User login
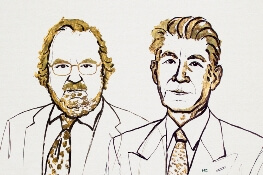
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”