User login
Mohs micrographic surgery (MMS) remains the gold standard for the removal of skin cancers in high-risk areas of the body while offering an excellent safety profile and sparing tissue.1 In the current health care environment, online patient reviews have grown in popularity and influence. More than 60% of consumers consult social media before making health care decisions.2 A recent analysis of online patient reviews of general dermatology practices demonstrated the perceived importance of physician empathy, thoroughness, and cognizance of cost in relation to patient-reported satisfaction.3 Because MMS is a well-recognized and unique outpatient-based surgical procedure, a review and analysis of online patient reviews specific to MMS can provide useful practice insights.
Materials and Methods
This study was conducted using an online platform (RealSelf [http://www.realself.com]) that connects patients and providers offering aesthetically oriented procedures; the site has 35 million unique visitors yearly.4 The community’s directory was used to identify and analyze all cumulative patient reviews from 2006 to December 20, 2015, using the search terms Mohs surgery or Mohs micrographic surgery. The study was exempt by the Northwestern University (Chicago, Illinois) institutional review board.
A standardized qualitative coding methodology was created and applied to all available comments regarding MMS. A broad list of positive and negative patient experiences was first created and agreed upon by all 3 investigators. Each individual comment was then attributed to 1 or more of these positive or negative themes. Of these comments, 10% were coded by 2 investigators (S.X. and Z.A.) to ensure internal validity; 1 investigator coded the remaining statements by patients (Z.A.). Patient-reported satisfaction ratings categorized as “worth it” or “not worth it” (as used by RealSelf to describe the patient-perceived value and utility of a given procedure) as well as cost of MMS were gathered. Cumulative patient ratings were collected for the procedure overall, physician’s bedside manner, answered questions, aftercare follow-up, time spent with patients, telephone/email responsiveness, staff professionalism/courtesy, payment process, and wait times. Patient-reported characteristics of MMS also were evaluated including physician specialty, lesion location, type of skin cancer, and type of closure. For lesion location, we graded whether the location represented a high-risk area as defined by the American Academy of Dermatology, American College of Mohs Surgery, and American Society for Dermatologic Surgery.5
Results
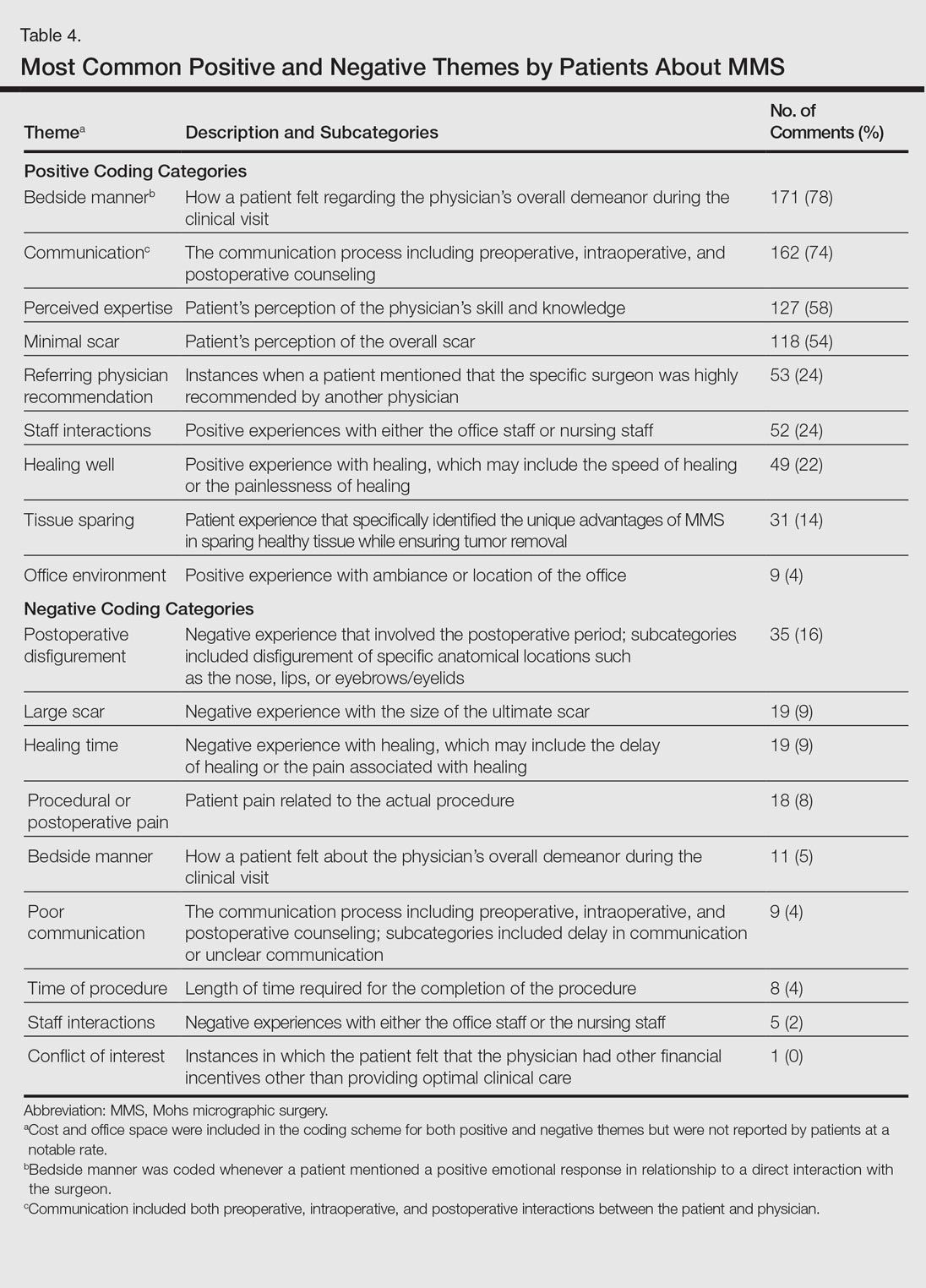
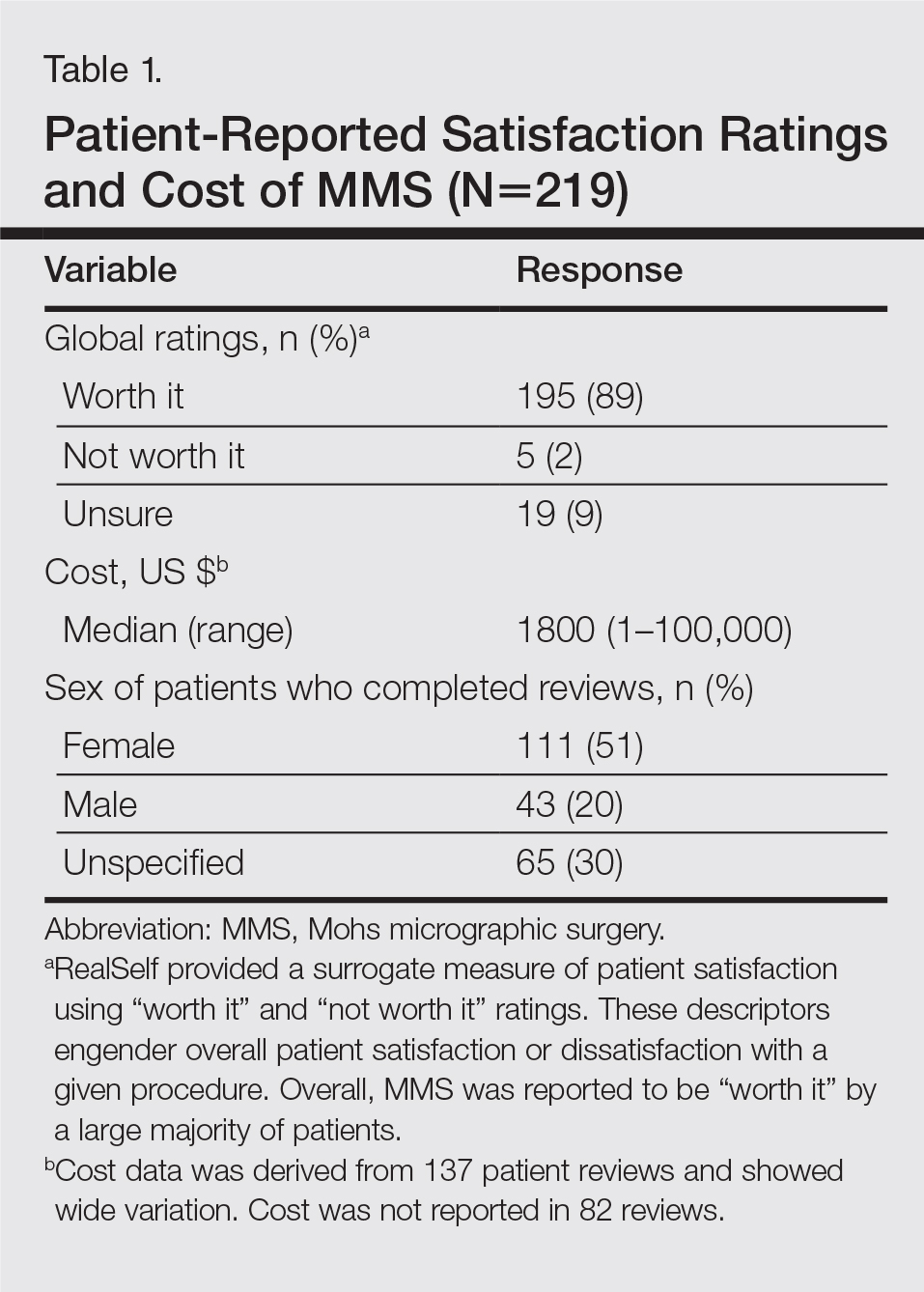
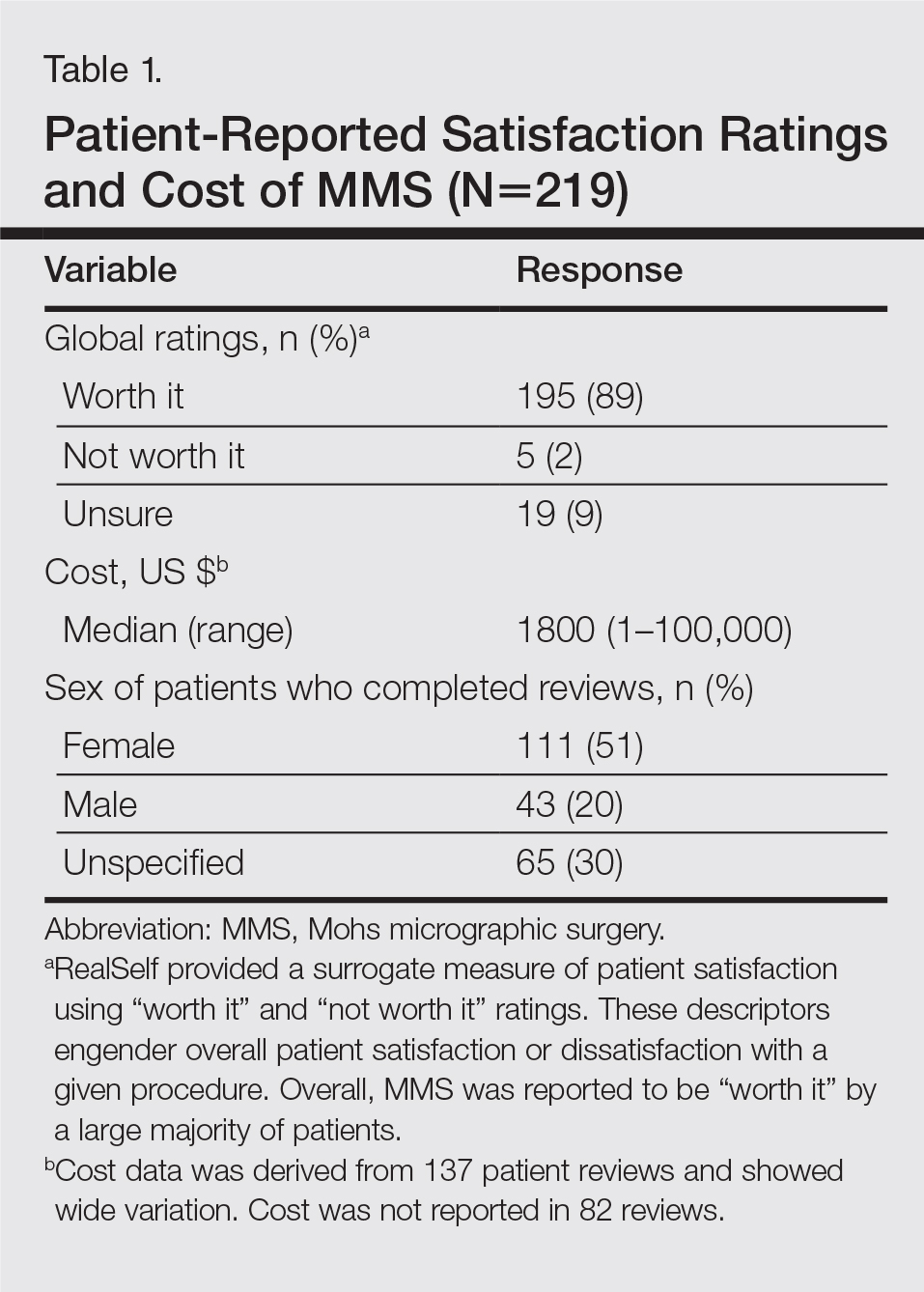
A total of 219 reviews related to MMS were collected as of December 20, 2015. Overall, MMS was considered “worth it” by 89% of patients (Table 1). Only 2% of patients described MMS as “not worth it.” There was a wide range reported for the cost of the procedure ($1–$100,000 [median, $1800]). Of those patients who reported their sex, females were 2.5-times more likely to post a review compared to males (51% vs 20%); however, 30% of reviewers did not report their sex. The mean (standard deviation) overall satisfaction rating was 4.8 (0.8). With regard to category-specific ratings (eg, bedside manner, aftercare follow-up, time spent with patients), the mean scores were all 4.7 or greater (Table 2).

Regarding the surgical aspects of the procedure, the majority of patients reported that the excision of the lesion was performed by a dermatologist (62%). However, a notable portion of patients reported that the excision was performed by a plastic surgeon (21%). Physician specialty was not reported in 16% of the reviews. For the lesion closure, the patient-reported specialty of the physician was only slightly higher for dermatologists versus plastic surgeons (46% vs 44%)(Table 3).

The majority of patients who reported the location of the lesion treated with MMS identified a high-risk location (45%), a medium-risk location (18%), or an unspecified region of the face (15%), according to the appropriate-use criteria for MMS (Table 3).5 Patients did not specify the site of surgery 17% of the time. Only 5% of reported procedures were performed on low-risk areas.
Basal cell carcinomas were the most commonly reported lesions removed by MMS (38%), though 48% of reviews did not specify the type of tumor being treated (Table 3). A large majority (76%) did not specify the type of closure performed. When specified, secondary intention was used 10% of the time, followed by either a flap (6%) or skin graft (6%). Only 5% of patients reported an estimated size of the primary lesion in our study (data not shown).
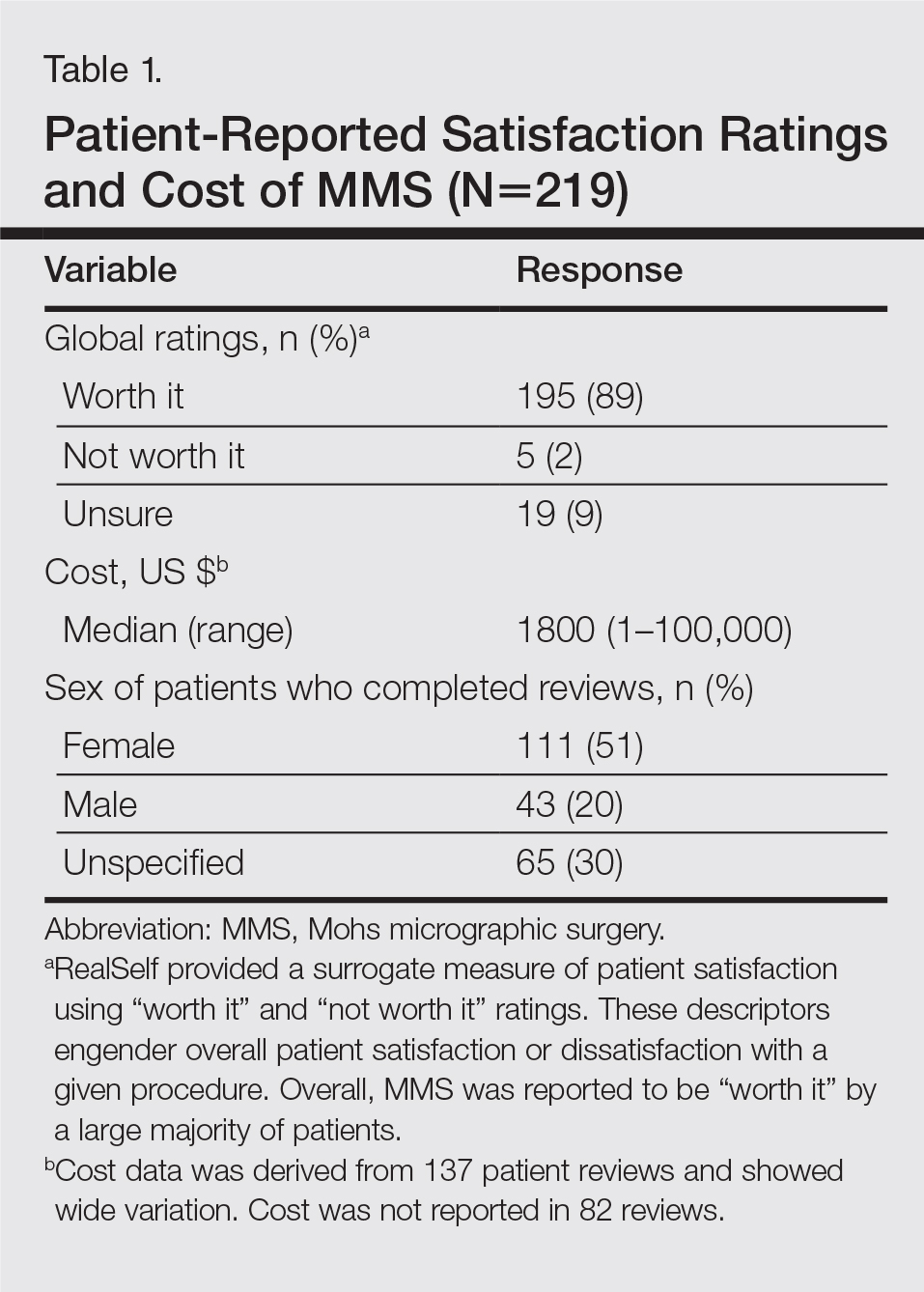
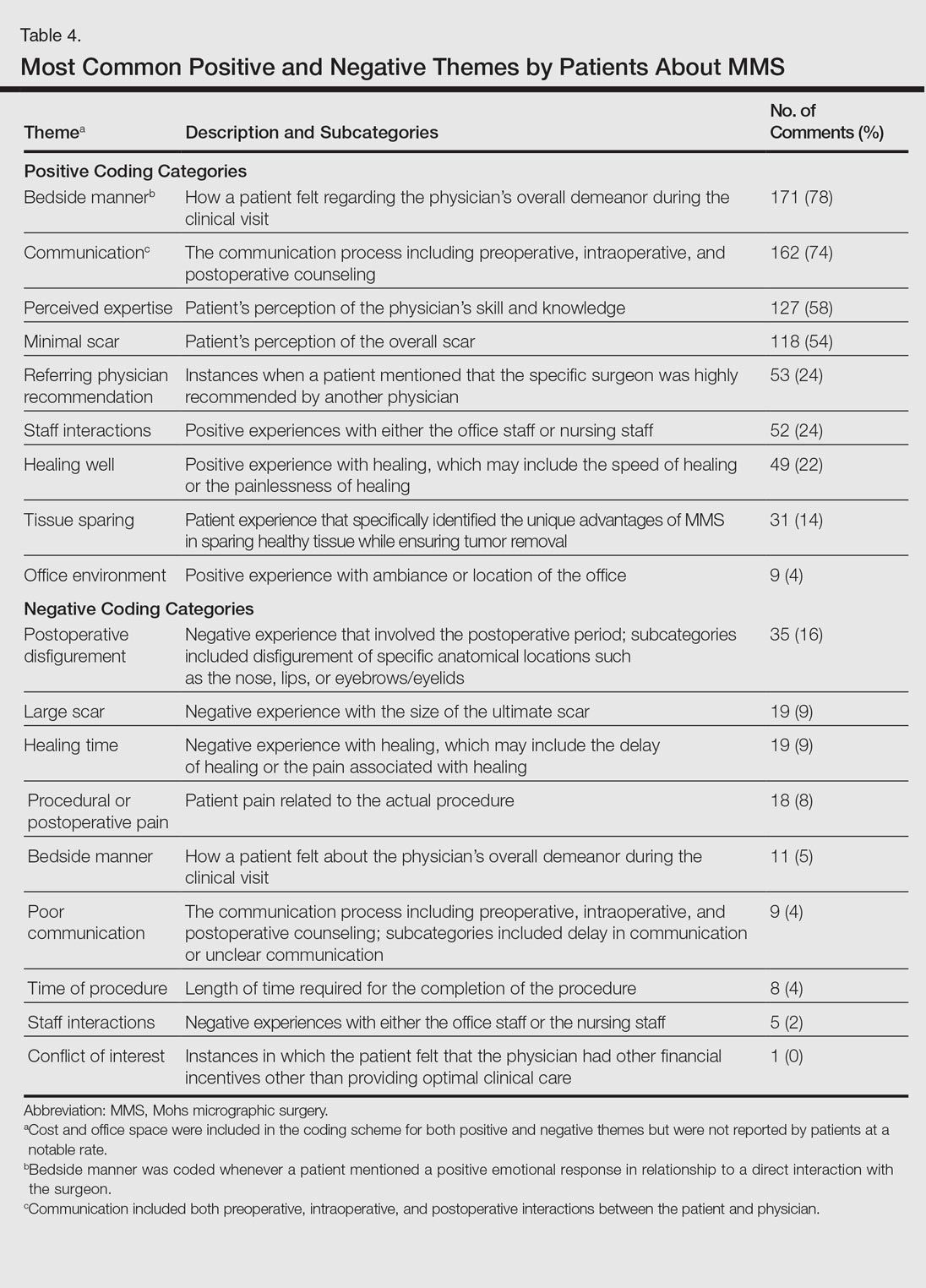
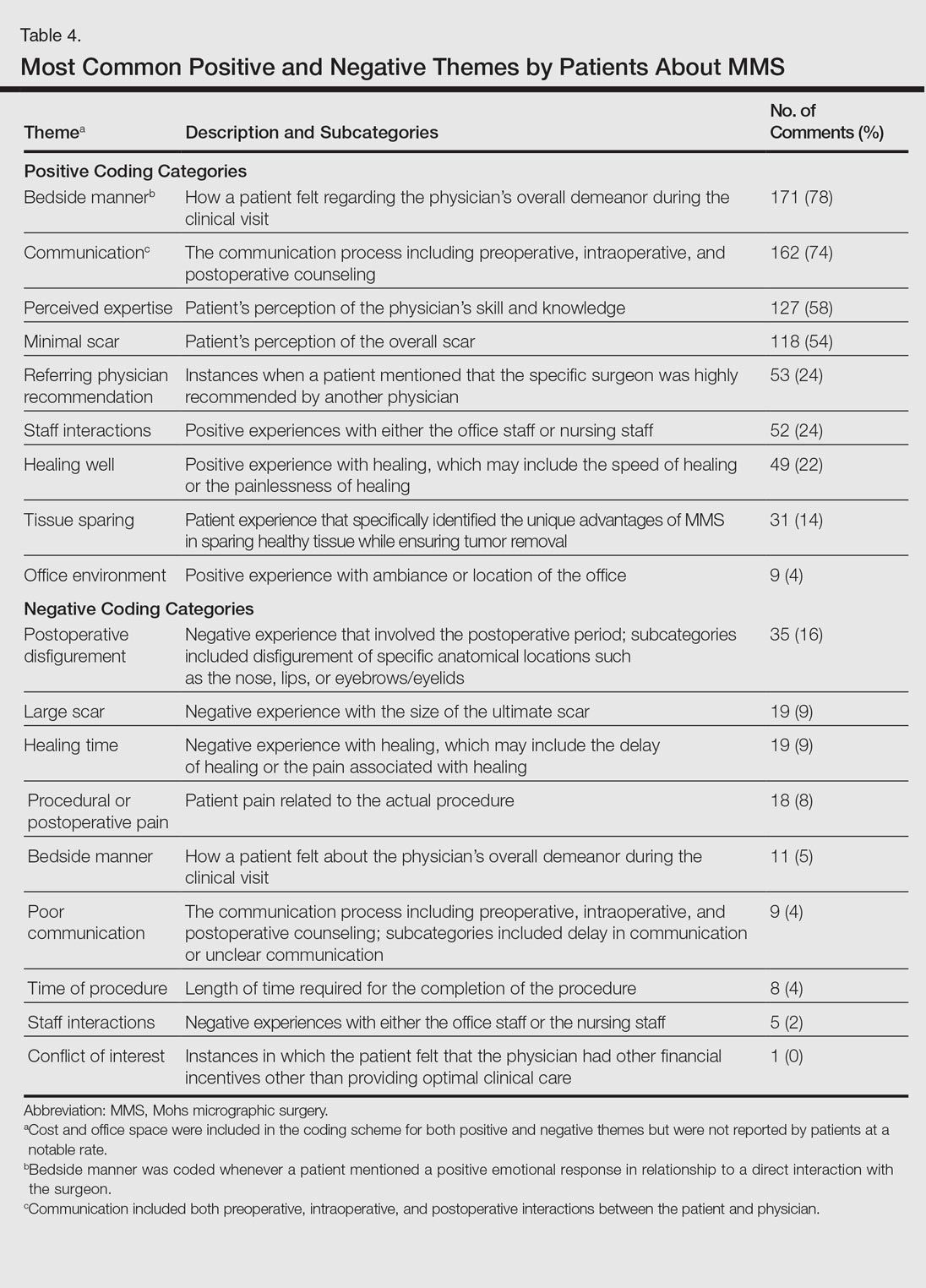
The qualitative analysis demonstrated variance in themes for positive and negative characteristics (Table 4). Surgeon characteristics encompassed the 3 most commonly cited themes of positive remarks, including bedside manner (78%), communication skills (74%), and perceived expertise (58%). Specific to MMS, the tissue-sparing nature of the technique was cited by 14% of reviews as a positive theme. The most commonly cited themes of negative remarks were intraoperative and postoperative concerns, including postoperative disfigurement (16%), large scar (9%), healing time (9%), and procedural or postoperative pain (8%). A subtheme analysis of postoperative disfigurement revealed that eyelid or eyebrow distortion was the most common concern (29%), followed by redness and swelling (23%), an open wound (14%), and nostril/nose distortion (14%)(data not shown). Themes not commonly cited as either positive or negative included office environment, cost, and procedure time (data not shown).
Comment
The overall satisfaction with MMS (89%) was one of the highest for any procedure on this online patient review site, albeit based on fewer reviews compared to other common aesthetic surgical procedures. In comparison, 78% of 13,500 reviewers rated breast augmentation as “worth it,” while 60% of 6800 reviewers rated rhinoplasty as “worth it” (as of December 2015). Overall, the online patient reviews evaluated in this study were consistent with a previously published structured data report on patient satisfaction with MMS.6
The results show a greater than expected proportion of both the MMS excision and closure being performed by plastic surgeons compared to dermatologists. In reality, the majority of MMS excisions are performed by dermatologists. Based on a survey of American College of Mohs Surgery (ACMS) members, only 6% of procedures were sent to other specialties for closure.7 Our results may reflect reporting bias or patients misconstruing true MMS with an excision and standard frozen sections, techniques that have lower cure rates. If so, there may be a need to educate patients regarding the specifics of MMS. Other possible explanations for the discrepancy between the online patient reviews and ACMS data include misinterpretation by patients on the exact definition of MMS or that a higher than expected number of procedures were performed by non-ACMS Mohs surgeons.
Our qualitative analysis revealed that patients most frequently commented on the interpersonal skills of their surgeons (eg, bedside manner, communication) as positive themes during MMS, similar to prior analyses of general dermatology practices.3 In comparison to a recent study assessing patient satisfaction with rhinoplasty on RealSelf, the final appearance of the nose represented the most common positive- and negative-cited theme.8 Mohs micrographic surgery procedures typically are done under local anesthesia, which may explain the greater importance of bedside manner and communication intraoperatively in comparison to final surgical outcomes for patient satisfaction. For negative themes, 3 of 4 most common concerns were directly related to the intraoperative and postoperative periods. Providers may be able to improve patient satisfaction by explaining the postoperative course, such as healing time and temporary physical restrictions, as well as possible sequelae in greater detail, which may be particularly pertinent for MMS involving the nose or near the eyes.
The global ratings for MMS are high, as shown in our data set of patient reviews; however, patient reviews are highly susceptible to reporting bias, recall bias, and missing information. Prior work using this online patient review website to investigate laser and light procedures also demonstrated the risk for imperfect information associated with patient reviews.9 Even so, the data does provide a glimpse into what is considered important to patients. Surgeon interpersonal skills and communication were the most frequently cited positive themes for MMS. The best surgical aspects of MMS focused on the unique tissue-sparing nature of the procedure and the removal of a cancerous lesion. Potential areas for improvement include a more thorough explanation of the intraoperative and postoperative process, specifically potential asymmetry related to the nose or the eyes, healing time, and scarring. These patient reviews underscore the importance of setting appropriate patient expectations. As patients become more connected and utilize online platforms to report their experiences, Mohs surgeons can take insights derived from online patient reviews for their own practice or geographic area to improve satisfaction and manage expectations.
- Alam M, Ibrahim O, Nodzenski M, et al. Adverse events associated with Mohs micrographic surgery: multicenter prospective cohort study of 20,821 cases at 23 centers. JAMA Dermatol. 2013;149:1378-1385.
- Fox S. The social life of health information. Pew Research Center website. http://www.pewresearch.org/fact-tank/2014/01/15/the-social-life-of-health-information/. Published January 15, 2014. Accessed February 11, 2017.
- Smith RJ, Lipoff JB. Evaluation of dermatology practice online reviews: lessons from qualitative analysis. JAMA Dermatol. 2016;152:153-157.
- Schlichte MJ, Karimkhani C, Jones T, et al. Patient use of social media to evaluate cosmetic treatments and procedures. Dermatol Online J. 2015;21. pii:13030/qt88z6r65x.
- American Academy of Dermatology; American College of Mohs Surgery; American Society for Dermatologic Surgery Association; American Society for Mohs Surgery; Ad Hoc Task Force, Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery [published online September 7, 2012]. Dermatol Surg. 2012;38:1582-1603.
- Asgari MM, Bertenthal D, Sen S, et al. Patient satisfaction after treatment of nonmelanoma skin cancer. Derm Surg. 2009;35:1041-1049.
- Campbell RM, Perlis CS, Malik MK, et al. Characteristics of Mohs practices in the United States: a recall survey of ACMS surgeons. Dermatol Surg. 2007;33:1413-1418; discussion, 1418.
- Khansa I, Khansa L, Pearson GD. Patient satisfaction after rhinoplasty: a social media analysis. Aesthet Surg J. 2016;36:NP1-5.
- Xu S, Walter J, Bhatia A. Patient-reported online satisfaction for laser and light procedures: need for caution. Dermatol Surg. 2017;43:154-158.
Mohs micrographic surgery (MMS) remains the gold standard for the removal of skin cancers in high-risk areas of the body while offering an excellent safety profile and sparing tissue.1 In the current health care environment, online patient reviews have grown in popularity and influence. More than 60% of consumers consult social media before making health care decisions.2 A recent analysis of online patient reviews of general dermatology practices demonstrated the perceived importance of physician empathy, thoroughness, and cognizance of cost in relation to patient-reported satisfaction.3 Because MMS is a well-recognized and unique outpatient-based surgical procedure, a review and analysis of online patient reviews specific to MMS can provide useful practice insights.
Materials and Methods
This study was conducted using an online platform (RealSelf [http://www.realself.com]) that connects patients and providers offering aesthetically oriented procedures; the site has 35 million unique visitors yearly.4 The community’s directory was used to identify and analyze all cumulative patient reviews from 2006 to December 20, 2015, using the search terms Mohs surgery or Mohs micrographic surgery. The study was exempt by the Northwestern University (Chicago, Illinois) institutional review board.
A standardized qualitative coding methodology was created and applied to all available comments regarding MMS. A broad list of positive and negative patient experiences was first created and agreed upon by all 3 investigators. Each individual comment was then attributed to 1 or more of these positive or negative themes. Of these comments, 10% were coded by 2 investigators (S.X. and Z.A.) to ensure internal validity; 1 investigator coded the remaining statements by patients (Z.A.). Patient-reported satisfaction ratings categorized as “worth it” or “not worth it” (as used by RealSelf to describe the patient-perceived value and utility of a given procedure) as well as cost of MMS were gathered. Cumulative patient ratings were collected for the procedure overall, physician’s bedside manner, answered questions, aftercare follow-up, time spent with patients, telephone/email responsiveness, staff professionalism/courtesy, payment process, and wait times. Patient-reported characteristics of MMS also were evaluated including physician specialty, lesion location, type of skin cancer, and type of closure. For lesion location, we graded whether the location represented a high-risk area as defined by the American Academy of Dermatology, American College of Mohs Surgery, and American Society for Dermatologic Surgery.5
Results
A total of 219 reviews related to MMS were collected as of December 20, 2015. Overall, MMS was considered “worth it” by 89% of patients (Table 1). Only 2% of patients described MMS as “not worth it.” There was a wide range reported for the cost of the procedure ($1–$100,000 [median, $1800]). Of those patients who reported their sex, females were 2.5-times more likely to post a review compared to males (51% vs 20%); however, 30% of reviewers did not report their sex. The mean (standard deviation) overall satisfaction rating was 4.8 (0.8). With regard to category-specific ratings (eg, bedside manner, aftercare follow-up, time spent with patients), the mean scores were all 4.7 or greater (Table 2).

Regarding the surgical aspects of the procedure, the majority of patients reported that the excision of the lesion was performed by a dermatologist (62%). However, a notable portion of patients reported that the excision was performed by a plastic surgeon (21%). Physician specialty was not reported in 16% of the reviews. For the lesion closure, the patient-reported specialty of the physician was only slightly higher for dermatologists versus plastic surgeons (46% vs 44%)(Table 3).

The majority of patients who reported the location of the lesion treated with MMS identified a high-risk location (45%), a medium-risk location (18%), or an unspecified region of the face (15%), according to the appropriate-use criteria for MMS (Table 3).5 Patients did not specify the site of surgery 17% of the time. Only 5% of reported procedures were performed on low-risk areas.
Basal cell carcinomas were the most commonly reported lesions removed by MMS (38%), though 48% of reviews did not specify the type of tumor being treated (Table 3). A large majority (76%) did not specify the type of closure performed. When specified, secondary intention was used 10% of the time, followed by either a flap (6%) or skin graft (6%). Only 5% of patients reported an estimated size of the primary lesion in our study (data not shown).
The qualitative analysis demonstrated variance in themes for positive and negative characteristics (Table 4). Surgeon characteristics encompassed the 3 most commonly cited themes of positive remarks, including bedside manner (78%), communication skills (74%), and perceived expertise (58%). Specific to MMS, the tissue-sparing nature of the technique was cited by 14% of reviews as a positive theme. The most commonly cited themes of negative remarks were intraoperative and postoperative concerns, including postoperative disfigurement (16%), large scar (9%), healing time (9%), and procedural or postoperative pain (8%). A subtheme analysis of postoperative disfigurement revealed that eyelid or eyebrow distortion was the most common concern (29%), followed by redness and swelling (23%), an open wound (14%), and nostril/nose distortion (14%)(data not shown). Themes not commonly cited as either positive or negative included office environment, cost, and procedure time (data not shown).
Comment
The overall satisfaction with MMS (89%) was one of the highest for any procedure on this online patient review site, albeit based on fewer reviews compared to other common aesthetic surgical procedures. In comparison, 78% of 13,500 reviewers rated breast augmentation as “worth it,” while 60% of 6800 reviewers rated rhinoplasty as “worth it” (as of December 2015). Overall, the online patient reviews evaluated in this study were consistent with a previously published structured data report on patient satisfaction with MMS.6
The results show a greater than expected proportion of both the MMS excision and closure being performed by plastic surgeons compared to dermatologists. In reality, the majority of MMS excisions are performed by dermatologists. Based on a survey of American College of Mohs Surgery (ACMS) members, only 6% of procedures were sent to other specialties for closure.7 Our results may reflect reporting bias or patients misconstruing true MMS with an excision and standard frozen sections, techniques that have lower cure rates. If so, there may be a need to educate patients regarding the specifics of MMS. Other possible explanations for the discrepancy between the online patient reviews and ACMS data include misinterpretation by patients on the exact definition of MMS or that a higher than expected number of procedures were performed by non-ACMS Mohs surgeons.
Our qualitative analysis revealed that patients most frequently commented on the interpersonal skills of their surgeons (eg, bedside manner, communication) as positive themes during MMS, similar to prior analyses of general dermatology practices.3 In comparison to a recent study assessing patient satisfaction with rhinoplasty on RealSelf, the final appearance of the nose represented the most common positive- and negative-cited theme.8 Mohs micrographic surgery procedures typically are done under local anesthesia, which may explain the greater importance of bedside manner and communication intraoperatively in comparison to final surgical outcomes for patient satisfaction. For negative themes, 3 of 4 most common concerns were directly related to the intraoperative and postoperative periods. Providers may be able to improve patient satisfaction by explaining the postoperative course, such as healing time and temporary physical restrictions, as well as possible sequelae in greater detail, which may be particularly pertinent for MMS involving the nose or near the eyes.
The global ratings for MMS are high, as shown in our data set of patient reviews; however, patient reviews are highly susceptible to reporting bias, recall bias, and missing information. Prior work using this online patient review website to investigate laser and light procedures also demonstrated the risk for imperfect information associated with patient reviews.9 Even so, the data does provide a glimpse into what is considered important to patients. Surgeon interpersonal skills and communication were the most frequently cited positive themes for MMS. The best surgical aspects of MMS focused on the unique tissue-sparing nature of the procedure and the removal of a cancerous lesion. Potential areas for improvement include a more thorough explanation of the intraoperative and postoperative process, specifically potential asymmetry related to the nose or the eyes, healing time, and scarring. These patient reviews underscore the importance of setting appropriate patient expectations. As patients become more connected and utilize online platforms to report their experiences, Mohs surgeons can take insights derived from online patient reviews for their own practice or geographic area to improve satisfaction and manage expectations.
Mohs micrographic surgery (MMS) remains the gold standard for the removal of skin cancers in high-risk areas of the body while offering an excellent safety profile and sparing tissue.1 In the current health care environment, online patient reviews have grown in popularity and influence. More than 60% of consumers consult social media before making health care decisions.2 A recent analysis of online patient reviews of general dermatology practices demonstrated the perceived importance of physician empathy, thoroughness, and cognizance of cost in relation to patient-reported satisfaction.3 Because MMS is a well-recognized and unique outpatient-based surgical procedure, a review and analysis of online patient reviews specific to MMS can provide useful practice insights.
Materials and Methods
This study was conducted using an online platform (RealSelf [http://www.realself.com]) that connects patients and providers offering aesthetically oriented procedures; the site has 35 million unique visitors yearly.4 The community’s directory was used to identify and analyze all cumulative patient reviews from 2006 to December 20, 2015, using the search terms Mohs surgery or Mohs micrographic surgery. The study was exempt by the Northwestern University (Chicago, Illinois) institutional review board.
A standardized qualitative coding methodology was created and applied to all available comments regarding MMS. A broad list of positive and negative patient experiences was first created and agreed upon by all 3 investigators. Each individual comment was then attributed to 1 or more of these positive or negative themes. Of these comments, 10% were coded by 2 investigators (S.X. and Z.A.) to ensure internal validity; 1 investigator coded the remaining statements by patients (Z.A.). Patient-reported satisfaction ratings categorized as “worth it” or “not worth it” (as used by RealSelf to describe the patient-perceived value and utility of a given procedure) as well as cost of MMS were gathered. Cumulative patient ratings were collected for the procedure overall, physician’s bedside manner, answered questions, aftercare follow-up, time spent with patients, telephone/email responsiveness, staff professionalism/courtesy, payment process, and wait times. Patient-reported characteristics of MMS also were evaluated including physician specialty, lesion location, type of skin cancer, and type of closure. For lesion location, we graded whether the location represented a high-risk area as defined by the American Academy of Dermatology, American College of Mohs Surgery, and American Society for Dermatologic Surgery.5
Results
A total of 219 reviews related to MMS were collected as of December 20, 2015. Overall, MMS was considered “worth it” by 89% of patients (Table 1). Only 2% of patients described MMS as “not worth it.” There was a wide range reported for the cost of the procedure ($1–$100,000 [median, $1800]). Of those patients who reported their sex, females were 2.5-times more likely to post a review compared to males (51% vs 20%); however, 30% of reviewers did not report their sex. The mean (standard deviation) overall satisfaction rating was 4.8 (0.8). With regard to category-specific ratings (eg, bedside manner, aftercare follow-up, time spent with patients), the mean scores were all 4.7 or greater (Table 2).

Regarding the surgical aspects of the procedure, the majority of patients reported that the excision of the lesion was performed by a dermatologist (62%). However, a notable portion of patients reported that the excision was performed by a plastic surgeon (21%). Physician specialty was not reported in 16% of the reviews. For the lesion closure, the patient-reported specialty of the physician was only slightly higher for dermatologists versus plastic surgeons (46% vs 44%)(Table 3).

The majority of patients who reported the location of the lesion treated with MMS identified a high-risk location (45%), a medium-risk location (18%), or an unspecified region of the face (15%), according to the appropriate-use criteria for MMS (Table 3).5 Patients did not specify the site of surgery 17% of the time. Only 5% of reported procedures were performed on low-risk areas.
Basal cell carcinomas were the most commonly reported lesions removed by MMS (38%), though 48% of reviews did not specify the type of tumor being treated (Table 3). A large majority (76%) did not specify the type of closure performed. When specified, secondary intention was used 10% of the time, followed by either a flap (6%) or skin graft (6%). Only 5% of patients reported an estimated size of the primary lesion in our study (data not shown).
The qualitative analysis demonstrated variance in themes for positive and negative characteristics (Table 4). Surgeon characteristics encompassed the 3 most commonly cited themes of positive remarks, including bedside manner (78%), communication skills (74%), and perceived expertise (58%). Specific to MMS, the tissue-sparing nature of the technique was cited by 14% of reviews as a positive theme. The most commonly cited themes of negative remarks were intraoperative and postoperative concerns, including postoperative disfigurement (16%), large scar (9%), healing time (9%), and procedural or postoperative pain (8%). A subtheme analysis of postoperative disfigurement revealed that eyelid or eyebrow distortion was the most common concern (29%), followed by redness and swelling (23%), an open wound (14%), and nostril/nose distortion (14%)(data not shown). Themes not commonly cited as either positive or negative included office environment, cost, and procedure time (data not shown).
Comment
The overall satisfaction with MMS (89%) was one of the highest for any procedure on this online patient review site, albeit based on fewer reviews compared to other common aesthetic surgical procedures. In comparison, 78% of 13,500 reviewers rated breast augmentation as “worth it,” while 60% of 6800 reviewers rated rhinoplasty as “worth it” (as of December 2015). Overall, the online patient reviews evaluated in this study were consistent with a previously published structured data report on patient satisfaction with MMS.6
The results show a greater than expected proportion of both the MMS excision and closure being performed by plastic surgeons compared to dermatologists. In reality, the majority of MMS excisions are performed by dermatologists. Based on a survey of American College of Mohs Surgery (ACMS) members, only 6% of procedures were sent to other specialties for closure.7 Our results may reflect reporting bias or patients misconstruing true MMS with an excision and standard frozen sections, techniques that have lower cure rates. If so, there may be a need to educate patients regarding the specifics of MMS. Other possible explanations for the discrepancy between the online patient reviews and ACMS data include misinterpretation by patients on the exact definition of MMS or that a higher than expected number of procedures were performed by non-ACMS Mohs surgeons.
Our qualitative analysis revealed that patients most frequently commented on the interpersonal skills of their surgeons (eg, bedside manner, communication) as positive themes during MMS, similar to prior analyses of general dermatology practices.3 In comparison to a recent study assessing patient satisfaction with rhinoplasty on RealSelf, the final appearance of the nose represented the most common positive- and negative-cited theme.8 Mohs micrographic surgery procedures typically are done under local anesthesia, which may explain the greater importance of bedside manner and communication intraoperatively in comparison to final surgical outcomes for patient satisfaction. For negative themes, 3 of 4 most common concerns were directly related to the intraoperative and postoperative periods. Providers may be able to improve patient satisfaction by explaining the postoperative course, such as healing time and temporary physical restrictions, as well as possible sequelae in greater detail, which may be particularly pertinent for MMS involving the nose or near the eyes.
The global ratings for MMS are high, as shown in our data set of patient reviews; however, patient reviews are highly susceptible to reporting bias, recall bias, and missing information. Prior work using this online patient review website to investigate laser and light procedures also demonstrated the risk for imperfect information associated with patient reviews.9 Even so, the data does provide a glimpse into what is considered important to patients. Surgeon interpersonal skills and communication were the most frequently cited positive themes for MMS. The best surgical aspects of MMS focused on the unique tissue-sparing nature of the procedure and the removal of a cancerous lesion. Potential areas for improvement include a more thorough explanation of the intraoperative and postoperative process, specifically potential asymmetry related to the nose or the eyes, healing time, and scarring. These patient reviews underscore the importance of setting appropriate patient expectations. As patients become more connected and utilize online platforms to report their experiences, Mohs surgeons can take insights derived from online patient reviews for their own practice or geographic area to improve satisfaction and manage expectations.
- Alam M, Ibrahim O, Nodzenski M, et al. Adverse events associated with Mohs micrographic surgery: multicenter prospective cohort study of 20,821 cases at 23 centers. JAMA Dermatol. 2013;149:1378-1385.
- Fox S. The social life of health information. Pew Research Center website. http://www.pewresearch.org/fact-tank/2014/01/15/the-social-life-of-health-information/. Published January 15, 2014. Accessed February 11, 2017.
- Smith RJ, Lipoff JB. Evaluation of dermatology practice online reviews: lessons from qualitative analysis. JAMA Dermatol. 2016;152:153-157.
- Schlichte MJ, Karimkhani C, Jones T, et al. Patient use of social media to evaluate cosmetic treatments and procedures. Dermatol Online J. 2015;21. pii:13030/qt88z6r65x.
- American Academy of Dermatology; American College of Mohs Surgery; American Society for Dermatologic Surgery Association; American Society for Mohs Surgery; Ad Hoc Task Force, Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery [published online September 7, 2012]. Dermatol Surg. 2012;38:1582-1603.
- Asgari MM, Bertenthal D, Sen S, et al. Patient satisfaction after treatment of nonmelanoma skin cancer. Derm Surg. 2009;35:1041-1049.
- Campbell RM, Perlis CS, Malik MK, et al. Characteristics of Mohs practices in the United States: a recall survey of ACMS surgeons. Dermatol Surg. 2007;33:1413-1418; discussion, 1418.
- Khansa I, Khansa L, Pearson GD. Patient satisfaction after rhinoplasty: a social media analysis. Aesthet Surg J. 2016;36:NP1-5.
- Xu S, Walter J, Bhatia A. Patient-reported online satisfaction for laser and light procedures: need for caution. Dermatol Surg. 2017;43:154-158.
- Alam M, Ibrahim O, Nodzenski M, et al. Adverse events associated with Mohs micrographic surgery: multicenter prospective cohort study of 20,821 cases at 23 centers. JAMA Dermatol. 2013;149:1378-1385.
- Fox S. The social life of health information. Pew Research Center website. http://www.pewresearch.org/fact-tank/2014/01/15/the-social-life-of-health-information/. Published January 15, 2014. Accessed February 11, 2017.
- Smith RJ, Lipoff JB. Evaluation of dermatology practice online reviews: lessons from qualitative analysis. JAMA Dermatol. 2016;152:153-157.
- Schlichte MJ, Karimkhani C, Jones T, et al. Patient use of social media to evaluate cosmetic treatments and procedures. Dermatol Online J. 2015;21. pii:13030/qt88z6r65x.
- American Academy of Dermatology; American College of Mohs Surgery; American Society for Dermatologic Surgery Association; American Society for Mohs Surgery; Ad Hoc Task Force, Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery [published online September 7, 2012]. Dermatol Surg. 2012;38:1582-1603.
- Asgari MM, Bertenthal D, Sen S, et al. Patient satisfaction after treatment of nonmelanoma skin cancer. Derm Surg. 2009;35:1041-1049.
- Campbell RM, Perlis CS, Malik MK, et al. Characteristics of Mohs practices in the United States: a recall survey of ACMS surgeons. Dermatol Surg. 2007;33:1413-1418; discussion, 1418.
- Khansa I, Khansa L, Pearson GD. Patient satisfaction after rhinoplasty: a social media analysis. Aesthet Surg J. 2016;36:NP1-5.
- Xu S, Walter J, Bhatia A. Patient-reported online satisfaction for laser and light procedures: need for caution. Dermatol Surg. 2017;43:154-158.
Resident Pearl
Patients are posting reviews online now more than ever regarding their experiences with dermatologic surgical procedures. Mohs micrographic surgery is rated highly by patients but suspect to missing information and a higher than expected attribution of the procedure to plastic surgeons.