User login
Among patients with Chagas cardiomyopathy, trypanocidal therapy with benznidazole significantly reduced serum parasite detection but did not reduce cardiac clinical deterioration through 5 years of follow-up, a randomized trial showed.
Those are key findings from the Benznidazole Evaluation for Interrupting Trypanosomiasis (BENEFIT) trial, which were presented at the annual congress of the European Society of Cardiology and published simultaneously in the New England Journal of Medicine (doi: 10.1056/NEJMoa1507574).
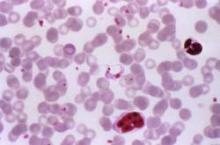
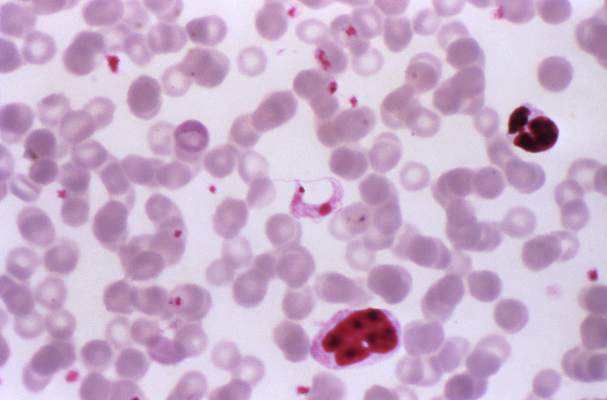
According to lead study authors Dr. Carlos A. Morillo of the Population Health Research Institute at Hamilton Health Sciences and McMaster University, Hamilton, Ont., and Dr. Jose Antonio Marin-Neto of the division of cardiology at the Medical School of Riberao Preto, Brazil, Chagas cardiomyopathy develops in about one-quarter of patients infected with Trypanosoma cruzi. “The identification of T. cruzi antigens in inflamed myocardium with the use of sensitive techniques, such as immunohistochemical analysis and polymerase chain reaction (PCR) assay, suggests that parasite persistence may be an important factor that, in conjunction with individual host factors, triggers the inflammatory process,” they wrote. “In assessing whether trypanocidal therapy prevents or reduces cardiac disease, experimental models of chronic Chagas infection have shown that trypanocidal therapy attenuates the pathologic consequences by reducing the parasite burden. A few small observational and randomized studies involving patients with Chagas disease have shown that benznidazole reduced the circulating parasite load, enhances seroconversion, and may halt the progression of cardiomyopathy.”
In a study of 2,854 patients with chronic Chagas cardiomyopathy conducted at 49 centers in Argentina, Bolivia, Brazil, Columbia, and El Salvador, the researchers set out to evaluate the efficacy and safety of benznidazole, compared with placebo, in reducing the clinical outcomes in patients with chronic Chagas cardiomyopathy. Of the 2,854 patients, slightly more than half (1,431) received benznidazole, while the remaining 1,423 received placebo for up to 80 days and were followed for a mean of 5.4 years. The primary outcome was the first event of any of the components of the composite outcome of death, resuscitated cardiac arrest, sustained ventricular tachycardia, insertion of a pacemaker or implantable cardioverter-defibrillator, cardiac transplantation, new heart failure, stroke, or other thromboembolic event. Secondary outcomes included the response to treatment on the basis of results on PCR assay overall and according to geographic region.
The proportion of study participants who achieved the primary outcome was statistically similar between the two groups: 27.% in the benznidazole group, compared with 29.1% in the placebo group (adjusted hazard ratio of .092; P = .26). The researchers observed no significant between-group differences in any component of the primary outcome.
In terms of secondary outcomes, the rates of conversion to negative PCR results were 66.2% in the benznidazole group, compared with 33.5% in the placebo group at the end of treatment. Between-group differences were sustained at 2 years (55.4% and 35.3%, respectively) and at 5 years or more (46.7% vs. 33.1%; P less than .001 for all comparisons). At the same time, rates of PCR conversion varied according to geographic region. For example, the odds ratio for PCR conversion was highest in Brazil (odds ratio, 3.03 at 2 years and OR, 1.87 at 5 or more years) and lowest in Columbia and El Salvador (OR, 1.33 at 2 years and OR, 0.96 at 5 years). “Since we do not have genotype information, we had to infer that patients in certain geographic regions were likely to have distinct T. cruzi strains,” the authors wrote.
They acknowledged certain limitations of the study, including the fact that “variable responses to benznidazole have been reported previously and may have contributed to our neutral findings. Further analyses of stored blood samples by means of quantitative PCR and genotyping may provide a more precise characterization of T. cruzi that can be used to assess whether genotype influences the clinical response to benznidazole.”
They concluded that the current findings “do not challenge current guidelines that recommend treatment with trypanocidal therapy in the early stages of chronic Chagas infection. ... and should not detract from the pursuit of general goals for exploring more effective or earlier treatments with new drugs or drug combinations.”
The study was funded by several sources, including the Population Health Research Institute, the Canadian Institutes of Health Research, the United Nations Children’s Fund, and the World Bank. Dr. Morillo disclosed that he has received lecture fees from Bayer and Boehringer Ingelheim and grant support from Boston Scientific and Merck & Co. Another study author, Dr. Janis Lazdins, disclosed having received consulting fees from Merck. The remaining study authors reporting having no financial disclosures.
Among patients with Chagas cardiomyopathy, trypanocidal therapy with benznidazole significantly reduced serum parasite detection but did not reduce cardiac clinical deterioration through 5 years of follow-up, a randomized trial showed.
Those are key findings from the Benznidazole Evaluation for Interrupting Trypanosomiasis (BENEFIT) trial, which were presented at the annual congress of the European Society of Cardiology and published simultaneously in the New England Journal of Medicine (doi: 10.1056/NEJMoa1507574).
According to lead study authors Dr. Carlos A. Morillo of the Population Health Research Institute at Hamilton Health Sciences and McMaster University, Hamilton, Ont., and Dr. Jose Antonio Marin-Neto of the division of cardiology at the Medical School of Riberao Preto, Brazil, Chagas cardiomyopathy develops in about one-quarter of patients infected with Trypanosoma cruzi. “The identification of T. cruzi antigens in inflamed myocardium with the use of sensitive techniques, such as immunohistochemical analysis and polymerase chain reaction (PCR) assay, suggests that parasite persistence may be an important factor that, in conjunction with individual host factors, triggers the inflammatory process,” they wrote. “In assessing whether trypanocidal therapy prevents or reduces cardiac disease, experimental models of chronic Chagas infection have shown that trypanocidal therapy attenuates the pathologic consequences by reducing the parasite burden. A few small observational and randomized studies involving patients with Chagas disease have shown that benznidazole reduced the circulating parasite load, enhances seroconversion, and may halt the progression of cardiomyopathy.”
In a study of 2,854 patients with chronic Chagas cardiomyopathy conducted at 49 centers in Argentina, Bolivia, Brazil, Columbia, and El Salvador, the researchers set out to evaluate the efficacy and safety of benznidazole, compared with placebo, in reducing the clinical outcomes in patients with chronic Chagas cardiomyopathy. Of the 2,854 patients, slightly more than half (1,431) received benznidazole, while the remaining 1,423 received placebo for up to 80 days and were followed for a mean of 5.4 years. The primary outcome was the first event of any of the components of the composite outcome of death, resuscitated cardiac arrest, sustained ventricular tachycardia, insertion of a pacemaker or implantable cardioverter-defibrillator, cardiac transplantation, new heart failure, stroke, or other thromboembolic event. Secondary outcomes included the response to treatment on the basis of results on PCR assay overall and according to geographic region.
The proportion of study participants who achieved the primary outcome was statistically similar between the two groups: 27.% in the benznidazole group, compared with 29.1% in the placebo group (adjusted hazard ratio of .092; P = .26). The researchers observed no significant between-group differences in any component of the primary outcome.
In terms of secondary outcomes, the rates of conversion to negative PCR results were 66.2% in the benznidazole group, compared with 33.5% in the placebo group at the end of treatment. Between-group differences were sustained at 2 years (55.4% and 35.3%, respectively) and at 5 years or more (46.7% vs. 33.1%; P less than .001 for all comparisons). At the same time, rates of PCR conversion varied according to geographic region. For example, the odds ratio for PCR conversion was highest in Brazil (odds ratio, 3.03 at 2 years and OR, 1.87 at 5 or more years) and lowest in Columbia and El Salvador (OR, 1.33 at 2 years and OR, 0.96 at 5 years). “Since we do not have genotype information, we had to infer that patients in certain geographic regions were likely to have distinct T. cruzi strains,” the authors wrote.
They acknowledged certain limitations of the study, including the fact that “variable responses to benznidazole have been reported previously and may have contributed to our neutral findings. Further analyses of stored blood samples by means of quantitative PCR and genotyping may provide a more precise characterization of T. cruzi that can be used to assess whether genotype influences the clinical response to benznidazole.”
They concluded that the current findings “do not challenge current guidelines that recommend treatment with trypanocidal therapy in the early stages of chronic Chagas infection. ... and should not detract from the pursuit of general goals for exploring more effective or earlier treatments with new drugs or drug combinations.”
The study was funded by several sources, including the Population Health Research Institute, the Canadian Institutes of Health Research, the United Nations Children’s Fund, and the World Bank. Dr. Morillo disclosed that he has received lecture fees from Bayer and Boehringer Ingelheim and grant support from Boston Scientific and Merck & Co. Another study author, Dr. Janis Lazdins, disclosed having received consulting fees from Merck. The remaining study authors reporting having no financial disclosures.
Among patients with Chagas cardiomyopathy, trypanocidal therapy with benznidazole significantly reduced serum parasite detection but did not reduce cardiac clinical deterioration through 5 years of follow-up, a randomized trial showed.
Those are key findings from the Benznidazole Evaluation for Interrupting Trypanosomiasis (BENEFIT) trial, which were presented at the annual congress of the European Society of Cardiology and published simultaneously in the New England Journal of Medicine (doi: 10.1056/NEJMoa1507574).
According to lead study authors Dr. Carlos A. Morillo of the Population Health Research Institute at Hamilton Health Sciences and McMaster University, Hamilton, Ont., and Dr. Jose Antonio Marin-Neto of the division of cardiology at the Medical School of Riberao Preto, Brazil, Chagas cardiomyopathy develops in about one-quarter of patients infected with Trypanosoma cruzi. “The identification of T. cruzi antigens in inflamed myocardium with the use of sensitive techniques, such as immunohistochemical analysis and polymerase chain reaction (PCR) assay, suggests that parasite persistence may be an important factor that, in conjunction with individual host factors, triggers the inflammatory process,” they wrote. “In assessing whether trypanocidal therapy prevents or reduces cardiac disease, experimental models of chronic Chagas infection have shown that trypanocidal therapy attenuates the pathologic consequences by reducing the parasite burden. A few small observational and randomized studies involving patients with Chagas disease have shown that benznidazole reduced the circulating parasite load, enhances seroconversion, and may halt the progression of cardiomyopathy.”
In a study of 2,854 patients with chronic Chagas cardiomyopathy conducted at 49 centers in Argentina, Bolivia, Brazil, Columbia, and El Salvador, the researchers set out to evaluate the efficacy and safety of benznidazole, compared with placebo, in reducing the clinical outcomes in patients with chronic Chagas cardiomyopathy. Of the 2,854 patients, slightly more than half (1,431) received benznidazole, while the remaining 1,423 received placebo for up to 80 days and were followed for a mean of 5.4 years. The primary outcome was the first event of any of the components of the composite outcome of death, resuscitated cardiac arrest, sustained ventricular tachycardia, insertion of a pacemaker or implantable cardioverter-defibrillator, cardiac transplantation, new heart failure, stroke, or other thromboembolic event. Secondary outcomes included the response to treatment on the basis of results on PCR assay overall and according to geographic region.
The proportion of study participants who achieved the primary outcome was statistically similar between the two groups: 27.% in the benznidazole group, compared with 29.1% in the placebo group (adjusted hazard ratio of .092; P = .26). The researchers observed no significant between-group differences in any component of the primary outcome.
In terms of secondary outcomes, the rates of conversion to negative PCR results were 66.2% in the benznidazole group, compared with 33.5% in the placebo group at the end of treatment. Between-group differences were sustained at 2 years (55.4% and 35.3%, respectively) and at 5 years or more (46.7% vs. 33.1%; P less than .001 for all comparisons). At the same time, rates of PCR conversion varied according to geographic region. For example, the odds ratio for PCR conversion was highest in Brazil (odds ratio, 3.03 at 2 years and OR, 1.87 at 5 or more years) and lowest in Columbia and El Salvador (OR, 1.33 at 2 years and OR, 0.96 at 5 years). “Since we do not have genotype information, we had to infer that patients in certain geographic regions were likely to have distinct T. cruzi strains,” the authors wrote.
They acknowledged certain limitations of the study, including the fact that “variable responses to benznidazole have been reported previously and may have contributed to our neutral findings. Further analyses of stored blood samples by means of quantitative PCR and genotyping may provide a more precise characterization of T. cruzi that can be used to assess whether genotype influences the clinical response to benznidazole.”
They concluded that the current findings “do not challenge current guidelines that recommend treatment with trypanocidal therapy in the early stages of chronic Chagas infection. ... and should not detract from the pursuit of general goals for exploring more effective or earlier treatments with new drugs or drug combinations.”
The study was funded by several sources, including the Population Health Research Institute, the Canadian Institutes of Health Research, the United Nations Children’s Fund, and the World Bank. Dr. Morillo disclosed that he has received lecture fees from Bayer and Boehringer Ingelheim and grant support from Boston Scientific and Merck & Co. Another study author, Dr. Janis Lazdins, disclosed having received consulting fees from Merck. The remaining study authors reporting having no financial disclosures.
FROM THE ESC CONGRESS 2015
Key clinical point: Benznidazole for Chagas cardiomyopathy did not reduce long-term cardiac clinical deterioration.
Major finding: The proportion of study participants who achieved the primary outcome was statistically similar between the two groups: 27.% in the benznidazole group, compared with 29.1% in the placebo group (adjusted hazard ratio of .92; P = .26).
Data source: A prospective, randomized trial in which 2,854 patients with Chagas cardiomyopathy received benznidazole or placebo for up to 80 days and were followed for a mean of 5.4 years.
Disclosures: The study was funded by several sources, including the Population Health Research Institute, the Canadian Institutes of Health Research, the United Nations Children’s Fund, and the World Bank. Dr. Morillo disclosed that he has received lecture fees from Bayer and Boehringer Ingelheim and grant support from Boston Scientific and Merck & Co. Another study author, Dr. Janis Lazdins, disclosed having received consulting fees from Merck. The remaining study authors reported having no financial disclosures.