User login
A program using “telehospitalists” to hasten and improve patient care won the top prize in the Innovations category of the RIV competition on Monday night at HM19. In the Research category, a study on workload to improve overnight cross-coverage care took the top prize.
Jeetinder Kaur Gujral, MD, a family medicine and palliative care physician at Northwell Health in Bay Shore, N.Y., said that the telehospitalist program at her institution uses a telehealth hub that is on call to consult with patients when the on-site hospitalist is unable to evaluate a patient in the emergency department within 30 minutes.
Dr. Gujral’s winning study – presented on Monday night and evaluated based on its novelty and the quality of the presentation and the poster – examined results at one of Northwell’s tertiary centers from January to October of 2018, where a telehospitalist works from 12 p.m. to 10 p.m.
Researchers found there was no significant difference in the severity of illness between the patients seen by the on-site hospitalist and the telehospitalist – if anything, the patients consulted by the telehospitalist were a bit sicker, Dr. Gujral said. But there was significantly less variation in the time it took for a telehospitalist to consult with a patient than the on-site physician.
“We are more predictable, because it’s a press of a button, and we are there,” Dr. Gujral said. “And the orders go in faster. I don’t have to leave to go down to the ED to see the patient. I’m seeing the patient right there.”
Kelly Sponsler, MD, assistant professor at Vanderbilt University Medical Center in Nashville, Tenn., who led the Innovations judging, said the project seems to be a brand-new idea: taking a concept built to cover long distances at rural centers and using it within a center’s own program to improve care.
“We really felt like this was something we had not seen before,” Dr. Sponsler said. “There was a clear problem that the team had identified, and it’s a common problem that I think can be scalable, or that other groups probably encounter.”
In the cross-coverage study that won in the Research category, an index developed by NASA to quantify perceived workload was used to assess the factors that boost workload during night shifts, said Ruth Bates, MD, an assistant professor at Mayo Clinic in Rochester, Minn.
The key finding was that it wasn’t the number of patients that boosts workload during these hours, but the number of pages, action items, and rapid-response team and ICU activations. The number of unnecessary pages that overnight hospitalists receive is the prime target as a way to reduce the workload.
The idea is to reduce “low-value communication,” Dr. Bates said. An example is a page about a lab value that is a “tiny bit off.”
“That’s just one example of really low-value communication that has interrupted somebody’s work flow and is not really increasing the quality of patient care.”
Trainee winners were Cameron Locke, MD, a resident physician at the University of California, San Francisco, for a study on a multidisciplinary approach to reduce endoscopy delays, which won in the Innovations category. That study was presented by Molly Kantor, MD, assistant clinical professor at UCSF.
The Research category trainee winner was Monisha Bhatia, MD, JD, MPH, of Jackson Memorial Hospital in Miami for her work on using phenotypic data from electronic health records to predict discharge destination.
On Tuesday afternoon, Erin Frost, MD, a resident in internal medicine and pediatrics at Duke University, Durham, N.C., won the top prize in the Clinical Vignettes category, for her presentation of a case of a woman with acute digital ischemia after an injection of sublingual buprenorphine and naloxone.
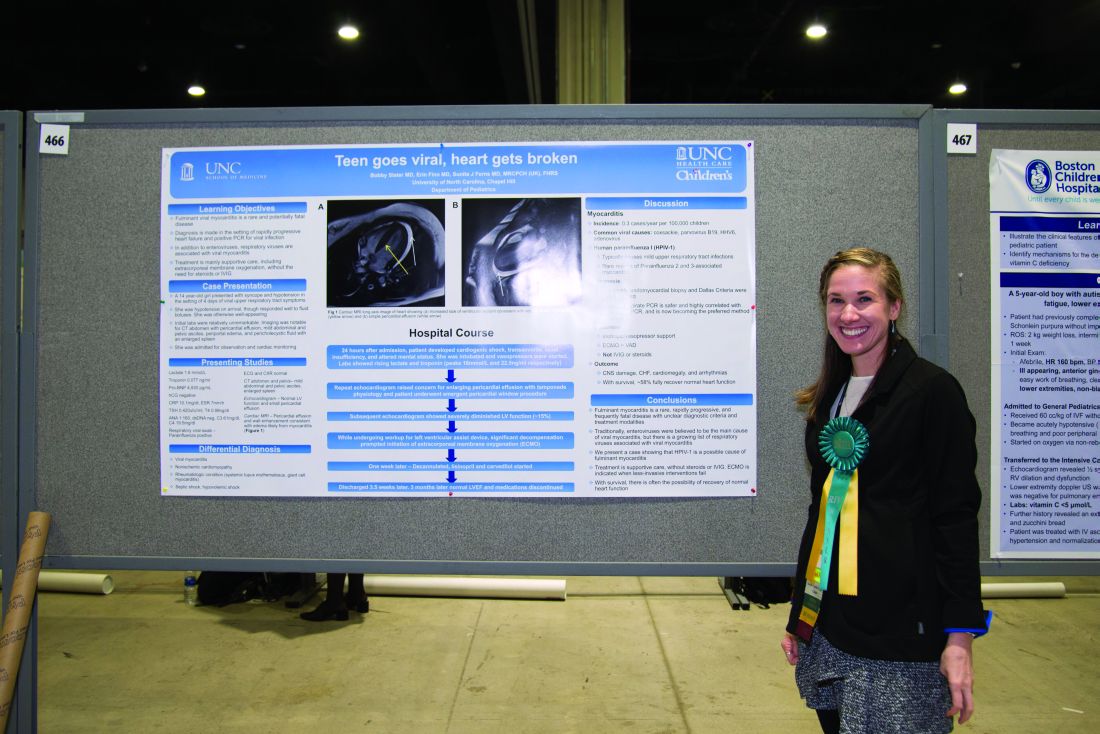
The trainee winner in Clinical Vignettes was a case of C. difficile infection of a total hip arthroplasty, presented by Benjamin Claxton, MPH, a medical student at Penn State University, Hershey. The category’s pediatrics winner was Erin Finn, MD, a resident at the University of North Carolina, Chapel Hill, for her presentation of a case of myocarditis in a 14-year-old.
The oral presentation winner for the Innovations category was Nainesh Shah, MD, of UT Southwestern Medical Center, Dallas, for his abstract presentation "Alert: Structured Radiology Reports are Here." For the Research category, the oral presentation winner was David Meltzer, MD, PhD, section chief of hospital medicine at University of Chicago Medicine, for his abstract presentation "Effects of Comprehensive Care Physicians on Patient Experience, Outcomes and Hospitalization."
A program using “telehospitalists” to hasten and improve patient care won the top prize in the Innovations category of the RIV competition on Monday night at HM19. In the Research category, a study on workload to improve overnight cross-coverage care took the top prize.
Jeetinder Kaur Gujral, MD, a family medicine and palliative care physician at Northwell Health in Bay Shore, N.Y., said that the telehospitalist program at her institution uses a telehealth hub that is on call to consult with patients when the on-site hospitalist is unable to evaluate a patient in the emergency department within 30 minutes.
Dr. Gujral’s winning study – presented on Monday night and evaluated based on its novelty and the quality of the presentation and the poster – examined results at one of Northwell’s tertiary centers from January to October of 2018, where a telehospitalist works from 12 p.m. to 10 p.m.
Researchers found there was no significant difference in the severity of illness between the patients seen by the on-site hospitalist and the telehospitalist – if anything, the patients consulted by the telehospitalist were a bit sicker, Dr. Gujral said. But there was significantly less variation in the time it took for a telehospitalist to consult with a patient than the on-site physician.
“We are more predictable, because it’s a press of a button, and we are there,” Dr. Gujral said. “And the orders go in faster. I don’t have to leave to go down to the ED to see the patient. I’m seeing the patient right there.”
Kelly Sponsler, MD, assistant professor at Vanderbilt University Medical Center in Nashville, Tenn., who led the Innovations judging, said the project seems to be a brand-new idea: taking a concept built to cover long distances at rural centers and using it within a center’s own program to improve care.
“We really felt like this was something we had not seen before,” Dr. Sponsler said. “There was a clear problem that the team had identified, and it’s a common problem that I think can be scalable, or that other groups probably encounter.”
In the cross-coverage study that won in the Research category, an index developed by NASA to quantify perceived workload was used to assess the factors that boost workload during night shifts, said Ruth Bates, MD, an assistant professor at Mayo Clinic in Rochester, Minn.
The key finding was that it wasn’t the number of patients that boosts workload during these hours, but the number of pages, action items, and rapid-response team and ICU activations. The number of unnecessary pages that overnight hospitalists receive is the prime target as a way to reduce the workload.
The idea is to reduce “low-value communication,” Dr. Bates said. An example is a page about a lab value that is a “tiny bit off.”
“That’s just one example of really low-value communication that has interrupted somebody’s work flow and is not really increasing the quality of patient care.”
Trainee winners were Cameron Locke, MD, a resident physician at the University of California, San Francisco, for a study on a multidisciplinary approach to reduce endoscopy delays, which won in the Innovations category. That study was presented by Molly Kantor, MD, assistant clinical professor at UCSF.
The Research category trainee winner was Monisha Bhatia, MD, JD, MPH, of Jackson Memorial Hospital in Miami for her work on using phenotypic data from electronic health records to predict discharge destination.
On Tuesday afternoon, Erin Frost, MD, a resident in internal medicine and pediatrics at Duke University, Durham, N.C., won the top prize in the Clinical Vignettes category, for her presentation of a case of a woman with acute digital ischemia after an injection of sublingual buprenorphine and naloxone.
The trainee winner in Clinical Vignettes was a case of C. difficile infection of a total hip arthroplasty, presented by Benjamin Claxton, MPH, a medical student at Penn State University, Hershey. The category’s pediatrics winner was Erin Finn, MD, a resident at the University of North Carolina, Chapel Hill, for her presentation of a case of myocarditis in a 14-year-old.
The oral presentation winner for the Innovations category was Nainesh Shah, MD, of UT Southwestern Medical Center, Dallas, for his abstract presentation "Alert: Structured Radiology Reports are Here." For the Research category, the oral presentation winner was David Meltzer, MD, PhD, section chief of hospital medicine at University of Chicago Medicine, for his abstract presentation "Effects of Comprehensive Care Physicians on Patient Experience, Outcomes and Hospitalization."
A program using “telehospitalists” to hasten and improve patient care won the top prize in the Innovations category of the RIV competition on Monday night at HM19. In the Research category, a study on workload to improve overnight cross-coverage care took the top prize.
Jeetinder Kaur Gujral, MD, a family medicine and palliative care physician at Northwell Health in Bay Shore, N.Y., said that the telehospitalist program at her institution uses a telehealth hub that is on call to consult with patients when the on-site hospitalist is unable to evaluate a patient in the emergency department within 30 minutes.
Dr. Gujral’s winning study – presented on Monday night and evaluated based on its novelty and the quality of the presentation and the poster – examined results at one of Northwell’s tertiary centers from January to October of 2018, where a telehospitalist works from 12 p.m. to 10 p.m.
Researchers found there was no significant difference in the severity of illness between the patients seen by the on-site hospitalist and the telehospitalist – if anything, the patients consulted by the telehospitalist were a bit sicker, Dr. Gujral said. But there was significantly less variation in the time it took for a telehospitalist to consult with a patient than the on-site physician.
“We are more predictable, because it’s a press of a button, and we are there,” Dr. Gujral said. “And the orders go in faster. I don’t have to leave to go down to the ED to see the patient. I’m seeing the patient right there.”
Kelly Sponsler, MD, assistant professor at Vanderbilt University Medical Center in Nashville, Tenn., who led the Innovations judging, said the project seems to be a brand-new idea: taking a concept built to cover long distances at rural centers and using it within a center’s own program to improve care.
“We really felt like this was something we had not seen before,” Dr. Sponsler said. “There was a clear problem that the team had identified, and it’s a common problem that I think can be scalable, or that other groups probably encounter.”
In the cross-coverage study that won in the Research category, an index developed by NASA to quantify perceived workload was used to assess the factors that boost workload during night shifts, said Ruth Bates, MD, an assistant professor at Mayo Clinic in Rochester, Minn.
The key finding was that it wasn’t the number of patients that boosts workload during these hours, but the number of pages, action items, and rapid-response team and ICU activations. The number of unnecessary pages that overnight hospitalists receive is the prime target as a way to reduce the workload.
The idea is to reduce “low-value communication,” Dr. Bates said. An example is a page about a lab value that is a “tiny bit off.”
“That’s just one example of really low-value communication that has interrupted somebody’s work flow and is not really increasing the quality of patient care.”
Trainee winners were Cameron Locke, MD, a resident physician at the University of California, San Francisco, for a study on a multidisciplinary approach to reduce endoscopy delays, which won in the Innovations category. That study was presented by Molly Kantor, MD, assistant clinical professor at UCSF.
The Research category trainee winner was Monisha Bhatia, MD, JD, MPH, of Jackson Memorial Hospital in Miami for her work on using phenotypic data from electronic health records to predict discharge destination.
On Tuesday afternoon, Erin Frost, MD, a resident in internal medicine and pediatrics at Duke University, Durham, N.C., won the top prize in the Clinical Vignettes category, for her presentation of a case of a woman with acute digital ischemia after an injection of sublingual buprenorphine and naloxone.
The trainee winner in Clinical Vignettes was a case of C. difficile infection of a total hip arthroplasty, presented by Benjamin Claxton, MPH, a medical student at Penn State University, Hershey. The category’s pediatrics winner was Erin Finn, MD, a resident at the University of North Carolina, Chapel Hill, for her presentation of a case of myocarditis in a 14-year-old.
The oral presentation winner for the Innovations category was Nainesh Shah, MD, of UT Southwestern Medical Center, Dallas, for his abstract presentation "Alert: Structured Radiology Reports are Here." For the Research category, the oral presentation winner was David Meltzer, MD, PhD, section chief of hospital medicine at University of Chicago Medicine, for his abstract presentation "Effects of Comprehensive Care Physicians on Patient Experience, Outcomes and Hospitalization."