User login
Tom Collins is a freelance writer in South Florida who has written about medical topics from nasty infections to ethical dilemmas, runaway tumors to tornado-chasing doctors. He travels the globe gathering conference health news and lives in West Palm Beach.
Best of RIV highlights delirium, alcohol detox, and med rec projects
A project to improve how hospitalists address inpatient delirium, which has led to reductions in length of stay and cost, took center stage on Tuesday morning at HM19 in the Best of RIV plenary session.
The project, conducted at the University of California, San Francisco (UCSF), was presented alongside projects on alcohol detox at the Cleveland Veterans Affairs Medical Center and on medication reconciliation at Brigham and Women’s Hospital in Boston.
“The plenary is the top three of the 1,000 that are out there – so, impressive work,” said Benji Mathews, MD, SFHM, the chair of the Research, Innovations and Vignettes competition.
At UCSF, the project was meant to tackle the huge problem of delirium in the hospital, said Catherine Lau, MD, SFHM, associate professor of medicine there. Each year delirium affects more than 7 million people who are hospitalized, and hospital-acquired delirium is linked with prolonged stays and more emergency department visits and hospital readmissions. But research has found that as many as a third of these hospital-acquired cases can be prevented, Dr. Lau said.
New admissions and transfers – a total of more than 2,800 patients – were assessed for delirium risk, and those deemed high risk were entered into a delirium care plan, aimed at prevention with nonpharmacologic steps such as maximizing their mobility and helping them sleep at night.
All patients also were screened on every nursing shift for delirium, and those diagnosed with the disorder were placed in the delirium care plan, with notification of the patient’s team for treatment.
The average length of stay decreased by 0.8 days (P less than .001), with a decrease of 1.9 days in patients with delirium, compared with outcomes for nearly 2,600 patients before the intervention was implemented, Dr. Lau said. Researchers also found a decrease in $850 spent per patient (P less than .001), with a direct savings to the hospital of a total of $997,000, she said. The 30-day readmission rate also fell significantly, from 18.9% to 15.9% (P = .03).
The screening itself seemed to be the most important factor in the project, Dr. Lau said.
“Just the recognition that their patient was at risk for delirium or actually had delirium really raised awareness,” she said.
The project on alcohol detox used careful risk assessments at emergency department discharge, e-consults, protocols to limit benzodiazepine prescribing, and telephone follow-up to reduce hospital admissions and 30-day readmissions, as well as length of stay.
Researchers used scores on CIWA – a 10-question measurement of the severity of someone’s alcohol withdrawal – and history of complicated alcohol-use withdrawal to determine whether ED patients should be admitted to the floor or sent home with or without prescriptions for gabapentin and lorazepam, said Robert Patrick, MD, a hospitalist at the Cleveland VA.
Perhaps the most innovative feature of the program was using systolic blood pressure and heart rate in addition to CIWA to determine whether someone should receive a benzodiazepine, he said. Someone with a CIWA of 9-12, for instance, would be prescribed one of these drugs only if their vitals were elevated, Dr. Patrick said.
He encouraged other hospitalists to try a similar program at their centers.
“You don’t have to be at a VA to do this,” he said. “And most importantly, you don’t have to have a cooperative ED to do this. You can do this just within your hospitalist group.”
In another presentation, Jeffrey Schnipper, MD, MPH, FHM, associate professor of medicine at Harvard Medical School, Boston, described the results from a project in which SHM’s MARQUIS program – an evidence-based “toolkit” on medication reconciliation – was implemented at 18 hospitals. The kit offers a plan to get the best possible medication history, give medication counseling on discharge, and identify patients at risk for medication discrepancies. The 18 sites were coached, with areas of improvement identified.
By months 13-18 of the study period, the number of medication discrepancies had fallen to 0.93 per patient for those who’d received at least one form of intervention, compared with 2.69 per patient among those who’d received none.
“The MARQUIS interventions, including the toolkit and mentored implementation,” Dr. Schnipper said, “are associated with a marked reduction in medication discrepancies.”
A project to improve how hospitalists address inpatient delirium, which has led to reductions in length of stay and cost, took center stage on Tuesday morning at HM19 in the Best of RIV plenary session.
The project, conducted at the University of California, San Francisco (UCSF), was presented alongside projects on alcohol detox at the Cleveland Veterans Affairs Medical Center and on medication reconciliation at Brigham and Women’s Hospital in Boston.
“The plenary is the top three of the 1,000 that are out there – so, impressive work,” said Benji Mathews, MD, SFHM, the chair of the Research, Innovations and Vignettes competition.
At UCSF, the project was meant to tackle the huge problem of delirium in the hospital, said Catherine Lau, MD, SFHM, associate professor of medicine there. Each year delirium affects more than 7 million people who are hospitalized, and hospital-acquired delirium is linked with prolonged stays and more emergency department visits and hospital readmissions. But research has found that as many as a third of these hospital-acquired cases can be prevented, Dr. Lau said.
New admissions and transfers – a total of more than 2,800 patients – were assessed for delirium risk, and those deemed high risk were entered into a delirium care plan, aimed at prevention with nonpharmacologic steps such as maximizing their mobility and helping them sleep at night.
All patients also were screened on every nursing shift for delirium, and those diagnosed with the disorder were placed in the delirium care plan, with notification of the patient’s team for treatment.
The average length of stay decreased by 0.8 days (P less than .001), with a decrease of 1.9 days in patients with delirium, compared with outcomes for nearly 2,600 patients before the intervention was implemented, Dr. Lau said. Researchers also found a decrease in $850 spent per patient (P less than .001), with a direct savings to the hospital of a total of $997,000, she said. The 30-day readmission rate also fell significantly, from 18.9% to 15.9% (P = .03).
The screening itself seemed to be the most important factor in the project, Dr. Lau said.
“Just the recognition that their patient was at risk for delirium or actually had delirium really raised awareness,” she said.
The project on alcohol detox used careful risk assessments at emergency department discharge, e-consults, protocols to limit benzodiazepine prescribing, and telephone follow-up to reduce hospital admissions and 30-day readmissions, as well as length of stay.
Researchers used scores on CIWA – a 10-question measurement of the severity of someone’s alcohol withdrawal – and history of complicated alcohol-use withdrawal to determine whether ED patients should be admitted to the floor or sent home with or without prescriptions for gabapentin and lorazepam, said Robert Patrick, MD, a hospitalist at the Cleveland VA.
Perhaps the most innovative feature of the program was using systolic blood pressure and heart rate in addition to CIWA to determine whether someone should receive a benzodiazepine, he said. Someone with a CIWA of 9-12, for instance, would be prescribed one of these drugs only if their vitals were elevated, Dr. Patrick said.
He encouraged other hospitalists to try a similar program at their centers.
“You don’t have to be at a VA to do this,” he said. “And most importantly, you don’t have to have a cooperative ED to do this. You can do this just within your hospitalist group.”
In another presentation, Jeffrey Schnipper, MD, MPH, FHM, associate professor of medicine at Harvard Medical School, Boston, described the results from a project in which SHM’s MARQUIS program – an evidence-based “toolkit” on medication reconciliation – was implemented at 18 hospitals. The kit offers a plan to get the best possible medication history, give medication counseling on discharge, and identify patients at risk for medication discrepancies. The 18 sites were coached, with areas of improvement identified.
By months 13-18 of the study period, the number of medication discrepancies had fallen to 0.93 per patient for those who’d received at least one form of intervention, compared with 2.69 per patient among those who’d received none.
“The MARQUIS interventions, including the toolkit and mentored implementation,” Dr. Schnipper said, “are associated with a marked reduction in medication discrepancies.”
A project to improve how hospitalists address inpatient delirium, which has led to reductions in length of stay and cost, took center stage on Tuesday morning at HM19 in the Best of RIV plenary session.
The project, conducted at the University of California, San Francisco (UCSF), was presented alongside projects on alcohol detox at the Cleveland Veterans Affairs Medical Center and on medication reconciliation at Brigham and Women’s Hospital in Boston.
“The plenary is the top three of the 1,000 that are out there – so, impressive work,” said Benji Mathews, MD, SFHM, the chair of the Research, Innovations and Vignettes competition.
At UCSF, the project was meant to tackle the huge problem of delirium in the hospital, said Catherine Lau, MD, SFHM, associate professor of medicine there. Each year delirium affects more than 7 million people who are hospitalized, and hospital-acquired delirium is linked with prolonged stays and more emergency department visits and hospital readmissions. But research has found that as many as a third of these hospital-acquired cases can be prevented, Dr. Lau said.
New admissions and transfers – a total of more than 2,800 patients – were assessed for delirium risk, and those deemed high risk were entered into a delirium care plan, aimed at prevention with nonpharmacologic steps such as maximizing their mobility and helping them sleep at night.
All patients also were screened on every nursing shift for delirium, and those diagnosed with the disorder were placed in the delirium care plan, with notification of the patient’s team for treatment.
The average length of stay decreased by 0.8 days (P less than .001), with a decrease of 1.9 days in patients with delirium, compared with outcomes for nearly 2,600 patients before the intervention was implemented, Dr. Lau said. Researchers also found a decrease in $850 spent per patient (P less than .001), with a direct savings to the hospital of a total of $997,000, she said. The 30-day readmission rate also fell significantly, from 18.9% to 15.9% (P = .03).
The screening itself seemed to be the most important factor in the project, Dr. Lau said.
“Just the recognition that their patient was at risk for delirium or actually had delirium really raised awareness,” she said.
The project on alcohol detox used careful risk assessments at emergency department discharge, e-consults, protocols to limit benzodiazepine prescribing, and telephone follow-up to reduce hospital admissions and 30-day readmissions, as well as length of stay.
Researchers used scores on CIWA – a 10-question measurement of the severity of someone’s alcohol withdrawal – and history of complicated alcohol-use withdrawal to determine whether ED patients should be admitted to the floor or sent home with or without prescriptions for gabapentin and lorazepam, said Robert Patrick, MD, a hospitalist at the Cleveland VA.
Perhaps the most innovative feature of the program was using systolic blood pressure and heart rate in addition to CIWA to determine whether someone should receive a benzodiazepine, he said. Someone with a CIWA of 9-12, for instance, would be prescribed one of these drugs only if their vitals were elevated, Dr. Patrick said.
He encouraged other hospitalists to try a similar program at their centers.
“You don’t have to be at a VA to do this,” he said. “And most importantly, you don’t have to have a cooperative ED to do this. You can do this just within your hospitalist group.”
In another presentation, Jeffrey Schnipper, MD, MPH, FHM, associate professor of medicine at Harvard Medical School, Boston, described the results from a project in which SHM’s MARQUIS program – an evidence-based “toolkit” on medication reconciliation – was implemented at 18 hospitals. The kit offers a plan to get the best possible medication history, give medication counseling on discharge, and identify patients at risk for medication discrepancies. The 18 sites were coached, with areas of improvement identified.
By months 13-18 of the study period, the number of medication discrepancies had fallen to 0.93 per patient for those who’d received at least one form of intervention, compared with 2.69 per patient among those who’d received none.
“The MARQUIS interventions, including the toolkit and mentored implementation,” Dr. Schnipper said, “are associated with a marked reduction in medication discrepancies.”
Medical cannabis brings complexity to hospitals
As the legalization of medical cannabis becomes more widespread, more and more patients admitted to the hospital are taking it. But once a patient crosses the hospital threshold, how do you incorporate into your care a product that is still illegal at the federal level?
Charles Reznikoff, MD, a physician and addiction specialist who treats medically complex hospitalized patients, walked the audience through the complexities of use of medical cannabis in these patients in a session Tuesday here at HM19. Dr. Reznikoff, from the Hennepin County (Minn.) Medical Center (HCMC), in the Minneapolis area, also discussed medical cannabis indications and contraindications in hospitalized patients.
In 2014, Minnesota passed a law allowing the use of state-based medical cannabis program products in the hospital setting. Two hospitals in the state – HCMC and the Mayo Clinic, which began allowing its use at those centers 3 years ago – illustrate the divergent ways in which different centers manage and oversee the products’ use, as they are forced to navigate nuances particular to their settings.
At Mayo, the medical cannabis is centrally stored, maintained, and administered by hospital nurses, physicians, and pharmacists. At HCMC, the situation is very different.
“Our nursing union told us, ‘Don’t make us handle schedule I substances,’ ” Dr. Reznikoff said. In addition, the hospital’s security officers – who are often off-duty police officers – said that their only interaction with medical cannabis would be to destroy it because of its illegal federal status.
So, at HCMC, the hospital documents which patients have medical cannabis, and the patients let nurses know when they take it and administer it themselves, with that administration documented. Only edibles and tinctures are allowed for use in the hospital – vaping is prohibited.
Despite the departure from the normal use of the hospital’s own formulary and pharmacy, the procedures have worked out, he said.
“For HCMC, it has been pretty straightforward – patients are happy and it has been a piece of cake,” he said, adding that in a few instances patients have been unaware that they could use their medical cannabis, or staff has been confused about the protocol.
Physicians in these situations should be on the lookout for contraindications and potential side effects, Dr. Reznikoff said.
“Medical cannabis has not a ton, but some, important side effects worth knowing about,” he said. “It can cause falls, it can cause dizziness. It can cause a little bit of tachycardia ... If they stop it, people can have mild withdrawal.”
Contraindications include altered mental status such as delirium, having had falls or having a risk of falling, hypotension or hypovolemia, and psychosis.
“For our patients, it is mostly HIV/AIDS and cancer patients who have contraindications, and that comes in the form of infectious diseases and their complications,” he said in an interview.
In the realm of palliative care, cancer, AIDS, and end-of-life care, the use of medical cannabis is a potential tool and should hinge on what patients report back as helpful or not helpful, he said.
But some claims being made about cannabidiol oil, whether as immunotherapy for autoimmune diseases, as an antipsychotic for schizophrenia, or as a cure for heroin addiction, for example, stretch credibility, Dr. Reznikoff said. But the evidence in favor of its use for seizure-reduction, for example, is persuasive, he added.
Overall, medical cannabis for hospitalized patients is no simple matter, but it is worth the fuss for some patients, he said.
“There are a few niches for it – and I think they are niches, but they’re there,” he said. “I don’t love medical cannabis. I think there are a lot of issues with it. I think a lot of physicians are very frustrated with it. But I think also, when we’re talking about palliative care–type issues and seizure disorders not otherwise treated by conventional means ... it’s very reasonable to bring cannabis into the hospital.”
As the legalization of medical cannabis becomes more widespread, more and more patients admitted to the hospital are taking it. But once a patient crosses the hospital threshold, how do you incorporate into your care a product that is still illegal at the federal level?
Charles Reznikoff, MD, a physician and addiction specialist who treats medically complex hospitalized patients, walked the audience through the complexities of use of medical cannabis in these patients in a session Tuesday here at HM19. Dr. Reznikoff, from the Hennepin County (Minn.) Medical Center (HCMC), in the Minneapolis area, also discussed medical cannabis indications and contraindications in hospitalized patients.
In 2014, Minnesota passed a law allowing the use of state-based medical cannabis program products in the hospital setting. Two hospitals in the state – HCMC and the Mayo Clinic, which began allowing its use at those centers 3 years ago – illustrate the divergent ways in which different centers manage and oversee the products’ use, as they are forced to navigate nuances particular to their settings.
At Mayo, the medical cannabis is centrally stored, maintained, and administered by hospital nurses, physicians, and pharmacists. At HCMC, the situation is very different.
“Our nursing union told us, ‘Don’t make us handle schedule I substances,’ ” Dr. Reznikoff said. In addition, the hospital’s security officers – who are often off-duty police officers – said that their only interaction with medical cannabis would be to destroy it because of its illegal federal status.
So, at HCMC, the hospital documents which patients have medical cannabis, and the patients let nurses know when they take it and administer it themselves, with that administration documented. Only edibles and tinctures are allowed for use in the hospital – vaping is prohibited.
Despite the departure from the normal use of the hospital’s own formulary and pharmacy, the procedures have worked out, he said.
“For HCMC, it has been pretty straightforward – patients are happy and it has been a piece of cake,” he said, adding that in a few instances patients have been unaware that they could use their medical cannabis, or staff has been confused about the protocol.
Physicians in these situations should be on the lookout for contraindications and potential side effects, Dr. Reznikoff said.
“Medical cannabis has not a ton, but some, important side effects worth knowing about,” he said. “It can cause falls, it can cause dizziness. It can cause a little bit of tachycardia ... If they stop it, people can have mild withdrawal.”
Contraindications include altered mental status such as delirium, having had falls or having a risk of falling, hypotension or hypovolemia, and psychosis.
“For our patients, it is mostly HIV/AIDS and cancer patients who have contraindications, and that comes in the form of infectious diseases and their complications,” he said in an interview.
In the realm of palliative care, cancer, AIDS, and end-of-life care, the use of medical cannabis is a potential tool and should hinge on what patients report back as helpful or not helpful, he said.
But some claims being made about cannabidiol oil, whether as immunotherapy for autoimmune diseases, as an antipsychotic for schizophrenia, or as a cure for heroin addiction, for example, stretch credibility, Dr. Reznikoff said. But the evidence in favor of its use for seizure-reduction, for example, is persuasive, he added.
Overall, medical cannabis for hospitalized patients is no simple matter, but it is worth the fuss for some patients, he said.
“There are a few niches for it – and I think they are niches, but they’re there,” he said. “I don’t love medical cannabis. I think there are a lot of issues with it. I think a lot of physicians are very frustrated with it. But I think also, when we’re talking about palliative care–type issues and seizure disorders not otherwise treated by conventional means ... it’s very reasonable to bring cannabis into the hospital.”
As the legalization of medical cannabis becomes more widespread, more and more patients admitted to the hospital are taking it. But once a patient crosses the hospital threshold, how do you incorporate into your care a product that is still illegal at the federal level?
Charles Reznikoff, MD, a physician and addiction specialist who treats medically complex hospitalized patients, walked the audience through the complexities of use of medical cannabis in these patients in a session Tuesday here at HM19. Dr. Reznikoff, from the Hennepin County (Minn.) Medical Center (HCMC), in the Minneapolis area, also discussed medical cannabis indications and contraindications in hospitalized patients.
In 2014, Minnesota passed a law allowing the use of state-based medical cannabis program products in the hospital setting. Two hospitals in the state – HCMC and the Mayo Clinic, which began allowing its use at those centers 3 years ago – illustrate the divergent ways in which different centers manage and oversee the products’ use, as they are forced to navigate nuances particular to their settings.
At Mayo, the medical cannabis is centrally stored, maintained, and administered by hospital nurses, physicians, and pharmacists. At HCMC, the situation is very different.
“Our nursing union told us, ‘Don’t make us handle schedule I substances,’ ” Dr. Reznikoff said. In addition, the hospital’s security officers – who are often off-duty police officers – said that their only interaction with medical cannabis would be to destroy it because of its illegal federal status.
So, at HCMC, the hospital documents which patients have medical cannabis, and the patients let nurses know when they take it and administer it themselves, with that administration documented. Only edibles and tinctures are allowed for use in the hospital – vaping is prohibited.
Despite the departure from the normal use of the hospital’s own formulary and pharmacy, the procedures have worked out, he said.
“For HCMC, it has been pretty straightforward – patients are happy and it has been a piece of cake,” he said, adding that in a few instances patients have been unaware that they could use their medical cannabis, or staff has been confused about the protocol.
Physicians in these situations should be on the lookout for contraindications and potential side effects, Dr. Reznikoff said.
“Medical cannabis has not a ton, but some, important side effects worth knowing about,” he said. “It can cause falls, it can cause dizziness. It can cause a little bit of tachycardia ... If they stop it, people can have mild withdrawal.”
Contraindications include altered mental status such as delirium, having had falls or having a risk of falling, hypotension or hypovolemia, and psychosis.
“For our patients, it is mostly HIV/AIDS and cancer patients who have contraindications, and that comes in the form of infectious diseases and their complications,” he said in an interview.
In the realm of palliative care, cancer, AIDS, and end-of-life care, the use of medical cannabis is a potential tool and should hinge on what patients report back as helpful or not helpful, he said.
But some claims being made about cannabidiol oil, whether as immunotherapy for autoimmune diseases, as an antipsychotic for schizophrenia, or as a cure for heroin addiction, for example, stretch credibility, Dr. Reznikoff said. But the evidence in favor of its use for seizure-reduction, for example, is persuasive, he added.
Overall, medical cannabis for hospitalized patients is no simple matter, but it is worth the fuss for some patients, he said.
“There are a few niches for it – and I think they are niches, but they’re there,” he said. “I don’t love medical cannabis. I think there are a lot of issues with it. I think a lot of physicians are very frustrated with it. But I think also, when we’re talking about palliative care–type issues and seizure disorders not otherwise treated by conventional means ... it’s very reasonable to bring cannabis into the hospital.”
Telehospitalist, workload projects win RIV competition
A program using “telehospitalists” to hasten and improve patient care won the top prize in the Innovations category of the RIV competition on Monday night at HM19. In the Research category, a study on workload to improve overnight cross-coverage care took the top prize.
Jeetinder Kaur Gujral, MD, a family medicine and palliative care physician at Northwell Health in Bay Shore, N.Y., said that the telehospitalist program at her institution uses a telehealth hub that is on call to consult with patients when the on-site hospitalist is unable to evaluate a patient in the emergency department within 30 minutes.
Dr. Gujral’s winning study – presented on Monday night and evaluated based on its novelty and the quality of the presentation and the poster – examined results at one of Northwell’s tertiary centers from January to October of 2018, where a telehospitalist works from 12 p.m. to 10 p.m.
Researchers found there was no significant difference in the severity of illness between the patients seen by the on-site hospitalist and the telehospitalist – if anything, the patients consulted by the telehospitalist were a bit sicker, Dr. Gujral said. But there was significantly less variation in the time it took for a telehospitalist to consult with a patient than the on-site physician.
“We are more predictable, because it’s a press of a button, and we are there,” Dr. Gujral said. “And the orders go in faster. I don’t have to leave to go down to the ED to see the patient. I’m seeing the patient right there.”
Kelly Sponsler, MD, assistant professor at Vanderbilt University Medical Center in Nashville, Tenn., who led the Innovations judging, said the project seems to be a brand-new idea: taking a concept built to cover long distances at rural centers and using it within a center’s own program to improve care.
“We really felt like this was something we had not seen before,” Dr. Sponsler said. “There was a clear problem that the team had identified, and it’s a common problem that I think can be scalable, or that other groups probably encounter.”
In the cross-coverage study that won in the Research category, an index developed by NASA to quantify perceived workload was used to assess the factors that boost workload during night shifts, said Ruth Bates, MD, an assistant professor at Mayo Clinic in Rochester, Minn.
The key finding was that it wasn’t the number of patients that boosts workload during these hours, but the number of pages, action items, and rapid-response team and ICU activations. The number of unnecessary pages that overnight hospitalists receive is the prime target as a way to reduce the workload.
The idea is to reduce “low-value communication,” Dr. Bates said. An example is a page about a lab value that is a “tiny bit off.”
“That’s just one example of really low-value communication that has interrupted somebody’s work flow and is not really increasing the quality of patient care.”
Trainee winners were Cameron Locke, MD, a resident physician at the University of California, San Francisco, for a study on a multidisciplinary approach to reduce endoscopy delays, which won in the Innovations category. That study was presented by Molly Kantor, MD, assistant clinical professor at UCSF.
The Research category trainee winner was Monisha Bhatia, MD, JD, MPH, of Jackson Memorial Hospital in Miami for her work on using phenotypic data from electronic health records to predict discharge destination.
On Tuesday afternoon, Erin Frost, MD, a resident in internal medicine and pediatrics at Duke University, Durham, N.C., won the top prize in the Clinical Vignettes category, for her presentation of a case of a woman with acute digital ischemia after an injection of sublingual buprenorphine and naloxone.
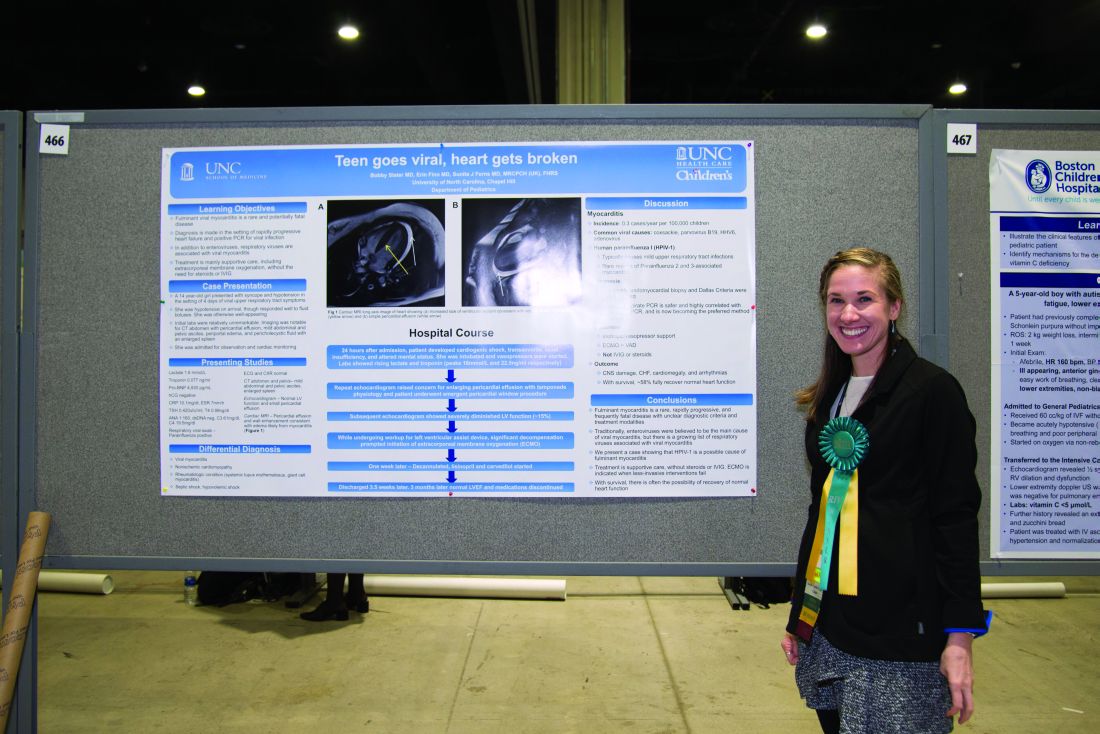
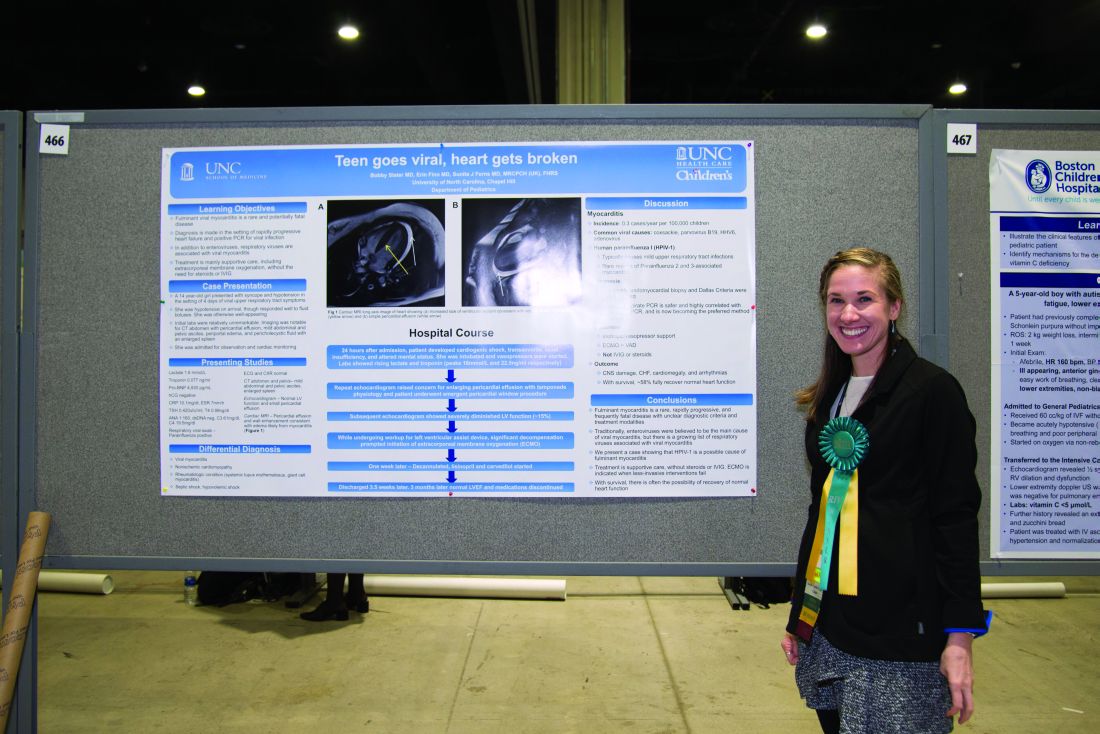
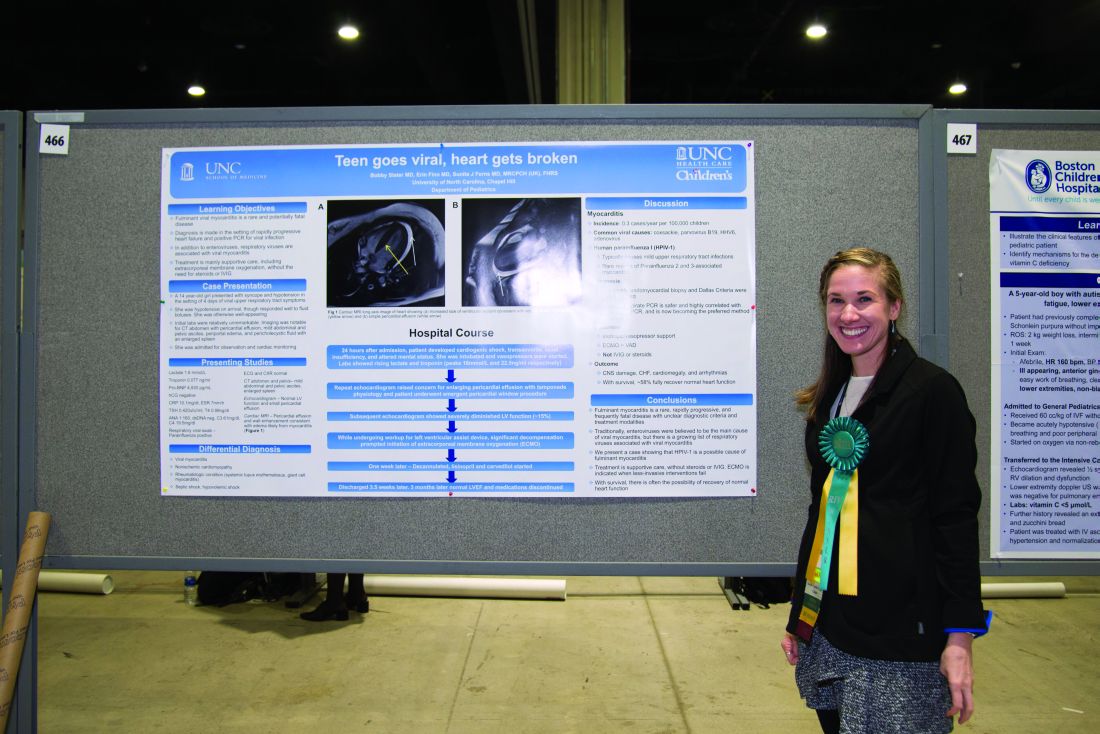
The trainee winner in Clinical Vignettes was a case of C. difficile infection of a total hip arthroplasty, presented by Benjamin Claxton, MPH, a medical student at Penn State University, Hershey. The category’s pediatrics winner was Erin Finn, MD, a resident at the University of North Carolina, Chapel Hill, for her presentation of a case of myocarditis in a 14-year-old.
The oral presentation winner for the Innovations category was Nainesh Shah, MD, of UT Southwestern Medical Center, Dallas, for his abstract presentation "Alert: Structured Radiology Reports are Here." For the Research category, the oral presentation winner was David Meltzer, MD, PhD, section chief of hospital medicine at University of Chicago Medicine, for his abstract presentation "Effects of Comprehensive Care Physicians on Patient Experience, Outcomes and Hospitalization."
A program using “telehospitalists” to hasten and improve patient care won the top prize in the Innovations category of the RIV competition on Monday night at HM19. In the Research category, a study on workload to improve overnight cross-coverage care took the top prize.
Jeetinder Kaur Gujral, MD, a family medicine and palliative care physician at Northwell Health in Bay Shore, N.Y., said that the telehospitalist program at her institution uses a telehealth hub that is on call to consult with patients when the on-site hospitalist is unable to evaluate a patient in the emergency department within 30 minutes.
Dr. Gujral’s winning study – presented on Monday night and evaluated based on its novelty and the quality of the presentation and the poster – examined results at one of Northwell’s tertiary centers from January to October of 2018, where a telehospitalist works from 12 p.m. to 10 p.m.
Researchers found there was no significant difference in the severity of illness between the patients seen by the on-site hospitalist and the telehospitalist – if anything, the patients consulted by the telehospitalist were a bit sicker, Dr. Gujral said. But there was significantly less variation in the time it took for a telehospitalist to consult with a patient than the on-site physician.
“We are more predictable, because it’s a press of a button, and we are there,” Dr. Gujral said. “And the orders go in faster. I don’t have to leave to go down to the ED to see the patient. I’m seeing the patient right there.”
Kelly Sponsler, MD, assistant professor at Vanderbilt University Medical Center in Nashville, Tenn., who led the Innovations judging, said the project seems to be a brand-new idea: taking a concept built to cover long distances at rural centers and using it within a center’s own program to improve care.
“We really felt like this was something we had not seen before,” Dr. Sponsler said. “There was a clear problem that the team had identified, and it’s a common problem that I think can be scalable, or that other groups probably encounter.”
In the cross-coverage study that won in the Research category, an index developed by NASA to quantify perceived workload was used to assess the factors that boost workload during night shifts, said Ruth Bates, MD, an assistant professor at Mayo Clinic in Rochester, Minn.
The key finding was that it wasn’t the number of patients that boosts workload during these hours, but the number of pages, action items, and rapid-response team and ICU activations. The number of unnecessary pages that overnight hospitalists receive is the prime target as a way to reduce the workload.
The idea is to reduce “low-value communication,” Dr. Bates said. An example is a page about a lab value that is a “tiny bit off.”
“That’s just one example of really low-value communication that has interrupted somebody’s work flow and is not really increasing the quality of patient care.”
Trainee winners were Cameron Locke, MD, a resident physician at the University of California, San Francisco, for a study on a multidisciplinary approach to reduce endoscopy delays, which won in the Innovations category. That study was presented by Molly Kantor, MD, assistant clinical professor at UCSF.
The Research category trainee winner was Monisha Bhatia, MD, JD, MPH, of Jackson Memorial Hospital in Miami for her work on using phenotypic data from electronic health records to predict discharge destination.
On Tuesday afternoon, Erin Frost, MD, a resident in internal medicine and pediatrics at Duke University, Durham, N.C., won the top prize in the Clinical Vignettes category, for her presentation of a case of a woman with acute digital ischemia after an injection of sublingual buprenorphine and naloxone.
The trainee winner in Clinical Vignettes was a case of C. difficile infection of a total hip arthroplasty, presented by Benjamin Claxton, MPH, a medical student at Penn State University, Hershey. The category’s pediatrics winner was Erin Finn, MD, a resident at the University of North Carolina, Chapel Hill, for her presentation of a case of myocarditis in a 14-year-old.
The oral presentation winner for the Innovations category was Nainesh Shah, MD, of UT Southwestern Medical Center, Dallas, for his abstract presentation "Alert: Structured Radiology Reports are Here." For the Research category, the oral presentation winner was David Meltzer, MD, PhD, section chief of hospital medicine at University of Chicago Medicine, for his abstract presentation "Effects of Comprehensive Care Physicians on Patient Experience, Outcomes and Hospitalization."
A program using “telehospitalists” to hasten and improve patient care won the top prize in the Innovations category of the RIV competition on Monday night at HM19. In the Research category, a study on workload to improve overnight cross-coverage care took the top prize.
Jeetinder Kaur Gujral, MD, a family medicine and palliative care physician at Northwell Health in Bay Shore, N.Y., said that the telehospitalist program at her institution uses a telehealth hub that is on call to consult with patients when the on-site hospitalist is unable to evaluate a patient in the emergency department within 30 minutes.
Dr. Gujral’s winning study – presented on Monday night and evaluated based on its novelty and the quality of the presentation and the poster – examined results at one of Northwell’s tertiary centers from January to October of 2018, where a telehospitalist works from 12 p.m. to 10 p.m.
Researchers found there was no significant difference in the severity of illness between the patients seen by the on-site hospitalist and the telehospitalist – if anything, the patients consulted by the telehospitalist were a bit sicker, Dr. Gujral said. But there was significantly less variation in the time it took for a telehospitalist to consult with a patient than the on-site physician.
“We are more predictable, because it’s a press of a button, and we are there,” Dr. Gujral said. “And the orders go in faster. I don’t have to leave to go down to the ED to see the patient. I’m seeing the patient right there.”
Kelly Sponsler, MD, assistant professor at Vanderbilt University Medical Center in Nashville, Tenn., who led the Innovations judging, said the project seems to be a brand-new idea: taking a concept built to cover long distances at rural centers and using it within a center’s own program to improve care.
“We really felt like this was something we had not seen before,” Dr. Sponsler said. “There was a clear problem that the team had identified, and it’s a common problem that I think can be scalable, or that other groups probably encounter.”
In the cross-coverage study that won in the Research category, an index developed by NASA to quantify perceived workload was used to assess the factors that boost workload during night shifts, said Ruth Bates, MD, an assistant professor at Mayo Clinic in Rochester, Minn.
The key finding was that it wasn’t the number of patients that boosts workload during these hours, but the number of pages, action items, and rapid-response team and ICU activations. The number of unnecessary pages that overnight hospitalists receive is the prime target as a way to reduce the workload.
The idea is to reduce “low-value communication,” Dr. Bates said. An example is a page about a lab value that is a “tiny bit off.”
“That’s just one example of really low-value communication that has interrupted somebody’s work flow and is not really increasing the quality of patient care.”
Trainee winners were Cameron Locke, MD, a resident physician at the University of California, San Francisco, for a study on a multidisciplinary approach to reduce endoscopy delays, which won in the Innovations category. That study was presented by Molly Kantor, MD, assistant clinical professor at UCSF.
The Research category trainee winner was Monisha Bhatia, MD, JD, MPH, of Jackson Memorial Hospital in Miami for her work on using phenotypic data from electronic health records to predict discharge destination.
On Tuesday afternoon, Erin Frost, MD, a resident in internal medicine and pediatrics at Duke University, Durham, N.C., won the top prize in the Clinical Vignettes category, for her presentation of a case of a woman with acute digital ischemia after an injection of sublingual buprenorphine and naloxone.
The trainee winner in Clinical Vignettes was a case of C. difficile infection of a total hip arthroplasty, presented by Benjamin Claxton, MPH, a medical student at Penn State University, Hershey. The category’s pediatrics winner was Erin Finn, MD, a resident at the University of North Carolina, Chapel Hill, for her presentation of a case of myocarditis in a 14-year-old.
The oral presentation winner for the Innovations category was Nainesh Shah, MD, of UT Southwestern Medical Center, Dallas, for his abstract presentation "Alert: Structured Radiology Reports are Here." For the Research category, the oral presentation winner was David Meltzer, MD, PhD, section chief of hospital medicine at University of Chicago Medicine, for his abstract presentation "Effects of Comprehensive Care Physicians on Patient Experience, Outcomes and Hospitalization."
Adapting to change key to hospitalists’ future, SHM president says
Society of Hospital Medicine President Nasim Afsar, MD, SFHM, told a packed ballroom of hospitalists at HM19 on Monday that it’s not change to the health care industry that is most central to their future, but it’s how they assume a role within it and how they spark it themselves.
With a tone that was, at times, almost ebullient about change, Dr. Afsar characterized the flux of health care as a series of opportunities to improve patient care.
“Run toward change,” said Dr. Afsar, chief ambulatory officer and chief medical officer for accountable care organizations at University of California, Irvine. “And be a force of positive change.”
The push toward affordability and value has made for some “unlikely partners,” she noted, including the health care venture launched by Amazon, Berkshire Hathaway, and JPMorgan Chase, as well as some newer corporations stepping into the health care sphere, such as Uber with its UberHealth and the creation of giants like the CVS-Aetna merger.
She acknowledged it brings “uncertainty and risk” but suggested that hospitalists are equipped to cope, saying that “we’ve all experienced this in our personal and professional lives.”
Dr. Afsar described four major themes of change to the health care landscape that will affect how hospitalists do their jobs.
- A new setting of care. “The care of the patients is moving from the hospital to the ambulatory setting,” she said. “Some of the surgeries that we used to do in the ER are now being done in ambulatory surgery centers. Antibiotics are being infused via IVs at patients’ homes.”
- Focus on health and well-being. “There’s a transition as a society on focusing on the sick to prevention of disease,” she said. “How can we prevent chronic illness once it occurs? How can we limit its progression? This is a very new focus for us in health care.”
- An increasing role of patient care teams – including primary care doctors, pharmacists, and case managers – rather than hospital-based teams.
- A new focus on patient-centered care. “It’s a focus about how we can be everywhere the patient is, at anytime that the patient needs us,” she said.
A sense of the way forward, Dr. Afsar said, came out of recent strategic meetings of the SHM board of directors, in which they talked about the role and future of hospitalists in population health management and value-based care. They agreed hospitalists should define themselves by their values and competencies, not by the hospital building itself. Hospitalists should use the acute care episode to make sure patients are connected to a larger system of care with wellness and prevention in mind.
“It’s not the strongest of the species that survive, nor the most intelligent,” Dr. Afsar said. “But the ones who are most adaptable to change. While there’s debate on the Internet about who originally said this, there’s absolutely no debate that the theme in life and in health care is adaptability in the face of constant change.”
In his own address at the Annual Conference of the Society of Hospital Medicine, Christopher Frost, MD, SFHM, the president-elect of SHM and national medical director of hospital-based services for LifePoint Health in Brentwood, Tenn., echoed Dr. Afsar’s theme of action in the context of change.
A key word, he said, is “multifarious” – the health care industry changes and the ways hospitalists are tackling these changes come in many and various types.
“We will not just react to – but actually help author – aspects of this change,” he said, including the continued move from fee for service to value-based and risk-based models of payment, and how to put new insights into disease processes to use and how they’re linked to social factors.
Increasing the diversity of hospitalist teams, maximizing the use of technology, and improving LGBTQ care are all themes of change being addressed at the meeting, he noted.
“When we summit one mountain of our own professional Alps,” Dr. Frost said, “and we see another on the horizon, we say, ‘Let’s climb that one. Let’s go there.’ ”
Society of Hospital Medicine President Nasim Afsar, MD, SFHM, told a packed ballroom of hospitalists at HM19 on Monday that it’s not change to the health care industry that is most central to their future, but it’s how they assume a role within it and how they spark it themselves.
With a tone that was, at times, almost ebullient about change, Dr. Afsar characterized the flux of health care as a series of opportunities to improve patient care.
“Run toward change,” said Dr. Afsar, chief ambulatory officer and chief medical officer for accountable care organizations at University of California, Irvine. “And be a force of positive change.”
The push toward affordability and value has made for some “unlikely partners,” she noted, including the health care venture launched by Amazon, Berkshire Hathaway, and JPMorgan Chase, as well as some newer corporations stepping into the health care sphere, such as Uber with its UberHealth and the creation of giants like the CVS-Aetna merger.
She acknowledged it brings “uncertainty and risk” but suggested that hospitalists are equipped to cope, saying that “we’ve all experienced this in our personal and professional lives.”
Dr. Afsar described four major themes of change to the health care landscape that will affect how hospitalists do their jobs.
- A new setting of care. “The care of the patients is moving from the hospital to the ambulatory setting,” she said. “Some of the surgeries that we used to do in the ER are now being done in ambulatory surgery centers. Antibiotics are being infused via IVs at patients’ homes.”
- Focus on health and well-being. “There’s a transition as a society on focusing on the sick to prevention of disease,” she said. “How can we prevent chronic illness once it occurs? How can we limit its progression? This is a very new focus for us in health care.”
- An increasing role of patient care teams – including primary care doctors, pharmacists, and case managers – rather than hospital-based teams.
- A new focus on patient-centered care. “It’s a focus about how we can be everywhere the patient is, at anytime that the patient needs us,” she said.
A sense of the way forward, Dr. Afsar said, came out of recent strategic meetings of the SHM board of directors, in which they talked about the role and future of hospitalists in population health management and value-based care. They agreed hospitalists should define themselves by their values and competencies, not by the hospital building itself. Hospitalists should use the acute care episode to make sure patients are connected to a larger system of care with wellness and prevention in mind.
“It’s not the strongest of the species that survive, nor the most intelligent,” Dr. Afsar said. “But the ones who are most adaptable to change. While there’s debate on the Internet about who originally said this, there’s absolutely no debate that the theme in life and in health care is adaptability in the face of constant change.”
In his own address at the Annual Conference of the Society of Hospital Medicine, Christopher Frost, MD, SFHM, the president-elect of SHM and national medical director of hospital-based services for LifePoint Health in Brentwood, Tenn., echoed Dr. Afsar’s theme of action in the context of change.
A key word, he said, is “multifarious” – the health care industry changes and the ways hospitalists are tackling these changes come in many and various types.
“We will not just react to – but actually help author – aspects of this change,” he said, including the continued move from fee for service to value-based and risk-based models of payment, and how to put new insights into disease processes to use and how they’re linked to social factors.
Increasing the diversity of hospitalist teams, maximizing the use of technology, and improving LGBTQ care are all themes of change being addressed at the meeting, he noted.
“When we summit one mountain of our own professional Alps,” Dr. Frost said, “and we see another on the horizon, we say, ‘Let’s climb that one. Let’s go there.’ ”
Society of Hospital Medicine President Nasim Afsar, MD, SFHM, told a packed ballroom of hospitalists at HM19 on Monday that it’s not change to the health care industry that is most central to their future, but it’s how they assume a role within it and how they spark it themselves.
With a tone that was, at times, almost ebullient about change, Dr. Afsar characterized the flux of health care as a series of opportunities to improve patient care.
“Run toward change,” said Dr. Afsar, chief ambulatory officer and chief medical officer for accountable care organizations at University of California, Irvine. “And be a force of positive change.”
The push toward affordability and value has made for some “unlikely partners,” she noted, including the health care venture launched by Amazon, Berkshire Hathaway, and JPMorgan Chase, as well as some newer corporations stepping into the health care sphere, such as Uber with its UberHealth and the creation of giants like the CVS-Aetna merger.
She acknowledged it brings “uncertainty and risk” but suggested that hospitalists are equipped to cope, saying that “we’ve all experienced this in our personal and professional lives.”
Dr. Afsar described four major themes of change to the health care landscape that will affect how hospitalists do their jobs.
- A new setting of care. “The care of the patients is moving from the hospital to the ambulatory setting,” she said. “Some of the surgeries that we used to do in the ER are now being done in ambulatory surgery centers. Antibiotics are being infused via IVs at patients’ homes.”
- Focus on health and well-being. “There’s a transition as a society on focusing on the sick to prevention of disease,” she said. “How can we prevent chronic illness once it occurs? How can we limit its progression? This is a very new focus for us in health care.”
- An increasing role of patient care teams – including primary care doctors, pharmacists, and case managers – rather than hospital-based teams.
- A new focus on patient-centered care. “It’s a focus about how we can be everywhere the patient is, at anytime that the patient needs us,” she said.
A sense of the way forward, Dr. Afsar said, came out of recent strategic meetings of the SHM board of directors, in which they talked about the role and future of hospitalists in population health management and value-based care. They agreed hospitalists should define themselves by their values and competencies, not by the hospital building itself. Hospitalists should use the acute care episode to make sure patients are connected to a larger system of care with wellness and prevention in mind.
“It’s not the strongest of the species that survive, nor the most intelligent,” Dr. Afsar said. “But the ones who are most adaptable to change. While there’s debate on the Internet about who originally said this, there’s absolutely no debate that the theme in life and in health care is adaptability in the face of constant change.”
In his own address at the Annual Conference of the Society of Hospital Medicine, Christopher Frost, MD, SFHM, the president-elect of SHM and national medical director of hospital-based services for LifePoint Health in Brentwood, Tenn., echoed Dr. Afsar’s theme of action in the context of change.
A key word, he said, is “multifarious” – the health care industry changes and the ways hospitalists are tackling these changes come in many and various types.
“We will not just react to – but actually help author – aspects of this change,” he said, including the continued move from fee for service to value-based and risk-based models of payment, and how to put new insights into disease processes to use and how they’re linked to social factors.
Increasing the diversity of hospitalist teams, maximizing the use of technology, and improving LGBTQ care are all themes of change being addressed at the meeting, he noted.
“When we summit one mountain of our own professional Alps,” Dr. Frost said, “and we see another on the horizon, we say, ‘Let’s climb that one. Let’s go there.’ ”
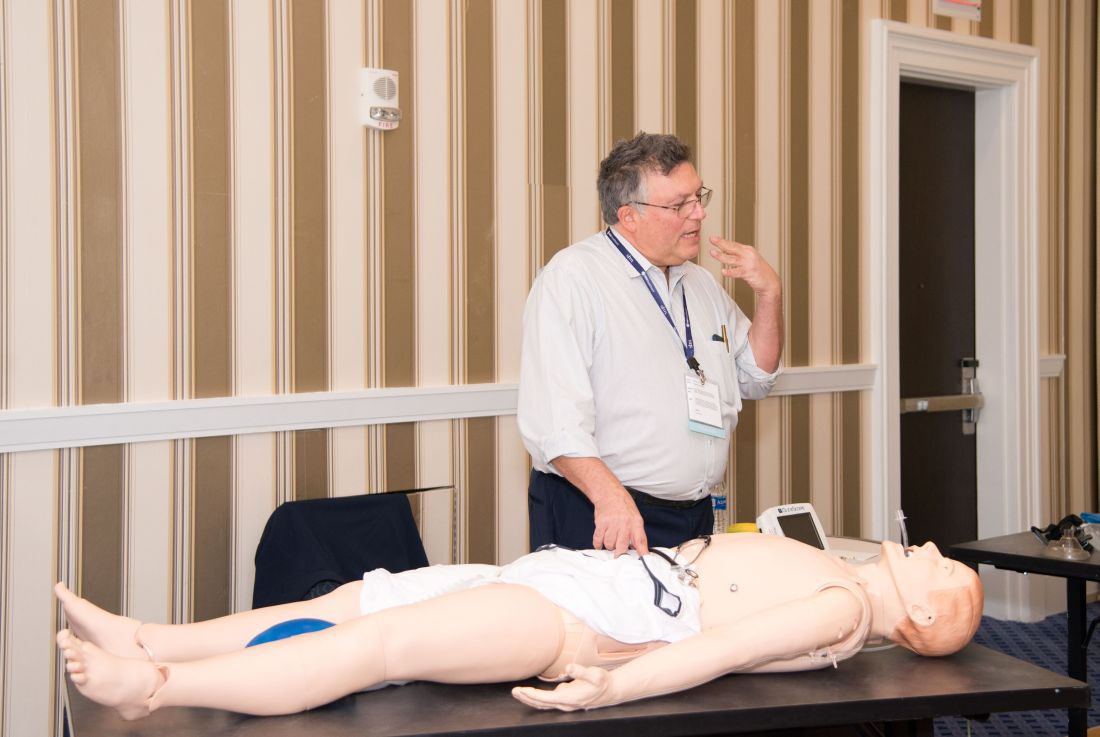
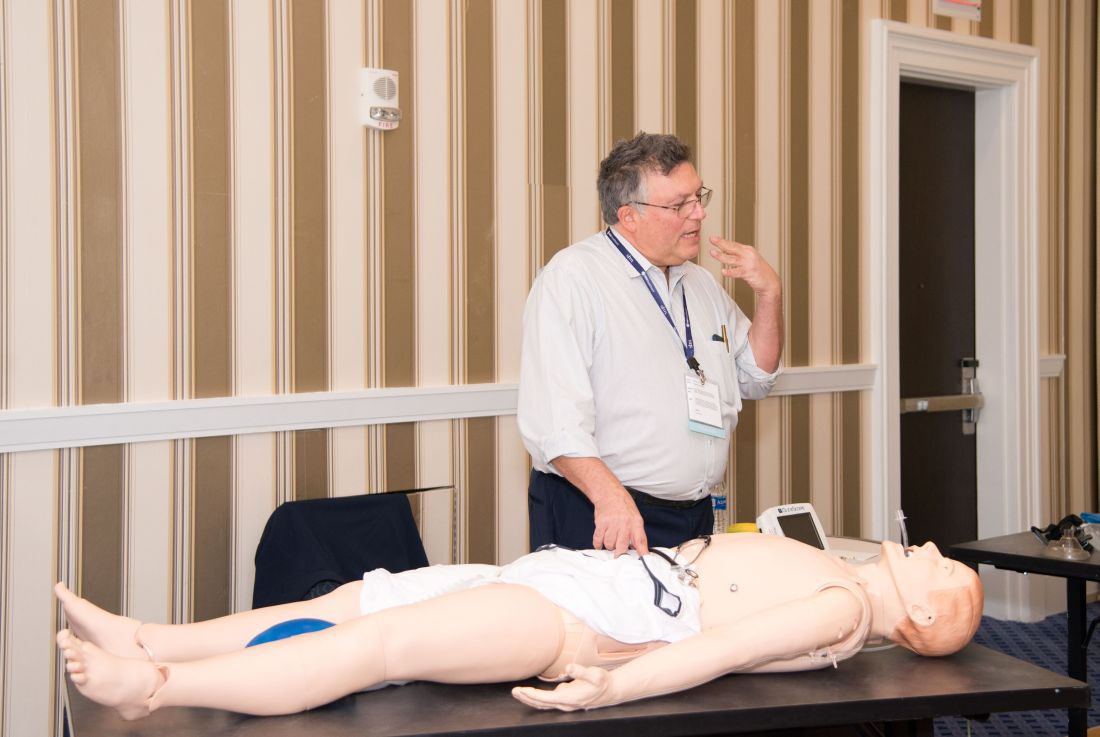
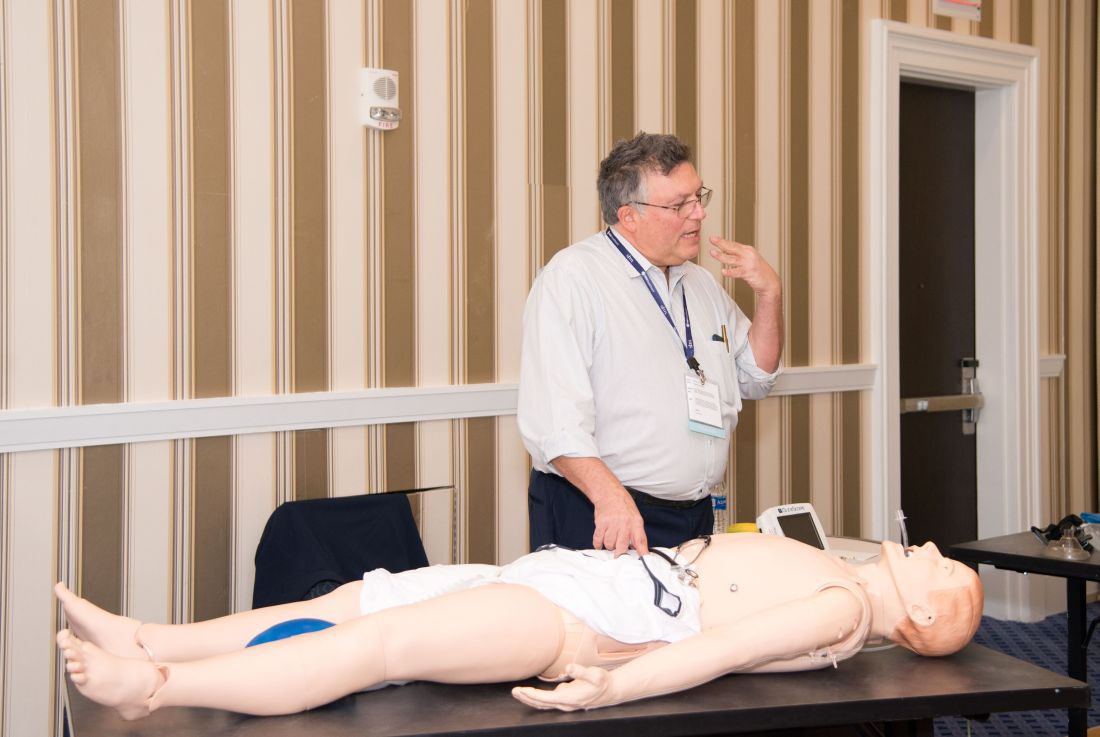
Hospitalists get emergency airway management training
A patient is having a medical emergency and is having difficulty breathing. If the airway isn’t managed well, the consequences could be tragic. If asked to step in, would you? Could you?
More hospitalists are being faced with this situation, said Joshua Lenchus, DO, RPh, SFHM, chief medical officer at the Broward Health Medical Center in South Florida. But when they are, they tend to be hesitant – usually with good reason, since training is frequently lacking.
Dr. Lenchus and a group of five other physicians who are experienced in airway management led 25 hospitalists in emergent airway management training on Monday at HM19, a first-of-its-kind session at the annual conference.
“Not all facilities that hospitalists practice at would require or even ask a hospitalist to step into a situation like this,” said Dr. Lenchus, who oversaw the training. “But as you walk around the exhibit hall at SHM, you find that of the locum tenens companies that ask for hospitalists to perform procedures, airway management is very high on the list.”
The trainers were Armando Ariza Giammaria, MD, an anesthesiologist and clinical assistant professor at Tulane University, New Orleans; Jorge Cabrera, DO, an intensivist and assistant professor of medicine at the University of Miami; Alice Gallo de Moraes, MD, a pulmonary critical care doctor at Mayo Clinic, Rochester, Minn.; Fernando Caceres, MD, a pulmonary critical care specialist at the Billings (Mont.) Clinic; and Aldo Pavon Canseco, MD, a hospitalist and assistant professor of medicine at the University of Miami who was trained as a pediatric anesthesiologist.
Over 3 hours, hospitalists first heard tips for airway management, with words of caution, and then did hands-on work using manikins under the guidance of the faculty members with a low trainee-to-instructor ratio.
“Do the basics well and the scary things will become manageable,” Dr. Cabrera said in the session.
Instructors said it was vital to have a checklist in the form of a mnemonic device, and to have not just Plan A for clearing an airway, but Plans B and C, too.
Dr. Ariza told the learners not to focus too much on intubation — it’s not always necessary. In fact, he said he couldn’t over-emphasize the importance of mastering bag-mask ventilation, a go-to method when other approaches fail.
Participants learned about devices that can be deployed through the nose to keep the airway clear, those that can be used in the mouth but that might not go down quite as far as the lung, an inflatable bag that can be placed over patients’ mouths and squeezed to help with their breathing, and endotracheal tubes.
Dr. Lenchus said that more training would likely be needed for most clinicians – perhaps with other faculty at their own institutions – before they could be expected to employ these techniques in a real-life emergency situation.
A patient is having a medical emergency and is having difficulty breathing. If the airway isn’t managed well, the consequences could be tragic. If asked to step in, would you? Could you?
More hospitalists are being faced with this situation, said Joshua Lenchus, DO, RPh, SFHM, chief medical officer at the Broward Health Medical Center in South Florida. But when they are, they tend to be hesitant – usually with good reason, since training is frequently lacking.
Dr. Lenchus and a group of five other physicians who are experienced in airway management led 25 hospitalists in emergent airway management training on Monday at HM19, a first-of-its-kind session at the annual conference.
“Not all facilities that hospitalists practice at would require or even ask a hospitalist to step into a situation like this,” said Dr. Lenchus, who oversaw the training. “But as you walk around the exhibit hall at SHM, you find that of the locum tenens companies that ask for hospitalists to perform procedures, airway management is very high on the list.”
The trainers were Armando Ariza Giammaria, MD, an anesthesiologist and clinical assistant professor at Tulane University, New Orleans; Jorge Cabrera, DO, an intensivist and assistant professor of medicine at the University of Miami; Alice Gallo de Moraes, MD, a pulmonary critical care doctor at Mayo Clinic, Rochester, Minn.; Fernando Caceres, MD, a pulmonary critical care specialist at the Billings (Mont.) Clinic; and Aldo Pavon Canseco, MD, a hospitalist and assistant professor of medicine at the University of Miami who was trained as a pediatric anesthesiologist.
Over 3 hours, hospitalists first heard tips for airway management, with words of caution, and then did hands-on work using manikins under the guidance of the faculty members with a low trainee-to-instructor ratio.
“Do the basics well and the scary things will become manageable,” Dr. Cabrera said in the session.
Instructors said it was vital to have a checklist in the form of a mnemonic device, and to have not just Plan A for clearing an airway, but Plans B and C, too.
Dr. Ariza told the learners not to focus too much on intubation — it’s not always necessary. In fact, he said he couldn’t over-emphasize the importance of mastering bag-mask ventilation, a go-to method when other approaches fail.
Participants learned about devices that can be deployed through the nose to keep the airway clear, those that can be used in the mouth but that might not go down quite as far as the lung, an inflatable bag that can be placed over patients’ mouths and squeezed to help with their breathing, and endotracheal tubes.
Dr. Lenchus said that more training would likely be needed for most clinicians – perhaps with other faculty at their own institutions – before they could be expected to employ these techniques in a real-life emergency situation.
A patient is having a medical emergency and is having difficulty breathing. If the airway isn’t managed well, the consequences could be tragic. If asked to step in, would you? Could you?
More hospitalists are being faced with this situation, said Joshua Lenchus, DO, RPh, SFHM, chief medical officer at the Broward Health Medical Center in South Florida. But when they are, they tend to be hesitant – usually with good reason, since training is frequently lacking.
Dr. Lenchus and a group of five other physicians who are experienced in airway management led 25 hospitalists in emergent airway management training on Monday at HM19, a first-of-its-kind session at the annual conference.
“Not all facilities that hospitalists practice at would require or even ask a hospitalist to step into a situation like this,” said Dr. Lenchus, who oversaw the training. “But as you walk around the exhibit hall at SHM, you find that of the locum tenens companies that ask for hospitalists to perform procedures, airway management is very high on the list.”
The trainers were Armando Ariza Giammaria, MD, an anesthesiologist and clinical assistant professor at Tulane University, New Orleans; Jorge Cabrera, DO, an intensivist and assistant professor of medicine at the University of Miami; Alice Gallo de Moraes, MD, a pulmonary critical care doctor at Mayo Clinic, Rochester, Minn.; Fernando Caceres, MD, a pulmonary critical care specialist at the Billings (Mont.) Clinic; and Aldo Pavon Canseco, MD, a hospitalist and assistant professor of medicine at the University of Miami who was trained as a pediatric anesthesiologist.
Over 3 hours, hospitalists first heard tips for airway management, with words of caution, and then did hands-on work using manikins under the guidance of the faculty members with a low trainee-to-instructor ratio.
“Do the basics well and the scary things will become manageable,” Dr. Cabrera said in the session.
Instructors said it was vital to have a checklist in the form of a mnemonic device, and to have not just Plan A for clearing an airway, but Plans B and C, too.
Dr. Ariza told the learners not to focus too much on intubation — it’s not always necessary. In fact, he said he couldn’t over-emphasize the importance of mastering bag-mask ventilation, a go-to method when other approaches fail.
Participants learned about devices that can be deployed through the nose to keep the airway clear, those that can be used in the mouth but that might not go down quite as far as the lung, an inflatable bag that can be placed over patients’ mouths and squeezed to help with their breathing, and endotracheal tubes.
Dr. Lenchus said that more training would likely be needed for most clinicians – perhaps with other faculty at their own institutions – before they could be expected to employ these techniques in a real-life emergency situation.
Hands-on critical care lessons provided at HM19
As the hospitalist tried to position the portable video laryngoscope properly in the airway of the critically ill “patient,” HM19 faculty moderator Brian Kaufman, MD, professor of medicine, anesthesiology, and neurology at New York University (NYU) School of Medicine, issued a word of caution: Rotating it into position should be done gently or there’s a risk of tearing tissue.
One step at a time, hospitalists attending the session grew more confident and knowledgeable in handling urgent matters involving patients who are critically ill, including cases of shock, mechanical ventilation, overdoses, and ultrasound.
Kevin Felner, MD, associate professor of medicine at NYU School of Medicine, said there’s a growing need for more exposure to caring for the critically ill, including intubation.
“There are a lot of hospitalists who are intubating, and they’re not formally trained in it because medicine residencies don’t typically train people to manage airways,” he said. “We’ve met hospitalists who’ve said, ‘I was hired and was told I had to manage an airway.’”
“It might massage some of the things you’re doing, make you afraid of things you should be afraid of, make you think about something that’s easy to do that you’re not doing, and make things safer,” Dr. Felner said.
In a simulation room, James Horowitz, MD, clinical assistant professor and cardiologist at NYU School of Medicine, demonstrated how to use a laryngeal mask airway (LMA), a simpler alternative to intubating the trachea for keeping an airway open. Dr. Kaufman, standing next to him, clarified how important a skill this is, especially when someone needs air in the next minute or is at risk of death.
“Knowing how to put an LMA in can be life-saving,” Dr. Kaufman said.
In a lecture on shock in the critically ill, Dr. Felner said it’s important to be nimble in handling this common problem –quickly identifying the cause, whether it’s a cardiogenic issue, a low-volume circulation problem, a question of vasodilation, or an obstructive problem. He said guidelines – such as aiming for a mean arterial pressure of 65 mm Hg –are helpful generally, but individuals routinely call for making exceptions to guidelines.
Anthony Andriotis, MD, a pulmonologist at NYU who specializes in critical care, offered an array of key points when managing patients with a ventilator. For instance, when you need to prolong a patient’s expiratory time so they can exhale air more effectively to get rid of entrapped air in their lungs, lowering their respiratory rate is far more effective than decreasing the time it takes them to breathe in or increasing the flow rate of the air they’re breathing.
Some basic points – such as remembering that it’s important to be aware of the pressure when volume control has been imposed and to be aware of volume control when the pressure has been set – are crucial, he said.
The idea behind the pre-course, Dr. Felner said, was to give hospitalists a chance to enter tricky situations with everything to gain, but nothing to lose. He described it as giving students “learning scars” – those times you made a serious error that left you with a lesson you’ll never forget.
“We’re trying to create learning scars, but in a safe scenario.”
As the hospitalist tried to position the portable video laryngoscope properly in the airway of the critically ill “patient,” HM19 faculty moderator Brian Kaufman, MD, professor of medicine, anesthesiology, and neurology at New York University (NYU) School of Medicine, issued a word of caution: Rotating it into position should be done gently or there’s a risk of tearing tissue.
One step at a time, hospitalists attending the session grew more confident and knowledgeable in handling urgent matters involving patients who are critically ill, including cases of shock, mechanical ventilation, overdoses, and ultrasound.
Kevin Felner, MD, associate professor of medicine at NYU School of Medicine, said there’s a growing need for more exposure to caring for the critically ill, including intubation.
“There are a lot of hospitalists who are intubating, and they’re not formally trained in it because medicine residencies don’t typically train people to manage airways,” he said. “We’ve met hospitalists who’ve said, ‘I was hired and was told I had to manage an airway.’”
“It might massage some of the things you’re doing, make you afraid of things you should be afraid of, make you think about something that’s easy to do that you’re not doing, and make things safer,” Dr. Felner said.
In a simulation room, James Horowitz, MD, clinical assistant professor and cardiologist at NYU School of Medicine, demonstrated how to use a laryngeal mask airway (LMA), a simpler alternative to intubating the trachea for keeping an airway open. Dr. Kaufman, standing next to him, clarified how important a skill this is, especially when someone needs air in the next minute or is at risk of death.
“Knowing how to put an LMA in can be life-saving,” Dr. Kaufman said.
In a lecture on shock in the critically ill, Dr. Felner said it’s important to be nimble in handling this common problem –quickly identifying the cause, whether it’s a cardiogenic issue, a low-volume circulation problem, a question of vasodilation, or an obstructive problem. He said guidelines – such as aiming for a mean arterial pressure of 65 mm Hg –are helpful generally, but individuals routinely call for making exceptions to guidelines.
Anthony Andriotis, MD, a pulmonologist at NYU who specializes in critical care, offered an array of key points when managing patients with a ventilator. For instance, when you need to prolong a patient’s expiratory time so they can exhale air more effectively to get rid of entrapped air in their lungs, lowering their respiratory rate is far more effective than decreasing the time it takes them to breathe in or increasing the flow rate of the air they’re breathing.
Some basic points – such as remembering that it’s important to be aware of the pressure when volume control has been imposed and to be aware of volume control when the pressure has been set – are crucial, he said.
The idea behind the pre-course, Dr. Felner said, was to give hospitalists a chance to enter tricky situations with everything to gain, but nothing to lose. He described it as giving students “learning scars” – those times you made a serious error that left you with a lesson you’ll never forget.
“We’re trying to create learning scars, but in a safe scenario.”
As the hospitalist tried to position the portable video laryngoscope properly in the airway of the critically ill “patient,” HM19 faculty moderator Brian Kaufman, MD, professor of medicine, anesthesiology, and neurology at New York University (NYU) School of Medicine, issued a word of caution: Rotating it into position should be done gently or there’s a risk of tearing tissue.
One step at a time, hospitalists attending the session grew more confident and knowledgeable in handling urgent matters involving patients who are critically ill, including cases of shock, mechanical ventilation, overdoses, and ultrasound.
Kevin Felner, MD, associate professor of medicine at NYU School of Medicine, said there’s a growing need for more exposure to caring for the critically ill, including intubation.
“There are a lot of hospitalists who are intubating, and they’re not formally trained in it because medicine residencies don’t typically train people to manage airways,” he said. “We’ve met hospitalists who’ve said, ‘I was hired and was told I had to manage an airway.’”
“It might massage some of the things you’re doing, make you afraid of things you should be afraid of, make you think about something that’s easy to do that you’re not doing, and make things safer,” Dr. Felner said.
In a simulation room, James Horowitz, MD, clinical assistant professor and cardiologist at NYU School of Medicine, demonstrated how to use a laryngeal mask airway (LMA), a simpler alternative to intubating the trachea for keeping an airway open. Dr. Kaufman, standing next to him, clarified how important a skill this is, especially when someone needs air in the next minute or is at risk of death.
“Knowing how to put an LMA in can be life-saving,” Dr. Kaufman said.
In a lecture on shock in the critically ill, Dr. Felner said it’s important to be nimble in handling this common problem –quickly identifying the cause, whether it’s a cardiogenic issue, a low-volume circulation problem, a question of vasodilation, or an obstructive problem. He said guidelines – such as aiming for a mean arterial pressure of 65 mm Hg –are helpful generally, but individuals routinely call for making exceptions to guidelines.
Anthony Andriotis, MD, a pulmonologist at NYU who specializes in critical care, offered an array of key points when managing patients with a ventilator. For instance, when you need to prolong a patient’s expiratory time so they can exhale air more effectively to get rid of entrapped air in their lungs, lowering their respiratory rate is far more effective than decreasing the time it takes them to breathe in or increasing the flow rate of the air they’re breathing.
Some basic points – such as remembering that it’s important to be aware of the pressure when volume control has been imposed and to be aware of volume control when the pressure has been set – are crucial, he said.
The idea behind the pre-course, Dr. Felner said, was to give hospitalists a chance to enter tricky situations with everything to gain, but nothing to lose. He described it as giving students “learning scars” – those times you made a serious error that left you with a lesson you’ll never forget.
“We’re trying to create learning scars, but in a safe scenario.”
Experts offer HM19 ‘must-see’ tips
There are about as many sessions at HM19 as there are cherry blossoms on the springtime trees in the nation’s capital. Attendees are bound to find something they love – probably too many somethings, in fact.
Fear not. Seasoned experts are here to ease your struggle with suggestions for sessions they consider the best of the best and tips on getting the most out of the conference.
“Download the HM19 At Hand app to plan your conference schedule, rate speakers and sessions, and participate in audience-response systems,” said Dustin Smith, MD, SFHM, the HM19 course director and associate professor of medicine at Emory University, Atlanta. “Read the track descriptions first before reviewing the individual sessions to determine which educational tracks initially pique your interest. Don’t be wedded to one track; pick and choose sessions from the different tracks to curate a schedule that best fits your educational needs.”
SHM staff and Annual Conference committee members will be easily identifiable and eager to help on site, Dr. Smith added.
HM19 was the first Annual Conference for which SHM issued a call for content to members and nonmembers alike. The contributions yielded a few new offerings. A new Clinical Mastery track includes sessions for hospitalists wanting to enhance or refine their skills in an effort to achieve a master clinician designation, Dr. Smith said, while the new Between the Guidelines track explores clinical conundrums and lessons from history that may not be covered in clinical practice guidelines.
There also is a new Palliative Care and Pain Management pre-course and a new course on emergent airway management, Dr. Smith noted. His suggestions for sessions that are new, have a new format, or are particularly timely, are too numerous to list in full but include a fun “Medical Jeopardy” session (Wednesday, 9:10 – 9:50 a.m., Maryland C), sessions on discharge dilemmas (Monday, 11:25 a.m. to 12:05 p.m., Maryland BD/4-6) and LGBTQ health (Wednesday, 10:50 to 11:30 a.m., Maryland BD/4-6) and the workshop “Being Fe(male) in Hospital Medicine Part 2: Diversifying the Discussion” (Tuesday, 2:10 to 3:40 p.m., Potomac 1-3).
The Hospitalist polled its editorial advisory board members for each of their top two suggestions for “must-see” sessions:
Raman Palabindala, MD, SFHM, hospital medicine division chief at the University of Mississippi Medical Center
“A Battle Plan Against Career Inertia: A Blueprint for an Education Series to Retain Hospitalists, Reduce Burnout and Advance Careers” (Monday, 10:35 a.m. – 12:05 p.m., Potomac 1-3)
“I strongly recommend this to all hospitalist leaders – in big or small programs – given the importance of burnout in recent years. [Speaker] Dan Hunt is one of the best,” Dr. Palabindala said.
Special Interest Forums (Monday, 4:30 – 5:25 p.m., Tuesday, 5:30 – 6:25 p.m., multiple rooms)
Dr. Palabindala said these are valuable, small sessions when you have a focused interest in a certain topic – whether IT, academics, policy, or others.
“This is the best place to make contacts with national leaders,” he said. “Be proactive in confirming your spot.”
James Kim, MD, assistant professor of medicine at Emory University
“Delirium and Dementia in the Inpatient Setting” (Tuesday, 11:50 a.m. – 12:30 p.m., Maryland BD/4-6)
“This session is a repeat from previous years, but it is an engaging lecture with a lot of great material,” Dr. Kim said. “It has changed my approach to my practice of inpatients.”
“The Role of Primary Palliative Care in Complex, Chronic Disease Management” (Tuesday, 3:50 – 4:50 p.m., National Harbor 12-13)
“As the population grows older, palliative care’s role in disease management is going to become more important,” he said. “I watched one of Dr. [Aziz] Ansari’s lectures in a previous SHM meeting, and he delivers a dynamic presentation that is both informative and entertaining.”
Hyung (Harry) Cho, MD, SFHM, chief value officer at NYC Health + Hospitals
“Tweet your Way to the Top? Social Media as a Career Development Tool in Hospital Medicine” (Monday, 12:45 – 2:15 p.m., Potomac 1-3)
This includes a team of presenters who are experienced in the use of Twitter in conjunction with the Journal of Hospital Medicine, Dr. Cho said.
“Research Shark Tank” (Monday, 1:35 – 2:35 p.m., Baltimore 3-5)
This session involves judging and critiquing the latest research proposals with “contestants” in a Shark Tank format. Among the judges is Andrew Auerbach, MD, SFHM, past editor of the JHM. It “looks very engaging,” Dr. Cho said.
Lonika Sood, MD, FHM, clinical education director of internal medicine at Washington State University
“Making Your Educational Activities Count Twice: What it Takes These Days to Publish in Medical Education Journals” (Wednesday, 8:40 – 9:40 a.m., Baltimore 3-5)
“This is an important topic for clinician educators who are interested in taking a scholarly approach to their teaching,” Dr. Sood said. “Having some form of a framework to guide us in the direction of publishing our hard work will be very helpful.”“Managing the Hidden Curriculum: Do
You Know What You’re Teaching?” (Monday, 10:35 – 11:35 a.m., Baltimore 3-5)
“This is also an important, yet ‘hidden’ topic for the clinician educator when they are in the clinical environment with learners. Having hospitalists be aware of what is actually being ‘learned’ as opposed to what they think is being ‘taught’ on the wards is a critical part of the teaching process.”
Raj Sehgal, MD, FHM, clinical associate professor at South Texas Veterans Health Care System and UT Health San Antonio
“Call Night: Common Scenarios Encountered and Strategies to Make It Through the Night” (Monday, 10:35 – 11:15 a.m., Annapolis) and “Nocturnal Admissions: Cases That Keep Me Up at Night” (Monday, 2 – 2:40 p.m., Maryland A/1-3)
“I’m glad to see several different sessions about issues hospitalists face when working nights,” Dr. Sehgal said. “After all, most hours of the week are actually ‘off-hours’ (nights and weekends), so it’s important to focus on how care is delivered during these times. Even though we see the same diagnoses regardless of the time of day, our management is often very different because of external forces, such as the availability of tests and consultants.”
Marina Farah, MD, MHA, a national expert on improving clinical quality, cost, and efficiency
"Delivering Population Health as a Hospitalist in a Value-Based Healthcare Era” (Monday, 3:45 – 4:25 p.m., Maryland A/1-3)
“Hospital care is responsible for a third of the U.S. health care spending,” Dr. Farah said. “Hospitalists serve 75% of total hospital patients and have a unique perspective and power to drive national health care outcomes. This session will offer guidance on what hospitalists can do to improve population health, decrease total cost of care, and succeed under value-based reimbursement models.”
“Things We Do for No Reason: The 2019 Clinical Update for Hospitalists” (Tuesday, 11:50 a.m. – 12:30 p.m., Woodrow Wilson)
“Every hospitalist needs to know clinical practices that aren’t evidence-based, costly, and do not improve patient outcomes,” she said.
Amith Skandhan, MD, SFHM, assistant professor and medical director/clinical liaison for clinical documentation improvement at Southeast Health Medical Center
“How To Be a Great Teaching Attending” (Wednesday, 10 – 10:40 a.m., Maryland C)
“Being an academic hospitalist, I look up to great inpatient teachers,” Dr. Skandhan said. “Dr. [Jeffrey] Wiese has an amazing presence when he talks. His book on bedside teaching has been quite a guide for me as I embarked on my journey as a teacher.”
“Amplify Your Impact: Leverage Data to Accelerate Your Efforts in Quality Improvement” (Tuesday, 3:50 – 5:20 p.m., Potomac 1-3)
“Hospital medicine is a fairly new branch of medicine, and we are now the leaders of inpatient quality improvement,” he said. “To understand data and to convert it to useful information that can be utilized in quality improvement strategies would be great.”
Danielle Scheurer, MD, SFHM, physician editor of The Hospitalist and chief quality officer, Medical University of South Carolina
“Top New Guidelines Every Hospitalist Needs to Know in Clinical Practice” (Monday, 10:35 - 11:15 a.m., Woodrow Wilson)
“It’s important to remain up to date on all the new guideline releases.”“
Your Hospital, Your Group and Yourself: Opportunities for Promoting Well Being and Reducing Burnout” (Monday, 1:35 - 2:35 p.m., National Harbor 12-13)
“This session will help you and your teams to garner ideas and tactics for reducing the prevalence of burnout,” she said.
For more information on the HM19 education sessions, check the latest version of the conference schedule at https://shmannualconference.org/interactive-schedule/ .
There are about as many sessions at HM19 as there are cherry blossoms on the springtime trees in the nation’s capital. Attendees are bound to find something they love – probably too many somethings, in fact.
Fear not. Seasoned experts are here to ease your struggle with suggestions for sessions they consider the best of the best and tips on getting the most out of the conference.
“Download the HM19 At Hand app to plan your conference schedule, rate speakers and sessions, and participate in audience-response systems,” said Dustin Smith, MD, SFHM, the HM19 course director and associate professor of medicine at Emory University, Atlanta. “Read the track descriptions first before reviewing the individual sessions to determine which educational tracks initially pique your interest. Don’t be wedded to one track; pick and choose sessions from the different tracks to curate a schedule that best fits your educational needs.”
SHM staff and Annual Conference committee members will be easily identifiable and eager to help on site, Dr. Smith added.
HM19 was the first Annual Conference for which SHM issued a call for content to members and nonmembers alike. The contributions yielded a few new offerings. A new Clinical Mastery track includes sessions for hospitalists wanting to enhance or refine their skills in an effort to achieve a master clinician designation, Dr. Smith said, while the new Between the Guidelines track explores clinical conundrums and lessons from history that may not be covered in clinical practice guidelines.
There also is a new Palliative Care and Pain Management pre-course and a new course on emergent airway management, Dr. Smith noted. His suggestions for sessions that are new, have a new format, or are particularly timely, are too numerous to list in full but include a fun “Medical Jeopardy” session (Wednesday, 9:10 – 9:50 a.m., Maryland C), sessions on discharge dilemmas (Monday, 11:25 a.m. to 12:05 p.m., Maryland BD/4-6) and LGBTQ health (Wednesday, 10:50 to 11:30 a.m., Maryland BD/4-6) and the workshop “Being Fe(male) in Hospital Medicine Part 2: Diversifying the Discussion” (Tuesday, 2:10 to 3:40 p.m., Potomac 1-3).
The Hospitalist polled its editorial advisory board members for each of their top two suggestions for “must-see” sessions:
Raman Palabindala, MD, SFHM, hospital medicine division chief at the University of Mississippi Medical Center
“A Battle Plan Against Career Inertia: A Blueprint for an Education Series to Retain Hospitalists, Reduce Burnout and Advance Careers” (Monday, 10:35 a.m. – 12:05 p.m., Potomac 1-3)
“I strongly recommend this to all hospitalist leaders – in big or small programs – given the importance of burnout in recent years. [Speaker] Dan Hunt is one of the best,” Dr. Palabindala said.
Special Interest Forums (Monday, 4:30 – 5:25 p.m., Tuesday, 5:30 – 6:25 p.m., multiple rooms)
Dr. Palabindala said these are valuable, small sessions when you have a focused interest in a certain topic – whether IT, academics, policy, or others.
“This is the best place to make contacts with national leaders,” he said. “Be proactive in confirming your spot.”
James Kim, MD, assistant professor of medicine at Emory University
“Delirium and Dementia in the Inpatient Setting” (Tuesday, 11:50 a.m. – 12:30 p.m., Maryland BD/4-6)
“This session is a repeat from previous years, but it is an engaging lecture with a lot of great material,” Dr. Kim said. “It has changed my approach to my practice of inpatients.”
“The Role of Primary Palliative Care in Complex, Chronic Disease Management” (Tuesday, 3:50 – 4:50 p.m., National Harbor 12-13)
“As the population grows older, palliative care’s role in disease management is going to become more important,” he said. “I watched one of Dr. [Aziz] Ansari’s lectures in a previous SHM meeting, and he delivers a dynamic presentation that is both informative and entertaining.”
Hyung (Harry) Cho, MD, SFHM, chief value officer at NYC Health + Hospitals
“Tweet your Way to the Top? Social Media as a Career Development Tool in Hospital Medicine” (Monday, 12:45 – 2:15 p.m., Potomac 1-3)
This includes a team of presenters who are experienced in the use of Twitter in conjunction with the Journal of Hospital Medicine, Dr. Cho said.
“Research Shark Tank” (Monday, 1:35 – 2:35 p.m., Baltimore 3-5)
This session involves judging and critiquing the latest research proposals with “contestants” in a Shark Tank format. Among the judges is Andrew Auerbach, MD, SFHM, past editor of the JHM. It “looks very engaging,” Dr. Cho said.
Lonika Sood, MD, FHM, clinical education director of internal medicine at Washington State University
“Making Your Educational Activities Count Twice: What it Takes These Days to Publish in Medical Education Journals” (Wednesday, 8:40 – 9:40 a.m., Baltimore 3-5)
“This is an important topic for clinician educators who are interested in taking a scholarly approach to their teaching,” Dr. Sood said. “Having some form of a framework to guide us in the direction of publishing our hard work will be very helpful.”“Managing the Hidden Curriculum: Do
You Know What You’re Teaching?” (Monday, 10:35 – 11:35 a.m., Baltimore 3-5)
“This is also an important, yet ‘hidden’ topic for the clinician educator when they are in the clinical environment with learners. Having hospitalists be aware of what is actually being ‘learned’ as opposed to what they think is being ‘taught’ on the wards is a critical part of the teaching process.”
Raj Sehgal, MD, FHM, clinical associate professor at South Texas Veterans Health Care System and UT Health San Antonio
“Call Night: Common Scenarios Encountered and Strategies to Make It Through the Night” (Monday, 10:35 – 11:15 a.m., Annapolis) and “Nocturnal Admissions: Cases That Keep Me Up at Night” (Monday, 2 – 2:40 p.m., Maryland A/1-3)
“I’m glad to see several different sessions about issues hospitalists face when working nights,” Dr. Sehgal said. “After all, most hours of the week are actually ‘off-hours’ (nights and weekends), so it’s important to focus on how care is delivered during these times. Even though we see the same diagnoses regardless of the time of day, our management is often very different because of external forces, such as the availability of tests and consultants.”
Marina Farah, MD, MHA, a national expert on improving clinical quality, cost, and efficiency
"Delivering Population Health as a Hospitalist in a Value-Based Healthcare Era” (Monday, 3:45 – 4:25 p.m., Maryland A/1-3)
“Hospital care is responsible for a third of the U.S. health care spending,” Dr. Farah said. “Hospitalists serve 75% of total hospital patients and have a unique perspective and power to drive national health care outcomes. This session will offer guidance on what hospitalists can do to improve population health, decrease total cost of care, and succeed under value-based reimbursement models.”
“Things We Do for No Reason: The 2019 Clinical Update for Hospitalists” (Tuesday, 11:50 a.m. – 12:30 p.m., Woodrow Wilson)
“Every hospitalist needs to know clinical practices that aren’t evidence-based, costly, and do not improve patient outcomes,” she said.
Amith Skandhan, MD, SFHM, assistant professor and medical director/clinical liaison for clinical documentation improvement at Southeast Health Medical Center
“How To Be a Great Teaching Attending” (Wednesday, 10 – 10:40 a.m., Maryland C)
“Being an academic hospitalist, I look up to great inpatient teachers,” Dr. Skandhan said. “Dr. [Jeffrey] Wiese has an amazing presence when he talks. His book on bedside teaching has been quite a guide for me as I embarked on my journey as a teacher.”
“Amplify Your Impact: Leverage Data to Accelerate Your Efforts in Quality Improvement” (Tuesday, 3:50 – 5:20 p.m., Potomac 1-3)
“Hospital medicine is a fairly new branch of medicine, and we are now the leaders of inpatient quality improvement,” he said. “To understand data and to convert it to useful information that can be utilized in quality improvement strategies would be great.”
Danielle Scheurer, MD, SFHM, physician editor of The Hospitalist and chief quality officer, Medical University of South Carolina
“Top New Guidelines Every Hospitalist Needs to Know in Clinical Practice” (Monday, 10:35 - 11:15 a.m., Woodrow Wilson)
“It’s important to remain up to date on all the new guideline releases.”“
Your Hospital, Your Group and Yourself: Opportunities for Promoting Well Being and Reducing Burnout” (Monday, 1:35 - 2:35 p.m., National Harbor 12-13)
“This session will help you and your teams to garner ideas and tactics for reducing the prevalence of burnout,” she said.
For more information on the HM19 education sessions, check the latest version of the conference schedule at https://shmannualconference.org/interactive-schedule/ .
There are about as many sessions at HM19 as there are cherry blossoms on the springtime trees in the nation’s capital. Attendees are bound to find something they love – probably too many somethings, in fact.
Fear not. Seasoned experts are here to ease your struggle with suggestions for sessions they consider the best of the best and tips on getting the most out of the conference.
“Download the HM19 At Hand app to plan your conference schedule, rate speakers and sessions, and participate in audience-response systems,” said Dustin Smith, MD, SFHM, the HM19 course director and associate professor of medicine at Emory University, Atlanta. “Read the track descriptions first before reviewing the individual sessions to determine which educational tracks initially pique your interest. Don’t be wedded to one track; pick and choose sessions from the different tracks to curate a schedule that best fits your educational needs.”
SHM staff and Annual Conference committee members will be easily identifiable and eager to help on site, Dr. Smith added.
HM19 was the first Annual Conference for which SHM issued a call for content to members and nonmembers alike. The contributions yielded a few new offerings. A new Clinical Mastery track includes sessions for hospitalists wanting to enhance or refine their skills in an effort to achieve a master clinician designation, Dr. Smith said, while the new Between the Guidelines track explores clinical conundrums and lessons from history that may not be covered in clinical practice guidelines.
There also is a new Palliative Care and Pain Management pre-course and a new course on emergent airway management, Dr. Smith noted. His suggestions for sessions that are new, have a new format, or are particularly timely, are too numerous to list in full but include a fun “Medical Jeopardy” session (Wednesday, 9:10 – 9:50 a.m., Maryland C), sessions on discharge dilemmas (Monday, 11:25 a.m. to 12:05 p.m., Maryland BD/4-6) and LGBTQ health (Wednesday, 10:50 to 11:30 a.m., Maryland BD/4-6) and the workshop “Being Fe(male) in Hospital Medicine Part 2: Diversifying the Discussion” (Tuesday, 2:10 to 3:40 p.m., Potomac 1-3).
The Hospitalist polled its editorial advisory board members for each of their top two suggestions for “must-see” sessions:
Raman Palabindala, MD, SFHM, hospital medicine division chief at the University of Mississippi Medical Center
“A Battle Plan Against Career Inertia: A Blueprint for an Education Series to Retain Hospitalists, Reduce Burnout and Advance Careers” (Monday, 10:35 a.m. – 12:05 p.m., Potomac 1-3)
“I strongly recommend this to all hospitalist leaders – in big or small programs – given the importance of burnout in recent years. [Speaker] Dan Hunt is one of the best,” Dr. Palabindala said.
Special Interest Forums (Monday, 4:30 – 5:25 p.m., Tuesday, 5:30 – 6:25 p.m., multiple rooms)
Dr. Palabindala said these are valuable, small sessions when you have a focused interest in a certain topic – whether IT, academics, policy, or others.
“This is the best place to make contacts with national leaders,” he said. “Be proactive in confirming your spot.”
James Kim, MD, assistant professor of medicine at Emory University
“Delirium and Dementia in the Inpatient Setting” (Tuesday, 11:50 a.m. – 12:30 p.m., Maryland BD/4-6)
“This session is a repeat from previous years, but it is an engaging lecture with a lot of great material,” Dr. Kim said. “It has changed my approach to my practice of inpatients.”
“The Role of Primary Palliative Care in Complex, Chronic Disease Management” (Tuesday, 3:50 – 4:50 p.m., National Harbor 12-13)
“As the population grows older, palliative care’s role in disease management is going to become more important,” he said. “I watched one of Dr. [Aziz] Ansari’s lectures in a previous SHM meeting, and he delivers a dynamic presentation that is both informative and entertaining.”
Hyung (Harry) Cho, MD, SFHM, chief value officer at NYC Health + Hospitals
“Tweet your Way to the Top? Social Media as a Career Development Tool in Hospital Medicine” (Monday, 12:45 – 2:15 p.m., Potomac 1-3)
This includes a team of presenters who are experienced in the use of Twitter in conjunction with the Journal of Hospital Medicine, Dr. Cho said.
“Research Shark Tank” (Monday, 1:35 – 2:35 p.m., Baltimore 3-5)
This session involves judging and critiquing the latest research proposals with “contestants” in a Shark Tank format. Among the judges is Andrew Auerbach, MD, SFHM, past editor of the JHM. It “looks very engaging,” Dr. Cho said.
Lonika Sood, MD, FHM, clinical education director of internal medicine at Washington State University
“Making Your Educational Activities Count Twice: What it Takes These Days to Publish in Medical Education Journals” (Wednesday, 8:40 – 9:40 a.m., Baltimore 3-5)
“This is an important topic for clinician educators who are interested in taking a scholarly approach to their teaching,” Dr. Sood said. “Having some form of a framework to guide us in the direction of publishing our hard work will be very helpful.”“Managing the Hidden Curriculum: Do
You Know What You’re Teaching?” (Monday, 10:35 – 11:35 a.m., Baltimore 3-5)
“This is also an important, yet ‘hidden’ topic for the clinician educator when they are in the clinical environment with learners. Having hospitalists be aware of what is actually being ‘learned’ as opposed to what they think is being ‘taught’ on the wards is a critical part of the teaching process.”
Raj Sehgal, MD, FHM, clinical associate professor at South Texas Veterans Health Care System and UT Health San Antonio
“Call Night: Common Scenarios Encountered and Strategies to Make It Through the Night” (Monday, 10:35 – 11:15 a.m., Annapolis) and “Nocturnal Admissions: Cases That Keep Me Up at Night” (Monday, 2 – 2:40 p.m., Maryland A/1-3)
“I’m glad to see several different sessions about issues hospitalists face when working nights,” Dr. Sehgal said. “After all, most hours of the week are actually ‘off-hours’ (nights and weekends), so it’s important to focus on how care is delivered during these times. Even though we see the same diagnoses regardless of the time of day, our management is often very different because of external forces, such as the availability of tests and consultants.”
Marina Farah, MD, MHA, a national expert on improving clinical quality, cost, and efficiency
"Delivering Population Health as a Hospitalist in a Value-Based Healthcare Era” (Monday, 3:45 – 4:25 p.m., Maryland A/1-3)
“Hospital care is responsible for a third of the U.S. health care spending,” Dr. Farah said. “Hospitalists serve 75% of total hospital patients and have a unique perspective and power to drive national health care outcomes. This session will offer guidance on what hospitalists can do to improve population health, decrease total cost of care, and succeed under value-based reimbursement models.”
“Things We Do for No Reason: The 2019 Clinical Update for Hospitalists” (Tuesday, 11:50 a.m. – 12:30 p.m., Woodrow Wilson)
“Every hospitalist needs to know clinical practices that aren’t evidence-based, costly, and do not improve patient outcomes,” she said.
Amith Skandhan, MD, SFHM, assistant professor and medical director/clinical liaison for clinical documentation improvement at Southeast Health Medical Center
“How To Be a Great Teaching Attending” (Wednesday, 10 – 10:40 a.m., Maryland C)
“Being an academic hospitalist, I look up to great inpatient teachers,” Dr. Skandhan said. “Dr. [Jeffrey] Wiese has an amazing presence when he talks. His book on bedside teaching has been quite a guide for me as I embarked on my journey as a teacher.”
“Amplify Your Impact: Leverage Data to Accelerate Your Efforts in Quality Improvement” (Tuesday, 3:50 – 5:20 p.m., Potomac 1-3)
“Hospital medicine is a fairly new branch of medicine, and we are now the leaders of inpatient quality improvement,” he said. “To understand data and to convert it to useful information that can be utilized in quality improvement strategies would be great.”
Danielle Scheurer, MD, SFHM, physician editor of The Hospitalist and chief quality officer, Medical University of South Carolina
“Top New Guidelines Every Hospitalist Needs to Know in Clinical Practice” (Monday, 10:35 - 11:15 a.m., Woodrow Wilson)
“It’s important to remain up to date on all the new guideline releases.”“
Your Hospital, Your Group and Yourself: Opportunities for Promoting Well Being and Reducing Burnout” (Monday, 1:35 - 2:35 p.m., National Harbor 12-13)
“This session will help you and your teams to garner ideas and tactics for reducing the prevalence of burnout,” she said.
For more information on the HM19 education sessions, check the latest version of the conference schedule at https://shmannualconference.org/interactive-schedule/ .
Luncheon makes connecting easy
There’s a senior faculty member you respect, and you want to pick their brain about a career decision you face. How do you go about this? Send an email, cold? What if you don’t hear back? Were they too busy or disinclined, or did it just get overlooked in the heap?
Do you try and catch up with them in the hallway at the annual conference and introduce yourself? What if it’s rushed or awkward?
How about someone plans a lunch for you to attend, and you sit down with this person with a block of time to chat? Now that sounds like a much better option.
This is the idea behind the Resident and Student Luncheon at HM19. At Monday’s luncheon, residents and students can have a conversation, facilitated by Society of Hospital Medicine committee members, with experienced faculty members in quality improvement, pediatrics, informatics, advocacy, and other areas.
Brian Kwan, MD, FHM, chair of the Physicians-in-Training SHM committee, said the event is meant to clear a path to interactions.
“Say you’re attending the tracks – you’ll meet people maybe next to you, but it’s sometimes hard to start those conversations,” he said. “So I think that what the luncheon allows them to do is provide a place [to meet]. And it’s a little bit more formal, because we have a structure to it. We have a program that we follow in order to kind of provide structure. That way it allows people to really get in and make the connection.”
The luncheon is open at no extra charge to resident and student SHM members. It is capped at a total of 100 attendees, including the 10 invited faculty experts – 1 per table – and Physicians-in-Training committee members, who will be there to help make introductions and move the discussion along. Residents and students first will sit at a table and hear faculty introductions – which might give them exposure to an area about which they are unfamiliar – and then have an opportunity to interact with faculty at their table. After that they will move to a table of their choosing for the second half of the event.
The luncheon often involves big names attendees see on stage. The details are still being ironed out for this year, but past luncheon guests have included keynote speakers and Bob Wachter, MD, MHM, chair of medicine at the University of California, San Francisco, who is considered the “father of hospital medicine.”
Dr. Kwan said the event can have big implications for a young hospitalist’s career. A current committee member, he said, met their current employer at the luncheon.
The event also is envisioned as a way for students and residents to meet and discuss their career options, Dr. Kwan said.
“It’s an opportunity to both have residents and students connect, but also for them to potentially connect to other aspects of hospital medicine that they might be interested in,” he said.
The luncheon is only one way that HM19 planners have made a point to meet the needs of those who have just embarked on their careers.
The Early-Career Hospitalist track, which runs from 10:35 a.m. to 1:50 p.m. on Monday, includes sessions on common scenarios encountered at night (“Call Night: Common Scenarios Encountered and Strategies to Make it Through the Night,” 10:35 a.m. – 11:15 a.m., Annapolis) an introduction to hospitalist billing (“Hospitalist Billing 101,” 11:25 a.m. – 12:05 p.m., Annapolis), and important bedrock literature (“A Whirlwind Tour of Famous Landmark [Articles]: Must-Know Literature to Impress Your Peers and Attendings,” 1:10 p.m. – 1:50 p.m., Annapolis).
An interview workshop is also planned (Tuesday, 6:00 p.m. – 7:00 p.m., Magnolia 3) and a Trivia Night for residents and students is also being considered, Dr. Kwan said.
Kevin Vuernick, membership engagement manager for SHM, said that these events are a response to feedback gleaned from those early in their career, including focus groups with students and residents.
“One of the things we heard was that they would love opportunities to network with other physicians or with members who have been at the Society for a while and are established in their careers, and how they can break into specifically hospital medicine,” he said. The luncheon is “just an hour but at least it gives them a healthy dose of being able to interact with people one on one or in a smaller setting.”
Resident and Student Luncheon
Monday, 12:00 p.m. –1:00 p.m.
National Harbor 4-5
There’s a senior faculty member you respect, and you want to pick their brain about a career decision you face. How do you go about this? Send an email, cold? What if you don’t hear back? Were they too busy or disinclined, or did it just get overlooked in the heap?
Do you try and catch up with them in the hallway at the annual conference and introduce yourself? What if it’s rushed or awkward?
How about someone plans a lunch for you to attend, and you sit down with this person with a block of time to chat? Now that sounds like a much better option.
This is the idea behind the Resident and Student Luncheon at HM19. At Monday’s luncheon, residents and students can have a conversation, facilitated by Society of Hospital Medicine committee members, with experienced faculty members in quality improvement, pediatrics, informatics, advocacy, and other areas.
Brian Kwan, MD, FHM, chair of the Physicians-in-Training SHM committee, said the event is meant to clear a path to interactions.
“Say you’re attending the tracks – you’ll meet people maybe next to you, but it’s sometimes hard to start those conversations,” he said. “So I think that what the luncheon allows them to do is provide a place [to meet]. And it’s a little bit more formal, because we have a structure to it. We have a program that we follow in order to kind of provide structure. That way it allows people to really get in and make the connection.”
The luncheon is open at no extra charge to resident and student SHM members. It is capped at a total of 100 attendees, including the 10 invited faculty experts – 1 per table – and Physicians-in-Training committee members, who will be there to help make introductions and move the discussion along. Residents and students first will sit at a table and hear faculty introductions – which might give them exposure to an area about which they are unfamiliar – and then have an opportunity to interact with faculty at their table. After that they will move to a table of their choosing for the second half of the event.
The luncheon often involves big names attendees see on stage. The details are still being ironed out for this year, but past luncheon guests have included keynote speakers and Bob Wachter, MD, MHM, chair of medicine at the University of California, San Francisco, who is considered the “father of hospital medicine.”
Dr. Kwan said the event can have big implications for a young hospitalist’s career. A current committee member, he said, met their current employer at the luncheon.
The event also is envisioned as a way for students and residents to meet and discuss their career options, Dr. Kwan said.
“It’s an opportunity to both have residents and students connect, but also for them to potentially connect to other aspects of hospital medicine that they might be interested in,” he said.
The luncheon is only one way that HM19 planners have made a point to meet the needs of those who have just embarked on their careers.
The Early-Career Hospitalist track, which runs from 10:35 a.m. to 1:50 p.m. on Monday, includes sessions on common scenarios encountered at night (“Call Night: Common Scenarios Encountered and Strategies to Make it Through the Night,” 10:35 a.m. – 11:15 a.m., Annapolis) an introduction to hospitalist billing (“Hospitalist Billing 101,” 11:25 a.m. – 12:05 p.m., Annapolis), and important bedrock literature (“A Whirlwind Tour of Famous Landmark [Articles]: Must-Know Literature to Impress Your Peers and Attendings,” 1:10 p.m. – 1:50 p.m., Annapolis).
An interview workshop is also planned (Tuesday, 6:00 p.m. – 7:00 p.m., Magnolia 3) and a Trivia Night for residents and students is also being considered, Dr. Kwan said.
Kevin Vuernick, membership engagement manager for SHM, said that these events are a response to feedback gleaned from those early in their career, including focus groups with students and residents.
“One of the things we heard was that they would love opportunities to network with other physicians or with members who have been at the Society for a while and are established in their careers, and how they can break into specifically hospital medicine,” he said. The luncheon is “just an hour but at least it gives them a healthy dose of being able to interact with people one on one or in a smaller setting.”
Resident and Student Luncheon
Monday, 12:00 p.m. –1:00 p.m.
National Harbor 4-5
There’s a senior faculty member you respect, and you want to pick their brain about a career decision you face. How do you go about this? Send an email, cold? What if you don’t hear back? Were they too busy or disinclined, or did it just get overlooked in the heap?
Do you try and catch up with them in the hallway at the annual conference and introduce yourself? What if it’s rushed or awkward?
How about someone plans a lunch for you to attend, and you sit down with this person with a block of time to chat? Now that sounds like a much better option.
This is the idea behind the Resident and Student Luncheon at HM19. At Monday’s luncheon, residents and students can have a conversation, facilitated by Society of Hospital Medicine committee members, with experienced faculty members in quality improvement, pediatrics, informatics, advocacy, and other areas.
Brian Kwan, MD, FHM, chair of the Physicians-in-Training SHM committee, said the event is meant to clear a path to interactions.
“Say you’re attending the tracks – you’ll meet people maybe next to you, but it’s sometimes hard to start those conversations,” he said. “So I think that what the luncheon allows them to do is provide a place [to meet]. And it’s a little bit more formal, because we have a structure to it. We have a program that we follow in order to kind of provide structure. That way it allows people to really get in and make the connection.”
The luncheon is open at no extra charge to resident and student SHM members. It is capped at a total of 100 attendees, including the 10 invited faculty experts – 1 per table – and Physicians-in-Training committee members, who will be there to help make introductions and move the discussion along. Residents and students first will sit at a table and hear faculty introductions – which might give them exposure to an area about which they are unfamiliar – and then have an opportunity to interact with faculty at their table. After that they will move to a table of their choosing for the second half of the event.
The luncheon often involves big names attendees see on stage. The details are still being ironed out for this year, but past luncheon guests have included keynote speakers and Bob Wachter, MD, MHM, chair of medicine at the University of California, San Francisco, who is considered the “father of hospital medicine.”
Dr. Kwan said the event can have big implications for a young hospitalist’s career. A current committee member, he said, met their current employer at the luncheon.
The event also is envisioned as a way for students and residents to meet and discuss their career options, Dr. Kwan said.
“It’s an opportunity to both have residents and students connect, but also for them to potentially connect to other aspects of hospital medicine that they might be interested in,” he said.
The luncheon is only one way that HM19 planners have made a point to meet the needs of those who have just embarked on their careers.
The Early-Career Hospitalist track, which runs from 10:35 a.m. to 1:50 p.m. on Monday, includes sessions on common scenarios encountered at night (“Call Night: Common Scenarios Encountered and Strategies to Make it Through the Night,” 10:35 a.m. – 11:15 a.m., Annapolis) an introduction to hospitalist billing (“Hospitalist Billing 101,” 11:25 a.m. – 12:05 p.m., Annapolis), and important bedrock literature (“A Whirlwind Tour of Famous Landmark [Articles]: Must-Know Literature to Impress Your Peers and Attendings,” 1:10 p.m. – 1:50 p.m., Annapolis).
An interview workshop is also planned (Tuesday, 6:00 p.m. – 7:00 p.m., Magnolia 3) and a Trivia Night for residents and students is also being considered, Dr. Kwan said.
Kevin Vuernick, membership engagement manager for SHM, said that these events are a response to feedback gleaned from those early in their career, including focus groups with students and residents.
“One of the things we heard was that they would love opportunities to network with other physicians or with members who have been at the Society for a while and are established in their careers, and how they can break into specifically hospital medicine,” he said. The luncheon is “just an hour but at least it gives them a healthy dose of being able to interact with people one on one or in a smaller setting.”
Resident and Student Luncheon
Monday, 12:00 p.m. –1:00 p.m.
National Harbor 4-5
RIV brings competition, collaboration to HM19
A few years ago, participants in the Research, Innovations and Clinical Vignettes (RIV) competition at the annual conference presented a project based on a novel concept: A longitudinal ultrasound training program with portfolios and assessments for hospitalists.
In a way, the poster predicted a future trend, said Benji Mathews, MD, SFHM, chair of this year’s RIV competition, which will be held Monday and Tuesday. “That program itself had trained over 50 people by the time of the poster,” Dr. Mathews said. “Since that time, it has trained an additional 100 more. That program has been a rubric for some of the national and regional clinical ultrasound courses. Now the Society of Hospital Medicine has similar regional centers in bedside ultrasound” training.
It is common, Dr. Mathews said, for research, ideas, and programs displayed in the innovations portion of the RIV to become widespread in the field over the next 5-10 years. “I think the influence of this RIV program extends not only to me personally but beyond the conference and to my larger community. You’re seeing implications for the field of hospital medicine, not just today and in the past year. You’re seeing the future.”
The RIV event schedule includes:
- Research and Innovations Poster Competition – Monday, 5:30 p.m. to 7:30 p.m. in the Prince George’s Exhibit Hall
- Best of Research and Innovations in 2019 – Tuesday, 7:30 a.m. to 8:30 a.m. in Potomac ABCD
- Oral Presentations on the Top 15 Advances in Research and Innovations – Tuesday, 11:00 a.m. to 12:00 p.m.; 2:50 p.m. to 4:05 p.m.; and 4:15 p.m. to 5:15 p.m. in Baltimore 3-5
- Clinical Vignettes Poster Competition – Tuesday, 12:00 p.m. to 1:30 p.m. in the Prince George’s Exhibit Hall.
The “Research” portion highlights work done with sound methodology that has the potential to be applied regionally, nationally, and even internationally, Dr. Mathews said.
“Clinical Vignettes” are interesting case studies that often involve unraveling a clinical mystery and leaving the medical team with a lesson that can be applied more broadly.
“I love that a hospitalist at one side of the country can help provide pearls on a case, an innovation, or a research idea that can help improve diagnosis for a patient at the other side of the country,” Dr. Mathews said.
The winners of the live competition are chosen based on both content and presentation style, while abstracts chosen for oral presentation are the “cream of the cream of the crop,” rated by volunteer judges who are blinded to the names and institutions of the researchers, and then given a final review by the category chairs and Dr. Mathews himself. All chairs take into account the judges’ comments and make an attempt to balance for topic (such as pediatric vs. adult) and the types of presenting centers (such as rural vs. academic centers).
A total of 1,093 posters are scheduled to be shown at the meeting – about 300 in the Research category, about 200 in Innovations, and nearly 700 in Clinical Vignettes. It’s the first time the number of posters has surpassed 1,000, Dr. Mathews said. They were chosen from 1,659 submitted abstracts, which surpasses the 1,540 submissions last year but is down slightly from 2016 and 2017, when there were 1,678 and 1,712 submissions, respectively.
Dr. Mathews noted there were more submissions this year than ever before in the Innovations category – 262, up from the previous record of 235 in 2015. He also said the raw scores – those given by the blinded judges – of the accepted submissions have been rising every year and that the trend has continued this year.
He said he hopes to further boost the RIV’s profile on social media – to “continue the conversation” on platforms such as Twitter, particularly during the judging rounds.
Again this year, the work presented will raise important questions and issues in the field. One study looks at how doctors from other countries who work in rural centers have affected care in those areas. Another presents data – actually collected in work done at last year’s annual meeting – that calls into question the usefulness of evaluating inferior vena cava ultrasounds in a quantitative fashion, rather than qualitatively.
Another looks at the value in outcome measures that has stemmed from the use of telemedicine. And another assesses the prevalence of diagnostic error in a previous admission as the cause for readmissions.
While the event is billed as a competition, Dr. Mathews said the RIV is not, at its heart, a competitive event.
“It’s not all about winning,” he said. “One of my goals as the chair is to make sure it’s an atmosphere where people can engage and collaborate with each other.”
As a volunteer judge for many years and lead of the Innovations category for many years, Dr. Mathews’s fondness for the event is clear. “The best part of the conference is the RIV.”
A few years ago, participants in the Research, Innovations and Clinical Vignettes (RIV) competition at the annual conference presented a project based on a novel concept: A longitudinal ultrasound training program with portfolios and assessments for hospitalists.
In a way, the poster predicted a future trend, said Benji Mathews, MD, SFHM, chair of this year’s RIV competition, which will be held Monday and Tuesday. “That program itself had trained over 50 people by the time of the poster,” Dr. Mathews said. “Since that time, it has trained an additional 100 more. That program has been a rubric for some of the national and regional clinical ultrasound courses. Now the Society of Hospital Medicine has similar regional centers in bedside ultrasound” training.
It is common, Dr. Mathews said, for research, ideas, and programs displayed in the innovations portion of the RIV to become widespread in the field over the next 5-10 years. “I think the influence of this RIV program extends not only to me personally but beyond the conference and to my larger community. You’re seeing implications for the field of hospital medicine, not just today and in the past year. You’re seeing the future.”
The RIV event schedule includes:
- Research and Innovations Poster Competition – Monday, 5:30 p.m. to 7:30 p.m. in the Prince George’s Exhibit Hall
- Best of Research and Innovations in 2019 – Tuesday, 7:30 a.m. to 8:30 a.m. in Potomac ABCD
- Oral Presentations on the Top 15 Advances in Research and Innovations – Tuesday, 11:00 a.m. to 12:00 p.m.; 2:50 p.m. to 4:05 p.m.; and 4:15 p.m. to 5:15 p.m. in Baltimore 3-5
- Clinical Vignettes Poster Competition – Tuesday, 12:00 p.m. to 1:30 p.m. in the Prince George’s Exhibit Hall.
The “Research” portion highlights work done with sound methodology that has the potential to be applied regionally, nationally, and even internationally, Dr. Mathews said.
“Clinical Vignettes” are interesting case studies that often involve unraveling a clinical mystery and leaving the medical team with a lesson that can be applied more broadly.
“I love that a hospitalist at one side of the country can help provide pearls on a case, an innovation, or a research idea that can help improve diagnosis for a patient at the other side of the country,” Dr. Mathews said.
The winners of the live competition are chosen based on both content and presentation style, while abstracts chosen for oral presentation are the “cream of the cream of the crop,” rated by volunteer judges who are blinded to the names and institutions of the researchers, and then given a final review by the category chairs and Dr. Mathews himself. All chairs take into account the judges’ comments and make an attempt to balance for topic (such as pediatric vs. adult) and the types of presenting centers (such as rural vs. academic centers).
A total of 1,093 posters are scheduled to be shown at the meeting – about 300 in the Research category, about 200 in Innovations, and nearly 700 in Clinical Vignettes. It’s the first time the number of posters has surpassed 1,000, Dr. Mathews said. They were chosen from 1,659 submitted abstracts, which surpasses the 1,540 submissions last year but is down slightly from 2016 and 2017, when there were 1,678 and 1,712 submissions, respectively.
Dr. Mathews noted there were more submissions this year than ever before in the Innovations category – 262, up from the previous record of 235 in 2015. He also said the raw scores – those given by the blinded judges – of the accepted submissions have been rising every year and that the trend has continued this year.
He said he hopes to further boost the RIV’s profile on social media – to “continue the conversation” on platforms such as Twitter, particularly during the judging rounds.
Again this year, the work presented will raise important questions and issues in the field. One study looks at how doctors from other countries who work in rural centers have affected care in those areas. Another presents data – actually collected in work done at last year’s annual meeting – that calls into question the usefulness of evaluating inferior vena cava ultrasounds in a quantitative fashion, rather than qualitatively.
Another looks at the value in outcome measures that has stemmed from the use of telemedicine. And another assesses the prevalence of diagnostic error in a previous admission as the cause for readmissions.
While the event is billed as a competition, Dr. Mathews said the RIV is not, at its heart, a competitive event.
“It’s not all about winning,” he said. “One of my goals as the chair is to make sure it’s an atmosphere where people can engage and collaborate with each other.”
As a volunteer judge for many years and lead of the Innovations category for many years, Dr. Mathews’s fondness for the event is clear. “The best part of the conference is the RIV.”
A few years ago, participants in the Research, Innovations and Clinical Vignettes (RIV) competition at the annual conference presented a project based on a novel concept: A longitudinal ultrasound training program with portfolios and assessments for hospitalists.
In a way, the poster predicted a future trend, said Benji Mathews, MD, SFHM, chair of this year’s RIV competition, which will be held Monday and Tuesday. “That program itself had trained over 50 people by the time of the poster,” Dr. Mathews said. “Since that time, it has trained an additional 100 more. That program has been a rubric for some of the national and regional clinical ultrasound courses. Now the Society of Hospital Medicine has similar regional centers in bedside ultrasound” training.
It is common, Dr. Mathews said, for research, ideas, and programs displayed in the innovations portion of the RIV to become widespread in the field over the next 5-10 years. “I think the influence of this RIV program extends not only to me personally but beyond the conference and to my larger community. You’re seeing implications for the field of hospital medicine, not just today and in the past year. You’re seeing the future.”
The RIV event schedule includes:
- Research and Innovations Poster Competition – Monday, 5:30 p.m. to 7:30 p.m. in the Prince George’s Exhibit Hall
- Best of Research and Innovations in 2019 – Tuesday, 7:30 a.m. to 8:30 a.m. in Potomac ABCD
- Oral Presentations on the Top 15 Advances in Research and Innovations – Tuesday, 11:00 a.m. to 12:00 p.m.; 2:50 p.m. to 4:05 p.m.; and 4:15 p.m. to 5:15 p.m. in Baltimore 3-5
- Clinical Vignettes Poster Competition – Tuesday, 12:00 p.m. to 1:30 p.m. in the Prince George’s Exhibit Hall.
The “Research” portion highlights work done with sound methodology that has the potential to be applied regionally, nationally, and even internationally, Dr. Mathews said.
“Clinical Vignettes” are interesting case studies that often involve unraveling a clinical mystery and leaving the medical team with a lesson that can be applied more broadly.
“I love that a hospitalist at one side of the country can help provide pearls on a case, an innovation, or a research idea that can help improve diagnosis for a patient at the other side of the country,” Dr. Mathews said.
The winners of the live competition are chosen based on both content and presentation style, while abstracts chosen for oral presentation are the “cream of the cream of the crop,” rated by volunteer judges who are blinded to the names and institutions of the researchers, and then given a final review by the category chairs and Dr. Mathews himself. All chairs take into account the judges’ comments and make an attempt to balance for topic (such as pediatric vs. adult) and the types of presenting centers (such as rural vs. academic centers).
A total of 1,093 posters are scheduled to be shown at the meeting – about 300 in the Research category, about 200 in Innovations, and nearly 700 in Clinical Vignettes. It’s the first time the number of posters has surpassed 1,000, Dr. Mathews said. They were chosen from 1,659 submitted abstracts, which surpasses the 1,540 submissions last year but is down slightly from 2016 and 2017, when there were 1,678 and 1,712 submissions, respectively.
Dr. Mathews noted there were more submissions this year than ever before in the Innovations category – 262, up from the previous record of 235 in 2015. He also said the raw scores – those given by the blinded judges – of the accepted submissions have been rising every year and that the trend has continued this year.
He said he hopes to further boost the RIV’s profile on social media – to “continue the conversation” on platforms such as Twitter, particularly during the judging rounds.
Again this year, the work presented will raise important questions and issues in the field. One study looks at how doctors from other countries who work in rural centers have affected care in those areas. Another presents data – actually collected in work done at last year’s annual meeting – that calls into question the usefulness of evaluating inferior vena cava ultrasounds in a quantitative fashion, rather than qualitatively.
Another looks at the value in outcome measures that has stemmed from the use of telemedicine. And another assesses the prevalence of diagnostic error in a previous admission as the cause for readmissions.
While the event is billed as a competition, Dr. Mathews said the RIV is not, at its heart, a competitive event.
“It’s not all about winning,” he said. “One of my goals as the chair is to make sure it’s an atmosphere where people can engage and collaborate with each other.”
As a volunteer judge for many years and lead of the Innovations category for many years, Dr. Mathews’s fondness for the event is clear. “The best part of the conference is the RIV.”
Alcohol abstinence questioned as addiction treatment goal
BONITA SPRINGS, FLA. – Reductions in alcohol use bring about significant improvement in adverse consequences, mental health status, and quality of life, even if the reductions do not reach the level of abstinence, according to recent research presented at the annual meeting of the American Academy of Addiction Psychiatry.
The findings, experts say, demonstrate how a fixation on abstinence or elimination of all heavy drinking – the endpoints the Food and Drug Administration now require in pivotal clinical trials on alcohol use disorder (AUD) treatments – is shortsighted and can unnecessarily discourage people with alcohol use disorder from pursuing treatment.
“We need to think a little differently, or a little out of the box, from the way we’ve been thinking in the past,” said Raymond F. Anton, MD, professor of psychiatry at the Medical University of South Carolina in Charleston and chair of the Alcohol Clinical Trials Initiative (ACTIVE), a group advocating for a new endpoint that recognizes the benefits of lesser reductions in alcohol intake.
In a new analysis using data from the COMBINE study, researchers looked at the associations between reduction in World Health Organization drinking risk levels of alcohol consumption and clinically meaningful outcomes among people in treatment.
There are four levels: very high (more than 7.1 14-g drinks a day for men and more than 4.3 for women); high (4.3-7.1 or 2.9-4.3, respectively); moderate (2.9-4.3 or 1.4-2.9); and low (less than 2.9 or less than 1.4).
Researchers assessed responses to treatment with acamprosate, naltrexone, and psychological intervention in patients an average of 44 years old with 71% of their days being heavy drinking days. They found significant improvement in consequences tied to drinking, according to the Drinker Inventory of Consequences, and in mental health according to the Short Form Health Survey and the WHO Quality of Life assessment – even when the improvement was only by one WHO risk level – or just a few drinks a day – and did not involve abstaining (P less than .001 for all improvement categories).
“Reductions in WHO drinking risk levels are predictive of clinical benefit” or how the patient feels and functions, said Daniel Falk, PhD, health scientist administrator at the National Institute on Alcohol Abuse and Alcoholism.
The ACTIVE group he chairs, Dr. Anton said, is proposing that the FDA add a new endpoint for phase 3 trials: percentage of subjects who attain a 1- or 2-level reduction in WHO drinking risk levels.
Stephanie O’Malley, PhD, professor of psychiatry at Yale University in New Haven, Conn., said a 30-year-old with a moderate drinking problem – occasionally missing a family function, but never letting it interfere with work, say – might be turned off by a treatment plan that preaches abstinence, she said. Varenicline, for example, results in abstinence just 7% of the time, with some risk of suicidality and nausea. That person might not want to stop drinking entirely for the rest of his or her life, but could benefit by reducing the drinking, she said.
But 55% of the time, varenicline produces a reduction of one level of risk, which is associated with clinically meaningful results. That will sound much more appealing to a prospective patient, she said.
“From a clinical perspective, these WHO outcomes have some advantages,” she said. “I think you’re going to, one, encourage more people to accept treatment, and … be more optimistic about the outcomes.”
Dr. Anton reported consulting and/or funding from Alkermes, Allergan, Indivior, Insys Life Epigenetics, and Laboratori Farmaceutico CT. Dr. O’Malley reported consulting and/or funding from Alkermes, Amygdala, Indivior, Mistubishi Tanabe, Opiant, and other sources. Dr. Falk reported no disclosures.
BONITA SPRINGS, FLA. – Reductions in alcohol use bring about significant improvement in adverse consequences, mental health status, and quality of life, even if the reductions do not reach the level of abstinence, according to recent research presented at the annual meeting of the American Academy of Addiction Psychiatry.
The findings, experts say, demonstrate how a fixation on abstinence or elimination of all heavy drinking – the endpoints the Food and Drug Administration now require in pivotal clinical trials on alcohol use disorder (AUD) treatments – is shortsighted and can unnecessarily discourage people with alcohol use disorder from pursuing treatment.
“We need to think a little differently, or a little out of the box, from the way we’ve been thinking in the past,” said Raymond F. Anton, MD, professor of psychiatry at the Medical University of South Carolina in Charleston and chair of the Alcohol Clinical Trials Initiative (ACTIVE), a group advocating for a new endpoint that recognizes the benefits of lesser reductions in alcohol intake.
In a new analysis using data from the COMBINE study, researchers looked at the associations between reduction in World Health Organization drinking risk levels of alcohol consumption and clinically meaningful outcomes among people in treatment.
There are four levels: very high (more than 7.1 14-g drinks a day for men and more than 4.3 for women); high (4.3-7.1 or 2.9-4.3, respectively); moderate (2.9-4.3 or 1.4-2.9); and low (less than 2.9 or less than 1.4).
Researchers assessed responses to treatment with acamprosate, naltrexone, and psychological intervention in patients an average of 44 years old with 71% of their days being heavy drinking days. They found significant improvement in consequences tied to drinking, according to the Drinker Inventory of Consequences, and in mental health according to the Short Form Health Survey and the WHO Quality of Life assessment – even when the improvement was only by one WHO risk level – or just a few drinks a day – and did not involve abstaining (P less than .001 for all improvement categories).
“Reductions in WHO drinking risk levels are predictive of clinical benefit” or how the patient feels and functions, said Daniel Falk, PhD, health scientist administrator at the National Institute on Alcohol Abuse and Alcoholism.
The ACTIVE group he chairs, Dr. Anton said, is proposing that the FDA add a new endpoint for phase 3 trials: percentage of subjects who attain a 1- or 2-level reduction in WHO drinking risk levels.
Stephanie O’Malley, PhD, professor of psychiatry at Yale University in New Haven, Conn., said a 30-year-old with a moderate drinking problem – occasionally missing a family function, but never letting it interfere with work, say – might be turned off by a treatment plan that preaches abstinence, she said. Varenicline, for example, results in abstinence just 7% of the time, with some risk of suicidality and nausea. That person might not want to stop drinking entirely for the rest of his or her life, but could benefit by reducing the drinking, she said.
But 55% of the time, varenicline produces a reduction of one level of risk, which is associated with clinically meaningful results. That will sound much more appealing to a prospective patient, she said.
“From a clinical perspective, these WHO outcomes have some advantages,” she said. “I think you’re going to, one, encourage more people to accept treatment, and … be more optimistic about the outcomes.”
Dr. Anton reported consulting and/or funding from Alkermes, Allergan, Indivior, Insys Life Epigenetics, and Laboratori Farmaceutico CT. Dr. O’Malley reported consulting and/or funding from Alkermes, Amygdala, Indivior, Mistubishi Tanabe, Opiant, and other sources. Dr. Falk reported no disclosures.
BONITA SPRINGS, FLA. – Reductions in alcohol use bring about significant improvement in adverse consequences, mental health status, and quality of life, even if the reductions do not reach the level of abstinence, according to recent research presented at the annual meeting of the American Academy of Addiction Psychiatry.
The findings, experts say, demonstrate how a fixation on abstinence or elimination of all heavy drinking – the endpoints the Food and Drug Administration now require in pivotal clinical trials on alcohol use disorder (AUD) treatments – is shortsighted and can unnecessarily discourage people with alcohol use disorder from pursuing treatment.
“We need to think a little differently, or a little out of the box, from the way we’ve been thinking in the past,” said Raymond F. Anton, MD, professor of psychiatry at the Medical University of South Carolina in Charleston and chair of the Alcohol Clinical Trials Initiative (ACTIVE), a group advocating for a new endpoint that recognizes the benefits of lesser reductions in alcohol intake.
In a new analysis using data from the COMBINE study, researchers looked at the associations between reduction in World Health Organization drinking risk levels of alcohol consumption and clinically meaningful outcomes among people in treatment.
There are four levels: very high (more than 7.1 14-g drinks a day for men and more than 4.3 for women); high (4.3-7.1 or 2.9-4.3, respectively); moderate (2.9-4.3 or 1.4-2.9); and low (less than 2.9 or less than 1.4).
Researchers assessed responses to treatment with acamprosate, naltrexone, and psychological intervention in patients an average of 44 years old with 71% of their days being heavy drinking days. They found significant improvement in consequences tied to drinking, according to the Drinker Inventory of Consequences, and in mental health according to the Short Form Health Survey and the WHO Quality of Life assessment – even when the improvement was only by one WHO risk level – or just a few drinks a day – and did not involve abstaining (P less than .001 for all improvement categories).
“Reductions in WHO drinking risk levels are predictive of clinical benefit” or how the patient feels and functions, said Daniel Falk, PhD, health scientist administrator at the National Institute on Alcohol Abuse and Alcoholism.
The ACTIVE group he chairs, Dr. Anton said, is proposing that the FDA add a new endpoint for phase 3 trials: percentage of subjects who attain a 1- or 2-level reduction in WHO drinking risk levels.
Stephanie O’Malley, PhD, professor of psychiatry at Yale University in New Haven, Conn., said a 30-year-old with a moderate drinking problem – occasionally missing a family function, but never letting it interfere with work, say – might be turned off by a treatment plan that preaches abstinence, she said. Varenicline, for example, results in abstinence just 7% of the time, with some risk of suicidality and nausea. That person might not want to stop drinking entirely for the rest of his or her life, but could benefit by reducing the drinking, she said.
But 55% of the time, varenicline produces a reduction of one level of risk, which is associated with clinically meaningful results. That will sound much more appealing to a prospective patient, she said.
“From a clinical perspective, these WHO outcomes have some advantages,” she said. “I think you’re going to, one, encourage more people to accept treatment, and … be more optimistic about the outcomes.”
Dr. Anton reported consulting and/or funding from Alkermes, Allergan, Indivior, Insys Life Epigenetics, and Laboratori Farmaceutico CT. Dr. O’Malley reported consulting and/or funding from Alkermes, Amygdala, Indivior, Mistubishi Tanabe, Opiant, and other sources. Dr. Falk reported no disclosures.
REPORTING FROM AAAP 2018