User login
Hematology analyzer cleared for use in US

Photo by William Weinert
The US Food and Drug Administration has granted 510(k) clearance for the BC-5390 Hematology Analyzer.
The product is designed to meet the testing needs of mid-volume hematology laboratories but offers features commonly found on large-volume analyzers.
The BC-5390 Hematology Analyzer provides a complete blood count with 21 parameters and a 5-part differential from a venous or capillary blood sample.
The product’s built-in autoloader has a 40-sample capacity, but it processes up to 60 samples per hour and stores up to 100,000 results with histograms.
The BC-5390 Hematology Analyzer’s barcode reader and optional laboratory information system connectivity enables seamless sample data transmission.
And nearly all scheduled maintenance procedures are automated by touch buttons.
The BC-5390 Hematology Analyzer is manufactured by Mindray, and MedTest will be the primary distributor of the analyzer in the US.
“We are excited to launch the BC-5390 Hematology Analyzer into the United States laboratory market,” said Caroline Li, general manager of Mindray IVD North America.
“The commercialization of the BC-5390 Hematology Analyzer in the US represents the first analyzer with a 5-part differential from Mindray.” ![]()

Photo by William Weinert
The US Food and Drug Administration has granted 510(k) clearance for the BC-5390 Hematology Analyzer.
The product is designed to meet the testing needs of mid-volume hematology laboratories but offers features commonly found on large-volume analyzers.
The BC-5390 Hematology Analyzer provides a complete blood count with 21 parameters and a 5-part differential from a venous or capillary blood sample.
The product’s built-in autoloader has a 40-sample capacity, but it processes up to 60 samples per hour and stores up to 100,000 results with histograms.
The BC-5390 Hematology Analyzer’s barcode reader and optional laboratory information system connectivity enables seamless sample data transmission.
And nearly all scheduled maintenance procedures are automated by touch buttons.
The BC-5390 Hematology Analyzer is manufactured by Mindray, and MedTest will be the primary distributor of the analyzer in the US.
“We are excited to launch the BC-5390 Hematology Analyzer into the United States laboratory market,” said Caroline Li, general manager of Mindray IVD North America.
“The commercialization of the BC-5390 Hematology Analyzer in the US represents the first analyzer with a 5-part differential from Mindray.” ![]()

Photo by William Weinert
The US Food and Drug Administration has granted 510(k) clearance for the BC-5390 Hematology Analyzer.
The product is designed to meet the testing needs of mid-volume hematology laboratories but offers features commonly found on large-volume analyzers.
The BC-5390 Hematology Analyzer provides a complete blood count with 21 parameters and a 5-part differential from a venous or capillary blood sample.
The product’s built-in autoloader has a 40-sample capacity, but it processes up to 60 samples per hour and stores up to 100,000 results with histograms.
The BC-5390 Hematology Analyzer’s barcode reader and optional laboratory information system connectivity enables seamless sample data transmission.
And nearly all scheduled maintenance procedures are automated by touch buttons.
The BC-5390 Hematology Analyzer is manufactured by Mindray, and MedTest will be the primary distributor of the analyzer in the US.
“We are excited to launch the BC-5390 Hematology Analyzer into the United States laboratory market,” said Caroline Li, general manager of Mindray IVD North America.
“The commercialization of the BC-5390 Hematology Analyzer in the US represents the first analyzer with a 5-part differential from Mindray.” ![]()
SpHb monitoring may reduce use of RBC transfusion

Photo by Elisa Amendola
HONG KONG—Continuous and noninvasive hemoglobin monitoring may reduce the excessive use of intraoperative red blood cell (RBC) transfusion, according to researchers.
The team conducted a retrospective study of patients who received intraoperative RBC transfusions at a single institution, comparing patients who had noninvasive and continuous monitoring of hemoglobin concentrations by spectrophotometry (SpHb) to those who did not.
The results showed a significantly lower mean RBC transfusion volume per 1 g of blood loss in the SpHb group than in the control group.
The researchers presented these findings at the 16th World Congress of Anaesthesiologists (abstract PR607).
The study included 371 patients who received intraoperative RBC transfusions between 2012 and 2014 at Fukushima Medical University in Japan.
The researchers compared 94 patients who had SpHb with the Radical-7® Pulse CO-Oximeter (a product of Masimo) to 277 patients who did not.
The team noted that measured SpHb values are similar to the Hb concentration values obtained by blood sampling, and the procedure allows for continuous monitoring of changes in SpHb levels over time.
The median blood loss during surgery was 1160 g in the SpHb group and 900 g in the control group.
There was no significant difference in the average RBC transfusion volume between the SpHb group and the control group—815 ± 819 mL and 785 ± 773 mL, respectively (P=0.75).
Likewise, there was no significant difference in the preoperative hemoglobin concentration in the SpHb group and the control group—10.4 ± 1.9 g/dL and 10.2 ± 2.4 g/dL, respectively (P=0.27).
However, the researchers did find that patients in the SpHb group had a significantly lower mean RBC transfusion volume per 1 g of blood loss when compared to controls—0.9 ± 1.0 mL/g blood loss and 2.4 ± 5.9 mL/g blood loss, respectively (P<0.01).
“This is the third study, published by different researchers on 3 continents (US1, Egypt2, and now Japan) that has shown that, in addition to other clinical tools, SpHb may be used to help clinicians make informed transfusion decisions during different types of surgery,” said Steven Barker, MD, PhD, chief science officer of Masimo.
Though Masimo’s Radical-7® Pulse CO-Oximeter was used in this study, the researchers declared no conflicts of interest. ![]()

Photo by Elisa Amendola
HONG KONG—Continuous and noninvasive hemoglobin monitoring may reduce the excessive use of intraoperative red blood cell (RBC) transfusion, according to researchers.
The team conducted a retrospective study of patients who received intraoperative RBC transfusions at a single institution, comparing patients who had noninvasive and continuous monitoring of hemoglobin concentrations by spectrophotometry (SpHb) to those who did not.
The results showed a significantly lower mean RBC transfusion volume per 1 g of blood loss in the SpHb group than in the control group.
The researchers presented these findings at the 16th World Congress of Anaesthesiologists (abstract PR607).
The study included 371 patients who received intraoperative RBC transfusions between 2012 and 2014 at Fukushima Medical University in Japan.
The researchers compared 94 patients who had SpHb with the Radical-7® Pulse CO-Oximeter (a product of Masimo) to 277 patients who did not.
The team noted that measured SpHb values are similar to the Hb concentration values obtained by blood sampling, and the procedure allows for continuous monitoring of changes in SpHb levels over time.
The median blood loss during surgery was 1160 g in the SpHb group and 900 g in the control group.
There was no significant difference in the average RBC transfusion volume between the SpHb group and the control group—815 ± 819 mL and 785 ± 773 mL, respectively (P=0.75).
Likewise, there was no significant difference in the preoperative hemoglobin concentration in the SpHb group and the control group—10.4 ± 1.9 g/dL and 10.2 ± 2.4 g/dL, respectively (P=0.27).
However, the researchers did find that patients in the SpHb group had a significantly lower mean RBC transfusion volume per 1 g of blood loss when compared to controls—0.9 ± 1.0 mL/g blood loss and 2.4 ± 5.9 mL/g blood loss, respectively (P<0.01).
“This is the third study, published by different researchers on 3 continents (US1, Egypt2, and now Japan) that has shown that, in addition to other clinical tools, SpHb may be used to help clinicians make informed transfusion decisions during different types of surgery,” said Steven Barker, MD, PhD, chief science officer of Masimo.
Though Masimo’s Radical-7® Pulse CO-Oximeter was used in this study, the researchers declared no conflicts of interest. ![]()

Photo by Elisa Amendola
HONG KONG—Continuous and noninvasive hemoglobin monitoring may reduce the excessive use of intraoperative red blood cell (RBC) transfusion, according to researchers.
The team conducted a retrospective study of patients who received intraoperative RBC transfusions at a single institution, comparing patients who had noninvasive and continuous monitoring of hemoglobin concentrations by spectrophotometry (SpHb) to those who did not.
The results showed a significantly lower mean RBC transfusion volume per 1 g of blood loss in the SpHb group than in the control group.
The researchers presented these findings at the 16th World Congress of Anaesthesiologists (abstract PR607).
The study included 371 patients who received intraoperative RBC transfusions between 2012 and 2014 at Fukushima Medical University in Japan.
The researchers compared 94 patients who had SpHb with the Radical-7® Pulse CO-Oximeter (a product of Masimo) to 277 patients who did not.
The team noted that measured SpHb values are similar to the Hb concentration values obtained by blood sampling, and the procedure allows for continuous monitoring of changes in SpHb levels over time.
The median blood loss during surgery was 1160 g in the SpHb group and 900 g in the control group.
There was no significant difference in the average RBC transfusion volume between the SpHb group and the control group—815 ± 819 mL and 785 ± 773 mL, respectively (P=0.75).
Likewise, there was no significant difference in the preoperative hemoglobin concentration in the SpHb group and the control group—10.4 ± 1.9 g/dL and 10.2 ± 2.4 g/dL, respectively (P=0.27).
However, the researchers did find that patients in the SpHb group had a significantly lower mean RBC transfusion volume per 1 g of blood loss when compared to controls—0.9 ± 1.0 mL/g blood loss and 2.4 ± 5.9 mL/g blood loss, respectively (P<0.01).
“This is the third study, published by different researchers on 3 continents (US1, Egypt2, and now Japan) that has shown that, in addition to other clinical tools, SpHb may be used to help clinicians make informed transfusion decisions during different types of surgery,” said Steven Barker, MD, PhD, chief science officer of Masimo.
Though Masimo’s Radical-7® Pulse CO-Oximeter was used in this study, the researchers declared no conflicts of interest. ![]()
Blood sample collection, storage impacts protein levels

Photo by Graham Colm
Factors related to blood sample collection and storage can have a substantial impact on the biomolecular composition of the sample, according to research published in EBioMedicine.
The study showed that freezer storage time and the month and season during which a blood sample is collected can affect protein concentrations.
In fact, researchers said these factors should be considered covariates of the same importance as the sample provider’s age or gender.
“This discovery will change the way the entire world works with biobank blood,” said study author Stefan Enroth, PhD, of Uppsala University in Sweden.
“All research on, and analysis of, biobank blood going forward should also take into account what we have discovered—namely, the time aspect. It is completely new.”
As part of their research on uterine cancer, Dr Enroth and his colleagues looked at plasma samples collected from 1988 to 2014. There were 380 samples from 106 women between the ages of 29 and 73.
The researchers looked at the duration of sample storage, the women’s chronological age at sample collection, and the season and month of the year the sample was collected, assessing the impact of these factors on the abundance levels of 108 proteins.
When studying the impact of storage time, the researchers used only samples from 50-year-old women in order to isolate the time effect. The team found that storage time affected 18 proteins and explained 4.8% to 34.9% of the variance observed.
The women’s chronological age at the time of sample collection, after the adjustment for storage time, affected 70 proteins and explained 1.1% to 33.5% of the variance.
“We suspected that we’d find an influence from storage time, but we thought it would be much less,” said study author Ulf Gyllensten, PhD, of Uppsala University.
“It has now been demonstrated that storage time can be a factor at least as important as the age of the individual at sampling.”
The other major finding of the study is that protein levels vary depending on the season or month in which the samples were taken.
The researchers said results in the month analysis corresponded with the seasonal analysis, so they hypothesized that sunlight hours at the time of sampling could explain some of the variance they observed in plasma protein abundance levels.
The team found the number of sunlight hours affected 36 proteins and explained up to 4.5% of the variance observed after adjusting for storage time and age.
The researchers said these results suggest that information on the sample handling history should be regarded as “equally prominent covariates” as age or gender. Therefore, the information should be included in epidemiological studies involving protein levels. ![]()

Photo by Graham Colm
Factors related to blood sample collection and storage can have a substantial impact on the biomolecular composition of the sample, according to research published in EBioMedicine.
The study showed that freezer storage time and the month and season during which a blood sample is collected can affect protein concentrations.
In fact, researchers said these factors should be considered covariates of the same importance as the sample provider’s age or gender.
“This discovery will change the way the entire world works with biobank blood,” said study author Stefan Enroth, PhD, of Uppsala University in Sweden.
“All research on, and analysis of, biobank blood going forward should also take into account what we have discovered—namely, the time aspect. It is completely new.”
As part of their research on uterine cancer, Dr Enroth and his colleagues looked at plasma samples collected from 1988 to 2014. There were 380 samples from 106 women between the ages of 29 and 73.
The researchers looked at the duration of sample storage, the women’s chronological age at sample collection, and the season and month of the year the sample was collected, assessing the impact of these factors on the abundance levels of 108 proteins.
When studying the impact of storage time, the researchers used only samples from 50-year-old women in order to isolate the time effect. The team found that storage time affected 18 proteins and explained 4.8% to 34.9% of the variance observed.
The women’s chronological age at the time of sample collection, after the adjustment for storage time, affected 70 proteins and explained 1.1% to 33.5% of the variance.
“We suspected that we’d find an influence from storage time, but we thought it would be much less,” said study author Ulf Gyllensten, PhD, of Uppsala University.
“It has now been demonstrated that storage time can be a factor at least as important as the age of the individual at sampling.”
The other major finding of the study is that protein levels vary depending on the season or month in which the samples were taken.
The researchers said results in the month analysis corresponded with the seasonal analysis, so they hypothesized that sunlight hours at the time of sampling could explain some of the variance they observed in plasma protein abundance levels.
The team found the number of sunlight hours affected 36 proteins and explained up to 4.5% of the variance observed after adjusting for storage time and age.
The researchers said these results suggest that information on the sample handling history should be regarded as “equally prominent covariates” as age or gender. Therefore, the information should be included in epidemiological studies involving protein levels. ![]()

Photo by Graham Colm
Factors related to blood sample collection and storage can have a substantial impact on the biomolecular composition of the sample, according to research published in EBioMedicine.
The study showed that freezer storage time and the month and season during which a blood sample is collected can affect protein concentrations.
In fact, researchers said these factors should be considered covariates of the same importance as the sample provider’s age or gender.
“This discovery will change the way the entire world works with biobank blood,” said study author Stefan Enroth, PhD, of Uppsala University in Sweden.
“All research on, and analysis of, biobank blood going forward should also take into account what we have discovered—namely, the time aspect. It is completely new.”
As part of their research on uterine cancer, Dr Enroth and his colleagues looked at plasma samples collected from 1988 to 2014. There were 380 samples from 106 women between the ages of 29 and 73.
The researchers looked at the duration of sample storage, the women’s chronological age at sample collection, and the season and month of the year the sample was collected, assessing the impact of these factors on the abundance levels of 108 proteins.
When studying the impact of storage time, the researchers used only samples from 50-year-old women in order to isolate the time effect. The team found that storage time affected 18 proteins and explained 4.8% to 34.9% of the variance observed.
The women’s chronological age at the time of sample collection, after the adjustment for storage time, affected 70 proteins and explained 1.1% to 33.5% of the variance.
“We suspected that we’d find an influence from storage time, but we thought it would be much less,” said study author Ulf Gyllensten, PhD, of Uppsala University.
“It has now been demonstrated that storage time can be a factor at least as important as the age of the individual at sampling.”
The other major finding of the study is that protein levels vary depending on the season or month in which the samples were taken.
The researchers said results in the month analysis corresponded with the seasonal analysis, so they hypothesized that sunlight hours at the time of sampling could explain some of the variance they observed in plasma protein abundance levels.
The team found the number of sunlight hours affected 36 proteins and explained up to 4.5% of the variance observed after adjusting for storage time and age.
The researchers said these results suggest that information on the sample handling history should be regarded as “equally prominent covariates” as age or gender. Therefore, the information should be included in epidemiological studies involving protein levels. ![]()
Study may explain why blood type affects cholera severity

Photo by Daniel Gay
Results of preclinical research may explain why people with blood type O often get more severely ill from cholera than people with other blood types.
The study suggests that, in people with blood type O, cholera toxin hyperactivates a key signaling molecule in intestinal cells.
And high levels of that molecule, cyclic adenosine monophosphate (cAMP), lead to excretion of electrolytes and water—in other words, diarrhea.
“We have shown that blood type influences how strongly cholera toxin activates intestinal cells, leading to diarrhea,” said study author James Fleckenstein, MD, of Washington University School of Medicine in Saint Louis, Missouri.
Dr Fleckenstein and his colleagues reported these findings in The American Journal of Tropical Medicine and Hygiene.
Cholera is caused by Vibrio cholerae, a bacterium that infects cells of the small intestine.
Epidemiologists first noticed 4 decades ago that people with blood type O were more likely to be hospitalized for cholera than people with other blood types, but the reasons for the difference had never been determined.
Although the blood group antigens—A, B, AB, and O—are best known for their presence on red blood cells, they also are found on the surface of many other cell types, including the cells that line the intestine.
To find out what effect cholera toxin has on intestinal cells carrying different blood group antigens, Dr Fleckenstein and his colleagues used clusters of intestinal epithelial stem cells, called enteroids, that can be grown in the lab and differentiated into mature intestinal cells.
The researchers treated 4 groups of enteroids with cholera toxin—2 derived from people with blood type A and 2 from people with blood type O—and measured the amount of cAMP inside the cells. Enteroids from the other 2 blood types—B and AB—were not available at the time the study was done.
The researchers found that levels of cAMP were roughly twice as high in the cells with the type O antigen than in the cells with type A antigen, suggesting that people with type O antigen who were exposed to cholera toxin would suffer more severe diarrhea.
“It is well-established that high levels of this molecule lead to diarrhea, so we’re making the assumption that higher levels lead to even more diarrhea,” said study author F. Matthew Kuhlmann, MD, of Washington University School of Medicine.
“Unfortunately, we have no way directly to link the responses to the volume of diarrhea and, therefore, the severity of disease.”
The researchers confirmed their enteroid results in an intestinal cell line originally derived from a person with blood type A. The cell line was modified to produce the type O antigen instead.
The team found that cholera toxin induced roughly double the amount of cAMP in cells with type O antigen than in those with type A.
Dr Fleckenstein said the researchers are not sure why cholera toxin induces different responses in cells with different blood group antigens on their surfaces.
“The cholera toxin is known to bind weakly to the ABO antigens, so they may be acting as decoys to draw the toxin away from its true target,” Dr Fleckenstein said. “It may be that the type O antigen just isn’t as good of a decoy as the type A antigen.” ![]()

Photo by Daniel Gay
Results of preclinical research may explain why people with blood type O often get more severely ill from cholera than people with other blood types.
The study suggests that, in people with blood type O, cholera toxin hyperactivates a key signaling molecule in intestinal cells.
And high levels of that molecule, cyclic adenosine monophosphate (cAMP), lead to excretion of electrolytes and water—in other words, diarrhea.
“We have shown that blood type influences how strongly cholera toxin activates intestinal cells, leading to diarrhea,” said study author James Fleckenstein, MD, of Washington University School of Medicine in Saint Louis, Missouri.
Dr Fleckenstein and his colleagues reported these findings in The American Journal of Tropical Medicine and Hygiene.
Cholera is caused by Vibrio cholerae, a bacterium that infects cells of the small intestine.
Epidemiologists first noticed 4 decades ago that people with blood type O were more likely to be hospitalized for cholera than people with other blood types, but the reasons for the difference had never been determined.
Although the blood group antigens—A, B, AB, and O—are best known for their presence on red blood cells, they also are found on the surface of many other cell types, including the cells that line the intestine.
To find out what effect cholera toxin has on intestinal cells carrying different blood group antigens, Dr Fleckenstein and his colleagues used clusters of intestinal epithelial stem cells, called enteroids, that can be grown in the lab and differentiated into mature intestinal cells.
The researchers treated 4 groups of enteroids with cholera toxin—2 derived from people with blood type A and 2 from people with blood type O—and measured the amount of cAMP inside the cells. Enteroids from the other 2 blood types—B and AB—were not available at the time the study was done.
The researchers found that levels of cAMP were roughly twice as high in the cells with the type O antigen than in the cells with type A antigen, suggesting that people with type O antigen who were exposed to cholera toxin would suffer more severe diarrhea.
“It is well-established that high levels of this molecule lead to diarrhea, so we’re making the assumption that higher levels lead to even more diarrhea,” said study author F. Matthew Kuhlmann, MD, of Washington University School of Medicine.
“Unfortunately, we have no way directly to link the responses to the volume of diarrhea and, therefore, the severity of disease.”
The researchers confirmed their enteroid results in an intestinal cell line originally derived from a person with blood type A. The cell line was modified to produce the type O antigen instead.
The team found that cholera toxin induced roughly double the amount of cAMP in cells with type O antigen than in those with type A.
Dr Fleckenstein said the researchers are not sure why cholera toxin induces different responses in cells with different blood group antigens on their surfaces.
“The cholera toxin is known to bind weakly to the ABO antigens, so they may be acting as decoys to draw the toxin away from its true target,” Dr Fleckenstein said. “It may be that the type O antigen just isn’t as good of a decoy as the type A antigen.” ![]()

Photo by Daniel Gay
Results of preclinical research may explain why people with blood type O often get more severely ill from cholera than people with other blood types.
The study suggests that, in people with blood type O, cholera toxin hyperactivates a key signaling molecule in intestinal cells.
And high levels of that molecule, cyclic adenosine monophosphate (cAMP), lead to excretion of electrolytes and water—in other words, diarrhea.
“We have shown that blood type influences how strongly cholera toxin activates intestinal cells, leading to diarrhea,” said study author James Fleckenstein, MD, of Washington University School of Medicine in Saint Louis, Missouri.
Dr Fleckenstein and his colleagues reported these findings in The American Journal of Tropical Medicine and Hygiene.
Cholera is caused by Vibrio cholerae, a bacterium that infects cells of the small intestine.
Epidemiologists first noticed 4 decades ago that people with blood type O were more likely to be hospitalized for cholera than people with other blood types, but the reasons for the difference had never been determined.
Although the blood group antigens—A, B, AB, and O—are best known for their presence on red blood cells, they also are found on the surface of many other cell types, including the cells that line the intestine.
To find out what effect cholera toxin has on intestinal cells carrying different blood group antigens, Dr Fleckenstein and his colleagues used clusters of intestinal epithelial stem cells, called enteroids, that can be grown in the lab and differentiated into mature intestinal cells.
The researchers treated 4 groups of enteroids with cholera toxin—2 derived from people with blood type A and 2 from people with blood type O—and measured the amount of cAMP inside the cells. Enteroids from the other 2 blood types—B and AB—were not available at the time the study was done.
The researchers found that levels of cAMP were roughly twice as high in the cells with the type O antigen than in the cells with type A antigen, suggesting that people with type O antigen who were exposed to cholera toxin would suffer more severe diarrhea.
“It is well-established that high levels of this molecule lead to diarrhea, so we’re making the assumption that higher levels lead to even more diarrhea,” said study author F. Matthew Kuhlmann, MD, of Washington University School of Medicine.
“Unfortunately, we have no way directly to link the responses to the volume of diarrhea and, therefore, the severity of disease.”
The researchers confirmed their enteroid results in an intestinal cell line originally derived from a person with blood type A. The cell line was modified to produce the type O antigen instead.
The team found that cholera toxin induced roughly double the amount of cAMP in cells with type O antigen than in those with type A.
Dr Fleckenstein said the researchers are not sure why cholera toxin induces different responses in cells with different blood group antigens on their surfaces.
“The cholera toxin is known to bind weakly to the ABO antigens, so they may be acting as decoys to draw the toxin away from its true target,” Dr Fleckenstein said. “It may be that the type O antigen just isn’t as good of a decoy as the type A antigen.” ![]()
FDA advises testing all donated blood for Zika virus

The US Food and Drug Administration (FDA) has issued a revised guidance intended to reduce the risk of Zika virus transmission via blood.
The guidance recommends that all states and US territories screen donated whole blood and blood components for the Zika virus with a test authorized under an investigational new drug application or a licensed test when available.
For plasma and certain platelet products, an FDA-approved pathogen-reduction device can be used instead of a screening test.
“There is still much uncertainty regarding the nature and extent of Zika virus transmission,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
“At this time, the recommendation for testing the entire blood supply will help ensure that safe blood is available for all individuals who might need transfusion.”
In February, the FDA issued a guidance recommending that areas with active Zika virus transmission screen donated whole blood and blood components for the Zika virus, use pathogen-reduction devices, or halt blood collection and obtain blood from areas of the US without active virus transmission.
The FDA decided to update its guidance after considering the available scientific evidence, consulting with other public health agencies, and taking into consideration the potential serious health consequences of Zika virus infection to pregnant women and children born to women exposed to Zika virus during pregnancy.
“As new scientific and epidemiological information regarding Zika virus has become available, it’s clear that additional precautionary measures are necessary,” said Luciana Borio, MD, the FDA’s acting chief scientist.
“We are issuing revised guidance for immediate implementation in order to help maintain the safety of the US blood supply.”
Testing of donated blood is already underway in Florida, Puerto Rico, and other areas, and it has proven effective in identifying donations infected with Zika virus.
The FDA said nationwide testing will be in effect until the risk of Zika virus transmission via transfusion is reduced. ![]()

The US Food and Drug Administration (FDA) has issued a revised guidance intended to reduce the risk of Zika virus transmission via blood.
The guidance recommends that all states and US territories screen donated whole blood and blood components for the Zika virus with a test authorized under an investigational new drug application or a licensed test when available.
For plasma and certain platelet products, an FDA-approved pathogen-reduction device can be used instead of a screening test.
“There is still much uncertainty regarding the nature and extent of Zika virus transmission,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
“At this time, the recommendation for testing the entire blood supply will help ensure that safe blood is available for all individuals who might need transfusion.”
In February, the FDA issued a guidance recommending that areas with active Zika virus transmission screen donated whole blood and blood components for the Zika virus, use pathogen-reduction devices, or halt blood collection and obtain blood from areas of the US without active virus transmission.
The FDA decided to update its guidance after considering the available scientific evidence, consulting with other public health agencies, and taking into consideration the potential serious health consequences of Zika virus infection to pregnant women and children born to women exposed to Zika virus during pregnancy.
“As new scientific and epidemiological information regarding Zika virus has become available, it’s clear that additional precautionary measures are necessary,” said Luciana Borio, MD, the FDA’s acting chief scientist.
“We are issuing revised guidance for immediate implementation in order to help maintain the safety of the US blood supply.”
Testing of donated blood is already underway in Florida, Puerto Rico, and other areas, and it has proven effective in identifying donations infected with Zika virus.
The FDA said nationwide testing will be in effect until the risk of Zika virus transmission via transfusion is reduced. ![]()

The US Food and Drug Administration (FDA) has issued a revised guidance intended to reduce the risk of Zika virus transmission via blood.
The guidance recommends that all states and US territories screen donated whole blood and blood components for the Zika virus with a test authorized under an investigational new drug application or a licensed test when available.
For plasma and certain platelet products, an FDA-approved pathogen-reduction device can be used instead of a screening test.
“There is still much uncertainty regarding the nature and extent of Zika virus transmission,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
“At this time, the recommendation for testing the entire blood supply will help ensure that safe blood is available for all individuals who might need transfusion.”
In February, the FDA issued a guidance recommending that areas with active Zika virus transmission screen donated whole blood and blood components for the Zika virus, use pathogen-reduction devices, or halt blood collection and obtain blood from areas of the US without active virus transmission.
The FDA decided to update its guidance after considering the available scientific evidence, consulting with other public health agencies, and taking into consideration the potential serious health consequences of Zika virus infection to pregnant women and children born to women exposed to Zika virus during pregnancy.
“As new scientific and epidemiological information regarding Zika virus has become available, it’s clear that additional precautionary measures are necessary,” said Luciana Borio, MD, the FDA’s acting chief scientist.
“We are issuing revised guidance for immediate implementation in order to help maintain the safety of the US blood supply.”
Testing of donated blood is already underway in Florida, Puerto Rico, and other areas, and it has proven effective in identifying donations infected with Zika virus.
The FDA said nationwide testing will be in effect until the risk of Zika virus transmission via transfusion is reduced. ![]()
Apparent Zika transmission via platelet transfusion

Photo from Flickr
Researchers have reported 2 cases in which the Zika virus seems to have been transmitted via platelet transfusion.
Brazilian health officials previously announced 2 cases of Zika virus—in a liver transplant recipient and a gunshot victim—that likely resulted from blood transfusions performed in 2015.
Now, researchers have reported possible transmission via transfusion in 2 more Brazilians—a patient with primary myelofibrosis (PMF) and one with acute myeloid leukemia (AML).
The researchers described these cases in a letter to NEJM.
An individual who donated platelets via apheresis on January 16, 2016, later tested positive for the Zika virus.
On January 19, platelets from that donor were transfused into a 54-year-old woman with PMF and a 14-year-old girl with AML who had also received a haploidentical bone marrow transplant on January 6.
The platelet donor called the blood bank on January 21 to report worrying symptoms—a cutaneous rash, retro-orbital pain, and pain in both knees—that had developed on January 18.
Subsequent testing revealed that the donor was negative for chikungunya and dengue virus. However, both plasma and urine samples tested positive for Zika virus.
Pre-transfusion samples collected from both of the recipients were negative for chikungunya, dengue, and Zika. However, samples collected after the transfusions—6 days after for the woman with PMF and 23 to 51 days after for the girl with AML—tested positive for Zika.
Researchers performed molecular sequencing and phylogenetic analysis of Zika virus RNA isolated from the donor and the recipients. Isolates from all 3 parties had nucleotide changes in the envelope gene (codons 11 and 186) that were not observed among other available isolates from Brazil.
The researchers said these results suggest the platelet transfusions were the source of Zika virus infection in the PMF patient and the AML patient.
Although both patients could have been exposed to Zika-carrying mosquitoes, both the RNA results and the timing of Zika infection suggest the transfusions were the cause. ![]()

Photo from Flickr
Researchers have reported 2 cases in which the Zika virus seems to have been transmitted via platelet transfusion.
Brazilian health officials previously announced 2 cases of Zika virus—in a liver transplant recipient and a gunshot victim—that likely resulted from blood transfusions performed in 2015.
Now, researchers have reported possible transmission via transfusion in 2 more Brazilians—a patient with primary myelofibrosis (PMF) and one with acute myeloid leukemia (AML).
The researchers described these cases in a letter to NEJM.
An individual who donated platelets via apheresis on January 16, 2016, later tested positive for the Zika virus.
On January 19, platelets from that donor were transfused into a 54-year-old woman with PMF and a 14-year-old girl with AML who had also received a haploidentical bone marrow transplant on January 6.
The platelet donor called the blood bank on January 21 to report worrying symptoms—a cutaneous rash, retro-orbital pain, and pain in both knees—that had developed on January 18.
Subsequent testing revealed that the donor was negative for chikungunya and dengue virus. However, both plasma and urine samples tested positive for Zika virus.
Pre-transfusion samples collected from both of the recipients were negative for chikungunya, dengue, and Zika. However, samples collected after the transfusions—6 days after for the woman with PMF and 23 to 51 days after for the girl with AML—tested positive for Zika.
Researchers performed molecular sequencing and phylogenetic analysis of Zika virus RNA isolated from the donor and the recipients. Isolates from all 3 parties had nucleotide changes in the envelope gene (codons 11 and 186) that were not observed among other available isolates from Brazil.
The researchers said these results suggest the platelet transfusions were the source of Zika virus infection in the PMF patient and the AML patient.
Although both patients could have been exposed to Zika-carrying mosquitoes, both the RNA results and the timing of Zika infection suggest the transfusions were the cause. ![]()

Photo from Flickr
Researchers have reported 2 cases in which the Zika virus seems to have been transmitted via platelet transfusion.
Brazilian health officials previously announced 2 cases of Zika virus—in a liver transplant recipient and a gunshot victim—that likely resulted from blood transfusions performed in 2015.
Now, researchers have reported possible transmission via transfusion in 2 more Brazilians—a patient with primary myelofibrosis (PMF) and one with acute myeloid leukemia (AML).
The researchers described these cases in a letter to NEJM.
An individual who donated platelets via apheresis on January 16, 2016, later tested positive for the Zika virus.
On January 19, platelets from that donor were transfused into a 54-year-old woman with PMF and a 14-year-old girl with AML who had also received a haploidentical bone marrow transplant on January 6.
The platelet donor called the blood bank on January 21 to report worrying symptoms—a cutaneous rash, retro-orbital pain, and pain in both knees—that had developed on January 18.
Subsequent testing revealed that the donor was negative for chikungunya and dengue virus. However, both plasma and urine samples tested positive for Zika virus.
Pre-transfusion samples collected from both of the recipients were negative for chikungunya, dengue, and Zika. However, samples collected after the transfusions—6 days after for the woman with PMF and 23 to 51 days after for the girl with AML—tested positive for Zika.
Researchers performed molecular sequencing and phylogenetic analysis of Zika virus RNA isolated from the donor and the recipients. Isolates from all 3 parties had nucleotide changes in the envelope gene (codons 11 and 186) that were not observed among other available isolates from Brazil.
The researchers said these results suggest the platelet transfusions were the source of Zika virus infection in the PMF patient and the AML patient.
Although both patients could have been exposed to Zika-carrying mosquitoes, both the RNA results and the timing of Zika infection suggest the transfusions were the cause. ![]()
Drug interferes with testing for blood transfusion

Photo by Daniel Gay
Research has shown that daratumumab, a monoclonal antibody approved to treat multiple myeloma, interferes with routine compatibility testing for blood transfusion.
And this interference can cause delays in providing patients with compatible blood.
Investigators have discovered ways to eliminate or circumvent the interference, but implementing these methods in hospital blood banks may be challenging.
Michael F. Murphy, MD, of John Radcliffe Hospital in Oxford, UK, and his colleagues discussed this issue in a letter to NEJM.
In a phase 1/2 trial of daratumumab, investigators at different study sites observed that the drug consistently interfered with routine blood compatibility testing. This meant that daratumumab-treated patients sometimes experienced delays in receiving blood transfusions.
Investigation revealed that daratumumab in patient plasma directly binds to CD38 on reagent red blood cells used in the blood bank, which causes false-positive antibody screens.
Unfortunately, standard serological methods to eliminate panreactive antibodies did not affect daratumumab’s interference.
However, an investigator-initiated study revealed a dithiothreitol-based method that can eliminate the interference.1
Another method, involving an anti-daratumumab idiotype, also appears effective, though not readily available.2 And a third method is to issue phenotypically or genotypically matched red cell units.3,4
However, establishing these approaches as routine methods in hospital blood banks will be a major challenge, according to Dr Murphy and his colleagues.
The team also said this issue with daratumumab suggests there is a pressing need to investigate whether new drugs interfere with routine blood bank testing.
Investigations should be performed early during drug development. And if interference with compatibility tests is found, it should be brought to the attention of clinicians and blood banks with advice about how to overcome the interference. ![]()

Photo by Daniel Gay
Research has shown that daratumumab, a monoclonal antibody approved to treat multiple myeloma, interferes with routine compatibility testing for blood transfusion.
And this interference can cause delays in providing patients with compatible blood.
Investigators have discovered ways to eliminate or circumvent the interference, but implementing these methods in hospital blood banks may be challenging.
Michael F. Murphy, MD, of John Radcliffe Hospital in Oxford, UK, and his colleagues discussed this issue in a letter to NEJM.
In a phase 1/2 trial of daratumumab, investigators at different study sites observed that the drug consistently interfered with routine blood compatibility testing. This meant that daratumumab-treated patients sometimes experienced delays in receiving blood transfusions.
Investigation revealed that daratumumab in patient plasma directly binds to CD38 on reagent red blood cells used in the blood bank, which causes false-positive antibody screens.
Unfortunately, standard serological methods to eliminate panreactive antibodies did not affect daratumumab’s interference.
However, an investigator-initiated study revealed a dithiothreitol-based method that can eliminate the interference.1
Another method, involving an anti-daratumumab idiotype, also appears effective, though not readily available.2 And a third method is to issue phenotypically or genotypically matched red cell units.3,4
However, establishing these approaches as routine methods in hospital blood banks will be a major challenge, according to Dr Murphy and his colleagues.
The team also said this issue with daratumumab suggests there is a pressing need to investigate whether new drugs interfere with routine blood bank testing.
Investigations should be performed early during drug development. And if interference with compatibility tests is found, it should be brought to the attention of clinicians and blood banks with advice about how to overcome the interference. ![]()

Photo by Daniel Gay
Research has shown that daratumumab, a monoclonal antibody approved to treat multiple myeloma, interferes with routine compatibility testing for blood transfusion.
And this interference can cause delays in providing patients with compatible blood.
Investigators have discovered ways to eliminate or circumvent the interference, but implementing these methods in hospital blood banks may be challenging.
Michael F. Murphy, MD, of John Radcliffe Hospital in Oxford, UK, and his colleagues discussed this issue in a letter to NEJM.
In a phase 1/2 trial of daratumumab, investigators at different study sites observed that the drug consistently interfered with routine blood compatibility testing. This meant that daratumumab-treated patients sometimes experienced delays in receiving blood transfusions.
Investigation revealed that daratumumab in patient plasma directly binds to CD38 on reagent red blood cells used in the blood bank, which causes false-positive antibody screens.
Unfortunately, standard serological methods to eliminate panreactive antibodies did not affect daratumumab’s interference.
However, an investigator-initiated study revealed a dithiothreitol-based method that can eliminate the interference.1
Another method, involving an anti-daratumumab idiotype, also appears effective, though not readily available.2 And a third method is to issue phenotypically or genotypically matched red cell units.3,4
However, establishing these approaches as routine methods in hospital blood banks will be a major challenge, according to Dr Murphy and his colleagues.
The team also said this issue with daratumumab suggests there is a pressing need to investigate whether new drugs interfere with routine blood bank testing.
Investigations should be performed early during drug development. And if interference with compatibility tests is found, it should be brought to the attention of clinicians and blood banks with advice about how to overcome the interference.
How iPSCs differentiate to blood cells

Image from Salk Institute
New research suggests the type of founder cell used to generate induced pluripotent stem cells (iPSCs) does not affect the iPSCs’ ability to differentiate into hematopoietic cells.
Instead, researchers found the expression of certain genes and DNA methylations were better indicators of the efficiency at which a cell line could be differentiated into the hematopoietic lineage.
The team reported these findings in Cell Stem Cell.
The researchers assessed the hematopoietic differentiation capacities of 35 iPSC lines derived from 4 types of somatic tissues—human dermal fibroblasts, hematopoietic cells such as cord blood and peripheral blood, dental pulp cells, and keratinocytes—from 15 donors.
The team also assessed 4 embryonic stem cell lines in early phase and late phase.
The researchers found that hematopoietic commitment capacity was associated with expression of IGF2 in undifferentiated iPSCs, but not with type of founder cell.
Higher expression of IFG2 was indicative of iPSCs initiating their conversion into hematopoietic cells. Even though IFG2 itself is not directly related to hematopoiesis, its uptake corresponded to an increase in the expression of genes that are.
Although IFG2 marked the beginnings of differentiation to hematopoietic lineage, the completion of differentiation was marked by the methylation profiles of the iPSC DNA.
“DNA methylation has an effect on a cell staying pluripotent or differentiating,” explained study author Yoshinori Yoshida, MD, PhD, of the Center for iPS Cell Research and Application at Kyoto University in Japan.
The completion of differentiation correlated with less aberrant methylation during the reprogramming process.
Hematopoietic founder cells showed a much lower propensity for aberrant methylation than did other founder cells, which could explain why, in the past, scientists attributed the founder cell to the effectiveness of differentiating iPSCs to the hematopoietic lineage.
Dr Yoshida and his colleagues said this research revealed molecular factors that can be used to evaluate the differentiation potential of different cell lines, which should expedite the progress of iPSCs to clinical use.

Image from Salk Institute
New research suggests the type of founder cell used to generate induced pluripotent stem cells (iPSCs) does not affect the iPSCs’ ability to differentiate into hematopoietic cells.
Instead, researchers found the expression of certain genes and DNA methylations were better indicators of the efficiency at which a cell line could be differentiated into the hematopoietic lineage.
The team reported these findings in Cell Stem Cell.
The researchers assessed the hematopoietic differentiation capacities of 35 iPSC lines derived from 4 types of somatic tissues—human dermal fibroblasts, hematopoietic cells such as cord blood and peripheral blood, dental pulp cells, and keratinocytes—from 15 donors.
The team also assessed 4 embryonic stem cell lines in early phase and late phase.
The researchers found that hematopoietic commitment capacity was associated with expression of IGF2 in undifferentiated iPSCs, but not with type of founder cell.
Higher expression of IFG2 was indicative of iPSCs initiating their conversion into hematopoietic cells. Even though IFG2 itself is not directly related to hematopoiesis, its uptake corresponded to an increase in the expression of genes that are.
Although IFG2 marked the beginnings of differentiation to hematopoietic lineage, the completion of differentiation was marked by the methylation profiles of the iPSC DNA.
“DNA methylation has an effect on a cell staying pluripotent or differentiating,” explained study author Yoshinori Yoshida, MD, PhD, of the Center for iPS Cell Research and Application at Kyoto University in Japan.
The completion of differentiation correlated with less aberrant methylation during the reprogramming process.
Hematopoietic founder cells showed a much lower propensity for aberrant methylation than did other founder cells, which could explain why, in the past, scientists attributed the founder cell to the effectiveness of differentiating iPSCs to the hematopoietic lineage.
Dr Yoshida and his colleagues said this research revealed molecular factors that can be used to evaluate the differentiation potential of different cell lines, which should expedite the progress of iPSCs to clinical use.

Image from Salk Institute
New research suggests the type of founder cell used to generate induced pluripotent stem cells (iPSCs) does not affect the iPSCs’ ability to differentiate into hematopoietic cells.
Instead, researchers found the expression of certain genes and DNA methylations were better indicators of the efficiency at which a cell line could be differentiated into the hematopoietic lineage.
The team reported these findings in Cell Stem Cell.
The researchers assessed the hematopoietic differentiation capacities of 35 iPSC lines derived from 4 types of somatic tissues—human dermal fibroblasts, hematopoietic cells such as cord blood and peripheral blood, dental pulp cells, and keratinocytes—from 15 donors.
The team also assessed 4 embryonic stem cell lines in early phase and late phase.
The researchers found that hematopoietic commitment capacity was associated with expression of IGF2 in undifferentiated iPSCs, but not with type of founder cell.
Higher expression of IFG2 was indicative of iPSCs initiating their conversion into hematopoietic cells. Even though IFG2 itself is not directly related to hematopoiesis, its uptake corresponded to an increase in the expression of genes that are.
Although IFG2 marked the beginnings of differentiation to hematopoietic lineage, the completion of differentiation was marked by the methylation profiles of the iPSC DNA.
“DNA methylation has an effect on a cell staying pluripotent or differentiating,” explained study author Yoshinori Yoshida, MD, PhD, of the Center for iPS Cell Research and Application at Kyoto University in Japan.
The completion of differentiation correlated with less aberrant methylation during the reprogramming process.
Hematopoietic founder cells showed a much lower propensity for aberrant methylation than did other founder cells, which could explain why, in the past, scientists attributed the founder cell to the effectiveness of differentiating iPSCs to the hematopoietic lineage.
Dr Yoshida and his colleagues said this research revealed molecular factors that can be used to evaluate the differentiation potential of different cell lines, which should expedite the progress of iPSCs to clinical use.
Microneedle system could replace blood draws, team says
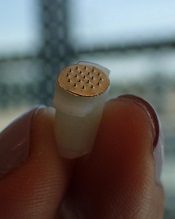
Photo courtesy of
Sahan Ranamukhaarachchi
A new microneedle drug monitoring system could one day replace invasive blood draws, according to researchers.
The system consists of a small, thin patch that is pressed against a patient’s arm during medical treatment and measures drugs in the bloodstream painlessly without drawing any blood.
The tiny projections on this patch resemble hollow cones and don’t pierce the skin like a standard hypodermic needle.
The researchers described this system in Scientific Reports.
“Many groups are researching microneedle technology for painless vaccines and drug delivery,” said study author Sahan Ranamukhaarachchi, a PhD student at the University of British Columbia (UBC) in Vancouver, British Columbia, Canada. “Using them to painlessly monitor drugs is a newer idea.”
The microneedle system Ranamukhaarachchi and his colleagues created was developed to monitor the antibiotic vancomycin. Patients taking vancomycin must be closely monitored because the drug can cause life-threatening side effects, so the patients undergo 3 to 4 blood draws per day.
The researchers discovered they could use fluid found just below the outer layer of skin, instead of blood, to monitor levels of vancomycin in the bloodstream.
The microneedle patch collects a tiny amount of the fluid, less than 1 nL, and a reaction occurs on the inside of the microneedles that can be detected using an optical sensor. This allows the user to quickly determine the concentration of vancomycin.
“This is probably one of the smallest probe volumes ever recorded for a medically relevant analysis,” said study author Urs Häfeli, PhD, of UBC.
This microneedle drug monitoring system was developed out of a research collaboration between Dr Häfeli and Boris Stoeber, PhD, also of UBC. The system is being commercialized by the UBC spin-off Microdermics Inc.
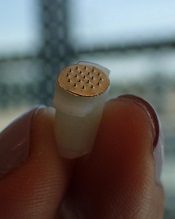
Photo courtesy of
Sahan Ranamukhaarachchi
A new microneedle drug monitoring system could one day replace invasive blood draws, according to researchers.
The system consists of a small, thin patch that is pressed against a patient’s arm during medical treatment and measures drugs in the bloodstream painlessly without drawing any blood.
The tiny projections on this patch resemble hollow cones and don’t pierce the skin like a standard hypodermic needle.
The researchers described this system in Scientific Reports.
“Many groups are researching microneedle technology for painless vaccines and drug delivery,” said study author Sahan Ranamukhaarachchi, a PhD student at the University of British Columbia (UBC) in Vancouver, British Columbia, Canada. “Using them to painlessly monitor drugs is a newer idea.”
The microneedle system Ranamukhaarachchi and his colleagues created was developed to monitor the antibiotic vancomycin. Patients taking vancomycin must be closely monitored because the drug can cause life-threatening side effects, so the patients undergo 3 to 4 blood draws per day.
The researchers discovered they could use fluid found just below the outer layer of skin, instead of blood, to monitor levels of vancomycin in the bloodstream.
The microneedle patch collects a tiny amount of the fluid, less than 1 nL, and a reaction occurs on the inside of the microneedles that can be detected using an optical sensor. This allows the user to quickly determine the concentration of vancomycin.
“This is probably one of the smallest probe volumes ever recorded for a medically relevant analysis,” said study author Urs Häfeli, PhD, of UBC.
This microneedle drug monitoring system was developed out of a research collaboration between Dr Häfeli and Boris Stoeber, PhD, also of UBC. The system is being commercialized by the UBC spin-off Microdermics Inc.
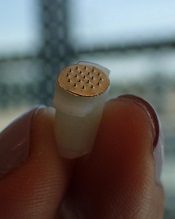
Photo courtesy of
Sahan Ranamukhaarachchi
A new microneedle drug monitoring system could one day replace invasive blood draws, according to researchers.
The system consists of a small, thin patch that is pressed against a patient’s arm during medical treatment and measures drugs in the bloodstream painlessly without drawing any blood.
The tiny projections on this patch resemble hollow cones and don’t pierce the skin like a standard hypodermic needle.
The researchers described this system in Scientific Reports.
“Many groups are researching microneedle technology for painless vaccines and drug delivery,” said study author Sahan Ranamukhaarachchi, a PhD student at the University of British Columbia (UBC) in Vancouver, British Columbia, Canada. “Using them to painlessly monitor drugs is a newer idea.”
The microneedle system Ranamukhaarachchi and his colleagues created was developed to monitor the antibiotic vancomycin. Patients taking vancomycin must be closely monitored because the drug can cause life-threatening side effects, so the patients undergo 3 to 4 blood draws per day.
The researchers discovered they could use fluid found just below the outer layer of skin, instead of blood, to monitor levels of vancomycin in the bloodstream.
The microneedle patch collects a tiny amount of the fluid, less than 1 nL, and a reaction occurs on the inside of the microneedles that can be detected using an optical sensor. This allows the user to quickly determine the concentration of vancomycin.
“This is probably one of the smallest probe volumes ever recorded for a medically relevant analysis,” said study author Urs Häfeli, PhD, of UBC.
This microneedle drug monitoring system was developed out of a research collaboration between Dr Häfeli and Boris Stoeber, PhD, also of UBC. The system is being commercialized by the UBC spin-off Microdermics Inc.
Local Zika transmission and the US blood supply

Photo courtesy of
Muhammad Mahdi Karim
Officials have announced what is likely the first known occurrence of local mosquito-borne Zika virus transmission in the continental US.*
Fourteen cases of Zika virus in 2 Florida counties are believed to have been caused by bites of local Aedes aegypti mosquitoes.
The Florida Department of Health (DOH) believes that active transmission of the Zika virus is only occurring in a small area in Miami-Dade County.
The US Centers for Disease Control and Prevention (CDC) has recommended that women who are pregnant or thinking of becoming pregnant avoid unnecessary travel to the impacted area. The agency has also issued a guidance for people living in or traveling to the area.
“All the evidence we have seen indicates that this is mosquito-borne transmission that occurred several weeks ago in several blocks in Miami,” said Tom Frieden, MD, director of the CDC.
The exact location is within the boundaries of the following area: NW 5th Avenue to the west, US 1 to the east, NW/NE 38th Street to the north and NW/NE 20th Street to the south. This is about one square mile.
Protecting the blood supply
The US Food and Drug Administration (FDA) has requested that all blood centers in Miami-Dade and Broward counties stop collecting blood immediately.
Blood centers in these counties can resume blood collection once they begin testing each unit of blood with an available investigational donor screening test for Zika virus RNA or once they implement the use of an approved or investigational pathogen inactivation technology.
The FDA also recommended that blood centers in nearby counties implement the same precautions as soon as possible to help maintain the safety of the blood supply. The agency has encouraged screening of the blood supply in regions of the US at risk of local mosquito-borne Zika transmission.
The FDA said it is working with companies that are making blood screening tests available under an Investigational New Drug (IND) application to ensure these companies are ready to expand testing as needed. Blood collection centers may choose to participate in testing under an IND even in the absence of local mosquito-borne transmission of Zika virus.
Florida/CDC response
Florida state officials have implemented mosquito control measures and a community-wide search for additional Zika cases. Thus far, Florida’s DOH has conducted testing for the Zika virus in more than 2300 people statewide.
The DOH has activated the Joint Information Center within the State Emergency Operations Center to ensure the area impacted by local transmission of the Zika virus has coordinated access to information and resources.
The DOH has also begun the process of contracting with commercial pest control companies to enhance and expand mosquito mitigation and abatement, including increased spraying, in the impacted area.
Earlier this year, Florida’s governor, Rick Scott, directed the State Surgeon General to activate a Zika Virus Information Hotline for Florida residents and visitors. The number for this hotline is 1-855-622-6735.
The CDC said it is coordinating with Florida officials leading the ongoing investigation into local transmission of the Zika virus. At the state’s request, the CDC sent a medical epidemiologist to provide additional assistance.
Governor Scott has also asked the CDC to activate a CDC Emergency Response Team to assist the DOH and other partners in their investigation, sample collection, and mosquito control efforts.
To date, the CDC has provided Florida with more than $8 million in Zika-specific funding and about $27 million in emergency preparedness funding that can be used for Zika response efforts.
“We have been working with state and local governments to prepare for the likelihood of local mosquito-borne Zika virus transmission in the continental United States and Hawaii,” said Lyle Petersen, MD, incident manager for CDC’s Zika virus response.
“We anticipate that there may be additional cases of ‘homegrown’ Zika in the coming weeks. Our top priority is to protect pregnant women from the potentially devastating harm caused by Zika.”
For more information about the Zika virus, visit http://www.cdc.gov/zika/.
*This story was updated on August 1.

Photo courtesy of
Muhammad Mahdi Karim
Officials have announced what is likely the first known occurrence of local mosquito-borne Zika virus transmission in the continental US.*
Fourteen cases of Zika virus in 2 Florida counties are believed to have been caused by bites of local Aedes aegypti mosquitoes.
The Florida Department of Health (DOH) believes that active transmission of the Zika virus is only occurring in a small area in Miami-Dade County.
The US Centers for Disease Control and Prevention (CDC) has recommended that women who are pregnant or thinking of becoming pregnant avoid unnecessary travel to the impacted area. The agency has also issued a guidance for people living in or traveling to the area.
“All the evidence we have seen indicates that this is mosquito-borne transmission that occurred several weeks ago in several blocks in Miami,” said Tom Frieden, MD, director of the CDC.
The exact location is within the boundaries of the following area: NW 5th Avenue to the west, US 1 to the east, NW/NE 38th Street to the north and NW/NE 20th Street to the south. This is about one square mile.
Protecting the blood supply
The US Food and Drug Administration (FDA) has requested that all blood centers in Miami-Dade and Broward counties stop collecting blood immediately.
Blood centers in these counties can resume blood collection once they begin testing each unit of blood with an available investigational donor screening test for Zika virus RNA or once they implement the use of an approved or investigational pathogen inactivation technology.
The FDA also recommended that blood centers in nearby counties implement the same precautions as soon as possible to help maintain the safety of the blood supply. The agency has encouraged screening of the blood supply in regions of the US at risk of local mosquito-borne Zika transmission.
The FDA said it is working with companies that are making blood screening tests available under an Investigational New Drug (IND) application to ensure these companies are ready to expand testing as needed. Blood collection centers may choose to participate in testing under an IND even in the absence of local mosquito-borne transmission of Zika virus.
Florida/CDC response
Florida state officials have implemented mosquito control measures and a community-wide search for additional Zika cases. Thus far, Florida’s DOH has conducted testing for the Zika virus in more than 2300 people statewide.
The DOH has activated the Joint Information Center within the State Emergency Operations Center to ensure the area impacted by local transmission of the Zika virus has coordinated access to information and resources.
The DOH has also begun the process of contracting with commercial pest control companies to enhance and expand mosquito mitigation and abatement, including increased spraying, in the impacted area.
Earlier this year, Florida’s governor, Rick Scott, directed the State Surgeon General to activate a Zika Virus Information Hotline for Florida residents and visitors. The number for this hotline is 1-855-622-6735.
The CDC said it is coordinating with Florida officials leading the ongoing investigation into local transmission of the Zika virus. At the state’s request, the CDC sent a medical epidemiologist to provide additional assistance.
Governor Scott has also asked the CDC to activate a CDC Emergency Response Team to assist the DOH and other partners in their investigation, sample collection, and mosquito control efforts.
To date, the CDC has provided Florida with more than $8 million in Zika-specific funding and about $27 million in emergency preparedness funding that can be used for Zika response efforts.
“We have been working with state and local governments to prepare for the likelihood of local mosquito-borne Zika virus transmission in the continental United States and Hawaii,” said Lyle Petersen, MD, incident manager for CDC’s Zika virus response.
“We anticipate that there may be additional cases of ‘homegrown’ Zika in the coming weeks. Our top priority is to protect pregnant women from the potentially devastating harm caused by Zika.”
For more information about the Zika virus, visit http://www.cdc.gov/zika/.
*This story was updated on August 1.

Photo courtesy of
Muhammad Mahdi Karim
Officials have announced what is likely the first known occurrence of local mosquito-borne Zika virus transmission in the continental US.*
Fourteen cases of Zika virus in 2 Florida counties are believed to have been caused by bites of local Aedes aegypti mosquitoes.
The Florida Department of Health (DOH) believes that active transmission of the Zika virus is only occurring in a small area in Miami-Dade County.
The US Centers for Disease Control and Prevention (CDC) has recommended that women who are pregnant or thinking of becoming pregnant avoid unnecessary travel to the impacted area. The agency has also issued a guidance for people living in or traveling to the area.
“All the evidence we have seen indicates that this is mosquito-borne transmission that occurred several weeks ago in several blocks in Miami,” said Tom Frieden, MD, director of the CDC.
The exact location is within the boundaries of the following area: NW 5th Avenue to the west, US 1 to the east, NW/NE 38th Street to the north and NW/NE 20th Street to the south. This is about one square mile.
Protecting the blood supply
The US Food and Drug Administration (FDA) has requested that all blood centers in Miami-Dade and Broward counties stop collecting blood immediately.
Blood centers in these counties can resume blood collection once they begin testing each unit of blood with an available investigational donor screening test for Zika virus RNA or once they implement the use of an approved or investigational pathogen inactivation technology.
The FDA also recommended that blood centers in nearby counties implement the same precautions as soon as possible to help maintain the safety of the blood supply. The agency has encouraged screening of the blood supply in regions of the US at risk of local mosquito-borne Zika transmission.
The FDA said it is working with companies that are making blood screening tests available under an Investigational New Drug (IND) application to ensure these companies are ready to expand testing as needed. Blood collection centers may choose to participate in testing under an IND even in the absence of local mosquito-borne transmission of Zika virus.
Florida/CDC response
Florida state officials have implemented mosquito control measures and a community-wide search for additional Zika cases. Thus far, Florida’s DOH has conducted testing for the Zika virus in more than 2300 people statewide.
The DOH has activated the Joint Information Center within the State Emergency Operations Center to ensure the area impacted by local transmission of the Zika virus has coordinated access to information and resources.
The DOH has also begun the process of contracting with commercial pest control companies to enhance and expand mosquito mitigation and abatement, including increased spraying, in the impacted area.
Earlier this year, Florida’s governor, Rick Scott, directed the State Surgeon General to activate a Zika Virus Information Hotline for Florida residents and visitors. The number for this hotline is 1-855-622-6735.
The CDC said it is coordinating with Florida officials leading the ongoing investigation into local transmission of the Zika virus. At the state’s request, the CDC sent a medical epidemiologist to provide additional assistance.
Governor Scott has also asked the CDC to activate a CDC Emergency Response Team to assist the DOH and other partners in their investigation, sample collection, and mosquito control efforts.
To date, the CDC has provided Florida with more than $8 million in Zika-specific funding and about $27 million in emergency preparedness funding that can be used for Zika response efforts.
“We have been working with state and local governments to prepare for the likelihood of local mosquito-borne Zika virus transmission in the continental United States and Hawaii,” said Lyle Petersen, MD, incident manager for CDC’s Zika virus response.
“We anticipate that there may be additional cases of ‘homegrown’ Zika in the coming weeks. Our top priority is to protect pregnant women from the potentially devastating harm caused by Zika.”
For more information about the Zika virus, visit http://www.cdc.gov/zika/.
*This story was updated on August 1.