User login
In a recent editorial, OBG Management Editor in Chief Dr. Robert L. Barbieri presented a draft checklist to guide clinicians during repair of third- and fourth-degree perineal lacerations. He also invited the journal’s readers to modify the checklist as they saw fit—and plenty of you responded! Here is a selection of the suggestions we received, with Dr. Barbieri’s reply.
How I adjusted my surgical protocol for the repair of severe perineal lacerations
I appreciate the clinical pearls offered by Dr. Robert Barbieri in his editorial on the repair of severe perineal lacerations. In response, I plan to change my protocol to initiate antibiotics prior to repair.
I would also offer this tip: When addressing the rectal mucosa, try to stay on a submucosal level, and perform a post-repair rectal exam to ensure that the mucosa has not been violated by a suture and to reduce the risk of rectovaginal fistula.
I repair the internal sphincter using an interrupted technique. And I place only three sutures in the external sphincter, at 8, 12, and 4 o’clock.
Martin E. Kanoff, DO
Sewell, New Jersey
A few pearls on checklist design
I am a big proponent of checklists and use them daily in my professional and personal life. However, as Atul Gawande, MD, MPH, mentioned in his book The Checklist Manifesto, checklists can’t teach a pilot how to fly a plane—that is best achieved through simulation. Dr. Gawande also noted that checklists should be short and to the point, usually containing no more than 10 items, and should highlight things more likely to be overlooked.
For the repair of perineal lacerations, a checklist might include:
- Call for help
- Consider repair in an OR
- Administer preoperative antibiotics
- Ensure adequate exposure and visualization
- Repair in layers (?)
- Postprocedure laxative
- Prophylaxis for deep venous thrombosis (?)
- Return to office in 1 week (?).
The items followed by a question mark are of uncertain value.
Ideally, each checklist should undergo validation via dry runs and team training. In my experience, it is not as difficult to design a checklist as to design a system where checklists get executed entirely and correctly.
Alex Shilkrut, MD
Safety Director, Department of Obstetrics and Gynecology, Metropolitan Hospital, New York, New York
A question about sphincters
I am grateful for Dr. Barbieri’s excellent editorial on using a checklist. I was taught that three sphincters require attention in 4th-degree lacerations: the internal anal sphincter, the external anal sphincter, and the superficial transverse perineal muscle. Would Dr. Barbieri agree?
John Lavin, MD
Kalispell, Montana
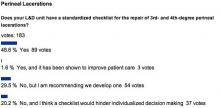
QUICK POLL RESULTS
Ensure adequate anesthesia
I appreciate the checklist. I would add to it an explicit statement that the patient must be well-anesthetized, up to and including any readministration of epidural anesthesia or intravenous conscious sedation.
Marcie Richardson, MD
Boston, Massachusetts
My experience repairing severe perineal lacerations
Dr. Barbieri’s column provided an excellent and timely summary! I have been repairing severe perineal lacerations consistently since I was taught a technique during my first year of residency in 1976. Since 1980, I have been at a community hospital with an average of 400 deliveries per year. In more than 33 years, I have had only one repair fail (knock wood!). It was readdressed without problems 1 month later after a low-residue diet, bowel prep, and other preparatory strategies. Interestingly, the patient delivered another 10-lb infant vaginally several years later with no problems, after a cesarean had been advised and declined.
Here is my rationale for the repair of severe lacerations:
- Identification of the extent of the laceration is the first and most important step. In many cases, a mucosal tear may be present in the setting of an intact transverse perineal muscle and even perineum.
- I have never had to move a patient to the OR, but sometimes I ask a nurse to hold retractors, as needed, especially if the patient is large. I use the Gelpi retractor for repair of every fourth-degree laceration.
- I have never given prophylactic antibiotics prior to repair of a third- or fourth-degree laceration. Known or suspected amnionitis or endometritis may be appropriate indications for such prophylaxis, however.
- The apex of the repair is critical, but I start a few millimeters above the laceration rather than 1 cm. Certainly more is better. The suture I use for the rectal mucosa is 3-0 GI chromic suture on a tapered needle in a running fashion, carried to the nadir of the tear. I tag that stitch to mark the lower limit of the repair. I then use the same type of suture to bring the internal anal sphincter and serosa together over the first layer in a running, interlocking fashion, knowing where to stop by virtue of the tagged stitch.
- I use 2-0 chromic figure-of-eight stitches for the external sphincter/transverse perineal muscle capsule at the 3, 6, 12, and 9 o’clock positions as suggested, which brings the clamps together in the midline. (They are removed prior to tying of the 9 o’clock stitch.) The position of the knots is not important, and I have always performed an end-to-end repair rather than overlapping. I always repair the vaginal portion of the tear or episiotomy before attending to the muscular portion of the perineal repair, as access to the vagina is more difficult to achieve afterward. If significant open space is noted behind or superior to the muscle repair, then interrupted stitches of 2-0 chromic suture can be used to approximate tissue and close dead space. The perineal skin is then closed in the usual fashion, down to the tagged initial stitch, or upward from it, if you prefer. Always perform a rectal exam at the conclusion to ensure that the repair is intact.
- I give stool softeners rather than laxatives twice daily for 2 weeks. After the initial 24 to 48 hours, I recommend use of a nonsteroidal anti-inflammatory drug for discomfort rather than medications that slow bowel transit time. I also recommend sitz baths four times daily for at least 1 week, after which they can be given as needed. Ice packs can be applied to the swollen perineum initially for relief of symptoms while the patient is on the postpartum service.
- Rarely has a patient needed to be seen before the normally scheduled postpartum visit. However, with reports of anal incontinence becoming more frequent in the literature, I make it a point to ask about this problem. I have had to refer only two patients for anal manometry, and neither patient had a fourth-degree laceration. Both patients delivered elsewhere.
I am not convinced that another checklist is needed, as we may end up with a cookbook approach if we aren’t careful. Just do the job correctly with a well-thought-out rationale for your approach.
Donald R. Wilson, MD
Maysville, Kentucky
A few questions about bowel preparation
I appreciate the clear-cut guidelines presented in this editorial. I have taught gynecology for 25 years at an Egyptian university. The addition of critical details to our surgical protocols will be of great help in improving outcomes. However, I have one major concern that was not mentioned in the article, and it involves bowel preparation.
Not all women undergo colon preparation and enema before coming to the labor room. Some are transferred from the emergency room or come to the hospital after home delivery. These women may have a full rectum and colon, sometimes even constipation with hard fecal matter, or they may have eaten recently.
How should these women be managed when a severe perineal laceration is present? Should the contaminated area be addressed first, followed by repair? Also, it seems to me that a full rectum and colon at the time of repair will place the sutures under undue stress, risking rupture with the patient’s first defecation.
In the past, we cleaned all areas of contamination with a povidone-iodine solution and administered a constipating regimen for 5 to 7 days postoperatively, with fluids and parenteral treatment, followed by laxatives and lactulose for 2 days before gradually incorporating a regular diet. Some physicians have proposed administering lactulose or a similar enema in the delivery room to evacuate bowel contents, followed by antisepsis, repair, and antibiotics.
I wonder how Dr. Barbieri would address this scenario?
Magdy Hassan Balaha, MD
Ahsaa, Saudi Arabia
More on the need for analgesia and anesthesia
I have a suggestion for checklists for the repair of severe perineal lacerations: Add an item mentioning the need to ensure adequate analgesia/anesthesia. Besides being kind to the patient, this step may facilitate exposure.
Also important is an environment that encourages consultation by any provider confronted with a perineal laceration of uncertain extent or unclear anatomy.
Nancy Kerr, MD, MPH
Telluride, Colorado, and Albuquerque, New Mexico
Fluids are important
When I repair fourth-degree lacerations, I use at least 1 L of normal saline in 100- to 200-cc aliquots throughout the repair.
Paul G. Crawford, MD
Shreveport, Louisiana
DR. BARBIERI RESPONDS:
We thank Dr. Kanoff, Dr. Shilkrut, Dr. Richardson, Dr. Wilson, Dr. Hassan Balaha, Dr. Kerr, and Dr. Crawford for their excellent additions to the perineal laceration checklist, all of which I support.
Dr. Richardson and Dr. Kerr specifically mention adequate analgesia/anesthesia, which is critically important to facilitate an optimal repair. Dr. Lavin mentions the repair of three sphincters: internal and external rectal sphincters and the superficial transverse perineal muscle. I am not aware that the superficial transverse perineal muscle is a classic “sphincter,” but it is important to include it in the repair of second-degree perineal lacerations.
Dr. Hassan Balaha asks about the handling of a contaminated field during repair. There are no randomized studies addressing this problem; most obstetricians will cleanse the area as well as possible and proceed with the repair. Dr. Hassan Balaha also recommends a two-step bowel regimen, involving a constipating regimen for 5 to 7 days, followed by laxatives and lactulose for 2 days BEFORE initiating a regular diet—a very interesting idea, which I will share with my colleagues. As noted in the editorial, the only clinical trial of this situation randomized women to a narcotic (constipating regimen) or a laxative regimen. The women in the laxative group reported earlier and less painful bowel movements than the women in the narcotic group.1
We want to hear from you! Tell us what you think.
Reference
- Mahony R, Behan M, O’Herlihy C, O’Connell PR. Randomised clinical trial of bowel confinement vs. laxative use after primary repair of a third degree obstetric anal sphincter tear. Dis Colon Rectum. 2004;47(1):12–17.
In a recent editorial, OBG Management Editor in Chief Dr. Robert L. Barbieri presented a draft checklist to guide clinicians during repair of third- and fourth-degree perineal lacerations. He also invited the journal’s readers to modify the checklist as they saw fit—and plenty of you responded! Here is a selection of the suggestions we received, with Dr. Barbieri’s reply.
How I adjusted my surgical protocol for the repair of severe perineal lacerations
I appreciate the clinical pearls offered by Dr. Robert Barbieri in his editorial on the repair of severe perineal lacerations. In response, I plan to change my protocol to initiate antibiotics prior to repair.
I would also offer this tip: When addressing the rectal mucosa, try to stay on a submucosal level, and perform a post-repair rectal exam to ensure that the mucosa has not been violated by a suture and to reduce the risk of rectovaginal fistula.
I repair the internal sphincter using an interrupted technique. And I place only three sutures in the external sphincter, at 8, 12, and 4 o’clock.
Martin E. Kanoff, DO
Sewell, New Jersey
A few pearls on checklist design
I am a big proponent of checklists and use them daily in my professional and personal life. However, as Atul Gawande, MD, MPH, mentioned in his book The Checklist Manifesto, checklists can’t teach a pilot how to fly a plane—that is best achieved through simulation. Dr. Gawande also noted that checklists should be short and to the point, usually containing no more than 10 items, and should highlight things more likely to be overlooked.
For the repair of perineal lacerations, a checklist might include:
- Call for help
- Consider repair in an OR
- Administer preoperative antibiotics
- Ensure adequate exposure and visualization
- Repair in layers (?)
- Postprocedure laxative
- Prophylaxis for deep venous thrombosis (?)
- Return to office in 1 week (?).
The items followed by a question mark are of uncertain value.
Ideally, each checklist should undergo validation via dry runs and team training. In my experience, it is not as difficult to design a checklist as to design a system where checklists get executed entirely and correctly.
Alex Shilkrut, MD
Safety Director, Department of Obstetrics and Gynecology, Metropolitan Hospital, New York, New York
A question about sphincters
I am grateful for Dr. Barbieri’s excellent editorial on using a checklist. I was taught that three sphincters require attention in 4th-degree lacerations: the internal anal sphincter, the external anal sphincter, and the superficial transverse perineal muscle. Would Dr. Barbieri agree?
John Lavin, MD
Kalispell, Montana
QUICK POLL RESULTS
Ensure adequate anesthesia
I appreciate the checklist. I would add to it an explicit statement that the patient must be well-anesthetized, up to and including any readministration of epidural anesthesia or intravenous conscious sedation.
Marcie Richardson, MD
Boston, Massachusetts
My experience repairing severe perineal lacerations
Dr. Barbieri’s column provided an excellent and timely summary! I have been repairing severe perineal lacerations consistently since I was taught a technique during my first year of residency in 1976. Since 1980, I have been at a community hospital with an average of 400 deliveries per year. In more than 33 years, I have had only one repair fail (knock wood!). It was readdressed without problems 1 month later after a low-residue diet, bowel prep, and other preparatory strategies. Interestingly, the patient delivered another 10-lb infant vaginally several years later with no problems, after a cesarean had been advised and declined.
Here is my rationale for the repair of severe lacerations:
- Identification of the extent of the laceration is the first and most important step. In many cases, a mucosal tear may be present in the setting of an intact transverse perineal muscle and even perineum.
- I have never had to move a patient to the OR, but sometimes I ask a nurse to hold retractors, as needed, especially if the patient is large. I use the Gelpi retractor for repair of every fourth-degree laceration.
- I have never given prophylactic antibiotics prior to repair of a third- or fourth-degree laceration. Known or suspected amnionitis or endometritis may be appropriate indications for such prophylaxis, however.
- The apex of the repair is critical, but I start a few millimeters above the laceration rather than 1 cm. Certainly more is better. The suture I use for the rectal mucosa is 3-0 GI chromic suture on a tapered needle in a running fashion, carried to the nadir of the tear. I tag that stitch to mark the lower limit of the repair. I then use the same type of suture to bring the internal anal sphincter and serosa together over the first layer in a running, interlocking fashion, knowing where to stop by virtue of the tagged stitch.
- I use 2-0 chromic figure-of-eight stitches for the external sphincter/transverse perineal muscle capsule at the 3, 6, 12, and 9 o’clock positions as suggested, which brings the clamps together in the midline. (They are removed prior to tying of the 9 o’clock stitch.) The position of the knots is not important, and I have always performed an end-to-end repair rather than overlapping. I always repair the vaginal portion of the tear or episiotomy before attending to the muscular portion of the perineal repair, as access to the vagina is more difficult to achieve afterward. If significant open space is noted behind or superior to the muscle repair, then interrupted stitches of 2-0 chromic suture can be used to approximate tissue and close dead space. The perineal skin is then closed in the usual fashion, down to the tagged initial stitch, or upward from it, if you prefer. Always perform a rectal exam at the conclusion to ensure that the repair is intact.
- I give stool softeners rather than laxatives twice daily for 2 weeks. After the initial 24 to 48 hours, I recommend use of a nonsteroidal anti-inflammatory drug for discomfort rather than medications that slow bowel transit time. I also recommend sitz baths four times daily for at least 1 week, after which they can be given as needed. Ice packs can be applied to the swollen perineum initially for relief of symptoms while the patient is on the postpartum service.
- Rarely has a patient needed to be seen before the normally scheduled postpartum visit. However, with reports of anal incontinence becoming more frequent in the literature, I make it a point to ask about this problem. I have had to refer only two patients for anal manometry, and neither patient had a fourth-degree laceration. Both patients delivered elsewhere.
I am not convinced that another checklist is needed, as we may end up with a cookbook approach if we aren’t careful. Just do the job correctly with a well-thought-out rationale for your approach.
Donald R. Wilson, MD
Maysville, Kentucky
A few questions about bowel preparation
I appreciate the clear-cut guidelines presented in this editorial. I have taught gynecology for 25 years at an Egyptian university. The addition of critical details to our surgical protocols will be of great help in improving outcomes. However, I have one major concern that was not mentioned in the article, and it involves bowel preparation.
Not all women undergo colon preparation and enema before coming to the labor room. Some are transferred from the emergency room or come to the hospital after home delivery. These women may have a full rectum and colon, sometimes even constipation with hard fecal matter, or they may have eaten recently.
How should these women be managed when a severe perineal laceration is present? Should the contaminated area be addressed first, followed by repair? Also, it seems to me that a full rectum and colon at the time of repair will place the sutures under undue stress, risking rupture with the patient’s first defecation.
In the past, we cleaned all areas of contamination with a povidone-iodine solution and administered a constipating regimen for 5 to 7 days postoperatively, with fluids and parenteral treatment, followed by laxatives and lactulose for 2 days before gradually incorporating a regular diet. Some physicians have proposed administering lactulose or a similar enema in the delivery room to evacuate bowel contents, followed by antisepsis, repair, and antibiotics.
I wonder how Dr. Barbieri would address this scenario?
Magdy Hassan Balaha, MD
Ahsaa, Saudi Arabia
More on the need for analgesia and anesthesia
I have a suggestion for checklists for the repair of severe perineal lacerations: Add an item mentioning the need to ensure adequate analgesia/anesthesia. Besides being kind to the patient, this step may facilitate exposure.
Also important is an environment that encourages consultation by any provider confronted with a perineal laceration of uncertain extent or unclear anatomy.
Nancy Kerr, MD, MPH
Telluride, Colorado, and Albuquerque, New Mexico
Fluids are important
When I repair fourth-degree lacerations, I use at least 1 L of normal saline in 100- to 200-cc aliquots throughout the repair.
Paul G. Crawford, MD
Shreveport, Louisiana
DR. BARBIERI RESPONDS:
We thank Dr. Kanoff, Dr. Shilkrut, Dr. Richardson, Dr. Wilson, Dr. Hassan Balaha, Dr. Kerr, and Dr. Crawford for their excellent additions to the perineal laceration checklist, all of which I support.
Dr. Richardson and Dr. Kerr specifically mention adequate analgesia/anesthesia, which is critically important to facilitate an optimal repair. Dr. Lavin mentions the repair of three sphincters: internal and external rectal sphincters and the superficial transverse perineal muscle. I am not aware that the superficial transverse perineal muscle is a classic “sphincter,” but it is important to include it in the repair of second-degree perineal lacerations.
Dr. Hassan Balaha asks about the handling of a contaminated field during repair. There are no randomized studies addressing this problem; most obstetricians will cleanse the area as well as possible and proceed with the repair. Dr. Hassan Balaha also recommends a two-step bowel regimen, involving a constipating regimen for 5 to 7 days, followed by laxatives and lactulose for 2 days BEFORE initiating a regular diet—a very interesting idea, which I will share with my colleagues. As noted in the editorial, the only clinical trial of this situation randomized women to a narcotic (constipating regimen) or a laxative regimen. The women in the laxative group reported earlier and less painful bowel movements than the women in the narcotic group.1
We want to hear from you! Tell us what you think.
In a recent editorial, OBG Management Editor in Chief Dr. Robert L. Barbieri presented a draft checklist to guide clinicians during repair of third- and fourth-degree perineal lacerations. He also invited the journal’s readers to modify the checklist as they saw fit—and plenty of you responded! Here is a selection of the suggestions we received, with Dr. Barbieri’s reply.
How I adjusted my surgical protocol for the repair of severe perineal lacerations
I appreciate the clinical pearls offered by Dr. Robert Barbieri in his editorial on the repair of severe perineal lacerations. In response, I plan to change my protocol to initiate antibiotics prior to repair.
I would also offer this tip: When addressing the rectal mucosa, try to stay on a submucosal level, and perform a post-repair rectal exam to ensure that the mucosa has not been violated by a suture and to reduce the risk of rectovaginal fistula.
I repair the internal sphincter using an interrupted technique. And I place only three sutures in the external sphincter, at 8, 12, and 4 o’clock.
Martin E. Kanoff, DO
Sewell, New Jersey
A few pearls on checklist design
I am a big proponent of checklists and use them daily in my professional and personal life. However, as Atul Gawande, MD, MPH, mentioned in his book The Checklist Manifesto, checklists can’t teach a pilot how to fly a plane—that is best achieved through simulation. Dr. Gawande also noted that checklists should be short and to the point, usually containing no more than 10 items, and should highlight things more likely to be overlooked.
For the repair of perineal lacerations, a checklist might include:
- Call for help
- Consider repair in an OR
- Administer preoperative antibiotics
- Ensure adequate exposure and visualization
- Repair in layers (?)
- Postprocedure laxative
- Prophylaxis for deep venous thrombosis (?)
- Return to office in 1 week (?).
The items followed by a question mark are of uncertain value.
Ideally, each checklist should undergo validation via dry runs and team training. In my experience, it is not as difficult to design a checklist as to design a system where checklists get executed entirely and correctly.
Alex Shilkrut, MD
Safety Director, Department of Obstetrics and Gynecology, Metropolitan Hospital, New York, New York
A question about sphincters
I am grateful for Dr. Barbieri’s excellent editorial on using a checklist. I was taught that three sphincters require attention in 4th-degree lacerations: the internal anal sphincter, the external anal sphincter, and the superficial transverse perineal muscle. Would Dr. Barbieri agree?
John Lavin, MD
Kalispell, Montana
QUICK POLL RESULTS
Ensure adequate anesthesia
I appreciate the checklist. I would add to it an explicit statement that the patient must be well-anesthetized, up to and including any readministration of epidural anesthesia or intravenous conscious sedation.
Marcie Richardson, MD
Boston, Massachusetts
My experience repairing severe perineal lacerations
Dr. Barbieri’s column provided an excellent and timely summary! I have been repairing severe perineal lacerations consistently since I was taught a technique during my first year of residency in 1976. Since 1980, I have been at a community hospital with an average of 400 deliveries per year. In more than 33 years, I have had only one repair fail (knock wood!). It was readdressed without problems 1 month later after a low-residue diet, bowel prep, and other preparatory strategies. Interestingly, the patient delivered another 10-lb infant vaginally several years later with no problems, after a cesarean had been advised and declined.
Here is my rationale for the repair of severe lacerations:
- Identification of the extent of the laceration is the first and most important step. In many cases, a mucosal tear may be present in the setting of an intact transverse perineal muscle and even perineum.
- I have never had to move a patient to the OR, but sometimes I ask a nurse to hold retractors, as needed, especially if the patient is large. I use the Gelpi retractor for repair of every fourth-degree laceration.
- I have never given prophylactic antibiotics prior to repair of a third- or fourth-degree laceration. Known or suspected amnionitis or endometritis may be appropriate indications for such prophylaxis, however.
- The apex of the repair is critical, but I start a few millimeters above the laceration rather than 1 cm. Certainly more is better. The suture I use for the rectal mucosa is 3-0 GI chromic suture on a tapered needle in a running fashion, carried to the nadir of the tear. I tag that stitch to mark the lower limit of the repair. I then use the same type of suture to bring the internal anal sphincter and serosa together over the first layer in a running, interlocking fashion, knowing where to stop by virtue of the tagged stitch.
- I use 2-0 chromic figure-of-eight stitches for the external sphincter/transverse perineal muscle capsule at the 3, 6, 12, and 9 o’clock positions as suggested, which brings the clamps together in the midline. (They are removed prior to tying of the 9 o’clock stitch.) The position of the knots is not important, and I have always performed an end-to-end repair rather than overlapping. I always repair the vaginal portion of the tear or episiotomy before attending to the muscular portion of the perineal repair, as access to the vagina is more difficult to achieve afterward. If significant open space is noted behind or superior to the muscle repair, then interrupted stitches of 2-0 chromic suture can be used to approximate tissue and close dead space. The perineal skin is then closed in the usual fashion, down to the tagged initial stitch, or upward from it, if you prefer. Always perform a rectal exam at the conclusion to ensure that the repair is intact.
- I give stool softeners rather than laxatives twice daily for 2 weeks. After the initial 24 to 48 hours, I recommend use of a nonsteroidal anti-inflammatory drug for discomfort rather than medications that slow bowel transit time. I also recommend sitz baths four times daily for at least 1 week, after which they can be given as needed. Ice packs can be applied to the swollen perineum initially for relief of symptoms while the patient is on the postpartum service.
- Rarely has a patient needed to be seen before the normally scheduled postpartum visit. However, with reports of anal incontinence becoming more frequent in the literature, I make it a point to ask about this problem. I have had to refer only two patients for anal manometry, and neither patient had a fourth-degree laceration. Both patients delivered elsewhere.
I am not convinced that another checklist is needed, as we may end up with a cookbook approach if we aren’t careful. Just do the job correctly with a well-thought-out rationale for your approach.
Donald R. Wilson, MD
Maysville, Kentucky
A few questions about bowel preparation
I appreciate the clear-cut guidelines presented in this editorial. I have taught gynecology for 25 years at an Egyptian university. The addition of critical details to our surgical protocols will be of great help in improving outcomes. However, I have one major concern that was not mentioned in the article, and it involves bowel preparation.
Not all women undergo colon preparation and enema before coming to the labor room. Some are transferred from the emergency room or come to the hospital after home delivery. These women may have a full rectum and colon, sometimes even constipation with hard fecal matter, or they may have eaten recently.
How should these women be managed when a severe perineal laceration is present? Should the contaminated area be addressed first, followed by repair? Also, it seems to me that a full rectum and colon at the time of repair will place the sutures under undue stress, risking rupture with the patient’s first defecation.
In the past, we cleaned all areas of contamination with a povidone-iodine solution and administered a constipating regimen for 5 to 7 days postoperatively, with fluids and parenteral treatment, followed by laxatives and lactulose for 2 days before gradually incorporating a regular diet. Some physicians have proposed administering lactulose or a similar enema in the delivery room to evacuate bowel contents, followed by antisepsis, repair, and antibiotics.
I wonder how Dr. Barbieri would address this scenario?
Magdy Hassan Balaha, MD
Ahsaa, Saudi Arabia
More on the need for analgesia and anesthesia
I have a suggestion for checklists for the repair of severe perineal lacerations: Add an item mentioning the need to ensure adequate analgesia/anesthesia. Besides being kind to the patient, this step may facilitate exposure.
Also important is an environment that encourages consultation by any provider confronted with a perineal laceration of uncertain extent or unclear anatomy.
Nancy Kerr, MD, MPH
Telluride, Colorado, and Albuquerque, New Mexico
Fluids are important
When I repair fourth-degree lacerations, I use at least 1 L of normal saline in 100- to 200-cc aliquots throughout the repair.
Paul G. Crawford, MD
Shreveport, Louisiana
DR. BARBIERI RESPONDS:
We thank Dr. Kanoff, Dr. Shilkrut, Dr. Richardson, Dr. Wilson, Dr. Hassan Balaha, Dr. Kerr, and Dr. Crawford for their excellent additions to the perineal laceration checklist, all of which I support.
Dr. Richardson and Dr. Kerr specifically mention adequate analgesia/anesthesia, which is critically important to facilitate an optimal repair. Dr. Lavin mentions the repair of three sphincters: internal and external rectal sphincters and the superficial transverse perineal muscle. I am not aware that the superficial transverse perineal muscle is a classic “sphincter,” but it is important to include it in the repair of second-degree perineal lacerations.
Dr. Hassan Balaha asks about the handling of a contaminated field during repair. There are no randomized studies addressing this problem; most obstetricians will cleanse the area as well as possible and proceed with the repair. Dr. Hassan Balaha also recommends a two-step bowel regimen, involving a constipating regimen for 5 to 7 days, followed by laxatives and lactulose for 2 days BEFORE initiating a regular diet—a very interesting idea, which I will share with my colleagues. As noted in the editorial, the only clinical trial of this situation randomized women to a narcotic (constipating regimen) or a laxative regimen. The women in the laxative group reported earlier and less painful bowel movements than the women in the narcotic group.1
We want to hear from you! Tell us what you think.
Reference
- Mahony R, Behan M, O’Herlihy C, O’Connell PR. Randomised clinical trial of bowel confinement vs. laxative use after primary repair of a third degree obstetric anal sphincter tear. Dis Colon Rectum. 2004;47(1):12–17.
Reference
- Mahony R, Behan M, O’Herlihy C, O’Connell PR. Randomised clinical trial of bowel confinement vs. laxative use after primary repair of a third degree obstetric anal sphincter tear. Dis Colon Rectum. 2004;47(1):12–17.