User login
Former Farmer Is Short of Breath
ANSWER
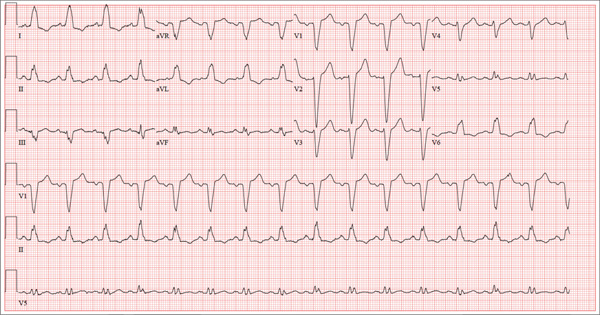
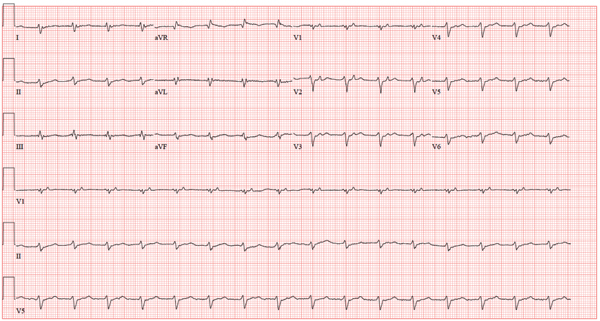
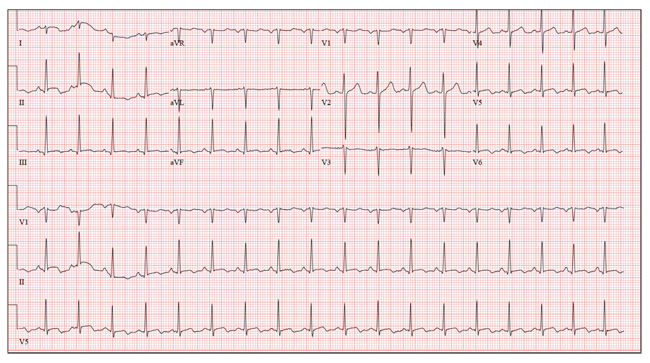
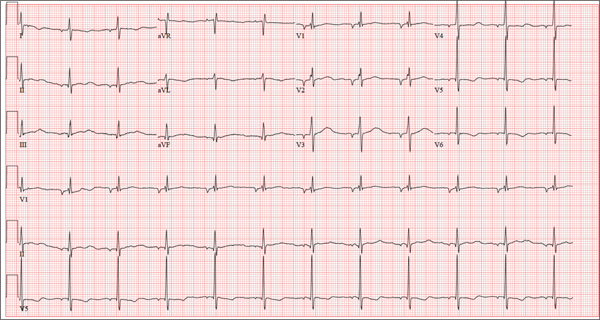
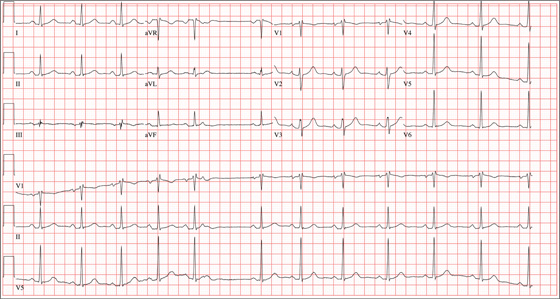
The correct interpretation of this ECG includes normal sinus rhythm with left atrial enlargement and a left bundle branch block (LBBB). Normal sinus rhythm is evidenced by a P wave associated with each QRS complex with a consistent PR interval.
Left atrial enlargement is evidenced by a P-wave duration ≥ 120 ms in lead II, a notched P wave in the limb leads with a peak duration ≥ 4 ms, and a terminal P-wave negativity in lead V1 with a duration ≥ 4 ms and a depth ≥ 1 mm.
An LBBB is illustrated by the QRS duration ≥ 120 ms, a dominant S wave in lead V1, broad monophasic R waves in the lateral leads (including I, aVL, V5, and V6), and R-wave peak times of > 60 ms in leads V5 and V6.
Further work-up revealed elevated left end-diastolic filling pressures, volume overload, and pulmonary edema consistent with diastolic heart failure. Given the unclear etiology of the LBBB, cardiac catheterization was performed. It revealed no significant coronary artery disease.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm with left atrial enlargement and a left bundle branch block (LBBB). Normal sinus rhythm is evidenced by a P wave associated with each QRS complex with a consistent PR interval.
Left atrial enlargement is evidenced by a P-wave duration ≥ 120 ms in lead II, a notched P wave in the limb leads with a peak duration ≥ 4 ms, and a terminal P-wave negativity in lead V1 with a duration ≥ 4 ms and a depth ≥ 1 mm.
An LBBB is illustrated by the QRS duration ≥ 120 ms, a dominant S wave in lead V1, broad monophasic R waves in the lateral leads (including I, aVL, V5, and V6), and R-wave peak times of > 60 ms in leads V5 and V6.
Further work-up revealed elevated left end-diastolic filling pressures, volume overload, and pulmonary edema consistent with diastolic heart failure. Given the unclear etiology of the LBBB, cardiac catheterization was performed. It revealed no significant coronary artery disease.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm with left atrial enlargement and a left bundle branch block (LBBB). Normal sinus rhythm is evidenced by a P wave associated with each QRS complex with a consistent PR interval.
Left atrial enlargement is evidenced by a P-wave duration ≥ 120 ms in lead II, a notched P wave in the limb leads with a peak duration ≥ 4 ms, and a terminal P-wave negativity in lead V1 with a duration ≥ 4 ms and a depth ≥ 1 mm.
An LBBB is illustrated by the QRS duration ≥ 120 ms, a dominant S wave in lead V1, broad monophasic R waves in the lateral leads (including I, aVL, V5, and V6), and R-wave peak times of > 60 ms in leads V5 and V6.
Further work-up revealed elevated left end-diastolic filling pressures, volume overload, and pulmonary edema consistent with diastolic heart failure. Given the unclear etiology of the LBBB, cardiac catheterization was performed. It revealed no significant coronary artery disease.
A 67-year-old man has a history of chronic dyspnea. He is a retired farmer who says he “never had time” to seek medical help for anything other than cuts or broken bones. In the past two months, he’s noticed that his dyspnea has progressively worsened. When questioned, he admits that his legs began swelling around that time as well. Two days ago, he awoke from sleep unable to catch his breath. This morning, while walking to his mailbox, he became profoundly short of breath. He sat down by the side of the road and called 911. When the ambulance arrived, he felt much better but agreed to be taken to the emergency department, since his wife is away and he’s home alone. When questioned by the paramedics, he denied having chest pain, palpitations, productive or nonproductive cough, polyuria, polydipsia, nausea, or vomiting. Medical history is positive for hypertension, gastroesophageal reflux disease (GERD), and hypertension. He has had several fractures in his right ankle and left femur, which are well healed. Surgical history is remarkable for a cholecystectomy and multiple laceration repairs on his arms and hands (also well healed). His current medications include one aspirin per day and “a handful” of calcium carbonate tablets. Although he was prescribed “several heart pills” for hypertension, he hasn’t taken them or refilled the prescriptions for at least five years. He is allergic to penicillin and sulfa. He denies recreational or homeopathic drug use. He has never smoked, and he drinks one or two shots of bourbon on weekends. Family history includes a father who died in a farming accident and a mother who died of cervical cancer at age 85. He has seven siblings, all of whom are alive and well. The review of systems is remarkable only for GERD. Physical exam reveals a well-developed, obese male with a height of 6 ft 4 in and a weight of 278 lb. Vital signs include a blood pressure of 184/98 mm Hg; pulse, 90 beats/min; and respiratory rate, 20 breaths/min-1. He is afebrile. The HEENT exam is remarkable for atrophic glossitis. The neck shows no evidence of thyromegaly, and there are no carotid bruits or jugular venous distention. The chest is remarkable for diffuse wheezing and crackles in all lung bases. The cardiac exam reveals a regular rate of 90 beats/min, with no evidence of murmurs, rubs, or gallops. The abdomen is obese. There is no evidence of ascites or masses. Evidence of 2+ pitting edema to the midcalf is present bilaterally. The neurologic exam is grossly intact, and the psychiatric exam reveals the patient to be alert and oriented, with a bright affect. The working diagnosis in the emergency department is acute or chronic heart failure. A chest x-ray reveals moderate-to-severe pulmonary edema, cardiomegaly, and small bilateral effusions. Pertinent laboratory data include a serum glucose of 200 mg/dL and a B-type natriuretic peptide level of 590 pg/mL. All other lab values are within normal limits. An ECG reveals the following: a ventricular rate of 93 beats/min; PR interval, 168 ms; QRS duration, 156 ms; QT/QTc interval, 430/534 ms; P axis, 52°; R axis, 9°; and T axis, 171°. What is your interpretation of this ECG?
Is Lingering “Flu” Responsible for Lethargy?
ANSWER
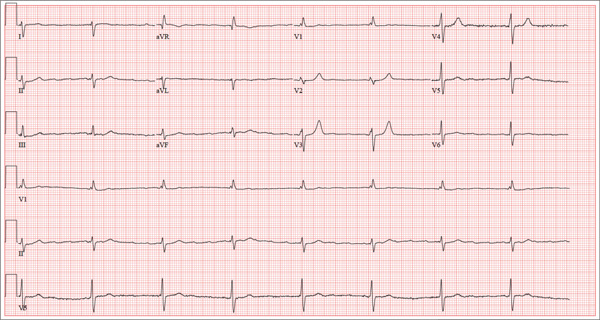
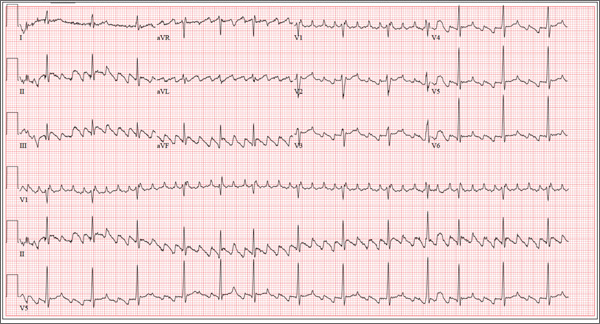
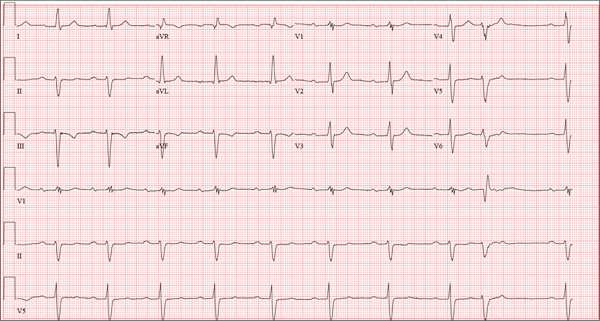
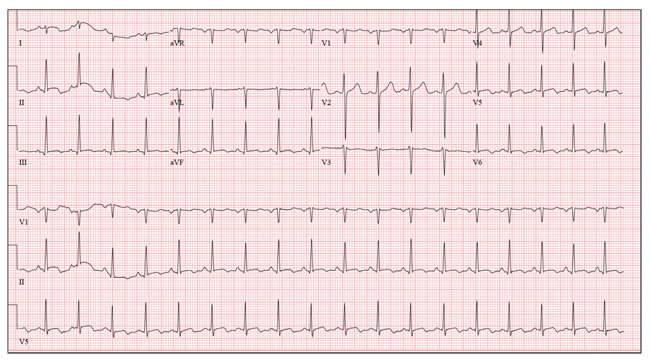
This ECG shows a junctional rhythm with a rate of 47 beats/min and an incomplete right bundle branch block (RBBB). The QRS complexes are narrow, indicating conduction originating at or above the atrioventricular (AV) node.
With the absence of a P wave for every QRS complex, the origin of each beat occurs at the level of the AV node, with depolarization of the ventricles via the normal conduction pathway. Intrinsic automaticity of the AV node results in a rate of 40 to 60 beats/min. There may be retrograde conduction from the AV node into the atria; however, it is not apparent in this ECG.
An incomplete RBBB is evidenced by a QRS complex with a duration > 100 ms and ≤ 120 ms with a terminal R wave (eg, rsR’) in lead V1 and a slurred S wave in leads I and V6 (more common with complete RBBB).
The presence of new-onset junctional rhythm with an incomplete RBBB is suspicious for conduction system disease. Given her symptomatic bradycardia, the patient underwent implantation of a dual-chamber permanent pacemaker. She has since returned to her normal activities.
Of note: Careful examination of the baseline in this tracing raises suspicion for atrial fibrillation (AF). However, according to her primary care provider, this patient had had no previous episodes of AF. Intracardiac electrograms taken during her pacemaker implantation ruled out this diagnosis.
ANSWER
This ECG shows a junctional rhythm with a rate of 47 beats/min and an incomplete right bundle branch block (RBBB). The QRS complexes are narrow, indicating conduction originating at or above the atrioventricular (AV) node.
With the absence of a P wave for every QRS complex, the origin of each beat occurs at the level of the AV node, with depolarization of the ventricles via the normal conduction pathway. Intrinsic automaticity of the AV node results in a rate of 40 to 60 beats/min. There may be retrograde conduction from the AV node into the atria; however, it is not apparent in this ECG.
An incomplete RBBB is evidenced by a QRS complex with a duration > 100 ms and ≤ 120 ms with a terminal R wave (eg, rsR’) in lead V1 and a slurred S wave in leads I and V6 (more common with complete RBBB).
The presence of new-onset junctional rhythm with an incomplete RBBB is suspicious for conduction system disease. Given her symptomatic bradycardia, the patient underwent implantation of a dual-chamber permanent pacemaker. She has since returned to her normal activities.
Of note: Careful examination of the baseline in this tracing raises suspicion for atrial fibrillation (AF). However, according to her primary care provider, this patient had had no previous episodes of AF. Intracardiac electrograms taken during her pacemaker implantation ruled out this diagnosis.
ANSWER
This ECG shows a junctional rhythm with a rate of 47 beats/min and an incomplete right bundle branch block (RBBB). The QRS complexes are narrow, indicating conduction originating at or above the atrioventricular (AV) node.
With the absence of a P wave for every QRS complex, the origin of each beat occurs at the level of the AV node, with depolarization of the ventricles via the normal conduction pathway. Intrinsic automaticity of the AV node results in a rate of 40 to 60 beats/min. There may be retrograde conduction from the AV node into the atria; however, it is not apparent in this ECG.
An incomplete RBBB is evidenced by a QRS complex with a duration > 100 ms and ≤ 120 ms with a terminal R wave (eg, rsR’) in lead V1 and a slurred S wave in leads I and V6 (more common with complete RBBB).
The presence of new-onset junctional rhythm with an incomplete RBBB is suspicious for conduction system disease. Given her symptomatic bradycardia, the patient underwent implantation of a dual-chamber permanent pacemaker. She has since returned to her normal activities.
Of note: Careful examination of the baseline in this tracing raises suspicion for atrial fibrillation (AF). However, according to her primary care provider, this patient had had no previous episodes of AF. Intracardiac electrograms taken during her pacemaker implantation ruled out this diagnosis.
Accompanied by her daughter, whom she is visiting from out of town, a 72-year-old woman presents with a two-week history of lethargy. She says she had “the flu” three weeks ago and just can’t seem to recover from it. According to her daughter, she doesn’t appear ill but seems to tire very easily after simple tasks such as walking from her bedroom to the kitchen. The patient denies fever, chills, orthopnea, dyspnea, and cough. There have been no episodes of near-syncope or syncope. She repeatedly states that she is “just so tired.” Prior to the onset of her flulike symptoms, she was very active in her retirement community, dancing, gardening, and going on sponsored trips to a local casino without difficulty. She says she wouldn’t even attempt those activities in her current state, as any activity immediately exhausts her. Medical history is remarkable for hypertension, hypothyroidism, osteoarthritis, and diabetes. Surgical history is remarkable for a cholecystectomy, abdominal hysterectomy, and removal of several lipomas from her upper extremities. Her current medications include aspirin, hydrochlorothiazide, lisinopril, metformin, and levothyroxine. She is allergic to penicillin and sulfa, both of which cause hives and flushing. Social history reveals that she is a retired junior high school librarian, the mother of three living children, and a widow. She is a smoker, with a one-pack-per-day history from age 14 until her husband died four years ago. She quit at that time but has recently started again, smoking half a pack per day (but “only” when she goes to the casino). She does not use alcohol or recreational drugs. The review of systems is positive for corrective lenses and symptoms suggestive of a urinary tract infection. On physical exam, her blood pressure is 138/92 mm Hg; pulse, 50 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 98.4°F. Her weight is 224 lb, and her height is 62 in. She walks with the assistance of a cane and appears tired and apprehensive. Pertinent physical findings include bilateral cataracts, clear lung fields, and a soft, early systolic murmur at the left lower sternal border. She has two well-healed scars on her abdomen and multiple well-healed scars on both upper extremities. Her hands show evidence of osteoarthritis, and she has limited range of motion but no pain in her right hip. The neurologic exam is grossly intact. Laboratory tests and an ECG are performed. The ECG findings include a ventricular rate of 47 beats/min; PR interval, not measured; QRS duration, 120 ms; QT/QTc interval, 454/401 ms; P axis, not measured; R axis, 171°; and T axis, 51°. What is your interpretation of this ECG—and does it provide an explanation for the patient’s recent lethargy?
Now Insured, Patient Wants to “Get Checked Out”
ANSWER
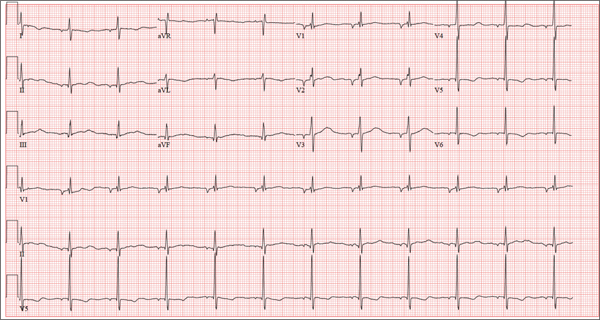
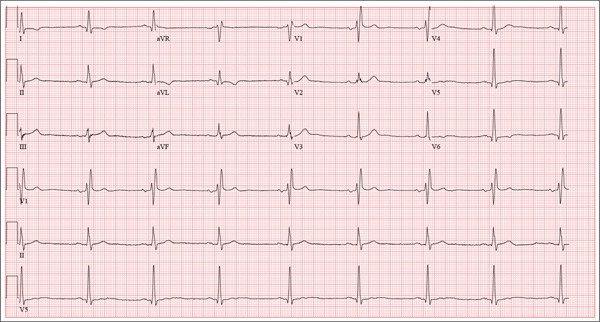
There are three findings on this ECG: unusual P waves consistent with a possible ectopic atrial rhythm, a prolonged QT interval, and T-wave abnormalities in the lateral leads.
Note that the P waves are negative in leads I and II, as well as in all chest leads. This is highly suggestive of an ectopic atrial rhythm originating low in the atria, conducting retrograde into the atria, and overriding the sinoatrial node. Limb lead reversal would result in negative P waves in lead I, but not in other leads.
A prolonged QT interval is determined by consulting any of the standard charts that correlate maximum heart rates with QT intervals and gender. In men, the QT interval is considered “prolonged” when it exceeds 440 ms, unless the heart rate is extremely slow.
Finally, T-wave inversions are present in the lateral leads (V5, V6). Although this may be an indication of lateral ischemia, there is no clinical correlation in this patient.
ANSWER
There are three findings on this ECG: unusual P waves consistent with a possible ectopic atrial rhythm, a prolonged QT interval, and T-wave abnormalities in the lateral leads.
Note that the P waves are negative in leads I and II, as well as in all chest leads. This is highly suggestive of an ectopic atrial rhythm originating low in the atria, conducting retrograde into the atria, and overriding the sinoatrial node. Limb lead reversal would result in negative P waves in lead I, but not in other leads.
A prolonged QT interval is determined by consulting any of the standard charts that correlate maximum heart rates with QT intervals and gender. In men, the QT interval is considered “prolonged” when it exceeds 440 ms, unless the heart rate is extremely slow.
Finally, T-wave inversions are present in the lateral leads (V5, V6). Although this may be an indication of lateral ischemia, there is no clinical correlation in this patient.
ANSWER
There are three findings on this ECG: unusual P waves consistent with a possible ectopic atrial rhythm, a prolonged QT interval, and T-wave abnormalities in the lateral leads.
Note that the P waves are negative in leads I and II, as well as in all chest leads. This is highly suggestive of an ectopic atrial rhythm originating low in the atria, conducting retrograde into the atria, and overriding the sinoatrial node. Limb lead reversal would result in negative P waves in lead I, but not in other leads.
A prolonged QT interval is determined by consulting any of the standard charts that correlate maximum heart rates with QT intervals and gender. In men, the QT interval is considered “prolonged” when it exceeds 440 ms, unless the heart rate is extremely slow.
Finally, T-wave inversions are present in the lateral leads (V5, V6). Although this may be an indication of lateral ischemia, there is no clinical correlation in this patient.
A 37-year-old man presents to your office to establish care. After being unemployed for two years, he recently obtained a position with a local manufacturing company and, as a result, has health benefits. He wants to “get checked out.” He has not seen a health care provider since having his tonsils removed at age 14. He says he is rarely ill, aside from an occasional cold. Besides the tonsillectomy, medical history is positive for a right clavicular fracture at age 6 and a left inguinal hernia repair at age 9. He had chickenpox and recalls that his immunizations were up to date until he graduated high school. His only medication is ibuprofen as needed for aches and pains. He has no known drug allergies. He uses two herbal supplements, fenugreek seed and horny goat weed, daily. He admits to recreational marijuana use. Family history is remarkable for coronary artery disease (father), diabetes (mother), and depression (sister). He consumes one six-pack of beer weekly and has smoked one pack of cigarettes per day for the past 23 years. He isn’t interested in quitting smoking. The patient is divorced, without children. He has been collecting unemployment since his last position was terminated due to budget constraints. A 20-point comprehensive review of systems is negative, with the exception of occasional palpitations and a productive morning smoker’s cough that quickly resolves. He states he’s “as healthy as a horse.” The physical exam reveals a thin, healthy-appearing middle-aged male. He is 72 in tall and weighs 167 lb. His blood pressure is 108/66 mm Hg; pulse, 70 beats/min and regular; respiratory rate, 14 breaths/min-1; and temperature, 98.4°F. The head, eyes, ears, nose, and throat (HEENT) exam is remarkable for poor dentition, with multiple caries readily visible. The tonsils are absent. Coarse expiratory crackles are present in both bases and clear with vigorous coughing. The abdominal exam is positive for a well-healed scar in the left inguinal crease. The remainder of the physical exam is normal. As part of a new patient visit, a chest x-ray and ECG are obtained. The ECG shows the following: a ventricular rate of 69 beats/min; PR interval, 178 ms; QRS duration, 90ms; QT/QTc interval, 442/473 ms; P axis, 231°; R axis, 84°; and T axis, 93°. What is your interpretation of this ECG?
Man Has “a Couple of Blocks Somewhere”
ANSWER
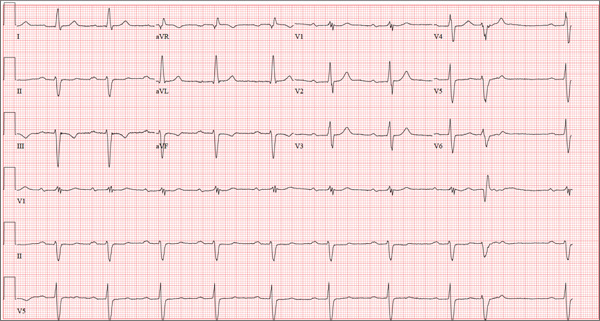
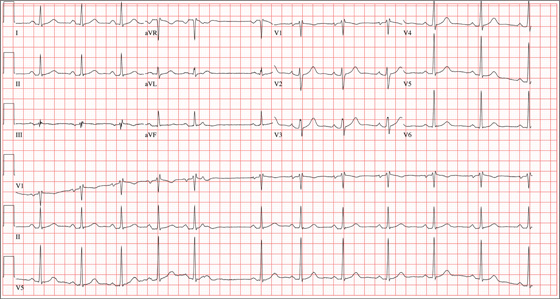
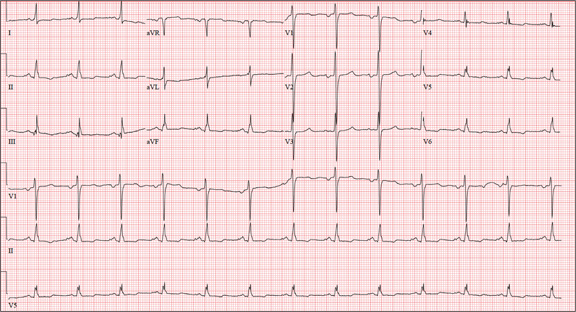
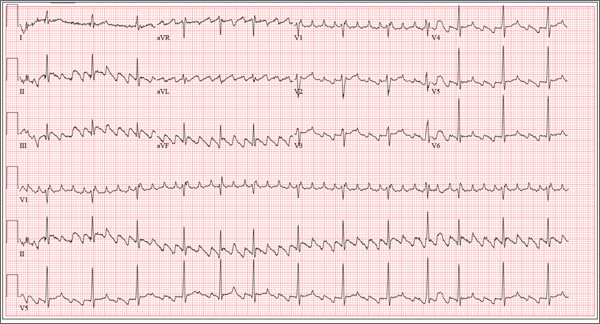
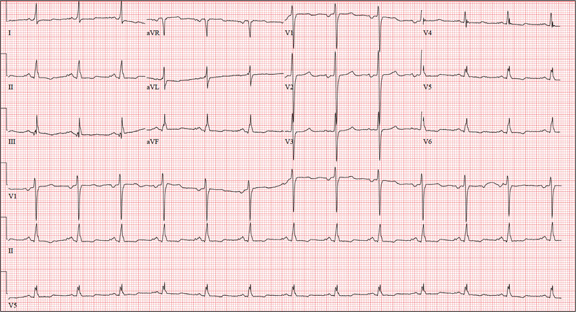
The correct interpretation includes sinus bradycardia with first-degree block, a single premature atrial beat with aberrancy, right bundle branch block, left anterior fascicular block (bifascicular block), left ventricular hypertrophy, and T-wave inversions in the inferior leads.
In sinus bradycardia, there is a P wave for every QRS complex with a rate less than 60 beats/min. First-degree block is evidenced by a PR interval ≥ 200 ms.
A single premature atrial contraction is seen as the ninth beat on the ECG. Aberrancy refers to the appearance of the QRS complex; the impulse arises above the AV node but propagates down the AV node and His-Purkinje system to the ventricles before the conduction system is fully repolarized. This results in a QRS complex with intrinsic conduction similar to a normally conducted beat, which then becomes wide and uncharacteristic. Additionally, it resets the sinus node, resulting in a pause before the next normally conducted P wave.
A right bundle branch block is evidenced by the presence of normal conduction with a QRS duration > 120 ms, a terminal R wave in lead V1 (R, rR’, rsR’, or qR), and slurred S waves in leads I and V6.
The presence of left anterior fascicular block is confirmed by the left-axis deviation (–59° in this ECG), a qR complex in leads I and aVL, and an rS pattern in leads II, III, and aVF. The presence of both a right bundle and left anterior fascicular block constitutes bifascicular block. (This is a conduction problem and does not refer to blockage in the arteries, as the patient believed!)
Criteria for left ventricular hypertrophy are met when the sum of the S wave in V1 and the R wave in either V5 or V6 is ≥ 35 mm and the R wave in aVL is ≥ 11 mm.
Two other things to note in this ECG are the presence of T-wave inversions in the inferior leads (II, III, aVF) which are of unclear reason; and the presence of biphasic P waves that do not meet criteria for either right or left atrial hypertrophy.
ANSWER
The correct interpretation includes sinus bradycardia with first-degree block, a single premature atrial beat with aberrancy, right bundle branch block, left anterior fascicular block (bifascicular block), left ventricular hypertrophy, and T-wave inversions in the inferior leads.
In sinus bradycardia, there is a P wave for every QRS complex with a rate less than 60 beats/min. First-degree block is evidenced by a PR interval ≥ 200 ms.
A single premature atrial contraction is seen as the ninth beat on the ECG. Aberrancy refers to the appearance of the QRS complex; the impulse arises above the AV node but propagates down the AV node and His-Purkinje system to the ventricles before the conduction system is fully repolarized. This results in a QRS complex with intrinsic conduction similar to a normally conducted beat, which then becomes wide and uncharacteristic. Additionally, it resets the sinus node, resulting in a pause before the next normally conducted P wave.
A right bundle branch block is evidenced by the presence of normal conduction with a QRS duration > 120 ms, a terminal R wave in lead V1 (R, rR’, rsR’, or qR), and slurred S waves in leads I and V6.
The presence of left anterior fascicular block is confirmed by the left-axis deviation (–59° in this ECG), a qR complex in leads I and aVL, and an rS pattern in leads II, III, and aVF. The presence of both a right bundle and left anterior fascicular block constitutes bifascicular block. (This is a conduction problem and does not refer to blockage in the arteries, as the patient believed!)
Criteria for left ventricular hypertrophy are met when the sum of the S wave in V1 and the R wave in either V5 or V6 is ≥ 35 mm and the R wave in aVL is ≥ 11 mm.
Two other things to note in this ECG are the presence of T-wave inversions in the inferior leads (II, III, aVF) which are of unclear reason; and the presence of biphasic P waves that do not meet criteria for either right or left atrial hypertrophy.
ANSWER
The correct interpretation includes sinus bradycardia with first-degree block, a single premature atrial beat with aberrancy, right bundle branch block, left anterior fascicular block (bifascicular block), left ventricular hypertrophy, and T-wave inversions in the inferior leads.
In sinus bradycardia, there is a P wave for every QRS complex with a rate less than 60 beats/min. First-degree block is evidenced by a PR interval ≥ 200 ms.
A single premature atrial contraction is seen as the ninth beat on the ECG. Aberrancy refers to the appearance of the QRS complex; the impulse arises above the AV node but propagates down the AV node and His-Purkinje system to the ventricles before the conduction system is fully repolarized. This results in a QRS complex with intrinsic conduction similar to a normally conducted beat, which then becomes wide and uncharacteristic. Additionally, it resets the sinus node, resulting in a pause before the next normally conducted P wave.
A right bundle branch block is evidenced by the presence of normal conduction with a QRS duration > 120 ms, a terminal R wave in lead V1 (R, rR’, rsR’, or qR), and slurred S waves in leads I and V6.
The presence of left anterior fascicular block is confirmed by the left-axis deviation (–59° in this ECG), a qR complex in leads I and aVL, and an rS pattern in leads II, III, and aVF. The presence of both a right bundle and left anterior fascicular block constitutes bifascicular block. (This is a conduction problem and does not refer to blockage in the arteries, as the patient believed!)
Criteria for left ventricular hypertrophy are met when the sum of the S wave in V1 and the R wave in either V5 or V6 is ≥ 35 mm and the R wave in aVL is ≥ 11 mm.
Two other things to note in this ECG are the presence of T-wave inversions in the inferior leads (II, III, aVF) which are of unclear reason; and the presence of biphasic P waves that do not meet criteria for either right or left atrial hypertrophy.
A 69-year-old man presents for a routine appointment. His cardiac history is remarkable for systemic hypertension, nonischemic cardiomyopathy, pulmonary hypertension, and dyspnea on exertion. He says a previous provider told him his ECG had “a couple of blocks,” which he believes are “somewhere in the arteries.” He regularly feels lightheaded if he rises from a lying or sitting position too quickly, but he has never lost consciousness. He denies any history of chest pain or symptoms suggestive of angina. Reviewing his prior cardiac workup, you find an echocardiogram that shows moderate left ventricular enlargement with a left ventricular ejection fraction estimated at 35% to 40%; a severely enlarged left atrium; and mild thickening of the mitral leaflets as well as mild mitral regurgitation. A report from an old ECG (conducted at an outside institution) reveals sinus bradycardia, bifascicular block, and left ventricular hypertrophy. Cardiac catheterization performed two years ago showed diffuse disease with no lesions > 30%. Pulmonary function testing showed mild airflow obstruction, no restrictive component, and mildly decreased diffusing capacity. Medical history is positive for two benign colonic polyps that were removed during his last colonoscopy and a remote history of malaria while traveling in Africa 10 years ago. He also has a history of depression, which has been well controlled by medication. His list of medications includes carvedilol, fluoxetine, melatonin, and lisinopril. He is allergic to atenolol and metoprolol. His family history is remarkable for type 1 diabetes (mother). He is a retired baggage handler for a major airline at a nearby international airport. Since high school, he has smoked between one-half and one pack of cigarettes per day. He typically consumes a 12-pack of beer on the weekends. The review of systems is remarkable for corrective lenses, occasional headaches, and dyspnea. The patient denies any other symptoms. Physical examination reveals a blood pressure of 138/80 mm Hg; pulse, 64 beats/min; respiratory rate, 14 breaths/min-1; and O2 saturation, 97%. His height is 188 cm; weight, 107 kg; and BMI, 30. The lungs are clear to auscultation and percussion. The cardiac exam reveals no jugular venous distention, a normal rate and rhythm with occasional skipped beats, and a soft, grade II/VI blowing systolic murmur best heard at the left lower sternal border. The point of maximum impulse is palpable in the left anterior axillary line. The abdomen is soft and nontender, with no organomegaly. The genitourinary exam is normal. Peripheral pulses are 2+ bilaterally in both upper and lower extremities. There is no peripheral edema, and the neurologic exam is grossly intact. The patient is sent for a chest x-ray and an ECG. The latter reveals the following: a ventricular rate of 59 beats/min; PR interval, 284 ms; QRS duration, 130 ms; QT/QTc interval, 472/467 ms; P axis, 70°; R axis, –59°; and T axis, –29°. What is your interpretation of this ECG?
Obese, Short of Breath, and Rationing Meds
ANSWER
The correct interpretation is sinus rhythm with a first-degree atrioventricular (AV) block, right superior axis deviation, and low voltage QRS complexes. The measured PR interval of 360 ms is correct!
The P waves are best seen in precordial leads V1 to V3. Notice that the P waves fall between the QRS complex and the T wave. The P wave is upright and not inverted, so it is not occurring retrograde from the preceding QRS complex. The sinus node depolarizes, and a long delay occurs within the atria and AV node before conducting down the normal conduction system in the ventricles. This conduction delay is so long that the preceding beat (QRS complex) is still repolarizing (T wave) by the time the sinus node depolarizes again. Thus, the P wave is responsible for the next QRS complex after duration of 360 ms.
A right superior axis deviation, also known as an extreme right axis deviation, is evidenced by an R-wave axis of 192°. Low-voltage QRS complexes are due to the patient’s body habitus. Morbid obesity significantly diminishes the electrical vectors measured by the surface ECG electrodes.
Finally, extra credit is due if you recognize the long QTc interval as well. The maximum normal QTc adjusted for a heart rate of 100 beats/min in men is 310 ms. This ECG barely meets that criteria; in this case, the prolonged QTc interval is of no significance.
ANSWER
The correct interpretation is sinus rhythm with a first-degree atrioventricular (AV) block, right superior axis deviation, and low voltage QRS complexes. The measured PR interval of 360 ms is correct!
The P waves are best seen in precordial leads V1 to V3. Notice that the P waves fall between the QRS complex and the T wave. The P wave is upright and not inverted, so it is not occurring retrograde from the preceding QRS complex. The sinus node depolarizes, and a long delay occurs within the atria and AV node before conducting down the normal conduction system in the ventricles. This conduction delay is so long that the preceding beat (QRS complex) is still repolarizing (T wave) by the time the sinus node depolarizes again. Thus, the P wave is responsible for the next QRS complex after duration of 360 ms.
A right superior axis deviation, also known as an extreme right axis deviation, is evidenced by an R-wave axis of 192°. Low-voltage QRS complexes are due to the patient’s body habitus. Morbid obesity significantly diminishes the electrical vectors measured by the surface ECG electrodes.
Finally, extra credit is due if you recognize the long QTc interval as well. The maximum normal QTc adjusted for a heart rate of 100 beats/min in men is 310 ms. This ECG barely meets that criteria; in this case, the prolonged QTc interval is of no significance.
ANSWER
The correct interpretation is sinus rhythm with a first-degree atrioventricular (AV) block, right superior axis deviation, and low voltage QRS complexes. The measured PR interval of 360 ms is correct!
The P waves are best seen in precordial leads V1 to V3. Notice that the P waves fall between the QRS complex and the T wave. The P wave is upright and not inverted, so it is not occurring retrograde from the preceding QRS complex. The sinus node depolarizes, and a long delay occurs within the atria and AV node before conducting down the normal conduction system in the ventricles. This conduction delay is so long that the preceding beat (QRS complex) is still repolarizing (T wave) by the time the sinus node depolarizes again. Thus, the P wave is responsible for the next QRS complex after duration of 360 ms.
A right superior axis deviation, also known as an extreme right axis deviation, is evidenced by an R-wave axis of 192°. Low-voltage QRS complexes are due to the patient’s body habitus. Morbid obesity significantly diminishes the electrical vectors measured by the surface ECG electrodes.
Finally, extra credit is due if you recognize the long QTc interval as well. The maximum normal QTc adjusted for a heart rate of 100 beats/min in men is 310 ms. This ECG barely meets that criteria; in this case, the prolonged QTc interval is of no significance.

A 64-year-old man who is morbidly obese is admitted to the medical service with a two-week history of increasing shortness of breath, orthopnea, and paroxysmal nocturnal dyspnea. He states that he has depleted his finances for the month and has resorted to taking his medications every other day in order to make them last until next payday. He denies chest pain but notes that he has had a lot of “heaviness” in his anterior chest for the past week and now has a persistent, nonproductive cough. His medical history is remarkable for a cardiomyopathy due to alcohol abuse, frequent pneumonias, and renal insufficiency. He has a history of sleep apnea and uses continuous positive airway pressure (CPAP) at night in order to sleep. The patient is divorced, unemployed, lives alone in a subsidized apartment, and collects disability. Prior to filing for disability, he worked as a longshoreman. He is a former smoker who quit two years ago after several pulmonary infections. He attributes quitting smoking to his current weight problem. He states he has been an alcoholic for many years, and at one point consumed one bottle of whiskey per day along with one or two six-packs of beer. He has been to two alcohol rehab programs in the past five years and says he recently started drinking again when he learned his disability checks were not going to be increased. Family history is positive for coronary artery disease (mother) and diabetes (father). His parents and both of his siblings are being treated for hypertension. He has no known drug allergies. Current medications include aspirin, extended-release metoprolol, hydralazine, isosorbide mononitrate, torsemide, docusate, and senna. The review of systems is remarkable for chronic low back pain, corrective lenses, and multiple small venous ulcers on both legs that he states will “just not go away.” The physical exam reveals a morbidly obese male in mild distress. His weight is 494 lb and his height, is 70 in. His blood pressure is 120/82 mm Hg; pulse, 90 beats/min and regular; respiratory rate, 18 breaths/min; temperature, 96.8°F; and O2 saturation, 92% on room air. Pertinent physical findings include jugular venous distension to 12 cm, coarse rales in both lower lung fields, distant heart sounds without evidence of a murmur or rub, an obese abdomen without palpable organomegaly or ascites, and 3+ pitting edema in both lower extremities to the level of the knees. There are multiple old and new small, superficial venous ulcers on both lower legs. The skin is warm and pink; however, pulses are not palpable. Upon his admission, a cardiac catheterization is performed, which shows a right dominant system with angiographically normal coronary arteries, a left ventricular ejection fraction of 44%, and no evidence of valvular disease. Right heart pressures include a pulmonary artery pressure of 70/62 mm Hg with a mean of 51 mm Hg. The wedge pressure is 35 mm Hg, the transpulmonary gradient is 10, and the cardiac output is 12.5 L/min with a cardiac index of 4.4 L/min. These data are consistent with moderate-to-severe pulmonary hypertension with severely elevated left-sided filling pressures. A transthoracic echocardiogram is remarkable for elevated left ventricular end diastolic volumes with diffuse hypokinesis and an ejection fraction of 40%. The patient is also found to have a small pericardial effusion and bilateral pleural effusions. An ECG reveals the following: a ventricular rate of 98 beats/min; PR interval, 360 ms; QRS duration, 116 ms; QT/QTc interval, 24/314 ms; P axis, 54°; R axis, 192°; and T axis, 24°. As you review these measurements, you are skeptical of a PR interval of 360 ms and refer to the tracing. What is your interpretation of this ECG, and is the PR interval of 360 ms correct?
Young Man Thinks He is Having a Heart Attack
ANSWER
The correct interpretation of this patient’s ECG is atrial flutter with variable atrioventricular block. Atrial flutter is a macro re-entrant supraventricular arrhythmia arising in the right atrium and usually (but not always!) identified by saw-tooth–appearing flutter waves.
The atrial rate in atrial flutter typically ranges from 200 to 350 beats/min. The QRS appearance will be narrow and similar to that of sinus rhythm, because conduction occurs normally down the atrioventricular node unless there is aberrant conduction.
The ventricular rate is dependent on the ability of the node to control rapid conduction. In this case, there appear to be three flutter waves for each QRS complex (3:1 flutter). If the ventricular rate is 80 beats/min, the rate in the atrium is approximately 240 beats/min. A regular ventricular rate of 150 beats/min should make you suspicious for atrial flutter (2:1 flutter).
The variable atrioventricular block on this ECG is evidenced by the presence of two, rather than three, flutter waves per QRS complex (seen after the fourth, fifth, and 10th QRS complexes on the rhythm strip). This case illustrates that flutter may be present with a ventricular rate of less than 100 beats/min.
ANSWER
The correct interpretation of this patient’s ECG is atrial flutter with variable atrioventricular block. Atrial flutter is a macro re-entrant supraventricular arrhythmia arising in the right atrium and usually (but not always!) identified by saw-tooth–appearing flutter waves.
The atrial rate in atrial flutter typically ranges from 200 to 350 beats/min. The QRS appearance will be narrow and similar to that of sinus rhythm, because conduction occurs normally down the atrioventricular node unless there is aberrant conduction.
The ventricular rate is dependent on the ability of the node to control rapid conduction. In this case, there appear to be three flutter waves for each QRS complex (3:1 flutter). If the ventricular rate is 80 beats/min, the rate in the atrium is approximately 240 beats/min. A regular ventricular rate of 150 beats/min should make you suspicious for atrial flutter (2:1 flutter).
The variable atrioventricular block on this ECG is evidenced by the presence of two, rather than three, flutter waves per QRS complex (seen after the fourth, fifth, and 10th QRS complexes on the rhythm strip). This case illustrates that flutter may be present with a ventricular rate of less than 100 beats/min.
ANSWER
The correct interpretation of this patient’s ECG is atrial flutter with variable atrioventricular block. Atrial flutter is a macro re-entrant supraventricular arrhythmia arising in the right atrium and usually (but not always!) identified by saw-tooth–appearing flutter waves.
The atrial rate in atrial flutter typically ranges from 200 to 350 beats/min. The QRS appearance will be narrow and similar to that of sinus rhythm, because conduction occurs normally down the atrioventricular node unless there is aberrant conduction.
The ventricular rate is dependent on the ability of the node to control rapid conduction. In this case, there appear to be three flutter waves for each QRS complex (3:1 flutter). If the ventricular rate is 80 beats/min, the rate in the atrium is approximately 240 beats/min. A regular ventricular rate of 150 beats/min should make you suspicious for atrial flutter (2:1 flutter).
The variable atrioventricular block on this ECG is evidenced by the presence of two, rather than three, flutter waves per QRS complex (seen after the fourth, fifth, and 10th QRS complexes on the rhythm strip). This case illustrates that flutter may be present with a ventricular rate of less than 100 beats/min.
The 24-year-old male graduate student whom you saw one month ago for palpitations (see July 2013 ECG Challenge) returns without an appointment, stating that his heart is “flip-flopping” just as it has in the past. The problem started abruptly about 45 minutes ago, and he is afraid he might be having a heart attack. A quick check of his pulse reveals a rate of 80 beats/min. At his previous visit, an ECG showed sinus rhythm with sinus arrhythmia and a blocked premature atrial contraction (PAC). A rhythm strip documented that his palpitations coincided with blocked PACs. You recall that he reported having two episodes of tachycardia in the past, while “pulling all-nighters” for finals as an undergraduate. Today, he denies shortness of breath, nausea, vomiting, chest pain, and symptoms of near-syncope or syncope, but says his heart is “flopping around” in his chest and he can feel his heart beat in his throat. He has no prior cardiac or pulmonary history and has not recently been ill. Medical history, medication list, allergies, family history, and review of systems are unchanged since his last visit: Medical history is remarkable only for fractures of the right ankle and the left clavicle. He takes no medications and has no drug allergies. Family history is significant for stroke (paternal grandfather), diabetes (maternal grandmother), and hypertension (father). The patient consumes alcohol socially, primarily on weekends, and does not binge drink. He smokes marijuana during snowboard season, but denies use at other times of the year. A 12-point review of systems is positive only for athlete’s foot and psoriasis on both upper extremities. The physical exam reveals an anxious but otherwise healthy, athletic-appearing male. Vital signs include a blood pressure of 140/88 mm Hg; pulse, 80 beats/min; respiratory rate, 20 breaths/min-1; and O2 saturation, 99% on room air. His height is 70” and his weight, 161 lb. His lungs are clear, there is no jugular venous distention, and cardiac auscultation reveals no murmurs, gallops, or rubs. The abdominal exam is normal without organomegaly, and peripheral pulses are regular and strong bilaterally. His neurologic exam yields normal results. As you examine the ECG, you note the following: a ventricular rate of 80 beats/min; PR interval, unmeasurable; QRS duration, 92 ms; QT/QTc interval, 388/444 ms; P axis, 265°; R axis, 72°; and T axis, 66°. What is your interpretation of this ECG?
Is Active Patient a “Picture of Health”?
ANSWER
The correct interpretation includes marked sinus bradycardia, a right bundle branch block, and T-wave abnormalities in the lateral leads.
Sinus bradycardia is evidenced by a sinus rate less than 60 beats/min and may be considered “marked” if the rate is less than 50 beats/min.
A right bundle branch block is indicated by a QRS duration ≥ 120 ms, a terminal broad S wave in lead I, and the presence of an RSR’ pattern in lead V1.
Small or nonexistent T waves in leads V5 and V6 are suggestive of lateral ischemia but are not diagnostic in this individual.
His marked bradycardia was attributed to his exceptional athleticism and the fact that the ECG was taken “at rest.” It was not of concern, nor did it require treatment.
ANSWER
The correct interpretation includes marked sinus bradycardia, a right bundle branch block, and T-wave abnormalities in the lateral leads.
Sinus bradycardia is evidenced by a sinus rate less than 60 beats/min and may be considered “marked” if the rate is less than 50 beats/min.
A right bundle branch block is indicated by a QRS duration ≥ 120 ms, a terminal broad S wave in lead I, and the presence of an RSR’ pattern in lead V1.
Small or nonexistent T waves in leads V5 and V6 are suggestive of lateral ischemia but are not diagnostic in this individual.
His marked bradycardia was attributed to his exceptional athleticism and the fact that the ECG was taken “at rest.” It was not of concern, nor did it require treatment.
ANSWER
The correct interpretation includes marked sinus bradycardia, a right bundle branch block, and T-wave abnormalities in the lateral leads.
Sinus bradycardia is evidenced by a sinus rate less than 60 beats/min and may be considered “marked” if the rate is less than 50 beats/min.
A right bundle branch block is indicated by a QRS duration ≥ 120 ms, a terminal broad S wave in lead I, and the presence of an RSR’ pattern in lead V1.
Small or nonexistent T waves in leads V5 and V6 are suggestive of lateral ischemia but are not diagnostic in this individual.
His marked bradycardia was attributed to his exceptional athleticism and the fact that the ECG was taken “at rest.” It was not of concern, nor did it require treatment.
A 62-year-old man presents for a preoperative history and physical exam prior to surgical repair of an injury to his right anterior cruciate ligament (ACL). He reports that he has been healthy all his life and has never had an injury or illness requiring hospitalization. He is an accountant at a local financial institution and has a very active lifestyle, which includes competitive cycling, running, and skiing. He recently completed his fourth triathlon and was training for his sixth marathon until his injury occurred. One week ago, he was skiing moguls on a black diamond course when he fell and tumbled about 20 feet before stopping. His right ski binding did not release from the boot. He felt his right knee “pop” and knew immediately that he had sustained a serious injury. When he tried to stand, he was unable to bear weight on his right leg. The ski patrol transported him off the slope via basket. He was then taken to a local hospital by a colleague. Physical exam and MRI confirmed an avulsion of the ACL. He has been convalescing at home (having delayed his surgery in order to catch up on paper-work for work) and is scheduled for surgery in two days’ time. Medical history is unremarkable. Aside from the usual childhood illnesses (eg, ear infections, chicken pox, mumps), he has been very healthy and attributes this to a strict diet and rigorous exercise. Social history reveals that he is married to an attorney and has no children. He has never smoked or taken recreational drugs, and he consumes approximately one bottle of wine per week. His current medications include naproxen as needed for pain, a daily aspirin, fish oil, a multivitamin, and omeprazole on rare occasions. The review of systems is remarkable only for occasional gastroesophageal re-flux, which is exacerbated by spicy dishes containing curry. Physical exam reveals a thin, athletic male in no acute distress. His weight is 168 lb, and his height is 74”. Vital signs include a blood pressure of 104/62 mm Hg; pulse, 50 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 98°F. Examination of the head, neck, lungs, heart, abdomen, skin, and nervous system yields normal findings. Lachman, pivot shift, and anterior drawer maneuvers of the right knee are all positive. A routine ECG is performed that reveals the following: a ventricular rate of 49 beats/min; PR interval, 176 ms; QRS dura-tion, 120 ms; QT/QTc interval, 430/388 ms; P axis, 14°; R axis, 38°; and T axis, 103°. What is your interpretation of this ECG?
Grad Student With Palpitations
ANSWER
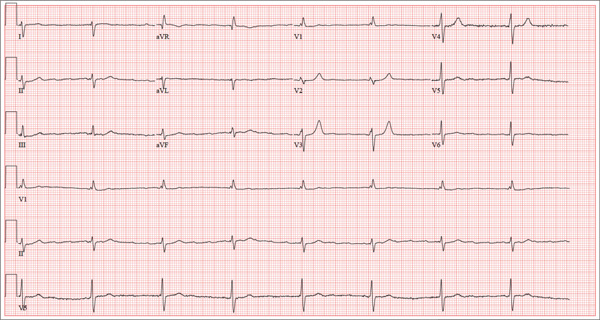
The correct interpretation of this ECG includes sinus rhythm with marked sinus arrhythmia and a blocked premature atrial contraction (PAC).
Sinus rhythm is defined as a heart rate between 60 and 100 beats/min, with a P wave for every QRS complex, a QRS complex for every P wave, and a consistent PR interval between 120 and 200 ms.
A sinus arrhythmia is defined as a variation of the P-P interval ≥ 120 ms in the presence of normal P waves and a normal PR interval. The most common cause of a sinus arrhythmia is respiratory variation.
A blocked PAC is seen following the fifth QRS complex. Careful inspection of the terminal portion of the T wave reveals a P wave without a corresponding QRS complex. There is no QRS complex because the PAC occurs while the AV node is refractory. The subsequent pause occurs because the PAC blocks the sinus node and resets the sinus rate.
The palpitations were correlated to PACs observed on a continuous rhythm strip, and the patient was reassured.
ANSWER
The correct interpretation of this ECG includes sinus rhythm with marked sinus arrhythmia and a blocked premature atrial contraction (PAC).
Sinus rhythm is defined as a heart rate between 60 and 100 beats/min, with a P wave for every QRS complex, a QRS complex for every P wave, and a consistent PR interval between 120 and 200 ms.
A sinus arrhythmia is defined as a variation of the P-P interval ≥ 120 ms in the presence of normal P waves and a normal PR interval. The most common cause of a sinus arrhythmia is respiratory variation.
A blocked PAC is seen following the fifth QRS complex. Careful inspection of the terminal portion of the T wave reveals a P wave without a corresponding QRS complex. There is no QRS complex because the PAC occurs while the AV node is refractory. The subsequent pause occurs because the PAC blocks the sinus node and resets the sinus rate.
The palpitations were correlated to PACs observed on a continuous rhythm strip, and the patient was reassured.
ANSWER
The correct interpretation of this ECG includes sinus rhythm with marked sinus arrhythmia and a blocked premature atrial contraction (PAC).
Sinus rhythm is defined as a heart rate between 60 and 100 beats/min, with a P wave for every QRS complex, a QRS complex for every P wave, and a consistent PR interval between 120 and 200 ms.
A sinus arrhythmia is defined as a variation of the P-P interval ≥ 120 ms in the presence of normal P waves and a normal PR interval. The most common cause of a sinus arrhythmia is respiratory variation.
A blocked PAC is seen following the fifth QRS complex. Careful inspection of the terminal portion of the T wave reveals a P wave without a corresponding QRS complex. There is no QRS complex because the PAC occurs while the AV node is refractory. The subsequent pause occurs because the PAC blocks the sinus node and resets the sinus rate.
The palpitations were correlated to PACs observed on a continuous rhythm strip, and the patient was reassured.
A 24-year-old graduate student presents to the student clinic with a history of palpitations. He first noticed them while snowboarding two months ago, but says they’re now occurring daily and much more frequently. He is concerned about the risk for “another” episode of tachycardia, which, through careful questioning, you learn he has experienced twice before. He recalls that each of the episodes—which occurred while he was “pulling all-nighters” for final exams during his undergrad years—began abruptly and lasted for approximately an hour. He had no chest pain, symptoms of near-syncope, or syncope, but recalls feeling very “jittery,” which he attributed to drinking a full pot of coffee while studying. The patient has no prior cardiac or pulmonary history and considers himself to be in excellent health. He has run two half-marathons in the preceding six months and is an avid snowboarder. He also competes in local road cycling competitions with reasonable success. Medical history is remarkable only for fractures of the right ankle and the left clavicle. He takes no medications and has no drug allergies. Family history is significant for stroke (paternal grandfather), diabetes (maternal grandmother), and hypertension (father). He consumes alcohol socially, primarily on weekends, and does not binge drink. He smokes marijuana during snowboard season but denies use at other times of the year. A 12-point review of systems is positive only for athlete’s foot and psoriasis on both upper extremities. The physical exam reveals a healthy, athletic-appearing male in no distress. Vital signs include a blood pressure of 126/68 mm Hg; pulse, 78 beats/min; respiratory rate, 14 breaths/min; and O2 saturation, 99% on room air. He is afebrile. His height is 70” and weight, 158 lb. Auscultation of the heart reveals no murmurs, rubs, or gallops, but you do detect several pauses. As you listen, he emphatically states, “There’s one … there’s another.” Following the physical exam, the patient asks you to order an ECG. The resultant tracing reveals the following: a ventricular rate of 70 beats/min; PR interval, 178 ms; QRS duration, 90 ms; QT/QTc interval, 402/434 ms; P axis, 23°, R axis, 38°; and T axis, 31°. What is your interpretation of this ECG?
Drug Abuse Follows a Broken Heart
ANSWER
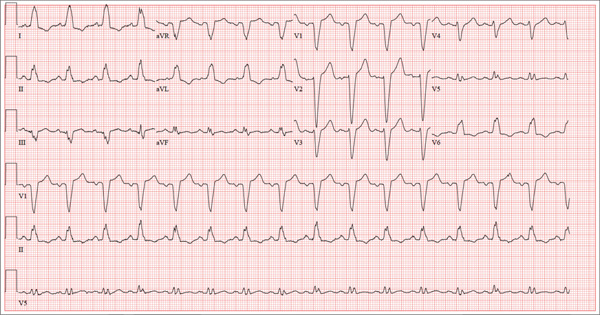
This ECG shows sinus tachycardia at a rate of 110 beats/min, evidenced by the presence of a P wave for every QRS complex with regular R-R intervals. Left atrial enlargement is evident from the presence of P waves ≥ 110 ms (admittedly difficult to see in this example) and a terminal negativity of the P wave in lead V1 ≥ 1 mm2. A rightward axis is evidenced by the presence of an R-wave axis of 96°; however, it does not meet criteria for a true right-axis deviation
(≥ 105°). Nonspecific T-wave abnormalities are observed in leads V5 and V6.
The most intriguing aspect of this ECG is observed in lead V3. Note the abrupt disruption of R-wave progression between leads V2 and V4. This was due to incorrect placement of the ECG electrode for V3, which occurred in the haste to obtain the ECG prior to the CT scan. This illustrates the importance of correct electrode placement for an accurate tracing.
ANSWER
This ECG shows sinus tachycardia at a rate of 110 beats/min, evidenced by the presence of a P wave for every QRS complex with regular R-R intervals. Left atrial enlargement is evident from the presence of P waves ≥ 110 ms (admittedly difficult to see in this example) and a terminal negativity of the P wave in lead V1 ≥ 1 mm2. A rightward axis is evidenced by the presence of an R-wave axis of 96°; however, it does not meet criteria for a true right-axis deviation
(≥ 105°). Nonspecific T-wave abnormalities are observed in leads V5 and V6.
The most intriguing aspect of this ECG is observed in lead V3. Note the abrupt disruption of R-wave progression between leads V2 and V4. This was due to incorrect placement of the ECG electrode for V3, which occurred in the haste to obtain the ECG prior to the CT scan. This illustrates the importance of correct electrode placement for an accurate tracing.
ANSWER
This ECG shows sinus tachycardia at a rate of 110 beats/min, evidenced by the presence of a P wave for every QRS complex with regular R-R intervals. Left atrial enlargement is evident from the presence of P waves ≥ 110 ms (admittedly difficult to see in this example) and a terminal negativity of the P wave in lead V1 ≥ 1 mm2. A rightward axis is evidenced by the presence of an R-wave axis of 96°; however, it does not meet criteria for a true right-axis deviation
(≥ 105°). Nonspecific T-wave abnormalities are observed in leads V5 and V6.
The most intriguing aspect of this ECG is observed in lead V3. Note the abrupt disruption of R-wave progression between leads V2 and V4. This was due to incorrect placement of the ECG electrode for V3, which occurred in the haste to obtain the ECG prior to the CT scan. This illustrates the importance of correct electrode placement for an accurate tracing.
A 26-year-old man is brought to the emergency department (ED) by three friends who hadn’t seen him for two days and went to his apartment to check on him. They found him unconscious on the floor with four empty syringes on the coffee table beside him. The patient was aroused with difficulty but remained incoherent. Rather than call 911, they carried him to their car and brought him to the ED. According to his friends, he has been an IV drug abuser since breaking up with his girlfriend two years ago. He has been increasingly despondent over the past few days after seeing her with anoth-er man. The friends state that they know he has used heroin, cocaine, marijuana, and methamphet-amines in the past, but do not know what he used on this occasion. He has not had any prior illnesses, surgical procedures, or medical conditions that they are aware of. They do not know whether the patient is taking any prescription medications, nor whether he is aller-gic to any medications. According to one of the friends, the patient works with him as a welder at a local factory. He states the patient has been absent from work since last seeing his ex-girlfriend. You are unable to obtain a review of systems. A cursory examination reveals a thin, disheveled male who is unconscious but arousable. Blood pressure is 102/62 mm Hg, and pulse, 110 beats/min. Res-pirations are shallow at a rate of 20 breaths/min-1. Examination of the skin is remarkable for multiple recent and mature needle tracks in both upper ex-tremities, as well as multiple excoriations and shallow ulcers on both lower extremities. The EENT exam is remarkable for constricted pupils that react to light. Corneal reflexes are intact. The teeth are in poor repair with multiple caries and missing teeth. The neck veins are not distended, the thyroid is normal, and there are palpable lymph nodes in the left anterior cervical chain. The lungs have diffuse, scattered dry rales. The cardiac exam reveals a regular rate at 110 beats/min with a soft, early systolic murmur best heard at the left upper sternal border. A rub is also present. Peripheral pulses are equal bilaterally in both upper and lower extremities. The abdomen is soft and nontender. The liver edge is palpable 2 cm below the right costal margin, and a firm spleen is palpable on the left. The neurologic exam reveals hyperactive deep tendon re-flexes in all four extremities. Laboratory samples are drawn; results are positive for cocaine, cannabis, and methamphetamine. Stat blood cultures are positive for Staphylococcus aureus, and the white blood count is 21,000/μL. A bedside echocardiogram performed in the ED shows evidence of a pericardial effusion and a perivalvular abscess on the septal side of the mitral valve, consistent with endocarditis. Prior to the patient’s transport to radiology for a CT scan, a quick ECG is performed. It reveals a ven-tricular rate of 110 beats/min; PR interval, 130 ms; QRS duration, 76 ms; QT/QTc interval, 352/476 ms; P axis, 59°; R axis, 96°; and T axis, 106°. What is your interpretation of this ECG?
Do Nausea and Vomiting Have Cardiac Cause?
ANSWER
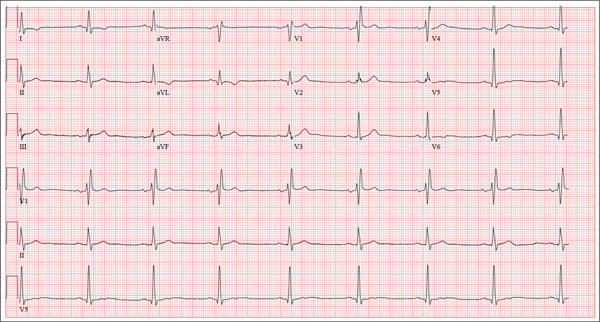
The correct interpretation of this ECG includes normal sinus rhythm, left atrial enlargement, and nonspecific T-wave abnormalities.
Normal sinus rhythm is evidenced by an atrial and ventricular rate of 77 beats/min with one-to-one association. Left atrial enlargement is evidenced by the presence of a biphasic P wave in lead V1 with a negative terminal portion of the P wave ≥ 1 mm2. (P waves in lead I ≥ 110 ms are also seen in left atrial enlargement, but are not evident in this ECG.) The small or inverted appearance of T waves in the inferior and lateral leads indicates nonspecific T waves.
These ECG findings are typical of patients with mitral valve disease, but were of no benefit in diagnosing acute pancreatitis in this patient. By the time she had the ECG done, she had been given sedation sufficient to reduce her heart rate from the 118 beats/min it had been at the time of examination.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm, left atrial enlargement, and nonspecific T-wave abnormalities.
Normal sinus rhythm is evidenced by an atrial and ventricular rate of 77 beats/min with one-to-one association. Left atrial enlargement is evidenced by the presence of a biphasic P wave in lead V1 with a negative terminal portion of the P wave ≥ 1 mm2. (P waves in lead I ≥ 110 ms are also seen in left atrial enlargement, but are not evident in this ECG.) The small or inverted appearance of T waves in the inferior and lateral leads indicates nonspecific T waves.
These ECG findings are typical of patients with mitral valve disease, but were of no benefit in diagnosing acute pancreatitis in this patient. By the time she had the ECG done, she had been given sedation sufficient to reduce her heart rate from the 118 beats/min it had been at the time of examination.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm, left atrial enlargement, and nonspecific T-wave abnormalities.
Normal sinus rhythm is evidenced by an atrial and ventricular rate of 77 beats/min with one-to-one association. Left atrial enlargement is evidenced by the presence of a biphasic P wave in lead V1 with a negative terminal portion of the P wave ≥ 1 mm2. (P waves in lead I ≥ 110 ms are also seen in left atrial enlargement, but are not evident in this ECG.) The small or inverted appearance of T waves in the inferior and lateral leads indicates nonspecific T waves.
These ECG findings are typical of patients with mitral valve disease, but were of no benefit in diagnosing acute pancreatitis in this patient. By the time she had the ECG done, she had been given sedation sufficient to reduce her heart rate from the 118 beats/min it had been at the time of examination.
A 58-year-old woman presents with epigastric pain that began gradually about four hours ago, re-maining constant for the past two. She describes it as a “dull, steady, aching” pain directly beneath her lower sternum. It is neither exacerbated by exertion nor relieved by rest, but it does improve if she bends from the waist. She denies radiation of pain into her neck or upper extremities but describes a band of pain radiating to her back. Additionally, she has experienced nausea and vomiting, starting about 12 hours before her pain, with a single episode of emesis immediately upon presentation. She has a history of mitral valve prolapse, which was surgically corrected with a mechanical heart valve two years ago. She also has a history of paroxysmal atrial fibrillation for which she has been cardioverted on two separate occasions. Her last episode was six months ago. Social history reveals that she is divorced, has smoked one pack of cigarettes a day for the past 30 years, and is a heavy alcohol user. She states she went on a binge last weekend (72 hours ago), drinking one bottle of whiskey and half a bottle of vodka over the course of one day. She has tried heroin, cocaine, and methamphetamines in the past and currently uses marijuana when she can get it. The patient has a primary care provider who prescribed aspirin, atorvastatin, clonidine, gabapentin, metoprolol, and warfarin; however, she hasn’t taken or refilled any of these prescriptions for approx-imately six months. She is allergic to codeine, erythromycin, and azithromycin. The review of sys-tems is positive for difficulty sleeping, anxiety, diffuse abdominal pain not related to her current symp-toms, dyspnea on exertion, “typical smoker’s cough,” and burning with urination. The physical examination reveals an unkempt, thin woman who is restless and easily agitated. Her weight is 125 lb, and her height, 64”. Her vital signs include a blood pressure of 168/102 mm Hg; pulse, 118 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 99.9°F. She has poor den-tition. There is no thyromegaly or jugular venous distention. Her respirations are shallow, and there are coarse rhonchi in both bases that change with coughing. The cardiac exam reveals a regular tachy-cardia with mechanical heart sounds and a grade II/VI systolic murmur. A well-healed median ster-notomy scar is present. The abdominal exam is remarkable for tenderness to palpation in the epigas-trium, with no evidence of rebound. There are no palpable masses. Bowel tones are present in all quadrants. The extremities are positive for 2+ pitting edema to the knees bilaterally. The neurologic exam is grossly intact. Following acute management of her pain, laboratory blood work, abdominal ultrasound and CT, chest x-ray, and ECG are ordered. The ECG is the last test to be obtained and reveals the following: a ventricular rate of 77 beats/min; PR interval, 142 ms; QRS duration, 104 ms; QT/QTc interval, 402/454 ms; P axis, 66°; R axis, 57°; and T axis, –11°. What is your interpretation of this ECG?