User login
Migraine is a neurologic disease characterized by episodes of throbbing, often unilateral, headache. These attacks are associated with visual or other sensory symptoms (classic aura) related to the central nervous system, nausea, and vomiting, and are often set off or exacerbated by physical activity. The age-adjusted prevalence is estimated at 15.9% across all adults, but migraine is much more common in women, with a prevalence of 21% in women and 10.7% in men.
On the basis of the patient's history, clinical suspicion for chronic migraine should be high. Hemiplegic migraine usually presents with temporary unilateral hemiparesis, sometimes with speech disturbance. Attacks of chronic paroxysmal hemicrania are also unilateral but are characterized by their highly intense but short duration. Clinical suspicion for a space-occupying lesion should be raised in cases where patients with a history of headache present with new symptoms or abnormal signs.
The diagnosis of chronic migraine is a clinical one. The American Headache Society defines chronic migraine as at least five attacks of migraine-like or tension type–like headache that must fulfill specific criteria. If the migraine occurs with aura, it must occur 8 days or more per month for more than 3 months and be relieved by a triptan or ergot derivative. If the migraine occurs without aura, the same criteria apply, but it is important that the aforementioned signs and symptoms cannot be accounted for by another diagnosis.
For moderate or severe attacks, migraine-specific agents are recommended: triptans, dihydroergotamine (DHE), small-molecule CGRP receptor antagonists (gepants), and selective serotonin (5-HT1F) receptor agonists (ditans). However, it is accepted that migraine treatment must be individualized, and that a trial-and-error period should be expected. Recent data suggest that about 30% of migraine patients who are prescribed a triptan have an insufficient response to this approach. Some research has shown that such patients have a better response after being switched to a second drug in the triptan class, while other studies have shown no difference. The patient in the current case might also be a candidate for preventive treatment, which should generally be considered when, in spite of acute treatment, migraine interferes with the patient's day-to-day routine or when attacks become frequent. The four CGRP monoclonal antibodies approved in the United States are eptinezumab, erenumab, fremanezumab, and galcanezumab.
Angeliki Vgontzas, MD, Instructor, Department of Neurology, Harvard Medical School; Associate Neurologist, Department of Neurology, Brigham and Women's Hospital/Brigham and Women's Faulkner Hospital, Boston, Massachusetts.
Angeliki Vgontzas, MD, has disclosed no relevant financial relationships.
Migraine is a neurologic disease characterized by episodes of throbbing, often unilateral, headache. These attacks are associated with visual or other sensory symptoms (classic aura) related to the central nervous system, nausea, and vomiting, and are often set off or exacerbated by physical activity. The age-adjusted prevalence is estimated at 15.9% across all adults, but migraine is much more common in women, with a prevalence of 21% in women and 10.7% in men.
On the basis of the patient's history, clinical suspicion for chronic migraine should be high. Hemiplegic migraine usually presents with temporary unilateral hemiparesis, sometimes with speech disturbance. Attacks of chronic paroxysmal hemicrania are also unilateral but are characterized by their highly intense but short duration. Clinical suspicion for a space-occupying lesion should be raised in cases where patients with a history of headache present with new symptoms or abnormal signs.
The diagnosis of chronic migraine is a clinical one. The American Headache Society defines chronic migraine as at least five attacks of migraine-like or tension type–like headache that must fulfill specific criteria. If the migraine occurs with aura, it must occur 8 days or more per month for more than 3 months and be relieved by a triptan or ergot derivative. If the migraine occurs without aura, the same criteria apply, but it is important that the aforementioned signs and symptoms cannot be accounted for by another diagnosis.
For moderate or severe attacks, migraine-specific agents are recommended: triptans, dihydroergotamine (DHE), small-molecule CGRP receptor antagonists (gepants), and selective serotonin (5-HT1F) receptor agonists (ditans). However, it is accepted that migraine treatment must be individualized, and that a trial-and-error period should be expected. Recent data suggest that about 30% of migraine patients who are prescribed a triptan have an insufficient response to this approach. Some research has shown that such patients have a better response after being switched to a second drug in the triptan class, while other studies have shown no difference. The patient in the current case might also be a candidate for preventive treatment, which should generally be considered when, in spite of acute treatment, migraine interferes with the patient's day-to-day routine or when attacks become frequent. The four CGRP monoclonal antibodies approved in the United States are eptinezumab, erenumab, fremanezumab, and galcanezumab.
Angeliki Vgontzas, MD, Instructor, Department of Neurology, Harvard Medical School; Associate Neurologist, Department of Neurology, Brigham and Women's Hospital/Brigham and Women's Faulkner Hospital, Boston, Massachusetts.
Angeliki Vgontzas, MD, has disclosed no relevant financial relationships.
Migraine is a neurologic disease characterized by episodes of throbbing, often unilateral, headache. These attacks are associated with visual or other sensory symptoms (classic aura) related to the central nervous system, nausea, and vomiting, and are often set off or exacerbated by physical activity. The age-adjusted prevalence is estimated at 15.9% across all adults, but migraine is much more common in women, with a prevalence of 21% in women and 10.7% in men.
On the basis of the patient's history, clinical suspicion for chronic migraine should be high. Hemiplegic migraine usually presents with temporary unilateral hemiparesis, sometimes with speech disturbance. Attacks of chronic paroxysmal hemicrania are also unilateral but are characterized by their highly intense but short duration. Clinical suspicion for a space-occupying lesion should be raised in cases where patients with a history of headache present with new symptoms or abnormal signs.
The diagnosis of chronic migraine is a clinical one. The American Headache Society defines chronic migraine as at least five attacks of migraine-like or tension type–like headache that must fulfill specific criteria. If the migraine occurs with aura, it must occur 8 days or more per month for more than 3 months and be relieved by a triptan or ergot derivative. If the migraine occurs without aura, the same criteria apply, but it is important that the aforementioned signs and symptoms cannot be accounted for by another diagnosis.
For moderate or severe attacks, migraine-specific agents are recommended: triptans, dihydroergotamine (DHE), small-molecule CGRP receptor antagonists (gepants), and selective serotonin (5-HT1F) receptor agonists (ditans). However, it is accepted that migraine treatment must be individualized, and that a trial-and-error period should be expected. Recent data suggest that about 30% of migraine patients who are prescribed a triptan have an insufficient response to this approach. Some research has shown that such patients have a better response after being switched to a second drug in the triptan class, while other studies have shown no difference. The patient in the current case might also be a candidate for preventive treatment, which should generally be considered when, in spite of acute treatment, migraine interferes with the patient's day-to-day routine or when attacks become frequent. The four CGRP monoclonal antibodies approved in the United States are eptinezumab, erenumab, fremanezumab, and galcanezumab.
Angeliki Vgontzas, MD, Instructor, Department of Neurology, Harvard Medical School; Associate Neurologist, Department of Neurology, Brigham and Women's Hospital/Brigham and Women's Faulkner Hospital, Boston, Massachusetts.
Angeliki Vgontzas, MD, has disclosed no relevant financial relationships.
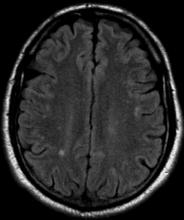
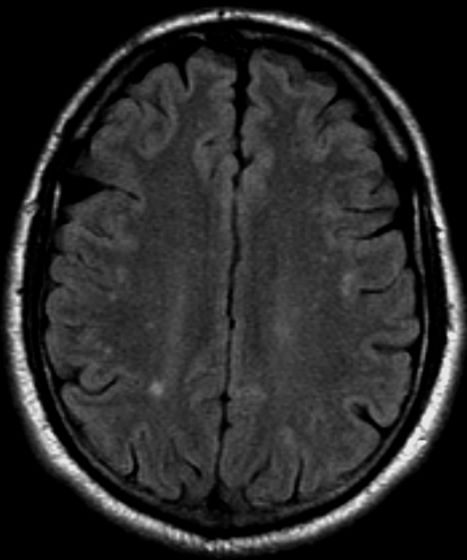
A 36-year-old man presents with severe pain in the frontotemporal area. He reports a history of severe headaches, sometimes with nausea. In the past year, these symptoms have begun to "knock him out" for nearly 2 weeks out of a month. The patient historically has been able to curtail his symptoms with a triptan. Physical examination is remarkable for Adie tonic pupil. A 1.5 T MRI of the brain is performed. Axial FLAIR sequence reveals scattered white matter lesions consistent with foci of demyelination.