User login
Repeat TAVR outcomes ‘reassuring’
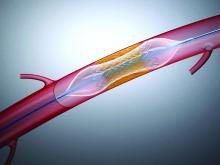
Redo transcatheter aortic valve replacement (TAVR) is a reasonably safe and effective option for selected patients with valve dysfunction after TAVR, new registry data suggest.
“Redo TAVR is about to become a much more common procedure and it’s reassuring to see that the outcomes that can be achieved by these procedures are quite good,” said Uri Landes, MD, Vancouver General Hospital, British Columbia, Canada.
Landes and colleagues reported results from the Redo-TAVR Registry in the April 28 issue of the Journal of the American College of Cardiology.
The Redo-TAVR Registry is an investigator-initiated effort designed to collect information on patients who undergo a second TAVR within a dysfunctional transcatheter heart valve (THV).
From 63,876 TAVR procedures done at 37 participating centers, 212 (0.33%) were redo-TAVR procedures. Seventy-four of the redo procedures were done within 1 year of the initial TAVR and the remaining 138 were beyond 1 year. Median time from TAVR-to-redo-TAVR for these two groups was 68 (38 to 154) days and 5 (3 to 6) years, respectively.
“It’s important to understand that this is probably a highly selected group of patients and these numbers do no reliably reflect the ratio of patients who will need a redo TAVR,” said Landes in an interview with theheart.org | Medscape Cardiology.
“We don’t know how many patients were excluded from redo TAVR because of prohibitive anatomical factors, such as an anticipated high risk for coronary occlusion, or a patient prosthesis mismatch. Also, some of these individuals received their THVs more recently, so if they will suffer THV valve dysfunction, it may not have happened yet,” he added.
In the early redo group, the indication for redo-TAVR was most often combined aortic THV stenosis and regurgitation (83.8%). Pure THV stenosis was seen in only 16.2% of patients.
For those with redo procedures after 1 year, THV stenosis was seen in 51 (37.0%) patients and regurgitation or combined stenosis-regurgitation in 86 (62.3%).
Device success using VARC-2 criteria was achieved in 85.1%, with no difference seen between those presenting within or beyond 1 year. Most failures were attributable to high residual gradients (14.1%) or regurgitation (8.9%).
No significant difference was seen in 30-day (94.6% and 98.5%) and 1-year survival (83.6% and 88.3%) in patients who presented within 1 year or later.
At 30-day and 1-year follow-up, residual gradients were 12.6 ± 7.5 mm Hg and 12.9 ± 9.0 mm Hg, respectively. High residual gradients (320 mm Hg) were seen in about 14% of patients.
Aortic valve areas were 1.63 ± 0.61 cm2 at 30 days and 1.51 ± 0.57 cm2 at 1 year. Regurgitation was mild or less in 91% of patients at both time points.
Periprocedural complication rates were relatively low. There were three strokes (1.4%), one valve malposition (3.3%), two coronary obstructions (0.9%), and 20 new permanent pacemaker implants (9.6%). Importantly, no procedure-related mortality was seen, only one patient converted to open heart surgery, and symptomatic improvements were substantial.
“We are currently working on an analysis that compares TAVI-in-TAVI versus TAVI in surgical valves, and we are happy to see that it appears as if TAVI-in-TAVI outcomes don’t fall short,” said Landes. More analysis is also needed to see if perhaps some THVs work better or worse for redo procedures.
“We also want to understand which of the many combinations of heart valves available are better than others, thinking that supra-annular leaflets inside intra-annular leaflet devices may function differently than vice versa,” said Landes.
Vinod Thourani, MD, chief of cardiovascular surgery at Piedmont Heart Institute, Atlanta, considers these new observational data “reassuring” and “robust,” albeit with some limitations. He was first author on an editorial comment on this paper and spoke to theheart.org | Medscape Cardiology.
“This is unadjudicated registry data but you can’t lie about death and I feel good seeing that if you need a second TAVR inside of a TAVR, your mortality risk is pretty good,” said Thourani.
That said, he questions whether these data can really be extrapolated to lower-risk patients. “I think this is an early snapshot and it’s a relatively big sample, but it’s a selected sample and we don’t know how many patients needed redo TAVR and didn’t get it or didn’t want it,” he added.
On the comforting side, there has been ongoing concern that a redo procedure that involves “propping open” a degenerated TAVR prosthesis’s leaflets with a new TAVR valve may occlude the coronary ostium by closing the flow within the open cells.
“Luckily, the investigators show an extremely low risk of coronary obstruction of only 0.9% in an anatomically high-risk patient population,” he said. This incidence, however, may increase as the use of TAVR rises in younger and less risky patients, he added.
Thourani would also like to see a longer follow-up on these patients. Median follow-up post redo TAVR was 15 months in this analysis.
“What I think we need to concentrate on as we do these studies is the life-long management of aortic stenosis wherein we try to minimize the overall number of invasive procedures as much as we can,” said Thourani.
Landes reported no conflict of interest. Thourani reported he is an advisor and/or researcher for Abbott Vascular, Boston Scientific, and Edwards Lifesciences.
This article first appeared on Medscape.com.
Redo transcatheter aortic valve replacement (TAVR) is a reasonably safe and effective option for selected patients with valve dysfunction after TAVR, new registry data suggest.
“Redo TAVR is about to become a much more common procedure and it’s reassuring to see that the outcomes that can be achieved by these procedures are quite good,” said Uri Landes, MD, Vancouver General Hospital, British Columbia, Canada.
Landes and colleagues reported results from the Redo-TAVR Registry in the April 28 issue of the Journal of the American College of Cardiology.
The Redo-TAVR Registry is an investigator-initiated effort designed to collect information on patients who undergo a second TAVR within a dysfunctional transcatheter heart valve (THV).
From 63,876 TAVR procedures done at 37 participating centers, 212 (0.33%) were redo-TAVR procedures. Seventy-four of the redo procedures were done within 1 year of the initial TAVR and the remaining 138 were beyond 1 year. Median time from TAVR-to-redo-TAVR for these two groups was 68 (38 to 154) days and 5 (3 to 6) years, respectively.
“It’s important to understand that this is probably a highly selected group of patients and these numbers do no reliably reflect the ratio of patients who will need a redo TAVR,” said Landes in an interview with theheart.org | Medscape Cardiology.
“We don’t know how many patients were excluded from redo TAVR because of prohibitive anatomical factors, such as an anticipated high risk for coronary occlusion, or a patient prosthesis mismatch. Also, some of these individuals received their THVs more recently, so if they will suffer THV valve dysfunction, it may not have happened yet,” he added.
In the early redo group, the indication for redo-TAVR was most often combined aortic THV stenosis and regurgitation (83.8%). Pure THV stenosis was seen in only 16.2% of patients.
For those with redo procedures after 1 year, THV stenosis was seen in 51 (37.0%) patients and regurgitation or combined stenosis-regurgitation in 86 (62.3%).
Device success using VARC-2 criteria was achieved in 85.1%, with no difference seen between those presenting within or beyond 1 year. Most failures were attributable to high residual gradients (14.1%) or regurgitation (8.9%).
No significant difference was seen in 30-day (94.6% and 98.5%) and 1-year survival (83.6% and 88.3%) in patients who presented within 1 year or later.
At 30-day and 1-year follow-up, residual gradients were 12.6 ± 7.5 mm Hg and 12.9 ± 9.0 mm Hg, respectively. High residual gradients (320 mm Hg) were seen in about 14% of patients.
Aortic valve areas were 1.63 ± 0.61 cm2 at 30 days and 1.51 ± 0.57 cm2 at 1 year. Regurgitation was mild or less in 91% of patients at both time points.
Periprocedural complication rates were relatively low. There were three strokes (1.4%), one valve malposition (3.3%), two coronary obstructions (0.9%), and 20 new permanent pacemaker implants (9.6%). Importantly, no procedure-related mortality was seen, only one patient converted to open heart surgery, and symptomatic improvements were substantial.
“We are currently working on an analysis that compares TAVI-in-TAVI versus TAVI in surgical valves, and we are happy to see that it appears as if TAVI-in-TAVI outcomes don’t fall short,” said Landes. More analysis is also needed to see if perhaps some THVs work better or worse for redo procedures.
“We also want to understand which of the many combinations of heart valves available are better than others, thinking that supra-annular leaflets inside intra-annular leaflet devices may function differently than vice versa,” said Landes.
Vinod Thourani, MD, chief of cardiovascular surgery at Piedmont Heart Institute, Atlanta, considers these new observational data “reassuring” and “robust,” albeit with some limitations. He was first author on an editorial comment on this paper and spoke to theheart.org | Medscape Cardiology.
“This is unadjudicated registry data but you can’t lie about death and I feel good seeing that if you need a second TAVR inside of a TAVR, your mortality risk is pretty good,” said Thourani.
That said, he questions whether these data can really be extrapolated to lower-risk patients. “I think this is an early snapshot and it’s a relatively big sample, but it’s a selected sample and we don’t know how many patients needed redo TAVR and didn’t get it or didn’t want it,” he added.
On the comforting side, there has been ongoing concern that a redo procedure that involves “propping open” a degenerated TAVR prosthesis’s leaflets with a new TAVR valve may occlude the coronary ostium by closing the flow within the open cells.
“Luckily, the investigators show an extremely low risk of coronary obstruction of only 0.9% in an anatomically high-risk patient population,” he said. This incidence, however, may increase as the use of TAVR rises in younger and less risky patients, he added.
Thourani would also like to see a longer follow-up on these patients. Median follow-up post redo TAVR was 15 months in this analysis.
“What I think we need to concentrate on as we do these studies is the life-long management of aortic stenosis wherein we try to minimize the overall number of invasive procedures as much as we can,” said Thourani.
Landes reported no conflict of interest. Thourani reported he is an advisor and/or researcher for Abbott Vascular, Boston Scientific, and Edwards Lifesciences.
This article first appeared on Medscape.com.
Redo transcatheter aortic valve replacement (TAVR) is a reasonably safe and effective option for selected patients with valve dysfunction after TAVR, new registry data suggest.
“Redo TAVR is about to become a much more common procedure and it’s reassuring to see that the outcomes that can be achieved by these procedures are quite good,” said Uri Landes, MD, Vancouver General Hospital, British Columbia, Canada.
Landes and colleagues reported results from the Redo-TAVR Registry in the April 28 issue of the Journal of the American College of Cardiology.
The Redo-TAVR Registry is an investigator-initiated effort designed to collect information on patients who undergo a second TAVR within a dysfunctional transcatheter heart valve (THV).
From 63,876 TAVR procedures done at 37 participating centers, 212 (0.33%) were redo-TAVR procedures. Seventy-four of the redo procedures were done within 1 year of the initial TAVR and the remaining 138 were beyond 1 year. Median time from TAVR-to-redo-TAVR for these two groups was 68 (38 to 154) days and 5 (3 to 6) years, respectively.
“It’s important to understand that this is probably a highly selected group of patients and these numbers do no reliably reflect the ratio of patients who will need a redo TAVR,” said Landes in an interview with theheart.org | Medscape Cardiology.
“We don’t know how many patients were excluded from redo TAVR because of prohibitive anatomical factors, such as an anticipated high risk for coronary occlusion, or a patient prosthesis mismatch. Also, some of these individuals received their THVs more recently, so if they will suffer THV valve dysfunction, it may not have happened yet,” he added.
In the early redo group, the indication for redo-TAVR was most often combined aortic THV stenosis and regurgitation (83.8%). Pure THV stenosis was seen in only 16.2% of patients.
For those with redo procedures after 1 year, THV stenosis was seen in 51 (37.0%) patients and regurgitation or combined stenosis-regurgitation in 86 (62.3%).
Device success using VARC-2 criteria was achieved in 85.1%, with no difference seen between those presenting within or beyond 1 year. Most failures were attributable to high residual gradients (14.1%) or regurgitation (8.9%).
No significant difference was seen in 30-day (94.6% and 98.5%) and 1-year survival (83.6% and 88.3%) in patients who presented within 1 year or later.
At 30-day and 1-year follow-up, residual gradients were 12.6 ± 7.5 mm Hg and 12.9 ± 9.0 mm Hg, respectively. High residual gradients (320 mm Hg) were seen in about 14% of patients.
Aortic valve areas were 1.63 ± 0.61 cm2 at 30 days and 1.51 ± 0.57 cm2 at 1 year. Regurgitation was mild or less in 91% of patients at both time points.
Periprocedural complication rates were relatively low. There were three strokes (1.4%), one valve malposition (3.3%), two coronary obstructions (0.9%), and 20 new permanent pacemaker implants (9.6%). Importantly, no procedure-related mortality was seen, only one patient converted to open heart surgery, and symptomatic improvements were substantial.
“We are currently working on an analysis that compares TAVI-in-TAVI versus TAVI in surgical valves, and we are happy to see that it appears as if TAVI-in-TAVI outcomes don’t fall short,” said Landes. More analysis is also needed to see if perhaps some THVs work better or worse for redo procedures.
“We also want to understand which of the many combinations of heart valves available are better than others, thinking that supra-annular leaflets inside intra-annular leaflet devices may function differently than vice versa,” said Landes.
Vinod Thourani, MD, chief of cardiovascular surgery at Piedmont Heart Institute, Atlanta, considers these new observational data “reassuring” and “robust,” albeit with some limitations. He was first author on an editorial comment on this paper and spoke to theheart.org | Medscape Cardiology.
“This is unadjudicated registry data but you can’t lie about death and I feel good seeing that if you need a second TAVR inside of a TAVR, your mortality risk is pretty good,” said Thourani.
That said, he questions whether these data can really be extrapolated to lower-risk patients. “I think this is an early snapshot and it’s a relatively big sample, but it’s a selected sample and we don’t know how many patients needed redo TAVR and didn’t get it or didn’t want it,” he added.
On the comforting side, there has been ongoing concern that a redo procedure that involves “propping open” a degenerated TAVR prosthesis’s leaflets with a new TAVR valve may occlude the coronary ostium by closing the flow within the open cells.
“Luckily, the investigators show an extremely low risk of coronary obstruction of only 0.9% in an anatomically high-risk patient population,” he said. This incidence, however, may increase as the use of TAVR rises in younger and less risky patients, he added.
Thourani would also like to see a longer follow-up on these patients. Median follow-up post redo TAVR was 15 months in this analysis.
“What I think we need to concentrate on as we do these studies is the life-long management of aortic stenosis wherein we try to minimize the overall number of invasive procedures as much as we can,” said Thourani.
Landes reported no conflict of interest. Thourani reported he is an advisor and/or researcher for Abbott Vascular, Boston Scientific, and Edwards Lifesciences.
This article first appeared on Medscape.com.
Substantial very late MACE risk after PCI for SIHD
Patients with stable ischemic heart disease remain at substantial risk for major adverse cardiovascular events 1-5 years after percutaneous coronary intervention, even with contemporary second-generation drug-eluting stents, according to a pooled analysis of long-term follow-up data on 10,987 patients in 19 prospective, randomized, head-to-head metallic stent trials.
The analysis showed that, although most major adverse cardiovascular events (MACE) occurred during the first year after stenting, no plateau in MACE was reached between years 1 and 5, Mahesh V. Madhavan, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“Further studies are required to understand the mechanisms of late events and whether improvements in stent technology, revascularization technique, and adjunctive therapies may improve outcomes in patients with SIHD [stable ischemic heart disease],” said Dr. Madhavan, a cardiology fellow at Columbia University Irving Medical Center and New York–Presbyterian Hospital.
This post hoc analysis of pooled individual patient-level data from 19 randomized trials included 10,987 metallic stent recipients with SIHD. Sixty-one percent got second-generation drug-eluting stents (DES), 25% received first-generation DES, and 15% got bare metal stents (BMS). The largest prospective head-to-head RCT was SPIRIT IV, with 2,130 patients. All five TAXUS trials were also included.
The 5-year rate of the primary composite MACE endpoint composed of cardiac death, MI, or ischemia-driven target lesion revascularization was 24.1% in patients with BMS stents, 17.9% with first-gen DES, and 13.4% with second-gen DES, reflecting the advances in stent technology over time. Most of these MACE events occurred during the first year after PCI, with rates of 18%, 8.6%, and 5.3%, respectively, in the three groups. However, the MACE rate beyond the first year out through year 5 remained substantial: 10.2% with first-gen DES, 8.5% with second-gen DES, and 7.4% in the BMS group.
The cardiac death rate from PCI through year 5 was 3.8% with second-gen DES, 3.6% with first-gen DES, and 3.3% with BMS. The MI rate was 7.7% with first-gen DES, 6.1% with BMS, and 5% with second-gen DES.
Stent thrombosis occurred during the first year in 0.9% of first-gen DES and BMS recipients and in 0.7% of patients with second-gen DES. During years 1-5, the rates were 1.6% with first-gen DES, 0.9% with second-gen devices, and 0.2% with BMS.
Second-gen DES provided a big advantage in terms of lessened need for ischemia-driven target lesion revascularization through the first 5 years, with a rate of 7.3%, compared to 18.7% in patients with first-gen DES and 10.5% with BMS.
In a multivariate regression analysis, independent predictors of MACE in the first 5 years post PCI included indicators of greater lesion and/or procedural complexity, such as left main or left anterior descending disease, greater lesion length, and more than one treated lesion, as well as standard cardiovascular risk factors, including recent smoking, hypertension, and diabetes.
In contrast, hyperlipidemia was associated with a significant 15% reduction in MACE risk, which in an interview Dr. Madhavan said may have been due to aggressive lipid-lowering therapy, although he added that this is conjecture because he and his coinvestigators didn’t have access to data on the use of guideline-directed medical therapy or antiplatelet regimens.
Asked about future prospects for reducing the substantial very late risk of MACE highlighted in his study, Dr. Madhavan cited the use of adjunctive imaging during PCI as promising.
“The currently enrolling ILUMEN IV trial, among other studies, will help determine whether imaging-guided intervention can help improve intermediate and long-term rates of MACE,” he observed.
Promising medical therapies that could potentially confer benefit in terms of reducing long-term MACE in patients who’ve undergone PCI for SIHD include novel lipid-lowering drugs, tailored antithrombotic strategies, new anti-inflammatory agents, and the SGLT2 inhibitors, Dr. Madhavan continued.
In terms of advances in stent design, he cited recent evidence that ultrathin-strut stents featuring bioresorbable polymer, such as the Orsiro stent, may reduce late stent-related MACE through 3 years.
“We’ll have to see if these benefits extend to longer-term follow-up up to 5 years,” he said.
He deemed his study results “fairly consistent” with those of the ISCHEMIA trial, where ischemic events in the patients with SIHD assigned to an initial invasive strategy continued to occur in the latter years of follow-up without any clear plateau effect (N Engl J Med. 2020 Apr 9;382[15]:1395-407).
Dr. Madhavan reported no financial conflicts regarding his study, funded by an institutional research grant from the National Heart, Lung, and Blood Institute.
Shortly following Dr. Madhavan’s presentation at ACC 2020, the study results were published online (Circ Cardiovasc Interv. 2020 Apr;13[4[:e008565. doi: 10.1161/CIRCINTERVENTIONS.119.008565).
SOURCE: Madhavan MV. ACC 2020, Abstract 909-10.
Patients with stable ischemic heart disease remain at substantial risk for major adverse cardiovascular events 1-5 years after percutaneous coronary intervention, even with contemporary second-generation drug-eluting stents, according to a pooled analysis of long-term follow-up data on 10,987 patients in 19 prospective, randomized, head-to-head metallic stent trials.
The analysis showed that, although most major adverse cardiovascular events (MACE) occurred during the first year after stenting, no plateau in MACE was reached between years 1 and 5, Mahesh V. Madhavan, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“Further studies are required to understand the mechanisms of late events and whether improvements in stent technology, revascularization technique, and adjunctive therapies may improve outcomes in patients with SIHD [stable ischemic heart disease],” said Dr. Madhavan, a cardiology fellow at Columbia University Irving Medical Center and New York–Presbyterian Hospital.
This post hoc analysis of pooled individual patient-level data from 19 randomized trials included 10,987 metallic stent recipients with SIHD. Sixty-one percent got second-generation drug-eluting stents (DES), 25% received first-generation DES, and 15% got bare metal stents (BMS). The largest prospective head-to-head RCT was SPIRIT IV, with 2,130 patients. All five TAXUS trials were also included.
The 5-year rate of the primary composite MACE endpoint composed of cardiac death, MI, or ischemia-driven target lesion revascularization was 24.1% in patients with BMS stents, 17.9% with first-gen DES, and 13.4% with second-gen DES, reflecting the advances in stent technology over time. Most of these MACE events occurred during the first year after PCI, with rates of 18%, 8.6%, and 5.3%, respectively, in the three groups. However, the MACE rate beyond the first year out through year 5 remained substantial: 10.2% with first-gen DES, 8.5% with second-gen DES, and 7.4% in the BMS group.
The cardiac death rate from PCI through year 5 was 3.8% with second-gen DES, 3.6% with first-gen DES, and 3.3% with BMS. The MI rate was 7.7% with first-gen DES, 6.1% with BMS, and 5% with second-gen DES.
Stent thrombosis occurred during the first year in 0.9% of first-gen DES and BMS recipients and in 0.7% of patients with second-gen DES. During years 1-5, the rates were 1.6% with first-gen DES, 0.9% with second-gen devices, and 0.2% with BMS.
Second-gen DES provided a big advantage in terms of lessened need for ischemia-driven target lesion revascularization through the first 5 years, with a rate of 7.3%, compared to 18.7% in patients with first-gen DES and 10.5% with BMS.
In a multivariate regression analysis, independent predictors of MACE in the first 5 years post PCI included indicators of greater lesion and/or procedural complexity, such as left main or left anterior descending disease, greater lesion length, and more than one treated lesion, as well as standard cardiovascular risk factors, including recent smoking, hypertension, and diabetes.
In contrast, hyperlipidemia was associated with a significant 15% reduction in MACE risk, which in an interview Dr. Madhavan said may have been due to aggressive lipid-lowering therapy, although he added that this is conjecture because he and his coinvestigators didn’t have access to data on the use of guideline-directed medical therapy or antiplatelet regimens.
Asked about future prospects for reducing the substantial very late risk of MACE highlighted in his study, Dr. Madhavan cited the use of adjunctive imaging during PCI as promising.
“The currently enrolling ILUMEN IV trial, among other studies, will help determine whether imaging-guided intervention can help improve intermediate and long-term rates of MACE,” he observed.
Promising medical therapies that could potentially confer benefit in terms of reducing long-term MACE in patients who’ve undergone PCI for SIHD include novel lipid-lowering drugs, tailored antithrombotic strategies, new anti-inflammatory agents, and the SGLT2 inhibitors, Dr. Madhavan continued.
In terms of advances in stent design, he cited recent evidence that ultrathin-strut stents featuring bioresorbable polymer, such as the Orsiro stent, may reduce late stent-related MACE through 3 years.
“We’ll have to see if these benefits extend to longer-term follow-up up to 5 years,” he said.
He deemed his study results “fairly consistent” with those of the ISCHEMIA trial, where ischemic events in the patients with SIHD assigned to an initial invasive strategy continued to occur in the latter years of follow-up without any clear plateau effect (N Engl J Med. 2020 Apr 9;382[15]:1395-407).
Dr. Madhavan reported no financial conflicts regarding his study, funded by an institutional research grant from the National Heart, Lung, and Blood Institute.
Shortly following Dr. Madhavan’s presentation at ACC 2020, the study results were published online (Circ Cardiovasc Interv. 2020 Apr;13[4[:e008565. doi: 10.1161/CIRCINTERVENTIONS.119.008565).
SOURCE: Madhavan MV. ACC 2020, Abstract 909-10.
Patients with stable ischemic heart disease remain at substantial risk for major adverse cardiovascular events 1-5 years after percutaneous coronary intervention, even with contemporary second-generation drug-eluting stents, according to a pooled analysis of long-term follow-up data on 10,987 patients in 19 prospective, randomized, head-to-head metallic stent trials.
The analysis showed that, although most major adverse cardiovascular events (MACE) occurred during the first year after stenting, no plateau in MACE was reached between years 1 and 5, Mahesh V. Madhavan, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
“Further studies are required to understand the mechanisms of late events and whether improvements in stent technology, revascularization technique, and adjunctive therapies may improve outcomes in patients with SIHD [stable ischemic heart disease],” said Dr. Madhavan, a cardiology fellow at Columbia University Irving Medical Center and New York–Presbyterian Hospital.
This post hoc analysis of pooled individual patient-level data from 19 randomized trials included 10,987 metallic stent recipients with SIHD. Sixty-one percent got second-generation drug-eluting stents (DES), 25% received first-generation DES, and 15% got bare metal stents (BMS). The largest prospective head-to-head RCT was SPIRIT IV, with 2,130 patients. All five TAXUS trials were also included.
The 5-year rate of the primary composite MACE endpoint composed of cardiac death, MI, or ischemia-driven target lesion revascularization was 24.1% in patients with BMS stents, 17.9% with first-gen DES, and 13.4% with second-gen DES, reflecting the advances in stent technology over time. Most of these MACE events occurred during the first year after PCI, with rates of 18%, 8.6%, and 5.3%, respectively, in the three groups. However, the MACE rate beyond the first year out through year 5 remained substantial: 10.2% with first-gen DES, 8.5% with second-gen DES, and 7.4% in the BMS group.
The cardiac death rate from PCI through year 5 was 3.8% with second-gen DES, 3.6% with first-gen DES, and 3.3% with BMS. The MI rate was 7.7% with first-gen DES, 6.1% with BMS, and 5% with second-gen DES.
Stent thrombosis occurred during the first year in 0.9% of first-gen DES and BMS recipients and in 0.7% of patients with second-gen DES. During years 1-5, the rates were 1.6% with first-gen DES, 0.9% with second-gen devices, and 0.2% with BMS.
Second-gen DES provided a big advantage in terms of lessened need for ischemia-driven target lesion revascularization through the first 5 years, with a rate of 7.3%, compared to 18.7% in patients with first-gen DES and 10.5% with BMS.
In a multivariate regression analysis, independent predictors of MACE in the first 5 years post PCI included indicators of greater lesion and/or procedural complexity, such as left main or left anterior descending disease, greater lesion length, and more than one treated lesion, as well as standard cardiovascular risk factors, including recent smoking, hypertension, and diabetes.
In contrast, hyperlipidemia was associated with a significant 15% reduction in MACE risk, which in an interview Dr. Madhavan said may have been due to aggressive lipid-lowering therapy, although he added that this is conjecture because he and his coinvestigators didn’t have access to data on the use of guideline-directed medical therapy or antiplatelet regimens.
Asked about future prospects for reducing the substantial very late risk of MACE highlighted in his study, Dr. Madhavan cited the use of adjunctive imaging during PCI as promising.
“The currently enrolling ILUMEN IV trial, among other studies, will help determine whether imaging-guided intervention can help improve intermediate and long-term rates of MACE,” he observed.
Promising medical therapies that could potentially confer benefit in terms of reducing long-term MACE in patients who’ve undergone PCI for SIHD include novel lipid-lowering drugs, tailored antithrombotic strategies, new anti-inflammatory agents, and the SGLT2 inhibitors, Dr. Madhavan continued.
In terms of advances in stent design, he cited recent evidence that ultrathin-strut stents featuring bioresorbable polymer, such as the Orsiro stent, may reduce late stent-related MACE through 3 years.
“We’ll have to see if these benefits extend to longer-term follow-up up to 5 years,” he said.
He deemed his study results “fairly consistent” with those of the ISCHEMIA trial, where ischemic events in the patients with SIHD assigned to an initial invasive strategy continued to occur in the latter years of follow-up without any clear plateau effect (N Engl J Med. 2020 Apr 9;382[15]:1395-407).
Dr. Madhavan reported no financial conflicts regarding his study, funded by an institutional research grant from the National Heart, Lung, and Blood Institute.
Shortly following Dr. Madhavan’s presentation at ACC 2020, the study results were published online (Circ Cardiovasc Interv. 2020 Apr;13[4[:e008565. doi: 10.1161/CIRCINTERVENTIONS.119.008565).
SOURCE: Madhavan MV. ACC 2020, Abstract 909-10.
FROM ACC 20
AUGUSTUS: After ACS or PCI, aspirin gives AFib patients scant benefit
When patients with atrial fibrillation have an acute coronary syndrome event or undergo percutaneous coronary intervention, their window of opportunity for benefiting from a triple antithrombotic regimen was, at best, about 30 days, according to a post hoc analysis of AUGUSTUS, a multicenter, randomized trial with more than 4,600 patients.
Beyond 30 days out to 180 days, the incremental benefit from reduced ischemic events fell to essentially zero, giving it a clear back seat to the ongoing, increased bleeding risk from adding a third antithrombotic drug.
Patients randomized to receive aspirin in addition to an anticoagulant, either apixaban or a vitamin K antagonist such as warfarin, and a P2Y12 inhibitor such as clopidogrel “for up to approximately 30 days” had a roughly similar decrease in severe ischemic events and increase in severe bleeding events, suggesting that even acutely the overall impact of adding aspirin on top of the other two antithrombotics was a wash, John H. Alexander, MD, said in a presentation of research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
Using aspirin as a third antithrombotic in patients with atrial fibrillation (AFib) who have also recently had either an acute coronary syndrome event (ACS) or underwent percutaneous coronary intervention (PCI), “may be reasonable,” for selected patients, but is a decision that requires careful individualization, cautioned Dr. Alexander, professor of medicine and director of Cardiovascular Research at the Duke Clinical Research Institute of Duke University, Durham, N.C.
“This is a superb secondary analysis looking at the time course of potential benefit and harm with aspirin, and they found that aspirin was beneficial only in the first 30 days. After 30 days, it’s startling and remarkable that the ischemic event curves were completely on top of each other,” commented Julia H. Indik, MD, a cardiac electrophysiologist at Banner–University Medical Center Tuscon and designated discussant for the report. “This substudy will be essential for updating the guidelines,” she predicted. “When a treatment’s benefit equals its risks,” which happened when aspirin was part of the regimen during the first 30 days, “then it’s not even a class IIb recommendation; it’s class III,” the classification used by the ACC and collaborating groups to identify treatments where net benefit and net risk are similar and hence the treatment is considered not recommended.
A key element in the analysis Dr. Alexander presented was to define a spectrum of clinical events as representing broad, intermediate, or severe ischemic or bleeding events. The severe category for bleeding events included fatal, intracranial, and any bleed rated as major by the International Society on Thrombosis and Haemostasis (ISTH) criteria, while the broad bleeding definition included all of these plus bleeds that directly resulted in hospitalization and clinically relevant nonmajor bleeds. For ischemic events, the severe group consisted of cardiovascular death, MI, stent thrombosis, and ischemic stroke, while the broad category also tallied urgent revascularizations and cardiovascular hospitalizations.
“I believe the severe bleeds and severe ischemic events we identified are roughly equal in severity,” Dr. Alexander noted. “Where I think we need more analysis is which patients have more bleeding risk and which have more ischemia risk. We need a more tailored approach to identify patient subgroups, perhaps based on angiographic characteristics, or something else,” that modifies the trade-off that, on a population level, seems very evenly balanced.
Applying this approach to scoring the severity of adverse outcomes, Dr. Alexander reported that, during the first 30 days on treatment, patients on aspirin had a net absolute gain of 1.0% in severe bleeding events, compared with placebo, and a 3.4% gain in broad bleeds, while showing a 0.9% drop in severe ischemic events but no between-group difference in the rate of broadly defined ischemic events. During days 31-180, the addition of aspirin resulted in virtually no reductions in ischemic events regardless of whether they were severe, intermediate, or broad, but adding aspirin continued to produce an excess of bleeding episodes in all three categories. The results also appeared in an article published online (Circulation. 2020 Mar 29. doi: 10.1161/CIRCULATIONAHA.120.046534).
“We did not see a time window when the ischemia risk was greater than the bleeding risk,” Dr. Alexander noted, and he also highlighted that the one option the analysis could not explore is never giving these patients any aspirin. “Patients received aspirin for some number of days before randomization,” a median of 6 days from the time of their ACS or PCI event until randomization, “so we don’t have great insight into whether no aspirin” is an reasonable option.
The AUGUSTUS trial randomized 4,614 patients with AFib and a recent ACS or PCI event at any of 492 sites in 33 countries during 2015-2018. The study’s primary endpoint was the rate of major or clinically relevant nonmajor bleeding by the ISTH criteria during 6 months on treatment, while composites of death or hospitalization, and death plus ischemic events served as secondary outcomes. All patients received an antiplatelet P2Y12 inhibitor, with 93% of patients receiving clopidogrel, and were randomized in a 2 x 2 factorial design to one of four regimens: either apixaban or a vitamin K antagonist (such as warfarin), and to aspirin or placebo. The study’s primary findings showed that using apixaban instead of a vitamin K antagonist significantly reduced bleeding events as well as the rate of death or hospitalization, but the rate of death and ischemic events was similar in the two arms. The primary AUGUSTUS finding for the aspirin versus placebo randomization was that overall throughout the study ischemic events were balanced in the these two treatment arms while aspirin boosted bleeding (N Engl J Med. 2019 Apr 18;380[16]:1509-24).
AUGUSTUS was sponsored by Bristol-Myers Squibb and Pfizer, the companies that market apixaban. Dr. Alexander has been a consultant to and received research funding from Bristol-Myers Squibb and Pfizer; has been a consultant to AbbVie, Bayer, CryoLife, CSL Behring, Novo Nordisk, Portola, Quantum Genomics, XaTek, and Zafgen; and has received research funding from Boehringer Ingelheim, CryoLife, CSL Behring, GlaxoSmithKline, and XaTek. Dr. Indik had no disclosures.
SOURCE: Alexander JH et al. ACC 2020, Abstract 409-08.
When patients with atrial fibrillation have an acute coronary syndrome event or undergo percutaneous coronary intervention, their window of opportunity for benefiting from a triple antithrombotic regimen was, at best, about 30 days, according to a post hoc analysis of AUGUSTUS, a multicenter, randomized trial with more than 4,600 patients.
Beyond 30 days out to 180 days, the incremental benefit from reduced ischemic events fell to essentially zero, giving it a clear back seat to the ongoing, increased bleeding risk from adding a third antithrombotic drug.
Patients randomized to receive aspirin in addition to an anticoagulant, either apixaban or a vitamin K antagonist such as warfarin, and a P2Y12 inhibitor such as clopidogrel “for up to approximately 30 days” had a roughly similar decrease in severe ischemic events and increase in severe bleeding events, suggesting that even acutely the overall impact of adding aspirin on top of the other two antithrombotics was a wash, John H. Alexander, MD, said in a presentation of research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
Using aspirin as a third antithrombotic in patients with atrial fibrillation (AFib) who have also recently had either an acute coronary syndrome event (ACS) or underwent percutaneous coronary intervention (PCI), “may be reasonable,” for selected patients, but is a decision that requires careful individualization, cautioned Dr. Alexander, professor of medicine and director of Cardiovascular Research at the Duke Clinical Research Institute of Duke University, Durham, N.C.
“This is a superb secondary analysis looking at the time course of potential benefit and harm with aspirin, and they found that aspirin was beneficial only in the first 30 days. After 30 days, it’s startling and remarkable that the ischemic event curves were completely on top of each other,” commented Julia H. Indik, MD, a cardiac electrophysiologist at Banner–University Medical Center Tuscon and designated discussant for the report. “This substudy will be essential for updating the guidelines,” she predicted. “When a treatment’s benefit equals its risks,” which happened when aspirin was part of the regimen during the first 30 days, “then it’s not even a class IIb recommendation; it’s class III,” the classification used by the ACC and collaborating groups to identify treatments where net benefit and net risk are similar and hence the treatment is considered not recommended.
A key element in the analysis Dr. Alexander presented was to define a spectrum of clinical events as representing broad, intermediate, or severe ischemic or bleeding events. The severe category for bleeding events included fatal, intracranial, and any bleed rated as major by the International Society on Thrombosis and Haemostasis (ISTH) criteria, while the broad bleeding definition included all of these plus bleeds that directly resulted in hospitalization and clinically relevant nonmajor bleeds. For ischemic events, the severe group consisted of cardiovascular death, MI, stent thrombosis, and ischemic stroke, while the broad category also tallied urgent revascularizations and cardiovascular hospitalizations.
“I believe the severe bleeds and severe ischemic events we identified are roughly equal in severity,” Dr. Alexander noted. “Where I think we need more analysis is which patients have more bleeding risk and which have more ischemia risk. We need a more tailored approach to identify patient subgroups, perhaps based on angiographic characteristics, or something else,” that modifies the trade-off that, on a population level, seems very evenly balanced.
Applying this approach to scoring the severity of adverse outcomes, Dr. Alexander reported that, during the first 30 days on treatment, patients on aspirin had a net absolute gain of 1.0% in severe bleeding events, compared with placebo, and a 3.4% gain in broad bleeds, while showing a 0.9% drop in severe ischemic events but no between-group difference in the rate of broadly defined ischemic events. During days 31-180, the addition of aspirin resulted in virtually no reductions in ischemic events regardless of whether they were severe, intermediate, or broad, but adding aspirin continued to produce an excess of bleeding episodes in all three categories. The results also appeared in an article published online (Circulation. 2020 Mar 29. doi: 10.1161/CIRCULATIONAHA.120.046534).
“We did not see a time window when the ischemia risk was greater than the bleeding risk,” Dr. Alexander noted, and he also highlighted that the one option the analysis could not explore is never giving these patients any aspirin. “Patients received aspirin for some number of days before randomization,” a median of 6 days from the time of their ACS or PCI event until randomization, “so we don’t have great insight into whether no aspirin” is an reasonable option.
The AUGUSTUS trial randomized 4,614 patients with AFib and a recent ACS or PCI event at any of 492 sites in 33 countries during 2015-2018. The study’s primary endpoint was the rate of major or clinically relevant nonmajor bleeding by the ISTH criteria during 6 months on treatment, while composites of death or hospitalization, and death plus ischemic events served as secondary outcomes. All patients received an antiplatelet P2Y12 inhibitor, with 93% of patients receiving clopidogrel, and were randomized in a 2 x 2 factorial design to one of four regimens: either apixaban or a vitamin K antagonist (such as warfarin), and to aspirin or placebo. The study’s primary findings showed that using apixaban instead of a vitamin K antagonist significantly reduced bleeding events as well as the rate of death or hospitalization, but the rate of death and ischemic events was similar in the two arms. The primary AUGUSTUS finding for the aspirin versus placebo randomization was that overall throughout the study ischemic events were balanced in the these two treatment arms while aspirin boosted bleeding (N Engl J Med. 2019 Apr 18;380[16]:1509-24).
AUGUSTUS was sponsored by Bristol-Myers Squibb and Pfizer, the companies that market apixaban. Dr. Alexander has been a consultant to and received research funding from Bristol-Myers Squibb and Pfizer; has been a consultant to AbbVie, Bayer, CryoLife, CSL Behring, Novo Nordisk, Portola, Quantum Genomics, XaTek, and Zafgen; and has received research funding from Boehringer Ingelheim, CryoLife, CSL Behring, GlaxoSmithKline, and XaTek. Dr. Indik had no disclosures.
SOURCE: Alexander JH et al. ACC 2020, Abstract 409-08.
When patients with atrial fibrillation have an acute coronary syndrome event or undergo percutaneous coronary intervention, their window of opportunity for benefiting from a triple antithrombotic regimen was, at best, about 30 days, according to a post hoc analysis of AUGUSTUS, a multicenter, randomized trial with more than 4,600 patients.
Beyond 30 days out to 180 days, the incremental benefit from reduced ischemic events fell to essentially zero, giving it a clear back seat to the ongoing, increased bleeding risk from adding a third antithrombotic drug.
Patients randomized to receive aspirin in addition to an anticoagulant, either apixaban or a vitamin K antagonist such as warfarin, and a P2Y12 inhibitor such as clopidogrel “for up to approximately 30 days” had a roughly similar decrease in severe ischemic events and increase in severe bleeding events, suggesting that even acutely the overall impact of adding aspirin on top of the other two antithrombotics was a wash, John H. Alexander, MD, said in a presentation of research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
Using aspirin as a third antithrombotic in patients with atrial fibrillation (AFib) who have also recently had either an acute coronary syndrome event (ACS) or underwent percutaneous coronary intervention (PCI), “may be reasonable,” for selected patients, but is a decision that requires careful individualization, cautioned Dr. Alexander, professor of medicine and director of Cardiovascular Research at the Duke Clinical Research Institute of Duke University, Durham, N.C.
“This is a superb secondary analysis looking at the time course of potential benefit and harm with aspirin, and they found that aspirin was beneficial only in the first 30 days. After 30 days, it’s startling and remarkable that the ischemic event curves were completely on top of each other,” commented Julia H. Indik, MD, a cardiac electrophysiologist at Banner–University Medical Center Tuscon and designated discussant for the report. “This substudy will be essential for updating the guidelines,” she predicted. “When a treatment’s benefit equals its risks,” which happened when aspirin was part of the regimen during the first 30 days, “then it’s not even a class IIb recommendation; it’s class III,” the classification used by the ACC and collaborating groups to identify treatments where net benefit and net risk are similar and hence the treatment is considered not recommended.
A key element in the analysis Dr. Alexander presented was to define a spectrum of clinical events as representing broad, intermediate, or severe ischemic or bleeding events. The severe category for bleeding events included fatal, intracranial, and any bleed rated as major by the International Society on Thrombosis and Haemostasis (ISTH) criteria, while the broad bleeding definition included all of these plus bleeds that directly resulted in hospitalization and clinically relevant nonmajor bleeds. For ischemic events, the severe group consisted of cardiovascular death, MI, stent thrombosis, and ischemic stroke, while the broad category also tallied urgent revascularizations and cardiovascular hospitalizations.
“I believe the severe bleeds and severe ischemic events we identified are roughly equal in severity,” Dr. Alexander noted. “Where I think we need more analysis is which patients have more bleeding risk and which have more ischemia risk. We need a more tailored approach to identify patient subgroups, perhaps based on angiographic characteristics, or something else,” that modifies the trade-off that, on a population level, seems very evenly balanced.
Applying this approach to scoring the severity of adverse outcomes, Dr. Alexander reported that, during the first 30 days on treatment, patients on aspirin had a net absolute gain of 1.0% in severe bleeding events, compared with placebo, and a 3.4% gain in broad bleeds, while showing a 0.9% drop in severe ischemic events but no between-group difference in the rate of broadly defined ischemic events. During days 31-180, the addition of aspirin resulted in virtually no reductions in ischemic events regardless of whether they were severe, intermediate, or broad, but adding aspirin continued to produce an excess of bleeding episodes in all three categories. The results also appeared in an article published online (Circulation. 2020 Mar 29. doi: 10.1161/CIRCULATIONAHA.120.046534).
“We did not see a time window when the ischemia risk was greater than the bleeding risk,” Dr. Alexander noted, and he also highlighted that the one option the analysis could not explore is never giving these patients any aspirin. “Patients received aspirin for some number of days before randomization,” a median of 6 days from the time of their ACS or PCI event until randomization, “so we don’t have great insight into whether no aspirin” is an reasonable option.
The AUGUSTUS trial randomized 4,614 patients with AFib and a recent ACS or PCI event at any of 492 sites in 33 countries during 2015-2018. The study’s primary endpoint was the rate of major or clinically relevant nonmajor bleeding by the ISTH criteria during 6 months on treatment, while composites of death or hospitalization, and death plus ischemic events served as secondary outcomes. All patients received an antiplatelet P2Y12 inhibitor, with 93% of patients receiving clopidogrel, and were randomized in a 2 x 2 factorial design to one of four regimens: either apixaban or a vitamin K antagonist (such as warfarin), and to aspirin or placebo. The study’s primary findings showed that using apixaban instead of a vitamin K antagonist significantly reduced bleeding events as well as the rate of death or hospitalization, but the rate of death and ischemic events was similar in the two arms. The primary AUGUSTUS finding for the aspirin versus placebo randomization was that overall throughout the study ischemic events were balanced in the these two treatment arms while aspirin boosted bleeding (N Engl J Med. 2019 Apr 18;380[16]:1509-24).
AUGUSTUS was sponsored by Bristol-Myers Squibb and Pfizer, the companies that market apixaban. Dr. Alexander has been a consultant to and received research funding from Bristol-Myers Squibb and Pfizer; has been a consultant to AbbVie, Bayer, CryoLife, CSL Behring, Novo Nordisk, Portola, Quantum Genomics, XaTek, and Zafgen; and has received research funding from Boehringer Ingelheim, CryoLife, CSL Behring, GlaxoSmithKline, and XaTek. Dr. Indik had no disclosures.
SOURCE: Alexander JH et al. ACC 2020, Abstract 409-08.
FROM ACC 2020
Signature STEMI sign may be less diagnostic in the COVID-19 age
The signature electrocardiographic sign indicating ST-segment-elevation MI may be a less-consistent indicator of actual STEMI at a time when patients with COVID-19 have come to overwhelm many hospital ICUs.
Many of the 18 such patients identified at six New York City hospitals who showed ST-segment elevation on their 12-lead ECG in the city’s first month of fighting the pandemic turned out to be free of either obstructive coronary artery disease by angiography or of regional wall-motion abnormalities (RWMA) by ECG, according to a letter published in the New England Journal of Medicine.
Those 10 patients in the 18-case series were said to have noncoronary myocardial injury, perhaps from myocarditis – a prevalent feature of severe COVID-19 – and the remaining 8 patients with obstructive coronary artery disease, RWMA, or both were diagnosed with STEMI. Of the latter patients, six went to the cath lab and five of those underwent percutaneous coronary intervention, Sripal Bangalore, MD, MHA, of New York University, and colleagues reported.
In an interview, Dr. Bangalore framed the case-series report as a caution against substituting fibrinolytic therapy for primary percutaneous coronary intervention in patients with STE while hospitals are unusually burdened by the COVID-19 pandemic and invasive procedures intensify the threat of SARS-CoV-2 exposure to clinicians.
The strategy was recently advanced as an option for highly selected patients in a statement from the American College of Cardiology and Society for Cardiovascular Angiography and Interventions (SCAI).
“During the COVID-19 pandemic, one of the main reasons fibrinolytic therapy has been pushed is to reduce the exposure to the cath-lab staff,” Dr. Bangalore observed. “But if you pursue that route, it’s problematic because more than half may not have obstructive disease and fibrinolytic therapy may not help. And if you give them fibrinolytics, you’re potentially increasing their risk of bleeding complications.
“The take-home from these 18 patients is that it’s very difficult to guess who is going to have obstructive disease and who is going to have nonobstructive disease,” Dr. Bangalore said. “Maybe we should assess these patients with not just an ECG but with a quick echo, then make a decision. Our practice so far has been to take these patients to the cath lab.”
The ACC/SCAI statement proposed that “fibrinolysis can be considered an option for the relatively stable STEMI patient with active COVID-19” after careful consideration of possible patient benefit versus the risks of cath-lab personnel exposure to the virus.
Only six patients in the current series, including five in the STEMI group, are reported to have had chest pain at about the time of STE, observed Michael J. Blaha, MD, MPH, of Johns Hopkins Hospital, Baltimore.
So, he said in an interview, “one of their points is that you have to take ST elevations with a grain of salt in this [COVID-19] era, because there are a lot of people presenting with ST elevations in the absence of chest pain.”
That, and the high prevalence of nonobstructive disease in the series, indeed argues against the use of fibrinolytic therapy in such patients, Dr. Blaha said.
Normally, when there is STE, “the pretest probability of STEMI is so high, and if you can’t make it to the cath lab for some reason, sure, it makes sense to give lytics.” However, he said, “COVID-19 is changing the clinical landscape. Now, with a variety of virus-mediated myocardial injury presentations, including myocarditis, the pretest probability of MI is lower.”
The current report “confirms that, in the COVID era, ST elevations are not diagnostic for MI and must be considered within the totality of clinical evidence, and a conservative approach to going to the cath lab is probably warranted,” Dr. Blaha said in an interview.
However, with the reduced pretest probability of STE for STEMI, he agreed, “I almost don’t see any scenario where I’d be comfortable, based on ECG changes alone, giving lytics at this time.”
Dr. Bangalore pointed out that all of the 18 patients in the series had elevated levels of the fibrin degradation product D-dimer, a biomarker that reflects ongoing hemostatic activation. Levels were higher in the 8 patients who ultimately received a STEMI diagnosis than in the remaining 10 patients.
But COVID-19 patients in general may have elevated D-dimer and “a lot of microthrombi,” he said. “So the question is, are those microthrombi also causal for any of the ECG changes we are also seeing?”
Aside from microthrombi, global hypoxia and myocarditis could be other potential causes of STE in COVID-19 patients in the absence of STEMI, Dr. Bangalore proposed. “At this point we just generally don’t know.”
Dr. Bangalore reported no conflicts; disclosures for the other authors are available at nejm.org. Dr. Blaha disclosed receiving grants from Amgen and serving on advisory boards for Amgen and other pharmaceutical companies.
A version of this article originally appeared on Medscape.com.
The signature electrocardiographic sign indicating ST-segment-elevation MI may be a less-consistent indicator of actual STEMI at a time when patients with COVID-19 have come to overwhelm many hospital ICUs.
Many of the 18 such patients identified at six New York City hospitals who showed ST-segment elevation on their 12-lead ECG in the city’s first month of fighting the pandemic turned out to be free of either obstructive coronary artery disease by angiography or of regional wall-motion abnormalities (RWMA) by ECG, according to a letter published in the New England Journal of Medicine.
Those 10 patients in the 18-case series were said to have noncoronary myocardial injury, perhaps from myocarditis – a prevalent feature of severe COVID-19 – and the remaining 8 patients with obstructive coronary artery disease, RWMA, or both were diagnosed with STEMI. Of the latter patients, six went to the cath lab and five of those underwent percutaneous coronary intervention, Sripal Bangalore, MD, MHA, of New York University, and colleagues reported.
In an interview, Dr. Bangalore framed the case-series report as a caution against substituting fibrinolytic therapy for primary percutaneous coronary intervention in patients with STE while hospitals are unusually burdened by the COVID-19 pandemic and invasive procedures intensify the threat of SARS-CoV-2 exposure to clinicians.
The strategy was recently advanced as an option for highly selected patients in a statement from the American College of Cardiology and Society for Cardiovascular Angiography and Interventions (SCAI).
“During the COVID-19 pandemic, one of the main reasons fibrinolytic therapy has been pushed is to reduce the exposure to the cath-lab staff,” Dr. Bangalore observed. “But if you pursue that route, it’s problematic because more than half may not have obstructive disease and fibrinolytic therapy may not help. And if you give them fibrinolytics, you’re potentially increasing their risk of bleeding complications.
“The take-home from these 18 patients is that it’s very difficult to guess who is going to have obstructive disease and who is going to have nonobstructive disease,” Dr. Bangalore said. “Maybe we should assess these patients with not just an ECG but with a quick echo, then make a decision. Our practice so far has been to take these patients to the cath lab.”
The ACC/SCAI statement proposed that “fibrinolysis can be considered an option for the relatively stable STEMI patient with active COVID-19” after careful consideration of possible patient benefit versus the risks of cath-lab personnel exposure to the virus.
Only six patients in the current series, including five in the STEMI group, are reported to have had chest pain at about the time of STE, observed Michael J. Blaha, MD, MPH, of Johns Hopkins Hospital, Baltimore.
So, he said in an interview, “one of their points is that you have to take ST elevations with a grain of salt in this [COVID-19] era, because there are a lot of people presenting with ST elevations in the absence of chest pain.”
That, and the high prevalence of nonobstructive disease in the series, indeed argues against the use of fibrinolytic therapy in such patients, Dr. Blaha said.
Normally, when there is STE, “the pretest probability of STEMI is so high, and if you can’t make it to the cath lab for some reason, sure, it makes sense to give lytics.” However, he said, “COVID-19 is changing the clinical landscape. Now, with a variety of virus-mediated myocardial injury presentations, including myocarditis, the pretest probability of MI is lower.”
The current report “confirms that, in the COVID era, ST elevations are not diagnostic for MI and must be considered within the totality of clinical evidence, and a conservative approach to going to the cath lab is probably warranted,” Dr. Blaha said in an interview.
However, with the reduced pretest probability of STE for STEMI, he agreed, “I almost don’t see any scenario where I’d be comfortable, based on ECG changes alone, giving lytics at this time.”
Dr. Bangalore pointed out that all of the 18 patients in the series had elevated levels of the fibrin degradation product D-dimer, a biomarker that reflects ongoing hemostatic activation. Levels were higher in the 8 patients who ultimately received a STEMI diagnosis than in the remaining 10 patients.
But COVID-19 patients in general may have elevated D-dimer and “a lot of microthrombi,” he said. “So the question is, are those microthrombi also causal for any of the ECG changes we are also seeing?”
Aside from microthrombi, global hypoxia and myocarditis could be other potential causes of STE in COVID-19 patients in the absence of STEMI, Dr. Bangalore proposed. “At this point we just generally don’t know.”
Dr. Bangalore reported no conflicts; disclosures for the other authors are available at nejm.org. Dr. Blaha disclosed receiving grants from Amgen and serving on advisory boards for Amgen and other pharmaceutical companies.
A version of this article originally appeared on Medscape.com.
The signature electrocardiographic sign indicating ST-segment-elevation MI may be a less-consistent indicator of actual STEMI at a time when patients with COVID-19 have come to overwhelm many hospital ICUs.
Many of the 18 such patients identified at six New York City hospitals who showed ST-segment elevation on their 12-lead ECG in the city’s first month of fighting the pandemic turned out to be free of either obstructive coronary artery disease by angiography or of regional wall-motion abnormalities (RWMA) by ECG, according to a letter published in the New England Journal of Medicine.
Those 10 patients in the 18-case series were said to have noncoronary myocardial injury, perhaps from myocarditis – a prevalent feature of severe COVID-19 – and the remaining 8 patients with obstructive coronary artery disease, RWMA, or both were diagnosed with STEMI. Of the latter patients, six went to the cath lab and five of those underwent percutaneous coronary intervention, Sripal Bangalore, MD, MHA, of New York University, and colleagues reported.
In an interview, Dr. Bangalore framed the case-series report as a caution against substituting fibrinolytic therapy for primary percutaneous coronary intervention in patients with STE while hospitals are unusually burdened by the COVID-19 pandemic and invasive procedures intensify the threat of SARS-CoV-2 exposure to clinicians.
The strategy was recently advanced as an option for highly selected patients in a statement from the American College of Cardiology and Society for Cardiovascular Angiography and Interventions (SCAI).
“During the COVID-19 pandemic, one of the main reasons fibrinolytic therapy has been pushed is to reduce the exposure to the cath-lab staff,” Dr. Bangalore observed. “But if you pursue that route, it’s problematic because more than half may not have obstructive disease and fibrinolytic therapy may not help. And if you give them fibrinolytics, you’re potentially increasing their risk of bleeding complications.
“The take-home from these 18 patients is that it’s very difficult to guess who is going to have obstructive disease and who is going to have nonobstructive disease,” Dr. Bangalore said. “Maybe we should assess these patients with not just an ECG but with a quick echo, then make a decision. Our practice so far has been to take these patients to the cath lab.”
The ACC/SCAI statement proposed that “fibrinolysis can be considered an option for the relatively stable STEMI patient with active COVID-19” after careful consideration of possible patient benefit versus the risks of cath-lab personnel exposure to the virus.
Only six patients in the current series, including five in the STEMI group, are reported to have had chest pain at about the time of STE, observed Michael J. Blaha, MD, MPH, of Johns Hopkins Hospital, Baltimore.
So, he said in an interview, “one of their points is that you have to take ST elevations with a grain of salt in this [COVID-19] era, because there are a lot of people presenting with ST elevations in the absence of chest pain.”
That, and the high prevalence of nonobstructive disease in the series, indeed argues against the use of fibrinolytic therapy in such patients, Dr. Blaha said.
Normally, when there is STE, “the pretest probability of STEMI is so high, and if you can’t make it to the cath lab for some reason, sure, it makes sense to give lytics.” However, he said, “COVID-19 is changing the clinical landscape. Now, with a variety of virus-mediated myocardial injury presentations, including myocarditis, the pretest probability of MI is lower.”
The current report “confirms that, in the COVID era, ST elevations are not diagnostic for MI and must be considered within the totality of clinical evidence, and a conservative approach to going to the cath lab is probably warranted,” Dr. Blaha said in an interview.
However, with the reduced pretest probability of STE for STEMI, he agreed, “I almost don’t see any scenario where I’d be comfortable, based on ECG changes alone, giving lytics at this time.”
Dr. Bangalore pointed out that all of the 18 patients in the series had elevated levels of the fibrin degradation product D-dimer, a biomarker that reflects ongoing hemostatic activation. Levels were higher in the 8 patients who ultimately received a STEMI diagnosis than in the remaining 10 patients.
But COVID-19 patients in general may have elevated D-dimer and “a lot of microthrombi,” he said. “So the question is, are those microthrombi also causal for any of the ECG changes we are also seeing?”
Aside from microthrombi, global hypoxia and myocarditis could be other potential causes of STE in COVID-19 patients in the absence of STEMI, Dr. Bangalore proposed. “At this point we just generally don’t know.”
Dr. Bangalore reported no conflicts; disclosures for the other authors are available at nejm.org. Dr. Blaha disclosed receiving grants from Amgen and serving on advisory boards for Amgen and other pharmaceutical companies.
A version of this article originally appeared on Medscape.com.
Mislabeled clopidogrel lot recalled, may contain simvastatin
International Laboratories has initiated a voluntary recall to the consumer level in the United States of a single lot of the antiplatelet clopidogrel because it is mislabeled and may contain simvastatin, a cholesterol-lowering drug, instead of clopidogrel.
The recalled product ― lot number 117099A of clopidogrel tablets (USP 75 mg) packaged in bottles of 30 tablets ― may contain clopidogrel 75 mg tablets or it could contain simvastatin tablets (USP 10 mg), according to a company announcement posted on the US Food and Drug Administration (FDA) website.
“Missed doses of clopidogrel increases the risk of heart attack and stroke which can be life threatening. Additionally, unintentional consumption of simvastatin could include the common side effects associated with its use and may cause fetal harm when administered to a pregnant woman,” the company cautions.
To date, the company has not received any reports of harm arising from the problem that prompted the recall.
The recalled product was distributed nationwide and was delivered to distribution centers in Arkansas, Georgia, Indiana, California, and Maryland and to retail stores in all US states.
International Laboratories is notifying distributors and customers by letter and is arranging for the return of all recalled products.
For questions regarding this recall, contact Inmar by phone 855-258-7280 (weekdays between 9:00 AM and 5:00 PM EST) or by email at internationallabs@inmar.com.
Adverse reactions or quality problems experienced with the use of this product should be reported to the FDA’s MedWatch adverse event reporting program.
This article first appeared on Medscape.com.
International Laboratories has initiated a voluntary recall to the consumer level in the United States of a single lot of the antiplatelet clopidogrel because it is mislabeled and may contain simvastatin, a cholesterol-lowering drug, instead of clopidogrel.
The recalled product ― lot number 117099A of clopidogrel tablets (USP 75 mg) packaged in bottles of 30 tablets ― may contain clopidogrel 75 mg tablets or it could contain simvastatin tablets (USP 10 mg), according to a company announcement posted on the US Food and Drug Administration (FDA) website.
“Missed doses of clopidogrel increases the risk of heart attack and stroke which can be life threatening. Additionally, unintentional consumption of simvastatin could include the common side effects associated with its use and may cause fetal harm when administered to a pregnant woman,” the company cautions.
To date, the company has not received any reports of harm arising from the problem that prompted the recall.
The recalled product was distributed nationwide and was delivered to distribution centers in Arkansas, Georgia, Indiana, California, and Maryland and to retail stores in all US states.
International Laboratories is notifying distributors and customers by letter and is arranging for the return of all recalled products.
For questions regarding this recall, contact Inmar by phone 855-258-7280 (weekdays between 9:00 AM and 5:00 PM EST) or by email at internationallabs@inmar.com.
Adverse reactions or quality problems experienced with the use of this product should be reported to the FDA’s MedWatch adverse event reporting program.
This article first appeared on Medscape.com.
International Laboratories has initiated a voluntary recall to the consumer level in the United States of a single lot of the antiplatelet clopidogrel because it is mislabeled and may contain simvastatin, a cholesterol-lowering drug, instead of clopidogrel.
The recalled product ― lot number 117099A of clopidogrel tablets (USP 75 mg) packaged in bottles of 30 tablets ― may contain clopidogrel 75 mg tablets or it could contain simvastatin tablets (USP 10 mg), according to a company announcement posted on the US Food and Drug Administration (FDA) website.
“Missed doses of clopidogrel increases the risk of heart attack and stroke which can be life threatening. Additionally, unintentional consumption of simvastatin could include the common side effects associated with its use and may cause fetal harm when administered to a pregnant woman,” the company cautions.
To date, the company has not received any reports of harm arising from the problem that prompted the recall.
The recalled product was distributed nationwide and was delivered to distribution centers in Arkansas, Georgia, Indiana, California, and Maryland and to retail stores in all US states.
International Laboratories is notifying distributors and customers by letter and is arranging for the return of all recalled products.
For questions regarding this recall, contact Inmar by phone 855-258-7280 (weekdays between 9:00 AM and 5:00 PM EST) or by email at internationallabs@inmar.com.
Adverse reactions or quality problems experienced with the use of this product should be reported to the FDA’s MedWatch adverse event reporting program.
This article first appeared on Medscape.com.
TWILIGHT-COMPLEX: Tap ticagrelor monotherapy early after complex PCI
Patients who underwent complex PCI for acute coronary syndrome followed by 3 months of dual-antiplatelet therapy (DAPT) with ticagrelor plus aspirin fared significantly better by dropping aspirin at that point in favor of long-term ticagrelor monotherapy than with continued dual-antiplatelet therapy in the TWILIGHT-COMPLEX study.
The rate of clinically relevant bleeding was significantly lower at 12 months of follow-up in the ticagrelor monotherapy group than it was in patients randomized to continued DAPT. Moreover, this major benefit came at no cost in terms of ischemic events, which were actually numerically less frequent in the ticagrelor plus placebo group, George D. Dangas, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“We found that the aspirin just doesn’t add that much, even in complex patients – just bleeding complications, for the most part,” explained Dr. Dangas, professor of medicine and of surgery at the Icahn School of Medicine at Mount Sinai, New York.
The TWILIGHT-COMPLEX study was a secondary post hoc analysis of outcomes in 2,342 participants in the previously reported larger parent TWILIGHT randomized trial who underwent complex PCI. The main TWILIGHT trial included 7,119 patients in 11 countries who underwent PCI for acute coronary syndrome, successfully completed 3 months of DAPT with ticagrelor plus aspirin without incident, and were then randomized double blind to 12 months of ticagrelor plus placebo or to another 12 months of ticagrelor and aspirin.
In the overall TWILIGHT trial, ticagrelor alone resulted in a significantly lower clinically relevant bleeding rate than did long-term ticagrelor plus aspirin, with no increase in the risk of death, MI, or stroke (N Engl J Med 2019; 381:2032-42). But the results left many interventional cardiologists wondering if a ticagrelor monotherapy strategy was really applicable to their more challenging patients undergoing complex PCI given that the risk of ischemic events is known to climb with PCI complexity. The TWILIGHT-COMPLEX study was specifically designed to address that concern.
To be eligible for TWILIGHT-COMPLEX, patients had to meet one or more prespecified angiographic or procedural criteria for complex PCI, such as a total stent length in excess of 60 mm, three or more treated lesions, use of an atherectomy device, or PCI of a left main lesion, a chronic total occlusion, or a bifurcation lesion with two stents. These complex PCI patients accounted for one-third of the total study population in TWILIGHT; 36% of them met more than one criteria for complex PCI.
TWILIGHT-COMPLEX findings
In the 12 months after randomization, patients who received ticagrelor plus placebo had a 4.2% incidence of clinically significant Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding, which was significantly lower than the 7.7% rate in the group on long-term DAPT and represented a 46% relative risk reduction. Severe or fatal bleeding – that is, BARC type 3 or 5 – occurred in 1.1% of those on ticagrelor monotherapy and 2.6% of the DAPT group, for a significant 59% relative risk reduction.
The composite ischemic endpoint comprising cardiovascular death, MI, or ischemic stroke occurred in 3.6% of the ticagrelor monotherapy group and 4.8% of patients on long-term DAPT, a trend that didn’t achieve statistical significance. The all-cause mortality rate was 0.9% in the ticagrelor monotherapy group and 1.5% with extended DAPT, again a nonsignificant difference. Similarly, the rate of definite or probable stent thrombosis was numerically lower with ticagrelor monotherapy, by a margin of 0.4% versus 0.8%, a nonsignificant difference.
The results were consistent regardless of which specific criteria for complex PCI a patient had or how many of them.
Results are ‘reassuring’
At a press conference where Dr. Dangas presented the TWILIGHT-COMPLEX results, discussant Claire S. Duvernoy, MD, said she was “very impressed” with just how complex the PCIs were in the study participants.
“Really, these are the patients that in my own practice we’ve always been the most cautious about, the most worried about thrombotic risk, and the ones where we get down on our house staff when they drop an antiplatelet agent. So this study is very reassuring,” said Dr. Duvernoy, professor of medicine at the University of Michigan, Ann Arbor.
She identified two key differences between TWILIGHT-COMPLEX and earlier studies that showed a benefit for extended DAPT in higher-risk patients. In the earlier studies, it was the P2Y12 inhibitor that was dropped; TWILIGHT was the first major randomized trial to discontinue the aspirin instead. And patients in the TWILIGHT study received second-generation drug-eluting stents.
“That makes a huge difference,” Dr. Duvernoy said. “We have stents now that are much safer than the old ones were, and that’s what allows us to gain this incredible benefit of reduced bleeding.”
Dr. Dangas cautioned that since this was a secondary post hoc analysis, the TWILIGHT-COMPLEX study must be viewed as hypothesis-generating.
The TWILIGHT trial was funded by AstraZeneca. Dr. Dangas reported receiving institutional research grants from that company as well as Bayer and Daichi-Sankyo. He also served as a paid consultant to Abbott Vascular, Boston Scientific, and Biosensors.
Simultaneous with his presentation at ACC 2020, the TWILIGHT-COMPLEX results were published online (J Am Coll Cardiol. 2020 Mar 13. doi: 10.1016/j.jacc.2020.03.011).
SOURCE: Dangas GD. ACC 20, Abstract 410-09.
Patients who underwent complex PCI for acute coronary syndrome followed by 3 months of dual-antiplatelet therapy (DAPT) with ticagrelor plus aspirin fared significantly better by dropping aspirin at that point in favor of long-term ticagrelor monotherapy than with continued dual-antiplatelet therapy in the TWILIGHT-COMPLEX study.
The rate of clinically relevant bleeding was significantly lower at 12 months of follow-up in the ticagrelor monotherapy group than it was in patients randomized to continued DAPT. Moreover, this major benefit came at no cost in terms of ischemic events, which were actually numerically less frequent in the ticagrelor plus placebo group, George D. Dangas, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“We found that the aspirin just doesn’t add that much, even in complex patients – just bleeding complications, for the most part,” explained Dr. Dangas, professor of medicine and of surgery at the Icahn School of Medicine at Mount Sinai, New York.
The TWILIGHT-COMPLEX study was a secondary post hoc analysis of outcomes in 2,342 participants in the previously reported larger parent TWILIGHT randomized trial who underwent complex PCI. The main TWILIGHT trial included 7,119 patients in 11 countries who underwent PCI for acute coronary syndrome, successfully completed 3 months of DAPT with ticagrelor plus aspirin without incident, and were then randomized double blind to 12 months of ticagrelor plus placebo or to another 12 months of ticagrelor and aspirin.
In the overall TWILIGHT trial, ticagrelor alone resulted in a significantly lower clinically relevant bleeding rate than did long-term ticagrelor plus aspirin, with no increase in the risk of death, MI, or stroke (N Engl J Med 2019; 381:2032-42). But the results left many interventional cardiologists wondering if a ticagrelor monotherapy strategy was really applicable to their more challenging patients undergoing complex PCI given that the risk of ischemic events is known to climb with PCI complexity. The TWILIGHT-COMPLEX study was specifically designed to address that concern.
To be eligible for TWILIGHT-COMPLEX, patients had to meet one or more prespecified angiographic or procedural criteria for complex PCI, such as a total stent length in excess of 60 mm, three or more treated lesions, use of an atherectomy device, or PCI of a left main lesion, a chronic total occlusion, or a bifurcation lesion with two stents. These complex PCI patients accounted for one-third of the total study population in TWILIGHT; 36% of them met more than one criteria for complex PCI.
TWILIGHT-COMPLEX findings
In the 12 months after randomization, patients who received ticagrelor plus placebo had a 4.2% incidence of clinically significant Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding, which was significantly lower than the 7.7% rate in the group on long-term DAPT and represented a 46% relative risk reduction. Severe or fatal bleeding – that is, BARC type 3 or 5 – occurred in 1.1% of those on ticagrelor monotherapy and 2.6% of the DAPT group, for a significant 59% relative risk reduction.
The composite ischemic endpoint comprising cardiovascular death, MI, or ischemic stroke occurred in 3.6% of the ticagrelor monotherapy group and 4.8% of patients on long-term DAPT, a trend that didn’t achieve statistical significance. The all-cause mortality rate was 0.9% in the ticagrelor monotherapy group and 1.5% with extended DAPT, again a nonsignificant difference. Similarly, the rate of definite or probable stent thrombosis was numerically lower with ticagrelor monotherapy, by a margin of 0.4% versus 0.8%, a nonsignificant difference.
The results were consistent regardless of which specific criteria for complex PCI a patient had or how many of them.
Results are ‘reassuring’
At a press conference where Dr. Dangas presented the TWILIGHT-COMPLEX results, discussant Claire S. Duvernoy, MD, said she was “very impressed” with just how complex the PCIs were in the study participants.
“Really, these are the patients that in my own practice we’ve always been the most cautious about, the most worried about thrombotic risk, and the ones where we get down on our house staff when they drop an antiplatelet agent. So this study is very reassuring,” said Dr. Duvernoy, professor of medicine at the University of Michigan, Ann Arbor.
She identified two key differences between TWILIGHT-COMPLEX and earlier studies that showed a benefit for extended DAPT in higher-risk patients. In the earlier studies, it was the P2Y12 inhibitor that was dropped; TWILIGHT was the first major randomized trial to discontinue the aspirin instead. And patients in the TWILIGHT study received second-generation drug-eluting stents.
“That makes a huge difference,” Dr. Duvernoy said. “We have stents now that are much safer than the old ones were, and that’s what allows us to gain this incredible benefit of reduced bleeding.”
Dr. Dangas cautioned that since this was a secondary post hoc analysis, the TWILIGHT-COMPLEX study must be viewed as hypothesis-generating.
The TWILIGHT trial was funded by AstraZeneca. Dr. Dangas reported receiving institutional research grants from that company as well as Bayer and Daichi-Sankyo. He also served as a paid consultant to Abbott Vascular, Boston Scientific, and Biosensors.
Simultaneous with his presentation at ACC 2020, the TWILIGHT-COMPLEX results were published online (J Am Coll Cardiol. 2020 Mar 13. doi: 10.1016/j.jacc.2020.03.011).
SOURCE: Dangas GD. ACC 20, Abstract 410-09.
Patients who underwent complex PCI for acute coronary syndrome followed by 3 months of dual-antiplatelet therapy (DAPT) with ticagrelor plus aspirin fared significantly better by dropping aspirin at that point in favor of long-term ticagrelor monotherapy than with continued dual-antiplatelet therapy in the TWILIGHT-COMPLEX study.
The rate of clinically relevant bleeding was significantly lower at 12 months of follow-up in the ticagrelor monotherapy group than it was in patients randomized to continued DAPT. Moreover, this major benefit came at no cost in terms of ischemic events, which were actually numerically less frequent in the ticagrelor plus placebo group, George D. Dangas, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“We found that the aspirin just doesn’t add that much, even in complex patients – just bleeding complications, for the most part,” explained Dr. Dangas, professor of medicine and of surgery at the Icahn School of Medicine at Mount Sinai, New York.
The TWILIGHT-COMPLEX study was a secondary post hoc analysis of outcomes in 2,342 participants in the previously reported larger parent TWILIGHT randomized trial who underwent complex PCI. The main TWILIGHT trial included 7,119 patients in 11 countries who underwent PCI for acute coronary syndrome, successfully completed 3 months of DAPT with ticagrelor plus aspirin without incident, and were then randomized double blind to 12 months of ticagrelor plus placebo or to another 12 months of ticagrelor and aspirin.
In the overall TWILIGHT trial, ticagrelor alone resulted in a significantly lower clinically relevant bleeding rate than did long-term ticagrelor plus aspirin, with no increase in the risk of death, MI, or stroke (N Engl J Med 2019; 381:2032-42). But the results left many interventional cardiologists wondering if a ticagrelor monotherapy strategy was really applicable to their more challenging patients undergoing complex PCI given that the risk of ischemic events is known to climb with PCI complexity. The TWILIGHT-COMPLEX study was specifically designed to address that concern.
To be eligible for TWILIGHT-COMPLEX, patients had to meet one or more prespecified angiographic or procedural criteria for complex PCI, such as a total stent length in excess of 60 mm, three or more treated lesions, use of an atherectomy device, or PCI of a left main lesion, a chronic total occlusion, or a bifurcation lesion with two stents. These complex PCI patients accounted for one-third of the total study population in TWILIGHT; 36% of them met more than one criteria for complex PCI.
TWILIGHT-COMPLEX findings
In the 12 months after randomization, patients who received ticagrelor plus placebo had a 4.2% incidence of clinically significant Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding, which was significantly lower than the 7.7% rate in the group on long-term DAPT and represented a 46% relative risk reduction. Severe or fatal bleeding – that is, BARC type 3 or 5 – occurred in 1.1% of those on ticagrelor monotherapy and 2.6% of the DAPT group, for a significant 59% relative risk reduction.
The composite ischemic endpoint comprising cardiovascular death, MI, or ischemic stroke occurred in 3.6% of the ticagrelor monotherapy group and 4.8% of patients on long-term DAPT, a trend that didn’t achieve statistical significance. The all-cause mortality rate was 0.9% in the ticagrelor monotherapy group and 1.5% with extended DAPT, again a nonsignificant difference. Similarly, the rate of definite or probable stent thrombosis was numerically lower with ticagrelor monotherapy, by a margin of 0.4% versus 0.8%, a nonsignificant difference.
The results were consistent regardless of which specific criteria for complex PCI a patient had or how many of them.
Results are ‘reassuring’
At a press conference where Dr. Dangas presented the TWILIGHT-COMPLEX results, discussant Claire S. Duvernoy, MD, said she was “very impressed” with just how complex the PCIs were in the study participants.
“Really, these are the patients that in my own practice we’ve always been the most cautious about, the most worried about thrombotic risk, and the ones where we get down on our house staff when they drop an antiplatelet agent. So this study is very reassuring,” said Dr. Duvernoy, professor of medicine at the University of Michigan, Ann Arbor.
She identified two key differences between TWILIGHT-COMPLEX and earlier studies that showed a benefit for extended DAPT in higher-risk patients. In the earlier studies, it was the P2Y12 inhibitor that was dropped; TWILIGHT was the first major randomized trial to discontinue the aspirin instead. And patients in the TWILIGHT study received second-generation drug-eluting stents.
“That makes a huge difference,” Dr. Duvernoy said. “We have stents now that are much safer than the old ones were, and that’s what allows us to gain this incredible benefit of reduced bleeding.”
Dr. Dangas cautioned that since this was a secondary post hoc analysis, the TWILIGHT-COMPLEX study must be viewed as hypothesis-generating.
The TWILIGHT trial was funded by AstraZeneca. Dr. Dangas reported receiving institutional research grants from that company as well as Bayer and Daichi-Sankyo. He also served as a paid consultant to Abbott Vascular, Boston Scientific, and Biosensors.
Simultaneous with his presentation at ACC 2020, the TWILIGHT-COMPLEX results were published online (J Am Coll Cardiol. 2020 Mar 13. doi: 10.1016/j.jacc.2020.03.011).
SOURCE: Dangas GD. ACC 20, Abstract 410-09.
FROM ACC 2020
Low-risk TAVR loses ground at 2 years in PARTNER 3
Transcatheter aortic valve replacement (TAVR) continued to show superiority over surgical replacement in terms of the primary composite endpoint in low-surgical-risk patients at 2 years of follow-up in the landmark randomized PARTNER 3 trial, but the between-group differences favoring the transcatheter procedure in some key outcomes have narrowed considerably, Michael J. Mack, MD, reported in a video presentation of his research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“On the basis of 1-year data, many physicians were counseling patients that TAVR outcomes were better than surgery. Now we see that the outcomes are roughly the same at 2 years,” said Dr. Mack, who is medical director of cardiothoracic surgery and chairman of the Baylor Scott & White The Heart Hospital – Plano (Tex.) Research Center.
PARTNER 3 randomized 1,000 patients with severe symptomatic aortic stenosis with a tricuspid valve and a very low mean Society of Thoracic Surgeons risk score of 1.9% to TAVR with the Sapien 3 valve or surgical aortic valve replacement (SAVR). The 1-year results presented at ACC 2019 caused a huge stir, with the primary composite outcome of death, stroke, or cardiovascular rehospitalization occurring in 8.5% of TAVR patients and 15.6% of the SAVR group, representing a 48% relative risk reduction and a resounding win for TAVR (N Engl J Med. 2019 May 2;380:1695-705). At 2 years, the difference in the composite outcome remained statistically significant, but the gap had closed: 11.5% with TAVR and 17.4% with SAVR for a 37% relative risk reduction.
Moreover, the between-group difference in stroke, which at 1 year was significantly in favor of TAVR at 1.2% versus 3.3%, was no longer significant at 2 years, with rates of 2.4% versus 3.6%. Nor was the difference in mortality significant: 2.4% with TAVR, 3.2% with SAVR.
What was a statistically significant between-group difference at 2 years – and an eye-catching one at that – involved the cumulative incidence of valve thrombosis confirmed by CT or echocardiography: 2.6% in the TAVR arm, compared with 0.7% with SAVR, with most of these unwanted events coming in year 2.
The good news was there was no echocardiographic evidence of deterioration in valve structure or function in either study arm at 2 years. The mean gradients and aortic valve areas remained unchanged in both arms between 1 and 2 years, as did the frequency of mild or moderate paravalvular leak. Prospective follow-up will continue annually out to 10 years.
“I think it’s way too early to expect to see a signal, but I think it’s somewhat comforting at this point that there’s no signal of early structural valve deterioration,” Dr. Mack said.
Discussant Howard C. Hermann, MD, commented: “I guess the biggest concern in looking at the data is the increase in stroke and valve thrombosis, both numerically and relative to SAVR, between years 1 and 2.”
Dr. Mack offered a note of reassurance regarding the valve thrombosis findings: The rates he presented were based upon the now-outdated second Valve Academic Research Consortium (VARC-2) definition, per study protocol. When he and his coinvestigators recalculated the valve thrombosis rates using the contemporary VARC-3 definition of valve deterioration and bioprosthetic valve failure, the incidence was very low and not significantly different in the two study arms, at roughly 1%.
Dr. Hermann, professor of medicine and director of the cardiac catheterization laboratories at the University of Pennsylvania, Philadelphia, had a question: As a clinician taking care of TAVR patients, what clinical or hemodynamic findings should prompt an imaging study looking for valve thrombus or deterioration that might prompt initiating oral anticoagulation?
“If there’s a change in hemodynamics, an increasing valve gradient, if there’s increasing paravalvular leak, or if there’s a change in symptoms, that should prompt an imaging study. Only with confirmation of valve thrombosis on an imaging study should anticoagulation be considered. Oral anticoagulation is not benign: Of the six clinical events associated with valve thrombosis in the study, two were related to anticoagulation,” Dr. Mack replied.
“Regarding whether patients should receive warfarin or a novel anticoagulant, I don’t think we have evidence that there’s benefit to anything other than warfarin at the current time,” he added.
Dr. Mack reported receiving research support from Edwards Lifesciences, the sponsor of PARTNER 3, as well as from Abbott, Gore, and Medtronic.
Transcatheter aortic valve replacement (TAVR) continued to show superiority over surgical replacement in terms of the primary composite endpoint in low-surgical-risk patients at 2 years of follow-up in the landmark randomized PARTNER 3 trial, but the between-group differences favoring the transcatheter procedure in some key outcomes have narrowed considerably, Michael J. Mack, MD, reported in a video presentation of his research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“On the basis of 1-year data, many physicians were counseling patients that TAVR outcomes were better than surgery. Now we see that the outcomes are roughly the same at 2 years,” said Dr. Mack, who is medical director of cardiothoracic surgery and chairman of the Baylor Scott & White The Heart Hospital – Plano (Tex.) Research Center.
PARTNER 3 randomized 1,000 patients with severe symptomatic aortic stenosis with a tricuspid valve and a very low mean Society of Thoracic Surgeons risk score of 1.9% to TAVR with the Sapien 3 valve or surgical aortic valve replacement (SAVR). The 1-year results presented at ACC 2019 caused a huge stir, with the primary composite outcome of death, stroke, or cardiovascular rehospitalization occurring in 8.5% of TAVR patients and 15.6% of the SAVR group, representing a 48% relative risk reduction and a resounding win for TAVR (N Engl J Med. 2019 May 2;380:1695-705). At 2 years, the difference in the composite outcome remained statistically significant, but the gap had closed: 11.5% with TAVR and 17.4% with SAVR for a 37% relative risk reduction.
Moreover, the between-group difference in stroke, which at 1 year was significantly in favor of TAVR at 1.2% versus 3.3%, was no longer significant at 2 years, with rates of 2.4% versus 3.6%. Nor was the difference in mortality significant: 2.4% with TAVR, 3.2% with SAVR.
What was a statistically significant between-group difference at 2 years – and an eye-catching one at that – involved the cumulative incidence of valve thrombosis confirmed by CT or echocardiography: 2.6% in the TAVR arm, compared with 0.7% with SAVR, with most of these unwanted events coming in year 2.
The good news was there was no echocardiographic evidence of deterioration in valve structure or function in either study arm at 2 years. The mean gradients and aortic valve areas remained unchanged in both arms between 1 and 2 years, as did the frequency of mild or moderate paravalvular leak. Prospective follow-up will continue annually out to 10 years.
“I think it’s way too early to expect to see a signal, but I think it’s somewhat comforting at this point that there’s no signal of early structural valve deterioration,” Dr. Mack said.
Discussant Howard C. Hermann, MD, commented: “I guess the biggest concern in looking at the data is the increase in stroke and valve thrombosis, both numerically and relative to SAVR, between years 1 and 2.”
Dr. Mack offered a note of reassurance regarding the valve thrombosis findings: The rates he presented were based upon the now-outdated second Valve Academic Research Consortium (VARC-2) definition, per study protocol. When he and his coinvestigators recalculated the valve thrombosis rates using the contemporary VARC-3 definition of valve deterioration and bioprosthetic valve failure, the incidence was very low and not significantly different in the two study arms, at roughly 1%.
Dr. Hermann, professor of medicine and director of the cardiac catheterization laboratories at the University of Pennsylvania, Philadelphia, had a question: As a clinician taking care of TAVR patients, what clinical or hemodynamic findings should prompt an imaging study looking for valve thrombus or deterioration that might prompt initiating oral anticoagulation?
“If there’s a change in hemodynamics, an increasing valve gradient, if there’s increasing paravalvular leak, or if there’s a change in symptoms, that should prompt an imaging study. Only with confirmation of valve thrombosis on an imaging study should anticoagulation be considered. Oral anticoagulation is not benign: Of the six clinical events associated with valve thrombosis in the study, two were related to anticoagulation,” Dr. Mack replied.
“Regarding whether patients should receive warfarin or a novel anticoagulant, I don’t think we have evidence that there’s benefit to anything other than warfarin at the current time,” he added.
Dr. Mack reported receiving research support from Edwards Lifesciences, the sponsor of PARTNER 3, as well as from Abbott, Gore, and Medtronic.
Transcatheter aortic valve replacement (TAVR) continued to show superiority over surgical replacement in terms of the primary composite endpoint in low-surgical-risk patients at 2 years of follow-up in the landmark randomized PARTNER 3 trial, but the between-group differences favoring the transcatheter procedure in some key outcomes have narrowed considerably, Michael J. Mack, MD, reported in a video presentation of his research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
“On the basis of 1-year data, many physicians were counseling patients that TAVR outcomes were better than surgery. Now we see that the outcomes are roughly the same at 2 years,” said Dr. Mack, who is medical director of cardiothoracic surgery and chairman of the Baylor Scott & White The Heart Hospital – Plano (Tex.) Research Center.
PARTNER 3 randomized 1,000 patients with severe symptomatic aortic stenosis with a tricuspid valve and a very low mean Society of Thoracic Surgeons risk score of 1.9% to TAVR with the Sapien 3 valve or surgical aortic valve replacement (SAVR). The 1-year results presented at ACC 2019 caused a huge stir, with the primary composite outcome of death, stroke, or cardiovascular rehospitalization occurring in 8.5% of TAVR patients and 15.6% of the SAVR group, representing a 48% relative risk reduction and a resounding win for TAVR (N Engl J Med. 2019 May 2;380:1695-705). At 2 years, the difference in the composite outcome remained statistically significant, but the gap had closed: 11.5% with TAVR and 17.4% with SAVR for a 37% relative risk reduction.
Moreover, the between-group difference in stroke, which at 1 year was significantly in favor of TAVR at 1.2% versus 3.3%, was no longer significant at 2 years, with rates of 2.4% versus 3.6%. Nor was the difference in mortality significant: 2.4% with TAVR, 3.2% with SAVR.
What was a statistically significant between-group difference at 2 years – and an eye-catching one at that – involved the cumulative incidence of valve thrombosis confirmed by CT or echocardiography: 2.6% in the TAVR arm, compared with 0.7% with SAVR, with most of these unwanted events coming in year 2.
The good news was there was no echocardiographic evidence of deterioration in valve structure or function in either study arm at 2 years. The mean gradients and aortic valve areas remained unchanged in both arms between 1 and 2 years, as did the frequency of mild or moderate paravalvular leak. Prospective follow-up will continue annually out to 10 years.
“I think it’s way too early to expect to see a signal, but I think it’s somewhat comforting at this point that there’s no signal of early structural valve deterioration,” Dr. Mack said.
Discussant Howard C. Hermann, MD, commented: “I guess the biggest concern in looking at the data is the increase in stroke and valve thrombosis, both numerically and relative to SAVR, between years 1 and 2.”
Dr. Mack offered a note of reassurance regarding the valve thrombosis findings: The rates he presented were based upon the now-outdated second Valve Academic Research Consortium (VARC-2) definition, per study protocol. When he and his coinvestigators recalculated the valve thrombosis rates using the contemporary VARC-3 definition of valve deterioration and bioprosthetic valve failure, the incidence was very low and not significantly different in the two study arms, at roughly 1%.
Dr. Hermann, professor of medicine and director of the cardiac catheterization laboratories at the University of Pennsylvania, Philadelphia, had a question: As a clinician taking care of TAVR patients, what clinical or hemodynamic findings should prompt an imaging study looking for valve thrombus or deterioration that might prompt initiating oral anticoagulation?
“If there’s a change in hemodynamics, an increasing valve gradient, if there’s increasing paravalvular leak, or if there’s a change in symptoms, that should prompt an imaging study. Only with confirmation of valve thrombosis on an imaging study should anticoagulation be considered. Oral anticoagulation is not benign: Of the six clinical events associated with valve thrombosis in the study, two were related to anticoagulation,” Dr. Mack replied.
“Regarding whether patients should receive warfarin or a novel anticoagulant, I don’t think we have evidence that there’s benefit to anything other than warfarin at the current time,” he added.
Dr. Mack reported receiving research support from Edwards Lifesciences, the sponsor of PARTNER 3, as well as from Abbott, Gore, and Medtronic.
FROM ACC 2020
National Watchman registry reports impressive procedural safety
Early results from the massive National Cardiovascular Data Registry Left Atrial Appendage Occlusion Registry indicate that the rollout of the Watchman device into routine clinical practice is going smoothly, with a higher implant success rate and a substantially lower in-hospital complication rate than that seen in the pivotal randomized clinical trials, James V. Freeman, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
These real-world results are particularly impressive because the 38,158 registry participants were on average significantly older and sicker than were patients in the clinical trials. They were at higher risk of both stroke and bleeding, yet they fared better in terms of procedural safety, observed Dr. Freeman, an electrophysiologist and director of the Yale University Atrial Fibrillation Center in New Haven, Conn.
“You always worry that once you get outside of the clinical trials setting and you roll out to a large number of centers, including some that are relatively low volume, that you’re going to start to see higher rates of complications. And overall, broadly speaking, the rates of adverse events were quite reassuring,” he said.
The registry, maintained by the ACC, serves as the postmarketing surveillance tool mandated by the Food and Drug Administration and Centers for Medicare & Medicaid Services. The 38,158 participants make this registry the world’s largest patient experience with the Watchman device by many orders of magnitude. Dr. Freeman’s report included patients enrolled during 2016-2018 who were treated at 495 hospitals by 1,318 physician interventionalists. CMS reimbursement requires participation in the registry, which captures more than 95% of all Watchman procedures done in the United States. Although Dr. Freeman presented only the acute in-hospital outcomes, active follow-up for adverse events and medical therapy will be conducted at 45 days, 6 months, and 1 and 2 years.
Participants in the Left Atrial Appendage Occlusion (LAAO) Registry averaged 76.1 years of age, which is 2-4 years older than patients in the pivotal PROTECT-AF and PREVAIL trials or the 1,025-patient EWOLUTION registry. The LAAO Registry participants had a mean CHA2DS2-VASc score of 4.6, compared with 3.4 in PROTECT-AF and 3.8 in PREVAIL. Their mean HAS BLED score was 3.0. Thirty percent had a prior ischemic stroke or transient ischemic attack, 12% had a prior intracranial hemorrhage, and 69% had a history of clinically relevant bleeding. Thirty percent had heart failure, 92% were hypertensive, and 30% had diabetes.
“The take home here is that these patients were at moderate to high risk of stroke and they also carried a high risk of bleeding and therefore had some relative contraindication to anticoagulation,” according to the cardiologist. “The patient population overall is really in accordance with the CMS guidance. We’re not seeing a lot of patients who are getting this device for a lifestyle indication. Most of these patients are really stuck between a rock and a hard place.”
Most hospitals offering the Watchman did 10-40 cases per year. The median annual physician volume was 12 cases. However, there was substantial variation in both hospital and physician volumes.
The device was deployed in 93% of procedures attempted; roughly half of cancellations were cause by LAAO thrombus detected on the day of the procedure. The acute procedural success rate when the device was deployed was 98.3%, compared with 90.9% in PROTECT-AF and 95.1% in PREVAIL. The rate of device margin residual leak of 5 mm or more among registry participants with an acutely successful procedure was 0.2%.
The rate of any major in-hospital complication in the LAAO Registry was 2.16%, the most common of which was pericardial effusion requiring intervention, which occurred in 1.39% of cases. The major bleeding rate was 1.25%. The stroke/transient ischemic attack rate was 0.17%. Systemic arterial embolism was a rare event, occurring in less than 0.01% of patients, as was acute MI, with an incidence of 0.04%. Device embolization occurred in 0.07% of patients.
By comparison, the 7-day rate of pericardial effusion requiring intervention was 4.0% in PROTECT-AF and 1.9% in PREVAIL, with procedure-related stroke rates of 1.1% and 0.7%, respectively, and device embolization rates of 0.4% and 0.7%. The major bleeding rate in PROTECT-AF was 3.5%, nearly triple that in the real-world registry.
Discussant Mark A. Estes, MD, characterized the acute outcomes in the LAAO Registry as “an improvement – a considerable improvement – over some of the early data in PREVAIL and PROTECT-AF.” He credited this to the “very robust validation procedure” the Watchman closure device has undergone, which included the clinical trials, regulatory requirements for training and patient selection, and mandatory reporting of outcomes in the registry.
He noted that a lot is happening now with the Watchman device. There are a couple of dozen prospective clinical trials, including one on the Watchman versus direct oral anticoagulant (DOAC) therapy and another on left atrial ablation plus left atrial appendage closure versus a DOAC. A new-generation Watchman device, the Watchman FLX, is approved in Europe and undergoing an ongoing FDA-mandated approval trial in the United States.
“It has a lot of technical advantages,” according to Dr. Estes, an electrophysiologist and professor of medicine at the University of Pittsburgh.
Current guidelines give LAAO a class IIb rating, meaning it “could be considered” in patients with atrial fibrillation at increased risk of stroke who have a contraindication to long-term anticoagulation. Dr. Estes asked: Does the LAAO Registry data warrant a rating upgrade to a stronger recommendation?
Dr. Freeman replied that the new data should allay the guideline writers’ and government regulators’ concerns regarding acute procedural safety. But that’s only part of the picture. He and his coinvestigators are busy gathering data on intermediate-term outcomes, analyzing the impact of various strategies for periprocedural and long-term management of antiplatelet and anticoagulant medications with an eye toward identifying best practices, and investigating the relationship between procedural volume and outcomes, information, which could have an impact on the next iteration of the guidelines.
Simultaneous with his presentation at ACC 2020, the study was published online (J Am Coll Cardiol. 2020 Mar 13;75[13]1503-18).
In an accompanying editorial, Dhanunjaya Lakkireddy, MD, commented that an important contribution of the LAAO Registry is its inclusion of an enormous number of patients with contraindications to oral anticoagulation, a population excluded from the PROTECT-AF and PREVAIL randomized trials.
The short-term results of the registry suggest a relaxation of the current strict requirement for surgical backup during Watchman procedures is in order, added Dr. Lakkireddy, professor of medicine at the University of Missouri, Columbia, and medical director of the Kansas City Heart Rhythm Institute (J Am Coll Cardiol. 2020 Mar 13;75[13]:1519-22).
Dr. Freeman reported serving as a consultant to Boston Scientific, which markets the Watchman, as well as to Medtronic, Janssen, and Biosense Webster.
SOURCE: Freeman JF. ACC 2020, Abstract 409-10.
Early results from the massive National Cardiovascular Data Registry Left Atrial Appendage Occlusion Registry indicate that the rollout of the Watchman device into routine clinical practice is going smoothly, with a higher implant success rate and a substantially lower in-hospital complication rate than that seen in the pivotal randomized clinical trials, James V. Freeman, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
These real-world results are particularly impressive because the 38,158 registry participants were on average significantly older and sicker than were patients in the clinical trials. They were at higher risk of both stroke and bleeding, yet they fared better in terms of procedural safety, observed Dr. Freeman, an electrophysiologist and director of the Yale University Atrial Fibrillation Center in New Haven, Conn.
“You always worry that once you get outside of the clinical trials setting and you roll out to a large number of centers, including some that are relatively low volume, that you’re going to start to see higher rates of complications. And overall, broadly speaking, the rates of adverse events were quite reassuring,” he said.
The registry, maintained by the ACC, serves as the postmarketing surveillance tool mandated by the Food and Drug Administration and Centers for Medicare & Medicaid Services. The 38,158 participants make this registry the world’s largest patient experience with the Watchman device by many orders of magnitude. Dr. Freeman’s report included patients enrolled during 2016-2018 who were treated at 495 hospitals by 1,318 physician interventionalists. CMS reimbursement requires participation in the registry, which captures more than 95% of all Watchman procedures done in the United States. Although Dr. Freeman presented only the acute in-hospital outcomes, active follow-up for adverse events and medical therapy will be conducted at 45 days, 6 months, and 1 and 2 years.
Participants in the Left Atrial Appendage Occlusion (LAAO) Registry averaged 76.1 years of age, which is 2-4 years older than patients in the pivotal PROTECT-AF and PREVAIL trials or the 1,025-patient EWOLUTION registry. The LAAO Registry participants had a mean CHA2DS2-VASc score of 4.6, compared with 3.4 in PROTECT-AF and 3.8 in PREVAIL. Their mean HAS BLED score was 3.0. Thirty percent had a prior ischemic stroke or transient ischemic attack, 12% had a prior intracranial hemorrhage, and 69% had a history of clinically relevant bleeding. Thirty percent had heart failure, 92% were hypertensive, and 30% had diabetes.
“The take home here is that these patients were at moderate to high risk of stroke and they also carried a high risk of bleeding and therefore had some relative contraindication to anticoagulation,” according to the cardiologist. “The patient population overall is really in accordance with the CMS guidance. We’re not seeing a lot of patients who are getting this device for a lifestyle indication. Most of these patients are really stuck between a rock and a hard place.”
Most hospitals offering the Watchman did 10-40 cases per year. The median annual physician volume was 12 cases. However, there was substantial variation in both hospital and physician volumes.
The device was deployed in 93% of procedures attempted; roughly half of cancellations were cause by LAAO thrombus detected on the day of the procedure. The acute procedural success rate when the device was deployed was 98.3%, compared with 90.9% in PROTECT-AF and 95.1% in PREVAIL. The rate of device margin residual leak of 5 mm or more among registry participants with an acutely successful procedure was 0.2%.
The rate of any major in-hospital complication in the LAAO Registry was 2.16%, the most common of which was pericardial effusion requiring intervention, which occurred in 1.39% of cases. The major bleeding rate was 1.25%. The stroke/transient ischemic attack rate was 0.17%. Systemic arterial embolism was a rare event, occurring in less than 0.01% of patients, as was acute MI, with an incidence of 0.04%. Device embolization occurred in 0.07% of patients.
By comparison, the 7-day rate of pericardial effusion requiring intervention was 4.0% in PROTECT-AF and 1.9% in PREVAIL, with procedure-related stroke rates of 1.1% and 0.7%, respectively, and device embolization rates of 0.4% and 0.7%. The major bleeding rate in PROTECT-AF was 3.5%, nearly triple that in the real-world registry.
Discussant Mark A. Estes, MD, characterized the acute outcomes in the LAAO Registry as “an improvement – a considerable improvement – over some of the early data in PREVAIL and PROTECT-AF.” He credited this to the “very robust validation procedure” the Watchman closure device has undergone, which included the clinical trials, regulatory requirements for training and patient selection, and mandatory reporting of outcomes in the registry.
He noted that a lot is happening now with the Watchman device. There are a couple of dozen prospective clinical trials, including one on the Watchman versus direct oral anticoagulant (DOAC) therapy and another on left atrial ablation plus left atrial appendage closure versus a DOAC. A new-generation Watchman device, the Watchman FLX, is approved in Europe and undergoing an ongoing FDA-mandated approval trial in the United States.
“It has a lot of technical advantages,” according to Dr. Estes, an electrophysiologist and professor of medicine at the University of Pittsburgh.
Current guidelines give LAAO a class IIb rating, meaning it “could be considered” in patients with atrial fibrillation at increased risk of stroke who have a contraindication to long-term anticoagulation. Dr. Estes asked: Does the LAAO Registry data warrant a rating upgrade to a stronger recommendation?
Dr. Freeman replied that the new data should allay the guideline writers’ and government regulators’ concerns regarding acute procedural safety. But that’s only part of the picture. He and his coinvestigators are busy gathering data on intermediate-term outcomes, analyzing the impact of various strategies for periprocedural and long-term management of antiplatelet and anticoagulant medications with an eye toward identifying best practices, and investigating the relationship between procedural volume and outcomes, information, which could have an impact on the next iteration of the guidelines.
Simultaneous with his presentation at ACC 2020, the study was published online (J Am Coll Cardiol. 2020 Mar 13;75[13]1503-18).
In an accompanying editorial, Dhanunjaya Lakkireddy, MD, commented that an important contribution of the LAAO Registry is its inclusion of an enormous number of patients with contraindications to oral anticoagulation, a population excluded from the PROTECT-AF and PREVAIL randomized trials.
The short-term results of the registry suggest a relaxation of the current strict requirement for surgical backup during Watchman procedures is in order, added Dr. Lakkireddy, professor of medicine at the University of Missouri, Columbia, and medical director of the Kansas City Heart Rhythm Institute (J Am Coll Cardiol. 2020 Mar 13;75[13]:1519-22).
Dr. Freeman reported serving as a consultant to Boston Scientific, which markets the Watchman, as well as to Medtronic, Janssen, and Biosense Webster.
SOURCE: Freeman JF. ACC 2020, Abstract 409-10.
Early results from the massive National Cardiovascular Data Registry Left Atrial Appendage Occlusion Registry indicate that the rollout of the Watchman device into routine clinical practice is going smoothly, with a higher implant success rate and a substantially lower in-hospital complication rate than that seen in the pivotal randomized clinical trials, James V. Freeman, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
These real-world results are particularly impressive because the 38,158 registry participants were on average significantly older and sicker than were patients in the clinical trials. They were at higher risk of both stroke and bleeding, yet they fared better in terms of procedural safety, observed Dr. Freeman, an electrophysiologist and director of the Yale University Atrial Fibrillation Center in New Haven, Conn.
“You always worry that once you get outside of the clinical trials setting and you roll out to a large number of centers, including some that are relatively low volume, that you’re going to start to see higher rates of complications. And overall, broadly speaking, the rates of adverse events were quite reassuring,” he said.
The registry, maintained by the ACC, serves as the postmarketing surveillance tool mandated by the Food and Drug Administration and Centers for Medicare & Medicaid Services. The 38,158 participants make this registry the world’s largest patient experience with the Watchman device by many orders of magnitude. Dr. Freeman’s report included patients enrolled during 2016-2018 who were treated at 495 hospitals by 1,318 physician interventionalists. CMS reimbursement requires participation in the registry, which captures more than 95% of all Watchman procedures done in the United States. Although Dr. Freeman presented only the acute in-hospital outcomes, active follow-up for adverse events and medical therapy will be conducted at 45 days, 6 months, and 1 and 2 years.
Participants in the Left Atrial Appendage Occlusion (LAAO) Registry averaged 76.1 years of age, which is 2-4 years older than patients in the pivotal PROTECT-AF and PREVAIL trials or the 1,025-patient EWOLUTION registry. The LAAO Registry participants had a mean CHA2DS2-VASc score of 4.6, compared with 3.4 in PROTECT-AF and 3.8 in PREVAIL. Their mean HAS BLED score was 3.0. Thirty percent had a prior ischemic stroke or transient ischemic attack, 12% had a prior intracranial hemorrhage, and 69% had a history of clinically relevant bleeding. Thirty percent had heart failure, 92% were hypertensive, and 30% had diabetes.
“The take home here is that these patients were at moderate to high risk of stroke and they also carried a high risk of bleeding and therefore had some relative contraindication to anticoagulation,” according to the cardiologist. “The patient population overall is really in accordance with the CMS guidance. We’re not seeing a lot of patients who are getting this device for a lifestyle indication. Most of these patients are really stuck between a rock and a hard place.”
Most hospitals offering the Watchman did 10-40 cases per year. The median annual physician volume was 12 cases. However, there was substantial variation in both hospital and physician volumes.
The device was deployed in 93% of procedures attempted; roughly half of cancellations were cause by LAAO thrombus detected on the day of the procedure. The acute procedural success rate when the device was deployed was 98.3%, compared with 90.9% in PROTECT-AF and 95.1% in PREVAIL. The rate of device margin residual leak of 5 mm or more among registry participants with an acutely successful procedure was 0.2%.
The rate of any major in-hospital complication in the LAAO Registry was 2.16%, the most common of which was pericardial effusion requiring intervention, which occurred in 1.39% of cases. The major bleeding rate was 1.25%. The stroke/transient ischemic attack rate was 0.17%. Systemic arterial embolism was a rare event, occurring in less than 0.01% of patients, as was acute MI, with an incidence of 0.04%. Device embolization occurred in 0.07% of patients.
By comparison, the 7-day rate of pericardial effusion requiring intervention was 4.0% in PROTECT-AF and 1.9% in PREVAIL, with procedure-related stroke rates of 1.1% and 0.7%, respectively, and device embolization rates of 0.4% and 0.7%. The major bleeding rate in PROTECT-AF was 3.5%, nearly triple that in the real-world registry.
Discussant Mark A. Estes, MD, characterized the acute outcomes in the LAAO Registry as “an improvement – a considerable improvement – over some of the early data in PREVAIL and PROTECT-AF.” He credited this to the “very robust validation procedure” the Watchman closure device has undergone, which included the clinical trials, regulatory requirements for training and patient selection, and mandatory reporting of outcomes in the registry.
He noted that a lot is happening now with the Watchman device. There are a couple of dozen prospective clinical trials, including one on the Watchman versus direct oral anticoagulant (DOAC) therapy and another on left atrial ablation plus left atrial appendage closure versus a DOAC. A new-generation Watchman device, the Watchman FLX, is approved in Europe and undergoing an ongoing FDA-mandated approval trial in the United States.
“It has a lot of technical advantages,” according to Dr. Estes, an electrophysiologist and professor of medicine at the University of Pittsburgh.
Current guidelines give LAAO a class IIb rating, meaning it “could be considered” in patients with atrial fibrillation at increased risk of stroke who have a contraindication to long-term anticoagulation. Dr. Estes asked: Does the LAAO Registry data warrant a rating upgrade to a stronger recommendation?
Dr. Freeman replied that the new data should allay the guideline writers’ and government regulators’ concerns regarding acute procedural safety. But that’s only part of the picture. He and his coinvestigators are busy gathering data on intermediate-term outcomes, analyzing the impact of various strategies for periprocedural and long-term management of antiplatelet and anticoagulant medications with an eye toward identifying best practices, and investigating the relationship between procedural volume and outcomes, information, which could have an impact on the next iteration of the guidelines.
Simultaneous with his presentation at ACC 2020, the study was published online (J Am Coll Cardiol. 2020 Mar 13;75[13]1503-18).
In an accompanying editorial, Dhanunjaya Lakkireddy, MD, commented that an important contribution of the LAAO Registry is its inclusion of an enormous number of patients with contraindications to oral anticoagulation, a population excluded from the PROTECT-AF and PREVAIL randomized trials.
The short-term results of the registry suggest a relaxation of the current strict requirement for surgical backup during Watchman procedures is in order, added Dr. Lakkireddy, professor of medicine at the University of Missouri, Columbia, and medical director of the Kansas City Heart Rhythm Institute (J Am Coll Cardiol. 2020 Mar 13;75[13]:1519-22).
Dr. Freeman reported serving as a consultant to Boston Scientific, which markets the Watchman, as well as to Medtronic, Janssen, and Biosense Webster.
SOURCE: Freeman JF. ACC 2020, Abstract 409-10.
FROM ACC 2020
Radial arteries show CABG survival advantage over saphenous veins
Coronary bypass surgery patients who received a radial artery as their second bypass conduit had significantly better 10-year survival than did patients who received a saphenous vein graft in a combined analysis of more than 1,000 randomized patients who had originally been enrolled in any of five independent studies.
“This is the first report of a survival benefit for CABG [coronary artery bypass grafting] using multiple arterial conduits based on randomized data,” Mario F.L. Gaudino, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
Dr. Gaudino acknowledged several limitations of the finding. First, the analysis included studies that enrolled patients during 1997-2009 in five diverse sites worldwide and, therefore, involved varying surgical methods. Second, the sample size was “relatively low and underpowered, even after 10-year follow-up.” And third, the survival analysis was post hoc, although the statistically significant 27% relative reduction in mortality during follow-up with radial artery bypass, compared with saphenous vein bypass, was fully consistent with both the primary endpoint of the five studies and also with the combined hard endpoint of death and myocardial infarction.
The primary outcome of all-cause death, MI, and repeat revascularization also fell by a relative 27% with radial artery bypass, compared with saphenous vein bypass, and the combined rate of death and MI fell by 23% with radial artery bypass, both statistically significant differences, reported Dr. Gaudino, professor of cardiothoracic surgery at Weill Cornell Medicine, New York.
“The overall message is that radial bypass is associated with better long-term outcomes and potentially better survival,” he concluded.
The left interior thoracic artery (also known as the left internal mammary artery) is well established as the primary CABG conduit, usually used for bypassing the left anterior descending coronary artery, but when a second conduit is needed, several options exist: a saphenous vein, the left radial artery, or possibly the right internal thoracic artery (RITA) as a different arterial option.
Dr. Gaudino claimed that his new results placed the left radial artery clearly superior to the RITA as the second arterial conduit of choice for CABG. Not only does the RITA lack a similar efficacy evidence base from randomized trials, but the method poses a higher risk for surgical wound infections, he noted. The most recent society recommendations on conduit choice for CABG, issued less than 2 years ago by the European Society of Cardiology and European Association for Cardio-Thoracic Surgery, tapped the left radial artery as a level I recommendation over a saphenous vein graft when patients have high-grade coronary stenosis, while the RITA trailed as a level IIa recommendation specified only for patients with a low risk for sternal-wound infection.
“This was a great study that brings home the point that, in general, the radial artery is better than a saphenous vein graft,” commented Marc R. Moon, MD, a designated discussant and a professor of surgery and chief of cardiac surgery at Washington University, St. Louis.
The long-term follow-up that Dr. Gaudino reported came from extended, patient-level data collection for all 1,036 patients included in the original RADIAL (Radial Artery Database International Alliance) analysis of 5-year outcomes and reported in 2018. Dr. Gaudino and his associates tracked down survival information for all those patients, with outcome records out to at least 10 years for 91% of the original participants and with a mean follow-up that was also 10 years. The prior 2018 report based on 5-year results had also shown a statistically significant reduction in the primary endpoint with radial artery grafting, but at that point, follow-up had not yet collected enough mortality endpoints to produce a statistically significant between-group difference in death from any cause, a shortcoming that may have limited the ability of the prior report to influence U.S. practice.
“In the United States, there has been very little uptake of multiarterial grafting,” commented Frederick G.P. Welt, MD, a designated discussant, interventional cardiologist, professor of medicine, and associate chief of cardiovascular medicine at the University of Utah, Salt Lake City. The results from several earlier studies did not show much benefit for graft patency using radial arteries, but more recently clinicians have made advances in radial artery harvesting methods, implantation techniques, and adjunctive medications including antispasmodic treatments, Dr. Welt noted. Improved methods for using radial artery grafts and the risk of wound infection with RITA grafts were summarized in an editorial that accompanied the report of the 5-year RADIAL findings.
Dr. Welt said that, among the new findings reported by Dr. Gaudino, “the mortality effect is the most impressive.” Despite the limitations of the post hoc survival analysis, the reduced mortality finding is “nevertheless really important. The patient-level data lend it more credence.”
The study received no commercial funding. Dr. Gaudino had no disclosures. Dr. Moon has been a consultant to Medtronic. Dr. Welt has been an adviser to Medtronic.
SOURCE: Gaudino MFL et al. ACC 20, Abstract 410-11.
Coronary bypass surgery patients who received a radial artery as their second bypass conduit had significantly better 10-year survival than did patients who received a saphenous vein graft in a combined analysis of more than 1,000 randomized patients who had originally been enrolled in any of five independent studies.
“This is the first report of a survival benefit for CABG [coronary artery bypass grafting] using multiple arterial conduits based on randomized data,” Mario F.L. Gaudino, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
Dr. Gaudino acknowledged several limitations of the finding. First, the analysis included studies that enrolled patients during 1997-2009 in five diverse sites worldwide and, therefore, involved varying surgical methods. Second, the sample size was “relatively low and underpowered, even after 10-year follow-up.” And third, the survival analysis was post hoc, although the statistically significant 27% relative reduction in mortality during follow-up with radial artery bypass, compared with saphenous vein bypass, was fully consistent with both the primary endpoint of the five studies and also with the combined hard endpoint of death and myocardial infarction.
The primary outcome of all-cause death, MI, and repeat revascularization also fell by a relative 27% with radial artery bypass, compared with saphenous vein bypass, and the combined rate of death and MI fell by 23% with radial artery bypass, both statistically significant differences, reported Dr. Gaudino, professor of cardiothoracic surgery at Weill Cornell Medicine, New York.
“The overall message is that radial bypass is associated with better long-term outcomes and potentially better survival,” he concluded.
The left interior thoracic artery (also known as the left internal mammary artery) is well established as the primary CABG conduit, usually used for bypassing the left anterior descending coronary artery, but when a second conduit is needed, several options exist: a saphenous vein, the left radial artery, or possibly the right internal thoracic artery (RITA) as a different arterial option.
Dr. Gaudino claimed that his new results placed the left radial artery clearly superior to the RITA as the second arterial conduit of choice for CABG. Not only does the RITA lack a similar efficacy evidence base from randomized trials, but the method poses a higher risk for surgical wound infections, he noted. The most recent society recommendations on conduit choice for CABG, issued less than 2 years ago by the European Society of Cardiology and European Association for Cardio-Thoracic Surgery, tapped the left radial artery as a level I recommendation over a saphenous vein graft when patients have high-grade coronary stenosis, while the RITA trailed as a level IIa recommendation specified only for patients with a low risk for sternal-wound infection.
“This was a great study that brings home the point that, in general, the radial artery is better than a saphenous vein graft,” commented Marc R. Moon, MD, a designated discussant and a professor of surgery and chief of cardiac surgery at Washington University, St. Louis.
The long-term follow-up that Dr. Gaudino reported came from extended, patient-level data collection for all 1,036 patients included in the original RADIAL (Radial Artery Database International Alliance) analysis of 5-year outcomes and reported in 2018. Dr. Gaudino and his associates tracked down survival information for all those patients, with outcome records out to at least 10 years for 91% of the original participants and with a mean follow-up that was also 10 years. The prior 2018 report based on 5-year results had also shown a statistically significant reduction in the primary endpoint with radial artery grafting, but at that point, follow-up had not yet collected enough mortality endpoints to produce a statistically significant between-group difference in death from any cause, a shortcoming that may have limited the ability of the prior report to influence U.S. practice.
“In the United States, there has been very little uptake of multiarterial grafting,” commented Frederick G.P. Welt, MD, a designated discussant, interventional cardiologist, professor of medicine, and associate chief of cardiovascular medicine at the University of Utah, Salt Lake City. The results from several earlier studies did not show much benefit for graft patency using radial arteries, but more recently clinicians have made advances in radial artery harvesting methods, implantation techniques, and adjunctive medications including antispasmodic treatments, Dr. Welt noted. Improved methods for using radial artery grafts and the risk of wound infection with RITA grafts were summarized in an editorial that accompanied the report of the 5-year RADIAL findings.
Dr. Welt said that, among the new findings reported by Dr. Gaudino, “the mortality effect is the most impressive.” Despite the limitations of the post hoc survival analysis, the reduced mortality finding is “nevertheless really important. The patient-level data lend it more credence.”
The study received no commercial funding. Dr. Gaudino had no disclosures. Dr. Moon has been a consultant to Medtronic. Dr. Welt has been an adviser to Medtronic.
SOURCE: Gaudino MFL et al. ACC 20, Abstract 410-11.
Coronary bypass surgery patients who received a radial artery as their second bypass conduit had significantly better 10-year survival than did patients who received a saphenous vein graft in a combined analysis of more than 1,000 randomized patients who had originally been enrolled in any of five independent studies.
“This is the first report of a survival benefit for CABG [coronary artery bypass grafting] using multiple arterial conduits based on randomized data,” Mario F.L. Gaudino, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
Dr. Gaudino acknowledged several limitations of the finding. First, the analysis included studies that enrolled patients during 1997-2009 in five diverse sites worldwide and, therefore, involved varying surgical methods. Second, the sample size was “relatively low and underpowered, even after 10-year follow-up.” And third, the survival analysis was post hoc, although the statistically significant 27% relative reduction in mortality during follow-up with radial artery bypass, compared with saphenous vein bypass, was fully consistent with both the primary endpoint of the five studies and also with the combined hard endpoint of death and myocardial infarction.
The primary outcome of all-cause death, MI, and repeat revascularization also fell by a relative 27% with radial artery bypass, compared with saphenous vein bypass, and the combined rate of death and MI fell by 23% with radial artery bypass, both statistically significant differences, reported Dr. Gaudino, professor of cardiothoracic surgery at Weill Cornell Medicine, New York.
“The overall message is that radial bypass is associated with better long-term outcomes and potentially better survival,” he concluded.
The left interior thoracic artery (also known as the left internal mammary artery) is well established as the primary CABG conduit, usually used for bypassing the left anterior descending coronary artery, but when a second conduit is needed, several options exist: a saphenous vein, the left radial artery, or possibly the right internal thoracic artery (RITA) as a different arterial option.
Dr. Gaudino claimed that his new results placed the left radial artery clearly superior to the RITA as the second arterial conduit of choice for CABG. Not only does the RITA lack a similar efficacy evidence base from randomized trials, but the method poses a higher risk for surgical wound infections, he noted. The most recent society recommendations on conduit choice for CABG, issued less than 2 years ago by the European Society of Cardiology and European Association for Cardio-Thoracic Surgery, tapped the left radial artery as a level I recommendation over a saphenous vein graft when patients have high-grade coronary stenosis, while the RITA trailed as a level IIa recommendation specified only for patients with a low risk for sternal-wound infection.
“This was a great study that brings home the point that, in general, the radial artery is better than a saphenous vein graft,” commented Marc R. Moon, MD, a designated discussant and a professor of surgery and chief of cardiac surgery at Washington University, St. Louis.
The long-term follow-up that Dr. Gaudino reported came from extended, patient-level data collection for all 1,036 patients included in the original RADIAL (Radial Artery Database International Alliance) analysis of 5-year outcomes and reported in 2018. Dr. Gaudino and his associates tracked down survival information for all those patients, with outcome records out to at least 10 years for 91% of the original participants and with a mean follow-up that was also 10 years. The prior 2018 report based on 5-year results had also shown a statistically significant reduction in the primary endpoint with radial artery grafting, but at that point, follow-up had not yet collected enough mortality endpoints to produce a statistically significant between-group difference in death from any cause, a shortcoming that may have limited the ability of the prior report to influence U.S. practice.
“In the United States, there has been very little uptake of multiarterial grafting,” commented Frederick G.P. Welt, MD, a designated discussant, interventional cardiologist, professor of medicine, and associate chief of cardiovascular medicine at the University of Utah, Salt Lake City. The results from several earlier studies did not show much benefit for graft patency using radial arteries, but more recently clinicians have made advances in radial artery harvesting methods, implantation techniques, and adjunctive medications including antispasmodic treatments, Dr. Welt noted. Improved methods for using radial artery grafts and the risk of wound infection with RITA grafts were summarized in an editorial that accompanied the report of the 5-year RADIAL findings.
Dr. Welt said that, among the new findings reported by Dr. Gaudino, “the mortality effect is the most impressive.” Despite the limitations of the post hoc survival analysis, the reduced mortality finding is “nevertheless really important. The patient-level data lend it more credence.”
The study received no commercial funding. Dr. Gaudino had no disclosures. Dr. Moon has been a consultant to Medtronic. Dr. Welt has been an adviser to Medtronic.
SOURCE: Gaudino MFL et al. ACC 20, Abstract 410-11.
FROM ACC 2020
VOYAGER PAD: Clopidogrel adds no benefit to rivaroxaban plus aspirin after PAD interventions
The VOYAGER PAD results from more than 6,500 patients created the biggest evidence base by far ever collected from patients with symptomatic peripheral artery disease (PAD) who underwent a vascular intervention, and showed that the combination of twice-daily rivaroxaban and once-daily aspirin was safe and more effective than aspirin alone for reducing future thrombotic and ischemic events.
Following that report on March 28, a prespecified subgroup analysis presented the next day showed that adding clopidogrel to this two-drug combination produced no added efficacy but caused additional bleeding episodes, suggesting that the common practice of using clopidogrel plus aspirin in these patients, especially those who receive a stent in a peripheral artery, should either fall by the wayside or be used very briefly.
“In the absence of clear benefit, clopidogrel exposure along with aspirin and rivaroxaban should be minimized or avoided to reduce this risk,” William R. Hiatt, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic. But he also cautioned that “we did not control for clopidogrel use, and so the patients who received clopidogrel look different [from patients who did not receive clopidogrel]. We must be cautious in interpreting differences between patients on or off clopidogrel,” warned Dr. Hiatt, a lead investigator for VOYAGER PAD, professor for cardiovascular research at the University of Colorado at Denver in Aurora and president of the affiliated Colorado Prevention Center.
In addition to this substantial caveat, the finding that clopidogrel appeared to add no extra benefit to the rivaroxaban/aspirin regimen “contradicts some dogmas that have been in the field for decades,” Dr. Hiatt said. Use of dual-antiplatelet therapy (DAPT), in this setting usually aspirin and clopidogrel, in patients who have just undergone lower-extremity revascularization is “current dogma,” even though it is not based on any direct evidence for efficacy, but instead came on the scene as “an extrapolation from the coronary artery literature, where it does have some benefit, particularly after percutaneous coronary intervention,” he explained.
The only reported study results to examine use of DAPT in patients who underwent peripheral artery revascularization focused entirely on patients who had a surgical procedure and showed no added benefit from DAPT over aspirin only in a multicenter, randomized trial with 851 patients (J Vasc Surg. 2010 Oct;52[4]:825-33), Dr. Hiatt noted. In VOYAGER PAD, two-thirds of all patients underwent an endovascular, not surgical, peripheral intervention, and among those treated with clopidogrel, 91% had endovascular treatment.
“We’re not saying don’t use DAPT, but patients on three drugs are at higher bleeding risk than patients on two drugs. I think our data also suggest starting rivaroxaban immediately after a procedure [as was done in VOYAGER PAD], and not waiting to complete a course of DAPT,” Dr. Hiatt said.
Other experts embraced Dr. Hiatt’s take on these findings, while warning that it may take some time for the message to penetrate into practice.
The overall VOYAGER PAD results “are practice changing for vascular interventions; it was by an order of magnitude the largest vascular intervention trial ever conducted,” commented Sahil A. Parikh, MD, a designated discussant, interventional cardiologist, and director of endovascular services at New York–Presbyterian Medical Center. “The data suggest that the value of clopidogrel is questionable, but the added hazard is not questionable” when given to patients on top of rivaroxaban and aspirin. The results “certainly beg the question of whether one should use DAPT at all, and if so, for how long.”
Use of DAPT in patients undergoing peripheral revascularization, especially patients receiving a stent, has been “dogma,” Dr. Parikh agreed. “It’s been pounded into our heads that DAPT is standard care, so it will take some time to penetrate into the practicing community.”
“Could there be patients who could benefit from triple therapy? That’s possible, but it needs testing,” commented Mark A. Creager, MD, professor of medicine and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center in Lebanon, N.H. “We’ve made terrific strides with the results from VOYAGER PAD,” and from the earlier COMPASS trial, which proved the benefit of rivaroxaban and aspirin in patients with stable atherosclerotic vascular disease including many PAD patients (N Engl J Med. 2017 Oct 5;377[14]:1319-30). Use of rivaroxaban and aspirin in PAD patients based on the COMPASS results “is beginning to make an impact, but has a long way to go,” Dr. Creager said in an interview.
In late 2018, the Food and Drug Administration gave rivaroxaban a revised labeling that included an indication for patients with PAD based on the COMPASS findings. The VOYAGER PAD and COMPASS trials are especially noteworthy because “they opened a whole area [of study] in patients with peripheral vascular disease, ” he added.
The prespecified analysis that Dr. Hiatt reported analyzed outcomes among the 51% of patients enrolled in VOYAGER PAD (Vascular Outcomes Study of Acetylsalicylic Acid Along With Rivaroxaban in Endovascular or Surgical Limb Revascularization for Peripheral Artery Disease) who received clopidogrel during follow-up at the discretion of their treating physician and the outcomes among the remainder who did not. The two subgroups showed several statistically significant differences in the prevalence of various comorbidities and in some baseline demographic and clinical metrics, and the analyses that Dr. Hiatt reported did not attempt to correct for these differences. Patients who received clopidogrel had the drug on board for a median of 29 days, and about 58% received it for 30 days or less.
The main finding of his analysis was that “adding clopidogrel did not modify benefit at all” from the perspective of the primary endpoint of VOYAGER PAD, the incidence of a five-item list of adverse events (acute limb ischemia, major amputation for vascular cause, myocardial infarction, ischemic stroke, and cardiovascular death) during a median follow-up of 28 months (N Engl J Med. 2020 Mar 28. doi: 10.1056/NEJMoa2000052), said Dr. Hiatt. Among patients on clopidogrel, those treated with both rivaroxaban and aspirin had a 16.0% incidence of the primary endpoint, compared with an 18.3% rate among patients on aspirin only, for a 15% relative risk reduction, identical to the study’s primary result. Among patients not on clopidogrel, the primary endpoint occurred in 18.7% of patients on rivaroxaban plus aspirin and in 21.5% of those on aspirin only, a 14% relative risk reduction. The analyses also showed that adding clopidogrel appeared to increase the rate of bleeding episodes, particularly the incidence of major bleeds by the criteria of the International Society on Thrombosis and Haemostasis (ISTH), which rose among patients on aspirin alone from 3.3% without clopidogrel treatment to 4.9% with clopidogrel, and in patients on rivaroxaban plus aspirin these major bleeds increased from 5.4% with no clopidogrel to 6.5% with clopidogrel.
An especially revealing further analysis showed that, among those who also received rivaroxaban and aspirin, clopidogrel treatment for more than 30 days led to substantially more bleeding problems, compared with patients who received the drug for 30 days or less. Patients who received clopidogrel for more than 30 days as part of a triple-drug regimen had a 3.0% rate of major ISTH bleeds during 180 days of follow-up, compared with a 0.9% rate for patients in the aspirin-alone group who also received clopidogrel, a 2.1% between-group difference. In contrast, the difference in major ISTH bleeds between the two treatment arms in the subgroup who received clopidogrel for 30 days or less was 0.7%.
“What’s inarguable is that the course of clopidogrel should be as short as possible, probably not more than 30 days unless there is a real extenuating rationale,” commented designated discussant Gregory Piazza, MD, a cardiologist at Brigham and Women’s Hospital in Boston.
VOYAGER PAD was sponsored by Bayer and Janssen, the companies that market rivaroxaban (Xarelto). The institution that Dr. Hiatt leads has received research funding from Bayer and Janssen and from Amgen. Dr. Parikh has been a consultant to Terumo; has received research funding from Shockwave, Surmodics, and Trireme; has worked on trial monitoring for Boston Scientific and Silk Road; and has had other financial relationships with Abbott, Boston Scientific, and Medtronic. Dr. Creager had no disclosures. Dr. Piazza has received research grants from Bayer and Janssen, as well as Bristol-Myers Squibb, Diiachi, EKOS, and Portola, and he has been a consultant to Optum, Pfizer, and Thrombolex.
SOURCE: Hiatt WR et al. ACC 20, Abstract 406-13.
The VOYAGER PAD results from more than 6,500 patients created the biggest evidence base by far ever collected from patients with symptomatic peripheral artery disease (PAD) who underwent a vascular intervention, and showed that the combination of twice-daily rivaroxaban and once-daily aspirin was safe and more effective than aspirin alone for reducing future thrombotic and ischemic events.
Following that report on March 28, a prespecified subgroup analysis presented the next day showed that adding clopidogrel to this two-drug combination produced no added efficacy but caused additional bleeding episodes, suggesting that the common practice of using clopidogrel plus aspirin in these patients, especially those who receive a stent in a peripheral artery, should either fall by the wayside or be used very briefly.
“In the absence of clear benefit, clopidogrel exposure along with aspirin and rivaroxaban should be minimized or avoided to reduce this risk,” William R. Hiatt, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic. But he also cautioned that “we did not control for clopidogrel use, and so the patients who received clopidogrel look different [from patients who did not receive clopidogrel]. We must be cautious in interpreting differences between patients on or off clopidogrel,” warned Dr. Hiatt, a lead investigator for VOYAGER PAD, professor for cardiovascular research at the University of Colorado at Denver in Aurora and president of the affiliated Colorado Prevention Center.
In addition to this substantial caveat, the finding that clopidogrel appeared to add no extra benefit to the rivaroxaban/aspirin regimen “contradicts some dogmas that have been in the field for decades,” Dr. Hiatt said. Use of dual-antiplatelet therapy (DAPT), in this setting usually aspirin and clopidogrel, in patients who have just undergone lower-extremity revascularization is “current dogma,” even though it is not based on any direct evidence for efficacy, but instead came on the scene as “an extrapolation from the coronary artery literature, where it does have some benefit, particularly after percutaneous coronary intervention,” he explained.
The only reported study results to examine use of DAPT in patients who underwent peripheral artery revascularization focused entirely on patients who had a surgical procedure and showed no added benefit from DAPT over aspirin only in a multicenter, randomized trial with 851 patients (J Vasc Surg. 2010 Oct;52[4]:825-33), Dr. Hiatt noted. In VOYAGER PAD, two-thirds of all patients underwent an endovascular, not surgical, peripheral intervention, and among those treated with clopidogrel, 91% had endovascular treatment.
“We’re not saying don’t use DAPT, but patients on three drugs are at higher bleeding risk than patients on two drugs. I think our data also suggest starting rivaroxaban immediately after a procedure [as was done in VOYAGER PAD], and not waiting to complete a course of DAPT,” Dr. Hiatt said.
Other experts embraced Dr. Hiatt’s take on these findings, while warning that it may take some time for the message to penetrate into practice.
The overall VOYAGER PAD results “are practice changing for vascular interventions; it was by an order of magnitude the largest vascular intervention trial ever conducted,” commented Sahil A. Parikh, MD, a designated discussant, interventional cardiologist, and director of endovascular services at New York–Presbyterian Medical Center. “The data suggest that the value of clopidogrel is questionable, but the added hazard is not questionable” when given to patients on top of rivaroxaban and aspirin. The results “certainly beg the question of whether one should use DAPT at all, and if so, for how long.”
Use of DAPT in patients undergoing peripheral revascularization, especially patients receiving a stent, has been “dogma,” Dr. Parikh agreed. “It’s been pounded into our heads that DAPT is standard care, so it will take some time to penetrate into the practicing community.”
“Could there be patients who could benefit from triple therapy? That’s possible, but it needs testing,” commented Mark A. Creager, MD, professor of medicine and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center in Lebanon, N.H. “We’ve made terrific strides with the results from VOYAGER PAD,” and from the earlier COMPASS trial, which proved the benefit of rivaroxaban and aspirin in patients with stable atherosclerotic vascular disease including many PAD patients (N Engl J Med. 2017 Oct 5;377[14]:1319-30). Use of rivaroxaban and aspirin in PAD patients based on the COMPASS results “is beginning to make an impact, but has a long way to go,” Dr. Creager said in an interview.
In late 2018, the Food and Drug Administration gave rivaroxaban a revised labeling that included an indication for patients with PAD based on the COMPASS findings. The VOYAGER PAD and COMPASS trials are especially noteworthy because “they opened a whole area [of study] in patients with peripheral vascular disease, ” he added.
The prespecified analysis that Dr. Hiatt reported analyzed outcomes among the 51% of patients enrolled in VOYAGER PAD (Vascular Outcomes Study of Acetylsalicylic Acid Along With Rivaroxaban in Endovascular or Surgical Limb Revascularization for Peripheral Artery Disease) who received clopidogrel during follow-up at the discretion of their treating physician and the outcomes among the remainder who did not. The two subgroups showed several statistically significant differences in the prevalence of various comorbidities and in some baseline demographic and clinical metrics, and the analyses that Dr. Hiatt reported did not attempt to correct for these differences. Patients who received clopidogrel had the drug on board for a median of 29 days, and about 58% received it for 30 days or less.
The main finding of his analysis was that “adding clopidogrel did not modify benefit at all” from the perspective of the primary endpoint of VOYAGER PAD, the incidence of a five-item list of adverse events (acute limb ischemia, major amputation for vascular cause, myocardial infarction, ischemic stroke, and cardiovascular death) during a median follow-up of 28 months (N Engl J Med. 2020 Mar 28. doi: 10.1056/NEJMoa2000052), said Dr. Hiatt. Among patients on clopidogrel, those treated with both rivaroxaban and aspirin had a 16.0% incidence of the primary endpoint, compared with an 18.3% rate among patients on aspirin only, for a 15% relative risk reduction, identical to the study’s primary result. Among patients not on clopidogrel, the primary endpoint occurred in 18.7% of patients on rivaroxaban plus aspirin and in 21.5% of those on aspirin only, a 14% relative risk reduction. The analyses also showed that adding clopidogrel appeared to increase the rate of bleeding episodes, particularly the incidence of major bleeds by the criteria of the International Society on Thrombosis and Haemostasis (ISTH), which rose among patients on aspirin alone from 3.3% without clopidogrel treatment to 4.9% with clopidogrel, and in patients on rivaroxaban plus aspirin these major bleeds increased from 5.4% with no clopidogrel to 6.5% with clopidogrel.
An especially revealing further analysis showed that, among those who also received rivaroxaban and aspirin, clopidogrel treatment for more than 30 days led to substantially more bleeding problems, compared with patients who received the drug for 30 days or less. Patients who received clopidogrel for more than 30 days as part of a triple-drug regimen had a 3.0% rate of major ISTH bleeds during 180 days of follow-up, compared with a 0.9% rate for patients in the aspirin-alone group who also received clopidogrel, a 2.1% between-group difference. In contrast, the difference in major ISTH bleeds between the two treatment arms in the subgroup who received clopidogrel for 30 days or less was 0.7%.
“What’s inarguable is that the course of clopidogrel should be as short as possible, probably not more than 30 days unless there is a real extenuating rationale,” commented designated discussant Gregory Piazza, MD, a cardiologist at Brigham and Women’s Hospital in Boston.
VOYAGER PAD was sponsored by Bayer and Janssen, the companies that market rivaroxaban (Xarelto). The institution that Dr. Hiatt leads has received research funding from Bayer and Janssen and from Amgen. Dr. Parikh has been a consultant to Terumo; has received research funding from Shockwave, Surmodics, and Trireme; has worked on trial monitoring for Boston Scientific and Silk Road; and has had other financial relationships with Abbott, Boston Scientific, and Medtronic. Dr. Creager had no disclosures. Dr. Piazza has received research grants from Bayer and Janssen, as well as Bristol-Myers Squibb, Diiachi, EKOS, and Portola, and he has been a consultant to Optum, Pfizer, and Thrombolex.
SOURCE: Hiatt WR et al. ACC 20, Abstract 406-13.
The VOYAGER PAD results from more than 6,500 patients created the biggest evidence base by far ever collected from patients with symptomatic peripheral artery disease (PAD) who underwent a vascular intervention, and showed that the combination of twice-daily rivaroxaban and once-daily aspirin was safe and more effective than aspirin alone for reducing future thrombotic and ischemic events.
Following that report on March 28, a prespecified subgroup analysis presented the next day showed that adding clopidogrel to this two-drug combination produced no added efficacy but caused additional bleeding episodes, suggesting that the common practice of using clopidogrel plus aspirin in these patients, especially those who receive a stent in a peripheral artery, should either fall by the wayside or be used very briefly.
“In the absence of clear benefit, clopidogrel exposure along with aspirin and rivaroxaban should be minimized or avoided to reduce this risk,” William R. Hiatt, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic. But he also cautioned that “we did not control for clopidogrel use, and so the patients who received clopidogrel look different [from patients who did not receive clopidogrel]. We must be cautious in interpreting differences between patients on or off clopidogrel,” warned Dr. Hiatt, a lead investigator for VOYAGER PAD, professor for cardiovascular research at the University of Colorado at Denver in Aurora and president of the affiliated Colorado Prevention Center.
In addition to this substantial caveat, the finding that clopidogrel appeared to add no extra benefit to the rivaroxaban/aspirin regimen “contradicts some dogmas that have been in the field for decades,” Dr. Hiatt said. Use of dual-antiplatelet therapy (DAPT), in this setting usually aspirin and clopidogrel, in patients who have just undergone lower-extremity revascularization is “current dogma,” even though it is not based on any direct evidence for efficacy, but instead came on the scene as “an extrapolation from the coronary artery literature, where it does have some benefit, particularly after percutaneous coronary intervention,” he explained.
The only reported study results to examine use of DAPT in patients who underwent peripheral artery revascularization focused entirely on patients who had a surgical procedure and showed no added benefit from DAPT over aspirin only in a multicenter, randomized trial with 851 patients (J Vasc Surg. 2010 Oct;52[4]:825-33), Dr. Hiatt noted. In VOYAGER PAD, two-thirds of all patients underwent an endovascular, not surgical, peripheral intervention, and among those treated with clopidogrel, 91% had endovascular treatment.
“We’re not saying don’t use DAPT, but patients on three drugs are at higher bleeding risk than patients on two drugs. I think our data also suggest starting rivaroxaban immediately after a procedure [as was done in VOYAGER PAD], and not waiting to complete a course of DAPT,” Dr. Hiatt said.
Other experts embraced Dr. Hiatt’s take on these findings, while warning that it may take some time for the message to penetrate into practice.
The overall VOYAGER PAD results “are practice changing for vascular interventions; it was by an order of magnitude the largest vascular intervention trial ever conducted,” commented Sahil A. Parikh, MD, a designated discussant, interventional cardiologist, and director of endovascular services at New York–Presbyterian Medical Center. “The data suggest that the value of clopidogrel is questionable, but the added hazard is not questionable” when given to patients on top of rivaroxaban and aspirin. The results “certainly beg the question of whether one should use DAPT at all, and if so, for how long.”
Use of DAPT in patients undergoing peripheral revascularization, especially patients receiving a stent, has been “dogma,” Dr. Parikh agreed. “It’s been pounded into our heads that DAPT is standard care, so it will take some time to penetrate into the practicing community.”
“Could there be patients who could benefit from triple therapy? That’s possible, but it needs testing,” commented Mark A. Creager, MD, professor of medicine and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center in Lebanon, N.H. “We’ve made terrific strides with the results from VOYAGER PAD,” and from the earlier COMPASS trial, which proved the benefit of rivaroxaban and aspirin in patients with stable atherosclerotic vascular disease including many PAD patients (N Engl J Med. 2017 Oct 5;377[14]:1319-30). Use of rivaroxaban and aspirin in PAD patients based on the COMPASS results “is beginning to make an impact, but has a long way to go,” Dr. Creager said in an interview.
In late 2018, the Food and Drug Administration gave rivaroxaban a revised labeling that included an indication for patients with PAD based on the COMPASS findings. The VOYAGER PAD and COMPASS trials are especially noteworthy because “they opened a whole area [of study] in patients with peripheral vascular disease, ” he added.
The prespecified analysis that Dr. Hiatt reported analyzed outcomes among the 51% of patients enrolled in VOYAGER PAD (Vascular Outcomes Study of Acetylsalicylic Acid Along With Rivaroxaban in Endovascular or Surgical Limb Revascularization for Peripheral Artery Disease) who received clopidogrel during follow-up at the discretion of their treating physician and the outcomes among the remainder who did not. The two subgroups showed several statistically significant differences in the prevalence of various comorbidities and in some baseline demographic and clinical metrics, and the analyses that Dr. Hiatt reported did not attempt to correct for these differences. Patients who received clopidogrel had the drug on board for a median of 29 days, and about 58% received it for 30 days or less.
The main finding of his analysis was that “adding clopidogrel did not modify benefit at all” from the perspective of the primary endpoint of VOYAGER PAD, the incidence of a five-item list of adverse events (acute limb ischemia, major amputation for vascular cause, myocardial infarction, ischemic stroke, and cardiovascular death) during a median follow-up of 28 months (N Engl J Med. 2020 Mar 28. doi: 10.1056/NEJMoa2000052), said Dr. Hiatt. Among patients on clopidogrel, those treated with both rivaroxaban and aspirin had a 16.0% incidence of the primary endpoint, compared with an 18.3% rate among patients on aspirin only, for a 15% relative risk reduction, identical to the study’s primary result. Among patients not on clopidogrel, the primary endpoint occurred in 18.7% of patients on rivaroxaban plus aspirin and in 21.5% of those on aspirin only, a 14% relative risk reduction. The analyses also showed that adding clopidogrel appeared to increase the rate of bleeding episodes, particularly the incidence of major bleeds by the criteria of the International Society on Thrombosis and Haemostasis (ISTH), which rose among patients on aspirin alone from 3.3% without clopidogrel treatment to 4.9% with clopidogrel, and in patients on rivaroxaban plus aspirin these major bleeds increased from 5.4% with no clopidogrel to 6.5% with clopidogrel.
An especially revealing further analysis showed that, among those who also received rivaroxaban and aspirin, clopidogrel treatment for more than 30 days led to substantially more bleeding problems, compared with patients who received the drug for 30 days or less. Patients who received clopidogrel for more than 30 days as part of a triple-drug regimen had a 3.0% rate of major ISTH bleeds during 180 days of follow-up, compared with a 0.9% rate for patients in the aspirin-alone group who also received clopidogrel, a 2.1% between-group difference. In contrast, the difference in major ISTH bleeds between the two treatment arms in the subgroup who received clopidogrel for 30 days or less was 0.7%.
“What’s inarguable is that the course of clopidogrel should be as short as possible, probably not more than 30 days unless there is a real extenuating rationale,” commented designated discussant Gregory Piazza, MD, a cardiologist at Brigham and Women’s Hospital in Boston.
VOYAGER PAD was sponsored by Bayer and Janssen, the companies that market rivaroxaban (Xarelto). The institution that Dr. Hiatt leads has received research funding from Bayer and Janssen and from Amgen. Dr. Parikh has been a consultant to Terumo; has received research funding from Shockwave, Surmodics, and Trireme; has worked on trial monitoring for Boston Scientific and Silk Road; and has had other financial relationships with Abbott, Boston Scientific, and Medtronic. Dr. Creager had no disclosures. Dr. Piazza has received research grants from Bayer and Janssen, as well as Bristol-Myers Squibb, Diiachi, EKOS, and Portola, and he has been a consultant to Optum, Pfizer, and Thrombolex.
SOURCE: Hiatt WR et al. ACC 20, Abstract 406-13.
FROM ACC 2020