User login
A 30-year-old G1P0 woman presents to your office for routine obstetric care at 18 weeks’ gestation. Her pregnancy has been uncomplicated, but her prenatal lab evaluation is notable for blood type A-negative. She wants to know if she really needs the anti-D immune globulin injection.
Rhesus (Rh)D-negative women carrying an RhD-positive fetus are at risk for anti-D antibodies, placing the fetus at risk for hemolytic disease of the fetus and newborn (HDFN). If undiagnosed and/or untreated, HDFN carries significant risk for perinatal morbidity and mortality.2
With routine postnatal anti-D immunoglobulin prophylaxis of RhD-negative women who delivered an RhD-positive child (which began around 1970), the risk for maternal alloimmunization was reduced from 16% to 1.12%-1.3%.3-5 The risk was further reduced to approximately 0.28% with the addition of consistent prophylaxis at 28 weeks’ gestation.4 As a result, the current standard of care is to administer anti-D immunoglobulin at 28 weeks’ gestation, within 72 hours of delivery of an RhD-positive fetus, and after events with risk for fetal-to-maternal transfusion (eg, spontaneous, threatened, or induced abortion; invasive prenatal diagnostic procedures such as amniocentesis; blunt abdominal trauma; external cephalic version; second or third trimester antepartum bleeding).6
The problem of unnecessary Tx. However, under this current practice, many RhD-negative women are receiving anti-D immunoglobulin unnecessarily. This is because the fetus’s RhD status is not routinely known during the prenatal period.
Enter cell-free DNA testing. Cell-free DNA testing analyzes fragments of fetal DNA found in maternal blood. The use of cell-free DNA testing at 10 to 13 weeks’ gestation to screen for fetal chromosomal abnormalities is reliable (91%-99% sensitivity for trisomies 21, 18, and 137) and becoming increasingly more common.
A notable meta-analysis. A 2017 meta-analysis of 30 studies of cell-free DNA testing of RhD status in the first and second trimesters calculated a sensitivity of 99.3% and a specificity of 98.4%.7 Denmark, the Netherlands, Sweden, France, and Finland are using this method routinely. As of this writing, the American College of Obstetricians and Gynecologists (ACOG) has not recommended the use of cell-free DNA RhD testing in the United States, but they do note that as the cost of the assay declines, this method may become preferred.8 The National Institute for Health and Care Excellence in England recommends its use as long as its cost remains below a set threshold.9
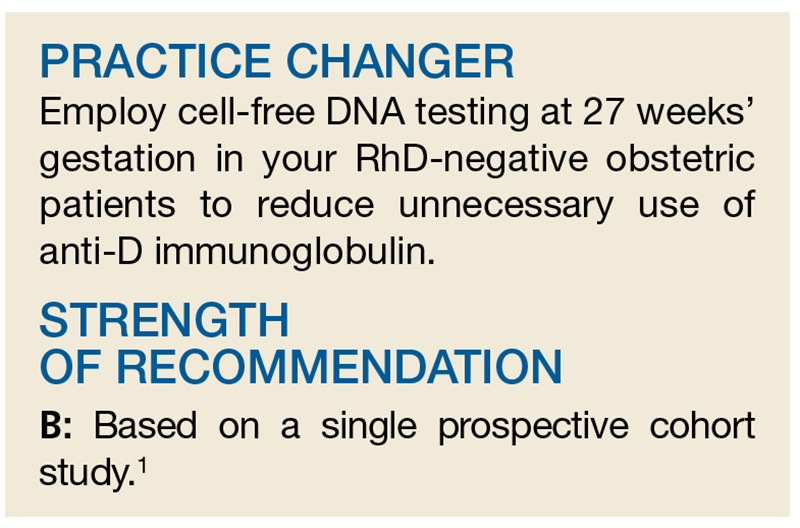
This study evaluated the accuracy of using cell-free DNA testing at 27 weeks’ gestation to determine fetal RhD status compared with serologic typing of cord blood at delivery.
Continue to: STUDY SUMMARY
STUDY SUMMARY
Test gets high marks in Netherlands trial
This large observational cohort trial from the Netherlands examined the accuracy of identifying RhD-positive fetuses using cell-free DNA isolates in maternal plasma. Over the 15-month study period, fetal RhD testing was conducted during Week 27 of gestation, and results were compared with those obtained using neonatal cord blood at birth. If the fetal RhD test was positive, providers administered 200 µg anti-D immunoglobulin during the 30th week of gestation and within 48 hours of birth. If fetal RhD was negative, providers were told immunoglobulin was unnecessary.
More than 32,000 RhD-negative women were screened. The cell-free DNA test showed fetal RhD-positive results 62% of the time and RhD-negative results in the remainder. Cord blood samples were available for 25,789 pregnancies (80%).
Sensitivity, specificity. The sensitivity for identifying fetal RhD was 99% and the specificity was 98%. Both negative and positive predictive values were 99%. Overall, there were 225 false-positive results and nine false-negative results. In the nine false negatives, six were due to a lack of fetal DNA in the sample and three were due to technical error (defined as an operator ignoring a failure of the robot pipetting the plasma or other technical failures).
The false-negative rate (0.03%) was lower than the predetermined estimated false-negative rate of cord blood serology (0.25%). In 22 of the supposed false positives, follow-up serology or molecular testing found an RhD gene was actually present, meaning the results of the neonatal cord blood serology in these cases were falsely negative. If you recalculate with these data in mind, the false-negative rate for fetal DNA testing was actually less than half that of typical serologic determination.
Continue to: WHAT'S NEW
WHAT’S NEW
Accurate test, potential to reduce unnecessary Tx
Fetal RhD testing at 27 weeks’ gestation appears to be highly accurate and could reduce the unnecessary use of anti-D immunoglobulin when the fetal RhD is negative.
CAVEATS
Different results by ethnicity?
Dutch participants are not necessarily reflective of the US population. Known variation in the rate of fetal RhD positivity among RhD-negative pregnant women by race and ethnicity could mean that the number of women able to forego anti-D immunoglobulin prophylaxis would be different in the United States than in other countries.
Also, in this study, polymerase chain reaction for two RhD sequences was run in triplicate, and a computer-based algorithm was used to automatically score samples to provide results. For safe implementation, the cell-free fetal RhD DNA testing process would need to follow similar methods.
CHALLENGES TO IMPLEMENTATION
Cost and availability are big unknowns
Cost and availability of the test may be barriers, but there is currently too little information on either subject in the United States to make a determination. A 2013 study indicated that the use of cell-free DNA testing to determine fetal RhD status was then approximately $682.10
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Copyright © 2018. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2018;67[5]: 306, 308, 319).
1. de Haas M, Thurik FF, van der Ploeg CP, et al. Sensitivity of fetal RHD screening for safe guidance of targeted anti-D immunoglobulin prophylaxis: prospective cohort study of a nationwide programme in the Netherlands. BMJ. 2016;355:i5789.
2. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 75: Management of alloimmunization during pregnancy. Obstet Gynecol. 2006; 108:457-464.
3. Urbaniak SJ, Greiss MA. RhD haemolytic disease of the fetus and the newborn. Blood Rev. 2000;14(1):44-61.
4. Mayne S, Parker JH, Harden TA, et al. Rate of RhD sensitisation before and after implementation of a community based antenatal prophylaxis programme. BMJ. 1997;315(7122):1588.
5. MacKenzie IZ, Bowell P, Gregory H, et al. Routine antenatal Rhesus D immunoglobulin prophylaxis: the results of a prospective 10 year study. Br J Obstet Gynecol. 1999;106:492-497.
6. Zolotor AJ, Carlough MC. Update on prenatal care. Am Fam Physician. 2014;89(3):199-208.
7. Mackie FL, Hemming K, Allen S, et al. The accuracy of cell-free fetal DNA-based non-invasive prenatal testing in singleton pregnancies: a systematic review and bivariate meta-analysis. BJOG. 2017;124(1):32-46.
8. American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 181: Prevention of Rh D Alloimmunization. Obstet Gynecol. 2017;130:e57-e70.
9. National Institute for Health and Care Excellence. High-throughput non-invasive prenatal testing for fetal RHD genotype 1: Recommendations. www.nice.org.uk/guidance/dg25/chapter/1-Recommendations. Accessed May 7, 2018.
10. Hawk AF, Chang EY, Shields SM, Simpson KN. Costs and clinical outcomes of noninvasive fetal RhD typing for targeted prophylaxis. Obstet Gynecol. 2013;122(3):579-585.
A 30-year-old G1P0 woman presents to your office for routine obstetric care at 18 weeks’ gestation. Her pregnancy has been uncomplicated, but her prenatal lab evaluation is notable for blood type A-negative. She wants to know if she really needs the anti-D immune globulin injection.
Rhesus (Rh)D-negative women carrying an RhD-positive fetus are at risk for anti-D antibodies, placing the fetus at risk for hemolytic disease of the fetus and newborn (HDFN). If undiagnosed and/or untreated, HDFN carries significant risk for perinatal morbidity and mortality.2
With routine postnatal anti-D immunoglobulin prophylaxis of RhD-negative women who delivered an RhD-positive child (which began around 1970), the risk for maternal alloimmunization was reduced from 16% to 1.12%-1.3%.3-5 The risk was further reduced to approximately 0.28% with the addition of consistent prophylaxis at 28 weeks’ gestation.4 As a result, the current standard of care is to administer anti-D immunoglobulin at 28 weeks’ gestation, within 72 hours of delivery of an RhD-positive fetus, and after events with risk for fetal-to-maternal transfusion (eg, spontaneous, threatened, or induced abortion; invasive prenatal diagnostic procedures such as amniocentesis; blunt abdominal trauma; external cephalic version; second or third trimester antepartum bleeding).6
The problem of unnecessary Tx. However, under this current practice, many RhD-negative women are receiving anti-D immunoglobulin unnecessarily. This is because the fetus’s RhD status is not routinely known during the prenatal period.
Enter cell-free DNA testing. Cell-free DNA testing analyzes fragments of fetal DNA found in maternal blood. The use of cell-free DNA testing at 10 to 13 weeks’ gestation to screen for fetal chromosomal abnormalities is reliable (91%-99% sensitivity for trisomies 21, 18, and 137) and becoming increasingly more common.
A notable meta-analysis. A 2017 meta-analysis of 30 studies of cell-free DNA testing of RhD status in the first and second trimesters calculated a sensitivity of 99.3% and a specificity of 98.4%.7 Denmark, the Netherlands, Sweden, France, and Finland are using this method routinely. As of this writing, the American College of Obstetricians and Gynecologists (ACOG) has not recommended the use of cell-free DNA RhD testing in the United States, but they do note that as the cost of the assay declines, this method may become preferred.8 The National Institute for Health and Care Excellence in England recommends its use as long as its cost remains below a set threshold.9
This study evaluated the accuracy of using cell-free DNA testing at 27 weeks’ gestation to determine fetal RhD status compared with serologic typing of cord blood at delivery.
Continue to: STUDY SUMMARY
STUDY SUMMARY
Test gets high marks in Netherlands trial
This large observational cohort trial from the Netherlands examined the accuracy of identifying RhD-positive fetuses using cell-free DNA isolates in maternal plasma. Over the 15-month study period, fetal RhD testing was conducted during Week 27 of gestation, and results were compared with those obtained using neonatal cord blood at birth. If the fetal RhD test was positive, providers administered 200 µg anti-D immunoglobulin during the 30th week of gestation and within 48 hours of birth. If fetal RhD was negative, providers were told immunoglobulin was unnecessary.
More than 32,000 RhD-negative women were screened. The cell-free DNA test showed fetal RhD-positive results 62% of the time and RhD-negative results in the remainder. Cord blood samples were available for 25,789 pregnancies (80%).
Sensitivity, specificity. The sensitivity for identifying fetal RhD was 99% and the specificity was 98%. Both negative and positive predictive values were 99%. Overall, there were 225 false-positive results and nine false-negative results. In the nine false negatives, six were due to a lack of fetal DNA in the sample and three were due to technical error (defined as an operator ignoring a failure of the robot pipetting the plasma or other technical failures).
The false-negative rate (0.03%) was lower than the predetermined estimated false-negative rate of cord blood serology (0.25%). In 22 of the supposed false positives, follow-up serology or molecular testing found an RhD gene was actually present, meaning the results of the neonatal cord blood serology in these cases were falsely negative. If you recalculate with these data in mind, the false-negative rate for fetal DNA testing was actually less than half that of typical serologic determination.
Continue to: WHAT'S NEW
WHAT’S NEW
Accurate test, potential to reduce unnecessary Tx
Fetal RhD testing at 27 weeks’ gestation appears to be highly accurate and could reduce the unnecessary use of anti-D immunoglobulin when the fetal RhD is negative.
CAVEATS
Different results by ethnicity?
Dutch participants are not necessarily reflective of the US population. Known variation in the rate of fetal RhD positivity among RhD-negative pregnant women by race and ethnicity could mean that the number of women able to forego anti-D immunoglobulin prophylaxis would be different in the United States than in other countries.
Also, in this study, polymerase chain reaction for two RhD sequences was run in triplicate, and a computer-based algorithm was used to automatically score samples to provide results. For safe implementation, the cell-free fetal RhD DNA testing process would need to follow similar methods.
CHALLENGES TO IMPLEMENTATION
Cost and availability are big unknowns
Cost and availability of the test may be barriers, but there is currently too little information on either subject in the United States to make a determination. A 2013 study indicated that the use of cell-free DNA testing to determine fetal RhD status was then approximately $682.10
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Copyright © 2018. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2018;67[5]: 306, 308, 319).
A 30-year-old G1P0 woman presents to your office for routine obstetric care at 18 weeks’ gestation. Her pregnancy has been uncomplicated, but her prenatal lab evaluation is notable for blood type A-negative. She wants to know if she really needs the anti-D immune globulin injection.
Rhesus (Rh)D-negative women carrying an RhD-positive fetus are at risk for anti-D antibodies, placing the fetus at risk for hemolytic disease of the fetus and newborn (HDFN). If undiagnosed and/or untreated, HDFN carries significant risk for perinatal morbidity and mortality.2
With routine postnatal anti-D immunoglobulin prophylaxis of RhD-negative women who delivered an RhD-positive child (which began around 1970), the risk for maternal alloimmunization was reduced from 16% to 1.12%-1.3%.3-5 The risk was further reduced to approximately 0.28% with the addition of consistent prophylaxis at 28 weeks’ gestation.4 As a result, the current standard of care is to administer anti-D immunoglobulin at 28 weeks’ gestation, within 72 hours of delivery of an RhD-positive fetus, and after events with risk for fetal-to-maternal transfusion (eg, spontaneous, threatened, or induced abortion; invasive prenatal diagnostic procedures such as amniocentesis; blunt abdominal trauma; external cephalic version; second or third trimester antepartum bleeding).6
The problem of unnecessary Tx. However, under this current practice, many RhD-negative women are receiving anti-D immunoglobulin unnecessarily. This is because the fetus’s RhD status is not routinely known during the prenatal period.
Enter cell-free DNA testing. Cell-free DNA testing analyzes fragments of fetal DNA found in maternal blood. The use of cell-free DNA testing at 10 to 13 weeks’ gestation to screen for fetal chromosomal abnormalities is reliable (91%-99% sensitivity for trisomies 21, 18, and 137) and becoming increasingly more common.
A notable meta-analysis. A 2017 meta-analysis of 30 studies of cell-free DNA testing of RhD status in the first and second trimesters calculated a sensitivity of 99.3% and a specificity of 98.4%.7 Denmark, the Netherlands, Sweden, France, and Finland are using this method routinely. As of this writing, the American College of Obstetricians and Gynecologists (ACOG) has not recommended the use of cell-free DNA RhD testing in the United States, but they do note that as the cost of the assay declines, this method may become preferred.8 The National Institute for Health and Care Excellence in England recommends its use as long as its cost remains below a set threshold.9
This study evaluated the accuracy of using cell-free DNA testing at 27 weeks’ gestation to determine fetal RhD status compared with serologic typing of cord blood at delivery.
Continue to: STUDY SUMMARY
STUDY SUMMARY
Test gets high marks in Netherlands trial
This large observational cohort trial from the Netherlands examined the accuracy of identifying RhD-positive fetuses using cell-free DNA isolates in maternal plasma. Over the 15-month study period, fetal RhD testing was conducted during Week 27 of gestation, and results were compared with those obtained using neonatal cord blood at birth. If the fetal RhD test was positive, providers administered 200 µg anti-D immunoglobulin during the 30th week of gestation and within 48 hours of birth. If fetal RhD was negative, providers were told immunoglobulin was unnecessary.
More than 32,000 RhD-negative women were screened. The cell-free DNA test showed fetal RhD-positive results 62% of the time and RhD-negative results in the remainder. Cord blood samples were available for 25,789 pregnancies (80%).
Sensitivity, specificity. The sensitivity for identifying fetal RhD was 99% and the specificity was 98%. Both negative and positive predictive values were 99%. Overall, there were 225 false-positive results and nine false-negative results. In the nine false negatives, six were due to a lack of fetal DNA in the sample and three were due to technical error (defined as an operator ignoring a failure of the robot pipetting the plasma or other technical failures).
The false-negative rate (0.03%) was lower than the predetermined estimated false-negative rate of cord blood serology (0.25%). In 22 of the supposed false positives, follow-up serology or molecular testing found an RhD gene was actually present, meaning the results of the neonatal cord blood serology in these cases were falsely negative. If you recalculate with these data in mind, the false-negative rate for fetal DNA testing was actually less than half that of typical serologic determination.
Continue to: WHAT'S NEW
WHAT’S NEW
Accurate test, potential to reduce unnecessary Tx
Fetal RhD testing at 27 weeks’ gestation appears to be highly accurate and could reduce the unnecessary use of anti-D immunoglobulin when the fetal RhD is negative.
CAVEATS
Different results by ethnicity?
Dutch participants are not necessarily reflective of the US population. Known variation in the rate of fetal RhD positivity among RhD-negative pregnant women by race and ethnicity could mean that the number of women able to forego anti-D immunoglobulin prophylaxis would be different in the United States than in other countries.
Also, in this study, polymerase chain reaction for two RhD sequences was run in triplicate, and a computer-based algorithm was used to automatically score samples to provide results. For safe implementation, the cell-free fetal RhD DNA testing process would need to follow similar methods.
CHALLENGES TO IMPLEMENTATION
Cost and availability are big unknowns
Cost and availability of the test may be barriers, but there is currently too little information on either subject in the United States to make a determination. A 2013 study indicated that the use of cell-free DNA testing to determine fetal RhD status was then approximately $682.10
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Copyright © 2018. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2018;67[5]: 306, 308, 319).
1. de Haas M, Thurik FF, van der Ploeg CP, et al. Sensitivity of fetal RHD screening for safe guidance of targeted anti-D immunoglobulin prophylaxis: prospective cohort study of a nationwide programme in the Netherlands. BMJ. 2016;355:i5789.
2. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 75: Management of alloimmunization during pregnancy. Obstet Gynecol. 2006; 108:457-464.
3. Urbaniak SJ, Greiss MA. RhD haemolytic disease of the fetus and the newborn. Blood Rev. 2000;14(1):44-61.
4. Mayne S, Parker JH, Harden TA, et al. Rate of RhD sensitisation before and after implementation of a community based antenatal prophylaxis programme. BMJ. 1997;315(7122):1588.
5. MacKenzie IZ, Bowell P, Gregory H, et al. Routine antenatal Rhesus D immunoglobulin prophylaxis: the results of a prospective 10 year study. Br J Obstet Gynecol. 1999;106:492-497.
6. Zolotor AJ, Carlough MC. Update on prenatal care. Am Fam Physician. 2014;89(3):199-208.
7. Mackie FL, Hemming K, Allen S, et al. The accuracy of cell-free fetal DNA-based non-invasive prenatal testing in singleton pregnancies: a systematic review and bivariate meta-analysis. BJOG. 2017;124(1):32-46.
8. American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 181: Prevention of Rh D Alloimmunization. Obstet Gynecol. 2017;130:e57-e70.
9. National Institute for Health and Care Excellence. High-throughput non-invasive prenatal testing for fetal RHD genotype 1: Recommendations. www.nice.org.uk/guidance/dg25/chapter/1-Recommendations. Accessed May 7, 2018.
10. Hawk AF, Chang EY, Shields SM, Simpson KN. Costs and clinical outcomes of noninvasive fetal RhD typing for targeted prophylaxis. Obstet Gynecol. 2013;122(3):579-585.
1. de Haas M, Thurik FF, van der Ploeg CP, et al. Sensitivity of fetal RHD screening for safe guidance of targeted anti-D immunoglobulin prophylaxis: prospective cohort study of a nationwide programme in the Netherlands. BMJ. 2016;355:i5789.
2. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 75: Management of alloimmunization during pregnancy. Obstet Gynecol. 2006; 108:457-464.
3. Urbaniak SJ, Greiss MA. RhD haemolytic disease of the fetus and the newborn. Blood Rev. 2000;14(1):44-61.
4. Mayne S, Parker JH, Harden TA, et al. Rate of RhD sensitisation before and after implementation of a community based antenatal prophylaxis programme. BMJ. 1997;315(7122):1588.
5. MacKenzie IZ, Bowell P, Gregory H, et al. Routine antenatal Rhesus D immunoglobulin prophylaxis: the results of a prospective 10 year study. Br J Obstet Gynecol. 1999;106:492-497.
6. Zolotor AJ, Carlough MC. Update on prenatal care. Am Fam Physician. 2014;89(3):199-208.
7. Mackie FL, Hemming K, Allen S, et al. The accuracy of cell-free fetal DNA-based non-invasive prenatal testing in singleton pregnancies: a systematic review and bivariate meta-analysis. BJOG. 2017;124(1):32-46.
8. American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 181: Prevention of Rh D Alloimmunization. Obstet Gynecol. 2017;130:e57-e70.
9. National Institute for Health and Care Excellence. High-throughput non-invasive prenatal testing for fetal RHD genotype 1: Recommendations. www.nice.org.uk/guidance/dg25/chapter/1-Recommendations. Accessed May 7, 2018.
10. Hawk AF, Chang EY, Shields SM, Simpson KN. Costs and clinical outcomes of noninvasive fetal RhD typing for targeted prophylaxis. Obstet Gynecol. 2013;122(3):579-585.