User login
ANSWER
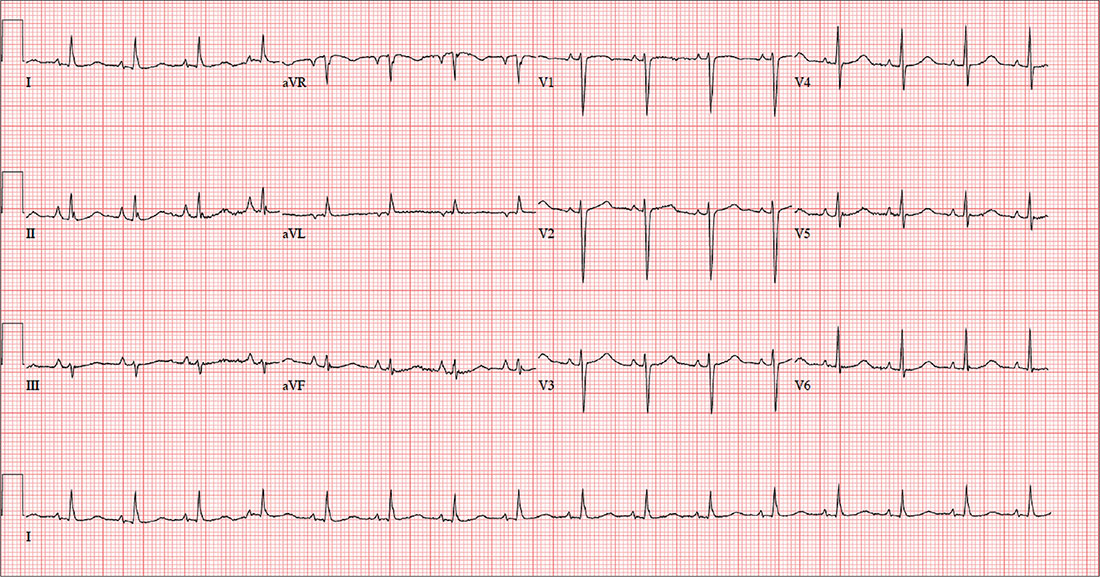
The correct interpretation includes normal sinus rhythm and right atrial enlargement. The latter is suggested by tall P waves in leads II, III, and aVF (typically ≥ 2.5 mm), which may be caused by pressure or volume overload of the right atrium or by conditions causing pulmonary hypertension.
Given this patient’s presentation of right-side chest pain with a history of COPD, smoking, palpable left saphenous vein, and right atrial enlargement, a chest CT was performed. It confirmed the suspicion of a pulmonary embolus.
ANSWER
The correct interpretation includes normal sinus rhythm and right atrial enlargement. The latter is suggested by tall P waves in leads II, III, and aVF (typically ≥ 2.5 mm), which may be caused by pressure or volume overload of the right atrium or by conditions causing pulmonary hypertension.
Given this patient’s presentation of right-side chest pain with a history of COPD, smoking, palpable left saphenous vein, and right atrial enlargement, a chest CT was performed. It confirmed the suspicion of a pulmonary embolus.
ANSWER
The correct interpretation includes normal sinus rhythm and right atrial enlargement. The latter is suggested by tall P waves in leads II, III, and aVF (typically ≥ 2.5 mm), which may be caused by pressure or volume overload of the right atrium or by conditions causing pulmonary hypertension.
Given this patient’s presentation of right-side chest pain with a history of COPD, smoking, palpable left saphenous vein, and right atrial enlargement, a chest CT was performed. It confirmed the suspicion of a pulmonary embolus.
A 64-year-old woman presents with nondescript pain throughout her right chest. One week ago, she developed aching in both lower extremities, worse in the left leg than in the right. Two days ago, she noticed a tender area on her lower left leg that “feels like a hard rope.” She denies constitutional symptoms and changes in bowel or bladder habits.
Initial history-taking produces only the vague response that she’s “had my share of medical problems” through the years. A review of the electronic medical record reveals a history of chronic obstructive pulmonary disease (COPD), tobacco use, and recurrent community-acquired pneumonia—as well as a pattern of missed appointments. Her most recent visit was five years ago.
On further questioning, the patient informs you that she was shocked for a rapid heartbeat in the past year, following a weekend of binge-drinking on a cruise. She also reveals that she has increased her per-day cigarette habit from one to 2.5 packs to “deal with the stress of the holidays.” However, she reports no changes in her respiratory status or her “usual” productive morning cough. She denies shortness of breath, as well as any history of hypertension, diabetes, thyroid disorder, or cardiac-related chest pain.
The patient has been divorced for 11 years. Her job keeps her on the road between eight and 10 hours a day. She drinks alcohol on the weekend—anywhere from one six-pack to an entire case of beer. She began smoking at age 13 and hasn’t stopped since, refusing any offers of smoking cessation. She tried marijuana a few years ago but “didn’t like” how it made her feel. She denies using illicit or prescription drugs.
Family history reveals that the patient’s parents and both sets of grandparents were chronic smokers. Her paternal grandfather died of complications from emphysema, her maternal grandfather of asbestosis, and both grandmothers of strokes. Her parents are alive and reside in an assisted living facility. Her mother is being treated for colon cancer, and her father has had two myocardial infarctions. She had one brother who died in a motorcycle accident at age 15.
Her height is 69 in and her weight, 142 lb. Vital signs include a blood pressure of 152/94 mm Hg; pulse, 90 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 97.2°F.
On physical exam, the patient appears older than her stated age but is in no distress. The HEENT exam is significant for corrective lenses, stained teeth, and leukoplakia on the oral mucosa. Neck veins are elevated, with a prominent A wave present. There is no thyromegaly or carotid bruits. The lungs reveal coarse rhonchi bilaterally in all lung fields, with no significant changes with coughing. The cardiac rate is regular with no evidence of a murmur or rub. Peripheral pulses are strong and equal bilaterally in both upper and lower extremities. The abdominal exam shows no evidence of organomegaly or masses, and the abdominal aorta is easily palpable. There is no edema in the lower extremities; however, a palpable cord is present along the entire length of the left greater saphenous vein. The neurologic exam is grossly intact without focal signs.
In addition to routine laboratory specimens, a chest x-ray and ECG are obtained. The ECG shows a ventricular rate of 96 beats/min; PR interval, 126 ms; QRS duration, 80 ms; QT/QTc interval, 384/485 ms; P axis, 79°; R axis, 18°; and T axis, 63°. What is your interpretation of this ECG?
