User login
ANSWER
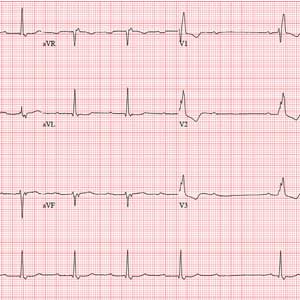
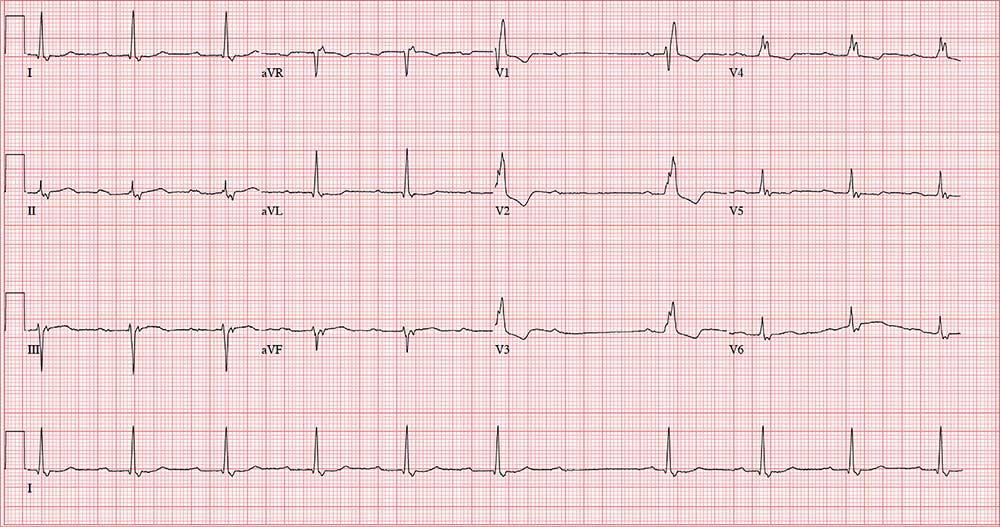
The correct answer includes sinus rhythm with second-degree atrioventricular (AV) block (Mobitz I) and a right bundle branch block (RBBB).
Sinus rhythm is evidenced by the consistent P-P intervals (best measured in the lead I rhythm strip). Mobitz I block is distinguished from Mobitz II block by the varying PR interval.
Remember that in Mobitz I (Wenckebach) block, the PR interval becomes progressively longer as the AV node fatigues, until there is blocked conduction between the atria and ventricles resulting in a P wave with no associated QRS complex. This is evident in the pause between the 6th and 7th QRS complexes. Notice also that the very next PR interval following the dropped QRS complex is much shorter than the PR interval immediately prior to that complex. In this example, the increasing PR interval before the pause is subtle compared to the PR intervals following the pause.
The skipped beats the patient feels are these pauses. Increased parasympathetic (vagal) activity occurs when a person is falling asleep, resulting in a reduction in heart rate and AV nodal conduction variability.
Finally, don’t forget the RBBB. It is indicated by a QRS duration > 120 ms, rSR’ complexes in precordial leads V1 to V3, and slurred S waves in leads I and aVF.
ANSWER
The correct answer includes sinus rhythm with second-degree atrioventricular (AV) block (Mobitz I) and a right bundle branch block (RBBB).
Sinus rhythm is evidenced by the consistent P-P intervals (best measured in the lead I rhythm strip). Mobitz I block is distinguished from Mobitz II block by the varying PR interval.
Remember that in Mobitz I (Wenckebach) block, the PR interval becomes progressively longer as the AV node fatigues, until there is blocked conduction between the atria and ventricles resulting in a P wave with no associated QRS complex. This is evident in the pause between the 6th and 7th QRS complexes. Notice also that the very next PR interval following the dropped QRS complex is much shorter than the PR interval immediately prior to that complex. In this example, the increasing PR interval before the pause is subtle compared to the PR intervals following the pause.
The skipped beats the patient feels are these pauses. Increased parasympathetic (vagal) activity occurs when a person is falling asleep, resulting in a reduction in heart rate and AV nodal conduction variability.
Finally, don’t forget the RBBB. It is indicated by a QRS duration > 120 ms, rSR’ complexes in precordial leads V1 to V3, and slurred S waves in leads I and aVF.
ANSWER
The correct answer includes sinus rhythm with second-degree atrioventricular (AV) block (Mobitz I) and a right bundle branch block (RBBB).
Sinus rhythm is evidenced by the consistent P-P intervals (best measured in the lead I rhythm strip). Mobitz I block is distinguished from Mobitz II block by the varying PR interval.
Remember that in Mobitz I (Wenckebach) block, the PR interval becomes progressively longer as the AV node fatigues, until there is blocked conduction between the atria and ventricles resulting in a P wave with no associated QRS complex. This is evident in the pause between the 6th and 7th QRS complexes. Notice also that the very next PR interval following the dropped QRS complex is much shorter than the PR interval immediately prior to that complex. In this example, the increasing PR interval before the pause is subtle compared to the PR intervals following the pause.
The skipped beats the patient feels are these pauses. Increased parasympathetic (vagal) activity occurs when a person is falling asleep, resulting in a reduction in heart rate and AV nodal conduction variability.
Finally, don’t forget the RBBB. It is indicated by a QRS duration > 120 ms, rSR’ complexes in precordial leads V1 to V3, and slurred S waves in leads I and aVF.
A 64-year-old man presents with a 6-month history of skipped heart beats. He says this occurs most often in the evenings, when he’s resting, and he has been awakened by it. He denies chest pain, dyspnea with exertion, syncope, or near-syncope. He has been otherwise asymptomatic from a cardiac and pulmonary standpoint.
However, he is increasingly concerned that his heart may “just stop beating” when he is asleep. When pressed further, he reveals he is afraid to go to sleep at night, knowing “my heart will start skipping beats and I’ll die!” He has discussed his fear of dying in his sleep with a psychologist, who told him that although he experiences fatigue and loss of energy and has recurrent thoughts of death, he does not meet DSM-5 criteria for major depressive disorder. The psychologist obtained an ECG and noticed pauses, which prompted referral of the patient to you.
Past medical history is remarkable for hypertension, cirrhosis, and osteoarthritis. Surgical history includes bilateral knee and left hip replacements. A screening colonoscopy 1 month ago yielded a diagnosis of stage 1 colorectal cancer.
The patient’s medication list includes hydrochlorothiazide and celecoxib. He is allergic to oxycodone (anaphylaxis).
The patient is divorced, which he attributes to his ongoing alcoholism. He drinks half a bottle of whiskey daily to “help with my nerves” and “get drunk enough to sleep.” He reports a lifetime of heavy drinking; he has tried Alcoholics Anonymous but kept dropping out to drink. He also smokes up to 1.5 packs/d of cigarettes. He has no children. He worked as a machinist in a factory but was laid off a year ago when the company downsized.
Family history is positive for alcoholism (father, 2 brothers) and hypothyroidism (mother).
Review of systems is positive for a chronic smoker’s cough, lower abdominal cramping following his colonoscopy, and arthritic pain in his wrists and ankles.
Vital signs include a blood pressure of 174/92 mm Hg; pulse, 74 beats/min; respiratory rate, 14 breaths/min; and O2 saturation, 97% on room air. His weight is 247 lb and his height, 69 in. His BMI is 36.5.
Physical exam reveals a somewhat disheveled male in no apparent distress. He wears corrective lenses and has tobacco stains on his mustache. His HEENT exam is surprisingly normal, and there is no evidence of rhinophyma. There is no jugular venous distention, thyromegaly, or lymphadenopathy. There are crackles and late expiratory wheezes in both lower lung fields.
The cardiac exam reveals a regular rate and rhythm of 74 beats/min, with no murmurs, rubs, or extra heart sounds. Peripheral pulses are strong and equal bilaterally. The abdomen is obese but nontender, and there are no palpable masses. There are surgical scars over both knees and the left hip. Arthritic changes are noticeable in the fingers on both hands. There are no neurologic deficits.
Through the electronic medical record, you access the ECG taken in the psychologist’s office. It shows a ventricular rate of 56 beats/min; no measurable PR interval; QRS duration, 144 ms; QT/QTc interval, 438/422 ms; P axis, 47°; R axis, –24°; and T axis, 55°. What is your interpretation of this ECG?