User login
Left liver grafts may benefit from hepatic vein/IVC anastomosis
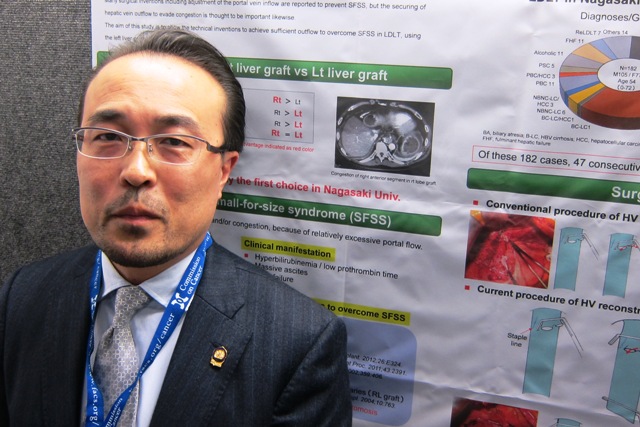
WASHINGTON – A novel anastomosis technique may help avoid small-for-size syndrome in adult living donor liver transplantation, according to Dr. Mitsuhisa Takatsuki.
Reconstructing the hepatic vein by cross-clamping with the inferior vena cava creates improved outflow from the graft. This can avert the potential failure of a left liver graft, which, because of its smaller size, is more prone to the syndrome than is a right liver graft, said Dr. Takatsuki of Nagasaki (Japan) University.
A left liver graft is the first choice for living donor transplant in Japan because this graft is less likely to experience congestion than is a right lobe graft. Donors with a left graft are also less likely to have serious postoperative complications or to die. However, the graft volume of the left liver is less than that of the right, making it susceptible to the problems of a high portal inflow. Dr. Takatsuki’s novel securing of the hepatic vein to the inferior vena cava increases liver outflow and, hopefully, prevents graft congestion, he said at the annual clinical congress of the American College of Surgeons.
The conventional hepatic vein reconstruction side clamps the middle and left hepatic veins. This common trunk is then joined to the graft hepatic vein. Dr. Takatsuki’s technique takes advantage of the inferior vena cava to increase graft outflow, he noted.
He closes the right hepatic vein with a vascular stapler. He then opens the common trunk of the middle and left hepatic veins and creates a wide cavotomy in the inferior vena cava. "This wide orifice of hepatic vein is anastomosed to the graft hepatic vein. The size of the hepatic vein orifice is easily adjustable to suit the size of the graft hepatic vein," Dr. Takatsuki said.
He reported the results of a study of 47 adult living donor transplants. Of these 47 patients, 21 had the side clamp hepatic vein reconstruction and 26, the new technique of cross-clamping the inferior vena cava.
The patients were a mean of 56 years old and evenly split between men and women. The mean Model for End-Stage Liver Disease(MELD) score was 15.5. Surgery lasted a mean of 915 minutes in the side clamp group and 746 minutes in the cross-clamp group – a significant difference. Blood loss was also significantly less in the cross-clamp group (3,800 g vs.5,450 g).
By postoperative day 7, there were no significant between-group differences in total bilirubin or prothrombin time. There was significantly less ascites in the cross-clamp group.
Dr. Takatsuki saw the same results in a subgroup of 17 patients (7 in the side clamp group and 10 in the cross-clamp group) in whom the graft weight/recipient standard liver volume was less than 30%.
Among these patients – who were at the highest risk for graft failure because of the weight/volume differential – those with the cross-clamped anastomosis had significantly higher graft survival (90% vs. 71%) at 1 year.
Dr. Takatsuki said he had no relevant financial disclosures.
WASHINGTON – A novel anastomosis technique may help avoid small-for-size syndrome in adult living donor liver transplantation, according to Dr. Mitsuhisa Takatsuki.
Reconstructing the hepatic vein by cross-clamping with the inferior vena cava creates improved outflow from the graft. This can avert the potential failure of a left liver graft, which, because of its smaller size, is more prone to the syndrome than is a right liver graft, said Dr. Takatsuki of Nagasaki (Japan) University.
A left liver graft is the first choice for living donor transplant in Japan because this graft is less likely to experience congestion than is a right lobe graft. Donors with a left graft are also less likely to have serious postoperative complications or to die. However, the graft volume of the left liver is less than that of the right, making it susceptible to the problems of a high portal inflow. Dr. Takatsuki’s novel securing of the hepatic vein to the inferior vena cava increases liver outflow and, hopefully, prevents graft congestion, he said at the annual clinical congress of the American College of Surgeons.
The conventional hepatic vein reconstruction side clamps the middle and left hepatic veins. This common trunk is then joined to the graft hepatic vein. Dr. Takatsuki’s technique takes advantage of the inferior vena cava to increase graft outflow, he noted.
He closes the right hepatic vein with a vascular stapler. He then opens the common trunk of the middle and left hepatic veins and creates a wide cavotomy in the inferior vena cava. "This wide orifice of hepatic vein is anastomosed to the graft hepatic vein. The size of the hepatic vein orifice is easily adjustable to suit the size of the graft hepatic vein," Dr. Takatsuki said.
He reported the results of a study of 47 adult living donor transplants. Of these 47 patients, 21 had the side clamp hepatic vein reconstruction and 26, the new technique of cross-clamping the inferior vena cava.
The patients were a mean of 56 years old and evenly split between men and women. The mean Model for End-Stage Liver Disease(MELD) score was 15.5. Surgery lasted a mean of 915 minutes in the side clamp group and 746 minutes in the cross-clamp group – a significant difference. Blood loss was also significantly less in the cross-clamp group (3,800 g vs.5,450 g).
By postoperative day 7, there were no significant between-group differences in total bilirubin or prothrombin time. There was significantly less ascites in the cross-clamp group.
Dr. Takatsuki saw the same results in a subgroup of 17 patients (7 in the side clamp group and 10 in the cross-clamp group) in whom the graft weight/recipient standard liver volume was less than 30%.
Among these patients – who were at the highest risk for graft failure because of the weight/volume differential – those with the cross-clamped anastomosis had significantly higher graft survival (90% vs. 71%) at 1 year.
Dr. Takatsuki said he had no relevant financial disclosures.
WASHINGTON – A novel anastomosis technique may help avoid small-for-size syndrome in adult living donor liver transplantation, according to Dr. Mitsuhisa Takatsuki.
Reconstructing the hepatic vein by cross-clamping with the inferior vena cava creates improved outflow from the graft. This can avert the potential failure of a left liver graft, which, because of its smaller size, is more prone to the syndrome than is a right liver graft, said Dr. Takatsuki of Nagasaki (Japan) University.
A left liver graft is the first choice for living donor transplant in Japan because this graft is less likely to experience congestion than is a right lobe graft. Donors with a left graft are also less likely to have serious postoperative complications or to die. However, the graft volume of the left liver is less than that of the right, making it susceptible to the problems of a high portal inflow. Dr. Takatsuki’s novel securing of the hepatic vein to the inferior vena cava increases liver outflow and, hopefully, prevents graft congestion, he said at the annual clinical congress of the American College of Surgeons.
The conventional hepatic vein reconstruction side clamps the middle and left hepatic veins. This common trunk is then joined to the graft hepatic vein. Dr. Takatsuki’s technique takes advantage of the inferior vena cava to increase graft outflow, he noted.
He closes the right hepatic vein with a vascular stapler. He then opens the common trunk of the middle and left hepatic veins and creates a wide cavotomy in the inferior vena cava. "This wide orifice of hepatic vein is anastomosed to the graft hepatic vein. The size of the hepatic vein orifice is easily adjustable to suit the size of the graft hepatic vein," Dr. Takatsuki said.
He reported the results of a study of 47 adult living donor transplants. Of these 47 patients, 21 had the side clamp hepatic vein reconstruction and 26, the new technique of cross-clamping the inferior vena cava.
The patients were a mean of 56 years old and evenly split between men and women. The mean Model for End-Stage Liver Disease(MELD) score was 15.5. Surgery lasted a mean of 915 minutes in the side clamp group and 746 minutes in the cross-clamp group – a significant difference. Blood loss was also significantly less in the cross-clamp group (3,800 g vs.5,450 g).
By postoperative day 7, there were no significant between-group differences in total bilirubin or prothrombin time. There was significantly less ascites in the cross-clamp group.
Dr. Takatsuki saw the same results in a subgroup of 17 patients (7 in the side clamp group and 10 in the cross-clamp group) in whom the graft weight/recipient standard liver volume was less than 30%.
Among these patients – who were at the highest risk for graft failure because of the weight/volume differential – those with the cross-clamped anastomosis had significantly higher graft survival (90% vs. 71%) at 1 year.
Dr. Takatsuki said he had no relevant financial disclosures.
AT THE ACS Clincal Congress
Major finding: One-year liver graft survival was significantly better in patients with a hepatic vein/inferior vena cava anastomosis than in those who had the traditional hepatic vein side clamp (90% vs. 71%).
Data source: A randomized study involving 47 patients who received a living donor left liver transplant.
Disclosures: Dr. Takatsuki said he had no relevant financial disclosures.
In HCC, histology and parenchyma more important than tumor size
ORLANDO – In hepatocellular carcinoma, tumor size did not independently influence recurrence or survival, whereas tumor histopathology and background parenchyma did, according to a retrospective, single-center study of 300 patients.
"These findings further support that prognosis and treatment guidelines cannot be effectively categorized based on tumor size," said Dr. Michael D. Kluger of the department of surgery at New York-Presbyterian Hospital–Cornell University, New York.
Although the procedure is hampered by high recurrence rates, resection is safe, readily available, and offers good overall survival, he said.
Also, "This strategy can allow for the more effective utilization of a limited (and dwindling) supply of transplantable livers; freeing other patients from the potential short- and long-term complications of undergoing unnecessary transplantation," Dr. Kluger said.
Meanwhile, "many treatments with curative intent remain available after recurrence, including re-resection, salvage transplantation, and ablation," he said.
He presented his abstract, which is not published, during the annual Digestive Disease Week.
Dr. Kluger and his colleagues studied 313 patients with hepatocellular carcinoma (HCC) who underwent liver resection between 1989 and 2010.
Patients were stratified based on tumor size of less than 50 mm (36%), 50-100 mm (36%), and more than 100 mm (28%).
Patients with larger tumors were more likely to have normal liver parenchyma: 43% of patients with tumors larger than 100 mm, compared with 1% of patients with tumors smaller than 50 mm (P less than .001).
The influence of tumor size on overall survival was significant in univariate analyses (less than 50 mm vs. 50-100 mm, P = .0321; less then 50 mm vs. more than 100 mm, P = 0.009; 50-100 mm vs. more than 100 mm, P = .57), said Dr. Kluger, but when the salvage transplantation cases were excluded, tumor size was no longer significant (P = .18, .07, and .65, respectively.)
Researchers found seven independent predictors that led to decreased overall survival: intraoperative transfusion (hazard ratio, 2.60), cirrhosis (HR, 2.42), poorly differentiated tumor (HR, 2.04), satellite lesions (HR, 1.68), microvascular invasion (HR, 1.48), alpha-fetoprotein more than 200 ng/mL (HR, 1.53), and salvage transplantation (HR, 0.23).
Median overall survival was 60 months. One-year overall survival was 76%, and 5-year overall survival was 50%. Meanwhile, 5-year survival of patients who underwent salvage transplantation from the time of occurrence was 90%, compared with 18% for those not undergoing the procedure (P less than .0001).
The median time to recurrence was 20 months, with 1-year recurrence-free survival at 61%, and 5-year recurrence-free survival at 28%.
Four variables independently affected recurrence-free survival, the authors noted: intra-operative transfusion (HR, 2.15), poorly differentiated tumor (HR, 1.87), cirrhosis (HR, 1.69), and microvascular invasion (HR, 1.71).
Patients with nontransplantable recurrences after resection of tumors smaller than 5 cm had similar overall survival, compared with patients whose tumors were originally 5 cm or larger.
The study also showed that the rate of complications decreased during the second decade of the study period. While the mortality rate between 1989 and 1999 was 14%, it dropped to 5% through 2010 (P less than .008).
"These improvements coincide with major advances in liver surgery, patient selection, anesthetic practices, liver imaging, and postoperative care," said Dr. Kluger in an interview. "We also believe that routine integration of laparoscopy for appropriate cases since 1998 was also critical to improvements in outcomes. Whereas 6% of the cases performed prior to 2000 utilized a laparoscopic technique, 30% performed after 2000 did."
Dr. Kluger said that "tumor size is a widely accepted but inadequate proxy for interactions within the tumor milieu. ... The onus is to determine which patients would most benefit from upfront listing for transplantation despite candidacy for resection, or resection with the future possibility of salvage transplantation for recurrence," he said.
Dr. Kluger had no disclosures.
On Twitter @NaseemSMiller
ORLANDO – In hepatocellular carcinoma, tumor size did not independently influence recurrence or survival, whereas tumor histopathology and background parenchyma did, according to a retrospective, single-center study of 300 patients.
"These findings further support that prognosis and treatment guidelines cannot be effectively categorized based on tumor size," said Dr. Michael D. Kluger of the department of surgery at New York-Presbyterian Hospital–Cornell University, New York.
Although the procedure is hampered by high recurrence rates, resection is safe, readily available, and offers good overall survival, he said.
Also, "This strategy can allow for the more effective utilization of a limited (and dwindling) supply of transplantable livers; freeing other patients from the potential short- and long-term complications of undergoing unnecessary transplantation," Dr. Kluger said.
Meanwhile, "many treatments with curative intent remain available after recurrence, including re-resection, salvage transplantation, and ablation," he said.
He presented his abstract, which is not published, during the annual Digestive Disease Week.
Dr. Kluger and his colleagues studied 313 patients with hepatocellular carcinoma (HCC) who underwent liver resection between 1989 and 2010.
Patients were stratified based on tumor size of less than 50 mm (36%), 50-100 mm (36%), and more than 100 mm (28%).
Patients with larger tumors were more likely to have normal liver parenchyma: 43% of patients with tumors larger than 100 mm, compared with 1% of patients with tumors smaller than 50 mm (P less than .001).
The influence of tumor size on overall survival was significant in univariate analyses (less than 50 mm vs. 50-100 mm, P = .0321; less then 50 mm vs. more than 100 mm, P = 0.009; 50-100 mm vs. more than 100 mm, P = .57), said Dr. Kluger, but when the salvage transplantation cases were excluded, tumor size was no longer significant (P = .18, .07, and .65, respectively.)
Researchers found seven independent predictors that led to decreased overall survival: intraoperative transfusion (hazard ratio, 2.60), cirrhosis (HR, 2.42), poorly differentiated tumor (HR, 2.04), satellite lesions (HR, 1.68), microvascular invasion (HR, 1.48), alpha-fetoprotein more than 200 ng/mL (HR, 1.53), and salvage transplantation (HR, 0.23).
Median overall survival was 60 months. One-year overall survival was 76%, and 5-year overall survival was 50%. Meanwhile, 5-year survival of patients who underwent salvage transplantation from the time of occurrence was 90%, compared with 18% for those not undergoing the procedure (P less than .0001).
The median time to recurrence was 20 months, with 1-year recurrence-free survival at 61%, and 5-year recurrence-free survival at 28%.
Four variables independently affected recurrence-free survival, the authors noted: intra-operative transfusion (HR, 2.15), poorly differentiated tumor (HR, 1.87), cirrhosis (HR, 1.69), and microvascular invasion (HR, 1.71).
Patients with nontransplantable recurrences after resection of tumors smaller than 5 cm had similar overall survival, compared with patients whose tumors were originally 5 cm or larger.
The study also showed that the rate of complications decreased during the second decade of the study period. While the mortality rate between 1989 and 1999 was 14%, it dropped to 5% through 2010 (P less than .008).
"These improvements coincide with major advances in liver surgery, patient selection, anesthetic practices, liver imaging, and postoperative care," said Dr. Kluger in an interview. "We also believe that routine integration of laparoscopy for appropriate cases since 1998 was also critical to improvements in outcomes. Whereas 6% of the cases performed prior to 2000 utilized a laparoscopic technique, 30% performed after 2000 did."
Dr. Kluger said that "tumor size is a widely accepted but inadequate proxy for interactions within the tumor milieu. ... The onus is to determine which patients would most benefit from upfront listing for transplantation despite candidacy for resection, or resection with the future possibility of salvage transplantation for recurrence," he said.
Dr. Kluger had no disclosures.
On Twitter @NaseemSMiller
ORLANDO – In hepatocellular carcinoma, tumor size did not independently influence recurrence or survival, whereas tumor histopathology and background parenchyma did, according to a retrospective, single-center study of 300 patients.
"These findings further support that prognosis and treatment guidelines cannot be effectively categorized based on tumor size," said Dr. Michael D. Kluger of the department of surgery at New York-Presbyterian Hospital–Cornell University, New York.
Although the procedure is hampered by high recurrence rates, resection is safe, readily available, and offers good overall survival, he said.
Also, "This strategy can allow for the more effective utilization of a limited (and dwindling) supply of transplantable livers; freeing other patients from the potential short- and long-term complications of undergoing unnecessary transplantation," Dr. Kluger said.
Meanwhile, "many treatments with curative intent remain available after recurrence, including re-resection, salvage transplantation, and ablation," he said.
He presented his abstract, which is not published, during the annual Digestive Disease Week.
Dr. Kluger and his colleagues studied 313 patients with hepatocellular carcinoma (HCC) who underwent liver resection between 1989 and 2010.
Patients were stratified based on tumor size of less than 50 mm (36%), 50-100 mm (36%), and more than 100 mm (28%).
Patients with larger tumors were more likely to have normal liver parenchyma: 43% of patients with tumors larger than 100 mm, compared with 1% of patients with tumors smaller than 50 mm (P less than .001).
The influence of tumor size on overall survival was significant in univariate analyses (less than 50 mm vs. 50-100 mm, P = .0321; less then 50 mm vs. more than 100 mm, P = 0.009; 50-100 mm vs. more than 100 mm, P = .57), said Dr. Kluger, but when the salvage transplantation cases were excluded, tumor size was no longer significant (P = .18, .07, and .65, respectively.)
Researchers found seven independent predictors that led to decreased overall survival: intraoperative transfusion (hazard ratio, 2.60), cirrhosis (HR, 2.42), poorly differentiated tumor (HR, 2.04), satellite lesions (HR, 1.68), microvascular invasion (HR, 1.48), alpha-fetoprotein more than 200 ng/mL (HR, 1.53), and salvage transplantation (HR, 0.23).
Median overall survival was 60 months. One-year overall survival was 76%, and 5-year overall survival was 50%. Meanwhile, 5-year survival of patients who underwent salvage transplantation from the time of occurrence was 90%, compared with 18% for those not undergoing the procedure (P less than .0001).
The median time to recurrence was 20 months, with 1-year recurrence-free survival at 61%, and 5-year recurrence-free survival at 28%.
Four variables independently affected recurrence-free survival, the authors noted: intra-operative transfusion (HR, 2.15), poorly differentiated tumor (HR, 1.87), cirrhosis (HR, 1.69), and microvascular invasion (HR, 1.71).
Patients with nontransplantable recurrences after resection of tumors smaller than 5 cm had similar overall survival, compared with patients whose tumors were originally 5 cm or larger.
The study also showed that the rate of complications decreased during the second decade of the study period. While the mortality rate between 1989 and 1999 was 14%, it dropped to 5% through 2010 (P less than .008).
"These improvements coincide with major advances in liver surgery, patient selection, anesthetic practices, liver imaging, and postoperative care," said Dr. Kluger in an interview. "We also believe that routine integration of laparoscopy for appropriate cases since 1998 was also critical to improvements in outcomes. Whereas 6% of the cases performed prior to 2000 utilized a laparoscopic technique, 30% performed after 2000 did."
Dr. Kluger said that "tumor size is a widely accepted but inadequate proxy for interactions within the tumor milieu. ... The onus is to determine which patients would most benefit from upfront listing for transplantation despite candidacy for resection, or resection with the future possibility of salvage transplantation for recurrence," he said.
Dr. Kluger had no disclosures.
On Twitter @NaseemSMiller
AT DDW 2013
Major finding: The influence of tumor size on overall survival was significant in univariate analyses but when the salvage transplantation cases were excluded, tumor size was no longer significant.
Data source: Study of 313 patients with hepatocellular carcinoma who underwent liver resection between 1989 and 2010 at a single center.
Disclosures: Dr. Kluger had no disclosures.
Home discharge with total artificial heart is feasible, safe
LOS ANGELES – Some patients with a total artificial heart can safely go home with the use of a small portable driver while awaiting heart transplantation, according to data from the first U.S. patient cohort in whom this was attempted.
Investigators assessed outcomes in 13 total artificial heart recipients who were stable enough clinically to be transitioned from the usual driver to SynCardia Systems’ investigational portable driver, the Freedom Driver System. The driver weighs 14 pounds and allows several hours of untethered activity.
Eight of the patients were able to go home for an average of 5.5 months, lead investigator Dr. Vigneshwar Kasirajan reported at the annual meeting of the Society of Thoracic Surgeons.
They had a low rate of major bleeding and no major infections. There were roughly five device malfunctions per patient-year, but in all cases, patients were able to switch to a backup driver uneventfully.
Twelve of the 13 total patients ultimately underwent transplantation, for a transplantation rate of 92%.
"The Freedom driver is effective in supporting circulation with a total artificial heart. Discharge home is safe and feasible," commented Dr. Kasirajan, who is director of heart transplantation, heart-lung transplantation, and mechanical circulatory support at Virginia Commonwealth University in Richmond.
"Further data on the completion of this study will help to demonstrate the efficacy and safety of the driver. In addition, important data on exercise capacity and quality of life will be valuable in finally moving the artificial heart technology to more widespread use," he said.
Session comoderator Dr. Todd M. Dewey, a cardiothoracic surgeon with Medical City Specialists in Dallas, noted, "The majority of patients on axial-flow left ventricular assist devices are discharged home. What percentage of total artificial heart patients do you think will ultimately leave the hospital?"
"We are close to 80% of our patients going home right now, at least in high-volume institutions," Dr. Kasirajan replied. Two patients have been at home for more than 2 years without readmissions related to the device, he added.
A pivotal study previously showed that the total artificial heart can be used as a bridge to transplantation in patients with irreversible biventricular failure (N. Engl. J. Med. 2004;351:859-67).
"Unfortunately, ... the widespread use of this technology is limited because of the inability to discharge these patients home, and that relates to the fact that the circulatory support system console has to be powered by compressed air either from the hospital or via a cylinder," Dr. Kasirajan explained.
However, once patients are stable, the driver settings need little adjustment, which spurred development of the portable driver. "The driver has two batteries that allow up to 3 hours of untethered activity. These can be charged in place using an alternating current output or car charger," he said.
The ongoing study of the driver will enroll up to 60 patients from 30 international sites. Patients are required to be wait-listed for heart transplantation and receive a total artificial heart, and to be clinically stable on the circulatory support system, with a cardiac index of at least 2.2 L/min/m2. They are then switched to the portable driver with the intent of discharge from the hospital.
Dr. Kasirajan reported results for the first 13 patients enrolled from four U.S. sites. Overall, 5 of the patients remained in the hospital (because of medical reasons, discharge logistics, or personal preference), whereas 8 went home with the driver. The median duration out of the hospital in the latter group was 162 days (range, 39-437 days).
The 13 patients had maintenance of cardiac function, with a cardiac index averaging 3.3 L/min/m2, and their laboratory values remained stable between baseline and 90 days. "Particularly, there was no evidence of hemolysis that was worse than at the beginning," he noted. "Increasing albumin levels reflect the increasing nutritional status in these patients."
The in-hospital group had a very similar rate of adverse events relative to an earlier comparison cohort of stable patients with a total artificial heart followed as part of postmarket surveillance, according to Dr. Kasirajan.
Within the study population, the out-of-hospital and in-hospital groups had similar rates of major bleeding (1.1 vs. 1.4 events per patient-year). The former had a lower rate of major infection (0 vs. 2.8 events per patient-year) but higher rates of device malfunction (4.6 vs. 0 events per patient-year) and hemolysis (2.3 vs. 0 events per patient-year).
The five device malfunctions in the out-of-hospital group were due to a Valsalva maneuver, a faulty sensor, hypertension, a kink in the driveline while a patient was getting into a car, and dropping of the driver while showering.
"All these patients remained stable and had no changes in cardiac output," Dr. Kasirajan pointed out. "They were able to switch to the backup driver as educated, and returned to the hospital."
Valsalva maneuvers can cause a sudden transient rise in intrathoracic pressure that a device sensor interprets as outside the set parameters, he explained; the software has since been modified to allow for these changes.
"The importance of hypertension management is critical," he commented. "The pump tolerates blood pressures at high levels for brief periods of time; however, prolonged hypertension leads to a decrease in left heart cardiac output and pulmonary edema."
The cases of hemolysis were due to transient rises in plasma free hemoglobin as a result of hemothorax and hydralazine-induced hemolytic anemia.
Only a single patient, in the out-of-hospital group, died before transplantation. This patient was stable on the driver for 437 days, but experienced a fall with a spinal cord hematoma, and developed fatal complications.
Dr. Kasirajan disclosed that he is a consultant to SynCardia Systems.
LOS ANGELES – Some patients with a total artificial heart can safely go home with the use of a small portable driver while awaiting heart transplantation, according to data from the first U.S. patient cohort in whom this was attempted.
Investigators assessed outcomes in 13 total artificial heart recipients who were stable enough clinically to be transitioned from the usual driver to SynCardia Systems’ investigational portable driver, the Freedom Driver System. The driver weighs 14 pounds and allows several hours of untethered activity.
Eight of the patients were able to go home for an average of 5.5 months, lead investigator Dr. Vigneshwar Kasirajan reported at the annual meeting of the Society of Thoracic Surgeons.
They had a low rate of major bleeding and no major infections. There were roughly five device malfunctions per patient-year, but in all cases, patients were able to switch to a backup driver uneventfully.
Twelve of the 13 total patients ultimately underwent transplantation, for a transplantation rate of 92%.
"The Freedom driver is effective in supporting circulation with a total artificial heart. Discharge home is safe and feasible," commented Dr. Kasirajan, who is director of heart transplantation, heart-lung transplantation, and mechanical circulatory support at Virginia Commonwealth University in Richmond.
"Further data on the completion of this study will help to demonstrate the efficacy and safety of the driver. In addition, important data on exercise capacity and quality of life will be valuable in finally moving the artificial heart technology to more widespread use," he said.
Session comoderator Dr. Todd M. Dewey, a cardiothoracic surgeon with Medical City Specialists in Dallas, noted, "The majority of patients on axial-flow left ventricular assist devices are discharged home. What percentage of total artificial heart patients do you think will ultimately leave the hospital?"
"We are close to 80% of our patients going home right now, at least in high-volume institutions," Dr. Kasirajan replied. Two patients have been at home for more than 2 years without readmissions related to the device, he added.
A pivotal study previously showed that the total artificial heart can be used as a bridge to transplantation in patients with irreversible biventricular failure (N. Engl. J. Med. 2004;351:859-67).
"Unfortunately, ... the widespread use of this technology is limited because of the inability to discharge these patients home, and that relates to the fact that the circulatory support system console has to be powered by compressed air either from the hospital or via a cylinder," Dr. Kasirajan explained.
However, once patients are stable, the driver settings need little adjustment, which spurred development of the portable driver. "The driver has two batteries that allow up to 3 hours of untethered activity. These can be charged in place using an alternating current output or car charger," he said.
The ongoing study of the driver will enroll up to 60 patients from 30 international sites. Patients are required to be wait-listed for heart transplantation and receive a total artificial heart, and to be clinically stable on the circulatory support system, with a cardiac index of at least 2.2 L/min/m2. They are then switched to the portable driver with the intent of discharge from the hospital.
Dr. Kasirajan reported results for the first 13 patients enrolled from four U.S. sites. Overall, 5 of the patients remained in the hospital (because of medical reasons, discharge logistics, or personal preference), whereas 8 went home with the driver. The median duration out of the hospital in the latter group was 162 days (range, 39-437 days).
The 13 patients had maintenance of cardiac function, with a cardiac index averaging 3.3 L/min/m2, and their laboratory values remained stable between baseline and 90 days. "Particularly, there was no evidence of hemolysis that was worse than at the beginning," he noted. "Increasing albumin levels reflect the increasing nutritional status in these patients."
The in-hospital group had a very similar rate of adverse events relative to an earlier comparison cohort of stable patients with a total artificial heart followed as part of postmarket surveillance, according to Dr. Kasirajan.
Within the study population, the out-of-hospital and in-hospital groups had similar rates of major bleeding (1.1 vs. 1.4 events per patient-year). The former had a lower rate of major infection (0 vs. 2.8 events per patient-year) but higher rates of device malfunction (4.6 vs. 0 events per patient-year) and hemolysis (2.3 vs. 0 events per patient-year).
The five device malfunctions in the out-of-hospital group were due to a Valsalva maneuver, a faulty sensor, hypertension, a kink in the driveline while a patient was getting into a car, and dropping of the driver while showering.
"All these patients remained stable and had no changes in cardiac output," Dr. Kasirajan pointed out. "They were able to switch to the backup driver as educated, and returned to the hospital."
Valsalva maneuvers can cause a sudden transient rise in intrathoracic pressure that a device sensor interprets as outside the set parameters, he explained; the software has since been modified to allow for these changes.
"The importance of hypertension management is critical," he commented. "The pump tolerates blood pressures at high levels for brief periods of time; however, prolonged hypertension leads to a decrease in left heart cardiac output and pulmonary edema."
The cases of hemolysis were due to transient rises in plasma free hemoglobin as a result of hemothorax and hydralazine-induced hemolytic anemia.
Only a single patient, in the out-of-hospital group, died before transplantation. This patient was stable on the driver for 437 days, but experienced a fall with a spinal cord hematoma, and developed fatal complications.
Dr. Kasirajan disclosed that he is a consultant to SynCardia Systems.
LOS ANGELES – Some patients with a total artificial heart can safely go home with the use of a small portable driver while awaiting heart transplantation, according to data from the first U.S. patient cohort in whom this was attempted.
Investigators assessed outcomes in 13 total artificial heart recipients who were stable enough clinically to be transitioned from the usual driver to SynCardia Systems’ investigational portable driver, the Freedom Driver System. The driver weighs 14 pounds and allows several hours of untethered activity.
Eight of the patients were able to go home for an average of 5.5 months, lead investigator Dr. Vigneshwar Kasirajan reported at the annual meeting of the Society of Thoracic Surgeons.
They had a low rate of major bleeding and no major infections. There were roughly five device malfunctions per patient-year, but in all cases, patients were able to switch to a backup driver uneventfully.
Twelve of the 13 total patients ultimately underwent transplantation, for a transplantation rate of 92%.
"The Freedom driver is effective in supporting circulation with a total artificial heart. Discharge home is safe and feasible," commented Dr. Kasirajan, who is director of heart transplantation, heart-lung transplantation, and mechanical circulatory support at Virginia Commonwealth University in Richmond.
"Further data on the completion of this study will help to demonstrate the efficacy and safety of the driver. In addition, important data on exercise capacity and quality of life will be valuable in finally moving the artificial heart technology to more widespread use," he said.
Session comoderator Dr. Todd M. Dewey, a cardiothoracic surgeon with Medical City Specialists in Dallas, noted, "The majority of patients on axial-flow left ventricular assist devices are discharged home. What percentage of total artificial heart patients do you think will ultimately leave the hospital?"
"We are close to 80% of our patients going home right now, at least in high-volume institutions," Dr. Kasirajan replied. Two patients have been at home for more than 2 years without readmissions related to the device, he added.
A pivotal study previously showed that the total artificial heart can be used as a bridge to transplantation in patients with irreversible biventricular failure (N. Engl. J. Med. 2004;351:859-67).
"Unfortunately, ... the widespread use of this technology is limited because of the inability to discharge these patients home, and that relates to the fact that the circulatory support system console has to be powered by compressed air either from the hospital or via a cylinder," Dr. Kasirajan explained.
However, once patients are stable, the driver settings need little adjustment, which spurred development of the portable driver. "The driver has two batteries that allow up to 3 hours of untethered activity. These can be charged in place using an alternating current output or car charger," he said.
The ongoing study of the driver will enroll up to 60 patients from 30 international sites. Patients are required to be wait-listed for heart transplantation and receive a total artificial heart, and to be clinically stable on the circulatory support system, with a cardiac index of at least 2.2 L/min/m2. They are then switched to the portable driver with the intent of discharge from the hospital.
Dr. Kasirajan reported results for the first 13 patients enrolled from four U.S. sites. Overall, 5 of the patients remained in the hospital (because of medical reasons, discharge logistics, or personal preference), whereas 8 went home with the driver. The median duration out of the hospital in the latter group was 162 days (range, 39-437 days).
The 13 patients had maintenance of cardiac function, with a cardiac index averaging 3.3 L/min/m2, and their laboratory values remained stable between baseline and 90 days. "Particularly, there was no evidence of hemolysis that was worse than at the beginning," he noted. "Increasing albumin levels reflect the increasing nutritional status in these patients."
The in-hospital group had a very similar rate of adverse events relative to an earlier comparison cohort of stable patients with a total artificial heart followed as part of postmarket surveillance, according to Dr. Kasirajan.
Within the study population, the out-of-hospital and in-hospital groups had similar rates of major bleeding (1.1 vs. 1.4 events per patient-year). The former had a lower rate of major infection (0 vs. 2.8 events per patient-year) but higher rates of device malfunction (4.6 vs. 0 events per patient-year) and hemolysis (2.3 vs. 0 events per patient-year).
The five device malfunctions in the out-of-hospital group were due to a Valsalva maneuver, a faulty sensor, hypertension, a kink in the driveline while a patient was getting into a car, and dropping of the driver while showering.
"All these patients remained stable and had no changes in cardiac output," Dr. Kasirajan pointed out. "They were able to switch to the backup driver as educated, and returned to the hospital."
Valsalva maneuvers can cause a sudden transient rise in intrathoracic pressure that a device sensor interprets as outside the set parameters, he explained; the software has since been modified to allow for these changes.
"The importance of hypertension management is critical," he commented. "The pump tolerates blood pressures at high levels for brief periods of time; however, prolonged hypertension leads to a decrease in left heart cardiac output and pulmonary edema."
The cases of hemolysis were due to transient rises in plasma free hemoglobin as a result of hemothorax and hydralazine-induced hemolytic anemia.
Only a single patient, in the out-of-hospital group, died before transplantation. This patient was stable on the driver for 437 days, but experienced a fall with a spinal cord hematoma, and developed fatal complications.
Dr. Kasirajan disclosed that he is a consultant to SynCardia Systems.
AT THE STS ANNUAL MEETING
Major finding: The eight patients who were able to go home had a low rate of major bleeding and no major infections. The rate of device malfunctions was 4.6 events per patient-year, but none of these patients experienced a change in cardiac output.
Data source: An interim analysis of a cohort study among 13 clinically stable patients with a total artificial heart powered by a portable driver.
Disclosures: Dr. Kasirajan disclosed that he is a consultant to SynCardia Systems.
Everolimus approval now includes prevention of liver transplant rejection
Food and Drug Administration approval of the immunosuppressant drug everolimus has been expanded to include prophylaxis of organ rejection in adults undergoing a liver transplant.
The approval, on Feb. 15, was announced by the manufacturer, Novartis. Everolimus, a mammalian target of rapamycin (mTOR) inhibitor, was first approved for prophylaxis of organ rejection in adults undergoing a kidney transplant in 2010, and is taken twice a day by mouth.
The approved indication states that in liver transplant recipients, everolimus is used in combination with the calcineurin inhibitor tacrolimus (at a reduced dose) and corticosteroids, and that it should be administered no earlier than 30 days post transplant. Safety and efficacy have not been established in pediatric patients, according to the prescribing information.
FDA approval was based on the 12-month results of a phase III, open-label international study of 719 liver transplant recipients (mean age, 54 years). At 12 months, the rate of the "efficacy failure" endpoint (defined as biopsy-proven acute rejection, graft loss, death, or loss to follow-up) was "comparable" between those patients treated with the reduced dose of everolimus, started 30 days after transplantation (9%), and the patients treated with the standard dose of tacrolimus, started 30 days after transplantation (13.6%), according to the Novartis statement and prescribing information. All patients were treated with corticosteroids.
Everolimus is the first mTOR inhibitor approved for liver transplant recipients, and is the first immunosuppressant approved by the FDA for use in liver transplant recipients in more than 10 years, according to Novartis.
Novartis markets everolimus in the United States as Zortress. It was approved in the European Union in the fourth quarter of 2012 for adult liver transplant recipients; it is marketed as Certican in Europe.
The new label is available here. Serious adverse events associated with everolimus should be reported to the FDA’s MedWatch program at 800-332-1088 or www.fda.gov/medwatch/.
Food and Drug Administration approval of the immunosuppressant drug everolimus has been expanded to include prophylaxis of organ rejection in adults undergoing a liver transplant.
The approval, on Feb. 15, was announced by the manufacturer, Novartis. Everolimus, a mammalian target of rapamycin (mTOR) inhibitor, was first approved for prophylaxis of organ rejection in adults undergoing a kidney transplant in 2010, and is taken twice a day by mouth.
The approved indication states that in liver transplant recipients, everolimus is used in combination with the calcineurin inhibitor tacrolimus (at a reduced dose) and corticosteroids, and that it should be administered no earlier than 30 days post transplant. Safety and efficacy have not been established in pediatric patients, according to the prescribing information.
FDA approval was based on the 12-month results of a phase III, open-label international study of 719 liver transplant recipients (mean age, 54 years). At 12 months, the rate of the "efficacy failure" endpoint (defined as biopsy-proven acute rejection, graft loss, death, or loss to follow-up) was "comparable" between those patients treated with the reduced dose of everolimus, started 30 days after transplantation (9%), and the patients treated with the standard dose of tacrolimus, started 30 days after transplantation (13.6%), according to the Novartis statement and prescribing information. All patients were treated with corticosteroids.
Everolimus is the first mTOR inhibitor approved for liver transplant recipients, and is the first immunosuppressant approved by the FDA for use in liver transplant recipients in more than 10 years, according to Novartis.
Novartis markets everolimus in the United States as Zortress. It was approved in the European Union in the fourth quarter of 2012 for adult liver transplant recipients; it is marketed as Certican in Europe.
The new label is available here. Serious adverse events associated with everolimus should be reported to the FDA’s MedWatch program at 800-332-1088 or www.fda.gov/medwatch/.
Food and Drug Administration approval of the immunosuppressant drug everolimus has been expanded to include prophylaxis of organ rejection in adults undergoing a liver transplant.
The approval, on Feb. 15, was announced by the manufacturer, Novartis. Everolimus, a mammalian target of rapamycin (mTOR) inhibitor, was first approved for prophylaxis of organ rejection in adults undergoing a kidney transplant in 2010, and is taken twice a day by mouth.
The approved indication states that in liver transplant recipients, everolimus is used in combination with the calcineurin inhibitor tacrolimus (at a reduced dose) and corticosteroids, and that it should be administered no earlier than 30 days post transplant. Safety and efficacy have not been established in pediatric patients, according to the prescribing information.
FDA approval was based on the 12-month results of a phase III, open-label international study of 719 liver transplant recipients (mean age, 54 years). At 12 months, the rate of the "efficacy failure" endpoint (defined as biopsy-proven acute rejection, graft loss, death, or loss to follow-up) was "comparable" between those patients treated with the reduced dose of everolimus, started 30 days after transplantation (9%), and the patients treated with the standard dose of tacrolimus, started 30 days after transplantation (13.6%), according to the Novartis statement and prescribing information. All patients were treated with corticosteroids.
Everolimus is the first mTOR inhibitor approved for liver transplant recipients, and is the first immunosuppressant approved by the FDA for use in liver transplant recipients in more than 10 years, according to Novartis.
Novartis markets everolimus in the United States as Zortress. It was approved in the European Union in the fourth quarter of 2012 for adult liver transplant recipients; it is marketed as Certican in Europe.
The new label is available here. Serious adverse events associated with everolimus should be reported to the FDA’s MedWatch program at 800-332-1088 or www.fda.gov/medwatch/.
Survey: Most support transfusing to increase organ donation
SCOTTSDALE, ARIZ. – The majority of trauma surgeons would aggressively manage patients with a lethal brain injury for the purposes of organ donation.
Consensus on how best to transfuse these patients to protect their organs appears to be another matter, a survey of Eastern Association for the Surgery of Trauma (EAST) members reveals.
"Further investigation is needed to determine what the transfusion triggers and limits should be in order to maximize our donor conversion rates," said Dr. Stancie Rhodes and her colleagues at Robert Wood Johnson University Hospital, New Brunswick, N.J.
Many institutions have set up aggressive donor management protocols to help address the worldwide shortage of transplantable organs. At press time, 117,090 candidates were on the U.S. Department of Health and Human Services’ Organ Procurement and Transplantation Network waiting list, with just 25,785 transplants performed between January and November 2012.
Aggressive donor management (ADM) protocols typically include guidelines for invasive monitoring and correction of metabolic disturbances that follow brain death, but many continue to lack guidelines on when and in what quantity to transfuse potential organ donors, explained Dr. Rhodes, a trauma surgeon at Robert Wood Johnson.
To further develop these guidelines, the investigators electronically surveyed all trauma surgeons in EAST regarding their transfusion practices in patients with nonsurvivable brain injury. In all, 285 members responded (24.5%). Among these respondents, 53.5% currently transfuse these patients.
Almost three-fourths, 72.5%, of respondents agreed with aggressive medical management of patients with lethal brain injury in the hope they could donate organs, while 9.4% strongly disagreed, Dr. Rhodes reported in a poster at the EAST’s annual meeting.
Trauma surgeons practicing in a suburban setting were significantly more likely to agree with transfusion than were those in rural or urban settings (77% vs. 52% vs. 55%; P less than .04).
Before deciding to aggressively manage a potential organ donor, respondents were divided on whether the testing for declaration of brain death must already be underway (111 strongly agree/26 strongly disagree), the patient must be declared brain dead (11 strongly agree/84 strongly disagree), or consent for donation of organs must have been obtained (6 strongly agree/114 strongly disagree, Dr. Rhodes reported.
"I think the important piece is that respondents overwhelmingly agreed that they would not wait for declaration of brain death to begin to aggressively manage these patients," she said in an interview. "This is important, as these patients succumb to hypoperfusion, coagulopathy, and acidosis if their ongoing hemorrhage is uncontrolled early in their course."
The majority of respondents (75%) agreed that they have a limit to the amount of product they would administer.
If the potential donor was in hemorrhagic shock, 6 respondents strongly agreed and 12 agreed they would consider transfusing blood products, while 114 disagreed and 119 strongly disagreed with the practice.
Respondents were more likely to consider transfusing, however, if the potential donor was having coagulopathic bleeding. In all, 47 strongly agreed and 106 agreed with transfusing in this setting, while 30 disagreed and 15 strongly disagreed.
If either hemorrhagic shock or coagulopathic bleeding were present, most respondents would limit packed red blood cells and fresh frozen plasma to no more than 5-8 units, and platelets to no more than 1-4 units, the authors reported.
Of those surgeons surveyed, 42% were between the ages of 40 and 49 years, 10.2% practiced primarily in a rural setting, 15.1% practiced in an suburban setting – defined as a population less than 500,000 – and 45.6% were in an urban setting, defined by a population in excess of 500,000 residents.
Dr. Rhodes and her coauthors have nothing to disclose.
transfuse, survey, Eastern Association for the Surgery of Trauma, EAST, Dr. Stancie Rhodes, aggressive donor management protocols, worldwide shortage of transplantable organs, U.S. Department of Health and Human Services’ Organ Procurement and Transplantation Network waiting list,
SCOTTSDALE, ARIZ. – The majority of trauma surgeons would aggressively manage patients with a lethal brain injury for the purposes of organ donation.
Consensus on how best to transfuse these patients to protect their organs appears to be another matter, a survey of Eastern Association for the Surgery of Trauma (EAST) members reveals.
"Further investigation is needed to determine what the transfusion triggers and limits should be in order to maximize our donor conversion rates," said Dr. Stancie Rhodes and her colleagues at Robert Wood Johnson University Hospital, New Brunswick, N.J.
Many institutions have set up aggressive donor management protocols to help address the worldwide shortage of transplantable organs. At press time, 117,090 candidates were on the U.S. Department of Health and Human Services’ Organ Procurement and Transplantation Network waiting list, with just 25,785 transplants performed between January and November 2012.
Aggressive donor management (ADM) protocols typically include guidelines for invasive monitoring and correction of metabolic disturbances that follow brain death, but many continue to lack guidelines on when and in what quantity to transfuse potential organ donors, explained Dr. Rhodes, a trauma surgeon at Robert Wood Johnson.
To further develop these guidelines, the investigators electronically surveyed all trauma surgeons in EAST regarding their transfusion practices in patients with nonsurvivable brain injury. In all, 285 members responded (24.5%). Among these respondents, 53.5% currently transfuse these patients.
Almost three-fourths, 72.5%, of respondents agreed with aggressive medical management of patients with lethal brain injury in the hope they could donate organs, while 9.4% strongly disagreed, Dr. Rhodes reported in a poster at the EAST’s annual meeting.
Trauma surgeons practicing in a suburban setting were significantly more likely to agree with transfusion than were those in rural or urban settings (77% vs. 52% vs. 55%; P less than .04).
Before deciding to aggressively manage a potential organ donor, respondents were divided on whether the testing for declaration of brain death must already be underway (111 strongly agree/26 strongly disagree), the patient must be declared brain dead (11 strongly agree/84 strongly disagree), or consent for donation of organs must have been obtained (6 strongly agree/114 strongly disagree, Dr. Rhodes reported.
"I think the important piece is that respondents overwhelmingly agreed that they would not wait for declaration of brain death to begin to aggressively manage these patients," she said in an interview. "This is important, as these patients succumb to hypoperfusion, coagulopathy, and acidosis if their ongoing hemorrhage is uncontrolled early in their course."
The majority of respondents (75%) agreed that they have a limit to the amount of product they would administer.
If the potential donor was in hemorrhagic shock, 6 respondents strongly agreed and 12 agreed they would consider transfusing blood products, while 114 disagreed and 119 strongly disagreed with the practice.
Respondents were more likely to consider transfusing, however, if the potential donor was having coagulopathic bleeding. In all, 47 strongly agreed and 106 agreed with transfusing in this setting, while 30 disagreed and 15 strongly disagreed.
If either hemorrhagic shock or coagulopathic bleeding were present, most respondents would limit packed red blood cells and fresh frozen plasma to no more than 5-8 units, and platelets to no more than 1-4 units, the authors reported.
Of those surgeons surveyed, 42% were between the ages of 40 and 49 years, 10.2% practiced primarily in a rural setting, 15.1% practiced in an suburban setting – defined as a population less than 500,000 – and 45.6% were in an urban setting, defined by a population in excess of 500,000 residents.
Dr. Rhodes and her coauthors have nothing to disclose.
SCOTTSDALE, ARIZ. – The majority of trauma surgeons would aggressively manage patients with a lethal brain injury for the purposes of organ donation.
Consensus on how best to transfuse these patients to protect their organs appears to be another matter, a survey of Eastern Association for the Surgery of Trauma (EAST) members reveals.
"Further investigation is needed to determine what the transfusion triggers and limits should be in order to maximize our donor conversion rates," said Dr. Stancie Rhodes and her colleagues at Robert Wood Johnson University Hospital, New Brunswick, N.J.
Many institutions have set up aggressive donor management protocols to help address the worldwide shortage of transplantable organs. At press time, 117,090 candidates were on the U.S. Department of Health and Human Services’ Organ Procurement and Transplantation Network waiting list, with just 25,785 transplants performed between January and November 2012.
Aggressive donor management (ADM) protocols typically include guidelines for invasive monitoring and correction of metabolic disturbances that follow brain death, but many continue to lack guidelines on when and in what quantity to transfuse potential organ donors, explained Dr. Rhodes, a trauma surgeon at Robert Wood Johnson.
To further develop these guidelines, the investigators electronically surveyed all trauma surgeons in EAST regarding their transfusion practices in patients with nonsurvivable brain injury. In all, 285 members responded (24.5%). Among these respondents, 53.5% currently transfuse these patients.
Almost three-fourths, 72.5%, of respondents agreed with aggressive medical management of patients with lethal brain injury in the hope they could donate organs, while 9.4% strongly disagreed, Dr. Rhodes reported in a poster at the EAST’s annual meeting.
Trauma surgeons practicing in a suburban setting were significantly more likely to agree with transfusion than were those in rural or urban settings (77% vs. 52% vs. 55%; P less than .04).
Before deciding to aggressively manage a potential organ donor, respondents were divided on whether the testing for declaration of brain death must already be underway (111 strongly agree/26 strongly disagree), the patient must be declared brain dead (11 strongly agree/84 strongly disagree), or consent for donation of organs must have been obtained (6 strongly agree/114 strongly disagree, Dr. Rhodes reported.
"I think the important piece is that respondents overwhelmingly agreed that they would not wait for declaration of brain death to begin to aggressively manage these patients," she said in an interview. "This is important, as these patients succumb to hypoperfusion, coagulopathy, and acidosis if their ongoing hemorrhage is uncontrolled early in their course."
The majority of respondents (75%) agreed that they have a limit to the amount of product they would administer.
If the potential donor was in hemorrhagic shock, 6 respondents strongly agreed and 12 agreed they would consider transfusing blood products, while 114 disagreed and 119 strongly disagreed with the practice.
Respondents were more likely to consider transfusing, however, if the potential donor was having coagulopathic bleeding. In all, 47 strongly agreed and 106 agreed with transfusing in this setting, while 30 disagreed and 15 strongly disagreed.
If either hemorrhagic shock or coagulopathic bleeding were present, most respondents would limit packed red blood cells and fresh frozen plasma to no more than 5-8 units, and platelets to no more than 1-4 units, the authors reported.
Of those surgeons surveyed, 42% were between the ages of 40 and 49 years, 10.2% practiced primarily in a rural setting, 15.1% practiced in an suburban setting – defined as a population less than 500,000 – and 45.6% were in an urban setting, defined by a population in excess of 500,000 residents.
Dr. Rhodes and her coauthors have nothing to disclose.
transfuse, survey, Eastern Association for the Surgery of Trauma, EAST, Dr. Stancie Rhodes, aggressive donor management protocols, worldwide shortage of transplantable organs, U.S. Department of Health and Human Services’ Organ Procurement and Transplantation Network waiting list,
transfuse, survey, Eastern Association for the Surgery of Trauma, EAST, Dr. Stancie Rhodes, aggressive donor management protocols, worldwide shortage of transplantable organs, U.S. Department of Health and Human Services’ Organ Procurement and Transplantation Network waiting list,
EXPERT ANALYSIS FROM THE EAST ANNUAL MEETING
Major Finding: Among respondents, 72.5% agreed with aggressive medical management of patients with lethal brain injury for the sake of organ donation, but there was less consensus on when and how to manage these patients.
Data Source: Electronic survey of 285 trauma surgeons in the Eastern Association for the Surgery of Trauma.
Disclosures: Dr. Rhodes and her coauthors have nothing to disclose.
No early cancer risk with donor lungs from heavy smokers
LOS ANGELES – Use of lungs from donors who smoked heavily does not worsen lung transplantation outcomes including risk for lung cancer death, at least in the medium term.
At a median follow-up of 2 years for 5,900 adults who had double-lung transplants, those who received lungs from heavy smokers had an actuarial median overall survival of roughly 5.5 years, and their lung function was essentially the same as that of patients who received lungs from other donors, Dr. Sharven Taghavi reported at the annual meeting of the Society of Thoracic Surgeons.
The study data came from the United Network for Organ Sharing (UNOS) database. A team led by Dr. Taghavi, of Temple University Hospital in Philadelphia, compared data for double-lung transplants from 2005-2011, comparing donors with a history of smoking exceeding 20 pack-years with other donors.
About 13% of the study patients received lungs from donors who had smoked heavily. Compared with other recipients, these recipients were more likely to have a primary diagnosis of chronic obstructive pulmonary disease and less likely to have a diagnosis of idiopathic pulmonary fibrosis. Otherwise, they were similar.
The rate of deaths due to cancer was based on case reports, as UNOS does not capture this outcome. Cancer deaths were 5.8% among recipients of lungs from heavy smokers and 3.6% among other recipients.
"There is a fairly low capture rate for this field, so it’s difficult to draw significant conclusions from it," cautioned Dr. Taghavi.
Patients who received lungs from heavy smokers had a 1-day longer length of stay in the hospital (18 days vs. 17 days), which "may not really be clinically relevant." Rates of acute rejection during hospitalization were comparable (10.7% vs. 8.8%), as was post-transplant airway dehiscence (1.8% vs. 1.8%).
Post-transplant peak forced expiratory volume in 1 second (FEV1) was the same (80% vs. 79%), as was decline in this measure over time. Median duration of freedom from bronchiolitis obliterans syndrome was 1,583 days vs. 1,827 days.
Risk-adjusted median all-cause survival – the study’s primary endpoint – did not differ significantly between the recipients given lungs from donors who smoked heavily and the other recipients (2,043 vs. 1,928 days).
The rate of cancer deaths did not differ significantly; however, the follow-up time is too short to address this concern in a meaningful way, Dr. Taghavi said.
"Currently, we recommend when evaluating a donor who has a heavy smoking history, that they undergo a thorough examination for lung tumors or evidence of cancer. This includes obtaining a chest x-ray, CT scans, and bronchoscopies. In addition, when the lungs are procured, they should undergo a very thorough visual inspection," he advised.
"Informed consent is very important. You have to discuss the donor’s smoking status with the recipient and explain the risks and the benefits," Dr. Taghavi said. Lung cancer risk, given the donor’s history, is about 1% to 2% annually, and that needs to be considered against the high likelihood of dying within 1 or 2 years without a transplant.
"One thing that is unquestionable is that survival will be better accepting these lungs than it will be sitting on a waiting list," he added. Only about half of the people listed for lung transplant in the United States each year actually undergo the surgery.
Recipients of lungs from heavy smokers do not need any extra follow-up or surveillance, as they are already diligently tested and monitored, according to Dr. Taghavi. The recipient’s immunosuppression does theoretically put one at additional risk for lung cancer.
Current guidelines of the International Society of Heart and Lung Transplantation advise against considering use of lungs from donors who have a smoking history of more than 20 pack-years, Dr. Taghavi noted. But he stopped short of saying that the study should prompt a formal revision of those guidelines.
"I think the findings start the conversation," he commented. "We should consider looking at these potential donors," especially when a recipient’s situation is dire.
Dr. Taghavi disclosed no conflicts of interest.
LOS ANGELES – Use of lungs from donors who smoked heavily does not worsen lung transplantation outcomes including risk for lung cancer death, at least in the medium term.
At a median follow-up of 2 years for 5,900 adults who had double-lung transplants, those who received lungs from heavy smokers had an actuarial median overall survival of roughly 5.5 years, and their lung function was essentially the same as that of patients who received lungs from other donors, Dr. Sharven Taghavi reported at the annual meeting of the Society of Thoracic Surgeons.
The study data came from the United Network for Organ Sharing (UNOS) database. A team led by Dr. Taghavi, of Temple University Hospital in Philadelphia, compared data for double-lung transplants from 2005-2011, comparing donors with a history of smoking exceeding 20 pack-years with other donors.
About 13% of the study patients received lungs from donors who had smoked heavily. Compared with other recipients, these recipients were more likely to have a primary diagnosis of chronic obstructive pulmonary disease and less likely to have a diagnosis of idiopathic pulmonary fibrosis. Otherwise, they were similar.
The rate of deaths due to cancer was based on case reports, as UNOS does not capture this outcome. Cancer deaths were 5.8% among recipients of lungs from heavy smokers and 3.6% among other recipients.
"There is a fairly low capture rate for this field, so it’s difficult to draw significant conclusions from it," cautioned Dr. Taghavi.
Patients who received lungs from heavy smokers had a 1-day longer length of stay in the hospital (18 days vs. 17 days), which "may not really be clinically relevant." Rates of acute rejection during hospitalization were comparable (10.7% vs. 8.8%), as was post-transplant airway dehiscence (1.8% vs. 1.8%).
Post-transplant peak forced expiratory volume in 1 second (FEV1) was the same (80% vs. 79%), as was decline in this measure over time. Median duration of freedom from bronchiolitis obliterans syndrome was 1,583 days vs. 1,827 days.
Risk-adjusted median all-cause survival – the study’s primary endpoint – did not differ significantly between the recipients given lungs from donors who smoked heavily and the other recipients (2,043 vs. 1,928 days).
The rate of cancer deaths did not differ significantly; however, the follow-up time is too short to address this concern in a meaningful way, Dr. Taghavi said.
"Currently, we recommend when evaluating a donor who has a heavy smoking history, that they undergo a thorough examination for lung tumors or evidence of cancer. This includes obtaining a chest x-ray, CT scans, and bronchoscopies. In addition, when the lungs are procured, they should undergo a very thorough visual inspection," he advised.
"Informed consent is very important. You have to discuss the donor’s smoking status with the recipient and explain the risks and the benefits," Dr. Taghavi said. Lung cancer risk, given the donor’s history, is about 1% to 2% annually, and that needs to be considered against the high likelihood of dying within 1 or 2 years without a transplant.
"One thing that is unquestionable is that survival will be better accepting these lungs than it will be sitting on a waiting list," he added. Only about half of the people listed for lung transplant in the United States each year actually undergo the surgery.
Recipients of lungs from heavy smokers do not need any extra follow-up or surveillance, as they are already diligently tested and monitored, according to Dr. Taghavi. The recipient’s immunosuppression does theoretically put one at additional risk for lung cancer.
Current guidelines of the International Society of Heart and Lung Transplantation advise against considering use of lungs from donors who have a smoking history of more than 20 pack-years, Dr. Taghavi noted. But he stopped short of saying that the study should prompt a formal revision of those guidelines.
"I think the findings start the conversation," he commented. "We should consider looking at these potential donors," especially when a recipient’s situation is dire.
Dr. Taghavi disclosed no conflicts of interest.
LOS ANGELES – Use of lungs from donors who smoked heavily does not worsen lung transplantation outcomes including risk for lung cancer death, at least in the medium term.
At a median follow-up of 2 years for 5,900 adults who had double-lung transplants, those who received lungs from heavy smokers had an actuarial median overall survival of roughly 5.5 years, and their lung function was essentially the same as that of patients who received lungs from other donors, Dr. Sharven Taghavi reported at the annual meeting of the Society of Thoracic Surgeons.
The study data came from the United Network for Organ Sharing (UNOS) database. A team led by Dr. Taghavi, of Temple University Hospital in Philadelphia, compared data for double-lung transplants from 2005-2011, comparing donors with a history of smoking exceeding 20 pack-years with other donors.
About 13% of the study patients received lungs from donors who had smoked heavily. Compared with other recipients, these recipients were more likely to have a primary diagnosis of chronic obstructive pulmonary disease and less likely to have a diagnosis of idiopathic pulmonary fibrosis. Otherwise, they were similar.
The rate of deaths due to cancer was based on case reports, as UNOS does not capture this outcome. Cancer deaths were 5.8% among recipients of lungs from heavy smokers and 3.6% among other recipients.
"There is a fairly low capture rate for this field, so it’s difficult to draw significant conclusions from it," cautioned Dr. Taghavi.
Patients who received lungs from heavy smokers had a 1-day longer length of stay in the hospital (18 days vs. 17 days), which "may not really be clinically relevant." Rates of acute rejection during hospitalization were comparable (10.7% vs. 8.8%), as was post-transplant airway dehiscence (1.8% vs. 1.8%).
Post-transplant peak forced expiratory volume in 1 second (FEV1) was the same (80% vs. 79%), as was decline in this measure over time. Median duration of freedom from bronchiolitis obliterans syndrome was 1,583 days vs. 1,827 days.
Risk-adjusted median all-cause survival – the study’s primary endpoint – did not differ significantly between the recipients given lungs from donors who smoked heavily and the other recipients (2,043 vs. 1,928 days).
The rate of cancer deaths did not differ significantly; however, the follow-up time is too short to address this concern in a meaningful way, Dr. Taghavi said.
"Currently, we recommend when evaluating a donor who has a heavy smoking history, that they undergo a thorough examination for lung tumors or evidence of cancer. This includes obtaining a chest x-ray, CT scans, and bronchoscopies. In addition, when the lungs are procured, they should undergo a very thorough visual inspection," he advised.
"Informed consent is very important. You have to discuss the donor’s smoking status with the recipient and explain the risks and the benefits," Dr. Taghavi said. Lung cancer risk, given the donor’s history, is about 1% to 2% annually, and that needs to be considered against the high likelihood of dying within 1 or 2 years without a transplant.
"One thing that is unquestionable is that survival will be better accepting these lungs than it will be sitting on a waiting list," he added. Only about half of the people listed for lung transplant in the United States each year actually undergo the surgery.
Recipients of lungs from heavy smokers do not need any extra follow-up or surveillance, as they are already diligently tested and monitored, according to Dr. Taghavi. The recipient’s immunosuppression does theoretically put one at additional risk for lung cancer.
Current guidelines of the International Society of Heart and Lung Transplantation advise against considering use of lungs from donors who have a smoking history of more than 20 pack-years, Dr. Taghavi noted. But he stopped short of saying that the study should prompt a formal revision of those guidelines.
"I think the findings start the conversation," he commented. "We should consider looking at these potential donors," especially when a recipient’s situation is dire.
Dr. Taghavi disclosed no conflicts of interest.
AT THE ANNUAL MEETING OF THE SOCIETY OF THROACIC SURGEONS
Major Finding: Risk-adjusted median all-cause survival did not differ significantly between patients given lungs from donors who smoked heavily and those receiving lungs from donors who did not smoke heavily (2,043 vs. 1,928 days).
Data Source: An observational cohort study of 5,900 adult primary double-lung transplant recipients in the UNOS database
Disclosures: Dr. Taghavi disclosed no relevant conflicts of interest.
New approaches expand kidney transplant pool
PALM BEACH, FLA. – Renal transplant surgeons are using novel methods to expand the pool of donor organs: Using kidneys from donors with acute kidney injury, and vetting and improving the function of kidneys by applying pulsatile machine perfusion to stored kidneys pending transplant.
These approaches can overlap, as machine perfusion has become an important tool for improving the function of kidneys from donors with acute kidney injury (AKI) as well as other marginal kidneys such as those from extended-criteria donors and donation after cardiac death.
Surgeons at Wake Forest University, Winston-Salem, N.C., began transplanting kidneys from AKI donors in 2007, and by mid-2012 they had placed 84 of these organs, resulting in actuarial 5-year patient-survival and graft-survival rates that matched transplants during the same period with kidneys from non-AKI donors, Dr. Alan C. Farney said at the annual meeting of the Southern Surgical Association.
Seventy-four of these kidneys (88%) underwent machine perfusion, for a minimum of 6 hours and more often overnight, said Dr. Farney’s colleague, Dr. Robert J. Stratta, professor of surgery at Wake Forest. "We try to pump whenever possible, and in a perfect world we’d like to see all kidneys pumped" before they are transplanted, Dr. Stratta said. In addition to improving function, mechanical perfusion allows surgeons to assess kidney function. If resistance in the kidney is more than 0.4 or 0.5 mm Hg/mL per minute, "we tend to discard it," he noted.
A second report at the meeting further documented the ability of mechanical perfusion to boost kidney function. In a review of more than 50,000 adult, isolated kidney transplants done on American patients during January 2005–March 2011, machine perfusion prior to transplant led to an average 8-percentage-point cut in the rate of delayed kidney function in a pair of analyses that accounted for baseline patient differences. This means that every 13 kidneys treated before transplant with mechanical perfusion prevented a case of delayed graft function (DGF) following transplantation, resulting in fewer patients requiring hemodialysis, Dr. Glen A. Franklin reported at the meeting.
Prevention of DGF mitigates edema, reduces the need for wound drainage, and decreases the risk for infection, factors that – along with the need for dialysis – drive up costs. Preventing these complications and their associated costs potentially offsets the extra expense of routinely perfusing each kidney before transplantation, Dr. Stratta said.
Dr. Stratta and his associates reviewed the outcomes of 84 transplants of kidneys from donors with AKI done at Wake Forest since 2007 and compared this against the outcomes of 283 concurrent kidney transplants performed during the same 2007-2012 period using organs from donors without AKI. A major, statistically significant difference in protocol for the two types of organs was that 88% of the AKI-derived kidneys underwent machine perfusion before transplant, compared with 51% of the kidneys that came from non-AKI donors, reported Dr. Farney, professor of surgery at Wake Forest.
A major difference in outcomes was that the incidence of DGF following transplantation occurred in 41% of patients who received a kidney from an AKI donor, compared with a 27% DGF rate among patients whose kidneys came from non-AKI donors, a statistically-significant difference.
Despite this, actuarial 5-year patient survival was 98% among the AKI kidney recipients and 90% among the non-AKI kidney recipients. Five-year graft survival was 78% in the AKI-kidney recipients and 71% in patients who received a non-AKI organ. The between-group differences were not statistically significant, Dr. Farney said.
The data also showed an unexpected difference in the way that DGF appeared to affect graft survival. Among patients whose kidneys came from non-AKI donors, the 5-year graft survival rate was 90% among the 206 patients who did not have DGF, but fell to 68% among the 77 patients in this group who had DGF, a statistically-significant difference. In contrast, among patients who received kidneys from AKI donors, the incidence of DGF had no significant impact on long-term graft survival.
The data also showed that the severity of AKI had no significant impact on graft survival. Donors with terminal estimated glomerular filtration rates of 10-20 mL/min per 1.73 m2 had graft survival rates similar to those of patients who received kidneys from AKI donors with terminal estimated glomerular filtration rates above 30 mL/min per 1.732.
Overall, the results suggest that "using kidneys from AKI donors is a safe method to significantly expand the donor pool for kidney transplantation," Dr. Farney concluded.
"I’m impressed with how, for several years, the Wake Forest group has used kidneys that others may have discarded. The outcomes they report are quite encouraging," commented Dr. Douglas P. Slakey, professor and chairman of surgery at Tulane Medical Center, New Orleans.
The impact that machine perfusion of kidneys can have on DGF before transplantation was examined in a much larger data set by Dr. Franklin and his associates at the University of Louisville (Ky.). They reviewed data collected by the United Network for Organ Sharing on 52,052 isolated, adult U.S. kidney transplants during January 2005–March 2011. The series included 19,372 kidneys (37%) that underwent machine perfusion before transplant.
A propensity-score analysis that compared 13,293 organ recipients who received perfused kidneys with 13,293 recipients who received nonperfused kidneys and matched by a variety of donor and recipient characteristics showed that the incidence of DGF during the first week following transplantation was 21% among the perfused organ recipients. The incidence among patients who received a nonperfused kidney was 29%, a statistically significant difference, said Dr. Franklin, a professor of surgery at the University of Louisville.
A second analysis focused on pairs of kidneys that came from 2,290 donors where one kidney underwent perfusion and the other did not. After adjustment for recipient differences, the incidence of DGF was 20% in recipients who received a perfused kidney and 28% in those who received a nonperfused kidney, again an 8% difference that was statistically significant.
The cost of machine perfusion of a kidney varies from region to region, but at Louisville runs about $1,000 to $2,000 per organ, said Dr. Robert M. Cannon, a surgeon at the University of Louisville and a collaborator on the study. "I think you can justify this cost based on the decrease in DGF," and because it allows scheduling of transplants during usual operating-room hours, eliminating the need for emergency transplant surgery in the middle of the night, Dr. Cannon said in an interview.
Several hours of machine perfusion also likely improves kidney function, he noted. "With cold storage, kidneys undergo intense vasospasm that damages the organ. Machine perfusion alleviates that to an extent, and gets more preservation fluid into the organ."
Dr. Farney, Dr. Stratta, Dr. Franklin, and Dr. Cannon, and Dr. Slakey had no disclosures to report.
On Twitter @mitchelzoler
PALM BEACH, FLA. – Renal transplant surgeons are using novel methods to expand the pool of donor organs: Using kidneys from donors with acute kidney injury, and vetting and improving the function of kidneys by applying pulsatile machine perfusion to stored kidneys pending transplant.
These approaches can overlap, as machine perfusion has become an important tool for improving the function of kidneys from donors with acute kidney injury (AKI) as well as other marginal kidneys such as those from extended-criteria donors and donation after cardiac death.
Surgeons at Wake Forest University, Winston-Salem, N.C., began transplanting kidneys from AKI donors in 2007, and by mid-2012 they had placed 84 of these organs, resulting in actuarial 5-year patient-survival and graft-survival rates that matched transplants during the same period with kidneys from non-AKI donors, Dr. Alan C. Farney said at the annual meeting of the Southern Surgical Association.
Seventy-four of these kidneys (88%) underwent machine perfusion, for a minimum of 6 hours and more often overnight, said Dr. Farney’s colleague, Dr. Robert J. Stratta, professor of surgery at Wake Forest. "We try to pump whenever possible, and in a perfect world we’d like to see all kidneys pumped" before they are transplanted, Dr. Stratta said. In addition to improving function, mechanical perfusion allows surgeons to assess kidney function. If resistance in the kidney is more than 0.4 or 0.5 mm Hg/mL per minute, "we tend to discard it," he noted.
A second report at the meeting further documented the ability of mechanical perfusion to boost kidney function. In a review of more than 50,000 adult, isolated kidney transplants done on American patients during January 2005–March 2011, machine perfusion prior to transplant led to an average 8-percentage-point cut in the rate of delayed kidney function in a pair of analyses that accounted for baseline patient differences. This means that every 13 kidneys treated before transplant with mechanical perfusion prevented a case of delayed graft function (DGF) following transplantation, resulting in fewer patients requiring hemodialysis, Dr. Glen A. Franklin reported at the meeting.
Prevention of DGF mitigates edema, reduces the need for wound drainage, and decreases the risk for infection, factors that – along with the need for dialysis – drive up costs. Preventing these complications and their associated costs potentially offsets the extra expense of routinely perfusing each kidney before transplantation, Dr. Stratta said.
Dr. Stratta and his associates reviewed the outcomes of 84 transplants of kidneys from donors with AKI done at Wake Forest since 2007 and compared this against the outcomes of 283 concurrent kidney transplants performed during the same 2007-2012 period using organs from donors without AKI. A major, statistically significant difference in protocol for the two types of organs was that 88% of the AKI-derived kidneys underwent machine perfusion before transplant, compared with 51% of the kidneys that came from non-AKI donors, reported Dr. Farney, professor of surgery at Wake Forest.
A major difference in outcomes was that the incidence of DGF following transplantation occurred in 41% of patients who received a kidney from an AKI donor, compared with a 27% DGF rate among patients whose kidneys came from non-AKI donors, a statistically-significant difference.
Despite this, actuarial 5-year patient survival was 98% among the AKI kidney recipients and 90% among the non-AKI kidney recipients. Five-year graft survival was 78% in the AKI-kidney recipients and 71% in patients who received a non-AKI organ. The between-group differences were not statistically significant, Dr. Farney said.
The data also showed an unexpected difference in the way that DGF appeared to affect graft survival. Among patients whose kidneys came from non-AKI donors, the 5-year graft survival rate was 90% among the 206 patients who did not have DGF, but fell to 68% among the 77 patients in this group who had DGF, a statistically-significant difference. In contrast, among patients who received kidneys from AKI donors, the incidence of DGF had no significant impact on long-term graft survival.
The data also showed that the severity of AKI had no significant impact on graft survival. Donors with terminal estimated glomerular filtration rates of 10-20 mL/min per 1.73 m2 had graft survival rates similar to those of patients who received kidneys from AKI donors with terminal estimated glomerular filtration rates above 30 mL/min per 1.732.
Overall, the results suggest that "using kidneys from AKI donors is a safe method to significantly expand the donor pool for kidney transplantation," Dr. Farney concluded.
"I’m impressed with how, for several years, the Wake Forest group has used kidneys that others may have discarded. The outcomes they report are quite encouraging," commented Dr. Douglas P. Slakey, professor and chairman of surgery at Tulane Medical Center, New Orleans.
The impact that machine perfusion of kidneys can have on DGF before transplantation was examined in a much larger data set by Dr. Franklin and his associates at the University of Louisville (Ky.). They reviewed data collected by the United Network for Organ Sharing on 52,052 isolated, adult U.S. kidney transplants during January 2005–March 2011. The series included 19,372 kidneys (37%) that underwent machine perfusion before transplant.
A propensity-score analysis that compared 13,293 organ recipients who received perfused kidneys with 13,293 recipients who received nonperfused kidneys and matched by a variety of donor and recipient characteristics showed that the incidence of DGF during the first week following transplantation was 21% among the perfused organ recipients. The incidence among patients who received a nonperfused kidney was 29%, a statistically significant difference, said Dr. Franklin, a professor of surgery at the University of Louisville.
A second analysis focused on pairs of kidneys that came from 2,290 donors where one kidney underwent perfusion and the other did not. After adjustment for recipient differences, the incidence of DGF was 20% in recipients who received a perfused kidney and 28% in those who received a nonperfused kidney, again an 8% difference that was statistically significant.
The cost of machine perfusion of a kidney varies from region to region, but at Louisville runs about $1,000 to $2,000 per organ, said Dr. Robert M. Cannon, a surgeon at the University of Louisville and a collaborator on the study. "I think you can justify this cost based on the decrease in DGF," and because it allows scheduling of transplants during usual operating-room hours, eliminating the need for emergency transplant surgery in the middle of the night, Dr. Cannon said in an interview.
Several hours of machine perfusion also likely improves kidney function, he noted. "With cold storage, kidneys undergo intense vasospasm that damages the organ. Machine perfusion alleviates that to an extent, and gets more preservation fluid into the organ."
Dr. Farney, Dr. Stratta, Dr. Franklin, and Dr. Cannon, and Dr. Slakey had no disclosures to report.
On Twitter @mitchelzoler
PALM BEACH, FLA. – Renal transplant surgeons are using novel methods to expand the pool of donor organs: Using kidneys from donors with acute kidney injury, and vetting and improving the function of kidneys by applying pulsatile machine perfusion to stored kidneys pending transplant.
These approaches can overlap, as machine perfusion has become an important tool for improving the function of kidneys from donors with acute kidney injury (AKI) as well as other marginal kidneys such as those from extended-criteria donors and donation after cardiac death.
Surgeons at Wake Forest University, Winston-Salem, N.C., began transplanting kidneys from AKI donors in 2007, and by mid-2012 they had placed 84 of these organs, resulting in actuarial 5-year patient-survival and graft-survival rates that matched transplants during the same period with kidneys from non-AKI donors, Dr. Alan C. Farney said at the annual meeting of the Southern Surgical Association.
Seventy-four of these kidneys (88%) underwent machine perfusion, for a minimum of 6 hours and more often overnight, said Dr. Farney’s colleague, Dr. Robert J. Stratta, professor of surgery at Wake Forest. "We try to pump whenever possible, and in a perfect world we’d like to see all kidneys pumped" before they are transplanted, Dr. Stratta said. In addition to improving function, mechanical perfusion allows surgeons to assess kidney function. If resistance in the kidney is more than 0.4 or 0.5 mm Hg/mL per minute, "we tend to discard it," he noted.
A second report at the meeting further documented the ability of mechanical perfusion to boost kidney function. In a review of more than 50,000 adult, isolated kidney transplants done on American patients during January 2005–March 2011, machine perfusion prior to transplant led to an average 8-percentage-point cut in the rate of delayed kidney function in a pair of analyses that accounted for baseline patient differences. This means that every 13 kidneys treated before transplant with mechanical perfusion prevented a case of delayed graft function (DGF) following transplantation, resulting in fewer patients requiring hemodialysis, Dr. Glen A. Franklin reported at the meeting.
Prevention of DGF mitigates edema, reduces the need for wound drainage, and decreases the risk for infection, factors that – along with the need for dialysis – drive up costs. Preventing these complications and their associated costs potentially offsets the extra expense of routinely perfusing each kidney before transplantation, Dr. Stratta said.
Dr. Stratta and his associates reviewed the outcomes of 84 transplants of kidneys from donors with AKI done at Wake Forest since 2007 and compared this against the outcomes of 283 concurrent kidney transplants performed during the same 2007-2012 period using organs from donors without AKI. A major, statistically significant difference in protocol for the two types of organs was that 88% of the AKI-derived kidneys underwent machine perfusion before transplant, compared with 51% of the kidneys that came from non-AKI donors, reported Dr. Farney, professor of surgery at Wake Forest.
A major difference in outcomes was that the incidence of DGF following transplantation occurred in 41% of patients who received a kidney from an AKI donor, compared with a 27% DGF rate among patients whose kidneys came from non-AKI donors, a statistically-significant difference.
Despite this, actuarial 5-year patient survival was 98% among the AKI kidney recipients and 90% among the non-AKI kidney recipients. Five-year graft survival was 78% in the AKI-kidney recipients and 71% in patients who received a non-AKI organ. The between-group differences were not statistically significant, Dr. Farney said.
The data also showed an unexpected difference in the way that DGF appeared to affect graft survival. Among patients whose kidneys came from non-AKI donors, the 5-year graft survival rate was 90% among the 206 patients who did not have DGF, but fell to 68% among the 77 patients in this group who had DGF, a statistically-significant difference. In contrast, among patients who received kidneys from AKI donors, the incidence of DGF had no significant impact on long-term graft survival.
The data also showed that the severity of AKI had no significant impact on graft survival. Donors with terminal estimated glomerular filtration rates of 10-20 mL/min per 1.73 m2 had graft survival rates similar to those of patients who received kidneys from AKI donors with terminal estimated glomerular filtration rates above 30 mL/min per 1.732.
Overall, the results suggest that "using kidneys from AKI donors is a safe method to significantly expand the donor pool for kidney transplantation," Dr. Farney concluded.
"I’m impressed with how, for several years, the Wake Forest group has used kidneys that others may have discarded. The outcomes they report are quite encouraging," commented Dr. Douglas P. Slakey, professor and chairman of surgery at Tulane Medical Center, New Orleans.
The impact that machine perfusion of kidneys can have on DGF before transplantation was examined in a much larger data set by Dr. Franklin and his associates at the University of Louisville (Ky.). They reviewed data collected by the United Network for Organ Sharing on 52,052 isolated, adult U.S. kidney transplants during January 2005–March 2011. The series included 19,372 kidneys (37%) that underwent machine perfusion before transplant.
A propensity-score analysis that compared 13,293 organ recipients who received perfused kidneys with 13,293 recipients who received nonperfused kidneys and matched by a variety of donor and recipient characteristics showed that the incidence of DGF during the first week following transplantation was 21% among the perfused organ recipients. The incidence among patients who received a nonperfused kidney was 29%, a statistically significant difference, said Dr. Franklin, a professor of surgery at the University of Louisville.
A second analysis focused on pairs of kidneys that came from 2,290 donors where one kidney underwent perfusion and the other did not. After adjustment for recipient differences, the incidence of DGF was 20% in recipients who received a perfused kidney and 28% in those who received a nonperfused kidney, again an 8% difference that was statistically significant.
The cost of machine perfusion of a kidney varies from region to region, but at Louisville runs about $1,000 to $2,000 per organ, said Dr. Robert M. Cannon, a surgeon at the University of Louisville and a collaborator on the study. "I think you can justify this cost based on the decrease in DGF," and because it allows scheduling of transplants during usual operating-room hours, eliminating the need for emergency transplant surgery in the middle of the night, Dr. Cannon said in an interview.
Several hours of machine perfusion also likely improves kidney function, he noted. "With cold storage, kidneys undergo intense vasospasm that damages the organ. Machine perfusion alleviates that to an extent, and gets more preservation fluid into the organ."
Dr. Farney, Dr. Stratta, Dr. Franklin, and Dr. Cannon, and Dr. Slakey had no disclosures to report.
On Twitter @mitchelzoler
AT THE ANNUAL MEETING OF THE SOUTHERN SURGICAL ASSOCIATION
Major Finding: Machine perfusion of donor kidneys before transplantation cut delayed-graft function rate by 8%.
Data Source: A review of 52,052 U.S. adults who received an isolated kidney transplant during 2007-2012.
Disclosures:. Dr. Farney, Dr. Stratta, Dr. Franklin, and Dr. Cannon, and Dr. Slakey had no disclosures to report.
Comprehensive mechanical circulatory support guidelines issued
As a further sign of how much mechanical circulatory support for advanced heart failure has matured, the International Society of Heart and Lung Transplantation issued on Jan. 10 the first comprehensive guidelines for all phases of evaluating, implanting, and managing patients who receive left ventricular assist devices or related equipment.
"Traditionally management of patients with mechanical circulatory support [MCS] was very center specific, but because the number of treated patients has increased, and because patients now live with these devices for years, we reached a point where we needed best practices guidelines, an expert consensus on what is the best way to approach this treatment" said Dr. Salpy V. Pamboukian, a cardiologist and one of three cochairs of the guidelines-writing project.
"When MSC started, the role of the devices was as a bridge to heart transplantation, but the field has evolved over the past decade and now MCS for destination therapy has opened a new array of patients who could benefit from these devices," said Dr. Pamboukian, medical director of the MCS device program at the University of Alabama, Birmingham. "We hope these guidelines will serve as a springboard for further research into the long-term management of these patients," she said in an interview.
"As pumps improve and the number of patients with advanced heart failure increases more and more patients will receive a ventricular assist device [VAD], and heart transplant will grow less relevant. These guidelines are much more comprehensive [than anything previously published] and they represent the opinions of the physicians, surgeons, nurses, and other providers who care for these patients," said Dr. David S. Feldman, a cardiologist who is director of the heart failure, VAD, and cardiac transplantation program at the Minneapolis Heart Institute at Abbott Northwestern Hospital, and another cochair of the guidelines committee.
The guidelines, which took about 3 years to produce, came from a committee of 35 health care providers, with initial review by three independent experts followed by additional peer review and then a period of open comment from the society’s membership. The 146-page document consists of more than 250 individual recommendations presented in five sections: patient selection; risk management prior to surgery; intraoperative procedures and immediate postoperative management; in-patient management during the immediate postoperative period; and long-term outpatient management (J. Heart Lung Transplant. 2013;32:157-87).
The writing committee admitted up front in the paper that most of the recommendations are consensus opinions with no clear evidence base. "It’s a limitation," admitted Dr. Pamboukian, "but you need a common approach to patients. Even a busy center may put in 50 or 60 VADs a year. Hopefully, a result of the guidelines is that they will help centers get together and produce the critical mass of patients needed to conduct meaningful trials. It was time to get something on paper; the new guidelines are what we will now work off of." But despite an absence of evidence on which to base many recommendations, "I was pleasantly surprised that there was more consensus than controversy. There was more commonality in our approaches than differences," she added.
The most limited number of recommendations came from the third task force of the panel, which handled intraoperative procedures and immediate postoperative care. Though this section runs 17 pages and deals with topics such as anesthesia, implantation techniques, establishing hemostasis, performing concomitant procedures, methods for explantation, and management of postoperative hemodynamics and bleeding, it contains just three specific recommendations, all dealing with anesthesia. "There are essentially no studies that have looked at how to make things better in the surgical suite," explained Dr. Feldman.
"It’s very challenging to standardize a surgical procedure," added Dr. Pamboukian. "We tried to summarize useful practices, but consensus-based recommendations are difficult to do."
Another topic the guidelines finesse is patient selection. The field is currently trying to sort out the best stage of advanced heart failure for patients to receive mechanical circulatory support. "You’d be amazed at the disparity of who gets these devices now," Dr. Feldman said. In addition, the guideline writing committee decided to defer definitive choices until results are available from a large study starting later this year. The study, Evaluation of VAD Intervention Before Inotropic Therapy (REVIVE-IT), will examine the outcomes of patients with advanced New York Heart Association stage III heart failure who receive a VAD. "It didn’t seem appropriate to address this because of the trial," he added.
Both Dr. Pamboukian and Dr. Feldman agreed that the newly released guidelines will likely be in place for only a couple of years before a revision comes out, testament to the rapid changes in this field. Dr. Feldman cited new VADs from at least two manufacturers expected to enter first-in-man studies this year, and the continued snowballing of VAD implantation rates. The most recent 2012 numbers (through Sept. 30, 2012) from the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) showed nearly 2,000 VADS getting implanted into U.S. patients last year, the highest annual rate ever.
"Because the field is growing, a lot of new centers want to establish programs. We want this treatment to reach as many appropriate patients as possible, but we want it to grow responsibly. These guidelines help establish the best practices, and help ensure that patients get the best care wherever they go," Dr. Pamboukian said.
Dr. Pamboukian said that she had no disclosures. Dr. Feldman said that he has received research support from Terumo.
As a further sign of how much mechanical circulatory support for advanced heart failure has matured, the International Society of Heart and Lung Transplantation issued on Jan. 10 the first comprehensive guidelines for all phases of evaluating, implanting, and managing patients who receive left ventricular assist devices or related equipment.
"Traditionally management of patients with mechanical circulatory support [MCS] was very center specific, but because the number of treated patients has increased, and because patients now live with these devices for years, we reached a point where we needed best practices guidelines, an expert consensus on what is the best way to approach this treatment" said Dr. Salpy V. Pamboukian, a cardiologist and one of three cochairs of the guidelines-writing project.
"When MSC started, the role of the devices was as a bridge to heart transplantation, but the field has evolved over the past decade and now MCS for destination therapy has opened a new array of patients who could benefit from these devices," said Dr. Pamboukian, medical director of the MCS device program at the University of Alabama, Birmingham. "We hope these guidelines will serve as a springboard for further research into the long-term management of these patients," she said in an interview.
"As pumps improve and the number of patients with advanced heart failure increases more and more patients will receive a ventricular assist device [VAD], and heart transplant will grow less relevant. These guidelines are much more comprehensive [than anything previously published] and they represent the opinions of the physicians, surgeons, nurses, and other providers who care for these patients," said Dr. David S. Feldman, a cardiologist who is director of the heart failure, VAD, and cardiac transplantation program at the Minneapolis Heart Institute at Abbott Northwestern Hospital, and another cochair of the guidelines committee.
The guidelines, which took about 3 years to produce, came from a committee of 35 health care providers, with initial review by three independent experts followed by additional peer review and then a period of open comment from the society’s membership. The 146-page document consists of more than 250 individual recommendations presented in five sections: patient selection; risk management prior to surgery; intraoperative procedures and immediate postoperative management; in-patient management during the immediate postoperative period; and long-term outpatient management (J. Heart Lung Transplant. 2013;32:157-87).
The writing committee admitted up front in the paper that most of the recommendations are consensus opinions with no clear evidence base. "It’s a limitation," admitted Dr. Pamboukian, "but you need a common approach to patients. Even a busy center may put in 50 or 60 VADs a year. Hopefully, a result of the guidelines is that they will help centers get together and produce the critical mass of patients needed to conduct meaningful trials. It was time to get something on paper; the new guidelines are what we will now work off of." But despite an absence of evidence on which to base many recommendations, "I was pleasantly surprised that there was more consensus than controversy. There was more commonality in our approaches than differences," she added.
The most limited number of recommendations came from the third task force of the panel, which handled intraoperative procedures and immediate postoperative care. Though this section runs 17 pages and deals with topics such as anesthesia, implantation techniques, establishing hemostasis, performing concomitant procedures, methods for explantation, and management of postoperative hemodynamics and bleeding, it contains just three specific recommendations, all dealing with anesthesia. "There are essentially no studies that have looked at how to make things better in the surgical suite," explained Dr. Feldman.
"It’s very challenging to standardize a surgical procedure," added Dr. Pamboukian. "We tried to summarize useful practices, but consensus-based recommendations are difficult to do."
Another topic the guidelines finesse is patient selection. The field is currently trying to sort out the best stage of advanced heart failure for patients to receive mechanical circulatory support. "You’d be amazed at the disparity of who gets these devices now," Dr. Feldman said. In addition, the guideline writing committee decided to defer definitive choices until results are available from a large study starting later this year. The study, Evaluation of VAD Intervention Before Inotropic Therapy (REVIVE-IT), will examine the outcomes of patients with advanced New York Heart Association stage III heart failure who receive a VAD. "It didn’t seem appropriate to address this because of the trial," he added.
Both Dr. Pamboukian and Dr. Feldman agreed that the newly released guidelines will likely be in place for only a couple of years before a revision comes out, testament to the rapid changes in this field. Dr. Feldman cited new VADs from at least two manufacturers expected to enter first-in-man studies this year, and the continued snowballing of VAD implantation rates. The most recent 2012 numbers (through Sept. 30, 2012) from the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) showed nearly 2,000 VADS getting implanted into U.S. patients last year, the highest annual rate ever.
"Because the field is growing, a lot of new centers want to establish programs. We want this treatment to reach as many appropriate patients as possible, but we want it to grow responsibly. These guidelines help establish the best practices, and help ensure that patients get the best care wherever they go," Dr. Pamboukian said.
Dr. Pamboukian said that she had no disclosures. Dr. Feldman said that he has received research support from Terumo.
As a further sign of how much mechanical circulatory support for advanced heart failure has matured, the International Society of Heart and Lung Transplantation issued on Jan. 10 the first comprehensive guidelines for all phases of evaluating, implanting, and managing patients who receive left ventricular assist devices or related equipment.
"Traditionally management of patients with mechanical circulatory support [MCS] was very center specific, but because the number of treated patients has increased, and because patients now live with these devices for years, we reached a point where we needed best practices guidelines, an expert consensus on what is the best way to approach this treatment" said Dr. Salpy V. Pamboukian, a cardiologist and one of three cochairs of the guidelines-writing project.
"When MSC started, the role of the devices was as a bridge to heart transplantation, but the field has evolved over the past decade and now MCS for destination therapy has opened a new array of patients who could benefit from these devices," said Dr. Pamboukian, medical director of the MCS device program at the University of Alabama, Birmingham. "We hope these guidelines will serve as a springboard for further research into the long-term management of these patients," she said in an interview.
"As pumps improve and the number of patients with advanced heart failure increases more and more patients will receive a ventricular assist device [VAD], and heart transplant will grow less relevant. These guidelines are much more comprehensive [than anything previously published] and they represent the opinions of the physicians, surgeons, nurses, and other providers who care for these patients," said Dr. David S. Feldman, a cardiologist who is director of the heart failure, VAD, and cardiac transplantation program at the Minneapolis Heart Institute at Abbott Northwestern Hospital, and another cochair of the guidelines committee.
The guidelines, which took about 3 years to produce, came from a committee of 35 health care providers, with initial review by three independent experts followed by additional peer review and then a period of open comment from the society’s membership. The 146-page document consists of more than 250 individual recommendations presented in five sections: patient selection; risk management prior to surgery; intraoperative procedures and immediate postoperative management; in-patient management during the immediate postoperative period; and long-term outpatient management (J. Heart Lung Transplant. 2013;32:157-87).
The writing committee admitted up front in the paper that most of the recommendations are consensus opinions with no clear evidence base. "It’s a limitation," admitted Dr. Pamboukian, "but you need a common approach to patients. Even a busy center may put in 50 or 60 VADs a year. Hopefully, a result of the guidelines is that they will help centers get together and produce the critical mass of patients needed to conduct meaningful trials. It was time to get something on paper; the new guidelines are what we will now work off of." But despite an absence of evidence on which to base many recommendations, "I was pleasantly surprised that there was more consensus than controversy. There was more commonality in our approaches than differences," she added.
The most limited number of recommendations came from the third task force of the panel, which handled intraoperative procedures and immediate postoperative care. Though this section runs 17 pages and deals with topics such as anesthesia, implantation techniques, establishing hemostasis, performing concomitant procedures, methods for explantation, and management of postoperative hemodynamics and bleeding, it contains just three specific recommendations, all dealing with anesthesia. "There are essentially no studies that have looked at how to make things better in the surgical suite," explained Dr. Feldman.
"It’s very challenging to standardize a surgical procedure," added Dr. Pamboukian. "We tried to summarize useful practices, but consensus-based recommendations are difficult to do."
Another topic the guidelines finesse is patient selection. The field is currently trying to sort out the best stage of advanced heart failure for patients to receive mechanical circulatory support. "You’d be amazed at the disparity of who gets these devices now," Dr. Feldman said. In addition, the guideline writing committee decided to defer definitive choices until results are available from a large study starting later this year. The study, Evaluation of VAD Intervention Before Inotropic Therapy (REVIVE-IT), will examine the outcomes of patients with advanced New York Heart Association stage III heart failure who receive a VAD. "It didn’t seem appropriate to address this because of the trial," he added.
Both Dr. Pamboukian and Dr. Feldman agreed that the newly released guidelines will likely be in place for only a couple of years before a revision comes out, testament to the rapid changes in this field. Dr. Feldman cited new VADs from at least two manufacturers expected to enter first-in-man studies this year, and the continued snowballing of VAD implantation rates. The most recent 2012 numbers (through Sept. 30, 2012) from the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) showed nearly 2,000 VADS getting implanted into U.S. patients last year, the highest annual rate ever.
"Because the field is growing, a lot of new centers want to establish programs. We want this treatment to reach as many appropriate patients as possible, but we want it to grow responsibly. These guidelines help establish the best practices, and help ensure that patients get the best care wherever they go," Dr. Pamboukian said.
Dr. Pamboukian said that she had no disclosures. Dr. Feldman said that he has received research support from Terumo.
FROM THE JOURNAL OF HEART AND LUNG TRANSPLANTATION
In Type 1 Diabetes, Cardiac Measures Improved After Pancreas Transplant
BERLIN -- A pancreas-only transplant improved cardiac function and morphology in a group of patients with type 1 diabetes.
After 5 years, the patients showed significantly improved posterior wall and interventricular septal thickness, as well as a significantly increased left ventricular ejection fraction, Dr. Margherita Occhipinti said at the annual meeting of the European Societies for the Study of Diabetes.
She reported 5-year follow-up data on 35 patients with type 1 diabetes who underwent the procedure. The patients were a mean of 38 years old and had a mean disease duration of 25 years. Their mean insulin requirement was 43 U/day.
Most of the transplants (74%) were performed with a portal-enteric drain technique; the remainder had systemic-enteric drainage, said Dr. Occhipinti of the University of Pisa (Italy). The majority (77%) had induction therapy with basiliximab; the rest had antithymocyte globulin (rabbit) induction. The maintenance immunosuppressant regimen was a combination of mycophenolate mofetil, tacrolimus, and steroids.
At last follow-up, fasting plasma glucose level had normalized, hemoglobin A1c level had fallen from 9% to just under 6%, and C-peptide level had increased from under 1 ng/mL to almost 3 ng/mL.
There were no significant changes in either systolic or diastolic blood pressure. However, the number of patients taking ACE inhibitors or angiotensin receptor blockers decreased from 59% to 43%. Total and LDL cholesterol levels decreased significantly, although there were no significant changes in HDL cholesterol or triglycerides.
Cardiac morphology changed significantly, Dr. Occhipinti said, including a significant decrease in posterior wall thickness during diastole, from 8.1 mm to 7.0 mm, and interventricular septum thickness during diastole, from 9.3 mm to 8.7 mm. The left ventricular mass index decreased significantly, from 82 mg/m2 to 73 mg/m2; and the left ventricular ejection fraction increased significantly, from 55.3% to 57.9%.
Dr. Occhipinti compared these changes to 2-year findings in a group of 11 control patients who were on a transplant waiting list or who had a failed pancreatic transplant.
In this group, there were no significant changes in HbA1c, left ventricular ejection fraction, or any of the measures of cardiac morphology.
Dr. Occhipinti said she had no relevant financial disclosures.
BERLIN -- A pancreas-only transplant improved cardiac function and morphology in a group of patients with type 1 diabetes.
After 5 years, the patients showed significantly improved posterior wall and interventricular septal thickness, as well as a significantly increased left ventricular ejection fraction, Dr. Margherita Occhipinti said at the annual meeting of the European Societies for the Study of Diabetes.
She reported 5-year follow-up data on 35 patients with type 1 diabetes who underwent the procedure. The patients were a mean of 38 years old and had a mean disease duration of 25 years. Their mean insulin requirement was 43 U/day.
Most of the transplants (74%) were performed with a portal-enteric drain technique; the remainder had systemic-enteric drainage, said Dr. Occhipinti of the University of Pisa (Italy). The majority (77%) had induction therapy with basiliximab; the rest had antithymocyte globulin (rabbit) induction. The maintenance immunosuppressant regimen was a combination of mycophenolate mofetil, tacrolimus, and steroids.
At last follow-up, fasting plasma glucose level had normalized, hemoglobin A1c level had fallen from 9% to just under 6%, and C-peptide level had increased from under 1 ng/mL to almost 3 ng/mL.
There were no significant changes in either systolic or diastolic blood pressure. However, the number of patients taking ACE inhibitors or angiotensin receptor blockers decreased from 59% to 43%. Total and LDL cholesterol levels decreased significantly, although there were no significant changes in HDL cholesterol or triglycerides.
Cardiac morphology changed significantly, Dr. Occhipinti said, including a significant decrease in posterior wall thickness during diastole, from 8.1 mm to 7.0 mm, and interventricular septum thickness during diastole, from 9.3 mm to 8.7 mm. The left ventricular mass index decreased significantly, from 82 mg/m2 to 73 mg/m2; and the left ventricular ejection fraction increased significantly, from 55.3% to 57.9%.
Dr. Occhipinti compared these changes to 2-year findings in a group of 11 control patients who were on a transplant waiting list or who had a failed pancreatic transplant.
In this group, there were no significant changes in HbA1c, left ventricular ejection fraction, or any of the measures of cardiac morphology.
Dr. Occhipinti said she had no relevant financial disclosures.
BERLIN -- A pancreas-only transplant improved cardiac function and morphology in a group of patients with type 1 diabetes.
After 5 years, the patients showed significantly improved posterior wall and interventricular septal thickness, as well as a significantly increased left ventricular ejection fraction, Dr. Margherita Occhipinti said at the annual meeting of the European Societies for the Study of Diabetes.
She reported 5-year follow-up data on 35 patients with type 1 diabetes who underwent the procedure. The patients were a mean of 38 years old and had a mean disease duration of 25 years. Their mean insulin requirement was 43 U/day.
Most of the transplants (74%) were performed with a portal-enteric drain technique; the remainder had systemic-enteric drainage, said Dr. Occhipinti of the University of Pisa (Italy). The majority (77%) had induction therapy with basiliximab; the rest had antithymocyte globulin (rabbit) induction. The maintenance immunosuppressant regimen was a combination of mycophenolate mofetil, tacrolimus, and steroids.
At last follow-up, fasting plasma glucose level had normalized, hemoglobin A1c level had fallen from 9% to just under 6%, and C-peptide level had increased from under 1 ng/mL to almost 3 ng/mL.
There were no significant changes in either systolic or diastolic blood pressure. However, the number of patients taking ACE inhibitors or angiotensin receptor blockers decreased from 59% to 43%. Total and LDL cholesterol levels decreased significantly, although there were no significant changes in HDL cholesterol or triglycerides.
Cardiac morphology changed significantly, Dr. Occhipinti said, including a significant decrease in posterior wall thickness during diastole, from 8.1 mm to 7.0 mm, and interventricular septum thickness during diastole, from 9.3 mm to 8.7 mm. The left ventricular mass index decreased significantly, from 82 mg/m2 to 73 mg/m2; and the left ventricular ejection fraction increased significantly, from 55.3% to 57.9%.
Dr. Occhipinti compared these changes to 2-year findings in a group of 11 control patients who were on a transplant waiting list or who had a failed pancreatic transplant.
In this group, there were no significant changes in HbA1c, left ventricular ejection fraction, or any of the measures of cardiac morphology.
Dr. Occhipinti said she had no relevant financial disclosures.
AT THE ANNUAL MEETING OF THE EUROPEAN SOCIETIES FOR THE STUDY OF DIABETES
Major Finding: Cardiac morphology and function improved significantly after pancreas-only transplant: Posterior wall thickness and interventricular septum thickness decreased during diastole, from 8.1 mm to 7.0 mm and from 9.3 mm to 8.7 mm, respectively; left ventricular mass index decreased from 82 mg/m2 to 73 mg/m2; and left ventricular ejection fraction increased, from 55.3% to 57.9%.
Data Source: Data are from 35 patients with longstanding type 1 diabetes.
Disclosures: Dr. Occhipinti said she had no relevant financial disclosures.
Triple Therapy Boosts HCV Response After Transplant
BOSTON – Liver transplant recipients with hepatitis C virus infection who underwent triple-drug therapy achieved a high extended rapid virologic response rate but often contended with treatment complications in a retrospective multicenter cohort study.
The extended rapid virologic response (eRVR) rate seen in 57% of patients was "encouraging, given a very difficult-to-cure population," Dr. James R. Burton, Jr., said at the annual meeting of the American Association for the Study of Liver Diseases. He noted, however, that it’s not clear if the encouraging eRVR rate will predict sustained virologic response (SVR) as it does in non-liver transplant patients.
The use of peginteferon plus ribavirin in liver transplant recipients with hepatitis C virus infection has an SVR of only 30%. While triple therapy with peginterferon, ribavirin, and a protease inhibitor (boceprevir or telaprevir) has significantly improved rates of SVR in patients infected with genotype 1 hepatitis C virus, its safety and efficacy in liver transplant recipients is unknown, said Dr. Burton, medical director of liver transplantation at the University of Colorado Hospital, Aurora.
With 101 patients, the five-center study is the largest involving triple therapy in liver transplant recipients with hepatitis C virus infection.
Telaprevir was the protease inhibitor used most often in patients (90% vs. 10% with boceprevir). Nearly all patients (96%) had a lead-in treatment phase with peginterferon plus ribavirin. A minority of patients (14%) had an extended lead-in phase of at least 90 days (median of 189 days) and were excluded from efficacy, but not safety, analyses. The other patients had a lead-in lasting a median of 29 days. The patients with a long lead-in phase had a median of 398 total treatment days, compared with a median of 154 days for those with a shorter lead-in time.
The efficacy study population involved genotype 1–infected patients (54% genotype 1a, 39% 1b, and 7% mixed) from five medical centers. Most patients were men (76%); they had a median age of 58 years and a median duration of 54 months from their liver transplant to starting a protease inhibitor. An unfavorable IL28B genotype was found in 69% of 45 patients tested. In the 60% of patients who had undergone previous antiviral therapy, 29% had a partial response. On liver biopsy, another 47% of patients had either bridging fibrosis or cirrhosis.
The immunosuppressive agents used by the patients included cyclosporine (66%) and tacrolimus (23%). A small percentage did not receive a calcineurin inhibitor or rapamycin. Another 27% were taking corticosteroids, and 72% were taking mycophenolate mofetil or mycophenolic acid.
On treatment, the percentage of patients who had an HCV RNA level less than the limit of detection increased from 55% at 4 weeks to 63% at 8 weeks. At 12 weeks the percentage was 71%. An eRVR, defined as negative HCV RNA tests at 4 and 12 weeks, occurred in 57%. An eRVR occurred significantly more often among patients who had at least a 1 log drop in HCV RNA levels during the lead-in phase than did those with less than a 1 log drop (76% vs. 35%).
Overall, 12% of patients experienced virologic breakthrough, and treatment was stopped. This occurred more often among those with a long lead-in vs. those with a short lead-in (21% vs. 10%, respectively). Another 14% discontinued treatment early because of an adverse event; discontinuations occurred more often among patients with a long lead-in (40% vs. 11%).
Protease inhibitors are known to inhibit the metabolism of calcineurin inhibitors, which was reflected in the study by the need to reduce the median daily doses of cyclosporine (from 200 mg to 50 mg) and tacrolimus (from 1.0 mg to 0.06 mg) after protease inhibitor therapy began.
Many patients (49%) required blood transfusions during triple therapy. During the first 16 weeks of therapy, these patients used a median of 2.5 units. The majority of patients (86%) used growth factors, including granulocyte-colony stimulating factor in 44% and erythropoietin in 79%. Medication dose reductions were most frequent for ribavirin (in 78%). A total of 7% were hospitalized for anemia, Dr. Burton said.
Renal insufficiency, defined as an increase in creatinine of greater than 0.5 mg/dL from baseline, developed in 32%. Of two rejection episodes in the study, one involved a patient coming off a protease inhibitor.
Dr. Burton suggested that future studies should focus on identifying predictors for nonresponse to avoid unnecessary treatment and associated toxicities such as complications of anemia and adverse events related to significant protease inhibitor–calcineurin inhibitor interactions, such as worsening renal function and graft rejection when transitioning off a protease inhibitor.
Dr. Burton disclosed that he is an investigator in a clinical trial sponsored by Vertex Pharmaceuticals, which makes telaprevir.☐
BOSTON – Liver transplant recipients with hepatitis C virus infection who underwent triple-drug therapy achieved a high extended rapid virologic response rate but often contended with treatment complications in a retrospective multicenter cohort study.
The extended rapid virologic response (eRVR) rate seen in 57% of patients was "encouraging, given a very difficult-to-cure population," Dr. James R. Burton, Jr., said at the annual meeting of the American Association for the Study of Liver Diseases. He noted, however, that it’s not clear if the encouraging eRVR rate will predict sustained virologic response (SVR) as it does in non-liver transplant patients.
The use of peginteferon plus ribavirin in liver transplant recipients with hepatitis C virus infection has an SVR of only 30%. While triple therapy with peginterferon, ribavirin, and a protease inhibitor (boceprevir or telaprevir) has significantly improved rates of SVR in patients infected with genotype 1 hepatitis C virus, its safety and efficacy in liver transplant recipients is unknown, said Dr. Burton, medical director of liver transplantation at the University of Colorado Hospital, Aurora.
With 101 patients, the five-center study is the largest involving triple therapy in liver transplant recipients with hepatitis C virus infection.
Telaprevir was the protease inhibitor used most often in patients (90% vs. 10% with boceprevir). Nearly all patients (96%) had a lead-in treatment phase with peginterferon plus ribavirin. A minority of patients (14%) had an extended lead-in phase of at least 90 days (median of 189 days) and were excluded from efficacy, but not safety, analyses. The other patients had a lead-in lasting a median of 29 days. The patients with a long lead-in phase had a median of 398 total treatment days, compared with a median of 154 days for those with a shorter lead-in time.
The efficacy study population involved genotype 1–infected patients (54% genotype 1a, 39% 1b, and 7% mixed) from five medical centers. Most patients were men (76%); they had a median age of 58 years and a median duration of 54 months from their liver transplant to starting a protease inhibitor. An unfavorable IL28B genotype was found in 69% of 45 patients tested. In the 60% of patients who had undergone previous antiviral therapy, 29% had a partial response. On liver biopsy, another 47% of patients had either bridging fibrosis or cirrhosis.
The immunosuppressive agents used by the patients included cyclosporine (66%) and tacrolimus (23%). A small percentage did not receive a calcineurin inhibitor or rapamycin. Another 27% were taking corticosteroids, and 72% were taking mycophenolate mofetil or mycophenolic acid.
On treatment, the percentage of patients who had an HCV RNA level less than the limit of detection increased from 55% at 4 weeks to 63% at 8 weeks. At 12 weeks the percentage was 71%. An eRVR, defined as negative HCV RNA tests at 4 and 12 weeks, occurred in 57%. An eRVR occurred significantly more often among patients who had at least a 1 log drop in HCV RNA levels during the lead-in phase than did those with less than a 1 log drop (76% vs. 35%).
Overall, 12% of patients experienced virologic breakthrough, and treatment was stopped. This occurred more often among those with a long lead-in vs. those with a short lead-in (21% vs. 10%, respectively). Another 14% discontinued treatment early because of an adverse event; discontinuations occurred more often among patients with a long lead-in (40% vs. 11%).
Protease inhibitors are known to inhibit the metabolism of calcineurin inhibitors, which was reflected in the study by the need to reduce the median daily doses of cyclosporine (from 200 mg to 50 mg) and tacrolimus (from 1.0 mg to 0.06 mg) after protease inhibitor therapy began.
Many patients (49%) required blood transfusions during triple therapy. During the first 16 weeks of therapy, these patients used a median of 2.5 units. The majority of patients (86%) used growth factors, including granulocyte-colony stimulating factor in 44% and erythropoietin in 79%. Medication dose reductions were most frequent for ribavirin (in 78%). A total of 7% were hospitalized for anemia, Dr. Burton said.
Renal insufficiency, defined as an increase in creatinine of greater than 0.5 mg/dL from baseline, developed in 32%. Of two rejection episodes in the study, one involved a patient coming off a protease inhibitor.
Dr. Burton suggested that future studies should focus on identifying predictors for nonresponse to avoid unnecessary treatment and associated toxicities such as complications of anemia and adverse events related to significant protease inhibitor–calcineurin inhibitor interactions, such as worsening renal function and graft rejection when transitioning off a protease inhibitor.
Dr. Burton disclosed that he is an investigator in a clinical trial sponsored by Vertex Pharmaceuticals, which makes telaprevir.☐
BOSTON – Liver transplant recipients with hepatitis C virus infection who underwent triple-drug therapy achieved a high extended rapid virologic response rate but often contended with treatment complications in a retrospective multicenter cohort study.
The extended rapid virologic response (eRVR) rate seen in 57% of patients was "encouraging, given a very difficult-to-cure population," Dr. James R. Burton, Jr., said at the annual meeting of the American Association for the Study of Liver Diseases. He noted, however, that it’s not clear if the encouraging eRVR rate will predict sustained virologic response (SVR) as it does in non-liver transplant patients.
The use of peginteferon plus ribavirin in liver transplant recipients with hepatitis C virus infection has an SVR of only 30%. While triple therapy with peginterferon, ribavirin, and a protease inhibitor (boceprevir or telaprevir) has significantly improved rates of SVR in patients infected with genotype 1 hepatitis C virus, its safety and efficacy in liver transplant recipients is unknown, said Dr. Burton, medical director of liver transplantation at the University of Colorado Hospital, Aurora.
With 101 patients, the five-center study is the largest involving triple therapy in liver transplant recipients with hepatitis C virus infection.
Telaprevir was the protease inhibitor used most often in patients (90% vs. 10% with boceprevir). Nearly all patients (96%) had a lead-in treatment phase with peginterferon plus ribavirin. A minority of patients (14%) had an extended lead-in phase of at least 90 days (median of 189 days) and were excluded from efficacy, but not safety, analyses. The other patients had a lead-in lasting a median of 29 days. The patients with a long lead-in phase had a median of 398 total treatment days, compared with a median of 154 days for those with a shorter lead-in time.
The efficacy study population involved genotype 1–infected patients (54% genotype 1a, 39% 1b, and 7% mixed) from five medical centers. Most patients were men (76%); they had a median age of 58 years and a median duration of 54 months from their liver transplant to starting a protease inhibitor. An unfavorable IL28B genotype was found in 69% of 45 patients tested. In the 60% of patients who had undergone previous antiviral therapy, 29% had a partial response. On liver biopsy, another 47% of patients had either bridging fibrosis or cirrhosis.
The immunosuppressive agents used by the patients included cyclosporine (66%) and tacrolimus (23%). A small percentage did not receive a calcineurin inhibitor or rapamycin. Another 27% were taking corticosteroids, and 72% were taking mycophenolate mofetil or mycophenolic acid.
On treatment, the percentage of patients who had an HCV RNA level less than the limit of detection increased from 55% at 4 weeks to 63% at 8 weeks. At 12 weeks the percentage was 71%. An eRVR, defined as negative HCV RNA tests at 4 and 12 weeks, occurred in 57%. An eRVR occurred significantly more often among patients who had at least a 1 log drop in HCV RNA levels during the lead-in phase than did those with less than a 1 log drop (76% vs. 35%).
Overall, 12% of patients experienced virologic breakthrough, and treatment was stopped. This occurred more often among those with a long lead-in vs. those with a short lead-in (21% vs. 10%, respectively). Another 14% discontinued treatment early because of an adverse event; discontinuations occurred more often among patients with a long lead-in (40% vs. 11%).
Protease inhibitors are known to inhibit the metabolism of calcineurin inhibitors, which was reflected in the study by the need to reduce the median daily doses of cyclosporine (from 200 mg to 50 mg) and tacrolimus (from 1.0 mg to 0.06 mg) after protease inhibitor therapy began.
Many patients (49%) required blood transfusions during triple therapy. During the first 16 weeks of therapy, these patients used a median of 2.5 units. The majority of patients (86%) used growth factors, including granulocyte-colony stimulating factor in 44% and erythropoietin in 79%. Medication dose reductions were most frequent for ribavirin (in 78%). A total of 7% were hospitalized for anemia, Dr. Burton said.
Renal insufficiency, defined as an increase in creatinine of greater than 0.5 mg/dL from baseline, developed in 32%. Of two rejection episodes in the study, one involved a patient coming off a protease inhibitor.
Dr. Burton suggested that future studies should focus on identifying predictors for nonresponse to avoid unnecessary treatment and associated toxicities such as complications of anemia and adverse events related to significant protease inhibitor–calcineurin inhibitor interactions, such as worsening renal function and graft rejection when transitioning off a protease inhibitor.
Dr. Burton disclosed that he is an investigator in a clinical trial sponsored by Vertex Pharmaceuticals, which makes telaprevir.☐
AT THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THE STUDY OF LIVER DISEASES
Major Finding: An extended rapid virologic response occurred significantly more often among patients who had at least a 1 log drop in HCV RNA levels during the lead-in phase than did those with less than a 1 log drop (76% vs. 35%)
Data Source: This was a multicenter retrospective cohort study of triple therapy for hepatitis C virus infection in 101 patients with post liver transplant.
Disclosures: Dr. Burton disclosed that he is an investigator in a clinical trial sponsored by Vertex Pharmaceuticals, which makes telaprevir.