User login
SAN FRANCISCO – There’s no need to wait for western blot results to differentiate Lyme arthritis from septic arthritis in children, as long as your lab, like many, uses the Liaison Borrelia burgdorferi assay, according to investigators at the University of Minnesota, Minneapolis.
Acute, isolated monoarthritis presents with a single swollen joint and pain whether it’s due to Lyme disease or infection, so it’s hard to tell them apart. Current guidelines recommend a two-tier approach to diagnose Lyme arthritis, an initial blood screen followed by western blot confirmation. Screening results come back in a few hours, but western blot confirmation can take days.
In the meantime, children are treated presumptively for the more concerning diagnosis – septic arthritis – which means hospitalization, surgical drainage, and IV antibiotics. Those who turn out to have Lyme are exposed to the risks and costs of unnecessary treatment and delays to proper diagnosis and doxycycline.
When “kids come in with a swollen knee, maybe 10% or 15% end up in the hospital being treated for septic arthritis that they never had. I wanted to see if we can diagnose Lyme arthritis more quickly,” said lead investigator Bazak Sharon, MD, a pediatric infectious disease specialist at the university’s Masonic Children’s Hospital.
Masonic and its affiliated health system use the Liaison Borrelia burgdorferi assay (DiaSorin) to screen for Lyme, and a careful parsing of the results seems to solve the problem.
Liaison is a chemiluminescence immunoassay that uses light to measure IgM and IgG antibodies to a B. burgdorferi surface protein in serum samples. Results are reported as relative light units (RLUs); below 0.9 RLUs is negative; 0.9-1.1 is equivocal, and over 1.1 is positive.
It’s where patients fall in the range of positivity that matters when it comes to differentiating Lyme from septic arthritis, Dr. Sharon said at ID Week, an annual scientific meeting on infectious diseases (Clin Vaccine Immunol. 2008 Dec;15[12]:1796-804).
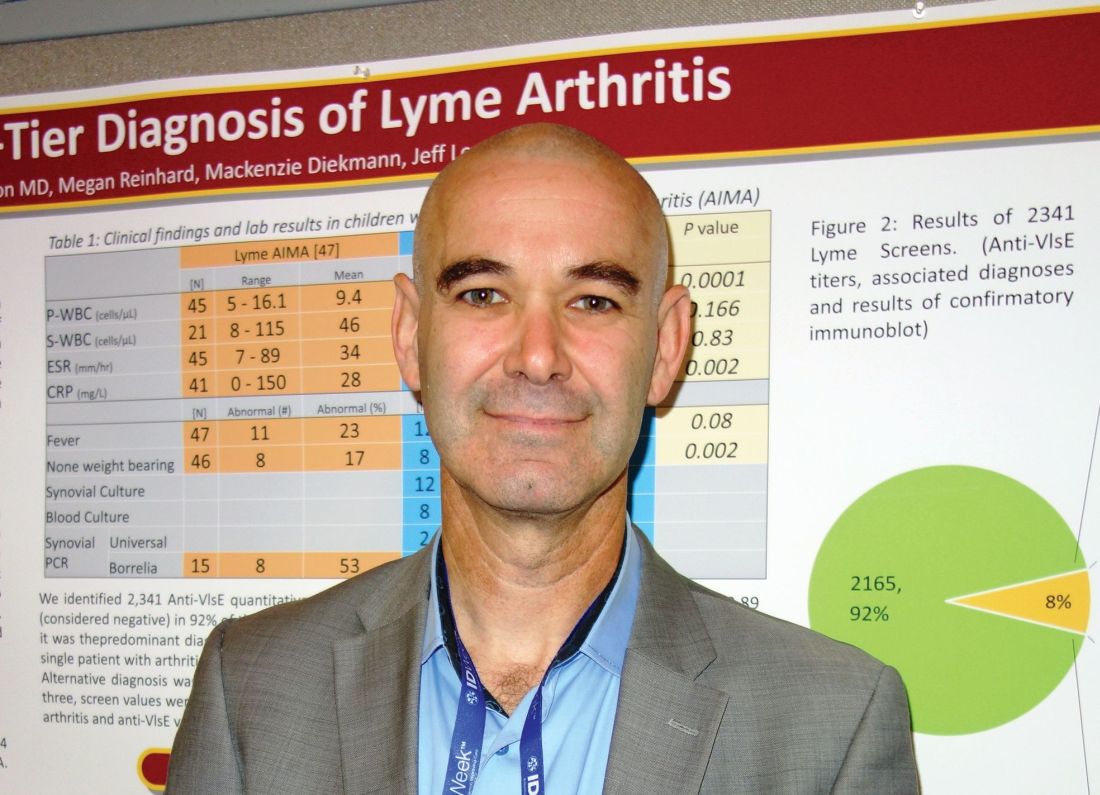
He and his team reviewed 60 cases of acute, isolated monoarthritis culled from more than 700 children who presented with joint complaints from 2011 to 2016; 47 had Lyme arthritis confirmed by western blot; 13 had septic arthritis.
It turned out that “every single patient with a” Liaison value of 9 RLUs or higher was confirmed on western blot for Lyme. “Under 9, there was not a single case of Lyme arthritis,” Dr. Sharon said. Three other patients with acute arthritis also tested positive on the screen, but their RLU values were below 4; two turned out to be trauma related and one was ultimately diagnosed with juvenile idiopathic arthritis. Western blots were negative in all three.
The RLU number reported on the screening test “appears to correlate very well with Lyme arthritis. In an otherwise healthy child presenting with acute joint swelling, utilizing this screening test can confirm clinical suspicion of Lyme arthritis within hours, and prevent the potential harmful interventions accompanying a misdiagnosis of septic arthritis. Just do the screening. If it comes up above 9, you’ve got Lyme arthritis,” and don’t need to wait for western blot results to treat, Dr. Sharon said.
In other words, above 9, treat for Lyme.
The investigators plan to delve further into their results with sensitivity/specificity and other analyses before publishing. Ultimately, “my goal is to have a better diagnosis algorithm for kids who present with acute, isolated monoarthritis,” Dr. Sharon said.
There was no industry funding for the work, and the investigators didn’t have any disclosures.
SOURCE: Sharon B et al. 2018 ID Week abstract 286.
SAN FRANCISCO – There’s no need to wait for western blot results to differentiate Lyme arthritis from septic arthritis in children, as long as your lab, like many, uses the Liaison Borrelia burgdorferi assay, according to investigators at the University of Minnesota, Minneapolis.
Acute, isolated monoarthritis presents with a single swollen joint and pain whether it’s due to Lyme disease or infection, so it’s hard to tell them apart. Current guidelines recommend a two-tier approach to diagnose Lyme arthritis, an initial blood screen followed by western blot confirmation. Screening results come back in a few hours, but western blot confirmation can take days.
In the meantime, children are treated presumptively for the more concerning diagnosis – septic arthritis – which means hospitalization, surgical drainage, and IV antibiotics. Those who turn out to have Lyme are exposed to the risks and costs of unnecessary treatment and delays to proper diagnosis and doxycycline.
When “kids come in with a swollen knee, maybe 10% or 15% end up in the hospital being treated for septic arthritis that they never had. I wanted to see if we can diagnose Lyme arthritis more quickly,” said lead investigator Bazak Sharon, MD, a pediatric infectious disease specialist at the university’s Masonic Children’s Hospital.
Masonic and its affiliated health system use the Liaison Borrelia burgdorferi assay (DiaSorin) to screen for Lyme, and a careful parsing of the results seems to solve the problem.
Liaison is a chemiluminescence immunoassay that uses light to measure IgM and IgG antibodies to a B. burgdorferi surface protein in serum samples. Results are reported as relative light units (RLUs); below 0.9 RLUs is negative; 0.9-1.1 is equivocal, and over 1.1 is positive.
It’s where patients fall in the range of positivity that matters when it comes to differentiating Lyme from septic arthritis, Dr. Sharon said at ID Week, an annual scientific meeting on infectious diseases (Clin Vaccine Immunol. 2008 Dec;15[12]:1796-804).
He and his team reviewed 60 cases of acute, isolated monoarthritis culled from more than 700 children who presented with joint complaints from 2011 to 2016; 47 had Lyme arthritis confirmed by western blot; 13 had septic arthritis.
It turned out that “every single patient with a” Liaison value of 9 RLUs or higher was confirmed on western blot for Lyme. “Under 9, there was not a single case of Lyme arthritis,” Dr. Sharon said. Three other patients with acute arthritis also tested positive on the screen, but their RLU values were below 4; two turned out to be trauma related and one was ultimately diagnosed with juvenile idiopathic arthritis. Western blots were negative in all three.
The RLU number reported on the screening test “appears to correlate very well with Lyme arthritis. In an otherwise healthy child presenting with acute joint swelling, utilizing this screening test can confirm clinical suspicion of Lyme arthritis within hours, and prevent the potential harmful interventions accompanying a misdiagnosis of septic arthritis. Just do the screening. If it comes up above 9, you’ve got Lyme arthritis,” and don’t need to wait for western blot results to treat, Dr. Sharon said.
In other words, above 9, treat for Lyme.
The investigators plan to delve further into their results with sensitivity/specificity and other analyses before publishing. Ultimately, “my goal is to have a better diagnosis algorithm for kids who present with acute, isolated monoarthritis,” Dr. Sharon said.
There was no industry funding for the work, and the investigators didn’t have any disclosures.
SOURCE: Sharon B et al. 2018 ID Week abstract 286.
SAN FRANCISCO – There’s no need to wait for western blot results to differentiate Lyme arthritis from septic arthritis in children, as long as your lab, like many, uses the Liaison Borrelia burgdorferi assay, according to investigators at the University of Minnesota, Minneapolis.
Acute, isolated monoarthritis presents with a single swollen joint and pain whether it’s due to Lyme disease or infection, so it’s hard to tell them apart. Current guidelines recommend a two-tier approach to diagnose Lyme arthritis, an initial blood screen followed by western blot confirmation. Screening results come back in a few hours, but western blot confirmation can take days.
In the meantime, children are treated presumptively for the more concerning diagnosis – septic arthritis – which means hospitalization, surgical drainage, and IV antibiotics. Those who turn out to have Lyme are exposed to the risks and costs of unnecessary treatment and delays to proper diagnosis and doxycycline.
When “kids come in with a swollen knee, maybe 10% or 15% end up in the hospital being treated for septic arthritis that they never had. I wanted to see if we can diagnose Lyme arthritis more quickly,” said lead investigator Bazak Sharon, MD, a pediatric infectious disease specialist at the university’s Masonic Children’s Hospital.
Masonic and its affiliated health system use the Liaison Borrelia burgdorferi assay (DiaSorin) to screen for Lyme, and a careful parsing of the results seems to solve the problem.
Liaison is a chemiluminescence immunoassay that uses light to measure IgM and IgG antibodies to a B. burgdorferi surface protein in serum samples. Results are reported as relative light units (RLUs); below 0.9 RLUs is negative; 0.9-1.1 is equivocal, and over 1.1 is positive.
It’s where patients fall in the range of positivity that matters when it comes to differentiating Lyme from septic arthritis, Dr. Sharon said at ID Week, an annual scientific meeting on infectious diseases (Clin Vaccine Immunol. 2008 Dec;15[12]:1796-804).
He and his team reviewed 60 cases of acute, isolated monoarthritis culled from more than 700 children who presented with joint complaints from 2011 to 2016; 47 had Lyme arthritis confirmed by western blot; 13 had septic arthritis.
It turned out that “every single patient with a” Liaison value of 9 RLUs or higher was confirmed on western blot for Lyme. “Under 9, there was not a single case of Lyme arthritis,” Dr. Sharon said. Three other patients with acute arthritis also tested positive on the screen, but their RLU values were below 4; two turned out to be trauma related and one was ultimately diagnosed with juvenile idiopathic arthritis. Western blots were negative in all three.
The RLU number reported on the screening test “appears to correlate very well with Lyme arthritis. In an otherwise healthy child presenting with acute joint swelling, utilizing this screening test can confirm clinical suspicion of Lyme arthritis within hours, and prevent the potential harmful interventions accompanying a misdiagnosis of septic arthritis. Just do the screening. If it comes up above 9, you’ve got Lyme arthritis,” and don’t need to wait for western blot results to treat, Dr. Sharon said.
In other words, above 9, treat for Lyme.
The investigators plan to delve further into their results with sensitivity/specificity and other analyses before publishing. Ultimately, “my goal is to have a better diagnosis algorithm for kids who present with acute, isolated monoarthritis,” Dr. Sharon said.
There was no industry funding for the work, and the investigators didn’t have any disclosures.
SOURCE: Sharon B et al. 2018 ID Week abstract 286.
REPORTING FROM IDWEEK 2018
Key clinical point:
Major finding: There was not a single case of Lyme arthritis under 9 RLUs on the screening test.
Study details: Review of 60 children with acute, isolated monoarthritis, culled from more than 700 with joint complaints.
Disclosures: There was no industry funding for the work, and the investigators didn’t have any disclosures.
Source: Sharon B et al. 2018 ID Week abstract 286.