User login
Psychiatric conditions affect 1 in 5 children,1,2 and having a comorbid psychiatric condition is associated with worse outcomes in children hospitalized for medical or surgical indications.3-7 Although little is known about interventions for improving outcomes for hospitalized children with psychiatric conditions,8 several interventions that integrate medical and psychiatric care are known to improve ambulatory patient outcomes.9-14 The success of initiatives that test whether integrated medical and psychiatric care models can improve pediatric hospital outcomes depends on reliable identification of comorbid psychiatric conditions and family and clinician having a shared understanding of a patient’s psychiatric diagnoses.
Mental health care system fragmentation, stigma, and privacy issues15-20 may contribute to clinical teams and families having disparate views of psychiatric comorbidities. Evidence suggests that hospital clinicians caring for pediatric medical and surgical inpatients are often unaware of a psychiatric condition that has been diagnosed or managed in the ambulatory setting,3,6 even in cases in which the patient and family are aware of the diagnosis. Conversely, for other patients, clinicians may be aware of a psychiatric diagnosis, but patient and family may not share that understanding or reliably report a psychiatric diagnosis.21-23 Although hospitalization may not be the ideal setting for identifying a new psychiatric diagnosis, given the short-term relationship between patient and clinical care team, addressing and managing a psychiatric comorbidity that is known to family or clinician are important elements of patient-centered hospital care.
The success of interventions in improving hospital outcomes for hospitalized children with psychiatric comorbidity depends on patients, families, and clinicians having a shared understanding of which patients have psychiatric conditions, and on accurate estimates of the scope of the population in need of psychiatric care during pediatric hospitalization.
We conducted a study to compare estimates of point prevalence of psychiatric comorbidity identified by family report (FR) or clinician documentation (CD) and to determine the degree of FR–CD agreement regarding the presence of psychiatric comorbidity in hospitalized children.
METHODS
We estimated point prevalence and determined FR–CD agreement regarding diagnosed psychiatric comorbidities in a cross-sectional sample of pediatric medical and surgical hospitalizations at Children’s Hospital of Philadelphia (CHOP). CHOP is a free-standing 535-bed children’s hospital that serves as a community hospital for the city of Philadelphia; a regional referral center for eastern Pennsylvania, Delaware, and southern New Jersey; and a national and international quaternary referral center. This study was approved by CHOP’s institutional review board.
Patients eligible for inclusion in the study were 4 to 21 years old and hospitalized for a medical or surgical indication. Patients were ineligible if they were hospitalized for a primary psychiatric indication, were medically unstable (eg, received end-of-life care or escalating interventions for a life-threatening condition), had significant cognitive impairment precluding communication (eg, history of severe hypoxic-ischemic encephalopathy), or did not speak English (pertains to consenting parent, guardian, or patient).
The cross-sectional patient sample was selected using a point prevalence recruitment strategy. All eligible patients on each of CHOP’s 20 inpatient medical, surgical, and critical care units were approached for study participation on 2 dates between July 2015 and March 2016. To avoid enrolling the same patient multiple times for a single hospitalization, we separated recruitment dates on each unit by at least 3 months. A goal sample size of 100 to 150 patients was selected to provide precision sufficient to achieve a confidence interval (CI) of 10% around an estimate of the point prevalence of any mental health condition.
To obtain family report of prior psychiatric diagnoses, we interviewed patients and/or their parents during the hospitalization. For 18- to 21-year-old patients, the adolescent patient completed the interview. For patients under 18 years old, parents completed the interview, and for 14- to 17-year-old adolescents,either the parent, the patient, or both could complete the interview. Adolescents were asked to complete the interview confidentially without a parent present. The structured interview included questions derived from the National Survey of Children’s Health24 and the Services Assessment for Children and Adolescents22 to report the patient’s active psychiatric conditions. Interviewees reported whether the patient had ever been diagnosed with any psychiatric disorder, whether the condition was ongoing in the year prior to hospitalization, and whether the patient received any mental health services in clinical settings or school in the 12 months prior to hospitalization.
For CD, we identified a psychiatric diagnosis associated with the index hospitalization if a psychiatric diagnosis was noted in the patient’s admission note, discharge summary, or hospital problem list, or if an International Classification of Diseases (ICD) code for a psychiatric diagnosis was submitted for billing for the index hospitalization. The Healthcare Cost and Utilization Project condition classification system was used to sort psychiatric condition codes25-27 into 5 categories: attention-deficit/hyperactivity disorder (ADHD), anxiety disorders, depression, disruptive behavior disorders, and autism spectrum disorders. A residual category of other, less common psychiatric conditions included eating disorders, attachment disorders, and bipolar disorder.
For each condition category, we determined the point prevalence of having a psychiatric diagnosis identified by FR and having a diagnosis identified by CD. We used McNemar tests to compare point prevalence estimates, the Clopper-Pearson method to calculate CIs around the estimates,28 and Cohen κ statistics to estimate FR–CD agreement regarding psychiatric diagnoses, grouping patients by type of psychiatric diagnosis and by clinical and demographic characteristics. All statistical tests were 2-sided, and P < 0.05 was used for statistical significance. All statistical analyses were performed with Stata Version 13.1 (StataCorp, College Station, Texas).
RESULTS
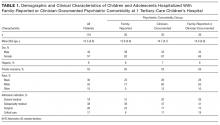
Of 640 patients hospitalized on study recruitment dates, 411 were ineligible for the study (282 were <4 or >21 years old, 42 were not English speakers, 37 had cognitive impairment, 30 were not medically stable, and 20 were admitted for a primary psychiatric diagnosis). Of the 229 eligible patients, 119 (52%) enrolled. Included patients were 57% female; 9% Hispanic; and 35% black, 55% white, and 15% other race. Forty-eight percent of the enrollees had Medicaid (48%), and 52% had private health insurance. Mean age was 12.3 years. Of enrolled patients, 38% were admitted to subspecialty medical services. Enrollee demographics were representative of hospital-level demographics for the study-eligible population; there were no significant differences in age, sex, race, ethnicity, payer type, or hospital service admission type between enrollees and patients who declined to participate (all Ps > 0.05). Table 1 lists demographic and clinical characteristics of the complete study sample and of the groups with FR- or CD-identified psychiatric diagnosis.
Of 119 enrollees, 26 (22%; 95% CI, 15%-30%) had at least 1 FR-identified comorbid psychiatric diagnosis, and 30 (25%; 95% CI, 17%-33%) had at least 1 CD-identified diagnosis. In 13 cases, adolescents (age, 14-17 years) and their parents both completed the structured interview; there were no discrepancies between interview results.
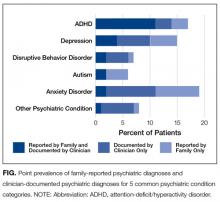
In total, 39 of 119 patients (33%, 95% CI: 24-42%) had either a family-reported or clinician-documented psychiatric diagnosis at the time of hospitalization. For 17 of 119 patients (14%; 95% CI: 9-22%), family-report and clinician-documentation both identified the patient as having a comorbid psychiatric diagnosis. For 9 of 119 patients (8%; 95% CI: 4-14%) families reported a psychiatric diagnosis, but clinicians did not document one. Conversely, for another 13 of 119 patients (11%; 95% CI: 6-18%), a clinician documented a psychiatric diagnosis but the family did not report one. The Figure shows the point prevalence of family-reported psychiatric diagnoses and clinician-documented psychiatric diagnoses for 5 common psychiatric condition categories.
The most common psychiatric conditions reported by families or documented by clinicians were ADHD (n=16, 13%),
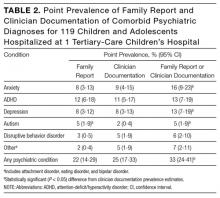
Although point prevalence estimates were similar for FR- and CD-identified comorbid psychiatric conditions, FR–CD agreement was modest. It was fair for any psychiatric diagnosis (κ = .49; 95% CI, .30-.67), highest for ADHD (κ = .79; 95% CI, .61-.96), and fair or poor for other psychiatric conditions (κ range, .11-.48). Table 3 lists the FR–CD agreement data for psychiatric diagnoses for hospitalized children and adolescents.
We compared the distribution of FR and CD psychiatric diagnoses with FR use of mental health services. Of the 119 patients, 47 (39%; 95% CI, 31%-49%) had used mental health services within the year before hospitalization. Of these 47 patients, 15 (32%; 95% CI, 19%-47%) had a psychiatric diagnosis identified by both FR and CD, 6 (13%; 95% CI, 5%-26%) had a diagnosis identified only by FR, 8 (17%; 95% CI, 8%-30%) had a diagnosis identified only by CD, and 18 (38%; 95% CI, 25%-54%) had no FR- or CD-identified diagnosis. For 5 (38%; 95% CI, 14%-68%) of the 13 patients with a CD-only diagnosis, the family reported no use of mental health services within the year before hospitalization.
DISCUSSION
At a tertiary-care children’s hospital, we found high point prevalence of comorbid psychiatric conditions and low agreement between FR- and CD-identified psychiatric conditions. Estimates of the prevalence of psychiatric comorbidity among pediatric medical and surgical inpatients were similar for FR- and CD-identified psychiatric conditions, though each method missed about one third of the cases identified by the other method. FR only and CD only each identified about 1 in 4 or 5 hospitalized children and adolescents with a psychiatric comorbidity. When FR and CD were combined, a comorbid psychiatric diagnosis was identified in about 1 in 3 medical and surgical inpatients aged 4 to 21 years. FR–CD agreement was substantial only for ADHD and was fair to slight for most other psychiatric conditions, including autism, depression, anxiety, and disruptive behavior disorders (eg, conduct disorder, oppositional defiant disorder).
Our finding that psychiatric conditions were more commonly reported by families and documented by clinicians for white patients is consistent with a large body of evidence showing that racial or ethnic minority patients experience more stigma related to mental health diagnoses and use mental health services less.29-33 Families were more likely to report use of mental health services than a known mental health diagnosis. This finding may reflect families’ willingness to use services even if they do not understand or experience stigma related to psychiatric diagnoses. Alternatively, use of mental health services without a diagnosis may reflect clinicians’ willingness to refer a child for services when the child is perceived to have an impairment even in the absence of a clear psychiatric diagnosis.
The low FR–CD agreement regarding psychiatric conditions in hospitalized children and adolescents raises 3 issues for pediatric hospital care. First, earlier studies likely underestimated the prevalence of these conditions. A 2014 study of a national sample found that 13% of children hospitalized for a physical health condition had psychiatric comorbidity.25 That study and other large-scale studies showing a high and increasing prevalence of primary psychiatric conditions in hospitalized children and adolescents have relied on administrative data derived from clinician-documented diagnoses.25-27 Our study findings suggest that reliance on administrative data could result in underestimation of the prevalence of psychiatric comorbidity in hospitalized children by as much as 40%. Pediatric hospitals are reporting a shortage of pediatric mental health specialists.34 Augmenting estimates of the prevalence of psychiatric comorbidity in hospitalized children with reports from other sources, including families or outpatient administrative records, may aid health systems in allocating mental health resources for pediatric inpatients.
The second issue is that the present data suggest that families and clinicians do not share the same information about a child’s psychiatric diagnoses when the child is hospitalized for a medical condition or surgical procedure. Low FR–CD agreement regarding psychiatric diagnoses suggests families and clinical teams are not always “on the same page” about psychiatric needs during hospitalization. Implications of this finding are relevant to inpatient and ambulatory care settings. In cases in which a clinician recognizes a psychiatric condition but the family does not, the family may not seek outpatient treatment. In the present study, one third of patients with a psychiatric diagnosis identified by CD but not FR were not engaged in ambulatory treatment for the condition. Conversely, a psychiatric diagnosis identified by FR but not CD suggests clinical teams lack the skills and knowledge needed to elicit information about psychiatric conditions and their potential relevance to inpatient care. As a result, clinicians may miss opportunities to provide interventions that may improve physical or mental health outcomes. For example, clinical teams with information about a patient’s anxiety disorder may be better able to provide brief interventions to prevent medical treatments from triggering anxiety symptoms and to mitigate the risk for traumatic stress symptoms related to the hospitalization.
The third issue is that anxiety disorders were most likely to be the subject of FR–CD disagreement. This finding identifies children with anxiety disorders as a priority population for research into differences between families and clinicians in understanding patients’ psychiatric diagnoses. Our findings suggest families and clinicians have different views of patients’ anxiety symptoms. Anxiety disorders are a risk factor for worse outcomes in children with chronic physical conditions,3,35-37 and acute hospitalization is associated with posthospital anxiety symptoms.38,39 Thus, anxiety disorders are particularly relevant to hospital care and are a priority for research on the differences between families’ and clinicians’ perspectives on children’s psychiatric diagnoses.
Our findings should be interpreted in the context of study limitations. First, because of resource limitations, we did not obtain psychiatric diagnostic evaluations or records to confirm FR- and CD-identified psychiatric diagnoses. Although this lack of clinical confirmation could have resulted in misclassification bias, the risk of bias was no higher than in many other studies that have successfully used hospital records21,25 and family reports to identify psychiatric comorbidity.40 Second, because the study included only English-speaking patients and families, results cannot be generalized to non-English-speaking populations. Third, this was a single-center study, conducted in a free-standing tertiary-care children’s hospital. Sample size was small, particularly for estimating the prevalence of individual psychiatric conditions. Patient characteristics and clinical practice patterns may differ at other types of hospitals. Larger multicenter studies are warranted. Despite these limitations, our results provide important new information that can further our understanding of the epidemiology of psychiatric conditions in hospitalized children. This information should interest clinical teams caring for children with comorbid physical and mental health conditions.
CONCLUSIONS
Low FR–CD agreement regarding hospitalized children’s psychiatric comorbidities suggests that patients and their families and clinicians do not always share the same information about these comorbidities, and that the prevalence of psychiatric comorbidity in hospitalized children is likely underestimated. To allocate adequate resources for these children, health systems may need to obtain information from multiple sources. Furthermore, we need to better our understanding of strategies for communicating about hospitalized children’s psychiatric conditions so that we can develop interventions to improve hospital outcomes for this vulnerable population.
Disclosures
The direct costs of this project were funded by an internal pilot grant from the Center for Pediatric Health Disparities at Children’s Hospital of Philadelphia. Dr. Doupnik was supported by Ruth L. Kirschstein National Research Service Award T32-HP010026-11, funded by the National Institutes of Health. The sponsors had no role in study design; collection, analysis, or interpretation of data; manuscript writing; or deciding to submit this article for publication.
1. Perou R, Bitsko RH, Blumberg SJ, et al; Centers for Disease Control and Prevention (CDC). Mental health surveillance among children—United States, 2005-2011. MMWR Suppl. 2013;62(2):1-35. PubMed
2. Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci. 2009;11(1):7-20. PubMed
3. Doupnik SK, Mitra N, Feudtner C, Marcus SC. The influence of comorbid mood and anxiety disorders on outcomes of pediatric patients hospitalized for pneumonia. Hosp Pediatr. 2016;6(3):135-142. PubMed
4. Snell C, Fernandes S, Bujoreanu IS, Garcia G. Depression, illness severity, and healthcare utilization in cystic fibrosis. Pediatr Pulmonol. 2014;49(12):1177-1181. PubMed
5. Garrison MM, Katon WJ, Richardson LP. The impact of psychiatric comorbidities on readmissions for diabetes in youth. Diabetes Care. 2005;28(9):2150-2154. PubMed
6. Myrvik MP, Campbell AD, Davis MM, Butcher JL. Impact of psychiatric diagnoses on hospital length of stay in children with sickle cell anemia. Pediatr Blood Cancer. 2012;58(2):239-243. PubMed
7. Myrvik MP, Burks LM, Hoffman RG, Dasgupta M, Panepinto JA. Mental health disorders influence admission rates for pain in children with sickle cell disease. Pediatr Blood Cancer. 2013;60(7):1211-1214. PubMed
8. Bujoreanu S, White MT, Gerber B, Ibeziako P. Effect of timing of psychiatry consultation on length of pediatric hospitalization and hospital charges. Hosp Pediatr. 2015;5(5):269-275. PubMed
9. Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525. PubMed
10. Aupont O, Doerfler L, Connor DF, Stille C, Tisminetzky M, McLaughlin TJ. A collaborative care model to improve access to pediatric mental health services. Adm Policy Ment Health. 2013;40(4):264-273. PubMed
11. Kolko DJ, Campo J, Kilbourne AM, Hart J, Sakolsky D, Wisniewski S. Collaborative care outcomes for pediatric behavioral health problems: a cluster randomized trial. Pediatrics. 2014;133(4):e981-e992. PubMed
12. Richardson L, McCauley E, Katon W. Collaborative care for adolescent depression: a pilot study. Gen Hosp Psychiatry. 2009;31(1):36-45. PubMed
13. Richardson LP, Ludman E, McCauley E, et al. Collaborative care for adolescents with depression in primary care: a randomized clinical trial. JAMA. 2014;312(8):809-816. PubMed
14. Huffman JC, Mastromauro CA, Beach SR, et al. Collaborative care for depression and anxiety disorders in patients with recent cardiac events: the Management of Sadness and Anxiety in Cardiology (MOSAIC) randomized clinical trial. JAMA Intern Med. 2014;174(6):927-935. PubMed
15. Henderson C, Noblett J, Parke H, et al. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry. 2014;1(6):467-482. PubMed
16. Pescosolido BA, Perry BL, Martin JK, McLeod JD, Jensen PS. Stigmatizing attitudes and beliefs about treatment and psychiatric medications for children with mental illness. Psychiatr Serv. 2007;58(5):613-618. PubMed
17. Pescosolido BA. Culture, children, and mental health treatment: special section on the National Stigma Study–Children. Psychiatr Serv. 2007;58(5):611-612. PubMed
18. Britt TW, Greene-Shortridge TM, Brink S, et al. Perceived stigma and barriers to care for psychological treatment: implications for reactions to stressors in different contexts. J Soc Clin Psychol. 2008;27(4):317-335.
19. Thornicroft G, Mehta N, Clement S, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. 2016;387(10023):1123-1132. PubMed
20. Health Insurance Portability and Accountability Act of 1996. Washington, DC: US Government Publishing Office; 1996. https://www.gpo.gov/fdsys/pkg/CRPT-104hrpt736/pdf/CRPT-104hrpt736.pdf. Accessed January 21, 2017.
21. Frayne SM, Miller DR, Sharkansky EJ, et al. Using administrative data to identify mental illness: what approach is best? Am J Med Qual. 2010;25(1):42-50. PubMed
22. Horwitz SM, Hoagwood K, Stiffman AR, et al. Reliability of the Services Assessment for Children and Adolescents. Psychiatr Serv. 2001;52(8):1088-1094. PubMed
23. Ascher BH, Farmer EM, Burns BJ, Angold A. The Child and Adolescent Services Assessment (CASA): description and psychometrics. J Emot Behav Disord. 1996;4(1):12-20.
24. Data Resource Center for Child & Adolescent Health, Child and Adolescent Health Measurement Initiative, Oregon Health & Science University. National Survey of Children’s Health (NSCH), 2011/12. http://childhealthdata.org/docs/drc/2011-12-guide-to-topics-questions-draft.pdf?sfvrsn=4. Accessed January 21, 2017.
25. Bardach NS, Coker TR, Zima BT, et al. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014;133(4):602-609. PubMed
26. Torio CM, Encinosa W, Berdahl T, McCormick MC, Simpson LA. Annual report on health care for children and youth in the United States: national estimates of cost, utilization and expenditures for children with mental health conditions. Acad Pediatr. 2015;15(1):19-35. PubMed
27. Zima BT, Rodean J, Hall M, Bardach NS, Coker TR, Berry JG. Ten year national trends in pediatric hospitalizations by psychiatric complexity. Abstract presented at: 62nd Annual Meeting of the American Academy of Child and Adolescent Psychiatry; October 2015; San Antonio, TX.
28. Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26:404-413.
29. Wu CH, Erickson SR, Piette JD, Balkrishnan R. Mental health resource utilization and health care costs associated with race and comorbid anxiety among Medicaid enrollees with major depressive disorder. J Nat Med Assoc. 2012;104(1-2):78-88. PubMed
30. Mapelli E, Black T, Doan Q. Trends in pediatric emergency department utilization for mental health-related visits. J Pediatr. 2015;167(4):905-910. PubMed
31. Berdahl T, Owens PL, Dougherty D, McCormick MC, Pylypchuk Y, Simpson LA. Annual report on health care for children and youth in the United States: racial/ethnic and socioeconomic disparities in children’s health care quality. Acad Pediatr. 2010;10(2):95-118. PubMed
32. Flores G; Committee on Pediatric Research. Technical report—racial and ethnic disparities in the health and health care of children. Pediatrics. 2010;125(4):e979-e1020. PubMed
33. Turner EA, Jensen-Doss A, Heffer RW. Ethnicity as a moderator of how parents’ attitudes and perceived stigma influence intentions to seek child mental health services. Cultur Divers Ethnic Minor Psychol. 2015;21(4):613-618. PubMed
34. Shaw RJ, Wamboldt M, Bursch B, Stuber M. Practice patterns in pediatric consultation-liaison psychiatry: a national survey. Psychosomatics. 2006;47(1):43-49. PubMed
35. Benton TD, Ifeagwu JA, Smith-Whitley K. Anxiety and depression in children and adolescents with sickle cell disease. Curr Psychiatry Rep. 2007;9(2):114-121. PubMed
36. Chavira DA, Garland AF, Daley S, Hough R. The impact of medical comorbidity on mental health and functional health outcomes among children with anxiety disorders. J Dev Behav Pediatr. 2008;29(5):394-402. PubMed
37. Knight A, Weiss P, Morales K, et al. Depression and anxiety and their association with healthcare utilization in pediatric lupus and mixed connective tissue disease patients: a cross-sectional study. Pediatr Rheumatol Online J. 2014;12:42. PubMed
38. Marsac ML, Kassam-Adams N, Delahanty DL, F. Widaman K, Barakat LP. Posttraumatic stress following acute medical trauma in children: a proposed model of bio-psycho-social processes during the peri-trauma period. Clin Child Fam Psychol Rev. 2014;17(4):399-411. PubMed
39. Marsac ML, Hildenbrand AK, Kohser KL, Winston FK, Li Y, Kassam-Adams N. Preventing posttraumatic stress following pediatric injury: a randomized controlled trial of a web-based psycho-educational intervention for parents. J Pediatr Psychol. 2013;38(10):1101-1111. PubMed
40. Petersen MC, Kube DA, Whitaker TM, Graff JC, Palmer FB. Prevalence of developmental and behavioral disorders in a pediatric hospital. Pediatrics. 2009;123(3):e490-e495. PubMed
Psychiatric conditions affect 1 in 5 children,1,2 and having a comorbid psychiatric condition is associated with worse outcomes in children hospitalized for medical or surgical indications.3-7 Although little is known about interventions for improving outcomes for hospitalized children with psychiatric conditions,8 several interventions that integrate medical and psychiatric care are known to improve ambulatory patient outcomes.9-14 The success of initiatives that test whether integrated medical and psychiatric care models can improve pediatric hospital outcomes depends on reliable identification of comorbid psychiatric conditions and family and clinician having a shared understanding of a patient’s psychiatric diagnoses.
Mental health care system fragmentation, stigma, and privacy issues15-20 may contribute to clinical teams and families having disparate views of psychiatric comorbidities. Evidence suggests that hospital clinicians caring for pediatric medical and surgical inpatients are often unaware of a psychiatric condition that has been diagnosed or managed in the ambulatory setting,3,6 even in cases in which the patient and family are aware of the diagnosis. Conversely, for other patients, clinicians may be aware of a psychiatric diagnosis, but patient and family may not share that understanding or reliably report a psychiatric diagnosis.21-23 Although hospitalization may not be the ideal setting for identifying a new psychiatric diagnosis, given the short-term relationship between patient and clinical care team, addressing and managing a psychiatric comorbidity that is known to family or clinician are important elements of patient-centered hospital care.
The success of interventions in improving hospital outcomes for hospitalized children with psychiatric comorbidity depends on patients, families, and clinicians having a shared understanding of which patients have psychiatric conditions, and on accurate estimates of the scope of the population in need of psychiatric care during pediatric hospitalization.
We conducted a study to compare estimates of point prevalence of psychiatric comorbidity identified by family report (FR) or clinician documentation (CD) and to determine the degree of FR–CD agreement regarding the presence of psychiatric comorbidity in hospitalized children.
METHODS
We estimated point prevalence and determined FR–CD agreement regarding diagnosed psychiatric comorbidities in a cross-sectional sample of pediatric medical and surgical hospitalizations at Children’s Hospital of Philadelphia (CHOP). CHOP is a free-standing 535-bed children’s hospital that serves as a community hospital for the city of Philadelphia; a regional referral center for eastern Pennsylvania, Delaware, and southern New Jersey; and a national and international quaternary referral center. This study was approved by CHOP’s institutional review board.
Patients eligible for inclusion in the study were 4 to 21 years old and hospitalized for a medical or surgical indication. Patients were ineligible if they were hospitalized for a primary psychiatric indication, were medically unstable (eg, received end-of-life care or escalating interventions for a life-threatening condition), had significant cognitive impairment precluding communication (eg, history of severe hypoxic-ischemic encephalopathy), or did not speak English (pertains to consenting parent, guardian, or patient).
The cross-sectional patient sample was selected using a point prevalence recruitment strategy. All eligible patients on each of CHOP’s 20 inpatient medical, surgical, and critical care units were approached for study participation on 2 dates between July 2015 and March 2016. To avoid enrolling the same patient multiple times for a single hospitalization, we separated recruitment dates on each unit by at least 3 months. A goal sample size of 100 to 150 patients was selected to provide precision sufficient to achieve a confidence interval (CI) of 10% around an estimate of the point prevalence of any mental health condition.
To obtain family report of prior psychiatric diagnoses, we interviewed patients and/or their parents during the hospitalization. For 18- to 21-year-old patients, the adolescent patient completed the interview. For patients under 18 years old, parents completed the interview, and for 14- to 17-year-old adolescents,either the parent, the patient, or both could complete the interview. Adolescents were asked to complete the interview confidentially without a parent present. The structured interview included questions derived from the National Survey of Children’s Health24 and the Services Assessment for Children and Adolescents22 to report the patient’s active psychiatric conditions. Interviewees reported whether the patient had ever been diagnosed with any psychiatric disorder, whether the condition was ongoing in the year prior to hospitalization, and whether the patient received any mental health services in clinical settings or school in the 12 months prior to hospitalization.
For CD, we identified a psychiatric diagnosis associated with the index hospitalization if a psychiatric diagnosis was noted in the patient’s admission note, discharge summary, or hospital problem list, or if an International Classification of Diseases (ICD) code for a psychiatric diagnosis was submitted for billing for the index hospitalization. The Healthcare Cost and Utilization Project condition classification system was used to sort psychiatric condition codes25-27 into 5 categories: attention-deficit/hyperactivity disorder (ADHD), anxiety disorders, depression, disruptive behavior disorders, and autism spectrum disorders. A residual category of other, less common psychiatric conditions included eating disorders, attachment disorders, and bipolar disorder.
For each condition category, we determined the point prevalence of having a psychiatric diagnosis identified by FR and having a diagnosis identified by CD. We used McNemar tests to compare point prevalence estimates, the Clopper-Pearson method to calculate CIs around the estimates,28 and Cohen κ statistics to estimate FR–CD agreement regarding psychiatric diagnoses, grouping patients by type of psychiatric diagnosis and by clinical and demographic characteristics. All statistical tests were 2-sided, and P < 0.05 was used for statistical significance. All statistical analyses were performed with Stata Version 13.1 (StataCorp, College Station, Texas).
RESULTS
Of 640 patients hospitalized on study recruitment dates, 411 were ineligible for the study (282 were <4 or >21 years old, 42 were not English speakers, 37 had cognitive impairment, 30 were not medically stable, and 20 were admitted for a primary psychiatric diagnosis). Of the 229 eligible patients, 119 (52%) enrolled. Included patients were 57% female; 9% Hispanic; and 35% black, 55% white, and 15% other race. Forty-eight percent of the enrollees had Medicaid (48%), and 52% had private health insurance. Mean age was 12.3 years. Of enrolled patients, 38% were admitted to subspecialty medical services. Enrollee demographics were representative of hospital-level demographics for the study-eligible population; there were no significant differences in age, sex, race, ethnicity, payer type, or hospital service admission type between enrollees and patients who declined to participate (all Ps > 0.05). Table 1 lists demographic and clinical characteristics of the complete study sample and of the groups with FR- or CD-identified psychiatric diagnosis.
Of 119 enrollees, 26 (22%; 95% CI, 15%-30%) had at least 1 FR-identified comorbid psychiatric diagnosis, and 30 (25%; 95% CI, 17%-33%) had at least 1 CD-identified diagnosis. In 13 cases, adolescents (age, 14-17 years) and their parents both completed the structured interview; there were no discrepancies between interview results.
In total, 39 of 119 patients (33%, 95% CI: 24-42%) had either a family-reported or clinician-documented psychiatric diagnosis at the time of hospitalization. For 17 of 119 patients (14%; 95% CI: 9-22%), family-report and clinician-documentation both identified the patient as having a comorbid psychiatric diagnosis. For 9 of 119 patients (8%; 95% CI: 4-14%) families reported a psychiatric diagnosis, but clinicians did not document one. Conversely, for another 13 of 119 patients (11%; 95% CI: 6-18%), a clinician documented a psychiatric diagnosis but the family did not report one. The Figure shows the point prevalence of family-reported psychiatric diagnoses and clinician-documented psychiatric diagnoses for 5 common psychiatric condition categories.
The most common psychiatric conditions reported by families or documented by clinicians were ADHD (n=16, 13%),
Although point prevalence estimates were similar for FR- and CD-identified comorbid psychiatric conditions, FR–CD agreement was modest. It was fair for any psychiatric diagnosis (κ = .49; 95% CI, .30-.67), highest for ADHD (κ = .79; 95% CI, .61-.96), and fair or poor for other psychiatric conditions (κ range, .11-.48). Table 3 lists the FR–CD agreement data for psychiatric diagnoses for hospitalized children and adolescents.
We compared the distribution of FR and CD psychiatric diagnoses with FR use of mental health services. Of the 119 patients, 47 (39%; 95% CI, 31%-49%) had used mental health services within the year before hospitalization. Of these 47 patients, 15 (32%; 95% CI, 19%-47%) had a psychiatric diagnosis identified by both FR and CD, 6 (13%; 95% CI, 5%-26%) had a diagnosis identified only by FR, 8 (17%; 95% CI, 8%-30%) had a diagnosis identified only by CD, and 18 (38%; 95% CI, 25%-54%) had no FR- or CD-identified diagnosis. For 5 (38%; 95% CI, 14%-68%) of the 13 patients with a CD-only diagnosis, the family reported no use of mental health services within the year before hospitalization.
DISCUSSION
At a tertiary-care children’s hospital, we found high point prevalence of comorbid psychiatric conditions and low agreement between FR- and CD-identified psychiatric conditions. Estimates of the prevalence of psychiatric comorbidity among pediatric medical and surgical inpatients were similar for FR- and CD-identified psychiatric conditions, though each method missed about one third of the cases identified by the other method. FR only and CD only each identified about 1 in 4 or 5 hospitalized children and adolescents with a psychiatric comorbidity. When FR and CD were combined, a comorbid psychiatric diagnosis was identified in about 1 in 3 medical and surgical inpatients aged 4 to 21 years. FR–CD agreement was substantial only for ADHD and was fair to slight for most other psychiatric conditions, including autism, depression, anxiety, and disruptive behavior disorders (eg, conduct disorder, oppositional defiant disorder).
Our finding that psychiatric conditions were more commonly reported by families and documented by clinicians for white patients is consistent with a large body of evidence showing that racial or ethnic minority patients experience more stigma related to mental health diagnoses and use mental health services less.29-33 Families were more likely to report use of mental health services than a known mental health diagnosis. This finding may reflect families’ willingness to use services even if they do not understand or experience stigma related to psychiatric diagnoses. Alternatively, use of mental health services without a diagnosis may reflect clinicians’ willingness to refer a child for services when the child is perceived to have an impairment even in the absence of a clear psychiatric diagnosis.
The low FR–CD agreement regarding psychiatric conditions in hospitalized children and adolescents raises 3 issues for pediatric hospital care. First, earlier studies likely underestimated the prevalence of these conditions. A 2014 study of a national sample found that 13% of children hospitalized for a physical health condition had psychiatric comorbidity.25 That study and other large-scale studies showing a high and increasing prevalence of primary psychiatric conditions in hospitalized children and adolescents have relied on administrative data derived from clinician-documented diagnoses.25-27 Our study findings suggest that reliance on administrative data could result in underestimation of the prevalence of psychiatric comorbidity in hospitalized children by as much as 40%. Pediatric hospitals are reporting a shortage of pediatric mental health specialists.34 Augmenting estimates of the prevalence of psychiatric comorbidity in hospitalized children with reports from other sources, including families or outpatient administrative records, may aid health systems in allocating mental health resources for pediatric inpatients.
The second issue is that the present data suggest that families and clinicians do not share the same information about a child’s psychiatric diagnoses when the child is hospitalized for a medical condition or surgical procedure. Low FR–CD agreement regarding psychiatric diagnoses suggests families and clinical teams are not always “on the same page” about psychiatric needs during hospitalization. Implications of this finding are relevant to inpatient and ambulatory care settings. In cases in which a clinician recognizes a psychiatric condition but the family does not, the family may not seek outpatient treatment. In the present study, one third of patients with a psychiatric diagnosis identified by CD but not FR were not engaged in ambulatory treatment for the condition. Conversely, a psychiatric diagnosis identified by FR but not CD suggests clinical teams lack the skills and knowledge needed to elicit information about psychiatric conditions and their potential relevance to inpatient care. As a result, clinicians may miss opportunities to provide interventions that may improve physical or mental health outcomes. For example, clinical teams with information about a patient’s anxiety disorder may be better able to provide brief interventions to prevent medical treatments from triggering anxiety symptoms and to mitigate the risk for traumatic stress symptoms related to the hospitalization.
The third issue is that anxiety disorders were most likely to be the subject of FR–CD disagreement. This finding identifies children with anxiety disorders as a priority population for research into differences between families and clinicians in understanding patients’ psychiatric diagnoses. Our findings suggest families and clinicians have different views of patients’ anxiety symptoms. Anxiety disorders are a risk factor for worse outcomes in children with chronic physical conditions,3,35-37 and acute hospitalization is associated with posthospital anxiety symptoms.38,39 Thus, anxiety disorders are particularly relevant to hospital care and are a priority for research on the differences between families’ and clinicians’ perspectives on children’s psychiatric diagnoses.
Our findings should be interpreted in the context of study limitations. First, because of resource limitations, we did not obtain psychiatric diagnostic evaluations or records to confirm FR- and CD-identified psychiatric diagnoses. Although this lack of clinical confirmation could have resulted in misclassification bias, the risk of bias was no higher than in many other studies that have successfully used hospital records21,25 and family reports to identify psychiatric comorbidity.40 Second, because the study included only English-speaking patients and families, results cannot be generalized to non-English-speaking populations. Third, this was a single-center study, conducted in a free-standing tertiary-care children’s hospital. Sample size was small, particularly for estimating the prevalence of individual psychiatric conditions. Patient characteristics and clinical practice patterns may differ at other types of hospitals. Larger multicenter studies are warranted. Despite these limitations, our results provide important new information that can further our understanding of the epidemiology of psychiatric conditions in hospitalized children. This information should interest clinical teams caring for children with comorbid physical and mental health conditions.
CONCLUSIONS
Low FR–CD agreement regarding hospitalized children’s psychiatric comorbidities suggests that patients and their families and clinicians do not always share the same information about these comorbidities, and that the prevalence of psychiatric comorbidity in hospitalized children is likely underestimated. To allocate adequate resources for these children, health systems may need to obtain information from multiple sources. Furthermore, we need to better our understanding of strategies for communicating about hospitalized children’s psychiatric conditions so that we can develop interventions to improve hospital outcomes for this vulnerable population.
Disclosures
The direct costs of this project were funded by an internal pilot grant from the Center for Pediatric Health Disparities at Children’s Hospital of Philadelphia. Dr. Doupnik was supported by Ruth L. Kirschstein National Research Service Award T32-HP010026-11, funded by the National Institutes of Health. The sponsors had no role in study design; collection, analysis, or interpretation of data; manuscript writing; or deciding to submit this article for publication.
Psychiatric conditions affect 1 in 5 children,1,2 and having a comorbid psychiatric condition is associated with worse outcomes in children hospitalized for medical or surgical indications.3-7 Although little is known about interventions for improving outcomes for hospitalized children with psychiatric conditions,8 several interventions that integrate medical and psychiatric care are known to improve ambulatory patient outcomes.9-14 The success of initiatives that test whether integrated medical and psychiatric care models can improve pediatric hospital outcomes depends on reliable identification of comorbid psychiatric conditions and family and clinician having a shared understanding of a patient’s psychiatric diagnoses.
Mental health care system fragmentation, stigma, and privacy issues15-20 may contribute to clinical teams and families having disparate views of psychiatric comorbidities. Evidence suggests that hospital clinicians caring for pediatric medical and surgical inpatients are often unaware of a psychiatric condition that has been diagnosed or managed in the ambulatory setting,3,6 even in cases in which the patient and family are aware of the diagnosis. Conversely, for other patients, clinicians may be aware of a psychiatric diagnosis, but patient and family may not share that understanding or reliably report a psychiatric diagnosis.21-23 Although hospitalization may not be the ideal setting for identifying a new psychiatric diagnosis, given the short-term relationship between patient and clinical care team, addressing and managing a psychiatric comorbidity that is known to family or clinician are important elements of patient-centered hospital care.
The success of interventions in improving hospital outcomes for hospitalized children with psychiatric comorbidity depends on patients, families, and clinicians having a shared understanding of which patients have psychiatric conditions, and on accurate estimates of the scope of the population in need of psychiatric care during pediatric hospitalization.
We conducted a study to compare estimates of point prevalence of psychiatric comorbidity identified by family report (FR) or clinician documentation (CD) and to determine the degree of FR–CD agreement regarding the presence of psychiatric comorbidity in hospitalized children.
METHODS
We estimated point prevalence and determined FR–CD agreement regarding diagnosed psychiatric comorbidities in a cross-sectional sample of pediatric medical and surgical hospitalizations at Children’s Hospital of Philadelphia (CHOP). CHOP is a free-standing 535-bed children’s hospital that serves as a community hospital for the city of Philadelphia; a regional referral center for eastern Pennsylvania, Delaware, and southern New Jersey; and a national and international quaternary referral center. This study was approved by CHOP’s institutional review board.
Patients eligible for inclusion in the study were 4 to 21 years old and hospitalized for a medical or surgical indication. Patients were ineligible if they were hospitalized for a primary psychiatric indication, were medically unstable (eg, received end-of-life care or escalating interventions for a life-threatening condition), had significant cognitive impairment precluding communication (eg, history of severe hypoxic-ischemic encephalopathy), or did not speak English (pertains to consenting parent, guardian, or patient).
The cross-sectional patient sample was selected using a point prevalence recruitment strategy. All eligible patients on each of CHOP’s 20 inpatient medical, surgical, and critical care units were approached for study participation on 2 dates between July 2015 and March 2016. To avoid enrolling the same patient multiple times for a single hospitalization, we separated recruitment dates on each unit by at least 3 months. A goal sample size of 100 to 150 patients was selected to provide precision sufficient to achieve a confidence interval (CI) of 10% around an estimate of the point prevalence of any mental health condition.
To obtain family report of prior psychiatric diagnoses, we interviewed patients and/or their parents during the hospitalization. For 18- to 21-year-old patients, the adolescent patient completed the interview. For patients under 18 years old, parents completed the interview, and for 14- to 17-year-old adolescents,either the parent, the patient, or both could complete the interview. Adolescents were asked to complete the interview confidentially without a parent present. The structured interview included questions derived from the National Survey of Children’s Health24 and the Services Assessment for Children and Adolescents22 to report the patient’s active psychiatric conditions. Interviewees reported whether the patient had ever been diagnosed with any psychiatric disorder, whether the condition was ongoing in the year prior to hospitalization, and whether the patient received any mental health services in clinical settings or school in the 12 months prior to hospitalization.
For CD, we identified a psychiatric diagnosis associated with the index hospitalization if a psychiatric diagnosis was noted in the patient’s admission note, discharge summary, or hospital problem list, or if an International Classification of Diseases (ICD) code for a psychiatric diagnosis was submitted for billing for the index hospitalization. The Healthcare Cost and Utilization Project condition classification system was used to sort psychiatric condition codes25-27 into 5 categories: attention-deficit/hyperactivity disorder (ADHD), anxiety disorders, depression, disruptive behavior disorders, and autism spectrum disorders. A residual category of other, less common psychiatric conditions included eating disorders, attachment disorders, and bipolar disorder.
For each condition category, we determined the point prevalence of having a psychiatric diagnosis identified by FR and having a diagnosis identified by CD. We used McNemar tests to compare point prevalence estimates, the Clopper-Pearson method to calculate CIs around the estimates,28 and Cohen κ statistics to estimate FR–CD agreement regarding psychiatric diagnoses, grouping patients by type of psychiatric diagnosis and by clinical and demographic characteristics. All statistical tests were 2-sided, and P < 0.05 was used for statistical significance. All statistical analyses were performed with Stata Version 13.1 (StataCorp, College Station, Texas).
RESULTS
Of 640 patients hospitalized on study recruitment dates, 411 were ineligible for the study (282 were <4 or >21 years old, 42 were not English speakers, 37 had cognitive impairment, 30 were not medically stable, and 20 were admitted for a primary psychiatric diagnosis). Of the 229 eligible patients, 119 (52%) enrolled. Included patients were 57% female; 9% Hispanic; and 35% black, 55% white, and 15% other race. Forty-eight percent of the enrollees had Medicaid (48%), and 52% had private health insurance. Mean age was 12.3 years. Of enrolled patients, 38% were admitted to subspecialty medical services. Enrollee demographics were representative of hospital-level demographics for the study-eligible population; there were no significant differences in age, sex, race, ethnicity, payer type, or hospital service admission type between enrollees and patients who declined to participate (all Ps > 0.05). Table 1 lists demographic and clinical characteristics of the complete study sample and of the groups with FR- or CD-identified psychiatric diagnosis.
Of 119 enrollees, 26 (22%; 95% CI, 15%-30%) had at least 1 FR-identified comorbid psychiatric diagnosis, and 30 (25%; 95% CI, 17%-33%) had at least 1 CD-identified diagnosis. In 13 cases, adolescents (age, 14-17 years) and their parents both completed the structured interview; there were no discrepancies between interview results.
In total, 39 of 119 patients (33%, 95% CI: 24-42%) had either a family-reported or clinician-documented psychiatric diagnosis at the time of hospitalization. For 17 of 119 patients (14%; 95% CI: 9-22%), family-report and clinician-documentation both identified the patient as having a comorbid psychiatric diagnosis. For 9 of 119 patients (8%; 95% CI: 4-14%) families reported a psychiatric diagnosis, but clinicians did not document one. Conversely, for another 13 of 119 patients (11%; 95% CI: 6-18%), a clinician documented a psychiatric diagnosis but the family did not report one. The Figure shows the point prevalence of family-reported psychiatric diagnoses and clinician-documented psychiatric diagnoses for 5 common psychiatric condition categories.
The most common psychiatric conditions reported by families or documented by clinicians were ADHD (n=16, 13%),
Although point prevalence estimates were similar for FR- and CD-identified comorbid psychiatric conditions, FR–CD agreement was modest. It was fair for any psychiatric diagnosis (κ = .49; 95% CI, .30-.67), highest for ADHD (κ = .79; 95% CI, .61-.96), and fair or poor for other psychiatric conditions (κ range, .11-.48). Table 3 lists the FR–CD agreement data for psychiatric diagnoses for hospitalized children and adolescents.
We compared the distribution of FR and CD psychiatric diagnoses with FR use of mental health services. Of the 119 patients, 47 (39%; 95% CI, 31%-49%) had used mental health services within the year before hospitalization. Of these 47 patients, 15 (32%; 95% CI, 19%-47%) had a psychiatric diagnosis identified by both FR and CD, 6 (13%; 95% CI, 5%-26%) had a diagnosis identified only by FR, 8 (17%; 95% CI, 8%-30%) had a diagnosis identified only by CD, and 18 (38%; 95% CI, 25%-54%) had no FR- or CD-identified diagnosis. For 5 (38%; 95% CI, 14%-68%) of the 13 patients with a CD-only diagnosis, the family reported no use of mental health services within the year before hospitalization.
DISCUSSION
At a tertiary-care children’s hospital, we found high point prevalence of comorbid psychiatric conditions and low agreement between FR- and CD-identified psychiatric conditions. Estimates of the prevalence of psychiatric comorbidity among pediatric medical and surgical inpatients were similar for FR- and CD-identified psychiatric conditions, though each method missed about one third of the cases identified by the other method. FR only and CD only each identified about 1 in 4 or 5 hospitalized children and adolescents with a psychiatric comorbidity. When FR and CD were combined, a comorbid psychiatric diagnosis was identified in about 1 in 3 medical and surgical inpatients aged 4 to 21 years. FR–CD agreement was substantial only for ADHD and was fair to slight for most other psychiatric conditions, including autism, depression, anxiety, and disruptive behavior disorders (eg, conduct disorder, oppositional defiant disorder).
Our finding that psychiatric conditions were more commonly reported by families and documented by clinicians for white patients is consistent with a large body of evidence showing that racial or ethnic minority patients experience more stigma related to mental health diagnoses and use mental health services less.29-33 Families were more likely to report use of mental health services than a known mental health diagnosis. This finding may reflect families’ willingness to use services even if they do not understand or experience stigma related to psychiatric diagnoses. Alternatively, use of mental health services without a diagnosis may reflect clinicians’ willingness to refer a child for services when the child is perceived to have an impairment even in the absence of a clear psychiatric diagnosis.
The low FR–CD agreement regarding psychiatric conditions in hospitalized children and adolescents raises 3 issues for pediatric hospital care. First, earlier studies likely underestimated the prevalence of these conditions. A 2014 study of a national sample found that 13% of children hospitalized for a physical health condition had psychiatric comorbidity.25 That study and other large-scale studies showing a high and increasing prevalence of primary psychiatric conditions in hospitalized children and adolescents have relied on administrative data derived from clinician-documented diagnoses.25-27 Our study findings suggest that reliance on administrative data could result in underestimation of the prevalence of psychiatric comorbidity in hospitalized children by as much as 40%. Pediatric hospitals are reporting a shortage of pediatric mental health specialists.34 Augmenting estimates of the prevalence of psychiatric comorbidity in hospitalized children with reports from other sources, including families or outpatient administrative records, may aid health systems in allocating mental health resources for pediatric inpatients.
The second issue is that the present data suggest that families and clinicians do not share the same information about a child’s psychiatric diagnoses when the child is hospitalized for a medical condition or surgical procedure. Low FR–CD agreement regarding psychiatric diagnoses suggests families and clinical teams are not always “on the same page” about psychiatric needs during hospitalization. Implications of this finding are relevant to inpatient and ambulatory care settings. In cases in which a clinician recognizes a psychiatric condition but the family does not, the family may not seek outpatient treatment. In the present study, one third of patients with a psychiatric diagnosis identified by CD but not FR were not engaged in ambulatory treatment for the condition. Conversely, a psychiatric diagnosis identified by FR but not CD suggests clinical teams lack the skills and knowledge needed to elicit information about psychiatric conditions and their potential relevance to inpatient care. As a result, clinicians may miss opportunities to provide interventions that may improve physical or mental health outcomes. For example, clinical teams with information about a patient’s anxiety disorder may be better able to provide brief interventions to prevent medical treatments from triggering anxiety symptoms and to mitigate the risk for traumatic stress symptoms related to the hospitalization.
The third issue is that anxiety disorders were most likely to be the subject of FR–CD disagreement. This finding identifies children with anxiety disorders as a priority population for research into differences between families and clinicians in understanding patients’ psychiatric diagnoses. Our findings suggest families and clinicians have different views of patients’ anxiety symptoms. Anxiety disorders are a risk factor for worse outcomes in children with chronic physical conditions,3,35-37 and acute hospitalization is associated with posthospital anxiety symptoms.38,39 Thus, anxiety disorders are particularly relevant to hospital care and are a priority for research on the differences between families’ and clinicians’ perspectives on children’s psychiatric diagnoses.
Our findings should be interpreted in the context of study limitations. First, because of resource limitations, we did not obtain psychiatric diagnostic evaluations or records to confirm FR- and CD-identified psychiatric diagnoses. Although this lack of clinical confirmation could have resulted in misclassification bias, the risk of bias was no higher than in many other studies that have successfully used hospital records21,25 and family reports to identify psychiatric comorbidity.40 Second, because the study included only English-speaking patients and families, results cannot be generalized to non-English-speaking populations. Third, this was a single-center study, conducted in a free-standing tertiary-care children’s hospital. Sample size was small, particularly for estimating the prevalence of individual psychiatric conditions. Patient characteristics and clinical practice patterns may differ at other types of hospitals. Larger multicenter studies are warranted. Despite these limitations, our results provide important new information that can further our understanding of the epidemiology of psychiatric conditions in hospitalized children. This information should interest clinical teams caring for children with comorbid physical and mental health conditions.
CONCLUSIONS
Low FR–CD agreement regarding hospitalized children’s psychiatric comorbidities suggests that patients and their families and clinicians do not always share the same information about these comorbidities, and that the prevalence of psychiatric comorbidity in hospitalized children is likely underestimated. To allocate adequate resources for these children, health systems may need to obtain information from multiple sources. Furthermore, we need to better our understanding of strategies for communicating about hospitalized children’s psychiatric conditions so that we can develop interventions to improve hospital outcomes for this vulnerable population.
Disclosures
The direct costs of this project were funded by an internal pilot grant from the Center for Pediatric Health Disparities at Children’s Hospital of Philadelphia. Dr. Doupnik was supported by Ruth L. Kirschstein National Research Service Award T32-HP010026-11, funded by the National Institutes of Health. The sponsors had no role in study design; collection, analysis, or interpretation of data; manuscript writing; or deciding to submit this article for publication.
1. Perou R, Bitsko RH, Blumberg SJ, et al; Centers for Disease Control and Prevention (CDC). Mental health surveillance among children—United States, 2005-2011. MMWR Suppl. 2013;62(2):1-35. PubMed
2. Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci. 2009;11(1):7-20. PubMed
3. Doupnik SK, Mitra N, Feudtner C, Marcus SC. The influence of comorbid mood and anxiety disorders on outcomes of pediatric patients hospitalized for pneumonia. Hosp Pediatr. 2016;6(3):135-142. PubMed
4. Snell C, Fernandes S, Bujoreanu IS, Garcia G. Depression, illness severity, and healthcare utilization in cystic fibrosis. Pediatr Pulmonol. 2014;49(12):1177-1181. PubMed
5. Garrison MM, Katon WJ, Richardson LP. The impact of psychiatric comorbidities on readmissions for diabetes in youth. Diabetes Care. 2005;28(9):2150-2154. PubMed
6. Myrvik MP, Campbell AD, Davis MM, Butcher JL. Impact of psychiatric diagnoses on hospital length of stay in children with sickle cell anemia. Pediatr Blood Cancer. 2012;58(2):239-243. PubMed
7. Myrvik MP, Burks LM, Hoffman RG, Dasgupta M, Panepinto JA. Mental health disorders influence admission rates for pain in children with sickle cell disease. Pediatr Blood Cancer. 2013;60(7):1211-1214. PubMed
8. Bujoreanu S, White MT, Gerber B, Ibeziako P. Effect of timing of psychiatry consultation on length of pediatric hospitalization and hospital charges. Hosp Pediatr. 2015;5(5):269-275. PubMed
9. Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525. PubMed
10. Aupont O, Doerfler L, Connor DF, Stille C, Tisminetzky M, McLaughlin TJ. A collaborative care model to improve access to pediatric mental health services. Adm Policy Ment Health. 2013;40(4):264-273. PubMed
11. Kolko DJ, Campo J, Kilbourne AM, Hart J, Sakolsky D, Wisniewski S. Collaborative care outcomes for pediatric behavioral health problems: a cluster randomized trial. Pediatrics. 2014;133(4):e981-e992. PubMed
12. Richardson L, McCauley E, Katon W. Collaborative care for adolescent depression: a pilot study. Gen Hosp Psychiatry. 2009;31(1):36-45. PubMed
13. Richardson LP, Ludman E, McCauley E, et al. Collaborative care for adolescents with depression in primary care: a randomized clinical trial. JAMA. 2014;312(8):809-816. PubMed
14. Huffman JC, Mastromauro CA, Beach SR, et al. Collaborative care for depression and anxiety disorders in patients with recent cardiac events: the Management of Sadness and Anxiety in Cardiology (MOSAIC) randomized clinical trial. JAMA Intern Med. 2014;174(6):927-935. PubMed
15. Henderson C, Noblett J, Parke H, et al. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry. 2014;1(6):467-482. PubMed
16. Pescosolido BA, Perry BL, Martin JK, McLeod JD, Jensen PS. Stigmatizing attitudes and beliefs about treatment and psychiatric medications for children with mental illness. Psychiatr Serv. 2007;58(5):613-618. PubMed
17. Pescosolido BA. Culture, children, and mental health treatment: special section on the National Stigma Study–Children. Psychiatr Serv. 2007;58(5):611-612. PubMed
18. Britt TW, Greene-Shortridge TM, Brink S, et al. Perceived stigma and barriers to care for psychological treatment: implications for reactions to stressors in different contexts. J Soc Clin Psychol. 2008;27(4):317-335.
19. Thornicroft G, Mehta N, Clement S, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. 2016;387(10023):1123-1132. PubMed
20. Health Insurance Portability and Accountability Act of 1996. Washington, DC: US Government Publishing Office; 1996. https://www.gpo.gov/fdsys/pkg/CRPT-104hrpt736/pdf/CRPT-104hrpt736.pdf. Accessed January 21, 2017.
21. Frayne SM, Miller DR, Sharkansky EJ, et al. Using administrative data to identify mental illness: what approach is best? Am J Med Qual. 2010;25(1):42-50. PubMed
22. Horwitz SM, Hoagwood K, Stiffman AR, et al. Reliability of the Services Assessment for Children and Adolescents. Psychiatr Serv. 2001;52(8):1088-1094. PubMed
23. Ascher BH, Farmer EM, Burns BJ, Angold A. The Child and Adolescent Services Assessment (CASA): description and psychometrics. J Emot Behav Disord. 1996;4(1):12-20.
24. Data Resource Center for Child & Adolescent Health, Child and Adolescent Health Measurement Initiative, Oregon Health & Science University. National Survey of Children’s Health (NSCH), 2011/12. http://childhealthdata.org/docs/drc/2011-12-guide-to-topics-questions-draft.pdf?sfvrsn=4. Accessed January 21, 2017.
25. Bardach NS, Coker TR, Zima BT, et al. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014;133(4):602-609. PubMed
26. Torio CM, Encinosa W, Berdahl T, McCormick MC, Simpson LA. Annual report on health care for children and youth in the United States: national estimates of cost, utilization and expenditures for children with mental health conditions. Acad Pediatr. 2015;15(1):19-35. PubMed
27. Zima BT, Rodean J, Hall M, Bardach NS, Coker TR, Berry JG. Ten year national trends in pediatric hospitalizations by psychiatric complexity. Abstract presented at: 62nd Annual Meeting of the American Academy of Child and Adolescent Psychiatry; October 2015; San Antonio, TX.
28. Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26:404-413.
29. Wu CH, Erickson SR, Piette JD, Balkrishnan R. Mental health resource utilization and health care costs associated with race and comorbid anxiety among Medicaid enrollees with major depressive disorder. J Nat Med Assoc. 2012;104(1-2):78-88. PubMed
30. Mapelli E, Black T, Doan Q. Trends in pediatric emergency department utilization for mental health-related visits. J Pediatr. 2015;167(4):905-910. PubMed
31. Berdahl T, Owens PL, Dougherty D, McCormick MC, Pylypchuk Y, Simpson LA. Annual report on health care for children and youth in the United States: racial/ethnic and socioeconomic disparities in children’s health care quality. Acad Pediatr. 2010;10(2):95-118. PubMed
32. Flores G; Committee on Pediatric Research. Technical report—racial and ethnic disparities in the health and health care of children. Pediatrics. 2010;125(4):e979-e1020. PubMed
33. Turner EA, Jensen-Doss A, Heffer RW. Ethnicity as a moderator of how parents’ attitudes and perceived stigma influence intentions to seek child mental health services. Cultur Divers Ethnic Minor Psychol. 2015;21(4):613-618. PubMed
34. Shaw RJ, Wamboldt M, Bursch B, Stuber M. Practice patterns in pediatric consultation-liaison psychiatry: a national survey. Psychosomatics. 2006;47(1):43-49. PubMed
35. Benton TD, Ifeagwu JA, Smith-Whitley K. Anxiety and depression in children and adolescents with sickle cell disease. Curr Psychiatry Rep. 2007;9(2):114-121. PubMed
36. Chavira DA, Garland AF, Daley S, Hough R. The impact of medical comorbidity on mental health and functional health outcomes among children with anxiety disorders. J Dev Behav Pediatr. 2008;29(5):394-402. PubMed
37. Knight A, Weiss P, Morales K, et al. Depression and anxiety and their association with healthcare utilization in pediatric lupus and mixed connective tissue disease patients: a cross-sectional study. Pediatr Rheumatol Online J. 2014;12:42. PubMed
38. Marsac ML, Kassam-Adams N, Delahanty DL, F. Widaman K, Barakat LP. Posttraumatic stress following acute medical trauma in children: a proposed model of bio-psycho-social processes during the peri-trauma period. Clin Child Fam Psychol Rev. 2014;17(4):399-411. PubMed
39. Marsac ML, Hildenbrand AK, Kohser KL, Winston FK, Li Y, Kassam-Adams N. Preventing posttraumatic stress following pediatric injury: a randomized controlled trial of a web-based psycho-educational intervention for parents. J Pediatr Psychol. 2013;38(10):1101-1111. PubMed
40. Petersen MC, Kube DA, Whitaker TM, Graff JC, Palmer FB. Prevalence of developmental and behavioral disorders in a pediatric hospital. Pediatrics. 2009;123(3):e490-e495. PubMed
1. Perou R, Bitsko RH, Blumberg SJ, et al; Centers for Disease Control and Prevention (CDC). Mental health surveillance among children—United States, 2005-2011. MMWR Suppl. 2013;62(2):1-35. PubMed
2. Merikangas KR, Nakamura EF, Kessler RC. Epidemiology of mental disorders in children and adolescents. Dialogues Clin Neurosci. 2009;11(1):7-20. PubMed
3. Doupnik SK, Mitra N, Feudtner C, Marcus SC. The influence of comorbid mood and anxiety disorders on outcomes of pediatric patients hospitalized for pneumonia. Hosp Pediatr. 2016;6(3):135-142. PubMed
4. Snell C, Fernandes S, Bujoreanu IS, Garcia G. Depression, illness severity, and healthcare utilization in cystic fibrosis. Pediatr Pulmonol. 2014;49(12):1177-1181. PubMed
5. Garrison MM, Katon WJ, Richardson LP. The impact of psychiatric comorbidities on readmissions for diabetes in youth. Diabetes Care. 2005;28(9):2150-2154. PubMed
6. Myrvik MP, Campbell AD, Davis MM, Butcher JL. Impact of psychiatric diagnoses on hospital length of stay in children with sickle cell anemia. Pediatr Blood Cancer. 2012;58(2):239-243. PubMed
7. Myrvik MP, Burks LM, Hoffman RG, Dasgupta M, Panepinto JA. Mental health disorders influence admission rates for pain in children with sickle cell disease. Pediatr Blood Cancer. 2013;60(7):1211-1214. PubMed
8. Bujoreanu S, White MT, Gerber B, Ibeziako P. Effect of timing of psychiatry consultation on length of pediatric hospitalization and hospital charges. Hosp Pediatr. 2015;5(5):269-275. PubMed
9. Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525. PubMed
10. Aupont O, Doerfler L, Connor DF, Stille C, Tisminetzky M, McLaughlin TJ. A collaborative care model to improve access to pediatric mental health services. Adm Policy Ment Health. 2013;40(4):264-273. PubMed
11. Kolko DJ, Campo J, Kilbourne AM, Hart J, Sakolsky D, Wisniewski S. Collaborative care outcomes for pediatric behavioral health problems: a cluster randomized trial. Pediatrics. 2014;133(4):e981-e992. PubMed
12. Richardson L, McCauley E, Katon W. Collaborative care for adolescent depression: a pilot study. Gen Hosp Psychiatry. 2009;31(1):36-45. PubMed
13. Richardson LP, Ludman E, McCauley E, et al. Collaborative care for adolescents with depression in primary care: a randomized clinical trial. JAMA. 2014;312(8):809-816. PubMed
14. Huffman JC, Mastromauro CA, Beach SR, et al. Collaborative care for depression and anxiety disorders in patients with recent cardiac events: the Management of Sadness and Anxiety in Cardiology (MOSAIC) randomized clinical trial. JAMA Intern Med. 2014;174(6):927-935. PubMed
15. Henderson C, Noblett J, Parke H, et al. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry. 2014;1(6):467-482. PubMed
16. Pescosolido BA, Perry BL, Martin JK, McLeod JD, Jensen PS. Stigmatizing attitudes and beliefs about treatment and psychiatric medications for children with mental illness. Psychiatr Serv. 2007;58(5):613-618. PubMed
17. Pescosolido BA. Culture, children, and mental health treatment: special section on the National Stigma Study–Children. Psychiatr Serv. 2007;58(5):611-612. PubMed
18. Britt TW, Greene-Shortridge TM, Brink S, et al. Perceived stigma and barriers to care for psychological treatment: implications for reactions to stressors in different contexts. J Soc Clin Psychol. 2008;27(4):317-335.
19. Thornicroft G, Mehta N, Clement S, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. 2016;387(10023):1123-1132. PubMed
20. Health Insurance Portability and Accountability Act of 1996. Washington, DC: US Government Publishing Office; 1996. https://www.gpo.gov/fdsys/pkg/CRPT-104hrpt736/pdf/CRPT-104hrpt736.pdf. Accessed January 21, 2017.
21. Frayne SM, Miller DR, Sharkansky EJ, et al. Using administrative data to identify mental illness: what approach is best? Am J Med Qual. 2010;25(1):42-50. PubMed
22. Horwitz SM, Hoagwood K, Stiffman AR, et al. Reliability of the Services Assessment for Children and Adolescents. Psychiatr Serv. 2001;52(8):1088-1094. PubMed
23. Ascher BH, Farmer EM, Burns BJ, Angold A. The Child and Adolescent Services Assessment (CASA): description and psychometrics. J Emot Behav Disord. 1996;4(1):12-20.
24. Data Resource Center for Child & Adolescent Health, Child and Adolescent Health Measurement Initiative, Oregon Health & Science University. National Survey of Children’s Health (NSCH), 2011/12. http://childhealthdata.org/docs/drc/2011-12-guide-to-topics-questions-draft.pdf?sfvrsn=4. Accessed January 21, 2017.
25. Bardach NS, Coker TR, Zima BT, et al. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014;133(4):602-609. PubMed
26. Torio CM, Encinosa W, Berdahl T, McCormick MC, Simpson LA. Annual report on health care for children and youth in the United States: national estimates of cost, utilization and expenditures for children with mental health conditions. Acad Pediatr. 2015;15(1):19-35. PubMed
27. Zima BT, Rodean J, Hall M, Bardach NS, Coker TR, Berry JG. Ten year national trends in pediatric hospitalizations by psychiatric complexity. Abstract presented at: 62nd Annual Meeting of the American Academy of Child and Adolescent Psychiatry; October 2015; San Antonio, TX.
28. Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26:404-413.
29. Wu CH, Erickson SR, Piette JD, Balkrishnan R. Mental health resource utilization and health care costs associated with race and comorbid anxiety among Medicaid enrollees with major depressive disorder. J Nat Med Assoc. 2012;104(1-2):78-88. PubMed
30. Mapelli E, Black T, Doan Q. Trends in pediatric emergency department utilization for mental health-related visits. J Pediatr. 2015;167(4):905-910. PubMed
31. Berdahl T, Owens PL, Dougherty D, McCormick MC, Pylypchuk Y, Simpson LA. Annual report on health care for children and youth in the United States: racial/ethnic and socioeconomic disparities in children’s health care quality. Acad Pediatr. 2010;10(2):95-118. PubMed
32. Flores G; Committee on Pediatric Research. Technical report—racial and ethnic disparities in the health and health care of children. Pediatrics. 2010;125(4):e979-e1020. PubMed
33. Turner EA, Jensen-Doss A, Heffer RW. Ethnicity as a moderator of how parents’ attitudes and perceived stigma influence intentions to seek child mental health services. Cultur Divers Ethnic Minor Psychol. 2015;21(4):613-618. PubMed
34. Shaw RJ, Wamboldt M, Bursch B, Stuber M. Practice patterns in pediatric consultation-liaison psychiatry: a national survey. Psychosomatics. 2006;47(1):43-49. PubMed
35. Benton TD, Ifeagwu JA, Smith-Whitley K. Anxiety and depression in children and adolescents with sickle cell disease. Curr Psychiatry Rep. 2007;9(2):114-121. PubMed
36. Chavira DA, Garland AF, Daley S, Hough R. The impact of medical comorbidity on mental health and functional health outcomes among children with anxiety disorders. J Dev Behav Pediatr. 2008;29(5):394-402. PubMed
37. Knight A, Weiss P, Morales K, et al. Depression and anxiety and their association with healthcare utilization in pediatric lupus and mixed connective tissue disease patients: a cross-sectional study. Pediatr Rheumatol Online J. 2014;12:42. PubMed
38. Marsac ML, Kassam-Adams N, Delahanty DL, F. Widaman K, Barakat LP. Posttraumatic stress following acute medical trauma in children: a proposed model of bio-psycho-social processes during the peri-trauma period. Clin Child Fam Psychol Rev. 2014;17(4):399-411. PubMed
39. Marsac ML, Hildenbrand AK, Kohser KL, Winston FK, Li Y, Kassam-Adams N. Preventing posttraumatic stress following pediatric injury: a randomized controlled trial of a web-based psycho-educational intervention for parents. J Pediatr Psychol. 2013;38(10):1101-1111. PubMed
40. Petersen MC, Kube DA, Whitaker TM, Graff JC, Palmer FB. Prevalence of developmental and behavioral disorders in a pediatric hospital. Pediatrics. 2009;123(3):e490-e495. PubMed
© 2017 Society of Hospital Medicine