User login
To the Editor:
Acne vulgaris and irritable bowel syndrome (IBS) are both associated with microbial dysbiosis and chronic inflammation.1-3 While the prevalence of IBS among patients with acne has been examined previously,4,5 there has been limited focus on the risk for new-onset IBS following acne diagnosis. Current evidence suggests isotretinoin may be associated with a lower risk for IBS compared to oral antibiotics6; however, evidence supporting this association is limited outside these cohorts, highlighting the need for further investigation. In this large-scale study, we sought to investigate the incidence of new-onset IBS among patients with acne compared with healthy controls as well as to evaluate whether oral acne treatments (ie, oral antibiotics or isotretinoin) are associated with new-onset IBS in this population.
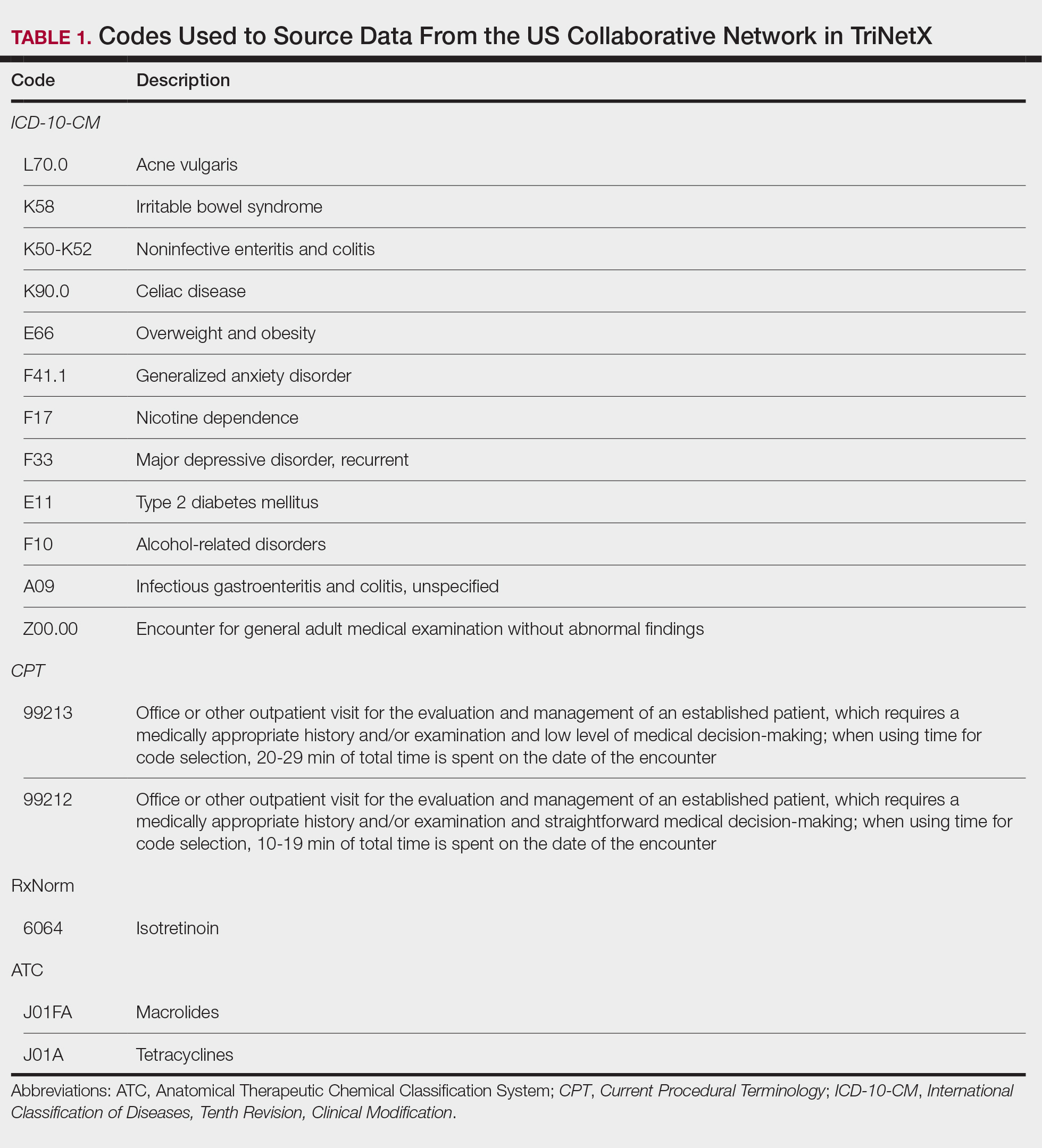
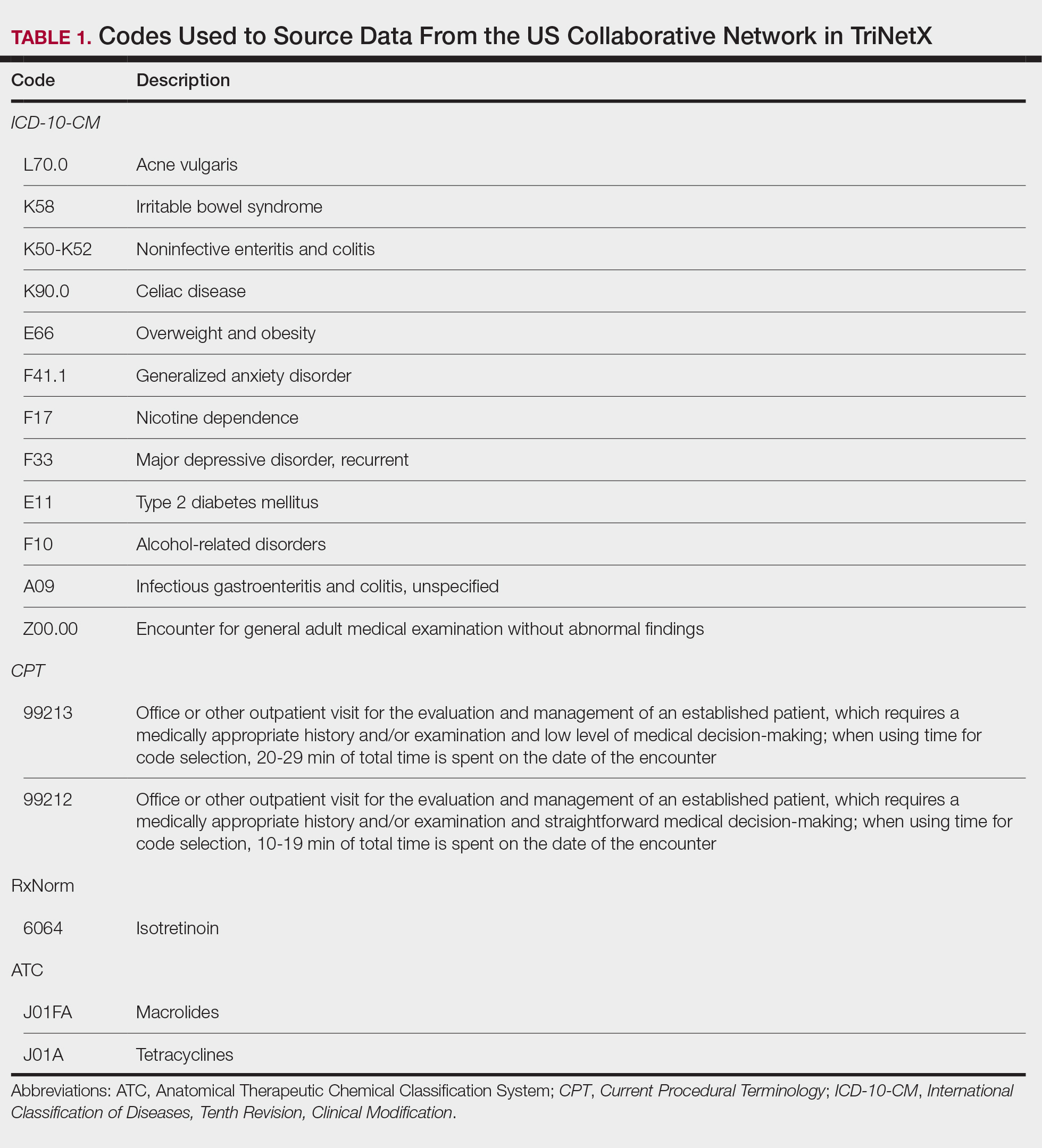
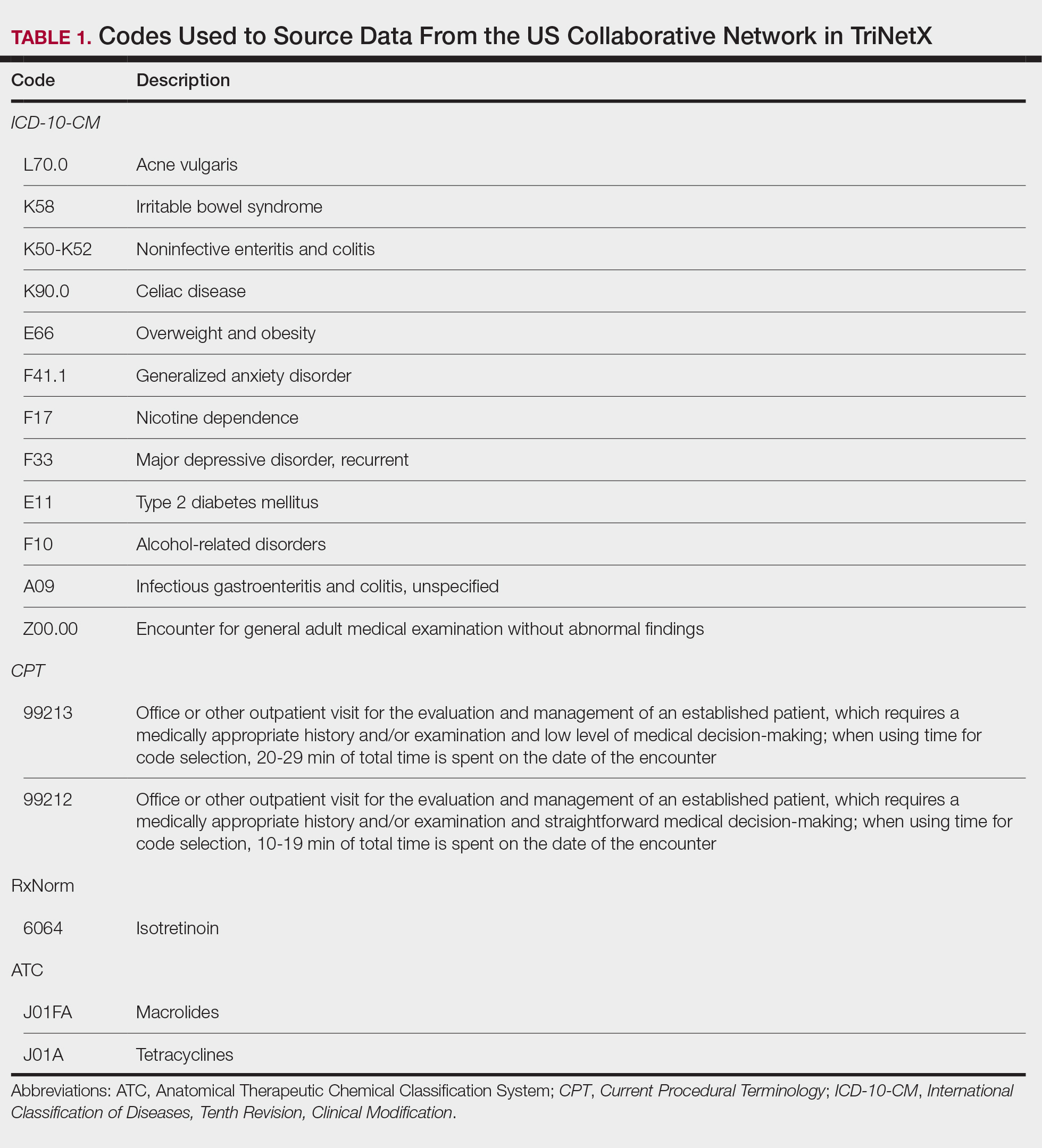
A retrospective cohort study was conducted using data from the US Collaborative Network in TriNetX from October 2014 to October 2024. Patients were identified using International Classification of Diseases, Tenth Revision, Clinical Modification codes, Current Procedural Terminology codes, Anatomical Therapeutic Chemical Classification System codes, and RxNorm codes (Table 1). These codes were selected based on prior literature review, clinical relevance, and their ability to capture diagnoses of acne and IBS as well as relevant exclusion criteria. Patients were considered eligible if they were between the ages of 18 and 90 years. Individuals with a history of IBS, inflammatory bowel disease, infectious gastroenteritis, or celiac disease were excluded from our analysis.
To examine potential associations between acne and IBS, 2 primary cohorts were established: patients with acne who were managed without systemic medications and healthy controls (ie, patients with no history of acne) who had no exposure to systemic acne treatments (Figure). Further, to assess the relationship between oral acne treatments (macrolides, tetracyclines, isotretinoin) and IBS, additional cohorts were created for each therapy and were compared to a cohort of patients with acne who were managed without systemic medications. To control for potential concomitant treatments, patients who had received any systemic treatment other than the specific therapy for their treatment cohort were excluded from our analysis.
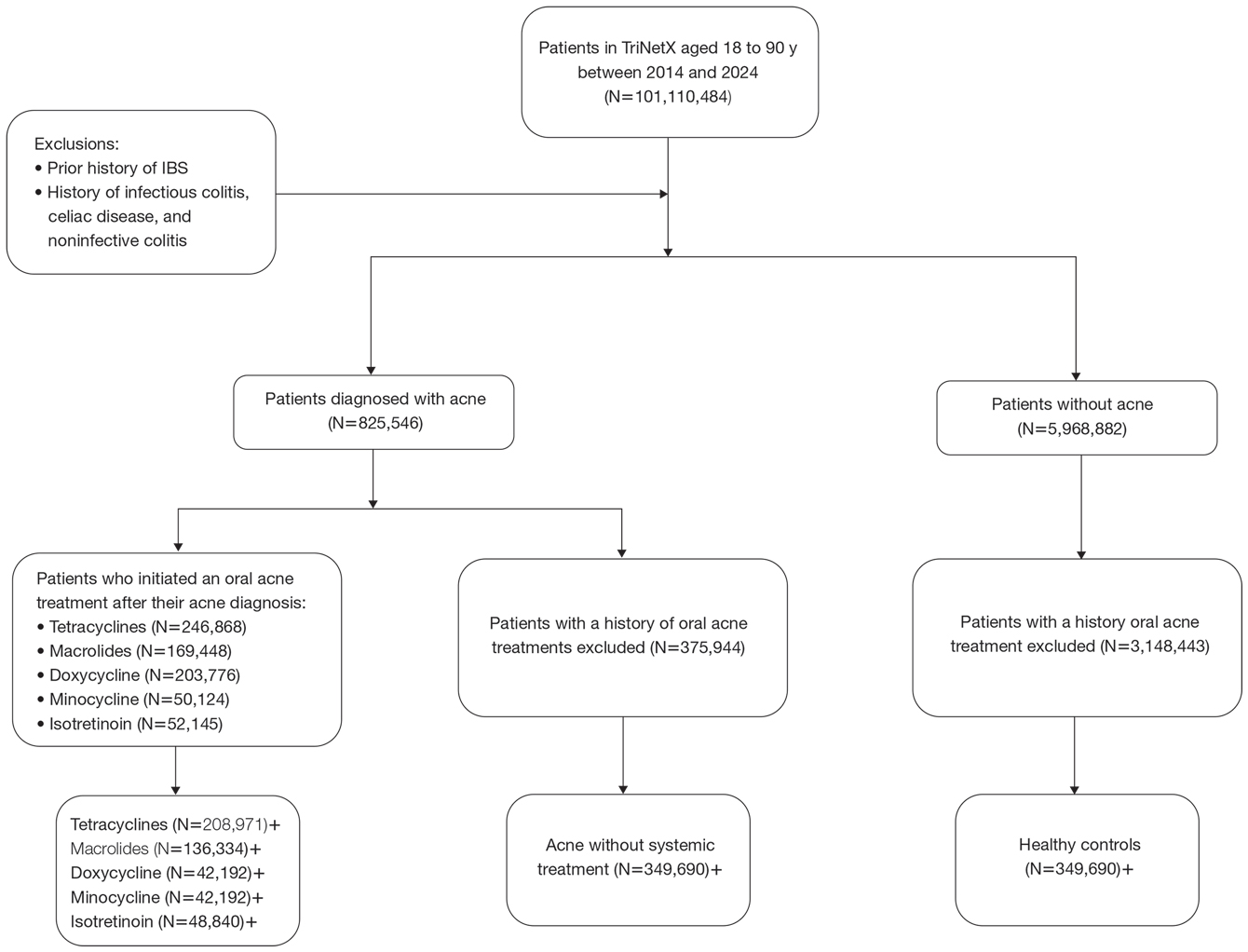
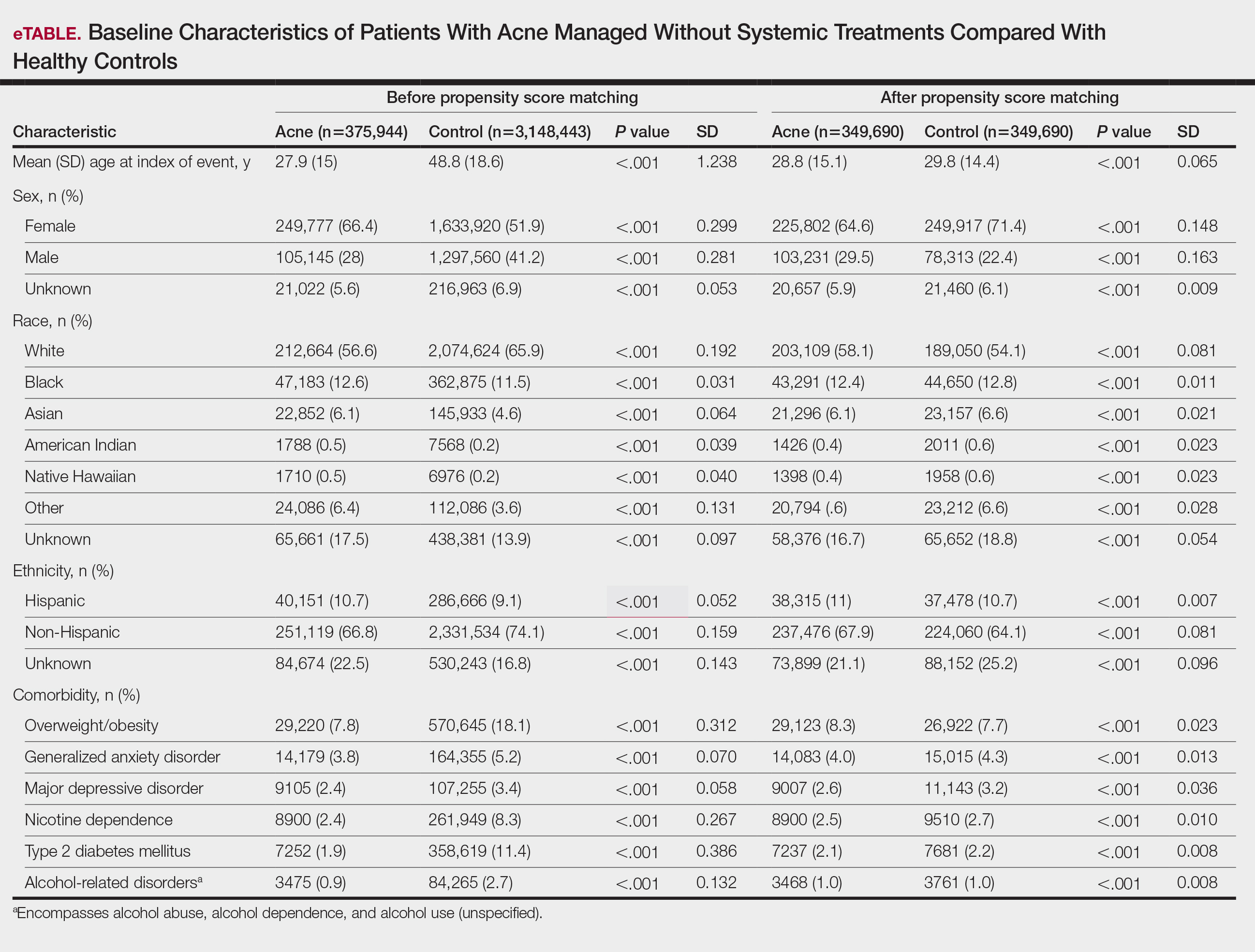
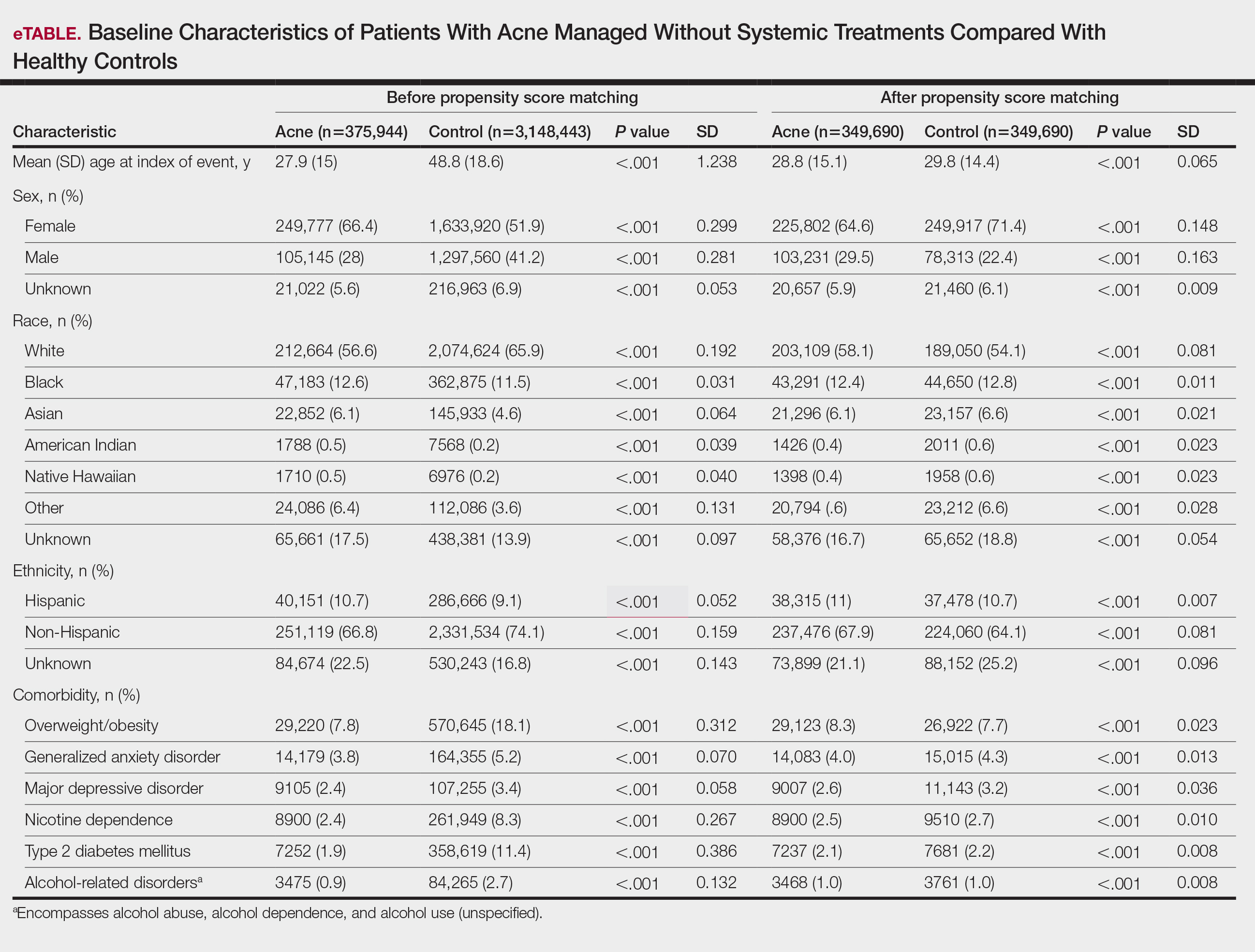
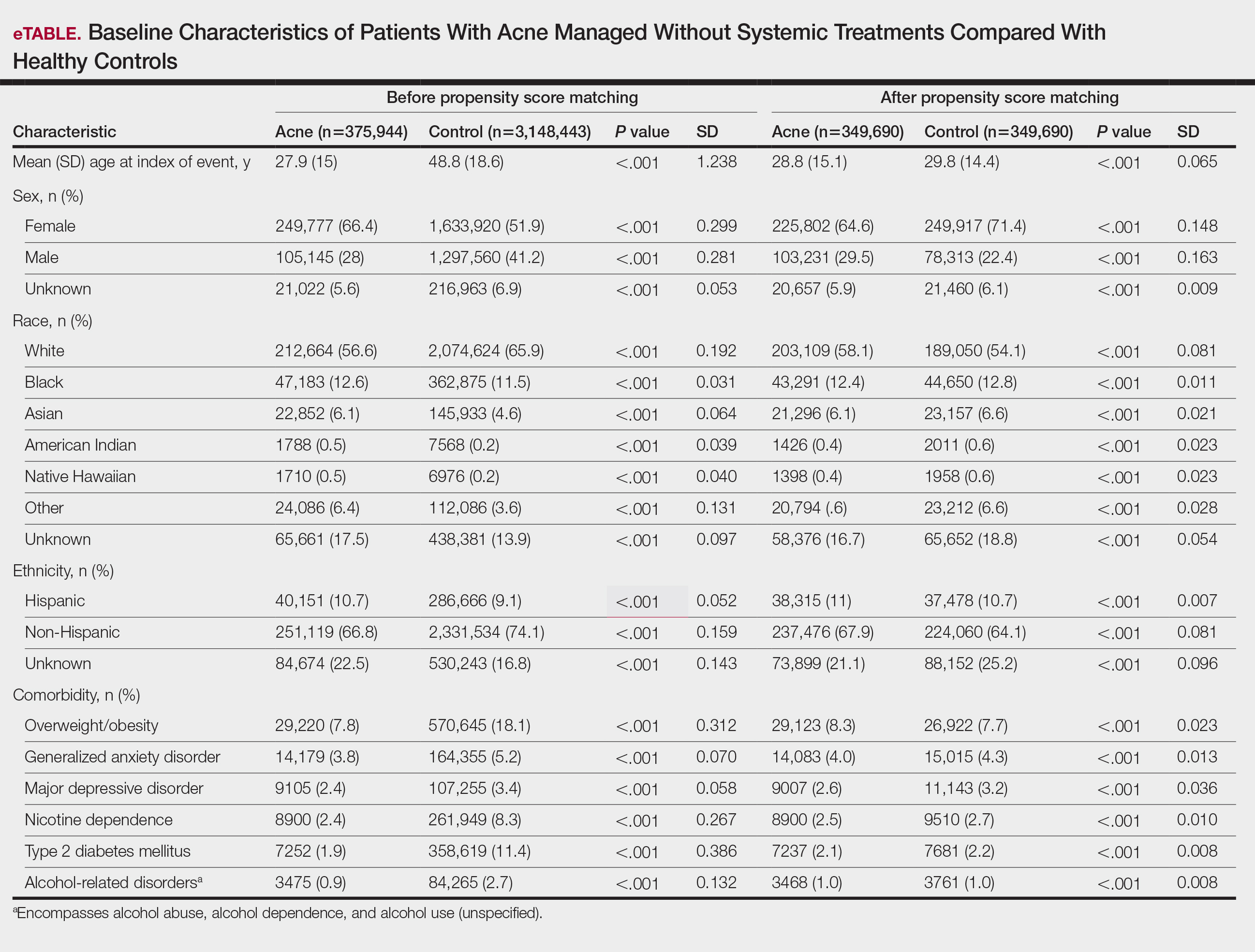
To account for potential confounders, all cohorts were 1:1 propensity score matched by demographics, tobacco and alcohol use, type 2 diabetes, obesity, anxiety, and depression (eTable). Each cohort was followed for 2 years after their index of event: the date of acne diagnosis for the acne cohort, the date of systemic treatment initiation for the treatment cohorts, and the date of the general adult encounter without abnormal findings for the control cohort. The primary outcome was the incidence of IBS, assessed by odds ratio (OR) and 95% CIs.
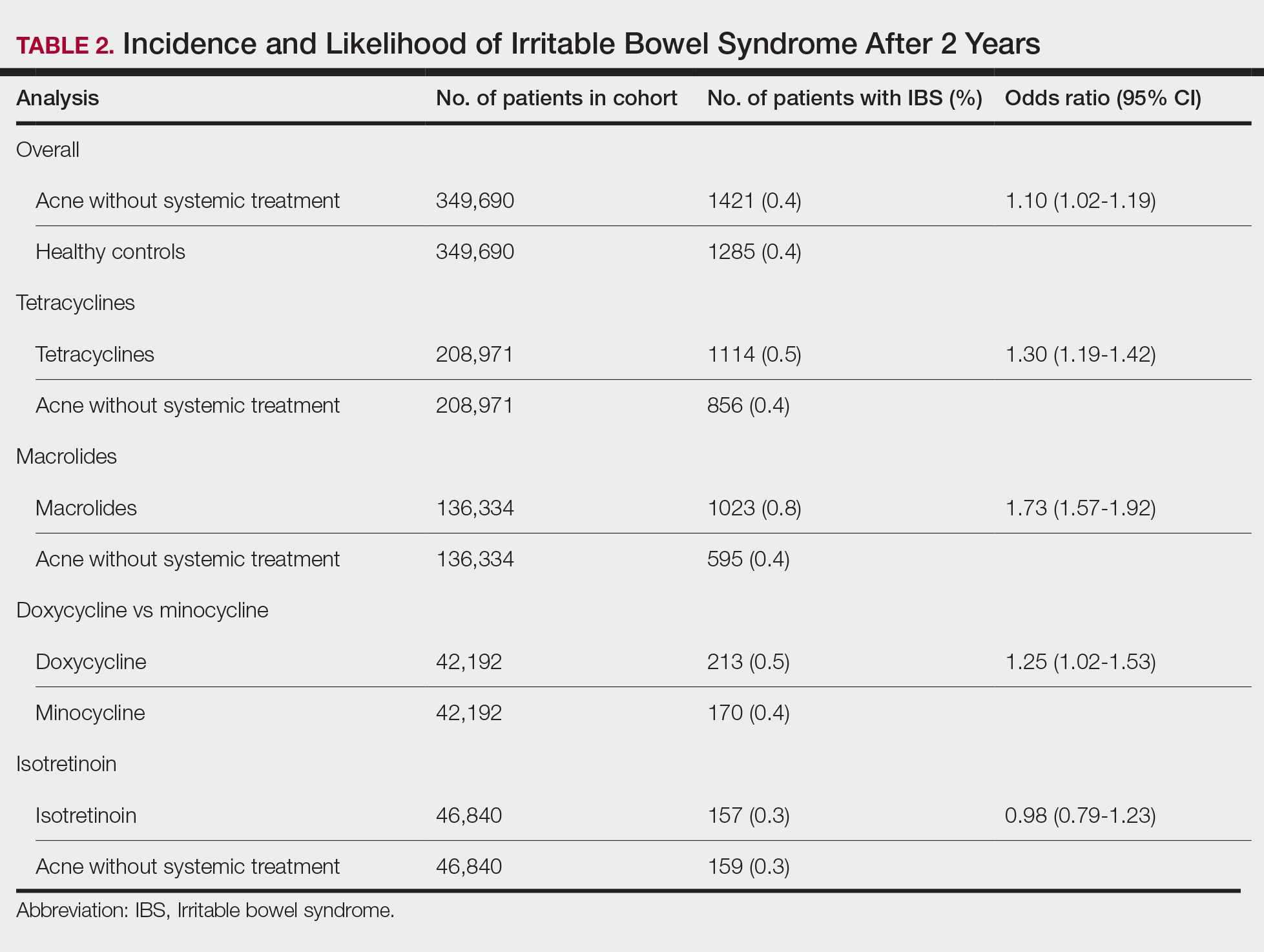
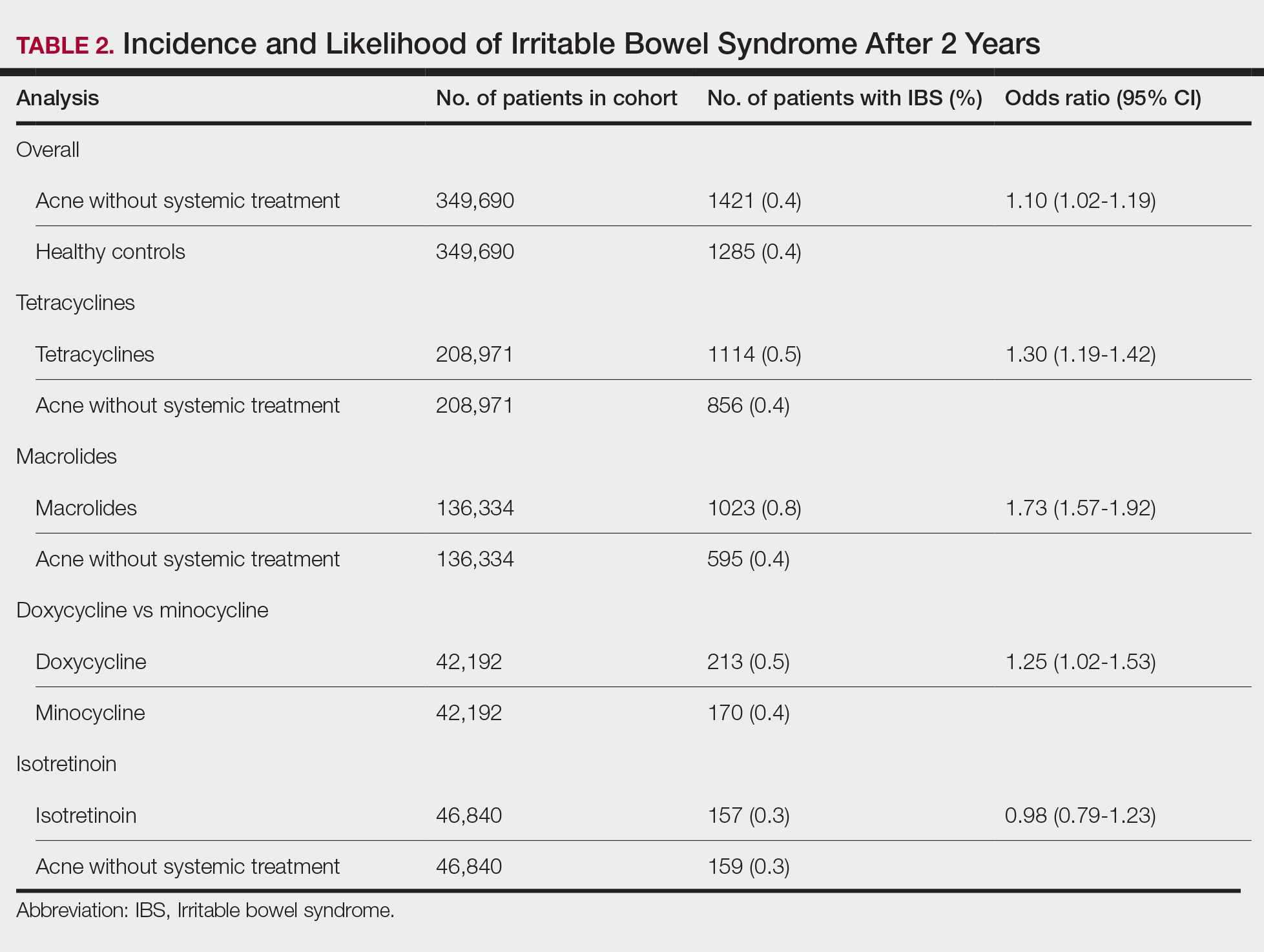
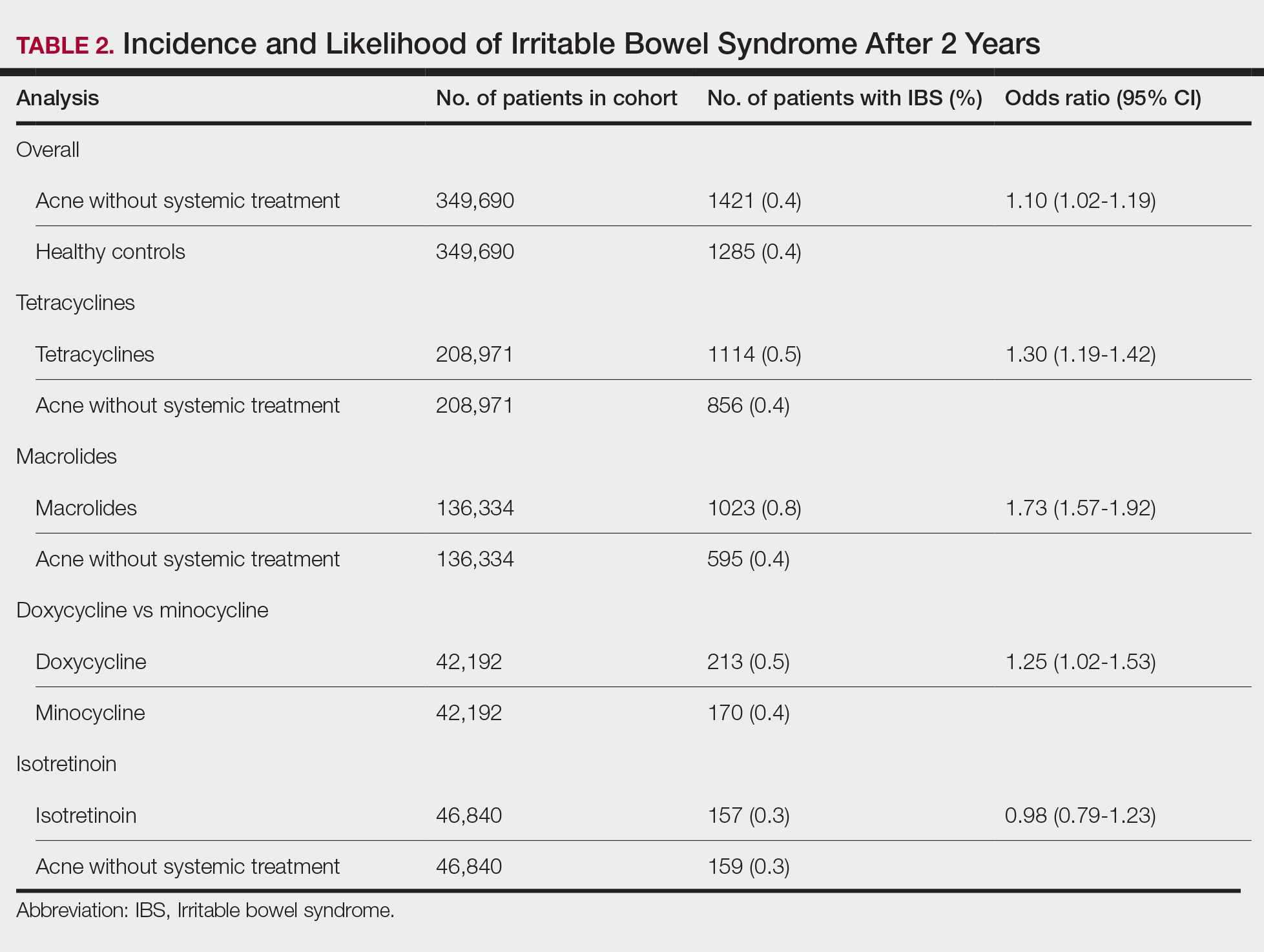
We identified 375,944 patients with acne managed without systemic treatment and 3,148,443 healthy controls who met study criteria. After the 1:1 propensity score match, each cohort included 49,690 patients (eTable). In the 2-year period after acne diagnosis, patients were more likely to develop IBS compared with controls (1421 vs 1285 [OR, 1.10; 95% CI, 1.02-1.19])(Table 2). Patients with acne who were treated with tetracyclines (n=208,971) were 30% more likely to develop IBS than those managed without systemic medications (1114 vs 856 [OR, 1.30; 95% CI, 1.19-1.42]). Within the tetracycline cohort, doxycycline-treated patients were 25% more likely to develop IBS compared with those treated with minocycline (213 vs 170 [OR, 1.25; 95% CI, 1.02-1.53]). Similarly, the use of macrolides (n=136,334) for acne treatment was significantly associated with an increased risk for IBS (1023 vs 595 [OR, 1.73; 95% CI, 1.57-1.92; P<.0001]) compared with controls. No statistically significant association was observed between isotretinoin and the incidence of IBS (Table 2).
In this large-scale cohort study, acne was associated with an increased likelihood of developing IBS within 2 years of an acne diagnosis compared with healthy controls. While a prior study also identified this association, it had a broader follow-up window ranging from 8 to 10 years.2 In contrast, our analysis specifically quantified the risk within the first 2 years of diagnosis. This distinction suggested potential for earlier IBS onset in patients with acne than has previously been recognized and may serve as an early clinical indicator for IBS risk in this population.
Our findings further suggested an association between oral tetracyclines and macrolides and an increased risk for IBS. This aligns with existing literature suggesting that oral antibiotic use can disrupt the gut microbiota and lead to potential gastrointestinal complications7 and reinforces the importance of careful antibiotic stewardship in dermatologic practice.
Although isotretinoin initially was surrounded by substantial controversy regarding its potential impact on gut health—particularly in inflammatory bowel disease8—our results do not support an increased risk for IBS among patients with acne who use isotretinoin. These findings challenge previous concerns and align with research suggesting that isotretinoin could be a safer alternative to antibiotic use for eligible patients who have a history of gastrointestinal disorders.6
This study highlights an important but underrecognized link between acne and IBS risk, emphasizing the need for early monitoring of gastrointestinal symptoms and careful antibiotic stewardship in dermatologic practice. Gastroenterology consultation may be advisable for patients with acne who have persistent gastrointestinal symptoms to facilitate a more integrated, patient-centered approach to care.
Limitations of this study include potential misclassification of International Classification of Diseases, Tenth Revision, Clinical Modification codes, selection bias, and residual confounding from unmeasured factors such as diet, lifestyle, disease severity, and treatment adherence due to the reliance on electronic health record data.
Our findings build upon prior evidence linking acne and IBS and offer important insights into the timing of this association following acne diagnosis. Future research should explore biological mechanisms underlying the gut-skin axis and evaluate targeted interventions to mitigate IBS risk in patients with acne.
Menees S, Chey W. The gut microbiome and irritable bowel syndrome. F1000Res. 2018;7:F1000 Faculty Rev-1029. doi:10.12688/f1000research.14592.1
Yu-Wen C, Chun-Ying W, Yi-Ju C. Gastrointestinal comorbidities in patients with acne vulgaris: a population-based retrospective study. JAAD Int. 2025;18:62-68. doi:10.1016/j.jdin.2024.08.022
Deng Y, Wang H, Zhou J, et al. Patients with acne vulgaris have a distinct gut microbiota in comparison with healthy controls. Acta Derm Venereol. 2018;98:783-790. doi:10.2340/00015555-2968
Demirbas¸ A, Elmas ÖF. The relationship between acne vulgaris and irritable bowel syndrome: a preliminary study. J Cosmet Dermatol. 2021;20:316-320. doi:10.1111/jocd.13481
Daye M, Cihan FG, Is¸ık B, et al. Evaluation of bowel habits in patients with acne vulgaris. Int J Clin Pract. 2021;75:e14903. doi:10.1111/ijcp.14903
Kridin K, Ludwig RJ. Isotretinoin and the risk of inflammatory bowel disease and irritable bowel syndrome: a large-scale global study. J Am Acad Dermatol. 2023;88:824-830. doi:10.1016/j.jaad.2022.12.015
Villarreal AA, Aberger FJ, Benrud R, et al. Use of broad-spectrum antibiotics and the development of irritable bowel syndrome. WMJ. 2012;111:17-20.
Yu C-L, Chou P-Y, Liang C-S, et al. Isotretinoin exposure and risk of inflammatory bowel disease: a systematic review with meta-analysis and trial sequential analysis. Am J Clin Dermatol. 2023;24:721-730. doi:10.1007/s40257-023-00765-9
To the Editor:
Acne vulgaris and irritable bowel syndrome (IBS) are both associated with microbial dysbiosis and chronic inflammation.1-3 While the prevalence of IBS among patients with acne has been examined previously,4,5 there has been limited focus on the risk for new-onset IBS following acne diagnosis. Current evidence suggests isotretinoin may be associated with a lower risk for IBS compared to oral antibiotics6; however, evidence supporting this association is limited outside these cohorts, highlighting the need for further investigation. In this large-scale study, we sought to investigate the incidence of new-onset IBS among patients with acne compared with healthy controls as well as to evaluate whether oral acne treatments (ie, oral antibiotics or isotretinoin) are associated with new-onset IBS in this population.
A retrospective cohort study was conducted using data from the US Collaborative Network in TriNetX from October 2014 to October 2024. Patients were identified using International Classification of Diseases, Tenth Revision, Clinical Modification codes, Current Procedural Terminology codes, Anatomical Therapeutic Chemical Classification System codes, and RxNorm codes (Table 1). These codes were selected based on prior literature review, clinical relevance, and their ability to capture diagnoses of acne and IBS as well as relevant exclusion criteria. Patients were considered eligible if they were between the ages of 18 and 90 years. Individuals with a history of IBS, inflammatory bowel disease, infectious gastroenteritis, or celiac disease were excluded from our analysis.
To examine potential associations between acne and IBS, 2 primary cohorts were established: patients with acne who were managed without systemic medications and healthy controls (ie, patients with no history of acne) who had no exposure to systemic acne treatments (Figure). Further, to assess the relationship between oral acne treatments (macrolides, tetracyclines, isotretinoin) and IBS, additional cohorts were created for each therapy and were compared to a cohort of patients with acne who were managed without systemic medications. To control for potential concomitant treatments, patients who had received any systemic treatment other than the specific therapy for their treatment cohort were excluded from our analysis.
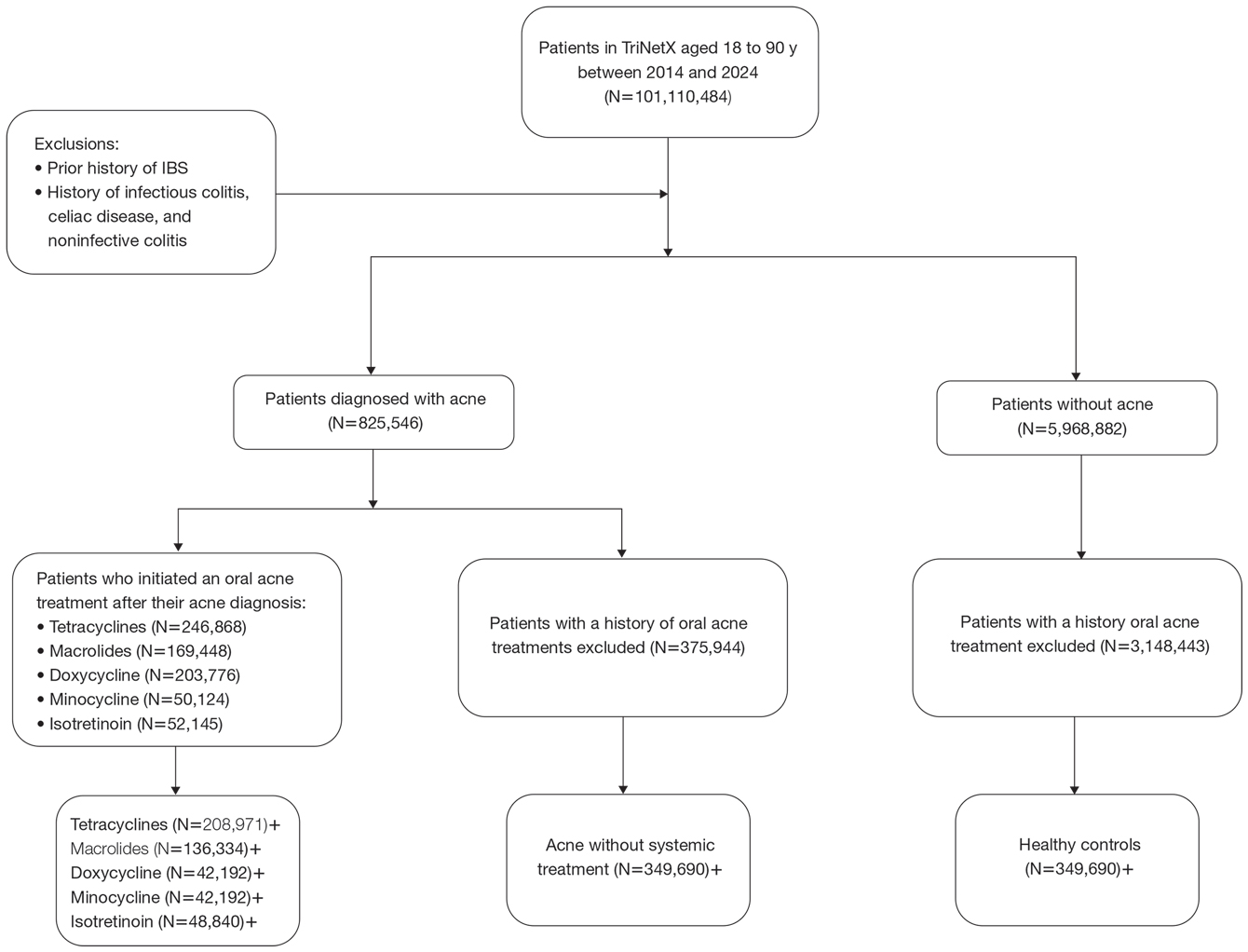
To account for potential confounders, all cohorts were 1:1 propensity score matched by demographics, tobacco and alcohol use, type 2 diabetes, obesity, anxiety, and depression (eTable). Each cohort was followed for 2 years after their index of event: the date of acne diagnosis for the acne cohort, the date of systemic treatment initiation for the treatment cohorts, and the date of the general adult encounter without abnormal findings for the control cohort. The primary outcome was the incidence of IBS, assessed by odds ratio (OR) and 95% CIs.
We identified 375,944 patients with acne managed without systemic treatment and 3,148,443 healthy controls who met study criteria. After the 1:1 propensity score match, each cohort included 49,690 patients (eTable). In the 2-year period after acne diagnosis, patients were more likely to develop IBS compared with controls (1421 vs 1285 [OR, 1.10; 95% CI, 1.02-1.19])(Table 2). Patients with acne who were treated with tetracyclines (n=208,971) were 30% more likely to develop IBS than those managed without systemic medications (1114 vs 856 [OR, 1.30; 95% CI, 1.19-1.42]). Within the tetracycline cohort, doxycycline-treated patients were 25% more likely to develop IBS compared with those treated with minocycline (213 vs 170 [OR, 1.25; 95% CI, 1.02-1.53]). Similarly, the use of macrolides (n=136,334) for acne treatment was significantly associated with an increased risk for IBS (1023 vs 595 [OR, 1.73; 95% CI, 1.57-1.92; P<.0001]) compared with controls. No statistically significant association was observed between isotretinoin and the incidence of IBS (Table 2).
In this large-scale cohort study, acne was associated with an increased likelihood of developing IBS within 2 years of an acne diagnosis compared with healthy controls. While a prior study also identified this association, it had a broader follow-up window ranging from 8 to 10 years.2 In contrast, our analysis specifically quantified the risk within the first 2 years of diagnosis. This distinction suggested potential for earlier IBS onset in patients with acne than has previously been recognized and may serve as an early clinical indicator for IBS risk in this population.
Our findings further suggested an association between oral tetracyclines and macrolides and an increased risk for IBS. This aligns with existing literature suggesting that oral antibiotic use can disrupt the gut microbiota and lead to potential gastrointestinal complications7 and reinforces the importance of careful antibiotic stewardship in dermatologic practice.
Although isotretinoin initially was surrounded by substantial controversy regarding its potential impact on gut health—particularly in inflammatory bowel disease8—our results do not support an increased risk for IBS among patients with acne who use isotretinoin. These findings challenge previous concerns and align with research suggesting that isotretinoin could be a safer alternative to antibiotic use for eligible patients who have a history of gastrointestinal disorders.6
This study highlights an important but underrecognized link between acne and IBS risk, emphasizing the need for early monitoring of gastrointestinal symptoms and careful antibiotic stewardship in dermatologic practice. Gastroenterology consultation may be advisable for patients with acne who have persistent gastrointestinal symptoms to facilitate a more integrated, patient-centered approach to care.
Limitations of this study include potential misclassification of International Classification of Diseases, Tenth Revision, Clinical Modification codes, selection bias, and residual confounding from unmeasured factors such as diet, lifestyle, disease severity, and treatment adherence due to the reliance on electronic health record data.
Our findings build upon prior evidence linking acne and IBS and offer important insights into the timing of this association following acne diagnosis. Future research should explore biological mechanisms underlying the gut-skin axis and evaluate targeted interventions to mitigate IBS risk in patients with acne.
To the Editor:
Acne vulgaris and irritable bowel syndrome (IBS) are both associated with microbial dysbiosis and chronic inflammation.1-3 While the prevalence of IBS among patients with acne has been examined previously,4,5 there has been limited focus on the risk for new-onset IBS following acne diagnosis. Current evidence suggests isotretinoin may be associated with a lower risk for IBS compared to oral antibiotics6; however, evidence supporting this association is limited outside these cohorts, highlighting the need for further investigation. In this large-scale study, we sought to investigate the incidence of new-onset IBS among patients with acne compared with healthy controls as well as to evaluate whether oral acne treatments (ie, oral antibiotics or isotretinoin) are associated with new-onset IBS in this population.
A retrospective cohort study was conducted using data from the US Collaborative Network in TriNetX from October 2014 to October 2024. Patients were identified using International Classification of Diseases, Tenth Revision, Clinical Modification codes, Current Procedural Terminology codes, Anatomical Therapeutic Chemical Classification System codes, and RxNorm codes (Table 1). These codes were selected based on prior literature review, clinical relevance, and their ability to capture diagnoses of acne and IBS as well as relevant exclusion criteria. Patients were considered eligible if they were between the ages of 18 and 90 years. Individuals with a history of IBS, inflammatory bowel disease, infectious gastroenteritis, or celiac disease were excluded from our analysis.
To examine potential associations between acne and IBS, 2 primary cohorts were established: patients with acne who were managed without systemic medications and healthy controls (ie, patients with no history of acne) who had no exposure to systemic acne treatments (Figure). Further, to assess the relationship between oral acne treatments (macrolides, tetracyclines, isotretinoin) and IBS, additional cohorts were created for each therapy and were compared to a cohort of patients with acne who were managed without systemic medications. To control for potential concomitant treatments, patients who had received any systemic treatment other than the specific therapy for their treatment cohort were excluded from our analysis.
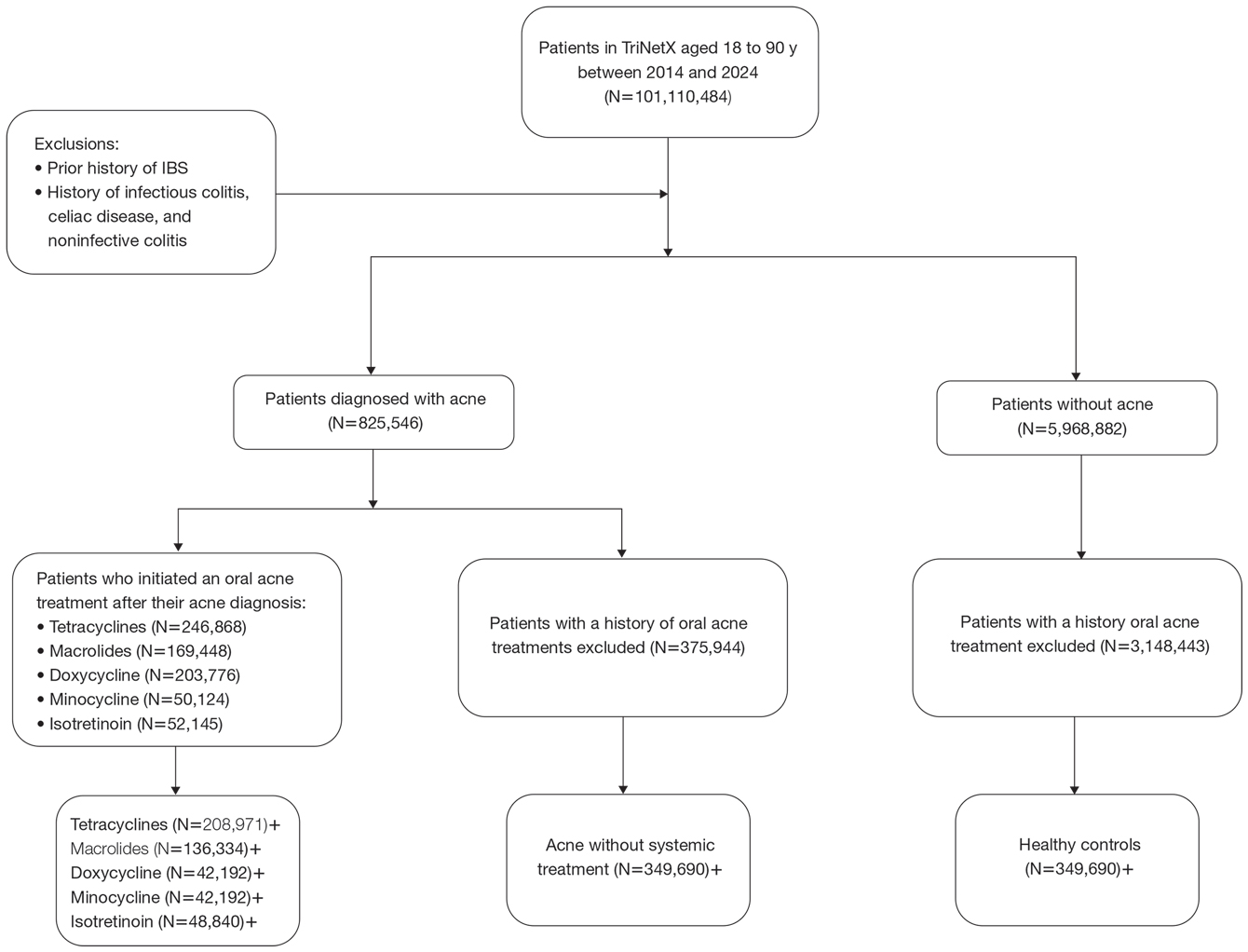
To account for potential confounders, all cohorts were 1:1 propensity score matched by demographics, tobacco and alcohol use, type 2 diabetes, obesity, anxiety, and depression (eTable). Each cohort was followed for 2 years after their index of event: the date of acne diagnosis for the acne cohort, the date of systemic treatment initiation for the treatment cohorts, and the date of the general adult encounter without abnormal findings for the control cohort. The primary outcome was the incidence of IBS, assessed by odds ratio (OR) and 95% CIs.
We identified 375,944 patients with acne managed without systemic treatment and 3,148,443 healthy controls who met study criteria. After the 1:1 propensity score match, each cohort included 49,690 patients (eTable). In the 2-year period after acne diagnosis, patients were more likely to develop IBS compared with controls (1421 vs 1285 [OR, 1.10; 95% CI, 1.02-1.19])(Table 2). Patients with acne who were treated with tetracyclines (n=208,971) were 30% more likely to develop IBS than those managed without systemic medications (1114 vs 856 [OR, 1.30; 95% CI, 1.19-1.42]). Within the tetracycline cohort, doxycycline-treated patients were 25% more likely to develop IBS compared with those treated with minocycline (213 vs 170 [OR, 1.25; 95% CI, 1.02-1.53]). Similarly, the use of macrolides (n=136,334) for acne treatment was significantly associated with an increased risk for IBS (1023 vs 595 [OR, 1.73; 95% CI, 1.57-1.92; P<.0001]) compared with controls. No statistically significant association was observed between isotretinoin and the incidence of IBS (Table 2).
In this large-scale cohort study, acne was associated with an increased likelihood of developing IBS within 2 years of an acne diagnosis compared with healthy controls. While a prior study also identified this association, it had a broader follow-up window ranging from 8 to 10 years.2 In contrast, our analysis specifically quantified the risk within the first 2 years of diagnosis. This distinction suggested potential for earlier IBS onset in patients with acne than has previously been recognized and may serve as an early clinical indicator for IBS risk in this population.
Our findings further suggested an association between oral tetracyclines and macrolides and an increased risk for IBS. This aligns with existing literature suggesting that oral antibiotic use can disrupt the gut microbiota and lead to potential gastrointestinal complications7 and reinforces the importance of careful antibiotic stewardship in dermatologic practice.
Although isotretinoin initially was surrounded by substantial controversy regarding its potential impact on gut health—particularly in inflammatory bowel disease8—our results do not support an increased risk for IBS among patients with acne who use isotretinoin. These findings challenge previous concerns and align with research suggesting that isotretinoin could be a safer alternative to antibiotic use for eligible patients who have a history of gastrointestinal disorders.6
This study highlights an important but underrecognized link between acne and IBS risk, emphasizing the need for early monitoring of gastrointestinal symptoms and careful antibiotic stewardship in dermatologic practice. Gastroenterology consultation may be advisable for patients with acne who have persistent gastrointestinal symptoms to facilitate a more integrated, patient-centered approach to care.
Limitations of this study include potential misclassification of International Classification of Diseases, Tenth Revision, Clinical Modification codes, selection bias, and residual confounding from unmeasured factors such as diet, lifestyle, disease severity, and treatment adherence due to the reliance on electronic health record data.
Our findings build upon prior evidence linking acne and IBS and offer important insights into the timing of this association following acne diagnosis. Future research should explore biological mechanisms underlying the gut-skin axis and evaluate targeted interventions to mitigate IBS risk in patients with acne.
Menees S, Chey W. The gut microbiome and irritable bowel syndrome. F1000Res. 2018;7:F1000 Faculty Rev-1029. doi:10.12688/f1000research.14592.1
Yu-Wen C, Chun-Ying W, Yi-Ju C. Gastrointestinal comorbidities in patients with acne vulgaris: a population-based retrospective study. JAAD Int. 2025;18:62-68. doi:10.1016/j.jdin.2024.08.022
Deng Y, Wang H, Zhou J, et al. Patients with acne vulgaris have a distinct gut microbiota in comparison with healthy controls. Acta Derm Venereol. 2018;98:783-790. doi:10.2340/00015555-2968
Demirbas¸ A, Elmas ÖF. The relationship between acne vulgaris and irritable bowel syndrome: a preliminary study. J Cosmet Dermatol. 2021;20:316-320. doi:10.1111/jocd.13481
Daye M, Cihan FG, Is¸ık B, et al. Evaluation of bowel habits in patients with acne vulgaris. Int J Clin Pract. 2021;75:e14903. doi:10.1111/ijcp.14903
Kridin K, Ludwig RJ. Isotretinoin and the risk of inflammatory bowel disease and irritable bowel syndrome: a large-scale global study. J Am Acad Dermatol. 2023;88:824-830. doi:10.1016/j.jaad.2022.12.015
Villarreal AA, Aberger FJ, Benrud R, et al. Use of broad-spectrum antibiotics and the development of irritable bowel syndrome. WMJ. 2012;111:17-20.
Yu C-L, Chou P-Y, Liang C-S, et al. Isotretinoin exposure and risk of inflammatory bowel disease: a systematic review with meta-analysis and trial sequential analysis. Am J Clin Dermatol. 2023;24:721-730. doi:10.1007/s40257-023-00765-9
Menees S, Chey W. The gut microbiome and irritable bowel syndrome. F1000Res. 2018;7:F1000 Faculty Rev-1029. doi:10.12688/f1000research.14592.1
Yu-Wen C, Chun-Ying W, Yi-Ju C. Gastrointestinal comorbidities in patients with acne vulgaris: a population-based retrospective study. JAAD Int. 2025;18:62-68. doi:10.1016/j.jdin.2024.08.022
Deng Y, Wang H, Zhou J, et al. Patients with acne vulgaris have a distinct gut microbiota in comparison with healthy controls. Acta Derm Venereol. 2018;98:783-790. doi:10.2340/00015555-2968
Demirbas¸ A, Elmas ÖF. The relationship between acne vulgaris and irritable bowel syndrome: a preliminary study. J Cosmet Dermatol. 2021;20:316-320. doi:10.1111/jocd.13481
Daye M, Cihan FG, Is¸ık B, et al. Evaluation of bowel habits in patients with acne vulgaris. Int J Clin Pract. 2021;75:e14903. doi:10.1111/ijcp.14903
Kridin K, Ludwig RJ. Isotretinoin and the risk of inflammatory bowel disease and irritable bowel syndrome: a large-scale global study. J Am Acad Dermatol. 2023;88:824-830. doi:10.1016/j.jaad.2022.12.015
Villarreal AA, Aberger FJ, Benrud R, et al. Use of broad-spectrum antibiotics and the development of irritable bowel syndrome. WMJ. 2012;111:17-20.
Yu C-L, Chou P-Y, Liang C-S, et al. Isotretinoin exposure and risk of inflammatory bowel disease: a systematic review with meta-analysis and trial sequential analysis. Am J Clin Dermatol. 2023;24:721-730. doi:10.1007/s40257-023-00765-9
