User login
During Veggie Harvest, Chest Pain Hits
ANSWER
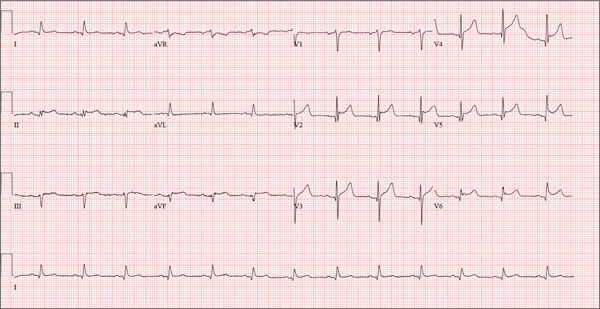
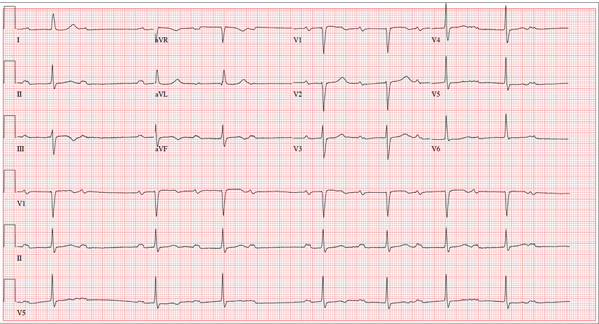
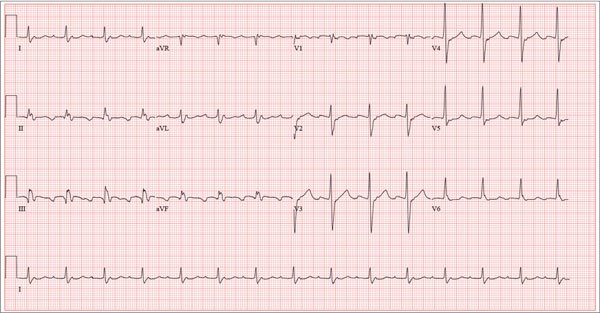
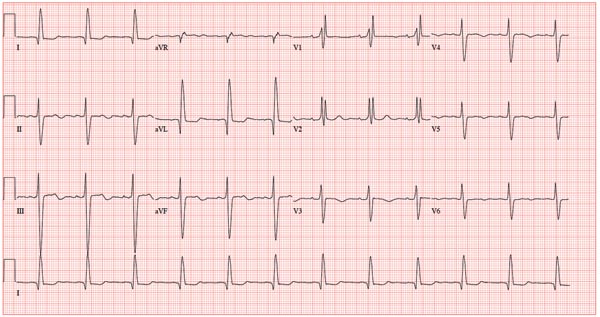
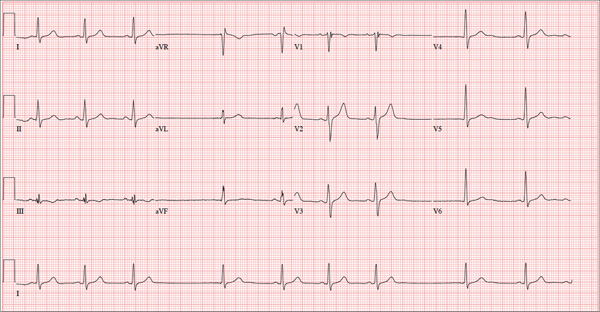
This ECG is representative of an acute anterior MI. This is evidenced by ST segment elevation in leads V2 through V4. Inferolateral injury is indicated by ST elevations in leads II, III, and aVF, as well as in leads V5 and V6.
Infarction was confirmed via laboratory data. Subsequent cardiac catheterization documented occlusion of the proximal left anterior descending artery.
ANSWER
This ECG is representative of an acute anterior MI. This is evidenced by ST segment elevation in leads V2 through V4. Inferolateral injury is indicated by ST elevations in leads II, III, and aVF, as well as in leads V5 and V6.
Infarction was confirmed via laboratory data. Subsequent cardiac catheterization documented occlusion of the proximal left anterior descending artery.
ANSWER
This ECG is representative of an acute anterior MI. This is evidenced by ST segment elevation in leads V2 through V4. Inferolateral injury is indicated by ST elevations in leads II, III, and aVF, as well as in leads V5 and V6.
Infarction was confirmed via laboratory data. Subsequent cardiac catheterization documented occlusion of the proximal left anterior descending artery.
A 48-year-old man arrives at your facility via emergency medical service (EMS). He is alert, oriented, and cooperative but reports substernal chest pain despite receiving two nitroglycerin tablets from the paramedics. The problem started while the patient was working in his garden, harvesting tomatoes and peppers but not doing anything particularly strenuous. The abrupt onset of chest pain caused him to stand up to catch his breath; he immediately became diaphoretic. The pain rated 10 out of 10 in severity and made him feel as if he’d been stabbed in the chest. After 10 minutes of persistent pain, he called to his neighbor, who contacted 911. The EMS arrived within six minutes. The paramedics found the patient conscious, profusely diaphoretic, and in severe pain; he was clutching his chest with his right fist. IV access was obtained, oxygen started, and sublingual nitroglycerin and aspirin given. The patient declined morphine due to a previous anaphylactic reaction to it. The pain subsided significantly, and the patient was loaded for transfer. During the 17-minute trip, his chest pain increased, and a second nitroglycerin tablet was given. It provided less relief than the previous one had. Medical history is remarkable for hypertension, smoking, adult-onset diabetes, and morbid obesity. The man has a primary care provider but hasn’t been seen in six years. He admits he is noncompliant with his medications because he just doesn’t like to take drugs—in fact, he hasn’t taken any of his prescribed medications for the past two years. He has never had chest pain prior to this event. Surgical history is remarkable for a cholecystectomy and a right knee replacement. His (unfilled) prescribed medications include a b-blocker, metformin, and a calcium channel blocker. He is allergic to morphine sulfate. He smokes marijuana on a daily basis because it calms his nerves. Review of systems is remarkable for multiple ulcers on the patient’s legs. He says he doesn’t require a cane for ambulation but prefers to walk with one. He also describes himself as a “nervous worrier,” hence his use of marijuana. Physical examination reveals an alert, anxious, and apprehensive man. His weight is 342 lb and his height, 70 in. He is afebrile and diaphoretic. Vital signs include a blood pressure of 164/98 mm Hg; pulse, 80 beats/min; respiratory rate, 20 breaths/min-1; and temperature, 97.4°F. Pertinent physical findings include no evidence of jugular venous distention or thyromegaly, clear lung sounds bilaterally, a regular rate and rhythm with distant muffled heart sounds, and no extra heart sounds or murmurs. The abdomen is obese, soft, and nontender. The peripheral pulses are equal bilaterally, and there is 2+ pitting edema present to the level of the knees. Multiple shallow ulcers are present on both lower legs, and a deep ulcer is present on the inferior surface of the left foot. After the patient is attached to telemetry monitoring and blood samples are drawn for analysis, an ECG is obtained. It reveals a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc interval, 370/426 ms; P axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation of this ECG?
Man Awakens With "Fluttering" in His Chest
ANSWER
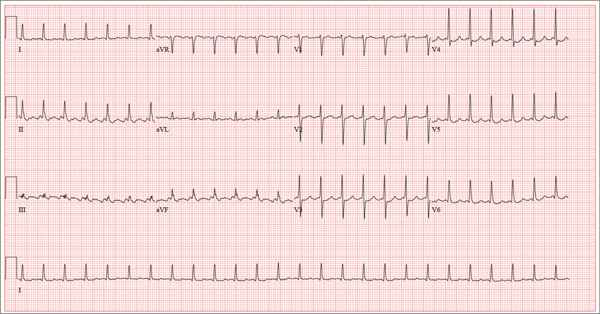
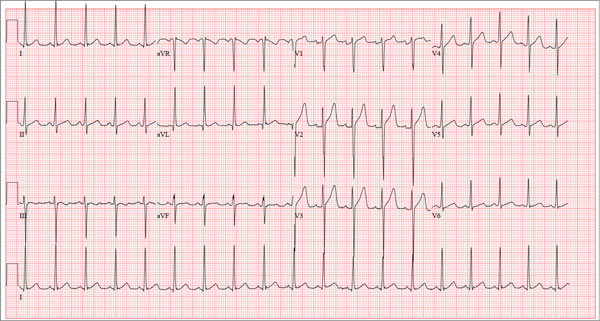
This ECG is consistent with coarse atrial fibrillation with a rapid ventricular response and a nonspecific T-wave abnormality. The patient’s presentation is strongly suggestive of lone atrial fibrillation: This was the first incidence, it occurred in the absence of an existing heart condition, and it presented with an abrupt onset of increased heart rate and dyspnea.
Lone atrial fibrillation most commonly occurs in men in their 40s and 50s. It is vagally mediated, occurring during sleep or relaxation and after food and/or alcohol consumption.
The patient was cardioverted to normal sinus rhythm in the ED without difficulty, and follow-up was arranged.
ANSWER
This ECG is consistent with coarse atrial fibrillation with a rapid ventricular response and a nonspecific T-wave abnormality. The patient’s presentation is strongly suggestive of lone atrial fibrillation: This was the first incidence, it occurred in the absence of an existing heart condition, and it presented with an abrupt onset of increased heart rate and dyspnea.
Lone atrial fibrillation most commonly occurs in men in their 40s and 50s. It is vagally mediated, occurring during sleep or relaxation and after food and/or alcohol consumption.
The patient was cardioverted to normal sinus rhythm in the ED without difficulty, and follow-up was arranged.
ANSWER
This ECG is consistent with coarse atrial fibrillation with a rapid ventricular response and a nonspecific T-wave abnormality. The patient’s presentation is strongly suggestive of lone atrial fibrillation: This was the first incidence, it occurred in the absence of an existing heart condition, and it presented with an abrupt onset of increased heart rate and dyspnea.
Lone atrial fibrillation most commonly occurs in men in their 40s and 50s. It is vagally mediated, occurring during sleep or relaxation and after food and/or alcohol consumption.
The patient was cardioverted to normal sinus rhythm in the ED without difficulty, and follow-up was arranged.
A 56-year-old man presents to the emergency department (ED) complaining of shortness of breath and a rapid heart rate. He went to bed at his regular time (10:30 pm) last night and woke up at 3:30 am with a fluttering sensation in his chest. He checked his pulse; it was 120 beats/min. Alarmed, he got out of bed and noted he was short of breath as he walked to the bathroom. He went back to bed, but after approximately 20 minutes without relief, he decided to call his son to take him to the ED. The time from onset of symptoms until arrival at the ED was two hours. During that time, his symptoms did not change. When you examine the patient, he states that he is typically in excellent health and has never experienced either shortness of breath or a rapid heart rate before. He denies a history of cardiac or pulmonary disease and has never had chest pain, syncope, or near-syncope. Medical history is unremarkable. Surgical history is remarkable for a tonsillectomy in childhood and an appendectomy for acute appendicitis at age 18. The patient has no known drug allergies and is taking ibuprofen for a recent ankle sprain but is on no other medications. He works as a certified public accountant and has a sedentary lifestyle. He drinks two to three glasses of wine each evening, does not smoke, and denies recreational or naturopathic medication use. He is a widower (his wife died of breast cancer at age 44) and has one son who lives in the same housing complex. The review of systems is remarkable for a recent left ankle sprain, which occurred when the patient slipped on the carpet at home. Vital signs include a blood pressure of 144/84 mm Hg; pulse, 130 beats/min; respiratory rate, 18 breaths/min-1; O2 saturation, 98%; and temperature, 98.9°F. His height is 5 ft 9 in and his weight, 223 lb. The physical exam reveals an obese white male in mild distress. The HEENT exam reveals corrective lenses and the absence of tonsils. The neck shows no evidence of thyromegaly or jugular venous distention. The lungs are clear in all fields. The cardiac rhythm is irregular with a rate of 130 beats/min. There are no murmurs or extra heart sounds audible. The abdomen is obese and nontender, with no palpable masses. An old surgical scar is evident in the right lower quadrant, consistent with his history of an appendectomy. The lower extremities show no evidence of peripheral edema. Mild discomfort is present with examination of the left ankle. Peripheral pulses are strong and equal, and the neurologic exam is intact. An ECG is obtained that reveals a ventricular rate of 131 beats/min; PR interval, not measured; QRS duration, 82 ms; QT/QTc interval, 374/552 ms; no P axis; R axis, 68°; and T axis, 36°. What is your interpretation of this ECG?
A Visiting Grandma Feels Short of Breath
ANSWER
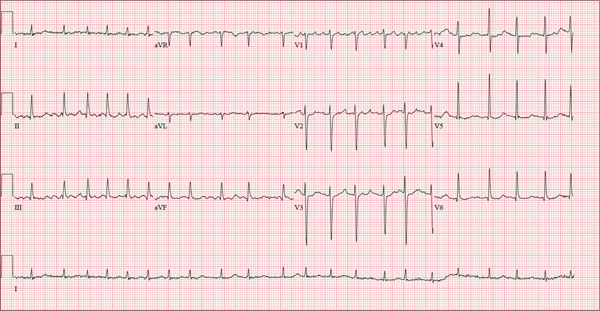
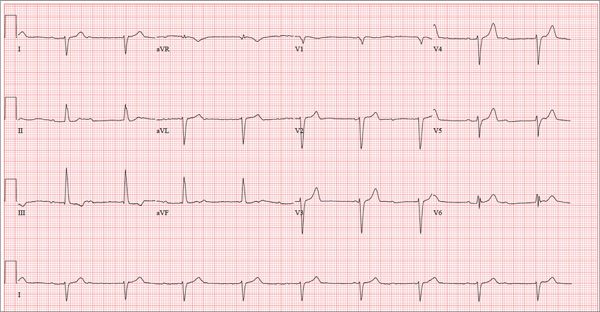
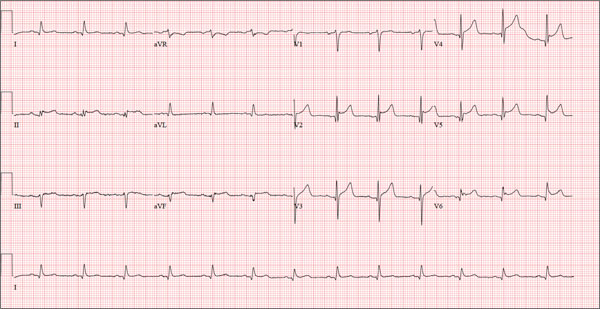
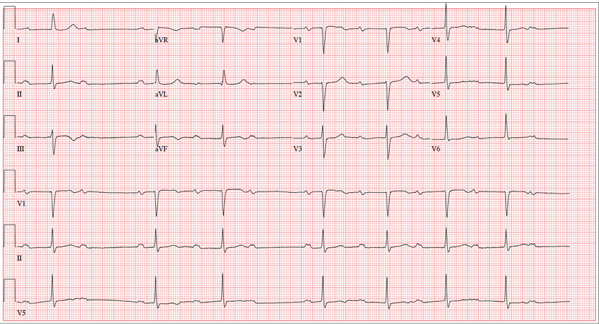
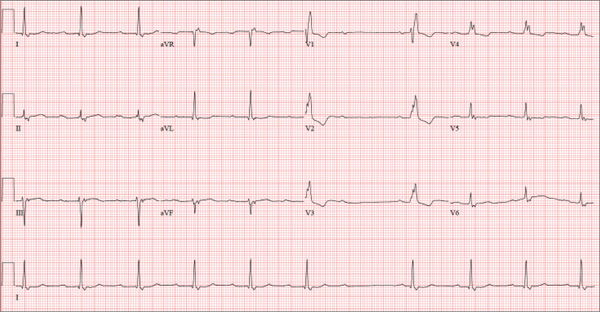
This ECG shows normal sinus rhythm, a right bundle branch block (RBBB), and a left anterior fascicular block (LAFB). RBBB and LAFB are consistent with bifascicular block.
Criteria for an RBBB include a prolonged total QRS complex of 120 ms or longer and an RSR’ complex (“rabbit ears”) in lead V1. LAFB criteria include a QRS of normal duration with an S wave greater than an R wave in leads II, III, and aVF and left-axis deviation (–48° in this case).
The astute reader may question the disparity between RBBB and LAFB, since the criteria for the former include a prolonged QRS interval and the criteria for the latter include a normal QRS interval. It should be noted that the requirements for QRS duration for RBBB vary.
Bifascicular block (RBBB and either LAFB or left posterior fascicular block [LPFB]) is indicative of more advanced conduction system disease. However, it is not an indication for permanent pacemaker placement in an asymptomatic patient.
This patient was treated for a community-acquired right lower lobe pneumonia and a UTI.
ANSWER
This ECG shows normal sinus rhythm, a right bundle branch block (RBBB), and a left anterior fascicular block (LAFB). RBBB and LAFB are consistent with bifascicular block.
Criteria for an RBBB include a prolonged total QRS complex of 120 ms or longer and an RSR’ complex (“rabbit ears”) in lead V1. LAFB criteria include a QRS of normal duration with an S wave greater than an R wave in leads II, III, and aVF and left-axis deviation (–48° in this case).
The astute reader may question the disparity between RBBB and LAFB, since the criteria for the former include a prolonged QRS interval and the criteria for the latter include a normal QRS interval. It should be noted that the requirements for QRS duration for RBBB vary.
Bifascicular block (RBBB and either LAFB or left posterior fascicular block [LPFB]) is indicative of more advanced conduction system disease. However, it is not an indication for permanent pacemaker placement in an asymptomatic patient.
This patient was treated for a community-acquired right lower lobe pneumonia and a UTI.
ANSWER
This ECG shows normal sinus rhythm, a right bundle branch block (RBBB), and a left anterior fascicular block (LAFB). RBBB and LAFB are consistent with bifascicular block.
Criteria for an RBBB include a prolonged total QRS complex of 120 ms or longer and an RSR’ complex (“rabbit ears”) in lead V1. LAFB criteria include a QRS of normal duration with an S wave greater than an R wave in leads II, III, and aVF and left-axis deviation (–48° in this case).
The astute reader may question the disparity between RBBB and LAFB, since the criteria for the former include a prolonged QRS interval and the criteria for the latter include a normal QRS interval. It should be noted that the requirements for QRS duration for RBBB vary.
Bifascicular block (RBBB and either LAFB or left posterior fascicular block [LPFB]) is indicative of more advanced conduction system disease. However, it is not an indication for permanent pacemaker placement in an asymptomatic patient.
This patient was treated for a community-acquired right lower lobe pneumonia and a UTI.
A 78-year-old woman presents to your urgent care clinic with a four-day history of lethargy. She lives in another state but currently is visiting her granddaughter, who happens to be your clinic manager. She says she felt weak prior to her trip but thought it was probably due to a urinary tract infection (UTI). Yesterday, however, she started feeling short of breath. The patient denies chest pain, orthopnea, paroxysmal nocturnal dyspnea, or productive cough. She reports feeling feverish this morning but did not record her temperature, adding that it seemed to subside after she got dressed. Her medical history is positive for frequent UTIs, a remote cholecystectomy, hypothyroidism, and paroxysmal atrial fibrillation. According to the patient’s daughter, who is present, her mother’s cardiologist recently mentioned some “funny” findings on an ECG; she didn’t really understand his explanation but they were told “not to worry.” The patient, a retired schoolteacher, lives in an assisted living center. She is independent and has been a widow for 14 years, since her husband died of an acute MI. She has two children who are in good health. She has never smoked, rarely consumes alcohol, and has never used recreational or homeopathic drugs. Her current medications include warfarin, levothyroxine, and conjugated estrogen. She was taking amiodarone for rhythm control of atrial fibrillation but stopped six months ago when her skin started turning blue. She is allergic to penicillin, which causes a true anaphylactic reaction, according to her daughter. Review of systems is positive for an infrequent, nonproductive cough, sun sensitivity due to amiodarone use, and infrequent burning with urination. Physical exam reveals a thin, elderly woman in no distress. Her blood pressure is 152/88 mm Hg; pulse, 70 beats/min and regular; respiratory rate, 14 breaths/min-1 with an infrequent, nonproductive cough; O2 saturation, 94% on room air; and temperature, 99°F. She is 5 ft 4 in tall and weighs 114 lb. Pertinent findings on physical exam include corrective lenses, pearly white skin with a blue hue on the nose and ears secondary to long-term amiodarone therapy, no evidence of thyromegaly or jugular distention, a regular rate and rhythm with a soft midsystolic murmur of mitral regurgitation, and no extra heart sounds. Her lungs are remarkable for consolidation in the right lower lobe, with crackles that change with coughing. Her abdomen is soft and nontender, and there is no peripheral edema. Her neurologic exam is intact. She is alert, attentive, and very witty in her responses to questions. Laboratory data include urinalysis findings suggestive of a UTI, a white blood cell count of 9.8 x 103/μL, and a hematocrit of 35%. A chest x-ray shows evidence of consolidation in the right lower lobe, which the radiologist says is strongly suggestive of pneumonia. An ECG shows a ventricular rate of 71 beats/min; PR interval, 152 ms; QRS duration, 142 ms; QT/QTc interval, 476/517 ms; P axis, 76°; R axis, –48°; and T axis, 161°. What is your interpretation of this ECG?
Does Young Athlete Have Cause for Concern?
ANSWER
The correct interpretation of this ECG includes sinus tachycardia and left ventricular hypertrophy.
Sinus tachycardia is evidenced by an atrial rate greater than 100 beats/min with a P wave for every QRS complex and a QRS complex for every P wave.
Left ventricular hypertrophy is present when either the sum of the R wave voltage in lead I and the S wave in lead III is 25 mm or higher or the sum of the S wave in lead V1 and the R wave in either V5 or V6 is 35 mm or higher.
In follow-up to these findings, an echocardiogram was recommended and performed. It revealed a normal heart consistent with that of a young athlete.
The patient and his parents were reassured as to the young man’s condition but decided to seek a second opinion.
ANSWER
The correct interpretation of this ECG includes sinus tachycardia and left ventricular hypertrophy.
Sinus tachycardia is evidenced by an atrial rate greater than 100 beats/min with a P wave for every QRS complex and a QRS complex for every P wave.
Left ventricular hypertrophy is present when either the sum of the R wave voltage in lead I and the S wave in lead III is 25 mm or higher or the sum of the S wave in lead V1 and the R wave in either V5 or V6 is 35 mm or higher.
In follow-up to these findings, an echocardiogram was recommended and performed. It revealed a normal heart consistent with that of a young athlete.
The patient and his parents were reassured as to the young man’s condition but decided to seek a second opinion.
ANSWER
The correct interpretation of this ECG includes sinus tachycardia and left ventricular hypertrophy.
Sinus tachycardia is evidenced by an atrial rate greater than 100 beats/min with a P wave for every QRS complex and a QRS complex for every P wave.
Left ventricular hypertrophy is present when either the sum of the R wave voltage in lead I and the S wave in lead III is 25 mm or higher or the sum of the S wave in lead V1 and the R wave in either V5 or V6 is 35 mm or higher.
In follow-up to these findings, an echocardiogram was recommended and performed. It revealed a normal heart consistent with that of a young athlete.
The patient and his parents were reassured as to the young man’s condition but decided to seek a second opinion.
A 17-year-old male athlete recently graduated high school and received a full scholarship to play baseball for a major university. As part of his preparation for college, his parents bring him to your clinic for a complete physical examination, noting that he contracted several colds during the past school year. He has been symptom free for the past two months. The patient asks to be examined without his parents present. After they exit the room, he informs you that he has recently become sexually active, hasn’t used condoms on two occasions, and wants to be tested for sexually transmitted infections (STIs). Medical history is unremarkable, with the exception of a fractured left clavicle sustained when the patient was 12. He currently takes no medications, denies tobacco, alcohol, or recreational drug use, and has no known drug allergies. He lives at home with his parents and two siblings. A detailed review of systems reveals no complaints or symptoms. Vital signs include a blood pressure of 104/58 mm Hg; pulse, 100 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 97.2°F. His weight is 204 lb and his height, 79 in. He appears anxious and apologizes for having sweaty palms. A thorough physical exam yields completely normal results, with the exception of a palpable callus over the mid portion of the left clavicle (consistent with his history of a fracture). Lung sounds are clear in all fields; there are no murmurs, bruits, rubs, or extra heart sounds; and a strong PMI (point of maximum impulse) is easily palpable over the left chest at the seventh and eighth intercostal spaces. The patient is sent to the lab, where blood is drawn for a routine chemistry panel, complete blood count, and STI surveillance panel. When he returns and his parents reenter the room, they insist on ECG for their son. You explain that there’s no clear indication for it; however, they insist and state they will pay out of pocket if not covered by insurance. You reluctantly agree. The ECG shows the following: a ventricular rate of 112 beats/min; PR interval, 132 ms; QRS duration, 756 ms; QT/QTc interval, 326/444 ms; P axis, 59°; R axis, –8°; and T axis, 26°. What is your interpretation?
Man’s Heart Rhythm Has Been “Strange”
ANSWER
The ECG reveals sinus bradycardia with second-degree atrioventricular (AV) block (Mobitz I), also known as Wenckebach block.
Mobitz I heart block often occurs with reversible reasons of conduction block at the level of the AV node. While the P-P intervals remain constant, conduction fatigue within the AV node results in the P-R interval becoming progressively longer, until the AV node completely blocks conduction from the atria to the ventricles. The process then repeats itself in a pattern of P to QRS groups.
In this case, there are three P waves for every two QRS complexes, resulting in a 3:2 pattern. The PR interval is longest prior to the blocked QRS and shortest immediately after it. The diagnosis of sinus bradycardia results from a constant P-P interval of 58 beats/min.
Further questioning of the patient revealed that he had inadvertently doubled his dose of metoprolol. Correcting this resulted in the return of normal sinus rhythm.
ANSWER
The ECG reveals sinus bradycardia with second-degree atrioventricular (AV) block (Mobitz I), also known as Wenckebach block.
Mobitz I heart block often occurs with reversible reasons of conduction block at the level of the AV node. While the P-P intervals remain constant, conduction fatigue within the AV node results in the P-R interval becoming progressively longer, until the AV node completely blocks conduction from the atria to the ventricles. The process then repeats itself in a pattern of P to QRS groups.
In this case, there are three P waves for every two QRS complexes, resulting in a 3:2 pattern. The PR interval is longest prior to the blocked QRS and shortest immediately after it. The diagnosis of sinus bradycardia results from a constant P-P interval of 58 beats/min.
Further questioning of the patient revealed that he had inadvertently doubled his dose of metoprolol. Correcting this resulted in the return of normal sinus rhythm.
ANSWER
The ECG reveals sinus bradycardia with second-degree atrioventricular (AV) block (Mobitz I), also known as Wenckebach block.
Mobitz I heart block often occurs with reversible reasons of conduction block at the level of the AV node. While the P-P intervals remain constant, conduction fatigue within the AV node results in the P-R interval becoming progressively longer, until the AV node completely blocks conduction from the atria to the ventricles. The process then repeats itself in a pattern of P to QRS groups.
In this case, there are three P waves for every two QRS complexes, resulting in a 3:2 pattern. The PR interval is longest prior to the blocked QRS and shortest immediately after it. The diagnosis of sinus bradycardia results from a constant P-P interval of 58 beats/min.
Further questioning of the patient revealed that he had inadvertently doubled his dose of metoprolol. Correcting this resulted in the return of normal sinus rhythm.
A 74-year-old man presents to your outpatient clinic for a routine appointment. He’s been your patient for years, but you’ve had difficulty convincing him of the importance of taking his hypertension medications regularly. For the most part, he has been compliant; however, recently, with finances becoming tight toward the end of the month, he often takes his β-blocker and diuretic every other day in order to stretch his prescription before refilling it. His health has remained excellent since you last saw him a year ago. However, while performing a review of systems, you learn that his heart rhythm has been “funny” in the past two weeks. He states it hasn’t affected his ability to perform his daily activities, including farming, but it was just “strange.” He denies chest pain, shortness of breath, dizziness, syncope or near-syncope, and peripheral edema. He still manages his 450-acre farm, as he has for most of his adult life. Medical history includes hypertension but no angina, MI, or other cardiac disease. Surgical history is remarkable for a right inguinal hernia repair, an appendectomy, and a right hip replacement. His medications include furosemide, potassium chloride, and metoprolol. He has no known drug allergies and does not use recreational drugs or naturopathic herbs. The patient has been a widower for 12 years. His two sons live nearby and help him on his farm. Due to his religious affiliation, he has never used alcohol or tobacco. Review of systems is remarkable for palpitations and an occasional skipped beat. Vital signs include a blood pressure of 108/58 mm Hg; pulse, 50 beats/min and “irregular”; respiratory rate, 14 breaths/min-1; temperature, 98.4°F; and O2 saturation, 96% on room air. His weight is 176 lb and his height, 74 in. Physical exam reveals a pulse that is regularly irregular at a rate of 56 beats/min. There are no murmurs, rubs, or gallops. The neck veins are not distended, and there is no peripheral edema. His lungs are clear to auscultation, and the remainder of his physical exam is unchanged from his previous visit. Given the change in his heart rhythm since his previous visit, you order an ECG and note the following: a ventricular rate of 44 beats/min; PR interval, not measured; QRS duration, 106 ms; QT/QTc interval, 484/413 ms; P axis, 65°; R axis, 11°; and T axis, 6°. What is your interpretation of this ECG?
No Time for Chest Pain When There Are Chores to Do
ANSWER
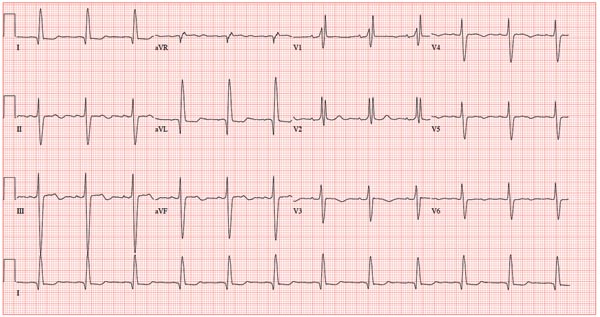
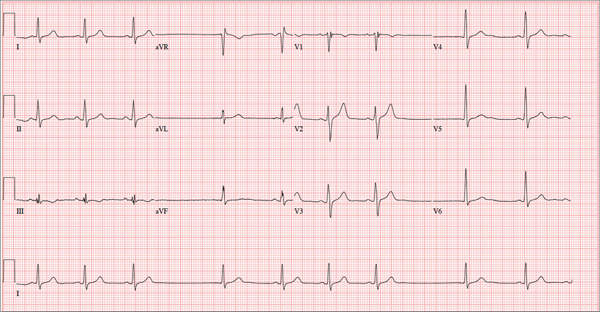
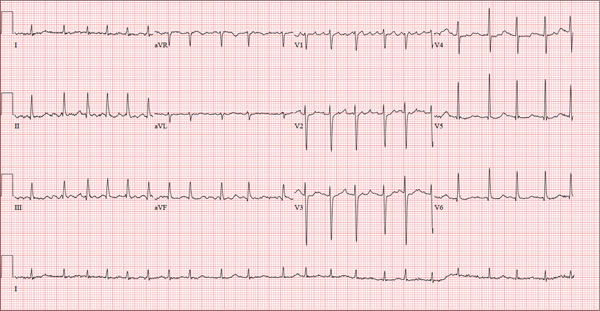
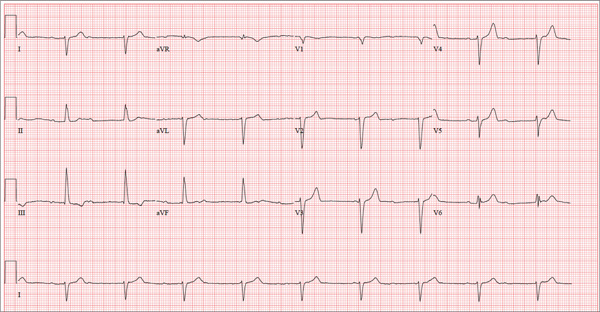
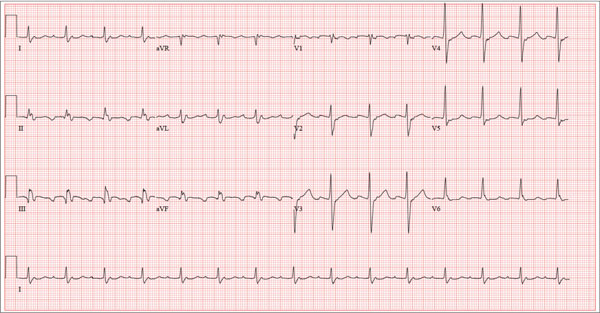
There are three significant findings on this ECG. First, the rhythm shows complete heart block. The ventricular rate is 56 beats/min, and the QRS complex is narrow, resulting in a junctional rhythm. The atrial rate is 98 beats/min (consistent with a sinus rhythm), and there is no relationship of the P waves to the QRS complexes.
The second finding is a rightward axis deviation. Note that the QRS complexes are negative in lead I and positive in lead aVF. To meet criteria for a right-axis deviation, the QRS complex must also be positive in lead aVR. In this case, the QRS complex appears to be isoelectric in aVR, so we call the axis rightward.
The presence of rightward axis deviation is a result of the third finding, an anterior MI. This is due to the LAD artery occlusion discovered at catheterization. It is evident on the ECG by the absence of significant R waves in leads V1 through V4.
Given the need for a β-blocker with titration of dose, the patient underwent implantation of a permanent pacemaker system.
ANSWER
There are three significant findings on this ECG. First, the rhythm shows complete heart block. The ventricular rate is 56 beats/min, and the QRS complex is narrow, resulting in a junctional rhythm. The atrial rate is 98 beats/min (consistent with a sinus rhythm), and there is no relationship of the P waves to the QRS complexes.
The second finding is a rightward axis deviation. Note that the QRS complexes are negative in lead I and positive in lead aVF. To meet criteria for a right-axis deviation, the QRS complex must also be positive in lead aVR. In this case, the QRS complex appears to be isoelectric in aVR, so we call the axis rightward.
The presence of rightward axis deviation is a result of the third finding, an anterior MI. This is due to the LAD artery occlusion discovered at catheterization. It is evident on the ECG by the absence of significant R waves in leads V1 through V4.
Given the need for a β-blocker with titration of dose, the patient underwent implantation of a permanent pacemaker system.
ANSWER
There are three significant findings on this ECG. First, the rhythm shows complete heart block. The ventricular rate is 56 beats/min, and the QRS complex is narrow, resulting in a junctional rhythm. The atrial rate is 98 beats/min (consistent with a sinus rhythm), and there is no relationship of the P waves to the QRS complexes.
The second finding is a rightward axis deviation. Note that the QRS complexes are negative in lead I and positive in lead aVF. To meet criteria for a right-axis deviation, the QRS complex must also be positive in lead aVR. In this case, the QRS complex appears to be isoelectric in aVR, so we call the axis rightward.
The presence of rightward axis deviation is a result of the third finding, an anterior MI. This is due to the LAD artery occlusion discovered at catheterization. It is evident on the ECG by the absence of significant R waves in leads V1 through V4.
Given the need for a β-blocker with titration of dose, the patient underwent implantation of a permanent pacemaker system.
Three days ago, a 62-year-old man was admitted with chest pain and an MI (confirmed by cardiac enzymes). The chest pain started while he was working on his farm, but he did not seek immediate help because he assumed it was heartburn and he had chores to finish. When the pain did not resolve overnight, he finally presented to the emergency department. Cardiac catheterization revealed an occluded left anterior descending (LAD) artery distal to the first diagonal branch and diffuse disease in the circumflex and right coronary arteries. An echocardiogram showed diffuse left ventricular hypokinesis and no evidence of valvular disease. His left ventricular ejection fraction was estimated to be 48%. Medical history is remarkable for hypertension and gout. Surgical history is remarkable for an appendectomy at age 7 and surgical repair of a fractured tibia from a high school football injury. Family history is positive for coronary artery disease; both parents died at young ages (father at 60, mother at 65) of MI, and his older brother had an MI at age 50 (but is currently doing well). The patient owns a 475-acre farm on which he grows corn and soybeans. He also tends to 23 cows and has a large chicken coop. There are five workers to help, but he states that he does most of the work himself. He is divorced and lives alone with five dogs, whom he refers to as his “kids.” He does not smoke, but he has one beer and one shot of bourbon with dinner each night. His only medication at the time of admission was ibuprofen. He had been prescribed lisinopril in the past but hadn’t taken it in six months because “it’s too far a drive to get it refilled.” He has no known drug allergies. Following admission, he was started on a β-blocker (metoprolol), aspirin, atorvastatin, and lisinopril. During rounds, you notice that his hypertension is well controlled. His blood pressure is 118/80 mm Hg, compared to 180/92 mm Hg on admission. He is comfortable and wants to know when he can go home. As you contemplate discharge, a technician hands you the patient’s daily ECG tracing. It shows a ventricular rate of 56 beats/min; QRS duration, 106 ms; QT/QTc interval, 400/386 ms; P axis, 36°; R axis, 120°; and T axis, 7°. What is your interpretation of this ECG?
Healthy and Active, but Getting Fatigued
ANSWER
The correct interpretation of this ECG includes sinus bradycardia with marked sinus arrhythmia and junctional escape beats with sinus arrest. An intraventricular conduction defect is also present.
Sinus bradycardia is indicated by the normal PQRST complexes at a rate of less than 60 beats/min. A marked sinus arrhythmia is evidenced by more than one pause (between third and fourth beats and seventh and eighth beats on the lead I rhythm strip) on the ECG.
Sinus arrest occurs when the sinus node fails to conduct (absence of P wave during the interval of the pause). A normal QRS complex without a preceding P wave indicates a junctional escape beat. Finally, an intraventricular conduction defect is documented by a QRS duration ≥ 110 ms in the absence of a right or left bundle branch block.
ANSWER
The correct interpretation of this ECG includes sinus bradycardia with marked sinus arrhythmia and junctional escape beats with sinus arrest. An intraventricular conduction defect is also present.
Sinus bradycardia is indicated by the normal PQRST complexes at a rate of less than 60 beats/min. A marked sinus arrhythmia is evidenced by more than one pause (between third and fourth beats and seventh and eighth beats on the lead I rhythm strip) on the ECG.
Sinus arrest occurs when the sinus node fails to conduct (absence of P wave during the interval of the pause). A normal QRS complex without a preceding P wave indicates a junctional escape beat. Finally, an intraventricular conduction defect is documented by a QRS duration ≥ 110 ms in the absence of a right or left bundle branch block.
ANSWER
The correct interpretation of this ECG includes sinus bradycardia with marked sinus arrhythmia and junctional escape beats with sinus arrest. An intraventricular conduction defect is also present.
Sinus bradycardia is indicated by the normal PQRST complexes at a rate of less than 60 beats/min. A marked sinus arrhythmia is evidenced by more than one pause (between third and fourth beats and seventh and eighth beats on the lead I rhythm strip) on the ECG.
Sinus arrest occurs when the sinus node fails to conduct (absence of P wave during the interval of the pause). A normal QRS complex without a preceding P wave indicates a junctional escape beat. Finally, an intraventricular conduction defect is documented by a QRS duration ≥ 110 ms in the absence of a right or left bundle branch block.
A 68-year-old retired high school teacher became fatigued while doing yardwork. After sitting down to rest, he noticed that his heart seemed to be skipping beats. He asked his daughter, a pediatric nurse, to come over and check his pulse. She confirmed his suspicion and recommended he go to the emergency department. The patient refused but made an appointment to see his primary care provider. Since you are covering for his usual provider (who is on maternity leave), the patient presents to you. Review of his chart indicates that he has been healthy and active his entire life and has never had any cardiac issues. He does not have hypertension, diabetes, hypothyroidism, or pulmonary problems. His history includes GERD, kidney stones, hyperlipidemia, and a fractured left clavicle. All immunizations and tetanus booster are current. The patient denies any history of chest pain, dyspnea, syncope, near-syncope, palpitations, or other heart rhythm issues (eg, tachycardia, bradycardia, or atrial fibrillation). His last ECG, performed three years ago during a routine visit, showed normal sinus rhythm with normal intervals and no evidence of chamber enlargement; hypertrophy; arrhythmia; P, QRS, or QT interval abnormalities; or blocks. His current medications include esomeprazole magnesium, simvastatin, niacin, and aspirin. He denies illicit or homeopathic drug use and has no known drug allergies. He is a widower who does not drink alcohol or smoke cigarettes. Vital signs include a blood pressure of 108/58 mm Hg; pulse, 60 beats/min with occasional pauses; respiratory rate, 14 breaths/min-1; O2 saturation, 98% on room air; and temperature, 98.9°F. His weight is 169 lb and his height, 74 in. Physical exam reveals a tall, thin, healthy-appearing male in no distress. The HEENT exam is remarkable only for corrective lenses. There is no thyromegaly, jugular venous distention, or lymphadenopathy. The lungs are clear in all fields. The cardiac exam reveals a regular rhythm with occasional pauses and no evidence of murmurs, rubs, or extra heart sounds. The abdomen is soft and nontender, without evidence of organomegaly or masses. The peripheral pulses are 2+ bilaterally in all extremities, and the neurologic exam is intact. An ECG is performed, which reveals a ventricular rate of 55 beats/min; PR interval, 146 ms; QRS duration, 122 ms; QT/QTc interval, 424/405 ms; P axis, 60°; R axis, 38°; and T axis, 29°. What is your interpretation of this ECG?
Too Tired to Stop and Smell the Roses
ANSWER
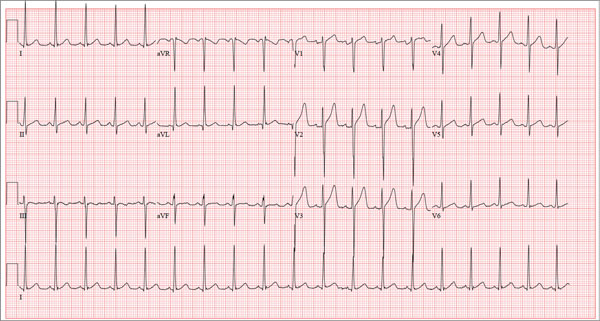
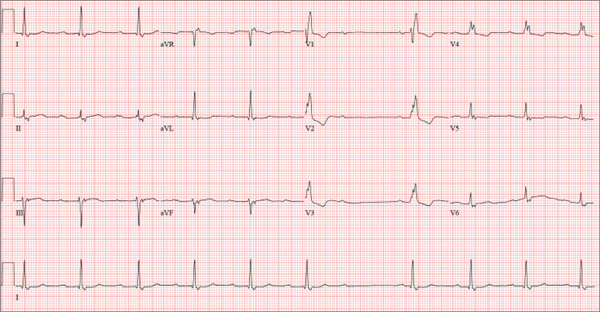
Findings on this ECG include sinus rhythm at a rate of 60 beats/min, evidence of a second-degree atrioventricular (AV) block (Mobitz I), and a right bundle branch block (RBBB).
To understand the rhythm, it is best to focus on the rhythm strip, particularly lead I at the bottom of the ECG. If you measure the P-to-P interval, you will notice that it is consistent and constant at a rate of 60 beats/min, regardless of the QRS complex. If you look at the PR interval from the second to the sixth QRS complex, you will notice that it is regular until the QRS is dropped after the P wave that follows the sixth QRS complex. Following the pause, the PR interval on the seventh, eighth, and ninth QRS complexes gradually prolongs. Although this is not a classic example of Mobitz I block, it is indicative of an AV node with a conduction abnormality.
Subsequent rhythm strips documented multiple blocked PR intervals that corresponded to the patient’s dizziness. The RBBB is evident by the RSR’ pattern seen in lead V1 with a QRS duration ≥ 120 ms.
ANSWER
Findings on this ECG include sinus rhythm at a rate of 60 beats/min, evidence of a second-degree atrioventricular (AV) block (Mobitz I), and a right bundle branch block (RBBB).
To understand the rhythm, it is best to focus on the rhythm strip, particularly lead I at the bottom of the ECG. If you measure the P-to-P interval, you will notice that it is consistent and constant at a rate of 60 beats/min, regardless of the QRS complex. If you look at the PR interval from the second to the sixth QRS complex, you will notice that it is regular until the QRS is dropped after the P wave that follows the sixth QRS complex. Following the pause, the PR interval on the seventh, eighth, and ninth QRS complexes gradually prolongs. Although this is not a classic example of Mobitz I block, it is indicative of an AV node with a conduction abnormality.
Subsequent rhythm strips documented multiple blocked PR intervals that corresponded to the patient’s dizziness. The RBBB is evident by the RSR’ pattern seen in lead V1 with a QRS duration ≥ 120 ms.
ANSWER
Findings on this ECG include sinus rhythm at a rate of 60 beats/min, evidence of a second-degree atrioventricular (AV) block (Mobitz I), and a right bundle branch block (RBBB).
To understand the rhythm, it is best to focus on the rhythm strip, particularly lead I at the bottom of the ECG. If you measure the P-to-P interval, you will notice that it is consistent and constant at a rate of 60 beats/min, regardless of the QRS complex. If you look at the PR interval from the second to the sixth QRS complex, you will notice that it is regular until the QRS is dropped after the P wave that follows the sixth QRS complex. Following the pause, the PR interval on the seventh, eighth, and ninth QRS complexes gradually prolongs. Although this is not a classic example of Mobitz I block, it is indicative of an AV node with a conduction abnormality.
Subsequent rhythm strips documented multiple blocked PR intervals that corresponded to the patient’s dizziness. The RBBB is evident by the RSR’ pattern seen in lead V1 with a QRS duration ≥ 120 ms.
A 74-year-old man lives alone in his home and cares for a large garden of which he is very proud. Recently, his granddaughter noticed that the garden had not been tended to. When asked, her grandfather told her he had been too tired to take care of it. Further questioning revealed that he had experienced frequent dizzy spells and had passed out in his garden about two weeks ago. Since then, he has been reluctant to go outside. Concerned, his granddaughter brings him to your urgent care clinic for evaluation. During the history, you learn that the patient has not seen a clinician in more than 10 years because he “doesn’t like to be a bother.” He has a long-standing diagnosis of hypertension that is untreated because he doesn’t like to take pills. Eliciting information is difficult, but his granddaughter reports that he had a cholecystectomy in the distant past; she cannot recall any other problems. The patient currently takes no medications; he is allergic to penicillin, which produces a true anaphylactic response. He has a remote history of smoking, but he stopped after his wife died of lung cancer 12 years ago. He drinks two or three cans of beer per week and does not use recreational drugs or herbal medicines. He had one son, who died in an automobile accident five years ago; his daughter-in-law visits infrequently and his granddaughter frequently. He has no living siblings. Review of systems is remarkable for knee and hip pain and stiffness from osteoarthritis, as well as occasional constipation. He denies palpitations, irregular or rapid heartbeats, shortness of breath, and lower extremity swelling. Aside from his dizzy spells, he claims to be “healthy as a horse.” Physical exam reveals a blood pressure of 192/102 mm Hg; pulse, 60 beats/min and irregular; respiratory rate, 18 breaths/min; and temperature, 98.1°F. His height is 66 in and his weight, 164 lb. The patient wears corrective lenses, and arcus senilis is present. There are multiple teeth missing, but those that remain are in good repair. There is no thyromegaly, and a soft bruit is present over the left carotid artery. The patient is somewhat barrel chested, and all breath sounds are clear. There is a harsh, early systolic murmur best heard at the left upper sternal border and no extra heart sounds or rubs. The abdomen is scaphoid and soft, and surprisingly, despite the history of a cholecystectomy, there is no abdominal scar. The extremities are consistent with signs of longstanding osteoarthritis. Peripheral pulses are strong bilaterally, and the neurologic exam is grossly intact. You order a chemistry panel, complete blood count, thyroid function studies, liver function studies, and an ECG. While the laboratory data are still pending, you receive the results of the ECG, which show a ventricular rate of 56 beats/min; PR interval, not measurable; QRS duration, 144 ms; QT/QTc interval, 438/422 ms; P axis, 47°; R axis, –24°; and T axis, 55°. What is your interpretation of this ECG—and have you found a reason for his dizziness?
For Lethargic Patient, Trouble Is Brewing
ANSWER
The correct interpretation is an atrial tachycardia with 2:1 ventricular conduction. The ventricular rate is 87 beats/min (690 ms), and the atrial rate is 174 beats/min (345 ms). Two P waves are present for each QRS, which excludes a first-degree atrioventricular block. The less obvious P wave is found in the terminal portion of the QRS complex. (You may convince yourself of this by using calipers to measure the R-R interval, dividing that measurement in half, and then applying it to the ECG. You will see the P waves march through without changing the ventricular response.)
A nonspecific intraventricular conduction delay is also present. The QRS duration is > 100 ms; however, the criteria for right or left bundle branch block are absent.
A thorough investigation revealed that the clerk formulating the herbs for the tea was using, among other things, dried foxglove. Foxglove has been used as a remedy for lethargy in the elderly, presumably because it inadvertently treats symptoms of congestive heart failure. It was the tea consumption that accounted for the presence of digoxin in the patient’s blood. (Recall that there is a substantial overlap between therapeutic and toxic serum concentrations of digoxin.) When the patient stopped consuming the tea, his atrial tachycardia resolved, as did his symptoms.
ANSWER
The correct interpretation is an atrial tachycardia with 2:1 ventricular conduction. The ventricular rate is 87 beats/min (690 ms), and the atrial rate is 174 beats/min (345 ms). Two P waves are present for each QRS, which excludes a first-degree atrioventricular block. The less obvious P wave is found in the terminal portion of the QRS complex. (You may convince yourself of this by using calipers to measure the R-R interval, dividing that measurement in half, and then applying it to the ECG. You will see the P waves march through without changing the ventricular response.)
A nonspecific intraventricular conduction delay is also present. The QRS duration is > 100 ms; however, the criteria for right or left bundle branch block are absent.
A thorough investigation revealed that the clerk formulating the herbs for the tea was using, among other things, dried foxglove. Foxglove has been used as a remedy for lethargy in the elderly, presumably because it inadvertently treats symptoms of congestive heart failure. It was the tea consumption that accounted for the presence of digoxin in the patient’s blood. (Recall that there is a substantial overlap between therapeutic and toxic serum concentrations of digoxin.) When the patient stopped consuming the tea, his atrial tachycardia resolved, as did his symptoms.
ANSWER
The correct interpretation is an atrial tachycardia with 2:1 ventricular conduction. The ventricular rate is 87 beats/min (690 ms), and the atrial rate is 174 beats/min (345 ms). Two P waves are present for each QRS, which excludes a first-degree atrioventricular block. The less obvious P wave is found in the terminal portion of the QRS complex. (You may convince yourself of this by using calipers to measure the R-R interval, dividing that measurement in half, and then applying it to the ECG. You will see the P waves march through without changing the ventricular response.)
A nonspecific intraventricular conduction delay is also present. The QRS duration is > 100 ms; however, the criteria for right or left bundle branch block are absent.
A thorough investigation revealed that the clerk formulating the herbs for the tea was using, among other things, dried foxglove. Foxglove has been used as a remedy for lethargy in the elderly, presumably because it inadvertently treats symptoms of congestive heart failure. It was the tea consumption that accounted for the presence of digoxin in the patient’s blood. (Recall that there is a substantial overlap between therapeutic and toxic serum concentrations of digoxin.) When the patient stopped consuming the tea, his atrial tachycardia resolved, as did his symptoms.
A 72-year-old man presents with a primary complaint of lethargy. He emigrated from Southeast Asia to the United States about a year ago and neither speaks nor understands English. His grandson, who is fluent, accompanies him to his appointment. Through his grandson, the patient explains that he has become increasingly tired in the past four months—to the extent that exercise and activities of daily living have become difficult. The patient’s libido also has been affected. In an effort to correct this, he visited a local Asian goods store, where he was given a mixture of herbs from which to brew tea to treat his symptoms. For three weeks, he consumed the tea twice daily. Initially, his energy, stamina, and libido improved. However, his symptoms eventually returned, so he doubled his tea consumption with the idea that this would improve his condition. Unfortunately, in addition to his lethargy, he is now experiencing palpitations, a fluttering sensation in his chest, and occasional dizziness. He denies chest pain, shortness of breath, nocturnal dyspnea, syncope, or near syncope. Medical history is difficult to elicit. He denies prior history of hypertension, myocardial infarction, congestive heart failure, or diabetes. Neither he nor his grandson understands the concept of arrhythmias (eg, atrial fibrillation). He was treated for tuberculosis as a child and has had no recurrence. He has had no surgeries. The patient takes no prescribed medications. He does, however, use herbal products including ginseng, horny goat weed, and fenugreek (in addition to his herbal tea). He has no known drug allergies. Social history reveals that the patient lives with his son’s family, having moved to the US from Thailand after his wife died of old age. He worked as a farmer his entire life. He drinks one ounce of whiskey daily and smokes 1 to 1.5 packs of cigarettes a day. The review of systems is noncontributory. His grandson is reluctant to ask the patient many questions regarding his health, once he notices his grandfather’s agitation at answering questions. The physical exam reveals a thin, elderly male with weathered skin who is in no acute distress. Vital signs include a blood pressure of 118/62 mm Hg; pulse, 80 beats/min and regular; respiratory rate, 16 breaths/min; and temperature, 97.8°F. His height is 62 in and his weight, 117 lb. The HEENT exam is remarkable for arcus senilis and multiple missing teeth. There is no jugular distention, and the thyroid is not enlarged. The lungs reveal coarse breath sounds that clear with coughing in all lung fields. (The patient has an occasional harsh cough.) The cardiac exam is positive for a grade II/VI systolic murmur best heard at the left upper sternal border, which radiates to the carotid arteries. The rhythm is regular at a rate of 80 beats/min, and there are no clicks or rubs. The abdomen is scaphoid, soft, and nontender, with no palpable masses. The peripheral pulses are strong and equal bilaterally. Extremities demonstrate full range of motion, and the neurologic exam is grossly intact. Routine laboratory tests including a complete blood count and electrolyte panel are obtained. Because you are unsure of his medication regimen, you order a toxicology screen. You are surprised to see a serum digoxin level of 0.7 ng/mL. Finally, given the patient’s symptoms of palpitations and dizziness, you order an ECG. It shows the following: a ventricular rate of 87 beats/min; PR interval, 218 ms; QRS duration, 130 ms; QT/QTc interval, 416/500 ms; P axis, 24°; R axis, 49°; and T axis, 45°. What is your interpretation of this ECG?
What Caused Patient’s Palpitations?
ANSWER
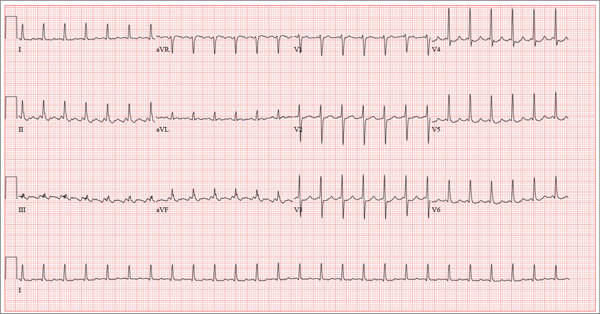
This ECG shows atrial flutter with 2:1 atrioventricular conduction. Additionally, ST depressions are seen in the anterior leads.
Typical sinus node P waves are absent, and atrial conduction at a rate of 310 beats/min is indicated by the sawtooth pattern in leads II and aVF. The ventricular rate is half that of the atrial rate (hence the 2:1 ratio). The ST depressions seen in the anterior leads, thought to be rate related, resolved upon cardioversion to terminate the atrial flutter.
Atrial flutter is uncommon in patients with structurally normal hearts and occurs far less frequently than atrial fibrillation. The etiology of this man’s arrhythmia may be due to pericarditis, based on his history and physical examination.
ANSWER
This ECG shows atrial flutter with 2:1 atrioventricular conduction. Additionally, ST depressions are seen in the anterior leads.
Typical sinus node P waves are absent, and atrial conduction at a rate of 310 beats/min is indicated by the sawtooth pattern in leads II and aVF. The ventricular rate is half that of the atrial rate (hence the 2:1 ratio). The ST depressions seen in the anterior leads, thought to be rate related, resolved upon cardioversion to terminate the atrial flutter.
Atrial flutter is uncommon in patients with structurally normal hearts and occurs far less frequently than atrial fibrillation. The etiology of this man’s arrhythmia may be due to pericarditis, based on his history and physical examination.
ANSWER
This ECG shows atrial flutter with 2:1 atrioventricular conduction. Additionally, ST depressions are seen in the anterior leads.
Typical sinus node P waves are absent, and atrial conduction at a rate of 310 beats/min is indicated by the sawtooth pattern in leads II and aVF. The ventricular rate is half that of the atrial rate (hence the 2:1 ratio). The ST depressions seen in the anterior leads, thought to be rate related, resolved upon cardioversion to terminate the atrial flutter.
Atrial flutter is uncommon in patients with structurally normal hearts and occurs far less frequently than atrial fibrillation. The etiology of this man’s arrhythmia may be due to pericarditis, based on his history and physical examination.
A 52-year-old man developed acute-onset palpitations, shortness of breath, and lightheadedness while sitting at his desk at work. He noticed his heart rate was rapid and asked a coworker to take his pulse for confirmation. He did not experience chest pain, syncope, or near syncope, but if he stood up and tried to walk, he very quickly became fatigued. His coworker tried to call 911; however, the patient asked to be driven to the urgent care center six blocks from their office instead. The patient’s heart rate and symptoms did not change en route. There is no previous history of heart disease. Although the patient works in an office, he is very active. He played hockey in high school and college and continues to play in an amateur league as well as coaching a youth group at the local ice rink. He is also an active member of a local bicycling club and recently completed a 150-mile recreational ride. He has no history of hypertension, diabetes, or pulmonary disease. Surgical history is remarkable for a medial meniscus repair of his right knee and a laparoscopic cholecystectomy, both performed more than 10 years ago. He works as a certified public accountant, does not smoke, and drinks one or two glasses of wine in the evening with meals. He is married and has two adult children. He denies using recreational drugs or herbal medicines. The only medication he uses is ibuprofen as needed for musculoskeletal aches and pains associated with his active lifestyle. He has no known drug allergies, and his immunizations are current. The review of systems is positive for a recent viral upper respiratory illness. He reports having vague, nonspecific substernal chest discomfort, but no pain, at the time of his illness. Symptoms have resolved. There are no other complaints. On arrival, the patient appears anxious and in mild distress, but without pain. Vital signs include a heart rate of 160 beats/min; blood pressure, 100/64 mm Hg; respiratory rate, 18 breaths/min-1; and temperature, 98.4°F. The HEENT exam is unremarkable except for corrective lenses. The chest is clear in all lung fields. There is no jugular venous distention, and carotid upstrokes are brisk. The cardiac exam reveals a regular rhythm at a rate of 150 beats/min with no murmurs or gallops; however, a rub is noted. The abdomen is soft and nontender with no organomegaly. Well-healed scars from his laparoscopic ports are present. The lower extremities show no evidence of edema. Peripheral pulses are strong and equal in both upper and lower extremities, and the neurologic exam is normal. Laboratory studies including a metabolic panel, complete blood count, and cardiac enzymes all yield normal results. An ECG reveals the following: a ventricular rate of 155 beats/min; PR interval, not measured; QRS duration, 78 ms; QT/QTc interval, 272/437 ms; P axis, unmeasurable; R axis, 34°; and T axis, –50°. What is your interpretation of this ECG?