User login
High-concern organisms were cultured from 92% of duodenoscopes immediately after endoscopic retrograde cholangiopancreatography (ERCP), and from 17% of scopes after reprocessing, based on a small single-center study reported at an annual scientific meeting on infectious diseases.
“We think the high percentage of high-concern organisms is key to highlight, because it shows the importance of vigilant reprocessing techniques,” said Dr. Michaela Gazdik, who led the study at Intermountain Healthcare in Salt Lake City. A 17% prevalence of clinically significant residual contamination after reprocessing “aligns with reports from the literature, indicating that reprocessing protocols are likely effective,” she added.
But “no growth” on a quantitative plate does not necessarily mean there are no microbes on a duodenoscope, Dr. Gazdik emphasized. Swabbing the duodenoscope, and particularly the notoriously hard to clean elevator mechanism, could improve sampling, she said.
In 2013 and 2014, the FDA received reports of about 135 multidrug resistant infections acquired after ERCP. “After investigation, many of these outbreaks were attributed to the duodenoscope’s elevator mechanism,” Dr. Gazdik noted. The elevator mechanism contains microscopic crevices that can remain contaminated even after cleaning with a manual brush as recommended by manufacturers. To study the efficacy of their reprocessing system, Dr. Gazdik and her associates cultured 12 scopes immediately after ERCP and again after reprocessing. They also took conducted surveillance cultures of 11 scopes stored at other Intermountain Healthcare facilities.
Immediately after ERCP, 91.7% (11 of 12) scopes cultured out high-concern organisms, including Pseudomonas aeruginosa, Enterococcus species, Klebsiella pneumoniae, Enterobacter asburiae, and E. cloacae, said Dr. Gazdik. Three-quarters of the scopes also yielded gram-negative organisms. No organisms were resistant to carbapenem or vancomycin, based on testing with selective media.
After reprocessing, 17% of the scopes still yielded high-concern organisms, and 9% had more quantitative growth than desired, Dr. Gazdik reported. “We did tell our reprocessing departments that their protocols seem to be as effective as others out there,” she said. “But two scopes showed growth in broth that matched the pre-reprocessing growth, indicating it was left over after reprocessing. We thought that was an interesting result, because the interim CDC guidance does not include a swab portion.”
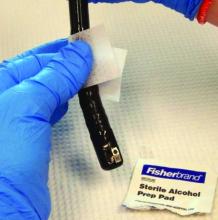
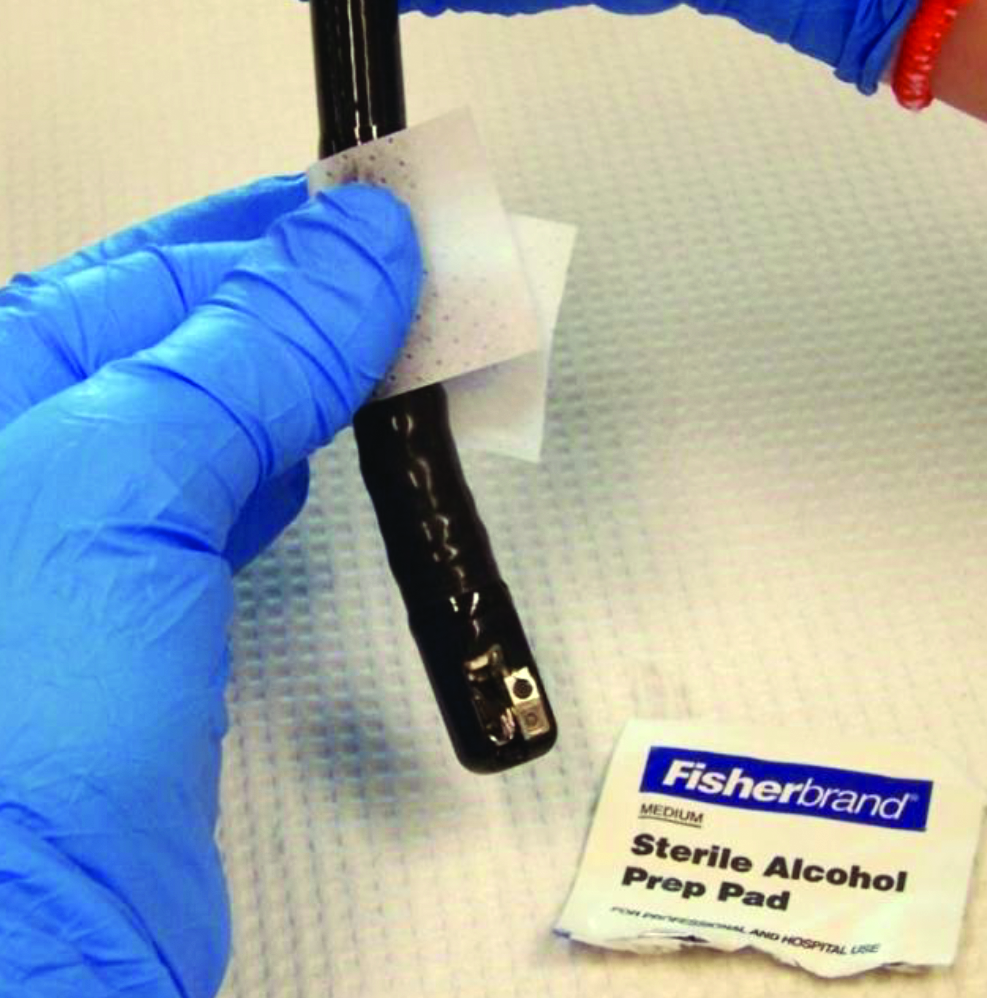
To culture the scopes, investigators flushed 5 mL of sterile saline through the elevator channel, brushed the cantilevered elevator mechanism in both the up and down positions, and rapidly swirled the brush in the flush saline. They performed quantitative colony counts by serially diluting the collected saline. For the swab-broth culture, they passed a sterile swab over and under the distal elevator mechanism and inoculating the swab into 5 mL tryptic soy broth. They also subcultured growth from the broth to identify bacteria.
Surveillance cultures of the 11 stored scopes identified no organisms from quantitative plate counts, but swab-inoculated broth cultures grew Micrococcus from three of 11 scopes, and non-CRE [carbapenem-resistant Enterobacteriaceae] K. pneumonia from one scope, Dr. Gazdik also reported. “Routine cultures play a role, mainly to continue heightened vigilance during reprocessing,” she said. “The sampling method we are going to be using will be simplified from the CDC procedure so that we can train endoscopy technicians to do it and then send samples to us.”
Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.
High-concern organisms were cultured from 92% of duodenoscopes immediately after endoscopic retrograde cholangiopancreatography (ERCP), and from 17% of scopes after reprocessing, based on a small single-center study reported at an annual scientific meeting on infectious diseases.
“We think the high percentage of high-concern organisms is key to highlight, because it shows the importance of vigilant reprocessing techniques,” said Dr. Michaela Gazdik, who led the study at Intermountain Healthcare in Salt Lake City. A 17% prevalence of clinically significant residual contamination after reprocessing “aligns with reports from the literature, indicating that reprocessing protocols are likely effective,” she added.
But “no growth” on a quantitative plate does not necessarily mean there are no microbes on a duodenoscope, Dr. Gazdik emphasized. Swabbing the duodenoscope, and particularly the notoriously hard to clean elevator mechanism, could improve sampling, she said.
In 2013 and 2014, the FDA received reports of about 135 multidrug resistant infections acquired after ERCP. “After investigation, many of these outbreaks were attributed to the duodenoscope’s elevator mechanism,” Dr. Gazdik noted. The elevator mechanism contains microscopic crevices that can remain contaminated even after cleaning with a manual brush as recommended by manufacturers. To study the efficacy of their reprocessing system, Dr. Gazdik and her associates cultured 12 scopes immediately after ERCP and again after reprocessing. They also took conducted surveillance cultures of 11 scopes stored at other Intermountain Healthcare facilities.
Immediately after ERCP, 91.7% (11 of 12) scopes cultured out high-concern organisms, including Pseudomonas aeruginosa, Enterococcus species, Klebsiella pneumoniae, Enterobacter asburiae, and E. cloacae, said Dr. Gazdik. Three-quarters of the scopes also yielded gram-negative organisms. No organisms were resistant to carbapenem or vancomycin, based on testing with selective media.
After reprocessing, 17% of the scopes still yielded high-concern organisms, and 9% had more quantitative growth than desired, Dr. Gazdik reported. “We did tell our reprocessing departments that their protocols seem to be as effective as others out there,” she said. “But two scopes showed growth in broth that matched the pre-reprocessing growth, indicating it was left over after reprocessing. We thought that was an interesting result, because the interim CDC guidance does not include a swab portion.”
To culture the scopes, investigators flushed 5 mL of sterile saline through the elevator channel, brushed the cantilevered elevator mechanism in both the up and down positions, and rapidly swirled the brush in the flush saline. They performed quantitative colony counts by serially diluting the collected saline. For the swab-broth culture, they passed a sterile swab over and under the distal elevator mechanism and inoculating the swab into 5 mL tryptic soy broth. They also subcultured growth from the broth to identify bacteria.
Surveillance cultures of the 11 stored scopes identified no organisms from quantitative plate counts, but swab-inoculated broth cultures grew Micrococcus from three of 11 scopes, and non-CRE [carbapenem-resistant Enterobacteriaceae] K. pneumonia from one scope, Dr. Gazdik also reported. “Routine cultures play a role, mainly to continue heightened vigilance during reprocessing,” she said. “The sampling method we are going to be using will be simplified from the CDC procedure so that we can train endoscopy technicians to do it and then send samples to us.”
Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.
High-concern organisms were cultured from 92% of duodenoscopes immediately after endoscopic retrograde cholangiopancreatography (ERCP), and from 17% of scopes after reprocessing, based on a small single-center study reported at an annual scientific meeting on infectious diseases.
“We think the high percentage of high-concern organisms is key to highlight, because it shows the importance of vigilant reprocessing techniques,” said Dr. Michaela Gazdik, who led the study at Intermountain Healthcare in Salt Lake City. A 17% prevalence of clinically significant residual contamination after reprocessing “aligns with reports from the literature, indicating that reprocessing protocols are likely effective,” she added.
But “no growth” on a quantitative plate does not necessarily mean there are no microbes on a duodenoscope, Dr. Gazdik emphasized. Swabbing the duodenoscope, and particularly the notoriously hard to clean elevator mechanism, could improve sampling, she said.
In 2013 and 2014, the FDA received reports of about 135 multidrug resistant infections acquired after ERCP. “After investigation, many of these outbreaks were attributed to the duodenoscope’s elevator mechanism,” Dr. Gazdik noted. The elevator mechanism contains microscopic crevices that can remain contaminated even after cleaning with a manual brush as recommended by manufacturers. To study the efficacy of their reprocessing system, Dr. Gazdik and her associates cultured 12 scopes immediately after ERCP and again after reprocessing. They also took conducted surveillance cultures of 11 scopes stored at other Intermountain Healthcare facilities.
Immediately after ERCP, 91.7% (11 of 12) scopes cultured out high-concern organisms, including Pseudomonas aeruginosa, Enterococcus species, Klebsiella pneumoniae, Enterobacter asburiae, and E. cloacae, said Dr. Gazdik. Three-quarters of the scopes also yielded gram-negative organisms. No organisms were resistant to carbapenem or vancomycin, based on testing with selective media.
After reprocessing, 17% of the scopes still yielded high-concern organisms, and 9% had more quantitative growth than desired, Dr. Gazdik reported. “We did tell our reprocessing departments that their protocols seem to be as effective as others out there,” she said. “But two scopes showed growth in broth that matched the pre-reprocessing growth, indicating it was left over after reprocessing. We thought that was an interesting result, because the interim CDC guidance does not include a swab portion.”
To culture the scopes, investigators flushed 5 mL of sterile saline through the elevator channel, brushed the cantilevered elevator mechanism in both the up and down positions, and rapidly swirled the brush in the flush saline. They performed quantitative colony counts by serially diluting the collected saline. For the swab-broth culture, they passed a sterile swab over and under the distal elevator mechanism and inoculating the swab into 5 mL tryptic soy broth. They also subcultured growth from the broth to identify bacteria.
Surveillance cultures of the 11 stored scopes identified no organisms from quantitative plate counts, but swab-inoculated broth cultures grew Micrococcus from three of 11 scopes, and non-CRE [carbapenem-resistant Enterobacteriaceae] K. pneumonia from one scope, Dr. Gazdik also reported. “Routine cultures play a role, mainly to continue heightened vigilance during reprocessing,” she said. “The sampling method we are going to be using will be simplified from the CDC procedure so that we can train endoscopy technicians to do it and then send samples to us.”
Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.
AT IDWEEK 2015
Key clinical point: High-concern organisms often contaminated duodenoscopes after ERCP.
Major finding: Investigators cultured these bacteria from 92% of duodenoscopes immediately after ERCP, and from 17% of scopes after reprocessing.
Data source: Cultures of 12 duodenoscopes immediately after ERCP and again after reprocessing, and surveillance cultures of 11 stored duodenoscopes.
Disclosures: Dr. Gazdik and her coauthors reported no funding sources and had no conflicts of interest.