User login
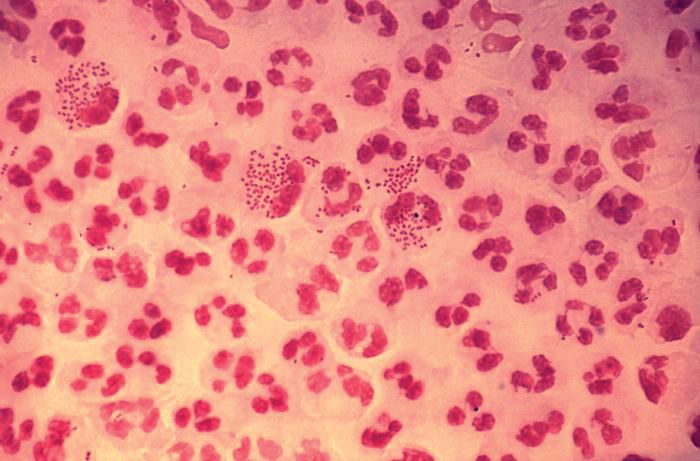
SEATTLE – Sexually-transmitted infections (STIs) such as gonorrhea, chlamydia, and syphilis are on the rise among HIV-infected individuals, and emerging antimicrobial resistance in these organisms is presenting serious challenges to physicians. The issue may be traceable to the introduction of preexposure prophylaxis (PrEP) in 2011, which previous studies have shown to be associated with less condom use.
In the United States, a 2017 report by the Centers for Disease Control and Prevention showed rising incidences of chlamydia (+5% from 2015 to 2017), gonorrhea (+19%), and syphilis (+18%). “We have an incidence among men who have sex with men [MSM] that is above the pre-AIDS era estimates, and we have evidence of spread into heterosexual networks, and a very scary collision with the methamphetamine and heroine using networks,” said Jeanne Marrazzo, MD, professor of infectious diseases at the University of Alabama at Birmingham.
But the numbers alone don’t tell the whole story. “It’s not just the burden of these infections. What’s characterizing these trends is that we have continuing evolution of microbial resistance, which is really a crisis,” Dr. Marrazzo added during a plenary she delivered at the Conference on Retroviruses & Opportunistic Infections.
These infections also remain intricately linked with HIV. An analysis of syphilis cases found that 88% occurred in men. Of those, 80% were MSM. Of the cases in MSM, 46% were coinfected with HIV. “Those are incredible rates,” said Dr. Marrazzo. Among women, the trends are even more alarming. There has been a greater than 150% increase in primary/secondary and congenital syphilis between 2013 and 2017.
Resistance to ceftriaxone and azithromycin remains on the rise in gonorrhea, with 24% of countries reporting at least a 5% incidence of strains that are less susceptible or resistant to ceftriaxone, and 81% of countries reporting similar trends with azithromycin.
In the absence of new drugs to overcome that resistance, or vaccines that can prevent gonorrhea and other infections, what are clinicians to do?
One option may be postexposure doxycycline. One trial in MSM showed that a 200-mg dose taken 24-72 hours after sex was associated with about a 70% increase in both time to first chlamydia and time to first syphilis infection, though no effect was seen on gonorrhea infections. “We shouldn’t be surprised. We know that gonorrhea is classically resistant to tetracyclines, and the MSM population has the highest prevalence of antimicrobial resistance in gonorrhea,” said Dr. Marrazzo.
There are pros and cons to this strategy, of course. On the one hand, doxycycline works for chlamydia and syphilis, it’s safe, and it’s easy to administer. “We’re up a tree when it comes to syphilis, so why not?” opined Dr. Marrazzo. In fact, some MSM have read the literature and are already using it prophylactically. But there are downsides, including adverse effects such as esophagitis/ulceration and photosensitivity, and it is contraindicated in pregnant women. And then there’s the potential for evolving greater resistance. “The horse is out of the barn with respect to gonorrhea, but I think it’s worth thinking about resistance to other pathogens, where we still rely on doxycycline [to treat] in rare cases,” said Dr. Marrazzo.
Finally, Dr. Marrazzo discussed the role of STI treatment in the effort to eradicate HIV. Should the Getting to 0 strategies include aggressive prevention and treatment of STIs? Despite the potentiating role of some STIs in the spread HIV, some urban areas are approaching zero new infections even as other STIs remain a problem. It could be that undetectable = untransmittable, regardless of the presence an STI. Some view targeting STIs as a regressive practice in a setting where the U=U mantra has opened up an era of sexual freedom living with or at risk of HIV.
On the other hand, there are also good arguments to target STIs while trying to eliminate HIV. Results from high-resource locales such as San Francisco and New York City are unlikely to be replicated in places like Sub-Saharan Africa. The public health burden of STIs is extensive, and antibiotic resistance and antibiotic shortages can make treatment difficult. The situation is also different for women, who may experience impacts on fertility or pregnancies, and do not have the same freedom as men in many countries. “Stigma is highly operative and I would wager that sexual pleasure and freedom remain a very elusive goal for women across the globe,” said Dr. Marrazzo.
Dr. Marrazzo has a research grant/grant pending from Cepheid, and is on the advisory panels of BioFire and Gilead.
SEATTLE – Sexually-transmitted infections (STIs) such as gonorrhea, chlamydia, and syphilis are on the rise among HIV-infected individuals, and emerging antimicrobial resistance in these organisms is presenting serious challenges to physicians. The issue may be traceable to the introduction of preexposure prophylaxis (PrEP) in 2011, which previous studies have shown to be associated with less condom use.
In the United States, a 2017 report by the Centers for Disease Control and Prevention showed rising incidences of chlamydia (+5% from 2015 to 2017), gonorrhea (+19%), and syphilis (+18%). “We have an incidence among men who have sex with men [MSM] that is above the pre-AIDS era estimates, and we have evidence of spread into heterosexual networks, and a very scary collision with the methamphetamine and heroine using networks,” said Jeanne Marrazzo, MD, professor of infectious diseases at the University of Alabama at Birmingham.
But the numbers alone don’t tell the whole story. “It’s not just the burden of these infections. What’s characterizing these trends is that we have continuing evolution of microbial resistance, which is really a crisis,” Dr. Marrazzo added during a plenary she delivered at the Conference on Retroviruses & Opportunistic Infections.
These infections also remain intricately linked with HIV. An analysis of syphilis cases found that 88% occurred in men. Of those, 80% were MSM. Of the cases in MSM, 46% were coinfected with HIV. “Those are incredible rates,” said Dr. Marrazzo. Among women, the trends are even more alarming. There has been a greater than 150% increase in primary/secondary and congenital syphilis between 2013 and 2017.
Resistance to ceftriaxone and azithromycin remains on the rise in gonorrhea, with 24% of countries reporting at least a 5% incidence of strains that are less susceptible or resistant to ceftriaxone, and 81% of countries reporting similar trends with azithromycin.
In the absence of new drugs to overcome that resistance, or vaccines that can prevent gonorrhea and other infections, what are clinicians to do?
One option may be postexposure doxycycline. One trial in MSM showed that a 200-mg dose taken 24-72 hours after sex was associated with about a 70% increase in both time to first chlamydia and time to first syphilis infection, though no effect was seen on gonorrhea infections. “We shouldn’t be surprised. We know that gonorrhea is classically resistant to tetracyclines, and the MSM population has the highest prevalence of antimicrobial resistance in gonorrhea,” said Dr. Marrazzo.
There are pros and cons to this strategy, of course. On the one hand, doxycycline works for chlamydia and syphilis, it’s safe, and it’s easy to administer. “We’re up a tree when it comes to syphilis, so why not?” opined Dr. Marrazzo. In fact, some MSM have read the literature and are already using it prophylactically. But there are downsides, including adverse effects such as esophagitis/ulceration and photosensitivity, and it is contraindicated in pregnant women. And then there’s the potential for evolving greater resistance. “The horse is out of the barn with respect to gonorrhea, but I think it’s worth thinking about resistance to other pathogens, where we still rely on doxycycline [to treat] in rare cases,” said Dr. Marrazzo.
Finally, Dr. Marrazzo discussed the role of STI treatment in the effort to eradicate HIV. Should the Getting to 0 strategies include aggressive prevention and treatment of STIs? Despite the potentiating role of some STIs in the spread HIV, some urban areas are approaching zero new infections even as other STIs remain a problem. It could be that undetectable = untransmittable, regardless of the presence an STI. Some view targeting STIs as a regressive practice in a setting where the U=U mantra has opened up an era of sexual freedom living with or at risk of HIV.
On the other hand, there are also good arguments to target STIs while trying to eliminate HIV. Results from high-resource locales such as San Francisco and New York City are unlikely to be replicated in places like Sub-Saharan Africa. The public health burden of STIs is extensive, and antibiotic resistance and antibiotic shortages can make treatment difficult. The situation is also different for women, who may experience impacts on fertility or pregnancies, and do not have the same freedom as men in many countries. “Stigma is highly operative and I would wager that sexual pleasure and freedom remain a very elusive goal for women across the globe,” said Dr. Marrazzo.
Dr. Marrazzo has a research grant/grant pending from Cepheid, and is on the advisory panels of BioFire and Gilead.
SEATTLE – Sexually-transmitted infections (STIs) such as gonorrhea, chlamydia, and syphilis are on the rise among HIV-infected individuals, and emerging antimicrobial resistance in these organisms is presenting serious challenges to physicians. The issue may be traceable to the introduction of preexposure prophylaxis (PrEP) in 2011, which previous studies have shown to be associated with less condom use.
In the United States, a 2017 report by the Centers for Disease Control and Prevention showed rising incidences of chlamydia (+5% from 2015 to 2017), gonorrhea (+19%), and syphilis (+18%). “We have an incidence among men who have sex with men [MSM] that is above the pre-AIDS era estimates, and we have evidence of spread into heterosexual networks, and a very scary collision with the methamphetamine and heroine using networks,” said Jeanne Marrazzo, MD, professor of infectious diseases at the University of Alabama at Birmingham.
But the numbers alone don’t tell the whole story. “It’s not just the burden of these infections. What’s characterizing these trends is that we have continuing evolution of microbial resistance, which is really a crisis,” Dr. Marrazzo added during a plenary she delivered at the Conference on Retroviruses & Opportunistic Infections.
These infections also remain intricately linked with HIV. An analysis of syphilis cases found that 88% occurred in men. Of those, 80% were MSM. Of the cases in MSM, 46% were coinfected with HIV. “Those are incredible rates,” said Dr. Marrazzo. Among women, the trends are even more alarming. There has been a greater than 150% increase in primary/secondary and congenital syphilis between 2013 and 2017.
Resistance to ceftriaxone and azithromycin remains on the rise in gonorrhea, with 24% of countries reporting at least a 5% incidence of strains that are less susceptible or resistant to ceftriaxone, and 81% of countries reporting similar trends with azithromycin.
In the absence of new drugs to overcome that resistance, or vaccines that can prevent gonorrhea and other infections, what are clinicians to do?
One option may be postexposure doxycycline. One trial in MSM showed that a 200-mg dose taken 24-72 hours after sex was associated with about a 70% increase in both time to first chlamydia and time to first syphilis infection, though no effect was seen on gonorrhea infections. “We shouldn’t be surprised. We know that gonorrhea is classically resistant to tetracyclines, and the MSM population has the highest prevalence of antimicrobial resistance in gonorrhea,” said Dr. Marrazzo.
There are pros and cons to this strategy, of course. On the one hand, doxycycline works for chlamydia and syphilis, it’s safe, and it’s easy to administer. “We’re up a tree when it comes to syphilis, so why not?” opined Dr. Marrazzo. In fact, some MSM have read the literature and are already using it prophylactically. But there are downsides, including adverse effects such as esophagitis/ulceration and photosensitivity, and it is contraindicated in pregnant women. And then there’s the potential for evolving greater resistance. “The horse is out of the barn with respect to gonorrhea, but I think it’s worth thinking about resistance to other pathogens, where we still rely on doxycycline [to treat] in rare cases,” said Dr. Marrazzo.
Finally, Dr. Marrazzo discussed the role of STI treatment in the effort to eradicate HIV. Should the Getting to 0 strategies include aggressive prevention and treatment of STIs? Despite the potentiating role of some STIs in the spread HIV, some urban areas are approaching zero new infections even as other STIs remain a problem. It could be that undetectable = untransmittable, regardless of the presence an STI. Some view targeting STIs as a regressive practice in a setting where the U=U mantra has opened up an era of sexual freedom living with or at risk of HIV.
On the other hand, there are also good arguments to target STIs while trying to eliminate HIV. Results from high-resource locales such as San Francisco and New York City are unlikely to be replicated in places like Sub-Saharan Africa. The public health burden of STIs is extensive, and antibiotic resistance and antibiotic shortages can make treatment difficult. The situation is also different for women, who may experience impacts on fertility or pregnancies, and do not have the same freedom as men in many countries. “Stigma is highly operative and I would wager that sexual pleasure and freedom remain a very elusive goal for women across the globe,” said Dr. Marrazzo.
Dr. Marrazzo has a research grant/grant pending from Cepheid, and is on the advisory panels of BioFire and Gilead.
EXPERT ANALYSIS FROM CROI 2019