User login
New Clinician Tool Aims to Stop ALS Diagnosis Delays
SAVANNAH, GEORGIA —
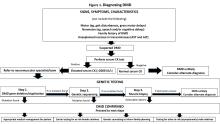
The one-page “thinkALS” tool, designed for clinicians who don’t specialize in neuromuscular disorders, offers a guide to recognize ALS symptoms and determine when it’s time to refer patients to ALS clinics.
“Time is of the essence. It’s really important because the paradigm of looking at ALS is shifting from this being a fatal disease that nobody can do anything about,” said Suma Babu, MBBS, MPH, assistant professor of neurology at Massachusetts General Hospital/Harvard Medical School in Boston, in a presentation at American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. “As a community, we need to think about how can get to the diagnosis point early and get patients started on therapies.”
On Average, ALS Diagnosis Takes 12-15 Months
As Babu noted, the percentage of patients initially diagnosed with something else may be as high as 52%. The time to diagnosis in ALS remained steady at a mean 12-15 months from 1996-1998 to 2000-2018.
“If you keep in mind that an average ALS patient lives only 3-5 years from symptom onset, they’re spending one third of their survival time in just trying to figure out what the diagnosis is,” Babu said. “Often, they may even undergo unnecessary testing and unnecessary surgeries — carpal tunnel releases, spinal surgeries, and so on.”
Babu’s own research, which is under review for publication, examined 2011-2021 Medicare claims to determine the typical time from first neurologist consult to confirmed ALS diagnosis. The mean for ALS/neuromuscular specialists is 9.6 months, while it’s 16.7 months for nonspecialist neurologists.
“It’s a hard pill to swallow,” Babu said, referring to the fact that neurologists are contributing to some of this situation. “But it is a challenge because ALS does not have a definitive diagnostic test, and you’re ruling out other possibilities.”
A ‘Sense of Nihilism’ About Prognoses
She added that “unless you’re seeing a lot of ALS patients, this is not going to be on a neurologist’s or a nurse practitioner’s radar to think about ALS early and then refer them to the right place.”
There’s also an unwarranted “sense of nihilism” about prognoses for patients, she said. “Sometimes people do not understand what’s going on within the ALS field in terms of ‘What are we going to do about it if it’s diagnosed?’ ”
The new one-page tool will be helpful in making diagnoses, she said. “If you have a patient who has asymmetric, progressive weakness, there is an instrument you can turn to that will walk you through the most common symptoms. It’ll also walk you through what to do next.”
The tool lists features of ALS and factors that support — or don’t support — an ALS diagnosis. Users are told to “think ALS” if features in two categories are present and no features in a third category are present.
Referral Wording Is Crucial
Babu added that the “important key feature of this instrument” is guidance for non-neurologists regarding what to write on a referral to neurology so the patient is channeled directly to an ALS clinic. The recommended wording: “CLINICAL SUSPICION FOR ALS.”
Neurologist Ximena Arcila-Londono, MD, of Henry Ford Health in Detroit, spoke after Babu’s presentation and agreed that wording is crucial in referrals. “Please include in your words ‘Rule out motor neuron disorder’ or ‘Rule out ALS,’ ” she said. “Some people in the community are very reluctant to use those words in their referral. If you don’t use the referral and you send them [regarding] weakness, that person is going to get stuck in the general neurology pile. The moment you use the word ‘motor neuron disorder’ or ALS, most of us will get to those patients within a month.”
The tool’s wording adds that “most ALS centers can accommodate urgent ALS referrals within 2 weeks.”
Babu disclosed receiving research funding from the AANEM Foundation, American Academy of Neurology, Muscular Dystrophy Association, OrphAI, Biogen, Ionis, Novartis, Denali, uniQure, and MarvelBiome. Arcila-Londono had no disclosures.
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA —
The one-page “thinkALS” tool, designed for clinicians who don’t specialize in neuromuscular disorders, offers a guide to recognize ALS symptoms and determine when it’s time to refer patients to ALS clinics.
“Time is of the essence. It’s really important because the paradigm of looking at ALS is shifting from this being a fatal disease that nobody can do anything about,” said Suma Babu, MBBS, MPH, assistant professor of neurology at Massachusetts General Hospital/Harvard Medical School in Boston, in a presentation at American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. “As a community, we need to think about how can get to the diagnosis point early and get patients started on therapies.”
On Average, ALS Diagnosis Takes 12-15 Months
As Babu noted, the percentage of patients initially diagnosed with something else may be as high as 52%. The time to diagnosis in ALS remained steady at a mean 12-15 months from 1996-1998 to 2000-2018.
“If you keep in mind that an average ALS patient lives only 3-5 years from symptom onset, they’re spending one third of their survival time in just trying to figure out what the diagnosis is,” Babu said. “Often, they may even undergo unnecessary testing and unnecessary surgeries — carpal tunnel releases, spinal surgeries, and so on.”
Babu’s own research, which is under review for publication, examined 2011-2021 Medicare claims to determine the typical time from first neurologist consult to confirmed ALS diagnosis. The mean for ALS/neuromuscular specialists is 9.6 months, while it’s 16.7 months for nonspecialist neurologists.
“It’s a hard pill to swallow,” Babu said, referring to the fact that neurologists are contributing to some of this situation. “But it is a challenge because ALS does not have a definitive diagnostic test, and you’re ruling out other possibilities.”
A ‘Sense of Nihilism’ About Prognoses
She added that “unless you’re seeing a lot of ALS patients, this is not going to be on a neurologist’s or a nurse practitioner’s radar to think about ALS early and then refer them to the right place.”
There’s also an unwarranted “sense of nihilism” about prognoses for patients, she said. “Sometimes people do not understand what’s going on within the ALS field in terms of ‘What are we going to do about it if it’s diagnosed?’ ”
The new one-page tool will be helpful in making diagnoses, she said. “If you have a patient who has asymmetric, progressive weakness, there is an instrument you can turn to that will walk you through the most common symptoms. It’ll also walk you through what to do next.”
The tool lists features of ALS and factors that support — or don’t support — an ALS diagnosis. Users are told to “think ALS” if features in two categories are present and no features in a third category are present.
Referral Wording Is Crucial
Babu added that the “important key feature of this instrument” is guidance for non-neurologists regarding what to write on a referral to neurology so the patient is channeled directly to an ALS clinic. The recommended wording: “CLINICAL SUSPICION FOR ALS.”
Neurologist Ximena Arcila-Londono, MD, of Henry Ford Health in Detroit, spoke after Babu’s presentation and agreed that wording is crucial in referrals. “Please include in your words ‘Rule out motor neuron disorder’ or ‘Rule out ALS,’ ” she said. “Some people in the community are very reluctant to use those words in their referral. If you don’t use the referral and you send them [regarding] weakness, that person is going to get stuck in the general neurology pile. The moment you use the word ‘motor neuron disorder’ or ALS, most of us will get to those patients within a month.”
The tool’s wording adds that “most ALS centers can accommodate urgent ALS referrals within 2 weeks.”
Babu disclosed receiving research funding from the AANEM Foundation, American Academy of Neurology, Muscular Dystrophy Association, OrphAI, Biogen, Ionis, Novartis, Denali, uniQure, and MarvelBiome. Arcila-Londono had no disclosures.
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA —
The one-page “thinkALS” tool, designed for clinicians who don’t specialize in neuromuscular disorders, offers a guide to recognize ALS symptoms and determine when it’s time to refer patients to ALS clinics.
“Time is of the essence. It’s really important because the paradigm of looking at ALS is shifting from this being a fatal disease that nobody can do anything about,” said Suma Babu, MBBS, MPH, assistant professor of neurology at Massachusetts General Hospital/Harvard Medical School in Boston, in a presentation at American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. “As a community, we need to think about how can get to the diagnosis point early and get patients started on therapies.”
On Average, ALS Diagnosis Takes 12-15 Months
As Babu noted, the percentage of patients initially diagnosed with something else may be as high as 52%. The time to diagnosis in ALS remained steady at a mean 12-15 months from 1996-1998 to 2000-2018.
“If you keep in mind that an average ALS patient lives only 3-5 years from symptom onset, they’re spending one third of their survival time in just trying to figure out what the diagnosis is,” Babu said. “Often, they may even undergo unnecessary testing and unnecessary surgeries — carpal tunnel releases, spinal surgeries, and so on.”
Babu’s own research, which is under review for publication, examined 2011-2021 Medicare claims to determine the typical time from first neurologist consult to confirmed ALS diagnosis. The mean for ALS/neuromuscular specialists is 9.6 months, while it’s 16.7 months for nonspecialist neurologists.
“It’s a hard pill to swallow,” Babu said, referring to the fact that neurologists are contributing to some of this situation. “But it is a challenge because ALS does not have a definitive diagnostic test, and you’re ruling out other possibilities.”
A ‘Sense of Nihilism’ About Prognoses
She added that “unless you’re seeing a lot of ALS patients, this is not going to be on a neurologist’s or a nurse practitioner’s radar to think about ALS early and then refer them to the right place.”
There’s also an unwarranted “sense of nihilism” about prognoses for patients, she said. “Sometimes people do not understand what’s going on within the ALS field in terms of ‘What are we going to do about it if it’s diagnosed?’ ”
The new one-page tool will be helpful in making diagnoses, she said. “If you have a patient who has asymmetric, progressive weakness, there is an instrument you can turn to that will walk you through the most common symptoms. It’ll also walk you through what to do next.”
The tool lists features of ALS and factors that support — or don’t support — an ALS diagnosis. Users are told to “think ALS” if features in two categories are present and no features in a third category are present.
Referral Wording Is Crucial
Babu added that the “important key feature of this instrument” is guidance for non-neurologists regarding what to write on a referral to neurology so the patient is channeled directly to an ALS clinic. The recommended wording: “CLINICAL SUSPICION FOR ALS.”
Neurologist Ximena Arcila-Londono, MD, of Henry Ford Health in Detroit, spoke after Babu’s presentation and agreed that wording is crucial in referrals. “Please include in your words ‘Rule out motor neuron disorder’ or ‘Rule out ALS,’ ” she said. “Some people in the community are very reluctant to use those words in their referral. If you don’t use the referral and you send them [regarding] weakness, that person is going to get stuck in the general neurology pile. The moment you use the word ‘motor neuron disorder’ or ALS, most of us will get to those patients within a month.”
The tool’s wording adds that “most ALS centers can accommodate urgent ALS referrals within 2 weeks.”
Babu disclosed receiving research funding from the AANEM Foundation, American Academy of Neurology, Muscular Dystrophy Association, OrphAI, Biogen, Ionis, Novartis, Denali, uniQure, and MarvelBiome. Arcila-Londono had no disclosures.
A version of this article appeared on Medscape.com.
FROM AANEM 2024
Cardiac Monitoring Is Crucial in Neuromuscular Disorder Care
SAVANNAH, GEORGIA — , a neurologist told an audience of nerve/muscle specialists.
The cardiac conditions can range from asymptomatic to potentially lethal, Nicholas J. Silvestri, MD, professor of neurology at the Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, in New York, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. “It’s really important to know when to do tests and refer to cardiology, and it’s really important to find a cardiologist who can work in concert in taking care of these patients.”
Protein Alterations May Disrupt Heart Muscles
In muscular dystrophies, a prevailing theory suggests that alterations to proteins such as dystrophin disrupt structural integrity in both muscle and cardiac cells, he said.
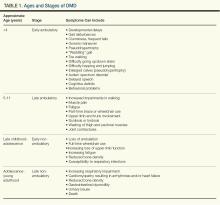
In Duchenne muscular dystrophy (DMD), cardiomyopathy, cardiac conduction abnormalities, or both usually appear in patients by age 10. “It’s important to know that it’s probably present to some degree before that, and it’s not going to get better over time,” he said.
Cardiac problems are universal in DMD by age 18, he said. “Men and boys are living longer, so they have the opportunity to develop the cardiac abnormalities that accrue with time.” Conduction abnormalities typically appear first. “In a lot of these boys, you’ll typically see persistent sinus tachycardia. But they can also develop atrial arrhythmias and bundle branch blocks.”
Sudden cardiac death is responsible for mortality in an estimated 15% patients with DMD. “Very sadly, I lost a patient this way just a few months ago,” Silvestri said.
ECGs and Echos Are Recommended
Screening is crucial. “Make sure that patients get that referral and get these tests done,” he said. “You need an ECG and echo by diagnosis or age 6. This is usually repeated annually or biannually, typically by the cardiologist you’re working with.”
The good news is that there’s evidence of survival benefits from treatment with angiotensin-converting enzyme inhibitors for dilated cardiomyopathy. “Some cardiac experts feel treatment with angiotensin receptor blockers (ARBs) is equivalent.”
Most boys will get echocardiograms, he said, “but there’s a lot of evidence showing that cardiac MRI is probably preferable for a number of reasons,” including better visualization. But the need for sedation limits access, he said, and cardiac MRI may not be available at some facilities.
Worse Outcomes in Becker Muscular Dystrophy (BMD)
Cardiac involvement is more common and more severe in BMD than in DMD. About 50% of deaths in BMD are attributed to malignant arrhythmias or congestive heart failure, he said.
Screening requirements and treatment options in BMD are similar to those in DMD, with the added option of heart transplantation.
Silvestri cautioned that up to 40% of female carriers of dystrophin mutations can develop cardiac dysfunction similar to that seen in DMD and BMD. Cardiac assessments are recommended every 5 years. “It’s important to genotype Mom,” he said, especially in light of the fact that two thirds of DMD cases may be inherited.
“When I send genetic testing on the mother and find her to be a carrier, I send her to a cardiologist so she has the appropriate screening done,” he said.
Pacemakers May Be Considered in Type 1 Myotonic Dystrophy
In type 1 myotonic dystrophy, cardiac conduction abnormalities are seen in two thirds of patients, and sudden cardiac death in up to 30% of patients. “When it is diagnosed, patients do need an ECG at that time, as well as annually,” he said.
Holter monitoring or implantable loop recorders may be recommended, and permanent pacing via an implantable cardioverter-defibrillator might be appropriate.
“Based on the literature to date, the exact timing is not is not clear,” Silvestri said. “The electrophysiologists in my area tend to be very aggressive, thankfully, and treat them fairly soon with pacemakers when we see the first sign of trouble.”
Silvestri disclosed consultant/advisory relationships with argenx, Alexion, Amgen, UCB, Immunovant, and Janssen.
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA — , a neurologist told an audience of nerve/muscle specialists.
The cardiac conditions can range from asymptomatic to potentially lethal, Nicholas J. Silvestri, MD, professor of neurology at the Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, in New York, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. “It’s really important to know when to do tests and refer to cardiology, and it’s really important to find a cardiologist who can work in concert in taking care of these patients.”
Protein Alterations May Disrupt Heart Muscles
In muscular dystrophies, a prevailing theory suggests that alterations to proteins such as dystrophin disrupt structural integrity in both muscle and cardiac cells, he said.
In Duchenne muscular dystrophy (DMD), cardiomyopathy, cardiac conduction abnormalities, or both usually appear in patients by age 10. “It’s important to know that it’s probably present to some degree before that, and it’s not going to get better over time,” he said.
Cardiac problems are universal in DMD by age 18, he said. “Men and boys are living longer, so they have the opportunity to develop the cardiac abnormalities that accrue with time.” Conduction abnormalities typically appear first. “In a lot of these boys, you’ll typically see persistent sinus tachycardia. But they can also develop atrial arrhythmias and bundle branch blocks.”
Sudden cardiac death is responsible for mortality in an estimated 15% patients with DMD. “Very sadly, I lost a patient this way just a few months ago,” Silvestri said.
ECGs and Echos Are Recommended
Screening is crucial. “Make sure that patients get that referral and get these tests done,” he said. “You need an ECG and echo by diagnosis or age 6. This is usually repeated annually or biannually, typically by the cardiologist you’re working with.”
The good news is that there’s evidence of survival benefits from treatment with angiotensin-converting enzyme inhibitors for dilated cardiomyopathy. “Some cardiac experts feel treatment with angiotensin receptor blockers (ARBs) is equivalent.”
Most boys will get echocardiograms, he said, “but there’s a lot of evidence showing that cardiac MRI is probably preferable for a number of reasons,” including better visualization. But the need for sedation limits access, he said, and cardiac MRI may not be available at some facilities.
Worse Outcomes in Becker Muscular Dystrophy (BMD)
Cardiac involvement is more common and more severe in BMD than in DMD. About 50% of deaths in BMD are attributed to malignant arrhythmias or congestive heart failure, he said.
Screening requirements and treatment options in BMD are similar to those in DMD, with the added option of heart transplantation.
Silvestri cautioned that up to 40% of female carriers of dystrophin mutations can develop cardiac dysfunction similar to that seen in DMD and BMD. Cardiac assessments are recommended every 5 years. “It’s important to genotype Mom,” he said, especially in light of the fact that two thirds of DMD cases may be inherited.
“When I send genetic testing on the mother and find her to be a carrier, I send her to a cardiologist so she has the appropriate screening done,” he said.
Pacemakers May Be Considered in Type 1 Myotonic Dystrophy
In type 1 myotonic dystrophy, cardiac conduction abnormalities are seen in two thirds of patients, and sudden cardiac death in up to 30% of patients. “When it is diagnosed, patients do need an ECG at that time, as well as annually,” he said.
Holter monitoring or implantable loop recorders may be recommended, and permanent pacing via an implantable cardioverter-defibrillator might be appropriate.
“Based on the literature to date, the exact timing is not is not clear,” Silvestri said. “The electrophysiologists in my area tend to be very aggressive, thankfully, and treat them fairly soon with pacemakers when we see the first sign of trouble.”
Silvestri disclosed consultant/advisory relationships with argenx, Alexion, Amgen, UCB, Immunovant, and Janssen.
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA — , a neurologist told an audience of nerve/muscle specialists.
The cardiac conditions can range from asymptomatic to potentially lethal, Nicholas J. Silvestri, MD, professor of neurology at the Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, in New York, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. “It’s really important to know when to do tests and refer to cardiology, and it’s really important to find a cardiologist who can work in concert in taking care of these patients.”
Protein Alterations May Disrupt Heart Muscles
In muscular dystrophies, a prevailing theory suggests that alterations to proteins such as dystrophin disrupt structural integrity in both muscle and cardiac cells, he said.
In Duchenne muscular dystrophy (DMD), cardiomyopathy, cardiac conduction abnormalities, or both usually appear in patients by age 10. “It’s important to know that it’s probably present to some degree before that, and it’s not going to get better over time,” he said.
Cardiac problems are universal in DMD by age 18, he said. “Men and boys are living longer, so they have the opportunity to develop the cardiac abnormalities that accrue with time.” Conduction abnormalities typically appear first. “In a lot of these boys, you’ll typically see persistent sinus tachycardia. But they can also develop atrial arrhythmias and bundle branch blocks.”
Sudden cardiac death is responsible for mortality in an estimated 15% patients with DMD. “Very sadly, I lost a patient this way just a few months ago,” Silvestri said.
ECGs and Echos Are Recommended
Screening is crucial. “Make sure that patients get that referral and get these tests done,” he said. “You need an ECG and echo by diagnosis or age 6. This is usually repeated annually or biannually, typically by the cardiologist you’re working with.”
The good news is that there’s evidence of survival benefits from treatment with angiotensin-converting enzyme inhibitors for dilated cardiomyopathy. “Some cardiac experts feel treatment with angiotensin receptor blockers (ARBs) is equivalent.”
Most boys will get echocardiograms, he said, “but there’s a lot of evidence showing that cardiac MRI is probably preferable for a number of reasons,” including better visualization. But the need for sedation limits access, he said, and cardiac MRI may not be available at some facilities.
Worse Outcomes in Becker Muscular Dystrophy (BMD)
Cardiac involvement is more common and more severe in BMD than in DMD. About 50% of deaths in BMD are attributed to malignant arrhythmias or congestive heart failure, he said.
Screening requirements and treatment options in BMD are similar to those in DMD, with the added option of heart transplantation.
Silvestri cautioned that up to 40% of female carriers of dystrophin mutations can develop cardiac dysfunction similar to that seen in DMD and BMD. Cardiac assessments are recommended every 5 years. “It’s important to genotype Mom,” he said, especially in light of the fact that two thirds of DMD cases may be inherited.
“When I send genetic testing on the mother and find her to be a carrier, I send her to a cardiologist so she has the appropriate screening done,” he said.
Pacemakers May Be Considered in Type 1 Myotonic Dystrophy
In type 1 myotonic dystrophy, cardiac conduction abnormalities are seen in two thirds of patients, and sudden cardiac death in up to 30% of patients. “When it is diagnosed, patients do need an ECG at that time, as well as annually,” he said.
Holter monitoring or implantable loop recorders may be recommended, and permanent pacing via an implantable cardioverter-defibrillator might be appropriate.
“Based on the literature to date, the exact timing is not is not clear,” Silvestri said. “The electrophysiologists in my area tend to be very aggressive, thankfully, and treat them fairly soon with pacemakers when we see the first sign of trouble.”
Silvestri disclosed consultant/advisory relationships with argenx, Alexion, Amgen, UCB, Immunovant, and Janssen.
A version of this article appeared on Medscape.com.
FROM AANEM 2024
ALS Update: Drug Therapy Continues to Offer Little Benefit
SAVANNAH, GEORGIA — , nerve specialists learned.
The glutamate blocker riluzole (Rilutek), which became the first ALS drug to receive US Food and Drug Administration (FDA) approval in 1995, continues to be used, Michael D. Weiss, MD, professor of neurology at University of Washington School of Medicine, Seattle, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Weiss highlighted a 2012 Cochrane Library review that examined research and found the drug is “reasonably safe” and prolongs median survival by about 2-3 months. “About 12% develop liver disease. It’s pretty rare that we stop the medicine due to liver toxicity.”
Earlier Treatment Could Pay Dividends
A recent study “suggests we might be able to get more bang for our buck from riluzole” by initiating treatment earlier, Weiss said.
Researchers tracked 4778 patients with ALS, including 3446 (72.1%) who took riluzole. Those who took the drug survived a median 2 extra months (22.6 vs 20.2 months; P < .001). The data suggested that delaying riluzole initiation by 1 year (from 6 months to 18 months after diagnosis) reduced the median survival by 1.9 months (from 40.1 to 38.2 months).
There’s “a relatively significant additional benefit” to earlier treatment, Weiss said, although patients will vary on whether they think it’s meaningful. As for limitations, “there’s no clear impact on disease progression, and there’s a need for periodic monitoring of liver function profile.”
He added that there’s an out-of-pocket co-pay. “Even as a generic, it’s not that cheap. Depending on the source, it could cost anywhere from $1800 to $8400 a year.”
Edaravone Could Lack Relevant Benefit
No other ALS treatment appeared until 2017, when the FDA approved the novel antioxidant edaravone (Radicava). In 2022, the agency approved an oral suspension version, but a study published that year suggested there may not be a clinically relevant benefit.
The University of Washington, where Weiss works, offered the drug to 144 patients, according to an analysis. Eighty percent of the patients wanted it, but insurers refused to cover it for more than 20%. The average time to treatment with the drug was 28 days after patients said they wanted it.
That’s a “substantial delay,” Weiss said.
The cost is about $171,000 a year, he said, and assistance is limited for underinsured patients.*
Other Options
As Weiss noted, another drug, AMX0035 (Relyvrio), received FDA approval in 2022, but its manufacturer pulled it from the US/Canada market in April 2024 following poor phase 3 trial findings.
In 2023, the FDA approved another drug, the antisense oligonucleotide tofersen (Qalsody), in patients with ALS associated with a mutation in the superoxide dismutase 1 gene. According to the FDA, reductions in plasma neurofilament light concentration were “reasonably likely to predict a clinical benefit in patients.”
Only 1%-2% of patients with ALS fit the criteria to get the drug, Weiss said. He noted other limitations such as the cost ($180,000 a year), the need for lifelong monthly intrathecal injections, and serious neurological side effects in 7% of patients per a 2022 trial.
Weiss disclosed advisory board (Alexion, Ra [now UCB], argenx, Biogen, Mitsubishi Tanabe Pharma, Amylyx), data safety monitoring board (Sanofi, AI), consulting (Cytokinetics, CSL Behring), and speaker (Soleo) relationships.
*Correction, 10/23/2024: This story originally quoted Weiss as saying the maker of edaravone provides no assistance to underinsured patients. Weiss has clarified that he should have said this coverage is “limited.”
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA — , nerve specialists learned.
The glutamate blocker riluzole (Rilutek), which became the first ALS drug to receive US Food and Drug Administration (FDA) approval in 1995, continues to be used, Michael D. Weiss, MD, professor of neurology at University of Washington School of Medicine, Seattle, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Weiss highlighted a 2012 Cochrane Library review that examined research and found the drug is “reasonably safe” and prolongs median survival by about 2-3 months. “About 12% develop liver disease. It’s pretty rare that we stop the medicine due to liver toxicity.”
Earlier Treatment Could Pay Dividends
A recent study “suggests we might be able to get more bang for our buck from riluzole” by initiating treatment earlier, Weiss said.
Researchers tracked 4778 patients with ALS, including 3446 (72.1%) who took riluzole. Those who took the drug survived a median 2 extra months (22.6 vs 20.2 months; P < .001). The data suggested that delaying riluzole initiation by 1 year (from 6 months to 18 months after diagnosis) reduced the median survival by 1.9 months (from 40.1 to 38.2 months).
There’s “a relatively significant additional benefit” to earlier treatment, Weiss said, although patients will vary on whether they think it’s meaningful. As for limitations, “there’s no clear impact on disease progression, and there’s a need for periodic monitoring of liver function profile.”
He added that there’s an out-of-pocket co-pay. “Even as a generic, it’s not that cheap. Depending on the source, it could cost anywhere from $1800 to $8400 a year.”
Edaravone Could Lack Relevant Benefit
No other ALS treatment appeared until 2017, when the FDA approved the novel antioxidant edaravone (Radicava). In 2022, the agency approved an oral suspension version, but a study published that year suggested there may not be a clinically relevant benefit.
The University of Washington, where Weiss works, offered the drug to 144 patients, according to an analysis. Eighty percent of the patients wanted it, but insurers refused to cover it for more than 20%. The average time to treatment with the drug was 28 days after patients said they wanted it.
That’s a “substantial delay,” Weiss said.
The cost is about $171,000 a year, he said, and assistance is limited for underinsured patients.*
Other Options
As Weiss noted, another drug, AMX0035 (Relyvrio), received FDA approval in 2022, but its manufacturer pulled it from the US/Canada market in April 2024 following poor phase 3 trial findings.
In 2023, the FDA approved another drug, the antisense oligonucleotide tofersen (Qalsody), in patients with ALS associated with a mutation in the superoxide dismutase 1 gene. According to the FDA, reductions in plasma neurofilament light concentration were “reasonably likely to predict a clinical benefit in patients.”
Only 1%-2% of patients with ALS fit the criteria to get the drug, Weiss said. He noted other limitations such as the cost ($180,000 a year), the need for lifelong monthly intrathecal injections, and serious neurological side effects in 7% of patients per a 2022 trial.
Weiss disclosed advisory board (Alexion, Ra [now UCB], argenx, Biogen, Mitsubishi Tanabe Pharma, Amylyx), data safety monitoring board (Sanofi, AI), consulting (Cytokinetics, CSL Behring), and speaker (Soleo) relationships.
*Correction, 10/23/2024: This story originally quoted Weiss as saying the maker of edaravone provides no assistance to underinsured patients. Weiss has clarified that he should have said this coverage is “limited.”
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA — , nerve specialists learned.
The glutamate blocker riluzole (Rilutek), which became the first ALS drug to receive US Food and Drug Administration (FDA) approval in 1995, continues to be used, Michael D. Weiss, MD, professor of neurology at University of Washington School of Medicine, Seattle, said in a presentation at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Weiss highlighted a 2012 Cochrane Library review that examined research and found the drug is “reasonably safe” and prolongs median survival by about 2-3 months. “About 12% develop liver disease. It’s pretty rare that we stop the medicine due to liver toxicity.”
Earlier Treatment Could Pay Dividends
A recent study “suggests we might be able to get more bang for our buck from riluzole” by initiating treatment earlier, Weiss said.
Researchers tracked 4778 patients with ALS, including 3446 (72.1%) who took riluzole. Those who took the drug survived a median 2 extra months (22.6 vs 20.2 months; P < .001). The data suggested that delaying riluzole initiation by 1 year (from 6 months to 18 months after diagnosis) reduced the median survival by 1.9 months (from 40.1 to 38.2 months).
There’s “a relatively significant additional benefit” to earlier treatment, Weiss said, although patients will vary on whether they think it’s meaningful. As for limitations, “there’s no clear impact on disease progression, and there’s a need for periodic monitoring of liver function profile.”
He added that there’s an out-of-pocket co-pay. “Even as a generic, it’s not that cheap. Depending on the source, it could cost anywhere from $1800 to $8400 a year.”
Edaravone Could Lack Relevant Benefit
No other ALS treatment appeared until 2017, when the FDA approved the novel antioxidant edaravone (Radicava). In 2022, the agency approved an oral suspension version, but a study published that year suggested there may not be a clinically relevant benefit.
The University of Washington, where Weiss works, offered the drug to 144 patients, according to an analysis. Eighty percent of the patients wanted it, but insurers refused to cover it for more than 20%. The average time to treatment with the drug was 28 days after patients said they wanted it.
That’s a “substantial delay,” Weiss said.
The cost is about $171,000 a year, he said, and assistance is limited for underinsured patients.*
Other Options
As Weiss noted, another drug, AMX0035 (Relyvrio), received FDA approval in 2022, but its manufacturer pulled it from the US/Canada market in April 2024 following poor phase 3 trial findings.
In 2023, the FDA approved another drug, the antisense oligonucleotide tofersen (Qalsody), in patients with ALS associated with a mutation in the superoxide dismutase 1 gene. According to the FDA, reductions in plasma neurofilament light concentration were “reasonably likely to predict a clinical benefit in patients.”
Only 1%-2% of patients with ALS fit the criteria to get the drug, Weiss said. He noted other limitations such as the cost ($180,000 a year), the need for lifelong monthly intrathecal injections, and serious neurological side effects in 7% of patients per a 2022 trial.
Weiss disclosed advisory board (Alexion, Ra [now UCB], argenx, Biogen, Mitsubishi Tanabe Pharma, Amylyx), data safety monitoring board (Sanofi, AI), consulting (Cytokinetics, CSL Behring), and speaker (Soleo) relationships.
*Correction, 10/23/2024: This story originally quoted Weiss as saying the maker of edaravone provides no assistance to underinsured patients. Weiss has clarified that he should have said this coverage is “limited.”
A version of this article appeared on Medscape.com.
FROM AANEM 2024
Myasthenia Gravis: Similar Symptoms in Relatives Raise Question of Genes
SAVANNAH, GEORGIA — One patient with autoimmune myasthenia gravis (MG) has a niece with the same diagnosis, and at least one of his other close relatives may have it too. Another patient with MG lost his father and brother to complications from the disease, while a surviving brother also has it. These two cases, reported at a meeting of nerve/muscle specialists, spotlight one of the mysteries of MG: What role does heredity play in this disorder?
“Clinical familial associations — when transmission appears to be vertical, from parent to offspring — suggest that there is much yet to learn about genetic bases for autoimmunity and how certain mutations could favor selection for specific immune disorders,” said Elena Shanina, MD, PhD, a neurology professor at the University of Texas Medical Branch, Galveston, in an interview. She and colleagues presented the two case reports at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
As Shanina noted, MG is usually sporadic without a link to heredity. However, she said, research suggests that up to 7% of patients have MG in their family history.
“There are well-described genetic causes for congenital myasthenic syndromes, in which mutations occur in genes for neuromuscular junction (NMJ) proteins affecting NMJ function. However, much less is known about genetic associations to autoimmune MG,” she said.
“More than a decade ago, differences in HLA DQ haplotype-associated presentation of AChR alpha-chain peptides were suggested to suffice in producing MG, and specific HLA DQ susceptibility links were found predisposing to MG. More recent studies have tried to identify specific genes such as CTLA4 mutations that enhance autoimmunity and neuroinflammation.”
Two Cases
In one of the case reports, a 75-year-old White man with hereditary coagulopathy presented with myasthenic crisis in the setting of acute pulmonary embolism. Chronic symptoms included diplopia, ptosis, and proximal muscle weakness.
A niece of the patient has been diagnosed with MG and suffers from ocular symptoms. Meanwhile, an uncle has ptosis but no diagnosis yet, and a daughter has dermatomyositis. Like MG, dermatomyositis is an autoimmune disease that causes muscle weakness.
The patient, who’s CTLA4 negative, is faring well on eculizumab after failing standard therapies, Shanina said.
In the other case, a 67-year-old Hispanic man presented with diplopia, generalized fatigue, and weakness. Like the other patient, he was seropositive for acetylcholine receptor antibodies.
This patient lost his father and brother to complications from MG. Another brother, who’s still living, also has MG.
“The patient has minimal manifestation status with disease and is currently controlled using oral immunomodulatory therapies,” Shanina said. “He is also CTLA4 negative.”
Genetics and Environment May Each Play a Role
Shanina called for research exploring mutations and inheritance patterns in families with MG.
“If there are genetic causes that increase autoimmunity with specific propensity for certain immune diseases, correcting those mutations could fundamentally change how we treat — and prevent — at least some autoimmune diseases,” she said. “For example, if HLA linkage is directly involved in determining susceptibility to MG, and if the presence of a specific HLA locus allele is sufficient to produce disease, HLA gene editing could be a future therapy to prevent such diseases. Likewise, monoclonal antibodies that target products of genes that increase risk for autoimmunity might be able to reduce such risks without modifying the patient’s genome.”
Henry J. Kaminski, MD, professor of neurology at George Washington University, Washington, DC, is familiar with the report’s findings. In an interview, he noted that while genetic profiles can make MG more likely, “the situation is not like Huntington’s or Alzheimer’s where there is a strong genetic risk.”
Instead, he said, there’s “a genetic risk coupled to some environmental stimulus that leads to the development of MG, which is true for many complex autoimmune conditions.”
While he doesn’t think the two new case reports are especially noteworthy, Kaminski said “the ability to assess genetic risk factors across patients will elucidate understanding of MG. Personalized medicine choices will likely require understanding of genetic risks.”
While understanding MG in families is “always good to know from a research perspective,” there’s no reason to launch surveillance of relatives to see if they also have the disease, he said.
Also, Kaminski cautioned that it’s important to differentiate autoimmune MG from congenital myasthenia, an even more rare genetic disorder of neuromuscular transmission. “Congenital myasthenias will not improve with immune therapy, and patients will suffer complications for no reason,” he said. “A patient who is seronegative should be assessed for congenital myasthenia with the right clinical presentation. The condition would be more likely in patients with a family history of symptoms similar to MG. It may be symptomatic at birth, but patients may present in adulthood.”
Kaminski noted that his team is collecting saliva samples from patients with MuSK-MG, a rare MG subtype linked to more severe cases, for genetic testing and genome-wide association studies.
There was no study funding, and the authors have no disclosures. Kaminski is principal investigator of a rare disease network dedicated to MG.
A version of this article first appeared on Medscape.com.
SAVANNAH, GEORGIA — One patient with autoimmune myasthenia gravis (MG) has a niece with the same diagnosis, and at least one of his other close relatives may have it too. Another patient with MG lost his father and brother to complications from the disease, while a surviving brother also has it. These two cases, reported at a meeting of nerve/muscle specialists, spotlight one of the mysteries of MG: What role does heredity play in this disorder?
“Clinical familial associations — when transmission appears to be vertical, from parent to offspring — suggest that there is much yet to learn about genetic bases for autoimmunity and how certain mutations could favor selection for specific immune disorders,” said Elena Shanina, MD, PhD, a neurology professor at the University of Texas Medical Branch, Galveston, in an interview. She and colleagues presented the two case reports at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
As Shanina noted, MG is usually sporadic without a link to heredity. However, she said, research suggests that up to 7% of patients have MG in their family history.
“There are well-described genetic causes for congenital myasthenic syndromes, in which mutations occur in genes for neuromuscular junction (NMJ) proteins affecting NMJ function. However, much less is known about genetic associations to autoimmune MG,” she said.
“More than a decade ago, differences in HLA DQ haplotype-associated presentation of AChR alpha-chain peptides were suggested to suffice in producing MG, and specific HLA DQ susceptibility links were found predisposing to MG. More recent studies have tried to identify specific genes such as CTLA4 mutations that enhance autoimmunity and neuroinflammation.”
Two Cases
In one of the case reports, a 75-year-old White man with hereditary coagulopathy presented with myasthenic crisis in the setting of acute pulmonary embolism. Chronic symptoms included diplopia, ptosis, and proximal muscle weakness.
A niece of the patient has been diagnosed with MG and suffers from ocular symptoms. Meanwhile, an uncle has ptosis but no diagnosis yet, and a daughter has dermatomyositis. Like MG, dermatomyositis is an autoimmune disease that causes muscle weakness.
The patient, who’s CTLA4 negative, is faring well on eculizumab after failing standard therapies, Shanina said.
In the other case, a 67-year-old Hispanic man presented with diplopia, generalized fatigue, and weakness. Like the other patient, he was seropositive for acetylcholine receptor antibodies.
This patient lost his father and brother to complications from MG. Another brother, who’s still living, also has MG.
“The patient has minimal manifestation status with disease and is currently controlled using oral immunomodulatory therapies,” Shanina said. “He is also CTLA4 negative.”
Genetics and Environment May Each Play a Role
Shanina called for research exploring mutations and inheritance patterns in families with MG.
“If there are genetic causes that increase autoimmunity with specific propensity for certain immune diseases, correcting those mutations could fundamentally change how we treat — and prevent — at least some autoimmune diseases,” she said. “For example, if HLA linkage is directly involved in determining susceptibility to MG, and if the presence of a specific HLA locus allele is sufficient to produce disease, HLA gene editing could be a future therapy to prevent such diseases. Likewise, monoclonal antibodies that target products of genes that increase risk for autoimmunity might be able to reduce such risks without modifying the patient’s genome.”
Henry J. Kaminski, MD, professor of neurology at George Washington University, Washington, DC, is familiar with the report’s findings. In an interview, he noted that while genetic profiles can make MG more likely, “the situation is not like Huntington’s or Alzheimer’s where there is a strong genetic risk.”
Instead, he said, there’s “a genetic risk coupled to some environmental stimulus that leads to the development of MG, which is true for many complex autoimmune conditions.”
While he doesn’t think the two new case reports are especially noteworthy, Kaminski said “the ability to assess genetic risk factors across patients will elucidate understanding of MG. Personalized medicine choices will likely require understanding of genetic risks.”
While understanding MG in families is “always good to know from a research perspective,” there’s no reason to launch surveillance of relatives to see if they also have the disease, he said.
Also, Kaminski cautioned that it’s important to differentiate autoimmune MG from congenital myasthenia, an even more rare genetic disorder of neuromuscular transmission. “Congenital myasthenias will not improve with immune therapy, and patients will suffer complications for no reason,” he said. “A patient who is seronegative should be assessed for congenital myasthenia with the right clinical presentation. The condition would be more likely in patients with a family history of symptoms similar to MG. It may be symptomatic at birth, but patients may present in adulthood.”
Kaminski noted that his team is collecting saliva samples from patients with MuSK-MG, a rare MG subtype linked to more severe cases, for genetic testing and genome-wide association studies.
There was no study funding, and the authors have no disclosures. Kaminski is principal investigator of a rare disease network dedicated to MG.
A version of this article first appeared on Medscape.com.
SAVANNAH, GEORGIA — One patient with autoimmune myasthenia gravis (MG) has a niece with the same diagnosis, and at least one of his other close relatives may have it too. Another patient with MG lost his father and brother to complications from the disease, while a surviving brother also has it. These two cases, reported at a meeting of nerve/muscle specialists, spotlight one of the mysteries of MG: What role does heredity play in this disorder?
“Clinical familial associations — when transmission appears to be vertical, from parent to offspring — suggest that there is much yet to learn about genetic bases for autoimmunity and how certain mutations could favor selection for specific immune disorders,” said Elena Shanina, MD, PhD, a neurology professor at the University of Texas Medical Branch, Galveston, in an interview. She and colleagues presented the two case reports at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
As Shanina noted, MG is usually sporadic without a link to heredity. However, she said, research suggests that up to 7% of patients have MG in their family history.
“There are well-described genetic causes for congenital myasthenic syndromes, in which mutations occur in genes for neuromuscular junction (NMJ) proteins affecting NMJ function. However, much less is known about genetic associations to autoimmune MG,” she said.
“More than a decade ago, differences in HLA DQ haplotype-associated presentation of AChR alpha-chain peptides were suggested to suffice in producing MG, and specific HLA DQ susceptibility links were found predisposing to MG. More recent studies have tried to identify specific genes such as CTLA4 mutations that enhance autoimmunity and neuroinflammation.”
Two Cases
In one of the case reports, a 75-year-old White man with hereditary coagulopathy presented with myasthenic crisis in the setting of acute pulmonary embolism. Chronic symptoms included diplopia, ptosis, and proximal muscle weakness.
A niece of the patient has been diagnosed with MG and suffers from ocular symptoms. Meanwhile, an uncle has ptosis but no diagnosis yet, and a daughter has dermatomyositis. Like MG, dermatomyositis is an autoimmune disease that causes muscle weakness.
The patient, who’s CTLA4 negative, is faring well on eculizumab after failing standard therapies, Shanina said.
In the other case, a 67-year-old Hispanic man presented with diplopia, generalized fatigue, and weakness. Like the other patient, he was seropositive for acetylcholine receptor antibodies.
This patient lost his father and brother to complications from MG. Another brother, who’s still living, also has MG.
“The patient has minimal manifestation status with disease and is currently controlled using oral immunomodulatory therapies,” Shanina said. “He is also CTLA4 negative.”
Genetics and Environment May Each Play a Role
Shanina called for research exploring mutations and inheritance patterns in families with MG.
“If there are genetic causes that increase autoimmunity with specific propensity for certain immune diseases, correcting those mutations could fundamentally change how we treat — and prevent — at least some autoimmune diseases,” she said. “For example, if HLA linkage is directly involved in determining susceptibility to MG, and if the presence of a specific HLA locus allele is sufficient to produce disease, HLA gene editing could be a future therapy to prevent such diseases. Likewise, monoclonal antibodies that target products of genes that increase risk for autoimmunity might be able to reduce such risks without modifying the patient’s genome.”
Henry J. Kaminski, MD, professor of neurology at George Washington University, Washington, DC, is familiar with the report’s findings. In an interview, he noted that while genetic profiles can make MG more likely, “the situation is not like Huntington’s or Alzheimer’s where there is a strong genetic risk.”
Instead, he said, there’s “a genetic risk coupled to some environmental stimulus that leads to the development of MG, which is true for many complex autoimmune conditions.”
While he doesn’t think the two new case reports are especially noteworthy, Kaminski said “the ability to assess genetic risk factors across patients will elucidate understanding of MG. Personalized medicine choices will likely require understanding of genetic risks.”
While understanding MG in families is “always good to know from a research perspective,” there’s no reason to launch surveillance of relatives to see if they also have the disease, he said.
Also, Kaminski cautioned that it’s important to differentiate autoimmune MG from congenital myasthenia, an even more rare genetic disorder of neuromuscular transmission. “Congenital myasthenias will not improve with immune therapy, and patients will suffer complications for no reason,” he said. “A patient who is seronegative should be assessed for congenital myasthenia with the right clinical presentation. The condition would be more likely in patients with a family history of symptoms similar to MG. It may be symptomatic at birth, but patients may present in adulthood.”
Kaminski noted that his team is collecting saliva samples from patients with MuSK-MG, a rare MG subtype linked to more severe cases, for genetic testing and genome-wide association studies.
There was no study funding, and the authors have no disclosures. Kaminski is principal investigator of a rare disease network dedicated to MG.
A version of this article first appeared on Medscape.com.
FROM AANEM 2024
At Last, Treatment Is in Sight for Charcot-Marie-Tooth Disease
SAVANNAH, GEORGIA — There’s no medical treatment for Charcot-Marie-Tooth (CMT) disease, a debilitating neurologic disorder that’s both progressive and incurable. But now, nerve specialists learned, new potential treatments are moving closer to clinical trials.
neurologists told an audience at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. But the neurologists also noted challenges, such as determining the best way to track disease progression — which can be slow — and the need to recruit high numbers of patients for trials.
A Common Genetic Neuromuscular Disorder
As Mario Saporta, MD, PhD, MBA, of the University of Miami, Coral Gables, Florida, explained, CMT is the most common genetic neuromuscular disorder, affecting 1 in 2500 people or about 130,000-150,000 in the United States. “Typically, it’s a length-dependent neuropathy, where your longest nerves would be affected earlier and more severely. That’s why we see foot deformities, inverted champagne bottle legs, and hand atrophy.”
Most patients with CMT in the United States have type 1A, which is linked to duplication of the PMP22 gene. All types lead to axonal degeneration, which appears to be the main cause of functional disability, Saporta said. “Patients become weaker and then progress with time, following the degree of axonal generation that they have.”
As many as 150 genes may eventually be deemed to cause CMT. The high number of genetically different forms makes diagnosis and genetic therapy difficult, he said, but that’s just part of the picture. Variations among mutations mean there’s “probably actually over 1000 different diseases” within CMT from a biologic perspective.
Genetic Therapy
In regard to genetic treatment, Bipasha Mukherjee-Clavin, MD, PhD, of Johns Hopkins University School of Medicine, Baltimore, Maryland, said a key factor is whether the patient’s form of CMT is passed on in an autosomal dominant or autosomal recessive manner.
“Autosomal dominant conditions are typically caused by gain of function mutations. So that means the goal of our genetic therapeutic would be to reduce expression of the mutated gene,” she said. “In contrast, autosomal recessive conditions are caused by loss-of-function mutations, which means the goal of our genetic therapeutic would be to replace the mutated gene with a normal, wild-type copy.”
A tool like CRISPR could be used to directly edit the part of the genome with a CMT-causing mutation or a viral vector could deliver a healthy, wild-type copy of a gene, she said. These approaches are both being tested.
Another approach is to reduce expression at the RNA level. “RNA therapeutics are FDA [Food and Drug Administration]–approved for other neuromuscular indications, and you may well be using some of these in your own clinical practice,” she said.
Currently, about seven different projects are in the works on the RNA therapeutics front in CMT, she said, including six focusing on type 1A. Mukherjee-Clavin believes that this subtype is a “great” target because it’s so common, affecting an estimated 1 in 5000 people.
“You actually have enough patients to power a clinical trial,” she said. Also, “it’s a homogeneous population, both in terms of the genetics and in terms of the clinical presentation.”
Preclinical Treatment Approaches
However, there are challenges. Drug delivery to Schwann cells, which insulate axons, is difficult, she said. “The other problem is that we want to avoid overly silencing PMP22 because that runs the theoretical risk of causing a different condition, HNPP [hereditary neuropathy with liability to pressure palsies]. HNPP is caused by deletions of PMP22, so we want to avoid that situation.”
Mukherjee-Clavin highlighted two RNA therapeutic products that she expects to move from preclinical to clinical research soon.
One is TVR110 by Armatus Bio, a microRNA intrathecal injection product, which aims to reduce PMP22 overexpression. “It targets basically reduces PMP22 mRNA expression and then normalizes the amount of PMP22 protein that is ultimately generated,” she said.
The other therapy, a small interfering RNA intravenous product delivered to Schwann cells, is being developed by DTx Pharma/Novartis.
Outside of the RNA arena, “there are a number of other programs that are in the preclinical phases that I think will be moving through this pipeline,” Mukherjee-Clavin said. “We’ll see if some of these enter first-in-human clinical trials.”
Meanwhile, Saporta highlighted small-molecule strategies that target a subtype of CMT called sorbitol dehydrogenase (SORD) deficiency that’s caused by mutations in the SORD gene. He noted that Applied Therapeutics is testing an investigational drug called govorestat (AT-007) in 56 patients in a double-blind, randomized, placebo-controlled phase 3 registrational study. The company recently reported that interim 12-month results are promising.
Saporta disclosed consulting for DTx Pharma/Novartis, Applied Therapeutics, and Pharnext. Mukherjee-Clavin had no disclosures.
A version of this article first appeared on Medscape.com.
SAVANNAH, GEORGIA — There’s no medical treatment for Charcot-Marie-Tooth (CMT) disease, a debilitating neurologic disorder that’s both progressive and incurable. But now, nerve specialists learned, new potential treatments are moving closer to clinical trials.
neurologists told an audience at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. But the neurologists also noted challenges, such as determining the best way to track disease progression — which can be slow — and the need to recruit high numbers of patients for trials.
A Common Genetic Neuromuscular Disorder
As Mario Saporta, MD, PhD, MBA, of the University of Miami, Coral Gables, Florida, explained, CMT is the most common genetic neuromuscular disorder, affecting 1 in 2500 people or about 130,000-150,000 in the United States. “Typically, it’s a length-dependent neuropathy, where your longest nerves would be affected earlier and more severely. That’s why we see foot deformities, inverted champagne bottle legs, and hand atrophy.”
Most patients with CMT in the United States have type 1A, which is linked to duplication of the PMP22 gene. All types lead to axonal degeneration, which appears to be the main cause of functional disability, Saporta said. “Patients become weaker and then progress with time, following the degree of axonal generation that they have.”
As many as 150 genes may eventually be deemed to cause CMT. The high number of genetically different forms makes diagnosis and genetic therapy difficult, he said, but that’s just part of the picture. Variations among mutations mean there’s “probably actually over 1000 different diseases” within CMT from a biologic perspective.
Genetic Therapy
In regard to genetic treatment, Bipasha Mukherjee-Clavin, MD, PhD, of Johns Hopkins University School of Medicine, Baltimore, Maryland, said a key factor is whether the patient’s form of CMT is passed on in an autosomal dominant or autosomal recessive manner.
“Autosomal dominant conditions are typically caused by gain of function mutations. So that means the goal of our genetic therapeutic would be to reduce expression of the mutated gene,” she said. “In contrast, autosomal recessive conditions are caused by loss-of-function mutations, which means the goal of our genetic therapeutic would be to replace the mutated gene with a normal, wild-type copy.”
A tool like CRISPR could be used to directly edit the part of the genome with a CMT-causing mutation or a viral vector could deliver a healthy, wild-type copy of a gene, she said. These approaches are both being tested.
Another approach is to reduce expression at the RNA level. “RNA therapeutics are FDA [Food and Drug Administration]–approved for other neuromuscular indications, and you may well be using some of these in your own clinical practice,” she said.
Currently, about seven different projects are in the works on the RNA therapeutics front in CMT, she said, including six focusing on type 1A. Mukherjee-Clavin believes that this subtype is a “great” target because it’s so common, affecting an estimated 1 in 5000 people.
“You actually have enough patients to power a clinical trial,” she said. Also, “it’s a homogeneous population, both in terms of the genetics and in terms of the clinical presentation.”
Preclinical Treatment Approaches
However, there are challenges. Drug delivery to Schwann cells, which insulate axons, is difficult, she said. “The other problem is that we want to avoid overly silencing PMP22 because that runs the theoretical risk of causing a different condition, HNPP [hereditary neuropathy with liability to pressure palsies]. HNPP is caused by deletions of PMP22, so we want to avoid that situation.”
Mukherjee-Clavin highlighted two RNA therapeutic products that she expects to move from preclinical to clinical research soon.
One is TVR110 by Armatus Bio, a microRNA intrathecal injection product, which aims to reduce PMP22 overexpression. “It targets basically reduces PMP22 mRNA expression and then normalizes the amount of PMP22 protein that is ultimately generated,” she said.
The other therapy, a small interfering RNA intravenous product delivered to Schwann cells, is being developed by DTx Pharma/Novartis.
Outside of the RNA arena, “there are a number of other programs that are in the preclinical phases that I think will be moving through this pipeline,” Mukherjee-Clavin said. “We’ll see if some of these enter first-in-human clinical trials.”
Meanwhile, Saporta highlighted small-molecule strategies that target a subtype of CMT called sorbitol dehydrogenase (SORD) deficiency that’s caused by mutations in the SORD gene. He noted that Applied Therapeutics is testing an investigational drug called govorestat (AT-007) in 56 patients in a double-blind, randomized, placebo-controlled phase 3 registrational study. The company recently reported that interim 12-month results are promising.
Saporta disclosed consulting for DTx Pharma/Novartis, Applied Therapeutics, and Pharnext. Mukherjee-Clavin had no disclosures.
A version of this article first appeared on Medscape.com.
SAVANNAH, GEORGIA — There’s no medical treatment for Charcot-Marie-Tooth (CMT) disease, a debilitating neurologic disorder that’s both progressive and incurable. But now, nerve specialists learned, new potential treatments are moving closer to clinical trials.
neurologists told an audience at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024. But the neurologists also noted challenges, such as determining the best way to track disease progression — which can be slow — and the need to recruit high numbers of patients for trials.
A Common Genetic Neuromuscular Disorder
As Mario Saporta, MD, PhD, MBA, of the University of Miami, Coral Gables, Florida, explained, CMT is the most common genetic neuromuscular disorder, affecting 1 in 2500 people or about 130,000-150,000 in the United States. “Typically, it’s a length-dependent neuropathy, where your longest nerves would be affected earlier and more severely. That’s why we see foot deformities, inverted champagne bottle legs, and hand atrophy.”
Most patients with CMT in the United States have type 1A, which is linked to duplication of the PMP22 gene. All types lead to axonal degeneration, which appears to be the main cause of functional disability, Saporta said. “Patients become weaker and then progress with time, following the degree of axonal generation that they have.”
As many as 150 genes may eventually be deemed to cause CMT. The high number of genetically different forms makes diagnosis and genetic therapy difficult, he said, but that’s just part of the picture. Variations among mutations mean there’s “probably actually over 1000 different diseases” within CMT from a biologic perspective.
Genetic Therapy
In regard to genetic treatment, Bipasha Mukherjee-Clavin, MD, PhD, of Johns Hopkins University School of Medicine, Baltimore, Maryland, said a key factor is whether the patient’s form of CMT is passed on in an autosomal dominant or autosomal recessive manner.
“Autosomal dominant conditions are typically caused by gain of function mutations. So that means the goal of our genetic therapeutic would be to reduce expression of the mutated gene,” she said. “In contrast, autosomal recessive conditions are caused by loss-of-function mutations, which means the goal of our genetic therapeutic would be to replace the mutated gene with a normal, wild-type copy.”
A tool like CRISPR could be used to directly edit the part of the genome with a CMT-causing mutation or a viral vector could deliver a healthy, wild-type copy of a gene, she said. These approaches are both being tested.
Another approach is to reduce expression at the RNA level. “RNA therapeutics are FDA [Food and Drug Administration]–approved for other neuromuscular indications, and you may well be using some of these in your own clinical practice,” she said.
Currently, about seven different projects are in the works on the RNA therapeutics front in CMT, she said, including six focusing on type 1A. Mukherjee-Clavin believes that this subtype is a “great” target because it’s so common, affecting an estimated 1 in 5000 people.
“You actually have enough patients to power a clinical trial,” she said. Also, “it’s a homogeneous population, both in terms of the genetics and in terms of the clinical presentation.”
Preclinical Treatment Approaches
However, there are challenges. Drug delivery to Schwann cells, which insulate axons, is difficult, she said. “The other problem is that we want to avoid overly silencing PMP22 because that runs the theoretical risk of causing a different condition, HNPP [hereditary neuropathy with liability to pressure palsies]. HNPP is caused by deletions of PMP22, so we want to avoid that situation.”
Mukherjee-Clavin highlighted two RNA therapeutic products that she expects to move from preclinical to clinical research soon.
One is TVR110 by Armatus Bio, a microRNA intrathecal injection product, which aims to reduce PMP22 overexpression. “It targets basically reduces PMP22 mRNA expression and then normalizes the amount of PMP22 protein that is ultimately generated,” she said.
The other therapy, a small interfering RNA intravenous product delivered to Schwann cells, is being developed by DTx Pharma/Novartis.
Outside of the RNA arena, “there are a number of other programs that are in the preclinical phases that I think will be moving through this pipeline,” Mukherjee-Clavin said. “We’ll see if some of these enter first-in-human clinical trials.”
Meanwhile, Saporta highlighted small-molecule strategies that target a subtype of CMT called sorbitol dehydrogenase (SORD) deficiency that’s caused by mutations in the SORD gene. He noted that Applied Therapeutics is testing an investigational drug called govorestat (AT-007) in 56 patients in a double-blind, randomized, placebo-controlled phase 3 registrational study. The company recently reported that interim 12-month results are promising.
Saporta disclosed consulting for DTx Pharma/Novartis, Applied Therapeutics, and Pharnext. Mukherjee-Clavin had no disclosures.
A version of this article first appeared on Medscape.com.
FROM AANEM 2024
Sustained Control with Investigational Monoclonal Antibody for Myasthenia Gravis
SAVANNAH, GEORGIA – , according to topline results from the phase 3 VIVACITY-MG3 study.
The VIVACITY-MG3 trial is the first registrational study of a neonatal fragment crystallizable receptor (FcRn) blocker to show sustained efficacy through 6 months of fixed schedule dosing.
Lead investigator Tuan Vu, MD, professor of neurology at the University of South Florida in Tampa, presented the findings at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Autoantibody Depletion
FcRN plays a crucial role in the transport of immunoglobulin G. Blocking it can reduce circulating immunoglobulin G antibodies, including pathogenic gMG autoantibodies.
The double-blind, placebo-controlled trial included 196 adults with a broad range of seropositive gMG – who account for approximately 95% of the gMG patient population – and 42 seronegative patients.
The mean age was 52 years, 92% were female, and 63% were White. The mean disease duration was about 8 years. Among seropositive patients, 87.6% were acetylcholine receptor autoantibody-positive (AChR+), 10.5% were muscle-specific kinase autoantibody-positive (MuSK+), and 2% were low-density lipoprotein receptor-related protein 4 antibody positive.
They were randomly assigned 1:1 to receive either nipocalimab IV plus standard of care, or placebo plus standard of care for 24 weeks. A total of 87 patients in the nipocalimab arm and 82 in the placebo arm completed the study.
The primary efficacy endpoint was the Myasthenia Gravis Activities of Daily Living (MG-ADL) score. Participants treated with nipocalimab demonstrated a statistically significant improvement of 4.70 points from baseline, compared to the 3.25-point improvement in those treated with placebo (P =.002).
Clinically Meaningful Changes?
“For someone living with gMG, a 1 to 2-point improvement on MG-ADL may be the difference between normal eating and frequent choking on food, or shortness of breath at rest and being on a ventilator,” the drug’s manufacturer noted in a release.
Secondary endpoints were also better in the nipocalimab group, compared with participants on placebo. Specifically, on the 13-item clinician assessed Quantitative Myasthenia Gravis disease severity score, patients who received nipocalimab had an average reduction of 4.86 points from baseline compared to a reduction of 2.05 points in the placebo arm (P <.001).
Similarly, MG-ADL response (defined as ≥ 2-point improvement from baseline) was significantly greater in the nipocalimab versus placebo arms (68.8% vs 52.6%; P =.021).
Subgroup analysis revealed similar results for the different types of seropositive patients, but there was no statistically significant difference in results for seronegative patients treated with nipocalimab versus placebo.
“The drug was pretty well tolerated and there was little difference, other than more patients with muscle spasm in the nipocalimab group (12.2% vs 3.1%),” said Vu.
In addition, peripheral edema occurred in 11.2% of the nipocalimab group and none of the placebo-treated patients. Cholesterol levels were also higher in the nipocalimab arm, but there were no cardiac side effects, he added.
Encouraging Findings
Commenting on the findings, Neelam Goyal, MD, clinical professor of neurology and neurological sciences at Stanford University School of Medicine in Palo Alto, California, was encouraged.
“It’s a phase 3 trial, it’s positive, which is great, so it’ll be another drug on the market, another option for our patients,” she said. However, she cautioned, “their placebo arm did better than most placebos, so I think the delta is not as robust, but it was still statistically significant.”
Goyal noted that, if approved, nipocalimab will be the third FcRn inhibitor in the MG field, preceded by efgartigimod (Vyvgart), which is approved for AChR antibody-positive disease, and rozanolixizumab-noli (Rystiggo) which is approved for both for AChR and MUSK antibody positive disease.
“Its target of action is similar to the two drugs that are already on the market, but one thing that is unique about nipocalimab is that it is continuous dosing versus the other two medications that are given cyclically,” she said.
“The reason that’s an upside, is that with cyclical dosing, patients have a return of symptoms. We treat, they get better, and then they get worse. That’s very disconcerting to patients. So, they want to be treated continuously.”
Additionally, she said there are some early data suggesting its safety in pregnancy.
Vu disclosed he is the USF Site Principal Investigator for MG clinical trials sponsored by Alexion/ AstraZeneca Rare Disease, Amgen, argenx, Cartesian Therapeutics, COUR Pharmaceuticals, Dianthus Therapeutics, Immunovant, Johnson & Johnson, NMD Pharmaceuticals, Regeneron Pharmaceuticals, and UCB, and has served as a speaker for Alexion/AstraZeneca Rare Disease, argenx, and CSL Behring. He performs consulting work for Alexion/AstraZeneca Rare Disease, argenx, Dianthus Therapeutics, ImmunAbs, and UCB. Goyal disclosed consultant, advisory or grant support from argenx, UCB, Alexion, and Janssen. The study was funded by Janssen.
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA – , according to topline results from the phase 3 VIVACITY-MG3 study.
The VIVACITY-MG3 trial is the first registrational study of a neonatal fragment crystallizable receptor (FcRn) blocker to show sustained efficacy through 6 months of fixed schedule dosing.
Lead investigator Tuan Vu, MD, professor of neurology at the University of South Florida in Tampa, presented the findings at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Autoantibody Depletion
FcRN plays a crucial role in the transport of immunoglobulin G. Blocking it can reduce circulating immunoglobulin G antibodies, including pathogenic gMG autoantibodies.
The double-blind, placebo-controlled trial included 196 adults with a broad range of seropositive gMG – who account for approximately 95% of the gMG patient population – and 42 seronegative patients.
The mean age was 52 years, 92% were female, and 63% were White. The mean disease duration was about 8 years. Among seropositive patients, 87.6% were acetylcholine receptor autoantibody-positive (AChR+), 10.5% were muscle-specific kinase autoantibody-positive (MuSK+), and 2% were low-density lipoprotein receptor-related protein 4 antibody positive.
They were randomly assigned 1:1 to receive either nipocalimab IV plus standard of care, or placebo plus standard of care for 24 weeks. A total of 87 patients in the nipocalimab arm and 82 in the placebo arm completed the study.
The primary efficacy endpoint was the Myasthenia Gravis Activities of Daily Living (MG-ADL) score. Participants treated with nipocalimab demonstrated a statistically significant improvement of 4.70 points from baseline, compared to the 3.25-point improvement in those treated with placebo (P =.002).
Clinically Meaningful Changes?
“For someone living with gMG, a 1 to 2-point improvement on MG-ADL may be the difference between normal eating and frequent choking on food, or shortness of breath at rest and being on a ventilator,” the drug’s manufacturer noted in a release.
Secondary endpoints were also better in the nipocalimab group, compared with participants on placebo. Specifically, on the 13-item clinician assessed Quantitative Myasthenia Gravis disease severity score, patients who received nipocalimab had an average reduction of 4.86 points from baseline compared to a reduction of 2.05 points in the placebo arm (P <.001).
Similarly, MG-ADL response (defined as ≥ 2-point improvement from baseline) was significantly greater in the nipocalimab versus placebo arms (68.8% vs 52.6%; P =.021).
Subgroup analysis revealed similar results for the different types of seropositive patients, but there was no statistically significant difference in results for seronegative patients treated with nipocalimab versus placebo.
“The drug was pretty well tolerated and there was little difference, other than more patients with muscle spasm in the nipocalimab group (12.2% vs 3.1%),” said Vu.
In addition, peripheral edema occurred in 11.2% of the nipocalimab group and none of the placebo-treated patients. Cholesterol levels were also higher in the nipocalimab arm, but there were no cardiac side effects, he added.
Encouraging Findings
Commenting on the findings, Neelam Goyal, MD, clinical professor of neurology and neurological sciences at Stanford University School of Medicine in Palo Alto, California, was encouraged.
“It’s a phase 3 trial, it’s positive, which is great, so it’ll be another drug on the market, another option for our patients,” she said. However, she cautioned, “their placebo arm did better than most placebos, so I think the delta is not as robust, but it was still statistically significant.”
Goyal noted that, if approved, nipocalimab will be the third FcRn inhibitor in the MG field, preceded by efgartigimod (Vyvgart), which is approved for AChR antibody-positive disease, and rozanolixizumab-noli (Rystiggo) which is approved for both for AChR and MUSK antibody positive disease.
“Its target of action is similar to the two drugs that are already on the market, but one thing that is unique about nipocalimab is that it is continuous dosing versus the other two medications that are given cyclically,” she said.
“The reason that’s an upside, is that with cyclical dosing, patients have a return of symptoms. We treat, they get better, and then they get worse. That’s very disconcerting to patients. So, they want to be treated continuously.”
Additionally, she said there are some early data suggesting its safety in pregnancy.
Vu disclosed he is the USF Site Principal Investigator for MG clinical trials sponsored by Alexion/ AstraZeneca Rare Disease, Amgen, argenx, Cartesian Therapeutics, COUR Pharmaceuticals, Dianthus Therapeutics, Immunovant, Johnson & Johnson, NMD Pharmaceuticals, Regeneron Pharmaceuticals, and UCB, and has served as a speaker for Alexion/AstraZeneca Rare Disease, argenx, and CSL Behring. He performs consulting work for Alexion/AstraZeneca Rare Disease, argenx, Dianthus Therapeutics, ImmunAbs, and UCB. Goyal disclosed consultant, advisory or grant support from argenx, UCB, Alexion, and Janssen. The study was funded by Janssen.
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA – , according to topline results from the phase 3 VIVACITY-MG3 study.
The VIVACITY-MG3 trial is the first registrational study of a neonatal fragment crystallizable receptor (FcRn) blocker to show sustained efficacy through 6 months of fixed schedule dosing.
Lead investigator Tuan Vu, MD, professor of neurology at the University of South Florida in Tampa, presented the findings at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Autoantibody Depletion
FcRN plays a crucial role in the transport of immunoglobulin G. Blocking it can reduce circulating immunoglobulin G antibodies, including pathogenic gMG autoantibodies.
The double-blind, placebo-controlled trial included 196 adults with a broad range of seropositive gMG – who account for approximately 95% of the gMG patient population – and 42 seronegative patients.
The mean age was 52 years, 92% were female, and 63% were White. The mean disease duration was about 8 years. Among seropositive patients, 87.6% were acetylcholine receptor autoantibody-positive (AChR+), 10.5% were muscle-specific kinase autoantibody-positive (MuSK+), and 2% were low-density lipoprotein receptor-related protein 4 antibody positive.
They were randomly assigned 1:1 to receive either nipocalimab IV plus standard of care, or placebo plus standard of care for 24 weeks. A total of 87 patients in the nipocalimab arm and 82 in the placebo arm completed the study.
The primary efficacy endpoint was the Myasthenia Gravis Activities of Daily Living (MG-ADL) score. Participants treated with nipocalimab demonstrated a statistically significant improvement of 4.70 points from baseline, compared to the 3.25-point improvement in those treated with placebo (P =.002).
Clinically Meaningful Changes?
“For someone living with gMG, a 1 to 2-point improvement on MG-ADL may be the difference between normal eating and frequent choking on food, or shortness of breath at rest and being on a ventilator,” the drug’s manufacturer noted in a release.
Secondary endpoints were also better in the nipocalimab group, compared with participants on placebo. Specifically, on the 13-item clinician assessed Quantitative Myasthenia Gravis disease severity score, patients who received nipocalimab had an average reduction of 4.86 points from baseline compared to a reduction of 2.05 points in the placebo arm (P <.001).
Similarly, MG-ADL response (defined as ≥ 2-point improvement from baseline) was significantly greater in the nipocalimab versus placebo arms (68.8% vs 52.6%; P =.021).
Subgroup analysis revealed similar results for the different types of seropositive patients, but there was no statistically significant difference in results for seronegative patients treated with nipocalimab versus placebo.
“The drug was pretty well tolerated and there was little difference, other than more patients with muscle spasm in the nipocalimab group (12.2% vs 3.1%),” said Vu.
In addition, peripheral edema occurred in 11.2% of the nipocalimab group and none of the placebo-treated patients. Cholesterol levels were also higher in the nipocalimab arm, but there were no cardiac side effects, he added.
Encouraging Findings
Commenting on the findings, Neelam Goyal, MD, clinical professor of neurology and neurological sciences at Stanford University School of Medicine in Palo Alto, California, was encouraged.
“It’s a phase 3 trial, it’s positive, which is great, so it’ll be another drug on the market, another option for our patients,” she said. However, she cautioned, “their placebo arm did better than most placebos, so I think the delta is not as robust, but it was still statistically significant.”
Goyal noted that, if approved, nipocalimab will be the third FcRn inhibitor in the MG field, preceded by efgartigimod (Vyvgart), which is approved for AChR antibody-positive disease, and rozanolixizumab-noli (Rystiggo) which is approved for both for AChR and MUSK antibody positive disease.
“Its target of action is similar to the two drugs that are already on the market, but one thing that is unique about nipocalimab is that it is continuous dosing versus the other two medications that are given cyclically,” she said.
“The reason that’s an upside, is that with cyclical dosing, patients have a return of symptoms. We treat, they get better, and then they get worse. That’s very disconcerting to patients. So, they want to be treated continuously.”
Additionally, she said there are some early data suggesting its safety in pregnancy.
Vu disclosed he is the USF Site Principal Investigator for MG clinical trials sponsored by Alexion/ AstraZeneca Rare Disease, Amgen, argenx, Cartesian Therapeutics, COUR Pharmaceuticals, Dianthus Therapeutics, Immunovant, Johnson & Johnson, NMD Pharmaceuticals, Regeneron Pharmaceuticals, and UCB, and has served as a speaker for Alexion/AstraZeneca Rare Disease, argenx, and CSL Behring. He performs consulting work for Alexion/AstraZeneca Rare Disease, argenx, Dianthus Therapeutics, ImmunAbs, and UCB. Goyal disclosed consultant, advisory or grant support from argenx, UCB, Alexion, and Janssen. The study was funded by Janssen.
A version of this article appeared on Medscape.com.
FROM AANEM 2024
First-in-Class B-Cell Depleting Agent Promising for Myasthenia Gravis
SAVANNAH, GEORGIA — , new phase 3 data showed.
“Based on these results, we have demonstrated that targeting B cells, including the antibody-secreting cells, is beneficial, and there is likely a role for this kind of therapeutic strategy for patients with myasthenia gravis,” said senior investigator Richard Nowak, MD.
The findings were published and presented at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Largest Cohort of Muscle-Specific Kinase (MuSK) Antibody–Positive Disease
The Myasthenia Gravis INebilizumab Trial study enrolled 238 participants, 60.8% women, mean age 47.5 years, from 79 sites in 18 countries. The participants were divided into two cohorts: 190 acetylcholine receptor (AChR) autoantibody–positive patients and 48 MuSK autoantibody–positive patients.
“This is the largest enrolled cohort of MuSK antibody–positive disease in a placebo-controlled trial to date,” said Nowak, director of the Yale Myasthenia Gravis Clinic and associate professor of neurology at Yale School of Medicine, in New Haven, Connecticut.
Both groups had similar gMG duration (mean 6.7 and 5.2 years for AChR+ and MuSK+ patients, respectively) and disease severity based on Myasthenia Gravis Activities of Daily Living (MG-ADL) and Quantitative Myasthenia Gravis (QMG) baseline score. In addition, more than 80% of participants were on a prednisone equivalent dose greater than 5 mg daily at study entry.
Participants were randomly assigned to receive intravenous (IV) inebilizumab or IV placebo for 52 weeks (AChR+ group) or 26 weeks (MuSK+ group). In addition, study participants who were taking corticosteroids were tapered down starting at week 4 to prednisone 5 mg per day by week 24.
The trial met its primary endpoint, with a statistically significant change from baseline in MG-ADL and with a reduction of 4.2 points for inebilizumab versus 2.2 for placebo (P < .0001) at week 26 for the combined study population.
“You can see that the trend is actually going toward separation of the two groups after week 8 in the combined population,” said Nowak. Key secondary endpoints also showed statistically significant and clinically meaningful change from baseline compared with placebo.
This included a statistically significant change in QMG score inebilizumab compared with placebo for the combined population, a reduction of 4.8 versus 2.3 points, respectively, at week 26 (P = .0002).
In addition, both MG-ADL and QMG scores in the AChR+ subgroup were superior for inebilizumab versus placebo at week 26, with reductions of 4.2 versus 2.4, and 4.4 versus 2.0; P = .0015 and P = .0011, respectively.
In the MuSK+ subgroup, inebilizumab-treated patients had better MG-ADL scores than placebo-treated patients, with reductions of 3.9 versus 1.7 points, respectively, at week 26, although this difference did not meet statistical significance.
“There were no increased safety incidents in the inebilizumab-treated patients versus placebo, and a similar percentage of safety incidents in the AChR–positive and MuSK–positive groups. There were three deaths reported, all likely related to myasthenic crisis,” he said.
Nowak said that inebilizumab is “unique from the other currently FDA-approved medications for myasthenia gravis in that it’s targeting the upstream immunopathogenic mechanism of disease, specifically B cells — and B cells that are actually antibody-secreting cells.”
“It is targeting the factories of autoantibody production, whereas an FcRn antagonist, for example, is not targeting those factories but rather targeting what’s being produced — the immunoglobulins, IgGs in general,” he added.
Nowak said that what is particularly exciting about the drug is that the schedule is not very frequent. It begins with an initial IV infusion, followed by a second infusion 2 weeks later and a third infusion 6 months after that, so that patients are treated approximately every 6 months. This is in contrast to some other targeted therapies, where failing to address the underlying factors driving immunopathogenesis necessitates more regular and frequent medication administration.
New, Novel, Exciting
Commenting on the research, Neelam Goyal, MD, who chaired the session, said, “It’s definitely new, novel, interesting, exciting.”
Goyal, clinical professor of neurology and neurological sciences at Stanford University School of Medicine in Palo Alto, California, also noted that while B-cell depletion has shown some previous success in MG, it was with rituximab, a CD20 B-cell depleting agent.
She noted that unlike rituximab, which targets CD20, inebilizumab targets CD19, although both medications lead to B-cell depletion. Rituximab has proven effective for MUSK–positive MG, which accounts for approximately 5% of cases.
However, Goyal noted that the results for AChR–positive MG have been mixed — “the BeatMG trial was negative and the RINOMAX trial was positive. So, I think this is really interesting. It is exciting, and this drug is already on the market.”
She added that although inebilizumab is already US Food and Drug Administration–approved for the treatment of neuromyelitis optica, it still faces approval and indication hurdles for MG.
The future of this drug in the management algorithm for MG remains uncertain. Goyal noted that it’s “quite costly,” and although its benefits are evident — particularly for FcRn and complement inhibitors — some early data from chimeric antigen receptor T-cell therapy studies appear significantly more impressive.
Nowak disclosed research support from the National Institutes of Health, Genentech, Alexion Pharmaceuticals, argenx, Annexon Biosciences, Ra Pharmaceuticals (now UCB S.A.), the Myasthenia Gravis Foundation of America, Momenta Pharmaceuticals (now Janssen), Immunovant, Grifols, S.A., and Viela Bio, Horizon Therapeutics (now Amgen). Served as a consultant and advisor for Alexion Pharmaceuticals, argenx, Cabaletta Bio, Cour Pharmaceuticals, Ra Pharmaceuticals (now UCB S.A.), Immunovant, Momenta Pharmaceuticals (now Janssen), and Viela Bio (Horizon Therapeutics, now Amgen).
Goyal disclosed consultant, advisory, or grant support from argenx, UCB, Alexion, and Janssen. The study was funded by Amgen.
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA — , new phase 3 data showed.
“Based on these results, we have demonstrated that targeting B cells, including the antibody-secreting cells, is beneficial, and there is likely a role for this kind of therapeutic strategy for patients with myasthenia gravis,” said senior investigator Richard Nowak, MD.
The findings were published and presented at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Largest Cohort of Muscle-Specific Kinase (MuSK) Antibody–Positive Disease
The Myasthenia Gravis INebilizumab Trial study enrolled 238 participants, 60.8% women, mean age 47.5 years, from 79 sites in 18 countries. The participants were divided into two cohorts: 190 acetylcholine receptor (AChR) autoantibody–positive patients and 48 MuSK autoantibody–positive patients.
“This is the largest enrolled cohort of MuSK antibody–positive disease in a placebo-controlled trial to date,” said Nowak, director of the Yale Myasthenia Gravis Clinic and associate professor of neurology at Yale School of Medicine, in New Haven, Connecticut.
Both groups had similar gMG duration (mean 6.7 and 5.2 years for AChR+ and MuSK+ patients, respectively) and disease severity based on Myasthenia Gravis Activities of Daily Living (MG-ADL) and Quantitative Myasthenia Gravis (QMG) baseline score. In addition, more than 80% of participants were on a prednisone equivalent dose greater than 5 mg daily at study entry.
Participants were randomly assigned to receive intravenous (IV) inebilizumab or IV placebo for 52 weeks (AChR+ group) or 26 weeks (MuSK+ group). In addition, study participants who were taking corticosteroids were tapered down starting at week 4 to prednisone 5 mg per day by week 24.
The trial met its primary endpoint, with a statistically significant change from baseline in MG-ADL and with a reduction of 4.2 points for inebilizumab versus 2.2 for placebo (P < .0001) at week 26 for the combined study population.
“You can see that the trend is actually going toward separation of the two groups after week 8 in the combined population,” said Nowak. Key secondary endpoints also showed statistically significant and clinically meaningful change from baseline compared with placebo.
This included a statistically significant change in QMG score inebilizumab compared with placebo for the combined population, a reduction of 4.8 versus 2.3 points, respectively, at week 26 (P = .0002).
In addition, both MG-ADL and QMG scores in the AChR+ subgroup were superior for inebilizumab versus placebo at week 26, with reductions of 4.2 versus 2.4, and 4.4 versus 2.0; P = .0015 and P = .0011, respectively.
In the MuSK+ subgroup, inebilizumab-treated patients had better MG-ADL scores than placebo-treated patients, with reductions of 3.9 versus 1.7 points, respectively, at week 26, although this difference did not meet statistical significance.
“There were no increased safety incidents in the inebilizumab-treated patients versus placebo, and a similar percentage of safety incidents in the AChR–positive and MuSK–positive groups. There were three deaths reported, all likely related to myasthenic crisis,” he said.
Nowak said that inebilizumab is “unique from the other currently FDA-approved medications for myasthenia gravis in that it’s targeting the upstream immunopathogenic mechanism of disease, specifically B cells — and B cells that are actually antibody-secreting cells.”
“It is targeting the factories of autoantibody production, whereas an FcRn antagonist, for example, is not targeting those factories but rather targeting what’s being produced — the immunoglobulins, IgGs in general,” he added.
Nowak said that what is particularly exciting about the drug is that the schedule is not very frequent. It begins with an initial IV infusion, followed by a second infusion 2 weeks later and a third infusion 6 months after that, so that patients are treated approximately every 6 months. This is in contrast to some other targeted therapies, where failing to address the underlying factors driving immunopathogenesis necessitates more regular and frequent medication administration.
New, Novel, Exciting
Commenting on the research, Neelam Goyal, MD, who chaired the session, said, “It’s definitely new, novel, interesting, exciting.”
Goyal, clinical professor of neurology and neurological sciences at Stanford University School of Medicine in Palo Alto, California, also noted that while B-cell depletion has shown some previous success in MG, it was with rituximab, a CD20 B-cell depleting agent.
She noted that unlike rituximab, which targets CD20, inebilizumab targets CD19, although both medications lead to B-cell depletion. Rituximab has proven effective for MUSK–positive MG, which accounts for approximately 5% of cases.
However, Goyal noted that the results for AChR–positive MG have been mixed — “the BeatMG trial was negative and the RINOMAX trial was positive. So, I think this is really interesting. It is exciting, and this drug is already on the market.”
She added that although inebilizumab is already US Food and Drug Administration–approved for the treatment of neuromyelitis optica, it still faces approval and indication hurdles for MG.
The future of this drug in the management algorithm for MG remains uncertain. Goyal noted that it’s “quite costly,” and although its benefits are evident — particularly for FcRn and complement inhibitors — some early data from chimeric antigen receptor T-cell therapy studies appear significantly more impressive.
Nowak disclosed research support from the National Institutes of Health, Genentech, Alexion Pharmaceuticals, argenx, Annexon Biosciences, Ra Pharmaceuticals (now UCB S.A.), the Myasthenia Gravis Foundation of America, Momenta Pharmaceuticals (now Janssen), Immunovant, Grifols, S.A., and Viela Bio, Horizon Therapeutics (now Amgen). Served as a consultant and advisor for Alexion Pharmaceuticals, argenx, Cabaletta Bio, Cour Pharmaceuticals, Ra Pharmaceuticals (now UCB S.A.), Immunovant, Momenta Pharmaceuticals (now Janssen), and Viela Bio (Horizon Therapeutics, now Amgen).
Goyal disclosed consultant, advisory, or grant support from argenx, UCB, Alexion, and Janssen. The study was funded by Amgen.
A version of this article appeared on Medscape.com.
SAVANNAH, GEORGIA — , new phase 3 data showed.
“Based on these results, we have demonstrated that targeting B cells, including the antibody-secreting cells, is beneficial, and there is likely a role for this kind of therapeutic strategy for patients with myasthenia gravis,” said senior investigator Richard Nowak, MD.
The findings were published and presented at the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) 2024.
Largest Cohort of Muscle-Specific Kinase (MuSK) Antibody–Positive Disease
The Myasthenia Gravis INebilizumab Trial study enrolled 238 participants, 60.8% women, mean age 47.5 years, from 79 sites in 18 countries. The participants were divided into two cohorts: 190 acetylcholine receptor (AChR) autoantibody–positive patients and 48 MuSK autoantibody–positive patients.
“This is the largest enrolled cohort of MuSK antibody–positive disease in a placebo-controlled trial to date,” said Nowak, director of the Yale Myasthenia Gravis Clinic and associate professor of neurology at Yale School of Medicine, in New Haven, Connecticut.
Both groups had similar gMG duration (mean 6.7 and 5.2 years for AChR+ and MuSK+ patients, respectively) and disease severity based on Myasthenia Gravis Activities of Daily Living (MG-ADL) and Quantitative Myasthenia Gravis (QMG) baseline score. In addition, more than 80% of participants were on a prednisone equivalent dose greater than 5 mg daily at study entry.
Participants were randomly assigned to receive intravenous (IV) inebilizumab or IV placebo for 52 weeks (AChR+ group) or 26 weeks (MuSK+ group). In addition, study participants who were taking corticosteroids were tapered down starting at week 4 to prednisone 5 mg per day by week 24.
The trial met its primary endpoint, with a statistically significant change from baseline in MG-ADL and with a reduction of 4.2 points for inebilizumab versus 2.2 for placebo (P < .0001) at week 26 for the combined study population.
“You can see that the trend is actually going toward separation of the two groups after week 8 in the combined population,” said Nowak. Key secondary endpoints also showed statistically significant and clinically meaningful change from baseline compared with placebo.
This included a statistically significant change in QMG score inebilizumab compared with placebo for the combined population, a reduction of 4.8 versus 2.3 points, respectively, at week 26 (P = .0002).
In addition, both MG-ADL and QMG scores in the AChR+ subgroup were superior for inebilizumab versus placebo at week 26, with reductions of 4.2 versus 2.4, and 4.4 versus 2.0; P = .0015 and P = .0011, respectively.
In the MuSK+ subgroup, inebilizumab-treated patients had better MG-ADL scores than placebo-treated patients, with reductions of 3.9 versus 1.7 points, respectively, at week 26, although this difference did not meet statistical significance.
“There were no increased safety incidents in the inebilizumab-treated patients versus placebo, and a similar percentage of safety incidents in the AChR–positive and MuSK–positive groups. There were three deaths reported, all likely related to myasthenic crisis,” he said.
Nowak said that inebilizumab is “unique from the other currently FDA-approved medications for myasthenia gravis in that it’s targeting the upstream immunopathogenic mechanism of disease, specifically B cells — and B cells that are actually antibody-secreting cells.”
“It is targeting the factories of autoantibody production, whereas an FcRn antagonist, for example, is not targeting those factories but rather targeting what’s being produced — the immunoglobulins, IgGs in general,” he added.
Nowak said that what is particularly exciting about the drug is that the schedule is not very frequent. It begins with an initial IV infusion, followed by a second infusion 2 weeks later and a third infusion 6 months after that, so that patients are treated approximately every 6 months. This is in contrast to some other targeted therapies, where failing to address the underlying factors driving immunopathogenesis necessitates more regular and frequent medication administration.
New, Novel, Exciting
Commenting on the research, Neelam Goyal, MD, who chaired the session, said, “It’s definitely new, novel, interesting, exciting.”
Goyal, clinical professor of neurology and neurological sciences at Stanford University School of Medicine in Palo Alto, California, also noted that while B-cell depletion has shown some previous success in MG, it was with rituximab, a CD20 B-cell depleting agent.
She noted that unlike rituximab, which targets CD20, inebilizumab targets CD19, although both medications lead to B-cell depletion. Rituximab has proven effective for MUSK–positive MG, which accounts for approximately 5% of cases.
However, Goyal noted that the results for AChR–positive MG have been mixed — “the BeatMG trial was negative and the RINOMAX trial was positive. So, I think this is really interesting. It is exciting, and this drug is already on the market.”
She added that although inebilizumab is already US Food and Drug Administration–approved for the treatment of neuromyelitis optica, it still faces approval and indication hurdles for MG.
The future of this drug in the management algorithm for MG remains uncertain. Goyal noted that it’s “quite costly,” and although its benefits are evident — particularly for FcRn and complement inhibitors — some early data from chimeric antigen receptor T-cell therapy studies appear significantly more impressive.
Nowak disclosed research support from the National Institutes of Health, Genentech, Alexion Pharmaceuticals, argenx, Annexon Biosciences, Ra Pharmaceuticals (now UCB S.A.), the Myasthenia Gravis Foundation of America, Momenta Pharmaceuticals (now Janssen), Immunovant, Grifols, S.A., and Viela Bio, Horizon Therapeutics (now Amgen). Served as a consultant and advisor for Alexion Pharmaceuticals, argenx, Cabaletta Bio, Cour Pharmaceuticals, Ra Pharmaceuticals (now UCB S.A.), Immunovant, Momenta Pharmaceuticals (now Janssen), and Viela Bio (Horizon Therapeutics, now Amgen).
Goyal disclosed consultant, advisory, or grant support from argenx, UCB, Alexion, and Janssen. The study was funded by Amgen.
A version of this article appeared on Medscape.com.
FROM AANEM 2024
Myasthenia Gravis: Patient Choice, Cultural Change
Used appropriately, newer treatments can provide dramatic results faster and more safely than broad immunosuppressants. However, according to experts, payers’ willingness to cover costly new therapies remains a work in progress.
The availability of more effective treatments with fewer side effects has brought about a cultural shift, said James F. Howard, Jr, MD. “The physician’s goal now is for the patient to be symptom free with grade 1 or less adverse events. And patients are demanding freedom from all the side effects that our usual course of immune therapy produces.” Dr. Howard is professor of neurology, medicine and allied health and director of the Myasthenia Gravis Clinical Trials and Translational Research Program at the University of North Carolina at Chapel Hill.
The shift has been long in coming. Although myasthenia gravis was identified in the mid-1600s, it took more than 340 years to get the first drug approved specifically for the disorder.
Worldwide prevalence estimates vary widely, from less than 200,000 to 700,000 cases.1,2 Pathophysiologically, myasthenia gravis stems from autoimmune destruction of neuromuscular junctions (NMJs), which transmit motor neuron impulses to muscle fibers.1 Symptoms include variable skeletal muscle weakness that can range from mild and transient to life-threatening.
In approximately 80% of cases, autoimmune antibodies target the postsynaptic acetylcholine receptor (AChR). Additional autoimmune targets mainly include muscle-specific kinase (MuSK) and lipoprotein receptor-related protein 4 (LRP4). However, around 10% of patients are seronegative, lacking autoantibodies detectable through conventional radioimmunoassays. Clinical disease does not always correspond with circulating antibody levels, and pathogenesis may require cooperation between multiple autoantibodies attacking the same target.3 Around 10% of MG cases are associated with thymomas.
Among myasthenia gravis treatments, immunosuppressants typically take 4-10 months to begin working and 18-36 months for maximum benefit. “Our new targeted therapies work within 1-2 weeks, with maximum improvement occurring somewhere between 8 and 12 weeks,” Dr. Howard said. Quick onset makes these drugs well suited for primary therapy in recalcitrant myasthenia gravis or as bridges to standard immunotherapy. Targeted drugs also appear to provide effective rescue therapy, although head-to-head studies are needed.
Complement Inhibition
In AChR antibody–positive myasthenia gravis, autoantibody binding with the postsynaptic AChR receptor activates complement to attack postsynaptic neuronal membrane. Complement inhibitors approved to date block activation of the terminal complement protein C5.
For many patients, complement inhibitors deliver dramatic results. Henry J. Kaminski, MD, said that the first patient for whom he prescribed a complement inhibitor outside a clinical trial went from being miserable to traveling internationally within a month. Dr. Kaminski is Meta A. Neumann Professor of Neurology at George Washington University, Washington, DC.
Eculizumab (Soliris, Alexion), earned Food and Drug Administration (FDA) approval for myasthenia gravis in 2017. Week 26 results in the phase 3 REGAIN trial showed no significant difference in Myasthenia Gravis–Activities of Daily Living (MG-ADL) scores between treatment and placebo. However, said Dr. Howard, primary investigator on the study, the negative result was a statistical aberration stemming from the FDA’s requirement to use worst-rank analysis rather than absolute change scores. What got eculizumab approved were highly positive results in the overwhelming majority of secondary endpoints.4 Subsequently, the FDA had the manufacturer rewrite the package insert using common statistical methods, which yielded positive primary results.
Ravulizumab (Ultomiris, Alexion), approved for myasthenia gravis in 2022, reduces eculizumab’s twice-monthly intravenous dosing to every 2 months (after loading doses), with very similar efficacy. The newest complement inhibitor, zilucoplan (Zilbrysq, UCB), administered once daily subcutaneously, earned FDA approval in 2023. Daily subcutaneous dosing provides patient convenience, said Dr. Howard. Because the body does not clear this small molecule as it would a full-size antibody, it is the only complement inhibitor that can be combined with a fragment crystallizable neonatal receptor (FcRn) inhibitor.
FcRn Inhibition
The FcRn exists on the surface and intracellular vesicles of many cells, including B cells, but not T cells.5FcRn inhibitors block binding of circulating IgG antibodies to the FcRn, preventing their normal recycling, significantly reducing circulating antibodies within days of treatment.
Efgartigimod (Vyvgart, Argenx), earned FDA approval in intravenous form in 2021, followed by a subcutaneous formulation that includes hyaluronidase (Vyvgart Hytrulo) in 2023. Rozanolixizumab (Rystiggo, UCB) earned FDA approval for both AChR antibody–positive and MuSK antibody–positive myasthenia gravis in 2023.
Along with rapid response, said Dr. Howard, complement inhibitors and FcRn inhibitors offer a “hugely improved” side-effect profile. In phase 3 research, the most common side effects for both classes included headache, nausea, and diarrhea.4,6,7 Because complement inhibitors increase the risk of Neisseria infection, users require immunization against meningococcal infection (or concurrent antibiotic prophylaxis) while on complement inhibitors.
Insurance Issues
With many clinicians wondering which targeted therapy to choose for a particular patient, said Dr. Howard and Dr. Kaminski, the main obstacle to wider use of these treatments is payer attitudes and practices. “While many of us would like to see these drugs used earlier in the course of disease,” Dr. Howard explained, “there are numerous restrictions placed on the physician and the patient by whatever insurance the individual has.”
Dr. Kaminski said: “There’s a lot of variability among insurance companies regarding what is expected in terms of getting approval for a certain medication. It frustrates me, thinking this patient may do well with a complement inhibitor or an FcRn inhibitor, but it takes weeks to get them approved.”
Some of his patients have been approved for, and flourished on, complement inhibitors and FcRn inhibitors, he added, and then denied a second round of treatment. Dr. Kaminski said he does not know why these patients were denied, and every time he requests reevaluation, the decision is reversed. “That’s a significant time frame for me and my staff to manage.”
When asked what can be done to address high drug prices, Dr. Howard replied, “I have no idea. I’m not an advocate of high drug prices. But I don’t think people realize the cost of doing clinical trials, which is hundreds of millions of dollars, particularly in rare diseases.”
Presently, Dr. Howard said, FcRn inhibitors are used more frequently than complement inhibitors solely because of cost. Zilucoplan will be priced below existing complement inhibitors, although it is too soon to compare its price with those of FcRn inhibitors.
When eculizumab debuted, said Dr. Howard, it cost nearly $750,000 annually. “But if you look at the number of patients treated, the cost of the drug over this population is probably less than the cost for using a cholesterol-lowering agent to treat hyperlipidemia.”
An Institute for Clinical and Economic Review (ICER) report stated that eculizumab and efgartigimod should both cost less than $20,000 annually to meet commonly used cost-effectiveness thresholds.8 However, Dr. Howard said ICER used models based on common diseases and ignored the economic impact of patients’ losing fewer workdays and avoiding long-term immunosuppressant side effects such as diabetes and osteoporosis and related treatment costs. “We’ve got to start looking at total societal cost,” he said.
Leapfrogging Ahead
Not all the new drugs work in every indicated patient, Dr. Howard said. For example, up to 30% of patients do not respond to complement inhibitors. “We don’t understand why. It’s as if we have leapfrogged way ahead in terms of therapeutics, and now we have to go back and answer all the questions – the who, what, where, and why of an individual drug and its response in folks.”
In this climate, said Dr. Kaminski, heavy direct-to-consumer advertising of newer myasthenia gravis therapies creates complications. “My patients are highly excited to see, ‘that’s my disease being advertised on Jeopardy.’ ” Many patients are frustrated with the general lack of awareness regarding myasthenia gravis, he added. “But then I’ve had patients who clearly would never qualify for a certain medication getting mailings to their homes.”
Dr. Howard countered that broader awareness of myasthenia gravis can only help. “There’s increasing recognition of the disease, not only by patients, but to some extent, by the treating clinician. Patients are coming to our offices and saying, ‘am I a candidate for this new drug?’ It’s the responsibility of the clinician to decide.”
Individual physicians’ practice patterns vary greatly, said Dr. Kaminski, and very little quantitative data exist here. But based on personal communications, academic-center neurologists tend to use targeted treatments on patients who have failed conventional treatments.
Conversely, Dr. Howard said that, because community physicians rarely see myasthenia gravis, and targeted treatments remain relatively new, many of these providers rely on prednisone, azathioprine, and mycophenolate mofetil.
B-Cell Blockers in Development
Overall, said Dr. Howard, the field of myasthenia gravis treatment development is “very rich. And pharma’s interest in myasthenia has taken off like a rocket. It’s exceptionally gratifying to those of us who take care of these patients whose life is miserable” because of adverse effects and/or nonresponse to current drugs.
“In myasthenia,” added Dr. Kaminski, “we know that T cells are promoting the activity of these auto-reactive B cells.” Many drugs currently in phase 2 or 3 development aim to eliminate B cells or signaling between T and B cells, he said. “That’s where most of the drug development is.”
Leading candidates include telitacicept (Tai’ai, RemeGen), which is both a B-lymphocyte stimulator and a proliferation-inducing ligand. A phase 3 trial (NCT05737160) is ongoing, with primary completion expected in late 2026. A second phase 3 trial (NCT06456580) recently began enrolling. Dr. Howard said that, although early results warranted phase 3 analysis, telitacicept’s phase 2 trial was open label and lacked a placebo group.9 The latter is a critical concern because placebo response rates in myasthenia gravis trials average 35%-40%.
Combined with standard care, the FcRn inhibitor nipocalimab (Johnson & Johnson) enabled patients with AChR, MuSK, and/or LRP4 autoantibodies to improve by 4.70 points on the MG-ADL vs 3.25 points for placebo (P = .002) over 24 weeks in phase 3.10All FcRn inhibitors in development can broadly reduce autoantibody levels, said Dr. Howard. “But what role they will play in myasthenia gravis when they’re several years behind leaders in the field in terms of capturing market remains to be seen.”
Additionally, batoclimab (Immunovant/Harbour BioMed) showed positive topline results in phase 3, and an elevated rate of hypercholesterolemia in treated patients that was transient and consistent with previous research.11 Subsequent to efgartigimod, Dr. Howard said, FcRn inhibitors are full-size antibodies. “I believe that contributes to the adverse events that we see. Efgartigimod is a small FcRn fragment. That’s why it’s a cleaner drug, if you will.”
FcRn inhibitors require periodic retreatment. For example, said Dr. Howard, the ADAPT phase 3 trial of efgartigimod, on which he was lead investigator, employed a cyclic dosing schedule – 4 weeks’ treatment, then observation until patients needed retreatment — because patients demanded it.12 In clinical practice, some patients have gone more than 25 weeks before needing retreatment. One of his patients went beyond 40 weeks. “Others only get around 6-9 weeks. So patient choice again enters the decision-making process.”
Rituximab targets the CD20 protein on B cells nonspecifically, producing general immunosuppression. “That’s problematic in producing significant immunosuppression,” said Dr. Kaminski. Nevertheless, he said, rituximab is very effective for most patients with MuSK-specific MG, and its application to this indication has revealed differences between the MuSK subtype and AChR antibody–positive myasthenia. Specifically, MuSK antibody–positive patients have short-lived plasmablasts, which rituximab eliminates.13
Conversely, said Dr. Kaminski, patients with AChR antibody-positive myasthenia, especially long-term, likely have long-lived plasmablasts producing antibodies. This fact, and these patients’ lack of CD20, likely explain their poor response to rituximab.
A phase 3 trial (NCT04524273) of the CD19 blocker inebilizumab (Uplinza, Amgen) reached primary completion in May. Dr. Howard said that if topline results (unreleased at press time) prove positive, inebilizumab could replace rituximab in MG — provided payers do not reject inebilizumab because of cost.
Packed Early-Development Pipeline
Regarding early-stage projects, said Dr. Howard, the pipeline is packed with compounds that target various aspects of the immune system. “The real question with those is, what’s going to be the side effect profile? All of the trials are very early. We need bigger trials with much longer observation for safety, durability, and degree of efficacy.”
The next potential B cell–targeting game changer, he said, is chimeric antigen receptor (CAR) T cell–based therapy. In a phase 2b trial of Descartes-08 (Cartesian Therapeutics), 71% of treated patients experienced clinically meaningful improvement in MG Composite score at 3 months vs 25% for placebo.14
In early clinical trials, said Dr. Howard, patients treated with Descartes-08 — which uses autologous mRNA to target B-cell maturation antigen — have shown “exceptional improvement” lasting 20 or more months. Because the drug is not ingrained permanently into the genome, Descartes-08 avoids potentially severe side effects of DNA-targeting CAR T candidates. Dr. Howard hopes a phase 3 trial will commence around January 2025.
The tolerance approach exemplified by CNP-106 (COUR Pharmaceuticals) and a myasthenia gravis tolerogen (Toleranzia) seeks to prevent the immune system from recognizing and reacting to the NMJ abnormalities that produce myasthenia gravis, potentially providing a cure. “We look forward to those trials as they come online in the next 1-2 years,” said Dr. Howard.
Unmet Needs
Historically, neurologists believed that all myasthenia gravis symptoms stemmed from muscle fatigue — the more active the muscle, the weaker it gets. However, said Dr. Kaminski, some patients might lack measurable weakness but still complain of fatigue.
Elevated levels of cytokines such as interleukin (IL)–6 or IL-17 also can produce fatigue, he noted. “With the drugs we’re using, certainly the new ones, we’re not specifically targeting this fatigue phenomenon, which has been studied in a very limited fashion.”
In the RAISE-XT zilucoplan trial, participants experienced significant improvement in fatigue scores for up to 60 weeks.15 Although zilucoplan does not address fatigue directly, said Dr. Howard, improving myasthenia gravis overall helps reduce fatigue.
The Myasthenia Gravis Symptoms Patient Reported Outcome (MG Symptoms PRO), which Dr. Kaminski helped develop, includes questions designed to distinguish muscular fatigue from overall physical fatigue.16 “I’m very interested in some of the information that’s coming out on long COVID and its effect on muscle,” Dr. Kaminski added. “We might be able to learn from there that there’s still some pathology going on beyond the neuromuscular junction.”
What the field desperately needs, said Dr. Howard, are biomarkers to identify which patients will and will not respond to certain therapeutics. “We’re not there yet.” Such biomarkers are at least 3-7 years from becoming clinical reality.
Promising antibody-independent serum markers include circulating microRNAs. For example, miRNA-150-5p and miRNA-21-5p are elevated in generalized AChR-positive myasthenia gravis and early-onset myasthenia gravis (occurring before age 50) and decline after immunosuppression and thymectomy.17
Among diagnostic modalities for patients with seronegative myasthenia gravis, said Dr. Kaminski, single-fiber EMG is the most sensitive, at approximately 95%. “It’s not perfect.” Moreover, he said, performing this test accurately requires a highly experienced expert, which many treatment centers lack.
Presently, added Dr. Kaminski, orbital MRI is neither specific nor sensitive enough to be clinically useful. “One needs to be careful with these specialized tests that are published from the best laboratory in the world that does the test, and does it repetitively.” As the search for effective myasthenia gravis biomarkers continues, avoiding false-positive results is as important as avoiding false negatives.
References
1. Bubuioc AM et al. J Med Life. 2021 Jan-Mar;14(1):7-16. doi: 10.25122/jml-2020-0145.
2. Deenen JC et al. J Neuromuscul Dis. 2015;2(1):73-85. doi: 10.3233/JND-140045.
3. Kaminski HJ et al. J Clin Invest. 2024 Jun 17;134(12):e179742. doi: 10.1172/JCI179742.
4. Howard JF Jr et al. Lancet Neurol. 2017 Dec;16(12):976-986. doi: 10.1016/S1474-4422(17)30369-1.
5. Huda R. Front Immunol. 2020 Feb 21:11:240. doi: 10.3389/fimmu.2020.00240.
6. Howard JF Jr et al. Lancet Neurol. 2023 May;22(5):395-406. doi: 10.1016/S1474-4422(23)00080-7.
7. Vu T et al. NEJM Evid. 2022 May;1(5):EVIDoa2100066. doi: 10.1056/EVIDoa2100066.
8. Tice JA et al. October 20, 2021. https://icer.org/assessment/myasthenia-gravis/.
9. Yin J et al. Eur J Neurol. 2024 Aug;31(8):e16322. doi: 10.1111/ene.16322.
10. Antozzi C et al. EAN 2024, Abstract EPR-116. https://www.neurology.org/doi/10.1212/WNL.0000000000203660.
11. Yan C et al. JAMA Neurol. 2024 Mar 4;81(4):336-345. doi: 10.1001/jamaneurol.2024.0044.
12. Howard JF Jr et al. Lancet Neurol. 2021 Jul;20(7):526-536. doi: 10.1016/S1474-4422(21)00159-9.
13. Stathopoulos P et al. JCI Insight. 2017 Sep 7;2(17):e94263. doi: 10.1172/jci.insight.94263.
14. Cartesian Therapeutics. Cartesian Therapeutics announces positive topline results from phase 2b trial of Descartes-08 in patients with myasthenia gravis. 2024 Jul 2. https://ir.cartesiantherapeutics.com/news-releases/news-release-details/cartesian-therapeutics-announces-positive-topline-results-phase.
15. Howard JF Jr et al. Ther Adv Neurol Disord. 2024 Apr 17:17:17562864241243186. doi: 10.1177/17562864241243186.
16. Cleanthous S et al. Orphanet J Rare Dis. 2021 Oct 30;16(1):457. doi: 10.1186/s13023-021-02064-0.
17. Sabre L et al. Front Immunol. 2020 Mar 4:11:213. doi: 10.3389/fimmu.2020.00213.
Used appropriately, newer treatments can provide dramatic results faster and more safely than broad immunosuppressants. However, according to experts, payers’ willingness to cover costly new therapies remains a work in progress.
The availability of more effective treatments with fewer side effects has brought about a cultural shift, said James F. Howard, Jr, MD. “The physician’s goal now is for the patient to be symptom free with grade 1 or less adverse events. And patients are demanding freedom from all the side effects that our usual course of immune therapy produces.” Dr. Howard is professor of neurology, medicine and allied health and director of the Myasthenia Gravis Clinical Trials and Translational Research Program at the University of North Carolina at Chapel Hill.
The shift has been long in coming. Although myasthenia gravis was identified in the mid-1600s, it took more than 340 years to get the first drug approved specifically for the disorder.
Worldwide prevalence estimates vary widely, from less than 200,000 to 700,000 cases.1,2 Pathophysiologically, myasthenia gravis stems from autoimmune destruction of neuromuscular junctions (NMJs), which transmit motor neuron impulses to muscle fibers.1 Symptoms include variable skeletal muscle weakness that can range from mild and transient to life-threatening.
In approximately 80% of cases, autoimmune antibodies target the postsynaptic acetylcholine receptor (AChR). Additional autoimmune targets mainly include muscle-specific kinase (MuSK) and lipoprotein receptor-related protein 4 (LRP4). However, around 10% of patients are seronegative, lacking autoantibodies detectable through conventional radioimmunoassays. Clinical disease does not always correspond with circulating antibody levels, and pathogenesis may require cooperation between multiple autoantibodies attacking the same target.3 Around 10% of MG cases are associated with thymomas.
Among myasthenia gravis treatments, immunosuppressants typically take 4-10 months to begin working and 18-36 months for maximum benefit. “Our new targeted therapies work within 1-2 weeks, with maximum improvement occurring somewhere between 8 and 12 weeks,” Dr. Howard said. Quick onset makes these drugs well suited for primary therapy in recalcitrant myasthenia gravis or as bridges to standard immunotherapy. Targeted drugs also appear to provide effective rescue therapy, although head-to-head studies are needed.
Complement Inhibition
In AChR antibody–positive myasthenia gravis, autoantibody binding with the postsynaptic AChR receptor activates complement to attack postsynaptic neuronal membrane. Complement inhibitors approved to date block activation of the terminal complement protein C5.
For many patients, complement inhibitors deliver dramatic results. Henry J. Kaminski, MD, said that the first patient for whom he prescribed a complement inhibitor outside a clinical trial went from being miserable to traveling internationally within a month. Dr. Kaminski is Meta A. Neumann Professor of Neurology at George Washington University, Washington, DC.
Eculizumab (Soliris, Alexion), earned Food and Drug Administration (FDA) approval for myasthenia gravis in 2017. Week 26 results in the phase 3 REGAIN trial showed no significant difference in Myasthenia Gravis–Activities of Daily Living (MG-ADL) scores between treatment and placebo. However, said Dr. Howard, primary investigator on the study, the negative result was a statistical aberration stemming from the FDA’s requirement to use worst-rank analysis rather than absolute change scores. What got eculizumab approved were highly positive results in the overwhelming majority of secondary endpoints.4 Subsequently, the FDA had the manufacturer rewrite the package insert using common statistical methods, which yielded positive primary results.
Ravulizumab (Ultomiris, Alexion), approved for myasthenia gravis in 2022, reduces eculizumab’s twice-monthly intravenous dosing to every 2 months (after loading doses), with very similar efficacy. The newest complement inhibitor, zilucoplan (Zilbrysq, UCB), administered once daily subcutaneously, earned FDA approval in 2023. Daily subcutaneous dosing provides patient convenience, said Dr. Howard. Because the body does not clear this small molecule as it would a full-size antibody, it is the only complement inhibitor that can be combined with a fragment crystallizable neonatal receptor (FcRn) inhibitor.
FcRn Inhibition
The FcRn exists on the surface and intracellular vesicles of many cells, including B cells, but not T cells.5FcRn inhibitors block binding of circulating IgG antibodies to the FcRn, preventing their normal recycling, significantly reducing circulating antibodies within days of treatment.
Efgartigimod (Vyvgart, Argenx), earned FDA approval in intravenous form in 2021, followed by a subcutaneous formulation that includes hyaluronidase (Vyvgart Hytrulo) in 2023. Rozanolixizumab (Rystiggo, UCB) earned FDA approval for both AChR antibody–positive and MuSK antibody–positive myasthenia gravis in 2023.
Along with rapid response, said Dr. Howard, complement inhibitors and FcRn inhibitors offer a “hugely improved” side-effect profile. In phase 3 research, the most common side effects for both classes included headache, nausea, and diarrhea.4,6,7 Because complement inhibitors increase the risk of Neisseria infection, users require immunization against meningococcal infection (or concurrent antibiotic prophylaxis) while on complement inhibitors.
Insurance Issues
With many clinicians wondering which targeted therapy to choose for a particular patient, said Dr. Howard and Dr. Kaminski, the main obstacle to wider use of these treatments is payer attitudes and practices. “While many of us would like to see these drugs used earlier in the course of disease,” Dr. Howard explained, “there are numerous restrictions placed on the physician and the patient by whatever insurance the individual has.”
Dr. Kaminski said: “There’s a lot of variability among insurance companies regarding what is expected in terms of getting approval for a certain medication. It frustrates me, thinking this patient may do well with a complement inhibitor or an FcRn inhibitor, but it takes weeks to get them approved.”
Some of his patients have been approved for, and flourished on, complement inhibitors and FcRn inhibitors, he added, and then denied a second round of treatment. Dr. Kaminski said he does not know why these patients were denied, and every time he requests reevaluation, the decision is reversed. “That’s a significant time frame for me and my staff to manage.”
When asked what can be done to address high drug prices, Dr. Howard replied, “I have no idea. I’m not an advocate of high drug prices. But I don’t think people realize the cost of doing clinical trials, which is hundreds of millions of dollars, particularly in rare diseases.”
Presently, Dr. Howard said, FcRn inhibitors are used more frequently than complement inhibitors solely because of cost. Zilucoplan will be priced below existing complement inhibitors, although it is too soon to compare its price with those of FcRn inhibitors.
When eculizumab debuted, said Dr. Howard, it cost nearly $750,000 annually. “But if you look at the number of patients treated, the cost of the drug over this population is probably less than the cost for using a cholesterol-lowering agent to treat hyperlipidemia.”
An Institute for Clinical and Economic Review (ICER) report stated that eculizumab and efgartigimod should both cost less than $20,000 annually to meet commonly used cost-effectiveness thresholds.8 However, Dr. Howard said ICER used models based on common diseases and ignored the economic impact of patients’ losing fewer workdays and avoiding long-term immunosuppressant side effects such as diabetes and osteoporosis and related treatment costs. “We’ve got to start looking at total societal cost,” he said.
Leapfrogging Ahead
Not all the new drugs work in every indicated patient, Dr. Howard said. For example, up to 30% of patients do not respond to complement inhibitors. “We don’t understand why. It’s as if we have leapfrogged way ahead in terms of therapeutics, and now we have to go back and answer all the questions – the who, what, where, and why of an individual drug and its response in folks.”
In this climate, said Dr. Kaminski, heavy direct-to-consumer advertising of newer myasthenia gravis therapies creates complications. “My patients are highly excited to see, ‘that’s my disease being advertised on Jeopardy.’ ” Many patients are frustrated with the general lack of awareness regarding myasthenia gravis, he added. “But then I’ve had patients who clearly would never qualify for a certain medication getting mailings to their homes.”
Dr. Howard countered that broader awareness of myasthenia gravis can only help. “There’s increasing recognition of the disease, not only by patients, but to some extent, by the treating clinician. Patients are coming to our offices and saying, ‘am I a candidate for this new drug?’ It’s the responsibility of the clinician to decide.”
Individual physicians’ practice patterns vary greatly, said Dr. Kaminski, and very little quantitative data exist here. But based on personal communications, academic-center neurologists tend to use targeted treatments on patients who have failed conventional treatments.
Conversely, Dr. Howard said that, because community physicians rarely see myasthenia gravis, and targeted treatments remain relatively new, many of these providers rely on prednisone, azathioprine, and mycophenolate mofetil.
B-Cell Blockers in Development
Overall, said Dr. Howard, the field of myasthenia gravis treatment development is “very rich. And pharma’s interest in myasthenia has taken off like a rocket. It’s exceptionally gratifying to those of us who take care of these patients whose life is miserable” because of adverse effects and/or nonresponse to current drugs.
“In myasthenia,” added Dr. Kaminski, “we know that T cells are promoting the activity of these auto-reactive B cells.” Many drugs currently in phase 2 or 3 development aim to eliminate B cells or signaling between T and B cells, he said. “That’s where most of the drug development is.”
Leading candidates include telitacicept (Tai’ai, RemeGen), which is both a B-lymphocyte stimulator and a proliferation-inducing ligand. A phase 3 trial (NCT05737160) is ongoing, with primary completion expected in late 2026. A second phase 3 trial (NCT06456580) recently began enrolling. Dr. Howard said that, although early results warranted phase 3 analysis, telitacicept’s phase 2 trial was open label and lacked a placebo group.9 The latter is a critical concern because placebo response rates in myasthenia gravis trials average 35%-40%.
Combined with standard care, the FcRn inhibitor nipocalimab (Johnson & Johnson) enabled patients with AChR, MuSK, and/or LRP4 autoantibodies to improve by 4.70 points on the MG-ADL vs 3.25 points for placebo (P = .002) over 24 weeks in phase 3.10All FcRn inhibitors in development can broadly reduce autoantibody levels, said Dr. Howard. “But what role they will play in myasthenia gravis when they’re several years behind leaders in the field in terms of capturing market remains to be seen.”
Additionally, batoclimab (Immunovant/Harbour BioMed) showed positive topline results in phase 3, and an elevated rate of hypercholesterolemia in treated patients that was transient and consistent with previous research.11 Subsequent to efgartigimod, Dr. Howard said, FcRn inhibitors are full-size antibodies. “I believe that contributes to the adverse events that we see. Efgartigimod is a small FcRn fragment. That’s why it’s a cleaner drug, if you will.”
FcRn inhibitors require periodic retreatment. For example, said Dr. Howard, the ADAPT phase 3 trial of efgartigimod, on which he was lead investigator, employed a cyclic dosing schedule – 4 weeks’ treatment, then observation until patients needed retreatment — because patients demanded it.12 In clinical practice, some patients have gone more than 25 weeks before needing retreatment. One of his patients went beyond 40 weeks. “Others only get around 6-9 weeks. So patient choice again enters the decision-making process.”
Rituximab targets the CD20 protein on B cells nonspecifically, producing general immunosuppression. “That’s problematic in producing significant immunosuppression,” said Dr. Kaminski. Nevertheless, he said, rituximab is very effective for most patients with MuSK-specific MG, and its application to this indication has revealed differences between the MuSK subtype and AChR antibody–positive myasthenia. Specifically, MuSK antibody–positive patients have short-lived plasmablasts, which rituximab eliminates.13
Conversely, said Dr. Kaminski, patients with AChR antibody-positive myasthenia, especially long-term, likely have long-lived plasmablasts producing antibodies. This fact, and these patients’ lack of CD20, likely explain their poor response to rituximab.
A phase 3 trial (NCT04524273) of the CD19 blocker inebilizumab (Uplinza, Amgen) reached primary completion in May. Dr. Howard said that if topline results (unreleased at press time) prove positive, inebilizumab could replace rituximab in MG — provided payers do not reject inebilizumab because of cost.
Packed Early-Development Pipeline
Regarding early-stage projects, said Dr. Howard, the pipeline is packed with compounds that target various aspects of the immune system. “The real question with those is, what’s going to be the side effect profile? All of the trials are very early. We need bigger trials with much longer observation for safety, durability, and degree of efficacy.”
The next potential B cell–targeting game changer, he said, is chimeric antigen receptor (CAR) T cell–based therapy. In a phase 2b trial of Descartes-08 (Cartesian Therapeutics), 71% of treated patients experienced clinically meaningful improvement in MG Composite score at 3 months vs 25% for placebo.14
In early clinical trials, said Dr. Howard, patients treated with Descartes-08 — which uses autologous mRNA to target B-cell maturation antigen — have shown “exceptional improvement” lasting 20 or more months. Because the drug is not ingrained permanently into the genome, Descartes-08 avoids potentially severe side effects of DNA-targeting CAR T candidates. Dr. Howard hopes a phase 3 trial will commence around January 2025.
The tolerance approach exemplified by CNP-106 (COUR Pharmaceuticals) and a myasthenia gravis tolerogen (Toleranzia) seeks to prevent the immune system from recognizing and reacting to the NMJ abnormalities that produce myasthenia gravis, potentially providing a cure. “We look forward to those trials as they come online in the next 1-2 years,” said Dr. Howard.
Unmet Needs
Historically, neurologists believed that all myasthenia gravis symptoms stemmed from muscle fatigue — the more active the muscle, the weaker it gets. However, said Dr. Kaminski, some patients might lack measurable weakness but still complain of fatigue.
Elevated levels of cytokines such as interleukin (IL)–6 or IL-17 also can produce fatigue, he noted. “With the drugs we’re using, certainly the new ones, we’re not specifically targeting this fatigue phenomenon, which has been studied in a very limited fashion.”
In the RAISE-XT zilucoplan trial, participants experienced significant improvement in fatigue scores for up to 60 weeks.15 Although zilucoplan does not address fatigue directly, said Dr. Howard, improving myasthenia gravis overall helps reduce fatigue.
The Myasthenia Gravis Symptoms Patient Reported Outcome (MG Symptoms PRO), which Dr. Kaminski helped develop, includes questions designed to distinguish muscular fatigue from overall physical fatigue.16 “I’m very interested in some of the information that’s coming out on long COVID and its effect on muscle,” Dr. Kaminski added. “We might be able to learn from there that there’s still some pathology going on beyond the neuromuscular junction.”
What the field desperately needs, said Dr. Howard, are biomarkers to identify which patients will and will not respond to certain therapeutics. “We’re not there yet.” Such biomarkers are at least 3-7 years from becoming clinical reality.
Promising antibody-independent serum markers include circulating microRNAs. For example, miRNA-150-5p and miRNA-21-5p are elevated in generalized AChR-positive myasthenia gravis and early-onset myasthenia gravis (occurring before age 50) and decline after immunosuppression and thymectomy.17
Among diagnostic modalities for patients with seronegative myasthenia gravis, said Dr. Kaminski, single-fiber EMG is the most sensitive, at approximately 95%. “It’s not perfect.” Moreover, he said, performing this test accurately requires a highly experienced expert, which many treatment centers lack.
Presently, added Dr. Kaminski, orbital MRI is neither specific nor sensitive enough to be clinically useful. “One needs to be careful with these specialized tests that are published from the best laboratory in the world that does the test, and does it repetitively.” As the search for effective myasthenia gravis biomarkers continues, avoiding false-positive results is as important as avoiding false negatives.
References
1. Bubuioc AM et al. J Med Life. 2021 Jan-Mar;14(1):7-16. doi: 10.25122/jml-2020-0145.
2. Deenen JC et al. J Neuromuscul Dis. 2015;2(1):73-85. doi: 10.3233/JND-140045.
3. Kaminski HJ et al. J Clin Invest. 2024 Jun 17;134(12):e179742. doi: 10.1172/JCI179742.
4. Howard JF Jr et al. Lancet Neurol. 2017 Dec;16(12):976-986. doi: 10.1016/S1474-4422(17)30369-1.
5. Huda R. Front Immunol. 2020 Feb 21:11:240. doi: 10.3389/fimmu.2020.00240.
6. Howard JF Jr et al. Lancet Neurol. 2023 May;22(5):395-406. doi: 10.1016/S1474-4422(23)00080-7.
7. Vu T et al. NEJM Evid. 2022 May;1(5):EVIDoa2100066. doi: 10.1056/EVIDoa2100066.
8. Tice JA et al. October 20, 2021. https://icer.org/assessment/myasthenia-gravis/.
9. Yin J et al. Eur J Neurol. 2024 Aug;31(8):e16322. doi: 10.1111/ene.16322.
10. Antozzi C et al. EAN 2024, Abstract EPR-116. https://www.neurology.org/doi/10.1212/WNL.0000000000203660.
11. Yan C et al. JAMA Neurol. 2024 Mar 4;81(4):336-345. doi: 10.1001/jamaneurol.2024.0044.
12. Howard JF Jr et al. Lancet Neurol. 2021 Jul;20(7):526-536. doi: 10.1016/S1474-4422(21)00159-9.
13. Stathopoulos P et al. JCI Insight. 2017 Sep 7;2(17):e94263. doi: 10.1172/jci.insight.94263.
14. Cartesian Therapeutics. Cartesian Therapeutics announces positive topline results from phase 2b trial of Descartes-08 in patients with myasthenia gravis. 2024 Jul 2. https://ir.cartesiantherapeutics.com/news-releases/news-release-details/cartesian-therapeutics-announces-positive-topline-results-phase.
15. Howard JF Jr et al. Ther Adv Neurol Disord. 2024 Apr 17:17:17562864241243186. doi: 10.1177/17562864241243186.
16. Cleanthous S et al. Orphanet J Rare Dis. 2021 Oct 30;16(1):457. doi: 10.1186/s13023-021-02064-0.
17. Sabre L et al. Front Immunol. 2020 Mar 4:11:213. doi: 10.3389/fimmu.2020.00213.
Used appropriately, newer treatments can provide dramatic results faster and more safely than broad immunosuppressants. However, according to experts, payers’ willingness to cover costly new therapies remains a work in progress.
The availability of more effective treatments with fewer side effects has brought about a cultural shift, said James F. Howard, Jr, MD. “The physician’s goal now is for the patient to be symptom free with grade 1 or less adverse events. And patients are demanding freedom from all the side effects that our usual course of immune therapy produces.” Dr. Howard is professor of neurology, medicine and allied health and director of the Myasthenia Gravis Clinical Trials and Translational Research Program at the University of North Carolina at Chapel Hill.
The shift has been long in coming. Although myasthenia gravis was identified in the mid-1600s, it took more than 340 years to get the first drug approved specifically for the disorder.
Worldwide prevalence estimates vary widely, from less than 200,000 to 700,000 cases.1,2 Pathophysiologically, myasthenia gravis stems from autoimmune destruction of neuromuscular junctions (NMJs), which transmit motor neuron impulses to muscle fibers.1 Symptoms include variable skeletal muscle weakness that can range from mild and transient to life-threatening.
In approximately 80% of cases, autoimmune antibodies target the postsynaptic acetylcholine receptor (AChR). Additional autoimmune targets mainly include muscle-specific kinase (MuSK) and lipoprotein receptor-related protein 4 (LRP4). However, around 10% of patients are seronegative, lacking autoantibodies detectable through conventional radioimmunoassays. Clinical disease does not always correspond with circulating antibody levels, and pathogenesis may require cooperation between multiple autoantibodies attacking the same target.3 Around 10% of MG cases are associated with thymomas.
Among myasthenia gravis treatments, immunosuppressants typically take 4-10 months to begin working and 18-36 months for maximum benefit. “Our new targeted therapies work within 1-2 weeks, with maximum improvement occurring somewhere between 8 and 12 weeks,” Dr. Howard said. Quick onset makes these drugs well suited for primary therapy in recalcitrant myasthenia gravis or as bridges to standard immunotherapy. Targeted drugs also appear to provide effective rescue therapy, although head-to-head studies are needed.
Complement Inhibition
In AChR antibody–positive myasthenia gravis, autoantibody binding with the postsynaptic AChR receptor activates complement to attack postsynaptic neuronal membrane. Complement inhibitors approved to date block activation of the terminal complement protein C5.
For many patients, complement inhibitors deliver dramatic results. Henry J. Kaminski, MD, said that the first patient for whom he prescribed a complement inhibitor outside a clinical trial went from being miserable to traveling internationally within a month. Dr. Kaminski is Meta A. Neumann Professor of Neurology at George Washington University, Washington, DC.
Eculizumab (Soliris, Alexion), earned Food and Drug Administration (FDA) approval for myasthenia gravis in 2017. Week 26 results in the phase 3 REGAIN trial showed no significant difference in Myasthenia Gravis–Activities of Daily Living (MG-ADL) scores between treatment and placebo. However, said Dr. Howard, primary investigator on the study, the negative result was a statistical aberration stemming from the FDA’s requirement to use worst-rank analysis rather than absolute change scores. What got eculizumab approved were highly positive results in the overwhelming majority of secondary endpoints.4 Subsequently, the FDA had the manufacturer rewrite the package insert using common statistical methods, which yielded positive primary results.
Ravulizumab (Ultomiris, Alexion), approved for myasthenia gravis in 2022, reduces eculizumab’s twice-monthly intravenous dosing to every 2 months (after loading doses), with very similar efficacy. The newest complement inhibitor, zilucoplan (Zilbrysq, UCB), administered once daily subcutaneously, earned FDA approval in 2023. Daily subcutaneous dosing provides patient convenience, said Dr. Howard. Because the body does not clear this small molecule as it would a full-size antibody, it is the only complement inhibitor that can be combined with a fragment crystallizable neonatal receptor (FcRn) inhibitor.
FcRn Inhibition
The FcRn exists on the surface and intracellular vesicles of many cells, including B cells, but not T cells.5FcRn inhibitors block binding of circulating IgG antibodies to the FcRn, preventing their normal recycling, significantly reducing circulating antibodies within days of treatment.
Efgartigimod (Vyvgart, Argenx), earned FDA approval in intravenous form in 2021, followed by a subcutaneous formulation that includes hyaluronidase (Vyvgart Hytrulo) in 2023. Rozanolixizumab (Rystiggo, UCB) earned FDA approval for both AChR antibody–positive and MuSK antibody–positive myasthenia gravis in 2023.
Along with rapid response, said Dr. Howard, complement inhibitors and FcRn inhibitors offer a “hugely improved” side-effect profile. In phase 3 research, the most common side effects for both classes included headache, nausea, and diarrhea.4,6,7 Because complement inhibitors increase the risk of Neisseria infection, users require immunization against meningococcal infection (or concurrent antibiotic prophylaxis) while on complement inhibitors.
Insurance Issues
With many clinicians wondering which targeted therapy to choose for a particular patient, said Dr. Howard and Dr. Kaminski, the main obstacle to wider use of these treatments is payer attitudes and practices. “While many of us would like to see these drugs used earlier in the course of disease,” Dr. Howard explained, “there are numerous restrictions placed on the physician and the patient by whatever insurance the individual has.”
Dr. Kaminski said: “There’s a lot of variability among insurance companies regarding what is expected in terms of getting approval for a certain medication. It frustrates me, thinking this patient may do well with a complement inhibitor or an FcRn inhibitor, but it takes weeks to get them approved.”
Some of his patients have been approved for, and flourished on, complement inhibitors and FcRn inhibitors, he added, and then denied a second round of treatment. Dr. Kaminski said he does not know why these patients were denied, and every time he requests reevaluation, the decision is reversed. “That’s a significant time frame for me and my staff to manage.”
When asked what can be done to address high drug prices, Dr. Howard replied, “I have no idea. I’m not an advocate of high drug prices. But I don’t think people realize the cost of doing clinical trials, which is hundreds of millions of dollars, particularly in rare diseases.”
Presently, Dr. Howard said, FcRn inhibitors are used more frequently than complement inhibitors solely because of cost. Zilucoplan will be priced below existing complement inhibitors, although it is too soon to compare its price with those of FcRn inhibitors.
When eculizumab debuted, said Dr. Howard, it cost nearly $750,000 annually. “But if you look at the number of patients treated, the cost of the drug over this population is probably less than the cost for using a cholesterol-lowering agent to treat hyperlipidemia.”
An Institute for Clinical and Economic Review (ICER) report stated that eculizumab and efgartigimod should both cost less than $20,000 annually to meet commonly used cost-effectiveness thresholds.8 However, Dr. Howard said ICER used models based on common diseases and ignored the economic impact of patients’ losing fewer workdays and avoiding long-term immunosuppressant side effects such as diabetes and osteoporosis and related treatment costs. “We’ve got to start looking at total societal cost,” he said.
Leapfrogging Ahead
Not all the new drugs work in every indicated patient, Dr. Howard said. For example, up to 30% of patients do not respond to complement inhibitors. “We don’t understand why. It’s as if we have leapfrogged way ahead in terms of therapeutics, and now we have to go back and answer all the questions – the who, what, where, and why of an individual drug and its response in folks.”
In this climate, said Dr. Kaminski, heavy direct-to-consumer advertising of newer myasthenia gravis therapies creates complications. “My patients are highly excited to see, ‘that’s my disease being advertised on Jeopardy.’ ” Many patients are frustrated with the general lack of awareness regarding myasthenia gravis, he added. “But then I’ve had patients who clearly would never qualify for a certain medication getting mailings to their homes.”
Dr. Howard countered that broader awareness of myasthenia gravis can only help. “There’s increasing recognition of the disease, not only by patients, but to some extent, by the treating clinician. Patients are coming to our offices and saying, ‘am I a candidate for this new drug?’ It’s the responsibility of the clinician to decide.”
Individual physicians’ practice patterns vary greatly, said Dr. Kaminski, and very little quantitative data exist here. But based on personal communications, academic-center neurologists tend to use targeted treatments on patients who have failed conventional treatments.
Conversely, Dr. Howard said that, because community physicians rarely see myasthenia gravis, and targeted treatments remain relatively new, many of these providers rely on prednisone, azathioprine, and mycophenolate mofetil.
B-Cell Blockers in Development
Overall, said Dr. Howard, the field of myasthenia gravis treatment development is “very rich. And pharma’s interest in myasthenia has taken off like a rocket. It’s exceptionally gratifying to those of us who take care of these patients whose life is miserable” because of adverse effects and/or nonresponse to current drugs.
“In myasthenia,” added Dr. Kaminski, “we know that T cells are promoting the activity of these auto-reactive B cells.” Many drugs currently in phase 2 or 3 development aim to eliminate B cells or signaling between T and B cells, he said. “That’s where most of the drug development is.”
Leading candidates include telitacicept (Tai’ai, RemeGen), which is both a B-lymphocyte stimulator and a proliferation-inducing ligand. A phase 3 trial (NCT05737160) is ongoing, with primary completion expected in late 2026. A second phase 3 trial (NCT06456580) recently began enrolling. Dr. Howard said that, although early results warranted phase 3 analysis, telitacicept’s phase 2 trial was open label and lacked a placebo group.9 The latter is a critical concern because placebo response rates in myasthenia gravis trials average 35%-40%.
Combined with standard care, the FcRn inhibitor nipocalimab (Johnson & Johnson) enabled patients with AChR, MuSK, and/or LRP4 autoantibodies to improve by 4.70 points on the MG-ADL vs 3.25 points for placebo (P = .002) over 24 weeks in phase 3.10All FcRn inhibitors in development can broadly reduce autoantibody levels, said Dr. Howard. “But what role they will play in myasthenia gravis when they’re several years behind leaders in the field in terms of capturing market remains to be seen.”
Additionally, batoclimab (Immunovant/Harbour BioMed) showed positive topline results in phase 3, and an elevated rate of hypercholesterolemia in treated patients that was transient and consistent with previous research.11 Subsequent to efgartigimod, Dr. Howard said, FcRn inhibitors are full-size antibodies. “I believe that contributes to the adverse events that we see. Efgartigimod is a small FcRn fragment. That’s why it’s a cleaner drug, if you will.”
FcRn inhibitors require periodic retreatment. For example, said Dr. Howard, the ADAPT phase 3 trial of efgartigimod, on which he was lead investigator, employed a cyclic dosing schedule – 4 weeks’ treatment, then observation until patients needed retreatment — because patients demanded it.12 In clinical practice, some patients have gone more than 25 weeks before needing retreatment. One of his patients went beyond 40 weeks. “Others only get around 6-9 weeks. So patient choice again enters the decision-making process.”
Rituximab targets the CD20 protein on B cells nonspecifically, producing general immunosuppression. “That’s problematic in producing significant immunosuppression,” said Dr. Kaminski. Nevertheless, he said, rituximab is very effective for most patients with MuSK-specific MG, and its application to this indication has revealed differences between the MuSK subtype and AChR antibody–positive myasthenia. Specifically, MuSK antibody–positive patients have short-lived plasmablasts, which rituximab eliminates.13
Conversely, said Dr. Kaminski, patients with AChR antibody-positive myasthenia, especially long-term, likely have long-lived plasmablasts producing antibodies. This fact, and these patients’ lack of CD20, likely explain their poor response to rituximab.
A phase 3 trial (NCT04524273) of the CD19 blocker inebilizumab (Uplinza, Amgen) reached primary completion in May. Dr. Howard said that if topline results (unreleased at press time) prove positive, inebilizumab could replace rituximab in MG — provided payers do not reject inebilizumab because of cost.
Packed Early-Development Pipeline
Regarding early-stage projects, said Dr. Howard, the pipeline is packed with compounds that target various aspects of the immune system. “The real question with those is, what’s going to be the side effect profile? All of the trials are very early. We need bigger trials with much longer observation for safety, durability, and degree of efficacy.”
The next potential B cell–targeting game changer, he said, is chimeric antigen receptor (CAR) T cell–based therapy. In a phase 2b trial of Descartes-08 (Cartesian Therapeutics), 71% of treated patients experienced clinically meaningful improvement in MG Composite score at 3 months vs 25% for placebo.14
In early clinical trials, said Dr. Howard, patients treated with Descartes-08 — which uses autologous mRNA to target B-cell maturation antigen — have shown “exceptional improvement” lasting 20 or more months. Because the drug is not ingrained permanently into the genome, Descartes-08 avoids potentially severe side effects of DNA-targeting CAR T candidates. Dr. Howard hopes a phase 3 trial will commence around January 2025.
The tolerance approach exemplified by CNP-106 (COUR Pharmaceuticals) and a myasthenia gravis tolerogen (Toleranzia) seeks to prevent the immune system from recognizing and reacting to the NMJ abnormalities that produce myasthenia gravis, potentially providing a cure. “We look forward to those trials as they come online in the next 1-2 years,” said Dr. Howard.
Unmet Needs
Historically, neurologists believed that all myasthenia gravis symptoms stemmed from muscle fatigue — the more active the muscle, the weaker it gets. However, said Dr. Kaminski, some patients might lack measurable weakness but still complain of fatigue.
Elevated levels of cytokines such as interleukin (IL)–6 or IL-17 also can produce fatigue, he noted. “With the drugs we’re using, certainly the new ones, we’re not specifically targeting this fatigue phenomenon, which has been studied in a very limited fashion.”
In the RAISE-XT zilucoplan trial, participants experienced significant improvement in fatigue scores for up to 60 weeks.15 Although zilucoplan does not address fatigue directly, said Dr. Howard, improving myasthenia gravis overall helps reduce fatigue.
The Myasthenia Gravis Symptoms Patient Reported Outcome (MG Symptoms PRO), which Dr. Kaminski helped develop, includes questions designed to distinguish muscular fatigue from overall physical fatigue.16 “I’m very interested in some of the information that’s coming out on long COVID and its effect on muscle,” Dr. Kaminski added. “We might be able to learn from there that there’s still some pathology going on beyond the neuromuscular junction.”
What the field desperately needs, said Dr. Howard, are biomarkers to identify which patients will and will not respond to certain therapeutics. “We’re not there yet.” Such biomarkers are at least 3-7 years from becoming clinical reality.
Promising antibody-independent serum markers include circulating microRNAs. For example, miRNA-150-5p and miRNA-21-5p are elevated in generalized AChR-positive myasthenia gravis and early-onset myasthenia gravis (occurring before age 50) and decline after immunosuppression and thymectomy.17
Among diagnostic modalities for patients with seronegative myasthenia gravis, said Dr. Kaminski, single-fiber EMG is the most sensitive, at approximately 95%. “It’s not perfect.” Moreover, he said, performing this test accurately requires a highly experienced expert, which many treatment centers lack.
Presently, added Dr. Kaminski, orbital MRI is neither specific nor sensitive enough to be clinically useful. “One needs to be careful with these specialized tests that are published from the best laboratory in the world that does the test, and does it repetitively.” As the search for effective myasthenia gravis biomarkers continues, avoiding false-positive results is as important as avoiding false negatives.
References
1. Bubuioc AM et al. J Med Life. 2021 Jan-Mar;14(1):7-16. doi: 10.25122/jml-2020-0145.
2. Deenen JC et al. J Neuromuscul Dis. 2015;2(1):73-85. doi: 10.3233/JND-140045.
3. Kaminski HJ et al. J Clin Invest. 2024 Jun 17;134(12):e179742. doi: 10.1172/JCI179742.
4. Howard JF Jr et al. Lancet Neurol. 2017 Dec;16(12):976-986. doi: 10.1016/S1474-4422(17)30369-1.
5. Huda R. Front Immunol. 2020 Feb 21:11:240. doi: 10.3389/fimmu.2020.00240.
6. Howard JF Jr et al. Lancet Neurol. 2023 May;22(5):395-406. doi: 10.1016/S1474-4422(23)00080-7.
7. Vu T et al. NEJM Evid. 2022 May;1(5):EVIDoa2100066. doi: 10.1056/EVIDoa2100066.
8. Tice JA et al. October 20, 2021. https://icer.org/assessment/myasthenia-gravis/.
9. Yin J et al. Eur J Neurol. 2024 Aug;31(8):e16322. doi: 10.1111/ene.16322.
10. Antozzi C et al. EAN 2024, Abstract EPR-116. https://www.neurology.org/doi/10.1212/WNL.0000000000203660.
11. Yan C et al. JAMA Neurol. 2024 Mar 4;81(4):336-345. doi: 10.1001/jamaneurol.2024.0044.
12. Howard JF Jr et al. Lancet Neurol. 2021 Jul;20(7):526-536. doi: 10.1016/S1474-4422(21)00159-9.
13. Stathopoulos P et al. JCI Insight. 2017 Sep 7;2(17):e94263. doi: 10.1172/jci.insight.94263.
14. Cartesian Therapeutics. Cartesian Therapeutics announces positive topline results from phase 2b trial of Descartes-08 in patients with myasthenia gravis. 2024 Jul 2. https://ir.cartesiantherapeutics.com/news-releases/news-release-details/cartesian-therapeutics-announces-positive-topline-results-phase.
15. Howard JF Jr et al. Ther Adv Neurol Disord. 2024 Apr 17:17:17562864241243186. doi: 10.1177/17562864241243186.
16. Cleanthous S et al. Orphanet J Rare Dis. 2021 Oct 30;16(1):457. doi: 10.1186/s13023-021-02064-0.
17. Sabre L et al. Front Immunol. 2020 Mar 4:11:213. doi: 10.3389/fimmu.2020.00213.
Untangling CIDP
Chronic inflammatory demyelinating polyradiculoneuropathy, or CIDP, is a rare immune-mediated nerve disorder characterized by progressive weakness and sensory impairment in the arms and legs, the result of an autoimmune attack on myelin.
Though some clustering of cases may occur in families, and susceptibility genes have been found, it is not considered a genetic disease. It can strike patients of either sex at any age, though most cases will occur in or after midlife.
Complicating matters further, CIDP has several variants whose symptoms differ from classical presentations.
Many patients who do not have CIDP end up being treated for it, and many CIDP patients experience delays to diagnosis and treatment that can potentially result in greater nerve damage and worse outcomes.
The good news, CIDP experts say, is that the last few years have seen important advances in diagnosis and treatment – including comprehensive new clinical guidelines and the June 2024 approval by the Food and Drug Administration of a new treatment, efgartigimod alfa and hyaluronidase-qvfc (Vyvgart, argenx). This antibody fragment represents the first non-steroid, non-immunoglobulin option for CIDP.
Despite the difficulties of recruiting patients with a tough-to-confirm disease that affects between 2 and 9 of every 100,000 people, according to the GPS-CIDP Foundation clinical trials have been successfully carried out in CIDP, and new ones continue to recruit. The experimental therapies being explored are based on a wide range of proposed disease pathways.
“It’s a very exciting time,” said Jeffrey Allen, MD, a neurologist at the University of Minnesota, Minneapolis, one of three CIDP experts who spoke about this challenging but treatable syndrome, its diagnosis and management, and the research questions that they hope to see answered.
Refining Diagnosis
In classical or typical CIDP, which accounts for most cases, patients present with progressive weakness and numbness that affects the arms and legs symmetrically, with the weakness being both proximal and distal. The disease usually evolves over a period of months, which helps distinguish it from Gullain-Barré syndrome, whose onset is more sudden and progression is less than 4 weeks.
CIDP was first described in the 1970s, and since that time more than a dozen sets of diagnostic criteria have been published. Starting about a decade ago, Dr. Allen and neurologist Richard Lewis, MD, of Cedars-Sinai Medical Center in Los Angeles, California, helped launch an effort to improve them.
“Experts in the field who were seeing patients with CIDP recognized that a lot of referrals coming to them were of people who actually didn’t have it, or they had the disease and were treated for it but didn’t need to be on treatment, or their treatment was very unconventional,” Dr. Allen said. “We wanted to try to put some data behind that.” In 2015 Dr. Allen and Dr. Lewis published a paper that found that nearly half of patients referred with a diagnosis of CIDP failed to meet basic diagnostic requirements.
Erroneous interpretation of nerve conduction studies “was a significant factor” contributing to the misdiagnoses, Dr. Lewis said. And another major problem was that patients’ response to standard treatment with intravenous immunoglobulins (current treatments have also come to include subcutaneous immunoglobulins) was not being measured objectively. Instead of evaluating patients using grip strength, walking tests, or other objective instruments, clinicians asked patients whether they felt better. “The problem is that IVIg makes people feel good,” Dr. Lewis said, “possibly by reducing normal inflammatory agents in the body.”
The 2015 paper caught the attention of neurologists and neuromuscular specialists worldwide, who reported similar problems with misdiagnosis. “And from there we did other work to try to dissect out what the more specific issues are,” Dr. Allen said. “The electrophysiology was a big one.”
Neurologist Nicholas Silvestri, MD, of the University at Buffalo in New York, one of the centers of excellence recognized by the CIDP-GBS Foundation, affirmed that nerve conduction studies, which essential to diagnosing CIDP, “are not as objective as we think they are. They’re very prone to user error and overinterpretation error. If they’re not performed appropriately, things can look like CIDP when they’re not. Very common forms of neuropathy, like diabetic neuropathy, can be misinterpreted as CIDP.”
The Challenge of Variants
After their 2015 paper on diagnostic pitfalls, Dr. Lewis and Dr. Allen, along with colleagues in the United States and Europe, started looking deeper into outcome measures and how to better follow and track patients with CIDP. In 2021 they helped create the first comprehensive clinical guidelines for CIDP in over a decade.
Much of their effort focused on atypical presentations, or what are now called variants, of CIDP — people with predominantly distal disease, asymmetrical symptomology, focal symptoms, or exclusively motor or sensory symptoms. With classical CIDP, “we don’t really have a problem with misdiagnosis,” Dr. Lewis said. With variants, however, misdiagnoses are extremely common. The 2021 guidelines try to address this, proposing differential diagnoses for each of the variants and ways to investigate them.
The guidelines also removed a subgroup of patients previously included as having CIDP. These patients, who comprise about 10% of cases, have antibodies to components of the Node of Ranvier, part of the axonal membrane, and the paranodal myelin. The autoimmune nodopathies do not respond to treatment with immunoglobulins or steroids in the way classical CIDP and its variants do. However, many patients have seen success with the immunotherapy rituximab.
“CIDP is a syndrome, not one disease,” Dr. Lewis said. “So it has been difficult to get guidelines or criteria that are sensitive to all the different forms of the disease, and yet specific for the disease and not overlapping. The nodopathies were pulled out because they don’t respond to usual treatments for CIDP. Hopefully over the years we’ll have even more specific diagnoses and can split out more patients.”
A Need for Better Biomarkers
With the neuromuscular autoimmune disease myasthenia gravis, 85% of patients have antibodies against the muscle acetylcholine receptor (AChR). Another 6% will have antibodies against muscle-specific kinase (MuSK).
Antibody profiles have long guided treatment decisions in myasthenia gravis, with AChR-positive patients responding to corticosteroids, IVIg, complement inhibitors, and other agents. MuSK-positive myasthenia gravis patients, similar to people with autoimmune nodopathies, respond poorly to IVIg but can have dramatic responses when treated with B cell–depleting therapies like rituximab.
Antibodies to nodal proteins neurofascin-155 and contactin-1 have been shown to be involved with the nodopathies. Assays for these are now commercially available, and Dr. Allen recommended that clinicians seek them for patients with a more rapid course, with tremor and ataxia, or who do not respond to standard CIDP treatments.
Still, no dominant autoantibody has been identified for the majority of presentations, including classical presentations. “I suspect it’s a heterogeneous group of multiple antibodies causing the disease,” Dr. Silvestri said. “That may explain to an extent the different manifestations and the different responses to treatment.”
Dr. Lewis said he thinks that, while more antibodies are likely to be discovered in the coming years, “we’re still identifying fewer than 20% of CIDP patients by specific antibodies, so we have a long way to go.”
Promising Trial Landscape
“CIDP is a challenging disease to study because of the diagnostic issues,” Dr. Allen said. “We know that a [nontrivial] percentage of patients ... can go into a drug-free remission. They actually don’t need treatment during that time. We don’t have any way to measure that. And if you put them in a clinical trial, it’s difficult to measure changes in the trial if they didn’t need the drug in the first place.”
In the global ADHERE trail, which looked at efgartigimod alfa and hyaluronidase-qvfc in CIDP patients, the investigators, led by Dr. Allen and Dr. Lewis, challenged patients to be off therapy for 12 weeks and allowed only those with active disease to enroll. They also used an adjudication panel of CIDP experts to review the records of each patient to assure patients had CIDP.
If two experts on the panel independently agreed that it was CIDP, Dr. Lewis said, then patients were eligible for enrollment. “If they both said they weren’t CIDP, they were not eligible. And if there was an argument between the two of them, then a third adjudicator would come in.”
About half of patients screened (n = 221) ended up included, and adjudication panels are now used in most CIDP trials.
The trial saw a positive outcome for efgartigimod alfa and hyaluronidase-qvfc, an antibody fragment that targets neonatal Fc receptor (FcRn), as a way to reduce to levels of pathogenic IgG autoantibodies. (The treatment was previously approved for myasthenia gravis.) The fact that two thirds of participants in the trial responded pointed to the likelihood that most CIDP patients have an IgG-related disease, Dr. Lewis said.
Different types of therapies are now being investigated in CIDP, among them other FcRn-inhibiting drugs and drugs inhibiting complement. Results from these trials may shed more light on the pathophysiology of the disease, which Dr. Silvestri said would be welcome.
“If I can test for antibodies, I can make a more timely diagnosis,” he said. “I’m assuming that some people with CIDP have non–antibody-driven disease. And in those cases, I want to avoid using drugs like Vyvgart, which are targeting antibodies. I want to give them a different therapy.”
Management: A Delicate Dance
Since the 1990s, the standard of care for CIDP has been IVIg and steroids. Newer subcutaneous immunoglobulin products, which take less time to administer, may be more convenient for patients than traditional IVIg and mitigate some concerning side effects.
Efgartigimod alfa and hyaluronidase-qvfc now offers an entirely different option that, while too new for clinicians to have much experience with in CIDP, represents further convenience for patients, with dosing in one 90-second subcutaneous injection per week.
In general, the sooner people are diagnosed and on therapy, the better they are likely to do, with fewer risks of irreversible axonal loss and disability. Referring to CIDP centers of excellence can help speed a definitive diagnosis.
Some patients will see a complete or near-complete recovery, while others will not. “It’s important to be up front with patients about what the benefit of treatments are, what are the expectations of treatment, what we can potentially get back, and what’s unlikely to come back,” Dr. Allen said. “We know that irreversible deficits are not uncommon in folks with CIDP. Part of that is driven by how severe their disease is or how long they’ve had it.”
Good CIDP management, according to the 2021 guidelines, involves making periodic dose reductions or withdrawing therapies on a trial basis, because people can and do experience remission. “We don’t have any test that tells us if somebody needs treatment or not. So this is the best we can do right now,” Dr. Allen said.
This process can be anxiety provoking for patients. “In my practice, there are no surprises,” he said. “We don’t typically say, ‘we’re going to stop your treatment today.’ It’s a discussion with a lead up that’s usually many months long.”
Management of CIDP also requires discussions to elicit when and whether worsening is occurring, along with a clear sense, by both patient and clinician, of what constitutes worsening.
Serial nerve conduction studies are not very useful, Dr. Lewis said, but objective disability measures are and should be more broadly adopted. These include the Medical Research Council sumscore, a test of 12 muscles that can determine weakness; a hand grip test; and functional disability scales such as Inflammatory Rasch Overall Disability Scale and Inflammatory Neuropathy Cause and Treatment scale. All are quick to administer in the office, and some can be done by the patient at home, providing the clinician useful information between visits.
“We could do a better job with educating [clinicians] on the value of different outcome measures that can really quantify disease activity,” Dr. Allen said, and pointed to the GBS-CIDP Foundation centers of excellence, which exist in most regions of the United States, as an outstanding resource for anyone wanting to know more.
“The centers are really, really helpful when you’re trying to work through some of these issues,” he said.
Suggested Reading
Allen JA and Lewis RA. Neurology. 2015 Aug 11;85(6):498-504. doi: 10.1212/WNL.0000000000001833.
Allen J et al. Neurology. 2024;102(17_supplement_1). doi: 10.1212/WNL-.0000000000206324.
Van den Bergh PYK et al. J Peripher Nerv Syst. 2021 Sep;26(3):242-268. doi: 10.1111/jns.12455.
Chronic inflammatory demyelinating polyradiculoneuropathy, or CIDP, is a rare immune-mediated nerve disorder characterized by progressive weakness and sensory impairment in the arms and legs, the result of an autoimmune attack on myelin.
Though some clustering of cases may occur in families, and susceptibility genes have been found, it is not considered a genetic disease. It can strike patients of either sex at any age, though most cases will occur in or after midlife.
Complicating matters further, CIDP has several variants whose symptoms differ from classical presentations.
Many patients who do not have CIDP end up being treated for it, and many CIDP patients experience delays to diagnosis and treatment that can potentially result in greater nerve damage and worse outcomes.
The good news, CIDP experts say, is that the last few years have seen important advances in diagnosis and treatment – including comprehensive new clinical guidelines and the June 2024 approval by the Food and Drug Administration of a new treatment, efgartigimod alfa and hyaluronidase-qvfc (Vyvgart, argenx). This antibody fragment represents the first non-steroid, non-immunoglobulin option for CIDP.
Despite the difficulties of recruiting patients with a tough-to-confirm disease that affects between 2 and 9 of every 100,000 people, according to the GPS-CIDP Foundation clinical trials have been successfully carried out in CIDP, and new ones continue to recruit. The experimental therapies being explored are based on a wide range of proposed disease pathways.
“It’s a very exciting time,” said Jeffrey Allen, MD, a neurologist at the University of Minnesota, Minneapolis, one of three CIDP experts who spoke about this challenging but treatable syndrome, its diagnosis and management, and the research questions that they hope to see answered.
Refining Diagnosis
In classical or typical CIDP, which accounts for most cases, patients present with progressive weakness and numbness that affects the arms and legs symmetrically, with the weakness being both proximal and distal. The disease usually evolves over a period of months, which helps distinguish it from Gullain-Barré syndrome, whose onset is more sudden and progression is less than 4 weeks.
CIDP was first described in the 1970s, and since that time more than a dozen sets of diagnostic criteria have been published. Starting about a decade ago, Dr. Allen and neurologist Richard Lewis, MD, of Cedars-Sinai Medical Center in Los Angeles, California, helped launch an effort to improve them.
“Experts in the field who were seeing patients with CIDP recognized that a lot of referrals coming to them were of people who actually didn’t have it, or they had the disease and were treated for it but didn’t need to be on treatment, or their treatment was very unconventional,” Dr. Allen said. “We wanted to try to put some data behind that.” In 2015 Dr. Allen and Dr. Lewis published a paper that found that nearly half of patients referred with a diagnosis of CIDP failed to meet basic diagnostic requirements.
Erroneous interpretation of nerve conduction studies “was a significant factor” contributing to the misdiagnoses, Dr. Lewis said. And another major problem was that patients’ response to standard treatment with intravenous immunoglobulins (current treatments have also come to include subcutaneous immunoglobulins) was not being measured objectively. Instead of evaluating patients using grip strength, walking tests, or other objective instruments, clinicians asked patients whether they felt better. “The problem is that IVIg makes people feel good,” Dr. Lewis said, “possibly by reducing normal inflammatory agents in the body.”
The 2015 paper caught the attention of neurologists and neuromuscular specialists worldwide, who reported similar problems with misdiagnosis. “And from there we did other work to try to dissect out what the more specific issues are,” Dr. Allen said. “The electrophysiology was a big one.”
Neurologist Nicholas Silvestri, MD, of the University at Buffalo in New York, one of the centers of excellence recognized by the CIDP-GBS Foundation, affirmed that nerve conduction studies, which essential to diagnosing CIDP, “are not as objective as we think they are. They’re very prone to user error and overinterpretation error. If they’re not performed appropriately, things can look like CIDP when they’re not. Very common forms of neuropathy, like diabetic neuropathy, can be misinterpreted as CIDP.”
The Challenge of Variants
After their 2015 paper on diagnostic pitfalls, Dr. Lewis and Dr. Allen, along with colleagues in the United States and Europe, started looking deeper into outcome measures and how to better follow and track patients with CIDP. In 2021 they helped create the first comprehensive clinical guidelines for CIDP in over a decade.
Much of their effort focused on atypical presentations, or what are now called variants, of CIDP — people with predominantly distal disease, asymmetrical symptomology, focal symptoms, or exclusively motor or sensory symptoms. With classical CIDP, “we don’t really have a problem with misdiagnosis,” Dr. Lewis said. With variants, however, misdiagnoses are extremely common. The 2021 guidelines try to address this, proposing differential diagnoses for each of the variants and ways to investigate them.
The guidelines also removed a subgroup of patients previously included as having CIDP. These patients, who comprise about 10% of cases, have antibodies to components of the Node of Ranvier, part of the axonal membrane, and the paranodal myelin. The autoimmune nodopathies do not respond to treatment with immunoglobulins or steroids in the way classical CIDP and its variants do. However, many patients have seen success with the immunotherapy rituximab.
“CIDP is a syndrome, not one disease,” Dr. Lewis said. “So it has been difficult to get guidelines or criteria that are sensitive to all the different forms of the disease, and yet specific for the disease and not overlapping. The nodopathies were pulled out because they don’t respond to usual treatments for CIDP. Hopefully over the years we’ll have even more specific diagnoses and can split out more patients.”
A Need for Better Biomarkers
With the neuromuscular autoimmune disease myasthenia gravis, 85% of patients have antibodies against the muscle acetylcholine receptor (AChR). Another 6% will have antibodies against muscle-specific kinase (MuSK).
Antibody profiles have long guided treatment decisions in myasthenia gravis, with AChR-positive patients responding to corticosteroids, IVIg, complement inhibitors, and other agents. MuSK-positive myasthenia gravis patients, similar to people with autoimmune nodopathies, respond poorly to IVIg but can have dramatic responses when treated with B cell–depleting therapies like rituximab.
Antibodies to nodal proteins neurofascin-155 and contactin-1 have been shown to be involved with the nodopathies. Assays for these are now commercially available, and Dr. Allen recommended that clinicians seek them for patients with a more rapid course, with tremor and ataxia, or who do not respond to standard CIDP treatments.
Still, no dominant autoantibody has been identified for the majority of presentations, including classical presentations. “I suspect it’s a heterogeneous group of multiple antibodies causing the disease,” Dr. Silvestri said. “That may explain to an extent the different manifestations and the different responses to treatment.”
Dr. Lewis said he thinks that, while more antibodies are likely to be discovered in the coming years, “we’re still identifying fewer than 20% of CIDP patients by specific antibodies, so we have a long way to go.”
Promising Trial Landscape
“CIDP is a challenging disease to study because of the diagnostic issues,” Dr. Allen said. “We know that a [nontrivial] percentage of patients ... can go into a drug-free remission. They actually don’t need treatment during that time. We don’t have any way to measure that. And if you put them in a clinical trial, it’s difficult to measure changes in the trial if they didn’t need the drug in the first place.”
In the global ADHERE trail, which looked at efgartigimod alfa and hyaluronidase-qvfc in CIDP patients, the investigators, led by Dr. Allen and Dr. Lewis, challenged patients to be off therapy for 12 weeks and allowed only those with active disease to enroll. They also used an adjudication panel of CIDP experts to review the records of each patient to assure patients had CIDP.
If two experts on the panel independently agreed that it was CIDP, Dr. Lewis said, then patients were eligible for enrollment. “If they both said they weren’t CIDP, they were not eligible. And if there was an argument between the two of them, then a third adjudicator would come in.”
About half of patients screened (n = 221) ended up included, and adjudication panels are now used in most CIDP trials.
The trial saw a positive outcome for efgartigimod alfa and hyaluronidase-qvfc, an antibody fragment that targets neonatal Fc receptor (FcRn), as a way to reduce to levels of pathogenic IgG autoantibodies. (The treatment was previously approved for myasthenia gravis.) The fact that two thirds of participants in the trial responded pointed to the likelihood that most CIDP patients have an IgG-related disease, Dr. Lewis said.
Different types of therapies are now being investigated in CIDP, among them other FcRn-inhibiting drugs and drugs inhibiting complement. Results from these trials may shed more light on the pathophysiology of the disease, which Dr. Silvestri said would be welcome.
“If I can test for antibodies, I can make a more timely diagnosis,” he said. “I’m assuming that some people with CIDP have non–antibody-driven disease. And in those cases, I want to avoid using drugs like Vyvgart, which are targeting antibodies. I want to give them a different therapy.”
Management: A Delicate Dance
Since the 1990s, the standard of care for CIDP has been IVIg and steroids. Newer subcutaneous immunoglobulin products, which take less time to administer, may be more convenient for patients than traditional IVIg and mitigate some concerning side effects.
Efgartigimod alfa and hyaluronidase-qvfc now offers an entirely different option that, while too new for clinicians to have much experience with in CIDP, represents further convenience for patients, with dosing in one 90-second subcutaneous injection per week.
In general, the sooner people are diagnosed and on therapy, the better they are likely to do, with fewer risks of irreversible axonal loss and disability. Referring to CIDP centers of excellence can help speed a definitive diagnosis.
Some patients will see a complete or near-complete recovery, while others will not. “It’s important to be up front with patients about what the benefit of treatments are, what are the expectations of treatment, what we can potentially get back, and what’s unlikely to come back,” Dr. Allen said. “We know that irreversible deficits are not uncommon in folks with CIDP. Part of that is driven by how severe their disease is or how long they’ve had it.”
Good CIDP management, according to the 2021 guidelines, involves making periodic dose reductions or withdrawing therapies on a trial basis, because people can and do experience remission. “We don’t have any test that tells us if somebody needs treatment or not. So this is the best we can do right now,” Dr. Allen said.
This process can be anxiety provoking for patients. “In my practice, there are no surprises,” he said. “We don’t typically say, ‘we’re going to stop your treatment today.’ It’s a discussion with a lead up that’s usually many months long.”
Management of CIDP also requires discussions to elicit when and whether worsening is occurring, along with a clear sense, by both patient and clinician, of what constitutes worsening.
Serial nerve conduction studies are not very useful, Dr. Lewis said, but objective disability measures are and should be more broadly adopted. These include the Medical Research Council sumscore, a test of 12 muscles that can determine weakness; a hand grip test; and functional disability scales such as Inflammatory Rasch Overall Disability Scale and Inflammatory Neuropathy Cause and Treatment scale. All are quick to administer in the office, and some can be done by the patient at home, providing the clinician useful information between visits.
“We could do a better job with educating [clinicians] on the value of different outcome measures that can really quantify disease activity,” Dr. Allen said, and pointed to the GBS-CIDP Foundation centers of excellence, which exist in most regions of the United States, as an outstanding resource for anyone wanting to know more.
“The centers are really, really helpful when you’re trying to work through some of these issues,” he said.
Suggested Reading
Allen JA and Lewis RA. Neurology. 2015 Aug 11;85(6):498-504. doi: 10.1212/WNL.0000000000001833.
Allen J et al. Neurology. 2024;102(17_supplement_1). doi: 10.1212/WNL-.0000000000206324.
Van den Bergh PYK et al. J Peripher Nerv Syst. 2021 Sep;26(3):242-268. doi: 10.1111/jns.12455.
Chronic inflammatory demyelinating polyradiculoneuropathy, or CIDP, is a rare immune-mediated nerve disorder characterized by progressive weakness and sensory impairment in the arms and legs, the result of an autoimmune attack on myelin.
Though some clustering of cases may occur in families, and susceptibility genes have been found, it is not considered a genetic disease. It can strike patients of either sex at any age, though most cases will occur in or after midlife.
Complicating matters further, CIDP has several variants whose symptoms differ from classical presentations.
Many patients who do not have CIDP end up being treated for it, and many CIDP patients experience delays to diagnosis and treatment that can potentially result in greater nerve damage and worse outcomes.
The good news, CIDP experts say, is that the last few years have seen important advances in diagnosis and treatment – including comprehensive new clinical guidelines and the June 2024 approval by the Food and Drug Administration of a new treatment, efgartigimod alfa and hyaluronidase-qvfc (Vyvgart, argenx). This antibody fragment represents the first non-steroid, non-immunoglobulin option for CIDP.
Despite the difficulties of recruiting patients with a tough-to-confirm disease that affects between 2 and 9 of every 100,000 people, according to the GPS-CIDP Foundation clinical trials have been successfully carried out in CIDP, and new ones continue to recruit. The experimental therapies being explored are based on a wide range of proposed disease pathways.
“It’s a very exciting time,” said Jeffrey Allen, MD, a neurologist at the University of Minnesota, Minneapolis, one of three CIDP experts who spoke about this challenging but treatable syndrome, its diagnosis and management, and the research questions that they hope to see answered.
Refining Diagnosis
In classical or typical CIDP, which accounts for most cases, patients present with progressive weakness and numbness that affects the arms and legs symmetrically, with the weakness being both proximal and distal. The disease usually evolves over a period of months, which helps distinguish it from Gullain-Barré syndrome, whose onset is more sudden and progression is less than 4 weeks.
CIDP was first described in the 1970s, and since that time more than a dozen sets of diagnostic criteria have been published. Starting about a decade ago, Dr. Allen and neurologist Richard Lewis, MD, of Cedars-Sinai Medical Center in Los Angeles, California, helped launch an effort to improve them.
“Experts in the field who were seeing patients with CIDP recognized that a lot of referrals coming to them were of people who actually didn’t have it, or they had the disease and were treated for it but didn’t need to be on treatment, or their treatment was very unconventional,” Dr. Allen said. “We wanted to try to put some data behind that.” In 2015 Dr. Allen and Dr. Lewis published a paper that found that nearly half of patients referred with a diagnosis of CIDP failed to meet basic diagnostic requirements.
Erroneous interpretation of nerve conduction studies “was a significant factor” contributing to the misdiagnoses, Dr. Lewis said. And another major problem was that patients’ response to standard treatment with intravenous immunoglobulins (current treatments have also come to include subcutaneous immunoglobulins) was not being measured objectively. Instead of evaluating patients using grip strength, walking tests, or other objective instruments, clinicians asked patients whether they felt better. “The problem is that IVIg makes people feel good,” Dr. Lewis said, “possibly by reducing normal inflammatory agents in the body.”
The 2015 paper caught the attention of neurologists and neuromuscular specialists worldwide, who reported similar problems with misdiagnosis. “And from there we did other work to try to dissect out what the more specific issues are,” Dr. Allen said. “The electrophysiology was a big one.”
Neurologist Nicholas Silvestri, MD, of the University at Buffalo in New York, one of the centers of excellence recognized by the CIDP-GBS Foundation, affirmed that nerve conduction studies, which essential to diagnosing CIDP, “are not as objective as we think they are. They’re very prone to user error and overinterpretation error. If they’re not performed appropriately, things can look like CIDP when they’re not. Very common forms of neuropathy, like diabetic neuropathy, can be misinterpreted as CIDP.”
The Challenge of Variants
After their 2015 paper on diagnostic pitfalls, Dr. Lewis and Dr. Allen, along with colleagues in the United States and Europe, started looking deeper into outcome measures and how to better follow and track patients with CIDP. In 2021 they helped create the first comprehensive clinical guidelines for CIDP in over a decade.
Much of their effort focused on atypical presentations, or what are now called variants, of CIDP — people with predominantly distal disease, asymmetrical symptomology, focal symptoms, or exclusively motor or sensory symptoms. With classical CIDP, “we don’t really have a problem with misdiagnosis,” Dr. Lewis said. With variants, however, misdiagnoses are extremely common. The 2021 guidelines try to address this, proposing differential diagnoses for each of the variants and ways to investigate them.
The guidelines also removed a subgroup of patients previously included as having CIDP. These patients, who comprise about 10% of cases, have antibodies to components of the Node of Ranvier, part of the axonal membrane, and the paranodal myelin. The autoimmune nodopathies do not respond to treatment with immunoglobulins or steroids in the way classical CIDP and its variants do. However, many patients have seen success with the immunotherapy rituximab.
“CIDP is a syndrome, not one disease,” Dr. Lewis said. “So it has been difficult to get guidelines or criteria that are sensitive to all the different forms of the disease, and yet specific for the disease and not overlapping. The nodopathies were pulled out because they don’t respond to usual treatments for CIDP. Hopefully over the years we’ll have even more specific diagnoses and can split out more patients.”
A Need for Better Biomarkers
With the neuromuscular autoimmune disease myasthenia gravis, 85% of patients have antibodies against the muscle acetylcholine receptor (AChR). Another 6% will have antibodies against muscle-specific kinase (MuSK).
Antibody profiles have long guided treatment decisions in myasthenia gravis, with AChR-positive patients responding to corticosteroids, IVIg, complement inhibitors, and other agents. MuSK-positive myasthenia gravis patients, similar to people with autoimmune nodopathies, respond poorly to IVIg but can have dramatic responses when treated with B cell–depleting therapies like rituximab.
Antibodies to nodal proteins neurofascin-155 and contactin-1 have been shown to be involved with the nodopathies. Assays for these are now commercially available, and Dr. Allen recommended that clinicians seek them for patients with a more rapid course, with tremor and ataxia, or who do not respond to standard CIDP treatments.
Still, no dominant autoantibody has been identified for the majority of presentations, including classical presentations. “I suspect it’s a heterogeneous group of multiple antibodies causing the disease,” Dr. Silvestri said. “That may explain to an extent the different manifestations and the different responses to treatment.”
Dr. Lewis said he thinks that, while more antibodies are likely to be discovered in the coming years, “we’re still identifying fewer than 20% of CIDP patients by specific antibodies, so we have a long way to go.”
Promising Trial Landscape
“CIDP is a challenging disease to study because of the diagnostic issues,” Dr. Allen said. “We know that a [nontrivial] percentage of patients ... can go into a drug-free remission. They actually don’t need treatment during that time. We don’t have any way to measure that. And if you put them in a clinical trial, it’s difficult to measure changes in the trial if they didn’t need the drug in the first place.”
In the global ADHERE trail, which looked at efgartigimod alfa and hyaluronidase-qvfc in CIDP patients, the investigators, led by Dr. Allen and Dr. Lewis, challenged patients to be off therapy for 12 weeks and allowed only those with active disease to enroll. They also used an adjudication panel of CIDP experts to review the records of each patient to assure patients had CIDP.
If two experts on the panel independently agreed that it was CIDP, Dr. Lewis said, then patients were eligible for enrollment. “If they both said they weren’t CIDP, they were not eligible. And if there was an argument between the two of them, then a third adjudicator would come in.”
About half of patients screened (n = 221) ended up included, and adjudication panels are now used in most CIDP trials.
The trial saw a positive outcome for efgartigimod alfa and hyaluronidase-qvfc, an antibody fragment that targets neonatal Fc receptor (FcRn), as a way to reduce to levels of pathogenic IgG autoantibodies. (The treatment was previously approved for myasthenia gravis.) The fact that two thirds of participants in the trial responded pointed to the likelihood that most CIDP patients have an IgG-related disease, Dr. Lewis said.
Different types of therapies are now being investigated in CIDP, among them other FcRn-inhibiting drugs and drugs inhibiting complement. Results from these trials may shed more light on the pathophysiology of the disease, which Dr. Silvestri said would be welcome.
“If I can test for antibodies, I can make a more timely diagnosis,” he said. “I’m assuming that some people with CIDP have non–antibody-driven disease. And in those cases, I want to avoid using drugs like Vyvgart, which are targeting antibodies. I want to give them a different therapy.”
Management: A Delicate Dance
Since the 1990s, the standard of care for CIDP has been IVIg and steroids. Newer subcutaneous immunoglobulin products, which take less time to administer, may be more convenient for patients than traditional IVIg and mitigate some concerning side effects.
Efgartigimod alfa and hyaluronidase-qvfc now offers an entirely different option that, while too new for clinicians to have much experience with in CIDP, represents further convenience for patients, with dosing in one 90-second subcutaneous injection per week.
In general, the sooner people are diagnosed and on therapy, the better they are likely to do, with fewer risks of irreversible axonal loss and disability. Referring to CIDP centers of excellence can help speed a definitive diagnosis.
Some patients will see a complete or near-complete recovery, while others will not. “It’s important to be up front with patients about what the benefit of treatments are, what are the expectations of treatment, what we can potentially get back, and what’s unlikely to come back,” Dr. Allen said. “We know that irreversible deficits are not uncommon in folks with CIDP. Part of that is driven by how severe their disease is or how long they’ve had it.”
Good CIDP management, according to the 2021 guidelines, involves making periodic dose reductions or withdrawing therapies on a trial basis, because people can and do experience remission. “We don’t have any test that tells us if somebody needs treatment or not. So this is the best we can do right now,” Dr. Allen said.
This process can be anxiety provoking for patients. “In my practice, there are no surprises,” he said. “We don’t typically say, ‘we’re going to stop your treatment today.’ It’s a discussion with a lead up that’s usually many months long.”
Management of CIDP also requires discussions to elicit when and whether worsening is occurring, along with a clear sense, by both patient and clinician, of what constitutes worsening.
Serial nerve conduction studies are not very useful, Dr. Lewis said, but objective disability measures are and should be more broadly adopted. These include the Medical Research Council sumscore, a test of 12 muscles that can determine weakness; a hand grip test; and functional disability scales such as Inflammatory Rasch Overall Disability Scale and Inflammatory Neuropathy Cause and Treatment scale. All are quick to administer in the office, and some can be done by the patient at home, providing the clinician useful information between visits.
“We could do a better job with educating [clinicians] on the value of different outcome measures that can really quantify disease activity,” Dr. Allen said, and pointed to the GBS-CIDP Foundation centers of excellence, which exist in most regions of the United States, as an outstanding resource for anyone wanting to know more.
“The centers are really, really helpful when you’re trying to work through some of these issues,” he said.
Suggested Reading
Allen JA and Lewis RA. Neurology. 2015 Aug 11;85(6):498-504. doi: 10.1212/WNL.0000000000001833.
Allen J et al. Neurology. 2024;102(17_supplement_1). doi: 10.1212/WNL-.0000000000206324.
Van den Bergh PYK et al. J Peripher Nerv Syst. 2021 Sep;26(3):242-268. doi: 10.1111/jns.12455.
Diagnosing and Managing Duchenne Muscular Dystrophy: Tips for Practicing Clinicians
Duchenne muscular dystrophy (DMD) is a severe progressive inherited disease characterized by muscle wasting and ultimately culminating in death. It’s a common enough neuromuscular disorder that pediatricians and family practice physicians are likely to see at least a couple of patients with DMD over the course of their career,” John Brandsema, MD, Neuromuscular Section Head, Division of Neurology, Children’s Hospital of Philadelphia in Pennsylvania, said in an interview. Healthcare providers should therefore be familiar with the disorder so as to provide timely diagnosis and early intervention as well as practical and emotional support to the patient and family/caregivers as they traverse the challenging and often heartbreaking journey with this condition.
Pathophysiology and Disease Trajectory
DMD is caused by pathogenic variants in the X-linked DMD gene, leading to reduction in dystrophin, a protein that serves as a cytoskeletal integrator, stabilizing the plasma membrane of striated muscle cells. Dystrophin is critical for muscle membrane stability.2 In particular, mutations in the gene that encodes for dystrophin lead to dysfunction in Dp427m, which is the muscle isoform of dystrophin.3,4
DMD is one of several types of muscular dystrophies. All are progressive disorders. Over time, healthy muscle fibers disappear and are replaced by fibrotic tissue and fat, making the muscles “less able to generate force for everyday activity.”2 Ultimately, the skeletal muscle dysfunction affects not only the patient’s day-to-day mobility but other systems as well. Most patients with DMD eventually die of cardiac and/or respiratory failure between the ages of 20 and 40 years, with a median life expectancy of 22 years — although children born after 1990 have a somewhat higher median life expectancy (28 years), because of the improving standard of care.3,5
Typically, DMD first presents with developmental delays and weakness in skeletal leg muscles. As the disease goes through stages of progression, it starts involving upper extremities and other systems. (Table 1)
Genetic Causes of DMD
The DMD gene, located on the X chromosome, encodes for the production of dystrophin. Variants of this gene result in the lack of dystrophin protein, leading in turn to muscle fiber degeneration and the progressive symptoms of DMD. Because of the gene’s location on the X chromosome, males (who don’t have a second copy of the X chromosome) cannot compensate for the mutated gene, which is why the disease affects male children. Females with this mutation are carriers and typically do not develop the same severity of symptoms, although they might have milder muscle cramps, weakness, and cardiac issues.3
A female carrier with DMD (or any other X-linked disorder) has a 25% chance to have a carrier daughter, a 25% change of having a noncarrier daughter, a 25% chance of having an affected son, and a 25% chance of having a nonaffected son. A male with the disorder will pass the mutated gene on to his daughters who then become carriers. He cannot pass the disorder on to his sons because males inherit only the Y chromosome from their fathers.3
Diagnosing DMD
“It can take as long as 1-3 years for a child to be diagnosed with DMD,” Dr. Brandsema said. “Parents typically have concerns and know that something is ‘off’ about their child and they’re sent to various specialists, but it usually takes time for an accurate diagnosis to be made.” The mean age at diagnosis of DMD is between ages 4 and 5 years.6
Early identification of infants at risk for developing DMD can help move the needle toward earlier diagnosis. Newborn screening for DMD has been researched and piloted in several programs.6 In 2023, DMD was nominated for inclusion in the Recommended Universal Screening Panel (RUSP) for universal newborn screening. But in May 2024, the advisory committee on Heritable Disorders in Newborns and Children decided to postpone the vote to include DMD in the RUSP, requesting additional information to ensure an evidence-based decision.
In the absence of universal newborn screening for DMD, alternative approaches have been proposed to reduce the delay in clinical diagnosis and specialist referral, including increasing awareness among healthcare providers (eg, pediatricians, pediatric neurologists, and primary care physicians).6
The National Task Force for Early Identification of Childhood Neuromuscular Disorders delineates the steps necessary to identify pediatric muscle weakness and signs of neuromuscular disease. Primary care providers are encouraged to engage in regular developmental surveillance. A surveillance aid lays out the timetable for recommended visits, typical developmental milestones, and components of surveillance. Clinical evaluation includes a detailed patient history, family history, and physical examination.
If a neuromuscular condition is suspected, laboratory work should include creatinine phosphokinase (CK).6 Elevated serum CK points to leakage of CK through the muscle membrane, suggesting muscle damage. If CK is elevated, genetic testing should be performed; and, if negative, it should be followed by genetic sequencing that tests for small-scale mutations in the DMD gene. If that test is negative, a muscle biopsy should be performed to test for deep intronic mutations in the DMD gene.4
The diagnostic process and immediate steps after a confirmed DMD diagnosis is found in Figure 1.
Targeting Inflammation in DMD
Traditionally, corticosteroids have been the only available medical treatment for DMD and they remain a cornerstone of DMD management. A meta-analysis found “moderate evidence” that corticosteroid therapy improves muscle strength and function in the short term (12 months), and strength up to 2 years.10
The two most common corticosteroids for DMD are prednisone and deflazacort. Deflazacort (Emflaza, PTC Therapeutics) was approved in 2017 to treat patients ages 5 years and older with DMD, subsequently expanded to 2 years and older. Deflazacort has been found to be more effective than prednisone in improving functional outcomes, delaying the onset of cardiomyopathy, and improving overall survival, with fewer adverse effects.11
In 2023, vamorolone (Agamree, Catalyst Pharmaceuticals) was approved by the Food and Drug Administration (FDA) to treat DMD patients (ages 2 years and older). Vamorolone is a dissociative steroidal anti-inflammatory that reduces bone morbidities and is regarded as a safer alternative than prednisone. A clinical trial comparing two doses of vamorolone with prednisone for 24 weeks found that vamorolone 6 mg/kg per day met the primary endpoint (time to stand velocity) and four sequential secondary motor function endpoints, with less bone morbidity, compared to prednisone.12 A more recent trial found improvements in motor outcomes at 48 weeks with a dose of 6 mg/kg per day of vamorolone. Bone morbidities of prednisone were reversed when the patient transitioned to vamorolone.13
“Steroid treatment has been proven to help, usually taken daily, although other schedules have been tried,” Dr. Brandsema said. However, all steroids are fraught with adverse effects and are suboptimal in the long term in reducing the disease burden.
The anti-inflammatory agent givinostat (Duvyzat, ITF Therapeutics), an oral histone deacetylase (HDAC) inhibitor, was approved in March 2024 for the treatment of DMD in patients 6 years of age and older. It is the first nonsteroidal drug to treat patients with all genetic variants of the disease, and it has a unique mechanism of action. Deficits in dystrophin can lead to increased HDAC activity in DMD, reducing the expression of genes involved in muscle regeneration. Givinostat therefore can help to counteract the pathogenic events downstream of dystrophin deficiency by inhibiting HDAC.14
Approval for givinostat was based on the phase 3 EPIDYS trial, which randomized 179 boys with DMD to receive either givinostat or placebo. Although results of a functional task worsened in both groups over the 12-month study period, the decline was significantly smaller with givinostat versus placebo. The most common adverse events were diarrhea and vomiting.14 Dr. Brandsema noted that monitoring of triglycerides and platelet count is required, as hypertriglyceridemia and thrombocytopenia can occur. This treatment was studied in tandem with corticosteroids as a combination approach to muscle stabilization.
New Pharmacotherapeutic Options: Exon-Skipping Agents
Today’s treatments have expanded beyond corticosteroids, with newer therapeutic options that include targeted exon-skipping therapies and, more recently, gene therapies. “These new treatment paradigms have changed the face of DMD treatment,” Dr. Brandsema said.
“Exon-skipping drugs in their current form have only a modest effect, but at least they’re a step in the right direction and a breakthrough, in terms of slowing disease progression,” Dr. Brandsema said.
Current exon-skipping agents use antisense phosphorodiamidate morpholino oligomers (PMOs) to restore a DMD open reading frame. Next-generation drugs called cell-penetrating peptide-conjugated PMOs (PPMOs) are being actively researched, Dr. Brandsema said. These agents have shown enhanced cellular uptake and more efficient dystrophin restoration, compared with unconjugated PMOs.15
There are currently four FDA-approved exon-skipping agents for DMD, all of which are administered via a weekly intravenous infusion: Casimersen (Amondys-45, SRP-4045), approved by the FDA in 2021; Eteplirsen (Exondys 51), approved in 2016; Golodirsen (Vyondys 53,SRP-4053), approved in 2019; and Vitolarsen (Viltepso), approved in 2020. They can be associated with multiple side effects, depending on the drug, including upper respiratory infection, fever, cough, rash, and gastrointestinal issues.16 These agents have the potential to help 30% of DMD patients, restoring low levels of dystrophin.16
Gene Transfer Therapies
Gene transfer therapies, a new class of agents, utilize a nonpathogenic viral vector (adeno-associated virus) to transfer specific genes to patients with DMD. Gene therapy involves overexpressing the micro-dystrophin gene to restore functional dystrophin expression.16
Multiple clinical trials of gene therapy are currently in progress. In 2023, delandistrogene moxeparvovec-rokl (Elevidys, Serepta) was granted accelerated FDA approval for ambulatory individuals with DMD between the ages of 4 and 5 years of age and a confirmed mutation in the DMD gene. It received expanded approval in June 2024 to include ambulatory and nonambulatory individuals aged 4 years and older with DMD and a confirmed mutation in the DMD gene (with the exception of exon 8 or 9 mutations).
The approval was based on preliminary data from two double-blind, placebo-controlled studies and two open-label studies, which enrolled a total of 218 male patients (including those who received placebo) with a confirmed disease-causing mutation in the DMD gene.
Delandistrogene moxeparvovec-rokl is delivered as a one-time infusion and has been associated with side effects and “a lot of potential issues,” Dr. Brandsema said. “We’ve seen cardiac effects, immune system effects, increased muscle inflammation and hepatic complications, and some people who became quite unwell were hospitalized for a long time.”
Fortunately, he added, “these seem to be rare but they do happen. Once the medication has been delivered, it’s permanently in the body, so you’re managing the side effects potentially on a long-term basis.”
It is critical to discuss the risks and benefits of this treatment with the family and caregivers and with the patient as well, if he old enough and able to participate in the decision-making progress. “We don’t want to give unrealistic expectations and we want people to be aware of the potential downside of this treatment,” he said. “This is a very complex discussion because the trajectory of the disease is so devastating and this treatment does hold out hope that other therapies don’t necessarily have.”
Nonpharmacologic Interventions
Physical therapy is a mainstay in DMD treatment, addressing protection of fragile muscles, preservation of strength, and prevention of muscle contractures.16 Given the respiratory impairments that occur with DMD progression, respiratory monitoring and therapy are essential; however, the number and type of evaluations and interventions vary with the stage of the disease, intensifying as the disease progresses.16 Similarly, cardiac monitoring should begin early, with patients screened for cardiac complications, and should intensify through the stages of disease progression.16
Bone health is compromised in patients with DMD, both as a result of corticosteroid treatment and as part of the disease itself. Fractures may be asymptomatic and may go unnoticed. Thus, bone health surveillance and maintenance are critical components of DMD management.16
Patients with DMD often experience gastrointestinal issues. They may experience weight gain because of lack of mobility and corticosteroid use in early stages, or weight loss as a result of diet or fluid imbalance, low bone density, or dysphagia in later stages. Patients should be closely followed by a nutritionist, a gastroenterologist as needed, and a physical therapist.16
Psychosocial support “should be developed and implemented across the lifespan in a manner that promotes thinking about the future and sets expectations that individuals will actively participate in their care and daily activities.”9 This includes psychological care, neuropsychological evaluations, and educational support.
Assisting Patients and Families Through the DMD Journey
DMD care is best delivered in a multidisciplinary setting, where physicians of relevant specialties, physical and occupational therapists, nutritionists, social workers, and genetic counselors collaborate. At Children’s Hospital of Philadelphia, DMD care is delivered through this collaborative model.
Unfortunately, Dr. Brandsema said, many patients don’t have this type of multidisciplinary resource available. “One specialist, such as a pulmonologist or neurologist, might have to be the sole source of care.” Or parents may have to ferry their child to multiple specialists in disparate locations, placing extra stress on an already-stressed family system.
“It’s helpful to connect the family with a comprehensive care center, if possible,” Dr. Brandsema advised. If that’s not available, then he suggests recommending educational opportunities and resources through national organizations such as the Muscular Dystrophy Association; Parent Project MD; NORD; Friends, Family and Duchenne; and Cure Duchenne. Families and caregivers, along with affected individuals, can get education and support from people who understand the day-to-day reality of living with this disease.
One of the major challenges that families face is navigating the high cost of treating DMD, especially the new medications, Dr. Brandsema said. “The authorization process can be intensive and long, and the family may need to take an active role, together with the provider team, in advocating for the patient to get access.”
Among her many responsibilities, Ms. Kaschak engages in care coordination tasks and management, helps patients and caregivers understand care plans, and provides psychosocial support and education about the disease process. She assists families in completing paperwork and navigating specialty authorizations, helping families understand and navigate the complex insurance process. “My role is to bridge gaps in care,” she said.
Dr. Brandsema noted that it’s important for couples to receive genetic counseling if they’re planning to have multiple children because there is a 50% chance that their next boy will be affected. About two thirds of mothers with children who have DMD are carriers, but many are not aware of it. Receiving counseling will enable them to understand their own risks of health complications, as well as the risk to future children.
Managing DMD Across the Lifespan
Another dimension of DMD care is providing resources and help to young people with DMD as they transition into adulthood. “In the past, we had limited treatment and mortality typically took place in the early 20s, so there weren’t a lot of patients who were adults. But as medication options have expanded and management of cardiac and respiratory failure has improved, we see a more significant proportion of adults who require adult-appropriate clinics — or, at the very least, specialists who are conversant in care or can provide care across the lifespan,” Dr. Brandsema said.
The DMD Care Considerations Working Group provides recommendations regarding care across the lifespan,9 as does the Adult North Star Network, of Muscular Dystrophy UK.17,18
Dr. Brandsema emphasized that, despite their disability, many adults with DMD “still engage with the community, and live life to its fullest.” It is to be hoped that, with ongoing research, earlier diagnosis, and improved treatment options, the future will look bright for people with DMD.
Dr. Brandsema has served as a consultant for Audentes, AveXis/Novartis, Biogen, Cytokinetics, Dyne, Edgewise, Fibrogen, Genentech, Marathon, Momenta/Janssen, NS Pharma, Pfizer, PTC Therapeutics, Sarepta, Scholar Rock, Takeda, and WaVe. He is on the medical advisory council member for Cure SMA and is a site investigator for clinical trials with Alexion, Astellas, AveXis/Novartis, Biogen, Biohaven, Catabasis, CSL Behring, Cytokinetics, Dyne, Fibrogen, Genentech, Ionis, Lilly, ML Bio, Pfizer, PTC Therapeutics, Sarepta, Scholar Rock, Summit, and WaVe. Ms. Kaschak has nothing to disclose.
References
1. Venugopal V and Pavlakis S. Duchenne Muscular Dystrophy. 2023 Jul 10. In: StatPearls [Internet]. Treasure Island, Florida: StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482346/.
2. Gao QQ and McNally EM. Compr Physiol. 2015 Jul 1;5(3):1223-39. doi: 10.1002/cphy.c140048.
3. Duan D et al. Nat Rev Dis Primers. 2021 Feb 18;7(1):13. doi: 10.1038/s41572-021-00248-3.
4. Aartsma-Rus A et al. J Pediatr. 2019 Jan:204:305-313.e14. doi: 10.1016/j.jpeds.2018.10.043.
5. Broomfield J et al. Neurology. 2021 Dec 7;97(23):e2304-e2314. doi: 10.1212/WNL.0000000000012910.
6. Mercuri E et al. Front Pediatr. 2023 Nov 10:11:1276144. doi: 10.1212/WNL.0000000000012910.
7. Birnkrant DJ et al. Lancet Neurol. 2018 Mar;17(3):251-267. doi: 10.1016/S1474-4422(18)30024-3.
8. Birnkrant DJ et al. Lancet Neurol. 2018 Apr;17(4):347-361. doi: 10.1016/S1474-4422(18)30025-5.
9. Birnkrant DJ et al. Lancet Neurol. 2018 May;17(5):445-455. doi: 10.1016/S1474-4422(18)30026-7.
10. Matthews E et al. Cochrane Database Syst Rev. 2016 May 5;2016(5):CD003725. doi: 10.1002/14651858.CD003725.pub4.
11. Bylo M et al. Ann Pharmacother. 2020 Aug;54(8):788-794. doi: 10.1177/1060028019900500.
12. Guglieri M et al. JAMA Neurol. 2022 Oct 1;79(10):1005-1014. doi: 10.1001/jamaneurol.2022.2480.
13. Dang UJ et al. Neurology. 2024 Mar 12;102(5):e208112. doi: 10.1212/WNL.0000000000208112.
14. Mercuri E et al. Lancet Neurol. 2024 Apr;23(4):393-403. doi: 10.1016/S1474-4422(24)00036-X.
15. Gushchina LV et al. Mol Ther Nucleic Acids. 2022 Nov 9:30:479-492. doi: 10.1016/j.omtn.2022.10.025.
16. Patterson G et al. Eur J Pharmacol. 2023 May 15:947:175675. doi: 10.1016/j.ejphar.2023.175675.
17. Quinlivan R et al. J Neuromuscul Dis. 2021;8(6):899-926. doi: 10.3233/JND-200609.
18. Narayan S et al. J Neuromuscul Dis. 2022;9(3):365-381. doi: 10.3233/JND-210707.
Duchenne muscular dystrophy (DMD) is a severe progressive inherited disease characterized by muscle wasting and ultimately culminating in death. It’s a common enough neuromuscular disorder that pediatricians and family practice physicians are likely to see at least a couple of patients with DMD over the course of their career,” John Brandsema, MD, Neuromuscular Section Head, Division of Neurology, Children’s Hospital of Philadelphia in Pennsylvania, said in an interview. Healthcare providers should therefore be familiar with the disorder so as to provide timely diagnosis and early intervention as well as practical and emotional support to the patient and family/caregivers as they traverse the challenging and often heartbreaking journey with this condition.
Pathophysiology and Disease Trajectory
DMD is caused by pathogenic variants in the X-linked DMD gene, leading to reduction in dystrophin, a protein that serves as a cytoskeletal integrator, stabilizing the plasma membrane of striated muscle cells. Dystrophin is critical for muscle membrane stability.2 In particular, mutations in the gene that encodes for dystrophin lead to dysfunction in Dp427m, which is the muscle isoform of dystrophin.3,4
DMD is one of several types of muscular dystrophies. All are progressive disorders. Over time, healthy muscle fibers disappear and are replaced by fibrotic tissue and fat, making the muscles “less able to generate force for everyday activity.”2 Ultimately, the skeletal muscle dysfunction affects not only the patient’s day-to-day mobility but other systems as well. Most patients with DMD eventually die of cardiac and/or respiratory failure between the ages of 20 and 40 years, with a median life expectancy of 22 years — although children born after 1990 have a somewhat higher median life expectancy (28 years), because of the improving standard of care.3,5
Typically, DMD first presents with developmental delays and weakness in skeletal leg muscles. As the disease goes through stages of progression, it starts involving upper extremities and other systems. (Table 1)
Genetic Causes of DMD
The DMD gene, located on the X chromosome, encodes for the production of dystrophin. Variants of this gene result in the lack of dystrophin protein, leading in turn to muscle fiber degeneration and the progressive symptoms of DMD. Because of the gene’s location on the X chromosome, males (who don’t have a second copy of the X chromosome) cannot compensate for the mutated gene, which is why the disease affects male children. Females with this mutation are carriers and typically do not develop the same severity of symptoms, although they might have milder muscle cramps, weakness, and cardiac issues.3
A female carrier with DMD (or any other X-linked disorder) has a 25% chance to have a carrier daughter, a 25% change of having a noncarrier daughter, a 25% chance of having an affected son, and a 25% chance of having a nonaffected son. A male with the disorder will pass the mutated gene on to his daughters who then become carriers. He cannot pass the disorder on to his sons because males inherit only the Y chromosome from their fathers.3
Diagnosing DMD
“It can take as long as 1-3 years for a child to be diagnosed with DMD,” Dr. Brandsema said. “Parents typically have concerns and know that something is ‘off’ about their child and they’re sent to various specialists, but it usually takes time for an accurate diagnosis to be made.” The mean age at diagnosis of DMD is between ages 4 and 5 years.6
Early identification of infants at risk for developing DMD can help move the needle toward earlier diagnosis. Newborn screening for DMD has been researched and piloted in several programs.6 In 2023, DMD was nominated for inclusion in the Recommended Universal Screening Panel (RUSP) for universal newborn screening. But in May 2024, the advisory committee on Heritable Disorders in Newborns and Children decided to postpone the vote to include DMD in the RUSP, requesting additional information to ensure an evidence-based decision.
In the absence of universal newborn screening for DMD, alternative approaches have been proposed to reduce the delay in clinical diagnosis and specialist referral, including increasing awareness among healthcare providers (eg, pediatricians, pediatric neurologists, and primary care physicians).6
The National Task Force for Early Identification of Childhood Neuromuscular Disorders delineates the steps necessary to identify pediatric muscle weakness and signs of neuromuscular disease. Primary care providers are encouraged to engage in regular developmental surveillance. A surveillance aid lays out the timetable for recommended visits, typical developmental milestones, and components of surveillance. Clinical evaluation includes a detailed patient history, family history, and physical examination.
If a neuromuscular condition is suspected, laboratory work should include creatinine phosphokinase (CK).6 Elevated serum CK points to leakage of CK through the muscle membrane, suggesting muscle damage. If CK is elevated, genetic testing should be performed; and, if negative, it should be followed by genetic sequencing that tests for small-scale mutations in the DMD gene. If that test is negative, a muscle biopsy should be performed to test for deep intronic mutations in the DMD gene.4
The diagnostic process and immediate steps after a confirmed DMD diagnosis is found in Figure 1.
Targeting Inflammation in DMD
Traditionally, corticosteroids have been the only available medical treatment for DMD and they remain a cornerstone of DMD management. A meta-analysis found “moderate evidence” that corticosteroid therapy improves muscle strength and function in the short term (12 months), and strength up to 2 years.10
The two most common corticosteroids for DMD are prednisone and deflazacort. Deflazacort (Emflaza, PTC Therapeutics) was approved in 2017 to treat patients ages 5 years and older with DMD, subsequently expanded to 2 years and older. Deflazacort has been found to be more effective than prednisone in improving functional outcomes, delaying the onset of cardiomyopathy, and improving overall survival, with fewer adverse effects.11
In 2023, vamorolone (Agamree, Catalyst Pharmaceuticals) was approved by the Food and Drug Administration (FDA) to treat DMD patients (ages 2 years and older). Vamorolone is a dissociative steroidal anti-inflammatory that reduces bone morbidities and is regarded as a safer alternative than prednisone. A clinical trial comparing two doses of vamorolone with prednisone for 24 weeks found that vamorolone 6 mg/kg per day met the primary endpoint (time to stand velocity) and four sequential secondary motor function endpoints, with less bone morbidity, compared to prednisone.12 A more recent trial found improvements in motor outcomes at 48 weeks with a dose of 6 mg/kg per day of vamorolone. Bone morbidities of prednisone were reversed when the patient transitioned to vamorolone.13
“Steroid treatment has been proven to help, usually taken daily, although other schedules have been tried,” Dr. Brandsema said. However, all steroids are fraught with adverse effects and are suboptimal in the long term in reducing the disease burden.
The anti-inflammatory agent givinostat (Duvyzat, ITF Therapeutics), an oral histone deacetylase (HDAC) inhibitor, was approved in March 2024 for the treatment of DMD in patients 6 years of age and older. It is the first nonsteroidal drug to treat patients with all genetic variants of the disease, and it has a unique mechanism of action. Deficits in dystrophin can lead to increased HDAC activity in DMD, reducing the expression of genes involved in muscle regeneration. Givinostat therefore can help to counteract the pathogenic events downstream of dystrophin deficiency by inhibiting HDAC.14
Approval for givinostat was based on the phase 3 EPIDYS trial, which randomized 179 boys with DMD to receive either givinostat or placebo. Although results of a functional task worsened in both groups over the 12-month study period, the decline was significantly smaller with givinostat versus placebo. The most common adverse events were diarrhea and vomiting.14 Dr. Brandsema noted that monitoring of triglycerides and platelet count is required, as hypertriglyceridemia and thrombocytopenia can occur. This treatment was studied in tandem with corticosteroids as a combination approach to muscle stabilization.
New Pharmacotherapeutic Options: Exon-Skipping Agents
Today’s treatments have expanded beyond corticosteroids, with newer therapeutic options that include targeted exon-skipping therapies and, more recently, gene therapies. “These new treatment paradigms have changed the face of DMD treatment,” Dr. Brandsema said.
“Exon-skipping drugs in their current form have only a modest effect, but at least they’re a step in the right direction and a breakthrough, in terms of slowing disease progression,” Dr. Brandsema said.
Current exon-skipping agents use antisense phosphorodiamidate morpholino oligomers (PMOs) to restore a DMD open reading frame. Next-generation drugs called cell-penetrating peptide-conjugated PMOs (PPMOs) are being actively researched, Dr. Brandsema said. These agents have shown enhanced cellular uptake and more efficient dystrophin restoration, compared with unconjugated PMOs.15
There are currently four FDA-approved exon-skipping agents for DMD, all of which are administered via a weekly intravenous infusion: Casimersen (Amondys-45, SRP-4045), approved by the FDA in 2021; Eteplirsen (Exondys 51), approved in 2016; Golodirsen (Vyondys 53,SRP-4053), approved in 2019; and Vitolarsen (Viltepso), approved in 2020. They can be associated with multiple side effects, depending on the drug, including upper respiratory infection, fever, cough, rash, and gastrointestinal issues.16 These agents have the potential to help 30% of DMD patients, restoring low levels of dystrophin.16
Gene Transfer Therapies
Gene transfer therapies, a new class of agents, utilize a nonpathogenic viral vector (adeno-associated virus) to transfer specific genes to patients with DMD. Gene therapy involves overexpressing the micro-dystrophin gene to restore functional dystrophin expression.16
Multiple clinical trials of gene therapy are currently in progress. In 2023, delandistrogene moxeparvovec-rokl (Elevidys, Serepta) was granted accelerated FDA approval for ambulatory individuals with DMD between the ages of 4 and 5 years of age and a confirmed mutation in the DMD gene. It received expanded approval in June 2024 to include ambulatory and nonambulatory individuals aged 4 years and older with DMD and a confirmed mutation in the DMD gene (with the exception of exon 8 or 9 mutations).
The approval was based on preliminary data from two double-blind, placebo-controlled studies and two open-label studies, which enrolled a total of 218 male patients (including those who received placebo) with a confirmed disease-causing mutation in the DMD gene.
Delandistrogene moxeparvovec-rokl is delivered as a one-time infusion and has been associated with side effects and “a lot of potential issues,” Dr. Brandsema said. “We’ve seen cardiac effects, immune system effects, increased muscle inflammation and hepatic complications, and some people who became quite unwell were hospitalized for a long time.”
Fortunately, he added, “these seem to be rare but they do happen. Once the medication has been delivered, it’s permanently in the body, so you’re managing the side effects potentially on a long-term basis.”
It is critical to discuss the risks and benefits of this treatment with the family and caregivers and with the patient as well, if he old enough and able to participate in the decision-making progress. “We don’t want to give unrealistic expectations and we want people to be aware of the potential downside of this treatment,” he said. “This is a very complex discussion because the trajectory of the disease is so devastating and this treatment does hold out hope that other therapies don’t necessarily have.”
Nonpharmacologic Interventions
Physical therapy is a mainstay in DMD treatment, addressing protection of fragile muscles, preservation of strength, and prevention of muscle contractures.16 Given the respiratory impairments that occur with DMD progression, respiratory monitoring and therapy are essential; however, the number and type of evaluations and interventions vary with the stage of the disease, intensifying as the disease progresses.16 Similarly, cardiac monitoring should begin early, with patients screened for cardiac complications, and should intensify through the stages of disease progression.16
Bone health is compromised in patients with DMD, both as a result of corticosteroid treatment and as part of the disease itself. Fractures may be asymptomatic and may go unnoticed. Thus, bone health surveillance and maintenance are critical components of DMD management.16
Patients with DMD often experience gastrointestinal issues. They may experience weight gain because of lack of mobility and corticosteroid use in early stages, or weight loss as a result of diet or fluid imbalance, low bone density, or dysphagia in later stages. Patients should be closely followed by a nutritionist, a gastroenterologist as needed, and a physical therapist.16
Psychosocial support “should be developed and implemented across the lifespan in a manner that promotes thinking about the future and sets expectations that individuals will actively participate in their care and daily activities.”9 This includes psychological care, neuropsychological evaluations, and educational support.
Assisting Patients and Families Through the DMD Journey
DMD care is best delivered in a multidisciplinary setting, where physicians of relevant specialties, physical and occupational therapists, nutritionists, social workers, and genetic counselors collaborate. At Children’s Hospital of Philadelphia, DMD care is delivered through this collaborative model.
Unfortunately, Dr. Brandsema said, many patients don’t have this type of multidisciplinary resource available. “One specialist, such as a pulmonologist or neurologist, might have to be the sole source of care.” Or parents may have to ferry their child to multiple specialists in disparate locations, placing extra stress on an already-stressed family system.
“It’s helpful to connect the family with a comprehensive care center, if possible,” Dr. Brandsema advised. If that’s not available, then he suggests recommending educational opportunities and resources through national organizations such as the Muscular Dystrophy Association; Parent Project MD; NORD; Friends, Family and Duchenne; and Cure Duchenne. Families and caregivers, along with affected individuals, can get education and support from people who understand the day-to-day reality of living with this disease.
One of the major challenges that families face is navigating the high cost of treating DMD, especially the new medications, Dr. Brandsema said. “The authorization process can be intensive and long, and the family may need to take an active role, together with the provider team, in advocating for the patient to get access.”
Among her many responsibilities, Ms. Kaschak engages in care coordination tasks and management, helps patients and caregivers understand care plans, and provides psychosocial support and education about the disease process. She assists families in completing paperwork and navigating specialty authorizations, helping families understand and navigate the complex insurance process. “My role is to bridge gaps in care,” she said.
Dr. Brandsema noted that it’s important for couples to receive genetic counseling if they’re planning to have multiple children because there is a 50% chance that their next boy will be affected. About two thirds of mothers with children who have DMD are carriers, but many are not aware of it. Receiving counseling will enable them to understand their own risks of health complications, as well as the risk to future children.
Managing DMD Across the Lifespan
Another dimension of DMD care is providing resources and help to young people with DMD as they transition into adulthood. “In the past, we had limited treatment and mortality typically took place in the early 20s, so there weren’t a lot of patients who were adults. But as medication options have expanded and management of cardiac and respiratory failure has improved, we see a more significant proportion of adults who require adult-appropriate clinics — or, at the very least, specialists who are conversant in care or can provide care across the lifespan,” Dr. Brandsema said.
The DMD Care Considerations Working Group provides recommendations regarding care across the lifespan,9 as does the Adult North Star Network, of Muscular Dystrophy UK.17,18
Dr. Brandsema emphasized that, despite their disability, many adults with DMD “still engage with the community, and live life to its fullest.” It is to be hoped that, with ongoing research, earlier diagnosis, and improved treatment options, the future will look bright for people with DMD.
Dr. Brandsema has served as a consultant for Audentes, AveXis/Novartis, Biogen, Cytokinetics, Dyne, Edgewise, Fibrogen, Genentech, Marathon, Momenta/Janssen, NS Pharma, Pfizer, PTC Therapeutics, Sarepta, Scholar Rock, Takeda, and WaVe. He is on the medical advisory council member for Cure SMA and is a site investigator for clinical trials with Alexion, Astellas, AveXis/Novartis, Biogen, Biohaven, Catabasis, CSL Behring, Cytokinetics, Dyne, Fibrogen, Genentech, Ionis, Lilly, ML Bio, Pfizer, PTC Therapeutics, Sarepta, Scholar Rock, Summit, and WaVe. Ms. Kaschak has nothing to disclose.
References
1. Venugopal V and Pavlakis S. Duchenne Muscular Dystrophy. 2023 Jul 10. In: StatPearls [Internet]. Treasure Island, Florida: StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482346/.
2. Gao QQ and McNally EM. Compr Physiol. 2015 Jul 1;5(3):1223-39. doi: 10.1002/cphy.c140048.
3. Duan D et al. Nat Rev Dis Primers. 2021 Feb 18;7(1):13. doi: 10.1038/s41572-021-00248-3.
4. Aartsma-Rus A et al. J Pediatr. 2019 Jan:204:305-313.e14. doi: 10.1016/j.jpeds.2018.10.043.
5. Broomfield J et al. Neurology. 2021 Dec 7;97(23):e2304-e2314. doi: 10.1212/WNL.0000000000012910.
6. Mercuri E et al. Front Pediatr. 2023 Nov 10:11:1276144. doi: 10.1212/WNL.0000000000012910.
7. Birnkrant DJ et al. Lancet Neurol. 2018 Mar;17(3):251-267. doi: 10.1016/S1474-4422(18)30024-3.
8. Birnkrant DJ et al. Lancet Neurol. 2018 Apr;17(4):347-361. doi: 10.1016/S1474-4422(18)30025-5.
9. Birnkrant DJ et al. Lancet Neurol. 2018 May;17(5):445-455. doi: 10.1016/S1474-4422(18)30026-7.
10. Matthews E et al. Cochrane Database Syst Rev. 2016 May 5;2016(5):CD003725. doi: 10.1002/14651858.CD003725.pub4.
11. Bylo M et al. Ann Pharmacother. 2020 Aug;54(8):788-794. doi: 10.1177/1060028019900500.
12. Guglieri M et al. JAMA Neurol. 2022 Oct 1;79(10):1005-1014. doi: 10.1001/jamaneurol.2022.2480.
13. Dang UJ et al. Neurology. 2024 Mar 12;102(5):e208112. doi: 10.1212/WNL.0000000000208112.
14. Mercuri E et al. Lancet Neurol. 2024 Apr;23(4):393-403. doi: 10.1016/S1474-4422(24)00036-X.
15. Gushchina LV et al. Mol Ther Nucleic Acids. 2022 Nov 9:30:479-492. doi: 10.1016/j.omtn.2022.10.025.
16. Patterson G et al. Eur J Pharmacol. 2023 May 15:947:175675. doi: 10.1016/j.ejphar.2023.175675.
17. Quinlivan R et al. J Neuromuscul Dis. 2021;8(6):899-926. doi: 10.3233/JND-200609.
18. Narayan S et al. J Neuromuscul Dis. 2022;9(3):365-381. doi: 10.3233/JND-210707.
Duchenne muscular dystrophy (DMD) is a severe progressive inherited disease characterized by muscle wasting and ultimately culminating in death. It’s a common enough neuromuscular disorder that pediatricians and family practice physicians are likely to see at least a couple of patients with DMD over the course of their career,” John Brandsema, MD, Neuromuscular Section Head, Division of Neurology, Children’s Hospital of Philadelphia in Pennsylvania, said in an interview. Healthcare providers should therefore be familiar with the disorder so as to provide timely diagnosis and early intervention as well as practical and emotional support to the patient and family/caregivers as they traverse the challenging and often heartbreaking journey with this condition.
Pathophysiology and Disease Trajectory
DMD is caused by pathogenic variants in the X-linked DMD gene, leading to reduction in dystrophin, a protein that serves as a cytoskeletal integrator, stabilizing the plasma membrane of striated muscle cells. Dystrophin is critical for muscle membrane stability.2 In particular, mutations in the gene that encodes for dystrophin lead to dysfunction in Dp427m, which is the muscle isoform of dystrophin.3,4
DMD is one of several types of muscular dystrophies. All are progressive disorders. Over time, healthy muscle fibers disappear and are replaced by fibrotic tissue and fat, making the muscles “less able to generate force for everyday activity.”2 Ultimately, the skeletal muscle dysfunction affects not only the patient’s day-to-day mobility but other systems as well. Most patients with DMD eventually die of cardiac and/or respiratory failure between the ages of 20 and 40 years, with a median life expectancy of 22 years — although children born after 1990 have a somewhat higher median life expectancy (28 years), because of the improving standard of care.3,5
Typically, DMD first presents with developmental delays and weakness in skeletal leg muscles. As the disease goes through stages of progression, it starts involving upper extremities and other systems. (Table 1)
Genetic Causes of DMD
The DMD gene, located on the X chromosome, encodes for the production of dystrophin. Variants of this gene result in the lack of dystrophin protein, leading in turn to muscle fiber degeneration and the progressive symptoms of DMD. Because of the gene’s location on the X chromosome, males (who don’t have a second copy of the X chromosome) cannot compensate for the mutated gene, which is why the disease affects male children. Females with this mutation are carriers and typically do not develop the same severity of symptoms, although they might have milder muscle cramps, weakness, and cardiac issues.3
A female carrier with DMD (or any other X-linked disorder) has a 25% chance to have a carrier daughter, a 25% change of having a noncarrier daughter, a 25% chance of having an affected son, and a 25% chance of having a nonaffected son. A male with the disorder will pass the mutated gene on to his daughters who then become carriers. He cannot pass the disorder on to his sons because males inherit only the Y chromosome from their fathers.3
Diagnosing DMD
“It can take as long as 1-3 years for a child to be diagnosed with DMD,” Dr. Brandsema said. “Parents typically have concerns and know that something is ‘off’ about their child and they’re sent to various specialists, but it usually takes time for an accurate diagnosis to be made.” The mean age at diagnosis of DMD is between ages 4 and 5 years.6
Early identification of infants at risk for developing DMD can help move the needle toward earlier diagnosis. Newborn screening for DMD has been researched and piloted in several programs.6 In 2023, DMD was nominated for inclusion in the Recommended Universal Screening Panel (RUSP) for universal newborn screening. But in May 2024, the advisory committee on Heritable Disorders in Newborns and Children decided to postpone the vote to include DMD in the RUSP, requesting additional information to ensure an evidence-based decision.
In the absence of universal newborn screening for DMD, alternative approaches have been proposed to reduce the delay in clinical diagnosis and specialist referral, including increasing awareness among healthcare providers (eg, pediatricians, pediatric neurologists, and primary care physicians).6
The National Task Force for Early Identification of Childhood Neuromuscular Disorders delineates the steps necessary to identify pediatric muscle weakness and signs of neuromuscular disease. Primary care providers are encouraged to engage in regular developmental surveillance. A surveillance aid lays out the timetable for recommended visits, typical developmental milestones, and components of surveillance. Clinical evaluation includes a detailed patient history, family history, and physical examination.
If a neuromuscular condition is suspected, laboratory work should include creatinine phosphokinase (CK).6 Elevated serum CK points to leakage of CK through the muscle membrane, suggesting muscle damage. If CK is elevated, genetic testing should be performed; and, if negative, it should be followed by genetic sequencing that tests for small-scale mutations in the DMD gene. If that test is negative, a muscle biopsy should be performed to test for deep intronic mutations in the DMD gene.4
The diagnostic process and immediate steps after a confirmed DMD diagnosis is found in Figure 1.
Targeting Inflammation in DMD
Traditionally, corticosteroids have been the only available medical treatment for DMD and they remain a cornerstone of DMD management. A meta-analysis found “moderate evidence” that corticosteroid therapy improves muscle strength and function in the short term (12 months), and strength up to 2 years.10
The two most common corticosteroids for DMD are prednisone and deflazacort. Deflazacort (Emflaza, PTC Therapeutics) was approved in 2017 to treat patients ages 5 years and older with DMD, subsequently expanded to 2 years and older. Deflazacort has been found to be more effective than prednisone in improving functional outcomes, delaying the onset of cardiomyopathy, and improving overall survival, with fewer adverse effects.11
In 2023, vamorolone (Agamree, Catalyst Pharmaceuticals) was approved by the Food and Drug Administration (FDA) to treat DMD patients (ages 2 years and older). Vamorolone is a dissociative steroidal anti-inflammatory that reduces bone morbidities and is regarded as a safer alternative than prednisone. A clinical trial comparing two doses of vamorolone with prednisone for 24 weeks found that vamorolone 6 mg/kg per day met the primary endpoint (time to stand velocity) and four sequential secondary motor function endpoints, with less bone morbidity, compared to prednisone.12 A more recent trial found improvements in motor outcomes at 48 weeks with a dose of 6 mg/kg per day of vamorolone. Bone morbidities of prednisone were reversed when the patient transitioned to vamorolone.13
“Steroid treatment has been proven to help, usually taken daily, although other schedules have been tried,” Dr. Brandsema said. However, all steroids are fraught with adverse effects and are suboptimal in the long term in reducing the disease burden.
The anti-inflammatory agent givinostat (Duvyzat, ITF Therapeutics), an oral histone deacetylase (HDAC) inhibitor, was approved in March 2024 for the treatment of DMD in patients 6 years of age and older. It is the first nonsteroidal drug to treat patients with all genetic variants of the disease, and it has a unique mechanism of action. Deficits in dystrophin can lead to increased HDAC activity in DMD, reducing the expression of genes involved in muscle regeneration. Givinostat therefore can help to counteract the pathogenic events downstream of dystrophin deficiency by inhibiting HDAC.14
Approval for givinostat was based on the phase 3 EPIDYS trial, which randomized 179 boys with DMD to receive either givinostat or placebo. Although results of a functional task worsened in both groups over the 12-month study period, the decline was significantly smaller with givinostat versus placebo. The most common adverse events were diarrhea and vomiting.14 Dr. Brandsema noted that monitoring of triglycerides and platelet count is required, as hypertriglyceridemia and thrombocytopenia can occur. This treatment was studied in tandem with corticosteroids as a combination approach to muscle stabilization.
New Pharmacotherapeutic Options: Exon-Skipping Agents
Today’s treatments have expanded beyond corticosteroids, with newer therapeutic options that include targeted exon-skipping therapies and, more recently, gene therapies. “These new treatment paradigms have changed the face of DMD treatment,” Dr. Brandsema said.
“Exon-skipping drugs in their current form have only a modest effect, but at least they’re a step in the right direction and a breakthrough, in terms of slowing disease progression,” Dr. Brandsema said.
Current exon-skipping agents use antisense phosphorodiamidate morpholino oligomers (PMOs) to restore a DMD open reading frame. Next-generation drugs called cell-penetrating peptide-conjugated PMOs (PPMOs) are being actively researched, Dr. Brandsema said. These agents have shown enhanced cellular uptake and more efficient dystrophin restoration, compared with unconjugated PMOs.15
There are currently four FDA-approved exon-skipping agents for DMD, all of which are administered via a weekly intravenous infusion: Casimersen (Amondys-45, SRP-4045), approved by the FDA in 2021; Eteplirsen (Exondys 51), approved in 2016; Golodirsen (Vyondys 53,SRP-4053), approved in 2019; and Vitolarsen (Viltepso), approved in 2020. They can be associated with multiple side effects, depending on the drug, including upper respiratory infection, fever, cough, rash, and gastrointestinal issues.16 These agents have the potential to help 30% of DMD patients, restoring low levels of dystrophin.16
Gene Transfer Therapies
Gene transfer therapies, a new class of agents, utilize a nonpathogenic viral vector (adeno-associated virus) to transfer specific genes to patients with DMD. Gene therapy involves overexpressing the micro-dystrophin gene to restore functional dystrophin expression.16
Multiple clinical trials of gene therapy are currently in progress. In 2023, delandistrogene moxeparvovec-rokl (Elevidys, Serepta) was granted accelerated FDA approval for ambulatory individuals with DMD between the ages of 4 and 5 years of age and a confirmed mutation in the DMD gene. It received expanded approval in June 2024 to include ambulatory and nonambulatory individuals aged 4 years and older with DMD and a confirmed mutation in the DMD gene (with the exception of exon 8 or 9 mutations).
The approval was based on preliminary data from two double-blind, placebo-controlled studies and two open-label studies, which enrolled a total of 218 male patients (including those who received placebo) with a confirmed disease-causing mutation in the DMD gene.
Delandistrogene moxeparvovec-rokl is delivered as a one-time infusion and has been associated with side effects and “a lot of potential issues,” Dr. Brandsema said. “We’ve seen cardiac effects, immune system effects, increased muscle inflammation and hepatic complications, and some people who became quite unwell were hospitalized for a long time.”
Fortunately, he added, “these seem to be rare but they do happen. Once the medication has been delivered, it’s permanently in the body, so you’re managing the side effects potentially on a long-term basis.”
It is critical to discuss the risks and benefits of this treatment with the family and caregivers and with the patient as well, if he old enough and able to participate in the decision-making progress. “We don’t want to give unrealistic expectations and we want people to be aware of the potential downside of this treatment,” he said. “This is a very complex discussion because the trajectory of the disease is so devastating and this treatment does hold out hope that other therapies don’t necessarily have.”
Nonpharmacologic Interventions
Physical therapy is a mainstay in DMD treatment, addressing protection of fragile muscles, preservation of strength, and prevention of muscle contractures.16 Given the respiratory impairments that occur with DMD progression, respiratory monitoring and therapy are essential; however, the number and type of evaluations and interventions vary with the stage of the disease, intensifying as the disease progresses.16 Similarly, cardiac monitoring should begin early, with patients screened for cardiac complications, and should intensify through the stages of disease progression.16
Bone health is compromised in patients with DMD, both as a result of corticosteroid treatment and as part of the disease itself. Fractures may be asymptomatic and may go unnoticed. Thus, bone health surveillance and maintenance are critical components of DMD management.16
Patients with DMD often experience gastrointestinal issues. They may experience weight gain because of lack of mobility and corticosteroid use in early stages, or weight loss as a result of diet or fluid imbalance, low bone density, or dysphagia in later stages. Patients should be closely followed by a nutritionist, a gastroenterologist as needed, and a physical therapist.16
Psychosocial support “should be developed and implemented across the lifespan in a manner that promotes thinking about the future and sets expectations that individuals will actively participate in their care and daily activities.”9 This includes psychological care, neuropsychological evaluations, and educational support.
Assisting Patients and Families Through the DMD Journey
DMD care is best delivered in a multidisciplinary setting, where physicians of relevant specialties, physical and occupational therapists, nutritionists, social workers, and genetic counselors collaborate. At Children’s Hospital of Philadelphia, DMD care is delivered through this collaborative model.
Unfortunately, Dr. Brandsema said, many patients don’t have this type of multidisciplinary resource available. “One specialist, such as a pulmonologist or neurologist, might have to be the sole source of care.” Or parents may have to ferry their child to multiple specialists in disparate locations, placing extra stress on an already-stressed family system.
“It’s helpful to connect the family with a comprehensive care center, if possible,” Dr. Brandsema advised. If that’s not available, then he suggests recommending educational opportunities and resources through national organizations such as the Muscular Dystrophy Association; Parent Project MD; NORD; Friends, Family and Duchenne; and Cure Duchenne. Families and caregivers, along with affected individuals, can get education and support from people who understand the day-to-day reality of living with this disease.
One of the major challenges that families face is navigating the high cost of treating DMD, especially the new medications, Dr. Brandsema said. “The authorization process can be intensive and long, and the family may need to take an active role, together with the provider team, in advocating for the patient to get access.”
Among her many responsibilities, Ms. Kaschak engages in care coordination tasks and management, helps patients and caregivers understand care plans, and provides psychosocial support and education about the disease process. She assists families in completing paperwork and navigating specialty authorizations, helping families understand and navigate the complex insurance process. “My role is to bridge gaps in care,” she said.
Dr. Brandsema noted that it’s important for couples to receive genetic counseling if they’re planning to have multiple children because there is a 50% chance that their next boy will be affected. About two thirds of mothers with children who have DMD are carriers, but many are not aware of it. Receiving counseling will enable them to understand their own risks of health complications, as well as the risk to future children.
Managing DMD Across the Lifespan
Another dimension of DMD care is providing resources and help to young people with DMD as they transition into adulthood. “In the past, we had limited treatment and mortality typically took place in the early 20s, so there weren’t a lot of patients who were adults. But as medication options have expanded and management of cardiac and respiratory failure has improved, we see a more significant proportion of adults who require adult-appropriate clinics — or, at the very least, specialists who are conversant in care or can provide care across the lifespan,” Dr. Brandsema said.
The DMD Care Considerations Working Group provides recommendations regarding care across the lifespan,9 as does the Adult North Star Network, of Muscular Dystrophy UK.17,18
Dr. Brandsema emphasized that, despite their disability, many adults with DMD “still engage with the community, and live life to its fullest.” It is to be hoped that, with ongoing research, earlier diagnosis, and improved treatment options, the future will look bright for people with DMD.
Dr. Brandsema has served as a consultant for Audentes, AveXis/Novartis, Biogen, Cytokinetics, Dyne, Edgewise, Fibrogen, Genentech, Marathon, Momenta/Janssen, NS Pharma, Pfizer, PTC Therapeutics, Sarepta, Scholar Rock, Takeda, and WaVe. He is on the medical advisory council member for Cure SMA and is a site investigator for clinical trials with Alexion, Astellas, AveXis/Novartis, Biogen, Biohaven, Catabasis, CSL Behring, Cytokinetics, Dyne, Fibrogen, Genentech, Ionis, Lilly, ML Bio, Pfizer, PTC Therapeutics, Sarepta, Scholar Rock, Summit, and WaVe. Ms. Kaschak has nothing to disclose.
References
1. Venugopal V and Pavlakis S. Duchenne Muscular Dystrophy. 2023 Jul 10. In: StatPearls [Internet]. Treasure Island, Florida: StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482346/.
2. Gao QQ and McNally EM. Compr Physiol. 2015 Jul 1;5(3):1223-39. doi: 10.1002/cphy.c140048.
3. Duan D et al. Nat Rev Dis Primers. 2021 Feb 18;7(1):13. doi: 10.1038/s41572-021-00248-3.
4. Aartsma-Rus A et al. J Pediatr. 2019 Jan:204:305-313.e14. doi: 10.1016/j.jpeds.2018.10.043.
5. Broomfield J et al. Neurology. 2021 Dec 7;97(23):e2304-e2314. doi: 10.1212/WNL.0000000000012910.
6. Mercuri E et al. Front Pediatr. 2023 Nov 10:11:1276144. doi: 10.1212/WNL.0000000000012910.
7. Birnkrant DJ et al. Lancet Neurol. 2018 Mar;17(3):251-267. doi: 10.1016/S1474-4422(18)30024-3.
8. Birnkrant DJ et al. Lancet Neurol. 2018 Apr;17(4):347-361. doi: 10.1016/S1474-4422(18)30025-5.
9. Birnkrant DJ et al. Lancet Neurol. 2018 May;17(5):445-455. doi: 10.1016/S1474-4422(18)30026-7.
10. Matthews E et al. Cochrane Database Syst Rev. 2016 May 5;2016(5):CD003725. doi: 10.1002/14651858.CD003725.pub4.
11. Bylo M et al. Ann Pharmacother. 2020 Aug;54(8):788-794. doi: 10.1177/1060028019900500.
12. Guglieri M et al. JAMA Neurol. 2022 Oct 1;79(10):1005-1014. doi: 10.1001/jamaneurol.2022.2480.
13. Dang UJ et al. Neurology. 2024 Mar 12;102(5):e208112. doi: 10.1212/WNL.0000000000208112.
14. Mercuri E et al. Lancet Neurol. 2024 Apr;23(4):393-403. doi: 10.1016/S1474-4422(24)00036-X.
15. Gushchina LV et al. Mol Ther Nucleic Acids. 2022 Nov 9:30:479-492. doi: 10.1016/j.omtn.2022.10.025.
16. Patterson G et al. Eur J Pharmacol. 2023 May 15:947:175675. doi: 10.1016/j.ejphar.2023.175675.
17. Quinlivan R et al. J Neuromuscul Dis. 2021;8(6):899-926. doi: 10.3233/JND-200609.
18. Narayan S et al. J Neuromuscul Dis. 2022;9(3):365-381. doi: 10.3233/JND-210707.