User login
Early response to eptinezumab connotes a long-term response in chronic migraine
Key clinical point: A higher proportion of patients with chronic migraine treated with eptinezumab vs. placebo showed an early treatment response, with most early responders maintaining the response for at least half of the entire 24-week treatment period.
Major finding: At 1 month, a ≥75% reduction in monthly migraine days was achieved by 30.9%, 36.9%, and 15.6% of patients receiving 100 mg eptinezumab, 300 mg eptinezumab, and placebo, respectively. Among patients who achieved a ≥75% migraine response at 1 month, more than one-third and two-thirds maintained the same for the next 5 months and ≥3 months, respectively.
Study details: This was a post hoc analysis of the PROMISE 2 trial, including 1,072 patients with chronic migraine who were randomly assigned to receive 100 mg eptinezumab, 300 mg eptinezumab, or placebo.
Disclosures: The study was funded by H. Lundbeck A/S, Copenhagen. R Cady and T Brevig declared being employees of Lundbeck or a subsidiary company or having equity in Lundbeck, and others declared serving on advisory panels for or receiving grant support, consulting support, or personal compensation from various sources, including Lundbeck.
Source: Buse DC et al. Early response to eptinezumab indicates high likelihood of continued response in patients with chronic migraine. J Headache Pain. 2022;23:29 (Feb 21). Doi: 10.1186/s10194-022-01387-y
Key clinical point: A higher proportion of patients with chronic migraine treated with eptinezumab vs. placebo showed an early treatment response, with most early responders maintaining the response for at least half of the entire 24-week treatment period.
Major finding: At 1 month, a ≥75% reduction in monthly migraine days was achieved by 30.9%, 36.9%, and 15.6% of patients receiving 100 mg eptinezumab, 300 mg eptinezumab, and placebo, respectively. Among patients who achieved a ≥75% migraine response at 1 month, more than one-third and two-thirds maintained the same for the next 5 months and ≥3 months, respectively.
Study details: This was a post hoc analysis of the PROMISE 2 trial, including 1,072 patients with chronic migraine who were randomly assigned to receive 100 mg eptinezumab, 300 mg eptinezumab, or placebo.
Disclosures: The study was funded by H. Lundbeck A/S, Copenhagen. R Cady and T Brevig declared being employees of Lundbeck or a subsidiary company or having equity in Lundbeck, and others declared serving on advisory panels for or receiving grant support, consulting support, or personal compensation from various sources, including Lundbeck.
Source: Buse DC et al. Early response to eptinezumab indicates high likelihood of continued response in patients with chronic migraine. J Headache Pain. 2022;23:29 (Feb 21). Doi: 10.1186/s10194-022-01387-y
Key clinical point: A higher proportion of patients with chronic migraine treated with eptinezumab vs. placebo showed an early treatment response, with most early responders maintaining the response for at least half of the entire 24-week treatment period.
Major finding: At 1 month, a ≥75% reduction in monthly migraine days was achieved by 30.9%, 36.9%, and 15.6% of patients receiving 100 mg eptinezumab, 300 mg eptinezumab, and placebo, respectively. Among patients who achieved a ≥75% migraine response at 1 month, more than one-third and two-thirds maintained the same for the next 5 months and ≥3 months, respectively.
Study details: This was a post hoc analysis of the PROMISE 2 trial, including 1,072 patients with chronic migraine who were randomly assigned to receive 100 mg eptinezumab, 300 mg eptinezumab, or placebo.
Disclosures: The study was funded by H. Lundbeck A/S, Copenhagen. R Cady and T Brevig declared being employees of Lundbeck or a subsidiary company or having equity in Lundbeck, and others declared serving on advisory panels for or receiving grant support, consulting support, or personal compensation from various sources, including Lundbeck.
Source: Buse DC et al. Early response to eptinezumab indicates high likelihood of continued response in patients with chronic migraine. J Headache Pain. 2022;23:29 (Feb 21). Doi: 10.1186/s10194-022-01387-y
Eptinezumab can prevent migraine in patients aged 50 years or older
Key clinical point: With its efficacy and safety in patients aged ≥50 years with migraine being similar to those in the overall study population in the PROMISE-1 and PROMISE-2 trials, eptinezumab could be an effective treatment option in this subpopulation.
Major finding: Compared with those in the total study population, similar changes in mean monthly migraine days were observed in patients with episodic (least squares mean [LSM] changes in days: 100 mg eptinezumab: −3.6; 300 mg eptinezumab: −4.4; placebo: −2.8) and chronic (LSM changes in days: 100 mg eptinezumab: −7.6; 300 mg `eptinezumab: −8.4; placebo: −6.0) migraine. The incidence of treatment-emergent adverse events was similar among treatment groups.
Study details: Of 1,960 patients with episodic or chronic migraine from the PROMISE-1 and PROMISE-2 trials, this post hoc analysis evaluated 385 patients aged ≥50 years who received eptinezumab or placebo.
Disclosures: H. Lundbeck A/S, Copenhagen, sponsored the study. V Martin and C Tassorelli declared being consultants, speakers, clinical trial investigators, or advisory board members for various companies, including Lundbeck; the rest are current/former employees of Lundbeck or a subsidiary/contracted company.
Source: Martin V et al. Eptinezumab for migraine prevention in patients 50 years or older. Acta Neurol Scand. 2022 (Feb 26). Doi: 10.1111/ane.13603
Key clinical point: With its efficacy and safety in patients aged ≥50 years with migraine being similar to those in the overall study population in the PROMISE-1 and PROMISE-2 trials, eptinezumab could be an effective treatment option in this subpopulation.
Major finding: Compared with those in the total study population, similar changes in mean monthly migraine days were observed in patients with episodic (least squares mean [LSM] changes in days: 100 mg eptinezumab: −3.6; 300 mg eptinezumab: −4.4; placebo: −2.8) and chronic (LSM changes in days: 100 mg eptinezumab: −7.6; 300 mg `eptinezumab: −8.4; placebo: −6.0) migraine. The incidence of treatment-emergent adverse events was similar among treatment groups.
Study details: Of 1,960 patients with episodic or chronic migraine from the PROMISE-1 and PROMISE-2 trials, this post hoc analysis evaluated 385 patients aged ≥50 years who received eptinezumab or placebo.
Disclosures: H. Lundbeck A/S, Copenhagen, sponsored the study. V Martin and C Tassorelli declared being consultants, speakers, clinical trial investigators, or advisory board members for various companies, including Lundbeck; the rest are current/former employees of Lundbeck or a subsidiary/contracted company.
Source: Martin V et al. Eptinezumab for migraine prevention in patients 50 years or older. Acta Neurol Scand. 2022 (Feb 26). Doi: 10.1111/ane.13603
Key clinical point: With its efficacy and safety in patients aged ≥50 years with migraine being similar to those in the overall study population in the PROMISE-1 and PROMISE-2 trials, eptinezumab could be an effective treatment option in this subpopulation.
Major finding: Compared with those in the total study population, similar changes in mean monthly migraine days were observed in patients with episodic (least squares mean [LSM] changes in days: 100 mg eptinezumab: −3.6; 300 mg eptinezumab: −4.4; placebo: −2.8) and chronic (LSM changes in days: 100 mg eptinezumab: −7.6; 300 mg `eptinezumab: −8.4; placebo: −6.0) migraine. The incidence of treatment-emergent adverse events was similar among treatment groups.
Study details: Of 1,960 patients with episodic or chronic migraine from the PROMISE-1 and PROMISE-2 trials, this post hoc analysis evaluated 385 patients aged ≥50 years who received eptinezumab or placebo.
Disclosures: H. Lundbeck A/S, Copenhagen, sponsored the study. V Martin and C Tassorelli declared being consultants, speakers, clinical trial investigators, or advisory board members for various companies, including Lundbeck; the rest are current/former employees of Lundbeck or a subsidiary/contracted company.
Source: Martin V et al. Eptinezumab for migraine prevention in patients 50 years or older. Acta Neurol Scand. 2022 (Feb 26). Doi: 10.1111/ane.13603
Intravenous sodium valproate outperforms ibuprofen in acute migraine
Key clinical point: A single intravenous (IV) dose of sodium valproate exerts a better analgesic effect than that of ibuprofen in the treatment of acute migraine attacks.
Major finding: Mean differences in the delta Numerical Rating Scale scores between the sodium valproate and ibuprofen groups were 1.69, 3.61, 4.11, and 3.92 (all P < .001) after 30, 60, 90, and 120 minutes from the time of presentation, respectively, with more patients achieving pain relief with IV sodium valproate (P < .001).
Study details: Findings are from a prospective, double-blinded study including 99 adult patients with migraine without aura who presented to the emergency department with acute headache and were randomly assigned to receive sodium valproate (n = 49) or ibuprofen (n = 50) by IV infusion over 5 minutes.
Disclosures: The authors reported receiving no financial support for the study and declared no conflict of interests.
Source: Dogruyol S et al. Intravenous ibuprofen versus sodium valproate in acute migraine attacks in the emergency department: A randomized clinical trial. Am J Emerg Med. 2022 (Mar 4). Doi: 10.1016/j.ajem.2022.02.046
Key clinical point: A single intravenous (IV) dose of sodium valproate exerts a better analgesic effect than that of ibuprofen in the treatment of acute migraine attacks.
Major finding: Mean differences in the delta Numerical Rating Scale scores between the sodium valproate and ibuprofen groups were 1.69, 3.61, 4.11, and 3.92 (all P < .001) after 30, 60, 90, and 120 minutes from the time of presentation, respectively, with more patients achieving pain relief with IV sodium valproate (P < .001).
Study details: Findings are from a prospective, double-blinded study including 99 adult patients with migraine without aura who presented to the emergency department with acute headache and were randomly assigned to receive sodium valproate (n = 49) or ibuprofen (n = 50) by IV infusion over 5 minutes.
Disclosures: The authors reported receiving no financial support for the study and declared no conflict of interests.
Source: Dogruyol S et al. Intravenous ibuprofen versus sodium valproate in acute migraine attacks in the emergency department: A randomized clinical trial. Am J Emerg Med. 2022 (Mar 4). Doi: 10.1016/j.ajem.2022.02.046
Key clinical point: A single intravenous (IV) dose of sodium valproate exerts a better analgesic effect than that of ibuprofen in the treatment of acute migraine attacks.
Major finding: Mean differences in the delta Numerical Rating Scale scores between the sodium valproate and ibuprofen groups were 1.69, 3.61, 4.11, and 3.92 (all P < .001) after 30, 60, 90, and 120 minutes from the time of presentation, respectively, with more patients achieving pain relief with IV sodium valproate (P < .001).
Study details: Findings are from a prospective, double-blinded study including 99 adult patients with migraine without aura who presented to the emergency department with acute headache and were randomly assigned to receive sodium valproate (n = 49) or ibuprofen (n = 50) by IV infusion over 5 minutes.
Disclosures: The authors reported receiving no financial support for the study and declared no conflict of interests.
Source: Dogruyol S et al. Intravenous ibuprofen versus sodium valproate in acute migraine attacks in the emergency department: A randomized clinical trial. Am J Emerg Med. 2022 (Mar 4). Doi: 10.1016/j.ajem.2022.02.046
Transcranial direct current stimulation: A promising prophylactic strategy for chronic migraine
Key clinical point: Anodal transcranial direct current stimulation (a-tDCS) of the left motor cortex shows significant prophylactic effects in patients with resistant chronic migraine (CM), including early and long-lasting beneficial effects after the stimulation period.
Major finding: The frequency of monthly migraine attacks reduced significantly in the a-tDCS vs. sham a-tDCS group from the end of the first month (−21.0% vs. −1.5%; P = .019) to the end of 3-month follow-up (−31.9% vs. −5.6%; P = .011), with the rate of responders being significantly higher in the a-tDCS vs. sham a-tDCS group at 3 months posttreatment (50% vs. 14%; P = .043).
Study details: Findings are from a patient-assessor–blinded trial including 36 patients with resistant CM who were randomly assigned to receive a-tDCS (n = 18) or sham a-tDCS (n = 18) over 2 months before a 3-month posttreatment follow-up.
Disclosures: The study received no specific funding. The authors declared no conflict of interests.
Source: Hodaj H et al. Long-term prophylactic efficacy of transcranial direct current stimulation in chronic migraine. A randomised, patient-assessor blinded, sham-controlled trial. Brain Stimul. 2022;15(2):441-453 (Feb 24). Doi: 10.1016/j.brs.2022.02.012
Key clinical point: Anodal transcranial direct current stimulation (a-tDCS) of the left motor cortex shows significant prophylactic effects in patients with resistant chronic migraine (CM), including early and long-lasting beneficial effects after the stimulation period.
Major finding: The frequency of monthly migraine attacks reduced significantly in the a-tDCS vs. sham a-tDCS group from the end of the first month (−21.0% vs. −1.5%; P = .019) to the end of 3-month follow-up (−31.9% vs. −5.6%; P = .011), with the rate of responders being significantly higher in the a-tDCS vs. sham a-tDCS group at 3 months posttreatment (50% vs. 14%; P = .043).
Study details: Findings are from a patient-assessor–blinded trial including 36 patients with resistant CM who were randomly assigned to receive a-tDCS (n = 18) or sham a-tDCS (n = 18) over 2 months before a 3-month posttreatment follow-up.
Disclosures: The study received no specific funding. The authors declared no conflict of interests.
Source: Hodaj H et al. Long-term prophylactic efficacy of transcranial direct current stimulation in chronic migraine. A randomised, patient-assessor blinded, sham-controlled trial. Brain Stimul. 2022;15(2):441-453 (Feb 24). Doi: 10.1016/j.brs.2022.02.012
Key clinical point: Anodal transcranial direct current stimulation (a-tDCS) of the left motor cortex shows significant prophylactic effects in patients with resistant chronic migraine (CM), including early and long-lasting beneficial effects after the stimulation period.
Major finding: The frequency of monthly migraine attacks reduced significantly in the a-tDCS vs. sham a-tDCS group from the end of the first month (−21.0% vs. −1.5%; P = .019) to the end of 3-month follow-up (−31.9% vs. −5.6%; P = .011), with the rate of responders being significantly higher in the a-tDCS vs. sham a-tDCS group at 3 months posttreatment (50% vs. 14%; P = .043).
Study details: Findings are from a patient-assessor–blinded trial including 36 patients with resistant CM who were randomly assigned to receive a-tDCS (n = 18) or sham a-tDCS (n = 18) over 2 months before a 3-month posttreatment follow-up.
Disclosures: The study received no specific funding. The authors declared no conflict of interests.
Source: Hodaj H et al. Long-term prophylactic efficacy of transcranial direct current stimulation in chronic migraine. A randomised, patient-assessor blinded, sham-controlled trial. Brain Stimul. 2022;15(2):441-453 (Feb 24). Doi: 10.1016/j.brs.2022.02.012
Anti-CGRP monoclonal antibodies offer long-term efficacy and safety in resistant chronic migraine
Key clinical point: Anti‐calcitonin gene‐related peptide (anti-CGRP) monoclonal antibodies were effective and safe over a 12-month treatment period in patients with treatment-resistant chronic migraine (CM) and medication overuse.
Major finding: Among patients followed up for 12 months, a ≥50% reduction in monthly migraine days and Migraine Disability Assessment score was achieved by 36.4%-66.6% and 84.4%-100% of patients, respectively. No severe treatment-related adverse events were observed.
Study details: Findings are from a prospective, monocentric, cohort study including 203 patients with CM (most also reporting medication overuse) who were resistant to ≥3 preventive treatments and commenced preventive therapy with erenumab, galcanezumab, or fremanezumab.
Disclosures: The study did not receive any financial support. P Geppetti and FD Cesaris reported receiving personal fees and research grants from various sources along with serving as an advisory board member or founding scientist for some sources.
Source: Iannone LF et al. Long-term effectiveness of three anti-CGRP monoclonal antibodies in resistant chronic migraine patients based on the MIDAS score. CNS Drugs. 2022;36:191-202 (Feb 11). Doi: 10.1007/s40263-021-00893-y
Key clinical point: Anti‐calcitonin gene‐related peptide (anti-CGRP) monoclonal antibodies were effective and safe over a 12-month treatment period in patients with treatment-resistant chronic migraine (CM) and medication overuse.
Major finding: Among patients followed up for 12 months, a ≥50% reduction in monthly migraine days and Migraine Disability Assessment score was achieved by 36.4%-66.6% and 84.4%-100% of patients, respectively. No severe treatment-related adverse events were observed.
Study details: Findings are from a prospective, monocentric, cohort study including 203 patients with CM (most also reporting medication overuse) who were resistant to ≥3 preventive treatments and commenced preventive therapy with erenumab, galcanezumab, or fremanezumab.
Disclosures: The study did not receive any financial support. P Geppetti and FD Cesaris reported receiving personal fees and research grants from various sources along with serving as an advisory board member or founding scientist for some sources.
Source: Iannone LF et al. Long-term effectiveness of three anti-CGRP monoclonal antibodies in resistant chronic migraine patients based on the MIDAS score. CNS Drugs. 2022;36:191-202 (Feb 11). Doi: 10.1007/s40263-021-00893-y
Key clinical point: Anti‐calcitonin gene‐related peptide (anti-CGRP) monoclonal antibodies were effective and safe over a 12-month treatment period in patients with treatment-resistant chronic migraine (CM) and medication overuse.
Major finding: Among patients followed up for 12 months, a ≥50% reduction in monthly migraine days and Migraine Disability Assessment score was achieved by 36.4%-66.6% and 84.4%-100% of patients, respectively. No severe treatment-related adverse events were observed.
Study details: Findings are from a prospective, monocentric, cohort study including 203 patients with CM (most also reporting medication overuse) who were resistant to ≥3 preventive treatments and commenced preventive therapy with erenumab, galcanezumab, or fremanezumab.
Disclosures: The study did not receive any financial support. P Geppetti and FD Cesaris reported receiving personal fees and research grants from various sources along with serving as an advisory board member or founding scientist for some sources.
Source: Iannone LF et al. Long-term effectiveness of three anti-CGRP monoclonal antibodies in resistant chronic migraine patients based on the MIDAS score. CNS Drugs. 2022;36:191-202 (Feb 11). Doi: 10.1007/s40263-021-00893-y
Migraine Pathophysiology
Pulsating unilateral headache and nausea
The patient is probably experiencing migraine without aura. Migraines are a complex disorder characterized by recurrent episodes of headache, most often unilateral. These attacks are associated with symptoms related to the central nervous system. Approximately 15% of patients with migraine experience aura (temporary visual, sensory, speech, or other motor disturbances). More research is needed to determine whether migraine with and without aura are potentially different diagnostic entities.
Classic migraine is a clinical diagnosis. When patients experience migraine symptoms routinely, however, it is important to consider whether these signs and symptoms can be accounted for by another diagnosis. Neuroimaging and, less commonly, lumbar puncture may be indicated in some presentations; red flags that call for additional workup are captured in the acronym SNOOP: systemic symptoms, neurologic symptoms, onset is acute, older patients, and previous history. In addition, classic migraine should be distinguished from common headaches as well as rare subtypes of migraine. For instance, hemiplegic migraine typically presents with temporary unilateral hemiparesis, sometimes accompanied by speech disturbance, and may be inherited (familial hemiplegic migraine). Basilar migraine is another rare subtype of migraine that manifests with signs of vertebrobasilar insufficiency. Attacks of chronic paroxysmal hemicrania are unilateral (just as migraines can be in about half of all cases); they are marked by their high intensity but short duration, and are accompanied by same-side facial autonomic symptoms (eg, tearing, congestion). Such patients' history and presentation do not fulfill criteria put forth by the American Headache Society (AHS) for chronic migraine, which specify having headaches 15 or more days per month for more than 3 months, and in which on at least 8 days per month those attacks are consistent with migraine or are relieved by a triptan or ergot derivative.
Migraine management must be personalized for each patient and is often associated with a marked trial-and-error period. Migraine without aura and migraine with aura are treated via similar approaches. AHS guidelines include several medications that may be effective in mitigating migraines, including both migraine-specific agents (ergotamine, ergotamine derivatives, and lasmiditan), and nonspecific agents (NSAIDs, combination analgesics, intravenous magnesium, isometheptene-containing compounds, and antiemetics). Triptans represent first-line acute treatment for migraine, but the FDA has approved five acute migraine treatments in total: celecoxib, lasmiditan, remote electrical neuromodulation (REN), rimegepant, and ubrogepant. For moderate or severe attacks, migraine-specific agents are recommended: beyond triptans, dihydroergotamine (DHE), small-molecule calcitonin gene-related peptide receptor antagonists (gepants), and selective serotonin (5-HT1F) receptor agonists (ditans). Patients should limit medication use to an average of two headache days per week, and those who do not find relief within these parameters are candidates for preventive migraine treatment.
Angeliki Vgontzas, MD, Instructor, Department of Neurology, Harvard Medical School; Associate Neurologist, Department of Neurology, Brigham and Women's Hospital/Brigham and Women's Faulkner Hospital, Boston, Massachusetts.
Angeliki Vgontzas, MD, has disclosed no relevant financial relationships.
The patient is probably experiencing migraine without aura. Migraines are a complex disorder characterized by recurrent episodes of headache, most often unilateral. These attacks are associated with symptoms related to the central nervous system. Approximately 15% of patients with migraine experience aura (temporary visual, sensory, speech, or other motor disturbances). More research is needed to determine whether migraine with and without aura are potentially different diagnostic entities.
Classic migraine is a clinical diagnosis. When patients experience migraine symptoms routinely, however, it is important to consider whether these signs and symptoms can be accounted for by another diagnosis. Neuroimaging and, less commonly, lumbar puncture may be indicated in some presentations; red flags that call for additional workup are captured in the acronym SNOOP: systemic symptoms, neurologic symptoms, onset is acute, older patients, and previous history. In addition, classic migraine should be distinguished from common headaches as well as rare subtypes of migraine. For instance, hemiplegic migraine typically presents with temporary unilateral hemiparesis, sometimes accompanied by speech disturbance, and may be inherited (familial hemiplegic migraine). Basilar migraine is another rare subtype of migraine that manifests with signs of vertebrobasilar insufficiency. Attacks of chronic paroxysmal hemicrania are unilateral (just as migraines can be in about half of all cases); they are marked by their high intensity but short duration, and are accompanied by same-side facial autonomic symptoms (eg, tearing, congestion). Such patients' history and presentation do not fulfill criteria put forth by the American Headache Society (AHS) for chronic migraine, which specify having headaches 15 or more days per month for more than 3 months, and in which on at least 8 days per month those attacks are consistent with migraine or are relieved by a triptan or ergot derivative.
Migraine management must be personalized for each patient and is often associated with a marked trial-and-error period. Migraine without aura and migraine with aura are treated via similar approaches. AHS guidelines include several medications that may be effective in mitigating migraines, including both migraine-specific agents (ergotamine, ergotamine derivatives, and lasmiditan), and nonspecific agents (NSAIDs, combination analgesics, intravenous magnesium, isometheptene-containing compounds, and antiemetics). Triptans represent first-line acute treatment for migraine, but the FDA has approved five acute migraine treatments in total: celecoxib, lasmiditan, remote electrical neuromodulation (REN), rimegepant, and ubrogepant. For moderate or severe attacks, migraine-specific agents are recommended: beyond triptans, dihydroergotamine (DHE), small-molecule calcitonin gene-related peptide receptor antagonists (gepants), and selective serotonin (5-HT1F) receptor agonists (ditans). Patients should limit medication use to an average of two headache days per week, and those who do not find relief within these parameters are candidates for preventive migraine treatment.
Angeliki Vgontzas, MD, Instructor, Department of Neurology, Harvard Medical School; Associate Neurologist, Department of Neurology, Brigham and Women's Hospital/Brigham and Women's Faulkner Hospital, Boston, Massachusetts.
Angeliki Vgontzas, MD, has disclosed no relevant financial relationships.
The patient is probably experiencing migraine without aura. Migraines are a complex disorder characterized by recurrent episodes of headache, most often unilateral. These attacks are associated with symptoms related to the central nervous system. Approximately 15% of patients with migraine experience aura (temporary visual, sensory, speech, or other motor disturbances). More research is needed to determine whether migraine with and without aura are potentially different diagnostic entities.
Classic migraine is a clinical diagnosis. When patients experience migraine symptoms routinely, however, it is important to consider whether these signs and symptoms can be accounted for by another diagnosis. Neuroimaging and, less commonly, lumbar puncture may be indicated in some presentations; red flags that call for additional workup are captured in the acronym SNOOP: systemic symptoms, neurologic symptoms, onset is acute, older patients, and previous history. In addition, classic migraine should be distinguished from common headaches as well as rare subtypes of migraine. For instance, hemiplegic migraine typically presents with temporary unilateral hemiparesis, sometimes accompanied by speech disturbance, and may be inherited (familial hemiplegic migraine). Basilar migraine is another rare subtype of migraine that manifests with signs of vertebrobasilar insufficiency. Attacks of chronic paroxysmal hemicrania are unilateral (just as migraines can be in about half of all cases); they are marked by their high intensity but short duration, and are accompanied by same-side facial autonomic symptoms (eg, tearing, congestion). Such patients' history and presentation do not fulfill criteria put forth by the American Headache Society (AHS) for chronic migraine, which specify having headaches 15 or more days per month for more than 3 months, and in which on at least 8 days per month those attacks are consistent with migraine or are relieved by a triptan or ergot derivative.
Migraine management must be personalized for each patient and is often associated with a marked trial-and-error period. Migraine without aura and migraine with aura are treated via similar approaches. AHS guidelines include several medications that may be effective in mitigating migraines, including both migraine-specific agents (ergotamine, ergotamine derivatives, and lasmiditan), and nonspecific agents (NSAIDs, combination analgesics, intravenous magnesium, isometheptene-containing compounds, and antiemetics). Triptans represent first-line acute treatment for migraine, but the FDA has approved five acute migraine treatments in total: celecoxib, lasmiditan, remote electrical neuromodulation (REN), rimegepant, and ubrogepant. For moderate or severe attacks, migraine-specific agents are recommended: beyond triptans, dihydroergotamine (DHE), small-molecule calcitonin gene-related peptide receptor antagonists (gepants), and selective serotonin (5-HT1F) receptor agonists (ditans). Patients should limit medication use to an average of two headache days per week, and those who do not find relief within these parameters are candidates for preventive migraine treatment.
Angeliki Vgontzas, MD, Instructor, Department of Neurology, Harvard Medical School; Associate Neurologist, Department of Neurology, Brigham and Women's Hospital/Brigham and Women's Faulkner Hospital, Boston, Massachusetts.
Angeliki Vgontzas, MD, has disclosed no relevant financial relationships.
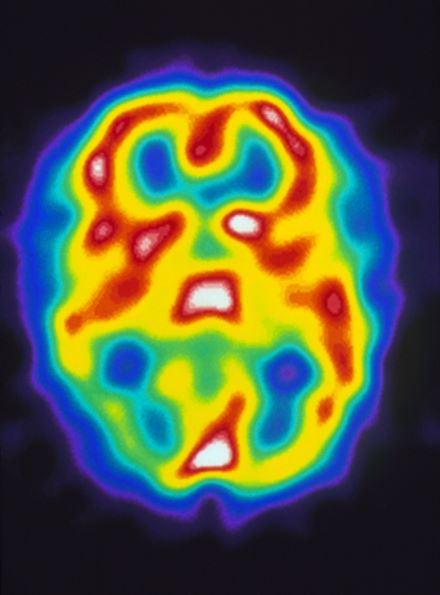
A 22-year-old woman presents with a pulsating unilateral headache (right side) and is very nauseated. The patient reports that since childhood, she has been prone to headaches, with no other significant medical history. Over the past year or so, the headaches have been occurring about once or twice a month, have taken on a throbbing quality, and usually last for several days without relief from nonsteroidal anti-inflammatory drugs (NSAIDs). While taking part in a clinical trial, the patient undergoes a single photon emission CT scan which shows reduced blood flow (lower left).