User login
Facial eruptions

This was a vigorous response to the 5-FU treatment and was actually within the range of expected outcomes for a patient with a heavy burden of AKs. The erythema and superficial skin flaking spared areas unaffected by pre-cancers.
AKs manifest as rough, pink to brown macules or papules on sun-damaged skin and represent a precancerous change in keratinocytes that can lead to invasive squamous cell carcinoma. For this reason, AKs are often treated when they are observed. When targeting an entire “field” of AKs, a gold standard therapy is topical 5-FU. Prescribing 5-FU is safe and effective, but requires patient education, therapy customization, and anticipatory guidance.
Compared with other field treatments (eg, photodynamic therapy, topical diclofenac, imiquimod), 5-FU is the most successful and cost effective; it is first-line therapy and has the longest track record.1,2 5-FU represses DNA synthesis. It’s helpful to describe 5-FU to patients as “fake DNA” that targets precancerous cells that are dividing rapidly. But a word of caution: Patients should be advised, in advance, to avoid significant sun exposure while using 5-FU, as the drug will lose its targeted effect and cause more generalized skin damage.
Physicians can modulate the severity of the response to 5-FU by decreasing the frequency or length of therapy by using a weaker (and more expensive) once daily 0.5% long-acting formulation. Additionally, to improve comfort, low-potency topical steroids such as hydrocortisone ointment 0.5% to 2.5% can be applied after completion of therapy to speed up the healing process. These adjustments improve tolerance of therapy, but the precise effect on efficacy is unknown.
Because of the degree of redness and erythema that developed in this patient, treatment was stopped a week early. There was also concern about possible bacterial involvement in the heavy skin sloughing, so the patient was given topical mupirocin ointment to apply TID for 7 days. Her skin cleared after 3 weeks and all previous AKs were clinically eliminated.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Gupta AK, Paquet M. Network meta-analysis of the outcome 'participant complete clearance' in nonimmunosuppressed participants of eight interventions for actinic keratosis: a follow-up on a Cochrane review. Br J Dermatol. 2013;169:250-259. doi: 10.1111/bjd.12343
2. Jansen MHE, Kessels JPHM, Merks I, et al. A trial-based cost-effectiveness analysis of topical 5-fluorouracil vs. imiquimod vs. ingenol mebutate vs. methyl aminolaevulinate conventional photodynamic therapy for the treatment of actinic keratosis in the head and neck area performed in the Netherlands. Br J Dermatol. 2020;183:738-744. doi: 10.1111/bjd.18884

This was a vigorous response to the 5-FU treatment and was actually within the range of expected outcomes for a patient with a heavy burden of AKs. The erythema and superficial skin flaking spared areas unaffected by pre-cancers.
AKs manifest as rough, pink to brown macules or papules on sun-damaged skin and represent a precancerous change in keratinocytes that can lead to invasive squamous cell carcinoma. For this reason, AKs are often treated when they are observed. When targeting an entire “field” of AKs, a gold standard therapy is topical 5-FU. Prescribing 5-FU is safe and effective, but requires patient education, therapy customization, and anticipatory guidance.
Compared with other field treatments (eg, photodynamic therapy, topical diclofenac, imiquimod), 5-FU is the most successful and cost effective; it is first-line therapy and has the longest track record.1,2 5-FU represses DNA synthesis. It’s helpful to describe 5-FU to patients as “fake DNA” that targets precancerous cells that are dividing rapidly. But a word of caution: Patients should be advised, in advance, to avoid significant sun exposure while using 5-FU, as the drug will lose its targeted effect and cause more generalized skin damage.
Physicians can modulate the severity of the response to 5-FU by decreasing the frequency or length of therapy by using a weaker (and more expensive) once daily 0.5% long-acting formulation. Additionally, to improve comfort, low-potency topical steroids such as hydrocortisone ointment 0.5% to 2.5% can be applied after completion of therapy to speed up the healing process. These adjustments improve tolerance of therapy, but the precise effect on efficacy is unknown.
Because of the degree of redness and erythema that developed in this patient, treatment was stopped a week early. There was also concern about possible bacterial involvement in the heavy skin sloughing, so the patient was given topical mupirocin ointment to apply TID for 7 days. Her skin cleared after 3 weeks and all previous AKs were clinically eliminated.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).

This was a vigorous response to the 5-FU treatment and was actually within the range of expected outcomes for a patient with a heavy burden of AKs. The erythema and superficial skin flaking spared areas unaffected by pre-cancers.
AKs manifest as rough, pink to brown macules or papules on sun-damaged skin and represent a precancerous change in keratinocytes that can lead to invasive squamous cell carcinoma. For this reason, AKs are often treated when they are observed. When targeting an entire “field” of AKs, a gold standard therapy is topical 5-FU. Prescribing 5-FU is safe and effective, but requires patient education, therapy customization, and anticipatory guidance.
Compared with other field treatments (eg, photodynamic therapy, topical diclofenac, imiquimod), 5-FU is the most successful and cost effective; it is first-line therapy and has the longest track record.1,2 5-FU represses DNA synthesis. It’s helpful to describe 5-FU to patients as “fake DNA” that targets precancerous cells that are dividing rapidly. But a word of caution: Patients should be advised, in advance, to avoid significant sun exposure while using 5-FU, as the drug will lose its targeted effect and cause more generalized skin damage.
Physicians can modulate the severity of the response to 5-FU by decreasing the frequency or length of therapy by using a weaker (and more expensive) once daily 0.5% long-acting formulation. Additionally, to improve comfort, low-potency topical steroids such as hydrocortisone ointment 0.5% to 2.5% can be applied after completion of therapy to speed up the healing process. These adjustments improve tolerance of therapy, but the precise effect on efficacy is unknown.
Because of the degree of redness and erythema that developed in this patient, treatment was stopped a week early. There was also concern about possible bacterial involvement in the heavy skin sloughing, so the patient was given topical mupirocin ointment to apply TID for 7 days. Her skin cleared after 3 weeks and all previous AKs were clinically eliminated.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Gupta AK, Paquet M. Network meta-analysis of the outcome 'participant complete clearance' in nonimmunosuppressed participants of eight interventions for actinic keratosis: a follow-up on a Cochrane review. Br J Dermatol. 2013;169:250-259. doi: 10.1111/bjd.12343
2. Jansen MHE, Kessels JPHM, Merks I, et al. A trial-based cost-effectiveness analysis of topical 5-fluorouracil vs. imiquimod vs. ingenol mebutate vs. methyl aminolaevulinate conventional photodynamic therapy for the treatment of actinic keratosis in the head and neck area performed in the Netherlands. Br J Dermatol. 2020;183:738-744. doi: 10.1111/bjd.18884
1. Gupta AK, Paquet M. Network meta-analysis of the outcome 'participant complete clearance' in nonimmunosuppressed participants of eight interventions for actinic keratosis: a follow-up on a Cochrane review. Br J Dermatol. 2013;169:250-259. doi: 10.1111/bjd.12343
2. Jansen MHE, Kessels JPHM, Merks I, et al. A trial-based cost-effectiveness analysis of topical 5-fluorouracil vs. imiquimod vs. ingenol mebutate vs. methyl aminolaevulinate conventional photodynamic therapy for the treatment of actinic keratosis in the head and neck area performed in the Netherlands. Br J Dermatol. 2020;183:738-744. doi: 10.1111/bjd.18884
Target lesion
The original diagnosis in this case was correct—Lyme disease (erythema chronicum migrans)—but unfortunately, the treatment was inadequate. Initially, this patient received a single dose of doxycycline 200 mg po, which is the appropriate preventative remedy when a deer tick has been attached for at least 36 hours and treatment can be initiated within 72 hours of tick removal. However, deer ticks, especially nymphs, are very small and their presence can go unnoticed, leading patients to guess (sometimes incorrectly) at the length of time a tick has been attached.
In this case, when the patient and his wife thought about it a bit more, they indicated that the tick may have been attached for several days before they removed it and went to see the PCP. Had the PCP known the tick had been attached longer, she would have advised watchful waiting and observation for signs and symptoms of Lyme disease.
Originally described in cases from Lyme, Connecticut, Lyme disease is now endemic to the northeastern United States from Maine to Virginia, and from the upper midwest to Minnesota. Laboratory diagnosis can be made by a 2-tiered serologic screening and confirmation with an enzyme-linked assay, followed by a western blot for positive or equivocal screening tests.
In 2019, the most recent year of reported Centers for Disease Control and Prevention (CDC) surveillance data, Maine recorded the highest incidence rate of Lyme disease.1 In 70% to 80% of cases, an expanding horizon of infection creates the characteristic targetoid pink patch centered on the site of the tick bite.2
If there is a targetoid rash present in a patient from an endemic area, the CDC recommends empiric therapy with doxycycline 100 mg po bid for 10 to 14 days.3 (Worth noting: Patches may appear rather small in diameter, as was true in this case, or may be many centimeters in size and mimic cellulitis.) Alternative regimens for early localized disease include amoxicillin 500 mg po qid for pregnant patients, and cefuroxime 500 mg bid daily for 14 days for patients who are allergic to doxycycline.
Once treatment has been initiated, it’s important to monitor patients for any worsening symptoms, including fever and weakness, as these may be an indication of treatment failure or co-occurrence of anaplasmosis, ehrlichiosis, or babesiosis. In this case, the patient was prescribed doxycycline 100 mg bid for 14 days without any further signs or symptoms.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Lyme disease maps: most recent year. Centers for Disease Control and Prevention. Updated April 29, 2021. Accessed August 12, 2021. https://www.cdc.gov/lyme/datasurveillance/maps-recent.html
2. Signs and symptoms of untreated Lyme disease. Centers for Disease Control and Prevention. Updated January 15, 2021. Accessed August 13, 2021. https://www.cdc.gov/lyme/signs_symptoms/index.html
3. Treatment of erythema migrans. Centers for Disease Control and Prevention. Updated November 3, 2020. Accessed August 12, 2021. https://www.cdc.gov/lyme/treatment/index.html
The original diagnosis in this case was correct—Lyme disease (erythema chronicum migrans)—but unfortunately, the treatment was inadequate. Initially, this patient received a single dose of doxycycline 200 mg po, which is the appropriate preventative remedy when a deer tick has been attached for at least 36 hours and treatment can be initiated within 72 hours of tick removal. However, deer ticks, especially nymphs, are very small and their presence can go unnoticed, leading patients to guess (sometimes incorrectly) at the length of time a tick has been attached.
In this case, when the patient and his wife thought about it a bit more, they indicated that the tick may have been attached for several days before they removed it and went to see the PCP. Had the PCP known the tick had been attached longer, she would have advised watchful waiting and observation for signs and symptoms of Lyme disease.
Originally described in cases from Lyme, Connecticut, Lyme disease is now endemic to the northeastern United States from Maine to Virginia, and from the upper midwest to Minnesota. Laboratory diagnosis can be made by a 2-tiered serologic screening and confirmation with an enzyme-linked assay, followed by a western blot for positive or equivocal screening tests.
In 2019, the most recent year of reported Centers for Disease Control and Prevention (CDC) surveillance data, Maine recorded the highest incidence rate of Lyme disease.1 In 70% to 80% of cases, an expanding horizon of infection creates the characteristic targetoid pink patch centered on the site of the tick bite.2
If there is a targetoid rash present in a patient from an endemic area, the CDC recommends empiric therapy with doxycycline 100 mg po bid for 10 to 14 days.3 (Worth noting: Patches may appear rather small in diameter, as was true in this case, or may be many centimeters in size and mimic cellulitis.) Alternative regimens for early localized disease include amoxicillin 500 mg po qid for pregnant patients, and cefuroxime 500 mg bid daily for 14 days for patients who are allergic to doxycycline.
Once treatment has been initiated, it’s important to monitor patients for any worsening symptoms, including fever and weakness, as these may be an indication of treatment failure or co-occurrence of anaplasmosis, ehrlichiosis, or babesiosis. In this case, the patient was prescribed doxycycline 100 mg bid for 14 days without any further signs or symptoms.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
The original diagnosis in this case was correct—Lyme disease (erythema chronicum migrans)—but unfortunately, the treatment was inadequate. Initially, this patient received a single dose of doxycycline 200 mg po, which is the appropriate preventative remedy when a deer tick has been attached for at least 36 hours and treatment can be initiated within 72 hours of tick removal. However, deer ticks, especially nymphs, are very small and their presence can go unnoticed, leading patients to guess (sometimes incorrectly) at the length of time a tick has been attached.
In this case, when the patient and his wife thought about it a bit more, they indicated that the tick may have been attached for several days before they removed it and went to see the PCP. Had the PCP known the tick had been attached longer, she would have advised watchful waiting and observation for signs and symptoms of Lyme disease.
Originally described in cases from Lyme, Connecticut, Lyme disease is now endemic to the northeastern United States from Maine to Virginia, and from the upper midwest to Minnesota. Laboratory diagnosis can be made by a 2-tiered serologic screening and confirmation with an enzyme-linked assay, followed by a western blot for positive or equivocal screening tests.
In 2019, the most recent year of reported Centers for Disease Control and Prevention (CDC) surveillance data, Maine recorded the highest incidence rate of Lyme disease.1 In 70% to 80% of cases, an expanding horizon of infection creates the characteristic targetoid pink patch centered on the site of the tick bite.2
If there is a targetoid rash present in a patient from an endemic area, the CDC recommends empiric therapy with doxycycline 100 mg po bid for 10 to 14 days.3 (Worth noting: Patches may appear rather small in diameter, as was true in this case, or may be many centimeters in size and mimic cellulitis.) Alternative regimens for early localized disease include amoxicillin 500 mg po qid for pregnant patients, and cefuroxime 500 mg bid daily for 14 days for patients who are allergic to doxycycline.
Once treatment has been initiated, it’s important to monitor patients for any worsening symptoms, including fever and weakness, as these may be an indication of treatment failure or co-occurrence of anaplasmosis, ehrlichiosis, or babesiosis. In this case, the patient was prescribed doxycycline 100 mg bid for 14 days without any further signs or symptoms.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Lyme disease maps: most recent year. Centers for Disease Control and Prevention. Updated April 29, 2021. Accessed August 12, 2021. https://www.cdc.gov/lyme/datasurveillance/maps-recent.html
2. Signs and symptoms of untreated Lyme disease. Centers for Disease Control and Prevention. Updated January 15, 2021. Accessed August 13, 2021. https://www.cdc.gov/lyme/signs_symptoms/index.html
3. Treatment of erythema migrans. Centers for Disease Control and Prevention. Updated November 3, 2020. Accessed August 12, 2021. https://www.cdc.gov/lyme/treatment/index.html
1. Lyme disease maps: most recent year. Centers for Disease Control and Prevention. Updated April 29, 2021. Accessed August 12, 2021. https://www.cdc.gov/lyme/datasurveillance/maps-recent.html
2. Signs and symptoms of untreated Lyme disease. Centers for Disease Control and Prevention. Updated January 15, 2021. Accessed August 13, 2021. https://www.cdc.gov/lyme/signs_symptoms/index.html
3. Treatment of erythema migrans. Centers for Disease Control and Prevention. Updated November 3, 2020. Accessed August 12, 2021. https://www.cdc.gov/lyme/treatment/index.html
Arm and neck rash
The manifestation of what appeared to be an exaggerated sunburn with associated pruritis and blistering (made worse after sun exposure), along with the recent initiation of HCTZ, led to the diagnosis of a phototoxic drug reaction.
There are 2 principal mechanisms of photosensitive drug reactions, phototoxic and photoallergic. Phototoxic reactions occur when the drug absorbs UVA light, causing a chemical reaction that produces either free radicals or stable photoproducts, both of which can cause DNA and tissue damage. This mechanism is more common; the time of onset between exposure and reaction is minutes to hours (as seen with this patient), and the reaction manifests with an exaggerated sunburn appearance.1
Photoallergic reactions typically occur by a delayed-immune response, mediated by photoallergic-specific T-cells reacting to photohaptens. This mechanism is less common, and the time of onset is greater than 24 hours. Photoallergic reactions often present as an eczematous dermatitis and can involve regions not directly exposed to sun.
In this case, the presumed offending agent—HCTZ—was discontinued, and the patient was advised to take sun-protective measures and use topical emollients, cool compresses, and oral analgesics for his acute symptoms. Photoallergic reactions look less like a discrete sunburn and can be treated symptomatically with topical or oral steroids. In addition, the implicated medication should be discontinued.
Text courtesy of Amanda Yaney, MD, and Daniel Stulberg, MD, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque. Image courtesy of Daniel Stulberg, MD.
Lozzi F, Di Raimondo C, Lanna C, et al. Latest evidence regarding the effects of photosensitive drugs on the skin: pathogenic mechanisms and clinical manifestations. Pharmaceutics 2020;12:1104. doi: 10.3390/pharmaceutics12111104
The manifestation of what appeared to be an exaggerated sunburn with associated pruritis and blistering (made worse after sun exposure), along with the recent initiation of HCTZ, led to the diagnosis of a phototoxic drug reaction.
There are 2 principal mechanisms of photosensitive drug reactions, phototoxic and photoallergic. Phototoxic reactions occur when the drug absorbs UVA light, causing a chemical reaction that produces either free radicals or stable photoproducts, both of which can cause DNA and tissue damage. This mechanism is more common; the time of onset between exposure and reaction is minutes to hours (as seen with this patient), and the reaction manifests with an exaggerated sunburn appearance.1
Photoallergic reactions typically occur by a delayed-immune response, mediated by photoallergic-specific T-cells reacting to photohaptens. This mechanism is less common, and the time of onset is greater than 24 hours. Photoallergic reactions often present as an eczematous dermatitis and can involve regions not directly exposed to sun.
In this case, the presumed offending agent—HCTZ—was discontinued, and the patient was advised to take sun-protective measures and use topical emollients, cool compresses, and oral analgesics for his acute symptoms. Photoallergic reactions look less like a discrete sunburn and can be treated symptomatically with topical or oral steroids. In addition, the implicated medication should be discontinued.
Text courtesy of Amanda Yaney, MD, and Daniel Stulberg, MD, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque. Image courtesy of Daniel Stulberg, MD.
The manifestation of what appeared to be an exaggerated sunburn with associated pruritis and blistering (made worse after sun exposure), along with the recent initiation of HCTZ, led to the diagnosis of a phototoxic drug reaction.
There are 2 principal mechanisms of photosensitive drug reactions, phototoxic and photoallergic. Phototoxic reactions occur when the drug absorbs UVA light, causing a chemical reaction that produces either free radicals or stable photoproducts, both of which can cause DNA and tissue damage. This mechanism is more common; the time of onset between exposure and reaction is minutes to hours (as seen with this patient), and the reaction manifests with an exaggerated sunburn appearance.1
Photoallergic reactions typically occur by a delayed-immune response, mediated by photoallergic-specific T-cells reacting to photohaptens. This mechanism is less common, and the time of onset is greater than 24 hours. Photoallergic reactions often present as an eczematous dermatitis and can involve regions not directly exposed to sun.
In this case, the presumed offending agent—HCTZ—was discontinued, and the patient was advised to take sun-protective measures and use topical emollients, cool compresses, and oral analgesics for his acute symptoms. Photoallergic reactions look less like a discrete sunburn and can be treated symptomatically with topical or oral steroids. In addition, the implicated medication should be discontinued.
Text courtesy of Amanda Yaney, MD, and Daniel Stulberg, MD, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque. Image courtesy of Daniel Stulberg, MD.
Lozzi F, Di Raimondo C, Lanna C, et al. Latest evidence regarding the effects of photosensitive drugs on the skin: pathogenic mechanisms and clinical manifestations. Pharmaceutics 2020;12:1104. doi: 10.3390/pharmaceutics12111104
Lozzi F, Di Raimondo C, Lanna C, et al. Latest evidence regarding the effects of photosensitive drugs on the skin: pathogenic mechanisms and clinical manifestations. Pharmaceutics 2020;12:1104. doi: 10.3390/pharmaceutics12111104
Annular lesions
This patient was given a diagnosis of disseminated granuloma annulare (DGA). While granuloma annulare usually manifests as a single lesion with a raised erythematous border (often with central pallor or hypopigmentation) it can also manifest as multiple large annular lesions on the extremities and occasionally the trunk, as was seen with this case of DGA.
Although the etiology of DGA is unknown, infections including HIV and hepatitis have been reported as possible triggers. Laboratory testing should be considered if the history or physical examination raises suspicion for either condition. Diabetes has also been associated with the disseminated form and the literature suggests a connection with autoimmune diseases of the liver and thyroid.1
Watchful waiting is usually the best treatment for localized disease, which can spontaneously regress within a year and is usually asymptomatic. Intralesional steroid injections into the raised annulus are more effective than topical steroids, as the effects of the topical steroids are sometimes augmented by occlusion.
Multiple treatments have been proposed for DGA, including UVA treatments, systemic retinoids, doxycycline, and hydroxychloroquine.1 Unfortunately, the disseminated form can persist for many years—even with treatment.
Due to the extent of the lesions, the patient in this case was not interested in intralesional steroid injections, and she had already tried topical steroids. She was prescribed topical tacrolimus to reduce the highly visible nature of her lesions.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
Beretta-Piccoli BT, Mainetti C, Peeters MA, et al. Cutaneous granulomatosis: a comprehensive review. Clin Rev Allergy Immunol. 2018;54:131-146. doi: 10.1007/s12016-017-8666-8
This patient was given a diagnosis of disseminated granuloma annulare (DGA). While granuloma annulare usually manifests as a single lesion with a raised erythematous border (often with central pallor or hypopigmentation) it can also manifest as multiple large annular lesions on the extremities and occasionally the trunk, as was seen with this case of DGA.
Although the etiology of DGA is unknown, infections including HIV and hepatitis have been reported as possible triggers. Laboratory testing should be considered if the history or physical examination raises suspicion for either condition. Diabetes has also been associated with the disseminated form and the literature suggests a connection with autoimmune diseases of the liver and thyroid.1
Watchful waiting is usually the best treatment for localized disease, which can spontaneously regress within a year and is usually asymptomatic. Intralesional steroid injections into the raised annulus are more effective than topical steroids, as the effects of the topical steroids are sometimes augmented by occlusion.
Multiple treatments have been proposed for DGA, including UVA treatments, systemic retinoids, doxycycline, and hydroxychloroquine.1 Unfortunately, the disseminated form can persist for many years—even with treatment.
Due to the extent of the lesions, the patient in this case was not interested in intralesional steroid injections, and she had already tried topical steroids. She was prescribed topical tacrolimus to reduce the highly visible nature of her lesions.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
This patient was given a diagnosis of disseminated granuloma annulare (DGA). While granuloma annulare usually manifests as a single lesion with a raised erythematous border (often with central pallor or hypopigmentation) it can also manifest as multiple large annular lesions on the extremities and occasionally the trunk, as was seen with this case of DGA.
Although the etiology of DGA is unknown, infections including HIV and hepatitis have been reported as possible triggers. Laboratory testing should be considered if the history or physical examination raises suspicion for either condition. Diabetes has also been associated with the disseminated form and the literature suggests a connection with autoimmune diseases of the liver and thyroid.1
Watchful waiting is usually the best treatment for localized disease, which can spontaneously regress within a year and is usually asymptomatic. Intralesional steroid injections into the raised annulus are more effective than topical steroids, as the effects of the topical steroids are sometimes augmented by occlusion.
Multiple treatments have been proposed for DGA, including UVA treatments, systemic retinoids, doxycycline, and hydroxychloroquine.1 Unfortunately, the disseminated form can persist for many years—even with treatment.
Due to the extent of the lesions, the patient in this case was not interested in intralesional steroid injections, and she had already tried topical steroids. She was prescribed topical tacrolimus to reduce the highly visible nature of her lesions.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
Beretta-Piccoli BT, Mainetti C, Peeters MA, et al. Cutaneous granulomatosis: a comprehensive review. Clin Rev Allergy Immunol. 2018;54:131-146. doi: 10.1007/s12016-017-8666-8
Beretta-Piccoli BT, Mainetti C, Peeters MA, et al. Cutaneous granulomatosis: a comprehensive review. Clin Rev Allergy Immunol. 2018;54:131-146. doi: 10.1007/s12016-017-8666-8
Multiple pigmented patches
This patient was given a diagnosis of erythema dyschromicum perstans (EDP), also known as ashy dermatosis because of the hyperpigmented macules that come together into confluent patches that look like burned wood. There is often an inflammatory erythematous aspect to EDP.
The etiology of EDP is unknown. It is not related to sun exposure and occurs most commonly on the trunk. Although there are case reports implicating medications or infections, no clear connection has been found. This patient’s chemotherapy may have been an inciting factor, based on her history, but it is not likely that cancer caused the EDP.
EDP tends to be chronic and difficult to treat. Fortunately, other than the itching and skin discoloration, it is usually asymptomatic and benign. Large-scale trials are lacking, but there are case reports showing benefit from narrow beam UVB treatments and topical tacrolimus.1 Laser has not proven very helpful, and the hyperpigmentation can recur.
Based on the clinical appearance of this patient’s lesion, and the fact that a previous biopsy in the same location was consistent with her diagnosis, no further testing was performed. The patient was advised to apply topical diphenhydramine to her back 4 times daily for a 2-week trial. If the diphenhydramine failed to provide relief, the next step in her treatment would have been topical tacrolimus.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Leung N, Oliveira M, Selim MA, et al. Erythema dyschromicum perstans: a case report and systematic review of histologic presentation and treatment. Int J Womens Dermatol. 2018;4:216-222. doi: 10.1016/j.ijwd.2018.08.003
This patient was given a diagnosis of erythema dyschromicum perstans (EDP), also known as ashy dermatosis because of the hyperpigmented macules that come together into confluent patches that look like burned wood. There is often an inflammatory erythematous aspect to EDP.
The etiology of EDP is unknown. It is not related to sun exposure and occurs most commonly on the trunk. Although there are case reports implicating medications or infections, no clear connection has been found. This patient’s chemotherapy may have been an inciting factor, based on her history, but it is not likely that cancer caused the EDP.
EDP tends to be chronic and difficult to treat. Fortunately, other than the itching and skin discoloration, it is usually asymptomatic and benign. Large-scale trials are lacking, but there are case reports showing benefit from narrow beam UVB treatments and topical tacrolimus.1 Laser has not proven very helpful, and the hyperpigmentation can recur.
Based on the clinical appearance of this patient’s lesion, and the fact that a previous biopsy in the same location was consistent with her diagnosis, no further testing was performed. The patient was advised to apply topical diphenhydramine to her back 4 times daily for a 2-week trial. If the diphenhydramine failed to provide relief, the next step in her treatment would have been topical tacrolimus.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
This patient was given a diagnosis of erythema dyschromicum perstans (EDP), also known as ashy dermatosis because of the hyperpigmented macules that come together into confluent patches that look like burned wood. There is often an inflammatory erythematous aspect to EDP.
The etiology of EDP is unknown. It is not related to sun exposure and occurs most commonly on the trunk. Although there are case reports implicating medications or infections, no clear connection has been found. This patient’s chemotherapy may have been an inciting factor, based on her history, but it is not likely that cancer caused the EDP.
EDP tends to be chronic and difficult to treat. Fortunately, other than the itching and skin discoloration, it is usually asymptomatic and benign. Large-scale trials are lacking, but there are case reports showing benefit from narrow beam UVB treatments and topical tacrolimus.1 Laser has not proven very helpful, and the hyperpigmentation can recur.
Based on the clinical appearance of this patient’s lesion, and the fact that a previous biopsy in the same location was consistent with her diagnosis, no further testing was performed. The patient was advised to apply topical diphenhydramine to her back 4 times daily for a 2-week trial. If the diphenhydramine failed to provide relief, the next step in her treatment would have been topical tacrolimus.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Leung N, Oliveira M, Selim MA, et al. Erythema dyschromicum perstans: a case report and systematic review of histologic presentation and treatment. Int J Womens Dermatol. 2018;4:216-222. doi: 10.1016/j.ijwd.2018.08.003
1. Leung N, Oliveira M, Selim MA, et al. Erythema dyschromicum perstans: a case report and systematic review of histologic presentation and treatment. Int J Womens Dermatol. 2018;4:216-222. doi: 10.1016/j.ijwd.2018.08.003
Pruritic welts
The patient’s history and the classic morphology of raised plaques was consistent with chronic spontaneous urticaria. Erythema may be subtle or not visible in patients with skin of color.
Individual urticarial lesions last less than 24 hours with itching and burning. Angioedema also occurs, and manifests as a deeper edema with itching, burning, and pain. Symptoms typically last for 2 to 3 days and involve the eyelids, lips, and tongue.
Chronic urticaria (CU) is defined as episodes of spontaneous wheals or angioedema lasting for more than 6 weeks and is subdivided into chronic spontaneous urticaria or inducible urticaria (if there is a known cause). Triggers include infection, emotional stressors, or medications (eg, angiotensin-converting enzyme inhibitors, nonsteroidal anti-inflammatory drugs). Autoimmunity is seen in one-third of CU patients.1
Only a limited routine-diagnostic work-up is necessary for CU and it may include a complete blood count with differential and erythrocyte sedimentation rate and C-reactive protein testing. Further diagnostic testing is based on history and may include functional autoantibodies, thyroid stimulating hormone, and thyroid autoantibodies.
The initial step in treatment involves identification and elimination of triggers. If this is not possible, first-line therapy includes second-generation antihistamines. If symptoms persist beyond 2 weeks, the dose of the antihistamine is increased up to 4-fold. Patients should be counseled that the lowest necessary dose needs to be taken habitually to prevent urticaria. If symptoms persist, omalizumab, a recombinant humanized IgG monoclonal antibody against serum IgE, cyclosporine, or montelukast, may be added. Leukotriene-receptor antagonists such as montelukast were previously second-line therapy, but they have had mixed results in randomized controlled trials. With a much lower cost than omalizumab, leukotriene-receptor antagonists are a reasonable alternative for patients who are refractory to antihistamines.1
This patient was given high-dose nonsedating antihistamines; she experienced sedation and inadequate relief. A prior authorization was successfully obtained, and she was prescribed omalizumab.
Image courtesy of Kriti Mishra, MD, Department of Dermatology, University of New Mexico School of Medicine, Albuquerque. Text courtesy of Kriti Mishra, MD, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Antia C, Baquerizo K, Korman A, et al. Urticaria: a comprehensive review: treatment of chronic urticaria, special populations, and disease outcomes. J Am Acad Dermatol. 2018;79:617-633. doi: 10.1016/j.jaad.2018.01.023
The patient’s history and the classic morphology of raised plaques was consistent with chronic spontaneous urticaria. Erythema may be subtle or not visible in patients with skin of color.
Individual urticarial lesions last less than 24 hours with itching and burning. Angioedema also occurs, and manifests as a deeper edema with itching, burning, and pain. Symptoms typically last for 2 to 3 days and involve the eyelids, lips, and tongue.
Chronic urticaria (CU) is defined as episodes of spontaneous wheals or angioedema lasting for more than 6 weeks and is subdivided into chronic spontaneous urticaria or inducible urticaria (if there is a known cause). Triggers include infection, emotional stressors, or medications (eg, angiotensin-converting enzyme inhibitors, nonsteroidal anti-inflammatory drugs). Autoimmunity is seen in one-third of CU patients.1
Only a limited routine-diagnostic work-up is necessary for CU and it may include a complete blood count with differential and erythrocyte sedimentation rate and C-reactive protein testing. Further diagnostic testing is based on history and may include functional autoantibodies, thyroid stimulating hormone, and thyroid autoantibodies.
The initial step in treatment involves identification and elimination of triggers. If this is not possible, first-line therapy includes second-generation antihistamines. If symptoms persist beyond 2 weeks, the dose of the antihistamine is increased up to 4-fold. Patients should be counseled that the lowest necessary dose needs to be taken habitually to prevent urticaria. If symptoms persist, omalizumab, a recombinant humanized IgG monoclonal antibody against serum IgE, cyclosporine, or montelukast, may be added. Leukotriene-receptor antagonists such as montelukast were previously second-line therapy, but they have had mixed results in randomized controlled trials. With a much lower cost than omalizumab, leukotriene-receptor antagonists are a reasonable alternative for patients who are refractory to antihistamines.1
This patient was given high-dose nonsedating antihistamines; she experienced sedation and inadequate relief. A prior authorization was successfully obtained, and she was prescribed omalizumab.
Image courtesy of Kriti Mishra, MD, Department of Dermatology, University of New Mexico School of Medicine, Albuquerque. Text courtesy of Kriti Mishra, MD, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
The patient’s history and the classic morphology of raised plaques was consistent with chronic spontaneous urticaria. Erythema may be subtle or not visible in patients with skin of color.
Individual urticarial lesions last less than 24 hours with itching and burning. Angioedema also occurs, and manifests as a deeper edema with itching, burning, and pain. Symptoms typically last for 2 to 3 days and involve the eyelids, lips, and tongue.
Chronic urticaria (CU) is defined as episodes of spontaneous wheals or angioedema lasting for more than 6 weeks and is subdivided into chronic spontaneous urticaria or inducible urticaria (if there is a known cause). Triggers include infection, emotional stressors, or medications (eg, angiotensin-converting enzyme inhibitors, nonsteroidal anti-inflammatory drugs). Autoimmunity is seen in one-third of CU patients.1
Only a limited routine-diagnostic work-up is necessary for CU and it may include a complete blood count with differential and erythrocyte sedimentation rate and C-reactive protein testing. Further diagnostic testing is based on history and may include functional autoantibodies, thyroid stimulating hormone, and thyroid autoantibodies.
The initial step in treatment involves identification and elimination of triggers. If this is not possible, first-line therapy includes second-generation antihistamines. If symptoms persist beyond 2 weeks, the dose of the antihistamine is increased up to 4-fold. Patients should be counseled that the lowest necessary dose needs to be taken habitually to prevent urticaria. If symptoms persist, omalizumab, a recombinant humanized IgG monoclonal antibody against serum IgE, cyclosporine, or montelukast, may be added. Leukotriene-receptor antagonists such as montelukast were previously second-line therapy, but they have had mixed results in randomized controlled trials. With a much lower cost than omalizumab, leukotriene-receptor antagonists are a reasonable alternative for patients who are refractory to antihistamines.1
This patient was given high-dose nonsedating antihistamines; she experienced sedation and inadequate relief. A prior authorization was successfully obtained, and she was prescribed omalizumab.
Image courtesy of Kriti Mishra, MD, Department of Dermatology, University of New Mexico School of Medicine, Albuquerque. Text courtesy of Kriti Mishra, MD, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Antia C, Baquerizo K, Korman A, et al. Urticaria: a comprehensive review: treatment of chronic urticaria, special populations, and disease outcomes. J Am Acad Dermatol. 2018;79:617-633. doi: 10.1016/j.jaad.2018.01.023
1. Antia C, Baquerizo K, Korman A, et al. Urticaria: a comprehensive review: treatment of chronic urticaria, special populations, and disease outcomes. J Am Acad Dermatol. 2018;79:617-633. doi: 10.1016/j.jaad.2018.01.023
Leg rash
The appearance and location of this rash are classic signs for necrobiosis lipoidica, a chronic granulomatous skin disease commonly associated with diabetes. The patient’s initial hemoglobin A1c was 12.4%, confirming a diagnosis of type 2 diabetes, and a punch biopsy of the lesion demonstrated a broad zone of necrobiosis in the mid to lower dermis and a chronic inflammatory infiltrate, including plasma cells.
Necrobiosis lipoidica is rare, typically affects middle-aged adults, and is more common in women than in men.1 Although commonly associated with diabetes (hence the historical name necrobiosis lipoidica diabeticorum), a significant number of cases occur in patients without diabetes.2 The pathogenesis is not fully understood. The condition first appears as asymptomatic yellow to red-brown papules and plaques, most commonly on the anterior legs. The lesions then flatten over time, forming broad, yellow-pink patches and plaques.1,2
Generally, the diagnosis can be made clinically but, if uncertain, a punch biopsy is the preferred technique for confirmation. The differential diagnosis includes chronic cutaneous lupus erythematosus (LE), sarcoidosis, and dermatophytosis. Although the appearance of lesions associated with LE or sarcoidosis can vary, neither one manifests with the yellow coloring seen here. Dermatophytosis typically demonstrates scale and pruritus with an active border; viewing a potassium hydroxide preparation of a skin scraping is usually sufficient to make a diagnosis.
Treatment for necrobiosis lipoidica includes counseling patients to avoid trauma to the affected areas, high-potency topical corticosteroids, and photodynamic therapy.3 Often, lesions are permanent.
For this patient’s diabetes treatment, she was prescribed metformin and insulin glargine and counseled extensively on weight loss, regular exercise, and appropriate diet adjustments. The rash was treated topically with triamcinolone 0.1% cream bid. At her 4-month follow-up, the patient’s hemoglobin A1c value had dropped to 5.4%, and the rash had become less prominent and widespread. The patient was pleased with the cosmetic outcome and declined referral to a dermatologist for further treatment.
Photo and text courtesy of Samuel Dickmann, MD, and James Medley, MD, University of Florida College of Medicine, Gainesville.
1. Hashemi DA, Brown-Joel ZO, Tkachenko E, et al. Clinical features and comorbidities of patients with necrobiosis lipoidica with or without diabetes. JAMA Dermatol. 2019;155:455-459. doi: 10.1001/jamadermatol.2018.5635
2. O’Toole EA, Kennedy U, Nolan JJ, et al. Necrobiosis lipoidica: only a minority of patients have diabetes mellitus. Br J Dermatol. 1999;140:283-286. doi: 10.1046/j.1365-2133.1999.02663.x
3. Heidenheim M, Jemec GBE. Successful treatment of necrobiosis lipoidica diabeticorum with photodynamic therapy. Arch Dermatol. 2006;142:1548-1550. doi: 10.1001/archderm.142.12.1548
The appearance and location of this rash are classic signs for necrobiosis lipoidica, a chronic granulomatous skin disease commonly associated with diabetes. The patient’s initial hemoglobin A1c was 12.4%, confirming a diagnosis of type 2 diabetes, and a punch biopsy of the lesion demonstrated a broad zone of necrobiosis in the mid to lower dermis and a chronic inflammatory infiltrate, including plasma cells.
Necrobiosis lipoidica is rare, typically affects middle-aged adults, and is more common in women than in men.1 Although commonly associated with diabetes (hence the historical name necrobiosis lipoidica diabeticorum), a significant number of cases occur in patients without diabetes.2 The pathogenesis is not fully understood. The condition first appears as asymptomatic yellow to red-brown papules and plaques, most commonly on the anterior legs. The lesions then flatten over time, forming broad, yellow-pink patches and plaques.1,2
Generally, the diagnosis can be made clinically but, if uncertain, a punch biopsy is the preferred technique for confirmation. The differential diagnosis includes chronic cutaneous lupus erythematosus (LE), sarcoidosis, and dermatophytosis. Although the appearance of lesions associated with LE or sarcoidosis can vary, neither one manifests with the yellow coloring seen here. Dermatophytosis typically demonstrates scale and pruritus with an active border; viewing a potassium hydroxide preparation of a skin scraping is usually sufficient to make a diagnosis.
Treatment for necrobiosis lipoidica includes counseling patients to avoid trauma to the affected areas, high-potency topical corticosteroids, and photodynamic therapy.3 Often, lesions are permanent.
For this patient’s diabetes treatment, she was prescribed metformin and insulin glargine and counseled extensively on weight loss, regular exercise, and appropriate diet adjustments. The rash was treated topically with triamcinolone 0.1% cream bid. At her 4-month follow-up, the patient’s hemoglobin A1c value had dropped to 5.4%, and the rash had become less prominent and widespread. The patient was pleased with the cosmetic outcome and declined referral to a dermatologist for further treatment.
Photo and text courtesy of Samuel Dickmann, MD, and James Medley, MD, University of Florida College of Medicine, Gainesville.
The appearance and location of this rash are classic signs for necrobiosis lipoidica, a chronic granulomatous skin disease commonly associated with diabetes. The patient’s initial hemoglobin A1c was 12.4%, confirming a diagnosis of type 2 diabetes, and a punch biopsy of the lesion demonstrated a broad zone of necrobiosis in the mid to lower dermis and a chronic inflammatory infiltrate, including plasma cells.
Necrobiosis lipoidica is rare, typically affects middle-aged adults, and is more common in women than in men.1 Although commonly associated with diabetes (hence the historical name necrobiosis lipoidica diabeticorum), a significant number of cases occur in patients without diabetes.2 The pathogenesis is not fully understood. The condition first appears as asymptomatic yellow to red-brown papules and plaques, most commonly on the anterior legs. The lesions then flatten over time, forming broad, yellow-pink patches and plaques.1,2
Generally, the diagnosis can be made clinically but, if uncertain, a punch biopsy is the preferred technique for confirmation. The differential diagnosis includes chronic cutaneous lupus erythematosus (LE), sarcoidosis, and dermatophytosis. Although the appearance of lesions associated with LE or sarcoidosis can vary, neither one manifests with the yellow coloring seen here. Dermatophytosis typically demonstrates scale and pruritus with an active border; viewing a potassium hydroxide preparation of a skin scraping is usually sufficient to make a diagnosis.
Treatment for necrobiosis lipoidica includes counseling patients to avoid trauma to the affected areas, high-potency topical corticosteroids, and photodynamic therapy.3 Often, lesions are permanent.
For this patient’s diabetes treatment, she was prescribed metformin and insulin glargine and counseled extensively on weight loss, regular exercise, and appropriate diet adjustments. The rash was treated topically with triamcinolone 0.1% cream bid. At her 4-month follow-up, the patient’s hemoglobin A1c value had dropped to 5.4%, and the rash had become less prominent and widespread. The patient was pleased with the cosmetic outcome and declined referral to a dermatologist for further treatment.
Photo and text courtesy of Samuel Dickmann, MD, and James Medley, MD, University of Florida College of Medicine, Gainesville.
1. Hashemi DA, Brown-Joel ZO, Tkachenko E, et al. Clinical features and comorbidities of patients with necrobiosis lipoidica with or without diabetes. JAMA Dermatol. 2019;155:455-459. doi: 10.1001/jamadermatol.2018.5635
2. O’Toole EA, Kennedy U, Nolan JJ, et al. Necrobiosis lipoidica: only a minority of patients have diabetes mellitus. Br J Dermatol. 1999;140:283-286. doi: 10.1046/j.1365-2133.1999.02663.x
3. Heidenheim M, Jemec GBE. Successful treatment of necrobiosis lipoidica diabeticorum with photodynamic therapy. Arch Dermatol. 2006;142:1548-1550. doi: 10.1001/archderm.142.12.1548
1. Hashemi DA, Brown-Joel ZO, Tkachenko E, et al. Clinical features and comorbidities of patients with necrobiosis lipoidica with or without diabetes. JAMA Dermatol. 2019;155:455-459. doi: 10.1001/jamadermatol.2018.5635
2. O’Toole EA, Kennedy U, Nolan JJ, et al. Necrobiosis lipoidica: only a minority of patients have diabetes mellitus. Br J Dermatol. 1999;140:283-286. doi: 10.1046/j.1365-2133.1999.02663.x
3. Heidenheim M, Jemec GBE. Successful treatment of necrobiosis lipoidica diabeticorum with photodynamic therapy. Arch Dermatol. 2006;142:1548-1550. doi: 10.1001/archderm.142.12.1548
Hand ulceration
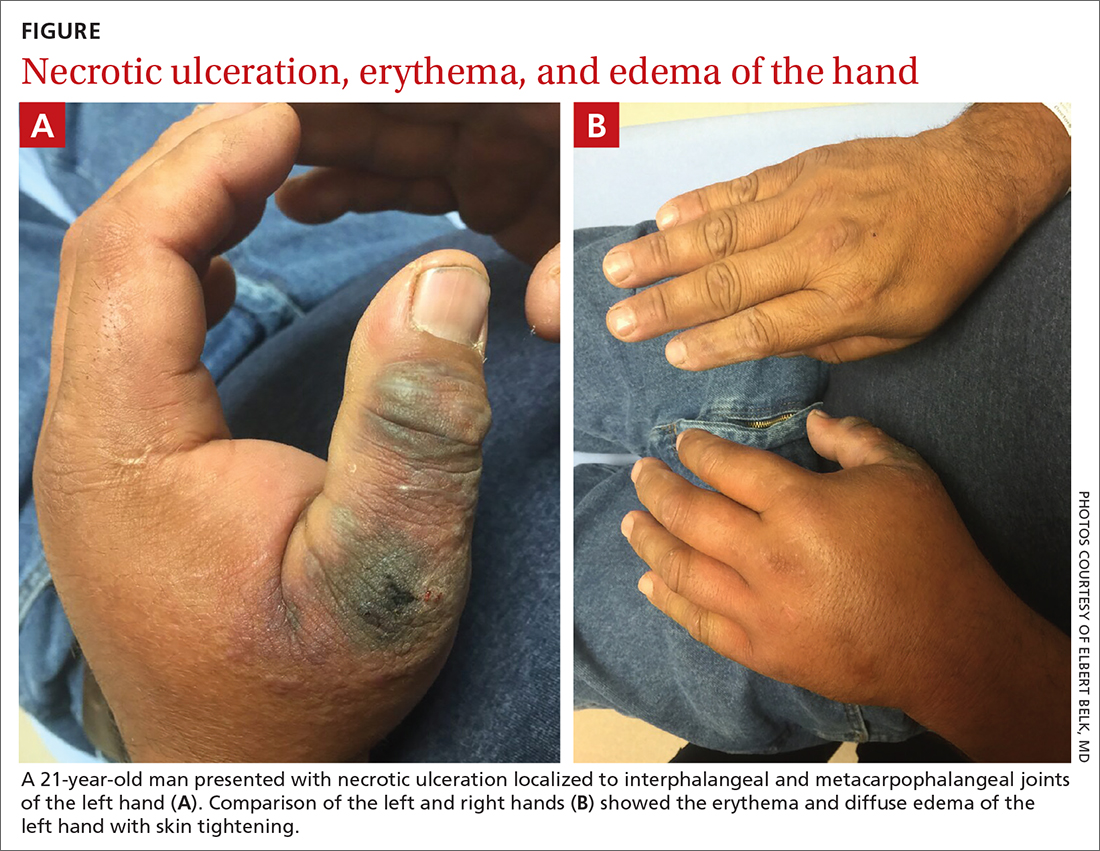
A 45-year-old man presented to a south Texas emergency department with a red, tender, edematous left hand. Earlier that day, he had been working in an oil field when his hand suddenly began to hurt.
On physical exam, puncture wounds were visible at the metacarpophalangeal joint of the thumb and the interphalangeal joint, dorsal aspect; the area was surrounded by necrotic black tissue (FIGURE). Additionally, erythema with extensive edema extended distally to the proximal interphalangeal joints of each digit. Upon palpation, the area was warm, firm, and tender, with the edema tracking proximally to his mid-forearm.
The patient had a temperature of 99.5 °F; his other vital signs were normal. His past medical history included hypertension.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Cellulitis, compartment syndrome by scorpion sting
Based on the necrotic puncture wounds, unilateral distribution of the swelling, and the patient’s acknowledgement that he’d seen a scorpion in his work environment prior to symptom onset, he was given a diagnosis of cellulitis with secondary compartment syndrome following a scorpion sting.
A geographic problem
In the United States, there are approximately 17,000 reported cases of scorpion stings every year, with fewer than 11 related deaths reported between 1999 and 2014.1 These cases tend to follow a geographic distribution along the American Southwest, with the highest incidence occurring in Arizona, followed by Texas; the majority of cases occur during the summer months.1
The most clinically relevant scorpion in the United States is the Centruroides sculpturatus, also known as the Arizona bark scorpion.2Centruroides spp can be recognized by a slender, yellow to light brown or tan body measuring 1.3 cm to 7.6 cm in length. There is a tubercule at the base of the stringer, a defining characteristic of the species.3
Urgent care is necessary for more severe symptoms
The most common complaint following a scorpion sting tends to be pain (88.7%), followed by numbness, edema, and erythema.1 Other signs and symptoms include muscle spasms, hypertension, and salivation. Symptoms can persist for 10 to 48 hours. Cardiovascular collapse and disseminated intravascular coagulation are 2 potentially fatal complications of a scorpion sting.
The diagnosis is made clinically based on history and physical exam findings; a complete blood count, coagulation panel, and creatine kinase and amylase/lipase bloodwork may be ordered to assess for end-organ complications. Local serious complications, such as compartment syndrome, should be urgently referred for surgical management.
Continue to: Signs of compartment syndrome...
Signs of compartment syndrome include tense, swollen compartments and pain with passive stretching of muscles within the compartment. Rapid progression of symptoms, as seen in this case, is also a red flag.
Differential diagnosis includes necrotizing fasciitis
The differential diagnosis includes uncomplicated cellulitis, as well as necrotizing fasciitis and methicillin-resistant Staphylococcus aureus (MRSA) cellulitis.
Necrotizing fasciitis. The lack of subcutaneous crackles and pain that is out of proportion to touch, as well as relatively normal vital signs, ruled out a diagnosis of necrotizing fasciitis in this case.
Community-acquired MRSA is seen with purulent cellulitis. However, this patient had no purulent discharge.
Antivenom is only needed for severe cases
Treatment is primarily supportive; all patients should have the wound thoroughly cleaned, and pain can be controlled using nonsteroidal anti-inflammatory drugs or opioid therapy.2 Tetanus prophylaxis should be given. The Centruroides antivenom, Anascorp, should be considered for patients with severe symptoms, including loss of muscle control, roving or abnormal eye movements, slurred speech, respiratory distress, excessive salivation, frothing at the mouth, and vomiting.4 In most cases, local poison control centers should be consulted for advice on management and to answer questions about antivenom availability.
Our patient was admitted to the hospital and an urgent surgery consult was obtained. The surgeon performed a fasciotomy to treat the compartment syndrome, and the patient survived without loss of his hand or arm.
1. Kang AM, Brooks DE. Nationwide scorpion exposures reported to US poison control centers from 2005 to 2015. J Med Toxicol. 2017;13:158-165. doi: 10.1007/s13181-016-0594-0
2. Barish RA, Arnold T. Scorpion Stings. Merck Manual. Updated April 2020. Accessed June 26, 2021. https://www.merckmanuals.com/professional/injuries-poisoning/bites-and-stings/scorpion-stings
3. González-Santillán E, Possani LD. North American scorpion species of public health importance with reappraisal of historical epidemiology. Acta Trop. 2018;187:264-274. doi: 10.1016/j.actatropica.2018.08.002
4. Anascorp. Package insert. Accredo Health Group, Inc; 2011.
A 45-year-old man presented to a south Texas emergency department with a red, tender, edematous left hand. Earlier that day, he had been working in an oil field when his hand suddenly began to hurt.
On physical exam, puncture wounds were visible at the metacarpophalangeal joint of the thumb and the interphalangeal joint, dorsal aspect; the area was surrounded by necrotic black tissue (FIGURE). Additionally, erythema with extensive edema extended distally to the proximal interphalangeal joints of each digit. Upon palpation, the area was warm, firm, and tender, with the edema tracking proximally to his mid-forearm.
The patient had a temperature of 99.5 °F; his other vital signs were normal. His past medical history included hypertension.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Cellulitis, compartment syndrome by scorpion sting
Based on the necrotic puncture wounds, unilateral distribution of the swelling, and the patient’s acknowledgement that he’d seen a scorpion in his work environment prior to symptom onset, he was given a diagnosis of cellulitis with secondary compartment syndrome following a scorpion sting.
A geographic problem
In the United States, there are approximately 17,000 reported cases of scorpion stings every year, with fewer than 11 related deaths reported between 1999 and 2014.1 These cases tend to follow a geographic distribution along the American Southwest, with the highest incidence occurring in Arizona, followed by Texas; the majority of cases occur during the summer months.1
The most clinically relevant scorpion in the United States is the Centruroides sculpturatus, also known as the Arizona bark scorpion.2Centruroides spp can be recognized by a slender, yellow to light brown or tan body measuring 1.3 cm to 7.6 cm in length. There is a tubercule at the base of the stringer, a defining characteristic of the species.3
Urgent care is necessary for more severe symptoms
The most common complaint following a scorpion sting tends to be pain (88.7%), followed by numbness, edema, and erythema.1 Other signs and symptoms include muscle spasms, hypertension, and salivation. Symptoms can persist for 10 to 48 hours. Cardiovascular collapse and disseminated intravascular coagulation are 2 potentially fatal complications of a scorpion sting.
The diagnosis is made clinically based on history and physical exam findings; a complete blood count, coagulation panel, and creatine kinase and amylase/lipase bloodwork may be ordered to assess for end-organ complications. Local serious complications, such as compartment syndrome, should be urgently referred for surgical management.
Continue to: Signs of compartment syndrome...
Signs of compartment syndrome include tense, swollen compartments and pain with passive stretching of muscles within the compartment. Rapid progression of symptoms, as seen in this case, is also a red flag.
Differential diagnosis includes necrotizing fasciitis
The differential diagnosis includes uncomplicated cellulitis, as well as necrotizing fasciitis and methicillin-resistant Staphylococcus aureus (MRSA) cellulitis.
Necrotizing fasciitis. The lack of subcutaneous crackles and pain that is out of proportion to touch, as well as relatively normal vital signs, ruled out a diagnosis of necrotizing fasciitis in this case.
Community-acquired MRSA is seen with purulent cellulitis. However, this patient had no purulent discharge.
Antivenom is only needed for severe cases
Treatment is primarily supportive; all patients should have the wound thoroughly cleaned, and pain can be controlled using nonsteroidal anti-inflammatory drugs or opioid therapy.2 Tetanus prophylaxis should be given. The Centruroides antivenom, Anascorp, should be considered for patients with severe symptoms, including loss of muscle control, roving or abnormal eye movements, slurred speech, respiratory distress, excessive salivation, frothing at the mouth, and vomiting.4 In most cases, local poison control centers should be consulted for advice on management and to answer questions about antivenom availability.
Our patient was admitted to the hospital and an urgent surgery consult was obtained. The surgeon performed a fasciotomy to treat the compartment syndrome, and the patient survived without loss of his hand or arm.
A 45-year-old man presented to a south Texas emergency department with a red, tender, edematous left hand. Earlier that day, he had been working in an oil field when his hand suddenly began to hurt.
On physical exam, puncture wounds were visible at the metacarpophalangeal joint of the thumb and the interphalangeal joint, dorsal aspect; the area was surrounded by necrotic black tissue (FIGURE). Additionally, erythema with extensive edema extended distally to the proximal interphalangeal joints of each digit. Upon palpation, the area was warm, firm, and tender, with the edema tracking proximally to his mid-forearm.
The patient had a temperature of 99.5 °F; his other vital signs were normal. His past medical history included hypertension.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Cellulitis, compartment syndrome by scorpion sting
Based on the necrotic puncture wounds, unilateral distribution of the swelling, and the patient’s acknowledgement that he’d seen a scorpion in his work environment prior to symptom onset, he was given a diagnosis of cellulitis with secondary compartment syndrome following a scorpion sting.
A geographic problem
In the United States, there are approximately 17,000 reported cases of scorpion stings every year, with fewer than 11 related deaths reported between 1999 and 2014.1 These cases tend to follow a geographic distribution along the American Southwest, with the highest incidence occurring in Arizona, followed by Texas; the majority of cases occur during the summer months.1
The most clinically relevant scorpion in the United States is the Centruroides sculpturatus, also known as the Arizona bark scorpion.2Centruroides spp can be recognized by a slender, yellow to light brown or tan body measuring 1.3 cm to 7.6 cm in length. There is a tubercule at the base of the stringer, a defining characteristic of the species.3
Urgent care is necessary for more severe symptoms
The most common complaint following a scorpion sting tends to be pain (88.7%), followed by numbness, edema, and erythema.1 Other signs and symptoms include muscle spasms, hypertension, and salivation. Symptoms can persist for 10 to 48 hours. Cardiovascular collapse and disseminated intravascular coagulation are 2 potentially fatal complications of a scorpion sting.
The diagnosis is made clinically based on history and physical exam findings; a complete blood count, coagulation panel, and creatine kinase and amylase/lipase bloodwork may be ordered to assess for end-organ complications. Local serious complications, such as compartment syndrome, should be urgently referred for surgical management.
Continue to: Signs of compartment syndrome...
Signs of compartment syndrome include tense, swollen compartments and pain with passive stretching of muscles within the compartment. Rapid progression of symptoms, as seen in this case, is also a red flag.
Differential diagnosis includes necrotizing fasciitis
The differential diagnosis includes uncomplicated cellulitis, as well as necrotizing fasciitis and methicillin-resistant Staphylococcus aureus (MRSA) cellulitis.
Necrotizing fasciitis. The lack of subcutaneous crackles and pain that is out of proportion to touch, as well as relatively normal vital signs, ruled out a diagnosis of necrotizing fasciitis in this case.
Community-acquired MRSA is seen with purulent cellulitis. However, this patient had no purulent discharge.
Antivenom is only needed for severe cases
Treatment is primarily supportive; all patients should have the wound thoroughly cleaned, and pain can be controlled using nonsteroidal anti-inflammatory drugs or opioid therapy.2 Tetanus prophylaxis should be given. The Centruroides antivenom, Anascorp, should be considered for patients with severe symptoms, including loss of muscle control, roving or abnormal eye movements, slurred speech, respiratory distress, excessive salivation, frothing at the mouth, and vomiting.4 In most cases, local poison control centers should be consulted for advice on management and to answer questions about antivenom availability.
Our patient was admitted to the hospital and an urgent surgery consult was obtained. The surgeon performed a fasciotomy to treat the compartment syndrome, and the patient survived without loss of his hand or arm.
1. Kang AM, Brooks DE. Nationwide scorpion exposures reported to US poison control centers from 2005 to 2015. J Med Toxicol. 2017;13:158-165. doi: 10.1007/s13181-016-0594-0
2. Barish RA, Arnold T. Scorpion Stings. Merck Manual. Updated April 2020. Accessed June 26, 2021. https://www.merckmanuals.com/professional/injuries-poisoning/bites-and-stings/scorpion-stings
3. González-Santillán E, Possani LD. North American scorpion species of public health importance with reappraisal of historical epidemiology. Acta Trop. 2018;187:264-274. doi: 10.1016/j.actatropica.2018.08.002
4. Anascorp. Package insert. Accredo Health Group, Inc; 2011.
1. Kang AM, Brooks DE. Nationwide scorpion exposures reported to US poison control centers from 2005 to 2015. J Med Toxicol. 2017;13:158-165. doi: 10.1007/s13181-016-0594-0
2. Barish RA, Arnold T. Scorpion Stings. Merck Manual. Updated April 2020. Accessed June 26, 2021. https://www.merckmanuals.com/professional/injuries-poisoning/bites-and-stings/scorpion-stings
3. González-Santillán E, Possani LD. North American scorpion species of public health importance with reappraisal of historical epidemiology. Acta Trop. 2018;187:264-274. doi: 10.1016/j.actatropica.2018.08.002
4. Anascorp. Package insert. Accredo Health Group, Inc; 2011.
Separation and discoloration of thumb nail
The color change in this case is subtle, but consistent with green nail syndrome also termed chloronychia.
Green nail syndrome is a form of chronic paronychia caused by Pseudomonas aeruginosa and is associated with frequent water exposure. Pseudomonas expresses pyocyanin and pyoverdine, leading to the characteristic blue or green coloration. A Woods lamp may reveal neon green fluorescence.
Risk factors include frequent water exposure, use of an instrument to relieve symptoms of an ingrown nail, and chronic immunosuppression. In this case, frequent hand washing being performed by this patient during the COVID-19 pandemic was the likely culprit.
The differential diagnosis includes simple structural onycholysis, onychomycosis, and nail psoriasis. Polymicrobial infection can occur. When in doubt, culture or pathologic examination of nail clippings with Grocott methenamine silver and periodic acid–Schiff can identify coincident fungal infection.1 While systemic pseudomonas infection could also occur with green nail syndrome, the latter is usually only a mild nuisance and not associated with severe disease.
Treatment consists of avoidance of water and instrumentation. Topical sodium hypochlorite 2% solution applied to the nail or acetic acid soaks for 2 to 3 weeks is often curative. Antibiotic therapy may also be used. Topical tobramycin or gentamicin are available as otic or ophthalmic drops and can be applied just under the nail.
The patient was advised to meticulously dry her hands after washing them and to apply 1 drop of topical gentamicin solution 0.3% tid for 3 weeks. The green discoloration cleared in 3 weeks and the onycholysis resolved within 4 months.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Ohn J, Yu D-A, Park H, et al. Green nail syndrome: analysis of the association with onychomycosis. J Am Acad Dermatol. 2020;83:940-942. doi: 10.1016/j.jaad.2020.01.040
The color change in this case is subtle, but consistent with green nail syndrome also termed chloronychia.
Green nail syndrome is a form of chronic paronychia caused by Pseudomonas aeruginosa and is associated with frequent water exposure. Pseudomonas expresses pyocyanin and pyoverdine, leading to the characteristic blue or green coloration. A Woods lamp may reveal neon green fluorescence.
Risk factors include frequent water exposure, use of an instrument to relieve symptoms of an ingrown nail, and chronic immunosuppression. In this case, frequent hand washing being performed by this patient during the COVID-19 pandemic was the likely culprit.
The differential diagnosis includes simple structural onycholysis, onychomycosis, and nail psoriasis. Polymicrobial infection can occur. When in doubt, culture or pathologic examination of nail clippings with Grocott methenamine silver and periodic acid–Schiff can identify coincident fungal infection.1 While systemic pseudomonas infection could also occur with green nail syndrome, the latter is usually only a mild nuisance and not associated with severe disease.
Treatment consists of avoidance of water and instrumentation. Topical sodium hypochlorite 2% solution applied to the nail or acetic acid soaks for 2 to 3 weeks is often curative. Antibiotic therapy may also be used. Topical tobramycin or gentamicin are available as otic or ophthalmic drops and can be applied just under the nail.
The patient was advised to meticulously dry her hands after washing them and to apply 1 drop of topical gentamicin solution 0.3% tid for 3 weeks. The green discoloration cleared in 3 weeks and the onycholysis resolved within 4 months.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
The color change in this case is subtle, but consistent with green nail syndrome also termed chloronychia.
Green nail syndrome is a form of chronic paronychia caused by Pseudomonas aeruginosa and is associated with frequent water exposure. Pseudomonas expresses pyocyanin and pyoverdine, leading to the characteristic blue or green coloration. A Woods lamp may reveal neon green fluorescence.
Risk factors include frequent water exposure, use of an instrument to relieve symptoms of an ingrown nail, and chronic immunosuppression. In this case, frequent hand washing being performed by this patient during the COVID-19 pandemic was the likely culprit.
The differential diagnosis includes simple structural onycholysis, onychomycosis, and nail psoriasis. Polymicrobial infection can occur. When in doubt, culture or pathologic examination of nail clippings with Grocott methenamine silver and periodic acid–Schiff can identify coincident fungal infection.1 While systemic pseudomonas infection could also occur with green nail syndrome, the latter is usually only a mild nuisance and not associated with severe disease.
Treatment consists of avoidance of water and instrumentation. Topical sodium hypochlorite 2% solution applied to the nail or acetic acid soaks for 2 to 3 weeks is often curative. Antibiotic therapy may also be used. Topical tobramycin or gentamicin are available as otic or ophthalmic drops and can be applied just under the nail.
The patient was advised to meticulously dry her hands after washing them and to apply 1 drop of topical gentamicin solution 0.3% tid for 3 weeks. The green discoloration cleared in 3 weeks and the onycholysis resolved within 4 months.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Ohn J, Yu D-A, Park H, et al. Green nail syndrome: analysis of the association with onychomycosis. J Am Acad Dermatol. 2020;83:940-942. doi: 10.1016/j.jaad.2020.01.040
1. Ohn J, Yu D-A, Park H, et al. Green nail syndrome: analysis of the association with onychomycosis. J Am Acad Dermatol. 2020;83:940-942. doi: 10.1016/j.jaad.2020.01.040