User login
Hormone therapy less effective in menopausal women with obesity
PHILADELPHIA – , according to a small, retrospective study presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
More than 40% of women over age 40 in the United States have obesity, presenter Anita Pershad, MD, an ob.gyn. medical resident at Eastern Virginia Medical School, Norfolk, told attendees. Yet most of the large-scale studies investigating perimenopausal and postmenopausal hormone therapy included participants without major medical comorbidities, so little data exist on how effectively HT works in women with these comorbidities, she said
“The main takeaway of our study is that obesity may worsen a woman’s menopausal symptoms and limit the amount of relief she gets from hormone therapy,” Dr. Pershad said in an interview. “It remains unclear if hormone therapy is less effective in women with obesity overall, or if the expected efficacy can be achieved with alternative design and administration routes. A potential mechanism of action for the observed decreased effect could be due to adipose tissue acting as a heat insulator, promoting the effects of vasomotor symptoms.”
Dr. Pershad and her colleagues conducted a retrospective review of the medical records of 119 patients who presented to a menopause clinic at a Midsouth urban academic medical center between July 2018 and December 2022. Obesity was defined as having a body mass index (BMI) of 30 kg/m2 or greater.
The patients with and without obesity were similar in terms of age, duration of menopause, use of hormone therapy, and therapy acceptance, but patients with obesity were more likely to identify themselves as Black (71% vs. 40%). Women with obesity were also significantly more likely than women without obesity to report vasomotor symptoms (74% vs. 45%, P = .002), genitourinary/vulvovaginal symptoms (60% vs. 21%, P < .001), mood disturbances (11% vs. 0%, P = .18), and decreased libido (29% vs. 11%, P = .017).
There were no significant differences in comorbidities between women with and without obesity, and among women who received systemic or localized HT, the same standard dosing was used for both groups.
Women with obesity were much less likely to see a satisfying reduction in their menopausal symptoms than women without obesity (odds ratio 0.07, 95% confidence interval, 0.01-0.64; P = .006), though the subgroups for each category of HT were small. Among the 20 women receiving systemic hormone therapy, only 1 of the 12 with obesity (8.3%) reported improvement in symptoms, compared with 7 of the 8 women without obesity (88%; P = .0004). Among 33 women using localized hormone therapy, 46% of the 24 women with obesity vs. 89% of the 9 women without obesity experienced symptom improvement (P = .026).
The proportions of women reporting relief from only lifestyle modifications or from nonhormonal medications, such as SSRIs/SNRIs, trazodone, and clonidine, were not statistically different. There were 33 women who relied only on lifestyle modifications, with 31% of the 16 women with obesity and 59% of the 17 women without obesity reporting improvement in their symptoms (P = .112). Similarly, among the 33 women using nonhormonal medications, 75% of the 20 women with obesity and 77% of the 13 women without obesity experienced relief (P = .9).
Women with obesity are undertreated
Dr. Pershad emphasized the need to improve care and counseling for diverse patients seeking treatment for menopausal symptoms.
“More research is needed to examine how women with medical comorbidities are uniquely impacted by menopause and respond to therapies,” Dr. Pershad said in an interview. “This can be achieved by actively including more diverse patient populations in women’s health studies, burdened by the social determinants of health and medical comorbidities such as obesity.”
Stephanie S. Faubion, MD, MBA, director for Mayo Clinic’s Center for Women’s Health, Rochester, Minn., and medical director for The Menopause Society, was not surprised by the findings, particularly given that women with obesity tend to have more hot flashes and night sweats as a result of their extra weight. However, dosage data was not adjusted for BMI in the study and data on hormone levels was unavailable, she said, so it’s difficult to determine from the data whether HT was less effective for women with obesity or whether they were underdosed.
“I think women with obesity are undertreated,” Dr. Faubion said in an interview. “My guess is people are afraid. Women with obesity also may have other comorbidities,” such as hypertension and diabetes, she said, and “the greater the number of cardiovascular risk factors, the higher risk hormone therapy is.” Providers may therefore be leery of prescribing HT or prescribing it at an appropriately high enough dose to treat menopausal symptoms.
Common practice is to start patients at the lowest dose and titrate up according to symptoms, but “if people are afraid of it, they’re going to start the lowest dose” and may not increase it, Dr. Faubion said. She noted that other nonhormonal options are available, though providers should be conscientious about selecting ones whose adverse events do not include weight gain.
Although the study focused on an understudied population within hormone therapy research, the study was limited by its small size, low overall use of hormone therapy, recall bias, and the researchers’ inability to control for other medications the participants may have been taking.
Dr. Pershad said she is continuing research to try to identify the mechanisms underlying the reduced efficacy in women with obesity.
The research did not use any external funding. Dr. Pershad had no industry disclosures, but her colleagues reported honoraria from or speaking for TherapeuticsMD, Astella Pharma, Scynexis, Pharmavite, and Pfizer. Dr. Faubion had no disclosures.
PHILADELPHIA – , according to a small, retrospective study presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
More than 40% of women over age 40 in the United States have obesity, presenter Anita Pershad, MD, an ob.gyn. medical resident at Eastern Virginia Medical School, Norfolk, told attendees. Yet most of the large-scale studies investigating perimenopausal and postmenopausal hormone therapy included participants without major medical comorbidities, so little data exist on how effectively HT works in women with these comorbidities, she said
“The main takeaway of our study is that obesity may worsen a woman’s menopausal symptoms and limit the amount of relief she gets from hormone therapy,” Dr. Pershad said in an interview. “It remains unclear if hormone therapy is less effective in women with obesity overall, or if the expected efficacy can be achieved with alternative design and administration routes. A potential mechanism of action for the observed decreased effect could be due to adipose tissue acting as a heat insulator, promoting the effects of vasomotor symptoms.”
Dr. Pershad and her colleagues conducted a retrospective review of the medical records of 119 patients who presented to a menopause clinic at a Midsouth urban academic medical center between July 2018 and December 2022. Obesity was defined as having a body mass index (BMI) of 30 kg/m2 or greater.
The patients with and without obesity were similar in terms of age, duration of menopause, use of hormone therapy, and therapy acceptance, but patients with obesity were more likely to identify themselves as Black (71% vs. 40%). Women with obesity were also significantly more likely than women without obesity to report vasomotor symptoms (74% vs. 45%, P = .002), genitourinary/vulvovaginal symptoms (60% vs. 21%, P < .001), mood disturbances (11% vs. 0%, P = .18), and decreased libido (29% vs. 11%, P = .017).
There were no significant differences in comorbidities between women with and without obesity, and among women who received systemic or localized HT, the same standard dosing was used for both groups.
Women with obesity were much less likely to see a satisfying reduction in their menopausal symptoms than women without obesity (odds ratio 0.07, 95% confidence interval, 0.01-0.64; P = .006), though the subgroups for each category of HT were small. Among the 20 women receiving systemic hormone therapy, only 1 of the 12 with obesity (8.3%) reported improvement in symptoms, compared with 7 of the 8 women without obesity (88%; P = .0004). Among 33 women using localized hormone therapy, 46% of the 24 women with obesity vs. 89% of the 9 women without obesity experienced symptom improvement (P = .026).
The proportions of women reporting relief from only lifestyle modifications or from nonhormonal medications, such as SSRIs/SNRIs, trazodone, and clonidine, were not statistically different. There were 33 women who relied only on lifestyle modifications, with 31% of the 16 women with obesity and 59% of the 17 women without obesity reporting improvement in their symptoms (P = .112). Similarly, among the 33 women using nonhormonal medications, 75% of the 20 women with obesity and 77% of the 13 women without obesity experienced relief (P = .9).
Women with obesity are undertreated
Dr. Pershad emphasized the need to improve care and counseling for diverse patients seeking treatment for menopausal symptoms.
“More research is needed to examine how women with medical comorbidities are uniquely impacted by menopause and respond to therapies,” Dr. Pershad said in an interview. “This can be achieved by actively including more diverse patient populations in women’s health studies, burdened by the social determinants of health and medical comorbidities such as obesity.”
Stephanie S. Faubion, MD, MBA, director for Mayo Clinic’s Center for Women’s Health, Rochester, Minn., and medical director for The Menopause Society, was not surprised by the findings, particularly given that women with obesity tend to have more hot flashes and night sweats as a result of their extra weight. However, dosage data was not adjusted for BMI in the study and data on hormone levels was unavailable, she said, so it’s difficult to determine from the data whether HT was less effective for women with obesity or whether they were underdosed.
“I think women with obesity are undertreated,” Dr. Faubion said in an interview. “My guess is people are afraid. Women with obesity also may have other comorbidities,” such as hypertension and diabetes, she said, and “the greater the number of cardiovascular risk factors, the higher risk hormone therapy is.” Providers may therefore be leery of prescribing HT or prescribing it at an appropriately high enough dose to treat menopausal symptoms.
Common practice is to start patients at the lowest dose and titrate up according to symptoms, but “if people are afraid of it, they’re going to start the lowest dose” and may not increase it, Dr. Faubion said. She noted that other nonhormonal options are available, though providers should be conscientious about selecting ones whose adverse events do not include weight gain.
Although the study focused on an understudied population within hormone therapy research, the study was limited by its small size, low overall use of hormone therapy, recall bias, and the researchers’ inability to control for other medications the participants may have been taking.
Dr. Pershad said she is continuing research to try to identify the mechanisms underlying the reduced efficacy in women with obesity.
The research did not use any external funding. Dr. Pershad had no industry disclosures, but her colleagues reported honoraria from or speaking for TherapeuticsMD, Astella Pharma, Scynexis, Pharmavite, and Pfizer. Dr. Faubion had no disclosures.
PHILADELPHIA – , according to a small, retrospective study presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
More than 40% of women over age 40 in the United States have obesity, presenter Anita Pershad, MD, an ob.gyn. medical resident at Eastern Virginia Medical School, Norfolk, told attendees. Yet most of the large-scale studies investigating perimenopausal and postmenopausal hormone therapy included participants without major medical comorbidities, so little data exist on how effectively HT works in women with these comorbidities, she said
“The main takeaway of our study is that obesity may worsen a woman’s menopausal symptoms and limit the amount of relief she gets from hormone therapy,” Dr. Pershad said in an interview. “It remains unclear if hormone therapy is less effective in women with obesity overall, or if the expected efficacy can be achieved with alternative design and administration routes. A potential mechanism of action for the observed decreased effect could be due to adipose tissue acting as a heat insulator, promoting the effects of vasomotor symptoms.”
Dr. Pershad and her colleagues conducted a retrospective review of the medical records of 119 patients who presented to a menopause clinic at a Midsouth urban academic medical center between July 2018 and December 2022. Obesity was defined as having a body mass index (BMI) of 30 kg/m2 or greater.
The patients with and without obesity were similar in terms of age, duration of menopause, use of hormone therapy, and therapy acceptance, but patients with obesity were more likely to identify themselves as Black (71% vs. 40%). Women with obesity were also significantly more likely than women without obesity to report vasomotor symptoms (74% vs. 45%, P = .002), genitourinary/vulvovaginal symptoms (60% vs. 21%, P < .001), mood disturbances (11% vs. 0%, P = .18), and decreased libido (29% vs. 11%, P = .017).
There were no significant differences in comorbidities between women with and without obesity, and among women who received systemic or localized HT, the same standard dosing was used for both groups.
Women with obesity were much less likely to see a satisfying reduction in their menopausal symptoms than women without obesity (odds ratio 0.07, 95% confidence interval, 0.01-0.64; P = .006), though the subgroups for each category of HT were small. Among the 20 women receiving systemic hormone therapy, only 1 of the 12 with obesity (8.3%) reported improvement in symptoms, compared with 7 of the 8 women without obesity (88%; P = .0004). Among 33 women using localized hormone therapy, 46% of the 24 women with obesity vs. 89% of the 9 women without obesity experienced symptom improvement (P = .026).
The proportions of women reporting relief from only lifestyle modifications or from nonhormonal medications, such as SSRIs/SNRIs, trazodone, and clonidine, were not statistically different. There were 33 women who relied only on lifestyle modifications, with 31% of the 16 women with obesity and 59% of the 17 women without obesity reporting improvement in their symptoms (P = .112). Similarly, among the 33 women using nonhormonal medications, 75% of the 20 women with obesity and 77% of the 13 women without obesity experienced relief (P = .9).
Women with obesity are undertreated
Dr. Pershad emphasized the need to improve care and counseling for diverse patients seeking treatment for menopausal symptoms.
“More research is needed to examine how women with medical comorbidities are uniquely impacted by menopause and respond to therapies,” Dr. Pershad said in an interview. “This can be achieved by actively including more diverse patient populations in women’s health studies, burdened by the social determinants of health and medical comorbidities such as obesity.”
Stephanie S. Faubion, MD, MBA, director for Mayo Clinic’s Center for Women’s Health, Rochester, Minn., and medical director for The Menopause Society, was not surprised by the findings, particularly given that women with obesity tend to have more hot flashes and night sweats as a result of their extra weight. However, dosage data was not adjusted for BMI in the study and data on hormone levels was unavailable, she said, so it’s difficult to determine from the data whether HT was less effective for women with obesity or whether they were underdosed.
“I think women with obesity are undertreated,” Dr. Faubion said in an interview. “My guess is people are afraid. Women with obesity also may have other comorbidities,” such as hypertension and diabetes, she said, and “the greater the number of cardiovascular risk factors, the higher risk hormone therapy is.” Providers may therefore be leery of prescribing HT or prescribing it at an appropriately high enough dose to treat menopausal symptoms.
Common practice is to start patients at the lowest dose and titrate up according to symptoms, but “if people are afraid of it, they’re going to start the lowest dose” and may not increase it, Dr. Faubion said. She noted that other nonhormonal options are available, though providers should be conscientious about selecting ones whose adverse events do not include weight gain.
Although the study focused on an understudied population within hormone therapy research, the study was limited by its small size, low overall use of hormone therapy, recall bias, and the researchers’ inability to control for other medications the participants may have been taking.
Dr. Pershad said she is continuing research to try to identify the mechanisms underlying the reduced efficacy in women with obesity.
The research did not use any external funding. Dr. Pershad had no industry disclosures, but her colleagues reported honoraria from or speaking for TherapeuticsMD, Astella Pharma, Scynexis, Pharmavite, and Pfizer. Dr. Faubion had no disclosures.
AT THE MENOPAUSE SOCIETY ANNUAL MEETING
Hyaluronic acid suppository improves menopause symptoms
TOPLINE:
Among women with genitourinary syndrome of menopause, 12 weeks of treatment with vaginal suppositories containing hyaluronic acid (HLA) reduces vulvovaginal symptoms, according to trial results presented at the annual Menopause Meeting. HLA may be a promising nonhormonal therapy for this condition, the researchers said.
METHODOLOGY:
- Investigators randomly assigned 49 women to receive treatment with a vaginal suppository containing 5 mg of HLA or standard-of-care treatment with vaginal estrogen cream (0.01%).
- The trial was conducted between September 2021 and August 2022.
TAKEAWAY:
- Patients in both treatment arms experienced improvements on the Vulvovaginal Symptom Questionnaire (VSQ), the study’s primary outcome.
- The VSQ assesses vulvovaginal symptoms associated with menopause such as itching, burning, and dryness, as well as the emotional toll of symptoms and their effect on sexual activity.
- Change in VSQ score did not significantly differ between the treatment groups. The measure improved from 5.2 to 1.7 in the group that received estrogen, and from 5.8 to 2.5 in those who received HLA (P = .81).
- No treatment-related severe adverse events were reported.
IN PRACTICE:
“Women often need to decide between different therapies for genitourinary syndrome of menopause,” study author Benjamin Brucker, MD, of New York University said in an interview. “Now we can help counsel them about this formulation of HLA.”
SOURCE:
Poster P-1 was presented at the 2023 meeting of the Menopause Society, held Sept. 27-30 in Philadelphia.
DISCLOSURES:
The study was funded by Bonafide Health, a company that sells supplements to treat menopause symptoms, including vaginal suppositories containing HLA.
A version of this article appeared on Medscape.com.
TOPLINE:
Among women with genitourinary syndrome of menopause, 12 weeks of treatment with vaginal suppositories containing hyaluronic acid (HLA) reduces vulvovaginal symptoms, according to trial results presented at the annual Menopause Meeting. HLA may be a promising nonhormonal therapy for this condition, the researchers said.
METHODOLOGY:
- Investigators randomly assigned 49 women to receive treatment with a vaginal suppository containing 5 mg of HLA or standard-of-care treatment with vaginal estrogen cream (0.01%).
- The trial was conducted between September 2021 and August 2022.
TAKEAWAY:
- Patients in both treatment arms experienced improvements on the Vulvovaginal Symptom Questionnaire (VSQ), the study’s primary outcome.
- The VSQ assesses vulvovaginal symptoms associated with menopause such as itching, burning, and dryness, as well as the emotional toll of symptoms and their effect on sexual activity.
- Change in VSQ score did not significantly differ between the treatment groups. The measure improved from 5.2 to 1.7 in the group that received estrogen, and from 5.8 to 2.5 in those who received HLA (P = .81).
- No treatment-related severe adverse events were reported.
IN PRACTICE:
“Women often need to decide between different therapies for genitourinary syndrome of menopause,” study author Benjamin Brucker, MD, of New York University said in an interview. “Now we can help counsel them about this formulation of HLA.”
SOURCE:
Poster P-1 was presented at the 2023 meeting of the Menopause Society, held Sept. 27-30 in Philadelphia.
DISCLOSURES:
The study was funded by Bonafide Health, a company that sells supplements to treat menopause symptoms, including vaginal suppositories containing HLA.
A version of this article appeared on Medscape.com.
TOPLINE:
Among women with genitourinary syndrome of menopause, 12 weeks of treatment with vaginal suppositories containing hyaluronic acid (HLA) reduces vulvovaginal symptoms, according to trial results presented at the annual Menopause Meeting. HLA may be a promising nonhormonal therapy for this condition, the researchers said.
METHODOLOGY:
- Investigators randomly assigned 49 women to receive treatment with a vaginal suppository containing 5 mg of HLA or standard-of-care treatment with vaginal estrogen cream (0.01%).
- The trial was conducted between September 2021 and August 2022.
TAKEAWAY:
- Patients in both treatment arms experienced improvements on the Vulvovaginal Symptom Questionnaire (VSQ), the study’s primary outcome.
- The VSQ assesses vulvovaginal symptoms associated with menopause such as itching, burning, and dryness, as well as the emotional toll of symptoms and their effect on sexual activity.
- Change in VSQ score did not significantly differ between the treatment groups. The measure improved from 5.2 to 1.7 in the group that received estrogen, and from 5.8 to 2.5 in those who received HLA (P = .81).
- No treatment-related severe adverse events were reported.
IN PRACTICE:
“Women often need to decide between different therapies for genitourinary syndrome of menopause,” study author Benjamin Brucker, MD, of New York University said in an interview. “Now we can help counsel them about this formulation of HLA.”
SOURCE:
Poster P-1 was presented at the 2023 meeting of the Menopause Society, held Sept. 27-30 in Philadelphia.
DISCLOSURES:
The study was funded by Bonafide Health, a company that sells supplements to treat menopause symptoms, including vaginal suppositories containing HLA.
A version of this article appeared on Medscape.com.
Artificial sweeteners in processed foods tied to increased depression risk
new data from the Nurses Health Study II (NHS II) suggest.
Nurses who consumed more than eight servings daily had about a 50% higher risk of developing depression than nurses who consumed four or fewer servings daily.
However, in a secondary analysis, in which the researchers tried to tease out specific foods that may be associated with increased risk, only artificial sweeteners and artificially sweetened beverages were associated with an increased risk of depression.
“Animal studies have shown that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” study investigator Andrew T. Chan, MD, MPH, of the clinical and translational epidemiology unit at Massachusetts General Hospital, Boston, said in an interview.
“Given this potential association between ultraprocessed food and multiple adverse health conditions, wherever possible individuals may wish to limit their intake of such foods. This may be a lifestyle change that could have important benefits, particularly for those who struggle with mental health,” Dr. Chan said.
The study was published online in JAMA Network Open.
Multiple potential mechanisms
The findings are based on 31,712 mostly non-Hispanic White women who were free of depression at baseline. The mean age of the patients at baseline was 52 years. As part of the NHS II, the women provided information on diet every 4 years using validated food frequency questionnaires.
Compared with women with low UPF intake, those with high UPF intake had greater body mass index (BMI). In addition, they were apt to smoke and have diabetes, hypertension, and dyslipidemia, and they were less apt to exercise regularly.
During the study period, there were 2,122 incident cases of depression, as determined using a strict definition that required self-reported clinician-diagnosed depression and regular antidepressant use. There were 4,840 incident cases, as determined using a broad definition that required clinical diagnosis and/or antidepressant use.
Compared with women in the lowest quintile of UPF consumption (fewer than four daily servings), those in the highest quintile (more than 8.8 daily servings) had an increased risk of depression.
This was noted for both the strict depression definition (hazard ratio, 1.49; 95% confidence interval, 1.26-1.76; P < .001) and the broad one (HR, 1.34; 95% CI, 1.20-1.50; P < .001).
“Models were not materially altered after inclusion of potential confounders. We did not observe differential associations in subgroups defined by age, BMI, physical activity, or smoking,” the researchers reported.
In secondary analyses, they classified UPF into their components, including ultraprocessed grain foods, sweet snacks, ready-to-eat meals, fats, sauces, ultraprocessed dairy products, savory snacks, processed meat, beverages, and artificial sweeteners.
Comparing the highest with the lowest quintiles, only high intake of artificially sweetened beverages (HR, 1.37; 95% CI, 1.19-1.57; P < .001) and artificial sweeteners (HR, 1.26; 95% CI, 1.10-1.43; P < .001) was associated with greater risk of depression and after multivariable regression.
In an exploratory analysis, women who reduced their UPF intake by at least three servings per day were at lower risk of depression (strict definition: HR, 0.84; 95% CI, 0.71-0.99), compared with those with relatively stable intake in each 4-year period.
“Ultraprocessed foods have been associated with several different health outcomes which may reflect an effect on common pathways that underlie chronic conditions,” said Dr. Chan.
For example, UPF intake has been associated with chronic inflammation, which in turns leads to multiple potential adverse health effects, including depression, he explained.
There is also a link between UPF and disruption of the gut microbiome.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” Dr. Chan said.
Association, not causation
Several experts weighed in on the study results in a statement from the U.K. nonprofit organization, Science Media Centre.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading (England), cautioned that the study only offers information on association – not causation.
“It is very possible that people with depression change their diet and might decide to consume foods that are easier to prepare – which would often be foods considered to be ultraprocessed,” Dr. Kuhnle said.
What’s most interesting is that the association between UPF intake and depression was driven by a single factor – artificial sweeteners.
“This supports one of the main criticisms of the UPF concept, that it combines a wide range of different foods and thereby makes it difficult to identify underlying causes,” Dr. Kuhnle added.
“There are currently no data that link artificial sweetener use to mental health, despite most of them having been available for some time. It is also important to note that there are a wide range of different artificial sweeteners that are metabolized very differently and that there might be reverse causality,” Dr. Kuhnle commented.
Paul Keedwell, MBChB, PhD, consultant psychiatrist and fellow of the Royal College of Psychiatrists, said this is an “interesting and important finding, but one that raises more questions. At this stage, we cannot say how big an effect diet has on depression risk compared to other risk factors, like family history of depression, stress levels, and having a supportive social network.”
Dr. Keedwell noted that the investigators carefully excluded the possibility that the effect is mediated by obesity or lack of exercise.
“However, an important consideration is that a diet based on ready meals and artificially sweetened drinks might indicate a hectic lifestyle or one with shift work. In other words, a fast-food diet could be an indirect marker of chronic stress. Prolonged stress probably remains the main risk factor for depression,” Dr. Keedwell said.
Keith Frayn, PhD, professor emeritus of human metabolism, University of Oxford (England), noted that the relationship between artificial sweeteners and depression “stands out clearly” even after adjusting for multiple confounding factors, including BMI, smoking, and exercise.
“This adds to growing concerns about artificial sweeteners and cardiometabolic health. The link with depression needs confirmation and further research to suggest how it might be brought about,” Dr. Frayn cautioned.
The NHS II was funded by a grant from the National Cancer Institute. Dr. Chan reported receiving grants from Bayer and Zoe and personal fees from Boehringer Ingelheim, Pfizer, and Freenome outside this work. Dr. Keedwell and Dr. Kuhnle disclosed no relevant financial relationships. Dr. Frayn is an author of books on nutrition and metabolism.
A version of this article first appeared on Medscape.com.
new data from the Nurses Health Study II (NHS II) suggest.
Nurses who consumed more than eight servings daily had about a 50% higher risk of developing depression than nurses who consumed four or fewer servings daily.
However, in a secondary analysis, in which the researchers tried to tease out specific foods that may be associated with increased risk, only artificial sweeteners and artificially sweetened beverages were associated with an increased risk of depression.
“Animal studies have shown that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” study investigator Andrew T. Chan, MD, MPH, of the clinical and translational epidemiology unit at Massachusetts General Hospital, Boston, said in an interview.
“Given this potential association between ultraprocessed food and multiple adverse health conditions, wherever possible individuals may wish to limit their intake of such foods. This may be a lifestyle change that could have important benefits, particularly for those who struggle with mental health,” Dr. Chan said.
The study was published online in JAMA Network Open.
Multiple potential mechanisms
The findings are based on 31,712 mostly non-Hispanic White women who were free of depression at baseline. The mean age of the patients at baseline was 52 years. As part of the NHS II, the women provided information on diet every 4 years using validated food frequency questionnaires.
Compared with women with low UPF intake, those with high UPF intake had greater body mass index (BMI). In addition, they were apt to smoke and have diabetes, hypertension, and dyslipidemia, and they were less apt to exercise regularly.
During the study period, there were 2,122 incident cases of depression, as determined using a strict definition that required self-reported clinician-diagnosed depression and regular antidepressant use. There were 4,840 incident cases, as determined using a broad definition that required clinical diagnosis and/or antidepressant use.
Compared with women in the lowest quintile of UPF consumption (fewer than four daily servings), those in the highest quintile (more than 8.8 daily servings) had an increased risk of depression.
This was noted for both the strict depression definition (hazard ratio, 1.49; 95% confidence interval, 1.26-1.76; P < .001) and the broad one (HR, 1.34; 95% CI, 1.20-1.50; P < .001).
“Models were not materially altered after inclusion of potential confounders. We did not observe differential associations in subgroups defined by age, BMI, physical activity, or smoking,” the researchers reported.
In secondary analyses, they classified UPF into their components, including ultraprocessed grain foods, sweet snacks, ready-to-eat meals, fats, sauces, ultraprocessed dairy products, savory snacks, processed meat, beverages, and artificial sweeteners.
Comparing the highest with the lowest quintiles, only high intake of artificially sweetened beverages (HR, 1.37; 95% CI, 1.19-1.57; P < .001) and artificial sweeteners (HR, 1.26; 95% CI, 1.10-1.43; P < .001) was associated with greater risk of depression and after multivariable regression.
In an exploratory analysis, women who reduced their UPF intake by at least three servings per day were at lower risk of depression (strict definition: HR, 0.84; 95% CI, 0.71-0.99), compared with those with relatively stable intake in each 4-year period.
“Ultraprocessed foods have been associated with several different health outcomes which may reflect an effect on common pathways that underlie chronic conditions,” said Dr. Chan.
For example, UPF intake has been associated with chronic inflammation, which in turns leads to multiple potential adverse health effects, including depression, he explained.
There is also a link between UPF and disruption of the gut microbiome.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” Dr. Chan said.
Association, not causation
Several experts weighed in on the study results in a statement from the U.K. nonprofit organization, Science Media Centre.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading (England), cautioned that the study only offers information on association – not causation.
“It is very possible that people with depression change their diet and might decide to consume foods that are easier to prepare – which would often be foods considered to be ultraprocessed,” Dr. Kuhnle said.
What’s most interesting is that the association between UPF intake and depression was driven by a single factor – artificial sweeteners.
“This supports one of the main criticisms of the UPF concept, that it combines a wide range of different foods and thereby makes it difficult to identify underlying causes,” Dr. Kuhnle added.
“There are currently no data that link artificial sweetener use to mental health, despite most of them having been available for some time. It is also important to note that there are a wide range of different artificial sweeteners that are metabolized very differently and that there might be reverse causality,” Dr. Kuhnle commented.
Paul Keedwell, MBChB, PhD, consultant psychiatrist and fellow of the Royal College of Psychiatrists, said this is an “interesting and important finding, but one that raises more questions. At this stage, we cannot say how big an effect diet has on depression risk compared to other risk factors, like family history of depression, stress levels, and having a supportive social network.”
Dr. Keedwell noted that the investigators carefully excluded the possibility that the effect is mediated by obesity or lack of exercise.
“However, an important consideration is that a diet based on ready meals and artificially sweetened drinks might indicate a hectic lifestyle or one with shift work. In other words, a fast-food diet could be an indirect marker of chronic stress. Prolonged stress probably remains the main risk factor for depression,” Dr. Keedwell said.
Keith Frayn, PhD, professor emeritus of human metabolism, University of Oxford (England), noted that the relationship between artificial sweeteners and depression “stands out clearly” even after adjusting for multiple confounding factors, including BMI, smoking, and exercise.
“This adds to growing concerns about artificial sweeteners and cardiometabolic health. The link with depression needs confirmation and further research to suggest how it might be brought about,” Dr. Frayn cautioned.
The NHS II was funded by a grant from the National Cancer Institute. Dr. Chan reported receiving grants from Bayer and Zoe and personal fees from Boehringer Ingelheim, Pfizer, and Freenome outside this work. Dr. Keedwell and Dr. Kuhnle disclosed no relevant financial relationships. Dr. Frayn is an author of books on nutrition and metabolism.
A version of this article first appeared on Medscape.com.
new data from the Nurses Health Study II (NHS II) suggest.
Nurses who consumed more than eight servings daily had about a 50% higher risk of developing depression than nurses who consumed four or fewer servings daily.
However, in a secondary analysis, in which the researchers tried to tease out specific foods that may be associated with increased risk, only artificial sweeteners and artificially sweetened beverages were associated with an increased risk of depression.
“Animal studies have shown that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” study investigator Andrew T. Chan, MD, MPH, of the clinical and translational epidemiology unit at Massachusetts General Hospital, Boston, said in an interview.
“Given this potential association between ultraprocessed food and multiple adverse health conditions, wherever possible individuals may wish to limit their intake of such foods. This may be a lifestyle change that could have important benefits, particularly for those who struggle with mental health,” Dr. Chan said.
The study was published online in JAMA Network Open.
Multiple potential mechanisms
The findings are based on 31,712 mostly non-Hispanic White women who were free of depression at baseline. The mean age of the patients at baseline was 52 years. As part of the NHS II, the women provided information on diet every 4 years using validated food frequency questionnaires.
Compared with women with low UPF intake, those with high UPF intake had greater body mass index (BMI). In addition, they were apt to smoke and have diabetes, hypertension, and dyslipidemia, and they were less apt to exercise regularly.
During the study period, there were 2,122 incident cases of depression, as determined using a strict definition that required self-reported clinician-diagnosed depression and regular antidepressant use. There were 4,840 incident cases, as determined using a broad definition that required clinical diagnosis and/or antidepressant use.
Compared with women in the lowest quintile of UPF consumption (fewer than four daily servings), those in the highest quintile (more than 8.8 daily servings) had an increased risk of depression.
This was noted for both the strict depression definition (hazard ratio, 1.49; 95% confidence interval, 1.26-1.76; P < .001) and the broad one (HR, 1.34; 95% CI, 1.20-1.50; P < .001).
“Models were not materially altered after inclusion of potential confounders. We did not observe differential associations in subgroups defined by age, BMI, physical activity, or smoking,” the researchers reported.
In secondary analyses, they classified UPF into their components, including ultraprocessed grain foods, sweet snacks, ready-to-eat meals, fats, sauces, ultraprocessed dairy products, savory snacks, processed meat, beverages, and artificial sweeteners.
Comparing the highest with the lowest quintiles, only high intake of artificially sweetened beverages (HR, 1.37; 95% CI, 1.19-1.57; P < .001) and artificial sweeteners (HR, 1.26; 95% CI, 1.10-1.43; P < .001) was associated with greater risk of depression and after multivariable regression.
In an exploratory analysis, women who reduced their UPF intake by at least three servings per day were at lower risk of depression (strict definition: HR, 0.84; 95% CI, 0.71-0.99), compared with those with relatively stable intake in each 4-year period.
“Ultraprocessed foods have been associated with several different health outcomes which may reflect an effect on common pathways that underlie chronic conditions,” said Dr. Chan.
For example, UPF intake has been associated with chronic inflammation, which in turns leads to multiple potential adverse health effects, including depression, he explained.
There is also a link between UPF and disruption of the gut microbiome.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” Dr. Chan said.
Association, not causation
Several experts weighed in on the study results in a statement from the U.K. nonprofit organization, Science Media Centre.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading (England), cautioned that the study only offers information on association – not causation.
“It is very possible that people with depression change their diet and might decide to consume foods that are easier to prepare – which would often be foods considered to be ultraprocessed,” Dr. Kuhnle said.
What’s most interesting is that the association between UPF intake and depression was driven by a single factor – artificial sweeteners.
“This supports one of the main criticisms of the UPF concept, that it combines a wide range of different foods and thereby makes it difficult to identify underlying causes,” Dr. Kuhnle added.
“There are currently no data that link artificial sweetener use to mental health, despite most of them having been available for some time. It is also important to note that there are a wide range of different artificial sweeteners that are metabolized very differently and that there might be reverse causality,” Dr. Kuhnle commented.
Paul Keedwell, MBChB, PhD, consultant psychiatrist and fellow of the Royal College of Psychiatrists, said this is an “interesting and important finding, but one that raises more questions. At this stage, we cannot say how big an effect diet has on depression risk compared to other risk factors, like family history of depression, stress levels, and having a supportive social network.”
Dr. Keedwell noted that the investigators carefully excluded the possibility that the effect is mediated by obesity or lack of exercise.
“However, an important consideration is that a diet based on ready meals and artificially sweetened drinks might indicate a hectic lifestyle or one with shift work. In other words, a fast-food diet could be an indirect marker of chronic stress. Prolonged stress probably remains the main risk factor for depression,” Dr. Keedwell said.
Keith Frayn, PhD, professor emeritus of human metabolism, University of Oxford (England), noted that the relationship between artificial sweeteners and depression “stands out clearly” even after adjusting for multiple confounding factors, including BMI, smoking, and exercise.
“This adds to growing concerns about artificial sweeteners and cardiometabolic health. The link with depression needs confirmation and further research to suggest how it might be brought about,” Dr. Frayn cautioned.
The NHS II was funded by a grant from the National Cancer Institute. Dr. Chan reported receiving grants from Bayer and Zoe and personal fees from Boehringer Ingelheim, Pfizer, and Freenome outside this work. Dr. Keedwell and Dr. Kuhnle disclosed no relevant financial relationships. Dr. Frayn is an author of books on nutrition and metabolism.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Night owls have higher risk of developing type 2 diabetes
, compared with their “early bird” counterparts, according to a new study, published in Annals of Internal Medicine.
The work focused on participants’ self-assessed chronotype – an individuals’ circadian preference, or natural preference to sleep and wake up earlier or later, commonly known as being an early bird or a night owl.
Analyzing the self-reported lifestyle behaviors and sleeping habits of more than 60,000 middle-aged female nurses, researchers from Brigham and Women’s Hospital and Harvard Medical School, both in Boston, found that those with a preference for waking up later had a 72% higher risk for diabetes and were 54% more likely to have unhealthy lifestyle behaviors, compared with participants who tended to wake up earlier.
After adjustment for six lifestyle factors – diet, alcohol use, body mass index (BMI), physical activity, smoking status, and sleep duration – the association between diabetes risk and evening chronotype weakened to a 19% higher risk of developing type 2 diabetes.
In a subgroup analysis, this association was stronger among women who either had had no night shifts over the previous 2 years or had worked night shifts for less than 10 years in their careers. For nurses who had worked night shifts recently, the study found no association between evening chronotype and diabetes risk.
The participants, drawn from the Nurses’ Health Study II, were between 45 and 62 years age, with no history of cancer, cardiovascular disease, or diabetes. Researchers followed the group from 2009 until 2017.
Is there a mismatch between natural circadian rhythm and work schedule?
The authors, led by Sina Kianersi, DVM, PhD, of Harvard Medical School, Boston, suggest that their results may be linked to a mismatch between a person’s circadian rhythm and their physical and social environment – for example, if someone lives on a schedule opposite to their circadian preference.
In one 2015 study, female nurses who had worked daytime shifts for more than 10 years but had an evening chronotype had the highest diabetes risk, compared with early chronotypes (51% more likely to develop type 2 diabetes).
In a 2022 study, an evening chronotype was associated with a 30% elevated risk for type 2 diabetes. The authors speculated that circadian misalignment could be to blame – for example, being a night owl but working early morning – which can disrupt glycemic and lipid metabolism.
Previous studies have found that shorter or irregular sleep habits are associated with a higher risk of type 2 diabetes. Other studies have also found that people with an evening chronotype are more likely than early birds to have unhealthy eating habits, have lower levels of physical activity, and smoke and drink.
This new study did not find that an evening chronotype was associated with unhealthy drinking, which the authors defined as having one or more drinks per day.
In an accompanying editorial, two physicians from the Harvard T.H. Chan School of Public Health in Boston caution that the statistical design of the study limits its ability to establish causation.
“Chronotype could change later, which might correlate with lifestyle changes,” write Kehuan Lin, MS, Mingyang Song, MBBS, and Edward Giovannucci, MD. “Experimental trials are required to determine whether chronotype is a marker of unhealthy lifestyle or an independent determinant.”
They also suggest that psychological factors and the type of work being performed by the participants could be potential confounders.
The authors of the study note that their findings might not be generalizable to groups other than middle-aged White female nurses. The study population also had a relatively high level of education and were socioeconomically advantaged.
Self-reporting chronotypes with a single question could also result in misclassification and measurement error, the authors acknowledge.
The findings underscore the value of assessing an individuals’ chronotype for scheduling shift work – for example, assigning night owls to night shifts may improve their metabolic health and sleeping habits, according to the authors of the study.
“Given the importance of lifestyle modification in diabetes prevention, future research is warranted to investigate whether improving lifestyle behaviors could effectively reduce diabetes risk in persons with an evening chronotype,” the authors conclude.
The study was supported by grants from the National Institutes of Health and the European Research Council.
A version of this article first appeared on Medscape.com.
, compared with their “early bird” counterparts, according to a new study, published in Annals of Internal Medicine.
The work focused on participants’ self-assessed chronotype – an individuals’ circadian preference, or natural preference to sleep and wake up earlier or later, commonly known as being an early bird or a night owl.
Analyzing the self-reported lifestyle behaviors and sleeping habits of more than 60,000 middle-aged female nurses, researchers from Brigham and Women’s Hospital and Harvard Medical School, both in Boston, found that those with a preference for waking up later had a 72% higher risk for diabetes and were 54% more likely to have unhealthy lifestyle behaviors, compared with participants who tended to wake up earlier.
After adjustment for six lifestyle factors – diet, alcohol use, body mass index (BMI), physical activity, smoking status, and sleep duration – the association between diabetes risk and evening chronotype weakened to a 19% higher risk of developing type 2 diabetes.
In a subgroup analysis, this association was stronger among women who either had had no night shifts over the previous 2 years or had worked night shifts for less than 10 years in their careers. For nurses who had worked night shifts recently, the study found no association between evening chronotype and diabetes risk.
The participants, drawn from the Nurses’ Health Study II, were between 45 and 62 years age, with no history of cancer, cardiovascular disease, or diabetes. Researchers followed the group from 2009 until 2017.
Is there a mismatch between natural circadian rhythm and work schedule?
The authors, led by Sina Kianersi, DVM, PhD, of Harvard Medical School, Boston, suggest that their results may be linked to a mismatch between a person’s circadian rhythm and their physical and social environment – for example, if someone lives on a schedule opposite to their circadian preference.
In one 2015 study, female nurses who had worked daytime shifts for more than 10 years but had an evening chronotype had the highest diabetes risk, compared with early chronotypes (51% more likely to develop type 2 diabetes).
In a 2022 study, an evening chronotype was associated with a 30% elevated risk for type 2 diabetes. The authors speculated that circadian misalignment could be to blame – for example, being a night owl but working early morning – which can disrupt glycemic and lipid metabolism.
Previous studies have found that shorter or irregular sleep habits are associated with a higher risk of type 2 diabetes. Other studies have also found that people with an evening chronotype are more likely than early birds to have unhealthy eating habits, have lower levels of physical activity, and smoke and drink.
This new study did not find that an evening chronotype was associated with unhealthy drinking, which the authors defined as having one or more drinks per day.
In an accompanying editorial, two physicians from the Harvard T.H. Chan School of Public Health in Boston caution that the statistical design of the study limits its ability to establish causation.
“Chronotype could change later, which might correlate with lifestyle changes,” write Kehuan Lin, MS, Mingyang Song, MBBS, and Edward Giovannucci, MD. “Experimental trials are required to determine whether chronotype is a marker of unhealthy lifestyle or an independent determinant.”
They also suggest that psychological factors and the type of work being performed by the participants could be potential confounders.
The authors of the study note that their findings might not be generalizable to groups other than middle-aged White female nurses. The study population also had a relatively high level of education and were socioeconomically advantaged.
Self-reporting chronotypes with a single question could also result in misclassification and measurement error, the authors acknowledge.
The findings underscore the value of assessing an individuals’ chronotype for scheduling shift work – for example, assigning night owls to night shifts may improve their metabolic health and sleeping habits, according to the authors of the study.
“Given the importance of lifestyle modification in diabetes prevention, future research is warranted to investigate whether improving lifestyle behaviors could effectively reduce diabetes risk in persons with an evening chronotype,” the authors conclude.
The study was supported by grants from the National Institutes of Health and the European Research Council.
A version of this article first appeared on Medscape.com.
, compared with their “early bird” counterparts, according to a new study, published in Annals of Internal Medicine.
The work focused on participants’ self-assessed chronotype – an individuals’ circadian preference, or natural preference to sleep and wake up earlier or later, commonly known as being an early bird or a night owl.
Analyzing the self-reported lifestyle behaviors and sleeping habits of more than 60,000 middle-aged female nurses, researchers from Brigham and Women’s Hospital and Harvard Medical School, both in Boston, found that those with a preference for waking up later had a 72% higher risk for diabetes and were 54% more likely to have unhealthy lifestyle behaviors, compared with participants who tended to wake up earlier.
After adjustment for six lifestyle factors – diet, alcohol use, body mass index (BMI), physical activity, smoking status, and sleep duration – the association between diabetes risk and evening chronotype weakened to a 19% higher risk of developing type 2 diabetes.
In a subgroup analysis, this association was stronger among women who either had had no night shifts over the previous 2 years or had worked night shifts for less than 10 years in their careers. For nurses who had worked night shifts recently, the study found no association between evening chronotype and diabetes risk.
The participants, drawn from the Nurses’ Health Study II, were between 45 and 62 years age, with no history of cancer, cardiovascular disease, or diabetes. Researchers followed the group from 2009 until 2017.
Is there a mismatch between natural circadian rhythm and work schedule?
The authors, led by Sina Kianersi, DVM, PhD, of Harvard Medical School, Boston, suggest that their results may be linked to a mismatch between a person’s circadian rhythm and their physical and social environment – for example, if someone lives on a schedule opposite to their circadian preference.
In one 2015 study, female nurses who had worked daytime shifts for more than 10 years but had an evening chronotype had the highest diabetes risk, compared with early chronotypes (51% more likely to develop type 2 diabetes).
In a 2022 study, an evening chronotype was associated with a 30% elevated risk for type 2 diabetes. The authors speculated that circadian misalignment could be to blame – for example, being a night owl but working early morning – which can disrupt glycemic and lipid metabolism.
Previous studies have found that shorter or irregular sleep habits are associated with a higher risk of type 2 diabetes. Other studies have also found that people with an evening chronotype are more likely than early birds to have unhealthy eating habits, have lower levels of physical activity, and smoke and drink.
This new study did not find that an evening chronotype was associated with unhealthy drinking, which the authors defined as having one or more drinks per day.
In an accompanying editorial, two physicians from the Harvard T.H. Chan School of Public Health in Boston caution that the statistical design of the study limits its ability to establish causation.
“Chronotype could change later, which might correlate with lifestyle changes,” write Kehuan Lin, MS, Mingyang Song, MBBS, and Edward Giovannucci, MD. “Experimental trials are required to determine whether chronotype is a marker of unhealthy lifestyle or an independent determinant.”
They also suggest that psychological factors and the type of work being performed by the participants could be potential confounders.
The authors of the study note that their findings might not be generalizable to groups other than middle-aged White female nurses. The study population also had a relatively high level of education and were socioeconomically advantaged.
Self-reporting chronotypes with a single question could also result in misclassification and measurement error, the authors acknowledge.
The findings underscore the value of assessing an individuals’ chronotype for scheduling shift work – for example, assigning night owls to night shifts may improve their metabolic health and sleeping habits, according to the authors of the study.
“Given the importance of lifestyle modification in diabetes prevention, future research is warranted to investigate whether improving lifestyle behaviors could effectively reduce diabetes risk in persons with an evening chronotype,” the authors conclude.
The study was supported by grants from the National Institutes of Health and the European Research Council.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
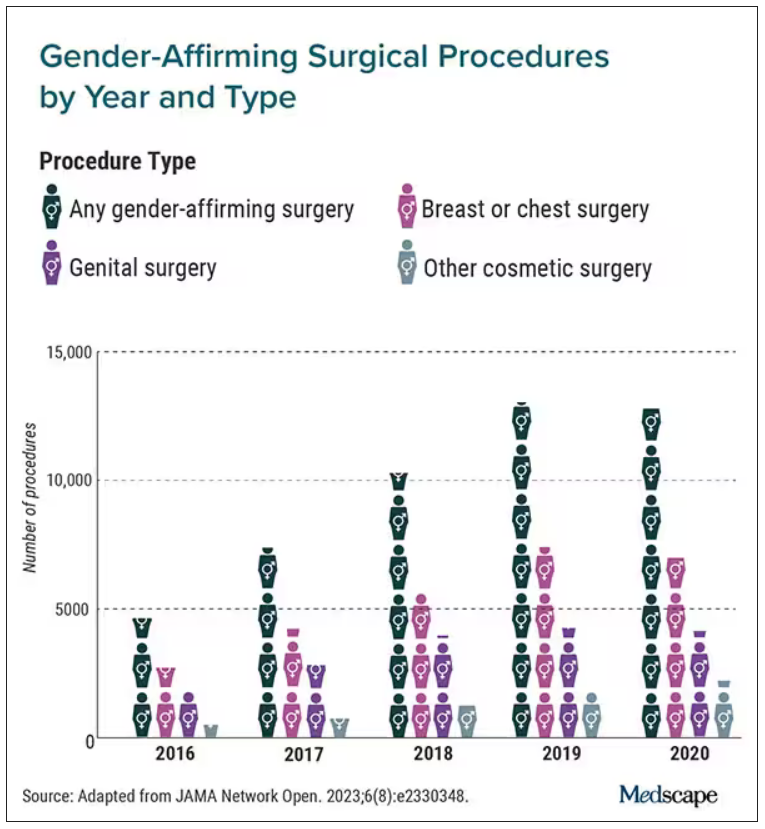
Gender-affirming surgeries nearly tripled between 2016 and 2019: Study
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
FDA okays first-ever new drug for rare bone disorder
Affecting roughly 400 people in the United States and 900 worldwide, FOP is an autosomal dominant condition in which bone develops in soft connective tissue areas of the body where it isn’t normally present (heterotopic ossification), such as the ligaments, tendons, and skeletal muscles. This leads to severe restriction in mobility and function, to the point that people lose the ability to feed or care for themselves. Most are completely disabled by age 30 years and median life expectancy is 56 years, with death often caused by bone formation around the rib cage restricting respiration.
“As a clinician caring for patients with FOP, I personally see the daily challenges and stresses that our patients and their families must contend with ... since the accumulation of heterotopic ossification in FOP is progressive, irreversible, and life altering. This medication is an important treatment option for our FOP community,” said endocrinologist Edward Hsiao, MD, professor of medicine at the University of California, San Francisco, in a statement from Ipsen.
Taken orally, palovarotene selectively targets the gamma subtype of retinoic acid receptors that regulate skeletal development and ectopic bone in the retinoid signaling pathway. The drug mediates interactions between these receptors, growth factors, and proteins within that pathway to reduce new abnormal bone formation.
It is now FDA approved for the treatment of FOP in female patients aged 8 years or older and male patients aged 10 years or older. The recommended dosing is 5 mg daily or weight-based equivalent for pediatric patients under 14 years of age, which can be modified or increased for flare-up symptoms. It is contraindicated during pregnancy.
The FDA approval was based on 18-month data from the phase 3, multicenter, open-label MOVE trial that included 107 adult and pediatric patients, over 10% of the world’s population with FOP. All received oral palovarotene and were compared with untreated individuals from a prior natural history study of the condition. The drug reduced annualized heterotopic ossification volume by 54%.
Side effects were typical of those seen with other systemic retinoid drugs, including mucocutaneous events such as dryness of the skin and mucous membranes, alopecia, drug eruption, rash, and pruritus, and musculoskeletal events, such as arthralgia and premature growth plate closure in growing children.
According to Dr. Hsiao, who was a MOVE investigator, the study “showed that Sohonos can decrease new heterotopic ossification, and that palovarotene can be tolerated by many patients with FOP. Sohonos is not for everyone. As with all medicines there are risks in this case especially for young children who may develop early growth plate closure. In addition, Sohonos has the same side effects as other retinoids.”
The FDA approval of palovarotene follows its rejection for marketing authorization in the European Union in July 2023.
Reached for comment, an Ipsen spokesperson said in an interview: “We reached the end of the regulatory process in the European Union for Sohonos and are disappointed the European Commission decided not to approved palovarotene for people with FOP in Europe.”
The company is developing another drug, fidrisertib, for treating FOP. A pivotal phase 2 trial for that drug is now recruiting patients. Asked where Ipsen might try to market fidrisertib, the spokesperson replied:“At this point, our focus is on the completion of the pivotal trial.”
Meanwhile, in the United States, the FOP community is celebrating the palovarotene approval. In a statement, Michelle Davis, executive director of the International Fibrodysplasia Ossificans Progressiva Association, said: “FOP is life altering to the individuals diagnosed and their families. There’s not a day that goes by where those impacted don’t worry about the debilitating physical pain of muscle that is replaced by bone, another joint locking, or the relentless emotional toll of losing the ability to do an activity they love, or hold a loved one close. ... The first treatment for FOP has been proven to reduce the volume of new abnormal bone growth, which may result in better health outcomes for people living with FOP.”
Ipsen is offering a patient support program to assist with education, coverage, and reimbursement (1-866-435-5677).
A version of this article appeared on Medscape.com.
Affecting roughly 400 people in the United States and 900 worldwide, FOP is an autosomal dominant condition in which bone develops in soft connective tissue areas of the body where it isn’t normally present (heterotopic ossification), such as the ligaments, tendons, and skeletal muscles. This leads to severe restriction in mobility and function, to the point that people lose the ability to feed or care for themselves. Most are completely disabled by age 30 years and median life expectancy is 56 years, with death often caused by bone formation around the rib cage restricting respiration.
“As a clinician caring for patients with FOP, I personally see the daily challenges and stresses that our patients and their families must contend with ... since the accumulation of heterotopic ossification in FOP is progressive, irreversible, and life altering. This medication is an important treatment option for our FOP community,” said endocrinologist Edward Hsiao, MD, professor of medicine at the University of California, San Francisco, in a statement from Ipsen.
Taken orally, palovarotene selectively targets the gamma subtype of retinoic acid receptors that regulate skeletal development and ectopic bone in the retinoid signaling pathway. The drug mediates interactions between these receptors, growth factors, and proteins within that pathway to reduce new abnormal bone formation.
It is now FDA approved for the treatment of FOP in female patients aged 8 years or older and male patients aged 10 years or older. The recommended dosing is 5 mg daily or weight-based equivalent for pediatric patients under 14 years of age, which can be modified or increased for flare-up symptoms. It is contraindicated during pregnancy.
The FDA approval was based on 18-month data from the phase 3, multicenter, open-label MOVE trial that included 107 adult and pediatric patients, over 10% of the world’s population with FOP. All received oral palovarotene and were compared with untreated individuals from a prior natural history study of the condition. The drug reduced annualized heterotopic ossification volume by 54%.
Side effects were typical of those seen with other systemic retinoid drugs, including mucocutaneous events such as dryness of the skin and mucous membranes, alopecia, drug eruption, rash, and pruritus, and musculoskeletal events, such as arthralgia and premature growth plate closure in growing children.
According to Dr. Hsiao, who was a MOVE investigator, the study “showed that Sohonos can decrease new heterotopic ossification, and that palovarotene can be tolerated by many patients with FOP. Sohonos is not for everyone. As with all medicines there are risks in this case especially for young children who may develop early growth plate closure. In addition, Sohonos has the same side effects as other retinoids.”
The FDA approval of palovarotene follows its rejection for marketing authorization in the European Union in July 2023.
Reached for comment, an Ipsen spokesperson said in an interview: “We reached the end of the regulatory process in the European Union for Sohonos and are disappointed the European Commission decided not to approved palovarotene for people with FOP in Europe.”
The company is developing another drug, fidrisertib, for treating FOP. A pivotal phase 2 trial for that drug is now recruiting patients. Asked where Ipsen might try to market fidrisertib, the spokesperson replied:“At this point, our focus is on the completion of the pivotal trial.”
Meanwhile, in the United States, the FOP community is celebrating the palovarotene approval. In a statement, Michelle Davis, executive director of the International Fibrodysplasia Ossificans Progressiva Association, said: “FOP is life altering to the individuals diagnosed and their families. There’s not a day that goes by where those impacted don’t worry about the debilitating physical pain of muscle that is replaced by bone, another joint locking, or the relentless emotional toll of losing the ability to do an activity they love, or hold a loved one close. ... The first treatment for FOP has been proven to reduce the volume of new abnormal bone growth, which may result in better health outcomes for people living with FOP.”
Ipsen is offering a patient support program to assist with education, coverage, and reimbursement (1-866-435-5677).
A version of this article appeared on Medscape.com.
Affecting roughly 400 people in the United States and 900 worldwide, FOP is an autosomal dominant condition in which bone develops in soft connective tissue areas of the body where it isn’t normally present (heterotopic ossification), such as the ligaments, tendons, and skeletal muscles. This leads to severe restriction in mobility and function, to the point that people lose the ability to feed or care for themselves. Most are completely disabled by age 30 years and median life expectancy is 56 years, with death often caused by bone formation around the rib cage restricting respiration.
“As a clinician caring for patients with FOP, I personally see the daily challenges and stresses that our patients and their families must contend with ... since the accumulation of heterotopic ossification in FOP is progressive, irreversible, and life altering. This medication is an important treatment option for our FOP community,” said endocrinologist Edward Hsiao, MD, professor of medicine at the University of California, San Francisco, in a statement from Ipsen.
Taken orally, palovarotene selectively targets the gamma subtype of retinoic acid receptors that regulate skeletal development and ectopic bone in the retinoid signaling pathway. The drug mediates interactions between these receptors, growth factors, and proteins within that pathway to reduce new abnormal bone formation.
It is now FDA approved for the treatment of FOP in female patients aged 8 years or older and male patients aged 10 years or older. The recommended dosing is 5 mg daily or weight-based equivalent for pediatric patients under 14 years of age, which can be modified or increased for flare-up symptoms. It is contraindicated during pregnancy.
The FDA approval was based on 18-month data from the phase 3, multicenter, open-label MOVE trial that included 107 adult and pediatric patients, over 10% of the world’s population with FOP. All received oral palovarotene and were compared with untreated individuals from a prior natural history study of the condition. The drug reduced annualized heterotopic ossification volume by 54%.
Side effects were typical of those seen with other systemic retinoid drugs, including mucocutaneous events such as dryness of the skin and mucous membranes, alopecia, drug eruption, rash, and pruritus, and musculoskeletal events, such as arthralgia and premature growth plate closure in growing children.
According to Dr. Hsiao, who was a MOVE investigator, the study “showed that Sohonos can decrease new heterotopic ossification, and that palovarotene can be tolerated by many patients with FOP. Sohonos is not for everyone. As with all medicines there are risks in this case especially for young children who may develop early growth plate closure. In addition, Sohonos has the same side effects as other retinoids.”
The FDA approval of palovarotene follows its rejection for marketing authorization in the European Union in July 2023.
Reached for comment, an Ipsen spokesperson said in an interview: “We reached the end of the regulatory process in the European Union for Sohonos and are disappointed the European Commission decided not to approved palovarotene for people with FOP in Europe.”
The company is developing another drug, fidrisertib, for treating FOP. A pivotal phase 2 trial for that drug is now recruiting patients. Asked where Ipsen might try to market fidrisertib, the spokesperson replied:“At this point, our focus is on the completion of the pivotal trial.”
Meanwhile, in the United States, the FOP community is celebrating the palovarotene approval. In a statement, Michelle Davis, executive director of the International Fibrodysplasia Ossificans Progressiva Association, said: “FOP is life altering to the individuals diagnosed and their families. There’s not a day that goes by where those impacted don’t worry about the debilitating physical pain of muscle that is replaced by bone, another joint locking, or the relentless emotional toll of losing the ability to do an activity they love, or hold a loved one close. ... The first treatment for FOP has been proven to reduce the volume of new abnormal bone growth, which may result in better health outcomes for people living with FOP.”
Ipsen is offering a patient support program to assist with education, coverage, and reimbursement (1-866-435-5677).
A version of this article appeared on Medscape.com.
Skin reactions common at insulin pump infusion sites
new research suggests.
Insulin pump use is increasingly common, but many patients experience infusion-site failure that in some cases leads to discontinuation. In a novel investigation, researchers at the University of Washington, Seattle, used biopsies and noninvasive imaging to compare insulin pump sites with control sites in 30 patients. Several differences were found at pump sites in comparison with control sites, including fibrosis, inflammation, eosinophils, and increased vessel density.
“These findings support allergic sensitization as a potentially common reaction at [insulin pump] sites. The leading candidates causing this include insulin preservatives, plastic materials, and adhesive glue used in device manufacturing,” wrote Andrea Kalus, MD, of the university’s dermatology division, and colleagues. The findings were published recently in Diabetes Care.
The inflammatory response, they wrote, “may result in tissue changes responsible for the infusion-site failures seen frequently in clinical practice.”
Such infusion site problems represent an “Achilles heel” of these otherwise highly beneficial devices, lead author Irl Hirsch, MD, professor of medicine in the division of metabolism, endocrinology, and nutrition, said in a statement. “It doesn’t really matter how good the technology is. We still don’t understand what is happening with the infusion sites, much less to [be able to] fix it.”
Significant differences between pump and nonpump sites
In the cross-sectional study, Dr. Kalus and colleagues used noninvasive optical coherence tomography (OCT) immediately prior to performing punch biopsies at three sites: the site currently in active use, the “recovery site” used 3-5 days prior to the procedures, and control sites never used for pump infusion. Punch biopsies were also performed at those sites.
The mean age of the patients was 48.3 years, the mean diabetes duration was 30.4 years, and the mean duration of pump use was 15.8 years. Nearly all patients (93.3%) reported itchiness at the site, and 76.7% reported skin redness.
Of the 25 patients for whom OCT imaging was successful, statistical analysis showed significant differences in vascular area density and the optical attenuation coefficient, a surrogate for skin inflammation, between the pump and control sites and between recovery sites and current pump sites. The greater vessel density is likely a result of injury and repair related to catheter insertion, the authors said.
In the biopsy samples, both current and recovery sites showed increased fibrosis, fibrin, inflammation, fat necrosis, vascularity, and eosinophils, compared with the control sites, but no significant differences were found between current and recovery sites.
Eosinophils: ‘The most surprising histologic finding’
Eosinophils were found in 73% of skin biopsy specimens from current sites and in 75% of specimens from recovery sites, compared with none from the control sites (for both, P < .01). In all study participants, eosinophils were found in at least one current and/or recovery infusion site deep in the dermis near the interface with fat. The number of eosinophils ranged from 0 to 31 per high-power field, with a median of 4.
The number of eosinophils didn’t vary by type of insulin or brand of pump, but higher counts were seen in those who had used pumps for less than 10 years, compared with more than 20 years (P = .02).
The prevalence and degree of eosinophils were “the most surprising histologic finding,” the authors wrote, adding that “eosinophils are not typically present as a component of resident inflammatory cells in the skin.”
While eosinophils may be present in normal wound healing, “the absolute number and density of eosinophil in these samples support a delayed-type hypersensitivity response, which is typically observed between 2 and 7 days after exposure to an allergen. ... Eosinophils are often correlated with symptoms of itchiness and likely explain the high percentage of participants who reported itchiness in this study,” Dr. Kalus and colleagues wrote.
Correlation found between inflammation and glycemic control
All participants used the Dexcom G6 continuous glucose monitor as part of their usual care. Inflammation scores were positively correlated with insulin dose (P = .009) and were negatively correlated with time in range (P = .01).
No other OCT or biopsy findings differed by duration of pump use, previous use of animal insulin, or type of insulin.
The reason for these findings is unclear, Dr. Hirsch said. “How much was the catheter or the insulin causing the irritation around the sites? How much was it from the preservatives, or is this because of the insulin pump itself? All these questions need to be answered in future studies. ... The real goal of all of this is to minimize skin damage and improve the experience for our patients.”
The study was funded by the Leona M. and Harry B. Helmsley Charitable Trust. Dr. Hirsch reported grants and contracts from Insulet, Medtronic, and Dexcom outside the submitted work; consulting fees from Abbott Diabetes Care, Lifescan, and Hagar outside the submitted work; and honoraria for lectures, presentations, participation on speaker’s bureaus, manuscript writing, or educational events as section editor for UpToDate outside the submitted work. Dr. Kalus has no disclosures.
A version of this article first appeared on Medscape.com.
new research suggests.
Insulin pump use is increasingly common, but many patients experience infusion-site failure that in some cases leads to discontinuation. In a novel investigation, researchers at the University of Washington, Seattle, used biopsies and noninvasive imaging to compare insulin pump sites with control sites in 30 patients. Several differences were found at pump sites in comparison with control sites, including fibrosis, inflammation, eosinophils, and increased vessel density.
“These findings support allergic sensitization as a potentially common reaction at [insulin pump] sites. The leading candidates causing this include insulin preservatives, plastic materials, and adhesive glue used in device manufacturing,” wrote Andrea Kalus, MD, of the university’s dermatology division, and colleagues. The findings were published recently in Diabetes Care.
The inflammatory response, they wrote, “may result in tissue changes responsible for the infusion-site failures seen frequently in clinical practice.”
Such infusion site problems represent an “Achilles heel” of these otherwise highly beneficial devices, lead author Irl Hirsch, MD, professor of medicine in the division of metabolism, endocrinology, and nutrition, said in a statement. “It doesn’t really matter how good the technology is. We still don’t understand what is happening with the infusion sites, much less to [be able to] fix it.”
Significant differences between pump and nonpump sites
In the cross-sectional study, Dr. Kalus and colleagues used noninvasive optical coherence tomography (OCT) immediately prior to performing punch biopsies at three sites: the site currently in active use, the “recovery site” used 3-5 days prior to the procedures, and control sites never used for pump infusion. Punch biopsies were also performed at those sites.
The mean age of the patients was 48.3 years, the mean diabetes duration was 30.4 years, and the mean duration of pump use was 15.8 years. Nearly all patients (93.3%) reported itchiness at the site, and 76.7% reported skin redness.
Of the 25 patients for whom OCT imaging was successful, statistical analysis showed significant differences in vascular area density and the optical attenuation coefficient, a surrogate for skin inflammation, between the pump and control sites and between recovery sites and current pump sites. The greater vessel density is likely a result of injury and repair related to catheter insertion, the authors said.
In the biopsy samples, both current and recovery sites showed increased fibrosis, fibrin, inflammation, fat necrosis, vascularity, and eosinophils, compared with the control sites, but no significant differences were found between current and recovery sites.
Eosinophils: ‘The most surprising histologic finding’
Eosinophils were found in 73% of skin biopsy specimens from current sites and in 75% of specimens from recovery sites, compared with none from the control sites (for both, P < .01). In all study participants, eosinophils were found in at least one current and/or recovery infusion site deep in the dermis near the interface with fat. The number of eosinophils ranged from 0 to 31 per high-power field, with a median of 4.
The number of eosinophils didn’t vary by type of insulin or brand of pump, but higher counts were seen in those who had used pumps for less than 10 years, compared with more than 20 years (P = .02).
The prevalence and degree of eosinophils were “the most surprising histologic finding,” the authors wrote, adding that “eosinophils are not typically present as a component of resident inflammatory cells in the skin.”
While eosinophils may be present in normal wound healing, “the absolute number and density of eosinophil in these samples support a delayed-type hypersensitivity response, which is typically observed between 2 and 7 days after exposure to an allergen. ... Eosinophils are often correlated with symptoms of itchiness and likely explain the high percentage of participants who reported itchiness in this study,” Dr. Kalus and colleagues wrote.
Correlation found between inflammation and glycemic control
All participants used the Dexcom G6 continuous glucose monitor as part of their usual care. Inflammation scores were positively correlated with insulin dose (P = .009) and were negatively correlated with time in range (P = .01).
No other OCT or biopsy findings differed by duration of pump use, previous use of animal insulin, or type of insulin.
The reason for these findings is unclear, Dr. Hirsch said. “How much was the catheter or the insulin causing the irritation around the sites? How much was it from the preservatives, or is this because of the insulin pump itself? All these questions need to be answered in future studies. ... The real goal of all of this is to minimize skin damage and improve the experience for our patients.”
The study was funded by the Leona M. and Harry B. Helmsley Charitable Trust. Dr. Hirsch reported grants and contracts from Insulet, Medtronic, and Dexcom outside the submitted work; consulting fees from Abbott Diabetes Care, Lifescan, and Hagar outside the submitted work; and honoraria for lectures, presentations, participation on speaker’s bureaus, manuscript writing, or educational events as section editor for UpToDate outside the submitted work. Dr. Kalus has no disclosures.
A version of this article first appeared on Medscape.com.
new research suggests.
Insulin pump use is increasingly common, but many patients experience infusion-site failure that in some cases leads to discontinuation. In a novel investigation, researchers at the University of Washington, Seattle, used biopsies and noninvasive imaging to compare insulin pump sites with control sites in 30 patients. Several differences were found at pump sites in comparison with control sites, including fibrosis, inflammation, eosinophils, and increased vessel density.
“These findings support allergic sensitization as a potentially common reaction at [insulin pump] sites. The leading candidates causing this include insulin preservatives, plastic materials, and adhesive glue used in device manufacturing,” wrote Andrea Kalus, MD, of the university’s dermatology division, and colleagues. The findings were published recently in Diabetes Care.
The inflammatory response, they wrote, “may result in tissue changes responsible for the infusion-site failures seen frequently in clinical practice.”
Such infusion site problems represent an “Achilles heel” of these otherwise highly beneficial devices, lead author Irl Hirsch, MD, professor of medicine in the division of metabolism, endocrinology, and nutrition, said in a statement. “It doesn’t really matter how good the technology is. We still don’t understand what is happening with the infusion sites, much less to [be able to] fix it.”
Significant differences between pump and nonpump sites
In the cross-sectional study, Dr. Kalus and colleagues used noninvasive optical coherence tomography (OCT) immediately prior to performing punch biopsies at three sites: the site currently in active use, the “recovery site” used 3-5 days prior to the procedures, and control sites never used for pump infusion. Punch biopsies were also performed at those sites.
The mean age of the patients was 48.3 years, the mean diabetes duration was 30.4 years, and the mean duration of pump use was 15.8 years. Nearly all patients (93.3%) reported itchiness at the site, and 76.7% reported skin redness.
Of the 25 patients for whom OCT imaging was successful, statistical analysis showed significant differences in vascular area density and the optical attenuation coefficient, a surrogate for skin inflammation, between the pump and control sites and between recovery sites and current pump sites. The greater vessel density is likely a result of injury and repair related to catheter insertion, the authors said.
In the biopsy samples, both current and recovery sites showed increased fibrosis, fibrin, inflammation, fat necrosis, vascularity, and eosinophils, compared with the control sites, but no significant differences were found between current and recovery sites.
Eosinophils: ‘The most surprising histologic finding’
Eosinophils were found in 73% of skin biopsy specimens from current sites and in 75% of specimens from recovery sites, compared with none from the control sites (for both, P < .01). In all study participants, eosinophils were found in at least one current and/or recovery infusion site deep in the dermis near the interface with fat. The number of eosinophils ranged from 0 to 31 per high-power field, with a median of 4.
The number of eosinophils didn’t vary by type of insulin or brand of pump, but higher counts were seen in those who had used pumps for less than 10 years, compared with more than 20 years (P = .02).
The prevalence and degree of eosinophils were “the most surprising histologic finding,” the authors wrote, adding that “eosinophils are not typically present as a component of resident inflammatory cells in the skin.”
While eosinophils may be present in normal wound healing, “the absolute number and density of eosinophil in these samples support a delayed-type hypersensitivity response, which is typically observed between 2 and 7 days after exposure to an allergen. ... Eosinophils are often correlated with symptoms of itchiness and likely explain the high percentage of participants who reported itchiness in this study,” Dr. Kalus and colleagues wrote.
Correlation found between inflammation and glycemic control
All participants used the Dexcom G6 continuous glucose monitor as part of their usual care. Inflammation scores were positively correlated with insulin dose (P = .009) and were negatively correlated with time in range (P = .01).
No other OCT or biopsy findings differed by duration of pump use, previous use of animal insulin, or type of insulin.
The reason for these findings is unclear, Dr. Hirsch said. “How much was the catheter or the insulin causing the irritation around the sites? How much was it from the preservatives, or is this because of the insulin pump itself? All these questions need to be answered in future studies. ... The real goal of all of this is to minimize skin damage and improve the experience for our patients.”
The study was funded by the Leona M. and Harry B. Helmsley Charitable Trust. Dr. Hirsch reported grants and contracts from Insulet, Medtronic, and Dexcom outside the submitted work; consulting fees from Abbott Diabetes Care, Lifescan, and Hagar outside the submitted work; and honoraria for lectures, presentations, participation on speaker’s bureaus, manuscript writing, or educational events as section editor for UpToDate outside the submitted work. Dr. Kalus has no disclosures.
A version of this article first appeared on Medscape.com.
FROM DIABETES CARE
The fertile future of fertility technology
Fifth pregnancy, first baby.
After four pregnancies resulted in losses – and doing things as natural as possible and leaving it up to the birds, bees, and fate – my husband and I decided to explore in vitro fertilization (IVF).
Drugs to direct my follicles to produce more eggs, an egg retrieval procedure, genetic testing of our embryos, a quick procedure to remove a residual uterine septum from my uterus, drugs to thicken my endometrial lining to prepare my body to receive an embryo, an embryo transfer, steroids to suppress my immune system so my body would accept the pregnancy, blood thinner shots to promote blood flow to the baby, and 10 weeks of progesterone in oil shots later and we’re days away from welcoming our first baby into our lives.
In short, there’s more than one way to define “miracle baby.”
Global estimates say 48 million couples and 186 million individuals struggle with infertility. On average, 2 million infants born in the United States each year are conceived through assisted reproductive technology and the demand for treatments like IVF have doubled in the last decade.
Now the need for treatments outweighs clinician availability. “We have about 1,250 practicing fertility physicians in the U.S. to serve the whole country, which is highly inadequate,” said Eduardo Hariton, MD, a reproductive endocrinology physician in San Francisco and managing director of the U.S. Fertility Innovation Fund. “We have people that want to get care waiting 1 to 3 months to be seen.”
Dr. Hariton explains that U.S. IVF clinics are performing around 250,000 to 300,000 IVF cycles per year and need to be doing a million-plus to meet demand. This, plus the cost of fertility treatments – an average IVF cycle runs $23,500 and the majority of patients need multiple cycles to conceive – keeps the barrier to entry high.
Enter technology: New advances are on the way to help the assisted fertility process to run smoother and be less costly. “The field is really coming into an age of great progress and innovation,” added S. Zev Williams, MD, PhD, chief of the division of reproductive endocrinology and Infertility at Columbia University Irving Medical Center, New York City.
I’m personally grateful that such technology exists.
AI will help, of course
Fertility treatments involve endless analysis, diagnosis, and recommendations – dozens if not hundreds of decisions from each physician for each patient. Human action and reaction can affect this process, Dr. Hariton explained.
For example, if he hyperstimulated a woman during the follicle growing stage of her egg retrieval and ended up with eggs too large to retrieve, Dr. Hariton said he may subconsciously be more inclined to be extra cautious with his patients the week after, and vice versa.
This is where AI can help. “Rather than me making decisions from a couple of thousands of cycles of experience, I get to leverage hundreds of thousands of cycles from different providers over different people,” said Dr. Hariton. “I get to use all the data from that patient today – her age, her weight, what happened last cycle, how she’s doing – and make a very objective decision about the optimal time to give that woman or that couple the best outcome possible.”
AI can also assist with tasks like embryo grading. “Once our embryos are made in the lab, we usually have an embryologist looking at those embryos, grading them on a three-variable scale, and then picking the nicest one for transfer,” said Dr. Hariton. Machine learning computer vision software can help doctors select the best embryo.
Many of these AI products are in trials in the United States and some AI-based technology is already being used in fertility labs, especially in other countries. “ALife recently launched a suite of products to help with their decisions during stimulation that can help with the quality KPIs [key performance indicators] in the lab,” said Dr. Hariton. “There’s also a company that does AI-based predictions of success to give patients a better estimate called Univfy.” More AI products are still in development or awaiting Food and Drug Administration clearance.
Robots lend a hand
Like artificial intelligence, robots can be a big help in the IVF lab. Columbia University Fertility Center recently became the first to use an articulated (ART) robot to handle precise and highly repetitive work.
“IVF, from the initial point, involves creating these special plates where embryos can grow, and you do that by making little droplets,” said Dr. Williams. “It’s very time-consuming to create tons of these little droplets for the embryos to grow.” Thus, the lab created a robot to help squirt drops of the media substance required to sustain embryos in a way that is 10 times more precise than that of a trained embryologist.
“It’s a win-win because you allow the robots to do things better than a human can and this allows the humans to do things that a robot just can’t do,” explained Dr. Williams. He and his team began using this technology in the beginning of November 2022.
Dr. Williams sees ART robots being used in many more parts of the fertility treatment journey along the way, like preparing eggs after they are retrieved and performing intracytoplasmic sperm injection (ICSI), with the robot injecting the sperm into the egg.
Launching with the plate making, said Dr. Williams, is a low stakes entry point for robotic technology in the lab. “It allows us to introduce robotics to automate and optimize each step along the way, but to do so in the safest possible way.”
Dr. Williams estimates that robots will have their hands on actual eggs and sperm in 5 years.
Updates in genetic testing
Currently, if a couple wants to have their embryos genetically tested, also known as preimplantation genetic testing, each embryo must be frozen, then a biopsy of that embryo is performed and sent to the lab.
“It takes time to get the results,” said Dr. Williams. “The whole time you’re waiting, you don’t know if you’re going to have any embryos that are transferable or if next month you’re going to have to do another IVF cycle.”
Columbia researchers recently developed a new in-house test that can determine if a fetus or embryo has the right number of chromosomes. This STORK (Short-read Transpore Rapid Karyotyping) can be performed without freezing embryos and sending them out, which Dr. Williams said can save couples money and time, as they won’t necessarily need to do a separate embryo transfer cycle and can transfer an embryo in the same cycle. “You can test in the morning and transfer in the afternoon,” said Dr. Williams.
The test is currently awaiting approval and will first be used to test miscarriage samples to see if embryos were genetically normal or not, which he said should cost around $200 vs. the $2,000 to $4,000 it can cost to have fetal tissue sent to the lab – and insurance doesn’t cover the procedure until after a second or third miscarriage.
This, said Dr. Williams, should be in the field in less than a year, and he estimates that the test will be used for fresh embryos in about a year and a half.
Sperm collection made simpler
Typically, a man delivers a sperm sample in a room at an IVF clinic or by collecting a sample at home and rushing it to the clinic before it degrades, which Dr. Williams said can happen in as little as 15 minutes.
In 2020, Dr. Williams and his team began using a custom at-home sperm collection box that houses sperm in a recyclable foam container that holds a sample cup, which is filled with special sperm-supporting media, at an angle that prevents evaporation and maintains temperature and pH. This allows patients to collect samples in the comfort of their homes and increases the clock to 3 hours.
“It’s great for the patients because it’s much more comfortable,” said Dr. Williams, who notes that having to “perform” on site can be stressful for men. Studies the team has conducted have shown sperm collected in this manner have a better success rate than those collected in the lab, and 90% of Columbia’s Fertility Center patients are now providing sperm samples this way.
Similar innovations to deliver sperm, like Protex, are now on the market, while companies like myLabBox and Legacy are offering at-home sperm testing kits to mail in for a full semen analysis.
At-home monitoring: More and better
Wearable reproductive health devices are also helping more women get pregnant. “I am very excited about biometric data harnessed in wearables to predict periods, ovulation, and fertility,” said Amander Clark, PhD, director of the UCLA Center for Reproductive Science, Health, and Education, Los Angeles.
The Tempdrop Fertility and Ovulation Tracker, for instance, is a wearable sensor with an accompanying charting app that helps a woman identify her most fertile days to conceive. The Bellabeat Ivy is a women’s health smart bracelet with a strong focus on tracking a woman’s cycle and fertility, pregnancy, and postnatal symptoms. And Mirvie, which is currently in development, is a blood test that will be able to predict pregnancy complications earlier.
Physicians are also looking to move as much of the lab experience as they can into a patient’s home, which streamlines processes while offering privacy and comfort. For example, Dr. Hariton, who runs a strategic venture capital fund for physicians, said his team is currently working with a company that does remote ultrasounds.
And Mira, an at-home hormone monitor, uses patented AI algorithms to accurately measure the levels of major reproductive health hormones (E3G, LH, PdG, FSH) in urine, said Meir Olcha, MD, chief medical officer at Sama Fertility. The product recently completed a clinical trial, which showed it was a viable alternative to blood serum for patients undergoing IVF.
Stem cells could make eggs ageless
Research shows that a woman’s egg quality decreases gradually but significantly starting at age 32 and more rapidly after 37. Sperm quality may also decrease with age. A possible workaround: Scientists are actively researching how to create eggs and sperm from stem cells.
“I think getting eggs from stem cells will happen in the future,” said Dr. Hariton, who notes that this type of technology would be a game changer in his clinic. “It will make some of the hardest diagnoses that I have – which is on a daily basis, ‘I’m so sorry, you’re in premature menopause’ or ‘I don’t think we’re going to be successful getting you pregnant with your own eggs; here are some other options like donor eggs’ – much better,” he added. And stem cells are currently being used to research causes of infertility.
Clinics like UCLA have already been making strides. “We are using stem cells to identify new genes required for reproduction and to define the role of these genes in human fertility and infertility,” said Dr. Clark, a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA, who recently led a study in this arena. “In vitro gametogenesis (IVG), another stem cell technology, is currently used in the research lab to understand causes of infertility.”
These stem cell-based embryo models, she said, can help researchers understand the first few days of embryo development after an embryo implants and be used to provide critical information on causes of early pregnancy loss or birth defects.
A version of this article appeared on Medscape.com.
Fifth pregnancy, first baby.
After four pregnancies resulted in losses – and doing things as natural as possible and leaving it up to the birds, bees, and fate – my husband and I decided to explore in vitro fertilization (IVF).
Drugs to direct my follicles to produce more eggs, an egg retrieval procedure, genetic testing of our embryos, a quick procedure to remove a residual uterine septum from my uterus, drugs to thicken my endometrial lining to prepare my body to receive an embryo, an embryo transfer, steroids to suppress my immune system so my body would accept the pregnancy, blood thinner shots to promote blood flow to the baby, and 10 weeks of progesterone in oil shots later and we’re days away from welcoming our first baby into our lives.
In short, there’s more than one way to define “miracle baby.”
Global estimates say 48 million couples and 186 million individuals struggle with infertility. On average, 2 million infants born in the United States each year are conceived through assisted reproductive technology and the demand for treatments like IVF have doubled in the last decade.
Now the need for treatments outweighs clinician availability. “We have about 1,250 practicing fertility physicians in the U.S. to serve the whole country, which is highly inadequate,” said Eduardo Hariton, MD, a reproductive endocrinology physician in San Francisco and managing director of the U.S. Fertility Innovation Fund. “We have people that want to get care waiting 1 to 3 months to be seen.”
Dr. Hariton explains that U.S. IVF clinics are performing around 250,000 to 300,000 IVF cycles per year and need to be doing a million-plus to meet demand. This, plus the cost of fertility treatments – an average IVF cycle runs $23,500 and the majority of patients need multiple cycles to conceive – keeps the barrier to entry high.
Enter technology: New advances are on the way to help the assisted fertility process to run smoother and be less costly. “The field is really coming into an age of great progress and innovation,” added S. Zev Williams, MD, PhD, chief of the division of reproductive endocrinology and Infertility at Columbia University Irving Medical Center, New York City.
I’m personally grateful that such technology exists.
AI will help, of course
Fertility treatments involve endless analysis, diagnosis, and recommendations – dozens if not hundreds of decisions from each physician for each patient. Human action and reaction can affect this process, Dr. Hariton explained.
For example, if he hyperstimulated a woman during the follicle growing stage of her egg retrieval and ended up with eggs too large to retrieve, Dr. Hariton said he may subconsciously be more inclined to be extra cautious with his patients the week after, and vice versa.
This is where AI can help. “Rather than me making decisions from a couple of thousands of cycles of experience, I get to leverage hundreds of thousands of cycles from different providers over different people,” said Dr. Hariton. “I get to use all the data from that patient today – her age, her weight, what happened last cycle, how she’s doing – and make a very objective decision about the optimal time to give that woman or that couple the best outcome possible.”
AI can also assist with tasks like embryo grading. “Once our embryos are made in the lab, we usually have an embryologist looking at those embryos, grading them on a three-variable scale, and then picking the nicest one for transfer,” said Dr. Hariton. Machine learning computer vision software can help doctors select the best embryo.
Many of these AI products are in trials in the United States and some AI-based technology is already being used in fertility labs, especially in other countries. “ALife recently launched a suite of products to help with their decisions during stimulation that can help with the quality KPIs [key performance indicators] in the lab,” said Dr. Hariton. “There’s also a company that does AI-based predictions of success to give patients a better estimate called Univfy.” More AI products are still in development or awaiting Food and Drug Administration clearance.
Robots lend a hand
Like artificial intelligence, robots can be a big help in the IVF lab. Columbia University Fertility Center recently became the first to use an articulated (ART) robot to handle precise and highly repetitive work.
“IVF, from the initial point, involves creating these special plates where embryos can grow, and you do that by making little droplets,” said Dr. Williams. “It’s very time-consuming to create tons of these little droplets for the embryos to grow.” Thus, the lab created a robot to help squirt drops of the media substance required to sustain embryos in a way that is 10 times more precise than that of a trained embryologist.
“It’s a win-win because you allow the robots to do things better than a human can and this allows the humans to do things that a robot just can’t do,” explained Dr. Williams. He and his team began using this technology in the beginning of November 2022.
Dr. Williams sees ART robots being used in many more parts of the fertility treatment journey along the way, like preparing eggs after they are retrieved and performing intracytoplasmic sperm injection (ICSI), with the robot injecting the sperm into the egg.
Launching with the plate making, said Dr. Williams, is a low stakes entry point for robotic technology in the lab. “It allows us to introduce robotics to automate and optimize each step along the way, but to do so in the safest possible way.”
Dr. Williams estimates that robots will have their hands on actual eggs and sperm in 5 years.
Updates in genetic testing
Currently, if a couple wants to have their embryos genetically tested, also known as preimplantation genetic testing, each embryo must be frozen, then a biopsy of that embryo is performed and sent to the lab.
“It takes time to get the results,” said Dr. Williams. “The whole time you’re waiting, you don’t know if you’re going to have any embryos that are transferable or if next month you’re going to have to do another IVF cycle.”
Columbia researchers recently developed a new in-house test that can determine if a fetus or embryo has the right number of chromosomes. This STORK (Short-read Transpore Rapid Karyotyping) can be performed without freezing embryos and sending them out, which Dr. Williams said can save couples money and time, as they won’t necessarily need to do a separate embryo transfer cycle and can transfer an embryo in the same cycle. “You can test in the morning and transfer in the afternoon,” said Dr. Williams.
The test is currently awaiting approval and will first be used to test miscarriage samples to see if embryos were genetically normal or not, which he said should cost around $200 vs. the $2,000 to $4,000 it can cost to have fetal tissue sent to the lab – and insurance doesn’t cover the procedure until after a second or third miscarriage.
This, said Dr. Williams, should be in the field in less than a year, and he estimates that the test will be used for fresh embryos in about a year and a half.
Sperm collection made simpler
Typically, a man delivers a sperm sample in a room at an IVF clinic or by collecting a sample at home and rushing it to the clinic before it degrades, which Dr. Williams said can happen in as little as 15 minutes.
In 2020, Dr. Williams and his team began using a custom at-home sperm collection box that houses sperm in a recyclable foam container that holds a sample cup, which is filled with special sperm-supporting media, at an angle that prevents evaporation and maintains temperature and pH. This allows patients to collect samples in the comfort of their homes and increases the clock to 3 hours.
“It’s great for the patients because it’s much more comfortable,” said Dr. Williams, who notes that having to “perform” on site can be stressful for men. Studies the team has conducted have shown sperm collected in this manner have a better success rate than those collected in the lab, and 90% of Columbia’s Fertility Center patients are now providing sperm samples this way.
Similar innovations to deliver sperm, like Protex, are now on the market, while companies like myLabBox and Legacy are offering at-home sperm testing kits to mail in for a full semen analysis.
At-home monitoring: More and better
Wearable reproductive health devices are also helping more women get pregnant. “I am very excited about biometric data harnessed in wearables to predict periods, ovulation, and fertility,” said Amander Clark, PhD, director of the UCLA Center for Reproductive Science, Health, and Education, Los Angeles.
The Tempdrop Fertility and Ovulation Tracker, for instance, is a wearable sensor with an accompanying charting app that helps a woman identify her most fertile days to conceive. The Bellabeat Ivy is a women’s health smart bracelet with a strong focus on tracking a woman’s cycle and fertility, pregnancy, and postnatal symptoms. And Mirvie, which is currently in development, is a blood test that will be able to predict pregnancy complications earlier.
Physicians are also looking to move as much of the lab experience as they can into a patient’s home, which streamlines processes while offering privacy and comfort. For example, Dr. Hariton, who runs a strategic venture capital fund for physicians, said his team is currently working with a company that does remote ultrasounds.
And Mira, an at-home hormone monitor, uses patented AI algorithms to accurately measure the levels of major reproductive health hormones (E3G, LH, PdG, FSH) in urine, said Meir Olcha, MD, chief medical officer at Sama Fertility. The product recently completed a clinical trial, which showed it was a viable alternative to blood serum for patients undergoing IVF.
Stem cells could make eggs ageless
Research shows that a woman’s egg quality decreases gradually but significantly starting at age 32 and more rapidly after 37. Sperm quality may also decrease with age. A possible workaround: Scientists are actively researching how to create eggs and sperm from stem cells.
“I think getting eggs from stem cells will happen in the future,” said Dr. Hariton, who notes that this type of technology would be a game changer in his clinic. “It will make some of the hardest diagnoses that I have – which is on a daily basis, ‘I’m so sorry, you’re in premature menopause’ or ‘I don’t think we’re going to be successful getting you pregnant with your own eggs; here are some other options like donor eggs’ – much better,” he added. And stem cells are currently being used to research causes of infertility.
Clinics like UCLA have already been making strides. “We are using stem cells to identify new genes required for reproduction and to define the role of these genes in human fertility and infertility,” said Dr. Clark, a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA, who recently led a study in this arena. “In vitro gametogenesis (IVG), another stem cell technology, is currently used in the research lab to understand causes of infertility.”
These stem cell-based embryo models, she said, can help researchers understand the first few days of embryo development after an embryo implants and be used to provide critical information on causes of early pregnancy loss or birth defects.
A version of this article appeared on Medscape.com.
Fifth pregnancy, first baby.
After four pregnancies resulted in losses – and doing things as natural as possible and leaving it up to the birds, bees, and fate – my husband and I decided to explore in vitro fertilization (IVF).
Drugs to direct my follicles to produce more eggs, an egg retrieval procedure, genetic testing of our embryos, a quick procedure to remove a residual uterine septum from my uterus, drugs to thicken my endometrial lining to prepare my body to receive an embryo, an embryo transfer, steroids to suppress my immune system so my body would accept the pregnancy, blood thinner shots to promote blood flow to the baby, and 10 weeks of progesterone in oil shots later and we’re days away from welcoming our first baby into our lives.
In short, there’s more than one way to define “miracle baby.”
Global estimates say 48 million couples and 186 million individuals struggle with infertility. On average, 2 million infants born in the United States each year are conceived through assisted reproductive technology and the demand for treatments like IVF have doubled in the last decade.
Now the need for treatments outweighs clinician availability. “We have about 1,250 practicing fertility physicians in the U.S. to serve the whole country, which is highly inadequate,” said Eduardo Hariton, MD, a reproductive endocrinology physician in San Francisco and managing director of the U.S. Fertility Innovation Fund. “We have people that want to get care waiting 1 to 3 months to be seen.”
Dr. Hariton explains that U.S. IVF clinics are performing around 250,000 to 300,000 IVF cycles per year and need to be doing a million-plus to meet demand. This, plus the cost of fertility treatments – an average IVF cycle runs $23,500 and the majority of patients need multiple cycles to conceive – keeps the barrier to entry high.
Enter technology: New advances are on the way to help the assisted fertility process to run smoother and be less costly. “The field is really coming into an age of great progress and innovation,” added S. Zev Williams, MD, PhD, chief of the division of reproductive endocrinology and Infertility at Columbia University Irving Medical Center, New York City.
I’m personally grateful that such technology exists.
AI will help, of course
Fertility treatments involve endless analysis, diagnosis, and recommendations – dozens if not hundreds of decisions from each physician for each patient. Human action and reaction can affect this process, Dr. Hariton explained.
For example, if he hyperstimulated a woman during the follicle growing stage of her egg retrieval and ended up with eggs too large to retrieve, Dr. Hariton said he may subconsciously be more inclined to be extra cautious with his patients the week after, and vice versa.
This is where AI can help. “Rather than me making decisions from a couple of thousands of cycles of experience, I get to leverage hundreds of thousands of cycles from different providers over different people,” said Dr. Hariton. “I get to use all the data from that patient today – her age, her weight, what happened last cycle, how she’s doing – and make a very objective decision about the optimal time to give that woman or that couple the best outcome possible.”
AI can also assist with tasks like embryo grading. “Once our embryos are made in the lab, we usually have an embryologist looking at those embryos, grading them on a three-variable scale, and then picking the nicest one for transfer,” said Dr. Hariton. Machine learning computer vision software can help doctors select the best embryo.
Many of these AI products are in trials in the United States and some AI-based technology is already being used in fertility labs, especially in other countries. “ALife recently launched a suite of products to help with their decisions during stimulation that can help with the quality KPIs [key performance indicators] in the lab,” said Dr. Hariton. “There’s also a company that does AI-based predictions of success to give patients a better estimate called Univfy.” More AI products are still in development or awaiting Food and Drug Administration clearance.
Robots lend a hand
Like artificial intelligence, robots can be a big help in the IVF lab. Columbia University Fertility Center recently became the first to use an articulated (ART) robot to handle precise and highly repetitive work.
“IVF, from the initial point, involves creating these special plates where embryos can grow, and you do that by making little droplets,” said Dr. Williams. “It’s very time-consuming to create tons of these little droplets for the embryos to grow.” Thus, the lab created a robot to help squirt drops of the media substance required to sustain embryos in a way that is 10 times more precise than that of a trained embryologist.
“It’s a win-win because you allow the robots to do things better than a human can and this allows the humans to do things that a robot just can’t do,” explained Dr. Williams. He and his team began using this technology in the beginning of November 2022.
Dr. Williams sees ART robots being used in many more parts of the fertility treatment journey along the way, like preparing eggs after they are retrieved and performing intracytoplasmic sperm injection (ICSI), with the robot injecting the sperm into the egg.
Launching with the plate making, said Dr. Williams, is a low stakes entry point for robotic technology in the lab. “It allows us to introduce robotics to automate and optimize each step along the way, but to do so in the safest possible way.”
Dr. Williams estimates that robots will have their hands on actual eggs and sperm in 5 years.
Updates in genetic testing
Currently, if a couple wants to have their embryos genetically tested, also known as preimplantation genetic testing, each embryo must be frozen, then a biopsy of that embryo is performed and sent to the lab.
“It takes time to get the results,” said Dr. Williams. “The whole time you’re waiting, you don’t know if you’re going to have any embryos that are transferable or if next month you’re going to have to do another IVF cycle.”
Columbia researchers recently developed a new in-house test that can determine if a fetus or embryo has the right number of chromosomes. This STORK (Short-read Transpore Rapid Karyotyping) can be performed without freezing embryos and sending them out, which Dr. Williams said can save couples money and time, as they won’t necessarily need to do a separate embryo transfer cycle and can transfer an embryo in the same cycle. “You can test in the morning and transfer in the afternoon,” said Dr. Williams.
The test is currently awaiting approval and will first be used to test miscarriage samples to see if embryos were genetically normal or not, which he said should cost around $200 vs. the $2,000 to $4,000 it can cost to have fetal tissue sent to the lab – and insurance doesn’t cover the procedure until after a second or third miscarriage.
This, said Dr. Williams, should be in the field in less than a year, and he estimates that the test will be used for fresh embryos in about a year and a half.
Sperm collection made simpler
Typically, a man delivers a sperm sample in a room at an IVF clinic or by collecting a sample at home and rushing it to the clinic before it degrades, which Dr. Williams said can happen in as little as 15 minutes.
In 2020, Dr. Williams and his team began using a custom at-home sperm collection box that houses sperm in a recyclable foam container that holds a sample cup, which is filled with special sperm-supporting media, at an angle that prevents evaporation and maintains temperature and pH. This allows patients to collect samples in the comfort of their homes and increases the clock to 3 hours.
“It’s great for the patients because it’s much more comfortable,” said Dr. Williams, who notes that having to “perform” on site can be stressful for men. Studies the team has conducted have shown sperm collected in this manner have a better success rate than those collected in the lab, and 90% of Columbia’s Fertility Center patients are now providing sperm samples this way.
Similar innovations to deliver sperm, like Protex, are now on the market, while companies like myLabBox and Legacy are offering at-home sperm testing kits to mail in for a full semen analysis.
At-home monitoring: More and better
Wearable reproductive health devices are also helping more women get pregnant. “I am very excited about biometric data harnessed in wearables to predict periods, ovulation, and fertility,” said Amander Clark, PhD, director of the UCLA Center for Reproductive Science, Health, and Education, Los Angeles.
The Tempdrop Fertility and Ovulation Tracker, for instance, is a wearable sensor with an accompanying charting app that helps a woman identify her most fertile days to conceive. The Bellabeat Ivy is a women’s health smart bracelet with a strong focus on tracking a woman’s cycle and fertility, pregnancy, and postnatal symptoms. And Mirvie, which is currently in development, is a blood test that will be able to predict pregnancy complications earlier.
Physicians are also looking to move as much of the lab experience as they can into a patient’s home, which streamlines processes while offering privacy and comfort. For example, Dr. Hariton, who runs a strategic venture capital fund for physicians, said his team is currently working with a company that does remote ultrasounds.
And Mira, an at-home hormone monitor, uses patented AI algorithms to accurately measure the levels of major reproductive health hormones (E3G, LH, PdG, FSH) in urine, said Meir Olcha, MD, chief medical officer at Sama Fertility. The product recently completed a clinical trial, which showed it was a viable alternative to blood serum for patients undergoing IVF.
Stem cells could make eggs ageless
Research shows that a woman’s egg quality decreases gradually but significantly starting at age 32 and more rapidly after 37. Sperm quality may also decrease with age. A possible workaround: Scientists are actively researching how to create eggs and sperm from stem cells.
“I think getting eggs from stem cells will happen in the future,” said Dr. Hariton, who notes that this type of technology would be a game changer in his clinic. “It will make some of the hardest diagnoses that I have – which is on a daily basis, ‘I’m so sorry, you’re in premature menopause’ or ‘I don’t think we’re going to be successful getting you pregnant with your own eggs; here are some other options like donor eggs’ – much better,” he added. And stem cells are currently being used to research causes of infertility.
Clinics like UCLA have already been making strides. “We are using stem cells to identify new genes required for reproduction and to define the role of these genes in human fertility and infertility,” said Dr. Clark, a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA, who recently led a study in this arena. “In vitro gametogenesis (IVG), another stem cell technology, is currently used in the research lab to understand causes of infertility.”
These stem cell-based embryo models, she said, can help researchers understand the first few days of embryo development after an embryo implants and be used to provide critical information on causes of early pregnancy loss or birth defects.
A version of this article appeared on Medscape.com.
Pregnancy risks elevated in women with chronic pancreatitis
TOPLINE:
METHODOLOGY:
- A retrospective analysis of hospital discharge records from the National Inpatient Sample database between 2009 and 2019 was conducted.
- The sample included 3,094 pregnancies with chronic pancreatitis and roughly 40.8 million pregnancies without this condition.
- The study focused on primary maternal outcomes and primary perinatal outcomes in pregnancies affected by chronic pancreatitis after accounting for relevant covariates.
TAKEAWAY:
- Chronic pancreatitis pregnancies had elevated rates of gestational diabetes (adjusted odds ratio, 1.63), gestational hypertensive complications (aOR, 2.48), preterm labor (aOR, 3.10), and small size for gestational age (aOR, 2.40).
- Women with chronic pancreatitis and a history of renal failure were more prone to gestational hypertensive complications (aOR, 20.09).
- Women with alcohol-induced chronic pancreatitis had a 17-fold higher risk for fetal death (aOR, 17.15).
- Pregnancies with chronic pancreatitis were associated with longer hospital stays and higher hospital costs.
IN PRACTICE:
“Our study provides novel insights into the impact of chronic pancreatitis on maternal and fetal health. The implications of our findings are critical for health care professionals, particularly those involved in preconception counseling. Pregnant women with chronic pancreatitis should be under the care of a multidisciplinary team of health care providers,” the authors advise.
SOURCE:
The study was led by Chengu Niu, MD, with Rochester General Hospital, Rochester, N.Y. It was published online July 18 in Digestive and Liver Disease. The study had no specific funding.
LIMITATIONS:
The authors note potential inaccuracies because of coding in the National Inpatient Sample database, a lack of detailed information regarding medication use, and a lack of follow-up clinical information. The findings are specific to the United States and may not be applicable to other countries.
DISCLOSURES:
The authors have no relevant disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- A retrospective analysis of hospital discharge records from the National Inpatient Sample database between 2009 and 2019 was conducted.
- The sample included 3,094 pregnancies with chronic pancreatitis and roughly 40.8 million pregnancies without this condition.
- The study focused on primary maternal outcomes and primary perinatal outcomes in pregnancies affected by chronic pancreatitis after accounting for relevant covariates.
TAKEAWAY:
- Chronic pancreatitis pregnancies had elevated rates of gestational diabetes (adjusted odds ratio, 1.63), gestational hypertensive complications (aOR, 2.48), preterm labor (aOR, 3.10), and small size for gestational age (aOR, 2.40).
- Women with chronic pancreatitis and a history of renal failure were more prone to gestational hypertensive complications (aOR, 20.09).
- Women with alcohol-induced chronic pancreatitis had a 17-fold higher risk for fetal death (aOR, 17.15).
- Pregnancies with chronic pancreatitis were associated with longer hospital stays and higher hospital costs.
IN PRACTICE:
“Our study provides novel insights into the impact of chronic pancreatitis on maternal and fetal health. The implications of our findings are critical for health care professionals, particularly those involved in preconception counseling. Pregnant women with chronic pancreatitis should be under the care of a multidisciplinary team of health care providers,” the authors advise.
SOURCE:
The study was led by Chengu Niu, MD, with Rochester General Hospital, Rochester, N.Y. It was published online July 18 in Digestive and Liver Disease. The study had no specific funding.
LIMITATIONS:
The authors note potential inaccuracies because of coding in the National Inpatient Sample database, a lack of detailed information regarding medication use, and a lack of follow-up clinical information. The findings are specific to the United States and may not be applicable to other countries.
DISCLOSURES:
The authors have no relevant disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- A retrospective analysis of hospital discharge records from the National Inpatient Sample database between 2009 and 2019 was conducted.
- The sample included 3,094 pregnancies with chronic pancreatitis and roughly 40.8 million pregnancies without this condition.
- The study focused on primary maternal outcomes and primary perinatal outcomes in pregnancies affected by chronic pancreatitis after accounting for relevant covariates.
TAKEAWAY:
- Chronic pancreatitis pregnancies had elevated rates of gestational diabetes (adjusted odds ratio, 1.63), gestational hypertensive complications (aOR, 2.48), preterm labor (aOR, 3.10), and small size for gestational age (aOR, 2.40).
- Women with chronic pancreatitis and a history of renal failure were more prone to gestational hypertensive complications (aOR, 20.09).
- Women with alcohol-induced chronic pancreatitis had a 17-fold higher risk for fetal death (aOR, 17.15).
- Pregnancies with chronic pancreatitis were associated with longer hospital stays and higher hospital costs.
IN PRACTICE:
“Our study provides novel insights into the impact of chronic pancreatitis on maternal and fetal health. The implications of our findings are critical for health care professionals, particularly those involved in preconception counseling. Pregnant women with chronic pancreatitis should be under the care of a multidisciplinary team of health care providers,” the authors advise.
SOURCE:
The study was led by Chengu Niu, MD, with Rochester General Hospital, Rochester, N.Y. It was published online July 18 in Digestive and Liver Disease. The study had no specific funding.
LIMITATIONS:
The authors note potential inaccuracies because of coding in the National Inpatient Sample database, a lack of detailed information regarding medication use, and a lack of follow-up clinical information. The findings are specific to the United States and may not be applicable to other countries.
DISCLOSURES:
The authors have no relevant disclosures.
A version of this article appeared on Medscape.com.
Stiff arteries may cause metabolic syndrome
New research published in the American Journal of Physiology found that arterial stiffness occurred before the presence of metabolic syndrome. A progressive rise in stiffness was associated with a cumulative increase in risk for the condition among the 3,862 people studied over a 7-year period starting in late adolescence.
Results revealed a notable sex difference: Arterial stiffness increased the risk for metabolic syndrome by 9% for males but only by 1% for females. Males were also five times more likely than females to have metabolic syndrome.
“It seems metabolic syndrome has a new risk factor we haven’t thought about,” said author Andrew O. Agbaje, MD, clinical epidemiologist and researcher, University of Eastern Finland, Kuopio.
Arterial stiffness previously was associated with metabolic syndrome in numerous studies. But the new work is the first to find evidence for causality, Dr. Agbaje said in an interview.
“Interventions have focused on addressing the components of metabolic syndrome such as obesity, dyslipidemia, hyperglycemia, and hypertension,” Dr. Agbaje said. “But arterial stiffness may independently cause metabolic syndrome in 1 out of 10 male teens. I encourage clinicians to think about its role in preventing and managing metabolic syndrome, not just as a consequence but as a cause.”
The results have important implications for physicians, according to Sissi Cossio, MD, pediatric endocrinologist, Pediatrix Medical Group, Fort Lauderdale, Fla.
“The fact that arterial stiffness progression preceded metabolic syndrome is important because it could be used as an earlier detection marker of disease,” Dr. Cossio said.
To conduct the study, Dr. Agbaje and his research team used data collected by the Avon Longitudinal Study of Parents and Children at the University of Bristol in England. Arterial stiffness was measured using carotid-femoral pulse wave velocity, the speed of blood flow from the upper to the lower aorta. They assessed for metabolic syndrome by the presence of three or more risk factors, including high cholesterol, high triglycerides, and high trunk fat mass.
Participants were studied starting in gestation in the early 1990s, and were measured for arterial stiffness and metabolic syndrome starting at age 17 through age 24.
The overall risk for metabolic syndrome doubled within the 7-year study period of follow-up between 2009 and 2017, indicating that early intervention during adolescence is essential.
Dr. Agbaje recommended that physicians start treating arterial stiffness and other markers of metabolic syndrome as early as possible, noting that, “potentially irreversible cardiovascular health damage might occur after age 17.”
Arterial stiffness can be negated through physical activity and dietary changes that lower inflammation. Physicians should refer at-risk teens to a preventative clinic where they can be monitored and receive repeated measurements of arterial stiffness, lipid levels, blood pressure, glucose levels, and obesity every 3 months, Dr. Agbaje said.
“The health progress made after a year would be an indicator for physicians whether a more aggressive therapeutic approach is needed since it takes about 7 years for the risk of metabolic syndrome attributed to arterial stiffness to worsen remarkably in the young population,” he said.
Dr. Agbaje pointed to a few potential pathways through which arterial stiffness might create a disease cascade. Stiffer arteries disrupt blood flow to the liver and pancreas, which could adversely affect their functioning, he said. Damage to these organs may increase insulin and LDL cholesterol blood levels, increasing the risk for metabolic syndrome.
Arterial stiffness also can lead to higher blood pressure and insulin resistance, potentially inducing musculogenesis and vasculogenesis. The resulting excessive muscle mass may also increase the risk for the condition, he said.
Dr. Cossio acknowledged that treatments for metabolic syndrome become less effective with age, but emphasized that reversal is possible in adults with lifestyle changes and medications.
“Early detection will give patients the best chance at reversing the disease, and [primary care physicians] are a key factor in this process,” she said.
Dr. Cossio said that at-risk teens should receive treatment in a weight loss or endocrinology clinic. Treatment may include behavioral, surgical, and pharmacotherapeutic interventions.
“Teens with signs of insulin resistance and impaired fasting glucose, acanthosis, or prediabetes, should start metformin as the first line of therapy,” Dr. Cossio said.
For weight management, she recommends antiobesity medications such as liraglutide, semaglutide, and the combination of phentermine/topiramate in children aged 12 years or older. In teenagers 16 years or older, phentermine alone is another option.
The research group that conducted the study reported received funding from the Jenny and Antti Wihuri Foundation, the North Savo Regional Fund and Central Finnish Cultural Foundation, the Aarne Koskelo Foundation, the Foundation for Pediatric Research, and the Finnish Foundation for Cardiovascular Research, among others. The authors declared no conflicts of interest, financial or otherwise.
A version of this article appeared on Medscape.com.
New research published in the American Journal of Physiology found that arterial stiffness occurred before the presence of metabolic syndrome. A progressive rise in stiffness was associated with a cumulative increase in risk for the condition among the 3,862 people studied over a 7-year period starting in late adolescence.
Results revealed a notable sex difference: Arterial stiffness increased the risk for metabolic syndrome by 9% for males but only by 1% for females. Males were also five times more likely than females to have metabolic syndrome.
“It seems metabolic syndrome has a new risk factor we haven’t thought about,” said author Andrew O. Agbaje, MD, clinical epidemiologist and researcher, University of Eastern Finland, Kuopio.
Arterial stiffness previously was associated with metabolic syndrome in numerous studies. But the new work is the first to find evidence for causality, Dr. Agbaje said in an interview.
“Interventions have focused on addressing the components of metabolic syndrome such as obesity, dyslipidemia, hyperglycemia, and hypertension,” Dr. Agbaje said. “But arterial stiffness may independently cause metabolic syndrome in 1 out of 10 male teens. I encourage clinicians to think about its role in preventing and managing metabolic syndrome, not just as a consequence but as a cause.”
The results have important implications for physicians, according to Sissi Cossio, MD, pediatric endocrinologist, Pediatrix Medical Group, Fort Lauderdale, Fla.
“The fact that arterial stiffness progression preceded metabolic syndrome is important because it could be used as an earlier detection marker of disease,” Dr. Cossio said.
To conduct the study, Dr. Agbaje and his research team used data collected by the Avon Longitudinal Study of Parents and Children at the University of Bristol in England. Arterial stiffness was measured using carotid-femoral pulse wave velocity, the speed of blood flow from the upper to the lower aorta. They assessed for metabolic syndrome by the presence of three or more risk factors, including high cholesterol, high triglycerides, and high trunk fat mass.
Participants were studied starting in gestation in the early 1990s, and were measured for arterial stiffness and metabolic syndrome starting at age 17 through age 24.
The overall risk for metabolic syndrome doubled within the 7-year study period of follow-up between 2009 and 2017, indicating that early intervention during adolescence is essential.
Dr. Agbaje recommended that physicians start treating arterial stiffness and other markers of metabolic syndrome as early as possible, noting that, “potentially irreversible cardiovascular health damage might occur after age 17.”
Arterial stiffness can be negated through physical activity and dietary changes that lower inflammation. Physicians should refer at-risk teens to a preventative clinic where they can be monitored and receive repeated measurements of arterial stiffness, lipid levels, blood pressure, glucose levels, and obesity every 3 months, Dr. Agbaje said.
“The health progress made after a year would be an indicator for physicians whether a more aggressive therapeutic approach is needed since it takes about 7 years for the risk of metabolic syndrome attributed to arterial stiffness to worsen remarkably in the young population,” he said.
Dr. Agbaje pointed to a few potential pathways through which arterial stiffness might create a disease cascade. Stiffer arteries disrupt blood flow to the liver and pancreas, which could adversely affect their functioning, he said. Damage to these organs may increase insulin and LDL cholesterol blood levels, increasing the risk for metabolic syndrome.
Arterial stiffness also can lead to higher blood pressure and insulin resistance, potentially inducing musculogenesis and vasculogenesis. The resulting excessive muscle mass may also increase the risk for the condition, he said.
Dr. Cossio acknowledged that treatments for metabolic syndrome become less effective with age, but emphasized that reversal is possible in adults with lifestyle changes and medications.
“Early detection will give patients the best chance at reversing the disease, and [primary care physicians] are a key factor in this process,” she said.
Dr. Cossio said that at-risk teens should receive treatment in a weight loss or endocrinology clinic. Treatment may include behavioral, surgical, and pharmacotherapeutic interventions.
“Teens with signs of insulin resistance and impaired fasting glucose, acanthosis, or prediabetes, should start metformin as the first line of therapy,” Dr. Cossio said.
For weight management, she recommends antiobesity medications such as liraglutide, semaglutide, and the combination of phentermine/topiramate in children aged 12 years or older. In teenagers 16 years or older, phentermine alone is another option.
The research group that conducted the study reported received funding from the Jenny and Antti Wihuri Foundation, the North Savo Regional Fund and Central Finnish Cultural Foundation, the Aarne Koskelo Foundation, the Foundation for Pediatric Research, and the Finnish Foundation for Cardiovascular Research, among others. The authors declared no conflicts of interest, financial or otherwise.
A version of this article appeared on Medscape.com.
New research published in the American Journal of Physiology found that arterial stiffness occurred before the presence of metabolic syndrome. A progressive rise in stiffness was associated with a cumulative increase in risk for the condition among the 3,862 people studied over a 7-year period starting in late adolescence.
Results revealed a notable sex difference: Arterial stiffness increased the risk for metabolic syndrome by 9% for males but only by 1% for females. Males were also five times more likely than females to have metabolic syndrome.
“It seems metabolic syndrome has a new risk factor we haven’t thought about,” said author Andrew O. Agbaje, MD, clinical epidemiologist and researcher, University of Eastern Finland, Kuopio.
Arterial stiffness previously was associated with metabolic syndrome in numerous studies. But the new work is the first to find evidence for causality, Dr. Agbaje said in an interview.
“Interventions have focused on addressing the components of metabolic syndrome such as obesity, dyslipidemia, hyperglycemia, and hypertension,” Dr. Agbaje said. “But arterial stiffness may independently cause metabolic syndrome in 1 out of 10 male teens. I encourage clinicians to think about its role in preventing and managing metabolic syndrome, not just as a consequence but as a cause.”
The results have important implications for physicians, according to Sissi Cossio, MD, pediatric endocrinologist, Pediatrix Medical Group, Fort Lauderdale, Fla.
“The fact that arterial stiffness progression preceded metabolic syndrome is important because it could be used as an earlier detection marker of disease,” Dr. Cossio said.
To conduct the study, Dr. Agbaje and his research team used data collected by the Avon Longitudinal Study of Parents and Children at the University of Bristol in England. Arterial stiffness was measured using carotid-femoral pulse wave velocity, the speed of blood flow from the upper to the lower aorta. They assessed for metabolic syndrome by the presence of three or more risk factors, including high cholesterol, high triglycerides, and high trunk fat mass.
Participants were studied starting in gestation in the early 1990s, and were measured for arterial stiffness and metabolic syndrome starting at age 17 through age 24.
The overall risk for metabolic syndrome doubled within the 7-year study period of follow-up between 2009 and 2017, indicating that early intervention during adolescence is essential.
Dr. Agbaje recommended that physicians start treating arterial stiffness and other markers of metabolic syndrome as early as possible, noting that, “potentially irreversible cardiovascular health damage might occur after age 17.”
Arterial stiffness can be negated through physical activity and dietary changes that lower inflammation. Physicians should refer at-risk teens to a preventative clinic where they can be monitored and receive repeated measurements of arterial stiffness, lipid levels, blood pressure, glucose levels, and obesity every 3 months, Dr. Agbaje said.
“The health progress made after a year would be an indicator for physicians whether a more aggressive therapeutic approach is needed since it takes about 7 years for the risk of metabolic syndrome attributed to arterial stiffness to worsen remarkably in the young population,” he said.
Dr. Agbaje pointed to a few potential pathways through which arterial stiffness might create a disease cascade. Stiffer arteries disrupt blood flow to the liver and pancreas, which could adversely affect their functioning, he said. Damage to these organs may increase insulin and LDL cholesterol blood levels, increasing the risk for metabolic syndrome.
Arterial stiffness also can lead to higher blood pressure and insulin resistance, potentially inducing musculogenesis and vasculogenesis. The resulting excessive muscle mass may also increase the risk for the condition, he said.
Dr. Cossio acknowledged that treatments for metabolic syndrome become less effective with age, but emphasized that reversal is possible in adults with lifestyle changes and medications.
“Early detection will give patients the best chance at reversing the disease, and [primary care physicians] are a key factor in this process,” she said.
Dr. Cossio said that at-risk teens should receive treatment in a weight loss or endocrinology clinic. Treatment may include behavioral, surgical, and pharmacotherapeutic interventions.
“Teens with signs of insulin resistance and impaired fasting glucose, acanthosis, or prediabetes, should start metformin as the first line of therapy,” Dr. Cossio said.
For weight management, she recommends antiobesity medications such as liraglutide, semaglutide, and the combination of phentermine/topiramate in children aged 12 years or older. In teenagers 16 years or older, phentermine alone is another option.
The research group that conducted the study reported received funding from the Jenny and Antti Wihuri Foundation, the North Savo Regional Fund and Central Finnish Cultural Foundation, the Aarne Koskelo Foundation, the Foundation for Pediatric Research, and the Finnish Foundation for Cardiovascular Research, among others. The authors declared no conflicts of interest, financial or otherwise.
A version of this article appeared on Medscape.com.
FROM AMERICAN JOURNAL OF PHYSIOLOGY