User login
Colorectal cancer is the second most common cause of death in the United States. 1 A colonoscopy is the current gold standard for prevention and early detection of colorectal cancers. During a colonoscopy procedure, polyps and lesions are biopsied and removed. The most effective method of colon cleansing for the procedure is achieved by using one of several commercially available colon lavage preparations. Before the colonoscopy, patients are prescribed and instructed to take one of these bowel preparations.
Background
Adequate bowel preparation is defined as sufficient for identification of polyps > 5 mm.2 The impact of inadequate bowel preparation extends beyond the need for additional or repeat procedure(s) and includes potentially missed polyps and cancers. Inferior bowel preparation quality is associated with a significant decrease in the detection of flat or sessile serrated polyps.3 Missed polyps increase the risk of interval colorectal cancers. A high-quality bowel preparation together with the individual skill and experience of the endoscopist are crucial for adequate polyp detection. In addition, other risks of inadequate bowel preparation and repeated colonoscopies reduce adenoma detection rates, undetected carcinomas, and increase the risk of complications, possibly resulting in lawsuits.3
A major difficulty facing the Veterans Health Administration (VHA) medical center gastroenterologists is what to do when a patient is not properly prepared after standard prescreening education and the bowel preparation regimen. Traditionally, the patient is given additional medication and asked to return the next day for a repeat colonoscopy. Alternatively, the patient is given a 2-day bowel preparation to be used prior to a new appointment.
The choice of bowel preparation has been standardized within the US Department of Veterans Affairs (VA) Connecticut Healthcare System in West Haven (
For patients who fail the standard 1-day preparation, the same trained RNs inquire about any difficulties in consuming the preparation and provide the standard 2-day bowel preparation instructions. Multiple factors impact the adherence with preparation directions. Several patient-specific factors, comorbidities, and medications can contribute to inadequate bowel preparation.4 These factors include failing to fast before the procedure; namely, consuming solid foods, not consuming the entire preparation, not taking the preparation as directed, and not consuming adequate amounts of clear liquids or calories. Other reasons for failing the preparation are nausea and vomiting, poor understanding of instructions (including illiteracy), chronic constipation, use of narcotics and psychotropic drugs, and lack of awareness of the consequences of inadequate bowel preparation.
A study by Hautefeuille and colleagues noted that approximately 20% of patients having colonoscopy failure were not adherent to bowel preparation instructions.5 Only 55% of patients were aware of these consequences; whereas 96% of physicians were convinced they had given appropriate and sufficient information.5 As noted earlier, approximately half of patients do not fully comprehend the need to follow all the instructions. Therefore, clear and concise cleansing instructions and patient adherence are key factors that contribute to efficiency and quality of colonoscopy. The preparation failure rate creates a large volume of repeat patients and contributes to reduced efficiency of outpatient endoscopic practice.
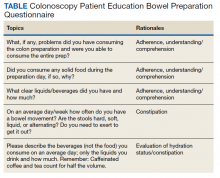
A meta-analysis conducted by Chang and colleagues demonstrated that a brief counseling session with patients before colonoscopy ensured better bowel preparation.6 The focus of this article is on using the Colonoscopy Patient Education Bowel Preparation Questionnaire to improve the outcomes of patient education (Table).
As this was part of ongoing care and medication education; the research did not require reviews by a research committee or need institutional review board approval.
Questionnaire
A gastroenterology (GI) advance practice registered nurse (APRN) developed a patient questionnaire after reviewing patient records from 2016 through 2018 and noting information gaps in patient re-education. The information was not clearly and completely documented relating to frequency of bowel movements, constipation, and daily hydration/fluid intake. Several questions were consistently asked of patients who had previously failed 2 bowel preparations to determine the issues preventing a successful bowel cleansing. Notes from the GI and nutrition clinics and the primary care provider (PCP) were reviewed for information on constipation, frequency and quality of bowel movements, average beverage consumption, and hydration status.
The GI APRN conducted the review and used notes from the past year as well as the notes for prior colon preparations documenting bowel preparations and their resulting quality. A review was conducted on each patient who failed the standard 2-day bowel preparation before the GI APRN bowel preparation education session. The review revealed that no single note provided all necessary information. All colonoscopy prescreening education notes contained information from the standard prescreening preparation education class presentation, and any individual patient issues related to preparation consumption. GI and PCP notes included constipation information; however, frequency of bowel movements was seldom mentioned; and no fluid consumption information was provided except for alcohol related to abuse/addiction issues. Of the patients that had been seen by the Nutrition Department staff, their notes included caloric intake, appropriate food/dietary choices, and soda consumption; alcohol use was documented but related only to caloric intake; again, no other fluid intake amounts were documented.
Design
The questionnaire consists of 5 closed-ended, patient-centered questions aimed at accomplishing patient education in a time-efficient manner. It also is a tool to achieve consistency among staff in determining barriers and issues, improve documentation, and then assist the patient in achieving a good-to-excellent quality bowel preparation. The questions elicit information that allow an RN or PCP determine the factors that contributed to bowel preparation failure and allow for a tailored patient-education session. With a clear picture of the patient’s issues and obstacles, the patient-centered prescreening preparation education could focus on solutions to specific barriers, increase patient comprehension and adherence to the instructions, and identify complicating behavioral factors of the prior bowel preparation. For example, question 1 was designed to discover whether the patient failed to consume the preparation and why, such as volume, timing, or taste; question 4 was designed to assist in figuring out whether constipation for any reason may be present, whether currently diagnosed or not; and question 5 determined the risk of dehydration with or without constipation as a key cleansing issue.
The answers to these few questions determined whether the inadequate bowel preparation quality was due to issues of poor understanding, poor following of the directions, or to other complicating factors.
The prescreening bowel preparation education classes are delivered in groups classes, telehealth group classes, and by phone.
Discussion
Following implementation of the questionnaire from 2018 to 2019, a clinical chart review was conducted in 2019 of the first 100 patients who failed the standardized 2-day preparation from 2018 to 2019. These patients were selected by the GI attending physicians based on their multiple prior research studies and the total number of veterans served within VACHS to reflect an adequate test of change. Twenty patients canceled their appointments or refused to obtain an additional colonoscopy. Of the remaining 80 patients, 68 (85%) improved on the bowel preparation screening to an adequate rating.
Within the VACHS, the result of inadequate colon preparation leads to either an aborted colonoscopy or a longer examination duration due to time spent washing the colon mucosa and then suctioning the liquified stool. Using newchoicehealth.com 2021 national data, the colonoscopy average price range was $1800 to $12,500; the national average amount paid is $2750.7 The average screening or diagnostic colonoscopy cost was $4469.8
Using the Colonoscopy Patient-Education Bowel Prep Questionnaire resulted in increased patient satisfaction, better use of current patient appointment slots, increased unique encounters, and direct and indirect fiscal savings. Patient satisfaction resulted from no additional repeat colonoscopies per patient’s statements. The other findings resulted from the reduction in repeat appointments: The appointment slots that would have been taken by repeat colonoscopies were available for new patients, resulting in an increase in unique encounters.
Fiscal savings resulted from avoiding the need for additional bowel preparations for those patients or using the GI staff time (nurses and clerks) to reschedule and educate patients. Prior to the use of the questionnaire, patients who failed preparations would be re-educated, given a new preparation prescription or mailed a new preparation, scheduled, and then mailed the appropriate paperwork, thus, increasing the workload for nurses and clerks.
Conclusions
Use of the questionnaire resulted in increased high-quality bowel preparation, an increase in the number of unique patients served, and improved efficiency. In addition, recovered appointment slots and modest reductions in additional purchases of preparation kits resulted in a potential cost savings for VACHS. Proper cleansing instructions as well as identifying and overcoming barriers to achieving adequate preparation for colonoscopy resulted in improved patient satisfaction, quality care, and cost savings.
Regardless of the type of colon preparation, addressing patient barriers to bowel preparation is translatable to other endoscopy facilities and practices that provide patient education within the VA.
1. American Cancer Society. Key statistics for colorectal cancer. Revised January 12, 2021. Accessed May 19, 2021. https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html. 2020.
2. Clark BT, Protiva P, Nagar A, et al. Quantification of adequate bowel preparation for screening or surveillance colonoscopy in men. Gastroenterology. 2016;150(2):396-405; quiz e14-e15. doi:10.1053/j.gastro.2015.09.041
3. Clark BT, Laine L. High-quality bowel preparation is required for detection of sessile serrated polyps. Clin Gastroenterol Hepatol. 2016;14(8):1155-1162. doi:10.1016/j.cgh.2016.03.044
4. D’Souza SM, Parekh PJ, Johnson DA. The dirty side of colonoscopy: predictors of poor bowel preparation and novel approaches to overcome the shortcomings. Br J Gastroenterology. 2019:1:1.
5. Hautefeuille G, Lapuelle J, Chaussade S, et al. Factors related to bowel cleansing failure before colonoscopy: results of the PACOME study. J United European Gastroenterol J. 2014; 2(1):22-29. doi:10.1177/2050640613518200
6. Chang CW, Shih SC, Wang HY, et al. Meta-analysis: the effect of patient education on bowel preparation for colonoscopy. Endosc Int Open. 2015;3(6):E646-E652. doi:10.1055/s-0034-1392365
7. New Choice Health. How much does a colonoscopy cost? Accessed May 19, 2021. https://www.newchoicehealth.com/colonoscopy/cost
8. MDsave.com. Colonoscopy. Accessed May 19, 2021. https://www.mdsave.com/f/procedure/colonoscopy/06516?q=colonoscopy&type=procedure
Colorectal cancer is the second most common cause of death in the United States. 1 A colonoscopy is the current gold standard for prevention and early detection of colorectal cancers. During a colonoscopy procedure, polyps and lesions are biopsied and removed. The most effective method of colon cleansing for the procedure is achieved by using one of several commercially available colon lavage preparations. Before the colonoscopy, patients are prescribed and instructed to take one of these bowel preparations.
Background
Adequate bowel preparation is defined as sufficient for identification of polyps > 5 mm.2 The impact of inadequate bowel preparation extends beyond the need for additional or repeat procedure(s) and includes potentially missed polyps and cancers. Inferior bowel preparation quality is associated with a significant decrease in the detection of flat or sessile serrated polyps.3 Missed polyps increase the risk of interval colorectal cancers. A high-quality bowel preparation together with the individual skill and experience of the endoscopist are crucial for adequate polyp detection. In addition, other risks of inadequate bowel preparation and repeated colonoscopies reduce adenoma detection rates, undetected carcinomas, and increase the risk of complications, possibly resulting in lawsuits.3
A major difficulty facing the Veterans Health Administration (VHA) medical center gastroenterologists is what to do when a patient is not properly prepared after standard prescreening education and the bowel preparation regimen. Traditionally, the patient is given additional medication and asked to return the next day for a repeat colonoscopy. Alternatively, the patient is given a 2-day bowel preparation to be used prior to a new appointment.
The choice of bowel preparation has been standardized within the US Department of Veterans Affairs (VA) Connecticut Healthcare System in West Haven (
For patients who fail the standard 1-day preparation, the same trained RNs inquire about any difficulties in consuming the preparation and provide the standard 2-day bowel preparation instructions. Multiple factors impact the adherence with preparation directions. Several patient-specific factors, comorbidities, and medications can contribute to inadequate bowel preparation.4 These factors include failing to fast before the procedure; namely, consuming solid foods, not consuming the entire preparation, not taking the preparation as directed, and not consuming adequate amounts of clear liquids or calories. Other reasons for failing the preparation are nausea and vomiting, poor understanding of instructions (including illiteracy), chronic constipation, use of narcotics and psychotropic drugs, and lack of awareness of the consequences of inadequate bowel preparation.
A study by Hautefeuille and colleagues noted that approximately 20% of patients having colonoscopy failure were not adherent to bowel preparation instructions.5 Only 55% of patients were aware of these consequences; whereas 96% of physicians were convinced they had given appropriate and sufficient information.5 As noted earlier, approximately half of patients do not fully comprehend the need to follow all the instructions. Therefore, clear and concise cleansing instructions and patient adherence are key factors that contribute to efficiency and quality of colonoscopy. The preparation failure rate creates a large volume of repeat patients and contributes to reduced efficiency of outpatient endoscopic practice.
A meta-analysis conducted by Chang and colleagues demonstrated that a brief counseling session with patients before colonoscopy ensured better bowel preparation.6 The focus of this article is on using the Colonoscopy Patient Education Bowel Preparation Questionnaire to improve the outcomes of patient education (Table).
As this was part of ongoing care and medication education; the research did not require reviews by a research committee or need institutional review board approval.
Questionnaire
A gastroenterology (GI) advance practice registered nurse (APRN) developed a patient questionnaire after reviewing patient records from 2016 through 2018 and noting information gaps in patient re-education. The information was not clearly and completely documented relating to frequency of bowel movements, constipation, and daily hydration/fluid intake. Several questions were consistently asked of patients who had previously failed 2 bowel preparations to determine the issues preventing a successful bowel cleansing. Notes from the GI and nutrition clinics and the primary care provider (PCP) were reviewed for information on constipation, frequency and quality of bowel movements, average beverage consumption, and hydration status.
The GI APRN conducted the review and used notes from the past year as well as the notes for prior colon preparations documenting bowel preparations and their resulting quality. A review was conducted on each patient who failed the standard 2-day bowel preparation before the GI APRN bowel preparation education session. The review revealed that no single note provided all necessary information. All colonoscopy prescreening education notes contained information from the standard prescreening preparation education class presentation, and any individual patient issues related to preparation consumption. GI and PCP notes included constipation information; however, frequency of bowel movements was seldom mentioned; and no fluid consumption information was provided except for alcohol related to abuse/addiction issues. Of the patients that had been seen by the Nutrition Department staff, their notes included caloric intake, appropriate food/dietary choices, and soda consumption; alcohol use was documented but related only to caloric intake; again, no other fluid intake amounts were documented.
Design
The questionnaire consists of 5 closed-ended, patient-centered questions aimed at accomplishing patient education in a time-efficient manner. It also is a tool to achieve consistency among staff in determining barriers and issues, improve documentation, and then assist the patient in achieving a good-to-excellent quality bowel preparation. The questions elicit information that allow an RN or PCP determine the factors that contributed to bowel preparation failure and allow for a tailored patient-education session. With a clear picture of the patient’s issues and obstacles, the patient-centered prescreening preparation education could focus on solutions to specific barriers, increase patient comprehension and adherence to the instructions, and identify complicating behavioral factors of the prior bowel preparation. For example, question 1 was designed to discover whether the patient failed to consume the preparation and why, such as volume, timing, or taste; question 4 was designed to assist in figuring out whether constipation for any reason may be present, whether currently diagnosed or not; and question 5 determined the risk of dehydration with or without constipation as a key cleansing issue.
The answers to these few questions determined whether the inadequate bowel preparation quality was due to issues of poor understanding, poor following of the directions, or to other complicating factors.
The prescreening bowel preparation education classes are delivered in groups classes, telehealth group classes, and by phone.
Discussion
Following implementation of the questionnaire from 2018 to 2019, a clinical chart review was conducted in 2019 of the first 100 patients who failed the standardized 2-day preparation from 2018 to 2019. These patients were selected by the GI attending physicians based on their multiple prior research studies and the total number of veterans served within VACHS to reflect an adequate test of change. Twenty patients canceled their appointments or refused to obtain an additional colonoscopy. Of the remaining 80 patients, 68 (85%) improved on the bowel preparation screening to an adequate rating.
Within the VACHS, the result of inadequate colon preparation leads to either an aborted colonoscopy or a longer examination duration due to time spent washing the colon mucosa and then suctioning the liquified stool. Using newchoicehealth.com 2021 national data, the colonoscopy average price range was $1800 to $12,500; the national average amount paid is $2750.7 The average screening or diagnostic colonoscopy cost was $4469.8
Using the Colonoscopy Patient-Education Bowel Prep Questionnaire resulted in increased patient satisfaction, better use of current patient appointment slots, increased unique encounters, and direct and indirect fiscal savings. Patient satisfaction resulted from no additional repeat colonoscopies per patient’s statements. The other findings resulted from the reduction in repeat appointments: The appointment slots that would have been taken by repeat colonoscopies were available for new patients, resulting in an increase in unique encounters.
Fiscal savings resulted from avoiding the need for additional bowel preparations for those patients or using the GI staff time (nurses and clerks) to reschedule and educate patients. Prior to the use of the questionnaire, patients who failed preparations would be re-educated, given a new preparation prescription or mailed a new preparation, scheduled, and then mailed the appropriate paperwork, thus, increasing the workload for nurses and clerks.
Conclusions
Use of the questionnaire resulted in increased high-quality bowel preparation, an increase in the number of unique patients served, and improved efficiency. In addition, recovered appointment slots and modest reductions in additional purchases of preparation kits resulted in a potential cost savings for VACHS. Proper cleansing instructions as well as identifying and overcoming barriers to achieving adequate preparation for colonoscopy resulted in improved patient satisfaction, quality care, and cost savings.
Regardless of the type of colon preparation, addressing patient barriers to bowel preparation is translatable to other endoscopy facilities and practices that provide patient education within the VA.
Colorectal cancer is the second most common cause of death in the United States. 1 A colonoscopy is the current gold standard for prevention and early detection of colorectal cancers. During a colonoscopy procedure, polyps and lesions are biopsied and removed. The most effective method of colon cleansing for the procedure is achieved by using one of several commercially available colon lavage preparations. Before the colonoscopy, patients are prescribed and instructed to take one of these bowel preparations.
Background
Adequate bowel preparation is defined as sufficient for identification of polyps > 5 mm.2 The impact of inadequate bowel preparation extends beyond the need for additional or repeat procedure(s) and includes potentially missed polyps and cancers. Inferior bowel preparation quality is associated with a significant decrease in the detection of flat or sessile serrated polyps.3 Missed polyps increase the risk of interval colorectal cancers. A high-quality bowel preparation together with the individual skill and experience of the endoscopist are crucial for adequate polyp detection. In addition, other risks of inadequate bowel preparation and repeated colonoscopies reduce adenoma detection rates, undetected carcinomas, and increase the risk of complications, possibly resulting in lawsuits.3
A major difficulty facing the Veterans Health Administration (VHA) medical center gastroenterologists is what to do when a patient is not properly prepared after standard prescreening education and the bowel preparation regimen. Traditionally, the patient is given additional medication and asked to return the next day for a repeat colonoscopy. Alternatively, the patient is given a 2-day bowel preparation to be used prior to a new appointment.
The choice of bowel preparation has been standardized within the US Department of Veterans Affairs (VA) Connecticut Healthcare System in West Haven (
For patients who fail the standard 1-day preparation, the same trained RNs inquire about any difficulties in consuming the preparation and provide the standard 2-day bowel preparation instructions. Multiple factors impact the adherence with preparation directions. Several patient-specific factors, comorbidities, and medications can contribute to inadequate bowel preparation.4 These factors include failing to fast before the procedure; namely, consuming solid foods, not consuming the entire preparation, not taking the preparation as directed, and not consuming adequate amounts of clear liquids or calories. Other reasons for failing the preparation are nausea and vomiting, poor understanding of instructions (including illiteracy), chronic constipation, use of narcotics and psychotropic drugs, and lack of awareness of the consequences of inadequate bowel preparation.
A study by Hautefeuille and colleagues noted that approximately 20% of patients having colonoscopy failure were not adherent to bowel preparation instructions.5 Only 55% of patients were aware of these consequences; whereas 96% of physicians were convinced they had given appropriate and sufficient information.5 As noted earlier, approximately half of patients do not fully comprehend the need to follow all the instructions. Therefore, clear and concise cleansing instructions and patient adherence are key factors that contribute to efficiency and quality of colonoscopy. The preparation failure rate creates a large volume of repeat patients and contributes to reduced efficiency of outpatient endoscopic practice.
A meta-analysis conducted by Chang and colleagues demonstrated that a brief counseling session with patients before colonoscopy ensured better bowel preparation.6 The focus of this article is on using the Colonoscopy Patient Education Bowel Preparation Questionnaire to improve the outcomes of patient education (Table).
As this was part of ongoing care and medication education; the research did not require reviews by a research committee or need institutional review board approval.
Questionnaire
A gastroenterology (GI) advance practice registered nurse (APRN) developed a patient questionnaire after reviewing patient records from 2016 through 2018 and noting information gaps in patient re-education. The information was not clearly and completely documented relating to frequency of bowel movements, constipation, and daily hydration/fluid intake. Several questions were consistently asked of patients who had previously failed 2 bowel preparations to determine the issues preventing a successful bowel cleansing. Notes from the GI and nutrition clinics and the primary care provider (PCP) were reviewed for information on constipation, frequency and quality of bowel movements, average beverage consumption, and hydration status.
The GI APRN conducted the review and used notes from the past year as well as the notes for prior colon preparations documenting bowel preparations and their resulting quality. A review was conducted on each patient who failed the standard 2-day bowel preparation before the GI APRN bowel preparation education session. The review revealed that no single note provided all necessary information. All colonoscopy prescreening education notes contained information from the standard prescreening preparation education class presentation, and any individual patient issues related to preparation consumption. GI and PCP notes included constipation information; however, frequency of bowel movements was seldom mentioned; and no fluid consumption information was provided except for alcohol related to abuse/addiction issues. Of the patients that had been seen by the Nutrition Department staff, their notes included caloric intake, appropriate food/dietary choices, and soda consumption; alcohol use was documented but related only to caloric intake; again, no other fluid intake amounts were documented.
Design
The questionnaire consists of 5 closed-ended, patient-centered questions aimed at accomplishing patient education in a time-efficient manner. It also is a tool to achieve consistency among staff in determining barriers and issues, improve documentation, and then assist the patient in achieving a good-to-excellent quality bowel preparation. The questions elicit information that allow an RN or PCP determine the factors that contributed to bowel preparation failure and allow for a tailored patient-education session. With a clear picture of the patient’s issues and obstacles, the patient-centered prescreening preparation education could focus on solutions to specific barriers, increase patient comprehension and adherence to the instructions, and identify complicating behavioral factors of the prior bowel preparation. For example, question 1 was designed to discover whether the patient failed to consume the preparation and why, such as volume, timing, or taste; question 4 was designed to assist in figuring out whether constipation for any reason may be present, whether currently diagnosed or not; and question 5 determined the risk of dehydration with or without constipation as a key cleansing issue.
The answers to these few questions determined whether the inadequate bowel preparation quality was due to issues of poor understanding, poor following of the directions, or to other complicating factors.
The prescreening bowel preparation education classes are delivered in groups classes, telehealth group classes, and by phone.
Discussion
Following implementation of the questionnaire from 2018 to 2019, a clinical chart review was conducted in 2019 of the first 100 patients who failed the standardized 2-day preparation from 2018 to 2019. These patients were selected by the GI attending physicians based on their multiple prior research studies and the total number of veterans served within VACHS to reflect an adequate test of change. Twenty patients canceled their appointments or refused to obtain an additional colonoscopy. Of the remaining 80 patients, 68 (85%) improved on the bowel preparation screening to an adequate rating.
Within the VACHS, the result of inadequate colon preparation leads to either an aborted colonoscopy or a longer examination duration due to time spent washing the colon mucosa and then suctioning the liquified stool. Using newchoicehealth.com 2021 national data, the colonoscopy average price range was $1800 to $12,500; the national average amount paid is $2750.7 The average screening or diagnostic colonoscopy cost was $4469.8
Using the Colonoscopy Patient-Education Bowel Prep Questionnaire resulted in increased patient satisfaction, better use of current patient appointment slots, increased unique encounters, and direct and indirect fiscal savings. Patient satisfaction resulted from no additional repeat colonoscopies per patient’s statements. The other findings resulted from the reduction in repeat appointments: The appointment slots that would have been taken by repeat colonoscopies were available for new patients, resulting in an increase in unique encounters.
Fiscal savings resulted from avoiding the need for additional bowel preparations for those patients or using the GI staff time (nurses and clerks) to reschedule and educate patients. Prior to the use of the questionnaire, patients who failed preparations would be re-educated, given a new preparation prescription or mailed a new preparation, scheduled, and then mailed the appropriate paperwork, thus, increasing the workload for nurses and clerks.
Conclusions
Use of the questionnaire resulted in increased high-quality bowel preparation, an increase in the number of unique patients served, and improved efficiency. In addition, recovered appointment slots and modest reductions in additional purchases of preparation kits resulted in a potential cost savings for VACHS. Proper cleansing instructions as well as identifying and overcoming barriers to achieving adequate preparation for colonoscopy resulted in improved patient satisfaction, quality care, and cost savings.
Regardless of the type of colon preparation, addressing patient barriers to bowel preparation is translatable to other endoscopy facilities and practices that provide patient education within the VA.
1. American Cancer Society. Key statistics for colorectal cancer. Revised January 12, 2021. Accessed May 19, 2021. https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html. 2020.
2. Clark BT, Protiva P, Nagar A, et al. Quantification of adequate bowel preparation for screening or surveillance colonoscopy in men. Gastroenterology. 2016;150(2):396-405; quiz e14-e15. doi:10.1053/j.gastro.2015.09.041
3. Clark BT, Laine L. High-quality bowel preparation is required for detection of sessile serrated polyps. Clin Gastroenterol Hepatol. 2016;14(8):1155-1162. doi:10.1016/j.cgh.2016.03.044
4. D’Souza SM, Parekh PJ, Johnson DA. The dirty side of colonoscopy: predictors of poor bowel preparation and novel approaches to overcome the shortcomings. Br J Gastroenterology. 2019:1:1.
5. Hautefeuille G, Lapuelle J, Chaussade S, et al. Factors related to bowel cleansing failure before colonoscopy: results of the PACOME study. J United European Gastroenterol J. 2014; 2(1):22-29. doi:10.1177/2050640613518200
6. Chang CW, Shih SC, Wang HY, et al. Meta-analysis: the effect of patient education on bowel preparation for colonoscopy. Endosc Int Open. 2015;3(6):E646-E652. doi:10.1055/s-0034-1392365
7. New Choice Health. How much does a colonoscopy cost? Accessed May 19, 2021. https://www.newchoicehealth.com/colonoscopy/cost
8. MDsave.com. Colonoscopy. Accessed May 19, 2021. https://www.mdsave.com/f/procedure/colonoscopy/06516?q=colonoscopy&type=procedure
1. American Cancer Society. Key statistics for colorectal cancer. Revised January 12, 2021. Accessed May 19, 2021. https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html. 2020.
2. Clark BT, Protiva P, Nagar A, et al. Quantification of adequate bowel preparation for screening or surveillance colonoscopy in men. Gastroenterology. 2016;150(2):396-405; quiz e14-e15. doi:10.1053/j.gastro.2015.09.041
3. Clark BT, Laine L. High-quality bowel preparation is required for detection of sessile serrated polyps. Clin Gastroenterol Hepatol. 2016;14(8):1155-1162. doi:10.1016/j.cgh.2016.03.044
4. D’Souza SM, Parekh PJ, Johnson DA. The dirty side of colonoscopy: predictors of poor bowel preparation and novel approaches to overcome the shortcomings. Br J Gastroenterology. 2019:1:1.
5. Hautefeuille G, Lapuelle J, Chaussade S, et al. Factors related to bowel cleansing failure before colonoscopy: results of the PACOME study. J United European Gastroenterol J. 2014; 2(1):22-29. doi:10.1177/2050640613518200
6. Chang CW, Shih SC, Wang HY, et al. Meta-analysis: the effect of patient education on bowel preparation for colonoscopy. Endosc Int Open. 2015;3(6):E646-E652. doi:10.1055/s-0034-1392365
7. New Choice Health. How much does a colonoscopy cost? Accessed May 19, 2021. https://www.newchoicehealth.com/colonoscopy/cost
8. MDsave.com. Colonoscopy. Accessed May 19, 2021. https://www.mdsave.com/f/procedure/colonoscopy/06516?q=colonoscopy&type=procedure