User login
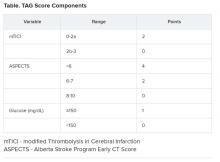
(ICH), new research suggests. In a study of nearly 600 patients undergoing thrombectomy, investigators combined a modified Thrombolysis in Cerebral Ischemia (TICI) score, an Alberta Stroke Program Early Computed Tomography Score (ASPECTS), and glucose levels (the “TAG score”) to predict risk. Results showed that each unit increase in the combination score was associated with a significant, nearly twofold greater likelihood of symptomatic ICH.
“It is very easy” to calculate the new score in a clinical setting, lead author Mayra Johana Montalvo Perero, MD, Department of Neurology, Brown University and Rhode Island Hospital, Providence, said. “You just need three variables.”
The findings were presented online as part of the 2020 American Academy of Neurology Science Highlights.
Limited data
High TAG scores are associated with symptomatic ICH in patients receiving mechanical thrombectomy, Dr. Montalvo Perero and colleagues said.
Although clinical predictors of symptomatic ICH are well established, “there is limited data in patients who underwent mechanical thrombectomy,” the researchers noted.
To learn more, they assessed 578 patients (52% women; mean age, 73 years) who had mechanical thrombectomy for acute ischemic stroke at a comprehensive stroke center. Within this cohort, 19 patients (3.3%) developed symptomatic ICH.
The investigators compared clinical and radiographic findings between patients who experienced symptomatic ICH and those who did not.
The TICI score emerged as a predictor when each unit decrease in this score was associated with greater risk for symptomatic ICH (odds ratio, 5.13; 95% confidence interval, 1.84-14.29; P = .002).
Each one-point decrease in the ASPECTS score also predicted increased risk (OR, 1.52; 95% CI, 1.1-2.0; P = .003).
“The main driver is the size of the stroke core, which is correlated with the ASPECTS score,” Dr. Montalvo Perero said.
Each 10 mg/dL increase in glucose level also correlated with increased risk (OR, 1.07; 95% CI, 1.01-1.13; P = .018).
Twice the risk
The investigators then combined these three independent variables into a weighted TAG score based on a multivariate analysis. Each unit increase in this composite score was associated with increased risk of symptomatic ICH (OR, 1.98; 95% CI, 1.48-2.66; P < .001).
There was no association between patients who received tissue plasminogen activator (tPA) and risk of symptomatic ICH, which Dr. Montalvo Perero said was surprising.
However, “that may be due to a small number” of patients with symptomatic ICH included in the study, she said. “Therefore, that would be an interesting question to ask in future studies with bigger cohorts.”
Larger studies are also needed to validate this scoring system and to test strategies to reduce risk of symptomatic ICH and make thrombectomy safer in patients with elevated TAG scores, Dr. Montalvo Perero said.
A step in the right direction?
Commenting on the study, Jeremy Payne, MD, PhD, director of the Stroke Center at Banner Health’s University Medicine Neuroscience Institute in Phoenix, Arizona, noted the importance of predicting which patients might have secondary bleeding after interventional treatment of a large vessel occlusion stroke
“In aggregate, the role of endovascular thrombectomy is quite clear, but we still struggle to predict at the individual patient level who will benefit,” said Dr. Payne, who was not involved with the research.
Transfer and treatment of these patients also carries an economic cost. “Just getting patients to our center, where about 80% of the complex stroke patients come by helicopter, costs upwards of $30,000,” Dr. Payne said. “The financial argument isn’t one we like to talk much about, but we’re committing to spending probably $100,000-$200,000 on each person’s care.”
This study “attempts to address an important issue,” he said.
Predicting who is more likely to benefit leads to the assumption that if that were to happen, “we could skip all the rigamarole of helicopters and procedures, avoid the extra expense and particularly not make things worse than they already are,” explained Dr. Payne.
Potential limitations include that this is a single-center study and is based on an analysis of 19 patients out of 578. As a result, it is not clear that these findings will necessarily be generalizable to other centers, said Dr. Payne.
The TICI and ASPECTS “are pretty obvious markers of risk,” he noted. “The glucose levels, however, are more subtly interesting.”
He also pointed out that an association between diabetes and worse stroke outcomes is well established.
“The mechanisms are poorly understood, but the role of glucose keeps popping up as a potential marker of risk, and so it’s interesting that it bubbles up in their work too,” Dr. Payne said.
Furthermore, unlike TICI and ASPECTS, glucose levels are modifiable.
“Overall, then, we will continue to study this,” Dr. Payne said. “It’s very important to refine our ability to predict which patients may receive benefit versus harm from such procedures, and this is a step in the right direction.”
Some findings were also published December 2019 in the Journal of Neurology, Neurosurgery & Psychiatry.
Montalvo Perero and Payne have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Motalvo Perero MJ et al. AAN 2020, Abstract S20.001.
(ICH), new research suggests. In a study of nearly 600 patients undergoing thrombectomy, investigators combined a modified Thrombolysis in Cerebral Ischemia (TICI) score, an Alberta Stroke Program Early Computed Tomography Score (ASPECTS), and glucose levels (the “TAG score”) to predict risk. Results showed that each unit increase in the combination score was associated with a significant, nearly twofold greater likelihood of symptomatic ICH.
“It is very easy” to calculate the new score in a clinical setting, lead author Mayra Johana Montalvo Perero, MD, Department of Neurology, Brown University and Rhode Island Hospital, Providence, said. “You just need three variables.”
The findings were presented online as part of the 2020 American Academy of Neurology Science Highlights.
Limited data
High TAG scores are associated with symptomatic ICH in patients receiving mechanical thrombectomy, Dr. Montalvo Perero and colleagues said.
Although clinical predictors of symptomatic ICH are well established, “there is limited data in patients who underwent mechanical thrombectomy,” the researchers noted.
To learn more, they assessed 578 patients (52% women; mean age, 73 years) who had mechanical thrombectomy for acute ischemic stroke at a comprehensive stroke center. Within this cohort, 19 patients (3.3%) developed symptomatic ICH.
The investigators compared clinical and radiographic findings between patients who experienced symptomatic ICH and those who did not.
The TICI score emerged as a predictor when each unit decrease in this score was associated with greater risk for symptomatic ICH (odds ratio, 5.13; 95% confidence interval, 1.84-14.29; P = .002).
Each one-point decrease in the ASPECTS score also predicted increased risk (OR, 1.52; 95% CI, 1.1-2.0; P = .003).
“The main driver is the size of the stroke core, which is correlated with the ASPECTS score,” Dr. Montalvo Perero said.
Each 10 mg/dL increase in glucose level also correlated with increased risk (OR, 1.07; 95% CI, 1.01-1.13; P = .018).
Twice the risk
The investigators then combined these three independent variables into a weighted TAG score based on a multivariate analysis. Each unit increase in this composite score was associated with increased risk of symptomatic ICH (OR, 1.98; 95% CI, 1.48-2.66; P < .001).
There was no association between patients who received tissue plasminogen activator (tPA) and risk of symptomatic ICH, which Dr. Montalvo Perero said was surprising.
However, “that may be due to a small number” of patients with symptomatic ICH included in the study, she said. “Therefore, that would be an interesting question to ask in future studies with bigger cohorts.”
Larger studies are also needed to validate this scoring system and to test strategies to reduce risk of symptomatic ICH and make thrombectomy safer in patients with elevated TAG scores, Dr. Montalvo Perero said.
A step in the right direction?
Commenting on the study, Jeremy Payne, MD, PhD, director of the Stroke Center at Banner Health’s University Medicine Neuroscience Institute in Phoenix, Arizona, noted the importance of predicting which patients might have secondary bleeding after interventional treatment of a large vessel occlusion stroke
“In aggregate, the role of endovascular thrombectomy is quite clear, but we still struggle to predict at the individual patient level who will benefit,” said Dr. Payne, who was not involved with the research.
Transfer and treatment of these patients also carries an economic cost. “Just getting patients to our center, where about 80% of the complex stroke patients come by helicopter, costs upwards of $30,000,” Dr. Payne said. “The financial argument isn’t one we like to talk much about, but we’re committing to spending probably $100,000-$200,000 on each person’s care.”
This study “attempts to address an important issue,” he said.
Predicting who is more likely to benefit leads to the assumption that if that were to happen, “we could skip all the rigamarole of helicopters and procedures, avoid the extra expense and particularly not make things worse than they already are,” explained Dr. Payne.
Potential limitations include that this is a single-center study and is based on an analysis of 19 patients out of 578. As a result, it is not clear that these findings will necessarily be generalizable to other centers, said Dr. Payne.
The TICI and ASPECTS “are pretty obvious markers of risk,” he noted. “The glucose levels, however, are more subtly interesting.”
He also pointed out that an association between diabetes and worse stroke outcomes is well established.
“The mechanisms are poorly understood, but the role of glucose keeps popping up as a potential marker of risk, and so it’s interesting that it bubbles up in their work too,” Dr. Payne said.
Furthermore, unlike TICI and ASPECTS, glucose levels are modifiable.
“Overall, then, we will continue to study this,” Dr. Payne said. “It’s very important to refine our ability to predict which patients may receive benefit versus harm from such procedures, and this is a step in the right direction.”
Some findings were also published December 2019 in the Journal of Neurology, Neurosurgery & Psychiatry.
Montalvo Perero and Payne have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Motalvo Perero MJ et al. AAN 2020, Abstract S20.001.
(ICH), new research suggests. In a study of nearly 600 patients undergoing thrombectomy, investigators combined a modified Thrombolysis in Cerebral Ischemia (TICI) score, an Alberta Stroke Program Early Computed Tomography Score (ASPECTS), and glucose levels (the “TAG score”) to predict risk. Results showed that each unit increase in the combination score was associated with a significant, nearly twofold greater likelihood of symptomatic ICH.
“It is very easy” to calculate the new score in a clinical setting, lead author Mayra Johana Montalvo Perero, MD, Department of Neurology, Brown University and Rhode Island Hospital, Providence, said. “You just need three variables.”
The findings were presented online as part of the 2020 American Academy of Neurology Science Highlights.
Limited data
High TAG scores are associated with symptomatic ICH in patients receiving mechanical thrombectomy, Dr. Montalvo Perero and colleagues said.
Although clinical predictors of symptomatic ICH are well established, “there is limited data in patients who underwent mechanical thrombectomy,” the researchers noted.
To learn more, they assessed 578 patients (52% women; mean age, 73 years) who had mechanical thrombectomy for acute ischemic stroke at a comprehensive stroke center. Within this cohort, 19 patients (3.3%) developed symptomatic ICH.
The investigators compared clinical and radiographic findings between patients who experienced symptomatic ICH and those who did not.
The TICI score emerged as a predictor when each unit decrease in this score was associated with greater risk for symptomatic ICH (odds ratio, 5.13; 95% confidence interval, 1.84-14.29; P = .002).
Each one-point decrease in the ASPECTS score also predicted increased risk (OR, 1.52; 95% CI, 1.1-2.0; P = .003).
“The main driver is the size of the stroke core, which is correlated with the ASPECTS score,” Dr. Montalvo Perero said.
Each 10 mg/dL increase in glucose level also correlated with increased risk (OR, 1.07; 95% CI, 1.01-1.13; P = .018).
Twice the risk
The investigators then combined these three independent variables into a weighted TAG score based on a multivariate analysis. Each unit increase in this composite score was associated with increased risk of symptomatic ICH (OR, 1.98; 95% CI, 1.48-2.66; P < .001).
There was no association between patients who received tissue plasminogen activator (tPA) and risk of symptomatic ICH, which Dr. Montalvo Perero said was surprising.
However, “that may be due to a small number” of patients with symptomatic ICH included in the study, she said. “Therefore, that would be an interesting question to ask in future studies with bigger cohorts.”
Larger studies are also needed to validate this scoring system and to test strategies to reduce risk of symptomatic ICH and make thrombectomy safer in patients with elevated TAG scores, Dr. Montalvo Perero said.
A step in the right direction?
Commenting on the study, Jeremy Payne, MD, PhD, director of the Stroke Center at Banner Health’s University Medicine Neuroscience Institute in Phoenix, Arizona, noted the importance of predicting which patients might have secondary bleeding after interventional treatment of a large vessel occlusion stroke
“In aggregate, the role of endovascular thrombectomy is quite clear, but we still struggle to predict at the individual patient level who will benefit,” said Dr. Payne, who was not involved with the research.
Transfer and treatment of these patients also carries an economic cost. “Just getting patients to our center, where about 80% of the complex stroke patients come by helicopter, costs upwards of $30,000,” Dr. Payne said. “The financial argument isn’t one we like to talk much about, but we’re committing to spending probably $100,000-$200,000 on each person’s care.”
This study “attempts to address an important issue,” he said.
Predicting who is more likely to benefit leads to the assumption that if that were to happen, “we could skip all the rigamarole of helicopters and procedures, avoid the extra expense and particularly not make things worse than they already are,” explained Dr. Payne.
Potential limitations include that this is a single-center study and is based on an analysis of 19 patients out of 578. As a result, it is not clear that these findings will necessarily be generalizable to other centers, said Dr. Payne.
The TICI and ASPECTS “are pretty obvious markers of risk,” he noted. “The glucose levels, however, are more subtly interesting.”
He also pointed out that an association between diabetes and worse stroke outcomes is well established.
“The mechanisms are poorly understood, but the role of glucose keeps popping up as a potential marker of risk, and so it’s interesting that it bubbles up in their work too,” Dr. Payne said.
Furthermore, unlike TICI and ASPECTS, glucose levels are modifiable.
“Overall, then, we will continue to study this,” Dr. Payne said. “It’s very important to refine our ability to predict which patients may receive benefit versus harm from such procedures, and this is a step in the right direction.”
Some findings were also published December 2019 in the Journal of Neurology, Neurosurgery & Psychiatry.
Montalvo Perero and Payne have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Motalvo Perero MJ et al. AAN 2020, Abstract S20.001.
AAN 2020