User login
Written communication is an essential skill for a consultation-liaison (C-L) psychiatrist, but unfortunately, how to write a consultation note is not part of formal didactics in medical school or residency training.1 Documentation of a consultation note is a permanent medical record entry that conveys current physician-to-physician information. While considerable literature describes the consultation process, little has been published about composing a consultation note.1,2 Residents and clinicians who do not have frequent consultations may be unfamiliar with the consultation environment and their role as an expert consultant. Therefore, more explicit guidance on documentation and optimal formatting of the consultation note is needed.
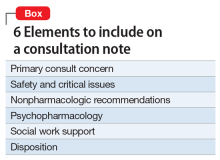
The Box provides an outline for completing the Recommendations/Treatment Plan section of psychiatric consultation notes. When providing your recommendations, it is best to use bullet points, numbering, or bold text; do not bury the information in a dense paragraph.3 Be sure to address each of the following 6 elements.
1. Primary consult concern. The first section of the Recommendations section should include the reason for the consult, which may be the most important part of the consultation process.1,2 It is important to recognize that an unclear consult question may be a sign of the primary team’s knowledge gap in psychiatry. The role of the C-L psychiatrist is to help the primary team organize their thoughts and concerns regarding their patient to decide on the final consult question.1 The active consult question may change as clinical issues evolve.
2. Safety and critical issues. Include an assessment of or recommendation on safety and critical issues. An important consideration is whether to recommend a patient sitter and to provide a reason for this recommendation. Occasionally, critical issues are more pressing than the primary consult concern. For example, there are several situations in which abnormal laboratory values and acute medical issues manifest as psychiatric symptoms, including hyponatremia, hypoglycemia, hypotension, low oxygen saturation, or infection. The connection between the 2 may not be clear to the primary treatment team; thus, include a statement to draw their attention to this.
3. Nonpharmacologic recommendations.
4. Psychopharmacology. In this section, the C-L psychiatrist should provide information on the use of any psychotropic medications and an explanation of their indications. If there are discrepancies between a patient’s home and hospital-ordered medications, clarify which medications the patient should be taking while hospitalized. If the C-L treatment team recommends initiating a new medication, provide details regarding the specific medication, dose, route, administration time, and titration schedule, as well as the specific situation for any as-needed medications. It is important to include the indication for any recommended medications, as well as any potential adverse effects. If psychotropic medications are not indicated, add a statement to emphasize this.
5. Social work support. Document any issues that need to be clarified by social work. This might include clarification of a patient’s insurance coverage, current living situation, or durable power of attorney. Also, document how the treatment team would prefer social work to assist with the patient’s care by (for example) providing the patient with resources for outpatient mental health and/or substance abuse treatment or housing options.
Continue to: Disposition
6. Disposition. Finally, include a recommendation regarding disposition. If transfer to a psychiatric facility is not indicated, provide a statement to affirm this. If transfer to a psychiatric facility is recommended, include a discussion of the patient’s appropriateness in the assessment and recommendations. It is helpful to inform the primary team of criteria that may or may not allow the patient to transfer to or be accepted by a psychiatry unit (eg, the patient will need to be off IV medications and able to tolerate oral intake prior to transfer). When transfer is not possible, communicate the reason to the primary treatment team and other ancillary staff.
Communicating responsibilities and expectations
After concluding the Recommendations section, end the consultation note with a brief sentence of gratitude (eg, “Thank you for this consultation and allowing us to assist in the care of your patient.”) and a comment regarding the C-L treatment team’s plan for follow-up. Also, include your contact information in case the primary treatment team has any questions or concerns.
The Recommendations section of a psychiatric consultation note is vital to convey current physician-to-physician recommendations. With the potential complexities in assessing and caring for a medically ill patient with comorbid psychiatric diagnoses, psychiatrists with less C-L experience may be unfamiliar with the essential elements of a consultation note. It is helpful to use a Template to ensure that the consultation and documentation are complete.
1. Garrick TR, Stotland, NL. How to write a psychiatric consultation. Am J Psychiatry. 1982;139(7):849-855.
2. Alexander T, Bloch S. The written report in consultation-liaison psychiatry: a proposed schema. Aust N Z J Psychiatry. 2002;36(2):251-258.
3. von Gunten CF, Weissman DE. Writing the consultation note #267. J Palliat Med. 2013;16(5):579-580.
Written communication is an essential skill for a consultation-liaison (C-L) psychiatrist, but unfortunately, how to write a consultation note is not part of formal didactics in medical school or residency training.1 Documentation of a consultation note is a permanent medical record entry that conveys current physician-to-physician information. While considerable literature describes the consultation process, little has been published about composing a consultation note.1,2 Residents and clinicians who do not have frequent consultations may be unfamiliar with the consultation environment and their role as an expert consultant. Therefore, more explicit guidance on documentation and optimal formatting of the consultation note is needed.
The Box provides an outline for completing the Recommendations/Treatment Plan section of psychiatric consultation notes. When providing your recommendations, it is best to use bullet points, numbering, or bold text; do not bury the information in a dense paragraph.3 Be sure to address each of the following 6 elements.
1. Primary consult concern. The first section of the Recommendations section should include the reason for the consult, which may be the most important part of the consultation process.1,2 It is important to recognize that an unclear consult question may be a sign of the primary team’s knowledge gap in psychiatry. The role of the C-L psychiatrist is to help the primary team organize their thoughts and concerns regarding their patient to decide on the final consult question.1 The active consult question may change as clinical issues evolve.
2. Safety and critical issues. Include an assessment of or recommendation on safety and critical issues. An important consideration is whether to recommend a patient sitter and to provide a reason for this recommendation. Occasionally, critical issues are more pressing than the primary consult concern. For example, there are several situations in which abnormal laboratory values and acute medical issues manifest as psychiatric symptoms, including hyponatremia, hypoglycemia, hypotension, low oxygen saturation, or infection. The connection between the 2 may not be clear to the primary treatment team; thus, include a statement to draw their attention to this.
3. Nonpharmacologic recommendations.
4. Psychopharmacology. In this section, the C-L psychiatrist should provide information on the use of any psychotropic medications and an explanation of their indications. If there are discrepancies between a patient’s home and hospital-ordered medications, clarify which medications the patient should be taking while hospitalized. If the C-L treatment team recommends initiating a new medication, provide details regarding the specific medication, dose, route, administration time, and titration schedule, as well as the specific situation for any as-needed medications. It is important to include the indication for any recommended medications, as well as any potential adverse effects. If psychotropic medications are not indicated, add a statement to emphasize this.
5. Social work support. Document any issues that need to be clarified by social work. This might include clarification of a patient’s insurance coverage, current living situation, or durable power of attorney. Also, document how the treatment team would prefer social work to assist with the patient’s care by (for example) providing the patient with resources for outpatient mental health and/or substance abuse treatment or housing options.
Continue to: Disposition
6. Disposition. Finally, include a recommendation regarding disposition. If transfer to a psychiatric facility is not indicated, provide a statement to affirm this. If transfer to a psychiatric facility is recommended, include a discussion of the patient’s appropriateness in the assessment and recommendations. It is helpful to inform the primary team of criteria that may or may not allow the patient to transfer to or be accepted by a psychiatry unit (eg, the patient will need to be off IV medications and able to tolerate oral intake prior to transfer). When transfer is not possible, communicate the reason to the primary treatment team and other ancillary staff.
Communicating responsibilities and expectations
After concluding the Recommendations section, end the consultation note with a brief sentence of gratitude (eg, “Thank you for this consultation and allowing us to assist in the care of your patient.”) and a comment regarding the C-L treatment team’s plan for follow-up. Also, include your contact information in case the primary treatment team has any questions or concerns.
The Recommendations section of a psychiatric consultation note is vital to convey current physician-to-physician recommendations. With the potential complexities in assessing and caring for a medically ill patient with comorbid psychiatric diagnoses, psychiatrists with less C-L experience may be unfamiliar with the essential elements of a consultation note. It is helpful to use a Template to ensure that the consultation and documentation are complete.
Written communication is an essential skill for a consultation-liaison (C-L) psychiatrist, but unfortunately, how to write a consultation note is not part of formal didactics in medical school or residency training.1 Documentation of a consultation note is a permanent medical record entry that conveys current physician-to-physician information. While considerable literature describes the consultation process, little has been published about composing a consultation note.1,2 Residents and clinicians who do not have frequent consultations may be unfamiliar with the consultation environment and their role as an expert consultant. Therefore, more explicit guidance on documentation and optimal formatting of the consultation note is needed.
The Box provides an outline for completing the Recommendations/Treatment Plan section of psychiatric consultation notes. When providing your recommendations, it is best to use bullet points, numbering, or bold text; do not bury the information in a dense paragraph.3 Be sure to address each of the following 6 elements.
1. Primary consult concern. The first section of the Recommendations section should include the reason for the consult, which may be the most important part of the consultation process.1,2 It is important to recognize that an unclear consult question may be a sign of the primary team’s knowledge gap in psychiatry. The role of the C-L psychiatrist is to help the primary team organize their thoughts and concerns regarding their patient to decide on the final consult question.1 The active consult question may change as clinical issues evolve.
2. Safety and critical issues. Include an assessment of or recommendation on safety and critical issues. An important consideration is whether to recommend a patient sitter and to provide a reason for this recommendation. Occasionally, critical issues are more pressing than the primary consult concern. For example, there are several situations in which abnormal laboratory values and acute medical issues manifest as psychiatric symptoms, including hyponatremia, hypoglycemia, hypotension, low oxygen saturation, or infection. The connection between the 2 may not be clear to the primary treatment team; thus, include a statement to draw their attention to this.
3. Nonpharmacologic recommendations.
4. Psychopharmacology. In this section, the C-L psychiatrist should provide information on the use of any psychotropic medications and an explanation of their indications. If there are discrepancies between a patient’s home and hospital-ordered medications, clarify which medications the patient should be taking while hospitalized. If the C-L treatment team recommends initiating a new medication, provide details regarding the specific medication, dose, route, administration time, and titration schedule, as well as the specific situation for any as-needed medications. It is important to include the indication for any recommended medications, as well as any potential adverse effects. If psychotropic medications are not indicated, add a statement to emphasize this.
5. Social work support. Document any issues that need to be clarified by social work. This might include clarification of a patient’s insurance coverage, current living situation, or durable power of attorney. Also, document how the treatment team would prefer social work to assist with the patient’s care by (for example) providing the patient with resources for outpatient mental health and/or substance abuse treatment or housing options.
Continue to: Disposition
6. Disposition. Finally, include a recommendation regarding disposition. If transfer to a psychiatric facility is not indicated, provide a statement to affirm this. If transfer to a psychiatric facility is recommended, include a discussion of the patient’s appropriateness in the assessment and recommendations. It is helpful to inform the primary team of criteria that may or may not allow the patient to transfer to or be accepted by a psychiatry unit (eg, the patient will need to be off IV medications and able to tolerate oral intake prior to transfer). When transfer is not possible, communicate the reason to the primary treatment team and other ancillary staff.
Communicating responsibilities and expectations
After concluding the Recommendations section, end the consultation note with a brief sentence of gratitude (eg, “Thank you for this consultation and allowing us to assist in the care of your patient.”) and a comment regarding the C-L treatment team’s plan for follow-up. Also, include your contact information in case the primary treatment team has any questions or concerns.
The Recommendations section of a psychiatric consultation note is vital to convey current physician-to-physician recommendations. With the potential complexities in assessing and caring for a medically ill patient with comorbid psychiatric diagnoses, psychiatrists with less C-L experience may be unfamiliar with the essential elements of a consultation note. It is helpful to use a Template to ensure that the consultation and documentation are complete.
1. Garrick TR, Stotland, NL. How to write a psychiatric consultation. Am J Psychiatry. 1982;139(7):849-855.
2. Alexander T, Bloch S. The written report in consultation-liaison psychiatry: a proposed schema. Aust N Z J Psychiatry. 2002;36(2):251-258.
3. von Gunten CF, Weissman DE. Writing the consultation note #267. J Palliat Med. 2013;16(5):579-580.
1. Garrick TR, Stotland, NL. How to write a psychiatric consultation. Am J Psychiatry. 1982;139(7):849-855.
2. Alexander T, Bloch S. The written report in consultation-liaison psychiatry: a proposed schema. Aust N Z J Psychiatry. 2002;36(2):251-258.
3. von Gunten CF, Weissman DE. Writing the consultation note #267. J Palliat Med. 2013;16(5):579-580.