User login
Held every two years International Society on Thrombosis and Haemostasis (ISTH): 2015 Congress
Routine screening sufficient for detecting occult cancer in patients with VTE
TORONTO – The prevalence of occult cancer is low in patients with a first unprovoked venous thromboembolism, according to results from a multicenter, randomized study presented at the International Society on Thrombosis and Haemostasis congress.
In addition, routine screening with the addition of a comprehensive CT scan of the abdomen and pelvis was no better than routine screening alone in detecting occult cancer in this population.
Those are key findings that Dr. Marc Carrier of the University of Ottawa presented from the Screening for Occult Malignancy in Patients with Idiopathic Venous Thromboembolism (SOME) trial, a multicenter, open-label, randomized controlled trial that compared the efficacy of conventional screening with or without comprehensive CT of the abdomen/pelvis for detecting occult cancers in patients with unprovoked venous thromboembolism (VTE). The results of this study were published the same day as his presentation in the New England Journal of Medicine.
“It has been described that up to 10% of patients with unprovoked VTE are diagnosed with cancer in the year following their VTE diagnosis,” Dr. Carrier said. “Therefore, it’s appealing for clinicians to screen these patients for occult cancer but it has led to a lot of great diversity in practices. Some clinicians prefer to use a limited screening strategy that would include a history, physical examination, routine blood tests, and a chest X-ray. Other clinicians prefer to use the limited screening strategy in combination with additional tests. That could be CT of the abdomen and pelvis, ultrasound, or tumor marker, or [computed axial tomography] scan. It’s hard for a physician to know what to use.”
For the SOME trial, a total of 854 patients with unprovoked VTE were randomized to two groups: 431 to limited occult cancer screening (basic blood work, chest X-ray, and breast/cervical/prostate cancer screening) and 423 to limited screening in combination with a comprehensive CT of the abdomen/pelvis. The comprehensive CT included a virtual colonoscopy and gastroscopy, a biphasic enhanced CT, a parenchymal pancreatogram, and a uniphasic enhanced CT of distended bladder. The primary outcome was confirmed cancer that was missed by the screening strategy and detected by the end of the 1-year follow-up period.
Dr. Carrier reported that 33 patients (3.9%) had a new diagnosis of cancer in the interval between randomization and 1-year follow-up: 14 in the limited-screening group and 19 in the limited-screening-plus-CT group, a difference that was not statistically significant (P = .28). In addition, the number of occult cancers missed by the end of the 1-year follow-up period was similar between the two groups: four in the limited-screening group and five in the limited-screening-plus-CT group.
He and his associates also found no significant differences between the limited-screening group and the limited-screening-plus-CT group in the rate of detection of early cancers (0.23% vs. 0.71%, respectively; P = .37), in overall mortality (1.4% vs. 1.2%; P > 0.99), or in cancer-related mortality (1.4% vs. 0.95%; P = .75).
“Occult cancers are not nearly as common as we thought they were, which is reassuring for clinicians and patients because then we don’t have to do a lot of investigations to try and find them, and often scare patients and expose them to radiation and additional procedures,” Dr. Carrier said in an interview. “Limited screening alone, which is what is recommended in Canada and in the United States for age- and gender-specific screening, is more than reasonable for these patients.”
The SOME trial was funded by the Heart and Stroke Foundation of Canada. Dr. Carrier had no relevant financial conflicts to disclose.
Therese Borden contributed to this article.
TORONTO – The prevalence of occult cancer is low in patients with a first unprovoked venous thromboembolism, according to results from a multicenter, randomized study presented at the International Society on Thrombosis and Haemostasis congress.
In addition, routine screening with the addition of a comprehensive CT scan of the abdomen and pelvis was no better than routine screening alone in detecting occult cancer in this population.
Those are key findings that Dr. Marc Carrier of the University of Ottawa presented from the Screening for Occult Malignancy in Patients with Idiopathic Venous Thromboembolism (SOME) trial, a multicenter, open-label, randomized controlled trial that compared the efficacy of conventional screening with or without comprehensive CT of the abdomen/pelvis for detecting occult cancers in patients with unprovoked venous thromboembolism (VTE). The results of this study were published the same day as his presentation in the New England Journal of Medicine.
“It has been described that up to 10% of patients with unprovoked VTE are diagnosed with cancer in the year following their VTE diagnosis,” Dr. Carrier said. “Therefore, it’s appealing for clinicians to screen these patients for occult cancer but it has led to a lot of great diversity in practices. Some clinicians prefer to use a limited screening strategy that would include a history, physical examination, routine blood tests, and a chest X-ray. Other clinicians prefer to use the limited screening strategy in combination with additional tests. That could be CT of the abdomen and pelvis, ultrasound, or tumor marker, or [computed axial tomography] scan. It’s hard for a physician to know what to use.”
For the SOME trial, a total of 854 patients with unprovoked VTE were randomized to two groups: 431 to limited occult cancer screening (basic blood work, chest X-ray, and breast/cervical/prostate cancer screening) and 423 to limited screening in combination with a comprehensive CT of the abdomen/pelvis. The comprehensive CT included a virtual colonoscopy and gastroscopy, a biphasic enhanced CT, a parenchymal pancreatogram, and a uniphasic enhanced CT of distended bladder. The primary outcome was confirmed cancer that was missed by the screening strategy and detected by the end of the 1-year follow-up period.
Dr. Carrier reported that 33 patients (3.9%) had a new diagnosis of cancer in the interval between randomization and 1-year follow-up: 14 in the limited-screening group and 19 in the limited-screening-plus-CT group, a difference that was not statistically significant (P = .28). In addition, the number of occult cancers missed by the end of the 1-year follow-up period was similar between the two groups: four in the limited-screening group and five in the limited-screening-plus-CT group.
He and his associates also found no significant differences between the limited-screening group and the limited-screening-plus-CT group in the rate of detection of early cancers (0.23% vs. 0.71%, respectively; P = .37), in overall mortality (1.4% vs. 1.2%; P > 0.99), or in cancer-related mortality (1.4% vs. 0.95%; P = .75).
“Occult cancers are not nearly as common as we thought they were, which is reassuring for clinicians and patients because then we don’t have to do a lot of investigations to try and find them, and often scare patients and expose them to radiation and additional procedures,” Dr. Carrier said in an interview. “Limited screening alone, which is what is recommended in Canada and in the United States for age- and gender-specific screening, is more than reasonable for these patients.”
The SOME trial was funded by the Heart and Stroke Foundation of Canada. Dr. Carrier had no relevant financial conflicts to disclose.
Therese Borden contributed to this article.
TORONTO – The prevalence of occult cancer is low in patients with a first unprovoked venous thromboembolism, according to results from a multicenter, randomized study presented at the International Society on Thrombosis and Haemostasis congress.
In addition, routine screening with the addition of a comprehensive CT scan of the abdomen and pelvis was no better than routine screening alone in detecting occult cancer in this population.
Those are key findings that Dr. Marc Carrier of the University of Ottawa presented from the Screening for Occult Malignancy in Patients with Idiopathic Venous Thromboembolism (SOME) trial, a multicenter, open-label, randomized controlled trial that compared the efficacy of conventional screening with or without comprehensive CT of the abdomen/pelvis for detecting occult cancers in patients with unprovoked venous thromboembolism (VTE). The results of this study were published the same day as his presentation in the New England Journal of Medicine.
“It has been described that up to 10% of patients with unprovoked VTE are diagnosed with cancer in the year following their VTE diagnosis,” Dr. Carrier said. “Therefore, it’s appealing for clinicians to screen these patients for occult cancer but it has led to a lot of great diversity in practices. Some clinicians prefer to use a limited screening strategy that would include a history, physical examination, routine blood tests, and a chest X-ray. Other clinicians prefer to use the limited screening strategy in combination with additional tests. That could be CT of the abdomen and pelvis, ultrasound, or tumor marker, or [computed axial tomography] scan. It’s hard for a physician to know what to use.”
For the SOME trial, a total of 854 patients with unprovoked VTE were randomized to two groups: 431 to limited occult cancer screening (basic blood work, chest X-ray, and breast/cervical/prostate cancer screening) and 423 to limited screening in combination with a comprehensive CT of the abdomen/pelvis. The comprehensive CT included a virtual colonoscopy and gastroscopy, a biphasic enhanced CT, a parenchymal pancreatogram, and a uniphasic enhanced CT of distended bladder. The primary outcome was confirmed cancer that was missed by the screening strategy and detected by the end of the 1-year follow-up period.
Dr. Carrier reported that 33 patients (3.9%) had a new diagnosis of cancer in the interval between randomization and 1-year follow-up: 14 in the limited-screening group and 19 in the limited-screening-plus-CT group, a difference that was not statistically significant (P = .28). In addition, the number of occult cancers missed by the end of the 1-year follow-up period was similar between the two groups: four in the limited-screening group and five in the limited-screening-plus-CT group.
He and his associates also found no significant differences between the limited-screening group and the limited-screening-plus-CT group in the rate of detection of early cancers (0.23% vs. 0.71%, respectively; P = .37), in overall mortality (1.4% vs. 1.2%; P > 0.99), or in cancer-related mortality (1.4% vs. 0.95%; P = .75).
“Occult cancers are not nearly as common as we thought they were, which is reassuring for clinicians and patients because then we don’t have to do a lot of investigations to try and find them, and often scare patients and expose them to radiation and additional procedures,” Dr. Carrier said in an interview. “Limited screening alone, which is what is recommended in Canada and in the United States for age- and gender-specific screening, is more than reasonable for these patients.”
The SOME trial was funded by the Heart and Stroke Foundation of Canada. Dr. Carrier had no relevant financial conflicts to disclose.
Therese Borden contributed to this article.
AT THE 2015 ISTH CONGRESS
Key clinical point: Occult cancers in patients with a first unprovoked VTE are not nearly as common as previously thought, and limited screening for such cancers is appropriate.
Major finding: There were no significant differences between the limited-screening group and the limited-screening-plus-CT group in the rate of detection of early cancers (0.23% vs. 0.71%); in overall mortality (1.4% vs. 1.2%), or in cancer-related mortality (1.4% vs. 0.95%).
Data source: A multicenter, open-label, randomized controlled trial of 854 patients with unprovoked VTE.
Disclosures: The trial was funded by the Heart and Stroke Foundation of Canada. Dr. Carrier reported having no financial disclosures.
Cardiovascular disease prevention should start in childhood
TORONTO – If you don’t think clinicians should be worried about the current state of cardiovascular disease (CVD) prevention, consider the arresting data from the 2011 World Health Organization Global Atlas on CVD Prevention and Control.
The atlas showed that CVD accounts for 31% of deaths worldwide: 17.5 million deaths in 2012, projected to increase to 23.3 million deaths in 2030.
At the same time, the American Heart Association projects that by 2030, more than 40% of the U.S. population will have some form of CVD, with total direct costs projected to increase from $273 billion to $818 billion – and real indirect costs because of lost productivity will increase from $172 billion to $276 billion.
“We are not preventing CVD, and the worldwide prevalence of risk factors predicts a grim future,” Dr. Brian W. McCrindle, a staff cardiologist at the Hospital for Sick Children, Toronto, said at the International Society on Thrombosis and Haemostasis congress.
“One of the biggest problems is that we don’t give health and we don’t give prevention their fair due,” Dr. McCrindle continued. “We spend proportionately more health care dollars on providing care for acute and chronic illnesses, much of which are preventable. Our expenditures are growing, leaving little for prevention, and even less for children.”
According to Dr. McCrindle, today’s clinicians miss the mark on preventing CVD “because we focus our efforts on tertiary prevention – the treatment of existing symptomatic disease in order to ameliorate its effects, or treatment to delay or prevent progression; or on secondary prevention – the early detection of the potential for development of a disease, or the prevention of events in those with asymptomatic disease.
“We do make some effort regarding primary prevention – the reduction of risk factors before the occurrence of disease, but tend to delay these efforts until much later in adulthood,” he noted. “We do very little regarding primordial prevention – the prevention of risk factors from developing.”
Dr. McCrindle noted that atherosclerosis has been shown to begin in youth, and that obesity and other cardiovascular risk factors in children track into adulthood. “These findings are of concern regarding current prevention strategies,” he said.
“However, there are some important evidence gaps that need to be addressed before embarking on screening and intervention strategies in youth,” Dr. McCrindle cautioned. “Unfortunately, direct evidence does not exist to assert that risk factors measured in childhood are related to clinical events in adults, although long-term follow-up of existing cohorts may provide that.
“We may never have direct evidence that detection and management of risk factors in children reduce CVD events in adults, since a 50- to 60-year-long randomized trial can never be done,” Dr. McCrindle noted. “However, a chain of indirect evidence can be established.”
Key to current efforts, he continued, are the use of noninvasive ways to measure subclinical atherosclerosis, including ultrasound to assess endothelial function, arterial stiffness and intima-media thickness, and ultrafast computed tomography to detect coronary artery calcium. “These have been important predictors of events in adults, and are increasingly used in pediatric studies,” he said.
While he characterized the current health care landscape as being “at odds with the current reality facing today’s youth,” Dr. McCrindle suggested several ways that attendees can improve the CVD outlook in children, starting with being a role model for a healthy lifestyle. “We need to practice what we preach,” he said.
He also encouraged clinicians to implement existing pediatric guidelines on CVD health, assess and intervene on risk factors in children, and become more effective counselors.
“Instead of telling children what to do, we need to use techniques such as motivational interviewing to guide our young patients in discovering what they want to achieve,” Dr. McCrindle said. “We need to let kids set their own agenda and respect their autonomy. We also need to focus on ideal health across the lifespan, particularly on preventing risk factors and behaviors.”
Dr. McCrindle had no disclosures.
dbrunk@frontlinemedcom.com
TORONTO – If you don’t think clinicians should be worried about the current state of cardiovascular disease (CVD) prevention, consider the arresting data from the 2011 World Health Organization Global Atlas on CVD Prevention and Control.
The atlas showed that CVD accounts for 31% of deaths worldwide: 17.5 million deaths in 2012, projected to increase to 23.3 million deaths in 2030.
At the same time, the American Heart Association projects that by 2030, more than 40% of the U.S. population will have some form of CVD, with total direct costs projected to increase from $273 billion to $818 billion – and real indirect costs because of lost productivity will increase from $172 billion to $276 billion.
“We are not preventing CVD, and the worldwide prevalence of risk factors predicts a grim future,” Dr. Brian W. McCrindle, a staff cardiologist at the Hospital for Sick Children, Toronto, said at the International Society on Thrombosis and Haemostasis congress.
“One of the biggest problems is that we don’t give health and we don’t give prevention their fair due,” Dr. McCrindle continued. “We spend proportionately more health care dollars on providing care for acute and chronic illnesses, much of which are preventable. Our expenditures are growing, leaving little for prevention, and even less for children.”
According to Dr. McCrindle, today’s clinicians miss the mark on preventing CVD “because we focus our efforts on tertiary prevention – the treatment of existing symptomatic disease in order to ameliorate its effects, or treatment to delay or prevent progression; or on secondary prevention – the early detection of the potential for development of a disease, or the prevention of events in those with asymptomatic disease.
“We do make some effort regarding primary prevention – the reduction of risk factors before the occurrence of disease, but tend to delay these efforts until much later in adulthood,” he noted. “We do very little regarding primordial prevention – the prevention of risk factors from developing.”
Dr. McCrindle noted that atherosclerosis has been shown to begin in youth, and that obesity and other cardiovascular risk factors in children track into adulthood. “These findings are of concern regarding current prevention strategies,” he said.
“However, there are some important evidence gaps that need to be addressed before embarking on screening and intervention strategies in youth,” Dr. McCrindle cautioned. “Unfortunately, direct evidence does not exist to assert that risk factors measured in childhood are related to clinical events in adults, although long-term follow-up of existing cohorts may provide that.
“We may never have direct evidence that detection and management of risk factors in children reduce CVD events in adults, since a 50- to 60-year-long randomized trial can never be done,” Dr. McCrindle noted. “However, a chain of indirect evidence can be established.”
Key to current efforts, he continued, are the use of noninvasive ways to measure subclinical atherosclerosis, including ultrasound to assess endothelial function, arterial stiffness and intima-media thickness, and ultrafast computed tomography to detect coronary artery calcium. “These have been important predictors of events in adults, and are increasingly used in pediatric studies,” he said.
While he characterized the current health care landscape as being “at odds with the current reality facing today’s youth,” Dr. McCrindle suggested several ways that attendees can improve the CVD outlook in children, starting with being a role model for a healthy lifestyle. “We need to practice what we preach,” he said.
He also encouraged clinicians to implement existing pediatric guidelines on CVD health, assess and intervene on risk factors in children, and become more effective counselors.
“Instead of telling children what to do, we need to use techniques such as motivational interviewing to guide our young patients in discovering what they want to achieve,” Dr. McCrindle said. “We need to let kids set their own agenda and respect their autonomy. We also need to focus on ideal health across the lifespan, particularly on preventing risk factors and behaviors.”
Dr. McCrindle had no disclosures.
dbrunk@frontlinemedcom.com
TORONTO – If you don’t think clinicians should be worried about the current state of cardiovascular disease (CVD) prevention, consider the arresting data from the 2011 World Health Organization Global Atlas on CVD Prevention and Control.
The atlas showed that CVD accounts for 31% of deaths worldwide: 17.5 million deaths in 2012, projected to increase to 23.3 million deaths in 2030.
At the same time, the American Heart Association projects that by 2030, more than 40% of the U.S. population will have some form of CVD, with total direct costs projected to increase from $273 billion to $818 billion – and real indirect costs because of lost productivity will increase from $172 billion to $276 billion.
“We are not preventing CVD, and the worldwide prevalence of risk factors predicts a grim future,” Dr. Brian W. McCrindle, a staff cardiologist at the Hospital for Sick Children, Toronto, said at the International Society on Thrombosis and Haemostasis congress.
“One of the biggest problems is that we don’t give health and we don’t give prevention their fair due,” Dr. McCrindle continued. “We spend proportionately more health care dollars on providing care for acute and chronic illnesses, much of which are preventable. Our expenditures are growing, leaving little for prevention, and even less for children.”
According to Dr. McCrindle, today’s clinicians miss the mark on preventing CVD “because we focus our efforts on tertiary prevention – the treatment of existing symptomatic disease in order to ameliorate its effects, or treatment to delay or prevent progression; or on secondary prevention – the early detection of the potential for development of a disease, or the prevention of events in those with asymptomatic disease.
“We do make some effort regarding primary prevention – the reduction of risk factors before the occurrence of disease, but tend to delay these efforts until much later in adulthood,” he noted. “We do very little regarding primordial prevention – the prevention of risk factors from developing.”
Dr. McCrindle noted that atherosclerosis has been shown to begin in youth, and that obesity and other cardiovascular risk factors in children track into adulthood. “These findings are of concern regarding current prevention strategies,” he said.
“However, there are some important evidence gaps that need to be addressed before embarking on screening and intervention strategies in youth,” Dr. McCrindle cautioned. “Unfortunately, direct evidence does not exist to assert that risk factors measured in childhood are related to clinical events in adults, although long-term follow-up of existing cohorts may provide that.
“We may never have direct evidence that detection and management of risk factors in children reduce CVD events in adults, since a 50- to 60-year-long randomized trial can never be done,” Dr. McCrindle noted. “However, a chain of indirect evidence can be established.”
Key to current efforts, he continued, are the use of noninvasive ways to measure subclinical atherosclerosis, including ultrasound to assess endothelial function, arterial stiffness and intima-media thickness, and ultrafast computed tomography to detect coronary artery calcium. “These have been important predictors of events in adults, and are increasingly used in pediatric studies,” he said.
While he characterized the current health care landscape as being “at odds with the current reality facing today’s youth,” Dr. McCrindle suggested several ways that attendees can improve the CVD outlook in children, starting with being a role model for a healthy lifestyle. “We need to practice what we preach,” he said.
He also encouraged clinicians to implement existing pediatric guidelines on CVD health, assess and intervene on risk factors in children, and become more effective counselors.
“Instead of telling children what to do, we need to use techniques such as motivational interviewing to guide our young patients in discovering what they want to achieve,” Dr. McCrindle said. “We need to let kids set their own agenda and respect their autonomy. We also need to focus on ideal health across the lifespan, particularly on preventing risk factors and behaviors.”
Dr. McCrindle had no disclosures.
dbrunk@frontlinemedcom.com
EXPERT ANALYSIS FROM THE 2015 ISTH CONGRESS
High VTE recurrence risk persists for at least 3 years
TORONTO – The risk of recurrence following an initial episode of venous thromboembolism is highest in the first 3 months, but remains high for up to 3 years, according to findings from a population-based study involving 2,989 adults.
Over a mean of 23 months (median, 30 months), there were 329 VTE recurrences in the study subjects. Cumulative incidence rates were 5.1% at 3 months, and 14.5% at 3 years. The corresponding rates were 8.7% and 24.8% among those with active cancer, 5.2% and 13.0% among those with provoked VTE, and 3.8% and 13.1% among those with unprovoked VTE, Dr. Wei Huang reported at the International Society on Thrombosis and Haemostasis congress.
Independent predictors of recurrence within 3 years after the index event were active cancer with chemotherapy (hazard ratio, 2.59), active cancer without chemotherapy (HR, 1.59), hypercoagulable state (HR, 2.53) superficial thrombophlebitis (HR, 1.62), varicose vein stripping (HR, 1.75), and inferior vena cava (IVC) filter placement (HR, 2.04), said Dr. Huang of the University of Massachusetts, Worcester.
Individuals included in the study were all residents of the Worcester Metropolitan Statistical Area (WMSA) who had a validated diagnosis of acute first-time deep vein thrombosis and/or pulmonary embolism in a hospital or ambulatory care center that provided short-term care for WMSA residents between 1999 and 2009. Medical records and national and local death registry data were reviewed to examine outcomes up to 3 years after the index event.
Subjects were adults with a mean age of 64 years; 44% were men, and 94% where white. Pulmonary embolism with or without deep vein thrombosis occurred in 42%, and 17% of cases were associated with cancer, 43% involved provoked VTE, and 40% involved unprovoked VTE.
Provoked VTE was defined as VTE occurring within 3 months of a prior surgery, pregnancy, trauma, fracture, or hospitalization in patients without presence of active cancer.
Though limited by the lack of information about variations in physician practices across regions, and by the high proportion of white resident in the WMSA, which both raise questions about whether the findings are generalizable to the U.S. population, the identification of these predictors could allow for improved estimation of risk for individual patients, and may aid in the design of new interventional studies, Dr. Huang concluded.
This study was supported by the National Institutes of Health.
TORONTO – The risk of recurrence following an initial episode of venous thromboembolism is highest in the first 3 months, but remains high for up to 3 years, according to findings from a population-based study involving 2,989 adults.
Over a mean of 23 months (median, 30 months), there were 329 VTE recurrences in the study subjects. Cumulative incidence rates were 5.1% at 3 months, and 14.5% at 3 years. The corresponding rates were 8.7% and 24.8% among those with active cancer, 5.2% and 13.0% among those with provoked VTE, and 3.8% and 13.1% among those with unprovoked VTE, Dr. Wei Huang reported at the International Society on Thrombosis and Haemostasis congress.
Independent predictors of recurrence within 3 years after the index event were active cancer with chemotherapy (hazard ratio, 2.59), active cancer without chemotherapy (HR, 1.59), hypercoagulable state (HR, 2.53) superficial thrombophlebitis (HR, 1.62), varicose vein stripping (HR, 1.75), and inferior vena cava (IVC) filter placement (HR, 2.04), said Dr. Huang of the University of Massachusetts, Worcester.
Individuals included in the study were all residents of the Worcester Metropolitan Statistical Area (WMSA) who had a validated diagnosis of acute first-time deep vein thrombosis and/or pulmonary embolism in a hospital or ambulatory care center that provided short-term care for WMSA residents between 1999 and 2009. Medical records and national and local death registry data were reviewed to examine outcomes up to 3 years after the index event.
Subjects were adults with a mean age of 64 years; 44% were men, and 94% where white. Pulmonary embolism with or without deep vein thrombosis occurred in 42%, and 17% of cases were associated with cancer, 43% involved provoked VTE, and 40% involved unprovoked VTE.
Provoked VTE was defined as VTE occurring within 3 months of a prior surgery, pregnancy, trauma, fracture, or hospitalization in patients without presence of active cancer.
Though limited by the lack of information about variations in physician practices across regions, and by the high proportion of white resident in the WMSA, which both raise questions about whether the findings are generalizable to the U.S. population, the identification of these predictors could allow for improved estimation of risk for individual patients, and may aid in the design of new interventional studies, Dr. Huang concluded.
This study was supported by the National Institutes of Health.
TORONTO – The risk of recurrence following an initial episode of venous thromboembolism is highest in the first 3 months, but remains high for up to 3 years, according to findings from a population-based study involving 2,989 adults.
Over a mean of 23 months (median, 30 months), there were 329 VTE recurrences in the study subjects. Cumulative incidence rates were 5.1% at 3 months, and 14.5% at 3 years. The corresponding rates were 8.7% and 24.8% among those with active cancer, 5.2% and 13.0% among those with provoked VTE, and 3.8% and 13.1% among those with unprovoked VTE, Dr. Wei Huang reported at the International Society on Thrombosis and Haemostasis congress.
Independent predictors of recurrence within 3 years after the index event were active cancer with chemotherapy (hazard ratio, 2.59), active cancer without chemotherapy (HR, 1.59), hypercoagulable state (HR, 2.53) superficial thrombophlebitis (HR, 1.62), varicose vein stripping (HR, 1.75), and inferior vena cava (IVC) filter placement (HR, 2.04), said Dr. Huang of the University of Massachusetts, Worcester.
Individuals included in the study were all residents of the Worcester Metropolitan Statistical Area (WMSA) who had a validated diagnosis of acute first-time deep vein thrombosis and/or pulmonary embolism in a hospital or ambulatory care center that provided short-term care for WMSA residents between 1999 and 2009. Medical records and national and local death registry data were reviewed to examine outcomes up to 3 years after the index event.
Subjects were adults with a mean age of 64 years; 44% were men, and 94% where white. Pulmonary embolism with or without deep vein thrombosis occurred in 42%, and 17% of cases were associated with cancer, 43% involved provoked VTE, and 40% involved unprovoked VTE.
Provoked VTE was defined as VTE occurring within 3 months of a prior surgery, pregnancy, trauma, fracture, or hospitalization in patients without presence of active cancer.
Though limited by the lack of information about variations in physician practices across regions, and by the high proportion of white resident in the WMSA, which both raise questions about whether the findings are generalizable to the U.S. population, the identification of these predictors could allow for improved estimation of risk for individual patients, and may aid in the design of new interventional studies, Dr. Huang concluded.
This study was supported by the National Institutes of Health.
AT THE 2015 ISTH CONGRESS
Key clinical point: The risk of recurrence following an initial episode of venous thromboembolism is highest in the first 3 months, but remains high for up to 3 years, according to findings from a population-based study involving 2,989 adults.
Major finding: Active cancer with chemotherapy was the strongest predictor of VTE recurrence (hazard ratio, 2.59).
Data source: Population-based surveillance of 2,989 adults patients.
Disclosures: The National Institutes of Health supported the study.
Statins showed no benefit in reducing risk of recurrent VTE
TORONTO – The use of statins showed no benefit in reducing the risk of recurrent venous thromboembolism in patients enrolled in phase III trials comparing direct oral anticoagulants with vitamin K antagonists, a large meta-analysis demonstrated.
Recurrence after an unprovoked VTE is 10%-15% in the first 6-12 months, and recurrence risk in the first 6 months is reduced by 80%-90% with anticoagulants, Dr. Mandy N. Lauw said at the International Society on Thrombosis and Haemostasis congress.
“However, the use of anticoagulants has the risk of bleeding, and therefore the long-term risk-benefit ratio is unclear,” said Dr. Lauw of the department of vascular medicine at Academic Medical Center, Amsterdam. “Therefore it’s interesting to look at modalities outside the coagulation cascade to treat patients for longer term and to prevent recurrent thrombosis. One of these modalities has been the use of statins, which are known to reduce arterial vascular events by lowering cholesterol levels. However, recent studies have also indicated that they may have an effect on VTE events.”
In an effort to evaluate the effects of statins on recurrent VTE, Dr. Lauw and her associates conducted a meta-analysis of statins in three randomized, phase III trials comparing non–vitamin K oral anticoagulant (NOAC) with vitamin K antagonist (VKA) therapy in patients with acute symptomatic VTE.
The trials included 5,153 patients enrolled in RE-COVER I and II (an analysis of dabigatran vs. standard therapy for acute VTE), 8,281 enrolled in the EINSTEIN clinical trials for DVT and pulmonary embolism (an analysis of rivaroxaban vs. standard therapy for symptomatic VTE), and 8,292 enrolled in a trial conducted by the Hokusai-DVT investigators (an analysis of edoxaban vs. standard therapy for symptomatic VTE). The researchers examined the effect of statin use on recurrent VTE or VTE-related death, recurrent DVT or PE, and major bleeding. To do this they conducted a pooled meta-analysis and an analysis per study, adjusted for age, gender, diabetes mellitus, creatinine clearance of less than 50 mL/min, hypertension, prior VTE, and use of aspirin.
Dr. Lauw reported results from 21,587 patients included in the analysis. Among all three studies, 2,754 patients (12.8%) used statins and 18,833 (87.2%) did not. In an unadjusted pooled analysis, the use of statins at baseline did not have an influence on the risk of recurrent VTE or VTE-related death, with an odds ratio of 0.91. There was also no effect of statins on the risk of recurrent PE or DVT (ORs of 0.84 and 1.05, respectively), while major bleeding seemed to be increased with the use of statins (OR, 1.65). A subanalysis in patients getting NOAC or VKA separately showed a non–statistically significant benefit of statins with NOACs, compared with VKAs on the risk of recurrent VTE or VTE-related death (ORs of 0.60 vs. OR 1.24, respectively). The results were similar for NOACs, compared with VKA, on the risk of recurrent DVT (ORs of 0.47 vs. OR 1.67) and the risk of recurrent PE (ORs of 0.73 vs. 1.02).
On adjusted analysis, the risk of recurrent VTE or VTE-related death between all three studies was similar and nonsignificant (hazard ratio of 0.99 in RE-COVER I and II, HR of 0.78 in the EINSTEIN clinical trials for DVT & PE, and HR of 0.99 in the trial conducted by the Hokusai-DVT Investigators). There also were no significant differences between the study groups in recurrent PE, recurrent DVT, or major bleeding. “So statins have no beneficial effect, but also no harmful effect,” Dr. Lauw said.
She acknowledged certain limitations of the study, including the fact that it was an on-treatment analysis, “so it could be that we had inadequate follow-up duration,” she said. “Also, we don’t have any assessment of statin effects without anticoagulation in these patients. Perhaps it would be interesting to use the extension trials to explore these results as well.”
For now, “there is no evidence that statins reduce the recurrence of VTE,” she concluded. “The only way to explore this is to do a randomized controlled trial properly designed and powered to estimate this effect prospectively.”
Dr. Lauw reported having no financial disclosures.
TORONTO – The use of statins showed no benefit in reducing the risk of recurrent venous thromboembolism in patients enrolled in phase III trials comparing direct oral anticoagulants with vitamin K antagonists, a large meta-analysis demonstrated.
Recurrence after an unprovoked VTE is 10%-15% in the first 6-12 months, and recurrence risk in the first 6 months is reduced by 80%-90% with anticoagulants, Dr. Mandy N. Lauw said at the International Society on Thrombosis and Haemostasis congress.
“However, the use of anticoagulants has the risk of bleeding, and therefore the long-term risk-benefit ratio is unclear,” said Dr. Lauw of the department of vascular medicine at Academic Medical Center, Amsterdam. “Therefore it’s interesting to look at modalities outside the coagulation cascade to treat patients for longer term and to prevent recurrent thrombosis. One of these modalities has been the use of statins, which are known to reduce arterial vascular events by lowering cholesterol levels. However, recent studies have also indicated that they may have an effect on VTE events.”
In an effort to evaluate the effects of statins on recurrent VTE, Dr. Lauw and her associates conducted a meta-analysis of statins in three randomized, phase III trials comparing non–vitamin K oral anticoagulant (NOAC) with vitamin K antagonist (VKA) therapy in patients with acute symptomatic VTE.
The trials included 5,153 patients enrolled in RE-COVER I and II (an analysis of dabigatran vs. standard therapy for acute VTE), 8,281 enrolled in the EINSTEIN clinical trials for DVT and pulmonary embolism (an analysis of rivaroxaban vs. standard therapy for symptomatic VTE), and 8,292 enrolled in a trial conducted by the Hokusai-DVT investigators (an analysis of edoxaban vs. standard therapy for symptomatic VTE). The researchers examined the effect of statin use on recurrent VTE or VTE-related death, recurrent DVT or PE, and major bleeding. To do this they conducted a pooled meta-analysis and an analysis per study, adjusted for age, gender, diabetes mellitus, creatinine clearance of less than 50 mL/min, hypertension, prior VTE, and use of aspirin.
Dr. Lauw reported results from 21,587 patients included in the analysis. Among all three studies, 2,754 patients (12.8%) used statins and 18,833 (87.2%) did not. In an unadjusted pooled analysis, the use of statins at baseline did not have an influence on the risk of recurrent VTE or VTE-related death, with an odds ratio of 0.91. There was also no effect of statins on the risk of recurrent PE or DVT (ORs of 0.84 and 1.05, respectively), while major bleeding seemed to be increased with the use of statins (OR, 1.65). A subanalysis in patients getting NOAC or VKA separately showed a non–statistically significant benefit of statins with NOACs, compared with VKAs on the risk of recurrent VTE or VTE-related death (ORs of 0.60 vs. OR 1.24, respectively). The results were similar for NOACs, compared with VKA, on the risk of recurrent DVT (ORs of 0.47 vs. OR 1.67) and the risk of recurrent PE (ORs of 0.73 vs. 1.02).
On adjusted analysis, the risk of recurrent VTE or VTE-related death between all three studies was similar and nonsignificant (hazard ratio of 0.99 in RE-COVER I and II, HR of 0.78 in the EINSTEIN clinical trials for DVT & PE, and HR of 0.99 in the trial conducted by the Hokusai-DVT Investigators). There also were no significant differences between the study groups in recurrent PE, recurrent DVT, or major bleeding. “So statins have no beneficial effect, but also no harmful effect,” Dr. Lauw said.
She acknowledged certain limitations of the study, including the fact that it was an on-treatment analysis, “so it could be that we had inadequate follow-up duration,” she said. “Also, we don’t have any assessment of statin effects without anticoagulation in these patients. Perhaps it would be interesting to use the extension trials to explore these results as well.”
For now, “there is no evidence that statins reduce the recurrence of VTE,” she concluded. “The only way to explore this is to do a randomized controlled trial properly designed and powered to estimate this effect prospectively.”
Dr. Lauw reported having no financial disclosures.
TORONTO – The use of statins showed no benefit in reducing the risk of recurrent venous thromboembolism in patients enrolled in phase III trials comparing direct oral anticoagulants with vitamin K antagonists, a large meta-analysis demonstrated.
Recurrence after an unprovoked VTE is 10%-15% in the first 6-12 months, and recurrence risk in the first 6 months is reduced by 80%-90% with anticoagulants, Dr. Mandy N. Lauw said at the International Society on Thrombosis and Haemostasis congress.
“However, the use of anticoagulants has the risk of bleeding, and therefore the long-term risk-benefit ratio is unclear,” said Dr. Lauw of the department of vascular medicine at Academic Medical Center, Amsterdam. “Therefore it’s interesting to look at modalities outside the coagulation cascade to treat patients for longer term and to prevent recurrent thrombosis. One of these modalities has been the use of statins, which are known to reduce arterial vascular events by lowering cholesterol levels. However, recent studies have also indicated that they may have an effect on VTE events.”
In an effort to evaluate the effects of statins on recurrent VTE, Dr. Lauw and her associates conducted a meta-analysis of statins in three randomized, phase III trials comparing non–vitamin K oral anticoagulant (NOAC) with vitamin K antagonist (VKA) therapy in patients with acute symptomatic VTE.
The trials included 5,153 patients enrolled in RE-COVER I and II (an analysis of dabigatran vs. standard therapy for acute VTE), 8,281 enrolled in the EINSTEIN clinical trials for DVT and pulmonary embolism (an analysis of rivaroxaban vs. standard therapy for symptomatic VTE), and 8,292 enrolled in a trial conducted by the Hokusai-DVT investigators (an analysis of edoxaban vs. standard therapy for symptomatic VTE). The researchers examined the effect of statin use on recurrent VTE or VTE-related death, recurrent DVT or PE, and major bleeding. To do this they conducted a pooled meta-analysis and an analysis per study, adjusted for age, gender, diabetes mellitus, creatinine clearance of less than 50 mL/min, hypertension, prior VTE, and use of aspirin.
Dr. Lauw reported results from 21,587 patients included in the analysis. Among all three studies, 2,754 patients (12.8%) used statins and 18,833 (87.2%) did not. In an unadjusted pooled analysis, the use of statins at baseline did not have an influence on the risk of recurrent VTE or VTE-related death, with an odds ratio of 0.91. There was also no effect of statins on the risk of recurrent PE or DVT (ORs of 0.84 and 1.05, respectively), while major bleeding seemed to be increased with the use of statins (OR, 1.65). A subanalysis in patients getting NOAC or VKA separately showed a non–statistically significant benefit of statins with NOACs, compared with VKAs on the risk of recurrent VTE or VTE-related death (ORs of 0.60 vs. OR 1.24, respectively). The results were similar for NOACs, compared with VKA, on the risk of recurrent DVT (ORs of 0.47 vs. OR 1.67) and the risk of recurrent PE (ORs of 0.73 vs. 1.02).
On adjusted analysis, the risk of recurrent VTE or VTE-related death between all three studies was similar and nonsignificant (hazard ratio of 0.99 in RE-COVER I and II, HR of 0.78 in the EINSTEIN clinical trials for DVT & PE, and HR of 0.99 in the trial conducted by the Hokusai-DVT Investigators). There also were no significant differences between the study groups in recurrent PE, recurrent DVT, or major bleeding. “So statins have no beneficial effect, but also no harmful effect,” Dr. Lauw said.
She acknowledged certain limitations of the study, including the fact that it was an on-treatment analysis, “so it could be that we had inadequate follow-up duration,” she said. “Also, we don’t have any assessment of statin effects without anticoagulation in these patients. Perhaps it would be interesting to use the extension trials to explore these results as well.”
For now, “there is no evidence that statins reduce the recurrence of VTE,” she concluded. “The only way to explore this is to do a randomized controlled trial properly designed and powered to estimate this effect prospectively.”
Dr. Lauw reported having no financial disclosures.
AT THE 2015 ISTH CONGRESS
Key clinical point: No beneficial effect of statins in reducing recurrent VTE was observed in patients threated in phase III acute VTE trials.
Major finding: On adjusted analysis, the risk of recurrent VTE or VTE-related death between all three studies was similar and nonsignificant (HR of 0.99 in RE-COVER I and II, HR of 0.78 in the EINSTEIN clinical trials for DVT and PE, and HR of 0.99 in the trial conducted by the Hokusai-DVT investigators).
Data source: A meta-analysis of 21,587 patients enrolled in three phase III trials comparing non–vitamin K oral anticoagulant (NOAC) with vitamin K antagonist (VKA) therapy in patients with acute symptomatic VTE.
Disclosures: Dr. Lauw reported having no financial disclosures.
Inhibitors increase burden of hemophilia care

TORONTO—When children with hemophilia develop inhibitors, their caregivers shoulder a greater burden, according to a pilot study.
Researchers surveyed 40 subjects on the burden of caring for a child with hemophilia and found that inhibitor development significantly increased the burden of care.
But other factors—such as the number of bleeds a child had experienced in the last 12 months—had no significant impact.
Sylvia von Mackensen, PhD, of the University Medical Centre Hamburg-Eppendorf in Hamburg, Germany, and her colleagues presented these findings at the ISTH 2015 Congress (abstract PO256-WED).
The study was a pilot test of the HEMOCAB questionnaire, which consists of 59 questions mapped to 13 domains. Caregivers were asked to select the response that best qualified their burden and were scored on a scale of 0 to 100, with higher values corresponding with greater burden.
Forty caregivers completed the questionnaire. All of them had children with hemophilia (n=40), with or without inhibitors, who were younger than 22 years of age.
Three-quarters of the caregivers were mothers, 17.5% were fathers, and 7.5% were grandmothers. The mean age of caregivers was 39.32 ± 8.9 years (range, 27-66), and the mean age of the hemophilia patients was 10.98 ± 5.5 years (range, 1-21).
Most of the patients had hemophilia A (95%), and most had severe disease (77.5%). Six children (15%) had inhibitors. Overall, patients had experienced an average of 4.83 ±8.9 bleeds (range, 0-52) in the previous 12 months.
Most of the patients (88.5%) were receiving prophylaxis. Caregivers said they spent 8.69 ± 7.7 hours per month on infusion and 3.84 ± 6.7 hours (range, 0-30) per month traveling to hemophilia treatment facilities.
Size of burden
Caregivers said the most burdensome aspects of care were the caregivers’ perception of the child (38%), emotional stress (36%), financial burden (34%), and the impact of care on the caregiver (31%).
For nearly all of the domains assessed—emotional stress, personal sacrifice, medical management, work situation, etc.—a caregivers’ burden was significantly higher if a child had inhibitors. The only exception was school-related burden.
When the researchers analyzed the impact of other factors on care burden, they found that only inhibitor development had a significant impact.
There was no impact for orthopedic joint score, age of the caregiver, age of the child, time for infusion, time traveling to a hemophilia treatment center, the number of bleeds in the past 12 months, the number of children with hemophilia per household, home treatment, caregiver marital status, location, or caregiver education.
Frequency of burden
The HEMOCAB questionnaire also included scales assessing the frequency of burden. Dr von Mackensen and her colleagues presented data from these scales for the caregivers’ perception of their child, emotional stress, and finances.
Sixty percent of caregivers said they sometimes, often, or always feel their child’s condition is a difficult situation. Seventy-three percent of caregivers expressed feelings of sadness about informing their child of what he can and cannot do due to his illness.
Seventy-four percent of caregivers said they sometimes, often, or always feel afraid their child might get injured when they are not around to help. Forty-six percent of caregivers reported feeling afraid their child’s condition might worsen, and 36% said they feared their child might die from his condition.
Forty-six percent of caregivers said their child’s hemophilia sometimes, often, or always causes financial problems. And 33% of caregivers said that, at least sometimes, their family does not have enough money because of their child’s hemophilia.
HEMOCAB is a trademark of Novo Nordisk Health Care AG. Dr von Mackensen received a consulting fee from Novo Nordisk for developing the HEMOCAB questionnaire. Leonard A. Valentino, MD, of Rush University Medical Center in Chicago, Illinois, was involved in developing the questionnaire as well but did not participate in the pilot study.
The other researchers involved in the study have received funding/consulting fees from—or are employees of—Novo Nordisk, Baxter, Bayer, OctaPharma, CSL Behring, OPKO Health, and Selexys. ![]()

TORONTO—When children with hemophilia develop inhibitors, their caregivers shoulder a greater burden, according to a pilot study.
Researchers surveyed 40 subjects on the burden of caring for a child with hemophilia and found that inhibitor development significantly increased the burden of care.
But other factors—such as the number of bleeds a child had experienced in the last 12 months—had no significant impact.
Sylvia von Mackensen, PhD, of the University Medical Centre Hamburg-Eppendorf in Hamburg, Germany, and her colleagues presented these findings at the ISTH 2015 Congress (abstract PO256-WED).
The study was a pilot test of the HEMOCAB questionnaire, which consists of 59 questions mapped to 13 domains. Caregivers were asked to select the response that best qualified their burden and were scored on a scale of 0 to 100, with higher values corresponding with greater burden.
Forty caregivers completed the questionnaire. All of them had children with hemophilia (n=40), with or without inhibitors, who were younger than 22 years of age.
Three-quarters of the caregivers were mothers, 17.5% were fathers, and 7.5% were grandmothers. The mean age of caregivers was 39.32 ± 8.9 years (range, 27-66), and the mean age of the hemophilia patients was 10.98 ± 5.5 years (range, 1-21).
Most of the patients had hemophilia A (95%), and most had severe disease (77.5%). Six children (15%) had inhibitors. Overall, patients had experienced an average of 4.83 ±8.9 bleeds (range, 0-52) in the previous 12 months.
Most of the patients (88.5%) were receiving prophylaxis. Caregivers said they spent 8.69 ± 7.7 hours per month on infusion and 3.84 ± 6.7 hours (range, 0-30) per month traveling to hemophilia treatment facilities.
Size of burden
Caregivers said the most burdensome aspects of care were the caregivers’ perception of the child (38%), emotional stress (36%), financial burden (34%), and the impact of care on the caregiver (31%).
For nearly all of the domains assessed—emotional stress, personal sacrifice, medical management, work situation, etc.—a caregivers’ burden was significantly higher if a child had inhibitors. The only exception was school-related burden.
When the researchers analyzed the impact of other factors on care burden, they found that only inhibitor development had a significant impact.
There was no impact for orthopedic joint score, age of the caregiver, age of the child, time for infusion, time traveling to a hemophilia treatment center, the number of bleeds in the past 12 months, the number of children with hemophilia per household, home treatment, caregiver marital status, location, or caregiver education.
Frequency of burden
The HEMOCAB questionnaire also included scales assessing the frequency of burden. Dr von Mackensen and her colleagues presented data from these scales for the caregivers’ perception of their child, emotional stress, and finances.
Sixty percent of caregivers said they sometimes, often, or always feel their child’s condition is a difficult situation. Seventy-three percent of caregivers expressed feelings of sadness about informing their child of what he can and cannot do due to his illness.
Seventy-four percent of caregivers said they sometimes, often, or always feel afraid their child might get injured when they are not around to help. Forty-six percent of caregivers reported feeling afraid their child’s condition might worsen, and 36% said they feared their child might die from his condition.
Forty-six percent of caregivers said their child’s hemophilia sometimes, often, or always causes financial problems. And 33% of caregivers said that, at least sometimes, their family does not have enough money because of their child’s hemophilia.
HEMOCAB is a trademark of Novo Nordisk Health Care AG. Dr von Mackensen received a consulting fee from Novo Nordisk for developing the HEMOCAB questionnaire. Leonard A. Valentino, MD, of Rush University Medical Center in Chicago, Illinois, was involved in developing the questionnaire as well but did not participate in the pilot study.
The other researchers involved in the study have received funding/consulting fees from—or are employees of—Novo Nordisk, Baxter, Bayer, OctaPharma, CSL Behring, OPKO Health, and Selexys. ![]()

TORONTO—When children with hemophilia develop inhibitors, their caregivers shoulder a greater burden, according to a pilot study.
Researchers surveyed 40 subjects on the burden of caring for a child with hemophilia and found that inhibitor development significantly increased the burden of care.
But other factors—such as the number of bleeds a child had experienced in the last 12 months—had no significant impact.
Sylvia von Mackensen, PhD, of the University Medical Centre Hamburg-Eppendorf in Hamburg, Germany, and her colleagues presented these findings at the ISTH 2015 Congress (abstract PO256-WED).
The study was a pilot test of the HEMOCAB questionnaire, which consists of 59 questions mapped to 13 domains. Caregivers were asked to select the response that best qualified their burden and were scored on a scale of 0 to 100, with higher values corresponding with greater burden.
Forty caregivers completed the questionnaire. All of them had children with hemophilia (n=40), with or without inhibitors, who were younger than 22 years of age.
Three-quarters of the caregivers were mothers, 17.5% were fathers, and 7.5% were grandmothers. The mean age of caregivers was 39.32 ± 8.9 years (range, 27-66), and the mean age of the hemophilia patients was 10.98 ± 5.5 years (range, 1-21).
Most of the patients had hemophilia A (95%), and most had severe disease (77.5%). Six children (15%) had inhibitors. Overall, patients had experienced an average of 4.83 ±8.9 bleeds (range, 0-52) in the previous 12 months.
Most of the patients (88.5%) were receiving prophylaxis. Caregivers said they spent 8.69 ± 7.7 hours per month on infusion and 3.84 ± 6.7 hours (range, 0-30) per month traveling to hemophilia treatment facilities.
Size of burden
Caregivers said the most burdensome aspects of care were the caregivers’ perception of the child (38%), emotional stress (36%), financial burden (34%), and the impact of care on the caregiver (31%).
For nearly all of the domains assessed—emotional stress, personal sacrifice, medical management, work situation, etc.—a caregivers’ burden was significantly higher if a child had inhibitors. The only exception was school-related burden.
When the researchers analyzed the impact of other factors on care burden, they found that only inhibitor development had a significant impact.
There was no impact for orthopedic joint score, age of the caregiver, age of the child, time for infusion, time traveling to a hemophilia treatment center, the number of bleeds in the past 12 months, the number of children with hemophilia per household, home treatment, caregiver marital status, location, or caregiver education.
Frequency of burden
The HEMOCAB questionnaire also included scales assessing the frequency of burden. Dr von Mackensen and her colleagues presented data from these scales for the caregivers’ perception of their child, emotional stress, and finances.
Sixty percent of caregivers said they sometimes, often, or always feel their child’s condition is a difficult situation. Seventy-three percent of caregivers expressed feelings of sadness about informing their child of what he can and cannot do due to his illness.
Seventy-four percent of caregivers said they sometimes, often, or always feel afraid their child might get injured when they are not around to help. Forty-six percent of caregivers reported feeling afraid their child’s condition might worsen, and 36% said they feared their child might die from his condition.
Forty-six percent of caregivers said their child’s hemophilia sometimes, often, or always causes financial problems. And 33% of caregivers said that, at least sometimes, their family does not have enough money because of their child’s hemophilia.
HEMOCAB is a trademark of Novo Nordisk Health Care AG. Dr von Mackensen received a consulting fee from Novo Nordisk for developing the HEMOCAB questionnaire. Leonard A. Valentino, MD, of Rush University Medical Center in Chicago, Illinois, was involved in developing the questionnaire as well but did not participate in the pilot study.
The other researchers involved in the study have received funding/consulting fees from—or are employees of—Novo Nordisk, Baxter, Bayer, OctaPharma, CSL Behring, OPKO Health, and Selexys. ![]()
Pain problems prevalent in adults with hemophilia

TORONTO—A survey of adult hemophilia patients suggests there is room for improvement in assessing and managing disease-related pain.
Roughly 85% of patients surveyed for this study, known as P-FiQ, said they had experienced acute and/or chronic pain in the past 6 months.
Although most patients had no trouble caring for themselves, the pain often had an impact on their daily lives, especially with regard to physical activity and overall mobility.
“Pain and discomfort are significant challenges for people with hemophilia,” said study investigator Michael Recht, MD, PhD, of Oregon Health Sciences University in Portland.
“These results emphasize the importance of providing comprehensive care and support beyond traditional therapy to people living with bleeding disorders.”
Dr Recht and his colleagues presented results of the P-FiQ study in 3 posters at the ISTH 2015 Congress (abstracts PO277-MON, PO297-WED, and PO298-WED).
The study included adult males with mild to severe hemophilia who had a history of joint pain or bleeding. Subjects were asked to assess pain and functional impairment using patient-reported outcome instruments.
During routine visits over the course of a year, 164 participants completed a pain history and 5 questionnaires: the EQ-5D-5L; Brief Pain Inventory Short Form, version 2; International Physical Activity Questionnaire; SF-36v2; and Hemophilia Activities List.
The patients had a median age of 34. More patients had hemophilia A (n=122) than hemophilia B (n=42), and few (n=10) had inhibitors. Sixty-one percent of patients had self-reported arthritis, bone, or joint problems.
Current patient-reported treatment regimens (n=163) were prophylaxis (42%), on-demand treatment (39%), or mostly on-demand treatment (19%). Twenty-five of the 31 patients using on-demand treatment reported using infusions ahead of activity.
Pain prevalence and management
Most participants (85.2%) said they had experienced acute and/or chronic pain over the past 6 months. Twenty-nine percent said they had experienced acute and chronic pain, 32.7% had chronic pain only, 23.5% had acute pain only, and 14.8% reported no pain.
Acute pain was most frequently described as sharp, aching, shooting, and throbbing. Chronic pain was often described as aching, nagging, throbbing, and sharp.
The most common analgesics used for acute or chronic pain were acetaminophen (69.4% and 58%, respectively), NSAIDs (40% and 52%, respectively), and hydrocodone-acetaminophen (29.4% and 33%, respectively).
The most common nonanalgesic strategies used for acute or chronic pain were ice (72.9% and 37%, respectively), rest (48.2% and 34%, respectively), factor VIII/IX or bypassing agent (48.2% and 24%, respectively), elevation (34.1% and 28%, respectively), relaxation (30.6% and 23.0%, respectively), compression (27.1% and 21%, respectively), and heat (24.7% and 15%, respectively).
Impact of pain on daily life
When completing the EQ-5D-5L questionnaire, most patients reported problems with mobility, performing usual activities, and pain or discomfort. However, most patients said they had no problems with self-care (78%) or anxiety/depression (58.5%).
A similar proportion of patients reported slight and moderate pain and discomfort (29.9% and 31.1%, respectively). Pain and discomfort was severe for 11% of patients and extreme for 1.2%, but 26.8% of patients reported no pain or discomfort.
When it came to mobility, patients reported slight (32.3%), moderate (19.5%), and severe (8.5%) problems, and 1.2% of patients said they were unable to get around. However, 38.4% of patients reported having no such problems.
About 44% of patients reported no problems performing usual activities, but 37.2% had slight problems, 14.6% had moderate problems, and 1.8% of patients each had severe problems or were unable to perform usual activities.
For the Brief Pain Inventory, pain severity and interference with daily activities were rated on a scale of 0 to 10, with 0 being no pain/no interference and 10 being pain as bad as you can imagine/pain that completely interferes with daily life.
The overall median pain severity and pain interference were 3.0 (range, 1.3-4.8) and 2.9 (range, 0.7-5.2), respectively. The median worst pain was 6.0, least pain 2.0, average pain 3.0, and current pain 2.0. Ankles were the most frequently reported site of pain.
When completing the International Physical Activity Questionnaire, 49.3% of patients (73/148) reported no activity in the prior week.
The median SF-36v2 scores were lower for physical health domains than mental health domains, and the overall median health score was 3.0 (range, 2.0-3.0).
The median score on the Hemophilia Activities List was 76.1 (range, 59.2-95.1). And patients said hemophilia had a greater impact on their lower extremities than upper extremities.
Dr Recht and his colleagues said these results substantiate the high prevalence of pain in adults with hemophilia. And the study highlights opportunities to improve the assessment and management of pain in these patients.
Study investigators have received funding/consulting fees from—or are employees/shareholders of—Novo Nordisk, Baxter, Biogen, Bayer, OctaPharma, Pfizer, CSL Behring, Kendrion, Alexion, Grifols, OPKO Health, Sanofi, Merck, and ProMeticLife Sciences. ![]()

TORONTO—A survey of adult hemophilia patients suggests there is room for improvement in assessing and managing disease-related pain.
Roughly 85% of patients surveyed for this study, known as P-FiQ, said they had experienced acute and/or chronic pain in the past 6 months.
Although most patients had no trouble caring for themselves, the pain often had an impact on their daily lives, especially with regard to physical activity and overall mobility.
“Pain and discomfort are significant challenges for people with hemophilia,” said study investigator Michael Recht, MD, PhD, of Oregon Health Sciences University in Portland.
“These results emphasize the importance of providing comprehensive care and support beyond traditional therapy to people living with bleeding disorders.”
Dr Recht and his colleagues presented results of the P-FiQ study in 3 posters at the ISTH 2015 Congress (abstracts PO277-MON, PO297-WED, and PO298-WED).
The study included adult males with mild to severe hemophilia who had a history of joint pain or bleeding. Subjects were asked to assess pain and functional impairment using patient-reported outcome instruments.
During routine visits over the course of a year, 164 participants completed a pain history and 5 questionnaires: the EQ-5D-5L; Brief Pain Inventory Short Form, version 2; International Physical Activity Questionnaire; SF-36v2; and Hemophilia Activities List.
The patients had a median age of 34. More patients had hemophilia A (n=122) than hemophilia B (n=42), and few (n=10) had inhibitors. Sixty-one percent of patients had self-reported arthritis, bone, or joint problems.
Current patient-reported treatment regimens (n=163) were prophylaxis (42%), on-demand treatment (39%), or mostly on-demand treatment (19%). Twenty-five of the 31 patients using on-demand treatment reported using infusions ahead of activity.
Pain prevalence and management
Most participants (85.2%) said they had experienced acute and/or chronic pain over the past 6 months. Twenty-nine percent said they had experienced acute and chronic pain, 32.7% had chronic pain only, 23.5% had acute pain only, and 14.8% reported no pain.
Acute pain was most frequently described as sharp, aching, shooting, and throbbing. Chronic pain was often described as aching, nagging, throbbing, and sharp.
The most common analgesics used for acute or chronic pain were acetaminophen (69.4% and 58%, respectively), NSAIDs (40% and 52%, respectively), and hydrocodone-acetaminophen (29.4% and 33%, respectively).
The most common nonanalgesic strategies used for acute or chronic pain were ice (72.9% and 37%, respectively), rest (48.2% and 34%, respectively), factor VIII/IX or bypassing agent (48.2% and 24%, respectively), elevation (34.1% and 28%, respectively), relaxation (30.6% and 23.0%, respectively), compression (27.1% and 21%, respectively), and heat (24.7% and 15%, respectively).
Impact of pain on daily life
When completing the EQ-5D-5L questionnaire, most patients reported problems with mobility, performing usual activities, and pain or discomfort. However, most patients said they had no problems with self-care (78%) or anxiety/depression (58.5%).
A similar proportion of patients reported slight and moderate pain and discomfort (29.9% and 31.1%, respectively). Pain and discomfort was severe for 11% of patients and extreme for 1.2%, but 26.8% of patients reported no pain or discomfort.
When it came to mobility, patients reported slight (32.3%), moderate (19.5%), and severe (8.5%) problems, and 1.2% of patients said they were unable to get around. However, 38.4% of patients reported having no such problems.
About 44% of patients reported no problems performing usual activities, but 37.2% had slight problems, 14.6% had moderate problems, and 1.8% of patients each had severe problems or were unable to perform usual activities.
For the Brief Pain Inventory, pain severity and interference with daily activities were rated on a scale of 0 to 10, with 0 being no pain/no interference and 10 being pain as bad as you can imagine/pain that completely interferes with daily life.
The overall median pain severity and pain interference were 3.0 (range, 1.3-4.8) and 2.9 (range, 0.7-5.2), respectively. The median worst pain was 6.0, least pain 2.0, average pain 3.0, and current pain 2.0. Ankles were the most frequently reported site of pain.
When completing the International Physical Activity Questionnaire, 49.3% of patients (73/148) reported no activity in the prior week.
The median SF-36v2 scores were lower for physical health domains than mental health domains, and the overall median health score was 3.0 (range, 2.0-3.0).
The median score on the Hemophilia Activities List was 76.1 (range, 59.2-95.1). And patients said hemophilia had a greater impact on their lower extremities than upper extremities.
Dr Recht and his colleagues said these results substantiate the high prevalence of pain in adults with hemophilia. And the study highlights opportunities to improve the assessment and management of pain in these patients.
Study investigators have received funding/consulting fees from—or are employees/shareholders of—Novo Nordisk, Baxter, Biogen, Bayer, OctaPharma, Pfizer, CSL Behring, Kendrion, Alexion, Grifols, OPKO Health, Sanofi, Merck, and ProMeticLife Sciences. ![]()

TORONTO—A survey of adult hemophilia patients suggests there is room for improvement in assessing and managing disease-related pain.
Roughly 85% of patients surveyed for this study, known as P-FiQ, said they had experienced acute and/or chronic pain in the past 6 months.
Although most patients had no trouble caring for themselves, the pain often had an impact on their daily lives, especially with regard to physical activity and overall mobility.
“Pain and discomfort are significant challenges for people with hemophilia,” said study investigator Michael Recht, MD, PhD, of Oregon Health Sciences University in Portland.
“These results emphasize the importance of providing comprehensive care and support beyond traditional therapy to people living with bleeding disorders.”
Dr Recht and his colleagues presented results of the P-FiQ study in 3 posters at the ISTH 2015 Congress (abstracts PO277-MON, PO297-WED, and PO298-WED).
The study included adult males with mild to severe hemophilia who had a history of joint pain or bleeding. Subjects were asked to assess pain and functional impairment using patient-reported outcome instruments.
During routine visits over the course of a year, 164 participants completed a pain history and 5 questionnaires: the EQ-5D-5L; Brief Pain Inventory Short Form, version 2; International Physical Activity Questionnaire; SF-36v2; and Hemophilia Activities List.
The patients had a median age of 34. More patients had hemophilia A (n=122) than hemophilia B (n=42), and few (n=10) had inhibitors. Sixty-one percent of patients had self-reported arthritis, bone, or joint problems.
Current patient-reported treatment regimens (n=163) were prophylaxis (42%), on-demand treatment (39%), or mostly on-demand treatment (19%). Twenty-five of the 31 patients using on-demand treatment reported using infusions ahead of activity.
Pain prevalence and management
Most participants (85.2%) said they had experienced acute and/or chronic pain over the past 6 months. Twenty-nine percent said they had experienced acute and chronic pain, 32.7% had chronic pain only, 23.5% had acute pain only, and 14.8% reported no pain.
Acute pain was most frequently described as sharp, aching, shooting, and throbbing. Chronic pain was often described as aching, nagging, throbbing, and sharp.
The most common analgesics used for acute or chronic pain were acetaminophen (69.4% and 58%, respectively), NSAIDs (40% and 52%, respectively), and hydrocodone-acetaminophen (29.4% and 33%, respectively).
The most common nonanalgesic strategies used for acute or chronic pain were ice (72.9% and 37%, respectively), rest (48.2% and 34%, respectively), factor VIII/IX or bypassing agent (48.2% and 24%, respectively), elevation (34.1% and 28%, respectively), relaxation (30.6% and 23.0%, respectively), compression (27.1% and 21%, respectively), and heat (24.7% and 15%, respectively).
Impact of pain on daily life
When completing the EQ-5D-5L questionnaire, most patients reported problems with mobility, performing usual activities, and pain or discomfort. However, most patients said they had no problems with self-care (78%) or anxiety/depression (58.5%).
A similar proportion of patients reported slight and moderate pain and discomfort (29.9% and 31.1%, respectively). Pain and discomfort was severe for 11% of patients and extreme for 1.2%, but 26.8% of patients reported no pain or discomfort.
When it came to mobility, patients reported slight (32.3%), moderate (19.5%), and severe (8.5%) problems, and 1.2% of patients said they were unable to get around. However, 38.4% of patients reported having no such problems.
About 44% of patients reported no problems performing usual activities, but 37.2% had slight problems, 14.6% had moderate problems, and 1.8% of patients each had severe problems or were unable to perform usual activities.
For the Brief Pain Inventory, pain severity and interference with daily activities were rated on a scale of 0 to 10, with 0 being no pain/no interference and 10 being pain as bad as you can imagine/pain that completely interferes with daily life.
The overall median pain severity and pain interference were 3.0 (range, 1.3-4.8) and 2.9 (range, 0.7-5.2), respectively. The median worst pain was 6.0, least pain 2.0, average pain 3.0, and current pain 2.0. Ankles were the most frequently reported site of pain.
When completing the International Physical Activity Questionnaire, 49.3% of patients (73/148) reported no activity in the prior week.
The median SF-36v2 scores were lower for physical health domains than mental health domains, and the overall median health score was 3.0 (range, 2.0-3.0).
The median score on the Hemophilia Activities List was 76.1 (range, 59.2-95.1). And patients said hemophilia had a greater impact on their lower extremities than upper extremities.
Dr Recht and his colleagues said these results substantiate the high prevalence of pain in adults with hemophilia. And the study highlights opportunities to improve the assessment and management of pain in these patients.
Study investigators have received funding/consulting fees from—or are employees/shareholders of—Novo Nordisk, Baxter, Biogen, Bayer, OctaPharma, Pfizer, CSL Behring, Kendrion, Alexion, Grifols, OPKO Health, Sanofi, Merck, and ProMeticLife Sciences. ![]()
Extended-interval dosing appears safe, effective

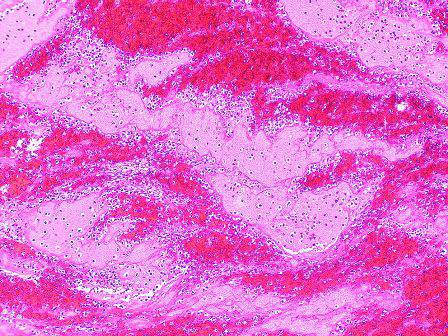
Photo courtesy of Biogen
TORONTO—Full results of a phase 3 study support extended-interval dosing with a recombinant factor IX Fc fusion protein (rFIXFc) over FIX products with a standard half-life, according to a speaker at the 2015 ISTH Congress.
Kathelijn Fischer, MD, PhD, of the University Medical Center Utrecht in The Netherlands, reported results with rFIXFc (also known as eftrenonacog alfa and Alprolix), in children with severe hemophilia B who were enrolled on the KIDS B-LONG study.
rFIXFc was successful in preventing and treating bleeding episodes in these patients. Furthermore, the patients did not develop inhibitors, and there were no serious adverse events related to treatment.
Dr Fischer presented these results as abstract LB009. Interim results of this study helped support the US approval of rFIXFc for use in children. The trial was sponsored by Sobi and Biogen, the companies developing rFIXFc.
KIDS B-LONG included 30 boys younger than 12 who had severe hemophilia B. The patients had at least 50 prior exposure days to FIX therapies and no history of inhibitors.
At baseline, all patients were receiving FIX prophylaxis. Seventy-seven percent of patients were receiving 2 or more doses a week.
On day 1 of the study, patients received rFIXFc at 50 IU/kg. They then received weekly prophylaxis at an initial dose of 50 IU/kg to 60 IU/kg. Doses were adjusted throughout the study, but the maximum was 100 IU/kg. The minimum dosing frequency was once a week, and the maximum was twice a week.
Twenty-seven patients (90%) completed the study. The median time spent on study was 49.4 weeks, and 24 patients (80%) received rFIXFc injections on at least 50 separate days.
Safety
None of the patients developed inhibitors or non-neutralizing anti-rFIXFc antibodies. There were no anaphylactic reactions, hypersensitivity reactions, thrombotic events, or deaths.
Adverse events occurred in 86.7% of patients. The most frequent were nanopharyngitis (23.3%) and falls (20%). Eleven serious adverse events occurred in 4 patients. None were considered related to treatment, and none led to study discontinuation.
One adverse event was considered related to rFIXFc. A 3-year-old child experienced decreased appetite.
Efficacy
The median annualized bleeding rate (ABR) was 2.0 overall, 1.1 in children under 6, and 2.1 in children ages 6 to 11.
For spontaneous bleeds, the median ABR was 0, both overall and in the 2 age groups. For joint bleeds, the median ABR was 0 overall and in the younger age group, but it was 1.1 for the older children.
Thirty-three percent of patients had no bleeding episodes while on study, and 63% had no joint bleeds.
Ninety-seven percent of patients receiving rFIXFc prophylaxis had no change in their dosing interval.
For patients under 6, the median prophylactic dose was 59.4 IU/kg/week (range, 53.0-64.8). For patients ages 6 to 11, the median dose was 57.8 IU/kg/week (range, 51.7-65.0)
When patients received rFIXFc to treat bleeding, 75% of bleeds were controlled with 1 infusion, and 91.7% were controlled with 1 or 2 infusions. The median dose per infusion was 63.5 IU/kg (range, 48.9-99.4).
Pharmacokinetics
The terminal half-life of rFIXFc was 66.5 hours for children under 6 and 70.3 hours for children ages 6 to 11. The clearance was 4.4 mL/hour/kg and 3.5 mL/hour/kg, respectively. The incremental recovery (IR) was 0.59 IU/dL per IU/kg and 0.72 IU/dL per IU/kg, respectively.
Compared to pre-study treatment with BeneFIX (recombinant FIX) at 50 IU/kg, rFIXFc at 50 IU/kg had a significantly longer half-life. In children younger than 6, the half-life was 66.5 hours for rFIXFc and 18.2 hours for BeneFIX (P<0.001). In children ages 6 to 11, the half-lives were 71.1 and 19.2 hours, respectively (P<0.001).
There was no significant difference between the treatments with regard to IR for children under 6. IR was 0.59 with rFIXFc and 0.52 with BeneFIX (P=0.109). However, there was a significant difference in IR for children ages 6 to 11—0.70 for rFIXFc and 0.54 for BeneFIX (P=0.003). ![]()

Photo courtesy of Biogen
TORONTO—Full results of a phase 3 study support extended-interval dosing with a recombinant factor IX Fc fusion protein (rFIXFc) over FIX products with a standard half-life, according to a speaker at the 2015 ISTH Congress.
Kathelijn Fischer, MD, PhD, of the University Medical Center Utrecht in The Netherlands, reported results with rFIXFc (also known as eftrenonacog alfa and Alprolix), in children with severe hemophilia B who were enrolled on the KIDS B-LONG study.
rFIXFc was successful in preventing and treating bleeding episodes in these patients. Furthermore, the patients did not develop inhibitors, and there were no serious adverse events related to treatment.
Dr Fischer presented these results as abstract LB009. Interim results of this study helped support the US approval of rFIXFc for use in children. The trial was sponsored by Sobi and Biogen, the companies developing rFIXFc.
KIDS B-LONG included 30 boys younger than 12 who had severe hemophilia B. The patients had at least 50 prior exposure days to FIX therapies and no history of inhibitors.
At baseline, all patients were receiving FIX prophylaxis. Seventy-seven percent of patients were receiving 2 or more doses a week.
On day 1 of the study, patients received rFIXFc at 50 IU/kg. They then received weekly prophylaxis at an initial dose of 50 IU/kg to 60 IU/kg. Doses were adjusted throughout the study, but the maximum was 100 IU/kg. The minimum dosing frequency was once a week, and the maximum was twice a week.
Twenty-seven patients (90%) completed the study. The median time spent on study was 49.4 weeks, and 24 patients (80%) received rFIXFc injections on at least 50 separate days.
Safety
None of the patients developed inhibitors or non-neutralizing anti-rFIXFc antibodies. There were no anaphylactic reactions, hypersensitivity reactions, thrombotic events, or deaths.
Adverse events occurred in 86.7% of patients. The most frequent were nanopharyngitis (23.3%) and falls (20%). Eleven serious adverse events occurred in 4 patients. None were considered related to treatment, and none led to study discontinuation.
One adverse event was considered related to rFIXFc. A 3-year-old child experienced decreased appetite.
Efficacy
The median annualized bleeding rate (ABR) was 2.0 overall, 1.1 in children under 6, and 2.1 in children ages 6 to 11.
For spontaneous bleeds, the median ABR was 0, both overall and in the 2 age groups. For joint bleeds, the median ABR was 0 overall and in the younger age group, but it was 1.1 for the older children.
Thirty-three percent of patients had no bleeding episodes while on study, and 63% had no joint bleeds.
Ninety-seven percent of patients receiving rFIXFc prophylaxis had no change in their dosing interval.
For patients under 6, the median prophylactic dose was 59.4 IU/kg/week (range, 53.0-64.8). For patients ages 6 to 11, the median dose was 57.8 IU/kg/week (range, 51.7-65.0)
When patients received rFIXFc to treat bleeding, 75% of bleeds were controlled with 1 infusion, and 91.7% were controlled with 1 or 2 infusions. The median dose per infusion was 63.5 IU/kg (range, 48.9-99.4).
Pharmacokinetics
The terminal half-life of rFIXFc was 66.5 hours for children under 6 and 70.3 hours for children ages 6 to 11. The clearance was 4.4 mL/hour/kg and 3.5 mL/hour/kg, respectively. The incremental recovery (IR) was 0.59 IU/dL per IU/kg and 0.72 IU/dL per IU/kg, respectively.
Compared to pre-study treatment with BeneFIX (recombinant FIX) at 50 IU/kg, rFIXFc at 50 IU/kg had a significantly longer half-life. In children younger than 6, the half-life was 66.5 hours for rFIXFc and 18.2 hours for BeneFIX (P<0.001). In children ages 6 to 11, the half-lives were 71.1 and 19.2 hours, respectively (P<0.001).
There was no significant difference between the treatments with regard to IR for children under 6. IR was 0.59 with rFIXFc and 0.52 with BeneFIX (P=0.109). However, there was a significant difference in IR for children ages 6 to 11—0.70 for rFIXFc and 0.54 for BeneFIX (P=0.003). ![]()

Photo courtesy of Biogen
TORONTO—Full results of a phase 3 study support extended-interval dosing with a recombinant factor IX Fc fusion protein (rFIXFc) over FIX products with a standard half-life, according to a speaker at the 2015 ISTH Congress.
Kathelijn Fischer, MD, PhD, of the University Medical Center Utrecht in The Netherlands, reported results with rFIXFc (also known as eftrenonacog alfa and Alprolix), in children with severe hemophilia B who were enrolled on the KIDS B-LONG study.
rFIXFc was successful in preventing and treating bleeding episodes in these patients. Furthermore, the patients did not develop inhibitors, and there were no serious adverse events related to treatment.
Dr Fischer presented these results as abstract LB009. Interim results of this study helped support the US approval of rFIXFc for use in children. The trial was sponsored by Sobi and Biogen, the companies developing rFIXFc.
KIDS B-LONG included 30 boys younger than 12 who had severe hemophilia B. The patients had at least 50 prior exposure days to FIX therapies and no history of inhibitors.
At baseline, all patients were receiving FIX prophylaxis. Seventy-seven percent of patients were receiving 2 or more doses a week.
On day 1 of the study, patients received rFIXFc at 50 IU/kg. They then received weekly prophylaxis at an initial dose of 50 IU/kg to 60 IU/kg. Doses were adjusted throughout the study, but the maximum was 100 IU/kg. The minimum dosing frequency was once a week, and the maximum was twice a week.
Twenty-seven patients (90%) completed the study. The median time spent on study was 49.4 weeks, and 24 patients (80%) received rFIXFc injections on at least 50 separate days.
Safety
None of the patients developed inhibitors or non-neutralizing anti-rFIXFc antibodies. There were no anaphylactic reactions, hypersensitivity reactions, thrombotic events, or deaths.
Adverse events occurred in 86.7% of patients. The most frequent were nanopharyngitis (23.3%) and falls (20%). Eleven serious adverse events occurred in 4 patients. None were considered related to treatment, and none led to study discontinuation.
One adverse event was considered related to rFIXFc. A 3-year-old child experienced decreased appetite.
Efficacy
The median annualized bleeding rate (ABR) was 2.0 overall, 1.1 in children under 6, and 2.1 in children ages 6 to 11.
For spontaneous bleeds, the median ABR was 0, both overall and in the 2 age groups. For joint bleeds, the median ABR was 0 overall and in the younger age group, but it was 1.1 for the older children.
Thirty-three percent of patients had no bleeding episodes while on study, and 63% had no joint bleeds.
Ninety-seven percent of patients receiving rFIXFc prophylaxis had no change in their dosing interval.
For patients under 6, the median prophylactic dose was 59.4 IU/kg/week (range, 53.0-64.8). For patients ages 6 to 11, the median dose was 57.8 IU/kg/week (range, 51.7-65.0)
When patients received rFIXFc to treat bleeding, 75% of bleeds were controlled with 1 infusion, and 91.7% were controlled with 1 or 2 infusions. The median dose per infusion was 63.5 IU/kg (range, 48.9-99.4).
Pharmacokinetics
The terminal half-life of rFIXFc was 66.5 hours for children under 6 and 70.3 hours for children ages 6 to 11. The clearance was 4.4 mL/hour/kg and 3.5 mL/hour/kg, respectively. The incremental recovery (IR) was 0.59 IU/dL per IU/kg and 0.72 IU/dL per IU/kg, respectively.
Compared to pre-study treatment with BeneFIX (recombinant FIX) at 50 IU/kg, rFIXFc at 50 IU/kg had a significantly longer half-life. In children younger than 6, the half-life was 66.5 hours for rFIXFc and 18.2 hours for BeneFIX (P<0.001). In children ages 6 to 11, the half-lives were 71.1 and 19.2 hours, respectively (P<0.001).
There was no significant difference between the treatments with regard to IR for children under 6. IR was 0.59 with rFIXFc and 0.52 with BeneFIX (P=0.109). However, there was a significant difference in IR for children ages 6 to 11—0.70 for rFIXFc and 0.54 for BeneFIX (P=0.003). ![]()
Anticoagulant antidote effective in healthy volunteers

TORONTO—An antidote to factor Xa inhibitors can safely reverse the anticoagulant effect of apixaban in healthy volunteers, results of the ANNEXA-A study suggest.
The first part of this study showed that a bolus of the antidote, andexanet alfa, was effective. And none of the volunteers had serious adverse events, thrombotic events, or antibodies to factor X or Xa.
In the second part of the study, researchers tested a bolus and a 2-hour infusion of andexanet alfa.
The drug normalized coagulation parameters immediately post-bolus, and this effect was sustained during the infusion. The reversal of anti-factor Xa activity lasted 1 to 2 hours post-infusion.
As in part 1, there were no serious adverse events or thrombotic events, and none of the subjects developed antibodies to factor X or Xa.
Mark Crowther, MD, of McMaster University in Hamilton, Ontario, Canada, presented details on part 2 of ANNEXA-A at the ISTH 2015 Congress (abstract LB004). The trial was sponsored by Portola Pharmaceuticals, Inc., the company developing andexanet alfa.
The goal of the randomized, double-blind ANNEXA-A study was to evaluate the safety and efficacy of andexanet alfa in reversing apixaban-induced anticoagulation in healthy volunteers ages 50 to 75.
In part 1, 33 healthy volunteers received apixaban at 5 mg twice daily for 4 days and were then randomized in a 3:1 ratio to andexanet alfa administered as a 400 mg intravenous bolus (n=24) or to placebo (n=9). Results from this part of the study were presented at the American Heart Association 2014 Scientific Sessions.
In the second part of the study, 32 healthy volunteers received apixaban at 5 mg twice daily for 4 days and were then randomized in a 3:1 ratio to andexanet alfa administered as a 400 mg intravenous bolus followed by a continuous infusion of 4 mg/min for 120 minutes (n=24) or to placebo (n=8).
Safety
One subject in the andexanet alfa arm discontinued treatment during the infusion due to mild hives. The subject did not have any other allergic
manifestations or cardiorespiratory effects.
Six subjects had mild infusion-related reactions, 4 (16.7%) in the andexanet alfa arm and 2 (25%) in the placebo arm.
None of the subjects had an increase in D-dimer (more than 2 times the upper limit of normal) on more than 1 day.
The majority of andexanet-alfa-treated subjects had transient elevation of F1 and F2, but, in all cases, levels returned to less than or equal to 2 times the upper limit of normal by the fourth day.
Efficacy
Twenty-three subjects in the andexanet alfa arm and all 8 subjects in the placebo arm were evaluable for efficacy.
All evaluable subjects in the andexanet alfa arm had an 80% or greater reduction in anti-factor Xa activity post-infusion nadir, compared to none of the subjects on placebo (P<0.0001).
The mean percent change in anti-factor Xa activity from baseline to post-infusion nadir was 92% in the andexanet alfa arm (P<0.0001 vs placebo). And the mean percent change from baseline to post-bolus nadir was 93% (P<0.0001 vs placebo).
The mean change in free apixaban concentration from baseline to post-infusion nadir was 1.39 ng/mL in the andexanet alfa arm (P=0.0002 vs placebo).
Thrombin generation was restored to the day 1, pre-apixaban baseline range in all 23 subjects on andexanet alfa (P<0.0001). And there was no long-term effect on thrombin generation.
The researchers said andexanet alfa demonstrated rapid onset and offset of action. Furthermore, it seems that either a bolus dose alone or a bolus plus infusion can reverse apixaban’s anticoagulant activity, which could provide flexibility for bleeding patients.
Andexanet alfa is also under investigation as an antidote to rivaroxaban, edoxaban, enoxaparin, and betrixaban. ![]()

TORONTO—An antidote to factor Xa inhibitors can safely reverse the anticoagulant effect of apixaban in healthy volunteers, results of the ANNEXA-A study suggest.
The first part of this study showed that a bolus of the antidote, andexanet alfa, was effective. And none of the volunteers had serious adverse events, thrombotic events, or antibodies to factor X or Xa.
In the second part of the study, researchers tested a bolus and a 2-hour infusion of andexanet alfa.
The drug normalized coagulation parameters immediately post-bolus, and this effect was sustained during the infusion. The reversal of anti-factor Xa activity lasted 1 to 2 hours post-infusion.
As in part 1, there were no serious adverse events or thrombotic events, and none of the subjects developed antibodies to factor X or Xa.
Mark Crowther, MD, of McMaster University in Hamilton, Ontario, Canada, presented details on part 2 of ANNEXA-A at the ISTH 2015 Congress (abstract LB004). The trial was sponsored by Portola Pharmaceuticals, Inc., the company developing andexanet alfa.
The goal of the randomized, double-blind ANNEXA-A study was to evaluate the safety and efficacy of andexanet alfa in reversing apixaban-induced anticoagulation in healthy volunteers ages 50 to 75.
In part 1, 33 healthy volunteers received apixaban at 5 mg twice daily for 4 days and were then randomized in a 3:1 ratio to andexanet alfa administered as a 400 mg intravenous bolus (n=24) or to placebo (n=9). Results from this part of the study were presented at the American Heart Association 2014 Scientific Sessions.
In the second part of the study, 32 healthy volunteers received apixaban at 5 mg twice daily for 4 days and were then randomized in a 3:1 ratio to andexanet alfa administered as a 400 mg intravenous bolus followed by a continuous infusion of 4 mg/min for 120 minutes (n=24) or to placebo (n=8).
Safety
One subject in the andexanet alfa arm discontinued treatment during the infusion due to mild hives. The subject did not have any other allergic
manifestations or cardiorespiratory effects.
Six subjects had mild infusion-related reactions, 4 (16.7%) in the andexanet alfa arm and 2 (25%) in the placebo arm.
None of the subjects had an increase in D-dimer (more than 2 times the upper limit of normal) on more than 1 day.
The majority of andexanet-alfa-treated subjects had transient elevation of F1 and F2, but, in all cases, levels returned to less than or equal to 2 times the upper limit of normal by the fourth day.
Efficacy
Twenty-three subjects in the andexanet alfa arm and all 8 subjects in the placebo arm were evaluable for efficacy.
All evaluable subjects in the andexanet alfa arm had an 80% or greater reduction in anti-factor Xa activity post-infusion nadir, compared to none of the subjects on placebo (P<0.0001).
The mean percent change in anti-factor Xa activity from baseline to post-infusion nadir was 92% in the andexanet alfa arm (P<0.0001 vs placebo). And the mean percent change from baseline to post-bolus nadir was 93% (P<0.0001 vs placebo).
The mean change in free apixaban concentration from baseline to post-infusion nadir was 1.39 ng/mL in the andexanet alfa arm (P=0.0002 vs placebo).
Thrombin generation was restored to the day 1, pre-apixaban baseline range in all 23 subjects on andexanet alfa (P<0.0001). And there was no long-term effect on thrombin generation.
The researchers said andexanet alfa demonstrated rapid onset and offset of action. Furthermore, it seems that either a bolus dose alone or a bolus plus infusion can reverse apixaban’s anticoagulant activity, which could provide flexibility for bleeding patients.
Andexanet alfa is also under investigation as an antidote to rivaroxaban, edoxaban, enoxaparin, and betrixaban. ![]()

TORONTO—An antidote to factor Xa inhibitors can safely reverse the anticoagulant effect of apixaban in healthy volunteers, results of the ANNEXA-A study suggest.
The first part of this study showed that a bolus of the antidote, andexanet alfa, was effective. And none of the volunteers had serious adverse events, thrombotic events, or antibodies to factor X or Xa.
In the second part of the study, researchers tested a bolus and a 2-hour infusion of andexanet alfa.
The drug normalized coagulation parameters immediately post-bolus, and this effect was sustained during the infusion. The reversal of anti-factor Xa activity lasted 1 to 2 hours post-infusion.
As in part 1, there were no serious adverse events or thrombotic events, and none of the subjects developed antibodies to factor X or Xa.
Mark Crowther, MD, of McMaster University in Hamilton, Ontario, Canada, presented details on part 2 of ANNEXA-A at the ISTH 2015 Congress (abstract LB004). The trial was sponsored by Portola Pharmaceuticals, Inc., the company developing andexanet alfa.
The goal of the randomized, double-blind ANNEXA-A study was to evaluate the safety and efficacy of andexanet alfa in reversing apixaban-induced anticoagulation in healthy volunteers ages 50 to 75.
In part 1, 33 healthy volunteers received apixaban at 5 mg twice daily for 4 days and were then randomized in a 3:1 ratio to andexanet alfa administered as a 400 mg intravenous bolus (n=24) or to placebo (n=9). Results from this part of the study were presented at the American Heart Association 2014 Scientific Sessions.
In the second part of the study, 32 healthy volunteers received apixaban at 5 mg twice daily for 4 days and were then randomized in a 3:1 ratio to andexanet alfa administered as a 400 mg intravenous bolus followed by a continuous infusion of 4 mg/min for 120 minutes (n=24) or to placebo (n=8).
Safety
One subject in the andexanet alfa arm discontinued treatment during the infusion due to mild hives. The subject did not have any other allergic
manifestations or cardiorespiratory effects.
Six subjects had mild infusion-related reactions, 4 (16.7%) in the andexanet alfa arm and 2 (25%) in the placebo arm.
None of the subjects had an increase in D-dimer (more than 2 times the upper limit of normal) on more than 1 day.
The majority of andexanet-alfa-treated subjects had transient elevation of F1 and F2, but, in all cases, levels returned to less than or equal to 2 times the upper limit of normal by the fourth day.
Efficacy
Twenty-three subjects in the andexanet alfa arm and all 8 subjects in the placebo arm were evaluable for efficacy.
All evaluable subjects in the andexanet alfa arm had an 80% or greater reduction in anti-factor Xa activity post-infusion nadir, compared to none of the subjects on placebo (P<0.0001).
The mean percent change in anti-factor Xa activity from baseline to post-infusion nadir was 92% in the andexanet alfa arm (P<0.0001 vs placebo). And the mean percent change from baseline to post-bolus nadir was 93% (P<0.0001 vs placebo).
The mean change in free apixaban concentration from baseline to post-infusion nadir was 1.39 ng/mL in the andexanet alfa arm (P=0.0002 vs placebo).
Thrombin generation was restored to the day 1, pre-apixaban baseline range in all 23 subjects on andexanet alfa (P<0.0001). And there was no long-term effect on thrombin generation.
The researchers said andexanet alfa demonstrated rapid onset and offset of action. Furthermore, it seems that either a bolus dose alone or a bolus plus infusion can reverse apixaban’s anticoagulant activity, which could provide flexibility for bleeding patients.
Andexanet alfa is also under investigation as an antidote to rivaroxaban, edoxaban, enoxaparin, and betrixaban. ![]()
Long-term data support use of FVIII treatment

TORONTO—The antihemophilic factor turoctocog alfa is safe and effective long-term, according to interim data from the phase 3 guardian 2 trial.
With more than 4 years of safety data, researchers have found turoctocog alfa to be well-tolerated in patients with hemophilia A.
The median annualized bleeding rate for patients on prophylactic treatment was 1.56 bleeds per patient per year. For patients who received turoctocog alfa on demand, a single injection stopped all bleeds.
And none of the patients developed factor VIII (FVIII) inhibitors.
Margareth Ozelo, MD, PhD, of the University of Campinas in Sao Paulo, Brazil and her colleagues presented these data at the ISTH 2015 Congress (abstract PO251-WED). The research is sponsored by Novo Nordisk, the company developing turoctocog alfa (as NovoEight).
Turoctocog alfa is a B-domain truncated recombinant human coagulation FVIII product indicated for the treatment and prevention of bleeding in patients with hemophilia A. The ongoing guardian 2 trial is a prospective safety and efficacy extension trial of the guardian 1 and guardian 3 studies.
Two hundred patients received turoctocog alfa in guardian 2. They had severe hemophilia A (FVIII activity ≤ 1%), no history of inhibitors, and had completed guardian 1, guardian 3, or a third pharmacokinetics trial. The patients’ mean age at first turoctocog alfa injection was 22.3 ± 14.4 years.
In guardian 1 and guardian 3, all patients switched from other FVIII products to turoctocog alfa prophylaxis every second day (adults/adolescents, 20–40 IU/kg; children, 25–50 IU/kg), or 3 times weekly (adults/adolescents, 20–50 IU/kg; children 25–60 IU/kg). Patients also received turoctocog alfa when bleeds arose.
Of the 200 patients enrolled on guardian 2, 133 were still participating in the trial at the interim cutoff date, December 31, 2013.
The interim analysis includes data for 451.6 patient-years and 72,320 days of exposure to turoctocog alfa. The total number of exposure days was 364.5
(range, 1-762) per patient for prophylaxis and 23.8 (range, 1-90) per patient for on-demand treatment.
The mean number of turoctocog alfa doses was 368.3 (range, 1-766) per patient for prophylaxis and 24.2 (range, 1-90) per patient for on-demand treatment.
Safety results
At the interim cutoff, none of the patients had developed FVIII inhibitors. Adverse events occurred in 84% of patients (n=168). The most common were
headache, nasopharyngitis, upper respiratory tract infection, and arthralgia.
Eight adverse events were considered possibly or probably related to turoctocog alfa in 5 patients (2.5%). These events were mild or moderate and included local swelling (n=1), increased aspartate aminotransferase (n=1), increased alanine aminotransferase (n=1), pain in extremity (n=1), musculoskeletal pain (n=1), lichenoid keratosis (n=1), and arthropathy (n=2).
There were 29 serious adverse events that were considered unlikely to be treatment-related. This included a death from subdural hemorrhage.
Efficacy results
For patients on prophylactic treatment (n=197), the median annualized bleeding rate was 1.56 bleeds per patient per year for all bleeds. It was 0.50 for
spontaneous bleeds, 0.49 for traumatic bleeds, 0.93 for joint bleeds, and 0.35 for nonjoint bleeds.
The success rate for treating bleeds during prophylaxis was 89.4%, and 90% of all bleeding episodes were successfully treated with 1 or 2 infusions of
turoctocog alfa. As for on-demand treatment, a single injection stopped all 73 bleeds.
“These interim results provide an extension to the body of evidence supporting the long-term use of NovoEight,” Dr Ozelo said. “For people with hemophilia A, finding treatments that are effective at preventing bleeding episodes long-term is essential.” ![]()

TORONTO—The antihemophilic factor turoctocog alfa is safe and effective long-term, according to interim data from the phase 3 guardian 2 trial.
With more than 4 years of safety data, researchers have found turoctocog alfa to be well-tolerated in patients with hemophilia A.
The median annualized bleeding rate for patients on prophylactic treatment was 1.56 bleeds per patient per year. For patients who received turoctocog alfa on demand, a single injection stopped all bleeds.
And none of the patients developed factor VIII (FVIII) inhibitors.
Margareth Ozelo, MD, PhD, of the University of Campinas in Sao Paulo, Brazil and her colleagues presented these data at the ISTH 2015 Congress (abstract PO251-WED). The research is sponsored by Novo Nordisk, the company developing turoctocog alfa (as NovoEight).
Turoctocog alfa is a B-domain truncated recombinant human coagulation FVIII product indicated for the treatment and prevention of bleeding in patients with hemophilia A. The ongoing guardian 2 trial is a prospective safety and efficacy extension trial of the guardian 1 and guardian 3 studies.
Two hundred patients received turoctocog alfa in guardian 2. They had severe hemophilia A (FVIII activity ≤ 1%), no history of inhibitors, and had completed guardian 1, guardian 3, or a third pharmacokinetics trial. The patients’ mean age at first turoctocog alfa injection was 22.3 ± 14.4 years.
In guardian 1 and guardian 3, all patients switched from other FVIII products to turoctocog alfa prophylaxis every second day (adults/adolescents, 20–40 IU/kg; children, 25–50 IU/kg), or 3 times weekly (adults/adolescents, 20–50 IU/kg; children 25–60 IU/kg). Patients also received turoctocog alfa when bleeds arose.
Of the 200 patients enrolled on guardian 2, 133 were still participating in the trial at the interim cutoff date, December 31, 2013.
The interim analysis includes data for 451.6 patient-years and 72,320 days of exposure to turoctocog alfa. The total number of exposure days was 364.5
(range, 1-762) per patient for prophylaxis and 23.8 (range, 1-90) per patient for on-demand treatment.
The mean number of turoctocog alfa doses was 368.3 (range, 1-766) per patient for prophylaxis and 24.2 (range, 1-90) per patient for on-demand treatment.
Safety results
At the interim cutoff, none of the patients had developed FVIII inhibitors. Adverse events occurred in 84% of patients (n=168). The most common were
headache, nasopharyngitis, upper respiratory tract infection, and arthralgia.
Eight adverse events were considered possibly or probably related to turoctocog alfa in 5 patients (2.5%). These events were mild or moderate and included local swelling (n=1), increased aspartate aminotransferase (n=1), increased alanine aminotransferase (n=1), pain in extremity (n=1), musculoskeletal pain (n=1), lichenoid keratosis (n=1), and arthropathy (n=2).
There were 29 serious adverse events that were considered unlikely to be treatment-related. This included a death from subdural hemorrhage.
Efficacy results
For patients on prophylactic treatment (n=197), the median annualized bleeding rate was 1.56 bleeds per patient per year for all bleeds. It was 0.50 for
spontaneous bleeds, 0.49 for traumatic bleeds, 0.93 for joint bleeds, and 0.35 for nonjoint bleeds.
The success rate for treating bleeds during prophylaxis was 89.4%, and 90% of all bleeding episodes were successfully treated with 1 or 2 infusions of
turoctocog alfa. As for on-demand treatment, a single injection stopped all 73 bleeds.
“These interim results provide an extension to the body of evidence supporting the long-term use of NovoEight,” Dr Ozelo said. “For people with hemophilia A, finding treatments that are effective at preventing bleeding episodes long-term is essential.” ![]()

TORONTO—The antihemophilic factor turoctocog alfa is safe and effective long-term, according to interim data from the phase 3 guardian 2 trial.
With more than 4 years of safety data, researchers have found turoctocog alfa to be well-tolerated in patients with hemophilia A.
The median annualized bleeding rate for patients on prophylactic treatment was 1.56 bleeds per patient per year. For patients who received turoctocog alfa on demand, a single injection stopped all bleeds.
And none of the patients developed factor VIII (FVIII) inhibitors.
Margareth Ozelo, MD, PhD, of the University of Campinas in Sao Paulo, Brazil and her colleagues presented these data at the ISTH 2015 Congress (abstract PO251-WED). The research is sponsored by Novo Nordisk, the company developing turoctocog alfa (as NovoEight).
Turoctocog alfa is a B-domain truncated recombinant human coagulation FVIII product indicated for the treatment and prevention of bleeding in patients with hemophilia A. The ongoing guardian 2 trial is a prospective safety and efficacy extension trial of the guardian 1 and guardian 3 studies.
Two hundred patients received turoctocog alfa in guardian 2. They had severe hemophilia A (FVIII activity ≤ 1%), no history of inhibitors, and had completed guardian 1, guardian 3, or a third pharmacokinetics trial. The patients’ mean age at first turoctocog alfa injection was 22.3 ± 14.4 years.
In guardian 1 and guardian 3, all patients switched from other FVIII products to turoctocog alfa prophylaxis every second day (adults/adolescents, 20–40 IU/kg; children, 25–50 IU/kg), or 3 times weekly (adults/adolescents, 20–50 IU/kg; children 25–60 IU/kg). Patients also received turoctocog alfa when bleeds arose.
Of the 200 patients enrolled on guardian 2, 133 were still participating in the trial at the interim cutoff date, December 31, 2013.
The interim analysis includes data for 451.6 patient-years and 72,320 days of exposure to turoctocog alfa. The total number of exposure days was 364.5
(range, 1-762) per patient for prophylaxis and 23.8 (range, 1-90) per patient for on-demand treatment.
The mean number of turoctocog alfa doses was 368.3 (range, 1-766) per patient for prophylaxis and 24.2 (range, 1-90) per patient for on-demand treatment.
Safety results
At the interim cutoff, none of the patients had developed FVIII inhibitors. Adverse events occurred in 84% of patients (n=168). The most common were
headache, nasopharyngitis, upper respiratory tract infection, and arthralgia.
Eight adverse events were considered possibly or probably related to turoctocog alfa in 5 patients (2.5%). These events were mild or moderate and included local swelling (n=1), increased aspartate aminotransferase (n=1), increased alanine aminotransferase (n=1), pain in extremity (n=1), musculoskeletal pain (n=1), lichenoid keratosis (n=1), and arthropathy (n=2).
There were 29 serious adverse events that were considered unlikely to be treatment-related. This included a death from subdural hemorrhage.
Efficacy results
For patients on prophylactic treatment (n=197), the median annualized bleeding rate was 1.56 bleeds per patient per year for all bleeds. It was 0.50 for
spontaneous bleeds, 0.49 for traumatic bleeds, 0.93 for joint bleeds, and 0.35 for nonjoint bleeds.
The success rate for treating bleeds during prophylaxis was 89.4%, and 90% of all bleeding episodes were successfully treated with 1 or 2 infusions of
turoctocog alfa. As for on-demand treatment, a single injection stopped all 73 bleeds.
“These interim results provide an extension to the body of evidence supporting the long-term use of NovoEight,” Dr Ozelo said. “For people with hemophilia A, finding treatments that are effective at preventing bleeding episodes long-term is essential.” ![]()
Earlier start to plasma transfusions for persistent postpartum hemorrhage does not improve maternal outcomes
TORONTO – For women with persistent postpartum hemorrhage, correction of coagulopathy by administering plasma is often an inevitable treatment decision. There are little clinical data, however, on whether an early or a late start for plasma transfusion leads to more positive maternal outcomes.
Data presented on Wednesday at the ISTH 2015 Congress by Dr. Dacia Henriquez of the department of obstetrics and gynecology at Leiden (the Netherlands) University Medical Center, may help answer that question.
“Our findings do not support the notion that plasma transfusion within 60 minutes after diagnosing persistent postpartum hemorrhage contributes to the reduction of the risk of adverse maternal outcomes,” Dr. Henriquez said in an interview.
The TeMpOh-1 (Transfusion Strategies in Women with Major Obstetric Hemorrhage) study included 1,217 women with postpartum hemorrhage (PPH) that was refractory to first-line obstetric interventions. The women were treated at 61 Dutch hospitals in 2011 and 2012.
“With this selection, our study results can be easily translated to daily clinical practice because of this clearly identifiable turning-point in treatment,” she said.
All women included in the study received either at least four units of red blood cells or a multicomponent transfusion within 24 hours after delivery (≥ 1000 mL). Median bleeding rate at baseline was 1.1 L at 1 hour, and median total blood loss was 3.0 L. Marginal structural models with inverse probability of treatment weighting were constructed to quantify the difference in maternal outcomes – including arterial embolism, hysterectomy, and maternal mortality – between an early (within 60 minutes) and a late (after 60 minutes) start of plasma transfusion (163 women vs. 1,054 women, respectively).
After adjustment for baseline parameters, bleeding severity, and changes over time, no significant differences were seen between the groups (odds ratios, 1.1 and 0.8, respectively).
“It seemed that after adjustment for patient and bleeding characteristics, plasma transfusion within 60 minutes after diagnosis of persistent PPH was not associated with a reduction in adverse maternal outcomes,” she said, noting that analyses are ongoing, and efforts are underway to determine whether time-dependent confounding was handled properly in the study.
Plans are also in place to perform subgroup analyses to assess whether treatment effect will differ between those with the most severe bleeding and those with initially milder hemorrhage, she said.
“With the TeMpOH-1 data, we were also able to demonstrate that dilutional coagulopathy due to volume resuscitation with crystalloids and colloids was associated with greater total blood loss and more adverse maternal outcomes when the clear fluids volume exceeded 4 L,” Dr. Henriquez said.
“A treatment strategy aiming at prevention rather than correction of coagulopathy in women with persistent PPH in daily clinical practice seems justified, because correction of coagulopathy by administering plasma appears to be of limited value in reducing adverse maternal outcomes,” Dr. Henriquez said.
Dr. Henriquez declared no disclosures.
TORONTO – For women with persistent postpartum hemorrhage, correction of coagulopathy by administering plasma is often an inevitable treatment decision. There are little clinical data, however, on whether an early or a late start for plasma transfusion leads to more positive maternal outcomes.
Data presented on Wednesday at the ISTH 2015 Congress by Dr. Dacia Henriquez of the department of obstetrics and gynecology at Leiden (the Netherlands) University Medical Center, may help answer that question.
“Our findings do not support the notion that plasma transfusion within 60 minutes after diagnosing persistent postpartum hemorrhage contributes to the reduction of the risk of adverse maternal outcomes,” Dr. Henriquez said in an interview.
The TeMpOh-1 (Transfusion Strategies in Women with Major Obstetric Hemorrhage) study included 1,217 women with postpartum hemorrhage (PPH) that was refractory to first-line obstetric interventions. The women were treated at 61 Dutch hospitals in 2011 and 2012.
“With this selection, our study results can be easily translated to daily clinical practice because of this clearly identifiable turning-point in treatment,” she said.
All women included in the study received either at least four units of red blood cells or a multicomponent transfusion within 24 hours after delivery (≥ 1000 mL). Median bleeding rate at baseline was 1.1 L at 1 hour, and median total blood loss was 3.0 L. Marginal structural models with inverse probability of treatment weighting were constructed to quantify the difference in maternal outcomes – including arterial embolism, hysterectomy, and maternal mortality – between an early (within 60 minutes) and a late (after 60 minutes) start of plasma transfusion (163 women vs. 1,054 women, respectively).
After adjustment for baseline parameters, bleeding severity, and changes over time, no significant differences were seen between the groups (odds ratios, 1.1 and 0.8, respectively).
“It seemed that after adjustment for patient and bleeding characteristics, plasma transfusion within 60 minutes after diagnosis of persistent PPH was not associated with a reduction in adverse maternal outcomes,” she said, noting that analyses are ongoing, and efforts are underway to determine whether time-dependent confounding was handled properly in the study.
Plans are also in place to perform subgroup analyses to assess whether treatment effect will differ between those with the most severe bleeding and those with initially milder hemorrhage, she said.
“With the TeMpOH-1 data, we were also able to demonstrate that dilutional coagulopathy due to volume resuscitation with crystalloids and colloids was associated with greater total blood loss and more adverse maternal outcomes when the clear fluids volume exceeded 4 L,” Dr. Henriquez said.
“A treatment strategy aiming at prevention rather than correction of coagulopathy in women with persistent PPH in daily clinical practice seems justified, because correction of coagulopathy by administering plasma appears to be of limited value in reducing adverse maternal outcomes,” Dr. Henriquez said.
Dr. Henriquez declared no disclosures.
TORONTO – For women with persistent postpartum hemorrhage, correction of coagulopathy by administering plasma is often an inevitable treatment decision. There are little clinical data, however, on whether an early or a late start for plasma transfusion leads to more positive maternal outcomes.
Data presented on Wednesday at the ISTH 2015 Congress by Dr. Dacia Henriquez of the department of obstetrics and gynecology at Leiden (the Netherlands) University Medical Center, may help answer that question.
“Our findings do not support the notion that plasma transfusion within 60 minutes after diagnosing persistent postpartum hemorrhage contributes to the reduction of the risk of adverse maternal outcomes,” Dr. Henriquez said in an interview.
The TeMpOh-1 (Transfusion Strategies in Women with Major Obstetric Hemorrhage) study included 1,217 women with postpartum hemorrhage (PPH) that was refractory to first-line obstetric interventions. The women were treated at 61 Dutch hospitals in 2011 and 2012.
“With this selection, our study results can be easily translated to daily clinical practice because of this clearly identifiable turning-point in treatment,” she said.
All women included in the study received either at least four units of red blood cells or a multicomponent transfusion within 24 hours after delivery (≥ 1000 mL). Median bleeding rate at baseline was 1.1 L at 1 hour, and median total blood loss was 3.0 L. Marginal structural models with inverse probability of treatment weighting were constructed to quantify the difference in maternal outcomes – including arterial embolism, hysterectomy, and maternal mortality – between an early (within 60 minutes) and a late (after 60 minutes) start of plasma transfusion (163 women vs. 1,054 women, respectively).
After adjustment for baseline parameters, bleeding severity, and changes over time, no significant differences were seen between the groups (odds ratios, 1.1 and 0.8, respectively).
“It seemed that after adjustment for patient and bleeding characteristics, plasma transfusion within 60 minutes after diagnosis of persistent PPH was not associated with a reduction in adverse maternal outcomes,” she said, noting that analyses are ongoing, and efforts are underway to determine whether time-dependent confounding was handled properly in the study.
Plans are also in place to perform subgroup analyses to assess whether treatment effect will differ between those with the most severe bleeding and those with initially milder hemorrhage, she said.
“With the TeMpOH-1 data, we were also able to demonstrate that dilutional coagulopathy due to volume resuscitation with crystalloids and colloids was associated with greater total blood loss and more adverse maternal outcomes when the clear fluids volume exceeded 4 L,” Dr. Henriquez said.
“A treatment strategy aiming at prevention rather than correction of coagulopathy in women with persistent PPH in daily clinical practice seems justified, because correction of coagulopathy by administering plasma appears to be of limited value in reducing adverse maternal outcomes,” Dr. Henriquez said.
Dr. Henriquez declared no disclosures.
AT 2015 ISTH
Key clinical point: Plasma transfusion within 60 minutes after diagnosis of persistent PPH was not associated with a reduction in adverse maternal outcomes.
Major finding: No significant differences were seen in maternal outcomes (ncluding arterial embolism, hysterectomy and maternal mortality) between the patients treated with plasma transfusions early (within 60 minutes) and late (after 60 minutes) (odds ratios, 1.1 and 0.8, respectively).
Data source: 1,217 women with postpartum hemorrhage (PPH) that was refractory to first-line obstetric interventions I.
Disclosures: Dr. Henriquez declared no disclosures.