User login
LAS VEGAS – Morcellation during laparoscopic hysterectomy or myomectomy for presumed large fibroids provides slightly better 5-year overall survival and higher quality of life scores than abdominal hysterectomy, according to a new study.
The strength of this soon-to-be-published decision analysis lies in its balance and comprehensive nature. It utilized the best-available published literature to estimate the mortality risk stemming from tissue dissemination of occult leiomyosarcoma through power morcellation – an issue of hot controversy – but it also incorporated the increased risks of procedure-related morbidity and mortality associated with the alternative to morcellation in patients with large fibroids: that is, abdominal hysterectomy, Dr. Matthew Siedhoff explained at the annual Minimally Invasive Surgery Week.
The decision analysis was undertaken in the wake of the Food and Drug Administration’s April 2014 safety warning citing a 1 in 350 risk of occult malignancy in women undergoing hysterectomies or myomectomies for removal of presumed fibroids and that laparoscopic surgeries involving power morcellation performed in women with unsuspected uterine sarcomas may spread cancerous tissue, potentially shortening survival. The attendant publicity has caused considerable alarm and confusion among patients and the general public. The FDA is currently deliberating possible actions ranging from a black box warning to outright banning of power morcellation.
Meanwhile, several prominent medical centers, including Brigham and Women’s Hospital, Massachusetts General Hospital, both in Boston, and the Cleveland Clinic, have banned the use of power morcellation – precipitously, in Dr. Siedhoff’s view.
Also since the FDA safety statement, Johnson & Johnson has taken its power morcellator off the market and several large insurance companies have announced plans to halt reimbursement when power morcellation is used in gynecologic surgery. However, exactly how that would happen is unclear because there is no billing code associated with power morcellation, and it would be arduous for insurers to actually read through all operative reports.
“This decision analysis is a tool for surgeons and patients to help make informed decisions. It balances the FDA analysis, which pretty much just emphasizes morcellation risk to the exclusion of all the known benefits of laparoscopy. The analysis argues that reducing the risk associated with morcellation – perhaps through the use of specimen containment or preoperative leiomyosarcoma diagnosis – is a better approach than abandoning minimally invasive gynecologic surgery for fibroids. That would be throwing the baby out with the bathwater,” declared Dr. Siedhoff, an ob.gyn. and director of the division of advanced laparoscopy and pelvic pain at the University of North Carolina, Chapel Hill.
A decision analysis entails probability modeling of outcomes based upon consensus event rates obtained from studies in the published literature.
“It’s helpful to do a decision analysis when you can’t do a randomized controlled trial, which you certainly can’t for this issue,” he observed at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
The decision analysis was carried out by Dr. Siedhoff and coinvestigators at the University of North Carolina at Chapel Hill, with department of obstetrics and gynecology chair Dr. Daniel Clarke-Peterson as senior author. The researchers assumed two hypothetical cohorts of 100,000 women undergoing hysterectomy for fibroids large enough that surgical options were limited to laparoscopic hysterectomy with morcellation or abdominal hysterectomy. The primary outcomes were 5-year overall mortality and quality of life as measured in quality-adjusted life-years (QALYs).
The analysis assumed that among the 100,000 women in each group there would be 120 FIGO Stage I or II occult leiomyosarcomas, with an associated 59% 5-year mortality from cancer. It was further assumed that intraperitoneal dissemination of tumor via morcellation would in effect boost those cancers to FIGO Stage III, with 72% mortality at 5 years. This would result in 86 deaths from leiomyosarcoma over 5 years in the morcellation group, compared with 71 in women who underwent abdominal hysterectomy. However, this was counterbalanced by more hysterectomy-related deaths in the abdominal hysterectomy group: 32, compared with 12 in women undergoing morcellation. The final 5-year tally: 98 deaths overall in the morcellation group and 103 in the abdominal hysterectomy group.
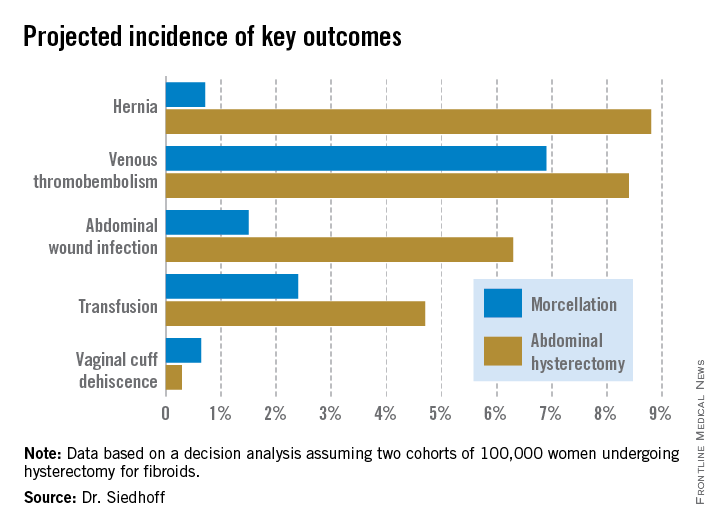
QALYs are calculated by estimating how much a given adverse event – for example, venous thromboembolism, along with its attendant treatment and potential further complications – would diminish a theoretical year of otherwise perfect health. The total QALYs in the group of 100,000 women undergoing morcellation was estimated at 499,171, compared with 490,711 over 5 years in the abdominal hysterectomy group. That’s because with the exception of vaginal cuff dehiscence, all of the other complications assessed in the decision analysis, including wound infections, transfusions, hernias, and venous thromboembolisms, were more frequent in the abdominal hysterectomy group. The forthcoming final publication will include the citations on which all of the event probabilities were based.
An alternative and perhaps more readily grasped way of expressing the QALY results is that patients undergoing laparoscopic hysterectomy enjoyed an additional 0.85 QALY, or roughly 1 extra month of life in perfect health over a 5-year time period, Dr. Siedhoff explained.
The decision analysis didn’t include the well-established facts that laparoscopic hysterectomy entails less postoperative pain, a shorter average hospital length of stay, and faster return to daily activities.
Dr. Siedhoff was quick to assert that the true incidence of occult leiomyosarcoma in women undergoing surgery for presumed fibroids is unknown. An American College of Obstetricians and Gynecologist’s position statement issued earlier this year quoted an estimate of 1 in 500. The FDA cited a figure of 1 in 350. But when the North Carolina researchers examined the 10 studies published during 1990-2013, upon which the FDA based its estimate, the investigators felt compelled to reject 6 of them because of poor quality. For example, several studies included morcellation in patients with preoperative known or suspected sarcoma, even though morcellation should absolutely never be done in that situation. Based upon a weighted analysis of the remaining four highest-quality studies, the investigators came up with an estimate of 12 cases/10,000 women.
Noting that the largest of the studies in the FDA analysis included just 1,584 women with 2 cases of leiomyosarcoma, Dr. Siedhoff said, “I think it’s important to point out that really important decisions are being made on awfully small numerators and denominators. The truth of the matter is we have no idea what the true number is. It could be twice as high as our estimate or half as low.”
He admitted that he has been personally affected by the rancorous tone of recent public debate regarding morcellation safety, in which the procedure’s defenders often are demonized.
“It’s been confusing to me why in the Wall Street Journal they talk about these evil doctors who want to use this technique, as if it somehow benefits us. It’s not easier to do laparoscopic surgery, and it’s certainly not easier to morcellate tissue. The only reason that we’re talking about this is because we care about the outcomes for our patients,” the gynecologic surgeon said at the meeting presented by the Society of Laparoendoscopic Surgeons and affiliated societies. “One of the things that has been most difficult about all this,” he continued, “is the way that the information has moved from some very vocal people who feel strongly about this issue to the level of the lay person that you see in the elevator, or worse yet, your own patient. I think it’s almost like a game of telephone, so that by the time it gets down to a person who’s not a surgeon, the message is ‘morcellation causes cancer.’”Not only is the true prevalence of occult malignancy in women undergoing laparoscopic surgery for removal of fibroids unclear, but the data on the adverse impact of morcellation in this situation is sketchy as well. To date, it consists of two single-center retrospective studies. The more recent report, from Brigham and Women’s Hospital, involved 19 patients who underwent morcellation and 39 who had a total abdominal hysterectomy, all found to have leiomyosarcoma. The cancer recurrence rate was significantly higher in women who had morcellation, by a margin of 74% to 51%. However, there was no significant difference in overall survival (Cancer 2014 [doi:10.1002/cncr.28844]).
In contrast, an earlier Korean study involving a consecutive series comprised of 25 patients with occult leiomyosarcoma who underwent morcellation and 31 with total abdominal hysterectomy found a significant difference in 5-year overall survival: 46% in the morcellation group, and what Dr. Siedhoff deemed an unusually favorable 73% in the total abdominal hysterectomy patients (Gynecol. Oncol. 2011;122:255-9).
There is a great unmet need for a reliable preoperative method to distinguish leiomyosarcomas from benign fibroids. Imaging is of limited value. Endometrial biopsy is rarely positive. No biomarkers have been identified. Clinical factors that increase the likelihood of leiomyosarcoma include rapid growth, African American ethnicity, older age, a history of pelvic radiation, and the presence of the retinoblastoma gene.
In his own practice, Dr. Siedhoff sometimes uses specimen retrieval bags when performing morcellation, but finds the currently available versions to be cumbersome and a challenge to work with. Besides, he noted, there is to date no evidence that they are actually effective in reducing leiomyosarcoma recurrence risk. He was a member of an AAGL task force which in May issued a position statement on morcellation, which noted, “Use of morcellation within specimen retrieval pouches for containment of benign or malignant uterine tissue requires significant skill and experience, and use of specimen retrieval pouches should be further investigated for safety and outcomes in a controlled setting.”
Dr. Siedhoff reported having no financial conflicts regarding the decision analysis, conducted with university funds.
LAS VEGAS – Morcellation during laparoscopic hysterectomy or myomectomy for presumed large fibroids provides slightly better 5-year overall survival and higher quality of life scores than abdominal hysterectomy, according to a new study.
The strength of this soon-to-be-published decision analysis lies in its balance and comprehensive nature. It utilized the best-available published literature to estimate the mortality risk stemming from tissue dissemination of occult leiomyosarcoma through power morcellation – an issue of hot controversy – but it also incorporated the increased risks of procedure-related morbidity and mortality associated with the alternative to morcellation in patients with large fibroids: that is, abdominal hysterectomy, Dr. Matthew Siedhoff explained at the annual Minimally Invasive Surgery Week.
The decision analysis was undertaken in the wake of the Food and Drug Administration’s April 2014 safety warning citing a 1 in 350 risk of occult malignancy in women undergoing hysterectomies or myomectomies for removal of presumed fibroids and that laparoscopic surgeries involving power morcellation performed in women with unsuspected uterine sarcomas may spread cancerous tissue, potentially shortening survival. The attendant publicity has caused considerable alarm and confusion among patients and the general public. The FDA is currently deliberating possible actions ranging from a black box warning to outright banning of power morcellation.
Meanwhile, several prominent medical centers, including Brigham and Women’s Hospital, Massachusetts General Hospital, both in Boston, and the Cleveland Clinic, have banned the use of power morcellation – precipitously, in Dr. Siedhoff’s view.
Also since the FDA safety statement, Johnson & Johnson has taken its power morcellator off the market and several large insurance companies have announced plans to halt reimbursement when power morcellation is used in gynecologic surgery. However, exactly how that would happen is unclear because there is no billing code associated with power morcellation, and it would be arduous for insurers to actually read through all operative reports.
“This decision analysis is a tool for surgeons and patients to help make informed decisions. It balances the FDA analysis, which pretty much just emphasizes morcellation risk to the exclusion of all the known benefits of laparoscopy. The analysis argues that reducing the risk associated with morcellation – perhaps through the use of specimen containment or preoperative leiomyosarcoma diagnosis – is a better approach than abandoning minimally invasive gynecologic surgery for fibroids. That would be throwing the baby out with the bathwater,” declared Dr. Siedhoff, an ob.gyn. and director of the division of advanced laparoscopy and pelvic pain at the University of North Carolina, Chapel Hill.
A decision analysis entails probability modeling of outcomes based upon consensus event rates obtained from studies in the published literature.
“It’s helpful to do a decision analysis when you can’t do a randomized controlled trial, which you certainly can’t for this issue,” he observed at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
The decision analysis was carried out by Dr. Siedhoff and coinvestigators at the University of North Carolina at Chapel Hill, with department of obstetrics and gynecology chair Dr. Daniel Clarke-Peterson as senior author. The researchers assumed two hypothetical cohorts of 100,000 women undergoing hysterectomy for fibroids large enough that surgical options were limited to laparoscopic hysterectomy with morcellation or abdominal hysterectomy. The primary outcomes were 5-year overall mortality and quality of life as measured in quality-adjusted life-years (QALYs).
The analysis assumed that among the 100,000 women in each group there would be 120 FIGO Stage I or II occult leiomyosarcomas, with an associated 59% 5-year mortality from cancer. It was further assumed that intraperitoneal dissemination of tumor via morcellation would in effect boost those cancers to FIGO Stage III, with 72% mortality at 5 years. This would result in 86 deaths from leiomyosarcoma over 5 years in the morcellation group, compared with 71 in women who underwent abdominal hysterectomy. However, this was counterbalanced by more hysterectomy-related deaths in the abdominal hysterectomy group: 32, compared with 12 in women undergoing morcellation. The final 5-year tally: 98 deaths overall in the morcellation group and 103 in the abdominal hysterectomy group.
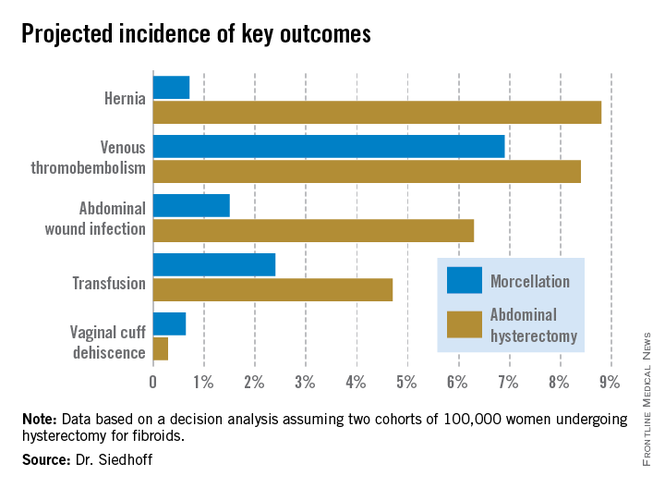
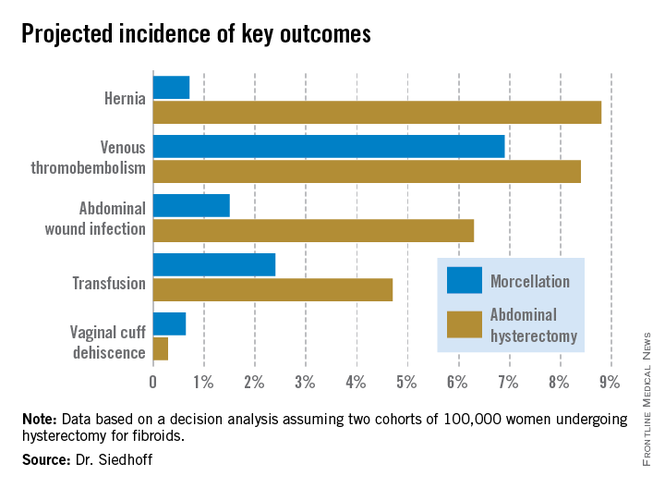
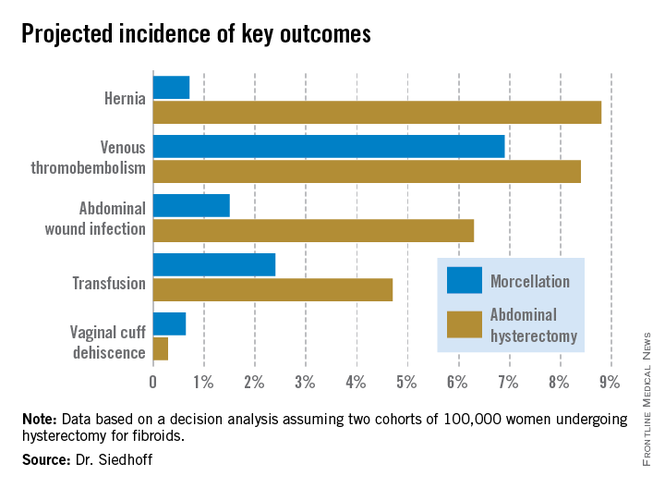
QALYs are calculated by estimating how much a given adverse event – for example, venous thromboembolism, along with its attendant treatment and potential further complications – would diminish a theoretical year of otherwise perfect health. The total QALYs in the group of 100,000 women undergoing morcellation was estimated at 499,171, compared with 490,711 over 5 years in the abdominal hysterectomy group. That’s because with the exception of vaginal cuff dehiscence, all of the other complications assessed in the decision analysis, including wound infections, transfusions, hernias, and venous thromboembolisms, were more frequent in the abdominal hysterectomy group. The forthcoming final publication will include the citations on which all of the event probabilities were based.
An alternative and perhaps more readily grasped way of expressing the QALY results is that patients undergoing laparoscopic hysterectomy enjoyed an additional 0.85 QALY, or roughly 1 extra month of life in perfect health over a 5-year time period, Dr. Siedhoff explained.
The decision analysis didn’t include the well-established facts that laparoscopic hysterectomy entails less postoperative pain, a shorter average hospital length of stay, and faster return to daily activities.
Dr. Siedhoff was quick to assert that the true incidence of occult leiomyosarcoma in women undergoing surgery for presumed fibroids is unknown. An American College of Obstetricians and Gynecologist’s position statement issued earlier this year quoted an estimate of 1 in 500. The FDA cited a figure of 1 in 350. But when the North Carolina researchers examined the 10 studies published during 1990-2013, upon which the FDA based its estimate, the investigators felt compelled to reject 6 of them because of poor quality. For example, several studies included morcellation in patients with preoperative known or suspected sarcoma, even though morcellation should absolutely never be done in that situation. Based upon a weighted analysis of the remaining four highest-quality studies, the investigators came up with an estimate of 12 cases/10,000 women.
Noting that the largest of the studies in the FDA analysis included just 1,584 women with 2 cases of leiomyosarcoma, Dr. Siedhoff said, “I think it’s important to point out that really important decisions are being made on awfully small numerators and denominators. The truth of the matter is we have no idea what the true number is. It could be twice as high as our estimate or half as low.”
He admitted that he has been personally affected by the rancorous tone of recent public debate regarding morcellation safety, in which the procedure’s defenders often are demonized.
“It’s been confusing to me why in the Wall Street Journal they talk about these evil doctors who want to use this technique, as if it somehow benefits us. It’s not easier to do laparoscopic surgery, and it’s certainly not easier to morcellate tissue. The only reason that we’re talking about this is because we care about the outcomes for our patients,” the gynecologic surgeon said at the meeting presented by the Society of Laparoendoscopic Surgeons and affiliated societies. “One of the things that has been most difficult about all this,” he continued, “is the way that the information has moved from some very vocal people who feel strongly about this issue to the level of the lay person that you see in the elevator, or worse yet, your own patient. I think it’s almost like a game of telephone, so that by the time it gets down to a person who’s not a surgeon, the message is ‘morcellation causes cancer.’”Not only is the true prevalence of occult malignancy in women undergoing laparoscopic surgery for removal of fibroids unclear, but the data on the adverse impact of morcellation in this situation is sketchy as well. To date, it consists of two single-center retrospective studies. The more recent report, from Brigham and Women’s Hospital, involved 19 patients who underwent morcellation and 39 who had a total abdominal hysterectomy, all found to have leiomyosarcoma. The cancer recurrence rate was significantly higher in women who had morcellation, by a margin of 74% to 51%. However, there was no significant difference in overall survival (Cancer 2014 [doi:10.1002/cncr.28844]).
In contrast, an earlier Korean study involving a consecutive series comprised of 25 patients with occult leiomyosarcoma who underwent morcellation and 31 with total abdominal hysterectomy found a significant difference in 5-year overall survival: 46% in the morcellation group, and what Dr. Siedhoff deemed an unusually favorable 73% in the total abdominal hysterectomy patients (Gynecol. Oncol. 2011;122:255-9).
There is a great unmet need for a reliable preoperative method to distinguish leiomyosarcomas from benign fibroids. Imaging is of limited value. Endometrial biopsy is rarely positive. No biomarkers have been identified. Clinical factors that increase the likelihood of leiomyosarcoma include rapid growth, African American ethnicity, older age, a history of pelvic radiation, and the presence of the retinoblastoma gene.
In his own practice, Dr. Siedhoff sometimes uses specimen retrieval bags when performing morcellation, but finds the currently available versions to be cumbersome and a challenge to work with. Besides, he noted, there is to date no evidence that they are actually effective in reducing leiomyosarcoma recurrence risk. He was a member of an AAGL task force which in May issued a position statement on morcellation, which noted, “Use of morcellation within specimen retrieval pouches for containment of benign or malignant uterine tissue requires significant skill and experience, and use of specimen retrieval pouches should be further investigated for safety and outcomes in a controlled setting.”
Dr. Siedhoff reported having no financial conflicts regarding the decision analysis, conducted with university funds.
LAS VEGAS – Morcellation during laparoscopic hysterectomy or myomectomy for presumed large fibroids provides slightly better 5-year overall survival and higher quality of life scores than abdominal hysterectomy, according to a new study.
The strength of this soon-to-be-published decision analysis lies in its balance and comprehensive nature. It utilized the best-available published literature to estimate the mortality risk stemming from tissue dissemination of occult leiomyosarcoma through power morcellation – an issue of hot controversy – but it also incorporated the increased risks of procedure-related morbidity and mortality associated with the alternative to morcellation in patients with large fibroids: that is, abdominal hysterectomy, Dr. Matthew Siedhoff explained at the annual Minimally Invasive Surgery Week.
The decision analysis was undertaken in the wake of the Food and Drug Administration’s April 2014 safety warning citing a 1 in 350 risk of occult malignancy in women undergoing hysterectomies or myomectomies for removal of presumed fibroids and that laparoscopic surgeries involving power morcellation performed in women with unsuspected uterine sarcomas may spread cancerous tissue, potentially shortening survival. The attendant publicity has caused considerable alarm and confusion among patients and the general public. The FDA is currently deliberating possible actions ranging from a black box warning to outright banning of power morcellation.
Meanwhile, several prominent medical centers, including Brigham and Women’s Hospital, Massachusetts General Hospital, both in Boston, and the Cleveland Clinic, have banned the use of power morcellation – precipitously, in Dr. Siedhoff’s view.
Also since the FDA safety statement, Johnson & Johnson has taken its power morcellator off the market and several large insurance companies have announced plans to halt reimbursement when power morcellation is used in gynecologic surgery. However, exactly how that would happen is unclear because there is no billing code associated with power morcellation, and it would be arduous for insurers to actually read through all operative reports.
“This decision analysis is a tool for surgeons and patients to help make informed decisions. It balances the FDA analysis, which pretty much just emphasizes morcellation risk to the exclusion of all the known benefits of laparoscopy. The analysis argues that reducing the risk associated with morcellation – perhaps through the use of specimen containment or preoperative leiomyosarcoma diagnosis – is a better approach than abandoning minimally invasive gynecologic surgery for fibroids. That would be throwing the baby out with the bathwater,” declared Dr. Siedhoff, an ob.gyn. and director of the division of advanced laparoscopy and pelvic pain at the University of North Carolina, Chapel Hill.
A decision analysis entails probability modeling of outcomes based upon consensus event rates obtained from studies in the published literature.
“It’s helpful to do a decision analysis when you can’t do a randomized controlled trial, which you certainly can’t for this issue,” he observed at the meeting presented by the Society of Laparoscopic Surgeons and affiliated societies.
The decision analysis was carried out by Dr. Siedhoff and coinvestigators at the University of North Carolina at Chapel Hill, with department of obstetrics and gynecology chair Dr. Daniel Clarke-Peterson as senior author. The researchers assumed two hypothetical cohorts of 100,000 women undergoing hysterectomy for fibroids large enough that surgical options were limited to laparoscopic hysterectomy with morcellation or abdominal hysterectomy. The primary outcomes were 5-year overall mortality and quality of life as measured in quality-adjusted life-years (QALYs).
The analysis assumed that among the 100,000 women in each group there would be 120 FIGO Stage I or II occult leiomyosarcomas, with an associated 59% 5-year mortality from cancer. It was further assumed that intraperitoneal dissemination of tumor via morcellation would in effect boost those cancers to FIGO Stage III, with 72% mortality at 5 years. This would result in 86 deaths from leiomyosarcoma over 5 years in the morcellation group, compared with 71 in women who underwent abdominal hysterectomy. However, this was counterbalanced by more hysterectomy-related deaths in the abdominal hysterectomy group: 32, compared with 12 in women undergoing morcellation. The final 5-year tally: 98 deaths overall in the morcellation group and 103 in the abdominal hysterectomy group.
QALYs are calculated by estimating how much a given adverse event – for example, venous thromboembolism, along with its attendant treatment and potential further complications – would diminish a theoretical year of otherwise perfect health. The total QALYs in the group of 100,000 women undergoing morcellation was estimated at 499,171, compared with 490,711 over 5 years in the abdominal hysterectomy group. That’s because with the exception of vaginal cuff dehiscence, all of the other complications assessed in the decision analysis, including wound infections, transfusions, hernias, and venous thromboembolisms, were more frequent in the abdominal hysterectomy group. The forthcoming final publication will include the citations on which all of the event probabilities were based.
An alternative and perhaps more readily grasped way of expressing the QALY results is that patients undergoing laparoscopic hysterectomy enjoyed an additional 0.85 QALY, or roughly 1 extra month of life in perfect health over a 5-year time period, Dr. Siedhoff explained.
The decision analysis didn’t include the well-established facts that laparoscopic hysterectomy entails less postoperative pain, a shorter average hospital length of stay, and faster return to daily activities.
Dr. Siedhoff was quick to assert that the true incidence of occult leiomyosarcoma in women undergoing surgery for presumed fibroids is unknown. An American College of Obstetricians and Gynecologist’s position statement issued earlier this year quoted an estimate of 1 in 500. The FDA cited a figure of 1 in 350. But when the North Carolina researchers examined the 10 studies published during 1990-2013, upon which the FDA based its estimate, the investigators felt compelled to reject 6 of them because of poor quality. For example, several studies included morcellation in patients with preoperative known or suspected sarcoma, even though morcellation should absolutely never be done in that situation. Based upon a weighted analysis of the remaining four highest-quality studies, the investigators came up with an estimate of 12 cases/10,000 women.
Noting that the largest of the studies in the FDA analysis included just 1,584 women with 2 cases of leiomyosarcoma, Dr. Siedhoff said, “I think it’s important to point out that really important decisions are being made on awfully small numerators and denominators. The truth of the matter is we have no idea what the true number is. It could be twice as high as our estimate or half as low.”
He admitted that he has been personally affected by the rancorous tone of recent public debate regarding morcellation safety, in which the procedure’s defenders often are demonized.
“It’s been confusing to me why in the Wall Street Journal they talk about these evil doctors who want to use this technique, as if it somehow benefits us. It’s not easier to do laparoscopic surgery, and it’s certainly not easier to morcellate tissue. The only reason that we’re talking about this is because we care about the outcomes for our patients,” the gynecologic surgeon said at the meeting presented by the Society of Laparoendoscopic Surgeons and affiliated societies. “One of the things that has been most difficult about all this,” he continued, “is the way that the information has moved from some very vocal people who feel strongly about this issue to the level of the lay person that you see in the elevator, or worse yet, your own patient. I think it’s almost like a game of telephone, so that by the time it gets down to a person who’s not a surgeon, the message is ‘morcellation causes cancer.’”Not only is the true prevalence of occult malignancy in women undergoing laparoscopic surgery for removal of fibroids unclear, but the data on the adverse impact of morcellation in this situation is sketchy as well. To date, it consists of two single-center retrospective studies. The more recent report, from Brigham and Women’s Hospital, involved 19 patients who underwent morcellation and 39 who had a total abdominal hysterectomy, all found to have leiomyosarcoma. The cancer recurrence rate was significantly higher in women who had morcellation, by a margin of 74% to 51%. However, there was no significant difference in overall survival (Cancer 2014 [doi:10.1002/cncr.28844]).
In contrast, an earlier Korean study involving a consecutive series comprised of 25 patients with occult leiomyosarcoma who underwent morcellation and 31 with total abdominal hysterectomy found a significant difference in 5-year overall survival: 46% in the morcellation group, and what Dr. Siedhoff deemed an unusually favorable 73% in the total abdominal hysterectomy patients (Gynecol. Oncol. 2011;122:255-9).
There is a great unmet need for a reliable preoperative method to distinguish leiomyosarcomas from benign fibroids. Imaging is of limited value. Endometrial biopsy is rarely positive. No biomarkers have been identified. Clinical factors that increase the likelihood of leiomyosarcoma include rapid growth, African American ethnicity, older age, a history of pelvic radiation, and the presence of the retinoblastoma gene.
In his own practice, Dr. Siedhoff sometimes uses specimen retrieval bags when performing morcellation, but finds the currently available versions to be cumbersome and a challenge to work with. Besides, he noted, there is to date no evidence that they are actually effective in reducing leiomyosarcoma recurrence risk. He was a member of an AAGL task force which in May issued a position statement on morcellation, which noted, “Use of morcellation within specimen retrieval pouches for containment of benign or malignant uterine tissue requires significant skill and experience, and use of specimen retrieval pouches should be further investigated for safety and outcomes in a controlled setting.”
Dr. Siedhoff reported having no financial conflicts regarding the decision analysis, conducted with university funds.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: Despite the much-publicized risk of intraperitoneal dissemination of tumor during morcellation in women undergoing laparoscopic hysterectomy for fibroids, the projected 5-year overall survival is better than with abdominal hysterectomy.
Major finding: In a hypothetical population of 200,000 women undergoing hysterectomy for presumed fibroids, laparoscopic surgery with morcellation would result in a projected 98 deaths from all causes during 5 years of follow-up and abdominal hysterectomy would result in 103 deaths.
Data source: This was a decision analysis in which the probabilities of various surgical outcomes based upon studies in the published literature were applied to a hypothetical cohort of 200,000 women undergoing hysterectomy for removal of fibroids, half laparoscopically with morcellation and half via abdominal hysterectomy.
Disclosures: The presenter reported having no financial conflicts of interest regarding the decision analysis study.