without need for CT pulmonary angiography – considered the standard in the diagnosis of PE – in 48% of patients. In contrast, adherence to the Wells rule would have meant that 62% of patients would have gotten a CT scan to rule out PE with a comparably high degree of accuracy.
But that 62% figure underestimates the actual CT rate in clinical practice. The reality is that although the guideline-recommended Wells rule and revised Geneva score have been shown to be safe and accurate, they are so complex, cumbersome, and out of sync with the flow of routine clinical practice that many physicians skip the algorithms and go straight to CT, Dr. van der Hulle said. This approach results in many unnecessary CTs, needlessly exposing patients to the risks of radiation and intravenous contrast material while driving up health care costs, he added.
Using the Wells rule or revised Geneva score, the patient evaluation begins with an assessment of the clinical probability of PE based upon a risk score involving seven or eight factors. Only patients with a low or intermediate clinical probability of PE get a D-dimer test; those with a high clinical probability go straight to CT.
The YEARS algorithm is much simpler than that, Dr. van der Hulle explained. Everyone who presents with suspected acute PE gets a D-dimer test while the physician simultaneously applies a brief, three-item clinical prediction rule. These three items were selected by the Dutch investigators because they were the three strongest predictors of PE out of the original seven in the Wells rule. They are hemoptysis, clinical signs of deep vein thrombosis such as leg swelling or hyperpigmentation, and the clinician’s global impression of PE as being the most likely diagnosis.
In the YEARS algorithm, the threshold for a positive D-dimer test warranting CT pulmonary angiography depends upon whether any of the three clinical predictors is present. If none is present, the threshold is 1,000 ng/mL or above; if one or more is present, the threshold for a positive D-dimer test drops to 500 ng/mL.
Using these criteria, PE was excluded without resort to CT in 1,306 patients with none of the three YEARS items and a D-dimer test result below 1,000 ng/mL, as well as in another 327 patients with one or more YEARS items present but a D-dimer below 500 ng/mL. Those two groups were left untreated and followed prospectively for 3 months.
The 964 patients with one or more YEARS predictors present and a D-dimer score of at least 500 ng/mL underwent CT imaging, as did the 352 with no YEARS items and a D-dimer of at least 1,000 ng/mL.
The prevalence of CT-confirmed PE in the study was 13.2%. Affected patients were treated with anticoagulants.
The primary study endpoint was the total rate of deep vein thrombosis during 3 months of follow-up after PE had been excluded. The rate was 0.61%, including a fatal PE rate of 0.20%. The rate in patients managed without CT was 0.43%, including a 0.12% rate of fatal PE. In patients managed with diagnostic CT, the deep vein thrombosis rate was 0.84%, with a fatal PE rate of 0.30%.
“I think these results are completely comparable to those in previous studies using the standard algorithms,” Dr. van der Hulle commented.
The study’s main limitation is that it wasn’t a randomized, controlled trial. But given the tiny event rates, detecting any small differences between management strategies would require an unrealistically huge sample size, he added.
Asked if he thinks physicians will actually use the new tool, Dr. van der Hulle replied that some physicians feel driven to be 100% sure that a patient doesn’t have PE, and they will probably keep overordering CT scans. But others will embrace the YEARS algorithm because it reduces wasted resources and minimizes radiation exposure, a particularly compelling consideration in young female patients.
Discussant Marion Delcroix, MD, had reservations. She said she appreciated the appeal of a simple algorithm, but she asked, “Couldn’t we do better with a bit more sophistication, perhaps by adjusting the D-dimer cutoff for age and also adding some other items, like oxygen saturation and estrogen use?
“My concern is about the applicability. The age of the study cohort is relatively young, at a mean of 53 years. The peak age of PE in a very large contemporary German database is 70-80 years. We don’t know if the YEARS score is any good in this older population,” asserted Dr. Delcroix, professor of medicine and respiratory physiology and head of the center for pulmonary vascular diseases at University Hospital in Leuven, Belgium.
“If the aim is to decrease the number of CT pulmonary angiograms for safety reasons, why not reintroduce compression ultrasound of the lower limbs in the diagnostic algorithm?” she continued. “It has been shown to effectively reduce the need for further imaging.”
Dr. Delcroix predicted that the YEARS algorithm study will prove “too optimistic” regarding the number of CT scans avoided, particularly in elderly patients.
The YEARS study was funded by the trial’s 12 participating Dutch hospitals. Dr. van der Hulle reported having no financial conflicts of interest.
ROME – A newly validated, simplified algorithm for the management of patients with suspected acute pulmonary embolism enables physicians to safely exclude the disorder in roughly half of patients without resorting to CT pulmonary angiography, Tom van der Hulle, MD, reported at the annual congress of the European Society of Cardiology.
“This is the largest study ever performed in the diagnostic management of suspected pulmonary embolism. Based on our results, I think the YEARS algorithm is ready to be used in daily clinical practice,” declared Dr. van der Hulle of the department of thrombosis and hemostasis at Leiden (the Netherlands) University Medical Center.
Using the YEARS algorithm, PE was reliably ruled out without need for CT pulmonary angiography – considered the standard in the diagnosis of PE – in 48% of patients. In contrast, adherence to the Wells rule would have meant that 62% of patients would have gotten a CT scan to rule out PE with a comparably high degree of accuracy.
But that 62% figure underestimates the actual CT rate in clinical practice. The reality is that although the guideline-recommended Wells rule and revised Geneva score have been shown to be safe and accurate, they are so complex, cumbersome, and out of sync with the flow of routine clinical practice that many physicians skip the algorithms and go straight to CT, Dr. van der Hulle said. This approach results in many unnecessary CTs, needlessly exposing patients to the risks of radiation and intravenous contrast material while driving up health care costs, he added.
Using the Wells rule or revised Geneva score, the patient evaluation begins with an assessment of the clinical probability of PE based upon a risk score involving seven or eight factors. Only patients with a low or intermediate clinical probability of PE get a D-dimer test; those with a high clinical probability go straight to CT.
The YEARS algorithm is much simpler than that, Dr. van der Hulle explained. Everyone who presents with suspected acute PE gets a D-dimer test while the physician simultaneously applies a brief, three-item clinical prediction rule. These three items were selected by the Dutch investigators because they were the three strongest predictors of PE out of the original seven in the Wells rule. They are hemoptysis, clinical signs of deep vein thrombosis such as leg swelling or hyperpigmentation, and the clinician’s global impression of PE as being the most likely diagnosis.
In the YEARS algorithm, the threshold for a positive D-dimer test warranting CT pulmonary angiography depends upon whether any of the three clinical predictors is present. If none is present, the threshold is 1,000 ng/mL or above; if one or more is present, the threshold for a positive D-dimer test drops to 500 ng/mL.
Using these criteria, PE was excluded without resort to CT in 1,306 patients with none of the three YEARS items and a D-dimer test result below 1,000 ng/mL, as well as in another 327 patients with one or more YEARS items present but a D-dimer below 500 ng/mL. Those two groups were left untreated and followed prospectively for 3 months.
The 964 patients with one or more YEARS predictors present and a D-dimer score of at least 500 ng/mL underwent CT imaging, as did the 352 with no YEARS items and a D-dimer of at least 1,000 ng/mL.
The prevalence of CT-confirmed PE in the study was 13.2%. Affected patients were treated with anticoagulants.
The primary study endpoint was the total rate of deep vein thrombosis during 3 months of follow-up after PE had been excluded. The rate was 0.61%, including a fatal PE rate of 0.20%. The rate in patients managed without CT was 0.43%, including a 0.12% rate of fatal PE. In patients managed with diagnostic CT, the deep vein thrombosis rate was 0.84%, with a fatal PE rate of 0.30%.
“I think these results are completely comparable to those in previous studies using the standard algorithms,” Dr. van der Hulle commented.
The study’s main limitation is that it wasn’t a randomized, controlled trial. But given the tiny event rates, detecting any small differences between management strategies would require an unrealistically huge sample size, he added.
Asked if he thinks physicians will actually use the new tool, Dr. van der Hulle replied that some physicians feel driven to be 100% sure that a patient doesn’t have PE, and they will probably keep overordering CT scans. But others will embrace the YEARS algorithm because it reduces wasted resources and minimizes radiation exposure, a particularly compelling consideration in young female patients.
Discussant Marion Delcroix, MD, had reservations. She said she appreciated the appeal of a simple algorithm, but she asked, “Couldn’t we do better with a bit more sophistication, perhaps by adjusting the D-dimer cutoff for age and also adding some other items, like oxygen saturation and estrogen use?
“My concern is about the applicability. The age of the study cohort is relatively young, at a mean of 53 years. The peak age of PE in a very large contemporary German database is 70-80 years. We don’t know if the YEARS score is any good in this older population,” asserted Dr. Delcroix, professor of medicine and respiratory physiology and head of the center for pulmonary vascular diseases at University Hospital in Leuven, Belgium.
“If the aim is to decrease the number of CT pulmonary angiograms for safety reasons, why not reintroduce compression ultrasound of the lower limbs in the diagnostic algorithm?” she continued. “It has been shown to effectively reduce the need for further imaging.”
Dr. Delcroix predicted that the YEARS algorithm study will prove “too optimistic” regarding the number of CT scans avoided, particularly in elderly patients.
The YEARS study was funded by the trial’s 12 participating Dutch hospitals. Dr. van der Hulle reported having no financial conflicts of interest.
ROME – A newly validated, simplified algorithm for the management of patients with suspected acute pulmonary embolism enables physicians to safely exclude the disorder in roughly half of patients without resorting to CT pulmonary angiography, Tom van der Hulle, MD, reported at the annual congress of the European Society of Cardiology.
“This is the largest study ever performed in the diagnostic management of suspected pulmonary embolism. Based on our results, I think the YEARS algorithm is ready to be used in daily clinical practice,” declared Dr. van der Hulle of the department of thrombosis and hemostasis at Leiden (the Netherlands) University Medical Center.
Using the YEARS algorithm, PE was reliably ruled out without need for CT pulmonary angiography – considered the standard in the diagnosis of PE – in 48% of patients. In contrast, adherence to the Wells rule would have meant that 62% of patients would have gotten a CT scan to rule out PE with a comparably high degree of accuracy.
But that 62% figure underestimates the actual CT rate in clinical practice. The reality is that although the guideline-recommended Wells rule and revised Geneva score have been shown to be safe and accurate, they are so complex, cumbersome, and out of sync with the flow of routine clinical practice that many physicians skip the algorithms and go straight to CT, Dr. van der Hulle said. This approach results in many unnecessary CTs, needlessly exposing patients to the risks of radiation and intravenous contrast material while driving up health care costs, he added.
Using the Wells rule or revised Geneva score, the patient evaluation begins with an assessment of the clinical probability of PE based upon a risk score involving seven or eight factors. Only patients with a low or intermediate clinical probability of PE get a D-dimer test; those with a high clinical probability go straight to CT.
The YEARS algorithm is much simpler than that, Dr. van der Hulle explained. Everyone who presents with suspected acute PE gets a D-dimer test while the physician simultaneously applies a brief, three-item clinical prediction rule. These three items were selected by the Dutch investigators because they were the three strongest predictors of PE out of the original seven in the Wells rule. They are hemoptysis, clinical signs of deep vein thrombosis such as leg swelling or hyperpigmentation, and the clinician’s global impression of PE as being the most likely diagnosis.
In the YEARS algorithm, the threshold for a positive D-dimer test warranting CT pulmonary angiography depends upon whether any of the three clinical predictors is present. If none is present, the threshold is 1,000 ng/mL or above; if one or more is present, the threshold for a positive D-dimer test drops to 500 ng/mL.
Using these criteria, PE was excluded without resort to CT in 1,306 patients with none of the three YEARS items and a D-dimer test result below 1,000 ng/mL, as well as in another 327 patients with one or more YEARS items present but a D-dimer below 500 ng/mL. Those two groups were left untreated and followed prospectively for 3 months.
The 964 patients with one or more YEARS predictors present and a D-dimer score of at least 500 ng/mL underwent CT imaging, as did the 352 with no YEARS items and a D-dimer of at least 1,000 ng/mL.
The prevalence of CT-confirmed PE in the study was 13.2%. Affected patients were treated with anticoagulants.
The primary study endpoint was the total rate of deep vein thrombosis during 3 months of follow-up after PE had been excluded. The rate was 0.61%, including a fatal PE rate of 0.20%. The rate in patients managed without CT was 0.43%, including a 0.12% rate of fatal PE. In patients managed with diagnostic CT, the deep vein thrombosis rate was 0.84%, with a fatal PE rate of 0.30%.
“I think these results are completely comparable to those in previous studies using the standard algorithms,” Dr. van der Hulle commented.
The study’s main limitation is that it wasn’t a randomized, controlled trial. But given the tiny event rates, detecting any small differences between management strategies would require an unrealistically huge sample size, he added.
Asked if he thinks physicians will actually use the new tool, Dr. van der Hulle replied that some physicians feel driven to be 100% sure that a patient doesn’t have PE, and they will probably keep overordering CT scans. But others will embrace the YEARS algorithm because it reduces wasted resources and minimizes radiation exposure, a particularly compelling consideration in young female patients.
Discussant Marion Delcroix, MD, had reservations. She said she appreciated the appeal of a simple algorithm, but she asked, “Couldn’t we do better with a bit more sophistication, perhaps by adjusting the D-dimer cutoff for age and also adding some other items, like oxygen saturation and estrogen use?
“My concern is about the applicability. The age of the study cohort is relatively young, at a mean of 53 years. The peak age of PE in a very large contemporary German database is 70-80 years. We don’t know if the YEARS score is any good in this older population,” asserted Dr. Delcroix, professor of medicine and respiratory physiology and head of the center for pulmonary vascular diseases at University Hospital in Leuven, Belgium.
“If the aim is to decrease the number of CT pulmonary angiograms for safety reasons, why not reintroduce compression ultrasound of the lower limbs in the diagnostic algorithm?” she continued. “It has been shown to effectively reduce the need for further imaging.”
Dr. Delcroix predicted that the YEARS algorithm study will prove “too optimistic” regarding the number of CT scans avoided, particularly in elderly patients.
The YEARS study was funded by the trial’s 12 participating Dutch hospitals. Dr. van der Hulle reported having no financial conflicts of interest.
Key clinical point:
Major finding: Applying the YEARS algorithm to a large population of patients with suspected PE, the 3-month incidence of deep vein thrombosis after PE had been excluded was 0.61%.
Data source: This was a prospective study of clinical outcomes in nearly 3,000 consecutive Dutch patients who presented with suspected acute PE and were managed in accord with the YEARS algorithm.
Disclosures: The YEARS algorithm validation study was funded by the trial’s 12 participating Dutch hospitals. The study presenter reported having no financial conflicts of interest.
CABG best for diabetes patients with CKD – or is it?
ROME – The use of coronary artery bypass graft surgery for revascularization in patients with multivessel CAD and comorbid diabetes plus chronic kidney disease was associated with a significantly lower risk of major cardiovascular and cerebrovascular events than was PCI with first-generation drug-eluting stents in a new secondary analysis from the landmark FREEDOM trial.
“The reason for this presentation is that even though chronic kidney disease is common in patients with diabetes, until now there has not been a large study of the efficacy and safety of coronary revascularization with drug-eluting stents versus CABG in this population in a randomized trial cohort,” explained Usman Baber, MD, who reported the results at the annual congress of the European Society of Cardiology.
FREEDOM (Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease) randomized 1,900 diabetic patients with multivessel CAD to PCI or CABG. As previously reported, CABG proved superior to PCI, with a significantly lower rate of the composite primary endpoint composed of all-cause mortality, MI, or stroke (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
Dr. Baber presented a post hoc analysis of the 451 FREEDOM participants with baseline comorbid chronic kidney disease (CKD). Their mean SYNTAX score was 27, and their mean baseline estimated glomerular filtration rate was 44 mL/min per 1.73 m2, indicative of mild to moderate CKD.
“Only 28 patients in the FREEDOM trial had an estimated GFR below 30, therefore we can’t make any inferences about revascularization in that setting, which I think is a completely different population,” he noted.
The 5-year rate of major adverse cardiovascular and cerebrovascular events in patients with CKD was 26% in the CABG group, an absolute 9.4% less than the 35.6% rate in subjects randomized to PCI.
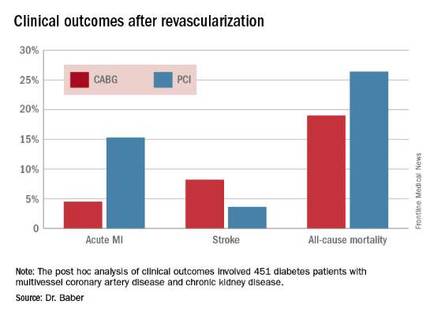
Roughly one-quarter of FREEDOM participants had CKD. They fared significantly worse than did those without CKD. The 5-year incidence of major adverse cardiovascular and cerebrovascular events was 30.8% in patients with CKD and 20.1% in patients without renal impairment. In a multivariate analysis adjusted for age, gender, hypertension, peripheral vascular disease, and other potential confounders, the risk of all-cause mortality was twofold higher in the CKD group. Their risk of cardiac death was increased 1.8-fold, and they were at 1.9-fold increased risk for stroke. Interestingly, however, the acute MI risk did not differ between patients with or without CKD, Dr. Baber observed.
Drilling deeper into the data, the cardiologist reported that CABG was associated with significantly lower rates of MI and a nonsignificant trend for fewer deaths, but with a significantly higher stroke rate than PCI.
One audience member rose to complain that this information won’t be helpful in counseling his diabetic patients with CKD and multivessel CAD because the choices look so grim: a higher risk of MI with percutaneous therapy, and a greater risk of stroke with surgery.
Dr. Baber replied by pointing out that the 10.8% absolute reduction in the risk of MI with CABG compared with PCI was more than twice as large as the absolute 4.6% increase in stroke risk with surgery.
“Most people would say that a heart attack is an inconvenience, and a stroke is a life-changing experience for them and their family,” said session cochair Kim A. Williams, MD, professor of medicine and chairman of cardiology at Rush University Medical Center in Chicago.
At that, Dr. Baber backtracked a bit, observing that since this was a post hoc analysis, the FREEDOM findings in patients with CKD must be viewed as hypothesis-generating rather than definitive. And, of course, contemporary second-generation drug-eluting stents have a better risk/benefit profile than do those used in FREEDOM.
“The number needed to treat/number needed to harm ratio for CABG and PCI probably ends up being roughly equal. The pertinence of an analysis like this is if you look at real-world registry-based data, you find a therapeutic nihilism that’s highly prevalent in CKD patients, where many patients who might benefit are not provided with revascularization therapy. It’s clear that we as clinicians – either because we don’t know there is a benefit or we are too concerned about potential harm – deprive patients of a treatment that might be beneficial. This analysis makes clinicians who might be concerned feel somewhat comforted that there is not unacceptable harm and that there is benefit,” Dr. Baber said.
Follow-up of FREEDOM participants continues and will be the subject of future reports, he added.
The FREEDOM trial was sponsored by the National Heart, Lung and Blood Institute. Dr. Baber reported having no financial conflicts of interest.
ROME – The use of coronary artery bypass graft surgery for revascularization in patients with multivessel CAD and comorbid diabetes plus chronic kidney disease was associated with a significantly lower risk of major cardiovascular and cerebrovascular events than was PCI with first-generation drug-eluting stents in a new secondary analysis from the landmark FREEDOM trial.
“The reason for this presentation is that even though chronic kidney disease is common in patients with diabetes, until now there has not been a large study of the efficacy and safety of coronary revascularization with drug-eluting stents versus CABG in this population in a randomized trial cohort,” explained Usman Baber, MD, who reported the results at the annual congress of the European Society of Cardiology.
FREEDOM (Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease) randomized 1,900 diabetic patients with multivessel CAD to PCI or CABG. As previously reported, CABG proved superior to PCI, with a significantly lower rate of the composite primary endpoint composed of all-cause mortality, MI, or stroke (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
Dr. Baber presented a post hoc analysis of the 451 FREEDOM participants with baseline comorbid chronic kidney disease (CKD). Their mean SYNTAX score was 27, and their mean baseline estimated glomerular filtration rate was 44 mL/min per 1.73 m2, indicative of mild to moderate CKD.
“Only 28 patients in the FREEDOM trial had an estimated GFR below 30, therefore we can’t make any inferences about revascularization in that setting, which I think is a completely different population,” he noted.
The 5-year rate of major adverse cardiovascular and cerebrovascular events in patients with CKD was 26% in the CABG group, an absolute 9.4% less than the 35.6% rate in subjects randomized to PCI.
Roughly one-quarter of FREEDOM participants had CKD. They fared significantly worse than did those without CKD. The 5-year incidence of major adverse cardiovascular and cerebrovascular events was 30.8% in patients with CKD and 20.1% in patients without renal impairment. In a multivariate analysis adjusted for age, gender, hypertension, peripheral vascular disease, and other potential confounders, the risk of all-cause mortality was twofold higher in the CKD group. Their risk of cardiac death was increased 1.8-fold, and they were at 1.9-fold increased risk for stroke. Interestingly, however, the acute MI risk did not differ between patients with or without CKD, Dr. Baber observed.
Drilling deeper into the data, the cardiologist reported that CABG was associated with significantly lower rates of MI and a nonsignificant trend for fewer deaths, but with a significantly higher stroke rate than PCI.
One audience member rose to complain that this information won’t be helpful in counseling his diabetic patients with CKD and multivessel CAD because the choices look so grim: a higher risk of MI with percutaneous therapy, and a greater risk of stroke with surgery.
Dr. Baber replied by pointing out that the 10.8% absolute reduction in the risk of MI with CABG compared with PCI was more than twice as large as the absolute 4.6% increase in stroke risk with surgery.
“Most people would say that a heart attack is an inconvenience, and a stroke is a life-changing experience for them and their family,” said session cochair Kim A. Williams, MD, professor of medicine and chairman of cardiology at Rush University Medical Center in Chicago.
At that, Dr. Baber backtracked a bit, observing that since this was a post hoc analysis, the FREEDOM findings in patients with CKD must be viewed as hypothesis-generating rather than definitive. And, of course, contemporary second-generation drug-eluting stents have a better risk/benefit profile than do those used in FREEDOM.
“The number needed to treat/number needed to harm ratio for CABG and PCI probably ends up being roughly equal. The pertinence of an analysis like this is if you look at real-world registry-based data, you find a therapeutic nihilism that’s highly prevalent in CKD patients, where many patients who might benefit are not provided with revascularization therapy. It’s clear that we as clinicians – either because we don’t know there is a benefit or we are too concerned about potential harm – deprive patients of a treatment that might be beneficial. This analysis makes clinicians who might be concerned feel somewhat comforted that there is not unacceptable harm and that there is benefit,” Dr. Baber said.
Follow-up of FREEDOM participants continues and will be the subject of future reports, he added.
The FREEDOM trial was sponsored by the National Heart, Lung and Blood Institute. Dr. Baber reported having no financial conflicts of interest.
ROME – The use of coronary artery bypass graft surgery for revascularization in patients with multivessel CAD and comorbid diabetes plus chronic kidney disease was associated with a significantly lower risk of major cardiovascular and cerebrovascular events than was PCI with first-generation drug-eluting stents in a new secondary analysis from the landmark FREEDOM trial.
“The reason for this presentation is that even though chronic kidney disease is common in patients with diabetes, until now there has not been a large study of the efficacy and safety of coronary revascularization with drug-eluting stents versus CABG in this population in a randomized trial cohort,” explained Usman Baber, MD, who reported the results at the annual congress of the European Society of Cardiology.
FREEDOM (Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease) randomized 1,900 diabetic patients with multivessel CAD to PCI or CABG. As previously reported, CABG proved superior to PCI, with a significantly lower rate of the composite primary endpoint composed of all-cause mortality, MI, or stroke (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
Dr. Baber presented a post hoc analysis of the 451 FREEDOM participants with baseline comorbid chronic kidney disease (CKD). Their mean SYNTAX score was 27, and their mean baseline estimated glomerular filtration rate was 44 mL/min per 1.73 m2, indicative of mild to moderate CKD.
“Only 28 patients in the FREEDOM trial had an estimated GFR below 30, therefore we can’t make any inferences about revascularization in that setting, which I think is a completely different population,” he noted.
The 5-year rate of major adverse cardiovascular and cerebrovascular events in patients with CKD was 26% in the CABG group, an absolute 9.4% less than the 35.6% rate in subjects randomized to PCI.
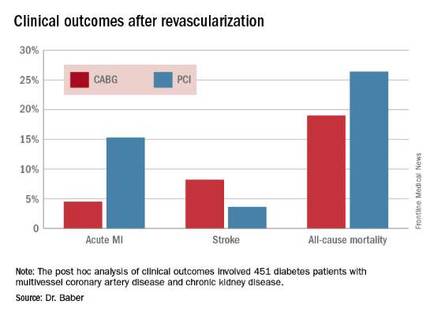
Roughly one-quarter of FREEDOM participants had CKD. They fared significantly worse than did those without CKD. The 5-year incidence of major adverse cardiovascular and cerebrovascular events was 30.8% in patients with CKD and 20.1% in patients without renal impairment. In a multivariate analysis adjusted for age, gender, hypertension, peripheral vascular disease, and other potential confounders, the risk of all-cause mortality was twofold higher in the CKD group. Their risk of cardiac death was increased 1.8-fold, and they were at 1.9-fold increased risk for stroke. Interestingly, however, the acute MI risk did not differ between patients with or without CKD, Dr. Baber observed.
Drilling deeper into the data, the cardiologist reported that CABG was associated with significantly lower rates of MI and a nonsignificant trend for fewer deaths, but with a significantly higher stroke rate than PCI.
One audience member rose to complain that this information won’t be helpful in counseling his diabetic patients with CKD and multivessel CAD because the choices look so grim: a higher risk of MI with percutaneous therapy, and a greater risk of stroke with surgery.
Dr. Baber replied by pointing out that the 10.8% absolute reduction in the risk of MI with CABG compared with PCI was more than twice as large as the absolute 4.6% increase in stroke risk with surgery.
“Most people would say that a heart attack is an inconvenience, and a stroke is a life-changing experience for them and their family,” said session cochair Kim A. Williams, MD, professor of medicine and chairman of cardiology at Rush University Medical Center in Chicago.
At that, Dr. Baber backtracked a bit, observing that since this was a post hoc analysis, the FREEDOM findings in patients with CKD must be viewed as hypothesis-generating rather than definitive. And, of course, contemporary second-generation drug-eluting stents have a better risk/benefit profile than do those used in FREEDOM.
“The number needed to treat/number needed to harm ratio for CABG and PCI probably ends up being roughly equal. The pertinence of an analysis like this is if you look at real-world registry-based data, you find a therapeutic nihilism that’s highly prevalent in CKD patients, where many patients who might benefit are not provided with revascularization therapy. It’s clear that we as clinicians – either because we don’t know there is a benefit or we are too concerned about potential harm – deprive patients of a treatment that might be beneficial. This analysis makes clinicians who might be concerned feel somewhat comforted that there is not unacceptable harm and that there is benefit,” Dr. Baber said.
Follow-up of FREEDOM participants continues and will be the subject of future reports, he added.
The FREEDOM trial was sponsored by the National Heart, Lung and Blood Institute. Dr. Baber reported having no financial conflicts of interest.
AT THE ESC CONGRESS 2016
Key clinical point: Coronary artery bypass graft surgery resulted in fewer myocardial infarctions but more strokes than did percutaneous coronary intervention at 5 years of follow-up in diabetic patients with multivessel coronary artery disease and chronic kidney disease.
Major finding: The cumulative MI rates in patients randomized to CABG versus PCI were 4.5% and 15.3%, respectively, while the stroke rates were 8.2% versus 3.6%.
Data source: A post hoc analysis of clinical outcomes in 451 diabetic patients with multivessel CAD and chronic kidney disease who were randomized to CABG or PCI in the prospective multicenter FREEDOM trial.
Disclosures: The FREEDOM trial was sponsored by the National Heart, Lung, and Blood Institute. The presenter reported having no financial conflicts of interest.