User login
Ulcerative colitis (UC) is an autoimmune-related inflammatory bowel disease (IBD). It typically develops in the rectum and extends to involve the large intestine. Pediatric UC can have a more severe phenotype than adult disease and may affect a child's pubertal development, bone mineral density, nutrition levels, and social life. It is currently theorized that the age at diagnosis and sex of the patient do not predict disease activity.
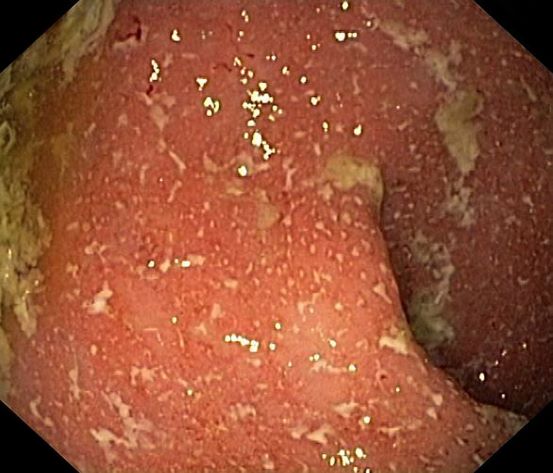
UC disease can announce itself as mild, moderate, or severe, and the Pediatric Ulcerative Colitis Activity Index (PUCAI) endoscopic grading is used as a clinical scoring system. The most common presenting symptoms are rectal bleeding, diarrhea, and abdominal pain; among children, the presentation can vary.
Crohns disease, another IBD, must be carefully ruled out of the differential. Colonoscopy represents the first-line approach in the diagnosis of IBD. The findings that would suggest Crohns disease are sparing of the rectal mucosa, aphthous ulceration, and noncontiguous (or skip) lesions. Micronutrient and vitamin levels are usually low in Crohns disease. And although weight loss, perineal disease, fistulae, and obstruction are commonly seen in the context of Crohns disease, they are uncommon or rare in UC. Bleeding is observed much more frequently in UC.
During UC workup, elevated erythrocyte sedimentation rate and C-reactive protein level often serve as markers of disease activity. Antineutrophil cytoplasmic antibody (ANCA) test is frequently used with suspected UC (though this measure may not correlate with disease activity). In addition, a broad metabolic panel should be performed, along with stool cultures, to rule out infection.
The goals of pediatric UC management are to maintain control of the disease, extend periods of remission, and reduce long-term damage caused by inflammation, all while potentially allowing the patient to function as normally as possible. Anti-inflammatory therapy with 5-aminosalicylic acid agents, such as sulfasalazine and mesalamine, is foundational to treatment. Acute flares of UC in the pediatric population are usually responsive to corticosteroids, but these regimens should be short-term only. Immunomodulatory agents, tumor necrosis factor inhibitors, and newer therapies such as monoclonal antibodies are also used during flares, but only a minority of patients will require these therapies. These are also considered treatment alternatives for patients who are steroid-dependent or steroid-refractory.
Bhupinder S. Anand, MD, Professor, Department of Medicine, Baylor College of Medicine, Houston, TX
Bhupinder S. Anand, MD, has disclosed no relevant financial relationships
Ulcerative colitis (UC) is an autoimmune-related inflammatory bowel disease (IBD). It typically develops in the rectum and extends to involve the large intestine. Pediatric UC can have a more severe phenotype than adult disease and may affect a child's pubertal development, bone mineral density, nutrition levels, and social life. It is currently theorized that the age at diagnosis and sex of the patient do not predict disease activity.
UC disease can announce itself as mild, moderate, or severe, and the Pediatric Ulcerative Colitis Activity Index (PUCAI) endoscopic grading is used as a clinical scoring system. The most common presenting symptoms are rectal bleeding, diarrhea, and abdominal pain; among children, the presentation can vary.
Crohns disease, another IBD, must be carefully ruled out of the differential. Colonoscopy represents the first-line approach in the diagnosis of IBD. The findings that would suggest Crohns disease are sparing of the rectal mucosa, aphthous ulceration, and noncontiguous (or skip) lesions. Micronutrient and vitamin levels are usually low in Crohns disease. And although weight loss, perineal disease, fistulae, and obstruction are commonly seen in the context of Crohns disease, they are uncommon or rare in UC. Bleeding is observed much more frequently in UC.
During UC workup, elevated erythrocyte sedimentation rate and C-reactive protein level often serve as markers of disease activity. Antineutrophil cytoplasmic antibody (ANCA) test is frequently used with suspected UC (though this measure may not correlate with disease activity). In addition, a broad metabolic panel should be performed, along with stool cultures, to rule out infection.
The goals of pediatric UC management are to maintain control of the disease, extend periods of remission, and reduce long-term damage caused by inflammation, all while potentially allowing the patient to function as normally as possible. Anti-inflammatory therapy with 5-aminosalicylic acid agents, such as sulfasalazine and mesalamine, is foundational to treatment. Acute flares of UC in the pediatric population are usually responsive to corticosteroids, but these regimens should be short-term only. Immunomodulatory agents, tumor necrosis factor inhibitors, and newer therapies such as monoclonal antibodies are also used during flares, but only a minority of patients will require these therapies. These are also considered treatment alternatives for patients who are steroid-dependent or steroid-refractory.
Bhupinder S. Anand, MD, Professor, Department of Medicine, Baylor College of Medicine, Houston, TX
Bhupinder S. Anand, MD, has disclosed no relevant financial relationships
Ulcerative colitis (UC) is an autoimmune-related inflammatory bowel disease (IBD). It typically develops in the rectum and extends to involve the large intestine. Pediatric UC can have a more severe phenotype than adult disease and may affect a child's pubertal development, bone mineral density, nutrition levels, and social life. It is currently theorized that the age at diagnosis and sex of the patient do not predict disease activity.
UC disease can announce itself as mild, moderate, or severe, and the Pediatric Ulcerative Colitis Activity Index (PUCAI) endoscopic grading is used as a clinical scoring system. The most common presenting symptoms are rectal bleeding, diarrhea, and abdominal pain; among children, the presentation can vary.
Crohns disease, another IBD, must be carefully ruled out of the differential. Colonoscopy represents the first-line approach in the diagnosis of IBD. The findings that would suggest Crohns disease are sparing of the rectal mucosa, aphthous ulceration, and noncontiguous (or skip) lesions. Micronutrient and vitamin levels are usually low in Crohns disease. And although weight loss, perineal disease, fistulae, and obstruction are commonly seen in the context of Crohns disease, they are uncommon or rare in UC. Bleeding is observed much more frequently in UC.
During UC workup, elevated erythrocyte sedimentation rate and C-reactive protein level often serve as markers of disease activity. Antineutrophil cytoplasmic antibody (ANCA) test is frequently used with suspected UC (though this measure may not correlate with disease activity). In addition, a broad metabolic panel should be performed, along with stool cultures, to rule out infection.
The goals of pediatric UC management are to maintain control of the disease, extend periods of remission, and reduce long-term damage caused by inflammation, all while potentially allowing the patient to function as normally as possible. Anti-inflammatory therapy with 5-aminosalicylic acid agents, such as sulfasalazine and mesalamine, is foundational to treatment. Acute flares of UC in the pediatric population are usually responsive to corticosteroids, but these regimens should be short-term only. Immunomodulatory agents, tumor necrosis factor inhibitors, and newer therapies such as monoclonal antibodies are also used during flares, but only a minority of patients will require these therapies. These are also considered treatment alternatives for patients who are steroid-dependent or steroid-refractory.
Bhupinder S. Anand, MD, Professor, Department of Medicine, Baylor College of Medicine, Houston, TX
Bhupinder S. Anand, MD, has disclosed no relevant financial relationships
A 5-year-old boy presents with abdominal cramping and bloody stools over the course of 2 days. His mother explains that the onset of diarrhea was insidious. Because the patient has a sensitive stomach, she tries to keep his diet relatively bland, but she worries about what he eats at school. He is slightly underweight for his age group. The family has not traveled recently. The patient does not have a fever, but skin turgor is decreased. There is no evidence of fistulae or abscesses. His complete blood cell count is 10.6 g/dL.