User login
Diabetes mellitus is a growing problem in the U.S., with the number of disease-related complications on the rise. It affects 29.1 million people of all ages; however, only 21 million people are diagnosed, leaving 8.1 million people undiagnosed.1 Heart disease death rates among adults with diabetes are 2 to 4 times higher than the rates for adults without diabetes.2 At least 68% of patients with diabetes aged > 65 years die of some form of heart disease; 16% die of stroke.2
Type 2 diabetes remains the leading cause for cardiovascular disorders, blindness, end-stage renal disease, amputations, and hospitalizations.3 Due to the long-term complications of diabetes, it is important to help patients control their disease. However, diabetes control in patients can be difficult because of the broad disease education needed and its medication administration.
Insulin requires the most extensive instruction when educating patients with diabetes. Specifically, patient counseling needs to incorporate the importance of proper insulin administration. If patients are not properly administering their insulin, controlling their diabetes will be very difficult. Many clinicians know to educate the patient about drawing insulin into a syringe and how to inject insulin properly. However, clinicians do not always think about other aspects of insulin administration education, such as the mixing of different insulins in 1 syringe. Patients and family members need to be taught about the types of insulins that can and cannot be mixed. The American Diabetes Association (ADA) provides recommendations on the appropriate time to mix insulin and the types of insulin that can and cannot be mixed (Table 1).4
CASE REPORT
A white male, aged 69 years, presented to a pharmacist-run pharmacotherapy clinic for a follow-up appointment for uncontrolled diabetes. The patient’s wife, who managed his medications, accompanied him. Significant past medical history included diabetes, nephropathy, retinopathy, degenerative joint disease, migraines, gastroesophageal reflux disease, depression, posttraumatic stress disorder, hyperlipidemia, hypertension, lumbago, panic attacks, medication noncompliance, status post cerebral vascular accident, and renal insufficiency.
The patient had a long history of type 2 diabetes, and his insulin had been titrated multiple times since he was established in this clinic in 2009. At his establishing visit, he was taken off his insulin pump due to noncompliance with blood glucose checks and placed on basal-bolus therapy with insulin glargine and insulin aspart. The patient then titrated his basal-bolus insulin for 6 weeks but stated his blood sugars were consistently elevated (reaching 600 mg/dL); therefore, he self-reinitiated the insulin pump. After restarting the insulin pump, the clinic made several attempts to follow-up with the patient, but none were successful. He was subsequently dismissed from the clinic following his admission to a local nursing home.
The patient was reestablished at the clinic in 2010 (about 1 year after dismissal). He reported discontinuing the insulin pump and using insulin glargine and insulin aspart injections but was self-adjusting insulin glargine based on readings. He was told not to self-adjust insulin glargine dose and was given a sliding scale for self-adjustment of his insulin aspart dose based on blood glucose readings. Since the reestablished visit, both insulin therapies were titrated without much success in controlling his blood glucose levels. He was also advised to check his fasting blood glucose (FBG) more often and was demonstrated correct insulin drawing technique.
At a follow-up visit in August 2012, the patient’s A1c was 10.7%, and FBG readings ranged from 108 mg/dL to 555 mg/dL. Goal A1c was between 8% and 8.5% per VA/DoD diabetes guidelines.5 After a discussion with the patient’s wife, it was discovered that the patient was improperly administrating his insulin. The patient had been administrating the insulin glargine and insulin aspart in the same syringe. Since the combined dose of insulin was greater than his syringe would allow, he adjusted the insulin glargine dose downward if more insulin aspart was needed per the sliding scale. He did this to avoid more injections than he thought were necessary. Based on his A1c and home blood glucose readings, it was also suspected that insulin doses were being missed. The patient and wife were instructed about the importance of adherence and not mixing these insulins in the same syringe.
At the most recent visit, the patient’s FBG readings (200 mg/dL-500 mg/dL) and A1c (10.7%) were still greatly elevated. He reported taking 40 units insulin glargine in the morning and 60 units at bedtime, along with 40 units insulin aspart plus sliding scale insulin (1:20 > 120 mg/dL) at breakfast and 40 to 70 units at lunch and supper. The patient reported compliance with insulin therapy; however, it was likely he was not dosing accurately, according to his sliding scale. He stated he was eating less and was worried about hypoglycemia. Due to the patient’s FBG and A1c still being elevated, insulin aspart was titrated again, which was closer to a 50% basal and 50% bolus regimen, and he was again educated about proper dosing.
DISCUSSION
Patients have many obstacles to managing their diseases. This is especially prevalent in patients with diabetes. These patients both experience the emotional stress of being diagnosed with diabetes and are given a wealth of information on diabetes, nutrition, therapy, and insulin-dosing technique at the same time. The information can be overwhelming for patients to hear and for the educator to present. Sometimes health care professionals (HCPs) overlook a patient’s hindrances due to the amount of information they have to give to the patient. For example, in this case, the patient was mixing insulin inappropriately, and it was overlooked by the HCP.
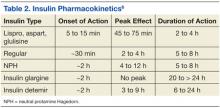
Insulin therapy has been used for several decades. It is obtained from either a pork pancreas or is chemically manufactured to be identical to human insulin. This can be achieved by recombinant DNA technology or chemical modification of pork insulin.4 Insulin is available as short-, intermediate-, or long-acting duration. The pharmacokinetics of available insulins is listed in Table 2.6
Some insulin can be mixed in the same syringe, but these mainly consist of the short- and intermediate-acting insulin. Insulin glargine, a long-acting formulation, should not be mixed with any other insulin due to its pharmacokinetic properties.7 Insulin glargine has been designed to have a low solubility at a neutral pH. After injection, the pH rises and leads to the formation of microprecipitates, causing a slow release of the insulin over 24 hours with no peak. If insulin glargine is mixed, it is likely the pH would be altered before entering the body. In addition, mixing insulin in the same syringe could likely contaminate the dose.
The maker of insulin glargine advises against mixing it with any other insulin.7 Several different studies have been done with admixtures of insulin glargine with short- or rapid-acting insulin. The studies revealed no differences in glycemic control, blunted and delayed rapid-acting insulin peak, the need for larger doses, or worsened glycemic control.8-12
Other education points about insulin administration that are often overlooked or sometimes ignored by patients and that require follow-up for compliance include the following:
• Manufacturers recommend discarding an open bottle of insulin at room temperature after 28 days.7
• Insulin should be kept in a temperature-controlled environment between 36°F and 86°F.4,7
• Rotation of injection sites is necessary to prevent lipodystrophy.4,7
• It is recommended that patients stick with 1 approved anatomical site for all insulin injections, such as the abdomen or leg, to maintain consistent pharmacokinetics.4,13,14
It is also important to know the constitution of the different insulins and whether they have been compromised. For example, if a clear solution insulin turns cloudy, it is considered compromised and should be thrown away.
CONCLUSION
Patients are diagnosed every day with diabetes, and many treatment regimens include insulin therapy. With the diagnosis of diabetes, patients are given extensive information on therapy, nutrition, preventative measures, and technique. Since controlling diabetes can call for intensive insulin therapy, medication administration instruction by HCPs is important. It is important to discuss in detail how the patient manages their insulin therapy at each visit so that issues will not be overlooked. Long-term, inappropriate use of insulin may lead to uncontrolled diabetes.
Diabetes is a complex disease to manage and takes a joint effort by both the HCP and patient to control. Patients need to understand the importance of compliance in all aspects of the disease, and the HCP needs to understand the importance of extensive counseling, including diet, exercise, and medication therapy.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: U.S. Department of Health and Human Services; 2014. http://www.cdc.gov/diabetes/pubs/statsreport14.htm. Updated July 28, 2014. Accessed August 12, 2014.
2. Roger VL, Go AS, Lloyd-Jones DM. et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: A report from the American Heart Association. Circulation. 2012;125(1):e2-e220.
3. Inzucchi SE, Bergenstal RM, Buse JB, et al; American Diabetes Association (ADA); European Association for the Study of Diabetes (EASD). Management of hyperglycemia in type 2 diabetes: A patient-centered approach: Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35(6):1364-1379.
4. American Diabetes Association. Insulin administration. Diabetes Care. 2004;27(suppl 1): S106-S109.
5. VA/DoD Clinical Practice Guidelines: Management of Diabetes Mellitus (DM). Version 4.0. Website: http://www.healthquality.va.gov/guidelines/CD/diabetes/DM2010_FUL-v4e.pdf. Updated August 2010. Accessed August 12, 2014.
6. McCulloch DK. General principles of isulin therapy in diabetes mellitus. UpToDate Website. http://www .uptodate.com /contents/general-principles-of-insulin-therapy-in-diabetes-mellitus. Accessed August 5, 2014.
7. Lantus [package insert]. Bridgewater, NJ: sanofi-aventis US; 2013.
8. Cengiz E, Tamborlane WV, Martin-Fredericksen M, Dziura J, Weinzimer SA. Early pharmacokinetic and pharmacodynamic effects of mixing lispro with glargine insulin: Results of glucose clamp studies in youth with type 1 diabetes. Diabetes Care. 2010;33(5):1009-1012.
9. Lucchesi MB, Komatsu WR, Gabbay MA, Dib SA. A 12-wk follow-up study to evaluate the effects of mixing insulin lispro and insulin glargine in young individuals with type 1 diabetes. Pediatr Diabetes. 2012;13(7):519-524.
10. Kaplan W, Rodriguez LM, Smith OE, Haymond MW, Heptulla RA. Effects of mixing glargine and short-acting insulin analogs on glucose control. Diabetes Care. 2004;27(11):2739-2740.
11. Fiallo-Scharer R, Horner B, McFann K, Walravens P, Chase HP. Mixing rapid-acting insulin analogs with insulin glargine in children with type 1 diabetes mellitus. J Pediatr. 2006;148(4):481-484.
12. Hassan K, Rodriguez LM, Johnson SE, Tadlock S, Heptulla RA. A randomized, controlled trial comparing twice-a-day insulin glargine mixed with rapid-acting insulin analogs versus standard neutral protamine Hagedorn (NPH) therapy in newly diagnosed type 1 diabetes. Pediatrics. 2008;121(3):e466 -e472.
13. Koivisto VA, Felig P. Alterations in insulin absorption and in blood glucose control associated with varying insulin injection sites in diabetic patients. Ann Intern Med. 1980;92(1):59-61.
14. Berger M, Cüppers HJ, Hegner H, Jörgens V, Berchtold P. Absorption kinetics and biologic effects of subcutaneously injected insulin preparations. Diabetes Care. 1982;5(2):77-91.
Diabetes mellitus is a growing problem in the U.S., with the number of disease-related complications on the rise. It affects 29.1 million people of all ages; however, only 21 million people are diagnosed, leaving 8.1 million people undiagnosed.1 Heart disease death rates among adults with diabetes are 2 to 4 times higher than the rates for adults without diabetes.2 At least 68% of patients with diabetes aged > 65 years die of some form of heart disease; 16% die of stroke.2
Type 2 diabetes remains the leading cause for cardiovascular disorders, blindness, end-stage renal disease, amputations, and hospitalizations.3 Due to the long-term complications of diabetes, it is important to help patients control their disease. However, diabetes control in patients can be difficult because of the broad disease education needed and its medication administration.
Insulin requires the most extensive instruction when educating patients with diabetes. Specifically, patient counseling needs to incorporate the importance of proper insulin administration. If patients are not properly administering their insulin, controlling their diabetes will be very difficult. Many clinicians know to educate the patient about drawing insulin into a syringe and how to inject insulin properly. However, clinicians do not always think about other aspects of insulin administration education, such as the mixing of different insulins in 1 syringe. Patients and family members need to be taught about the types of insulins that can and cannot be mixed. The American Diabetes Association (ADA) provides recommendations on the appropriate time to mix insulin and the types of insulin that can and cannot be mixed (Table 1).4
CASE REPORT
A white male, aged 69 years, presented to a pharmacist-run pharmacotherapy clinic for a follow-up appointment for uncontrolled diabetes. The patient’s wife, who managed his medications, accompanied him. Significant past medical history included diabetes, nephropathy, retinopathy, degenerative joint disease, migraines, gastroesophageal reflux disease, depression, posttraumatic stress disorder, hyperlipidemia, hypertension, lumbago, panic attacks, medication noncompliance, status post cerebral vascular accident, and renal insufficiency.
The patient had a long history of type 2 diabetes, and his insulin had been titrated multiple times since he was established in this clinic in 2009. At his establishing visit, he was taken off his insulin pump due to noncompliance with blood glucose checks and placed on basal-bolus therapy with insulin glargine and insulin aspart. The patient then titrated his basal-bolus insulin for 6 weeks but stated his blood sugars were consistently elevated (reaching 600 mg/dL); therefore, he self-reinitiated the insulin pump. After restarting the insulin pump, the clinic made several attempts to follow-up with the patient, but none were successful. He was subsequently dismissed from the clinic following his admission to a local nursing home.
The patient was reestablished at the clinic in 2010 (about 1 year after dismissal). He reported discontinuing the insulin pump and using insulin glargine and insulin aspart injections but was self-adjusting insulin glargine based on readings. He was told not to self-adjust insulin glargine dose and was given a sliding scale for self-adjustment of his insulin aspart dose based on blood glucose readings. Since the reestablished visit, both insulin therapies were titrated without much success in controlling his blood glucose levels. He was also advised to check his fasting blood glucose (FBG) more often and was demonstrated correct insulin drawing technique.
At a follow-up visit in August 2012, the patient’s A1c was 10.7%, and FBG readings ranged from 108 mg/dL to 555 mg/dL. Goal A1c was between 8% and 8.5% per VA/DoD diabetes guidelines.5 After a discussion with the patient’s wife, it was discovered that the patient was improperly administrating his insulin. The patient had been administrating the insulin glargine and insulin aspart in the same syringe. Since the combined dose of insulin was greater than his syringe would allow, he adjusted the insulin glargine dose downward if more insulin aspart was needed per the sliding scale. He did this to avoid more injections than he thought were necessary. Based on his A1c and home blood glucose readings, it was also suspected that insulin doses were being missed. The patient and wife were instructed about the importance of adherence and not mixing these insulins in the same syringe.
At the most recent visit, the patient’s FBG readings (200 mg/dL-500 mg/dL) and A1c (10.7%) were still greatly elevated. He reported taking 40 units insulin glargine in the morning and 60 units at bedtime, along with 40 units insulin aspart plus sliding scale insulin (1:20 > 120 mg/dL) at breakfast and 40 to 70 units at lunch and supper. The patient reported compliance with insulin therapy; however, it was likely he was not dosing accurately, according to his sliding scale. He stated he was eating less and was worried about hypoglycemia. Due to the patient’s FBG and A1c still being elevated, insulin aspart was titrated again, which was closer to a 50% basal and 50% bolus regimen, and he was again educated about proper dosing.
DISCUSSION
Patients have many obstacles to managing their diseases. This is especially prevalent in patients with diabetes. These patients both experience the emotional stress of being diagnosed with diabetes and are given a wealth of information on diabetes, nutrition, therapy, and insulin-dosing technique at the same time. The information can be overwhelming for patients to hear and for the educator to present. Sometimes health care professionals (HCPs) overlook a patient’s hindrances due to the amount of information they have to give to the patient. For example, in this case, the patient was mixing insulin inappropriately, and it was overlooked by the HCP.
Insulin therapy has been used for several decades. It is obtained from either a pork pancreas or is chemically manufactured to be identical to human insulin. This can be achieved by recombinant DNA technology or chemical modification of pork insulin.4 Insulin is available as short-, intermediate-, or long-acting duration. The pharmacokinetics of available insulins is listed in Table 2.6
Some insulin can be mixed in the same syringe, but these mainly consist of the short- and intermediate-acting insulin. Insulin glargine, a long-acting formulation, should not be mixed with any other insulin due to its pharmacokinetic properties.7 Insulin glargine has been designed to have a low solubility at a neutral pH. After injection, the pH rises and leads to the formation of microprecipitates, causing a slow release of the insulin over 24 hours with no peak. If insulin glargine is mixed, it is likely the pH would be altered before entering the body. In addition, mixing insulin in the same syringe could likely contaminate the dose.
The maker of insulin glargine advises against mixing it with any other insulin.7 Several different studies have been done with admixtures of insulin glargine with short- or rapid-acting insulin. The studies revealed no differences in glycemic control, blunted and delayed rapid-acting insulin peak, the need for larger doses, or worsened glycemic control.8-12
Other education points about insulin administration that are often overlooked or sometimes ignored by patients and that require follow-up for compliance include the following:
• Manufacturers recommend discarding an open bottle of insulin at room temperature after 28 days.7
• Insulin should be kept in a temperature-controlled environment between 36°F and 86°F.4,7
• Rotation of injection sites is necessary to prevent lipodystrophy.4,7
• It is recommended that patients stick with 1 approved anatomical site for all insulin injections, such as the abdomen or leg, to maintain consistent pharmacokinetics.4,13,14
It is also important to know the constitution of the different insulins and whether they have been compromised. For example, if a clear solution insulin turns cloudy, it is considered compromised and should be thrown away.
CONCLUSION
Patients are diagnosed every day with diabetes, and many treatment regimens include insulin therapy. With the diagnosis of diabetes, patients are given extensive information on therapy, nutrition, preventative measures, and technique. Since controlling diabetes can call for intensive insulin therapy, medication administration instruction by HCPs is important. It is important to discuss in detail how the patient manages their insulin therapy at each visit so that issues will not be overlooked. Long-term, inappropriate use of insulin may lead to uncontrolled diabetes.
Diabetes is a complex disease to manage and takes a joint effort by both the HCP and patient to control. Patients need to understand the importance of compliance in all aspects of the disease, and the HCP needs to understand the importance of extensive counseling, including diet, exercise, and medication therapy.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Diabetes mellitus is a growing problem in the U.S., with the number of disease-related complications on the rise. It affects 29.1 million people of all ages; however, only 21 million people are diagnosed, leaving 8.1 million people undiagnosed.1 Heart disease death rates among adults with diabetes are 2 to 4 times higher than the rates for adults without diabetes.2 At least 68% of patients with diabetes aged > 65 years die of some form of heart disease; 16% die of stroke.2
Type 2 diabetes remains the leading cause for cardiovascular disorders, blindness, end-stage renal disease, amputations, and hospitalizations.3 Due to the long-term complications of diabetes, it is important to help patients control their disease. However, diabetes control in patients can be difficult because of the broad disease education needed and its medication administration.
Insulin requires the most extensive instruction when educating patients with diabetes. Specifically, patient counseling needs to incorporate the importance of proper insulin administration. If patients are not properly administering their insulin, controlling their diabetes will be very difficult. Many clinicians know to educate the patient about drawing insulin into a syringe and how to inject insulin properly. However, clinicians do not always think about other aspects of insulin administration education, such as the mixing of different insulins in 1 syringe. Patients and family members need to be taught about the types of insulins that can and cannot be mixed. The American Diabetes Association (ADA) provides recommendations on the appropriate time to mix insulin and the types of insulin that can and cannot be mixed (Table 1).4
CASE REPORT
A white male, aged 69 years, presented to a pharmacist-run pharmacotherapy clinic for a follow-up appointment for uncontrolled diabetes. The patient’s wife, who managed his medications, accompanied him. Significant past medical history included diabetes, nephropathy, retinopathy, degenerative joint disease, migraines, gastroesophageal reflux disease, depression, posttraumatic stress disorder, hyperlipidemia, hypertension, lumbago, panic attacks, medication noncompliance, status post cerebral vascular accident, and renal insufficiency.
The patient had a long history of type 2 diabetes, and his insulin had been titrated multiple times since he was established in this clinic in 2009. At his establishing visit, he was taken off his insulin pump due to noncompliance with blood glucose checks and placed on basal-bolus therapy with insulin glargine and insulin aspart. The patient then titrated his basal-bolus insulin for 6 weeks but stated his blood sugars were consistently elevated (reaching 600 mg/dL); therefore, he self-reinitiated the insulin pump. After restarting the insulin pump, the clinic made several attempts to follow-up with the patient, but none were successful. He was subsequently dismissed from the clinic following his admission to a local nursing home.
The patient was reestablished at the clinic in 2010 (about 1 year after dismissal). He reported discontinuing the insulin pump and using insulin glargine and insulin aspart injections but was self-adjusting insulin glargine based on readings. He was told not to self-adjust insulin glargine dose and was given a sliding scale for self-adjustment of his insulin aspart dose based on blood glucose readings. Since the reestablished visit, both insulin therapies were titrated without much success in controlling his blood glucose levels. He was also advised to check his fasting blood glucose (FBG) more often and was demonstrated correct insulin drawing technique.
At a follow-up visit in August 2012, the patient’s A1c was 10.7%, and FBG readings ranged from 108 mg/dL to 555 mg/dL. Goal A1c was between 8% and 8.5% per VA/DoD diabetes guidelines.5 After a discussion with the patient’s wife, it was discovered that the patient was improperly administrating his insulin. The patient had been administrating the insulin glargine and insulin aspart in the same syringe. Since the combined dose of insulin was greater than his syringe would allow, he adjusted the insulin glargine dose downward if more insulin aspart was needed per the sliding scale. He did this to avoid more injections than he thought were necessary. Based on his A1c and home blood glucose readings, it was also suspected that insulin doses were being missed. The patient and wife were instructed about the importance of adherence and not mixing these insulins in the same syringe.
At the most recent visit, the patient’s FBG readings (200 mg/dL-500 mg/dL) and A1c (10.7%) were still greatly elevated. He reported taking 40 units insulin glargine in the morning and 60 units at bedtime, along with 40 units insulin aspart plus sliding scale insulin (1:20 > 120 mg/dL) at breakfast and 40 to 70 units at lunch and supper. The patient reported compliance with insulin therapy; however, it was likely he was not dosing accurately, according to his sliding scale. He stated he was eating less and was worried about hypoglycemia. Due to the patient’s FBG and A1c still being elevated, insulin aspart was titrated again, which was closer to a 50% basal and 50% bolus regimen, and he was again educated about proper dosing.
DISCUSSION
Patients have many obstacles to managing their diseases. This is especially prevalent in patients with diabetes. These patients both experience the emotional stress of being diagnosed with diabetes and are given a wealth of information on diabetes, nutrition, therapy, and insulin-dosing technique at the same time. The information can be overwhelming for patients to hear and for the educator to present. Sometimes health care professionals (HCPs) overlook a patient’s hindrances due to the amount of information they have to give to the patient. For example, in this case, the patient was mixing insulin inappropriately, and it was overlooked by the HCP.
Insulin therapy has been used for several decades. It is obtained from either a pork pancreas or is chemically manufactured to be identical to human insulin. This can be achieved by recombinant DNA technology or chemical modification of pork insulin.4 Insulin is available as short-, intermediate-, or long-acting duration. The pharmacokinetics of available insulins is listed in Table 2.6
Some insulin can be mixed in the same syringe, but these mainly consist of the short- and intermediate-acting insulin. Insulin glargine, a long-acting formulation, should not be mixed with any other insulin due to its pharmacokinetic properties.7 Insulin glargine has been designed to have a low solubility at a neutral pH. After injection, the pH rises and leads to the formation of microprecipitates, causing a slow release of the insulin over 24 hours with no peak. If insulin glargine is mixed, it is likely the pH would be altered before entering the body. In addition, mixing insulin in the same syringe could likely contaminate the dose.
The maker of insulin glargine advises against mixing it with any other insulin.7 Several different studies have been done with admixtures of insulin glargine with short- or rapid-acting insulin. The studies revealed no differences in glycemic control, blunted and delayed rapid-acting insulin peak, the need for larger doses, or worsened glycemic control.8-12
Other education points about insulin administration that are often overlooked or sometimes ignored by patients and that require follow-up for compliance include the following:
• Manufacturers recommend discarding an open bottle of insulin at room temperature after 28 days.7
• Insulin should be kept in a temperature-controlled environment between 36°F and 86°F.4,7
• Rotation of injection sites is necessary to prevent lipodystrophy.4,7
• It is recommended that patients stick with 1 approved anatomical site for all insulin injections, such as the abdomen or leg, to maintain consistent pharmacokinetics.4,13,14
It is also important to know the constitution of the different insulins and whether they have been compromised. For example, if a clear solution insulin turns cloudy, it is considered compromised and should be thrown away.
CONCLUSION
Patients are diagnosed every day with diabetes, and many treatment regimens include insulin therapy. With the diagnosis of diabetes, patients are given extensive information on therapy, nutrition, preventative measures, and technique. Since controlling diabetes can call for intensive insulin therapy, medication administration instruction by HCPs is important. It is important to discuss in detail how the patient manages their insulin therapy at each visit so that issues will not be overlooked. Long-term, inappropriate use of insulin may lead to uncontrolled diabetes.
Diabetes is a complex disease to manage and takes a joint effort by both the HCP and patient to control. Patients need to understand the importance of compliance in all aspects of the disease, and the HCP needs to understand the importance of extensive counseling, including diet, exercise, and medication therapy.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: U.S. Department of Health and Human Services; 2014. http://www.cdc.gov/diabetes/pubs/statsreport14.htm. Updated July 28, 2014. Accessed August 12, 2014.
2. Roger VL, Go AS, Lloyd-Jones DM. et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: A report from the American Heart Association. Circulation. 2012;125(1):e2-e220.
3. Inzucchi SE, Bergenstal RM, Buse JB, et al; American Diabetes Association (ADA); European Association for the Study of Diabetes (EASD). Management of hyperglycemia in type 2 diabetes: A patient-centered approach: Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35(6):1364-1379.
4. American Diabetes Association. Insulin administration. Diabetes Care. 2004;27(suppl 1): S106-S109.
5. VA/DoD Clinical Practice Guidelines: Management of Diabetes Mellitus (DM). Version 4.0. Website: http://www.healthquality.va.gov/guidelines/CD/diabetes/DM2010_FUL-v4e.pdf. Updated August 2010. Accessed August 12, 2014.
6. McCulloch DK. General principles of isulin therapy in diabetes mellitus. UpToDate Website. http://www .uptodate.com /contents/general-principles-of-insulin-therapy-in-diabetes-mellitus. Accessed August 5, 2014.
7. Lantus [package insert]. Bridgewater, NJ: sanofi-aventis US; 2013.
8. Cengiz E, Tamborlane WV, Martin-Fredericksen M, Dziura J, Weinzimer SA. Early pharmacokinetic and pharmacodynamic effects of mixing lispro with glargine insulin: Results of glucose clamp studies in youth with type 1 diabetes. Diabetes Care. 2010;33(5):1009-1012.
9. Lucchesi MB, Komatsu WR, Gabbay MA, Dib SA. A 12-wk follow-up study to evaluate the effects of mixing insulin lispro and insulin glargine in young individuals with type 1 diabetes. Pediatr Diabetes. 2012;13(7):519-524.
10. Kaplan W, Rodriguez LM, Smith OE, Haymond MW, Heptulla RA. Effects of mixing glargine and short-acting insulin analogs on glucose control. Diabetes Care. 2004;27(11):2739-2740.
11. Fiallo-Scharer R, Horner B, McFann K, Walravens P, Chase HP. Mixing rapid-acting insulin analogs with insulin glargine in children with type 1 diabetes mellitus. J Pediatr. 2006;148(4):481-484.
12. Hassan K, Rodriguez LM, Johnson SE, Tadlock S, Heptulla RA. A randomized, controlled trial comparing twice-a-day insulin glargine mixed with rapid-acting insulin analogs versus standard neutral protamine Hagedorn (NPH) therapy in newly diagnosed type 1 diabetes. Pediatrics. 2008;121(3):e466 -e472.
13. Koivisto VA, Felig P. Alterations in insulin absorption and in blood glucose control associated with varying insulin injection sites in diabetic patients. Ann Intern Med. 1980;92(1):59-61.
14. Berger M, Cüppers HJ, Hegner H, Jörgens V, Berchtold P. Absorption kinetics and biologic effects of subcutaneously injected insulin preparations. Diabetes Care. 1982;5(2):77-91.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: U.S. Department of Health and Human Services; 2014. http://www.cdc.gov/diabetes/pubs/statsreport14.htm. Updated July 28, 2014. Accessed August 12, 2014.
2. Roger VL, Go AS, Lloyd-Jones DM. et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: A report from the American Heart Association. Circulation. 2012;125(1):e2-e220.
3. Inzucchi SE, Bergenstal RM, Buse JB, et al; American Diabetes Association (ADA); European Association for the Study of Diabetes (EASD). Management of hyperglycemia in type 2 diabetes: A patient-centered approach: Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35(6):1364-1379.
4. American Diabetes Association. Insulin administration. Diabetes Care. 2004;27(suppl 1): S106-S109.
5. VA/DoD Clinical Practice Guidelines: Management of Diabetes Mellitus (DM). Version 4.0. Website: http://www.healthquality.va.gov/guidelines/CD/diabetes/DM2010_FUL-v4e.pdf. Updated August 2010. Accessed August 12, 2014.
6. McCulloch DK. General principles of isulin therapy in diabetes mellitus. UpToDate Website. http://www .uptodate.com /contents/general-principles-of-insulin-therapy-in-diabetes-mellitus. Accessed August 5, 2014.
7. Lantus [package insert]. Bridgewater, NJ: sanofi-aventis US; 2013.
8. Cengiz E, Tamborlane WV, Martin-Fredericksen M, Dziura J, Weinzimer SA. Early pharmacokinetic and pharmacodynamic effects of mixing lispro with glargine insulin: Results of glucose clamp studies in youth with type 1 diabetes. Diabetes Care. 2010;33(5):1009-1012.
9. Lucchesi MB, Komatsu WR, Gabbay MA, Dib SA. A 12-wk follow-up study to evaluate the effects of mixing insulin lispro and insulin glargine in young individuals with type 1 diabetes. Pediatr Diabetes. 2012;13(7):519-524.
10. Kaplan W, Rodriguez LM, Smith OE, Haymond MW, Heptulla RA. Effects of mixing glargine and short-acting insulin analogs on glucose control. Diabetes Care. 2004;27(11):2739-2740.
11. Fiallo-Scharer R, Horner B, McFann K, Walravens P, Chase HP. Mixing rapid-acting insulin analogs with insulin glargine in children with type 1 diabetes mellitus. J Pediatr. 2006;148(4):481-484.
12. Hassan K, Rodriguez LM, Johnson SE, Tadlock S, Heptulla RA. A randomized, controlled trial comparing twice-a-day insulin glargine mixed with rapid-acting insulin analogs versus standard neutral protamine Hagedorn (NPH) therapy in newly diagnosed type 1 diabetes. Pediatrics. 2008;121(3):e466 -e472.
13. Koivisto VA, Felig P. Alterations in insulin absorption and in blood glucose control associated with varying insulin injection sites in diabetic patients. Ann Intern Med. 1980;92(1):59-61.
14. Berger M, Cüppers HJ, Hegner H, Jörgens V, Berchtold P. Absorption kinetics and biologic effects of subcutaneously injected insulin preparations. Diabetes Care. 1982;5(2):77-91.