User login
Inspired by the ABIM Foundation’s Choosing Wisel y ® campaign, the “Things We Do for No Reason ™ ” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
The hospitalist admits an 18-year-old man for newly diagnosed granulomatosis with polyangiitis to receive expedited pulse-dose steroids and plasma exchange. After consulting interventional radiology for catheter placement the following day, the hospitalist places a “strict” nil per os (nothing by mouth, NPO) after midnight order. During rounds the following morning, the patient reports that he wants to eat. At 9
BACKGROUND
Hospitalists commonly order “NPO after midnight” diets in anticipation of procedures requiring sedation or general anesthesia. Typically, NPO refers to no food or drink, but in some instances, NPO includes no oral medications. Up to half of medical patients experience some time of fasting while hospitalized.1 However, NPO practices vary widely across institutions.2,3 A study from 2014 notes that, on average, patients fast preprocedure for approximately 13.5 hours for solids and 9.6 hours for liquids.2 Prolonged fasting times offer little benefit to patients and may lead to frequent patient dissatisfaction and complaints.
WHY YOU MIGHT THINK THAT MAKING PATIENTS NPO AFTER MIDNIGHT IS APPROPRIATE
In 1883, Sir Joseph Lister described 19th century NPO practices distinguishing solids from liquids, allowing patients “tea or beef tea” until 2 to 3 hours prior to surgery.4 However, in 1946, Mendelson published an influential account of 66 pregnant women who aspirated during delivery under general anesthesia.5 Two of the 66 patients, both of whom had eaten a full meal 6 to 8 hours prior to general anesthesia, died. The study not only increased awareness of the risk of aspiration with general anesthesia in pregnancy, but it influenced the care for the nonpregnant population of patients as well. By the 1960s, anesthesia texts recommended “NPO after midnight” for both liquids and solids in all patients, regardless of pregnancy status.4 To minimize the risk to patients, we have continued to pass down the practice of NPO after midnight to subsequent generations.
Additionally, medical centers and hospitals feel pressure to provide efficient, patient-centered, high-value care. Given the complexity of procedural scheduling and the penalties associated with delays, keeping patients NPO ensures their availability for the next open procedural slot. NPO after midnight orders aim to prevent potential delays in treatment that occur when inadvertent ingestion of food and drink leads to cancellation of procedures.
WHY THE INDISCRIMINATE USE OF NPO AFTER MIDNIGHT IS UNNECESSARY
Recent studies have led to a more sophisticated understanding of gastric emptying and the risks of aspiration during sedation and intubation. Gastric emptying studies routinely show that transit of clear liquids out of the stomach is virtually complete within two hours of drinking.6 Age, body mass index, and alcohol have no effect on gastric emptying time, and almost all patients return to preingestion gastric residual volumes within 2 hours of clear liquid consumption.6,7 While morbidly obese patients tend to have higher gastric fluid volumes after 9 hours of fasting, their stomachs empty at rates similar to nonobese individuals.6 Note that, regardless of fasting times, morbid obesity predisposes patients to a higher overall gastric volume and lower pH of gastric contents, which may increase risk of aspiration.8 A Cochrane review found no statistical difference in gastric volumes or stomach pH in patients on a standard fast vs shortened (<180 minutes) liquid fast.9 The review included nine studies that found patients who consumed a clear liquid beverage had reduced gastric volumes, compared with patients in a fasting state (P < .001).9
In a pediatric retrospective study of pulmonary aspiration events, the researchers demonstrated that clinically significant aspiration (presence of bilious secretions in the tracheobronchial airways) occurred at a rate of 0.04% with emergency surgery.10 Bowel obstruction or ileus accounted for approximately 54% of those cases. Importantly, the reported aspiration rate approximates the rate of pregnant patients from the 1946 Mendelson study of 0.14% (66 out of 44,016), which originally prompted the use of the prolonged NPO status. Based on the Cochrane review of perioperative fasting recommendations for those older than 18 years, consuming fluids more than 90 minutes preoperatively confers a negligible (0 adverse events reported in 9 studies) risk for aspiration or regurgitation events.9
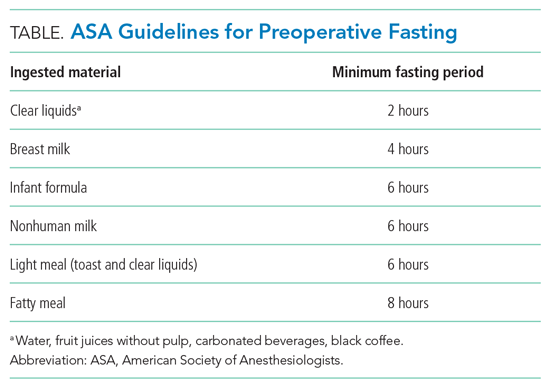
In 1998, as a result of these and other similar studies, the American Society of Anesthesiologists (ASA) along with global anesthesia partners adopted guidelines that allowed clear liquids up until 2 hours prior to anesthesia or sedation in low-aspiration-risk patients undergoing elective cases.11 The guidelines allowed for other beverages and food based on their standard transit times (Table). The ASA guidelines do not define low-aspiration-risk patients. Anesthesiologists generally exclude from the low-risk category patients who may have delayed gastric emptying from medical or iatrogenic causes. The updated 2017 ASA guidelines remain unchanged regarding fasting guidelines.12 Studies suggest that approximately 10% to 20% of NPO after midnight orders are avoidable.1,3 For those instances, procedures are often deemed not necessary or do not require NPO status.1
In a study evaluating the reasons that necessary procedures are canceled, only 0.5% of inpatient procedures are cancelled due to the inappropriate ingestion of food or drink.3 In addition, NPO status creates risk. Patients with prolonged NPO status report greater hunger, thirst, tiredness, and weakness prior to surgery when compared with patients receiving a carbohydrate-rich drink 2 hours prior to procedures.9,13,14 In fact, multiple studies have suggested that preoperative carbohydrate-rich drinks 2 hours before surgery can be associated with decreased insulin resistance in the perioperative period, decreased length of stay, and improvement in perioperative metabolic, cardiac, and psychosomatic status.9,13-15 These types of studies have informed the enhanced recovery after surgery program, which recommends a carbohydrate beverage 2 to 3 hours prior to surgery.
WHEN TO ORDER LONGER PREPROCEDURAL NPO TIMES
Prescribe the minimum recommended fasting times only for low-aspiration-risk patients undergoing elective procedures. Risk for regurgitation or aspiration increases for patients with conditions resulting in decreased gastric emptying, gastric or bowel obstruction, or lower esophageal sphincter incompetence. Those patients may require longer NPO time periods.8 Higher-risk diagnoses and clinical conditions include gastroparesis, trauma, and pregnancy.5,8,16 Specific risk factors for aspiration in children may include trauma, bowel obstruction, depressed consciousness, shock, or ileus.10 For surgical emergencies, balance the risk of surgical delay vs perceived aspiration risk.
WHAT WE SHOULD DO INSTEAD OF ROUTINELY ORDERING NPO AFTER MIDNIGHT
Use evidence-based guidelines to assess periprocedural aspiration risk. The ASA guidelines suggest that healthy, nonpregnant patients should fast for 8 hours after heavy meals, 6 hours after a light, nonfatty meal, and 2 hours after clear liquids (eg, water, fruit juices without pulp, carbonated beverages, black coffee).12 Focus on the type of food or drink rather than the volume ingested.12 Additionally, patients should ingest, with small amounts of clear fluids, appropriate home medications for acute and chronic conditions regardless of NPO status.
While procedure delays or cancellations for any reason upset patients and families and can disrupt the flow of the operating room and procedural suite, we can achieve the delicate balance between efficiency and patient safety and comfort. Since complex inpatient procedural scheduling may not allow for liberalization of solids requiring 6 to 8 hours of fasting time, focus on liberalizing liquids 2 hours prior to anesthesia. This allows staff to minimize the time low-risk patients fast while still maintaining flexibility for operating room case scheduling. We must promote communication between operating room and floor staff to anticipate timing of procedures each day. Healthcare facilities should aim to achieve time-based preprocedural NPO status as opposed to an arbitrary starting time like midnight.4
RECOMMENDATIONS
- Risk stratify patients for anesthesia-related aspiration with the aim of identifying those at low aspiration risk.
- For low-risk patients, adhere to recommended fasting times: 2 hours for a clear carbohydrate beverage, 4 hours for breast milk, 6 hours for a light meal or formula, and 8 hours for a fatty meal.
- For patients not deemed low risk, determine the appropriate length of preprocedural fasting by consulting with the anesthesia and surgical teams.
CONCLUSION
NPO after midnight represents a low-value and arbitrary practice that leaves patients fasting longer than necessary.2,3,12 In addition to the 2017 ASA guidelines, newer studies and protocols are improving patient satisfaction, minimizing patient dehydration and electrolyte disturbances, and incorporating enhanced recovery after surgery factors into a better patient experience. Returning to the clinical scenario, the hospitalist team can increase patient satisfaction by focusing on liberalizing clear fluids with a carbohydrate beverage up to 2 hours prior to elective surgery while still allowing for schedule flexibility. For this patient, a 3
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
Disclaimer: The opinions expressed in this article are those of the authors alone and do not reflect the views of the Department of Veterans Affairs. The Veterans Affairs Quality Scholars Program is supported by the Veterans Affairs Office of Academic Affiliations, Washington, DC.
1. Sorita A, Thongprayoon C, Ahmed A, et al. Frequency and appropriateness of fasting orders in the hospital. Mayo Clin Proc. 2015;90(9):1225-1232. https://doi.org/10.1016/j.mayocp.2015.07.013
2. Falconer R, Skouras C, Carter T, Greenway L, Paisley AM. Preoperative fasting: current practice and areas for improvement. Updates Surg. 2014;66(1):31-39. https://doi.org/10.1007/s13304-013-0242-z
3. Sorita A, Thongprayoon C, Ratelle JT, et al. Characteristics and outcomes of fasting orders among medical inpatients. J Hosp Med. 2017;12(1):36-39. https://doi.org/10.1002/jhm.2674
4. Maltby JR. Fasting from midnight–the history behind the dogma. Best Pract Res Clin Anaesthesiol. 2006;20(3):363-378. https://doi.org/10.1016/j.bpa.2006.02.001
5. Mendelson CL. The aspiration of stomach contents into the lungs during obstetric anesthesia. Am J Obstet Gynecol. 1946;52:191-205. https://doi.org/10.1016/s0002-9378(16)39829-5
6. Shiraishi T, Kurosaki D, Nakamura M, et al. Gastric fluid volume change after oral rehydration solution intake in morbidly obese and normal controls: a magnetic resonance imaging-based analysis. Anesth Analg. 2017;124(4):1174-1178. https://doi.org/10.1213/ane.0000000000001886
7. Vasavid P, Chaiwatanarat T, Pusuwan P, et al. Normal solid gastric emptying values measured by scintigraphy using Asian-style meal: a multicenter study in healthy volunteers. J Neurogastroenterol Motil. 2014;20(3):371-378. https://doi.org/10.5056/jnm13114
8. Mahajan V, Hashmi J, Singh R, Samra T, Aneja S. Comparative evaluation of gastric pH and volume in morbidly obese and lean patients undergoing elective surgery and effect of aspiration prophylaxis. J Clin Anesth. 2015;27(5):396-400. https://doi.org/10.1016/j.jclinane.2015.03.004
9. Brady MC, Kinn S, Stuart P, Ness V. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev. 2003;(4):CD004423. https://doi.org/10.1002/14651858.cd004423
10. Warner MA, Warner ME, Warner DO, Warner LO, Warner EJ. Perioperative pulmonary aspiration in infants and children. Anesthesiology. 1999;90(1):66-71. https://doi.org/10.1097/00000542-199901000-00011
11. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: a report by the American Society of Anesthesiologist Task Force on Preoperative Fasting. Anesthesiology. 1999;90(3):896-905. https://doi.org/10.1097/00000542-199903000-00034
12. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists task force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126(3):376-393. https://doi.org/10.1097/aln.0000000000001452
13. Hausel J, Nygren J, Lagerkranser M, et al. A carbohydrate-rich drink reduces preoperative discomfort in elective surgery patients. Anesth Analg. 2001;93(5):1344-1350. https://doi.org/10.1097/00000539-200111000-00063
14. Awad S, Varadhan KK, Ljungqvist O, Lobo DN. A meta-analysis of randomised controlled trials on preoperative oral carbohydrate treatment in elective surgery. Clin Nutr. 2013;32(1):34-44. https://doi.org/10.1016/j.clnu.2012.10.011
15. Kaška M, Grosmanová T, Havel E, et al. The impact and safety of preoperative oral or intravenous carbohydrate administration versus fasting in colorectal surgery–a randomized controlled trial. Wien Klin Wochenschr. 2010;122(1-2):23-30. https://doi.org/10.1007/s00508-009-1291-7
16. Tokumine J, Sugahara K, Fuchigami T, Teruya K, Nitta K, Satou K. Unanticipated full stomach at anesthesia induction in a type I diabetic patient with asymptomatic gastroparesis. J Anesth. 2005;19(3):247-248. https://doi.org/10.1007/s00540-005-0321-5
Inspired by the ABIM Foundation’s Choosing Wisel y ® campaign, the “Things We Do for No Reason ™ ” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
The hospitalist admits an 18-year-old man for newly diagnosed granulomatosis with polyangiitis to receive expedited pulse-dose steroids and plasma exchange. After consulting interventional radiology for catheter placement the following day, the hospitalist places a “strict” nil per os (nothing by mouth, NPO) after midnight order. During rounds the following morning, the patient reports that he wants to eat. At 9
BACKGROUND
Hospitalists commonly order “NPO after midnight” diets in anticipation of procedures requiring sedation or general anesthesia. Typically, NPO refers to no food or drink, but in some instances, NPO includes no oral medications. Up to half of medical patients experience some time of fasting while hospitalized.1 However, NPO practices vary widely across institutions.2,3 A study from 2014 notes that, on average, patients fast preprocedure for approximately 13.5 hours for solids and 9.6 hours for liquids.2 Prolonged fasting times offer little benefit to patients and may lead to frequent patient dissatisfaction and complaints.
WHY YOU MIGHT THINK THAT MAKING PATIENTS NPO AFTER MIDNIGHT IS APPROPRIATE
In 1883, Sir Joseph Lister described 19th century NPO practices distinguishing solids from liquids, allowing patients “tea or beef tea” until 2 to 3 hours prior to surgery.4 However, in 1946, Mendelson published an influential account of 66 pregnant women who aspirated during delivery under general anesthesia.5 Two of the 66 patients, both of whom had eaten a full meal 6 to 8 hours prior to general anesthesia, died. The study not only increased awareness of the risk of aspiration with general anesthesia in pregnancy, but it influenced the care for the nonpregnant population of patients as well. By the 1960s, anesthesia texts recommended “NPO after midnight” for both liquids and solids in all patients, regardless of pregnancy status.4 To minimize the risk to patients, we have continued to pass down the practice of NPO after midnight to subsequent generations.
Additionally, medical centers and hospitals feel pressure to provide efficient, patient-centered, high-value care. Given the complexity of procedural scheduling and the penalties associated with delays, keeping patients NPO ensures their availability for the next open procedural slot. NPO after midnight orders aim to prevent potential delays in treatment that occur when inadvertent ingestion of food and drink leads to cancellation of procedures.
WHY THE INDISCRIMINATE USE OF NPO AFTER MIDNIGHT IS UNNECESSARY
Recent studies have led to a more sophisticated understanding of gastric emptying and the risks of aspiration during sedation and intubation. Gastric emptying studies routinely show that transit of clear liquids out of the stomach is virtually complete within two hours of drinking.6 Age, body mass index, and alcohol have no effect on gastric emptying time, and almost all patients return to preingestion gastric residual volumes within 2 hours of clear liquid consumption.6,7 While morbidly obese patients tend to have higher gastric fluid volumes after 9 hours of fasting, their stomachs empty at rates similar to nonobese individuals.6 Note that, regardless of fasting times, morbid obesity predisposes patients to a higher overall gastric volume and lower pH of gastric contents, which may increase risk of aspiration.8 A Cochrane review found no statistical difference in gastric volumes or stomach pH in patients on a standard fast vs shortened (<180 minutes) liquid fast.9 The review included nine studies that found patients who consumed a clear liquid beverage had reduced gastric volumes, compared with patients in a fasting state (P < .001).9
In a pediatric retrospective study of pulmonary aspiration events, the researchers demonstrated that clinically significant aspiration (presence of bilious secretions in the tracheobronchial airways) occurred at a rate of 0.04% with emergency surgery.10 Bowel obstruction or ileus accounted for approximately 54% of those cases. Importantly, the reported aspiration rate approximates the rate of pregnant patients from the 1946 Mendelson study of 0.14% (66 out of 44,016), which originally prompted the use of the prolonged NPO status. Based on the Cochrane review of perioperative fasting recommendations for those older than 18 years, consuming fluids more than 90 minutes preoperatively confers a negligible (0 adverse events reported in 9 studies) risk for aspiration or regurgitation events.9
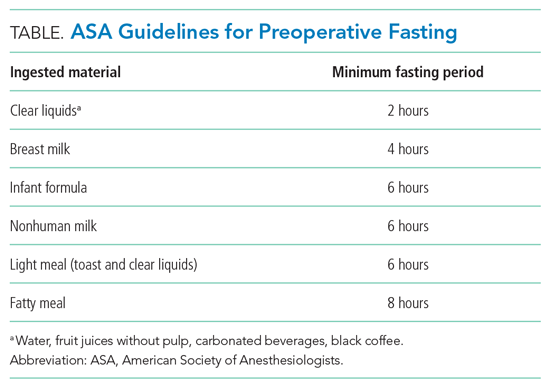
In 1998, as a result of these and other similar studies, the American Society of Anesthesiologists (ASA) along with global anesthesia partners adopted guidelines that allowed clear liquids up until 2 hours prior to anesthesia or sedation in low-aspiration-risk patients undergoing elective cases.11 The guidelines allowed for other beverages and food based on their standard transit times (Table). The ASA guidelines do not define low-aspiration-risk patients. Anesthesiologists generally exclude from the low-risk category patients who may have delayed gastric emptying from medical or iatrogenic causes. The updated 2017 ASA guidelines remain unchanged regarding fasting guidelines.12 Studies suggest that approximately 10% to 20% of NPO after midnight orders are avoidable.1,3 For those instances, procedures are often deemed not necessary or do not require NPO status.1
In a study evaluating the reasons that necessary procedures are canceled, only 0.5% of inpatient procedures are cancelled due to the inappropriate ingestion of food or drink.3 In addition, NPO status creates risk. Patients with prolonged NPO status report greater hunger, thirst, tiredness, and weakness prior to surgery when compared with patients receiving a carbohydrate-rich drink 2 hours prior to procedures.9,13,14 In fact, multiple studies have suggested that preoperative carbohydrate-rich drinks 2 hours before surgery can be associated with decreased insulin resistance in the perioperative period, decreased length of stay, and improvement in perioperative metabolic, cardiac, and psychosomatic status.9,13-15 These types of studies have informed the enhanced recovery after surgery program, which recommends a carbohydrate beverage 2 to 3 hours prior to surgery.
WHEN TO ORDER LONGER PREPROCEDURAL NPO TIMES
Prescribe the minimum recommended fasting times only for low-aspiration-risk patients undergoing elective procedures. Risk for regurgitation or aspiration increases for patients with conditions resulting in decreased gastric emptying, gastric or bowel obstruction, or lower esophageal sphincter incompetence. Those patients may require longer NPO time periods.8 Higher-risk diagnoses and clinical conditions include gastroparesis, trauma, and pregnancy.5,8,16 Specific risk factors for aspiration in children may include trauma, bowel obstruction, depressed consciousness, shock, or ileus.10 For surgical emergencies, balance the risk of surgical delay vs perceived aspiration risk.
WHAT WE SHOULD DO INSTEAD OF ROUTINELY ORDERING NPO AFTER MIDNIGHT
Use evidence-based guidelines to assess periprocedural aspiration risk. The ASA guidelines suggest that healthy, nonpregnant patients should fast for 8 hours after heavy meals, 6 hours after a light, nonfatty meal, and 2 hours after clear liquids (eg, water, fruit juices without pulp, carbonated beverages, black coffee).12 Focus on the type of food or drink rather than the volume ingested.12 Additionally, patients should ingest, with small amounts of clear fluids, appropriate home medications for acute and chronic conditions regardless of NPO status.
While procedure delays or cancellations for any reason upset patients and families and can disrupt the flow of the operating room and procedural suite, we can achieve the delicate balance between efficiency and patient safety and comfort. Since complex inpatient procedural scheduling may not allow for liberalization of solids requiring 6 to 8 hours of fasting time, focus on liberalizing liquids 2 hours prior to anesthesia. This allows staff to minimize the time low-risk patients fast while still maintaining flexibility for operating room case scheduling. We must promote communication between operating room and floor staff to anticipate timing of procedures each day. Healthcare facilities should aim to achieve time-based preprocedural NPO status as opposed to an arbitrary starting time like midnight.4
RECOMMENDATIONS
- Risk stratify patients for anesthesia-related aspiration with the aim of identifying those at low aspiration risk.
- For low-risk patients, adhere to recommended fasting times: 2 hours for a clear carbohydrate beverage, 4 hours for breast milk, 6 hours for a light meal or formula, and 8 hours for a fatty meal.
- For patients not deemed low risk, determine the appropriate length of preprocedural fasting by consulting with the anesthesia and surgical teams.
CONCLUSION
NPO after midnight represents a low-value and arbitrary practice that leaves patients fasting longer than necessary.2,3,12 In addition to the 2017 ASA guidelines, newer studies and protocols are improving patient satisfaction, minimizing patient dehydration and electrolyte disturbances, and incorporating enhanced recovery after surgery factors into a better patient experience. Returning to the clinical scenario, the hospitalist team can increase patient satisfaction by focusing on liberalizing clear fluids with a carbohydrate beverage up to 2 hours prior to elective surgery while still allowing for schedule flexibility. For this patient, a 3
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
Disclaimer: The opinions expressed in this article are those of the authors alone and do not reflect the views of the Department of Veterans Affairs. The Veterans Affairs Quality Scholars Program is supported by the Veterans Affairs Office of Academic Affiliations, Washington, DC.
Inspired by the ABIM Foundation’s Choosing Wisel y ® campaign, the “Things We Do for No Reason ™ ” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
The hospitalist admits an 18-year-old man for newly diagnosed granulomatosis with polyangiitis to receive expedited pulse-dose steroids and plasma exchange. After consulting interventional radiology for catheter placement the following day, the hospitalist places a “strict” nil per os (nothing by mouth, NPO) after midnight order. During rounds the following morning, the patient reports that he wants to eat. At 9
BACKGROUND
Hospitalists commonly order “NPO after midnight” diets in anticipation of procedures requiring sedation or general anesthesia. Typically, NPO refers to no food or drink, but in some instances, NPO includes no oral medications. Up to half of medical patients experience some time of fasting while hospitalized.1 However, NPO practices vary widely across institutions.2,3 A study from 2014 notes that, on average, patients fast preprocedure for approximately 13.5 hours for solids and 9.6 hours for liquids.2 Prolonged fasting times offer little benefit to patients and may lead to frequent patient dissatisfaction and complaints.
WHY YOU MIGHT THINK THAT MAKING PATIENTS NPO AFTER MIDNIGHT IS APPROPRIATE
In 1883, Sir Joseph Lister described 19th century NPO practices distinguishing solids from liquids, allowing patients “tea or beef tea” until 2 to 3 hours prior to surgery.4 However, in 1946, Mendelson published an influential account of 66 pregnant women who aspirated during delivery under general anesthesia.5 Two of the 66 patients, both of whom had eaten a full meal 6 to 8 hours prior to general anesthesia, died. The study not only increased awareness of the risk of aspiration with general anesthesia in pregnancy, but it influenced the care for the nonpregnant population of patients as well. By the 1960s, anesthesia texts recommended “NPO after midnight” for both liquids and solids in all patients, regardless of pregnancy status.4 To minimize the risk to patients, we have continued to pass down the practice of NPO after midnight to subsequent generations.
Additionally, medical centers and hospitals feel pressure to provide efficient, patient-centered, high-value care. Given the complexity of procedural scheduling and the penalties associated with delays, keeping patients NPO ensures their availability for the next open procedural slot. NPO after midnight orders aim to prevent potential delays in treatment that occur when inadvertent ingestion of food and drink leads to cancellation of procedures.
WHY THE INDISCRIMINATE USE OF NPO AFTER MIDNIGHT IS UNNECESSARY
Recent studies have led to a more sophisticated understanding of gastric emptying and the risks of aspiration during sedation and intubation. Gastric emptying studies routinely show that transit of clear liquids out of the stomach is virtually complete within two hours of drinking.6 Age, body mass index, and alcohol have no effect on gastric emptying time, and almost all patients return to preingestion gastric residual volumes within 2 hours of clear liquid consumption.6,7 While morbidly obese patients tend to have higher gastric fluid volumes after 9 hours of fasting, their stomachs empty at rates similar to nonobese individuals.6 Note that, regardless of fasting times, morbid obesity predisposes patients to a higher overall gastric volume and lower pH of gastric contents, which may increase risk of aspiration.8 A Cochrane review found no statistical difference in gastric volumes or stomach pH in patients on a standard fast vs shortened (<180 minutes) liquid fast.9 The review included nine studies that found patients who consumed a clear liquid beverage had reduced gastric volumes, compared with patients in a fasting state (P < .001).9
In a pediatric retrospective study of pulmonary aspiration events, the researchers demonstrated that clinically significant aspiration (presence of bilious secretions in the tracheobronchial airways) occurred at a rate of 0.04% with emergency surgery.10 Bowel obstruction or ileus accounted for approximately 54% of those cases. Importantly, the reported aspiration rate approximates the rate of pregnant patients from the 1946 Mendelson study of 0.14% (66 out of 44,016), which originally prompted the use of the prolonged NPO status. Based on the Cochrane review of perioperative fasting recommendations for those older than 18 years, consuming fluids more than 90 minutes preoperatively confers a negligible (0 adverse events reported in 9 studies) risk for aspiration or regurgitation events.9
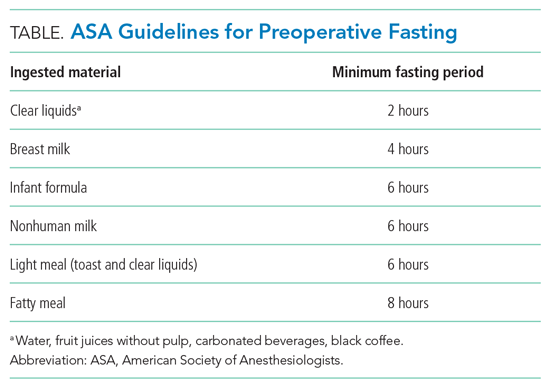
In 1998, as a result of these and other similar studies, the American Society of Anesthesiologists (ASA) along with global anesthesia partners adopted guidelines that allowed clear liquids up until 2 hours prior to anesthesia or sedation in low-aspiration-risk patients undergoing elective cases.11 The guidelines allowed for other beverages and food based on their standard transit times (Table). The ASA guidelines do not define low-aspiration-risk patients. Anesthesiologists generally exclude from the low-risk category patients who may have delayed gastric emptying from medical or iatrogenic causes. The updated 2017 ASA guidelines remain unchanged regarding fasting guidelines.12 Studies suggest that approximately 10% to 20% of NPO after midnight orders are avoidable.1,3 For those instances, procedures are often deemed not necessary or do not require NPO status.1
In a study evaluating the reasons that necessary procedures are canceled, only 0.5% of inpatient procedures are cancelled due to the inappropriate ingestion of food or drink.3 In addition, NPO status creates risk. Patients with prolonged NPO status report greater hunger, thirst, tiredness, and weakness prior to surgery when compared with patients receiving a carbohydrate-rich drink 2 hours prior to procedures.9,13,14 In fact, multiple studies have suggested that preoperative carbohydrate-rich drinks 2 hours before surgery can be associated with decreased insulin resistance in the perioperative period, decreased length of stay, and improvement in perioperative metabolic, cardiac, and psychosomatic status.9,13-15 These types of studies have informed the enhanced recovery after surgery program, which recommends a carbohydrate beverage 2 to 3 hours prior to surgery.
WHEN TO ORDER LONGER PREPROCEDURAL NPO TIMES
Prescribe the minimum recommended fasting times only for low-aspiration-risk patients undergoing elective procedures. Risk for regurgitation or aspiration increases for patients with conditions resulting in decreased gastric emptying, gastric or bowel obstruction, or lower esophageal sphincter incompetence. Those patients may require longer NPO time periods.8 Higher-risk diagnoses and clinical conditions include gastroparesis, trauma, and pregnancy.5,8,16 Specific risk factors for aspiration in children may include trauma, bowel obstruction, depressed consciousness, shock, or ileus.10 For surgical emergencies, balance the risk of surgical delay vs perceived aspiration risk.
WHAT WE SHOULD DO INSTEAD OF ROUTINELY ORDERING NPO AFTER MIDNIGHT
Use evidence-based guidelines to assess periprocedural aspiration risk. The ASA guidelines suggest that healthy, nonpregnant patients should fast for 8 hours after heavy meals, 6 hours after a light, nonfatty meal, and 2 hours after clear liquids (eg, water, fruit juices without pulp, carbonated beverages, black coffee).12 Focus on the type of food or drink rather than the volume ingested.12 Additionally, patients should ingest, with small amounts of clear fluids, appropriate home medications for acute and chronic conditions regardless of NPO status.
While procedure delays or cancellations for any reason upset patients and families and can disrupt the flow of the operating room and procedural suite, we can achieve the delicate balance between efficiency and patient safety and comfort. Since complex inpatient procedural scheduling may not allow for liberalization of solids requiring 6 to 8 hours of fasting time, focus on liberalizing liquids 2 hours prior to anesthesia. This allows staff to minimize the time low-risk patients fast while still maintaining flexibility for operating room case scheduling. We must promote communication between operating room and floor staff to anticipate timing of procedures each day. Healthcare facilities should aim to achieve time-based preprocedural NPO status as opposed to an arbitrary starting time like midnight.4
RECOMMENDATIONS
- Risk stratify patients for anesthesia-related aspiration with the aim of identifying those at low aspiration risk.
- For low-risk patients, adhere to recommended fasting times: 2 hours for a clear carbohydrate beverage, 4 hours for breast milk, 6 hours for a light meal or formula, and 8 hours for a fatty meal.
- For patients not deemed low risk, determine the appropriate length of preprocedural fasting by consulting with the anesthesia and surgical teams.
CONCLUSION
NPO after midnight represents a low-value and arbitrary practice that leaves patients fasting longer than necessary.2,3,12 In addition to the 2017 ASA guidelines, newer studies and protocols are improving patient satisfaction, minimizing patient dehydration and electrolyte disturbances, and incorporating enhanced recovery after surgery factors into a better patient experience. Returning to the clinical scenario, the hospitalist team can increase patient satisfaction by focusing on liberalizing clear fluids with a carbohydrate beverage up to 2 hours prior to elective surgery while still allowing for schedule flexibility. For this patient, a 3
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
Disclaimer: The opinions expressed in this article are those of the authors alone and do not reflect the views of the Department of Veterans Affairs. The Veterans Affairs Quality Scholars Program is supported by the Veterans Affairs Office of Academic Affiliations, Washington, DC.
1. Sorita A, Thongprayoon C, Ahmed A, et al. Frequency and appropriateness of fasting orders in the hospital. Mayo Clin Proc. 2015;90(9):1225-1232. https://doi.org/10.1016/j.mayocp.2015.07.013
2. Falconer R, Skouras C, Carter T, Greenway L, Paisley AM. Preoperative fasting: current practice and areas for improvement. Updates Surg. 2014;66(1):31-39. https://doi.org/10.1007/s13304-013-0242-z
3. Sorita A, Thongprayoon C, Ratelle JT, et al. Characteristics and outcomes of fasting orders among medical inpatients. J Hosp Med. 2017;12(1):36-39. https://doi.org/10.1002/jhm.2674
4. Maltby JR. Fasting from midnight–the history behind the dogma. Best Pract Res Clin Anaesthesiol. 2006;20(3):363-378. https://doi.org/10.1016/j.bpa.2006.02.001
5. Mendelson CL. The aspiration of stomach contents into the lungs during obstetric anesthesia. Am J Obstet Gynecol. 1946;52:191-205. https://doi.org/10.1016/s0002-9378(16)39829-5
6. Shiraishi T, Kurosaki D, Nakamura M, et al. Gastric fluid volume change after oral rehydration solution intake in morbidly obese and normal controls: a magnetic resonance imaging-based analysis. Anesth Analg. 2017;124(4):1174-1178. https://doi.org/10.1213/ane.0000000000001886
7. Vasavid P, Chaiwatanarat T, Pusuwan P, et al. Normal solid gastric emptying values measured by scintigraphy using Asian-style meal: a multicenter study in healthy volunteers. J Neurogastroenterol Motil. 2014;20(3):371-378. https://doi.org/10.5056/jnm13114
8. Mahajan V, Hashmi J, Singh R, Samra T, Aneja S. Comparative evaluation of gastric pH and volume in morbidly obese and lean patients undergoing elective surgery and effect of aspiration prophylaxis. J Clin Anesth. 2015;27(5):396-400. https://doi.org/10.1016/j.jclinane.2015.03.004
9. Brady MC, Kinn S, Stuart P, Ness V. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev. 2003;(4):CD004423. https://doi.org/10.1002/14651858.cd004423
10. Warner MA, Warner ME, Warner DO, Warner LO, Warner EJ. Perioperative pulmonary aspiration in infants and children. Anesthesiology. 1999;90(1):66-71. https://doi.org/10.1097/00000542-199901000-00011
11. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: a report by the American Society of Anesthesiologist Task Force on Preoperative Fasting. Anesthesiology. 1999;90(3):896-905. https://doi.org/10.1097/00000542-199903000-00034
12. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists task force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126(3):376-393. https://doi.org/10.1097/aln.0000000000001452
13. Hausel J, Nygren J, Lagerkranser M, et al. A carbohydrate-rich drink reduces preoperative discomfort in elective surgery patients. Anesth Analg. 2001;93(5):1344-1350. https://doi.org/10.1097/00000539-200111000-00063
14. Awad S, Varadhan KK, Ljungqvist O, Lobo DN. A meta-analysis of randomised controlled trials on preoperative oral carbohydrate treatment in elective surgery. Clin Nutr. 2013;32(1):34-44. https://doi.org/10.1016/j.clnu.2012.10.011
15. Kaška M, Grosmanová T, Havel E, et al. The impact and safety of preoperative oral or intravenous carbohydrate administration versus fasting in colorectal surgery–a randomized controlled trial. Wien Klin Wochenschr. 2010;122(1-2):23-30. https://doi.org/10.1007/s00508-009-1291-7
16. Tokumine J, Sugahara K, Fuchigami T, Teruya K, Nitta K, Satou K. Unanticipated full stomach at anesthesia induction in a type I diabetic patient with asymptomatic gastroparesis. J Anesth. 2005;19(3):247-248. https://doi.org/10.1007/s00540-005-0321-5
1. Sorita A, Thongprayoon C, Ahmed A, et al. Frequency and appropriateness of fasting orders in the hospital. Mayo Clin Proc. 2015;90(9):1225-1232. https://doi.org/10.1016/j.mayocp.2015.07.013
2. Falconer R, Skouras C, Carter T, Greenway L, Paisley AM. Preoperative fasting: current practice and areas for improvement. Updates Surg. 2014;66(1):31-39. https://doi.org/10.1007/s13304-013-0242-z
3. Sorita A, Thongprayoon C, Ratelle JT, et al. Characteristics and outcomes of fasting orders among medical inpatients. J Hosp Med. 2017;12(1):36-39. https://doi.org/10.1002/jhm.2674
4. Maltby JR. Fasting from midnight–the history behind the dogma. Best Pract Res Clin Anaesthesiol. 2006;20(3):363-378. https://doi.org/10.1016/j.bpa.2006.02.001
5. Mendelson CL. The aspiration of stomach contents into the lungs during obstetric anesthesia. Am J Obstet Gynecol. 1946;52:191-205. https://doi.org/10.1016/s0002-9378(16)39829-5
6. Shiraishi T, Kurosaki D, Nakamura M, et al. Gastric fluid volume change after oral rehydration solution intake in morbidly obese and normal controls: a magnetic resonance imaging-based analysis. Anesth Analg. 2017;124(4):1174-1178. https://doi.org/10.1213/ane.0000000000001886
7. Vasavid P, Chaiwatanarat T, Pusuwan P, et al. Normal solid gastric emptying values measured by scintigraphy using Asian-style meal: a multicenter study in healthy volunteers. J Neurogastroenterol Motil. 2014;20(3):371-378. https://doi.org/10.5056/jnm13114
8. Mahajan V, Hashmi J, Singh R, Samra T, Aneja S. Comparative evaluation of gastric pH and volume in morbidly obese and lean patients undergoing elective surgery and effect of aspiration prophylaxis. J Clin Anesth. 2015;27(5):396-400. https://doi.org/10.1016/j.jclinane.2015.03.004
9. Brady MC, Kinn S, Stuart P, Ness V. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev. 2003;(4):CD004423. https://doi.org/10.1002/14651858.cd004423
10. Warner MA, Warner ME, Warner DO, Warner LO, Warner EJ. Perioperative pulmonary aspiration in infants and children. Anesthesiology. 1999;90(1):66-71. https://doi.org/10.1097/00000542-199901000-00011
11. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: a report by the American Society of Anesthesiologist Task Force on Preoperative Fasting. Anesthesiology. 1999;90(3):896-905. https://doi.org/10.1097/00000542-199903000-00034
12. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists task force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126(3):376-393. https://doi.org/10.1097/aln.0000000000001452
13. Hausel J, Nygren J, Lagerkranser M, et al. A carbohydrate-rich drink reduces preoperative discomfort in elective surgery patients. Anesth Analg. 2001;93(5):1344-1350. https://doi.org/10.1097/00000539-200111000-00063
14. Awad S, Varadhan KK, Ljungqvist O, Lobo DN. A meta-analysis of randomised controlled trials on preoperative oral carbohydrate treatment in elective surgery. Clin Nutr. 2013;32(1):34-44. https://doi.org/10.1016/j.clnu.2012.10.011
15. Kaška M, Grosmanová T, Havel E, et al. The impact and safety of preoperative oral or intravenous carbohydrate administration versus fasting in colorectal surgery–a randomized controlled trial. Wien Klin Wochenschr. 2010;122(1-2):23-30. https://doi.org/10.1007/s00508-009-1291-7
16. Tokumine J, Sugahara K, Fuchigami T, Teruya K, Nitta K, Satou K. Unanticipated full stomach at anesthesia induction in a type I diabetic patient with asymptomatic gastroparesis. J Anesth. 2005;19(3):247-248. https://doi.org/10.1007/s00540-005-0321-5
© 2021 Society of Hospital Medicine