User login
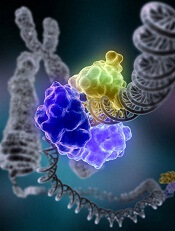
FA pathway key to DNA repair after CRISPR cutting
New research suggests the Fanconi anemia (FA) pathway plays a key role in repairing double-strand breaks (DSBs) created by CRISPR-Cas9 genome editing.
Researchers said they found that Cas9-induced single-strand template repair requires the FA pathway, and the protein FANCD2 localizes to Cas9-induced DSBs.
The team said this research provides insight into why CRISPR-Cas9 does not produce equal success in all cells.
Furthermore, the work might help researchers boost the efficiency with which cells insert new DNA into the genome and generally tweak CRISPR-Cas9 editing to get the desired outcome.
“If you want to treat sickle cell anemia, your chances of success are inextricably tied to the efficiency with which you can replace the mutated sickle cell gene with the correct one,” said study author Chris Richardson, PhD, formerly of the University of California, Berkeley, but now at Spotlight Therapeutics in Hayward, California.
“If you harvest a million cells from a patient and you have a 10% insertion rate, that is not as good as if you have 30% to 40%. Being able to manipulate those cells to increase the frequency of this process, called homology-directed repair, is exciting.”
Dr Richardson and his colleagues described this work in Nature Genetics.
CRISPR relies on DNA repair
The researchers noted that CRISPR-Cas9 creates targeted DSBs, and it’s up to the cell to repair the DNA.
This can happen in 2 ways. Enzymes can stitch the dangling ends back together, which often results in one or more bases being added or deleted, disrupting the function of the gene.
Alternatively, other enzymes can patch the break with a single strand of DNA that matches the DNA sequence upstream and downstream of the cut. A complementary DNA strand is created to complete the double-strand repair.
The former method, called non-homologous end-joining, appears to be the most common outcome after CRISPR cutting.
The latter method, homology-directed repair, happens more frequently in some cells than others and requires the presence of DNA that can be used to patch the break. Researchers often supply a single-stranded piece of DNA and hope the cell uses it to replace the faulty sequence with the new one.
Both processes are a bit mysterious, however, and no one knows why some cells readily patch in DNA while others do so infrequently.
“The enthusiasm for using CRISPR-Cas9 for medical or synthetic biology applications is great, but no one really knows what happens after you put it into cells,” Dr Richardson said. “It goes and creates these breaks, and you count on the cells to fix them, but people don’t really understand how that process works.”
To find out which DNA repair enzymes are critical to homology-directed repair after CRISPR cutting, Dr Richardson and his colleagues used a technique called CRISPR interference. They knocked out, one at a time, more than 2000 genes known or suspected to be involved in DNA repair.
The researchers were surprised to find that many of the genes that proved important—homology-directed repair dropped dramatically when they were silenced—were involved in the FA pathway.
FA pathway
The FA pathway was largely understood to repair DNA interstrand crosslinks, where a nucleotide on one strand of DNA bonds tightly with a nucleotide on the adjacent strand, interfering with DNA replication and often killing the cell.
“Based on our work, we believe that the Fanconi anemia pathway plays a major role in fixing other types of lesions as well, but is best understood as the pathway that repairs double-strand breaks,” Dr Richardson said. “After Cas9 editing, the Fanconi anemia pathway is required if you want to insert new DNA.”
The importance of the FA pathway in repairing DSBs casts doubt on some planned CRISPR treatments for Fanconi anemia itself.
Without an active FA pathway, cells may not be able to replace their mutated genes with normal genes after Cas9 makes a cut. In fact, the activity level of the FA pathway may affect how efficiently CRISPR can insert DNA in a specific cell.
The researchers concluded that, while end-joining is the default repair mechanism after a DSB, the FA pathway competes with it, and that higher activity results in more homology-directed repair and less end-joining.
Dr Richardson and his colleagues also found that 1 of the 21 proteins in the FA pathway, FANCD2, always homes in on the site of the DSB created by CRISPR-Cas9. This suggests FANCD2 plays an important role in regulating the insertion of new DNA at the cut site.
The researchers therefore believe FANCD2 could be tweaked to boost the frequency with which a cell inserts DNA via homology-directed repair.
“Also, since FANCD2 localizes to the site of Cas9 breaks, you can use FANCD2 to map where Cas9 is cutting in any cell type,” Dr Richardson said. “If you edit a population of cells and you want to know where the on- and off-target cuts are, you can just map where FANCD2 was found in the genome and you can find the cuts.”
New research suggests the Fanconi anemia (FA) pathway plays a key role in repairing double-strand breaks (DSBs) created by CRISPR-Cas9 genome editing.
Researchers said they found that Cas9-induced single-strand template repair requires the FA pathway, and the protein FANCD2 localizes to Cas9-induced DSBs.
The team said this research provides insight into why CRISPR-Cas9 does not produce equal success in all cells.
Furthermore, the work might help researchers boost the efficiency with which cells insert new DNA into the genome and generally tweak CRISPR-Cas9 editing to get the desired outcome.
“If you want to treat sickle cell anemia, your chances of success are inextricably tied to the efficiency with which you can replace the mutated sickle cell gene with the correct one,” said study author Chris Richardson, PhD, formerly of the University of California, Berkeley, but now at Spotlight Therapeutics in Hayward, California.
“If you harvest a million cells from a patient and you have a 10% insertion rate, that is not as good as if you have 30% to 40%. Being able to manipulate those cells to increase the frequency of this process, called homology-directed repair, is exciting.”
Dr Richardson and his colleagues described this work in Nature Genetics.
CRISPR relies on DNA repair
The researchers noted that CRISPR-Cas9 creates targeted DSBs, and it’s up to the cell to repair the DNA.
This can happen in 2 ways. Enzymes can stitch the dangling ends back together, which often results in one or more bases being added or deleted, disrupting the function of the gene.
Alternatively, other enzymes can patch the break with a single strand of DNA that matches the DNA sequence upstream and downstream of the cut. A complementary DNA strand is created to complete the double-strand repair.
The former method, called non-homologous end-joining, appears to be the most common outcome after CRISPR cutting.
The latter method, homology-directed repair, happens more frequently in some cells than others and requires the presence of DNA that can be used to patch the break. Researchers often supply a single-stranded piece of DNA and hope the cell uses it to replace the faulty sequence with the new one.
Both processes are a bit mysterious, however, and no one knows why some cells readily patch in DNA while others do so infrequently.
“The enthusiasm for using CRISPR-Cas9 for medical or synthetic biology applications is great, but no one really knows what happens after you put it into cells,” Dr Richardson said. “It goes and creates these breaks, and you count on the cells to fix them, but people don’t really understand how that process works.”
To find out which DNA repair enzymes are critical to homology-directed repair after CRISPR cutting, Dr Richardson and his colleagues used a technique called CRISPR interference. They knocked out, one at a time, more than 2000 genes known or suspected to be involved in DNA repair.
The researchers were surprised to find that many of the genes that proved important—homology-directed repair dropped dramatically when they were silenced—were involved in the FA pathway.
FA pathway
The FA pathway was largely understood to repair DNA interstrand crosslinks, where a nucleotide on one strand of DNA bonds tightly with a nucleotide on the adjacent strand, interfering with DNA replication and often killing the cell.
“Based on our work, we believe that the Fanconi anemia pathway plays a major role in fixing other types of lesions as well, but is best understood as the pathway that repairs double-strand breaks,” Dr Richardson said. “After Cas9 editing, the Fanconi anemia pathway is required if you want to insert new DNA.”
The importance of the FA pathway in repairing DSBs casts doubt on some planned CRISPR treatments for Fanconi anemia itself.
Without an active FA pathway, cells may not be able to replace their mutated genes with normal genes after Cas9 makes a cut. In fact, the activity level of the FA pathway may affect how efficiently CRISPR can insert DNA in a specific cell.
The researchers concluded that, while end-joining is the default repair mechanism after a DSB, the FA pathway competes with it, and that higher activity results in more homology-directed repair and less end-joining.
Dr Richardson and his colleagues also found that 1 of the 21 proteins in the FA pathway, FANCD2, always homes in on the site of the DSB created by CRISPR-Cas9. This suggests FANCD2 plays an important role in regulating the insertion of new DNA at the cut site.
The researchers therefore believe FANCD2 could be tweaked to boost the frequency with which a cell inserts DNA via homology-directed repair.
“Also, since FANCD2 localizes to the site of Cas9 breaks, you can use FANCD2 to map where Cas9 is cutting in any cell type,” Dr Richardson said. “If you edit a population of cells and you want to know where the on- and off-target cuts are, you can just map where FANCD2 was found in the genome and you can find the cuts.”
New research suggests the Fanconi anemia (FA) pathway plays a key role in repairing double-strand breaks (DSBs) created by CRISPR-Cas9 genome editing.
Researchers said they found that Cas9-induced single-strand template repair requires the FA pathway, and the protein FANCD2 localizes to Cas9-induced DSBs.
The team said this research provides insight into why CRISPR-Cas9 does not produce equal success in all cells.
Furthermore, the work might help researchers boost the efficiency with which cells insert new DNA into the genome and generally tweak CRISPR-Cas9 editing to get the desired outcome.
“If you want to treat sickle cell anemia, your chances of success are inextricably tied to the efficiency with which you can replace the mutated sickle cell gene with the correct one,” said study author Chris Richardson, PhD, formerly of the University of California, Berkeley, but now at Spotlight Therapeutics in Hayward, California.
“If you harvest a million cells from a patient and you have a 10% insertion rate, that is not as good as if you have 30% to 40%. Being able to manipulate those cells to increase the frequency of this process, called homology-directed repair, is exciting.”
Dr Richardson and his colleagues described this work in Nature Genetics.
CRISPR relies on DNA repair
The researchers noted that CRISPR-Cas9 creates targeted DSBs, and it’s up to the cell to repair the DNA.
This can happen in 2 ways. Enzymes can stitch the dangling ends back together, which often results in one or more bases being added or deleted, disrupting the function of the gene.
Alternatively, other enzymes can patch the break with a single strand of DNA that matches the DNA sequence upstream and downstream of the cut. A complementary DNA strand is created to complete the double-strand repair.
The former method, called non-homologous end-joining, appears to be the most common outcome after CRISPR cutting.
The latter method, homology-directed repair, happens more frequently in some cells than others and requires the presence of DNA that can be used to patch the break. Researchers often supply a single-stranded piece of DNA and hope the cell uses it to replace the faulty sequence with the new one.
Both processes are a bit mysterious, however, and no one knows why some cells readily patch in DNA while others do so infrequently.
“The enthusiasm for using CRISPR-Cas9 for medical or synthetic biology applications is great, but no one really knows what happens after you put it into cells,” Dr Richardson said. “It goes and creates these breaks, and you count on the cells to fix them, but people don’t really understand how that process works.”
To find out which DNA repair enzymes are critical to homology-directed repair after CRISPR cutting, Dr Richardson and his colleagues used a technique called CRISPR interference. They knocked out, one at a time, more than 2000 genes known or suspected to be involved in DNA repair.
The researchers were surprised to find that many of the genes that proved important—homology-directed repair dropped dramatically when they were silenced—were involved in the FA pathway.
FA pathway
The FA pathway was largely understood to repair DNA interstrand crosslinks, where a nucleotide on one strand of DNA bonds tightly with a nucleotide on the adjacent strand, interfering with DNA replication and often killing the cell.
“Based on our work, we believe that the Fanconi anemia pathway plays a major role in fixing other types of lesions as well, but is best understood as the pathway that repairs double-strand breaks,” Dr Richardson said. “After Cas9 editing, the Fanconi anemia pathway is required if you want to insert new DNA.”
The importance of the FA pathway in repairing DSBs casts doubt on some planned CRISPR treatments for Fanconi anemia itself.
Without an active FA pathway, cells may not be able to replace their mutated genes with normal genes after Cas9 makes a cut. In fact, the activity level of the FA pathway may affect how efficiently CRISPR can insert DNA in a specific cell.
The researchers concluded that, while end-joining is the default repair mechanism after a DSB, the FA pathway competes with it, and that higher activity results in more homology-directed repair and less end-joining.
Dr Richardson and his colleagues also found that 1 of the 21 proteins in the FA pathway, FANCD2, always homes in on the site of the DSB created by CRISPR-Cas9. This suggests FANCD2 plays an important role in regulating the insertion of new DNA at the cut site.
The researchers therefore believe FANCD2 could be tweaked to boost the frequency with which a cell inserts DNA via homology-directed repair.
“Also, since FANCD2 localizes to the site of Cas9 breaks, you can use FANCD2 to map where Cas9 is cutting in any cell type,” Dr Richardson said. “If you edit a population of cells and you want to know where the on- and off-target cuts are, you can just map where FANCD2 was found in the genome and you can find the cuts.”
Fitness trackers help monitor cancer patients
A small study suggests fitness trackers can be used to assess the quality of life and daily functioning of cancer patients during treatment.
Results indicated that objective data collected from these wearable activity monitors can supplement current assessments of health status and physical function.
This is important because current assessments are limited by their subjectivity and potential for bias, according to Gillian Gresham, PhD, of Cedars-Sinai Medical Center in Los Angeles, California.
Dr Gresham and her colleagues conducted this study and reported the results in npj Digital Medicine.
“One of the challenges in treating patients with advanced cancer is obtaining ongoing, timely, objective data about their physical status during therapy,” said study author Andrew Hendifar, MD, of Cedars-Sinai.
“After all, patients typically spend most of their time at home or work, not in a clinic, and their health statuses change from day to day.”
With this in mind, the researchers studied 37 patients undergoing treatment for advanced cancer at Cedars-Sinai.
The patients wore wrist-mounted fitness trackers throughout the study except when showering or swimming. These devices log the wearer’s step counts, stairs climbed, calories, heart rate, and sleep.
Sets of activity data were collected for 3 consecutive visits during treatment. After the final clinical visit, patients were followed for 6 months to gather additional clinical and survival outcomes.
The researchers compared data from the trackers with patients’ assessments of their own symptoms, including pain, fatigue, and sleep quality, as collected from a National Institutes of Health questionnaire.
These data sets were also compared with Eastern Cooperative Oncology Group Performance Status (ECOG-PS) and Karnofsky Performance Status (KPS) scores.
Results
Patients had a median age of 62 (range, 34-81), about 54% were male, and most (73%) had pancreatic cancer. On average, the patients walked 3700 steps (1.7 miles) per day, climbed 3 flights of stairs per day, and slept 8 hours per night.
The researchers found that activity metrics correlated with ECOG-PS and KPS scores. As scores increased, daily steps and flights of stairs decreased.
The team said the largest correlation coefficients (r) were observed between average steps and increasing ECOG-PS (r=0.63, P<0.01) and KPS (r=0.69, P<0.01) scores.
Patient-reported outcomes also correlated with activity metrics. Average steps were significantly (P<0.05 for all) associated with physical functioning (r=0.57), pain (r=—0.46), and fatigue (r=—0.53). There were significant associations for distance walked and stairs climbed as well.
Finally, the researchers observed an association between activity and grade 3/4 adverse events, hospitalizations, and survival.
An increase of 1000 steps per day, on average, was associated with significantly lower odds of hospitalization (odds ratio: 0.21, 95% CI 0.56, 0.79) and grade 3/4 adverse events (odds ratio: 0.34, 95% CI 0.13, 0.94) as well as increased survival (hazard ratio: 0.48, 95% CI 0.28, 0.83).
“Data gathered through advancements in technology has the potential to help physicians measure the impact of a particular treatment on a patient’s daily functioning,” Dr Gresham said. “Furthermore, continuous activity monitoring may help predict and monitor treatment complications and allow for more timely and appropriate interventions.”
As a next step, the researchers plan to study long-term use of activity monitors in a larger, more diverse group of advanced cancer patients and correlate that data with clinical and self-reported outcomes.
“Our hope is that findings from future studies with wearable activity monitors could lead to development of individualized treatment and exercise plans that may result in increased treatment tolerability and improved survival outcomes for patients,” Dr Hendifar said.
A small study suggests fitness trackers can be used to assess the quality of life and daily functioning of cancer patients during treatment.
Results indicated that objective data collected from these wearable activity monitors can supplement current assessments of health status and physical function.
This is important because current assessments are limited by their subjectivity and potential for bias, according to Gillian Gresham, PhD, of Cedars-Sinai Medical Center in Los Angeles, California.
Dr Gresham and her colleagues conducted this study and reported the results in npj Digital Medicine.
“One of the challenges in treating patients with advanced cancer is obtaining ongoing, timely, objective data about their physical status during therapy,” said study author Andrew Hendifar, MD, of Cedars-Sinai.
“After all, patients typically spend most of their time at home or work, not in a clinic, and their health statuses change from day to day.”
With this in mind, the researchers studied 37 patients undergoing treatment for advanced cancer at Cedars-Sinai.
The patients wore wrist-mounted fitness trackers throughout the study except when showering or swimming. These devices log the wearer’s step counts, stairs climbed, calories, heart rate, and sleep.
Sets of activity data were collected for 3 consecutive visits during treatment. After the final clinical visit, patients were followed for 6 months to gather additional clinical and survival outcomes.
The researchers compared data from the trackers with patients’ assessments of their own symptoms, including pain, fatigue, and sleep quality, as collected from a National Institutes of Health questionnaire.
These data sets were also compared with Eastern Cooperative Oncology Group Performance Status (ECOG-PS) and Karnofsky Performance Status (KPS) scores.
Results
Patients had a median age of 62 (range, 34-81), about 54% were male, and most (73%) had pancreatic cancer. On average, the patients walked 3700 steps (1.7 miles) per day, climbed 3 flights of stairs per day, and slept 8 hours per night.
The researchers found that activity metrics correlated with ECOG-PS and KPS scores. As scores increased, daily steps and flights of stairs decreased.
The team said the largest correlation coefficients (r) were observed between average steps and increasing ECOG-PS (r=0.63, P<0.01) and KPS (r=0.69, P<0.01) scores.
Patient-reported outcomes also correlated with activity metrics. Average steps were significantly (P<0.05 for all) associated with physical functioning (r=0.57), pain (r=—0.46), and fatigue (r=—0.53). There were significant associations for distance walked and stairs climbed as well.
Finally, the researchers observed an association between activity and grade 3/4 adverse events, hospitalizations, and survival.
An increase of 1000 steps per day, on average, was associated with significantly lower odds of hospitalization (odds ratio: 0.21, 95% CI 0.56, 0.79) and grade 3/4 adverse events (odds ratio: 0.34, 95% CI 0.13, 0.94) as well as increased survival (hazard ratio: 0.48, 95% CI 0.28, 0.83).
“Data gathered through advancements in technology has the potential to help physicians measure the impact of a particular treatment on a patient’s daily functioning,” Dr Gresham said. “Furthermore, continuous activity monitoring may help predict and monitor treatment complications and allow for more timely and appropriate interventions.”
As a next step, the researchers plan to study long-term use of activity monitors in a larger, more diverse group of advanced cancer patients and correlate that data with clinical and self-reported outcomes.
“Our hope is that findings from future studies with wearable activity monitors could lead to development of individualized treatment and exercise plans that may result in increased treatment tolerability and improved survival outcomes for patients,” Dr Hendifar said.
A small study suggests fitness trackers can be used to assess the quality of life and daily functioning of cancer patients during treatment.
Results indicated that objective data collected from these wearable activity monitors can supplement current assessments of health status and physical function.
This is important because current assessments are limited by their subjectivity and potential for bias, according to Gillian Gresham, PhD, of Cedars-Sinai Medical Center in Los Angeles, California.
Dr Gresham and her colleagues conducted this study and reported the results in npj Digital Medicine.
“One of the challenges in treating patients with advanced cancer is obtaining ongoing, timely, objective data about their physical status during therapy,” said study author Andrew Hendifar, MD, of Cedars-Sinai.
“After all, patients typically spend most of their time at home or work, not in a clinic, and their health statuses change from day to day.”
With this in mind, the researchers studied 37 patients undergoing treatment for advanced cancer at Cedars-Sinai.
The patients wore wrist-mounted fitness trackers throughout the study except when showering or swimming. These devices log the wearer’s step counts, stairs climbed, calories, heart rate, and sleep.
Sets of activity data were collected for 3 consecutive visits during treatment. After the final clinical visit, patients were followed for 6 months to gather additional clinical and survival outcomes.
The researchers compared data from the trackers with patients’ assessments of their own symptoms, including pain, fatigue, and sleep quality, as collected from a National Institutes of Health questionnaire.
These data sets were also compared with Eastern Cooperative Oncology Group Performance Status (ECOG-PS) and Karnofsky Performance Status (KPS) scores.
Results
Patients had a median age of 62 (range, 34-81), about 54% were male, and most (73%) had pancreatic cancer. On average, the patients walked 3700 steps (1.7 miles) per day, climbed 3 flights of stairs per day, and slept 8 hours per night.
The researchers found that activity metrics correlated with ECOG-PS and KPS scores. As scores increased, daily steps and flights of stairs decreased.
The team said the largest correlation coefficients (r) were observed between average steps and increasing ECOG-PS (r=0.63, P<0.01) and KPS (r=0.69, P<0.01) scores.
Patient-reported outcomes also correlated with activity metrics. Average steps were significantly (P<0.05 for all) associated with physical functioning (r=0.57), pain (r=—0.46), and fatigue (r=—0.53). There were significant associations for distance walked and stairs climbed as well.
Finally, the researchers observed an association between activity and grade 3/4 adverse events, hospitalizations, and survival.
An increase of 1000 steps per day, on average, was associated with significantly lower odds of hospitalization (odds ratio: 0.21, 95% CI 0.56, 0.79) and grade 3/4 adverse events (odds ratio: 0.34, 95% CI 0.13, 0.94) as well as increased survival (hazard ratio: 0.48, 95% CI 0.28, 0.83).
“Data gathered through advancements in technology has the potential to help physicians measure the impact of a particular treatment on a patient’s daily functioning,” Dr Gresham said. “Furthermore, continuous activity monitoring may help predict and monitor treatment complications and allow for more timely and appropriate interventions.”
As a next step, the researchers plan to study long-term use of activity monitors in a larger, more diverse group of advanced cancer patients and correlate that data with clinical and self-reported outcomes.
“Our hope is that findings from future studies with wearable activity monitors could lead to development of individualized treatment and exercise plans that may result in increased treatment tolerability and improved survival outcomes for patients,” Dr Hendifar said.
NIH aims to improve access to cloud computing
The National Institutes of Health (NIH) is attempting to improve biomedical researchers’ access to cloud computing.
With its new STRIDES* initiative, the NIH intends to establish partnerships with commercial cloud service providers (CSPs) to reduce economic and technological barriers to accessing and computing on large biomedical data sets.
The CSPs will work with the NIH and its funded researchers to develop and test new ways to make large data sets and associated computational tools available to wider audiences.
The NIH’s initial efforts with the STRIDES initiative will focus on making NIH high-value data sets more accessible through the cloud, leveraging partnerships with CSPs to take advantage of data-related innovations such as machine learning and artificial intelligence, and experimenting with new ways to optimize technology-intensive research.
The goals of the STRIDES initiative are to:
- Support researchers’ transition to conducting biomedical research using commercial cloud technologies through cost-effective storage and computing arrangements with CSPs
- Provide NIH researchers access to and training on new and emerging cloud-based tools and services
- Facilitate researchers’ access to and use of high-value NIH research data that are currently stored on, or will be moved into, cloud environments
- Enable the formation of an interconnected ecosystem that breaks down silos related to generating, analyzing, and sharing research data.
The NIH has already partnered with Google Cloud for the STRIDES initiative, but the agency hopes to create partnerships with other CSPs as well.
“NIH is in a unique position to bring together academic and innovation industry partners to create a biomedical data ecosystem that maximizes the use of NIH-supported biomedical research data for the greatest benefit to human health,” said NIH Principal Deputy Director Lawrence A. Tabak, DDS, PhD.
The NIH says its agreement with Google Cloud creates a cost-efficient framework for NIH researchers, as well as researchers receiving NIH support, to make use of Google Cloud’s storage, computing, and machine learning technologies.
The partnership will also enable the creation of training programs for researchers at NIH-funded institutions on how to use the Google Cloud platform. And the partnership will involve collaboration with NIH’s Data Commons Pilot—a group of projects testing new tools and methods for working with and sharing data in the cloud.
“Through our partnership with NIH, we are bringing the power of data and the cloud to the biomedical research community globally,” said Gregory Moore, MD, PhD, vice-president of healthcare at Google Cloud.
“Together, we are making it easier for scientists and physicians to access and garner insights from NIH-funded data sets with appropriate privacy protections, which will ultimately accelerate biomedical research progress toward finding treatments and cures for the most devastating diseases of our time.”
A central tenet of STRIDES is that data made available through these partnerships will incorporate standards endorsed by the biomedical research community to make data findable, accessible, interoperable, and reusable.
*Science and Technology Research Infrastructure for Discovery, Experimentation, and Sustainability
The National Institutes of Health (NIH) is attempting to improve biomedical researchers’ access to cloud computing.
With its new STRIDES* initiative, the NIH intends to establish partnerships with commercial cloud service providers (CSPs) to reduce economic and technological barriers to accessing and computing on large biomedical data sets.
The CSPs will work with the NIH and its funded researchers to develop and test new ways to make large data sets and associated computational tools available to wider audiences.
The NIH’s initial efforts with the STRIDES initiative will focus on making NIH high-value data sets more accessible through the cloud, leveraging partnerships with CSPs to take advantage of data-related innovations such as machine learning and artificial intelligence, and experimenting with new ways to optimize technology-intensive research.
The goals of the STRIDES initiative are to:
- Support researchers’ transition to conducting biomedical research using commercial cloud technologies through cost-effective storage and computing arrangements with CSPs
- Provide NIH researchers access to and training on new and emerging cloud-based tools and services
- Facilitate researchers’ access to and use of high-value NIH research data that are currently stored on, or will be moved into, cloud environments
- Enable the formation of an interconnected ecosystem that breaks down silos related to generating, analyzing, and sharing research data.
The NIH has already partnered with Google Cloud for the STRIDES initiative, but the agency hopes to create partnerships with other CSPs as well.
“NIH is in a unique position to bring together academic and innovation industry partners to create a biomedical data ecosystem that maximizes the use of NIH-supported biomedical research data for the greatest benefit to human health,” said NIH Principal Deputy Director Lawrence A. Tabak, DDS, PhD.
The NIH says its agreement with Google Cloud creates a cost-efficient framework for NIH researchers, as well as researchers receiving NIH support, to make use of Google Cloud’s storage, computing, and machine learning technologies.
The partnership will also enable the creation of training programs for researchers at NIH-funded institutions on how to use the Google Cloud platform. And the partnership will involve collaboration with NIH’s Data Commons Pilot—a group of projects testing new tools and methods for working with and sharing data in the cloud.
“Through our partnership with NIH, we are bringing the power of data and the cloud to the biomedical research community globally,” said Gregory Moore, MD, PhD, vice-president of healthcare at Google Cloud.
“Together, we are making it easier for scientists and physicians to access and garner insights from NIH-funded data sets with appropriate privacy protections, which will ultimately accelerate biomedical research progress toward finding treatments and cures for the most devastating diseases of our time.”
A central tenet of STRIDES is that data made available through these partnerships will incorporate standards endorsed by the biomedical research community to make data findable, accessible, interoperable, and reusable.
*Science and Technology Research Infrastructure for Discovery, Experimentation, and Sustainability
The National Institutes of Health (NIH) is attempting to improve biomedical researchers’ access to cloud computing.
With its new STRIDES* initiative, the NIH intends to establish partnerships with commercial cloud service providers (CSPs) to reduce economic and technological barriers to accessing and computing on large biomedical data sets.
The CSPs will work with the NIH and its funded researchers to develop and test new ways to make large data sets and associated computational tools available to wider audiences.
The NIH’s initial efforts with the STRIDES initiative will focus on making NIH high-value data sets more accessible through the cloud, leveraging partnerships with CSPs to take advantage of data-related innovations such as machine learning and artificial intelligence, and experimenting with new ways to optimize technology-intensive research.
The goals of the STRIDES initiative are to:
- Support researchers’ transition to conducting biomedical research using commercial cloud technologies through cost-effective storage and computing arrangements with CSPs
- Provide NIH researchers access to and training on new and emerging cloud-based tools and services
- Facilitate researchers’ access to and use of high-value NIH research data that are currently stored on, or will be moved into, cloud environments
- Enable the formation of an interconnected ecosystem that breaks down silos related to generating, analyzing, and sharing research data.
The NIH has already partnered with Google Cloud for the STRIDES initiative, but the agency hopes to create partnerships with other CSPs as well.
“NIH is in a unique position to bring together academic and innovation industry partners to create a biomedical data ecosystem that maximizes the use of NIH-supported biomedical research data for the greatest benefit to human health,” said NIH Principal Deputy Director Lawrence A. Tabak, DDS, PhD.
The NIH says its agreement with Google Cloud creates a cost-efficient framework for NIH researchers, as well as researchers receiving NIH support, to make use of Google Cloud’s storage, computing, and machine learning technologies.
The partnership will also enable the creation of training programs for researchers at NIH-funded institutions on how to use the Google Cloud platform. And the partnership will involve collaboration with NIH’s Data Commons Pilot—a group of projects testing new tools and methods for working with and sharing data in the cloud.
“Through our partnership with NIH, we are bringing the power of data and the cloud to the biomedical research community globally,” said Gregory Moore, MD, PhD, vice-president of healthcare at Google Cloud.
“Together, we are making it easier for scientists and physicians to access and garner insights from NIH-funded data sets with appropriate privacy protections, which will ultimately accelerate biomedical research progress toward finding treatments and cures for the most devastating diseases of our time.”
A central tenet of STRIDES is that data made available through these partnerships will incorporate standards endorsed by the biomedical research community to make data findable, accessible, interoperable, and reusable.
*Science and Technology Research Infrastructure for Discovery, Experimentation, and Sustainability
Drug approved for radical cure of P vivax malaria
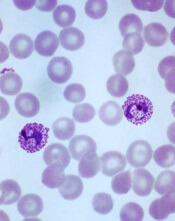
The US Food and Drug Administration (FDA) has approved tafenoquine (Krintafel) for the radical cure of Plasmodium vivax malaria.
Tafenoquine is a single-dose medicine that is now approved to prevent relapse of P vivax malaria in patients age 16 and older who are receiving appropriate antimalarial therapy for acute P vivax infection.
Tafenoquine is the first new treatment approved for P vivax malaria in more than 60 years.
Tafenoquine is an 8-aminoquinoline derivative with activity against all stages of the P vivax lifecycle, including hypnozoites. The product was first synthesized by scientists at the Walter Reed Army Institute of Research in 1978.
GSK began developing tafenoquine as a potential medicine for malaria more than 20 years ago. In 2008, GSK entered into a collaboration with Medicines for Malaria Venture to develop tafenoquine as an anti-relapse medicine for patients infected with P vivax.
The primary evidence for the clinical efficacy and safety of the 300 mg, single dose of tafenoquine was provided by a pair of phase 3 studies—DETECTIVE (NCT01376167, TAF112582) and GATHER (NCT02216123, TAF116564).
Results from these studies were presented at the 6th International Conference on Plasmodium vivax Research (ICPVR) in 2017 (abstract 63245 and abstract 63246).
DETECTIVE trial
In this double-blind, double-dummy study, researchers evaluated the efficacy, safety, and tolerability of tafenoquine. The trial included 522 patients with P vivax malaria who were randomized to receive one of the following:
- A single dose (1 day) of tafenoquine (300 mg)
- A 14-day course of primaquine (15 mg)
- Placebo.
All patients also received a 3-day course of chloroquine to treat the acute blood stage of the infection.
A significantly greater proportion of patients remained relapse-free over the 6-month follow-up period if they were treated with tafenoquine rather than placebo—60% and 26%, respectively—with an odds ratio for risk of relapse of 0.24 (P<0.001).
Likewise, a significantly greater proportion of patients were relapse-free when treated with primaquine rather than placebo—64% and 26%, respectively—with an odds ratio of 0.20 (P<0.001).
The frequency of adverse events (AEs) was 63% for the tafenoquine group, 59% for the primaquine group, and 65% for the placebo group. The frequency of serious AEs was 8%, 3%, and 5%, respectively.
GATHER trial
This study enrolled 251 patients, ages 16 and older, with microscopy-confirmed parasitemia.
Researchers compared how a single dose of tafenoquine (300 mg) and a 14-day course of primaquine (15 mg) affected hemoglobin levels in these patients. All patients also received a standard 3-day course of chloroquine.
The incidence of decline in hemoglobin (the primary endpoint) was similar between the 2 treatment groups—2.4% in the tafenoquine arm and 1.2% in the primaquine arm. The difference in proportion was 1.23% (95% CI, -4.16%, 4.98%).
None of the patients in this study required a blood transfusion.
The frequency of AEs was 72% for the tafenoquine group and 75% for the primaquine group. The frequency of serious AEs was 4% and 1%, respectively.
The US Food and Drug Administration (FDA) has approved tafenoquine (Krintafel) for the radical cure of Plasmodium vivax malaria.
Tafenoquine is a single-dose medicine that is now approved to prevent relapse of P vivax malaria in patients age 16 and older who are receiving appropriate antimalarial therapy for acute P vivax infection.
Tafenoquine is the first new treatment approved for P vivax malaria in more than 60 years.
Tafenoquine is an 8-aminoquinoline derivative with activity against all stages of the P vivax lifecycle, including hypnozoites. The product was first synthesized by scientists at the Walter Reed Army Institute of Research in 1978.
GSK began developing tafenoquine as a potential medicine for malaria more than 20 years ago. In 2008, GSK entered into a collaboration with Medicines for Malaria Venture to develop tafenoquine as an anti-relapse medicine for patients infected with P vivax.
The primary evidence for the clinical efficacy and safety of the 300 mg, single dose of tafenoquine was provided by a pair of phase 3 studies—DETECTIVE (NCT01376167, TAF112582) and GATHER (NCT02216123, TAF116564).
Results from these studies were presented at the 6th International Conference on Plasmodium vivax Research (ICPVR) in 2017 (abstract 63245 and abstract 63246).
DETECTIVE trial
In this double-blind, double-dummy study, researchers evaluated the efficacy, safety, and tolerability of tafenoquine. The trial included 522 patients with P vivax malaria who were randomized to receive one of the following:
- A single dose (1 day) of tafenoquine (300 mg)
- A 14-day course of primaquine (15 mg)
- Placebo.
All patients also received a 3-day course of chloroquine to treat the acute blood stage of the infection.
A significantly greater proportion of patients remained relapse-free over the 6-month follow-up period if they were treated with tafenoquine rather than placebo—60% and 26%, respectively—with an odds ratio for risk of relapse of 0.24 (P<0.001).
Likewise, a significantly greater proportion of patients were relapse-free when treated with primaquine rather than placebo—64% and 26%, respectively—with an odds ratio of 0.20 (P<0.001).
The frequency of adverse events (AEs) was 63% for the tafenoquine group, 59% for the primaquine group, and 65% for the placebo group. The frequency of serious AEs was 8%, 3%, and 5%, respectively.
GATHER trial
This study enrolled 251 patients, ages 16 and older, with microscopy-confirmed parasitemia.
Researchers compared how a single dose of tafenoquine (300 mg) and a 14-day course of primaquine (15 mg) affected hemoglobin levels in these patients. All patients also received a standard 3-day course of chloroquine.
The incidence of decline in hemoglobin (the primary endpoint) was similar between the 2 treatment groups—2.4% in the tafenoquine arm and 1.2% in the primaquine arm. The difference in proportion was 1.23% (95% CI, -4.16%, 4.98%).
None of the patients in this study required a blood transfusion.
The frequency of AEs was 72% for the tafenoquine group and 75% for the primaquine group. The frequency of serious AEs was 4% and 1%, respectively.
The US Food and Drug Administration (FDA) has approved tafenoquine (Krintafel) for the radical cure of Plasmodium vivax malaria.
Tafenoquine is a single-dose medicine that is now approved to prevent relapse of P vivax malaria in patients age 16 and older who are receiving appropriate antimalarial therapy for acute P vivax infection.
Tafenoquine is the first new treatment approved for P vivax malaria in more than 60 years.
Tafenoquine is an 8-aminoquinoline derivative with activity against all stages of the P vivax lifecycle, including hypnozoites. The product was first synthesized by scientists at the Walter Reed Army Institute of Research in 1978.
GSK began developing tafenoquine as a potential medicine for malaria more than 20 years ago. In 2008, GSK entered into a collaboration with Medicines for Malaria Venture to develop tafenoquine as an anti-relapse medicine for patients infected with P vivax.
The primary evidence for the clinical efficacy and safety of the 300 mg, single dose of tafenoquine was provided by a pair of phase 3 studies—DETECTIVE (NCT01376167, TAF112582) and GATHER (NCT02216123, TAF116564).
Results from these studies were presented at the 6th International Conference on Plasmodium vivax Research (ICPVR) in 2017 (abstract 63245 and abstract 63246).
DETECTIVE trial
In this double-blind, double-dummy study, researchers evaluated the efficacy, safety, and tolerability of tafenoquine. The trial included 522 patients with P vivax malaria who were randomized to receive one of the following:
- A single dose (1 day) of tafenoquine (300 mg)
- A 14-day course of primaquine (15 mg)
- Placebo.
All patients also received a 3-day course of chloroquine to treat the acute blood stage of the infection.
A significantly greater proportion of patients remained relapse-free over the 6-month follow-up period if they were treated with tafenoquine rather than placebo—60% and 26%, respectively—with an odds ratio for risk of relapse of 0.24 (P<0.001).
Likewise, a significantly greater proportion of patients were relapse-free when treated with primaquine rather than placebo—64% and 26%, respectively—with an odds ratio of 0.20 (P<0.001).
The frequency of adverse events (AEs) was 63% for the tafenoquine group, 59% for the primaquine group, and 65% for the placebo group. The frequency of serious AEs was 8%, 3%, and 5%, respectively.
GATHER trial
This study enrolled 251 patients, ages 16 and older, with microscopy-confirmed parasitemia.
Researchers compared how a single dose of tafenoquine (300 mg) and a 14-day course of primaquine (15 mg) affected hemoglobin levels in these patients. All patients also received a standard 3-day course of chloroquine.
The incidence of decline in hemoglobin (the primary endpoint) was similar between the 2 treatment groups—2.4% in the tafenoquine arm and 1.2% in the primaquine arm. The difference in proportion was 1.23% (95% CI, -4.16%, 4.98%).
None of the patients in this study required a blood transfusion.
The frequency of AEs was 72% for the tafenoquine group and 75% for the primaquine group. The frequency of serious AEs was 4% and 1%, respectively.
Breakthrough drugs approved with less stringent criteria
Clinical trials supporting the approval of drugs with breakthrough therapy designation1 do not meet the same standards as trials for non-breakthrough drugs, according to researchers.
Between 2012 and 2017, the US Food and Drug Administration (FDA) approved 46 breakthrough therapeutics on the basis of 89 pivotal trials.
Researchers found these trials “commonly lacked randomization, double-blinding, and control groups, used surrogate markers as primary endpoints, and enrolled small numbers of patients.”
Joseph S. Ross, MD, of the Yale School of Medicine in New Haven, Connecticut, and his colleagues detailed these findings in a letter to JAMA.
“To be clear, I think the FDA, as directed by Congress, is doing everything it can to expedite the development and review of drugs that treat serious and life-threatening conditions,” Dr Ross said.
“Our research suggests that FDA approval of these breakthrough therapies is generally based on shorter and smaller clinical trials than those that support FDA approval of non-breakthrough therapy drugs.”
Analyzing the approvals
More than half of the 46 approvals analyzed were for cancer therapeutics (n=25; 54.3%), and an equal number were considered first-in-class.
All 46 products received priority review2, 30 (65.2%) received orphan designation3, 24 qualified for fast track4 review (52.2%), and 18 received accelerated approval5 (39.1%).
The median time from an investigational new drug activation to final FDA approval was 4.9 years. The median time from the submission of the new drug application to FDA approval was 6.9 months.
The median number of pivotal trials per indication was 1, and the median number of patients supporting an indication was 222.
Of all the approvals, 27 (58.7%) were made based on randomized trials, 21 (45.7%) were based on double-blind allocation, and 25 (54.3%) used an active or placebo comparator. Only 10 (21.7%) used a clinical primary endpoint.
The analysis also showed that trials supporting breakthrough drugs with accelerated approval were significantly less likely to be randomized, double-blinded, or have an active/placebo control group.
Of 18 trials that were used to grant drugs accelerated approval, 3 (16.7%) trials were randomized, 1 (5.6%) was double-blinded, and 3 (16.7%) had an active/placebo control group.
Of 28 trials supporting drugs without accelerated approval, 24 (85.7%) trials were randomized, 20 (71.4%) were double-blinded, and 22 (78.6%) had an active/placebo control group.
All 18 accelerated approvals had at least 1 safety analysis or efficacy-focused postmarketing requirement.
Dr Ross pointed out that when approvals are based on shorter and smaller clinical trials, there is greater uncertainty at the time of approval.
For example, will effects observed in a small, single trial be observed in a larger population or in another independent study? Will effects observed over a short period persist over time? Will new risks (or benefits) be observed over a longer period? And will the effect observed on the outcomes used in these shorter trials—usually surrogate endpoints believed to predict a clinical benefit—be confirmed by clinical outcomes?
“If we are going to be making this trade-off to allow novel drugs to come to market on the basis of evidence that is generally accompanied by greater uncertainty, we must be committed as a clinical and scientific community to ensuring that high-quality, rigorous postmarketing trials are conducted within a reasonable period of time,” Dr Ross said.
He noted that postmarketing trials will resolve some of the uncertainty and will ensure that drugs are associated with the benefit/safety profile that is expected based on the initial clinical studies.
“This will allow clinicians and patients to make fully informed decisions about whether to use these novel treatments,” he said.
1. The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. Breakthrough designation entitles sponsors to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review. To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
2. The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
3. The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US. Orphan designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
4. The FDA’s fast track program is designed to expedite clinical development and submission of applications for drugs with the potential to treat serious or life-threatening conditions and address unmet medical needs. Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the drug’s development plan and written communications about issues such as trial design and use of biomarkers. Drugs that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Fast track drugs may also be eligible for rolling review, which allows a developer to submit individual sections of a drug’s application for review as they are ready, rather than waiting until all sections are complete.
5. The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition. Accelerated approval is based on surrogate or intermediate endpoints that are reasonably likely to predict clinical benefit. Continued approval of drugs granted accelerated approval may be contingent upon verification of clinical benefit in confirmatory trials.
Clinical trials supporting the approval of drugs with breakthrough therapy designation1 do not meet the same standards as trials for non-breakthrough drugs, according to researchers.
Between 2012 and 2017, the US Food and Drug Administration (FDA) approved 46 breakthrough therapeutics on the basis of 89 pivotal trials.
Researchers found these trials “commonly lacked randomization, double-blinding, and control groups, used surrogate markers as primary endpoints, and enrolled small numbers of patients.”
Joseph S. Ross, MD, of the Yale School of Medicine in New Haven, Connecticut, and his colleagues detailed these findings in a letter to JAMA.
“To be clear, I think the FDA, as directed by Congress, is doing everything it can to expedite the development and review of drugs that treat serious and life-threatening conditions,” Dr Ross said.
“Our research suggests that FDA approval of these breakthrough therapies is generally based on shorter and smaller clinical trials than those that support FDA approval of non-breakthrough therapy drugs.”
Analyzing the approvals
More than half of the 46 approvals analyzed were for cancer therapeutics (n=25; 54.3%), and an equal number were considered first-in-class.
All 46 products received priority review2, 30 (65.2%) received orphan designation3, 24 qualified for fast track4 review (52.2%), and 18 received accelerated approval5 (39.1%).
The median time from an investigational new drug activation to final FDA approval was 4.9 years. The median time from the submission of the new drug application to FDA approval was 6.9 months.
The median number of pivotal trials per indication was 1, and the median number of patients supporting an indication was 222.
Of all the approvals, 27 (58.7%) were made based on randomized trials, 21 (45.7%) were based on double-blind allocation, and 25 (54.3%) used an active or placebo comparator. Only 10 (21.7%) used a clinical primary endpoint.
The analysis also showed that trials supporting breakthrough drugs with accelerated approval were significantly less likely to be randomized, double-blinded, or have an active/placebo control group.
Of 18 trials that were used to grant drugs accelerated approval, 3 (16.7%) trials were randomized, 1 (5.6%) was double-blinded, and 3 (16.7%) had an active/placebo control group.
Of 28 trials supporting drugs without accelerated approval, 24 (85.7%) trials were randomized, 20 (71.4%) were double-blinded, and 22 (78.6%) had an active/placebo control group.
All 18 accelerated approvals had at least 1 safety analysis or efficacy-focused postmarketing requirement.
Dr Ross pointed out that when approvals are based on shorter and smaller clinical trials, there is greater uncertainty at the time of approval.
For example, will effects observed in a small, single trial be observed in a larger population or in another independent study? Will effects observed over a short period persist over time? Will new risks (or benefits) be observed over a longer period? And will the effect observed on the outcomes used in these shorter trials—usually surrogate endpoints believed to predict a clinical benefit—be confirmed by clinical outcomes?
“If we are going to be making this trade-off to allow novel drugs to come to market on the basis of evidence that is generally accompanied by greater uncertainty, we must be committed as a clinical and scientific community to ensuring that high-quality, rigorous postmarketing trials are conducted within a reasonable period of time,” Dr Ross said.
He noted that postmarketing trials will resolve some of the uncertainty and will ensure that drugs are associated with the benefit/safety profile that is expected based on the initial clinical studies.
“This will allow clinicians and patients to make fully informed decisions about whether to use these novel treatments,” he said.
1. The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. Breakthrough designation entitles sponsors to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review. To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
2. The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
3. The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US. Orphan designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
4. The FDA’s fast track program is designed to expedite clinical development and submission of applications for drugs with the potential to treat serious or life-threatening conditions and address unmet medical needs. Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the drug’s development plan and written communications about issues such as trial design and use of biomarkers. Drugs that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Fast track drugs may also be eligible for rolling review, which allows a developer to submit individual sections of a drug’s application for review as they are ready, rather than waiting until all sections are complete.
5. The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition. Accelerated approval is based on surrogate or intermediate endpoints that are reasonably likely to predict clinical benefit. Continued approval of drugs granted accelerated approval may be contingent upon verification of clinical benefit in confirmatory trials.
Clinical trials supporting the approval of drugs with breakthrough therapy designation1 do not meet the same standards as trials for non-breakthrough drugs, according to researchers.
Between 2012 and 2017, the US Food and Drug Administration (FDA) approved 46 breakthrough therapeutics on the basis of 89 pivotal trials.
Researchers found these trials “commonly lacked randomization, double-blinding, and control groups, used surrogate markers as primary endpoints, and enrolled small numbers of patients.”
Joseph S. Ross, MD, of the Yale School of Medicine in New Haven, Connecticut, and his colleagues detailed these findings in a letter to JAMA.
“To be clear, I think the FDA, as directed by Congress, is doing everything it can to expedite the development and review of drugs that treat serious and life-threatening conditions,” Dr Ross said.
“Our research suggests that FDA approval of these breakthrough therapies is generally based on shorter and smaller clinical trials than those that support FDA approval of non-breakthrough therapy drugs.”
Analyzing the approvals
More than half of the 46 approvals analyzed were for cancer therapeutics (n=25; 54.3%), and an equal number were considered first-in-class.
All 46 products received priority review2, 30 (65.2%) received orphan designation3, 24 qualified for fast track4 review (52.2%), and 18 received accelerated approval5 (39.1%).
The median time from an investigational new drug activation to final FDA approval was 4.9 years. The median time from the submission of the new drug application to FDA approval was 6.9 months.
The median number of pivotal trials per indication was 1, and the median number of patients supporting an indication was 222.
Of all the approvals, 27 (58.7%) were made based on randomized trials, 21 (45.7%) were based on double-blind allocation, and 25 (54.3%) used an active or placebo comparator. Only 10 (21.7%) used a clinical primary endpoint.
The analysis also showed that trials supporting breakthrough drugs with accelerated approval were significantly less likely to be randomized, double-blinded, or have an active/placebo control group.
Of 18 trials that were used to grant drugs accelerated approval, 3 (16.7%) trials were randomized, 1 (5.6%) was double-blinded, and 3 (16.7%) had an active/placebo control group.
Of 28 trials supporting drugs without accelerated approval, 24 (85.7%) trials were randomized, 20 (71.4%) were double-blinded, and 22 (78.6%) had an active/placebo control group.
All 18 accelerated approvals had at least 1 safety analysis or efficacy-focused postmarketing requirement.
Dr Ross pointed out that when approvals are based on shorter and smaller clinical trials, there is greater uncertainty at the time of approval.
For example, will effects observed in a small, single trial be observed in a larger population or in another independent study? Will effects observed over a short period persist over time? Will new risks (or benefits) be observed over a longer period? And will the effect observed on the outcomes used in these shorter trials—usually surrogate endpoints believed to predict a clinical benefit—be confirmed by clinical outcomes?
“If we are going to be making this trade-off to allow novel drugs to come to market on the basis of evidence that is generally accompanied by greater uncertainty, we must be committed as a clinical and scientific community to ensuring that high-quality, rigorous postmarketing trials are conducted within a reasonable period of time,” Dr Ross said.
He noted that postmarketing trials will resolve some of the uncertainty and will ensure that drugs are associated with the benefit/safety profile that is expected based on the initial clinical studies.
“This will allow clinicians and patients to make fully informed decisions about whether to use these novel treatments,” he said.
1. The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. Breakthrough designation entitles sponsors to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review. To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
2. The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
3. The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US. Orphan designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
4. The FDA’s fast track program is designed to expedite clinical development and submission of applications for drugs with the potential to treat serious or life-threatening conditions and address unmet medical needs. Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the drug’s development plan and written communications about issues such as trial design and use of biomarkers. Drugs that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Fast track drugs may also be eligible for rolling review, which allows a developer to submit individual sections of a drug’s application for review as they are ready, rather than waiting until all sections are complete.
5. The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition. Accelerated approval is based on surrogate or intermediate endpoints that are reasonably likely to predict clinical benefit. Continued approval of drugs granted accelerated approval may be contingent upon verification of clinical benefit in confirmatory trials.
Vaccine protects mice from malaria
An RNA replicon-based vaccine can fight malaria infection in mice, according to research published in Nature Communications.
The vaccine targets a protein, Plasmodium macrophage migration inhibitory factor (PMIF), which is produced by malaria parasites and suppresses memory T cells.
The vaccine provided improved control of existing malaria infection as well as protection from reinfection in mice.
This work was funded by National Institutes of Health grants and Novartis Vaccines, Inc.
The research began with a strain of Plasmodium berghei in which PMIF was genetically deleted. Investigators found that mice infected with this strain developed memory T cells and showed stronger anti-parasite immunity.
This led the researchers to test a vaccine targeting PMIF in 2 mouse models of malaria. One model was an early stage liver infection, and the other was a severe, late-stage blood infection.
The vaccine reduced parasitemia in both models and prolonged survival in mice with the late-stage blood infection.
The investigators then cured vaccinated mice of malaria (via treatment with chloroquine) and reinfected them.
Mice reinfected with late-stage malaria had no evidence of parasites in the blood or organs after reinfection.
The mice reinfected with liver-stage malaria had a 70% reduction in liver parasites (compared to control mice) upon reinfection, and they did not develop blood-stage infection.
“If you vaccinate with this specific protein used by the malaria parasite to evade an immune response, you can elicit protection against reinfection,” said study author Richard Bucala, MD, of Yale School of Medicine in New Haven, Connecticut.
“To our knowledge, this has never been shown using a single antigen in fulminant blood-stage infection.”
The researchers also transferred memory T cells from immunized mice to naïve mice that had never been exposed to malaria. The T-cell recipients were completely protected from malaria infection.
The investigators’ next step with this work is to develop a vaccine for humans who have never had malaria, primarily young children.
“The vaccine would be used in children so that they would already have an immune response to this particular malaria product, and when they became infected with malaria, they would have a normal T-cell response, clear the parasite, and be protected from future infection,” Dr Bucala said.
An RNA replicon-based vaccine can fight malaria infection in mice, according to research published in Nature Communications.
The vaccine targets a protein, Plasmodium macrophage migration inhibitory factor (PMIF), which is produced by malaria parasites and suppresses memory T cells.
The vaccine provided improved control of existing malaria infection as well as protection from reinfection in mice.
This work was funded by National Institutes of Health grants and Novartis Vaccines, Inc.
The research began with a strain of Plasmodium berghei in which PMIF was genetically deleted. Investigators found that mice infected with this strain developed memory T cells and showed stronger anti-parasite immunity.
This led the researchers to test a vaccine targeting PMIF in 2 mouse models of malaria. One model was an early stage liver infection, and the other was a severe, late-stage blood infection.
The vaccine reduced parasitemia in both models and prolonged survival in mice with the late-stage blood infection.
The investigators then cured vaccinated mice of malaria (via treatment with chloroquine) and reinfected them.
Mice reinfected with late-stage malaria had no evidence of parasites in the blood or organs after reinfection.
The mice reinfected with liver-stage malaria had a 70% reduction in liver parasites (compared to control mice) upon reinfection, and they did not develop blood-stage infection.
“If you vaccinate with this specific protein used by the malaria parasite to evade an immune response, you can elicit protection against reinfection,” said study author Richard Bucala, MD, of Yale School of Medicine in New Haven, Connecticut.
“To our knowledge, this has never been shown using a single antigen in fulminant blood-stage infection.”
The researchers also transferred memory T cells from immunized mice to naïve mice that had never been exposed to malaria. The T-cell recipients were completely protected from malaria infection.
The investigators’ next step with this work is to develop a vaccine for humans who have never had malaria, primarily young children.
“The vaccine would be used in children so that they would already have an immune response to this particular malaria product, and when they became infected with malaria, they would have a normal T-cell response, clear the parasite, and be protected from future infection,” Dr Bucala said.
An RNA replicon-based vaccine can fight malaria infection in mice, according to research published in Nature Communications.
The vaccine targets a protein, Plasmodium macrophage migration inhibitory factor (PMIF), which is produced by malaria parasites and suppresses memory T cells.
The vaccine provided improved control of existing malaria infection as well as protection from reinfection in mice.
This work was funded by National Institutes of Health grants and Novartis Vaccines, Inc.
The research began with a strain of Plasmodium berghei in which PMIF was genetically deleted. Investigators found that mice infected with this strain developed memory T cells and showed stronger anti-parasite immunity.
This led the researchers to test a vaccine targeting PMIF in 2 mouse models of malaria. One model was an early stage liver infection, and the other was a severe, late-stage blood infection.
The vaccine reduced parasitemia in both models and prolonged survival in mice with the late-stage blood infection.
The investigators then cured vaccinated mice of malaria (via treatment with chloroquine) and reinfected them.
Mice reinfected with late-stage malaria had no evidence of parasites in the blood or organs after reinfection.
The mice reinfected with liver-stage malaria had a 70% reduction in liver parasites (compared to control mice) upon reinfection, and they did not develop blood-stage infection.
“If you vaccinate with this specific protein used by the malaria parasite to evade an immune response, you can elicit protection against reinfection,” said study author Richard Bucala, MD, of Yale School of Medicine in New Haven, Connecticut.
“To our knowledge, this has never been shown using a single antigen in fulminant blood-stage infection.”
The researchers also transferred memory T cells from immunized mice to naïve mice that had never been exposed to malaria. The T-cell recipients were completely protected from malaria infection.
The investigators’ next step with this work is to develop a vaccine for humans who have never had malaria, primarily young children.
“The vaccine would be used in children so that they would already have an immune response to this particular malaria product, and when they became infected with malaria, they would have a normal T-cell response, clear the parasite, and be protected from future infection,” Dr Bucala said.
FDA releases guidance docs on gene therapy
The US Food and Drug Administration (FDA) has released several draft guidance documents on gene therapy.
Three are disease-specific guidances—for hemophilia, rare diseases, and retinal disorders—and 3 are guidances on manufacturing gene therapies.
These 6 documents are intended to serve as the building blocks of a modern, comprehensive framework for advancing the field of gene therapy, according to FDA Commissioner Scott Gottlieb, MD.
He said the documents are being issued in draft form so the FDA can solicit public input on these new policies. As with all draft guidances, all comments received will be considered before the FDA finalizes the documents.
Disease-specific guidances
The Human Gene Therapy for Rare Diseases Draft Guidance and the Human Gene Therapy for Retinal Disorders Draft Guidance include considerations for product development, preclinical research, clinical trials, expedited programs, and communication with the FDA.
The Human Gene Therapy for Hemophilia Draft Guidance covers the same topics but also includes considerations for measuring factor VIII and factor IX activity.
The draft guidance for rare diseases encompasses diseases affecting fewer than 200,000 people in the US.
Manufacturing guidances
The 3 remaining draft guidances are actually updates to existing guidances that address manufacturing issues related to gene therapy.
The first updated draft guidance, Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs), provides sponsors with recommendations on how to provide sufficient CMC information to ensure safety, identity, quality, purity, and strength/potency of investigational gene therapy products. This guidance applies to gene therapies alone and products that contain a gene therapy in combination with a drug or device.
The second draft guidance, Testing of Retroviral Vector-Based Gene Therapy Products for Replication Competent Retrovirus (RCR) during Product Manufacture and Patient Follow-up, provides recommendations regarding the proper testing for RCR during the manufacture of retroviral vector-based gene therapy products, as well as during the follow-up monitoring of patients who have received retroviral vector-based gene therapy products.
The third draft guidance, Long Term Follow-Up (LTFU) After Administration of Human Gene Therapy Products, provides recommendations regarding the design of LTFU observational studies for the collection of data on delayed adverse events after gene therapy.
Once finalized, these draft guidances will replace previous guidances issued by the FDA in April 2008 (CMC) and November 2006 (RCR and LTFU).
The US Food and Drug Administration (FDA) has released several draft guidance documents on gene therapy.
Three are disease-specific guidances—for hemophilia, rare diseases, and retinal disorders—and 3 are guidances on manufacturing gene therapies.
These 6 documents are intended to serve as the building blocks of a modern, comprehensive framework for advancing the field of gene therapy, according to FDA Commissioner Scott Gottlieb, MD.
He said the documents are being issued in draft form so the FDA can solicit public input on these new policies. As with all draft guidances, all comments received will be considered before the FDA finalizes the documents.
Disease-specific guidances
The Human Gene Therapy for Rare Diseases Draft Guidance and the Human Gene Therapy for Retinal Disorders Draft Guidance include considerations for product development, preclinical research, clinical trials, expedited programs, and communication with the FDA.
The Human Gene Therapy for Hemophilia Draft Guidance covers the same topics but also includes considerations for measuring factor VIII and factor IX activity.
The draft guidance for rare diseases encompasses diseases affecting fewer than 200,000 people in the US.
Manufacturing guidances
The 3 remaining draft guidances are actually updates to existing guidances that address manufacturing issues related to gene therapy.
The first updated draft guidance, Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs), provides sponsors with recommendations on how to provide sufficient CMC information to ensure safety, identity, quality, purity, and strength/potency of investigational gene therapy products. This guidance applies to gene therapies alone and products that contain a gene therapy in combination with a drug or device.
The second draft guidance, Testing of Retroviral Vector-Based Gene Therapy Products for Replication Competent Retrovirus (RCR) during Product Manufacture and Patient Follow-up, provides recommendations regarding the proper testing for RCR during the manufacture of retroviral vector-based gene therapy products, as well as during the follow-up monitoring of patients who have received retroviral vector-based gene therapy products.
The third draft guidance, Long Term Follow-Up (LTFU) After Administration of Human Gene Therapy Products, provides recommendations regarding the design of LTFU observational studies for the collection of data on delayed adverse events after gene therapy.
Once finalized, these draft guidances will replace previous guidances issued by the FDA in April 2008 (CMC) and November 2006 (RCR and LTFU).
The US Food and Drug Administration (FDA) has released several draft guidance documents on gene therapy.
Three are disease-specific guidances—for hemophilia, rare diseases, and retinal disorders—and 3 are guidances on manufacturing gene therapies.
These 6 documents are intended to serve as the building blocks of a modern, comprehensive framework for advancing the field of gene therapy, according to FDA Commissioner Scott Gottlieb, MD.
He said the documents are being issued in draft form so the FDA can solicit public input on these new policies. As with all draft guidances, all comments received will be considered before the FDA finalizes the documents.
Disease-specific guidances
The Human Gene Therapy for Rare Diseases Draft Guidance and the Human Gene Therapy for Retinal Disorders Draft Guidance include considerations for product development, preclinical research, clinical trials, expedited programs, and communication with the FDA.
The Human Gene Therapy for Hemophilia Draft Guidance covers the same topics but also includes considerations for measuring factor VIII and factor IX activity.
The draft guidance for rare diseases encompasses diseases affecting fewer than 200,000 people in the US.
Manufacturing guidances
The 3 remaining draft guidances are actually updates to existing guidances that address manufacturing issues related to gene therapy.
The first updated draft guidance, Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs), provides sponsors with recommendations on how to provide sufficient CMC information to ensure safety, identity, quality, purity, and strength/potency of investigational gene therapy products. This guidance applies to gene therapies alone and products that contain a gene therapy in combination with a drug or device.
The second draft guidance, Testing of Retroviral Vector-Based Gene Therapy Products for Replication Competent Retrovirus (RCR) during Product Manufacture and Patient Follow-up, provides recommendations regarding the proper testing for RCR during the manufacture of retroviral vector-based gene therapy products, as well as during the follow-up monitoring of patients who have received retroviral vector-based gene therapy products.
The third draft guidance, Long Term Follow-Up (LTFU) After Administration of Human Gene Therapy Products, provides recommendations regarding the design of LTFU observational studies for the collection of data on delayed adverse events after gene therapy.
Once finalized, these draft guidances will replace previous guidances issued by the FDA in April 2008 (CMC) and November 2006 (RCR and LTFU).
Conflicts of interest among FDA advisers
An investigative report has unearthed potential conflicts of interest among physicians who serve on advisory panels for the US Food and Drug Administration (FDA).
The investigation revealed that some FDA advisers are receiving significant post-hoc payments from the makers of drugs they reviewed.
The investigation also uncovered relationships between advisers and drug companies that predate drug reviews.
Journalist Charles Piller and his colleagues conducted this investigation and detailed the results in Science.
The report includes data—from the federal Open Payments website—on 107 physicians who voted on FDA advisory committees between 2013 and 2016.
Forty of these advisers received more than $10,000 in post-hoc earnings or research support from the makers of drugs they reviewed or from competing drug companies.
Twenty-six advisers received more than $100,000, and 7 advisers received more than $1 million.
The 17 top earners received more than $300,000 each. For these advisers, 94% of their earnings came from the makers of drugs they previously reviewed or from those companies’ competitors.
The data also show that some advisers received funds from drug companies concurrent with or in the year before their advisory service.
Of the 17 top-earning advisers, 11 received financial support from competing companies on one or more of the drugs they reviewed. Five advisers also received support from the makers of one or more of the drugs reviewed.
The FDA did not disclose this information to the public or issue waivers for these potential conflicts. The FDA can issue a waiver to allow the participation of an adviser with an active conflict or one that ended in the year before a vote, as long as the adviser in question can provide expertise that cannot be provided by someone else.
It is possible that the FDA dismissed the aforementioned financial ties that predated drug reviews, deciding these relationships were not conflicts and did not require a waiver. However, it is also possible that the FDA did not know about these potential conflicts.
Piller and his colleagues were unable to determine what the FDA knew, as the agency refused to release disclosure documents, discuss individual advisers, or explain what steps, if any, the FDA takes to validate advisers’ disclosures.
An investigative report has unearthed potential conflicts of interest among physicians who serve on advisory panels for the US Food and Drug Administration (FDA).
The investigation revealed that some FDA advisers are receiving significant post-hoc payments from the makers of drugs they reviewed.
The investigation also uncovered relationships between advisers and drug companies that predate drug reviews.
Journalist Charles Piller and his colleagues conducted this investigation and detailed the results in Science.
The report includes data—from the federal Open Payments website—on 107 physicians who voted on FDA advisory committees between 2013 and 2016.
Forty of these advisers received more than $10,000 in post-hoc earnings or research support from the makers of drugs they reviewed or from competing drug companies.
Twenty-six advisers received more than $100,000, and 7 advisers received more than $1 million.
The 17 top earners received more than $300,000 each. For these advisers, 94% of their earnings came from the makers of drugs they previously reviewed or from those companies’ competitors.
The data also show that some advisers received funds from drug companies concurrent with or in the year before their advisory service.
Of the 17 top-earning advisers, 11 received financial support from competing companies on one or more of the drugs they reviewed. Five advisers also received support from the makers of one or more of the drugs reviewed.
The FDA did not disclose this information to the public or issue waivers for these potential conflicts. The FDA can issue a waiver to allow the participation of an adviser with an active conflict or one that ended in the year before a vote, as long as the adviser in question can provide expertise that cannot be provided by someone else.
It is possible that the FDA dismissed the aforementioned financial ties that predated drug reviews, deciding these relationships were not conflicts and did not require a waiver. However, it is also possible that the FDA did not know about these potential conflicts.
Piller and his colleagues were unable to determine what the FDA knew, as the agency refused to release disclosure documents, discuss individual advisers, or explain what steps, if any, the FDA takes to validate advisers’ disclosures.
An investigative report has unearthed potential conflicts of interest among physicians who serve on advisory panels for the US Food and Drug Administration (FDA).
The investigation revealed that some FDA advisers are receiving significant post-hoc payments from the makers of drugs they reviewed.
The investigation also uncovered relationships between advisers and drug companies that predate drug reviews.
Journalist Charles Piller and his colleagues conducted this investigation and detailed the results in Science.
The report includes data—from the federal Open Payments website—on 107 physicians who voted on FDA advisory committees between 2013 and 2016.
Forty of these advisers received more than $10,000 in post-hoc earnings or research support from the makers of drugs they reviewed or from competing drug companies.
Twenty-six advisers received more than $100,000, and 7 advisers received more than $1 million.
The 17 top earners received more than $300,000 each. For these advisers, 94% of their earnings came from the makers of drugs they previously reviewed or from those companies’ competitors.
The data also show that some advisers received funds from drug companies concurrent with or in the year before their advisory service.
Of the 17 top-earning advisers, 11 received financial support from competing companies on one or more of the drugs they reviewed. Five advisers also received support from the makers of one or more of the drugs reviewed.
The FDA did not disclose this information to the public or issue waivers for these potential conflicts. The FDA can issue a waiver to allow the participation of an adviser with an active conflict or one that ended in the year before a vote, as long as the adviser in question can provide expertise that cannot be provided by someone else.
It is possible that the FDA dismissed the aforementioned financial ties that predated drug reviews, deciding these relationships were not conflicts and did not require a waiver. However, it is also possible that the FDA did not know about these potential conflicts.
Piller and his colleagues were unable to determine what the FDA knew, as the agency refused to release disclosure documents, discuss individual advisers, or explain what steps, if any, the FDA takes to validate advisers’ disclosures.
Many CCSs not concerned about future health
A survey of more than 15,000 childhood cancer survivors (CCSs) revealed that many were unconcerned about their risk of health problems.
Thirty-one percent of CCSs said they were “not at all” or “not very” concerned about their future health, and 40% said they were “not at all” or “not very” concerned about developing new cancers.
Researchers say it isn’t clear what’s driving this lack of concern, but it is possible that some CCSs don’t know they have an increased risk of new malignancies and other health problems.
“Other possibilities include that some survivors may actually be aware of their increased risks and choose not to be concerned, or it may even be that some survivors are, indeed, following health guidelines and working with healthcare providers, leading to their lack of concern,” said Todd Gibson, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Gibson and his colleagues conducted this research and reported the results in Cancer.
The researchers analyzed data on 15,620 CCSs and 3991 of their siblings who did not have a history of cancer. The data came from questionnaires administered to participants in the Childhood Cancer Survivor Study.
At baseline, the median time from CCSs’ cancer diagnosis was 17 years (interquartile range [IQR], 14-21). Their median age at baseline was 26 (IQR, 22-31 years), and the siblings’ median age was 29 (IQR, 24-35).
When respondents were asked about their level of concern regarding their future health, the answers were as follows:
- 12% of both CCSs and siblings were “not at all concerned”
- 18.7% of CCSs and 21.6% of siblings were “not very concerned”
- 23.2% of CCSs and 24.1% of siblings were “concerned”
- 21.4% of CCSs and 22.2% of siblings were “somewhat concerned”
- 24.8% of CCSs and 20.1% of siblings were “very concerned.”
When respondents were asked to rate their level of concern about developing a new cancer, the answers were as follows:
- 17.2% of CCSs and 16.3% of siblings were “not at all concerned”
- 22.8% of CCSs and 22.2% of siblings were “not very concerned”
- 21.1% of CCSs and 25.1% of siblings were “concerned”
- 18.3% of CCSs and 18.4% of siblings were “somewhat concerned”
- 20.6% of CCSs and 18.1% of siblings were “very concerned.”
When the researchers adjusted for age, sex, race/ethnicity, education, and decade of diagnosis, CCSs were only slightly more likely than siblings to report concern about future health (relative risk, 1.12) or subsequent cancer (relative risk, 1.02).
“That similarity [between CCS and sibling answers] was really the major surprise in our findings,” Dr Gibson said. “Despite the fact that survivors have such a greatly increased risk of both second cancers and other health problems, their perception of risk was not always commensurate with their actual risk.”
The researchers did find that CCSs were more likely to report concern about future health or developing cancer if they were female, non-Hispanic black or Hispanic, older, identified as having clinical anxiety, or had already experienced a grade 3/4 chronic condition or subsequent cancer.
However, it isn’t clear why some CCSs are concerned about their future health and others are not.
“At this point, we can only speculate, but the most obvious reason [for lack of concern] would be that survivors may not fully understand their risks,” Dr Gibson said. “We do know from prior studies that not all survivors are fully aware of the specific treatments they received and how those might increase their risks of late effects.”
“If, however, survivors are aware but not motivated or sufficiently aroused to be concerned, then more motivational education will have to be developed. In any case, these findings offer a teaching point that we can use to emphasize to all survivors that they need to understand their risks.”
A survey of more than 15,000 childhood cancer survivors (CCSs) revealed that many were unconcerned about their risk of health problems.
Thirty-one percent of CCSs said they were “not at all” or “not very” concerned about their future health, and 40% said they were “not at all” or “not very” concerned about developing new cancers.
Researchers say it isn’t clear what’s driving this lack of concern, but it is possible that some CCSs don’t know they have an increased risk of new malignancies and other health problems.
“Other possibilities include that some survivors may actually be aware of their increased risks and choose not to be concerned, or it may even be that some survivors are, indeed, following health guidelines and working with healthcare providers, leading to their lack of concern,” said Todd Gibson, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Gibson and his colleagues conducted this research and reported the results in Cancer.
The researchers analyzed data on 15,620 CCSs and 3991 of their siblings who did not have a history of cancer. The data came from questionnaires administered to participants in the Childhood Cancer Survivor Study.
At baseline, the median time from CCSs’ cancer diagnosis was 17 years (interquartile range [IQR], 14-21). Their median age at baseline was 26 (IQR, 22-31 years), and the siblings’ median age was 29 (IQR, 24-35).
When respondents were asked about their level of concern regarding their future health, the answers were as follows:
- 12% of both CCSs and siblings were “not at all concerned”
- 18.7% of CCSs and 21.6% of siblings were “not very concerned”
- 23.2% of CCSs and 24.1% of siblings were “concerned”
- 21.4% of CCSs and 22.2% of siblings were “somewhat concerned”
- 24.8% of CCSs and 20.1% of siblings were “very concerned.”
When respondents were asked to rate their level of concern about developing a new cancer, the answers were as follows:
- 17.2% of CCSs and 16.3% of siblings were “not at all concerned”
- 22.8% of CCSs and 22.2% of siblings were “not very concerned”
- 21.1% of CCSs and 25.1% of siblings were “concerned”
- 18.3% of CCSs and 18.4% of siblings were “somewhat concerned”
- 20.6% of CCSs and 18.1% of siblings were “very concerned.”
When the researchers adjusted for age, sex, race/ethnicity, education, and decade of diagnosis, CCSs were only slightly more likely than siblings to report concern about future health (relative risk, 1.12) or subsequent cancer (relative risk, 1.02).
“That similarity [between CCS and sibling answers] was really the major surprise in our findings,” Dr Gibson said. “Despite the fact that survivors have such a greatly increased risk of both second cancers and other health problems, their perception of risk was not always commensurate with their actual risk.”
The researchers did find that CCSs were more likely to report concern about future health or developing cancer if they were female, non-Hispanic black or Hispanic, older, identified as having clinical anxiety, or had already experienced a grade 3/4 chronic condition or subsequent cancer.
However, it isn’t clear why some CCSs are concerned about their future health and others are not.
“At this point, we can only speculate, but the most obvious reason [for lack of concern] would be that survivors may not fully understand their risks,” Dr Gibson said. “We do know from prior studies that not all survivors are fully aware of the specific treatments they received and how those might increase their risks of late effects.”
“If, however, survivors are aware but not motivated or sufficiently aroused to be concerned, then more motivational education will have to be developed. In any case, these findings offer a teaching point that we can use to emphasize to all survivors that they need to understand their risks.”
A survey of more than 15,000 childhood cancer survivors (CCSs) revealed that many were unconcerned about their risk of health problems.
Thirty-one percent of CCSs said they were “not at all” or “not very” concerned about their future health, and 40% said they were “not at all” or “not very” concerned about developing new cancers.
Researchers say it isn’t clear what’s driving this lack of concern, but it is possible that some CCSs don’t know they have an increased risk of new malignancies and other health problems.
“Other possibilities include that some survivors may actually be aware of their increased risks and choose not to be concerned, or it may even be that some survivors are, indeed, following health guidelines and working with healthcare providers, leading to their lack of concern,” said Todd Gibson, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Gibson and his colleagues conducted this research and reported the results in Cancer.
The researchers analyzed data on 15,620 CCSs and 3991 of their siblings who did not have a history of cancer. The data came from questionnaires administered to participants in the Childhood Cancer Survivor Study.
At baseline, the median time from CCSs’ cancer diagnosis was 17 years (interquartile range [IQR], 14-21). Their median age at baseline was 26 (IQR, 22-31 years), and the siblings’ median age was 29 (IQR, 24-35).
When respondents were asked about their level of concern regarding their future health, the answers were as follows:
- 12% of both CCSs and siblings were “not at all concerned”
- 18.7% of CCSs and 21.6% of siblings were “not very concerned”
- 23.2% of CCSs and 24.1% of siblings were “concerned”
- 21.4% of CCSs and 22.2% of siblings were “somewhat concerned”
- 24.8% of CCSs and 20.1% of siblings were “very concerned.”
When respondents were asked to rate their level of concern about developing a new cancer, the answers were as follows:
- 17.2% of CCSs and 16.3% of siblings were “not at all concerned”
- 22.8% of CCSs and 22.2% of siblings were “not very concerned”
- 21.1% of CCSs and 25.1% of siblings were “concerned”
- 18.3% of CCSs and 18.4% of siblings were “somewhat concerned”
- 20.6% of CCSs and 18.1% of siblings were “very concerned.”
When the researchers adjusted for age, sex, race/ethnicity, education, and decade of diagnosis, CCSs were only slightly more likely than siblings to report concern about future health (relative risk, 1.12) or subsequent cancer (relative risk, 1.02).
“That similarity [between CCS and sibling answers] was really the major surprise in our findings,” Dr Gibson said. “Despite the fact that survivors have such a greatly increased risk of both second cancers and other health problems, their perception of risk was not always commensurate with their actual risk.”
The researchers did find that CCSs were more likely to report concern about future health or developing cancer if they were female, non-Hispanic black or Hispanic, older, identified as having clinical anxiety, or had already experienced a grade 3/4 chronic condition or subsequent cancer.
However, it isn’t clear why some CCSs are concerned about their future health and others are not.
“At this point, we can only speculate, but the most obvious reason [for lack of concern] would be that survivors may not fully understand their risks,” Dr Gibson said. “We do know from prior studies that not all survivors are fully aware of the specific treatments they received and how those might increase their risks of late effects.”
“If, however, survivors are aware but not motivated or sufficiently aroused to be concerned, then more motivational education will have to be developed. In any case, these findings offer a teaching point that we can use to emphasize to all survivors that they need to understand their risks.”
Drug makers may be blocking generic competition
The US Food and Drug Administration (FDA) has released a list of companies that “may be pursuing gaming tactics to delay generic competition.”
FDA Commissioner Scott Gottlieb, MD, said the agency is taking steps to improve access to drugs and make them more affordable.
One of these steps is trying to prevent companies that market brand-name drugs from delaying the release of generic equivalents.
Dr Gottlieb explained that brand companies may create obstacles for generic developers to purchase samples of a brand-name drug.
“In general, generic drug developers need the samples of the brand drug to develop their generic product and/or to conduct testing to show that their product is bioequivalent to the brand drug for FDA approval,” he said.
“Without these samples, generic drug makers may not be able to develop generic alternatives. Yet the FDA has heard that some brand companies will adopt tactics to make it hard for the generic companies to purchase these brand drugs at a fair value and in the open marketplace.”
One such tactic is for brand companies to place restrictions in their commercial contracts or agreements with prescription drug distributors, wholesalers, or specialty pharmacies that limit their ability to sell samples to generic drug developers.
In other cases, brand companies may be preventing generic drug developers from accessing samples due to limited distribution programs required by a Risk Evaluation and Mitigation Strategy (REMS) with Elements to Assure Safe Use (ETASU).
“But I want to be very clear: a path to securing samples of brand drugs for the purpose of generic drug development should always be available,” Dr Gottlieb said. “Even in the case of limited distribution programs, such as those required by certain REMS, there should be a path forward for generic drug development.”
With this in mind, the FDA has released a list of brand companies that may have prevented generic drug developers from accessing samples. The list contains 52 brand-name drugs, including Pomalyst, Promacta, Revlimid, Tasigna, and Thalidomid.
Generic drug developers have reported trouble obtaining samples of these drugs and asked the FDA for assistance.
When the FDA receives such a request, the agency first determines whether the product in question has a REMS program with ETASU that may impact distribution.
If the FDA confirms the existence of such a program, the generic company can submit its bioequivalence testing protocol to the FDA. The agency then evaluates this protocol to ensure the plan for testing the product contains safety protections comparable to the brand product’s REMS program.
If a generic developer’s plans include appropriate protections, the developer can request that the FDA send a Safety Determination Letter to the brand company. This letter notes that the REMS program doesn’t prevent the brand company from selling its product to generic drug developers.
The FDA has issued 21 Safety Determination Letters to date, according to Dr Gottlieb.
If a generic drug developer has trouble obtaining samples of a drug for which there is no REMS program with ETASU, the FDA informs the developer that there are no FDA-required restrictions that would prevent it from obtaining samples.
The FDA also notifies the Federal Trade Commission (FTC) of requests from generic drug developers seeking assistance in obtaining samples from brand companies. And the FDA encourages generic drug developers to raise these cases with the FTC if they believe that anticompetitive conduct has taken place.
The US Food and Drug Administration (FDA) has released a list of companies that “may be pursuing gaming tactics to delay generic competition.”
FDA Commissioner Scott Gottlieb, MD, said the agency is taking steps to improve access to drugs and make them more affordable.
One of these steps is trying to prevent companies that market brand-name drugs from delaying the release of generic equivalents.
Dr Gottlieb explained that brand companies may create obstacles for generic developers to purchase samples of a brand-name drug.
“In general, generic drug developers need the samples of the brand drug to develop their generic product and/or to conduct testing to show that their product is bioequivalent to the brand drug for FDA approval,” he said.
“Without these samples, generic drug makers may not be able to develop generic alternatives. Yet the FDA has heard that some brand companies will adopt tactics to make it hard for the generic companies to purchase these brand drugs at a fair value and in the open marketplace.”
One such tactic is for brand companies to place restrictions in their commercial contracts or agreements with prescription drug distributors, wholesalers, or specialty pharmacies that limit their ability to sell samples to generic drug developers.
In other cases, brand companies may be preventing generic drug developers from accessing samples due to limited distribution programs required by a Risk Evaluation and Mitigation Strategy (REMS) with Elements to Assure Safe Use (ETASU).
“But I want to be very clear: a path to securing samples of brand drugs for the purpose of generic drug development should always be available,” Dr Gottlieb said. “Even in the case of limited distribution programs, such as those required by certain REMS, there should be a path forward for generic drug development.”
With this in mind, the FDA has released a list of brand companies that may have prevented generic drug developers from accessing samples. The list contains 52 brand-name drugs, including Pomalyst, Promacta, Revlimid, Tasigna, and Thalidomid.
Generic drug developers have reported trouble obtaining samples of these drugs and asked the FDA for assistance.
When the FDA receives such a request, the agency first determines whether the product in question has a REMS program with ETASU that may impact distribution.
If the FDA confirms the existence of such a program, the generic company can submit its bioequivalence testing protocol to the FDA. The agency then evaluates this protocol to ensure the plan for testing the product contains safety protections comparable to the brand product’s REMS program.
If a generic developer’s plans include appropriate protections, the developer can request that the FDA send a Safety Determination Letter to the brand company. This letter notes that the REMS program doesn’t prevent the brand company from selling its product to generic drug developers.
The FDA has issued 21 Safety Determination Letters to date, according to Dr Gottlieb.
If a generic drug developer has trouble obtaining samples of a drug for which there is no REMS program with ETASU, the FDA informs the developer that there are no FDA-required restrictions that would prevent it from obtaining samples.
The FDA also notifies the Federal Trade Commission (FTC) of requests from generic drug developers seeking assistance in obtaining samples from brand companies. And the FDA encourages generic drug developers to raise these cases with the FTC if they believe that anticompetitive conduct has taken place.
The US Food and Drug Administration (FDA) has released a list of companies that “may be pursuing gaming tactics to delay generic competition.”
FDA Commissioner Scott Gottlieb, MD, said the agency is taking steps to improve access to drugs and make them more affordable.
One of these steps is trying to prevent companies that market brand-name drugs from delaying the release of generic equivalents.
Dr Gottlieb explained that brand companies may create obstacles for generic developers to purchase samples of a brand-name drug.
“In general, generic drug developers need the samples of the brand drug to develop their generic product and/or to conduct testing to show that their product is bioequivalent to the brand drug for FDA approval,” he said.
“Without these samples, generic drug makers may not be able to develop generic alternatives. Yet the FDA has heard that some brand companies will adopt tactics to make it hard for the generic companies to purchase these brand drugs at a fair value and in the open marketplace.”
One such tactic is for brand companies to place restrictions in their commercial contracts or agreements with prescription drug distributors, wholesalers, or specialty pharmacies that limit their ability to sell samples to generic drug developers.
In other cases, brand companies may be preventing generic drug developers from accessing samples due to limited distribution programs required by a Risk Evaluation and Mitigation Strategy (REMS) with Elements to Assure Safe Use (ETASU).
“But I want to be very clear: a path to securing samples of brand drugs for the purpose of generic drug development should always be available,” Dr Gottlieb said. “Even in the case of limited distribution programs, such as those required by certain REMS, there should be a path forward for generic drug development.”
With this in mind, the FDA has released a list of brand companies that may have prevented generic drug developers from accessing samples. The list contains 52 brand-name drugs, including Pomalyst, Promacta, Revlimid, Tasigna, and Thalidomid.
Generic drug developers have reported trouble obtaining samples of these drugs and asked the FDA for assistance.
When the FDA receives such a request, the agency first determines whether the product in question has a REMS program with ETASU that may impact distribution.
If the FDA confirms the existence of such a program, the generic company can submit its bioequivalence testing protocol to the FDA. The agency then evaluates this protocol to ensure the plan for testing the product contains safety protections comparable to the brand product’s REMS program.
If a generic developer’s plans include appropriate protections, the developer can request that the FDA send a Safety Determination Letter to the brand company. This letter notes that the REMS program doesn’t prevent the brand company from selling its product to generic drug developers.
The FDA has issued 21 Safety Determination Letters to date, according to Dr Gottlieb.
If a generic drug developer has trouble obtaining samples of a drug for which there is no REMS program with ETASU, the FDA informs the developer that there are no FDA-required restrictions that would prevent it from obtaining samples.
The FDA also notifies the Federal Trade Commission (FTC) of requests from generic drug developers seeking assistance in obtaining samples from brand companies. And the FDA encourages generic drug developers to raise these cases with the FTC if they believe that anticompetitive conduct has taken place.