User login
› Ask all patients with migraines about their use of complementary and alternative medicine and what modalities, if any, they have found helpful. A
› Advise patients that while butterbur has been proven effective at reducing migraine frequency, its use requires caution, as products not processed properly may contain hepatotoxic compounds. A
› Caution women who are pregnant or attempting to conceive to avoid feverfew, which may cause uterine contractions. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Americans who suffer from migraine headaches are far more likely than those who don’t to turn to complementary and alternative medicine (CAM). A 2007 National Health Interview Survey and a subsequent analysis of the results found that just under 50% of adults with migraine headaches used alternative therapies; among those without migraine, 34% did.1,2 What’s more, only about half of the migraine patients who reported the use of CAM modalities mentioned it to their health care providers.2
With migraine affecting some 36 million Americans,3 chances are you are caring for many of them. It is likely, too, that you are unaware of which of your headache patients are using alternative treatments, or what modalities they have tried. The only way to find out is to ask.
Women, who are 3 times more likely than men to suffer from migraine headache,4 are also the greatest users of CAM, particularly biologically based therapies and mind-body practices.5 Use is highly individualized and typically does not involve professional supervision.5
A number of alternative modalities look promising for migraine prevention. As a family physician, you are in an ideal position to guide patients in the use of safe and effective CAM therapies. To do so, however, you need to be familiar with the evidence for or against various options—many of which can be used in conjunction with pharmacotherapy.
An integrative approach to the treatment of migraine headaches makes use of the best available evidence for both conventional and alternative therapies and takes into account the whole person, including all aspects of his or her belief system and lifestyle. It also emphasizes a strong physician-patient relationship, which can have a powerful therapeutic effect.
We wrote this evidence-based update with such an approach in mind. In the text and table that follow, we present the latest findings. But first, a brief review of what constitutes migraine headache and an overview of conventional treatment.
A conventional approach to migraine
Migraine headache is a common and disabling neurologic disorder that frequently goes unrecognized and undertreated.6 It is generally characterized as recurrent headaches that are unilateral, pulsating, moderately severe, aggravated by physical activity, and associated with nausea, vomiting, photophobia, phonophobia, and sometimes a preceding aura. Conventional treatment typically includes abortive treatment for acute migraine, with medications such as the triptans and dihydroergotamine. Acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and the combination of acetaminophen/aspirin/caffeine are also effective. Opiates are efficacious, but not recommended.7
Prophylactic medications are generally offered to patients experiencing more than 4 migraines per month. The American Academy of Neurology cites strong evidence for the use of divalproex, valproate, topiramate, and beta-blockers, including metoprolol, propranolol, and timolol. Frovatriptan has strong evidence for prevention of menstrual-associated migraine. Common adverse effects include weight loss and parasthesias with topiramate and weight gain and somnolence with valproate, divalproex, and beta-blockers. There is also moderate evidence for the use of amitriptyline, venlafaxine, atenolol, and nadolol. Potential adverse effects must be considered to determine the optimal therapy for individual patients, and trial and error are often required.8
Addressing triggers
Conventional treatment also focuses on identifying and avoiding triggers to the extent possible. Physicians typically advise patients to keep a headache diary, recording details about diet and lifestyle, triggers, frequency and intensity of attacks, and possible patterns of headaches due to medication overuse.
Sleep disturbances and stress are common triggers, and instruction in sleep hygiene and stress reduction, as well as screening for anxiety or depression, can be beneficial. Other frequently reported factors believed to trigger or aggravate migraine attacks are skipping meals, particular foods, alcohol, weather changes, and exposure to light, sounds, and odors.
Despite the focus on migraine triggers, however, clinical studies of the role they play have shown conflicting results. A recent study involving 27 patients7 found that when attempting to provoke migraine with aura using participants’ self-reported triggers, only 3 individuals reported that the provocation actually led to a migraine.9 Additional studies suggest that exposure to headache triggers has the same effect as exposure to anxiety, with short-term exposure associated with an increased pain response and prolonged exposure leading to a decreased response.10,11 Thus, it may be beneficial to advise patients to learn to cope with controlled exposure to triggers rather than to aim for trigger avoidance.12
If noise is identified as a trigger, for instance, repeated exposure in a relaxed environment can help desensitize the patient. Triggers such as visual disturbances and odors are also good candidates for desensitization, while others, such as sleep deprivation and skipping meals, are better served by avoidance.12
CAM approaches: A look at the evidence
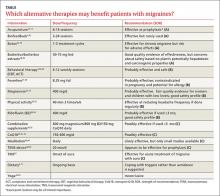
Acupuncture, butterbur, feverfew, magnesium, riboflavin, and biofeedback look promising for migraine prevention. Many of our patients are already using these and other alternative therapies. Here’s what the latest studies show (TABLE).2,9-11, 13-51
Can acupuncture help?
A 2009 Cochrane review of 22 high-quality studies with a total of 4419 participants supports the use of acupuncture for migraine prophylaxis.13 Acupuncture was found to be superior to no prophylactic treatment and acute treatment alone, and as effective as conventional preventive medications. Interestingly, though, among studies included in the Cochrane review that compared true acupuncture with sham interventions, no significant difference in results was found.
A more recent meta-analysis of 29 studies representing nearly 18,000 patients did show true acupuncture to be statistically superior to sham acupuncture, although the difference was of small clinical significance. Sham acupuncture was also shown to have a larger clinical effect than oral placebos, raising questions about the importance of exact point location.14
In a 2015 study comparing real and sham acupuncture over a 20-week period, however, the differences were more marked. Those who received real acupuncture reported significantly fewer migraine days and less severe headaches, and there were more responders in the treatment group compared with recipients of the sham procedures.15 Overall, the evidence indicates that acupuncture is at least as effective as conventional drug treatment for migraine prophylaxis, but with fewer adverse effects.13-17
Butterbur raises concerns about toxicity
Butterbur (Petasites hybridus) is one of the best-studied natural remedies for migraine. The research has primarily focused on an extract of 15% petasin and isopetasin sold under the trade name Petadolex. A study of patients using this herbal preparation for 16 weeks showed a response rate of 48% for reduction in headache frequency among those taking 75 mg twice daily and a 36% reduction in those taking 50 mg twice a day. The primary adverse effect was burping.18
Proper processing is crucial. The key concern about butterbur is that it naturally contains hepatotoxic compounds called pyrrolizidine alkaloids (PA), which may remain if the product is not properly processed.18-20 The labeling on many butterbur products states that they are “PA-free,” but because the manufacturers, rather than the US Food and Drug Administration (FDA), bear the responsibility for the safety and labeling of supplements, there is little oversight.
In fact, supplement quality is of considerable concern and subject to ongoing research. DNA bar-coding studies have confirmed that many common herbal preparations either contain ingredients not listed on the label or, conversely, fail to contain all the ingredients that are listed.52 Patients should be advised to look for evidence of quality assurance when purchasing herbal supplements, such as that offered by the US Pharmacopeia (USP) on a limited range of products. (We have not found any butterbur supplements with USP verification.)
Feverfew yields mixed results
Studies of feverfew extract for migraine have had conflicting results, probably because different extracts have been tested. A recent Cochrane review, however, cited one clinical trial (N=218) that added positive evidence to previously inconclusive findings.21
The study in question assessed a proprietary extract of feverfew (MIG-99) and found a small decrease in frequency of migraines (0.6 per month) compared with placebo. Adverse effects were gastrointestinal disturbances and mouth ulcers.22
Warn women of childbearing age that feverfew may cause uterine contractions and is contraindicated for those who are pregnant or trying to conceive.23 In addition, patients who are allergic to ragweed, chrysanthemums, or other members of the daisy family may be allergic to feverfew, as well.24
Magnesium is helpful for some
While magnesium is used for both acute relief of migraine and as prophylaxis, evidence of its efficacy is mixed. Studies have been promising in women with low magnesium levels and those who suffer from menstrual migraines, and for use in children with migraine headaches as both acute and preventive treatment.25,26
One RCT involving 160 children ages 5 to 16 years found magnesium to have a synergistic effect with acetaminophen or ibuprofen, leading to greater acute pain relief and reducing migraine frequency.27 A recent meta-analysis, however, concluded that intravenous magnesium is not likely to be effective for acute treatment.53 The main adverse effects seen with magnesium are diarrhea and soft stools.
Patients with renal disease should avoid magnesium supplementation. Food sources of magnesium include whole grains, spinach, nuts, legumes, and white potatoes.54
Riboflavin shows promise
Riboflavin (B2) plays an important role in cellular energy production and is an important antioxidant in mitochondria. Several small studies have shown promising results with high-dose (400 mg) riboflavin in migraine prevention, with evidence suggesting that it may be as effective as beta-blockers such as bisoprolol and metoprolol.28-30 Discoloration of urine, which turns bright yellow, is the primary adverse effect.
CoQ10 helps those with low levels
Like riboflavin, coenzyme Q10 (CoQ10) is involved in mitochondrial transport and plays an important role in cellular energy metabolism. Several small studies have shown efficacy in migraine prevention in doses of 150 to 300 mg/d, with response rates between 30% and 50%.31,32 Based on data in adults, the American Academy of Neurology guidelines give CoQ10 a Level C rating, indicating that it is possibly effective in preventing migraine.29
An open label study of children with migraine found that close to a third were below the reference range for CoQ10 levels. Their serum levels increased when they began taking CoQ10 supplements, resulting in a significant reduction in headache frequency and an improvement in migraine-related disability.33
Combination supplements have little efficacy
In a study published in 2015,34 a proprietary supplement containing magnesium 600 mg, riboflavin 400 mg, CoQ10 150 mg, and low-dose multivitamins, taken daily, did not show statistically significant efficacy in the reduction of migraine days. After 3 months of supplementation, however, the severity of migraine pain improved. Adverse effects included abdominal discomfort and diarrhea.
Another study compared a combination of riboflavin 400 mg, magnesium 300 mg, and feverfew 100 mg with low-dose riboflavin (25 mg) as placebo, and found that the combination did not reduce the frequency or severity of migraine any more than the placebo.35
Botox may relieve chronic migraine
Onabotulinumtoxin A (Botox) has FDA approval for the prevention of chronic migraines—ie, migraines that occur >15 days per month and at least 4 hours or more per day.55 Botox is administered by injection every 12 weeks, across 31 sites on the head and neck. The recommended dose is 155 units, with 5 units delivered into each injection site.
This protocol has been found to reduce the number of headache days by 50% in half of those being treated after one cycle, and in more than 70% of patients after 3 cycles.36 Potential adverse effects include blepharoptosis, neck muscle weakness, and the risk of botulism at sites distant from the injections.37-39
Mind-body therapies are most widely used
Of all the CAM therapies used by patients with migraine headaches, mind-body modalities are the most prevalent. Overall, 30% of headache patients use them, compared with 17% of the general population.2
Many of these modalities have been found to be effective and safe to use with the conventional migraine treatments with which patients commonly combine them.
Meditation. Both spiritual and secular forms of meditation have been studied for acute and preventive treatment of migraine and found to be effective. A recent small study suggests that spiritual meditation may be more effective,40 but secular mindfulness-based stress reduction training has also shown promise in migraine treatment.
One positive effect is that those who meditate typically use less migraine medication,41 decreasing the burden of disease. Meditation is increasingly available via a range of options, including both in-person groups and online sessions, and can easily augment conventional medical treatments.
Yoga, which typically combines physical postures, breathing techniques, and mental concentration/meditation, is increasingly widespread. While there is compelling evidence of its effect in treating chronic pain and stress-related conditions,42 studies specific to migraine are lacking. Several small studies comparing yoga to NSAIDs, educational handouts, and conventional care for headache suggest that yoga has efficacy for the treatment of migraine, but the findings are limited by methodology and sample size.42,43
Relaxation training. Various types of relaxation are described in the literature, often combining progressive muscle relaxation, diaphragmatic breathing, and relaxation-inducing imagery. Although the consensus is that these techniques are effective, differences in standards, frequency, and duration of training make it hard to draw conclusions.44
Biofeedback is similar to relaxation training, with the key difference being that it uses monitoring to train patients to alter their physiological state, thereby leading to desired changes—eg, fewer headaches and lower intensity of pain. Monitors evaluate skin temperature, electromyography, heart rate variability (blood-volume-pulse), and skin conductance, among other measures.
A robust collection of studies has shown the efficacy of skin temperature feedback, blood-volume-pulse feedback, and electromyography feedback as treatment for migraine.45 Blood-volume-pulse feedback in combination with additional home training is perhaps more effective than other modalities. Despite convincing evidence of its efficacy for migraine headaches, however, only about 1% of patients with migraine use biofeedback. That’s likely due to a lack of availability outside of urban medical centers, limited insurance coverage, and time constraints.2,45
Behavioral therapy can be of help
Cognitive behavioral therapy (CBT) focuses on adjusting maladaptive thoughts and behaviors. For migraine patients, this may include identifying and changing the patient’s response to migraine triggers such as stress, sleep deprivation, and fear of headache pain. Relaxation techniques may be incorporated into the therapy.
The effect size of CBT for prevention is comparable to prophylactic medication use, with 34% to 40% of patients achieving a clinically significant decrease in the number of attacks. Additive effects are especially promising, with more than two-thirds of patients achieving decreased frequency when CBT is combined with preventative medications.2,44,46
Acceptance and commitment therapy (ACT) is a newer variant of CBT that has recently been studied.44 Unlike CBT, in which patients are taught to control and revise their maladaptive thoughts and feelings, ACT focuses on noticing and accepting such unwanted thoughts and feelings and changing the way individuals respond to them rather than changing the thoughts themselves. Further study is needed to determine whether ACT is an effective treatment for migraine.
FDA-approved devices take aim at migraine
A transcranial magnetic stimulator (TMS) (Cerena, eNeura Inc, Sunnyvale, Calif) received FDA approval in 2013.56 The single-pulse TMS is the first device authorized for the treatment of migraine headache pain. It is geared specifically to patients suffering from migraine with aura and requires a prescription.
In a study of 201 patients, the group using the TMS device at the onset of aura had a 38% response rate, compared with a 17% response among those in the sham control group. Dizziness was reported as an adverse effect. Caution patients who express an interest in it that the device should not be used by those who are at risk for seizures or have an implanted device, such as a pacemaker or deep brain stimulator.47
Transcutaneous electrical nerve stimulation (TENS) has long been used for chronic pain, but in 2014 the FDA approved the first TENS device aimed at the prevention of migraine headaches in patients age 18 and older.57 It is also the first such device approved for use prior to the onset of pain.
The Cefaly (Cefaly US, Inc., Wilton, Conn), which requires a prescription, is worn like a headband. It is positioned on the forehead just above the eyes, using an adhesive electrode, and is worn once a day for 20 minutes. The device applies an electrical current to the skin and underlying tissues to stimulate branches of the trigeminal nerve, which can cause a tingling or massaging sensation. Several small studies have shown a decrease in migraine frequency comparable with other preventive treatments. The main adverse effect reported was sedation, but more than half of those who used it were satisfied and willing to purchase the device.48,49
Regular exercise has little downside
While physical activity can be a trigger for acute migraine, regular exercise has been shown to decrease the frequency of migraine attacks. And, although aerobic exercise is no more effective as migraine prophylaxis than conventional drug treatments, it has few adverse effects. For patients who want to stay fit and avoid taking preventive medications, exercise is a valuable adjunct to conventional treatments.50,51
CORRESPONDENCE
Laura Armstrong, MD, Memorial Hermann Family Medicine Residency Program, 14023 Southwest Freeway, Sugar Land, TX 77478; laura.armstrong@memorialhermann.org.
1. National Center for Complementary and Integrative Health. 2007 Statistics on CAM Use in the United States. National Center for Complementary and Integrative Health Web site. Available at: https://nccih.nih.gov/news/camstats/2007. Accessed January 6, 2016.
2. Wells RE, Bertisch SM, Buettner C, et al. Complementary and alternative medicine use among adults with migraines/severe headaches. Headache. 2011;51:1087-1097.
3. Lipton RB, Silberstein SD. Episodic and chronic migraine headache: breaking down barriers to optimal treatment and prevention. Headache. 2015;55:S103-S122.
4. Migraine Research Foundation. Migraine in women. Migraine Research Foundation Web site. Available at: http://www.migraineresearchfoundation.org/Migraine%20in%20Women.html. Accessed January 7, 2016.
5. Clarke TC, Black LI, Stussman BJ, et al. Trends in the use of complementary health approaches among adults: United States, 2002-2012. Natl Health Stat Report. 2015:1-16.
6. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd ed. Cephalalgia. 2013;33:629-808.
7. Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the American Headache Society evidence assessment of migraine pharmacotherapies. Headache. 2015;55:3-20.
8. Silberstein SD, Holland S, Freitag F, et al; Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78:1337-1345.
9. Hougaard A, Amin FM, Hauge AW, et al. Provocation of migraine with aura using natural trigger factors. Neurology. 2013;80:428-431.
10. Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27:394-402.
11. Martin PR. Managing headache triggers: Think ‘coping’ not ‘avoidance’. Cephalalgia. 2010;30:634-637.
12. Martin PR, MacLeod C. Behavioral management of headache triggers: Avoidance of triggers is an inadequate strategy. Clin Psychol Rev. 2009;29:483-495.
13. Linde K, Allais G, Brinkhaus B, et al. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009:CD001218.
14. Vickers AJ, Cronin AM, Maschino AC, et al; Acupuncture Trialists’ Collaboration. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444-1453.
15. Wang Y, Xue CC, Helme R, et al. Acupuncture for frequent migraine: A randomized, patient/assessor blinded, controlled trial with one-year follow-up. Evid Based Complement Alternat Med. 2015;2015:920353.
16. Da Silva AN. Acupuncture for migraine prevention. Headache. 2015;55:470-473.
17. Meissner K, Fassler M, Rücker G, et al. Differential effectiveness of placebo treatments: a systematic review of migraine prophylaxis. JAMA Intern Med. 2013;173:1941-1951.
18. Lipton RB, Göbel H, Einhäupl KM, et al. Petasites hybridus root (butterbur) is an effective preventive treatment for migraine. Neurology. 2004;63:2240-2244.
19. Grossman W, Schmidramsl H. An extract of Petasites hybridus is effective in the prophylaxis of migraine. Altern Med Rev. 2001;6:303-310.
20. Diener HC, Rahlfs VW, Danesch U. The first placebo-controlled trial of a special butterbur root extract for the prevention of migraine: Reanalysis of efficacy criteria. Eur Neurol. 2004;51:89-97.
21. Wider B, Pittler MH, Ernst E. Feverfew for preventing migraine. Cochrane Database Syst Rev. 2015;4:CD002286.
22. Pfaffenrath V, Diener HC, Fischer M, et al; Investigators. The efficacy and safety of Tanacetum parthenium (feverfew) in migraine prophylaxis--a double-blind, multicentre, randomized placebo-controlled dose-response study. Cephalalgia. 2002;22:523-532.
23. Ernst E, Pittler MH. The efficacy and safety of feverfew (Tanacetum parthenium L.): an update of a systematic review. Public Health Nutr. 2000;3:509-514.
24. Natural Medicines. Feverfew Professional Monograph, 2016. Natural Medicines Web site. Available at: https://naturalmedicines.therapeuticresearch.com/. Accessed January 1, 2016.
25. Wang F, Van Den Eeden SK, Ackerson LM, et al. Oral magnesium oxide prophylaxis of frequent migrainous headache in children: a randomized, double-blind, placebo-controlled trial. Headache. 2003;43:601-610.
26. Facchinetti F, Sances G, Borella P, et al. Magnesium prophylaxis of menstrual migraine: effects on intracellular magnesium. Headache. 1991;31:298-301.
27. Gallelli L, Avenoso T, Falcone D, et al. Effects of acetaminophen and ibuprofen in children with migraine receiving preventive treatment with magnesium. Headache. 2014;54:313-324.
28. Sándor PS, Afra J, Ambrosini A, et al. Prophylactic treatment of migraine with beta-blockers and riboflavin: differential effects on the intensity dependence of auditory evoked cortical potentials. Headache. 2000;40:30-35.
29. Holland S, Silberstein SD, Freitag F, et al; Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78:1346-1353.
30. Boehnke C, Reuter U, Flach U, et al. High-dose riboflavin treatment is efficacious in migraine prophylaxis: an open study in a tertiary care centre. Eur J Neurol. 2004;11:475-477.
31. Sándor PS, Di Clemente L, Coppola G, et al. Efficacy of coenzyme Q10 in migraine prophylaxis: a randomized controlled trial. Neurology. 2005;64:713-715.
32. Rozen TD, Oshinsky ML, Gebeline CA, et al. Open label trial of coenzyme Q10 as a migraine preventive. Cephalalgia. 2002;22:137-141.
33. Hershey AD, Powers SW, Vockell AL, et al. Coenzyme Q10 deficiency and response to supplementation in pediatric and adolescent migraine. Headache. 2007;47:73-80.
34. Gaul C, Diener HC, Danesch U; Migravent Study Group. Improvement of migraine symptoms with a proprietary supplement containing riboflavin, magnesium and Q10: a randomized, placebo-controlled, double-blind, multicenter trial. J Headache Pain. 2015;16:516.
35. Maizels M, Blumenfeld A, Burchette R. A combination of riboflavin, magnesium, and feverfew for migraine prophylaxis: a randomized trial. Headache. 2004;44:885-890.
36. Silberstein SD, Dodick DW, Aurora SK, et al. Percent of patients with chronic migraine who responded per onabotulinumtoxin A treatment cycle: PREEMPT. J Neurol Neurosurg Psychiatry. 2015;86:996-1001.
37. Estemalik E, Tepper S. Preventive treatment in migraine and the new US guidelines. Neuropsychiatr Dis Treat. 2013;9:709-720.
38. Aurora SK, Winner P, Freeman MC, et al. Onabotulinumtoxin A for treatment of chronic migraine: pooled analyses of the 56-week PREEMPT clinical program. Headache. 2011;51:1358-1373.
39. Diener HC, Dodick DW, Aurora SK, et al; PREEMPT 2 Chronic Migraine Study Group. Onabotulinumtoxin A for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 2 trial. Cephalalgia. 2010;30:804-814.
40. Wachholtz AB, Malone CD, Pargament KI. Effect of different meditation types on migraine headache medication use. Behav Med. 2015:1-8.
41. Smitherman TA, Wells RE, Ford SG. Emerging behavioral treatments for migraine. Curr Pain Headache Rep. 2015;19:13.
42. Kisan R, Sujan M, Adoor M, et al. Effect of yoga on migraine: A comprehensive study using clinical profile and cardiac autonomic functions. Int J Yoga. 2014;7:126-132.
43. Büssing A, Ostermann T, Lüdtke R, et al. Effects of yoga interventions on pain and pain-associated disability: a meta-analysis. J Pain. 2012;13:1-9.
44. Penzien DB, Irby MB, Smitherman TA, et al. Well-established and empirically supported behavioral treatments for migraine. Curr Pain Headache Rep. 2015;19:34.
45. Nestoriuc Y, Martin A. Efficacy of biofeedback for migraine: a meta-analysis. Pain. 2007;128:111-127.
46. Fritsche G, Kröner-Herwig B, Kropp P, et al. Psychological therapy of migraine: systematic review. Schmerz. 2013;27:263-274.
47. Lipton RB, Dodick DW, Silberstein SD, et al. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomised, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. 2010;9:373-380.
48. Schoenen J, Vandersmissen B, Jeangette S, et al. Migraine prevention with a supraorbital transcutaneous stimulator: a randomized controlled trial. Neurology. 2013;80:697-704.
49. Piquet M, Balestra C, Sava SL, et al. Supraorbital transcutaneous neurostimulation has sedative effects in healthy subjects. BMC Neurol. 2011;11:135.
50. Gil-Martínez A, Kindelan-Calvo P, Agudo-Carmona D, et al. Therapeutic exercise as treatment for migraine and tension-type headaches: a systematic review of randomised clinical trials. Rev Neurol. 2013;57:433-443.
51. Varkey E, Cider A, Carlsson J, et al. Exercise as migraine prophylaxis: a randomized study using relaxation and topiramate as controls. Cephalalgia. 2011;31:1428-1438.
52. Newmaster SG, Grguric M, Shanmughanandhan D, et al. DNA barcoding detects contamination and substitution in North American herbal products. BMC Med. 2013;11:222.
53. Choi H, Parmar N. The use of intravenous magnesium sulphate for acute migraine: meta-analysis of randomized controlled trials. Eur J Emerg Med. 2014;21:2-9.
54. Volpe SL. Magnesium in disease prevention and overall health. Adv Nutr. 2013;4:S378-S383.
55. US Food and Drug Administration. FDA approves Botox to treat chronic migraine. US Food and Drug Administration Web site. October 15, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm229782.htm. Accessed January 7, 2016.
56. US Food and Drug Administration. FDA allows marketing of first device to relieve migraine headache pain. US Food and Drug Administration Web site. December 13, 2013. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm378608.htm. Accessed January 7, 2016.
57. US Food and Drug Administration. FDA allows marketing of first medical device to prevent migraine headache. US Food and Drug Administration Web site. March 11, 2014. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm388765.htm. Accessed January 7, 2016.
› Ask all patients with migraines about their use of complementary and alternative medicine and what modalities, if any, they have found helpful. A
› Advise patients that while butterbur has been proven effective at reducing migraine frequency, its use requires caution, as products not processed properly may contain hepatotoxic compounds. A
› Caution women who are pregnant or attempting to conceive to avoid feverfew, which may cause uterine contractions. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Americans who suffer from migraine headaches are far more likely than those who don’t to turn to complementary and alternative medicine (CAM). A 2007 National Health Interview Survey and a subsequent analysis of the results found that just under 50% of adults with migraine headaches used alternative therapies; among those without migraine, 34% did.1,2 What’s more, only about half of the migraine patients who reported the use of CAM modalities mentioned it to their health care providers.2
With migraine affecting some 36 million Americans,3 chances are you are caring for many of them. It is likely, too, that you are unaware of which of your headache patients are using alternative treatments, or what modalities they have tried. The only way to find out is to ask.
Women, who are 3 times more likely than men to suffer from migraine headache,4 are also the greatest users of CAM, particularly biologically based therapies and mind-body practices.5 Use is highly individualized and typically does not involve professional supervision.5
A number of alternative modalities look promising for migraine prevention. As a family physician, you are in an ideal position to guide patients in the use of safe and effective CAM therapies. To do so, however, you need to be familiar with the evidence for or against various options—many of which can be used in conjunction with pharmacotherapy.
An integrative approach to the treatment of migraine headaches makes use of the best available evidence for both conventional and alternative therapies and takes into account the whole person, including all aspects of his or her belief system and lifestyle. It also emphasizes a strong physician-patient relationship, which can have a powerful therapeutic effect.
We wrote this evidence-based update with such an approach in mind. In the text and table that follow, we present the latest findings. But first, a brief review of what constitutes migraine headache and an overview of conventional treatment.
A conventional approach to migraine
Migraine headache is a common and disabling neurologic disorder that frequently goes unrecognized and undertreated.6 It is generally characterized as recurrent headaches that are unilateral, pulsating, moderately severe, aggravated by physical activity, and associated with nausea, vomiting, photophobia, phonophobia, and sometimes a preceding aura. Conventional treatment typically includes abortive treatment for acute migraine, with medications such as the triptans and dihydroergotamine. Acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and the combination of acetaminophen/aspirin/caffeine are also effective. Opiates are efficacious, but not recommended.7
Prophylactic medications are generally offered to patients experiencing more than 4 migraines per month. The American Academy of Neurology cites strong evidence for the use of divalproex, valproate, topiramate, and beta-blockers, including metoprolol, propranolol, and timolol. Frovatriptan has strong evidence for prevention of menstrual-associated migraine. Common adverse effects include weight loss and parasthesias with topiramate and weight gain and somnolence with valproate, divalproex, and beta-blockers. There is also moderate evidence for the use of amitriptyline, venlafaxine, atenolol, and nadolol. Potential adverse effects must be considered to determine the optimal therapy for individual patients, and trial and error are often required.8
Addressing triggers
Conventional treatment also focuses on identifying and avoiding triggers to the extent possible. Physicians typically advise patients to keep a headache diary, recording details about diet and lifestyle, triggers, frequency and intensity of attacks, and possible patterns of headaches due to medication overuse.
Sleep disturbances and stress are common triggers, and instruction in sleep hygiene and stress reduction, as well as screening for anxiety or depression, can be beneficial. Other frequently reported factors believed to trigger or aggravate migraine attacks are skipping meals, particular foods, alcohol, weather changes, and exposure to light, sounds, and odors.
Despite the focus on migraine triggers, however, clinical studies of the role they play have shown conflicting results. A recent study involving 27 patients7 found that when attempting to provoke migraine with aura using participants’ self-reported triggers, only 3 individuals reported that the provocation actually led to a migraine.9 Additional studies suggest that exposure to headache triggers has the same effect as exposure to anxiety, with short-term exposure associated with an increased pain response and prolonged exposure leading to a decreased response.10,11 Thus, it may be beneficial to advise patients to learn to cope with controlled exposure to triggers rather than to aim for trigger avoidance.12
If noise is identified as a trigger, for instance, repeated exposure in a relaxed environment can help desensitize the patient. Triggers such as visual disturbances and odors are also good candidates for desensitization, while others, such as sleep deprivation and skipping meals, are better served by avoidance.12
CAM approaches: A look at the evidence
Acupuncture, butterbur, feverfew, magnesium, riboflavin, and biofeedback look promising for migraine prevention. Many of our patients are already using these and other alternative therapies. Here’s what the latest studies show (TABLE).2,9-11, 13-51
Can acupuncture help?
A 2009 Cochrane review of 22 high-quality studies with a total of 4419 participants supports the use of acupuncture for migraine prophylaxis.13 Acupuncture was found to be superior to no prophylactic treatment and acute treatment alone, and as effective as conventional preventive medications. Interestingly, though, among studies included in the Cochrane review that compared true acupuncture with sham interventions, no significant difference in results was found.
A more recent meta-analysis of 29 studies representing nearly 18,000 patients did show true acupuncture to be statistically superior to sham acupuncture, although the difference was of small clinical significance. Sham acupuncture was also shown to have a larger clinical effect than oral placebos, raising questions about the importance of exact point location.14
In a 2015 study comparing real and sham acupuncture over a 20-week period, however, the differences were more marked. Those who received real acupuncture reported significantly fewer migraine days and less severe headaches, and there were more responders in the treatment group compared with recipients of the sham procedures.15 Overall, the evidence indicates that acupuncture is at least as effective as conventional drug treatment for migraine prophylaxis, but with fewer adverse effects.13-17
Butterbur raises concerns about toxicity
Butterbur (Petasites hybridus) is one of the best-studied natural remedies for migraine. The research has primarily focused on an extract of 15% petasin and isopetasin sold under the trade name Petadolex. A study of patients using this herbal preparation for 16 weeks showed a response rate of 48% for reduction in headache frequency among those taking 75 mg twice daily and a 36% reduction in those taking 50 mg twice a day. The primary adverse effect was burping.18
Proper processing is crucial. The key concern about butterbur is that it naturally contains hepatotoxic compounds called pyrrolizidine alkaloids (PA), which may remain if the product is not properly processed.18-20 The labeling on many butterbur products states that they are “PA-free,” but because the manufacturers, rather than the US Food and Drug Administration (FDA), bear the responsibility for the safety and labeling of supplements, there is little oversight.
In fact, supplement quality is of considerable concern and subject to ongoing research. DNA bar-coding studies have confirmed that many common herbal preparations either contain ingredients not listed on the label or, conversely, fail to contain all the ingredients that are listed.52 Patients should be advised to look for evidence of quality assurance when purchasing herbal supplements, such as that offered by the US Pharmacopeia (USP) on a limited range of products. (We have not found any butterbur supplements with USP verification.)
Feverfew yields mixed results
Studies of feverfew extract for migraine have had conflicting results, probably because different extracts have been tested. A recent Cochrane review, however, cited one clinical trial (N=218) that added positive evidence to previously inconclusive findings.21
The study in question assessed a proprietary extract of feverfew (MIG-99) and found a small decrease in frequency of migraines (0.6 per month) compared with placebo. Adverse effects were gastrointestinal disturbances and mouth ulcers.22
Warn women of childbearing age that feverfew may cause uterine contractions and is contraindicated for those who are pregnant or trying to conceive.23 In addition, patients who are allergic to ragweed, chrysanthemums, or other members of the daisy family may be allergic to feverfew, as well.24
Magnesium is helpful for some
While magnesium is used for both acute relief of migraine and as prophylaxis, evidence of its efficacy is mixed. Studies have been promising in women with low magnesium levels and those who suffer from menstrual migraines, and for use in children with migraine headaches as both acute and preventive treatment.25,26
One RCT involving 160 children ages 5 to 16 years found magnesium to have a synergistic effect with acetaminophen or ibuprofen, leading to greater acute pain relief and reducing migraine frequency.27 A recent meta-analysis, however, concluded that intravenous magnesium is not likely to be effective for acute treatment.53 The main adverse effects seen with magnesium are diarrhea and soft stools.
Patients with renal disease should avoid magnesium supplementation. Food sources of magnesium include whole grains, spinach, nuts, legumes, and white potatoes.54
Riboflavin shows promise
Riboflavin (B2) plays an important role in cellular energy production and is an important antioxidant in mitochondria. Several small studies have shown promising results with high-dose (400 mg) riboflavin in migraine prevention, with evidence suggesting that it may be as effective as beta-blockers such as bisoprolol and metoprolol.28-30 Discoloration of urine, which turns bright yellow, is the primary adverse effect.
CoQ10 helps those with low levels
Like riboflavin, coenzyme Q10 (CoQ10) is involved in mitochondrial transport and plays an important role in cellular energy metabolism. Several small studies have shown efficacy in migraine prevention in doses of 150 to 300 mg/d, with response rates between 30% and 50%.31,32 Based on data in adults, the American Academy of Neurology guidelines give CoQ10 a Level C rating, indicating that it is possibly effective in preventing migraine.29
An open label study of children with migraine found that close to a third were below the reference range for CoQ10 levels. Their serum levels increased when they began taking CoQ10 supplements, resulting in a significant reduction in headache frequency and an improvement in migraine-related disability.33
Combination supplements have little efficacy
In a study published in 2015,34 a proprietary supplement containing magnesium 600 mg, riboflavin 400 mg, CoQ10 150 mg, and low-dose multivitamins, taken daily, did not show statistically significant efficacy in the reduction of migraine days. After 3 months of supplementation, however, the severity of migraine pain improved. Adverse effects included abdominal discomfort and diarrhea.
Another study compared a combination of riboflavin 400 mg, magnesium 300 mg, and feverfew 100 mg with low-dose riboflavin (25 mg) as placebo, and found that the combination did not reduce the frequency or severity of migraine any more than the placebo.35
Botox may relieve chronic migraine
Onabotulinumtoxin A (Botox) has FDA approval for the prevention of chronic migraines—ie, migraines that occur >15 days per month and at least 4 hours or more per day.55 Botox is administered by injection every 12 weeks, across 31 sites on the head and neck. The recommended dose is 155 units, with 5 units delivered into each injection site.
This protocol has been found to reduce the number of headache days by 50% in half of those being treated after one cycle, and in more than 70% of patients after 3 cycles.36 Potential adverse effects include blepharoptosis, neck muscle weakness, and the risk of botulism at sites distant from the injections.37-39
Mind-body therapies are most widely used
Of all the CAM therapies used by patients with migraine headaches, mind-body modalities are the most prevalent. Overall, 30% of headache patients use them, compared with 17% of the general population.2
Many of these modalities have been found to be effective and safe to use with the conventional migraine treatments with which patients commonly combine them.
Meditation. Both spiritual and secular forms of meditation have been studied for acute and preventive treatment of migraine and found to be effective. A recent small study suggests that spiritual meditation may be more effective,40 but secular mindfulness-based stress reduction training has also shown promise in migraine treatment.
One positive effect is that those who meditate typically use less migraine medication,41 decreasing the burden of disease. Meditation is increasingly available via a range of options, including both in-person groups and online sessions, and can easily augment conventional medical treatments.
Yoga, which typically combines physical postures, breathing techniques, and mental concentration/meditation, is increasingly widespread. While there is compelling evidence of its effect in treating chronic pain and stress-related conditions,42 studies specific to migraine are lacking. Several small studies comparing yoga to NSAIDs, educational handouts, and conventional care for headache suggest that yoga has efficacy for the treatment of migraine, but the findings are limited by methodology and sample size.42,43
Relaxation training. Various types of relaxation are described in the literature, often combining progressive muscle relaxation, diaphragmatic breathing, and relaxation-inducing imagery. Although the consensus is that these techniques are effective, differences in standards, frequency, and duration of training make it hard to draw conclusions.44
Biofeedback is similar to relaxation training, with the key difference being that it uses monitoring to train patients to alter their physiological state, thereby leading to desired changes—eg, fewer headaches and lower intensity of pain. Monitors evaluate skin temperature, electromyography, heart rate variability (blood-volume-pulse), and skin conductance, among other measures.
A robust collection of studies has shown the efficacy of skin temperature feedback, blood-volume-pulse feedback, and electromyography feedback as treatment for migraine.45 Blood-volume-pulse feedback in combination with additional home training is perhaps more effective than other modalities. Despite convincing evidence of its efficacy for migraine headaches, however, only about 1% of patients with migraine use biofeedback. That’s likely due to a lack of availability outside of urban medical centers, limited insurance coverage, and time constraints.2,45
Behavioral therapy can be of help
Cognitive behavioral therapy (CBT) focuses on adjusting maladaptive thoughts and behaviors. For migraine patients, this may include identifying and changing the patient’s response to migraine triggers such as stress, sleep deprivation, and fear of headache pain. Relaxation techniques may be incorporated into the therapy.
The effect size of CBT for prevention is comparable to prophylactic medication use, with 34% to 40% of patients achieving a clinically significant decrease in the number of attacks. Additive effects are especially promising, with more than two-thirds of patients achieving decreased frequency when CBT is combined with preventative medications.2,44,46
Acceptance and commitment therapy (ACT) is a newer variant of CBT that has recently been studied.44 Unlike CBT, in which patients are taught to control and revise their maladaptive thoughts and feelings, ACT focuses on noticing and accepting such unwanted thoughts and feelings and changing the way individuals respond to them rather than changing the thoughts themselves. Further study is needed to determine whether ACT is an effective treatment for migraine.
FDA-approved devices take aim at migraine
A transcranial magnetic stimulator (TMS) (Cerena, eNeura Inc, Sunnyvale, Calif) received FDA approval in 2013.56 The single-pulse TMS is the first device authorized for the treatment of migraine headache pain. It is geared specifically to patients suffering from migraine with aura and requires a prescription.
In a study of 201 patients, the group using the TMS device at the onset of aura had a 38% response rate, compared with a 17% response among those in the sham control group. Dizziness was reported as an adverse effect. Caution patients who express an interest in it that the device should not be used by those who are at risk for seizures or have an implanted device, such as a pacemaker or deep brain stimulator.47
Transcutaneous electrical nerve stimulation (TENS) has long been used for chronic pain, but in 2014 the FDA approved the first TENS device aimed at the prevention of migraine headaches in patients age 18 and older.57 It is also the first such device approved for use prior to the onset of pain.
The Cefaly (Cefaly US, Inc., Wilton, Conn), which requires a prescription, is worn like a headband. It is positioned on the forehead just above the eyes, using an adhesive electrode, and is worn once a day for 20 minutes. The device applies an electrical current to the skin and underlying tissues to stimulate branches of the trigeminal nerve, which can cause a tingling or massaging sensation. Several small studies have shown a decrease in migraine frequency comparable with other preventive treatments. The main adverse effect reported was sedation, but more than half of those who used it were satisfied and willing to purchase the device.48,49
Regular exercise has little downside
While physical activity can be a trigger for acute migraine, regular exercise has been shown to decrease the frequency of migraine attacks. And, although aerobic exercise is no more effective as migraine prophylaxis than conventional drug treatments, it has few adverse effects. For patients who want to stay fit and avoid taking preventive medications, exercise is a valuable adjunct to conventional treatments.50,51
CORRESPONDENCE
Laura Armstrong, MD, Memorial Hermann Family Medicine Residency Program, 14023 Southwest Freeway, Sugar Land, TX 77478; laura.armstrong@memorialhermann.org.
› Ask all patients with migraines about their use of complementary and alternative medicine and what modalities, if any, they have found helpful. A
› Advise patients that while butterbur has been proven effective at reducing migraine frequency, its use requires caution, as products not processed properly may contain hepatotoxic compounds. A
› Caution women who are pregnant or attempting to conceive to avoid feverfew, which may cause uterine contractions. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Americans who suffer from migraine headaches are far more likely than those who don’t to turn to complementary and alternative medicine (CAM). A 2007 National Health Interview Survey and a subsequent analysis of the results found that just under 50% of adults with migraine headaches used alternative therapies; among those without migraine, 34% did.1,2 What’s more, only about half of the migraine patients who reported the use of CAM modalities mentioned it to their health care providers.2
With migraine affecting some 36 million Americans,3 chances are you are caring for many of them. It is likely, too, that you are unaware of which of your headache patients are using alternative treatments, or what modalities they have tried. The only way to find out is to ask.
Women, who are 3 times more likely than men to suffer from migraine headache,4 are also the greatest users of CAM, particularly biologically based therapies and mind-body practices.5 Use is highly individualized and typically does not involve professional supervision.5
A number of alternative modalities look promising for migraine prevention. As a family physician, you are in an ideal position to guide patients in the use of safe and effective CAM therapies. To do so, however, you need to be familiar with the evidence for or against various options—many of which can be used in conjunction with pharmacotherapy.
An integrative approach to the treatment of migraine headaches makes use of the best available evidence for both conventional and alternative therapies and takes into account the whole person, including all aspects of his or her belief system and lifestyle. It also emphasizes a strong physician-patient relationship, which can have a powerful therapeutic effect.
We wrote this evidence-based update with such an approach in mind. In the text and table that follow, we present the latest findings. But first, a brief review of what constitutes migraine headache and an overview of conventional treatment.
A conventional approach to migraine
Migraine headache is a common and disabling neurologic disorder that frequently goes unrecognized and undertreated.6 It is generally characterized as recurrent headaches that are unilateral, pulsating, moderately severe, aggravated by physical activity, and associated with nausea, vomiting, photophobia, phonophobia, and sometimes a preceding aura. Conventional treatment typically includes abortive treatment for acute migraine, with medications such as the triptans and dihydroergotamine. Acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and the combination of acetaminophen/aspirin/caffeine are also effective. Opiates are efficacious, but not recommended.7
Prophylactic medications are generally offered to patients experiencing more than 4 migraines per month. The American Academy of Neurology cites strong evidence for the use of divalproex, valproate, topiramate, and beta-blockers, including metoprolol, propranolol, and timolol. Frovatriptan has strong evidence for prevention of menstrual-associated migraine. Common adverse effects include weight loss and parasthesias with topiramate and weight gain and somnolence with valproate, divalproex, and beta-blockers. There is also moderate evidence for the use of amitriptyline, venlafaxine, atenolol, and nadolol. Potential adverse effects must be considered to determine the optimal therapy for individual patients, and trial and error are often required.8
Addressing triggers
Conventional treatment also focuses on identifying and avoiding triggers to the extent possible. Physicians typically advise patients to keep a headache diary, recording details about diet and lifestyle, triggers, frequency and intensity of attacks, and possible patterns of headaches due to medication overuse.
Sleep disturbances and stress are common triggers, and instruction in sleep hygiene and stress reduction, as well as screening for anxiety or depression, can be beneficial. Other frequently reported factors believed to trigger or aggravate migraine attacks are skipping meals, particular foods, alcohol, weather changes, and exposure to light, sounds, and odors.
Despite the focus on migraine triggers, however, clinical studies of the role they play have shown conflicting results. A recent study involving 27 patients7 found that when attempting to provoke migraine with aura using participants’ self-reported triggers, only 3 individuals reported that the provocation actually led to a migraine.9 Additional studies suggest that exposure to headache triggers has the same effect as exposure to anxiety, with short-term exposure associated with an increased pain response and prolonged exposure leading to a decreased response.10,11 Thus, it may be beneficial to advise patients to learn to cope with controlled exposure to triggers rather than to aim for trigger avoidance.12
If noise is identified as a trigger, for instance, repeated exposure in a relaxed environment can help desensitize the patient. Triggers such as visual disturbances and odors are also good candidates for desensitization, while others, such as sleep deprivation and skipping meals, are better served by avoidance.12
CAM approaches: A look at the evidence
Acupuncture, butterbur, feverfew, magnesium, riboflavin, and biofeedback look promising for migraine prevention. Many of our patients are already using these and other alternative therapies. Here’s what the latest studies show (TABLE).2,9-11, 13-51
Can acupuncture help?
A 2009 Cochrane review of 22 high-quality studies with a total of 4419 participants supports the use of acupuncture for migraine prophylaxis.13 Acupuncture was found to be superior to no prophylactic treatment and acute treatment alone, and as effective as conventional preventive medications. Interestingly, though, among studies included in the Cochrane review that compared true acupuncture with sham interventions, no significant difference in results was found.
A more recent meta-analysis of 29 studies representing nearly 18,000 patients did show true acupuncture to be statistically superior to sham acupuncture, although the difference was of small clinical significance. Sham acupuncture was also shown to have a larger clinical effect than oral placebos, raising questions about the importance of exact point location.14
In a 2015 study comparing real and sham acupuncture over a 20-week period, however, the differences were more marked. Those who received real acupuncture reported significantly fewer migraine days and less severe headaches, and there were more responders in the treatment group compared with recipients of the sham procedures.15 Overall, the evidence indicates that acupuncture is at least as effective as conventional drug treatment for migraine prophylaxis, but with fewer adverse effects.13-17
Butterbur raises concerns about toxicity
Butterbur (Petasites hybridus) is one of the best-studied natural remedies for migraine. The research has primarily focused on an extract of 15% petasin and isopetasin sold under the trade name Petadolex. A study of patients using this herbal preparation for 16 weeks showed a response rate of 48% for reduction in headache frequency among those taking 75 mg twice daily and a 36% reduction in those taking 50 mg twice a day. The primary adverse effect was burping.18
Proper processing is crucial. The key concern about butterbur is that it naturally contains hepatotoxic compounds called pyrrolizidine alkaloids (PA), which may remain if the product is not properly processed.18-20 The labeling on many butterbur products states that they are “PA-free,” but because the manufacturers, rather than the US Food and Drug Administration (FDA), bear the responsibility for the safety and labeling of supplements, there is little oversight.
In fact, supplement quality is of considerable concern and subject to ongoing research. DNA bar-coding studies have confirmed that many common herbal preparations either contain ingredients not listed on the label or, conversely, fail to contain all the ingredients that are listed.52 Patients should be advised to look for evidence of quality assurance when purchasing herbal supplements, such as that offered by the US Pharmacopeia (USP) on a limited range of products. (We have not found any butterbur supplements with USP verification.)
Feverfew yields mixed results
Studies of feverfew extract for migraine have had conflicting results, probably because different extracts have been tested. A recent Cochrane review, however, cited one clinical trial (N=218) that added positive evidence to previously inconclusive findings.21
The study in question assessed a proprietary extract of feverfew (MIG-99) and found a small decrease in frequency of migraines (0.6 per month) compared with placebo. Adverse effects were gastrointestinal disturbances and mouth ulcers.22
Warn women of childbearing age that feverfew may cause uterine contractions and is contraindicated for those who are pregnant or trying to conceive.23 In addition, patients who are allergic to ragweed, chrysanthemums, or other members of the daisy family may be allergic to feverfew, as well.24
Magnesium is helpful for some
While magnesium is used for both acute relief of migraine and as prophylaxis, evidence of its efficacy is mixed. Studies have been promising in women with low magnesium levels and those who suffer from menstrual migraines, and for use in children with migraine headaches as both acute and preventive treatment.25,26
One RCT involving 160 children ages 5 to 16 years found magnesium to have a synergistic effect with acetaminophen or ibuprofen, leading to greater acute pain relief and reducing migraine frequency.27 A recent meta-analysis, however, concluded that intravenous magnesium is not likely to be effective for acute treatment.53 The main adverse effects seen with magnesium are diarrhea and soft stools.
Patients with renal disease should avoid magnesium supplementation. Food sources of magnesium include whole grains, spinach, nuts, legumes, and white potatoes.54
Riboflavin shows promise
Riboflavin (B2) plays an important role in cellular energy production and is an important antioxidant in mitochondria. Several small studies have shown promising results with high-dose (400 mg) riboflavin in migraine prevention, with evidence suggesting that it may be as effective as beta-blockers such as bisoprolol and metoprolol.28-30 Discoloration of urine, which turns bright yellow, is the primary adverse effect.
CoQ10 helps those with low levels
Like riboflavin, coenzyme Q10 (CoQ10) is involved in mitochondrial transport and plays an important role in cellular energy metabolism. Several small studies have shown efficacy in migraine prevention in doses of 150 to 300 mg/d, with response rates between 30% and 50%.31,32 Based on data in adults, the American Academy of Neurology guidelines give CoQ10 a Level C rating, indicating that it is possibly effective in preventing migraine.29
An open label study of children with migraine found that close to a third were below the reference range for CoQ10 levels. Their serum levels increased when they began taking CoQ10 supplements, resulting in a significant reduction in headache frequency and an improvement in migraine-related disability.33
Combination supplements have little efficacy
In a study published in 2015,34 a proprietary supplement containing magnesium 600 mg, riboflavin 400 mg, CoQ10 150 mg, and low-dose multivitamins, taken daily, did not show statistically significant efficacy in the reduction of migraine days. After 3 months of supplementation, however, the severity of migraine pain improved. Adverse effects included abdominal discomfort and diarrhea.
Another study compared a combination of riboflavin 400 mg, magnesium 300 mg, and feverfew 100 mg with low-dose riboflavin (25 mg) as placebo, and found that the combination did not reduce the frequency or severity of migraine any more than the placebo.35
Botox may relieve chronic migraine
Onabotulinumtoxin A (Botox) has FDA approval for the prevention of chronic migraines—ie, migraines that occur >15 days per month and at least 4 hours or more per day.55 Botox is administered by injection every 12 weeks, across 31 sites on the head and neck. The recommended dose is 155 units, with 5 units delivered into each injection site.
This protocol has been found to reduce the number of headache days by 50% in half of those being treated after one cycle, and in more than 70% of patients after 3 cycles.36 Potential adverse effects include blepharoptosis, neck muscle weakness, and the risk of botulism at sites distant from the injections.37-39
Mind-body therapies are most widely used
Of all the CAM therapies used by patients with migraine headaches, mind-body modalities are the most prevalent. Overall, 30% of headache patients use them, compared with 17% of the general population.2
Many of these modalities have been found to be effective and safe to use with the conventional migraine treatments with which patients commonly combine them.
Meditation. Both spiritual and secular forms of meditation have been studied for acute and preventive treatment of migraine and found to be effective. A recent small study suggests that spiritual meditation may be more effective,40 but secular mindfulness-based stress reduction training has also shown promise in migraine treatment.
One positive effect is that those who meditate typically use less migraine medication,41 decreasing the burden of disease. Meditation is increasingly available via a range of options, including both in-person groups and online sessions, and can easily augment conventional medical treatments.
Yoga, which typically combines physical postures, breathing techniques, and mental concentration/meditation, is increasingly widespread. While there is compelling evidence of its effect in treating chronic pain and stress-related conditions,42 studies specific to migraine are lacking. Several small studies comparing yoga to NSAIDs, educational handouts, and conventional care for headache suggest that yoga has efficacy for the treatment of migraine, but the findings are limited by methodology and sample size.42,43
Relaxation training. Various types of relaxation are described in the literature, often combining progressive muscle relaxation, diaphragmatic breathing, and relaxation-inducing imagery. Although the consensus is that these techniques are effective, differences in standards, frequency, and duration of training make it hard to draw conclusions.44
Biofeedback is similar to relaxation training, with the key difference being that it uses monitoring to train patients to alter their physiological state, thereby leading to desired changes—eg, fewer headaches and lower intensity of pain. Monitors evaluate skin temperature, electromyography, heart rate variability (blood-volume-pulse), and skin conductance, among other measures.
A robust collection of studies has shown the efficacy of skin temperature feedback, blood-volume-pulse feedback, and electromyography feedback as treatment for migraine.45 Blood-volume-pulse feedback in combination with additional home training is perhaps more effective than other modalities. Despite convincing evidence of its efficacy for migraine headaches, however, only about 1% of patients with migraine use biofeedback. That’s likely due to a lack of availability outside of urban medical centers, limited insurance coverage, and time constraints.2,45
Behavioral therapy can be of help
Cognitive behavioral therapy (CBT) focuses on adjusting maladaptive thoughts and behaviors. For migraine patients, this may include identifying and changing the patient’s response to migraine triggers such as stress, sleep deprivation, and fear of headache pain. Relaxation techniques may be incorporated into the therapy.
The effect size of CBT for prevention is comparable to prophylactic medication use, with 34% to 40% of patients achieving a clinically significant decrease in the number of attacks. Additive effects are especially promising, with more than two-thirds of patients achieving decreased frequency when CBT is combined with preventative medications.2,44,46
Acceptance and commitment therapy (ACT) is a newer variant of CBT that has recently been studied.44 Unlike CBT, in which patients are taught to control and revise their maladaptive thoughts and feelings, ACT focuses on noticing and accepting such unwanted thoughts and feelings and changing the way individuals respond to them rather than changing the thoughts themselves. Further study is needed to determine whether ACT is an effective treatment for migraine.
FDA-approved devices take aim at migraine
A transcranial magnetic stimulator (TMS) (Cerena, eNeura Inc, Sunnyvale, Calif) received FDA approval in 2013.56 The single-pulse TMS is the first device authorized for the treatment of migraine headache pain. It is geared specifically to patients suffering from migraine with aura and requires a prescription.
In a study of 201 patients, the group using the TMS device at the onset of aura had a 38% response rate, compared with a 17% response among those in the sham control group. Dizziness was reported as an adverse effect. Caution patients who express an interest in it that the device should not be used by those who are at risk for seizures or have an implanted device, such as a pacemaker or deep brain stimulator.47
Transcutaneous electrical nerve stimulation (TENS) has long been used for chronic pain, but in 2014 the FDA approved the first TENS device aimed at the prevention of migraine headaches in patients age 18 and older.57 It is also the first such device approved for use prior to the onset of pain.
The Cefaly (Cefaly US, Inc., Wilton, Conn), which requires a prescription, is worn like a headband. It is positioned on the forehead just above the eyes, using an adhesive electrode, and is worn once a day for 20 minutes. The device applies an electrical current to the skin and underlying tissues to stimulate branches of the trigeminal nerve, which can cause a tingling or massaging sensation. Several small studies have shown a decrease in migraine frequency comparable with other preventive treatments. The main adverse effect reported was sedation, but more than half of those who used it were satisfied and willing to purchase the device.48,49
Regular exercise has little downside
While physical activity can be a trigger for acute migraine, regular exercise has been shown to decrease the frequency of migraine attacks. And, although aerobic exercise is no more effective as migraine prophylaxis than conventional drug treatments, it has few adverse effects. For patients who want to stay fit and avoid taking preventive medications, exercise is a valuable adjunct to conventional treatments.50,51
CORRESPONDENCE
Laura Armstrong, MD, Memorial Hermann Family Medicine Residency Program, 14023 Southwest Freeway, Sugar Land, TX 77478; laura.armstrong@memorialhermann.org.
1. National Center for Complementary and Integrative Health. 2007 Statistics on CAM Use in the United States. National Center for Complementary and Integrative Health Web site. Available at: https://nccih.nih.gov/news/camstats/2007. Accessed January 6, 2016.
2. Wells RE, Bertisch SM, Buettner C, et al. Complementary and alternative medicine use among adults with migraines/severe headaches. Headache. 2011;51:1087-1097.
3. Lipton RB, Silberstein SD. Episodic and chronic migraine headache: breaking down barriers to optimal treatment and prevention. Headache. 2015;55:S103-S122.
4. Migraine Research Foundation. Migraine in women. Migraine Research Foundation Web site. Available at: http://www.migraineresearchfoundation.org/Migraine%20in%20Women.html. Accessed January 7, 2016.
5. Clarke TC, Black LI, Stussman BJ, et al. Trends in the use of complementary health approaches among adults: United States, 2002-2012. Natl Health Stat Report. 2015:1-16.
6. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd ed. Cephalalgia. 2013;33:629-808.
7. Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the American Headache Society evidence assessment of migraine pharmacotherapies. Headache. 2015;55:3-20.
8. Silberstein SD, Holland S, Freitag F, et al; Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78:1337-1345.
9. Hougaard A, Amin FM, Hauge AW, et al. Provocation of migraine with aura using natural trigger factors. Neurology. 2013;80:428-431.
10. Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27:394-402.
11. Martin PR. Managing headache triggers: Think ‘coping’ not ‘avoidance’. Cephalalgia. 2010;30:634-637.
12. Martin PR, MacLeod C. Behavioral management of headache triggers: Avoidance of triggers is an inadequate strategy. Clin Psychol Rev. 2009;29:483-495.
13. Linde K, Allais G, Brinkhaus B, et al. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009:CD001218.
14. Vickers AJ, Cronin AM, Maschino AC, et al; Acupuncture Trialists’ Collaboration. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444-1453.
15. Wang Y, Xue CC, Helme R, et al. Acupuncture for frequent migraine: A randomized, patient/assessor blinded, controlled trial with one-year follow-up. Evid Based Complement Alternat Med. 2015;2015:920353.
16. Da Silva AN. Acupuncture for migraine prevention. Headache. 2015;55:470-473.
17. Meissner K, Fassler M, Rücker G, et al. Differential effectiveness of placebo treatments: a systematic review of migraine prophylaxis. JAMA Intern Med. 2013;173:1941-1951.
18. Lipton RB, Göbel H, Einhäupl KM, et al. Petasites hybridus root (butterbur) is an effective preventive treatment for migraine. Neurology. 2004;63:2240-2244.
19. Grossman W, Schmidramsl H. An extract of Petasites hybridus is effective in the prophylaxis of migraine. Altern Med Rev. 2001;6:303-310.
20. Diener HC, Rahlfs VW, Danesch U. The first placebo-controlled trial of a special butterbur root extract for the prevention of migraine: Reanalysis of efficacy criteria. Eur Neurol. 2004;51:89-97.
21. Wider B, Pittler MH, Ernst E. Feverfew for preventing migraine. Cochrane Database Syst Rev. 2015;4:CD002286.
22. Pfaffenrath V, Diener HC, Fischer M, et al; Investigators. The efficacy and safety of Tanacetum parthenium (feverfew) in migraine prophylaxis--a double-blind, multicentre, randomized placebo-controlled dose-response study. Cephalalgia. 2002;22:523-532.
23. Ernst E, Pittler MH. The efficacy and safety of feverfew (Tanacetum parthenium L.): an update of a systematic review. Public Health Nutr. 2000;3:509-514.
24. Natural Medicines. Feverfew Professional Monograph, 2016. Natural Medicines Web site. Available at: https://naturalmedicines.therapeuticresearch.com/. Accessed January 1, 2016.
25. Wang F, Van Den Eeden SK, Ackerson LM, et al. Oral magnesium oxide prophylaxis of frequent migrainous headache in children: a randomized, double-blind, placebo-controlled trial. Headache. 2003;43:601-610.
26. Facchinetti F, Sances G, Borella P, et al. Magnesium prophylaxis of menstrual migraine: effects on intracellular magnesium. Headache. 1991;31:298-301.
27. Gallelli L, Avenoso T, Falcone D, et al. Effects of acetaminophen and ibuprofen in children with migraine receiving preventive treatment with magnesium. Headache. 2014;54:313-324.
28. Sándor PS, Afra J, Ambrosini A, et al. Prophylactic treatment of migraine with beta-blockers and riboflavin: differential effects on the intensity dependence of auditory evoked cortical potentials. Headache. 2000;40:30-35.
29. Holland S, Silberstein SD, Freitag F, et al; Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78:1346-1353.
30. Boehnke C, Reuter U, Flach U, et al. High-dose riboflavin treatment is efficacious in migraine prophylaxis: an open study in a tertiary care centre. Eur J Neurol. 2004;11:475-477.
31. Sándor PS, Di Clemente L, Coppola G, et al. Efficacy of coenzyme Q10 in migraine prophylaxis: a randomized controlled trial. Neurology. 2005;64:713-715.
32. Rozen TD, Oshinsky ML, Gebeline CA, et al. Open label trial of coenzyme Q10 as a migraine preventive. Cephalalgia. 2002;22:137-141.
33. Hershey AD, Powers SW, Vockell AL, et al. Coenzyme Q10 deficiency and response to supplementation in pediatric and adolescent migraine. Headache. 2007;47:73-80.
34. Gaul C, Diener HC, Danesch U; Migravent Study Group. Improvement of migraine symptoms with a proprietary supplement containing riboflavin, magnesium and Q10: a randomized, placebo-controlled, double-blind, multicenter trial. J Headache Pain. 2015;16:516.
35. Maizels M, Blumenfeld A, Burchette R. A combination of riboflavin, magnesium, and feverfew for migraine prophylaxis: a randomized trial. Headache. 2004;44:885-890.
36. Silberstein SD, Dodick DW, Aurora SK, et al. Percent of patients with chronic migraine who responded per onabotulinumtoxin A treatment cycle: PREEMPT. J Neurol Neurosurg Psychiatry. 2015;86:996-1001.
37. Estemalik E, Tepper S. Preventive treatment in migraine and the new US guidelines. Neuropsychiatr Dis Treat. 2013;9:709-720.
38. Aurora SK, Winner P, Freeman MC, et al. Onabotulinumtoxin A for treatment of chronic migraine: pooled analyses of the 56-week PREEMPT clinical program. Headache. 2011;51:1358-1373.
39. Diener HC, Dodick DW, Aurora SK, et al; PREEMPT 2 Chronic Migraine Study Group. Onabotulinumtoxin A for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 2 trial. Cephalalgia. 2010;30:804-814.
40. Wachholtz AB, Malone CD, Pargament KI. Effect of different meditation types on migraine headache medication use. Behav Med. 2015:1-8.
41. Smitherman TA, Wells RE, Ford SG. Emerging behavioral treatments for migraine. Curr Pain Headache Rep. 2015;19:13.
42. Kisan R, Sujan M, Adoor M, et al. Effect of yoga on migraine: A comprehensive study using clinical profile and cardiac autonomic functions. Int J Yoga. 2014;7:126-132.
43. Büssing A, Ostermann T, Lüdtke R, et al. Effects of yoga interventions on pain and pain-associated disability: a meta-analysis. J Pain. 2012;13:1-9.
44. Penzien DB, Irby MB, Smitherman TA, et al. Well-established and empirically supported behavioral treatments for migraine. Curr Pain Headache Rep. 2015;19:34.
45. Nestoriuc Y, Martin A. Efficacy of biofeedback for migraine: a meta-analysis. Pain. 2007;128:111-127.
46. Fritsche G, Kröner-Herwig B, Kropp P, et al. Psychological therapy of migraine: systematic review. Schmerz. 2013;27:263-274.
47. Lipton RB, Dodick DW, Silberstein SD, et al. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomised, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. 2010;9:373-380.
48. Schoenen J, Vandersmissen B, Jeangette S, et al. Migraine prevention with a supraorbital transcutaneous stimulator: a randomized controlled trial. Neurology. 2013;80:697-704.
49. Piquet M, Balestra C, Sava SL, et al. Supraorbital transcutaneous neurostimulation has sedative effects in healthy subjects. BMC Neurol. 2011;11:135.
50. Gil-Martínez A, Kindelan-Calvo P, Agudo-Carmona D, et al. Therapeutic exercise as treatment for migraine and tension-type headaches: a systematic review of randomised clinical trials. Rev Neurol. 2013;57:433-443.
51. Varkey E, Cider A, Carlsson J, et al. Exercise as migraine prophylaxis: a randomized study using relaxation and topiramate as controls. Cephalalgia. 2011;31:1428-1438.
52. Newmaster SG, Grguric M, Shanmughanandhan D, et al. DNA barcoding detects contamination and substitution in North American herbal products. BMC Med. 2013;11:222.
53. Choi H, Parmar N. The use of intravenous magnesium sulphate for acute migraine: meta-analysis of randomized controlled trials. Eur J Emerg Med. 2014;21:2-9.
54. Volpe SL. Magnesium in disease prevention and overall health. Adv Nutr. 2013;4:S378-S383.
55. US Food and Drug Administration. FDA approves Botox to treat chronic migraine. US Food and Drug Administration Web site. October 15, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm229782.htm. Accessed January 7, 2016.
56. US Food and Drug Administration. FDA allows marketing of first device to relieve migraine headache pain. US Food and Drug Administration Web site. December 13, 2013. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm378608.htm. Accessed January 7, 2016.
57. US Food and Drug Administration. FDA allows marketing of first medical device to prevent migraine headache. US Food and Drug Administration Web site. March 11, 2014. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm388765.htm. Accessed January 7, 2016.
1. National Center for Complementary and Integrative Health. 2007 Statistics on CAM Use in the United States. National Center for Complementary and Integrative Health Web site. Available at: https://nccih.nih.gov/news/camstats/2007. Accessed January 6, 2016.
2. Wells RE, Bertisch SM, Buettner C, et al. Complementary and alternative medicine use among adults with migraines/severe headaches. Headache. 2011;51:1087-1097.
3. Lipton RB, Silberstein SD. Episodic and chronic migraine headache: breaking down barriers to optimal treatment and prevention. Headache. 2015;55:S103-S122.
4. Migraine Research Foundation. Migraine in women. Migraine Research Foundation Web site. Available at: http://www.migraineresearchfoundation.org/Migraine%20in%20Women.html. Accessed January 7, 2016.
5. Clarke TC, Black LI, Stussman BJ, et al. Trends in the use of complementary health approaches among adults: United States, 2002-2012. Natl Health Stat Report. 2015:1-16.
6. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd ed. Cephalalgia. 2013;33:629-808.
7. Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the American Headache Society evidence assessment of migraine pharmacotherapies. Headache. 2015;55:3-20.
8. Silberstein SD, Holland S, Freitag F, et al; Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78:1337-1345.
9. Hougaard A, Amin FM, Hauge AW, et al. Provocation of migraine with aura using natural trigger factors. Neurology. 2013;80:428-431.
10. Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27:394-402.
11. Martin PR. Managing headache triggers: Think ‘coping’ not ‘avoidance’. Cephalalgia. 2010;30:634-637.
12. Martin PR, MacLeod C. Behavioral management of headache triggers: Avoidance of triggers is an inadequate strategy. Clin Psychol Rev. 2009;29:483-495.
13. Linde K, Allais G, Brinkhaus B, et al. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009:CD001218.
14. Vickers AJ, Cronin AM, Maschino AC, et al; Acupuncture Trialists’ Collaboration. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444-1453.
15. Wang Y, Xue CC, Helme R, et al. Acupuncture for frequent migraine: A randomized, patient/assessor blinded, controlled trial with one-year follow-up. Evid Based Complement Alternat Med. 2015;2015:920353.
16. Da Silva AN. Acupuncture for migraine prevention. Headache. 2015;55:470-473.
17. Meissner K, Fassler M, Rücker G, et al. Differential effectiveness of placebo treatments: a systematic review of migraine prophylaxis. JAMA Intern Med. 2013;173:1941-1951.
18. Lipton RB, Göbel H, Einhäupl KM, et al. Petasites hybridus root (butterbur) is an effective preventive treatment for migraine. Neurology. 2004;63:2240-2244.
19. Grossman W, Schmidramsl H. An extract of Petasites hybridus is effective in the prophylaxis of migraine. Altern Med Rev. 2001;6:303-310.
20. Diener HC, Rahlfs VW, Danesch U. The first placebo-controlled trial of a special butterbur root extract for the prevention of migraine: Reanalysis of efficacy criteria. Eur Neurol. 2004;51:89-97.
21. Wider B, Pittler MH, Ernst E. Feverfew for preventing migraine. Cochrane Database Syst Rev. 2015;4:CD002286.
22. Pfaffenrath V, Diener HC, Fischer M, et al; Investigators. The efficacy and safety of Tanacetum parthenium (feverfew) in migraine prophylaxis--a double-blind, multicentre, randomized placebo-controlled dose-response study. Cephalalgia. 2002;22:523-532.
23. Ernst E, Pittler MH. The efficacy and safety of feverfew (Tanacetum parthenium L.): an update of a systematic review. Public Health Nutr. 2000;3:509-514.
24. Natural Medicines. Feverfew Professional Monograph, 2016. Natural Medicines Web site. Available at: https://naturalmedicines.therapeuticresearch.com/. Accessed January 1, 2016.
25. Wang F, Van Den Eeden SK, Ackerson LM, et al. Oral magnesium oxide prophylaxis of frequent migrainous headache in children: a randomized, double-blind, placebo-controlled trial. Headache. 2003;43:601-610.
26. Facchinetti F, Sances G, Borella P, et al. Magnesium prophylaxis of menstrual migraine: effects on intracellular magnesium. Headache. 1991;31:298-301.
27. Gallelli L, Avenoso T, Falcone D, et al. Effects of acetaminophen and ibuprofen in children with migraine receiving preventive treatment with magnesium. Headache. 2014;54:313-324.
28. Sándor PS, Afra J, Ambrosini A, et al. Prophylactic treatment of migraine with beta-blockers and riboflavin: differential effects on the intensity dependence of auditory evoked cortical potentials. Headache. 2000;40:30-35.
29. Holland S, Silberstein SD, Freitag F, et al; Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78:1346-1353.
30. Boehnke C, Reuter U, Flach U, et al. High-dose riboflavin treatment is efficacious in migraine prophylaxis: an open study in a tertiary care centre. Eur J Neurol. 2004;11:475-477.
31. Sándor PS, Di Clemente L, Coppola G, et al. Efficacy of coenzyme Q10 in migraine prophylaxis: a randomized controlled trial. Neurology. 2005;64:713-715.
32. Rozen TD, Oshinsky ML, Gebeline CA, et al. Open label trial of coenzyme Q10 as a migraine preventive. Cephalalgia. 2002;22:137-141.
33. Hershey AD, Powers SW, Vockell AL, et al. Coenzyme Q10 deficiency and response to supplementation in pediatric and adolescent migraine. Headache. 2007;47:73-80.
34. Gaul C, Diener HC, Danesch U; Migravent Study Group. Improvement of migraine symptoms with a proprietary supplement containing riboflavin, magnesium and Q10: a randomized, placebo-controlled, double-blind, multicenter trial. J Headache Pain. 2015;16:516.
35. Maizels M, Blumenfeld A, Burchette R. A combination of riboflavin, magnesium, and feverfew for migraine prophylaxis: a randomized trial. Headache. 2004;44:885-890.
36. Silberstein SD, Dodick DW, Aurora SK, et al. Percent of patients with chronic migraine who responded per onabotulinumtoxin A treatment cycle: PREEMPT. J Neurol Neurosurg Psychiatry. 2015;86:996-1001.
37. Estemalik E, Tepper S. Preventive treatment in migraine and the new US guidelines. Neuropsychiatr Dis Treat. 2013;9:709-720.
38. Aurora SK, Winner P, Freeman MC, et al. Onabotulinumtoxin A for treatment of chronic migraine: pooled analyses of the 56-week PREEMPT clinical program. Headache. 2011;51:1358-1373.
39. Diener HC, Dodick DW, Aurora SK, et al; PREEMPT 2 Chronic Migraine Study Group. Onabotulinumtoxin A for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 2 trial. Cephalalgia. 2010;30:804-814.
40. Wachholtz AB, Malone CD, Pargament KI. Effect of different meditation types on migraine headache medication use. Behav Med. 2015:1-8.
41. Smitherman TA, Wells RE, Ford SG. Emerging behavioral treatments for migraine. Curr Pain Headache Rep. 2015;19:13.
42. Kisan R, Sujan M, Adoor M, et al. Effect of yoga on migraine: A comprehensive study using clinical profile and cardiac autonomic functions. Int J Yoga. 2014;7:126-132.
43. Büssing A, Ostermann T, Lüdtke R, et al. Effects of yoga interventions on pain and pain-associated disability: a meta-analysis. J Pain. 2012;13:1-9.
44. Penzien DB, Irby MB, Smitherman TA, et al. Well-established and empirically supported behavioral treatments for migraine. Curr Pain Headache Rep. 2015;19:34.
45. Nestoriuc Y, Martin A. Efficacy of biofeedback for migraine: a meta-analysis. Pain. 2007;128:111-127.
46. Fritsche G, Kröner-Herwig B, Kropp P, et al. Psychological therapy of migraine: systematic review. Schmerz. 2013;27:263-274.
47. Lipton RB, Dodick DW, Silberstein SD, et al. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomised, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. 2010;9:373-380.
48. Schoenen J, Vandersmissen B, Jeangette S, et al. Migraine prevention with a supraorbital transcutaneous stimulator: a randomized controlled trial. Neurology. 2013;80:697-704.
49. Piquet M, Balestra C, Sava SL, et al. Supraorbital transcutaneous neurostimulation has sedative effects in healthy subjects. BMC Neurol. 2011;11:135.
50. Gil-Martínez A, Kindelan-Calvo P, Agudo-Carmona D, et al. Therapeutic exercise as treatment for migraine and tension-type headaches: a systematic review of randomised clinical trials. Rev Neurol. 2013;57:433-443.
51. Varkey E, Cider A, Carlsson J, et al. Exercise as migraine prophylaxis: a randomized study using relaxation and topiramate as controls. Cephalalgia. 2011;31:1428-1438.
52. Newmaster SG, Grguric M, Shanmughanandhan D, et al. DNA barcoding detects contamination and substitution in North American herbal products. BMC Med. 2013;11:222.
53. Choi H, Parmar N. The use of intravenous magnesium sulphate for acute migraine: meta-analysis of randomized controlled trials. Eur J Emerg Med. 2014;21:2-9.
54. Volpe SL. Magnesium in disease prevention and overall health. Adv Nutr. 2013;4:S378-S383.
55. US Food and Drug Administration. FDA approves Botox to treat chronic migraine. US Food and Drug Administration Web site. October 15, 2010. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm229782.htm. Accessed January 7, 2016.
56. US Food and Drug Administration. FDA allows marketing of first device to relieve migraine headache pain. US Food and Drug Administration Web site. December 13, 2013. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm378608.htm. Accessed January 7, 2016.
57. US Food and Drug Administration. FDA allows marketing of first medical device to prevent migraine headache. US Food and Drug Administration Web site. March 11, 2014. Available at: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm388765.htm. Accessed January 7, 2016.