User login
Diseases of the American Civil War, Part I
If cleanliness is next to godliness, then the average soldier in the American Civil War lived just down the street from hell. In a land at war, before the formal tenets of germ theory had spread beyond the confines of Louis Pasteur’s laboratory in France, the lack of basic hygiene, both cultural and situational, coupled to an almost complete lack of curative therapies created an appalling death toll. Waterborne diseases in particular spared neither general nor private, and neither doctor nor nurse.
“Of all the adversities that Union and Confederate soldiers confronted, none was more deadly or more prevalent than contaminated water,” according to Jeffrey S. Sartin, MD, in his survey of Civil War diseases.1
The Union Army records list 1,765,000 cases of diarrhea or dysentery with 45,000 deaths and 149,000 cases of typhoid fever with 35,000 deaths. Add to these the 1,316,000 cases of malaria (borne by mosquitoes breeding in the waters) with its 10,000 deaths, and it is easy to see how the battlefield itself took second place in service to the grim reaper. (Overall, there were roughly two deaths from disease for every one from wounds.)
The chief waterborne plague, infectious diarrhea – including bacterial, amoebic, and other parasites – as well as cholera and typhoid, was an all-year-long problem, and, with the typical wry humor of soldiers, these maladies were given popular names, including the “Tennessee trots” and the “Virginia quick-step.”
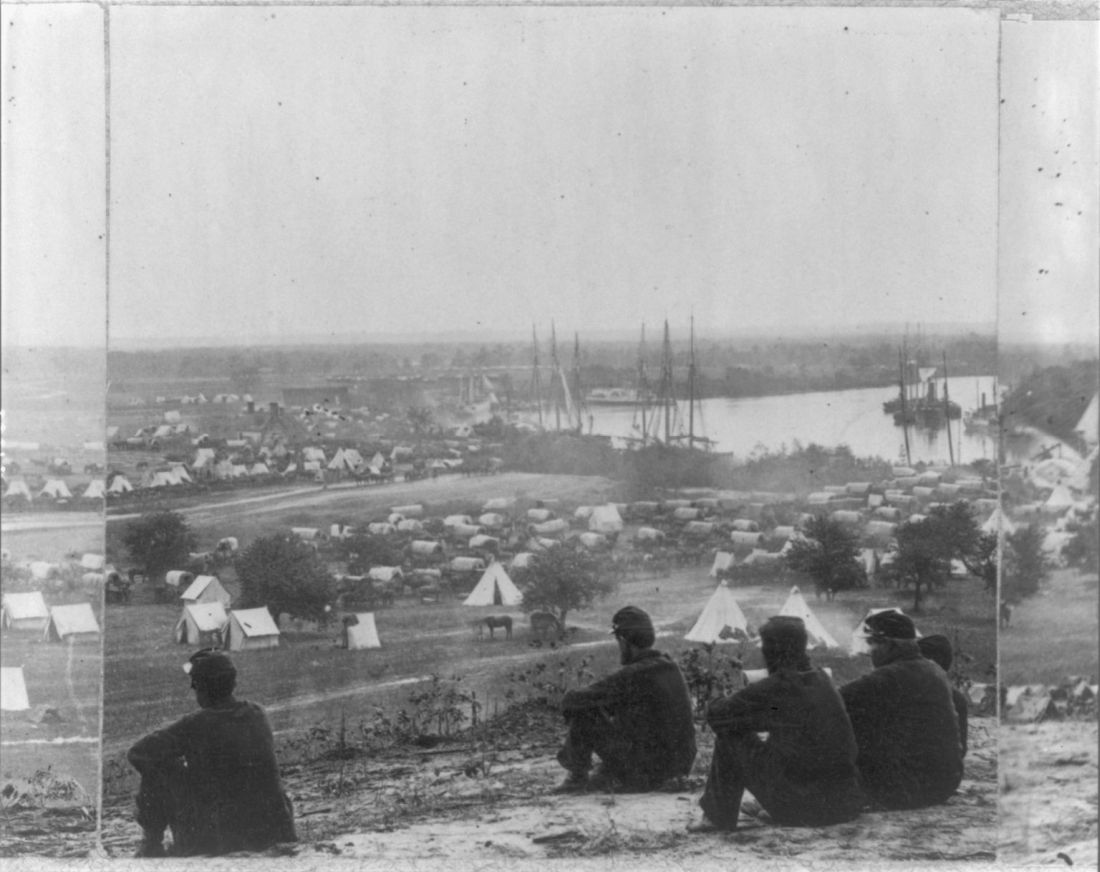
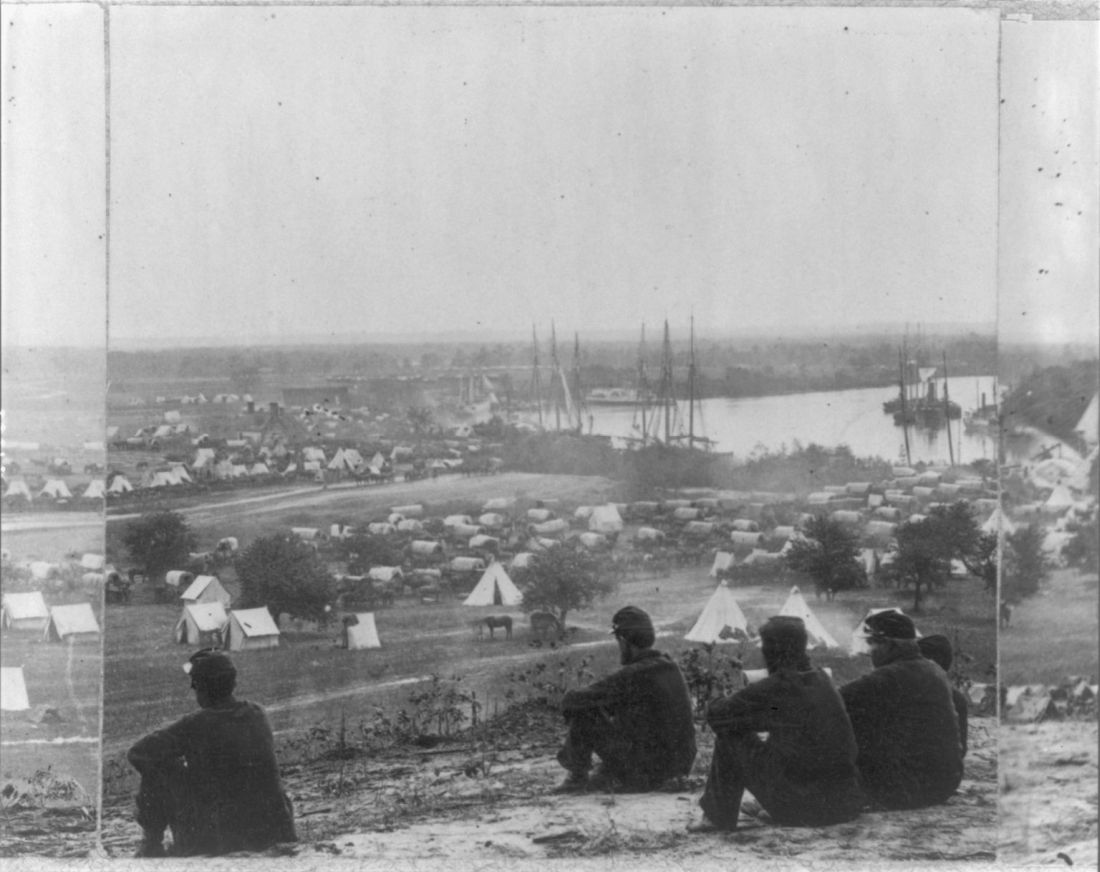
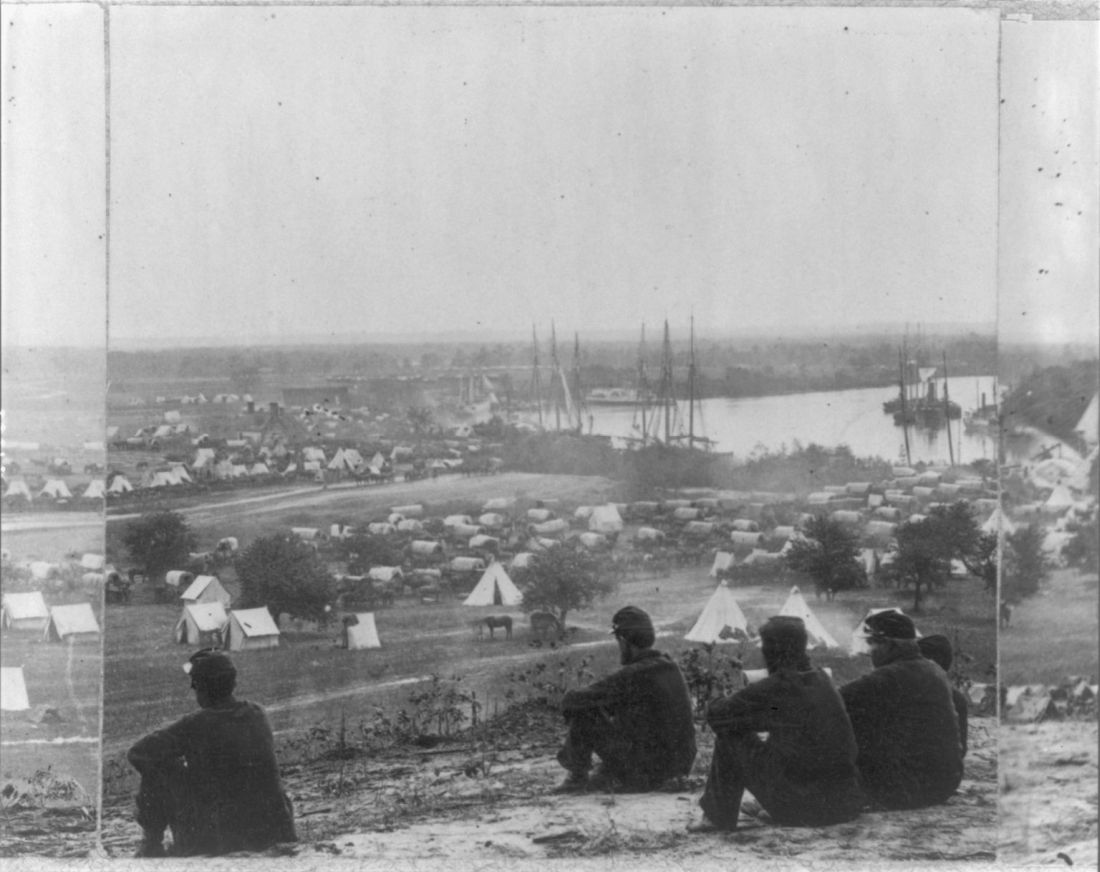
Unsanitary conditions in the camps were primarily to blame, and this problem of sanitation was obvious to many observers at the time.
Despite a lack of knowledge of germ theory, doctors were fully aware of the relationship of unsanitary conditions to disease, even if they ascribed the link to miasmas or particles of filth.
Hospitals, which were under more strict control than the regular army camps, were meticulous about the placement of latrines and about keeping high standards of cleanliness among the patients, including routine washing. However, this was insufficient for complete protection, because what passed for clean in the absence of the knowledge of bacterial contamination was often totally ineffective. As one Civil War surgeon stated: “We operated in old bloodstained and often pus-stained coats, we used undisinfected instruments from undisinfected plush-lined cases. If a sponge (if they had sponges) or instrument fell on the floor it was washed and squeezed in a basin of water and used as if it was clean.”2
Overall, efforts at what passed for sanitation remained a constant goal and constant struggle in the field.
After the First Battle of Bull Run, Women’s Central Association of Relief President Henry W. Bellows met with Secretary of War Simon Cameron to discuss the abysmal sanitary conditions witnessed by WCAR volunteers. This meeting led to the creation of what would become the U.S. Sanitary Commission, which was approved by President Abraham Lincoln on June 13, 1861.
The U.S. Sanitary Commission served as a means for funneling civilian assistance to the military, with volunteers providing assistance in the organization of military hospitals and camps and aiding in the transportation of the wounded. However, despite these efforts, the setup of army camps and the behavior of the soldiers were not often directed toward proper sanitation. “The principal causes of disease, however, in our camps were the same that we have always to deplore and find it so difficult to remedy, simply because citizens suddenly called to the field cannot comprehend that men in masses require the attention of their officers to enforce certain hygienic conditions without which health cannot be preserved.”3
Breaches of sanitation were common in the confines of the camps, despite regulations designed to protect the soldiers. According to one U.S. Army surgeon of the time: “Especially [needed] was policing of the latrines. The trench is generally too shallow, the daily covering ... with dirt is entirely neglected. Large numbers of the men will not use the sinks [latrines], ... but instead every clump of bushes, every fence border in the vicinity.” Another pointed out that, after the Battle of Seven Pines, “the only water was infiltrated with the decaying animal matter of the battlefield.” Commenting on the placement of latrines in one encampment, another surgeon described how “the sink [latrine] is the ground in the vicinity, which slopes down to the stream, from which all water from the camp is obtained.”4
Treatment for diarrhea and dysentery was varied. Opiates were one of the most common treatments for diarrhea, whether in an alcohol solution as laudanum or in pill form, with belladonna being used to treat intestinal cramps, according to Glenna R. Schroeder-Lein in her book “The Encyclopedia of Civil War Medicine.” However, useless or damaging treatments were also prescribed, including the use of calomel (a mercury compound), turpentine, castor oil, and quinine.5
Acute diarrhea and dysentery illnesses occurred in at least 641/1,000 troops per year in the Union army. And even though the death rate was comparatively low (20/1,000 cases), it frequently led to chronic diarrhea, which was responsible for 288 deaths per 1,000 cases, and was the third highest cause of medical discharge after gunshot wounds and tuberculosis, according to Ms. Schroeder-Lein.
Although the American Civil War was the last major conflict before the spread of the knowledge of germ theory, the struggle to prevent the spread of waterborne diseases under wartime conditions remains ongoing. Hygiene is difficult under conditions of abject poverty and especially under conditions of armed conflict, and until the era of curative antibiotics there was no recourse.
Antibiotics are not the final solution for antibiotic resistance in intestinal disease pathogens, as outlined in a recent CDC report, is an increasing problem.6 For example, nontyphoidal Salmonella causes an estimated 1.35 million infections, 26,500 hospitalizations, and 420 deaths each year in the United States, with 16% of strains being resistant to at least one essential antibiotic. On a global scale, according to the World Health Organization, poor sanitation causes up to 432,000 diarrheal deaths annually and is linked to the transmission of other diseases like cholera, dysentery, typhoid, hepatitis A, and polio.7
With regard to actual epidemics, the world is only a hygienic crisis away from a major outbreak of dysentery (the last occurring between 1969 and 1972, when 20,000 people in Central America died), according to researchers who have detected antibiotic resistance in all but 1% of circulating Shigella dysenteriae strains surveyed since the 1990s. “This bacterium is still in circulation, and could be responsible for future epidemics if conditions should prove favorable – such as a large gathering of people without access to drinking water or treatment of human waste,” wrote François-Xavier Weill of the Pasteur Institute’s Enteric Bacterial Pathogens Unit.8
References
1. Sartin JS. Clin Infec Dis. 1993;16:580-4. (Correction published in 2002).
2. Civil War Battlefield Surgery. eHistory. The Ohio State University.
3. “Myths About Antiseptics and Camp Life – George Wunderlich,” published online Oct. 11, 2011. http://civilwarscholars.com/2011/10/myths-about-antiseptics-and-camp-life-george-wunderlich/
4. Dorwart BB. “Death is in the Breeze: Disease during the American Civil War” (The National Museum of the American Civil War Press, 2009).
5. Glenna R, Schroeder-Lein GR. “The Encyclopedia of Civil War Medicine” (New York: M. E. Sharpe, 2008).
6. “Antibiotic resistance threats in the United States 2019” Centers for Disease Control and Prevention.
7. “New report exposes horror of working conditions for millions of sanitation workers in the developing world,” World Health Organization. 2019 Nov 14.
8. Grant B. Origins of Dysentery. The Scientist. Published online March 22, 2016.
Mark Lesney is the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has served as an adjunct assistant professor of the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
Diseases of the American Civil War, Part I
Diseases of the American Civil War, Part I
If cleanliness is next to godliness, then the average soldier in the American Civil War lived just down the street from hell. In a land at war, before the formal tenets of germ theory had spread beyond the confines of Louis Pasteur’s laboratory in France, the lack of basic hygiene, both cultural and situational, coupled to an almost complete lack of curative therapies created an appalling death toll. Waterborne diseases in particular spared neither general nor private, and neither doctor nor nurse.
“Of all the adversities that Union and Confederate soldiers confronted, none was more deadly or more prevalent than contaminated water,” according to Jeffrey S. Sartin, MD, in his survey of Civil War diseases.1
The Union Army records list 1,765,000 cases of diarrhea or dysentery with 45,000 deaths and 149,000 cases of typhoid fever with 35,000 deaths. Add to these the 1,316,000 cases of malaria (borne by mosquitoes breeding in the waters) with its 10,000 deaths, and it is easy to see how the battlefield itself took second place in service to the grim reaper. (Overall, there were roughly two deaths from disease for every one from wounds.)
The chief waterborne plague, infectious diarrhea – including bacterial, amoebic, and other parasites – as well as cholera and typhoid, was an all-year-long problem, and, with the typical wry humor of soldiers, these maladies were given popular names, including the “Tennessee trots” and the “Virginia quick-step.”
Unsanitary conditions in the camps were primarily to blame, and this problem of sanitation was obvious to many observers at the time.
Despite a lack of knowledge of germ theory, doctors were fully aware of the relationship of unsanitary conditions to disease, even if they ascribed the link to miasmas or particles of filth.
Hospitals, which were under more strict control than the regular army camps, were meticulous about the placement of latrines and about keeping high standards of cleanliness among the patients, including routine washing. However, this was insufficient for complete protection, because what passed for clean in the absence of the knowledge of bacterial contamination was often totally ineffective. As one Civil War surgeon stated: “We operated in old bloodstained and often pus-stained coats, we used undisinfected instruments from undisinfected plush-lined cases. If a sponge (if they had sponges) or instrument fell on the floor it was washed and squeezed in a basin of water and used as if it was clean.”2
Overall, efforts at what passed for sanitation remained a constant goal and constant struggle in the field.
After the First Battle of Bull Run, Women’s Central Association of Relief President Henry W. Bellows met with Secretary of War Simon Cameron to discuss the abysmal sanitary conditions witnessed by WCAR volunteers. This meeting led to the creation of what would become the U.S. Sanitary Commission, which was approved by President Abraham Lincoln on June 13, 1861.
The U.S. Sanitary Commission served as a means for funneling civilian assistance to the military, with volunteers providing assistance in the organization of military hospitals and camps and aiding in the transportation of the wounded. However, despite these efforts, the setup of army camps and the behavior of the soldiers were not often directed toward proper sanitation. “The principal causes of disease, however, in our camps were the same that we have always to deplore and find it so difficult to remedy, simply because citizens suddenly called to the field cannot comprehend that men in masses require the attention of their officers to enforce certain hygienic conditions without which health cannot be preserved.”3
Breaches of sanitation were common in the confines of the camps, despite regulations designed to protect the soldiers. According to one U.S. Army surgeon of the time: “Especially [needed] was policing of the latrines. The trench is generally too shallow, the daily covering ... with dirt is entirely neglected. Large numbers of the men will not use the sinks [latrines], ... but instead every clump of bushes, every fence border in the vicinity.” Another pointed out that, after the Battle of Seven Pines, “the only water was infiltrated with the decaying animal matter of the battlefield.” Commenting on the placement of latrines in one encampment, another surgeon described how “the sink [latrine] is the ground in the vicinity, which slopes down to the stream, from which all water from the camp is obtained.”4
Treatment for diarrhea and dysentery was varied. Opiates were one of the most common treatments for diarrhea, whether in an alcohol solution as laudanum or in pill form, with belladonna being used to treat intestinal cramps, according to Glenna R. Schroeder-Lein in her book “The Encyclopedia of Civil War Medicine.” However, useless or damaging treatments were also prescribed, including the use of calomel (a mercury compound), turpentine, castor oil, and quinine.5
Acute diarrhea and dysentery illnesses occurred in at least 641/1,000 troops per year in the Union army. And even though the death rate was comparatively low (20/1,000 cases), it frequently led to chronic diarrhea, which was responsible for 288 deaths per 1,000 cases, and was the third highest cause of medical discharge after gunshot wounds and tuberculosis, according to Ms. Schroeder-Lein.
Although the American Civil War was the last major conflict before the spread of the knowledge of germ theory, the struggle to prevent the spread of waterborne diseases under wartime conditions remains ongoing. Hygiene is difficult under conditions of abject poverty and especially under conditions of armed conflict, and until the era of curative antibiotics there was no recourse.
Antibiotics are not the final solution for antibiotic resistance in intestinal disease pathogens, as outlined in a recent CDC report, is an increasing problem.6 For example, nontyphoidal Salmonella causes an estimated 1.35 million infections, 26,500 hospitalizations, and 420 deaths each year in the United States, with 16% of strains being resistant to at least one essential antibiotic. On a global scale, according to the World Health Organization, poor sanitation causes up to 432,000 diarrheal deaths annually and is linked to the transmission of other diseases like cholera, dysentery, typhoid, hepatitis A, and polio.7
With regard to actual epidemics, the world is only a hygienic crisis away from a major outbreak of dysentery (the last occurring between 1969 and 1972, when 20,000 people in Central America died), according to researchers who have detected antibiotic resistance in all but 1% of circulating Shigella dysenteriae strains surveyed since the 1990s. “This bacterium is still in circulation, and could be responsible for future epidemics if conditions should prove favorable – such as a large gathering of people without access to drinking water or treatment of human waste,” wrote François-Xavier Weill of the Pasteur Institute’s Enteric Bacterial Pathogens Unit.8
References
1. Sartin JS. Clin Infec Dis. 1993;16:580-4. (Correction published in 2002).
2. Civil War Battlefield Surgery. eHistory. The Ohio State University.
3. “Myths About Antiseptics and Camp Life – George Wunderlich,” published online Oct. 11, 2011. http://civilwarscholars.com/2011/10/myths-about-antiseptics-and-camp-life-george-wunderlich/
4. Dorwart BB. “Death is in the Breeze: Disease during the American Civil War” (The National Museum of the American Civil War Press, 2009).
5. Glenna R, Schroeder-Lein GR. “The Encyclopedia of Civil War Medicine” (New York: M. E. Sharpe, 2008).
6. “Antibiotic resistance threats in the United States 2019” Centers for Disease Control and Prevention.
7. “New report exposes horror of working conditions for millions of sanitation workers in the developing world,” World Health Organization. 2019 Nov 14.
8. Grant B. Origins of Dysentery. The Scientist. Published online March 22, 2016.
Mark Lesney is the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has served as an adjunct assistant professor of the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
If cleanliness is next to godliness, then the average soldier in the American Civil War lived just down the street from hell. In a land at war, before the formal tenets of germ theory had spread beyond the confines of Louis Pasteur’s laboratory in France, the lack of basic hygiene, both cultural and situational, coupled to an almost complete lack of curative therapies created an appalling death toll. Waterborne diseases in particular spared neither general nor private, and neither doctor nor nurse.
“Of all the adversities that Union and Confederate soldiers confronted, none was more deadly or more prevalent than contaminated water,” according to Jeffrey S. Sartin, MD, in his survey of Civil War diseases.1
The Union Army records list 1,765,000 cases of diarrhea or dysentery with 45,000 deaths and 149,000 cases of typhoid fever with 35,000 deaths. Add to these the 1,316,000 cases of malaria (borne by mosquitoes breeding in the waters) with its 10,000 deaths, and it is easy to see how the battlefield itself took second place in service to the grim reaper. (Overall, there were roughly two deaths from disease for every one from wounds.)
The chief waterborne plague, infectious diarrhea – including bacterial, amoebic, and other parasites – as well as cholera and typhoid, was an all-year-long problem, and, with the typical wry humor of soldiers, these maladies were given popular names, including the “Tennessee trots” and the “Virginia quick-step.”
Unsanitary conditions in the camps were primarily to blame, and this problem of sanitation was obvious to many observers at the time.
Despite a lack of knowledge of germ theory, doctors were fully aware of the relationship of unsanitary conditions to disease, even if they ascribed the link to miasmas or particles of filth.
Hospitals, which were under more strict control than the regular army camps, were meticulous about the placement of latrines and about keeping high standards of cleanliness among the patients, including routine washing. However, this was insufficient for complete protection, because what passed for clean in the absence of the knowledge of bacterial contamination was often totally ineffective. As one Civil War surgeon stated: “We operated in old bloodstained and often pus-stained coats, we used undisinfected instruments from undisinfected plush-lined cases. If a sponge (if they had sponges) or instrument fell on the floor it was washed and squeezed in a basin of water and used as if it was clean.”2
Overall, efforts at what passed for sanitation remained a constant goal and constant struggle in the field.
After the First Battle of Bull Run, Women’s Central Association of Relief President Henry W. Bellows met with Secretary of War Simon Cameron to discuss the abysmal sanitary conditions witnessed by WCAR volunteers. This meeting led to the creation of what would become the U.S. Sanitary Commission, which was approved by President Abraham Lincoln on June 13, 1861.
The U.S. Sanitary Commission served as a means for funneling civilian assistance to the military, with volunteers providing assistance in the organization of military hospitals and camps and aiding in the transportation of the wounded. However, despite these efforts, the setup of army camps and the behavior of the soldiers were not often directed toward proper sanitation. “The principal causes of disease, however, in our camps were the same that we have always to deplore and find it so difficult to remedy, simply because citizens suddenly called to the field cannot comprehend that men in masses require the attention of their officers to enforce certain hygienic conditions without which health cannot be preserved.”3
Breaches of sanitation were common in the confines of the camps, despite regulations designed to protect the soldiers. According to one U.S. Army surgeon of the time: “Especially [needed] was policing of the latrines. The trench is generally too shallow, the daily covering ... with dirt is entirely neglected. Large numbers of the men will not use the sinks [latrines], ... but instead every clump of bushes, every fence border in the vicinity.” Another pointed out that, after the Battle of Seven Pines, “the only water was infiltrated with the decaying animal matter of the battlefield.” Commenting on the placement of latrines in one encampment, another surgeon described how “the sink [latrine] is the ground in the vicinity, which slopes down to the stream, from which all water from the camp is obtained.”4
Treatment for diarrhea and dysentery was varied. Opiates were one of the most common treatments for diarrhea, whether in an alcohol solution as laudanum or in pill form, with belladonna being used to treat intestinal cramps, according to Glenna R. Schroeder-Lein in her book “The Encyclopedia of Civil War Medicine.” However, useless or damaging treatments were also prescribed, including the use of calomel (a mercury compound), turpentine, castor oil, and quinine.5
Acute diarrhea and dysentery illnesses occurred in at least 641/1,000 troops per year in the Union army. And even though the death rate was comparatively low (20/1,000 cases), it frequently led to chronic diarrhea, which was responsible for 288 deaths per 1,000 cases, and was the third highest cause of medical discharge after gunshot wounds and tuberculosis, according to Ms. Schroeder-Lein.
Although the American Civil War was the last major conflict before the spread of the knowledge of germ theory, the struggle to prevent the spread of waterborne diseases under wartime conditions remains ongoing. Hygiene is difficult under conditions of abject poverty and especially under conditions of armed conflict, and until the era of curative antibiotics there was no recourse.
Antibiotics are not the final solution for antibiotic resistance in intestinal disease pathogens, as outlined in a recent CDC report, is an increasing problem.6 For example, nontyphoidal Salmonella causes an estimated 1.35 million infections, 26,500 hospitalizations, and 420 deaths each year in the United States, with 16% of strains being resistant to at least one essential antibiotic. On a global scale, according to the World Health Organization, poor sanitation causes up to 432,000 diarrheal deaths annually and is linked to the transmission of other diseases like cholera, dysentery, typhoid, hepatitis A, and polio.7
With regard to actual epidemics, the world is only a hygienic crisis away from a major outbreak of dysentery (the last occurring between 1969 and 1972, when 20,000 people in Central America died), according to researchers who have detected antibiotic resistance in all but 1% of circulating Shigella dysenteriae strains surveyed since the 1990s. “This bacterium is still in circulation, and could be responsible for future epidemics if conditions should prove favorable – such as a large gathering of people without access to drinking water or treatment of human waste,” wrote François-Xavier Weill of the Pasteur Institute’s Enteric Bacterial Pathogens Unit.8
References
1. Sartin JS. Clin Infec Dis. 1993;16:580-4. (Correction published in 2002).
2. Civil War Battlefield Surgery. eHistory. The Ohio State University.
3. “Myths About Antiseptics and Camp Life – George Wunderlich,” published online Oct. 11, 2011. http://civilwarscholars.com/2011/10/myths-about-antiseptics-and-camp-life-george-wunderlich/
4. Dorwart BB. “Death is in the Breeze: Disease during the American Civil War” (The National Museum of the American Civil War Press, 2009).
5. Glenna R, Schroeder-Lein GR. “The Encyclopedia of Civil War Medicine” (New York: M. E. Sharpe, 2008).
6. “Antibiotic resistance threats in the United States 2019” Centers for Disease Control and Prevention.
7. “New report exposes horror of working conditions for millions of sanitation workers in the developing world,” World Health Organization. 2019 Nov 14.
8. Grant B. Origins of Dysentery. The Scientist. Published online March 22, 2016.
Mark Lesney is the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has served as an adjunct assistant professor of the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.