User login
Ticagrelor may be superior to clopidogrel in poor metabolizers
LOS ANGELES – In patients who had experienced a minor stroke or a transient ischemic attack with a moderate to high risk of stroke, the combination of ticagrelor and aspirin reduced the 90-day incidence of high on-treatment platelet reactivity, according to results from the PRINCE trial.
Although the combination outperformed clopidogrel (Plavix) plus aspirin, ticagrelor (Brilinta) was associated with higher bleeding risk.
The researchers also saw a trend toward a reduction in strokes that did not reach statistical significance, but the trial was halted following an interim analysis showing that the high on-treatment platelet reactivity (HOPR) endpoint, defined as P2Y12 reaction unit (PRU) greater than 208, showed a statistically significant difference. “To prove the clinical benefit, we will need a larger sample size,” study first author and presenter Yilong Wang, MD, PhD, of Beijing Tiantan Hospital, Capital Medical University, said in an interview at the International Stroke Conference, sponsored by the American Heart Association.
Previously, the SOCRATES trial found no advantage to treatment with ticagrelor over aspirin, but a prespecified exploratory analysis focusing on Asian patients (Stroke. 2017;48:167-73) found a trend toward reducing vascular events in the ticagrelor group, compared with patients taking aspirin.
In the Platelet Reactivity in Acute Stroke or Transient Ischemic Attack (PRINCE) trial, the researchers sought to examine the safety and efficacy of ticagrelor when compared with clopidogrel in 675 Asian patients (mean age 61 years, one-quarter of whom were female) from 26 centers in China and randomized them to ticagrelor plus aspirin (Tica) or clopidogrel plus aspirin (Clop). Within 24 hours of symptom onset, patients received 180 mg ticagrelor or 300 mg clopidogrel plus 100-300 mg aspirin. During days 1-21, they received 90 mg ticagrelor twice per day or 75 mg clopidogrel once per day. Both groups received 100 mg aspirin once per day. From day 21 to day 90, they received 90 mg ticagrelor twice per day or 75 mg clopidogrel once per day, with no aspirin.
At 90 days, the mean PRU value was 175.44 in the Clop group, compared with 69.24 in the Tica group. Overall, 27.7% of the Clop group experienced HOPR in the first 7 days, compared with 3.9% of the Tica group. At 90 days, 29.7% of the Clop group had experienced HOPR, compared with 12.5% of the Tica group (odds ratio, 0.33; 95% confidence interval, 0.21-0.51; P less than .001).
Ticagrelor was associated with greater benefit among those with impaired ability to metabolize clopidogrel. Among poor metabolizers, HOPR occurred in 10.5% in the Tica group and 42.4% of the Clop group (OR, 0.16; 95% CI, 0.05-0.56; P = .004). A similar favorable effect was seen in intermediate metabolizers in the Tica group (OR, 0.24; 95% CI, 0.12-0.49; P less than .001).
The 90-day stroke rate was no different between the Tica and Clop groups (6.3% vs. 8.8%, respectively; P = .20).
Minimal bleeding was higher in the Tica group (19.0% vs. 10.6%; hazard ratio, 1.86; P = .003), as was any bleeding (22.3% vs. 14.2%; HR, 1.65; P = .007). There were three deaths in the Tica group and two in the Clop group.
Dyspnea was the most common cause of drug discontinuation, and occurred in 4.2% of patients taking ticagrelor but none of the patients taking clopidogrel (P = .0001).
The researchers hope to demonstrate the clinical benefits of the combination in the upcoming PRINCE 2 trial. The results will have an important impact because CYP2C19 loss of function alleles are more common in Asian population. “It’s a very big problem for us,” Dr. Wang said.
The study was funded by the National Natural Science Foundation of China, the Beijing Institute for Brain, and the Beijing Municipal Science & Technology Commission of Cerebral Vascular Disease. AstraZeneca provided study drugs. Dr. Wang reported having no financial disclosures.
SOURCE: Wang Y et al. ISC 2018, abstract LB8
LOS ANGELES – In patients who had experienced a minor stroke or a transient ischemic attack with a moderate to high risk of stroke, the combination of ticagrelor and aspirin reduced the 90-day incidence of high on-treatment platelet reactivity, according to results from the PRINCE trial.
Although the combination outperformed clopidogrel (Plavix) plus aspirin, ticagrelor (Brilinta) was associated with higher bleeding risk.
The researchers also saw a trend toward a reduction in strokes that did not reach statistical significance, but the trial was halted following an interim analysis showing that the high on-treatment platelet reactivity (HOPR) endpoint, defined as P2Y12 reaction unit (PRU) greater than 208, showed a statistically significant difference. “To prove the clinical benefit, we will need a larger sample size,” study first author and presenter Yilong Wang, MD, PhD, of Beijing Tiantan Hospital, Capital Medical University, said in an interview at the International Stroke Conference, sponsored by the American Heart Association.
Previously, the SOCRATES trial found no advantage to treatment with ticagrelor over aspirin, but a prespecified exploratory analysis focusing on Asian patients (Stroke. 2017;48:167-73) found a trend toward reducing vascular events in the ticagrelor group, compared with patients taking aspirin.
In the Platelet Reactivity in Acute Stroke or Transient Ischemic Attack (PRINCE) trial, the researchers sought to examine the safety and efficacy of ticagrelor when compared with clopidogrel in 675 Asian patients (mean age 61 years, one-quarter of whom were female) from 26 centers in China and randomized them to ticagrelor plus aspirin (Tica) or clopidogrel plus aspirin (Clop). Within 24 hours of symptom onset, patients received 180 mg ticagrelor or 300 mg clopidogrel plus 100-300 mg aspirin. During days 1-21, they received 90 mg ticagrelor twice per day or 75 mg clopidogrel once per day. Both groups received 100 mg aspirin once per day. From day 21 to day 90, they received 90 mg ticagrelor twice per day or 75 mg clopidogrel once per day, with no aspirin.
At 90 days, the mean PRU value was 175.44 in the Clop group, compared with 69.24 in the Tica group. Overall, 27.7% of the Clop group experienced HOPR in the first 7 days, compared with 3.9% of the Tica group. At 90 days, 29.7% of the Clop group had experienced HOPR, compared with 12.5% of the Tica group (odds ratio, 0.33; 95% confidence interval, 0.21-0.51; P less than .001).
Ticagrelor was associated with greater benefit among those with impaired ability to metabolize clopidogrel. Among poor metabolizers, HOPR occurred in 10.5% in the Tica group and 42.4% of the Clop group (OR, 0.16; 95% CI, 0.05-0.56; P = .004). A similar favorable effect was seen in intermediate metabolizers in the Tica group (OR, 0.24; 95% CI, 0.12-0.49; P less than .001).
The 90-day stroke rate was no different between the Tica and Clop groups (6.3% vs. 8.8%, respectively; P = .20).
Minimal bleeding was higher in the Tica group (19.0% vs. 10.6%; hazard ratio, 1.86; P = .003), as was any bleeding (22.3% vs. 14.2%; HR, 1.65; P = .007). There were three deaths in the Tica group and two in the Clop group.
Dyspnea was the most common cause of drug discontinuation, and occurred in 4.2% of patients taking ticagrelor but none of the patients taking clopidogrel (P = .0001).
The researchers hope to demonstrate the clinical benefits of the combination in the upcoming PRINCE 2 trial. The results will have an important impact because CYP2C19 loss of function alleles are more common in Asian population. “It’s a very big problem for us,” Dr. Wang said.
The study was funded by the National Natural Science Foundation of China, the Beijing Institute for Brain, and the Beijing Municipal Science & Technology Commission of Cerebral Vascular Disease. AstraZeneca provided study drugs. Dr. Wang reported having no financial disclosures.
SOURCE: Wang Y et al. ISC 2018, abstract LB8
LOS ANGELES – In patients who had experienced a minor stroke or a transient ischemic attack with a moderate to high risk of stroke, the combination of ticagrelor and aspirin reduced the 90-day incidence of high on-treatment platelet reactivity, according to results from the PRINCE trial.
Although the combination outperformed clopidogrel (Plavix) plus aspirin, ticagrelor (Brilinta) was associated with higher bleeding risk.
The researchers also saw a trend toward a reduction in strokes that did not reach statistical significance, but the trial was halted following an interim analysis showing that the high on-treatment platelet reactivity (HOPR) endpoint, defined as P2Y12 reaction unit (PRU) greater than 208, showed a statistically significant difference. “To prove the clinical benefit, we will need a larger sample size,” study first author and presenter Yilong Wang, MD, PhD, of Beijing Tiantan Hospital, Capital Medical University, said in an interview at the International Stroke Conference, sponsored by the American Heart Association.
Previously, the SOCRATES trial found no advantage to treatment with ticagrelor over aspirin, but a prespecified exploratory analysis focusing on Asian patients (Stroke. 2017;48:167-73) found a trend toward reducing vascular events in the ticagrelor group, compared with patients taking aspirin.
In the Platelet Reactivity in Acute Stroke or Transient Ischemic Attack (PRINCE) trial, the researchers sought to examine the safety and efficacy of ticagrelor when compared with clopidogrel in 675 Asian patients (mean age 61 years, one-quarter of whom were female) from 26 centers in China and randomized them to ticagrelor plus aspirin (Tica) or clopidogrel plus aspirin (Clop). Within 24 hours of symptom onset, patients received 180 mg ticagrelor or 300 mg clopidogrel plus 100-300 mg aspirin. During days 1-21, they received 90 mg ticagrelor twice per day or 75 mg clopidogrel once per day. Both groups received 100 mg aspirin once per day. From day 21 to day 90, they received 90 mg ticagrelor twice per day or 75 mg clopidogrel once per day, with no aspirin.
At 90 days, the mean PRU value was 175.44 in the Clop group, compared with 69.24 in the Tica group. Overall, 27.7% of the Clop group experienced HOPR in the first 7 days, compared with 3.9% of the Tica group. At 90 days, 29.7% of the Clop group had experienced HOPR, compared with 12.5% of the Tica group (odds ratio, 0.33; 95% confidence interval, 0.21-0.51; P less than .001).
Ticagrelor was associated with greater benefit among those with impaired ability to metabolize clopidogrel. Among poor metabolizers, HOPR occurred in 10.5% in the Tica group and 42.4% of the Clop group (OR, 0.16; 95% CI, 0.05-0.56; P = .004). A similar favorable effect was seen in intermediate metabolizers in the Tica group (OR, 0.24; 95% CI, 0.12-0.49; P less than .001).
The 90-day stroke rate was no different between the Tica and Clop groups (6.3% vs. 8.8%, respectively; P = .20).
Minimal bleeding was higher in the Tica group (19.0% vs. 10.6%; hazard ratio, 1.86; P = .003), as was any bleeding (22.3% vs. 14.2%; HR, 1.65; P = .007). There were three deaths in the Tica group and two in the Clop group.
Dyspnea was the most common cause of drug discontinuation, and occurred in 4.2% of patients taking ticagrelor but none of the patients taking clopidogrel (P = .0001).
The researchers hope to demonstrate the clinical benefits of the combination in the upcoming PRINCE 2 trial. The results will have an important impact because CYP2C19 loss of function alleles are more common in Asian population. “It’s a very big problem for us,” Dr. Wang said.
The study was funded by the National Natural Science Foundation of China, the Beijing Institute for Brain, and the Beijing Municipal Science & Technology Commission of Cerebral Vascular Disease. AstraZeneca provided study drugs. Dr. Wang reported having no financial disclosures.
SOURCE: Wang Y et al. ISC 2018, abstract LB8
REPORTING FROM ISC 2018
Key clinical point: Ticagrelor may be a better option than clopidogrel in patients with loss-of-function CYP2C19 alleles.
Major finding: Patients on ticagrelor had a lower 90-day risk of high on-treatment platelet reactivity (OR, 0.33).
Data source: Randomized, open-label trial with blinded assessments (n = 675).
Disclosures: The study was funded by the National Natural Science Foundation of China, the Beijing Institute for Brain, and the Beijing Municipal Science & Technology Commission of Cerebral Vascular Disease. AstraZeneca provided study drugs. Dr. Wang reported having no financial disclosures.
Source: Wang Y et al. ISC 2018, abstract LB8
Tenecteplase surpasses alteplase for thrombolysing acute ischemic stroke
LOS ANGELES – Thrombolysis with tenecteplase beat alteplase on an acute imaging endpoint in patients with acute ischemic stroke who were on their way to also get thrombectomy in a randomized, multicenter study with 202 patients in Australia and New Zealand.
The results of the trial, called Tenecteplase Versus Alteplase Before Endovascular Therapy for Ischemic Stroke (EXTEND-IA TNK), showed that when the patients underwent their initial angiogram after receiving thrombolysis and before their thrombectomy procedure, the percentage of patients with robust blood flow – a Thrombolysis in Cerebral Infarction (TICI) score of 2b or 3 or no retrievable thrombus – was 22% in the patients treated with tenecteplase 0.25 mg/kg and 10% among those who received alteplase 0.9 mg/kg. After adjustment, the 12% incremental change in robust reperfusion with tenecteplase calculated into a 2.6-fold higher rate of robust reperfusion, statistically significant for both noninferiority and for superiority, Bruce C. Campbell, MBBS, PhD, said at the International Stroke Conference, sponsored by the American Heart Association.
Tenecteplase is a genetically-modified tissue plasminogen activator with enhanced fibrin specificity that increases the drug’s half life and allows for bolus administration, unlike alteplase, which needs continuous infusion (CNS Drugs. 2015 Oct;29[10]:811-8). Tenecteplase also has a U.S. wholesale price that is about $3,000 cheaper per vial than alteplase, said Dr. Campbell, professor of neurology at the University of Melbourne and head of hyperacute stroke at Royal Melbourne Hospital.
But further data are needed before tenecteplase is ready for routine use, conceded Dr. Campbell, an assessment other experts agreed with. Dr. Campbell cited two studies in progress that are comparing tenecteplase with alteplase in acute ischemic stroke patients not headed for endovascular thrombectomy, as well as a study he is leading that compares the tenecteplase dose he just tested, 0.25 mg/kg, with a higher dose, 0.40 mg/kg.
Several reports have appeared in recent years suggesting that treatment with tenecteplase seems to be at least as good as alteplase in ischemic stroke patients. For example, a randomized trial with 75 ischemic stroke patients selected by imaging at three Australian centers showed that treatment with tenecteplase produced a significant 24% improvement in the rate of arterial reperfusion and an average 5-point improvement in NIH Stroke Scale score (N Engl J Med. 2012;366[12]:1099-107). And results from the NOR-TEST study recently showed that among 1,100 patients randomized at 13 Norwegian centers, the primary outcome of a 90-day modified Rankin Scale score of 0-1 was achieved by 64% of the tenecteplase patients and by 63% of those who received alteplase (Lancet Neurol. 2017 Oct;16[10]:781-8).
The EXTEND-IA TNK trial ran during 2015-2017 at 18 hospitals. All enrolled patients received their thrombolytic treatment within 4.5 hours of their stroke onset, and underwent endovascular thrombectomy within 6 hours of onset. The safety outcomes of death, symptomatic intracranial hemorrhage, and parenchymal hematoma occurred at statistically similar rates in both treatment arms.
The study was investigator initiated and funded chiefly by the Australian government. Medtronic provided an unrestricted grant for trial infrastructure but had no role in study design conduct or analysis. Dr. Campbell and Dr. Powers had no disclosures.
SOURCE: Campbell B et al. ISC 2018, abstract LB2.
In the EXTEND-IA TNK study, tenecteplase appeared to act better than alteplase and has the extra advantage of being administered as a bolus injection. Alteplase is delivered as a drip, and it’s often hard to get patients with an intravenous infusion out of the hospital quickly when you have to transport the patient. You need a nurse in the ambulance monitoring the drip. With tenecteplase you administer the bolus and can then send the patient without an intravenous line.
Jeffrey L. Saver, MD, is professor of neurology and director of the stroke unit at the University of California, Los Angeles. He has received research support and personal fees from Medtronic-Abbott and Neuravia. He made these comments in an interview.
In the EXTEND-IA TNK study, tenecteplase appeared to act better than alteplase and has the extra advantage of being administered as a bolus injection. Alteplase is delivered as a drip, and it’s often hard to get patients with an intravenous infusion out of the hospital quickly when you have to transport the patient. You need a nurse in the ambulance monitoring the drip. With tenecteplase you administer the bolus and can then send the patient without an intravenous line.
Jeffrey L. Saver, MD, is professor of neurology and director of the stroke unit at the University of California, Los Angeles. He has received research support and personal fees from Medtronic-Abbott and Neuravia. He made these comments in an interview.
In the EXTEND-IA TNK study, tenecteplase appeared to act better than alteplase and has the extra advantage of being administered as a bolus injection. Alteplase is delivered as a drip, and it’s often hard to get patients with an intravenous infusion out of the hospital quickly when you have to transport the patient. You need a nurse in the ambulance monitoring the drip. With tenecteplase you administer the bolus and can then send the patient without an intravenous line.
Jeffrey L. Saver, MD, is professor of neurology and director of the stroke unit at the University of California, Los Angeles. He has received research support and personal fees from Medtronic-Abbott and Neuravia. He made these comments in an interview.
LOS ANGELES – Thrombolysis with tenecteplase beat alteplase on an acute imaging endpoint in patients with acute ischemic stroke who were on their way to also get thrombectomy in a randomized, multicenter study with 202 patients in Australia and New Zealand.
The results of the trial, called Tenecteplase Versus Alteplase Before Endovascular Therapy for Ischemic Stroke (EXTEND-IA TNK), showed that when the patients underwent their initial angiogram after receiving thrombolysis and before their thrombectomy procedure, the percentage of patients with robust blood flow – a Thrombolysis in Cerebral Infarction (TICI) score of 2b or 3 or no retrievable thrombus – was 22% in the patients treated with tenecteplase 0.25 mg/kg and 10% among those who received alteplase 0.9 mg/kg. After adjustment, the 12% incremental change in robust reperfusion with tenecteplase calculated into a 2.6-fold higher rate of robust reperfusion, statistically significant for both noninferiority and for superiority, Bruce C. Campbell, MBBS, PhD, said at the International Stroke Conference, sponsored by the American Heart Association.
Tenecteplase is a genetically-modified tissue plasminogen activator with enhanced fibrin specificity that increases the drug’s half life and allows for bolus administration, unlike alteplase, which needs continuous infusion (CNS Drugs. 2015 Oct;29[10]:811-8). Tenecteplase also has a U.S. wholesale price that is about $3,000 cheaper per vial than alteplase, said Dr. Campbell, professor of neurology at the University of Melbourne and head of hyperacute stroke at Royal Melbourne Hospital.
But further data are needed before tenecteplase is ready for routine use, conceded Dr. Campbell, an assessment other experts agreed with. Dr. Campbell cited two studies in progress that are comparing tenecteplase with alteplase in acute ischemic stroke patients not headed for endovascular thrombectomy, as well as a study he is leading that compares the tenecteplase dose he just tested, 0.25 mg/kg, with a higher dose, 0.40 mg/kg.
Several reports have appeared in recent years suggesting that treatment with tenecteplase seems to be at least as good as alteplase in ischemic stroke patients. For example, a randomized trial with 75 ischemic stroke patients selected by imaging at three Australian centers showed that treatment with tenecteplase produced a significant 24% improvement in the rate of arterial reperfusion and an average 5-point improvement in NIH Stroke Scale score (N Engl J Med. 2012;366[12]:1099-107). And results from the NOR-TEST study recently showed that among 1,100 patients randomized at 13 Norwegian centers, the primary outcome of a 90-day modified Rankin Scale score of 0-1 was achieved by 64% of the tenecteplase patients and by 63% of those who received alteplase (Lancet Neurol. 2017 Oct;16[10]:781-8).
The EXTEND-IA TNK trial ran during 2015-2017 at 18 hospitals. All enrolled patients received their thrombolytic treatment within 4.5 hours of their stroke onset, and underwent endovascular thrombectomy within 6 hours of onset. The safety outcomes of death, symptomatic intracranial hemorrhage, and parenchymal hematoma occurred at statistically similar rates in both treatment arms.
The study was investigator initiated and funded chiefly by the Australian government. Medtronic provided an unrestricted grant for trial infrastructure but had no role in study design conduct or analysis. Dr. Campbell and Dr. Powers had no disclosures.
SOURCE: Campbell B et al. ISC 2018, abstract LB2.
LOS ANGELES – Thrombolysis with tenecteplase beat alteplase on an acute imaging endpoint in patients with acute ischemic stroke who were on their way to also get thrombectomy in a randomized, multicenter study with 202 patients in Australia and New Zealand.
The results of the trial, called Tenecteplase Versus Alteplase Before Endovascular Therapy for Ischemic Stroke (EXTEND-IA TNK), showed that when the patients underwent their initial angiogram after receiving thrombolysis and before their thrombectomy procedure, the percentage of patients with robust blood flow – a Thrombolysis in Cerebral Infarction (TICI) score of 2b or 3 or no retrievable thrombus – was 22% in the patients treated with tenecteplase 0.25 mg/kg and 10% among those who received alteplase 0.9 mg/kg. After adjustment, the 12% incremental change in robust reperfusion with tenecteplase calculated into a 2.6-fold higher rate of robust reperfusion, statistically significant for both noninferiority and for superiority, Bruce C. Campbell, MBBS, PhD, said at the International Stroke Conference, sponsored by the American Heart Association.
Tenecteplase is a genetically-modified tissue plasminogen activator with enhanced fibrin specificity that increases the drug’s half life and allows for bolus administration, unlike alteplase, which needs continuous infusion (CNS Drugs. 2015 Oct;29[10]:811-8). Tenecteplase also has a U.S. wholesale price that is about $3,000 cheaper per vial than alteplase, said Dr. Campbell, professor of neurology at the University of Melbourne and head of hyperacute stroke at Royal Melbourne Hospital.
But further data are needed before tenecteplase is ready for routine use, conceded Dr. Campbell, an assessment other experts agreed with. Dr. Campbell cited two studies in progress that are comparing tenecteplase with alteplase in acute ischemic stroke patients not headed for endovascular thrombectomy, as well as a study he is leading that compares the tenecteplase dose he just tested, 0.25 mg/kg, with a higher dose, 0.40 mg/kg.
Several reports have appeared in recent years suggesting that treatment with tenecteplase seems to be at least as good as alteplase in ischemic stroke patients. For example, a randomized trial with 75 ischemic stroke patients selected by imaging at three Australian centers showed that treatment with tenecteplase produced a significant 24% improvement in the rate of arterial reperfusion and an average 5-point improvement in NIH Stroke Scale score (N Engl J Med. 2012;366[12]:1099-107). And results from the NOR-TEST study recently showed that among 1,100 patients randomized at 13 Norwegian centers, the primary outcome of a 90-day modified Rankin Scale score of 0-1 was achieved by 64% of the tenecteplase patients and by 63% of those who received alteplase (Lancet Neurol. 2017 Oct;16[10]:781-8).
The EXTEND-IA TNK trial ran during 2015-2017 at 18 hospitals. All enrolled patients received their thrombolytic treatment within 4.5 hours of their stroke onset, and underwent endovascular thrombectomy within 6 hours of onset. The safety outcomes of death, symptomatic intracranial hemorrhage, and parenchymal hematoma occurred at statistically similar rates in both treatment arms.
The study was investigator initiated and funded chiefly by the Australian government. Medtronic provided an unrestricted grant for trial infrastructure but had no role in study design conduct or analysis. Dr. Campbell and Dr. Powers had no disclosures.
SOURCE: Campbell B et al. ISC 2018, abstract LB2.
REPORTING FROM ISC 2018
Key clinical point: Tenecteplase thrombolysis produced better reperfusion than did alteplase.
Major finding: Robust reperfusion occurred in 22% of tenecteplase patients and in 10% of patients who received alteplase.
Study details: EXTEND-IA TNK, a multicenter, randomized trial with 202 patients.
Disclosures: The study was investigator initiated and funded chiefly by the Australian government. Medtronic provided an unrestricted grant for trial infrastructure but had no role in study design conduct or analysis. Dr. Campbell and Dr. Powers had no disclosures.
Source: Campbell B et al. ISC 2018, abstract LB2
Late thrombectomy for stroke has low number needed to treat for benefit
LOS ANGELES – The number of ischemic stroke patients with a clinical core mismatch showing salvageable tissue who need to be treated with thrombectomy to obtain a significant benefit on functional outcomes is just 2 when the time frame from last known well extends out to 24 hours, according a subanalysis of results from the DAWN trial.
The Jan. 4, 2018, publication of the DAWN trial revealed that patients with ischemic strokes can benefit from thrombectomy long after the time window generally thought to afford benefits had closed (N Engl J Med. 2018;378:11-21). The procedure yielded significant benefits in functional outcomes at 90 days in patients with a clinical core mismatch showing salvageable tissue.
The results are important because health care systems must now make decisions about allocating resources for the treatment of these patients, which will include installing imaging techniques and expertise at various centers. “It will be practical in some primary stroke centers and not in others. We’re going to see a lot of interesting research about what frontline hospitals should do. There are lots of options at that screening step, and we’re going to need experience to see what’s best. It won’t be the same answer for everyone,” Jeffrey Saver, MD, said during a press conference announcing the results at the meeting, which was sponsored by the American Heart Association. Dr. Saver is director of the stroke unit at the University of California, Los Angeles, and professor of clinical neurology at the university.
The DAWN trial randomized 206 patients to thrombectomy plus standard care or standard care alone. The study was halted at an enrollment of 206 patients because of overwhelming efficacy. To be eligible, the patients had to have a mismatch between the severity of clinical deficit and the infarct volume as measured via automated analysis (RAPID software, SchemaView) of diffusion-weighted MRI or perfusion CT. They had to have substantial clinical deficits, but limited infarct size, with specific criteria varying with age, National Institutes of Health Stroke Scale score, and infarct size.
The NNT for an mRS score of 0 (asymptomatic) was 19. For freedom from disability (mRS, 0-1), the NNT was 4. For functional independence (mRS, 0-2), it was 3. To achieve ambulatory status (mRS, 0-3), it was 3. To avoid a requirement for constant care (mRS, 0-4), the NNT was 9.
To achieve any reduction in disability at all, the NNT was 2. This value was identical when looking at patients in the 6- to 12-hour window and those in the 12- to 24-hour window. However, the nature of the benefit was different. “In the late window (12-24 hours), outcomes went from really bad to pretty good. In the early window, it was somewhat bad to very good. So it’s still better to be treated early,” Dr. Saver said.
In short, for every 100 patients treated, 50 would gain an improvement in disability-related quality of life, and 36 would gain functional independence. In the 6- to 12-hour group, 45 of every 100 patients would experience lower disability as a result of treatment, as would 56 of every 100 treated patients in the 12- to 24-hour group.
Stryker Neurovascular funded the study. Dr. Saver has consulted for Stryker and received travel reimbursement.
LOS ANGELES – The number of ischemic stroke patients with a clinical core mismatch showing salvageable tissue who need to be treated with thrombectomy to obtain a significant benefit on functional outcomes is just 2 when the time frame from last known well extends out to 24 hours, according a subanalysis of results from the DAWN trial.
The Jan. 4, 2018, publication of the DAWN trial revealed that patients with ischemic strokes can benefit from thrombectomy long after the time window generally thought to afford benefits had closed (N Engl J Med. 2018;378:11-21). The procedure yielded significant benefits in functional outcomes at 90 days in patients with a clinical core mismatch showing salvageable tissue.
The results are important because health care systems must now make decisions about allocating resources for the treatment of these patients, which will include installing imaging techniques and expertise at various centers. “It will be practical in some primary stroke centers and not in others. We’re going to see a lot of interesting research about what frontline hospitals should do. There are lots of options at that screening step, and we’re going to need experience to see what’s best. It won’t be the same answer for everyone,” Jeffrey Saver, MD, said during a press conference announcing the results at the meeting, which was sponsored by the American Heart Association. Dr. Saver is director of the stroke unit at the University of California, Los Angeles, and professor of clinical neurology at the university.
The DAWN trial randomized 206 patients to thrombectomy plus standard care or standard care alone. The study was halted at an enrollment of 206 patients because of overwhelming efficacy. To be eligible, the patients had to have a mismatch between the severity of clinical deficit and the infarct volume as measured via automated analysis (RAPID software, SchemaView) of diffusion-weighted MRI or perfusion CT. They had to have substantial clinical deficits, but limited infarct size, with specific criteria varying with age, National Institutes of Health Stroke Scale score, and infarct size.
The NNT for an mRS score of 0 (asymptomatic) was 19. For freedom from disability (mRS, 0-1), the NNT was 4. For functional independence (mRS, 0-2), it was 3. To achieve ambulatory status (mRS, 0-3), it was 3. To avoid a requirement for constant care (mRS, 0-4), the NNT was 9.
To achieve any reduction in disability at all, the NNT was 2. This value was identical when looking at patients in the 6- to 12-hour window and those in the 12- to 24-hour window. However, the nature of the benefit was different. “In the late window (12-24 hours), outcomes went from really bad to pretty good. In the early window, it was somewhat bad to very good. So it’s still better to be treated early,” Dr. Saver said.
In short, for every 100 patients treated, 50 would gain an improvement in disability-related quality of life, and 36 would gain functional independence. In the 6- to 12-hour group, 45 of every 100 patients would experience lower disability as a result of treatment, as would 56 of every 100 treated patients in the 12- to 24-hour group.
Stryker Neurovascular funded the study. Dr. Saver has consulted for Stryker and received travel reimbursement.
LOS ANGELES – The number of ischemic stroke patients with a clinical core mismatch showing salvageable tissue who need to be treated with thrombectomy to obtain a significant benefit on functional outcomes is just 2 when the time frame from last known well extends out to 24 hours, according a subanalysis of results from the DAWN trial.
The Jan. 4, 2018, publication of the DAWN trial revealed that patients with ischemic strokes can benefit from thrombectomy long after the time window generally thought to afford benefits had closed (N Engl J Med. 2018;378:11-21). The procedure yielded significant benefits in functional outcomes at 90 days in patients with a clinical core mismatch showing salvageable tissue.
The results are important because health care systems must now make decisions about allocating resources for the treatment of these patients, which will include installing imaging techniques and expertise at various centers. “It will be practical in some primary stroke centers and not in others. We’re going to see a lot of interesting research about what frontline hospitals should do. There are lots of options at that screening step, and we’re going to need experience to see what’s best. It won’t be the same answer for everyone,” Jeffrey Saver, MD, said during a press conference announcing the results at the meeting, which was sponsored by the American Heart Association. Dr. Saver is director of the stroke unit at the University of California, Los Angeles, and professor of clinical neurology at the university.
The DAWN trial randomized 206 patients to thrombectomy plus standard care or standard care alone. The study was halted at an enrollment of 206 patients because of overwhelming efficacy. To be eligible, the patients had to have a mismatch between the severity of clinical deficit and the infarct volume as measured via automated analysis (RAPID software, SchemaView) of diffusion-weighted MRI or perfusion CT. They had to have substantial clinical deficits, but limited infarct size, with specific criteria varying with age, National Institutes of Health Stroke Scale score, and infarct size.
The NNT for an mRS score of 0 (asymptomatic) was 19. For freedom from disability (mRS, 0-1), the NNT was 4. For functional independence (mRS, 0-2), it was 3. To achieve ambulatory status (mRS, 0-3), it was 3. To avoid a requirement for constant care (mRS, 0-4), the NNT was 9.
To achieve any reduction in disability at all, the NNT was 2. This value was identical when looking at patients in the 6- to 12-hour window and those in the 12- to 24-hour window. However, the nature of the benefit was different. “In the late window (12-24 hours), outcomes went from really bad to pretty good. In the early window, it was somewhat bad to very good. So it’s still better to be treated early,” Dr. Saver said.
In short, for every 100 patients treated, 50 would gain an improvement in disability-related quality of life, and 36 would gain functional independence. In the 6- to 12-hour group, 45 of every 100 patients would experience lower disability as a result of treatment, as would 56 of every 100 treated patients in the 12- to 24-hour group.
Stryker Neurovascular funded the study. Dr. Saver has consulted for Stryker and received travel reimbursement.
REPORTING FROM ISC 2018
Key clinical point:
Major finding: To achieve a functional improvement at 90 days, the number needed to treat was 2.
Data source: Subanalysis of the randomized, controlled DAWN trial (n = 206).
Disclosures: Stryker Neurovascular funded the study. Dr. Saver has consulted for Stryker and received travel reimbursement.
Source: Saver J et al. ISC 2018 abstract LB3
Heart attacks bring 12 weeks of higher stroke risk
LOS ANGELES – , based on a sample of Medicare beneficiaries.
The period of elevated stroke risk following an MI extends beyond the 30-day window that has traditionally been considered the interval of highest risk, Alexander E. Merkler, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Beyond 12 weeks after MI discharge, the stroke incidence showed no significant difference compared with people without a recent MI history, said Dr. Merkler, a neurologist at Weill Cornell Medicine in New York.
He calculated these statistically significant elevated risk rates after adjusting for demographic measures, stroke risk factors, and the comorbidities included in the Charlson Comorbidity Index.
These increased stroke rates were independent of periprocedural strokes that might have happened during MI interventions, as the analysis excluded MI patients with a history of a stroke either before or during their MI hospitalization.
To run this analysis, Dr. Merkler and his associates used data collected in a 5% sample of Medicare beneficiaries who were at least 66 years old during 2008-2015. Among these 1.7 million people were 46,182 who were hospitalized for an MI.
Several factors associated with an acute MI likely contribute to an elevated stroke risk, including stasis in the heart and generation of microthrombi, and a possibly systemic proinflammatory state, Dr. Merkler suggested.
Dr. Merkler had no disclosures.
SOURCE: Merkler AE et al., International Stroke Conference abstract 172 (Stroke. 2018 Jan; 49[Suppl 1]:A172).
LOS ANGELES – , based on a sample of Medicare beneficiaries.
The period of elevated stroke risk following an MI extends beyond the 30-day window that has traditionally been considered the interval of highest risk, Alexander E. Merkler, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Beyond 12 weeks after MI discharge, the stroke incidence showed no significant difference compared with people without a recent MI history, said Dr. Merkler, a neurologist at Weill Cornell Medicine in New York.
He calculated these statistically significant elevated risk rates after adjusting for demographic measures, stroke risk factors, and the comorbidities included in the Charlson Comorbidity Index.
These increased stroke rates were independent of periprocedural strokes that might have happened during MI interventions, as the analysis excluded MI patients with a history of a stroke either before or during their MI hospitalization.
To run this analysis, Dr. Merkler and his associates used data collected in a 5% sample of Medicare beneficiaries who were at least 66 years old during 2008-2015. Among these 1.7 million people were 46,182 who were hospitalized for an MI.
Several factors associated with an acute MI likely contribute to an elevated stroke risk, including stasis in the heart and generation of microthrombi, and a possibly systemic proinflammatory state, Dr. Merkler suggested.
Dr. Merkler had no disclosures.
SOURCE: Merkler AE et al., International Stroke Conference abstract 172 (Stroke. 2018 Jan; 49[Suppl 1]:A172).
LOS ANGELES – , based on a sample of Medicare beneficiaries.
The period of elevated stroke risk following an MI extends beyond the 30-day window that has traditionally been considered the interval of highest risk, Alexander E. Merkler, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Beyond 12 weeks after MI discharge, the stroke incidence showed no significant difference compared with people without a recent MI history, said Dr. Merkler, a neurologist at Weill Cornell Medicine in New York.
He calculated these statistically significant elevated risk rates after adjusting for demographic measures, stroke risk factors, and the comorbidities included in the Charlson Comorbidity Index.
These increased stroke rates were independent of periprocedural strokes that might have happened during MI interventions, as the analysis excluded MI patients with a history of a stroke either before or during their MI hospitalization.
To run this analysis, Dr. Merkler and his associates used data collected in a 5% sample of Medicare beneficiaries who were at least 66 years old during 2008-2015. Among these 1.7 million people were 46,182 who were hospitalized for an MI.
Several factors associated with an acute MI likely contribute to an elevated stroke risk, including stasis in the heart and generation of microthrombi, and a possibly systemic proinflammatory state, Dr. Merkler suggested.
Dr. Merkler had no disclosures.
SOURCE: Merkler AE et al., International Stroke Conference abstract 172 (Stroke. 2018 Jan; 49[Suppl 1]:A172).
REPORTING FROM ISC 2018
Key clinical point: A patient’s stroke risk is elevated for 12 weeks following a myocardial infarction.
Major finding: The stroke rate was 2.7-fold, 2.0-fold, and 1.6-fold above background at 4, 8, and 12 weeks after an MI.
Study details: A review of 1.7 million Medicare beneficiaries during 2008-2015.
Disclosures: Dr. Merkler had no disclosures.
Source: Merkler AE et al., International Stroke Conference abstract 172 (Stroke. 2018 Jan;49[Suppl 1]:A172).
Cerebrospinal tract may help decide mild stroke treatment
LOS ANGELES – In acute ischemic stroke patients with small perfusion lesions of less than 15 mL, involvement of the corticospinal tract (CST) may help guide the decision whether to treat with alteplase.
Specifically, patients with hypoperfusion in the CST, but without CST infarction, were more likely to have a modified Rankin Scale score (mRS) of 0-2 at 90 days after treatment with alteplase. Patients with no CST involvement, or with a CST infarct, had worse outcomes with treatment.
The better outcomes “might indicate that hypoperfused CST tissue at baseline could be salvaged by timely reperfusion,” said Min Lou, MD, PhD, vice chair of neurology at Zhejiang University, Hangzhou, China, during her presentation of the study at the International Stroke Conference sponsored by the American Heart Association.
Previous studies have left physicians uncertain what to do with patients presenting with mild stroke, especially strokes that are judged to be potentially disabling despite a low National Institutes of Health Stroke Scale (NIHSS) score. These patients have a lower risk of hemorrhagic conversion, estimated at 0%-2%.
A meta-analysis showed that alteplase treatment in patients with a baseline NIHSS score of 0-4 was associated with a 48% increase in the chance of an excellent outcome. But another study showed that, among patients with a perfusion lesion smaller than 15 mL, treatment with alteplase was less likely than no treatment at all to confer an excellent outcome.
“The challenge is to identify what kind of minor stroke patient would benefit from thrombolysis therapy,” said Dr. Lou.
The researchers analyzed data from the International Stroke Perfusion Imaging Registry (INSPIRE) database, selecting 412 patients with an acute perfusion lesion less than 15 mL who had undergone computed tomography perfusion or magnetic resonance perfusion imaging within 4.5 hours of symptom onset, had had the scan repeated at 24 hours, and who were followed up at 90 days.
Among the patients, 248 were treated with alteplase, and 164 were not. The alteplase-treated group had a mean NIHSS score of 5.0, compared with 4.0 in the untreated group (P = .001). CST hypoperfusion was more common in the treated group (32.3% versus 15.9%, P less than .001), as was CST infarction (14.9% versus 5.5%, P = .004) and 24-hour intracerebral hemorrhage (ICH) (9.3% versus 0.6%, P less than .001).
The researchers divided subjects into three groups: no CST lesion (306 patients), CST hypoperfusion with no CST infarct (60), and CST infarct (46). The 24-hour ICH frequency varied between the groups, with the highest frequency in the CST infarct group (15.2%), followed by the CST hypoperfusion with no infarct group (10.0%), and the no CST lesion group (3.6%, P = .002).
At 90 days, higher frequency of an mRS score of 0-1 was only associated with alteplase treatment in the CST hypoperfusion with no infarct group (76.7% versus 47.1%, P = .035).
The reverse was true in the other groups: No treatment was associated with better odds of an mRS score of 0-1 in the group with no CST lesion (87.7% versus 79.8%, P = .067) and particularly in the group with CST infarct (88.9% versus 32.4%, P = .006).
The study is limited by the fact that it is a retrospective analysis, the investigators cautioned.
The National Natural Science Foundation of China funded the study. Dr. Lou reported having no financial disclosures.
LOS ANGELES – In acute ischemic stroke patients with small perfusion lesions of less than 15 mL, involvement of the corticospinal tract (CST) may help guide the decision whether to treat with alteplase.
Specifically, patients with hypoperfusion in the CST, but without CST infarction, were more likely to have a modified Rankin Scale score (mRS) of 0-2 at 90 days after treatment with alteplase. Patients with no CST involvement, or with a CST infarct, had worse outcomes with treatment.
The better outcomes “might indicate that hypoperfused CST tissue at baseline could be salvaged by timely reperfusion,” said Min Lou, MD, PhD, vice chair of neurology at Zhejiang University, Hangzhou, China, during her presentation of the study at the International Stroke Conference sponsored by the American Heart Association.
Previous studies have left physicians uncertain what to do with patients presenting with mild stroke, especially strokes that are judged to be potentially disabling despite a low National Institutes of Health Stroke Scale (NIHSS) score. These patients have a lower risk of hemorrhagic conversion, estimated at 0%-2%.
A meta-analysis showed that alteplase treatment in patients with a baseline NIHSS score of 0-4 was associated with a 48% increase in the chance of an excellent outcome. But another study showed that, among patients with a perfusion lesion smaller than 15 mL, treatment with alteplase was less likely than no treatment at all to confer an excellent outcome.
“The challenge is to identify what kind of minor stroke patient would benefit from thrombolysis therapy,” said Dr. Lou.
The researchers analyzed data from the International Stroke Perfusion Imaging Registry (INSPIRE) database, selecting 412 patients with an acute perfusion lesion less than 15 mL who had undergone computed tomography perfusion or magnetic resonance perfusion imaging within 4.5 hours of symptom onset, had had the scan repeated at 24 hours, and who were followed up at 90 days.
Among the patients, 248 were treated with alteplase, and 164 were not. The alteplase-treated group had a mean NIHSS score of 5.0, compared with 4.0 in the untreated group (P = .001). CST hypoperfusion was more common in the treated group (32.3% versus 15.9%, P less than .001), as was CST infarction (14.9% versus 5.5%, P = .004) and 24-hour intracerebral hemorrhage (ICH) (9.3% versus 0.6%, P less than .001).
The researchers divided subjects into three groups: no CST lesion (306 patients), CST hypoperfusion with no CST infarct (60), and CST infarct (46). The 24-hour ICH frequency varied between the groups, with the highest frequency in the CST infarct group (15.2%), followed by the CST hypoperfusion with no infarct group (10.0%), and the no CST lesion group (3.6%, P = .002).
At 90 days, higher frequency of an mRS score of 0-1 was only associated with alteplase treatment in the CST hypoperfusion with no infarct group (76.7% versus 47.1%, P = .035).
The reverse was true in the other groups: No treatment was associated with better odds of an mRS score of 0-1 in the group with no CST lesion (87.7% versus 79.8%, P = .067) and particularly in the group with CST infarct (88.9% versus 32.4%, P = .006).
The study is limited by the fact that it is a retrospective analysis, the investigators cautioned.
The National Natural Science Foundation of China funded the study. Dr. Lou reported having no financial disclosures.
LOS ANGELES – In acute ischemic stroke patients with small perfusion lesions of less than 15 mL, involvement of the corticospinal tract (CST) may help guide the decision whether to treat with alteplase.
Specifically, patients with hypoperfusion in the CST, but without CST infarction, were more likely to have a modified Rankin Scale score (mRS) of 0-2 at 90 days after treatment with alteplase. Patients with no CST involvement, or with a CST infarct, had worse outcomes with treatment.
The better outcomes “might indicate that hypoperfused CST tissue at baseline could be salvaged by timely reperfusion,” said Min Lou, MD, PhD, vice chair of neurology at Zhejiang University, Hangzhou, China, during her presentation of the study at the International Stroke Conference sponsored by the American Heart Association.
Previous studies have left physicians uncertain what to do with patients presenting with mild stroke, especially strokes that are judged to be potentially disabling despite a low National Institutes of Health Stroke Scale (NIHSS) score. These patients have a lower risk of hemorrhagic conversion, estimated at 0%-2%.
A meta-analysis showed that alteplase treatment in patients with a baseline NIHSS score of 0-4 was associated with a 48% increase in the chance of an excellent outcome. But another study showed that, among patients with a perfusion lesion smaller than 15 mL, treatment with alteplase was less likely than no treatment at all to confer an excellent outcome.
“The challenge is to identify what kind of minor stroke patient would benefit from thrombolysis therapy,” said Dr. Lou.
The researchers analyzed data from the International Stroke Perfusion Imaging Registry (INSPIRE) database, selecting 412 patients with an acute perfusion lesion less than 15 mL who had undergone computed tomography perfusion or magnetic resonance perfusion imaging within 4.5 hours of symptom onset, had had the scan repeated at 24 hours, and who were followed up at 90 days.
Among the patients, 248 were treated with alteplase, and 164 were not. The alteplase-treated group had a mean NIHSS score of 5.0, compared with 4.0 in the untreated group (P = .001). CST hypoperfusion was more common in the treated group (32.3% versus 15.9%, P less than .001), as was CST infarction (14.9% versus 5.5%, P = .004) and 24-hour intracerebral hemorrhage (ICH) (9.3% versus 0.6%, P less than .001).
The researchers divided subjects into three groups: no CST lesion (306 patients), CST hypoperfusion with no CST infarct (60), and CST infarct (46). The 24-hour ICH frequency varied between the groups, with the highest frequency in the CST infarct group (15.2%), followed by the CST hypoperfusion with no infarct group (10.0%), and the no CST lesion group (3.6%, P = .002).
At 90 days, higher frequency of an mRS score of 0-1 was only associated with alteplase treatment in the CST hypoperfusion with no infarct group (76.7% versus 47.1%, P = .035).
The reverse was true in the other groups: No treatment was associated with better odds of an mRS score of 0-1 in the group with no CST lesion (87.7% versus 79.8%, P = .067) and particularly in the group with CST infarct (88.9% versus 32.4%, P = .006).
The study is limited by the fact that it is a retrospective analysis, the investigators cautioned.
The National Natural Science Foundation of China funded the study. Dr. Lou reported having no financial disclosures.
AT ISC 2018
Key clinical point:
Major finding: 76.7% of patients with cerebrospinal tract hypoperfusion but no infarct achieved a modified Rankin Scale score of 0-1, compared with 47.1% of untreated patients.
Data source: A retrospective analysis of 412 patients drawn from the International Stroke Perfusion Imaging Registry.
Disclosures: The National Natural Science Foundation of China funded the study. Dr. Lou reported having no financial disclosures.
VIDEO: COMPASS shows stroke-clot aspiration noninferior to retrieval
LOS ANGELES – Clot removal in acute ischemic stroke patients using an aspiration catheter was noninferior to clot removal using the standard method, a stent retriever, in a multicenter, randomized trial with 270 patients.
“There is now level I evidence that stent retrievers and primary aspiration have equivalent outcomes in emergent large vessel occlusions,” J Mocco, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
The results “will give physicians more choice,” Dr. Mocco said in a video interview. Until now, “many physicians felt that they had to use stent retrievers” because these devices had an much bigger evidence base of efficacy and safety. The new findings provide evidence that supports aspiration as an alternative strategy, said Dr. Mocco, professor of neurosurgery and director of the Cerebrovascular Center at Mount Sinai Medical Center in New York.
The results Dr. Mocco reported from the COMPASS trial (Comparison of Direct Aspiration vs. Stent Retriever as a First Approach) were the second time that clot aspiration was shown to produce outcomes similar to stent retrieval. Similar findings came from a French multicenter trial, ASTER, reported in 2017 (JAMA. 2017 Aug 1;318[5]:443-52).
The study ran at 15 U.S. centers during 2015-2017 and randomized patients with emergent large vessel occlusion strokes to receive initial treatment with either an aspiration catheter or a stent retriever. The specific type of catheter or stent used was left up to each operator. In 83% of the aspiration cases and 81% of the stent retriever cases, the initial device used produced a moderately high or better level of restored blood flow within the occluded artery, with thrombolysis in cerebral infarction (TICI) 2b flow or greater.
The study’s primary efficacy endpoint was the percentage of patients with a modified Rankin Scale score of 0-2 at 90 days after treatment, which occurred in 52% of patients treated with aspiration first and in 49% of those treated by retrieval first, which met the study’s prespecified criterion for noninferiority of the aspiration strategy, Dr. Mocco reported.
The results also showed suggestions of faster responses in the patients treated by aspiration first, although these did not reach statistical significance. The highest rate of restored blood flow within the occluded artery, TICI 3 flow, occurred in 34% of patients treated by aspiration first and in 23% of those treated with retrieval first. The average time to produce TICI 2b flow or greater was 22 minutes in the aspiration-first patients, compared with 33 minutes among retrieval-first patients.
“I prefer to start with aspiration first because it’s fast and efficient,” Dr. Mocco said. “I find encouragement in the nonsignificant faster rate of reperfusion” seen in the results.
The study’s safety endpoints, the rate of all-cause mortality after 90 days, all intracranial hemorrhages, and symptomatic intracranial hemorrhages, were all similar in the two study arms.
The COMPASS study was funded by Penumbra, but the company had no role in the trial’s design or analysis. Dr. Mocco has been a consultant to Cerebrotech Medical, EndoStream, Rebound Medical, Synchron, and Viseon and has investments in some of these companies. Dr. Sacco had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Mocco J et al. ISC 2018, Abstract LB4.
LOS ANGELES – Clot removal in acute ischemic stroke patients using an aspiration catheter was noninferior to clot removal using the standard method, a stent retriever, in a multicenter, randomized trial with 270 patients.
“There is now level I evidence that stent retrievers and primary aspiration have equivalent outcomes in emergent large vessel occlusions,” J Mocco, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
The results “will give physicians more choice,” Dr. Mocco said in a video interview. Until now, “many physicians felt that they had to use stent retrievers” because these devices had an much bigger evidence base of efficacy and safety. The new findings provide evidence that supports aspiration as an alternative strategy, said Dr. Mocco, professor of neurosurgery and director of the Cerebrovascular Center at Mount Sinai Medical Center in New York.
The results Dr. Mocco reported from the COMPASS trial (Comparison of Direct Aspiration vs. Stent Retriever as a First Approach) were the second time that clot aspiration was shown to produce outcomes similar to stent retrieval. Similar findings came from a French multicenter trial, ASTER, reported in 2017 (JAMA. 2017 Aug 1;318[5]:443-52).
The study ran at 15 U.S. centers during 2015-2017 and randomized patients with emergent large vessel occlusion strokes to receive initial treatment with either an aspiration catheter or a stent retriever. The specific type of catheter or stent used was left up to each operator. In 83% of the aspiration cases and 81% of the stent retriever cases, the initial device used produced a moderately high or better level of restored blood flow within the occluded artery, with thrombolysis in cerebral infarction (TICI) 2b flow or greater.
The study’s primary efficacy endpoint was the percentage of patients with a modified Rankin Scale score of 0-2 at 90 days after treatment, which occurred in 52% of patients treated with aspiration first and in 49% of those treated by retrieval first, which met the study’s prespecified criterion for noninferiority of the aspiration strategy, Dr. Mocco reported.
The results also showed suggestions of faster responses in the patients treated by aspiration first, although these did not reach statistical significance. The highest rate of restored blood flow within the occluded artery, TICI 3 flow, occurred in 34% of patients treated by aspiration first and in 23% of those treated with retrieval first. The average time to produce TICI 2b flow or greater was 22 minutes in the aspiration-first patients, compared with 33 minutes among retrieval-first patients.
“I prefer to start with aspiration first because it’s fast and efficient,” Dr. Mocco said. “I find encouragement in the nonsignificant faster rate of reperfusion” seen in the results.
The study’s safety endpoints, the rate of all-cause mortality after 90 days, all intracranial hemorrhages, and symptomatic intracranial hemorrhages, were all similar in the two study arms.
The COMPASS study was funded by Penumbra, but the company had no role in the trial’s design or analysis. Dr. Mocco has been a consultant to Cerebrotech Medical, EndoStream, Rebound Medical, Synchron, and Viseon and has investments in some of these companies. Dr. Sacco had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Mocco J et al. ISC 2018, Abstract LB4.
LOS ANGELES – Clot removal in acute ischemic stroke patients using an aspiration catheter was noninferior to clot removal using the standard method, a stent retriever, in a multicenter, randomized trial with 270 patients.
“There is now level I evidence that stent retrievers and primary aspiration have equivalent outcomes in emergent large vessel occlusions,” J Mocco, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
The results “will give physicians more choice,” Dr. Mocco said in a video interview. Until now, “many physicians felt that they had to use stent retrievers” because these devices had an much bigger evidence base of efficacy and safety. The new findings provide evidence that supports aspiration as an alternative strategy, said Dr. Mocco, professor of neurosurgery and director of the Cerebrovascular Center at Mount Sinai Medical Center in New York.
The results Dr. Mocco reported from the COMPASS trial (Comparison of Direct Aspiration vs. Stent Retriever as a First Approach) were the second time that clot aspiration was shown to produce outcomes similar to stent retrieval. Similar findings came from a French multicenter trial, ASTER, reported in 2017 (JAMA. 2017 Aug 1;318[5]:443-52).
The study ran at 15 U.S. centers during 2015-2017 and randomized patients with emergent large vessel occlusion strokes to receive initial treatment with either an aspiration catheter or a stent retriever. The specific type of catheter or stent used was left up to each operator. In 83% of the aspiration cases and 81% of the stent retriever cases, the initial device used produced a moderately high or better level of restored blood flow within the occluded artery, with thrombolysis in cerebral infarction (TICI) 2b flow or greater.
The study’s primary efficacy endpoint was the percentage of patients with a modified Rankin Scale score of 0-2 at 90 days after treatment, which occurred in 52% of patients treated with aspiration first and in 49% of those treated by retrieval first, which met the study’s prespecified criterion for noninferiority of the aspiration strategy, Dr. Mocco reported.
The results also showed suggestions of faster responses in the patients treated by aspiration first, although these did not reach statistical significance. The highest rate of restored blood flow within the occluded artery, TICI 3 flow, occurred in 34% of patients treated by aspiration first and in 23% of those treated with retrieval first. The average time to produce TICI 2b flow or greater was 22 minutes in the aspiration-first patients, compared with 33 minutes among retrieval-first patients.
“I prefer to start with aspiration first because it’s fast and efficient,” Dr. Mocco said. “I find encouragement in the nonsignificant faster rate of reperfusion” seen in the results.
The study’s safety endpoints, the rate of all-cause mortality after 90 days, all intracranial hemorrhages, and symptomatic intracranial hemorrhages, were all similar in the two study arms.
The COMPASS study was funded by Penumbra, but the company had no role in the trial’s design or analysis. Dr. Mocco has been a consultant to Cerebrotech Medical, EndoStream, Rebound Medical, Synchron, and Viseon and has investments in some of these companies. Dr. Sacco had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SOURCE: Mocco J et al. ISC 2018, Abstract LB4.
REPORTING FROM ISC 2018
Key clinical point:
Major finding: The 90-day modified Rankin Scale score was 0-2 in 52% of aspiration patients and 49% of clot retrieval patients.
Study details: COMPASS, a multicenter, U.S. randomized trial with 270 patients.
Disclosures: The COMPASS study was funded by Penumbra, but the company had no role in the trial’s design or analysis. Dr. Mocco has been a consultant to Cerebrotech Medical, EndoStream, Rebound Medical, Synchron, and Viseon and has investments in some of these companies. Dr. Sacco had no disclosures.
Source: Mocco J et al. ISC 2018, Abstract LB4.
Modeling data suggest how to increase access to endovascular therapy
LOS ANGELES – , according to modeling of geomapping data.
The model showed that installing endovascular therapy (EVT) capability at 50 key hospitals could improve the proportion of Americans within 60 minutes of access to EVT from 63% to 71%, benefiting 22 million.
But another option could provide a stronger boost at a much lower cost. Emergency medical personnel could bypass nearby stroke centers that do not have EVT capability in favor of locations that do, even if they are a bit further away. That’s an option if the patient is clinically stable, and if they can successfully diagnose the patient with a large vessel occlusion, according to Amrou Sarraj, MD, director of the vascular neurology fellowship program at the University of Texas, Houston, who presented the study at the International Stroke Conference sponsored by the American Heart Association.
In fact, taking patients to a hospital that does not conduct EVT can lead to delays. By the time the hospital admits the patient, determines that EVT therapy is appropriate, and transfers the patient to another facility, 3 hours can easily pass, he said. “That’s just an estimation from our experience. But if the other hospital is 15 miles away, that can be driven in a few minutes.”
To estimate time to access EVT centers, the researchers identified 1,645 U.S. stroke centers and stratified them into EVT (n = 577) or non-EVT (n = 1,068), based on whether they had reported at least one thrombectomy code for acute ischemic stroke in 2016 to the Centers for Medicare & Medicaid Services or if they had been designated as a comprehensive stroke center. The researchers broke down geographical units into areas with census tracts encompassing 2,500-8,000 people, and then calculated ground and air transportation times to EVT centers.
They used a ‘greedy’ algorithm to maximize the number of people with 60-minute access. This iterative approach yields the highest incremental increases in patient access and eliminates overlap. They conducted a similar optimization for 30-minute travel time.
The researchers found that 137 million Americans (44%) live within 30 minutes of an EVT center, 195 million (63%) live within 60 minutes, and 234 million (76%) within 90 minutes. By air, 172 million (56%) live within 30 minutes of an EVT center, 268 million (87%) within 60 minutes, and 296 million (96%) within 90 minutes.
“Flipping” the top 50 non-EVT centers to EVT centers would increase the number of Americans living within 60 minutes of an EVT center by 22 million, upping the percentage from 63% to 71%. The proportion within 30 minutes would increase by 15 million, from 44% to 49%.
In fact, the number of EVT-capable centers is rapidly expanding, having grown from 577 to 797 since 2016. But this is an expensive proposition, requiring the hiring of interventionists and other changes.
Another option is the “bypass” approach, in which emergency responders transport a patient with a large vessel occlusion to the nearest EVT-capable facility, if the distance isn’t too great. In Houston, the researchers calculated the impact of 15-, 30-, 45-, and 60-minute bypass limits. A total of 45% of the city’s population lives closest to a stroke center that performs EVT. If emergency responders were granted an additional 15 minutes to reach an EVT facility, 82% could go directly to a stroke center. That proportion rose to 91% for a 15- to 30-minute bypass, 94% for a 30- to 45-minute bypass, and 95% for a bypass up to 60 minutes.
In Texas overall, flipping the top five non-EVT centers would place an additional 1.8 million people (+7.0%) within 30 minutes of an EVT center, while a 30-minute bypass would add 11.3 million (+45%).
The study did not receive outside funding. Dr. Sarraj reported receiving a research grant from Stryker and serving as a consultant to or on the advisory board of the company.
SOURCE: Sarraj A et al. ISC 2018 abstract 92.
LOS ANGELES – , according to modeling of geomapping data.
The model showed that installing endovascular therapy (EVT) capability at 50 key hospitals could improve the proportion of Americans within 60 minutes of access to EVT from 63% to 71%, benefiting 22 million.
But another option could provide a stronger boost at a much lower cost. Emergency medical personnel could bypass nearby stroke centers that do not have EVT capability in favor of locations that do, even if they are a bit further away. That’s an option if the patient is clinically stable, and if they can successfully diagnose the patient with a large vessel occlusion, according to Amrou Sarraj, MD, director of the vascular neurology fellowship program at the University of Texas, Houston, who presented the study at the International Stroke Conference sponsored by the American Heart Association.
In fact, taking patients to a hospital that does not conduct EVT can lead to delays. By the time the hospital admits the patient, determines that EVT therapy is appropriate, and transfers the patient to another facility, 3 hours can easily pass, he said. “That’s just an estimation from our experience. But if the other hospital is 15 miles away, that can be driven in a few minutes.”
To estimate time to access EVT centers, the researchers identified 1,645 U.S. stroke centers and stratified them into EVT (n = 577) or non-EVT (n = 1,068), based on whether they had reported at least one thrombectomy code for acute ischemic stroke in 2016 to the Centers for Medicare & Medicaid Services or if they had been designated as a comprehensive stroke center. The researchers broke down geographical units into areas with census tracts encompassing 2,500-8,000 people, and then calculated ground and air transportation times to EVT centers.
They used a ‘greedy’ algorithm to maximize the number of people with 60-minute access. This iterative approach yields the highest incremental increases in patient access and eliminates overlap. They conducted a similar optimization for 30-minute travel time.
The researchers found that 137 million Americans (44%) live within 30 minutes of an EVT center, 195 million (63%) live within 60 minutes, and 234 million (76%) within 90 minutes. By air, 172 million (56%) live within 30 minutes of an EVT center, 268 million (87%) within 60 minutes, and 296 million (96%) within 90 minutes.
“Flipping” the top 50 non-EVT centers to EVT centers would increase the number of Americans living within 60 minutes of an EVT center by 22 million, upping the percentage from 63% to 71%. The proportion within 30 minutes would increase by 15 million, from 44% to 49%.
In fact, the number of EVT-capable centers is rapidly expanding, having grown from 577 to 797 since 2016. But this is an expensive proposition, requiring the hiring of interventionists and other changes.
Another option is the “bypass” approach, in which emergency responders transport a patient with a large vessel occlusion to the nearest EVT-capable facility, if the distance isn’t too great. In Houston, the researchers calculated the impact of 15-, 30-, 45-, and 60-minute bypass limits. A total of 45% of the city’s population lives closest to a stroke center that performs EVT. If emergency responders were granted an additional 15 minutes to reach an EVT facility, 82% could go directly to a stroke center. That proportion rose to 91% for a 15- to 30-minute bypass, 94% for a 30- to 45-minute bypass, and 95% for a bypass up to 60 minutes.
In Texas overall, flipping the top five non-EVT centers would place an additional 1.8 million people (+7.0%) within 30 minutes of an EVT center, while a 30-minute bypass would add 11.3 million (+45%).
The study did not receive outside funding. Dr. Sarraj reported receiving a research grant from Stryker and serving as a consultant to or on the advisory board of the company.
SOURCE: Sarraj A et al. ISC 2018 abstract 92.
LOS ANGELES – , according to modeling of geomapping data.
The model showed that installing endovascular therapy (EVT) capability at 50 key hospitals could improve the proportion of Americans within 60 minutes of access to EVT from 63% to 71%, benefiting 22 million.
But another option could provide a stronger boost at a much lower cost. Emergency medical personnel could bypass nearby stroke centers that do not have EVT capability in favor of locations that do, even if they are a bit further away. That’s an option if the patient is clinically stable, and if they can successfully diagnose the patient with a large vessel occlusion, according to Amrou Sarraj, MD, director of the vascular neurology fellowship program at the University of Texas, Houston, who presented the study at the International Stroke Conference sponsored by the American Heart Association.
In fact, taking patients to a hospital that does not conduct EVT can lead to delays. By the time the hospital admits the patient, determines that EVT therapy is appropriate, and transfers the patient to another facility, 3 hours can easily pass, he said. “That’s just an estimation from our experience. But if the other hospital is 15 miles away, that can be driven in a few minutes.”
To estimate time to access EVT centers, the researchers identified 1,645 U.S. stroke centers and stratified them into EVT (n = 577) or non-EVT (n = 1,068), based on whether they had reported at least one thrombectomy code for acute ischemic stroke in 2016 to the Centers for Medicare & Medicaid Services or if they had been designated as a comprehensive stroke center. The researchers broke down geographical units into areas with census tracts encompassing 2,500-8,000 people, and then calculated ground and air transportation times to EVT centers.
They used a ‘greedy’ algorithm to maximize the number of people with 60-minute access. This iterative approach yields the highest incremental increases in patient access and eliminates overlap. They conducted a similar optimization for 30-minute travel time.
The researchers found that 137 million Americans (44%) live within 30 minutes of an EVT center, 195 million (63%) live within 60 minutes, and 234 million (76%) within 90 minutes. By air, 172 million (56%) live within 30 minutes of an EVT center, 268 million (87%) within 60 minutes, and 296 million (96%) within 90 minutes.
“Flipping” the top 50 non-EVT centers to EVT centers would increase the number of Americans living within 60 minutes of an EVT center by 22 million, upping the percentage from 63% to 71%. The proportion within 30 minutes would increase by 15 million, from 44% to 49%.
In fact, the number of EVT-capable centers is rapidly expanding, having grown from 577 to 797 since 2016. But this is an expensive proposition, requiring the hiring of interventionists and other changes.
Another option is the “bypass” approach, in which emergency responders transport a patient with a large vessel occlusion to the nearest EVT-capable facility, if the distance isn’t too great. In Houston, the researchers calculated the impact of 15-, 30-, 45-, and 60-minute bypass limits. A total of 45% of the city’s population lives closest to a stroke center that performs EVT. If emergency responders were granted an additional 15 minutes to reach an EVT facility, 82% could go directly to a stroke center. That proportion rose to 91% for a 15- to 30-minute bypass, 94% for a 30- to 45-minute bypass, and 95% for a bypass up to 60 minutes.
In Texas overall, flipping the top five non-EVT centers would place an additional 1.8 million people (+7.0%) within 30 minutes of an EVT center, while a 30-minute bypass would add 11.3 million (+45%).
The study did not receive outside funding. Dr. Sarraj reported receiving a research grant from Stryker and serving as a consultant to or on the advisory board of the company.
SOURCE: Sarraj A et al. ISC 2018 abstract 92.
REPORTING FROM ISC 2018
Key clinical point: Several options are available to increase access to endovascular therapy for many Americans.
Major finding: Just 63% of Americans live within 60 minutes of a stroke center that provides endovascular therapy.
Data source: A geomapping study of the availability of endovascular therapy across the United States.
Disclosures: The study did not receive outside funding. Dr. Sarraj reported receiving a research grant from Stryker and serving as a consultant to or on the advisory board of the company.
Source: Sarraj A et al. ISC 2018 abstract 92.
VIDEO: New stroke guideline embraces imaging-guided thrombectomy
LOS ANGELES – When a panel organized by the American Heart Association’s Stroke Council recently revised the group’s guideline for early management of acute ischemic stroke, they were clear on the overarching change they had to make: Incorporate recent evidence collected in two trials that established brain imaging as the way to identify patients eligible for clot removal treatment by thrombectomy, a change in practice that has made this outcome-altering intervention available to more patients.
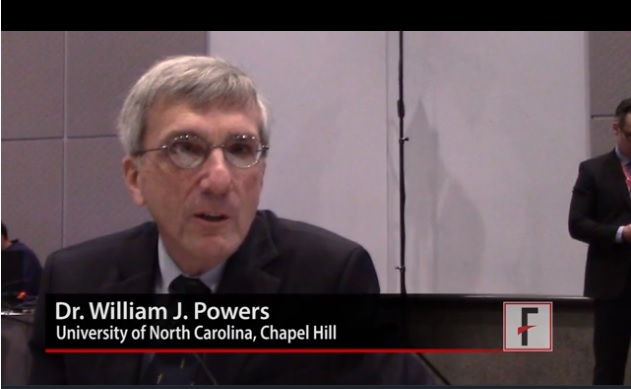
“The major take-home message [of the new guideline] is the extension of the time window for treating acute ischemic stroke,” said William J. Powers, MD, chair of the guideline group (Stroke. 2018 Jan 24. doi: 10.1161/STR.0000000000000158).
Based on recently reported results from the DAWN (N Engl J Med. 2018;378[1]:11-21) and DEFUSE 3 (N Engl J Med. 2018 Jan 24. doi: 10.1056/NEJMoa1713973) trials “we know that there are patients out to 24 hours from their stroke onset who may benefit” from thrombectomy. “This is a major, major change in how we view care for patients with stroke,” Dr. Powers said in a video interview. “Now there’s much more time. Ideally, we’ll see smaller hospitals develop the ability to do the imaging” that makes it possible to select acute ischemic stroke patients eligible for thrombectomy despite a delay of up to 24 hours from their stroke onset to the time of thrombectomy, said Dr. Powers, professor and chair of neurology at the University of North Carolina, Chapel Hill.
The big priority for the stroke community now that this major change in patient selection was incorporated into a U.S. practice guideline will be acting quickly to implement the steps needed to make this change happen, Dr. Powers and others said.
The new guideline will mean “changes in process and systems of care,” agreed Jeffrey L. Saver, MD, professor of neurology and director of the stroke unit at the University of California, Los Angeles. The imaging called for “will be practical at some primary stroke centers but not others,” he said, although most hospitals certified to provide stroke care as primary stroke centers or acute stroke–ready hospitals have a CT scanner that could provide the basic imaging needed to assess many patients. (CT angiography and perfusion CT are more informative for determining thrombectomy eligibility.) But interpretation of the brain images to distinguish patients eligible for thrombectomy from those who aren’t will likely happen at comprehensive stroke centers that perform thrombectomy or by experts using remote image reading.
Dr. Saver expects that the new guideline will translate most quickly into changes in the imaging and transfer protocols that the Joint Commission may now require from hospitals certified as primary stroke centers or acute stroke-ready hospitals, changes that could be in place sometime later in 2018, he predicted. These are steps “that would really help drive system change.”
Dr. Powers and Dr. Furie had no disclosures. Dr. Saver has received research support and personal fees from Medtronic-Abbott and Neuravia.
LOS ANGELES – When a panel organized by the American Heart Association’s Stroke Council recently revised the group’s guideline for early management of acute ischemic stroke, they were clear on the overarching change they had to make: Incorporate recent evidence collected in two trials that established brain imaging as the way to identify patients eligible for clot removal treatment by thrombectomy, a change in practice that has made this outcome-altering intervention available to more patients.
“The major take-home message [of the new guideline] is the extension of the time window for treating acute ischemic stroke,” said William J. Powers, MD, chair of the guideline group (Stroke. 2018 Jan 24. doi: 10.1161/STR.0000000000000158).
Based on recently reported results from the DAWN (N Engl J Med. 2018;378[1]:11-21) and DEFUSE 3 (N Engl J Med. 2018 Jan 24. doi: 10.1056/NEJMoa1713973) trials “we know that there are patients out to 24 hours from their stroke onset who may benefit” from thrombectomy. “This is a major, major change in how we view care for patients with stroke,” Dr. Powers said in a video interview. “Now there’s much more time. Ideally, we’ll see smaller hospitals develop the ability to do the imaging” that makes it possible to select acute ischemic stroke patients eligible for thrombectomy despite a delay of up to 24 hours from their stroke onset to the time of thrombectomy, said Dr. Powers, professor and chair of neurology at the University of North Carolina, Chapel Hill.
The big priority for the stroke community now that this major change in patient selection was incorporated into a U.S. practice guideline will be acting quickly to implement the steps needed to make this change happen, Dr. Powers and others said.
The new guideline will mean “changes in process and systems of care,” agreed Jeffrey L. Saver, MD, professor of neurology and director of the stroke unit at the University of California, Los Angeles. The imaging called for “will be practical at some primary stroke centers but not others,” he said, although most hospitals certified to provide stroke care as primary stroke centers or acute stroke–ready hospitals have a CT scanner that could provide the basic imaging needed to assess many patients. (CT angiography and perfusion CT are more informative for determining thrombectomy eligibility.) But interpretation of the brain images to distinguish patients eligible for thrombectomy from those who aren’t will likely happen at comprehensive stroke centers that perform thrombectomy or by experts using remote image reading.
Dr. Saver expects that the new guideline will translate most quickly into changes in the imaging and transfer protocols that the Joint Commission may now require from hospitals certified as primary stroke centers or acute stroke-ready hospitals, changes that could be in place sometime later in 2018, he predicted. These are steps “that would really help drive system change.”
Dr. Powers and Dr. Furie had no disclosures. Dr. Saver has received research support and personal fees from Medtronic-Abbott and Neuravia.
LOS ANGELES – When a panel organized by the American Heart Association’s Stroke Council recently revised the group’s guideline for early management of acute ischemic stroke, they were clear on the overarching change they had to make: Incorporate recent evidence collected in two trials that established brain imaging as the way to identify patients eligible for clot removal treatment by thrombectomy, a change in practice that has made this outcome-altering intervention available to more patients.
“The major take-home message [of the new guideline] is the extension of the time window for treating acute ischemic stroke,” said William J. Powers, MD, chair of the guideline group (Stroke. 2018 Jan 24. doi: 10.1161/STR.0000000000000158).
Based on recently reported results from the DAWN (N Engl J Med. 2018;378[1]:11-21) and DEFUSE 3 (N Engl J Med. 2018 Jan 24. doi: 10.1056/NEJMoa1713973) trials “we know that there are patients out to 24 hours from their stroke onset who may benefit” from thrombectomy. “This is a major, major change in how we view care for patients with stroke,” Dr. Powers said in a video interview. “Now there’s much more time. Ideally, we’ll see smaller hospitals develop the ability to do the imaging” that makes it possible to select acute ischemic stroke patients eligible for thrombectomy despite a delay of up to 24 hours from their stroke onset to the time of thrombectomy, said Dr. Powers, professor and chair of neurology at the University of North Carolina, Chapel Hill.
The big priority for the stroke community now that this major change in patient selection was incorporated into a U.S. practice guideline will be acting quickly to implement the steps needed to make this change happen, Dr. Powers and others said.
The new guideline will mean “changes in process and systems of care,” agreed Jeffrey L. Saver, MD, professor of neurology and director of the stroke unit at the University of California, Los Angeles. The imaging called for “will be practical at some primary stroke centers but not others,” he said, although most hospitals certified to provide stroke care as primary stroke centers or acute stroke–ready hospitals have a CT scanner that could provide the basic imaging needed to assess many patients. (CT angiography and perfusion CT are more informative for determining thrombectomy eligibility.) But interpretation of the brain images to distinguish patients eligible for thrombectomy from those who aren’t will likely happen at comprehensive stroke centers that perform thrombectomy or by experts using remote image reading.
Dr. Saver expects that the new guideline will translate most quickly into changes in the imaging and transfer protocols that the Joint Commission may now require from hospitals certified as primary stroke centers or acute stroke-ready hospitals, changes that could be in place sometime later in 2018, he predicted. These are steps “that would really help drive system change.”
Dr. Powers and Dr. Furie had no disclosures. Dr. Saver has received research support and personal fees from Medtronic-Abbott and Neuravia.
EXPERT ANALYSIS FROM ISC 2018
DEFUSE 3: Thrombectomy time window broadens
LOS ANGELES – The final results of the DEFUSE 3 trial are in, and the results are unequivocal: Thrombectomy performed 6-16 hours after the stroke patient was last known to be well was associated with dramatically improved outcomes in 90-day death and disability.
It has long been said that time is brain. Time is still vital, but some strokes progress at a slower rate. “We have the opportunity to treat these patients in a time window that we never thought was possible,” Gregory W. Albers, MD, said in presenting the findings at the International Stroke Conference sponsored by the American Heart Association.
The subjects included those with proximal middle-cerebral artery or internal-carotid artery occlusion and infarcts of 70 mL or less in size, and a ratio of the volume of ischemic tissue on perfusion imaging to infarct tissue of 1.8 or higher. Both DAWN and DEFUSE 3 used the RAPID software from iSchemaView to assess infarct volume.
The DEFUSE 3 results aren’t a surprise, as the trial was stopped early after an interim analysis showed efficacy. But they are immediately practice changing. “This will perhaps be a once in a lifetime situation where a study gets published and within 2 hours gets incorporated into new guidelines,” said Dr. Albers, lead author of the study, who is the Coyote Foundation Professor, neurology and neurological sciences, and professor, by courtesy, of neurosurgery at the Stanford (Calif.) University Medical Center. Minutes later at the press conference, it was announced that the results of both DEFUSE 3 and DAWN had indeed been included in the guidelines.
The DEFUSE (Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke) 3 trial included 182 patients from 38 U.S. centers who were recruited during May 2016–May 2017. Of these, 92 were randomized to thrombectomy and standard medical therapy, and 90 to standard medical therapy only.
Patients who underwent thrombectomy were more likely to have a favorable distribution of disability scores on the modified Rankin scale at 90 days (unadjusted odds ratio, 2.77; adjusted OR, 3.36; both P less than .001). “The odds ratio [of 2.77] was the largest ever reported for a thrombectomy study,” Dr. Albers said, and the ISC audience erupted into spontaneous applause. “We couldn’t be happier,” he responded.
Nearly half (45%) of patients in the thrombectomy group scored as functionally independent at 90 days (Rankin score 0-2), compared with 17% in the medical-therapy group (risk ratio, 2.67; P less than .001). Mortality was also lower in the intervention group (14% vs. 26%; P = .05).
The rates of symptomatic intracranial hemorrhage (7% thrombectomy, 4% medical therapy only) did not differ significantly between the two groups. Serious complications occurred in 43% of patients in the thrombectomy group, compared with 53% in the medical therapy–only group (P = .018).
A subanalysis showed consistent benefit of thrombectomy, even in patients with a longer elapsed time between stroke onset and randomization, while the patients who received medical therapy had worse outcomes as more time passed. In 50 patients in the under 9-hour group, 40% of those who received thrombectomy were functionally independent at 9 weeks, compared with 28% in the medical therapy–only group. Among 72 patients in the 9- to 12-hour group, 50% were functionally independent (vs. 17%), and in the greater than 12-hour group, 42% (7%).
The study filled up rapidly, at about twice the rate that the researchers anticipated, and that suggests that the procedure could find broad use. “It shows that these patients are not difficult to find,” said Dr. Albers.
The National Institutes of Health funded the study. Dr. Albers has a financial stake in iSchemaView and is on the scientific advisory board for iSchemaView and Medtronic.
The DEFUSE 3 results were published online concurrently with Dr. Albers’s presentation (N Engl J Med. 2018 Jan 24; doi: 10.1056/nejmoa1713973).
SOURCE: Albers G et al. ISC 2018
LOS ANGELES – The final results of the DEFUSE 3 trial are in, and the results are unequivocal: Thrombectomy performed 6-16 hours after the stroke patient was last known to be well was associated with dramatically improved outcomes in 90-day death and disability.
It has long been said that time is brain. Time is still vital, but some strokes progress at a slower rate. “We have the opportunity to treat these patients in a time window that we never thought was possible,” Gregory W. Albers, MD, said in presenting the findings at the International Stroke Conference sponsored by the American Heart Association.
The subjects included those with proximal middle-cerebral artery or internal-carotid artery occlusion and infarcts of 70 mL or less in size, and a ratio of the volume of ischemic tissue on perfusion imaging to infarct tissue of 1.8 or higher. Both DAWN and DEFUSE 3 used the RAPID software from iSchemaView to assess infarct volume.
The DEFUSE 3 results aren’t a surprise, as the trial was stopped early after an interim analysis showed efficacy. But they are immediately practice changing. “This will perhaps be a once in a lifetime situation where a study gets published and within 2 hours gets incorporated into new guidelines,” said Dr. Albers, lead author of the study, who is the Coyote Foundation Professor, neurology and neurological sciences, and professor, by courtesy, of neurosurgery at the Stanford (Calif.) University Medical Center. Minutes later at the press conference, it was announced that the results of both DEFUSE 3 and DAWN had indeed been included in the guidelines.
The DEFUSE (Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke) 3 trial included 182 patients from 38 U.S. centers who were recruited during May 2016–May 2017. Of these, 92 were randomized to thrombectomy and standard medical therapy, and 90 to standard medical therapy only.
Patients who underwent thrombectomy were more likely to have a favorable distribution of disability scores on the modified Rankin scale at 90 days (unadjusted odds ratio, 2.77; adjusted OR, 3.36; both P less than .001). “The odds ratio [of 2.77] was the largest ever reported for a thrombectomy study,” Dr. Albers said, and the ISC audience erupted into spontaneous applause. “We couldn’t be happier,” he responded.
Nearly half (45%) of patients in the thrombectomy group scored as functionally independent at 90 days (Rankin score 0-2), compared with 17% in the medical-therapy group (risk ratio, 2.67; P less than .001). Mortality was also lower in the intervention group (14% vs. 26%; P = .05).
The rates of symptomatic intracranial hemorrhage (7% thrombectomy, 4% medical therapy only) did not differ significantly between the two groups. Serious complications occurred in 43% of patients in the thrombectomy group, compared with 53% in the medical therapy–only group (P = .018).
A subanalysis showed consistent benefit of thrombectomy, even in patients with a longer elapsed time between stroke onset and randomization, while the patients who received medical therapy had worse outcomes as more time passed. In 50 patients in the under 9-hour group, 40% of those who received thrombectomy were functionally independent at 9 weeks, compared with 28% in the medical therapy–only group. Among 72 patients in the 9- to 12-hour group, 50% were functionally independent (vs. 17%), and in the greater than 12-hour group, 42% (7%).
The study filled up rapidly, at about twice the rate that the researchers anticipated, and that suggests that the procedure could find broad use. “It shows that these patients are not difficult to find,” said Dr. Albers.
The National Institutes of Health funded the study. Dr. Albers has a financial stake in iSchemaView and is on the scientific advisory board for iSchemaView and Medtronic.
The DEFUSE 3 results were published online concurrently with Dr. Albers’s presentation (N Engl J Med. 2018 Jan 24; doi: 10.1056/nejmoa1713973).
SOURCE: Albers G et al. ISC 2018
LOS ANGELES – The final results of the DEFUSE 3 trial are in, and the results are unequivocal: Thrombectomy performed 6-16 hours after the stroke patient was last known to be well was associated with dramatically improved outcomes in 90-day death and disability.
It has long been said that time is brain. Time is still vital, but some strokes progress at a slower rate. “We have the opportunity to treat these patients in a time window that we never thought was possible,” Gregory W. Albers, MD, said in presenting the findings at the International Stroke Conference sponsored by the American Heart Association.
The subjects included those with proximal middle-cerebral artery or internal-carotid artery occlusion and infarcts of 70 mL or less in size, and a ratio of the volume of ischemic tissue on perfusion imaging to infarct tissue of 1.8 or higher. Both DAWN and DEFUSE 3 used the RAPID software from iSchemaView to assess infarct volume.
The DEFUSE 3 results aren’t a surprise, as the trial was stopped early after an interim analysis showed efficacy. But they are immediately practice changing. “This will perhaps be a once in a lifetime situation where a study gets published and within 2 hours gets incorporated into new guidelines,” said Dr. Albers, lead author of the study, who is the Coyote Foundation Professor, neurology and neurological sciences, and professor, by courtesy, of neurosurgery at the Stanford (Calif.) University Medical Center. Minutes later at the press conference, it was announced that the results of both DEFUSE 3 and DAWN had indeed been included in the guidelines.
The DEFUSE (Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke) 3 trial included 182 patients from 38 U.S. centers who were recruited during May 2016–May 2017. Of these, 92 were randomized to thrombectomy and standard medical therapy, and 90 to standard medical therapy only.
Patients who underwent thrombectomy were more likely to have a favorable distribution of disability scores on the modified Rankin scale at 90 days (unadjusted odds ratio, 2.77; adjusted OR, 3.36; both P less than .001). “The odds ratio [of 2.77] was the largest ever reported for a thrombectomy study,” Dr. Albers said, and the ISC audience erupted into spontaneous applause. “We couldn’t be happier,” he responded.
Nearly half (45%) of patients in the thrombectomy group scored as functionally independent at 90 days (Rankin score 0-2), compared with 17% in the medical-therapy group (risk ratio, 2.67; P less than .001). Mortality was also lower in the intervention group (14% vs. 26%; P = .05).
The rates of symptomatic intracranial hemorrhage (7% thrombectomy, 4% medical therapy only) did not differ significantly between the two groups. Serious complications occurred in 43% of patients in the thrombectomy group, compared with 53% in the medical therapy–only group (P = .018).
A subanalysis showed consistent benefit of thrombectomy, even in patients with a longer elapsed time between stroke onset and randomization, while the patients who received medical therapy had worse outcomes as more time passed. In 50 patients in the under 9-hour group, 40% of those who received thrombectomy were functionally independent at 9 weeks, compared with 28% in the medical therapy–only group. Among 72 patients in the 9- to 12-hour group, 50% were functionally independent (vs. 17%), and in the greater than 12-hour group, 42% (7%).
The study filled up rapidly, at about twice the rate that the researchers anticipated, and that suggests that the procedure could find broad use. “It shows that these patients are not difficult to find,” said Dr. Albers.
The National Institutes of Health funded the study. Dr. Albers has a financial stake in iSchemaView and is on the scientific advisory board for iSchemaView and Medtronic.
The DEFUSE 3 results were published online concurrently with Dr. Albers’s presentation (N Engl J Med. 2018 Jan 24; doi: 10.1056/nejmoa1713973).
SOURCE: Albers G et al. ISC 2018
REPORTING FROM ISC 2018
Key clinical point: Stroke patients with clinical imaging mismatch had significantly better 90-day disability outcomes with thrombectomy.
Major finding: The odds ratio of a favorable outcome at 90 days was 2.77.
Data source: DEFUSE 3, a multicenter, randomized, controlled trial in 182 stroke patients.
Disclosures: The National Institutes of Health funded the study. Dr. Albers has a financial stake in iSchemaView and is on the scientific advisor board for iSchemaView and Medtronic.
Source: Albers G. et al. ISC 2018