User login
Improving Patient Safety and Quality of Care
Patient safety and improved quality of care have become priority issues in the American healthcare system. The potential for medical errors was highlighted in 1999 when the Quality of Health Care in America Committee of the Institute of Medicine (IOM) published its first report, To Err is Human: Building a Safer Health System. The committee estimated that between 44,000 and 98,000 people die annually from inpatient medical errors. The eighth leading cause of death in this country, preventable medical errors, cost the U.S. approximately $17 billion annually in direct and indirect costs (IOM). These alarming statistics in the IOM report ignited the patient safety movement (I).
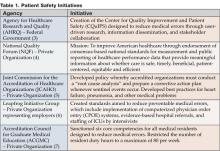
The IOM report made a series of recommendations that included the creation of a center for patient safety, the development of a national public reporting system, the establishment of oversight agencies, and the incorporation of safety principles into monitoring systems. Public and private agencies have responded with a series of initiatives that address these recommendations (See Table 1).
One healthcare expert describes three reasons as to why the potential for medical errors has increased. First, technology has created a sophisticated array of test, x-rays, laboratory procedures, and diagnostic tools. Second, pharmaceutical research has introduced thousands of new medications to the marketplace. Finally, specialization has led to experts, both physician and non-physician, in a wide range of body systems, diseases, settings, procedures, and therapies. Hospital medicine represents a new type of medical specialty that has the potential to address this increased complexity and sophistication and to improve patient care in the hospital inpatient environment (2).
Hospitalists as Team Coordinators
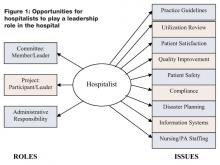
To achieve maximum positive outcomes in the complex inpatient environment, a qualified coordinator must educate others and facilitate activity revolving around patient care. Hospitalists as inpatient experts possess the necessary qualifications to integrate hospital systems and maximize efforts to enhance patient safety by monitoring medication distribution, chairing pharmaceuticals and therapeutics (P&T) committees, overseeing computerized physician order entry (CPOE), directing quality/performance improvement projects, and collaborating with discharge planning and case management.
Lakshmi Halasyamani, MD, is vice chair of the department of Internal Medicine at St. Joseph Mercy Hospital in Michigan and chairperson of the Society of Hospital Medicine (SHM) Hospital Quality and Patient Safety Committee. She says, Hospitalists have a ‘lens of understanding the systems under which they care for patients.’ They take care of patients in the hospital every single day so they can examine the processes with which they work. Hospitalists have an ideal perspective from which to reform ineffective systems.”
In spite of all the guidelines established by federal agencies and expert groups, Dr. Halasyamani points out that implementation barriers exist that prevent well-intentioned protocols and best practices from being carried out. Part of the challenge is the performance of a critical piece of the infrastructure—the multidisciplinary team. The very nature of healthcare demands an inherent need to coordinate and communicate. “Treating the patient is not the responsibility of one single individual,” says Halasyamani. “This is a team effort. The hospitalist recognizes that he is part of that team.” By elevating the ideals of teamwork, hospitalists can deliver to the patients the essential care that patients need, both while in the hospital and after they are discharged. In managing hospital inpatients, physicians must cope with high intensity of illness, pressures to reduce length of stay (LOS), and the coordination of handoffs among many specialists. According to Halasyamani, this can be a “recipe for disaster.”
Halasyamani acknowledges the vital role of protocols in reducing medical errors and improving quality of care. The training, education, and experience a hospitalist has acquired enables him to optimize communication and implement protocols, thus facilitating the practice of delivering safe and consistent care to all patients. In fact, with this smaller core group of inpatient physicians, the development and implementation of protocols can potentially be more effective because it targets a smaller group of physicians than the traditional inpatient model (8).
Kaveh C. Shojania, MD, is assistant professor of medicine at the University of Ottawa and co-author of Internal Bleeding: The Terrifying Truth Behind America's Epidemic Medical Mistakes. He points out that the current inpatient medical landscape involves a significant number of clinicians who practice at the hospital but not all their activity is centered there. “From a clinical perspective, no one has ownership,” he says. “On the other hand, hospitalists are based in a single hospital and have a vested interest in that particular hospital.” Typically generalists, hospitalists tend to interact with all specialists and therefore have a good sense of all interests.
Medical errors occur most often during transition times, from the ICU to the floor or from inpatient to outpatient status. There is the potential for a loss of clinical information during these transfers. According to Shojania, a significant portion of the hospitalist’s time is spent managing these transitions and overseeing patients as they are relocated from floor to floor and discharge to home, rehabilitation facility, or nursing home. He notes that the regulatory agencies have begun to acknowledge the importance of hospitalists. “The JCAHO (Joint Commission for the Accreditation of Healthcare Organizations) recognizes hospitalists as a resource because they are always in the hospital and have a vested interest,” he says (9).
Stakeholder Analysis
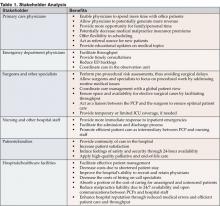
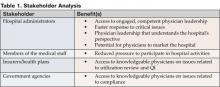
Patients stand to gain the most benefit from hospitalists insofar as safety and quality of care is concerned. Through the efforts and oversight of hospitalists, patients may experience reduced medical errors and lower mortality rates. For primary care physicians and hospitals, this lower rate of medical error means fewer medical malpractice cases, the potential for lower insurance premiums and, as a result, enhanced reputations. When hospitals are run more efficiently and provide a greater sense of trust and efficient management practices, society in general becomes the benefactor.
Clinical Trials
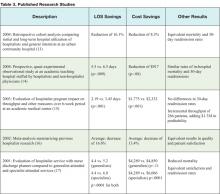
To date, few research studies measuring the impact of hospitalists on patient safety and quality of care have been conducted. Quality of care has been assessed largely through the surrogate markers of mortality and readmission rates. One study showed decreased in-hospital and 1-year mortality rates for hospitalist patients (10), and another indicated a decrease in 30-day readmission rates (11).
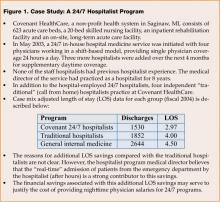
In addition, data from individual programs demonstrate positive findings. For example, Stacy Goldsholl, MD, medical director of the Covenant Healthcare hospital medicine program in Michigan, reports a 17% decrease in the expected mortality rate in the first year of the hospital medicine program. The information was drawn from the Michigan Hospital Association (MHA) databank and matched for severity and diagnosis (See Table 2). “This was significant when compared to the internal medicine comparison group with similar case mix index (CMI),” says Goldsholl. “In the first half of our second year, we have demonstrated a 46% decrease in expected mortality, while internal medicine had a 4% increase” (12).
Additionally, Goldsholl reports that Covenant initiated a Code Blue and emergency consult service to improve patient outcome and experienced a marked increase in efficiency. Table 3 represents elementary data collected during the first 6 months pre- and post-initiation of the hospital medicine program at Covenant (12).
Conclusion
Patient safety and quality of care in the hospital require a team of dedicated people to effect change. Orchestrating the team effectively is the responsibility of an attending physician. With the numerous “handoffs” that take place during hospitalization, the potential for medical errors increases exponentially. Federal mandates requiring the conversion to electronic medical records, which includes basic health information as well as critical data regarding medications, procedures, and surgeries, further complicates efficient and safe patient management. According to Robert Wachter, “Those doctors with the best outcomes were those who tended to treat similar patients with similar problems using similar techniques.” By definition, the hospitalist is a “physician who focuses his practice on the care, coordination, and safety of hospitalized patients.” Who better to stand at the center of the issue of reduced medical errors, improved patient care, and enhanced quality of care than hospitalists (13)?
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
References
- To Err is Human: Building a Safer Health System, Institute of Medicine, November 1999.
- Wachter R. The end of the beginning: patient safety five years after ‘To Err Is Human.’ Health Affairs. November 30, 2004.
- Mission Statement: Center for Quality Improvement and Patient Safety. February 2004. Agency for Healthcare Research and Quality, Rockville, MD. www.ahrq.gov/about/cquips/cquipsmiss.htm.
- Safe Practices for Better Healthcare: a Consensus. The National Quality Forum, 2003.
- Joint Commission for Accreditation of Healthcare Organizations (JCAHO), www.jcaho.org.
- Leapfrog Group, www.leapfroggroup.org.
- Accreditation Council for Graduate Medical Education (ACGME), www.acgme.org.
- Halasyamani L. Telephone interview. February 7, 2005.
- Shojania KG. Assistant professor of medicine, University of Ottawa. Telephone interview. January 31, 2005.
- Auerbach AD, Wachter RM, Katz P. et al. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137:859-65.
- Kulaga ME, Charney P, O’Mahoney SP, et al. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19:293-301.
- Goldsholl S. Medical director. Covenant Healthcare hospital medicine program, Saginaw, Michigan, email interview. January 31, 2005.
- Wachter R, Shojania K. Internal bleeding: the truth behind America’s terrifying epidemic of medical mistakes. Rugged Land, LLC, 2004.
Patient safety and improved quality of care have become priority issues in the American healthcare system. The potential for medical errors was highlighted in 1999 when the Quality of Health Care in America Committee of the Institute of Medicine (IOM) published its first report, To Err is Human: Building a Safer Health System. The committee estimated that between 44,000 and 98,000 people die annually from inpatient medical errors. The eighth leading cause of death in this country, preventable medical errors, cost the U.S. approximately $17 billion annually in direct and indirect costs (IOM). These alarming statistics in the IOM report ignited the patient safety movement (I).
The IOM report made a series of recommendations that included the creation of a center for patient safety, the development of a national public reporting system, the establishment of oversight agencies, and the incorporation of safety principles into monitoring systems. Public and private agencies have responded with a series of initiatives that address these recommendations (See Table 1).
One healthcare expert describes three reasons as to why the potential for medical errors has increased. First, technology has created a sophisticated array of test, x-rays, laboratory procedures, and diagnostic tools. Second, pharmaceutical research has introduced thousands of new medications to the marketplace. Finally, specialization has led to experts, both physician and non-physician, in a wide range of body systems, diseases, settings, procedures, and therapies. Hospital medicine represents a new type of medical specialty that has the potential to address this increased complexity and sophistication and to improve patient care in the hospital inpatient environment (2).
Hospitalists as Team Coordinators
To achieve maximum positive outcomes in the complex inpatient environment, a qualified coordinator must educate others and facilitate activity revolving around patient care. Hospitalists as inpatient experts possess the necessary qualifications to integrate hospital systems and maximize efforts to enhance patient safety by monitoring medication distribution, chairing pharmaceuticals and therapeutics (P&T) committees, overseeing computerized physician order entry (CPOE), directing quality/performance improvement projects, and collaborating with discharge planning and case management.
Lakshmi Halasyamani, MD, is vice chair of the department of Internal Medicine at St. Joseph Mercy Hospital in Michigan and chairperson of the Society of Hospital Medicine (SHM) Hospital Quality and Patient Safety Committee. She says, Hospitalists have a ‘lens of understanding the systems under which they care for patients.’ They take care of patients in the hospital every single day so they can examine the processes with which they work. Hospitalists have an ideal perspective from which to reform ineffective systems.”
In spite of all the guidelines established by federal agencies and expert groups, Dr. Halasyamani points out that implementation barriers exist that prevent well-intentioned protocols and best practices from being carried out. Part of the challenge is the performance of a critical piece of the infrastructure—the multidisciplinary team. The very nature of healthcare demands an inherent need to coordinate and communicate. “Treating the patient is not the responsibility of one single individual,” says Halasyamani. “This is a team effort. The hospitalist recognizes that he is part of that team.” By elevating the ideals of teamwork, hospitalists can deliver to the patients the essential care that patients need, both while in the hospital and after they are discharged. In managing hospital inpatients, physicians must cope with high intensity of illness, pressures to reduce length of stay (LOS), and the coordination of handoffs among many specialists. According to Halasyamani, this can be a “recipe for disaster.”
Halasyamani acknowledges the vital role of protocols in reducing medical errors and improving quality of care. The training, education, and experience a hospitalist has acquired enables him to optimize communication and implement protocols, thus facilitating the practice of delivering safe and consistent care to all patients. In fact, with this smaller core group of inpatient physicians, the development and implementation of protocols can potentially be more effective because it targets a smaller group of physicians than the traditional inpatient model (8).
Kaveh C. Shojania, MD, is assistant professor of medicine at the University of Ottawa and co-author of Internal Bleeding: The Terrifying Truth Behind America's Epidemic Medical Mistakes. He points out that the current inpatient medical landscape involves a significant number of clinicians who practice at the hospital but not all their activity is centered there. “From a clinical perspective, no one has ownership,” he says. “On the other hand, hospitalists are based in a single hospital and have a vested interest in that particular hospital.” Typically generalists, hospitalists tend to interact with all specialists and therefore have a good sense of all interests.
Medical errors occur most often during transition times, from the ICU to the floor or from inpatient to outpatient status. There is the potential for a loss of clinical information during these transfers. According to Shojania, a significant portion of the hospitalist’s time is spent managing these transitions and overseeing patients as they are relocated from floor to floor and discharge to home, rehabilitation facility, or nursing home. He notes that the regulatory agencies have begun to acknowledge the importance of hospitalists. “The JCAHO (Joint Commission for the Accreditation of Healthcare Organizations) recognizes hospitalists as a resource because they are always in the hospital and have a vested interest,” he says (9).
Stakeholder Analysis
Patients stand to gain the most benefit from hospitalists insofar as safety and quality of care is concerned. Through the efforts and oversight of hospitalists, patients may experience reduced medical errors and lower mortality rates. For primary care physicians and hospitals, this lower rate of medical error means fewer medical malpractice cases, the potential for lower insurance premiums and, as a result, enhanced reputations. When hospitals are run more efficiently and provide a greater sense of trust and efficient management practices, society in general becomes the benefactor.
Clinical Trials
To date, few research studies measuring the impact of hospitalists on patient safety and quality of care have been conducted. Quality of care has been assessed largely through the surrogate markers of mortality and readmission rates. One study showed decreased in-hospital and 1-year mortality rates for hospitalist patients (10), and another indicated a decrease in 30-day readmission rates (11).
In addition, data from individual programs demonstrate positive findings. For example, Stacy Goldsholl, MD, medical director of the Covenant Healthcare hospital medicine program in Michigan, reports a 17% decrease in the expected mortality rate in the first year of the hospital medicine program. The information was drawn from the Michigan Hospital Association (MHA) databank and matched for severity and diagnosis (See Table 2). “This was significant when compared to the internal medicine comparison group with similar case mix index (CMI),” says Goldsholl. “In the first half of our second year, we have demonstrated a 46% decrease in expected mortality, while internal medicine had a 4% increase” (12).
Additionally, Goldsholl reports that Covenant initiated a Code Blue and emergency consult service to improve patient outcome and experienced a marked increase in efficiency. Table 3 represents elementary data collected during the first 6 months pre- and post-initiation of the hospital medicine program at Covenant (12).
Conclusion
Patient safety and quality of care in the hospital require a team of dedicated people to effect change. Orchestrating the team effectively is the responsibility of an attending physician. With the numerous “handoffs” that take place during hospitalization, the potential for medical errors increases exponentially. Federal mandates requiring the conversion to electronic medical records, which includes basic health information as well as critical data regarding medications, procedures, and surgeries, further complicates efficient and safe patient management. According to Robert Wachter, “Those doctors with the best outcomes were those who tended to treat similar patients with similar problems using similar techniques.” By definition, the hospitalist is a “physician who focuses his practice on the care, coordination, and safety of hospitalized patients.” Who better to stand at the center of the issue of reduced medical errors, improved patient care, and enhanced quality of care than hospitalists (13)?
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
References
- To Err is Human: Building a Safer Health System, Institute of Medicine, November 1999.
- Wachter R. The end of the beginning: patient safety five years after ‘To Err Is Human.’ Health Affairs. November 30, 2004.
- Mission Statement: Center for Quality Improvement and Patient Safety. February 2004. Agency for Healthcare Research and Quality, Rockville, MD. www.ahrq.gov/about/cquips/cquipsmiss.htm.
- Safe Practices for Better Healthcare: a Consensus. The National Quality Forum, 2003.
- Joint Commission for Accreditation of Healthcare Organizations (JCAHO), www.jcaho.org.
- Leapfrog Group, www.leapfroggroup.org.
- Accreditation Council for Graduate Medical Education (ACGME), www.acgme.org.
- Halasyamani L. Telephone interview. February 7, 2005.
- Shojania KG. Assistant professor of medicine, University of Ottawa. Telephone interview. January 31, 2005.
- Auerbach AD, Wachter RM, Katz P. et al. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137:859-65.
- Kulaga ME, Charney P, O’Mahoney SP, et al. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19:293-301.
- Goldsholl S. Medical director. Covenant Healthcare hospital medicine program, Saginaw, Michigan, email interview. January 31, 2005.
- Wachter R, Shojania K. Internal bleeding: the truth behind America’s terrifying epidemic of medical mistakes. Rugged Land, LLC, 2004.
Patient safety and improved quality of care have become priority issues in the American healthcare system. The potential for medical errors was highlighted in 1999 when the Quality of Health Care in America Committee of the Institute of Medicine (IOM) published its first report, To Err is Human: Building a Safer Health System. The committee estimated that between 44,000 and 98,000 people die annually from inpatient medical errors. The eighth leading cause of death in this country, preventable medical errors, cost the U.S. approximately $17 billion annually in direct and indirect costs (IOM). These alarming statistics in the IOM report ignited the patient safety movement (I).
The IOM report made a series of recommendations that included the creation of a center for patient safety, the development of a national public reporting system, the establishment of oversight agencies, and the incorporation of safety principles into monitoring systems. Public and private agencies have responded with a series of initiatives that address these recommendations (See Table 1).
One healthcare expert describes three reasons as to why the potential for medical errors has increased. First, technology has created a sophisticated array of test, x-rays, laboratory procedures, and diagnostic tools. Second, pharmaceutical research has introduced thousands of new medications to the marketplace. Finally, specialization has led to experts, both physician and non-physician, in a wide range of body systems, diseases, settings, procedures, and therapies. Hospital medicine represents a new type of medical specialty that has the potential to address this increased complexity and sophistication and to improve patient care in the hospital inpatient environment (2).
Hospitalists as Team Coordinators
To achieve maximum positive outcomes in the complex inpatient environment, a qualified coordinator must educate others and facilitate activity revolving around patient care. Hospitalists as inpatient experts possess the necessary qualifications to integrate hospital systems and maximize efforts to enhance patient safety by monitoring medication distribution, chairing pharmaceuticals and therapeutics (P&T) committees, overseeing computerized physician order entry (CPOE), directing quality/performance improvement projects, and collaborating with discharge planning and case management.
Lakshmi Halasyamani, MD, is vice chair of the department of Internal Medicine at St. Joseph Mercy Hospital in Michigan and chairperson of the Society of Hospital Medicine (SHM) Hospital Quality and Patient Safety Committee. She says, Hospitalists have a ‘lens of understanding the systems under which they care for patients.’ They take care of patients in the hospital every single day so they can examine the processes with which they work. Hospitalists have an ideal perspective from which to reform ineffective systems.”
In spite of all the guidelines established by federal agencies and expert groups, Dr. Halasyamani points out that implementation barriers exist that prevent well-intentioned protocols and best practices from being carried out. Part of the challenge is the performance of a critical piece of the infrastructure—the multidisciplinary team. The very nature of healthcare demands an inherent need to coordinate and communicate. “Treating the patient is not the responsibility of one single individual,” says Halasyamani. “This is a team effort. The hospitalist recognizes that he is part of that team.” By elevating the ideals of teamwork, hospitalists can deliver to the patients the essential care that patients need, both while in the hospital and after they are discharged. In managing hospital inpatients, physicians must cope with high intensity of illness, pressures to reduce length of stay (LOS), and the coordination of handoffs among many specialists. According to Halasyamani, this can be a “recipe for disaster.”
Halasyamani acknowledges the vital role of protocols in reducing medical errors and improving quality of care. The training, education, and experience a hospitalist has acquired enables him to optimize communication and implement protocols, thus facilitating the practice of delivering safe and consistent care to all patients. In fact, with this smaller core group of inpatient physicians, the development and implementation of protocols can potentially be more effective because it targets a smaller group of physicians than the traditional inpatient model (8).
Kaveh C. Shojania, MD, is assistant professor of medicine at the University of Ottawa and co-author of Internal Bleeding: The Terrifying Truth Behind America's Epidemic Medical Mistakes. He points out that the current inpatient medical landscape involves a significant number of clinicians who practice at the hospital but not all their activity is centered there. “From a clinical perspective, no one has ownership,” he says. “On the other hand, hospitalists are based in a single hospital and have a vested interest in that particular hospital.” Typically generalists, hospitalists tend to interact with all specialists and therefore have a good sense of all interests.
Medical errors occur most often during transition times, from the ICU to the floor or from inpatient to outpatient status. There is the potential for a loss of clinical information during these transfers. According to Shojania, a significant portion of the hospitalist’s time is spent managing these transitions and overseeing patients as they are relocated from floor to floor and discharge to home, rehabilitation facility, or nursing home. He notes that the regulatory agencies have begun to acknowledge the importance of hospitalists. “The JCAHO (Joint Commission for the Accreditation of Healthcare Organizations) recognizes hospitalists as a resource because they are always in the hospital and have a vested interest,” he says (9).
Stakeholder Analysis
Patients stand to gain the most benefit from hospitalists insofar as safety and quality of care is concerned. Through the efforts and oversight of hospitalists, patients may experience reduced medical errors and lower mortality rates. For primary care physicians and hospitals, this lower rate of medical error means fewer medical malpractice cases, the potential for lower insurance premiums and, as a result, enhanced reputations. When hospitals are run more efficiently and provide a greater sense of trust and efficient management practices, society in general becomes the benefactor.
Clinical Trials
To date, few research studies measuring the impact of hospitalists on patient safety and quality of care have been conducted. Quality of care has been assessed largely through the surrogate markers of mortality and readmission rates. One study showed decreased in-hospital and 1-year mortality rates for hospitalist patients (10), and another indicated a decrease in 30-day readmission rates (11).
In addition, data from individual programs demonstrate positive findings. For example, Stacy Goldsholl, MD, medical director of the Covenant Healthcare hospital medicine program in Michigan, reports a 17% decrease in the expected mortality rate in the first year of the hospital medicine program. The information was drawn from the Michigan Hospital Association (MHA) databank and matched for severity and diagnosis (See Table 2). “This was significant when compared to the internal medicine comparison group with similar case mix index (CMI),” says Goldsholl. “In the first half of our second year, we have demonstrated a 46% decrease in expected mortality, while internal medicine had a 4% increase” (12).
Additionally, Goldsholl reports that Covenant initiated a Code Blue and emergency consult service to improve patient outcome and experienced a marked increase in efficiency. Table 3 represents elementary data collected during the first 6 months pre- and post-initiation of the hospital medicine program at Covenant (12).
Conclusion
Patient safety and quality of care in the hospital require a team of dedicated people to effect change. Orchestrating the team effectively is the responsibility of an attending physician. With the numerous “handoffs” that take place during hospitalization, the potential for medical errors increases exponentially. Federal mandates requiring the conversion to electronic medical records, which includes basic health information as well as critical data regarding medications, procedures, and surgeries, further complicates efficient and safe patient management. According to Robert Wachter, “Those doctors with the best outcomes were those who tended to treat similar patients with similar problems using similar techniques.” By definition, the hospitalist is a “physician who focuses his practice on the care, coordination, and safety of hospitalized patients.” Who better to stand at the center of the issue of reduced medical errors, improved patient care, and enhanced quality of care than hospitalists (13)?
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
References
- To Err is Human: Building a Safer Health System, Institute of Medicine, November 1999.
- Wachter R. The end of the beginning: patient safety five years after ‘To Err Is Human.’ Health Affairs. November 30, 2004.
- Mission Statement: Center for Quality Improvement and Patient Safety. February 2004. Agency for Healthcare Research and Quality, Rockville, MD. www.ahrq.gov/about/cquips/cquipsmiss.htm.
- Safe Practices for Better Healthcare: a Consensus. The National Quality Forum, 2003.
- Joint Commission for Accreditation of Healthcare Organizations (JCAHO), www.jcaho.org.
- Leapfrog Group, www.leapfroggroup.org.
- Accreditation Council for Graduate Medical Education (ACGME), www.acgme.org.
- Halasyamani L. Telephone interview. February 7, 2005.
- Shojania KG. Assistant professor of medicine, University of Ottawa. Telephone interview. January 31, 2005.
- Auerbach AD, Wachter RM, Katz P. et al. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137:859-65.
- Kulaga ME, Charney P, O’Mahoney SP, et al. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19:293-301.
- Goldsholl S. Medical director. Covenant Healthcare hospital medicine program, Saginaw, Michigan, email interview. January 31, 2005.
- Wachter R, Shojania K. Internal bleeding: the truth behind America’s terrifying epidemic of medical mistakes. Rugged Land, LLC, 2004.
Maximizing Throughput and Improving Patient Flow
According to data from the American Hospital Association (1), in 1985, the United States had 5732 operational community hospitals; by 2002, the latest year for which figures are available, the number had decreased to 4927, a loss of approximately 14% (1). In that same timeframe, these hospitals lost approximately 18% of their beds, dropping from just over 1 million to 820,653 beds. This reduction in bed capacity has been accompanied by hospital cost-cutting efforts, staff downsizing, and elimination of services. Many explanations for these trends have been suggested, including changes in Medicare reimbursement and the growth of managed care organizations (MCOs).
However, as the current baby boom generation ages, rising inpatient demands are presenting hospitals with significant challenges. According to a 2001 report from Solucient (2), who maintains the nation’s largest health care database, the senior population—individuals age 65 and older—are projected to experience an 85% growth rate over the next two decades. Since this age group utilizes inpatient services 4.5 times more than younger populations, the number of admissions and beds to accommodate those cases will soar. By the year 2027, hospitals can anticipate a 46% rise in demand for acute inpatient beds as admissions escalate by approximately 13 million cases. Currently, the nation’s healthcare facilities admit 31 million cases; this number will jump to more than 44 million, representing a 41% growth from present admissions figures. For hospitals that maintain an 80% census rate, an additional 238,000 beds will be needed to meet demands (1).
Adding to this increase in demand and pressure on bed capacity, hospitals must address the requirements of the Emergency Medical Treatment and Active Labor Act (EMTALA) passed by the US Congress in 1986 as part of the Consolidated Omnibus Reconciliation Act (COBRA). The law’s initial intent was to ensure patient access to emergency medical care and to prevent the practice of patient dumping, in which uninsured patients were transferred, solely for financial reasons, from private to public hospitals without consideration of their medical condition or stability for the transfer (3). EMTALA mandates that hospitals rank the severity of patients. Thus, tertiary referral centers are required to admit the sickest patients first. This directive presents a significant challenge to many healthcare facilities. High census rates prohibit the admission of elective surgical cases, which, although profitable, are considered second tier. Routine medical cases or complicated emergency surgical cases have the potential to adversely affect the institution’s financial performance.
In addition to the challenge of increased bed demands and EMTALA, hospitals also cite an increasingly smaller number of on-site community physicians. Longstanding trends from inpatient to outpatient care have prompted many community physicians to concentrate their efforts on serving the needs of office-based patients, limiting their accessibility to hospital cases.
To address these pressures, hospitals must execute innovative strategies that deliver efficient throughput and enhance revenue, while still preserving high-quality services. Since 1996, hospital medicine programs have demonstrated a positive impact on the healthcare facility’s ability to increase overall productivity and profitability and still maintain high quality Patients today present to the doctor sicker than in the past and require more careful and frequent outpatient care. Since hospitalists operate solely on an inpatient basis, their availability to efficiently admit and manage hospitalized patients enables delivery of quality care that expedites appropriate treatment and shortens length of stay.
Two Roles of the Hospitalist
According to the Society of Hospital Medicine (SHM), “Hospitalists are physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to hospital medicine.” Coined by Drs. Robert Wachter and Lee Goldman in 1996 (4), the term implies an additional point of emphasis. Part of a new paradigm in clinical care, the hospitalist enhances the processes of care surrounding patients and adopts an attitude of accountability for that care. In practice, hospitalists play two key roles.
Primarily, the hospitalist is a practicing clinician — managing throughput on a case-by-case, patient-by-patient basis. In addition, a hospitalist performs a non-clinical role as an “inpatient expert,” taking the lead in creating system changes and communicating those changes to other hospital personnel as well as to community physicians. As an inpatient expert, hospitalists are often asked to lead organization-wide throughput initiatives to identify and implement strategies to facilitate patient flow and efficiency. As dedicated members of multi-disciplinary in-house teams, the hospitalist is in a prime position to foster change and improve systems.
Throughput as Continuum of Care
As suggested by Heffner (5), the process of admission, hospitalization, and discharge resembles a “bell-shaped curve.” To achieve effective throughput, hospitals must expedite patient care and also maintain careful oversight throughout a patient’s entire hospital stay. The hospitalist, as an integral part of a multidisciplinary team, coordinates care to promote a positive outcome and shorten length of stay. Drawing on strong leadership qualities, as well as on intimate knowledge of hospital procedures, layout design and infrastructure, and available community resources, the hospitalist plays a pivotal role in creating efficient throughput from admission to discharge.
Emergency Department
At the front end of the bell-shaped curve, the hospitalist may be engaged by emergency department (ED) physicians to assist in ensuring smooth patient flow and, more important, identifies the “intensity of service” needed. Through the use of clinical criteria, such as lnterQual, the hospitalist, together with the ED physician, may be asked to quantitatively rate the patient’s illness for degree of severity.
Timely patient evaluation helps prevent a backlog of ED cases and enables more patients to be seen. Immediate attention to and initiation of appropriate therapy guarantees a better outcome while minimizing the potential risk for complications, which could possibly lead to longer inpatient stays.
Inpatient Unit
Once a patient has been admitted to an inpatient unit, the hospitalist, together with a multidisciplinary team, facilitates care and determines the inpatient services that will optimize patient recovery through strong interdepartmental communications. Working together with admissions, medical records, nursing, laboratory and diagnostic services, information technology and other pertinent departments, the hospitalist maintains a pulse on all activity surrounding the patient and his care.
Judicious inpatient consultations and treatment decisions result in timely changes in therapy, potentially reducing the length of stay. The frequency with which the hospitalist sees the patient allows him to monitor any changes in condition and reduce possible decompensation, a practice known as vertical continuity (6). Such careful attention may reduce inpatient length of stay significantly. When aggressive management is mandated, the presence of the hospitalist enables initiation of effective therapy and results in quicker discharge and a reduction in potential readmission (7).
Surgery
The surgeon and hospitalist are ideally suited to work together in managing a surgical patient. The hospitalist focuses on the peri-operative management of medical issues and risk reduction, which allows the surgeon to concentrate more on surgical indications and the surgery itself. The hospitalist’s role in the management of a surgical patient enables vertical continuity when the surgeon may be occupied in the operating room with another patient as documented by Huddleston’s Hospitalist Orthopedic Team (HOT) approach (8).
Intensive Care Unit (ICU)
In many hospitals, particularly those that do not have intensivists, hospitalists are able to provide quality care to patients. Even in hospitals where intensivists manage ICU patients, hospitalists work together with the intensivist to ensure smoother transition into and out of the unit.
Discharge
Timing is a critical issue with regard to discharge. Since the hospitalist operates solely in-house and in collaboration with a multidisciplinary team, he is able to round early in the day to discharge patients by mid- or late-morning, freeing a bed for a new patient. In some cases, the hospitalist, in anticipation of early discharge, may begin pre-planning the day prior to discharge, which further expedites the process. Early discharge applies to the ICU, step-down areas and general inpatient care areas, as well as to full discharge from the healthcare facility. Moving a patient from one of these areas enables other patients to fill those empty beds thus optimizing throughput.
Having managed the patient throughout his hospital stay, the hospitalist — again working together with a multidisciplinary team —can facilitate arrangements to send the patient home or to a rehabilitation or skilled nursing facility or alternative housing situation upon discharge, as well as coordinating post-discharge care, whether it be arranging for a visiting nursing or social services or communicating with the primary care physician regarding follow-up appointments. If additional outpatient care is prescribed, the hospitalist will work with the discharge planning staff to contact various community agencies to arrange services best suited to the patient’s needs. Efficient discharge makes possible the admission of other, more critically ill patients, potentially enhancing the hospital’s revenue stream.
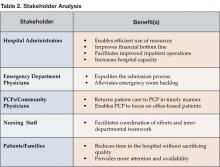
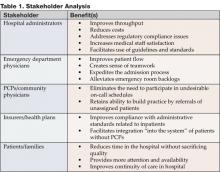
Stakeholder Analysis
Five specific stakeholders need to be examined to document the value-added by hospitalists. Anecdotal evidence, as well as documented studies, has demonstrated numerous returns—physical, social, psychological and financial—to stakeholders involved in the hospital process. With regard to throughput, the hospitalist provides benefits to each of the stakeholders listed in Table 1.
Study Results
A dozen studies have been conducted that document the impact of hospital medicine programs on cost and clinical outcomes. Of these trials, nine found a significant decrease in the average length of stay (15%) as well as reductions in cost (9). Two other studies, one from an academic medical center and the other from a community teaching hospital, demonstrate similar reductions during a 2-year follow-up period. At the Western Penn Hospital, a 54% reduction in readmissions was reported with a 12% decrease in hospital costs, while the average LOS was 17% shorter. Additionally, an unpublished study from the University of California, San Francisco Medical Center revealed a consistent 10-15% decline in cost and length of stay between hospitalists and non-hospitalist teaching faculty. More important, those differences remained stable through 6 years of follow-up. In general, hospitals with hospitalist programs realized a 5-39% decrease in costs and a shortened average LOS of 7-25% (6).
According to Robert M. Wachter, author of the 2002 study, “If the average U.S. hospitalist cares for 600 inpatients each year and generates a 10% savings over the average medical inpatient cost of $8,000, the nation’s 4500 hospitalists save approximately $2.2 billion per year while potentially improving quality” (6).
In a study conducted by Douglas Gregory, Walter Baigelman, and Ira B. Wilson, hospitalists at Tufts-New England Medical Center in Boston, MA were found to substantially improve throughput with high baseline occupancy levels. Compared with a control group, the hospitalist group reduced LOS from 3.45 days to 2.19 days (p<.001). Additionally, the total cost of hospital admission decreased from $2,332 to $1,775 (p<.001) when hospitalists were involved. According to the study authors, improved throughput generated an incremental 266 patients per year with a related incremental hospital profitability of $1.3 million with the use of hospitalists (7).
Conclusion
As hospital administrators attempt to address the issue of expeditiously admitting, treating and discharging patients in these days of restricted budgets and increased demand, hospitalist programs are poised as an invaluable factor in the throughput process.
Dr. Cawley can be contacted at pcawley@ushosp.com.
References
- Hospital Statistics: the comprehensive reference source for analysis and comparison of hospital trends. Published annually by Health Forum, an affiliate of the American Hospital Association.
- National and local impact of long-term demographic change on inpatient acute care. 2001. Solucient, LLC.
- Zibulewsky J. The Emergency Medical Treatment and Active Labor Act (EMTALA): what it is and what it means for physicians. Baylor University Medical Center (BUMC) Proceedings. 2001;14:339-46.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Eng J Med. 1996;335:514-7.
- Heffner JE. Executive medical director, Medical University of South Carolina (MUSC). Personal interview. June 24, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Serv Res. 2003;38:905-18.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical co-management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141:28-38.
- Wachter RM. The evolution of the hospitalist model in the United States. Med Clin North Am. 2002;86:687-706.
According to data from the American Hospital Association (1), in 1985, the United States had 5732 operational community hospitals; by 2002, the latest year for which figures are available, the number had decreased to 4927, a loss of approximately 14% (1). In that same timeframe, these hospitals lost approximately 18% of their beds, dropping from just over 1 million to 820,653 beds. This reduction in bed capacity has been accompanied by hospital cost-cutting efforts, staff downsizing, and elimination of services. Many explanations for these trends have been suggested, including changes in Medicare reimbursement and the growth of managed care organizations (MCOs).
However, as the current baby boom generation ages, rising inpatient demands are presenting hospitals with significant challenges. According to a 2001 report from Solucient (2), who maintains the nation’s largest health care database, the senior population—individuals age 65 and older—are projected to experience an 85% growth rate over the next two decades. Since this age group utilizes inpatient services 4.5 times more than younger populations, the number of admissions and beds to accommodate those cases will soar. By the year 2027, hospitals can anticipate a 46% rise in demand for acute inpatient beds as admissions escalate by approximately 13 million cases. Currently, the nation’s healthcare facilities admit 31 million cases; this number will jump to more than 44 million, representing a 41% growth from present admissions figures. For hospitals that maintain an 80% census rate, an additional 238,000 beds will be needed to meet demands (1).
Adding to this increase in demand and pressure on bed capacity, hospitals must address the requirements of the Emergency Medical Treatment and Active Labor Act (EMTALA) passed by the US Congress in 1986 as part of the Consolidated Omnibus Reconciliation Act (COBRA). The law’s initial intent was to ensure patient access to emergency medical care and to prevent the practice of patient dumping, in which uninsured patients were transferred, solely for financial reasons, from private to public hospitals without consideration of their medical condition or stability for the transfer (3). EMTALA mandates that hospitals rank the severity of patients. Thus, tertiary referral centers are required to admit the sickest patients first. This directive presents a significant challenge to many healthcare facilities. High census rates prohibit the admission of elective surgical cases, which, although profitable, are considered second tier. Routine medical cases or complicated emergency surgical cases have the potential to adversely affect the institution’s financial performance.
In addition to the challenge of increased bed demands and EMTALA, hospitals also cite an increasingly smaller number of on-site community physicians. Longstanding trends from inpatient to outpatient care have prompted many community physicians to concentrate their efforts on serving the needs of office-based patients, limiting their accessibility to hospital cases.
To address these pressures, hospitals must execute innovative strategies that deliver efficient throughput and enhance revenue, while still preserving high-quality services. Since 1996, hospital medicine programs have demonstrated a positive impact on the healthcare facility’s ability to increase overall productivity and profitability and still maintain high quality Patients today present to the doctor sicker than in the past and require more careful and frequent outpatient care. Since hospitalists operate solely on an inpatient basis, their availability to efficiently admit and manage hospitalized patients enables delivery of quality care that expedites appropriate treatment and shortens length of stay.
Two Roles of the Hospitalist
According to the Society of Hospital Medicine (SHM), “Hospitalists are physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to hospital medicine.” Coined by Drs. Robert Wachter and Lee Goldman in 1996 (4), the term implies an additional point of emphasis. Part of a new paradigm in clinical care, the hospitalist enhances the processes of care surrounding patients and adopts an attitude of accountability for that care. In practice, hospitalists play two key roles.
Primarily, the hospitalist is a practicing clinician — managing throughput on a case-by-case, patient-by-patient basis. In addition, a hospitalist performs a non-clinical role as an “inpatient expert,” taking the lead in creating system changes and communicating those changes to other hospital personnel as well as to community physicians. As an inpatient expert, hospitalists are often asked to lead organization-wide throughput initiatives to identify and implement strategies to facilitate patient flow and efficiency. As dedicated members of multi-disciplinary in-house teams, the hospitalist is in a prime position to foster change and improve systems.
Throughput as Continuum of Care
As suggested by Heffner (5), the process of admission, hospitalization, and discharge resembles a “bell-shaped curve.” To achieve effective throughput, hospitals must expedite patient care and also maintain careful oversight throughout a patient’s entire hospital stay. The hospitalist, as an integral part of a multidisciplinary team, coordinates care to promote a positive outcome and shorten length of stay. Drawing on strong leadership qualities, as well as on intimate knowledge of hospital procedures, layout design and infrastructure, and available community resources, the hospitalist plays a pivotal role in creating efficient throughput from admission to discharge.
Emergency Department
At the front end of the bell-shaped curve, the hospitalist may be engaged by emergency department (ED) physicians to assist in ensuring smooth patient flow and, more important, identifies the “intensity of service” needed. Through the use of clinical criteria, such as lnterQual, the hospitalist, together with the ED physician, may be asked to quantitatively rate the patient’s illness for degree of severity.
Timely patient evaluation helps prevent a backlog of ED cases and enables more patients to be seen. Immediate attention to and initiation of appropriate therapy guarantees a better outcome while minimizing the potential risk for complications, which could possibly lead to longer inpatient stays.
Inpatient Unit
Once a patient has been admitted to an inpatient unit, the hospitalist, together with a multidisciplinary team, facilitates care and determines the inpatient services that will optimize patient recovery through strong interdepartmental communications. Working together with admissions, medical records, nursing, laboratory and diagnostic services, information technology and other pertinent departments, the hospitalist maintains a pulse on all activity surrounding the patient and his care.
Judicious inpatient consultations and treatment decisions result in timely changes in therapy, potentially reducing the length of stay. The frequency with which the hospitalist sees the patient allows him to monitor any changes in condition and reduce possible decompensation, a practice known as vertical continuity (6). Such careful attention may reduce inpatient length of stay significantly. When aggressive management is mandated, the presence of the hospitalist enables initiation of effective therapy and results in quicker discharge and a reduction in potential readmission (7).
Surgery
The surgeon and hospitalist are ideally suited to work together in managing a surgical patient. The hospitalist focuses on the peri-operative management of medical issues and risk reduction, which allows the surgeon to concentrate more on surgical indications and the surgery itself. The hospitalist’s role in the management of a surgical patient enables vertical continuity when the surgeon may be occupied in the operating room with another patient as documented by Huddleston’s Hospitalist Orthopedic Team (HOT) approach (8).
Intensive Care Unit (ICU)
In many hospitals, particularly those that do not have intensivists, hospitalists are able to provide quality care to patients. Even in hospitals where intensivists manage ICU patients, hospitalists work together with the intensivist to ensure smoother transition into and out of the unit.
Discharge
Timing is a critical issue with regard to discharge. Since the hospitalist operates solely in-house and in collaboration with a multidisciplinary team, he is able to round early in the day to discharge patients by mid- or late-morning, freeing a bed for a new patient. In some cases, the hospitalist, in anticipation of early discharge, may begin pre-planning the day prior to discharge, which further expedites the process. Early discharge applies to the ICU, step-down areas and general inpatient care areas, as well as to full discharge from the healthcare facility. Moving a patient from one of these areas enables other patients to fill those empty beds thus optimizing throughput.
Having managed the patient throughout his hospital stay, the hospitalist — again working together with a multidisciplinary team —can facilitate arrangements to send the patient home or to a rehabilitation or skilled nursing facility or alternative housing situation upon discharge, as well as coordinating post-discharge care, whether it be arranging for a visiting nursing or social services or communicating with the primary care physician regarding follow-up appointments. If additional outpatient care is prescribed, the hospitalist will work with the discharge planning staff to contact various community agencies to arrange services best suited to the patient’s needs. Efficient discharge makes possible the admission of other, more critically ill patients, potentially enhancing the hospital’s revenue stream.
Stakeholder Analysis
Five specific stakeholders need to be examined to document the value-added by hospitalists. Anecdotal evidence, as well as documented studies, has demonstrated numerous returns—physical, social, psychological and financial—to stakeholders involved in the hospital process. With regard to throughput, the hospitalist provides benefits to each of the stakeholders listed in Table 1.
Study Results
A dozen studies have been conducted that document the impact of hospital medicine programs on cost and clinical outcomes. Of these trials, nine found a significant decrease in the average length of stay (15%) as well as reductions in cost (9). Two other studies, one from an academic medical center and the other from a community teaching hospital, demonstrate similar reductions during a 2-year follow-up period. At the Western Penn Hospital, a 54% reduction in readmissions was reported with a 12% decrease in hospital costs, while the average LOS was 17% shorter. Additionally, an unpublished study from the University of California, San Francisco Medical Center revealed a consistent 10-15% decline in cost and length of stay between hospitalists and non-hospitalist teaching faculty. More important, those differences remained stable through 6 years of follow-up. In general, hospitals with hospitalist programs realized a 5-39% decrease in costs and a shortened average LOS of 7-25% (6).
According to Robert M. Wachter, author of the 2002 study, “If the average U.S. hospitalist cares for 600 inpatients each year and generates a 10% savings over the average medical inpatient cost of $8,000, the nation’s 4500 hospitalists save approximately $2.2 billion per year while potentially improving quality” (6).
In a study conducted by Douglas Gregory, Walter Baigelman, and Ira B. Wilson, hospitalists at Tufts-New England Medical Center in Boston, MA were found to substantially improve throughput with high baseline occupancy levels. Compared with a control group, the hospitalist group reduced LOS from 3.45 days to 2.19 days (p<.001). Additionally, the total cost of hospital admission decreased from $2,332 to $1,775 (p<.001) when hospitalists were involved. According to the study authors, improved throughput generated an incremental 266 patients per year with a related incremental hospital profitability of $1.3 million with the use of hospitalists (7).
Conclusion
As hospital administrators attempt to address the issue of expeditiously admitting, treating and discharging patients in these days of restricted budgets and increased demand, hospitalist programs are poised as an invaluable factor in the throughput process.
Dr. Cawley can be contacted at pcawley@ushosp.com.
References
- Hospital Statistics: the comprehensive reference source for analysis and comparison of hospital trends. Published annually by Health Forum, an affiliate of the American Hospital Association.
- National and local impact of long-term demographic change on inpatient acute care. 2001. Solucient, LLC.
- Zibulewsky J. The Emergency Medical Treatment and Active Labor Act (EMTALA): what it is and what it means for physicians. Baylor University Medical Center (BUMC) Proceedings. 2001;14:339-46.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Eng J Med. 1996;335:514-7.
- Heffner JE. Executive medical director, Medical University of South Carolina (MUSC). Personal interview. June 24, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Serv Res. 2003;38:905-18.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical co-management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141:28-38.
- Wachter RM. The evolution of the hospitalist model in the United States. Med Clin North Am. 2002;86:687-706.
According to data from the American Hospital Association (1), in 1985, the United States had 5732 operational community hospitals; by 2002, the latest year for which figures are available, the number had decreased to 4927, a loss of approximately 14% (1). In that same timeframe, these hospitals lost approximately 18% of their beds, dropping from just over 1 million to 820,653 beds. This reduction in bed capacity has been accompanied by hospital cost-cutting efforts, staff downsizing, and elimination of services. Many explanations for these trends have been suggested, including changes in Medicare reimbursement and the growth of managed care organizations (MCOs).
However, as the current baby boom generation ages, rising inpatient demands are presenting hospitals with significant challenges. According to a 2001 report from Solucient (2), who maintains the nation’s largest health care database, the senior population—individuals age 65 and older—are projected to experience an 85% growth rate over the next two decades. Since this age group utilizes inpatient services 4.5 times more than younger populations, the number of admissions and beds to accommodate those cases will soar. By the year 2027, hospitals can anticipate a 46% rise in demand for acute inpatient beds as admissions escalate by approximately 13 million cases. Currently, the nation’s healthcare facilities admit 31 million cases; this number will jump to more than 44 million, representing a 41% growth from present admissions figures. For hospitals that maintain an 80% census rate, an additional 238,000 beds will be needed to meet demands (1).
Adding to this increase in demand and pressure on bed capacity, hospitals must address the requirements of the Emergency Medical Treatment and Active Labor Act (EMTALA) passed by the US Congress in 1986 as part of the Consolidated Omnibus Reconciliation Act (COBRA). The law’s initial intent was to ensure patient access to emergency medical care and to prevent the practice of patient dumping, in which uninsured patients were transferred, solely for financial reasons, from private to public hospitals without consideration of their medical condition or stability for the transfer (3). EMTALA mandates that hospitals rank the severity of patients. Thus, tertiary referral centers are required to admit the sickest patients first. This directive presents a significant challenge to many healthcare facilities. High census rates prohibit the admission of elective surgical cases, which, although profitable, are considered second tier. Routine medical cases or complicated emergency surgical cases have the potential to adversely affect the institution’s financial performance.
In addition to the challenge of increased bed demands and EMTALA, hospitals also cite an increasingly smaller number of on-site community physicians. Longstanding trends from inpatient to outpatient care have prompted many community physicians to concentrate their efforts on serving the needs of office-based patients, limiting their accessibility to hospital cases.
To address these pressures, hospitals must execute innovative strategies that deliver efficient throughput and enhance revenue, while still preserving high-quality services. Since 1996, hospital medicine programs have demonstrated a positive impact on the healthcare facility’s ability to increase overall productivity and profitability and still maintain high quality Patients today present to the doctor sicker than in the past and require more careful and frequent outpatient care. Since hospitalists operate solely on an inpatient basis, their availability to efficiently admit and manage hospitalized patients enables delivery of quality care that expedites appropriate treatment and shortens length of stay.
Two Roles of the Hospitalist
According to the Society of Hospital Medicine (SHM), “Hospitalists are physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to hospital medicine.” Coined by Drs. Robert Wachter and Lee Goldman in 1996 (4), the term implies an additional point of emphasis. Part of a new paradigm in clinical care, the hospitalist enhances the processes of care surrounding patients and adopts an attitude of accountability for that care. In practice, hospitalists play two key roles.
Primarily, the hospitalist is a practicing clinician — managing throughput on a case-by-case, patient-by-patient basis. In addition, a hospitalist performs a non-clinical role as an “inpatient expert,” taking the lead in creating system changes and communicating those changes to other hospital personnel as well as to community physicians. As an inpatient expert, hospitalists are often asked to lead organization-wide throughput initiatives to identify and implement strategies to facilitate patient flow and efficiency. As dedicated members of multi-disciplinary in-house teams, the hospitalist is in a prime position to foster change and improve systems.
Throughput as Continuum of Care
As suggested by Heffner (5), the process of admission, hospitalization, and discharge resembles a “bell-shaped curve.” To achieve effective throughput, hospitals must expedite patient care and also maintain careful oversight throughout a patient’s entire hospital stay. The hospitalist, as an integral part of a multidisciplinary team, coordinates care to promote a positive outcome and shorten length of stay. Drawing on strong leadership qualities, as well as on intimate knowledge of hospital procedures, layout design and infrastructure, and available community resources, the hospitalist plays a pivotal role in creating efficient throughput from admission to discharge.
Emergency Department
At the front end of the bell-shaped curve, the hospitalist may be engaged by emergency department (ED) physicians to assist in ensuring smooth patient flow and, more important, identifies the “intensity of service” needed. Through the use of clinical criteria, such as lnterQual, the hospitalist, together with the ED physician, may be asked to quantitatively rate the patient’s illness for degree of severity.
Timely patient evaluation helps prevent a backlog of ED cases and enables more patients to be seen. Immediate attention to and initiation of appropriate therapy guarantees a better outcome while minimizing the potential risk for complications, which could possibly lead to longer inpatient stays.
Inpatient Unit
Once a patient has been admitted to an inpatient unit, the hospitalist, together with a multidisciplinary team, facilitates care and determines the inpatient services that will optimize patient recovery through strong interdepartmental communications. Working together with admissions, medical records, nursing, laboratory and diagnostic services, information technology and other pertinent departments, the hospitalist maintains a pulse on all activity surrounding the patient and his care.
Judicious inpatient consultations and treatment decisions result in timely changes in therapy, potentially reducing the length of stay. The frequency with which the hospitalist sees the patient allows him to monitor any changes in condition and reduce possible decompensation, a practice known as vertical continuity (6). Such careful attention may reduce inpatient length of stay significantly. When aggressive management is mandated, the presence of the hospitalist enables initiation of effective therapy and results in quicker discharge and a reduction in potential readmission (7).
Surgery
The surgeon and hospitalist are ideally suited to work together in managing a surgical patient. The hospitalist focuses on the peri-operative management of medical issues and risk reduction, which allows the surgeon to concentrate more on surgical indications and the surgery itself. The hospitalist’s role in the management of a surgical patient enables vertical continuity when the surgeon may be occupied in the operating room with another patient as documented by Huddleston’s Hospitalist Orthopedic Team (HOT) approach (8).
Intensive Care Unit (ICU)
In many hospitals, particularly those that do not have intensivists, hospitalists are able to provide quality care to patients. Even in hospitals where intensivists manage ICU patients, hospitalists work together with the intensivist to ensure smoother transition into and out of the unit.
Discharge
Timing is a critical issue with regard to discharge. Since the hospitalist operates solely in-house and in collaboration with a multidisciplinary team, he is able to round early in the day to discharge patients by mid- or late-morning, freeing a bed for a new patient. In some cases, the hospitalist, in anticipation of early discharge, may begin pre-planning the day prior to discharge, which further expedites the process. Early discharge applies to the ICU, step-down areas and general inpatient care areas, as well as to full discharge from the healthcare facility. Moving a patient from one of these areas enables other patients to fill those empty beds thus optimizing throughput.
Having managed the patient throughout his hospital stay, the hospitalist — again working together with a multidisciplinary team —can facilitate arrangements to send the patient home or to a rehabilitation or skilled nursing facility or alternative housing situation upon discharge, as well as coordinating post-discharge care, whether it be arranging for a visiting nursing or social services or communicating with the primary care physician regarding follow-up appointments. If additional outpatient care is prescribed, the hospitalist will work with the discharge planning staff to contact various community agencies to arrange services best suited to the patient’s needs. Efficient discharge makes possible the admission of other, more critically ill patients, potentially enhancing the hospital’s revenue stream.
Stakeholder Analysis
Five specific stakeholders need to be examined to document the value-added by hospitalists. Anecdotal evidence, as well as documented studies, has demonstrated numerous returns—physical, social, psychological and financial—to stakeholders involved in the hospital process. With regard to throughput, the hospitalist provides benefits to each of the stakeholders listed in Table 1.
Study Results
A dozen studies have been conducted that document the impact of hospital medicine programs on cost and clinical outcomes. Of these trials, nine found a significant decrease in the average length of stay (15%) as well as reductions in cost (9). Two other studies, one from an academic medical center and the other from a community teaching hospital, demonstrate similar reductions during a 2-year follow-up period. At the Western Penn Hospital, a 54% reduction in readmissions was reported with a 12% decrease in hospital costs, while the average LOS was 17% shorter. Additionally, an unpublished study from the University of California, San Francisco Medical Center revealed a consistent 10-15% decline in cost and length of stay between hospitalists and non-hospitalist teaching faculty. More important, those differences remained stable through 6 years of follow-up. In general, hospitals with hospitalist programs realized a 5-39% decrease in costs and a shortened average LOS of 7-25% (6).
According to Robert M. Wachter, author of the 2002 study, “If the average U.S. hospitalist cares for 600 inpatients each year and generates a 10% savings over the average medical inpatient cost of $8,000, the nation’s 4500 hospitalists save approximately $2.2 billion per year while potentially improving quality” (6).
In a study conducted by Douglas Gregory, Walter Baigelman, and Ira B. Wilson, hospitalists at Tufts-New England Medical Center in Boston, MA were found to substantially improve throughput with high baseline occupancy levels. Compared with a control group, the hospitalist group reduced LOS from 3.45 days to 2.19 days (p<.001). Additionally, the total cost of hospital admission decreased from $2,332 to $1,775 (p<.001) when hospitalists were involved. According to the study authors, improved throughput generated an incremental 266 patients per year with a related incremental hospital profitability of $1.3 million with the use of hospitalists (7).
Conclusion
As hospital administrators attempt to address the issue of expeditiously admitting, treating and discharging patients in these days of restricted budgets and increased demand, hospitalist programs are poised as an invaluable factor in the throughput process.
Dr. Cawley can be contacted at pcawley@ushosp.com.
References
- Hospital Statistics: the comprehensive reference source for analysis and comparison of hospital trends. Published annually by Health Forum, an affiliate of the American Hospital Association.
- National and local impact of long-term demographic change on inpatient acute care. 2001. Solucient, LLC.
- Zibulewsky J. The Emergency Medical Treatment and Active Labor Act (EMTALA): what it is and what it means for physicians. Baylor University Medical Center (BUMC) Proceedings. 2001;14:339-46.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Eng J Med. 1996;335:514-7.
- Heffner JE. Executive medical director, Medical University of South Carolina (MUSC). Personal interview. June 24, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Serv Res. 2003;38:905-18.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical co-management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141:28-38.
- Wachter RM. The evolution of the hospitalist model in the United States. Med Clin North Am. 2002;86:687-706.
Improving Resource Utilization
Today’s hospitals must address a variety of challenges stemming from the expectation to provide more services and better quality with fewer financial, material, and human resources. According to the annual survey conducted by the American Hospital Association (AHA) in 2003, total expenses for all U.S. community hospitals were more than $450 billion. In managing these expenditures, hospitals face the following pressures:
- Cost increases in medical supplies and pharmaceuticals.
- Record shortages of nurses, pharmacists, and technicians.
- A growing uncompensated patient pool.
- Annual potential reductions in Medicare and Medicaid reimbursements.
- Rising bad debt resulting from greater patient responsibility for the cost of care.
- The diversion of more profitable cases to specialty and freestanding ambulatory care facilities and surgery centers.
- Soaring costs associated with adequately serving high-risk conditions, such as cancer, heart disease, and HIV/AIDS.
- Discounted reimbursement rates with insurers.
- Increasing pressure to commit financial resources to clinical information technology.
- The need to fund infrastructure improvements and physical plant renovations as well as expansions to address increasing demand (1).
To overcome these challenges, hospitals must find innovative ways to balance revenues and expenses, fund necessary capital investments, and satisfy the public’s demand for quality, safety, and accessibility.
Hospitalist Programs: A Good Investment
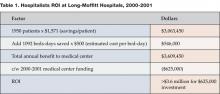
One solution to the above-mentioned situations is a hospitalist program, which, in its short history, has already had a profound impact on inpatient care. Robert M. Wachter, MD, associate chair in the department of medicine at the University of California, San Francisco (UCSF) and medical service chief at Moffitt-Long Hospitals, coined the term Hospitalist in an article in the New England Journal of Medicine in 1996 (2). At the 2002 annual meeting of the Society of Hospital Medicine (SHM), Wachter presented findings from a study conducted at his institution. The results demonstrate a significant return on investment (ROI) of 5.8:1 when a hospitalist program is utilized (See Table 1 for details) (3).
How do hospitalists reduce length of stay (LOS) and cost per stay? William David Rifkin, MD, associate director of the Yale Primary Care Residency Program, offers three basic reasons why hospitalist programs contribute to effective and efficient use of resources. Since hospitalists are physically onsite, they are better able to react to condition changes and requests for consultations in a timely manner, he asserts. Also, being familiar with the hospital’s systems of care, the hospitalist knows who to call and how to utilize the services of social workers and other contingency staff when arranging for post-discharge care. Third, Rifkin indicates that inpatients today are sicker than they were in past years, a fact well known and understood by hospitalists. “There is an increased level of acuity,” he says. “Hospitalists are used to seeing these kinds of patients. They are more comfortable taking care of these patients and will see more of them with any given diagnosis” (4).
In one of his studies, Rifkin noted a reduction in LOS for inpatients with a pneumonia diagnosis. “The hospitalist had switched the patient from IV (intravenous) to oral antibiotics,” he says. Reacting quickly to indications that the patient was ready for a change in treatment modality facilitated an earlier discharge (5).
L. Craig Miller, MD, senior vice president of medical affairs at Baptist Health Care, reports that his hospital saved $2.56 million in 2 years as a direct result of its inpatient management program (6). Although attention to technical and clinical details is important, Miller emphasizes the critical role the human factor plays, specifically the impact of teamwork, on achieving resource utilization savings.
“Hospitalists work as a team, collaborating with physicians and ED doctors,” he says. This cooperative spirit enables the efficient use of manpower in patient care. Miller adds that at Baptist, as is the case at most hospitals, the medical complexity of patients dictates a need for cooperation in order to successfully treat illness. The presence of hospitalists facilitates the team effort, causing a positive trickle down effect regarding LOS, readmission and mortality rates, he affirms. “The hospitalist provides focused leadership to utilization resource management,” says Miller (7).
In the role of inpatient leader, the hospitalist also facilitates ED throughput, which results in another area of cost savings for the hospital. Paola Coppola, MD, ED director at Brookhaven Memorial Hospital Medical Center, says, “From an ER perspective, a call to the hospitalist replaces multiple calls to specialists. In general, hospitalists feel much more comfortable treating a wide array of conditions including infectious disease, pneumonias, strokes, and chest pain without the intervention of specialists in that field. Hence, hospital consumption of resources decreases, which in turn lowers length of stay.” He echoes Rifkin’s thoughts on quick response time. “Hospitalists provide an immediately available service, thus saving ER physicians valuable time. This ensures faster turnover, better throughput, makes more ER beds available, and services more patients, eventually helping the hospital’s bottom line,” says Coppola (8).
In addition to teamwork, 24/7 availability is vital to the wise utilization of resources, according to Anthony Shallash, MD, vice president of medical affairs at Brookhaven. “The fact of 24/7 presence allows rapid responses to patient condition and problems. Continuous and close monitoring of patients allows them to be upgraded or downgraded as needed,” he says. “As such, LOS is decreased and quite favorable as compared to peer practitioners for similar disease severity. Resources consumed and tests ordered also show a favorable trend” (9).
A recently published study (10) by researchers at Dartmouth Medical School documents the variation in the volume and cost of services that academic medical centers use in treating patients. Hospitals were categorized as low- and high-intensity, with significant differences in cost per case. For example, the high-intensity hospitals spent up to 47% more on care for acute myocardial infarction. In an interview in Today’s Hospitalist (11), the lead author, Elliott S. Fisher, MD, professor of medicine and community and family medicine at Dartmouth Medical School, described the importance of coordination in achieving efficient care. Fisher says, “I think there’s a real opportunity for hospitalists to improve the care of patients in both high- and low- intensity hospitals. Having ten doctors involved in a given patient’s care may not be a good thing, unless someone [i.e., the hospitalist] is doing a really good job of coordinating that care.”
Hospitalists focus only on inpatient medicine. They are familiar with managing the most common medical diagnoses, such as community acquired pneumonia, diabetes. and congestive heart failure. Hospitalist programs often develop uniform and consistent ways of treating these patients. Cogent Healthcare, a national hospitalist management company has implemented the “Cogent Care Guides,” best practice guidelines for high-volume hospital diagnoses. Ron Greeno, MD, FCCP and Cogent’s chief medical officer, says “The Cogent Care Guides ensure best practices are implemented at critical points in the patient’s care… decreasing the variability of care that results in inefficiencies.” Greeno added, “The care guidelines [also] support the timely notification of the primary care physician of nine critical landmark events related to patient status that can affect outcomes” (12).
Stacy Goldsholl, Director of the Covenant HealthCare Hospital Medicine Program in Saginaw, MI, suggests other ways that hospitalists can generate utilization savings for their hospitals. “Hospitalists often eliminate unnecessary admissions and shift work-ups to the ambulatory setting. For example, I recently arranged an outpatient colonoscopy for a pneumonia patient with a stable hemoglobin and heme positive stool. Because of my experience treating patients with pneumonia, I was able to determine that the circumstances did not require an inpatient stay.” In addition, Dr. Goldsholl has found that the hospitalists in her program are quite effective in classifying “observation” patients, eliminating reimbursement conflicts with Medicare, Medicaid, and other insurers.
Finally, because they are always in the hospital rather than sharing time between the office and hospital, hospitalists can improve inpatient continuity of care, resulting in lower costs and better outcomes. Adrienne Bennett, MD, chief of the hospital medicine service at Newton-Wellesley Hospital near Boston, examined cases managed by hospitalists and non-hospitalist community physicians, comparing the number of “handoffs” of responsibility that occur among attending physicians. Community physicians share inpatient responsibility in their practices and sometimes their partners round on their patients. Every time another physician assumes responsibility for a patient, there is the potential for a loss of information and a discontinuity of care. At Newton-Wellesley Hospital, the hospitalists work a schedule of 14 days on, followed by 7 days off. “We found that hospitalists averaged less than half the number of handoffs as the community physicians,” says Bennett. “This may be one of the reasons that hospitalists have better case mix adjusted utilization performance.”
Stakeholder Analysis
Anecdotal evidence, as well as documented studies, has demonstrated that hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. With regard to resource utilization savings, the hospitalist provides benefits to each of the listed stakeholders (Table 2).
Published Research Results
Dozens of studies demonstrate the positive effects hospitalist programs have on resource utilization. Observational, retrospective, and prospective data analyses have been conducted at community-based hospitals as well as at academic medical institutions. Findings consistently indicate that hospitalist programs result in resource savings for patients, physicians. and hospital medicine. A range of studies shown in Table 3 represent the most recent efforts at tracking hospitalist programs and their effects on resource utilization.
Conclusion
According to the AHA’s 2003 survey of healthcare trends, the fiscal health of the nation’s hospitals will most likely remain fragile and variable in the coming years. The survey cites declining operating margins, a continued decrease in reimbursement, labor shortages, and rising insurance and pharmaceutical costs, as well as the need to invest in technology and facility maintenance and upkeep as key factors. However, hospitalists have proven time and again in clinical studies that they can bring value to the operation of a healthcare facility. With reduced lengths of stay, decreased overall hospital costs, and equivalent — if not superior — quality, hospitalists can contribute significantly to a hospital’s healthy bottom line.
Dr. Syed can be contacted at syed.saeed@CogentHealthcare.com.
References
- ACP Research Center, Environmental Assessment: Trends in hospital financing. 2003. www.aha.org.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-7
- Wachter RM. Presentation, Society of Hospital Medicine (SHM) annual meeting 2002. 4. Rifkin WD. Telephone interview December 15, 2004.
- Rifkin WD, Conner D, Silver A, Eichom A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- “Hospitalists save $2.5 million and decrease LOS.” Healthcare Benchmarks and Quality Improvement, May 2004.
- Miller LC. Telephone intewiew, November 16, 2004.
- Coppola P. Email interview, December 15,2004.
- Shallash A. Email interview, December17, 2004.
- Healthaffairs.org, “Use of Medicare claims data to monitor provider-specific performance among patients with severe chronic illness.” 10.1377/hlthaff.var.5. Posting date: October 7, 2004.
- Why less really can be more when it comes to teaching hospitals. Today’s Hospitalist. 2004 December.
- Greeno R. Chief medical officer, Cogent Healthcare, Irvine, California. Telephone interview. December 16, 2004.
- Everett GD, Anton MP Jackson BK, Swigert C, Uddin N. Comparison of hospital costs and length of stay associated with general internists and hospitalist physicians at a community hospital. Am J Manag Care. 2004;10:626-30.
- Kaboli PJ, Barnett MJ, Rosenthal GE. Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10:561-8.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Services Research. 2003:38(3):905-18; discussion 919-22.
- Wachter RM, Goldman L The hospitalist movement 5 years later. JAMA. 2002;287:487-94.
- Palmer HC, Armistead NS, Elnicki DM, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med. 2001;111:627-32.
Today’s hospitals must address a variety of challenges stemming from the expectation to provide more services and better quality with fewer financial, material, and human resources. According to the annual survey conducted by the American Hospital Association (AHA) in 2003, total expenses for all U.S. community hospitals were more than $450 billion. In managing these expenditures, hospitals face the following pressures:
- Cost increases in medical supplies and pharmaceuticals.
- Record shortages of nurses, pharmacists, and technicians.
- A growing uncompensated patient pool.
- Annual potential reductions in Medicare and Medicaid reimbursements.
- Rising bad debt resulting from greater patient responsibility for the cost of care.
- The diversion of more profitable cases to specialty and freestanding ambulatory care facilities and surgery centers.
- Soaring costs associated with adequately serving high-risk conditions, such as cancer, heart disease, and HIV/AIDS.
- Discounted reimbursement rates with insurers.
- Increasing pressure to commit financial resources to clinical information technology.
- The need to fund infrastructure improvements and physical plant renovations as well as expansions to address increasing demand (1).
To overcome these challenges, hospitals must find innovative ways to balance revenues and expenses, fund necessary capital investments, and satisfy the public’s demand for quality, safety, and accessibility.
Hospitalist Programs: A Good Investment
One solution to the above-mentioned situations is a hospitalist program, which, in its short history, has already had a profound impact on inpatient care. Robert M. Wachter, MD, associate chair in the department of medicine at the University of California, San Francisco (UCSF) and medical service chief at Moffitt-Long Hospitals, coined the term Hospitalist in an article in the New England Journal of Medicine in 1996 (2). At the 2002 annual meeting of the Society of Hospital Medicine (SHM), Wachter presented findings from a study conducted at his institution. The results demonstrate a significant return on investment (ROI) of 5.8:1 when a hospitalist program is utilized (See Table 1 for details) (3).
How do hospitalists reduce length of stay (LOS) and cost per stay? William David Rifkin, MD, associate director of the Yale Primary Care Residency Program, offers three basic reasons why hospitalist programs contribute to effective and efficient use of resources. Since hospitalists are physically onsite, they are better able to react to condition changes and requests for consultations in a timely manner, he asserts. Also, being familiar with the hospital’s systems of care, the hospitalist knows who to call and how to utilize the services of social workers and other contingency staff when arranging for post-discharge care. Third, Rifkin indicates that inpatients today are sicker than they were in past years, a fact well known and understood by hospitalists. “There is an increased level of acuity,” he says. “Hospitalists are used to seeing these kinds of patients. They are more comfortable taking care of these patients and will see more of them with any given diagnosis” (4).
In one of his studies, Rifkin noted a reduction in LOS for inpatients with a pneumonia diagnosis. “The hospitalist had switched the patient from IV (intravenous) to oral antibiotics,” he says. Reacting quickly to indications that the patient was ready for a change in treatment modality facilitated an earlier discharge (5).
L. Craig Miller, MD, senior vice president of medical affairs at Baptist Health Care, reports that his hospital saved $2.56 million in 2 years as a direct result of its inpatient management program (6). Although attention to technical and clinical details is important, Miller emphasizes the critical role the human factor plays, specifically the impact of teamwork, on achieving resource utilization savings.
“Hospitalists work as a team, collaborating with physicians and ED doctors,” he says. This cooperative spirit enables the efficient use of manpower in patient care. Miller adds that at Baptist, as is the case at most hospitals, the medical complexity of patients dictates a need for cooperation in order to successfully treat illness. The presence of hospitalists facilitates the team effort, causing a positive trickle down effect regarding LOS, readmission and mortality rates, he affirms. “The hospitalist provides focused leadership to utilization resource management,” says Miller (7).
In the role of inpatient leader, the hospitalist also facilitates ED throughput, which results in another area of cost savings for the hospital. Paola Coppola, MD, ED director at Brookhaven Memorial Hospital Medical Center, says, “From an ER perspective, a call to the hospitalist replaces multiple calls to specialists. In general, hospitalists feel much more comfortable treating a wide array of conditions including infectious disease, pneumonias, strokes, and chest pain without the intervention of specialists in that field. Hence, hospital consumption of resources decreases, which in turn lowers length of stay.” He echoes Rifkin’s thoughts on quick response time. “Hospitalists provide an immediately available service, thus saving ER physicians valuable time. This ensures faster turnover, better throughput, makes more ER beds available, and services more patients, eventually helping the hospital’s bottom line,” says Coppola (8).
In addition to teamwork, 24/7 availability is vital to the wise utilization of resources, according to Anthony Shallash, MD, vice president of medical affairs at Brookhaven. “The fact of 24/7 presence allows rapid responses to patient condition and problems. Continuous and close monitoring of patients allows them to be upgraded or downgraded as needed,” he says. “As such, LOS is decreased and quite favorable as compared to peer practitioners for similar disease severity. Resources consumed and tests ordered also show a favorable trend” (9).
A recently published study (10) by researchers at Dartmouth Medical School documents the variation in the volume and cost of services that academic medical centers use in treating patients. Hospitals were categorized as low- and high-intensity, with significant differences in cost per case. For example, the high-intensity hospitals spent up to 47% more on care for acute myocardial infarction. In an interview in Today’s Hospitalist (11), the lead author, Elliott S. Fisher, MD, professor of medicine and community and family medicine at Dartmouth Medical School, described the importance of coordination in achieving efficient care. Fisher says, “I think there’s a real opportunity for hospitalists to improve the care of patients in both high- and low- intensity hospitals. Having ten doctors involved in a given patient’s care may not be a good thing, unless someone [i.e., the hospitalist] is doing a really good job of coordinating that care.”
Hospitalists focus only on inpatient medicine. They are familiar with managing the most common medical diagnoses, such as community acquired pneumonia, diabetes. and congestive heart failure. Hospitalist programs often develop uniform and consistent ways of treating these patients. Cogent Healthcare, a national hospitalist management company has implemented the “Cogent Care Guides,” best practice guidelines for high-volume hospital diagnoses. Ron Greeno, MD, FCCP and Cogent’s chief medical officer, says “The Cogent Care Guides ensure best practices are implemented at critical points in the patient’s care… decreasing the variability of care that results in inefficiencies.” Greeno added, “The care guidelines [also] support the timely notification of the primary care physician of nine critical landmark events related to patient status that can affect outcomes” (12).
Stacy Goldsholl, Director of the Covenant HealthCare Hospital Medicine Program in Saginaw, MI, suggests other ways that hospitalists can generate utilization savings for their hospitals. “Hospitalists often eliminate unnecessary admissions and shift work-ups to the ambulatory setting. For example, I recently arranged an outpatient colonoscopy for a pneumonia patient with a stable hemoglobin and heme positive stool. Because of my experience treating patients with pneumonia, I was able to determine that the circumstances did not require an inpatient stay.” In addition, Dr. Goldsholl has found that the hospitalists in her program are quite effective in classifying “observation” patients, eliminating reimbursement conflicts with Medicare, Medicaid, and other insurers.
Finally, because they are always in the hospital rather than sharing time between the office and hospital, hospitalists can improve inpatient continuity of care, resulting in lower costs and better outcomes. Adrienne Bennett, MD, chief of the hospital medicine service at Newton-Wellesley Hospital near Boston, examined cases managed by hospitalists and non-hospitalist community physicians, comparing the number of “handoffs” of responsibility that occur among attending physicians. Community physicians share inpatient responsibility in their practices and sometimes their partners round on their patients. Every time another physician assumes responsibility for a patient, there is the potential for a loss of information and a discontinuity of care. At Newton-Wellesley Hospital, the hospitalists work a schedule of 14 days on, followed by 7 days off. “We found that hospitalists averaged less than half the number of handoffs as the community physicians,” says Bennett. “This may be one of the reasons that hospitalists have better case mix adjusted utilization performance.”
Stakeholder Analysis
Anecdotal evidence, as well as documented studies, has demonstrated that hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. With regard to resource utilization savings, the hospitalist provides benefits to each of the listed stakeholders (Table 2).
Published Research Results
Dozens of studies demonstrate the positive effects hospitalist programs have on resource utilization. Observational, retrospective, and prospective data analyses have been conducted at community-based hospitals as well as at academic medical institutions. Findings consistently indicate that hospitalist programs result in resource savings for patients, physicians. and hospital medicine. A range of studies shown in Table 3 represent the most recent efforts at tracking hospitalist programs and their effects on resource utilization.
Conclusion
According to the AHA’s 2003 survey of healthcare trends, the fiscal health of the nation’s hospitals will most likely remain fragile and variable in the coming years. The survey cites declining operating margins, a continued decrease in reimbursement, labor shortages, and rising insurance and pharmaceutical costs, as well as the need to invest in technology and facility maintenance and upkeep as key factors. However, hospitalists have proven time and again in clinical studies that they can bring value to the operation of a healthcare facility. With reduced lengths of stay, decreased overall hospital costs, and equivalent — if not superior — quality, hospitalists can contribute significantly to a hospital’s healthy bottom line.
Dr. Syed can be contacted at syed.saeed@CogentHealthcare.com.
References
- ACP Research Center, Environmental Assessment: Trends in hospital financing. 2003. www.aha.org.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-7
- Wachter RM. Presentation, Society of Hospital Medicine (SHM) annual meeting 2002. 4. Rifkin WD. Telephone interview December 15, 2004.
- Rifkin WD, Conner D, Silver A, Eichom A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- “Hospitalists save $2.5 million and decrease LOS.” Healthcare Benchmarks and Quality Improvement, May 2004.
- Miller LC. Telephone intewiew, November 16, 2004.
- Coppola P. Email interview, December 15,2004.
- Shallash A. Email interview, December17, 2004.
- Healthaffairs.org, “Use of Medicare claims data to monitor provider-specific performance among patients with severe chronic illness.” 10.1377/hlthaff.var.5. Posting date: October 7, 2004.
- Why less really can be more when it comes to teaching hospitals. Today’s Hospitalist. 2004 December.
- Greeno R. Chief medical officer, Cogent Healthcare, Irvine, California. Telephone interview. December 16, 2004.
- Everett GD, Anton MP Jackson BK, Swigert C, Uddin N. Comparison of hospital costs and length of stay associated with general internists and hospitalist physicians at a community hospital. Am J Manag Care. 2004;10:626-30.
- Kaboli PJ, Barnett MJ, Rosenthal GE. Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10:561-8.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Services Research. 2003:38(3):905-18; discussion 919-22.
- Wachter RM, Goldman L The hospitalist movement 5 years later. JAMA. 2002;287:487-94.
- Palmer HC, Armistead NS, Elnicki DM, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med. 2001;111:627-32.
Today’s hospitals must address a variety of challenges stemming from the expectation to provide more services and better quality with fewer financial, material, and human resources. According to the annual survey conducted by the American Hospital Association (AHA) in 2003, total expenses for all U.S. community hospitals were more than $450 billion. In managing these expenditures, hospitals face the following pressures:
- Cost increases in medical supplies and pharmaceuticals.
- Record shortages of nurses, pharmacists, and technicians.
- A growing uncompensated patient pool.
- Annual potential reductions in Medicare and Medicaid reimbursements.
- Rising bad debt resulting from greater patient responsibility for the cost of care.
- The diversion of more profitable cases to specialty and freestanding ambulatory care facilities and surgery centers.
- Soaring costs associated with adequately serving high-risk conditions, such as cancer, heart disease, and HIV/AIDS.
- Discounted reimbursement rates with insurers.
- Increasing pressure to commit financial resources to clinical information technology.
- The need to fund infrastructure improvements and physical plant renovations as well as expansions to address increasing demand (1).
To overcome these challenges, hospitals must find innovative ways to balance revenues and expenses, fund necessary capital investments, and satisfy the public’s demand for quality, safety, and accessibility.
Hospitalist Programs: A Good Investment
One solution to the above-mentioned situations is a hospitalist program, which, in its short history, has already had a profound impact on inpatient care. Robert M. Wachter, MD, associate chair in the department of medicine at the University of California, San Francisco (UCSF) and medical service chief at Moffitt-Long Hospitals, coined the term Hospitalist in an article in the New England Journal of Medicine in 1996 (2). At the 2002 annual meeting of the Society of Hospital Medicine (SHM), Wachter presented findings from a study conducted at his institution. The results demonstrate a significant return on investment (ROI) of 5.8:1 when a hospitalist program is utilized (See Table 1 for details) (3).
How do hospitalists reduce length of stay (LOS) and cost per stay? William David Rifkin, MD, associate director of the Yale Primary Care Residency Program, offers three basic reasons why hospitalist programs contribute to effective and efficient use of resources. Since hospitalists are physically onsite, they are better able to react to condition changes and requests for consultations in a timely manner, he asserts. Also, being familiar with the hospital’s systems of care, the hospitalist knows who to call and how to utilize the services of social workers and other contingency staff when arranging for post-discharge care. Third, Rifkin indicates that inpatients today are sicker than they were in past years, a fact well known and understood by hospitalists. “There is an increased level of acuity,” he says. “Hospitalists are used to seeing these kinds of patients. They are more comfortable taking care of these patients and will see more of them with any given diagnosis” (4).
In one of his studies, Rifkin noted a reduction in LOS for inpatients with a pneumonia diagnosis. “The hospitalist had switched the patient from IV (intravenous) to oral antibiotics,” he says. Reacting quickly to indications that the patient was ready for a change in treatment modality facilitated an earlier discharge (5).
L. Craig Miller, MD, senior vice president of medical affairs at Baptist Health Care, reports that his hospital saved $2.56 million in 2 years as a direct result of its inpatient management program (6). Although attention to technical and clinical details is important, Miller emphasizes the critical role the human factor plays, specifically the impact of teamwork, on achieving resource utilization savings.
“Hospitalists work as a team, collaborating with physicians and ED doctors,” he says. This cooperative spirit enables the efficient use of manpower in patient care. Miller adds that at Baptist, as is the case at most hospitals, the medical complexity of patients dictates a need for cooperation in order to successfully treat illness. The presence of hospitalists facilitates the team effort, causing a positive trickle down effect regarding LOS, readmission and mortality rates, he affirms. “The hospitalist provides focused leadership to utilization resource management,” says Miller (7).
In the role of inpatient leader, the hospitalist also facilitates ED throughput, which results in another area of cost savings for the hospital. Paola Coppola, MD, ED director at Brookhaven Memorial Hospital Medical Center, says, “From an ER perspective, a call to the hospitalist replaces multiple calls to specialists. In general, hospitalists feel much more comfortable treating a wide array of conditions including infectious disease, pneumonias, strokes, and chest pain without the intervention of specialists in that field. Hence, hospital consumption of resources decreases, which in turn lowers length of stay.” He echoes Rifkin’s thoughts on quick response time. “Hospitalists provide an immediately available service, thus saving ER physicians valuable time. This ensures faster turnover, better throughput, makes more ER beds available, and services more patients, eventually helping the hospital’s bottom line,” says Coppola (8).
In addition to teamwork, 24/7 availability is vital to the wise utilization of resources, according to Anthony Shallash, MD, vice president of medical affairs at Brookhaven. “The fact of 24/7 presence allows rapid responses to patient condition and problems. Continuous and close monitoring of patients allows them to be upgraded or downgraded as needed,” he says. “As such, LOS is decreased and quite favorable as compared to peer practitioners for similar disease severity. Resources consumed and tests ordered also show a favorable trend” (9).
A recently published study (10) by researchers at Dartmouth Medical School documents the variation in the volume and cost of services that academic medical centers use in treating patients. Hospitals were categorized as low- and high-intensity, with significant differences in cost per case. For example, the high-intensity hospitals spent up to 47% more on care for acute myocardial infarction. In an interview in Today’s Hospitalist (11), the lead author, Elliott S. Fisher, MD, professor of medicine and community and family medicine at Dartmouth Medical School, described the importance of coordination in achieving efficient care. Fisher says, “I think there’s a real opportunity for hospitalists to improve the care of patients in both high- and low- intensity hospitals. Having ten doctors involved in a given patient’s care may not be a good thing, unless someone [i.e., the hospitalist] is doing a really good job of coordinating that care.”
Hospitalists focus only on inpatient medicine. They are familiar with managing the most common medical diagnoses, such as community acquired pneumonia, diabetes. and congestive heart failure. Hospitalist programs often develop uniform and consistent ways of treating these patients. Cogent Healthcare, a national hospitalist management company has implemented the “Cogent Care Guides,” best practice guidelines for high-volume hospital diagnoses. Ron Greeno, MD, FCCP and Cogent’s chief medical officer, says “The Cogent Care Guides ensure best practices are implemented at critical points in the patient’s care… decreasing the variability of care that results in inefficiencies.” Greeno added, “The care guidelines [also] support the timely notification of the primary care physician of nine critical landmark events related to patient status that can affect outcomes” (12).
Stacy Goldsholl, Director of the Covenant HealthCare Hospital Medicine Program in Saginaw, MI, suggests other ways that hospitalists can generate utilization savings for their hospitals. “Hospitalists often eliminate unnecessary admissions and shift work-ups to the ambulatory setting. For example, I recently arranged an outpatient colonoscopy for a pneumonia patient with a stable hemoglobin and heme positive stool. Because of my experience treating patients with pneumonia, I was able to determine that the circumstances did not require an inpatient stay.” In addition, Dr. Goldsholl has found that the hospitalists in her program are quite effective in classifying “observation” patients, eliminating reimbursement conflicts with Medicare, Medicaid, and other insurers.
Finally, because they are always in the hospital rather than sharing time between the office and hospital, hospitalists can improve inpatient continuity of care, resulting in lower costs and better outcomes. Adrienne Bennett, MD, chief of the hospital medicine service at Newton-Wellesley Hospital near Boston, examined cases managed by hospitalists and non-hospitalist community physicians, comparing the number of “handoffs” of responsibility that occur among attending physicians. Community physicians share inpatient responsibility in their practices and sometimes their partners round on their patients. Every time another physician assumes responsibility for a patient, there is the potential for a loss of information and a discontinuity of care. At Newton-Wellesley Hospital, the hospitalists work a schedule of 14 days on, followed by 7 days off. “We found that hospitalists averaged less than half the number of handoffs as the community physicians,” says Bennett. “This may be one of the reasons that hospitalists have better case mix adjusted utilization performance.”
Stakeholder Analysis
Anecdotal evidence, as well as documented studies, has demonstrated that hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. With regard to resource utilization savings, the hospitalist provides benefits to each of the listed stakeholders (Table 2).
Published Research Results
Dozens of studies demonstrate the positive effects hospitalist programs have on resource utilization. Observational, retrospective, and prospective data analyses have been conducted at community-based hospitals as well as at academic medical institutions. Findings consistently indicate that hospitalist programs result in resource savings for patients, physicians. and hospital medicine. A range of studies shown in Table 3 represent the most recent efforts at tracking hospitalist programs and their effects on resource utilization.
Conclusion
According to the AHA’s 2003 survey of healthcare trends, the fiscal health of the nation’s hospitals will most likely remain fragile and variable in the coming years. The survey cites declining operating margins, a continued decrease in reimbursement, labor shortages, and rising insurance and pharmaceutical costs, as well as the need to invest in technology and facility maintenance and upkeep as key factors. However, hospitalists have proven time and again in clinical studies that they can bring value to the operation of a healthcare facility. With reduced lengths of stay, decreased overall hospital costs, and equivalent — if not superior — quality, hospitalists can contribute significantly to a hospital’s healthy bottom line.
Dr. Syed can be contacted at syed.saeed@CogentHealthcare.com.
References
- ACP Research Center, Environmental Assessment: Trends in hospital financing. 2003. www.aha.org.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-7
- Wachter RM. Presentation, Society of Hospital Medicine (SHM) annual meeting 2002. 4. Rifkin WD. Telephone interview December 15, 2004.
- Rifkin WD, Conner D, Silver A, Eichom A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- “Hospitalists save $2.5 million and decrease LOS.” Healthcare Benchmarks and Quality Improvement, May 2004.
- Miller LC. Telephone intewiew, November 16, 2004.
- Coppola P. Email interview, December 15,2004.
- Shallash A. Email interview, December17, 2004.
- Healthaffairs.org, “Use of Medicare claims data to monitor provider-specific performance among patients with severe chronic illness.” 10.1377/hlthaff.var.5. Posting date: October 7, 2004.
- Why less really can be more when it comes to teaching hospitals. Today’s Hospitalist. 2004 December.
- Greeno R. Chief medical officer, Cogent Healthcare, Irvine, California. Telephone interview. December 16, 2004.
- Everett GD, Anton MP Jackson BK, Swigert C, Uddin N. Comparison of hospital costs and length of stay associated with general internists and hospitalist physicians at a community hospital. Am J Manag Care. 2004;10:626-30.
- Kaboli PJ, Barnett MJ, Rosenthal GE. Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10:561-8.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Services Research. 2003:38(3):905-18; discussion 919-22.
- Wachter RM, Goldman L The hospitalist movement 5 years later. JAMA. 2002;287:487-94.
- Palmer HC, Armistead NS, Elnicki DM, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med. 2001;111:627-32.
Providing Extraordinary Availability
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.
Leading Hospital Medical Staffs
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.
Improving Physician's Practices
Hospitals face a range of critical issues and need members of their medical staff to assume a role in addressing them. These concerns include declining payments and pressures on the bottom line; staffing shortages and dissatisfaction; questions about quality and patient safety; constantly changing technologies; employer and consumer demands for performance metrics; capacity constraints; and increased competition from independent, niche providers of clinical services.
Many physicians are no longer able or willing to serve on hospital committees or play a leadership role for the medical staff. As a result of the pressures of lost income, managed care requirements, on-call responsibilities, and competition for patients, as well as life-style concerns, many physicians are reluctant to perform volunteer work that hospitals used to take for granted. A 2004 survey of CEOs and physician leaders at 55 hospitals in the Northeast conducted by Mitretek, a healthcare consulting firm, noted that "volunteerism is dead." Physicians expect to be paid for time spent on hospital business. Sixty-four percent of the respondents said their hospitals compensate physicians to serve as officers or department heads (1).
"It used to be that most doctors needed the hospital to be successful; now that is not the case," says Larry Wellikson, MD, CEO of the Society of Hospital Medicine (SHM), the national professional society for hospitalists. Trends have shifted and a growing number of specialists do not even practice in the hospital (2).
Hospitalists: Stepping Up to the Medical Staff Leadership Challenge
Wellikson predicts that doctors on the hospital's "home team" - hospitalists, intensivists, and emergency department physicians - will assume more prominent positions on hospital committees. Hospitalists emerge as strong candidates for providing medical staff leadership for the following reasons:
- Hospitalists spend the majority of their time in the in-patient environment, making them familiar with hospital systems, policies, services, departments, and staff.
- Hospitalists are inpatient experts who possess clinical credibility when addressing key issues regarding the inpatient environment.
- Many hospitalists are hospital employees who can understand the tradeoffs involved in balancing the needs of the institution with those of the medical staff. Even hospitalists not employed by the hospital have an intimate knowledge of the issues that the hospital is facing and are invested in finding solutions to these problems.
Figure 1. describes a range of roles that a hospitalist could assume and a range of topics that a hospitalist could address in providing medical staff leadership in a hospital.
The left side of the diagram describes three leadership roles that a hospitalist might play in the hospital. First, a hospitalist can volunteer to participate on a hospital committee, either as a member of the committee or as its chairperson. Second, a hospitalist can volunteer to work on a hospital project, either in a staff/expert role or in the role of project leader. Third, a hospitalist can assume a direct administrative role in the hospital, directing a service or program.
Whether it is through a committee, project, or direct administrative responsibility, a hospitalist has the knowledge and expertise to become involved in a wide range of hospital issues. As characterized on the right side of Figure 1, these topics include:
- Practice Guidelines: Many hospitals have adopted practice guidelines as a tool for improving the quality and efficiency of care. When properly developed, guidelines can improve patient safety, facilitate the adoption of best practices, and reduce hospital costs. Hospitalists can be asked to participate in all aspects of guideline development, including research, authorship, implementation, outcome measurement, and on-going revision and educational efforts.
- Utilization Review: Hospitals or medical groups routinely arrange for physicians to perform utilization review or improve the utilization review process. A hospitalist can: 1) facilitate the discharge process for individual patients, reducing length of stay and hospital costs; and 2) globally improve throughput by identifying and addressing system problems that create inefficiencies in the patient care or discharge process (e.g., paperwork or dictations not completed on time, poor communication across healthcare team disciplines, administrative deficiencies that delay therapies, etc.).
- Patient Satisfaction: Hospitals are increasingly being asked to capture and disseminate performance metrics so that employers and consumers can make informed decisions about their provider of choice. Patient satisfaction is a key measure of a hospital's performance. Hospitalists can become engaged in efforts to review patient satisfaction survey results, identify problems, and propose/implement solutions.
- Quality Improvement: Many hospitals look to hospitalists to become involved in or lead the hospital's quality improvement (QI) efforts. Specific activities may include championing individual QI projects, working with QI staff to develop and analyze outcomes data, educating colleagues regarding new projects and protocols, etc.
- Patient Safety: Preventing harmful errors from occurring in the inpatient environment has become a major priority for the hospitals across the country. Identifying the causes of these errors and developing methods of error prevention require detailed investigations and analyses of the diagnostic and/or treatment process. Increasingly, hospitalists are being asked to provide leadership to patient safety initiatives.
- Compliance: Hospitals must comply with many federal, state, and local rules and regulations. For example, a great deal of coordination and planning is required to meet the requirements of the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO), the Health Insurance Portability and Accountability Act (HIPAA) of 1996, and/or the Accreditation Council for Graduate Medical Education (ACGME). In some hospitals, hospitalists assume leadership roles in these compliance efforts.
- Disaster Planning: Hospitals need to demonstrate the ability to respond to a range of potential crises, including those related to bioterrorism, industrial accidents, and natural disasters (e.g., hurricanes, tornados, and earthquakes). In light of their knowledge of patient flow, hospitalists can be asked to work with emergency physicians to do disaster planning for the hospital and the local region.
- Information Systems: Several organizations have issued reports identifying information technology as a critical tool for improving healthcare quality (e.g., Institute of Medicine [IOM], the Leapfrog Group, eHealth Initiative, the Markle Foundation, and the Federal Office of the National Coordinator for Health Information Technology). Hospitals are being encouraged and incentivized to implement electronic health records (EHRs) and computerized physician order entry (CPOE) systems. Implementing these systems requires significant clinical input. Many hospitals have asked hospitalists to champion and lead the implementation process of new information systems.
- Nursing/Physician Assistant Staffing: There exists a wide range of roles for nurses and physician assistants in the inpatient setting. Every institution needs to find a staffing model that is efficient, effective, and results in provider satisfaction. Hospitalists are considered leaders of the inpatient medical team and can be asked to help design and evaluate staffing models.
Hospitalists as Physician Leaders: The Facts
A 1999 survey (3) conducted by the National Association of Inpatient Physicians (NAIP, now SHM) documented the medical staff leadership roles of hospitalists. Of the survey respondents, 53% held responsibility for quality assurance and/or utilization review; 46% were responsible for practice guideline development; 23% had administrative responsibilities; and 22% were charged with information systems development.
There are several different types of hospitalist programs and, as shown by the examples below, each model offers opportunities for hospitalists to play a medical staff leadership role.
Academic Medical Centers
The hospitalists that practice at University of California at San Francisco Medical Center (UCSF) are making a significant impact on many critical hospital issues. Robert Wächter, MD, chief of the hospitalist program at UCSF and a former president of SI IM says, while it is still important to have other specialists serve on medical staff committees, UCSF hospitalists participate on all committees, chairing some of the crucial ones, such as patient safety. "The structure of the medical staff won't change, but the doctors who participate will," Wächter says. "They [hospitalists] will be more invested in the hospital, so the nature of the committee work will change. It will become more effective" (4). Selected QI projects led by UCSF hospitalists include:
- Medical Service Discharge Planning Improvement Project
- Collaborative Daily Bedside Rounds— a program to improve physician-nurse communication
- Protocol for Management of Alcohol Withdrawal
- Protocol for Prevention and Management of Delirium
- Medical Service Intern Signout— an educational program to enhance physician signout in the setting of new resident duty hours requirements
- Perioperative Performance Improvement Project— assessing the use of beta-blockers, glucose management surgical site infection and DVT prophylaxis
- DVT Treatment and DVT Prophylaxis Protocols
- JCAHO Core Measures in community acquired pneumonia and smoking cessation
- Post-Discharge Home Visits— a collaborative pharmacy-hospitalist project for patients at high risk for readmission
UCSF hospitalists are also leaders and key participants in many interdisciplinary medical center performance improvement committees including the Patient Safety Committee, Clinical Performance Improvement Committee, Physicians Advisory Group for Clinical Information Systems, Patient Satisfaction Committee, Pharmacy and Therapeutics Committee, and the Patient Flow Committee (4).
Community Hospitals
At Mercy Medical Center in Springfield, MA, 10% of the hospitalist's bonus is based on participation in "good citizenship" activities for the hospital. To earn his bonus, Winthrop Whitcomb, MD, director of the Mercy Inpatient Medical Service (MIMS), organizes the hospital's CME accredited medical education series, which is offered to the entire medical staff. Every month, Whitcomb is responsible for developing learning objectives, identifying speakers, and coordinating the program logistics.
Other MIMS hospitalists have chosen the following good citizenship activities:
- Chairperson of the Medication Reconciliation Committee, a statewide initiative designed to assure medication information is consistently communicated across different care settings
- Leadership of a tribunal that evaluated a physician for ethical issues and made a decision whether or not medical staff privileges should be revoked
- Clinical expert and resource for the implementation of a new hospital information system
Medical Groups
Harvard Vanguard Medical Associates (HVMA) is a 550-physician group practice with 14 practice locations in the greater Boston area. Joseph L. Dorsey, MD, director of the medical group's hospitalist program, described the following medical staff leadership roles that HVMA hospitalists execute at their six affiliated hospitals:
- Quality Improvement Committee
- Interdepartmental Committee, which reviews cases for possible reporting to state healthcare agencies
- Medical Executive Committee
- Clinical and Education Planning Task Force, which is preparing plans to move approximately 60 medical inpatients off the house staff covered service onto a Physician Assistant-supported alternative
- Advisory Committee to the Department of Medicine Chairperson, consisting of all sub-specialty Chiefs
- Credentialing Committee
- Clinical Teaching Initiative
Stakeholder analysis
By playing a medical staff leadership role, hospitalists provide value to several stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Conclusion
Hospital administrators need physician leaders to address critical strategic and operational issues. Given their position as "inpatient experts," hospitalists are a logical choice to play this role. In the years ahead, it is likely that hospitalists will assume an increasingly important leadership role within community hospitals and academic medical centers around the country.
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
Ms. Kerr can be contacted at kkerr@medicine.ucsf.edu.
References
- McGowan RA. Strengthening hospital-physician relationships. HFMA Business December 2004.
- Hospitals & Health Networks, Vol. 77, No. 11. Health Forum, November 2003.
- Lindenauer PK, Pantilat SZ, Katz PP, Wachter RM. Hospitalists and the practice of inpatient medicine: result of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130: 343-9.
- UCSF hospitalist Web site: http://medicine.ucsf.edu/hospitalists/quality.html.
Hospitals face a range of critical issues and need members of their medical staff to assume a role in addressing them. These concerns include declining payments and pressures on the bottom line; staffing shortages and dissatisfaction; questions about quality and patient safety; constantly changing technologies; employer and consumer demands for performance metrics; capacity constraints; and increased competition from independent, niche providers of clinical services.
Many physicians are no longer able or willing to serve on hospital committees or play a leadership role for the medical staff. As a result of the pressures of lost income, managed care requirements, on-call responsibilities, and competition for patients, as well as life-style concerns, many physicians are reluctant to perform volunteer work that hospitals used to take for granted. A 2004 survey of CEOs and physician leaders at 55 hospitals in the Northeast conducted by Mitretek, a healthcare consulting firm, noted that "volunteerism is dead." Physicians expect to be paid for time spent on hospital business. Sixty-four percent of the respondents said their hospitals compensate physicians to serve as officers or department heads (1).
"It used to be that most doctors needed the hospital to be successful; now that is not the case," says Larry Wellikson, MD, CEO of the Society of Hospital Medicine (SHM), the national professional society for hospitalists. Trends have shifted and a growing number of specialists do not even practice in the hospital (2).
Hospitalists: Stepping Up to the Medical Staff Leadership Challenge
Wellikson predicts that doctors on the hospital's "home team" - hospitalists, intensivists, and emergency department physicians - will assume more prominent positions on hospital committees. Hospitalists emerge as strong candidates for providing medical staff leadership for the following reasons:
- Hospitalists spend the majority of their time in the in-patient environment, making them familiar with hospital systems, policies, services, departments, and staff.
- Hospitalists are inpatient experts who possess clinical credibility when addressing key issues regarding the inpatient environment.
- Many hospitalists are hospital employees who can understand the tradeoffs involved in balancing the needs of the institution with those of the medical staff. Even hospitalists not employed by the hospital have an intimate knowledge of the issues that the hospital is facing and are invested in finding solutions to these problems.
Figure 1. describes a range of roles that a hospitalist could assume and a range of topics that a hospitalist could address in providing medical staff leadership in a hospital.
The left side of the diagram describes three leadership roles that a hospitalist might play in the hospital. First, a hospitalist can volunteer to participate on a hospital committee, either as a member of the committee or as its chairperson. Second, a hospitalist can volunteer to work on a hospital project, either in a staff/expert role or in the role of project leader. Third, a hospitalist can assume a direct administrative role in the hospital, directing a service or program.
Whether it is through a committee, project, or direct administrative responsibility, a hospitalist has the knowledge and expertise to become involved in a wide range of hospital issues. As characterized on the right side of Figure 1, these topics include:
- Practice Guidelines: Many hospitals have adopted practice guidelines as a tool for improving the quality and efficiency of care. When properly developed, guidelines can improve patient safety, facilitate the adoption of best practices, and reduce hospital costs. Hospitalists can be asked to participate in all aspects of guideline development, including research, authorship, implementation, outcome measurement, and on-going revision and educational efforts.
- Utilization Review: Hospitals or medical groups routinely arrange for physicians to perform utilization review or improve the utilization review process. A hospitalist can: 1) facilitate the discharge process for individual patients, reducing length of stay and hospital costs; and 2) globally improve throughput by identifying and addressing system problems that create inefficiencies in the patient care or discharge process (e.g., paperwork or dictations not completed on time, poor communication across healthcare team disciplines, administrative deficiencies that delay therapies, etc.).
- Patient Satisfaction: Hospitals are increasingly being asked to capture and disseminate performance metrics so that employers and consumers can make informed decisions about their provider of choice. Patient satisfaction is a key measure of a hospital's performance. Hospitalists can become engaged in efforts to review patient satisfaction survey results, identify problems, and propose/implement solutions.
- Quality Improvement: Many hospitals look to hospitalists to become involved in or lead the hospital's quality improvement (QI) efforts. Specific activities may include championing individual QI projects, working with QI staff to develop and analyze outcomes data, educating colleagues regarding new projects and protocols, etc.
- Patient Safety: Preventing harmful errors from occurring in the inpatient environment has become a major priority for the hospitals across the country. Identifying the causes of these errors and developing methods of error prevention require detailed investigations and analyses of the diagnostic and/or treatment process. Increasingly, hospitalists are being asked to provide leadership to patient safety initiatives.
- Compliance: Hospitals must comply with many federal, state, and local rules and regulations. For example, a great deal of coordination and planning is required to meet the requirements of the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO), the Health Insurance Portability and Accountability Act (HIPAA) of 1996, and/or the Accreditation Council for Graduate Medical Education (ACGME). In some hospitals, hospitalists assume leadership roles in these compliance efforts.
- Disaster Planning: Hospitals need to demonstrate the ability to respond to a range of potential crises, including those related to bioterrorism, industrial accidents, and natural disasters (e.g., hurricanes, tornados, and earthquakes). In light of their knowledge of patient flow, hospitalists can be asked to work with emergency physicians to do disaster planning for the hospital and the local region.
- Information Systems: Several organizations have issued reports identifying information technology as a critical tool for improving healthcare quality (e.g., Institute of Medicine [IOM], the Leapfrog Group, eHealth Initiative, the Markle Foundation, and the Federal Office of the National Coordinator for Health Information Technology). Hospitals are being encouraged and incentivized to implement electronic health records (EHRs) and computerized physician order entry (CPOE) systems. Implementing these systems requires significant clinical input. Many hospitals have asked hospitalists to champion and lead the implementation process of new information systems.
- Nursing/Physician Assistant Staffing: There exists a wide range of roles for nurses and physician assistants in the inpatient setting. Every institution needs to find a staffing model that is efficient, effective, and results in provider satisfaction. Hospitalists are considered leaders of the inpatient medical team and can be asked to help design and evaluate staffing models.
Hospitalists as Physician Leaders: The Facts
A 1999 survey (3) conducted by the National Association of Inpatient Physicians (NAIP, now SHM) documented the medical staff leadership roles of hospitalists. Of the survey respondents, 53% held responsibility for quality assurance and/or utilization review; 46% were responsible for practice guideline development; 23% had administrative responsibilities; and 22% were charged with information systems development.
There are several different types of hospitalist programs and, as shown by the examples below, each model offers opportunities for hospitalists to play a medical staff leadership role.
Academic Medical Centers
The hospitalists that practice at University of California at San Francisco Medical Center (UCSF) are making a significant impact on many critical hospital issues. Robert Wächter, MD, chief of the hospitalist program at UCSF and a former president of SI IM says, while it is still important to have other specialists serve on medical staff committees, UCSF hospitalists participate on all committees, chairing some of the crucial ones, such as patient safety. "The structure of the medical staff won't change, but the doctors who participate will," Wächter says. "They [hospitalists] will be more invested in the hospital, so the nature of the committee work will change. It will become more effective" (4). Selected QI projects led by UCSF hospitalists include:
- Medical Service Discharge Planning Improvement Project
- Collaborative Daily Bedside Rounds— a program to improve physician-nurse communication
- Protocol for Management of Alcohol Withdrawal
- Protocol for Prevention and Management of Delirium
- Medical Service Intern Signout— an educational program to enhance physician signout in the setting of new resident duty hours requirements
- Perioperative Performance Improvement Project— assessing the use of beta-blockers, glucose management surgical site infection and DVT prophylaxis
- DVT Treatment and DVT Prophylaxis Protocols
- JCAHO Core Measures in community acquired pneumonia and smoking cessation
- Post-Discharge Home Visits— a collaborative pharmacy-hospitalist project for patients at high risk for readmission
UCSF hospitalists are also leaders and key participants in many interdisciplinary medical center performance improvement committees including the Patient Safety Committee, Clinical Performance Improvement Committee, Physicians Advisory Group for Clinical Information Systems, Patient Satisfaction Committee, Pharmacy and Therapeutics Committee, and the Patient Flow Committee (4).
Community Hospitals
At Mercy Medical Center in Springfield, MA, 10% of the hospitalist's bonus is based on participation in "good citizenship" activities for the hospital. To earn his bonus, Winthrop Whitcomb, MD, director of the Mercy Inpatient Medical Service (MIMS), organizes the hospital's CME accredited medical education series, which is offered to the entire medical staff. Every month, Whitcomb is responsible for developing learning objectives, identifying speakers, and coordinating the program logistics.
Other MIMS hospitalists have chosen the following good citizenship activities:
- Chairperson of the Medication Reconciliation Committee, a statewide initiative designed to assure medication information is consistently communicated across different care settings
- Leadership of a tribunal that evaluated a physician for ethical issues and made a decision whether or not medical staff privileges should be revoked
- Clinical expert and resource for the implementation of a new hospital information system
Medical Groups
Harvard Vanguard Medical Associates (HVMA) is a 550-physician group practice with 14 practice locations in the greater Boston area. Joseph L. Dorsey, MD, director of the medical group's hospitalist program, described the following medical staff leadership roles that HVMA hospitalists execute at their six affiliated hospitals:
- Quality Improvement Committee
- Interdepartmental Committee, which reviews cases for possible reporting to state healthcare agencies
- Medical Executive Committee
- Clinical and Education Planning Task Force, which is preparing plans to move approximately 60 medical inpatients off the house staff covered service onto a Physician Assistant-supported alternative
- Advisory Committee to the Department of Medicine Chairperson, consisting of all sub-specialty Chiefs
- Credentialing Committee
- Clinical Teaching Initiative
Stakeholder analysis
By playing a medical staff leadership role, hospitalists provide value to several stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Conclusion
Hospital administrators need physician leaders to address critical strategic and operational issues. Given their position as "inpatient experts," hospitalists are a logical choice to play this role. In the years ahead, it is likely that hospitalists will assume an increasingly important leadership role within community hospitals and academic medical centers around the country.
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
Ms. Kerr can be contacted at kkerr@medicine.ucsf.edu.
References
- McGowan RA. Strengthening hospital-physician relationships. HFMA Business December 2004.
- Hospitals & Health Networks, Vol. 77, No. 11. Health Forum, November 2003.
- Lindenauer PK, Pantilat SZ, Katz PP, Wachter RM. Hospitalists and the practice of inpatient medicine: result of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130: 343-9.
- UCSF hospitalist Web site: http://medicine.ucsf.edu/hospitalists/quality.html.
Hospitals face a range of critical issues and need members of their medical staff to assume a role in addressing them. These concerns include declining payments and pressures on the bottom line; staffing shortages and dissatisfaction; questions about quality and patient safety; constantly changing technologies; employer and consumer demands for performance metrics; capacity constraints; and increased competition from independent, niche providers of clinical services.
Many physicians are no longer able or willing to serve on hospital committees or play a leadership role for the medical staff. As a result of the pressures of lost income, managed care requirements, on-call responsibilities, and competition for patients, as well as life-style concerns, many physicians are reluctant to perform volunteer work that hospitals used to take for granted. A 2004 survey of CEOs and physician leaders at 55 hospitals in the Northeast conducted by Mitretek, a healthcare consulting firm, noted that "volunteerism is dead." Physicians expect to be paid for time spent on hospital business. Sixty-four percent of the respondents said their hospitals compensate physicians to serve as officers or department heads (1).
"It used to be that most doctors needed the hospital to be successful; now that is not the case," says Larry Wellikson, MD, CEO of the Society of Hospital Medicine (SHM), the national professional society for hospitalists. Trends have shifted and a growing number of specialists do not even practice in the hospital (2).
Hospitalists: Stepping Up to the Medical Staff Leadership Challenge
Wellikson predicts that doctors on the hospital's "home team" - hospitalists, intensivists, and emergency department physicians - will assume more prominent positions on hospital committees. Hospitalists emerge as strong candidates for providing medical staff leadership for the following reasons:
- Hospitalists spend the majority of their time in the in-patient environment, making them familiar with hospital systems, policies, services, departments, and staff.
- Hospitalists are inpatient experts who possess clinical credibility when addressing key issues regarding the inpatient environment.
- Many hospitalists are hospital employees who can understand the tradeoffs involved in balancing the needs of the institution with those of the medical staff. Even hospitalists not employed by the hospital have an intimate knowledge of the issues that the hospital is facing and are invested in finding solutions to these problems.
Figure 1. describes a range of roles that a hospitalist could assume and a range of topics that a hospitalist could address in providing medical staff leadership in a hospital.
The left side of the diagram describes three leadership roles that a hospitalist might play in the hospital. First, a hospitalist can volunteer to participate on a hospital committee, either as a member of the committee or as its chairperson. Second, a hospitalist can volunteer to work on a hospital project, either in a staff/expert role or in the role of project leader. Third, a hospitalist can assume a direct administrative role in the hospital, directing a service or program.
Whether it is through a committee, project, or direct administrative responsibility, a hospitalist has the knowledge and expertise to become involved in a wide range of hospital issues. As characterized on the right side of Figure 1, these topics include:
- Practice Guidelines: Many hospitals have adopted practice guidelines as a tool for improving the quality and efficiency of care. When properly developed, guidelines can improve patient safety, facilitate the adoption of best practices, and reduce hospital costs. Hospitalists can be asked to participate in all aspects of guideline development, including research, authorship, implementation, outcome measurement, and on-going revision and educational efforts.
- Utilization Review: Hospitals or medical groups routinely arrange for physicians to perform utilization review or improve the utilization review process. A hospitalist can: 1) facilitate the discharge process for individual patients, reducing length of stay and hospital costs; and 2) globally improve throughput by identifying and addressing system problems that create inefficiencies in the patient care or discharge process (e.g., paperwork or dictations not completed on time, poor communication across healthcare team disciplines, administrative deficiencies that delay therapies, etc.).
- Patient Satisfaction: Hospitals are increasingly being asked to capture and disseminate performance metrics so that employers and consumers can make informed decisions about their provider of choice. Patient satisfaction is a key measure of a hospital's performance. Hospitalists can become engaged in efforts to review patient satisfaction survey results, identify problems, and propose/implement solutions.
- Quality Improvement: Many hospitals look to hospitalists to become involved in or lead the hospital's quality improvement (QI) efforts. Specific activities may include championing individual QI projects, working with QI staff to develop and analyze outcomes data, educating colleagues regarding new projects and protocols, etc.
- Patient Safety: Preventing harmful errors from occurring in the inpatient environment has become a major priority for the hospitals across the country. Identifying the causes of these errors and developing methods of error prevention require detailed investigations and analyses of the diagnostic and/or treatment process. Increasingly, hospitalists are being asked to provide leadership to patient safety initiatives.
- Compliance: Hospitals must comply with many federal, state, and local rules and regulations. For example, a great deal of coordination and planning is required to meet the requirements of the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO), the Health Insurance Portability and Accountability Act (HIPAA) of 1996, and/or the Accreditation Council for Graduate Medical Education (ACGME). In some hospitals, hospitalists assume leadership roles in these compliance efforts.
- Disaster Planning: Hospitals need to demonstrate the ability to respond to a range of potential crises, including those related to bioterrorism, industrial accidents, and natural disasters (e.g., hurricanes, tornados, and earthquakes). In light of their knowledge of patient flow, hospitalists can be asked to work with emergency physicians to do disaster planning for the hospital and the local region.
- Information Systems: Several organizations have issued reports identifying information technology as a critical tool for improving healthcare quality (e.g., Institute of Medicine [IOM], the Leapfrog Group, eHealth Initiative, the Markle Foundation, and the Federal Office of the National Coordinator for Health Information Technology). Hospitals are being encouraged and incentivized to implement electronic health records (EHRs) and computerized physician order entry (CPOE) systems. Implementing these systems requires significant clinical input. Many hospitals have asked hospitalists to champion and lead the implementation process of new information systems.
- Nursing/Physician Assistant Staffing: There exists a wide range of roles for nurses and physician assistants in the inpatient setting. Every institution needs to find a staffing model that is efficient, effective, and results in provider satisfaction. Hospitalists are considered leaders of the inpatient medical team and can be asked to help design and evaluate staffing models.
Hospitalists as Physician Leaders: The Facts
A 1999 survey (3) conducted by the National Association of Inpatient Physicians (NAIP, now SHM) documented the medical staff leadership roles of hospitalists. Of the survey respondents, 53% held responsibility for quality assurance and/or utilization review; 46% were responsible for practice guideline development; 23% had administrative responsibilities; and 22% were charged with information systems development.
There are several different types of hospitalist programs and, as shown by the examples below, each model offers opportunities for hospitalists to play a medical staff leadership role.
Academic Medical Centers
The hospitalists that practice at University of California at San Francisco Medical Center (UCSF) are making a significant impact on many critical hospital issues. Robert Wächter, MD, chief of the hospitalist program at UCSF and a former president of SI IM says, while it is still important to have other specialists serve on medical staff committees, UCSF hospitalists participate on all committees, chairing some of the crucial ones, such as patient safety. "The structure of the medical staff won't change, but the doctors who participate will," Wächter says. "They [hospitalists] will be more invested in the hospital, so the nature of the committee work will change. It will become more effective" (4). Selected QI projects led by UCSF hospitalists include:
- Medical Service Discharge Planning Improvement Project
- Collaborative Daily Bedside Rounds— a program to improve physician-nurse communication
- Protocol for Management of Alcohol Withdrawal
- Protocol for Prevention and Management of Delirium
- Medical Service Intern Signout— an educational program to enhance physician signout in the setting of new resident duty hours requirements
- Perioperative Performance Improvement Project— assessing the use of beta-blockers, glucose management surgical site infection and DVT prophylaxis
- DVT Treatment and DVT Prophylaxis Protocols
- JCAHO Core Measures in community acquired pneumonia and smoking cessation
- Post-Discharge Home Visits— a collaborative pharmacy-hospitalist project for patients at high risk for readmission
UCSF hospitalists are also leaders and key participants in many interdisciplinary medical center performance improvement committees including the Patient Safety Committee, Clinical Performance Improvement Committee, Physicians Advisory Group for Clinical Information Systems, Patient Satisfaction Committee, Pharmacy and Therapeutics Committee, and the Patient Flow Committee (4).
Community Hospitals
At Mercy Medical Center in Springfield, MA, 10% of the hospitalist's bonus is based on participation in "good citizenship" activities for the hospital. To earn his bonus, Winthrop Whitcomb, MD, director of the Mercy Inpatient Medical Service (MIMS), organizes the hospital's CME accredited medical education series, which is offered to the entire medical staff. Every month, Whitcomb is responsible for developing learning objectives, identifying speakers, and coordinating the program logistics.
Other MIMS hospitalists have chosen the following good citizenship activities:
- Chairperson of the Medication Reconciliation Committee, a statewide initiative designed to assure medication information is consistently communicated across different care settings
- Leadership of a tribunal that evaluated a physician for ethical issues and made a decision whether or not medical staff privileges should be revoked
- Clinical expert and resource for the implementation of a new hospital information system
Medical Groups
Harvard Vanguard Medical Associates (HVMA) is a 550-physician group practice with 14 practice locations in the greater Boston area. Joseph L. Dorsey, MD, director of the medical group's hospitalist program, described the following medical staff leadership roles that HVMA hospitalists execute at their six affiliated hospitals:
- Quality Improvement Committee
- Interdepartmental Committee, which reviews cases for possible reporting to state healthcare agencies
- Medical Executive Committee
- Clinical and Education Planning Task Force, which is preparing plans to move approximately 60 medical inpatients off the house staff covered service onto a Physician Assistant-supported alternative
- Advisory Committee to the Department of Medicine Chairperson, consisting of all sub-specialty Chiefs
- Credentialing Committee
- Clinical Teaching Initiative
Stakeholder analysis
By playing a medical staff leadership role, hospitalists provide value to several stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Conclusion
Hospital administrators need physician leaders to address critical strategic and operational issues. Given their position as "inpatient experts," hospitalists are a logical choice to play this role. In the years ahead, it is likely that hospitalists will assume an increasingly important leadership role within community hospitals and academic medical centers around the country.
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
Ms. Kerr can be contacted at kkerr@medicine.ucsf.edu.
References
- McGowan RA. Strengthening hospital-physician relationships. HFMA Business December 2004.
- Hospitals & Health Networks, Vol. 77, No. 11. Health Forum, November 2003.
- Lindenauer PK, Pantilat SZ, Katz PP, Wachter RM. Hospitalists and the practice of inpatient medicine: result of a survey of the National Association of Inpatient Physicians. Ann Intern Med. 1999;130: 343-9.
- UCSF hospitalist Web site: http://medicine.ucsf.edu/hospitalists/quality.html.
Treating Unassigned Patients
In the 1970s and 1980s, indigent patients experienced problems at hospital Emergency Departments (EDs) around the country. They were refused care and shuttled to other facilities for services. To protect patients against these types of abuses, Congress passed The Emergency Medical Treatment and Labor Act (EMTALA) in 1986 as part of the Consolidated Omnibus Budget Reconciliation Act (COBRA).·
EMTALA mandates that all patients presenting to the ED - regardless of insurance status - receive a medical screening examination and be medically stable prior to transfer to another facility. If a hospital has the facilities to treat the emergency, the patient can not be transferred to another ED. To address these requirements, every hospital must have physicians on call to assist emergency physicians in assessing and treating unassigned patients.
By the late 1990s, as EMTALA requirements took hold, inadequate on-call physician coverage reached crisis proportions and became a front page issue. In 1999, USA Today carried the following headline: "A Care Crisis in ERs: Nation's Hospitals Plagued by Shortage of On-Call Specialists" (1). In that same year, Modem Healthcare ran an article with the following headline: "Blaming the Docs: Patient Dumping Probes See Physicians as Culprits in Turning Away Indigent from ERs" (2). In California, a task force was formed to address the matter (3), and the American Medical Association (AMA) began exploring solutions at the highest levels (4).
Why do hospitals have problems organizing their medical staff to be available to provide on-call treatment of unassigned patients in the ED and subsequent to admission? There appear to be three major reasons for this problem.
First, at a minimum, on-call treatment of unassigned patients creates an inconvenience for physicians, taking away from their personal time; worse. it can reduce the number of available hours they have to spend with their office-based patients.
Second, there are financial disincentives to on-call coverage. Often unassigned patients presenting in the ED are uninsured or under-insured. On-call physicians frequently do not receive adequate compensation for the task of treating these patients.
Finally, on-call duty can bring bureaucratic hassles and/or legal liability for physicians. Dealing with state Medicaid agencies may require addressing administrative requirements, completing paperwork, and paying penalties for not following the rules.
Richard Frankenstein, MD, a pulmonologist in Southern California, admitted an uninsured patient with multiple chronic illnesses when he was the on-call physician at one of his affiliated hospitals. The patient spent 8 weeks in the hospital, much of that time in intensive care. Frankenstein often visited this patient twice a day, so his already busy schedule began hour earlier and ended 1 hour later. He received no compensation for these efforts. That commitment dragged me away from my primary responsibilities,” said Frankenstein. "I'm no longer on staff there, and that situation was a major reason that I resigned (5).
During the past 5 years, the crisis of on-call physician coverage has been significantly reduced and hospitalists emerge as one of the major reasons why. Although there are still issues related to the availability of on-call specialists and surgeons, hospitals that have implemented hospital medicine programs are able to make available experienced general internists to triage, admit, and treat unassigned patients.
Hospital Medicine Programs:
A Value Added Resource to Hospitals
Hospital medicine programs are characterized by several unique features that facilitate the treatment of unassigned patients and result in significant benefits for hospitals. Figure 1 above illustrates these relationships.
Mark Aronson, MD, serves as a member of the Department of Medicine at Beth Israel Deaconess Medical Center (BIDMC), a 5O0-bed academic medical center in Boston and is also Vice Chairman for Quality and Professor of Medicine at Harvard Medical School. BIDMC has a mature hospital medicine program, and approximately 55-60% of the program's patients are unassigned, representing more than 25% of the hospital's general medicine census. Aronson believes that the hospital medicine program provides value to both patients and the institution. He described a case in which a nursing home patient without health insurance presented in the ED. After the initial evaluation, the ED attending decided to admit the patient. One of the hospitalists recognized the patient as someone he had treated several times before. He knew that her medical condition would not require hospitalization and arranged the appropriate treatment, allowing for transfer back to the nursing home. “In this situation, because the hospitalist had a relationship and history with the unassigned patient, the patient received timely, quality medical care and the hospital saved a significant amount of money” (5).
In the ED, the prompt and efficient treatment of unassigned patients can reduce backlogs and minimize hassles for emergency physicians. There is no need for the emergency physician to track down an on-call physician to admit the patient. The ED maintains a better work flow and makes better use of their resources, especially of physician and nursing time as well as space. Most hospitalists are familiar with pertinent laws (e.g., EMTALA) and insurance company policies, thereby spending less time investigating and resolving problems. The hospitals benefits through improved throughput.
"We have a high-volume ED with a large percentage of unassigned patients. In addition our hospital census is often 120% at midday and 90% at midnight. Efficient flow of patients though the ED at all hours is a critical issue at our hospital," says Patrick Cawley, MD, Director of Hospitalist Services at the Medical University of South Carolina in Charleston. "We have been asked to lead throughput initiatives which have resulted in a dramatic reduction in backlogs and the movement of patients out of the ED either to a bed or possibly to an alternative setting.”
The members of the medical staff of a hospital are often the driving force for the creation of a hospital medicine program. Having hopitalists at their institution may mean that affiliated physicians do not have to assume the undesirable responsibilities of participating in an on-call schedule. Furthermore, since hospitalists typically do not have an office practice, community physicians still have the opportunity to care for the unassigned patients once they are discharged, thereby building their practice. Hospitals can refer the patients according to an equitable schedule approved by the medical staff. By addressing issues related to on-call physician coverage, a hospital can improve medical staff relations.
At Winchester Medical Center in Virginia, family practitioners in the area surrendered their admitting privileges, creating an onerous call schedule for generalist internists. The hospital hired four hospitalists to admit and treat all unassigned patients. Instead of taking call, the internists are part of a primary care roster and rotate responsibility for unassigned patients once they are discharged (6). It has been a win-win solution for the hospital and the medical staff.
Often the unassigned patients have significant discharge planning and placement problems, especially those that are uninsured. While these issues can be daunting to the office-based physicians, hospitalists usually have a more comprehensive knowledge of the resources of the hospital and the community to help solve these placement and post-discharge care issues.
In treating unassigned patients, hospitalists blend their clinical skills with knowledge of their hospital’s objectives, concerns, policies, and procedures. Since they are a relatively small, cohesive group within the institution, hospitalists are often familiar with practice guidelines, medical records documentation requirements, computerized physician order entry (CPOE) systems, quality initiatives, and utilization management requirements.
"The hospitalists’ responsibilities in our program must have a good citizenship component," says Winthrop Whitcomb, MD, Director of the Inpatient Medicine Service at Merry Medical Center in Springfield, MA and co-founder of the Society of Hospital Medicine (SHM). "Each physician must serve on a committee, a project, or a program that serves the hospital. Hospitalists are often the leaders of hospital-wide initiatives directed at quality of care, utilization management, and throughput.”
Stakeholder Analysis
By treating unassigned patients, hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Assigning Value to Hospitalists' Work
Hospitalists typically manage unassigned and uninsured patients as part of their regular job duties. It is important that the administrator or leader of the hospital medicine group have a budgetary understanding of how to "score" the services that the hospitalists provide to these patients.
If the hospitalist service is provided by an independent, contracted group, they may be paid for treating the unassigned, uninsured patients. Often the payment is in the form of a case rate, based on the "average" number of services provided in an admission and using a Medicare or other mutually agreed upon fee schedule.
If the hospitalists are employees of the hospital, it is expected that they will assume responsibility for unassigned, uninsured patients. Although the hospital medicine group will not receive direct reimbursement for seeing these patients (unlike a contracted hospitalist group), the value of this service to the hospital must be recognized. In these situations, hospital administrators should acknowledge the critical need to credit the hospitalists for real work that must be performed but that generates little or no revenue. An equivalent case rate can be credited as a paper transaction to the hospitalist group to address the value of these services.
Conclusion
Given the current economic environment, the issue of treating unassigned and uninsured patients will not soon diminish. Demand is likely to increase with the nationwide growth in the number of uninsured patients. Physician resistance to call coverage and the rise of malpractice premiums will continue to create more pressure for hospitals to find solutions to this crisis. "We recognize that hospitalists are only part of the solution," says Ron Angus, MS, Past President of SHM. "Hospitals and government agencies must provide funding to cover the costs of inpatient care for acutely ill, uninsured - and usually unassigned - patients. Hospitals must also find ways to ensure that other specialists are available to hospitalists for acutely ill inpatients who require specialty expertise or procedures. With such cooperation and participation, hospitalists can be an important part of the solution to the problems now reaching crisis proportions in American emergency rooms" (7).
References
- Appleby J. Hospitals plagued by on-call shortage. USA Today June 16. 1999.
- Blaming the docs: patient dumping probes see physicians as culprits in turning away indigent from ERs. Modern Healthcare August 9, 1999.
- Winston K, The Advisory Board Company, Clinical Initiatives Center. Cause for concern: ensuring adequate and timely on-call physician coverage in the emergency department. ED Watch Issue #4, May 2, 2000.
- Foubister V. Is there a dearth of specialists in the ED? American Medical News July 12, 1999.
- Wanted: doctors willing to take ER call. ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, November 2001.
- Aronson M, Beth Israel Deaconess Medical Center. Personal interview. December 2004.
- Angus R, letter to the editor, ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, December 2001.
In the 1970s and 1980s, indigent patients experienced problems at hospital Emergency Departments (EDs) around the country. They were refused care and shuttled to other facilities for services. To protect patients against these types of abuses, Congress passed The Emergency Medical Treatment and Labor Act (EMTALA) in 1986 as part of the Consolidated Omnibus Budget Reconciliation Act (COBRA).·
EMTALA mandates that all patients presenting to the ED - regardless of insurance status - receive a medical screening examination and be medically stable prior to transfer to another facility. If a hospital has the facilities to treat the emergency, the patient can not be transferred to another ED. To address these requirements, every hospital must have physicians on call to assist emergency physicians in assessing and treating unassigned patients.
By the late 1990s, as EMTALA requirements took hold, inadequate on-call physician coverage reached crisis proportions and became a front page issue. In 1999, USA Today carried the following headline: "A Care Crisis in ERs: Nation's Hospitals Plagued by Shortage of On-Call Specialists" (1). In that same year, Modem Healthcare ran an article with the following headline: "Blaming the Docs: Patient Dumping Probes See Physicians as Culprits in Turning Away Indigent from ERs" (2). In California, a task force was formed to address the matter (3), and the American Medical Association (AMA) began exploring solutions at the highest levels (4).
Why do hospitals have problems organizing their medical staff to be available to provide on-call treatment of unassigned patients in the ED and subsequent to admission? There appear to be three major reasons for this problem.
First, at a minimum, on-call treatment of unassigned patients creates an inconvenience for physicians, taking away from their personal time; worse. it can reduce the number of available hours they have to spend with their office-based patients.
Second, there are financial disincentives to on-call coverage. Often unassigned patients presenting in the ED are uninsured or under-insured. On-call physicians frequently do not receive adequate compensation for the task of treating these patients.
Finally, on-call duty can bring bureaucratic hassles and/or legal liability for physicians. Dealing with state Medicaid agencies may require addressing administrative requirements, completing paperwork, and paying penalties for not following the rules.
Richard Frankenstein, MD, a pulmonologist in Southern California, admitted an uninsured patient with multiple chronic illnesses when he was the on-call physician at one of his affiliated hospitals. The patient spent 8 weeks in the hospital, much of that time in intensive care. Frankenstein often visited this patient twice a day, so his already busy schedule began hour earlier and ended 1 hour later. He received no compensation for these efforts. That commitment dragged me away from my primary responsibilities,” said Frankenstein. "I'm no longer on staff there, and that situation was a major reason that I resigned (5).
During the past 5 years, the crisis of on-call physician coverage has been significantly reduced and hospitalists emerge as one of the major reasons why. Although there are still issues related to the availability of on-call specialists and surgeons, hospitals that have implemented hospital medicine programs are able to make available experienced general internists to triage, admit, and treat unassigned patients.
Hospital Medicine Programs:
A Value Added Resource to Hospitals
Hospital medicine programs are characterized by several unique features that facilitate the treatment of unassigned patients and result in significant benefits for hospitals. Figure 1 above illustrates these relationships.
Mark Aronson, MD, serves as a member of the Department of Medicine at Beth Israel Deaconess Medical Center (BIDMC), a 5O0-bed academic medical center in Boston and is also Vice Chairman for Quality and Professor of Medicine at Harvard Medical School. BIDMC has a mature hospital medicine program, and approximately 55-60% of the program's patients are unassigned, representing more than 25% of the hospital's general medicine census. Aronson believes that the hospital medicine program provides value to both patients and the institution. He described a case in which a nursing home patient without health insurance presented in the ED. After the initial evaluation, the ED attending decided to admit the patient. One of the hospitalists recognized the patient as someone he had treated several times before. He knew that her medical condition would not require hospitalization and arranged the appropriate treatment, allowing for transfer back to the nursing home. “In this situation, because the hospitalist had a relationship and history with the unassigned patient, the patient received timely, quality medical care and the hospital saved a significant amount of money” (5).
In the ED, the prompt and efficient treatment of unassigned patients can reduce backlogs and minimize hassles for emergency physicians. There is no need for the emergency physician to track down an on-call physician to admit the patient. The ED maintains a better work flow and makes better use of their resources, especially of physician and nursing time as well as space. Most hospitalists are familiar with pertinent laws (e.g., EMTALA) and insurance company policies, thereby spending less time investigating and resolving problems. The hospitals benefits through improved throughput.
"We have a high-volume ED with a large percentage of unassigned patients. In addition our hospital census is often 120% at midday and 90% at midnight. Efficient flow of patients though the ED at all hours is a critical issue at our hospital," says Patrick Cawley, MD, Director of Hospitalist Services at the Medical University of South Carolina in Charleston. "We have been asked to lead throughput initiatives which have resulted in a dramatic reduction in backlogs and the movement of patients out of the ED either to a bed or possibly to an alternative setting.”
The members of the medical staff of a hospital are often the driving force for the creation of a hospital medicine program. Having hopitalists at their institution may mean that affiliated physicians do not have to assume the undesirable responsibilities of participating in an on-call schedule. Furthermore, since hospitalists typically do not have an office practice, community physicians still have the opportunity to care for the unassigned patients once they are discharged, thereby building their practice. Hospitals can refer the patients according to an equitable schedule approved by the medical staff. By addressing issues related to on-call physician coverage, a hospital can improve medical staff relations.
At Winchester Medical Center in Virginia, family practitioners in the area surrendered their admitting privileges, creating an onerous call schedule for generalist internists. The hospital hired four hospitalists to admit and treat all unassigned patients. Instead of taking call, the internists are part of a primary care roster and rotate responsibility for unassigned patients once they are discharged (6). It has been a win-win solution for the hospital and the medical staff.
Often the unassigned patients have significant discharge planning and placement problems, especially those that are uninsured. While these issues can be daunting to the office-based physicians, hospitalists usually have a more comprehensive knowledge of the resources of the hospital and the community to help solve these placement and post-discharge care issues.
In treating unassigned patients, hospitalists blend their clinical skills with knowledge of their hospital’s objectives, concerns, policies, and procedures. Since they are a relatively small, cohesive group within the institution, hospitalists are often familiar with practice guidelines, medical records documentation requirements, computerized physician order entry (CPOE) systems, quality initiatives, and utilization management requirements.
"The hospitalists’ responsibilities in our program must have a good citizenship component," says Winthrop Whitcomb, MD, Director of the Inpatient Medicine Service at Merry Medical Center in Springfield, MA and co-founder of the Society of Hospital Medicine (SHM). "Each physician must serve on a committee, a project, or a program that serves the hospital. Hospitalists are often the leaders of hospital-wide initiatives directed at quality of care, utilization management, and throughput.”
Stakeholder Analysis
By treating unassigned patients, hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Assigning Value to Hospitalists' Work
Hospitalists typically manage unassigned and uninsured patients as part of their regular job duties. It is important that the administrator or leader of the hospital medicine group have a budgetary understanding of how to "score" the services that the hospitalists provide to these patients.
If the hospitalist service is provided by an independent, contracted group, they may be paid for treating the unassigned, uninsured patients. Often the payment is in the form of a case rate, based on the "average" number of services provided in an admission and using a Medicare or other mutually agreed upon fee schedule.
If the hospitalists are employees of the hospital, it is expected that they will assume responsibility for unassigned, uninsured patients. Although the hospital medicine group will not receive direct reimbursement for seeing these patients (unlike a contracted hospitalist group), the value of this service to the hospital must be recognized. In these situations, hospital administrators should acknowledge the critical need to credit the hospitalists for real work that must be performed but that generates little or no revenue. An equivalent case rate can be credited as a paper transaction to the hospitalist group to address the value of these services.
Conclusion
Given the current economic environment, the issue of treating unassigned and uninsured patients will not soon diminish. Demand is likely to increase with the nationwide growth in the number of uninsured patients. Physician resistance to call coverage and the rise of malpractice premiums will continue to create more pressure for hospitals to find solutions to this crisis. "We recognize that hospitalists are only part of the solution," says Ron Angus, MS, Past President of SHM. "Hospitals and government agencies must provide funding to cover the costs of inpatient care for acutely ill, uninsured - and usually unassigned - patients. Hospitals must also find ways to ensure that other specialists are available to hospitalists for acutely ill inpatients who require specialty expertise or procedures. With such cooperation and participation, hospitalists can be an important part of the solution to the problems now reaching crisis proportions in American emergency rooms" (7).
References
- Appleby J. Hospitals plagued by on-call shortage. USA Today June 16. 1999.
- Blaming the docs: patient dumping probes see physicians as culprits in turning away indigent from ERs. Modern Healthcare August 9, 1999.
- Winston K, The Advisory Board Company, Clinical Initiatives Center. Cause for concern: ensuring adequate and timely on-call physician coverage in the emergency department. ED Watch Issue #4, May 2, 2000.
- Foubister V. Is there a dearth of specialists in the ED? American Medical News July 12, 1999.
- Wanted: doctors willing to take ER call. ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, November 2001.
- Aronson M, Beth Israel Deaconess Medical Center. Personal interview. December 2004.
- Angus R, letter to the editor, ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, December 2001.
In the 1970s and 1980s, indigent patients experienced problems at hospital Emergency Departments (EDs) around the country. They were refused care and shuttled to other facilities for services. To protect patients against these types of abuses, Congress passed The Emergency Medical Treatment and Labor Act (EMTALA) in 1986 as part of the Consolidated Omnibus Budget Reconciliation Act (COBRA).·
EMTALA mandates that all patients presenting to the ED - regardless of insurance status - receive a medical screening examination and be medically stable prior to transfer to another facility. If a hospital has the facilities to treat the emergency, the patient can not be transferred to another ED. To address these requirements, every hospital must have physicians on call to assist emergency physicians in assessing and treating unassigned patients.
By the late 1990s, as EMTALA requirements took hold, inadequate on-call physician coverage reached crisis proportions and became a front page issue. In 1999, USA Today carried the following headline: "A Care Crisis in ERs: Nation's Hospitals Plagued by Shortage of On-Call Specialists" (1). In that same year, Modem Healthcare ran an article with the following headline: "Blaming the Docs: Patient Dumping Probes See Physicians as Culprits in Turning Away Indigent from ERs" (2). In California, a task force was formed to address the matter (3), and the American Medical Association (AMA) began exploring solutions at the highest levels (4).
Why do hospitals have problems organizing their medical staff to be available to provide on-call treatment of unassigned patients in the ED and subsequent to admission? There appear to be three major reasons for this problem.
First, at a minimum, on-call treatment of unassigned patients creates an inconvenience for physicians, taking away from their personal time; worse. it can reduce the number of available hours they have to spend with their office-based patients.
Second, there are financial disincentives to on-call coverage. Often unassigned patients presenting in the ED are uninsured or under-insured. On-call physicians frequently do not receive adequate compensation for the task of treating these patients.
Finally, on-call duty can bring bureaucratic hassles and/or legal liability for physicians. Dealing with state Medicaid agencies may require addressing administrative requirements, completing paperwork, and paying penalties for not following the rules.
Richard Frankenstein, MD, a pulmonologist in Southern California, admitted an uninsured patient with multiple chronic illnesses when he was the on-call physician at one of his affiliated hospitals. The patient spent 8 weeks in the hospital, much of that time in intensive care. Frankenstein often visited this patient twice a day, so his already busy schedule began hour earlier and ended 1 hour later. He received no compensation for these efforts. That commitment dragged me away from my primary responsibilities,” said Frankenstein. "I'm no longer on staff there, and that situation was a major reason that I resigned (5).
During the past 5 years, the crisis of on-call physician coverage has been significantly reduced and hospitalists emerge as one of the major reasons why. Although there are still issues related to the availability of on-call specialists and surgeons, hospitals that have implemented hospital medicine programs are able to make available experienced general internists to triage, admit, and treat unassigned patients.
Hospital Medicine Programs:
A Value Added Resource to Hospitals
Hospital medicine programs are characterized by several unique features that facilitate the treatment of unassigned patients and result in significant benefits for hospitals. Figure 1 above illustrates these relationships.
Mark Aronson, MD, serves as a member of the Department of Medicine at Beth Israel Deaconess Medical Center (BIDMC), a 5O0-bed academic medical center in Boston and is also Vice Chairman for Quality and Professor of Medicine at Harvard Medical School. BIDMC has a mature hospital medicine program, and approximately 55-60% of the program's patients are unassigned, representing more than 25% of the hospital's general medicine census. Aronson believes that the hospital medicine program provides value to both patients and the institution. He described a case in which a nursing home patient without health insurance presented in the ED. After the initial evaluation, the ED attending decided to admit the patient. One of the hospitalists recognized the patient as someone he had treated several times before. He knew that her medical condition would not require hospitalization and arranged the appropriate treatment, allowing for transfer back to the nursing home. “In this situation, because the hospitalist had a relationship and history with the unassigned patient, the patient received timely, quality medical care and the hospital saved a significant amount of money” (5).
In the ED, the prompt and efficient treatment of unassigned patients can reduce backlogs and minimize hassles for emergency physicians. There is no need for the emergency physician to track down an on-call physician to admit the patient. The ED maintains a better work flow and makes better use of their resources, especially of physician and nursing time as well as space. Most hospitalists are familiar with pertinent laws (e.g., EMTALA) and insurance company policies, thereby spending less time investigating and resolving problems. The hospitals benefits through improved throughput.
"We have a high-volume ED with a large percentage of unassigned patients. In addition our hospital census is often 120% at midday and 90% at midnight. Efficient flow of patients though the ED at all hours is a critical issue at our hospital," says Patrick Cawley, MD, Director of Hospitalist Services at the Medical University of South Carolina in Charleston. "We have been asked to lead throughput initiatives which have resulted in a dramatic reduction in backlogs and the movement of patients out of the ED either to a bed or possibly to an alternative setting.”
The members of the medical staff of a hospital are often the driving force for the creation of a hospital medicine program. Having hopitalists at their institution may mean that affiliated physicians do not have to assume the undesirable responsibilities of participating in an on-call schedule. Furthermore, since hospitalists typically do not have an office practice, community physicians still have the opportunity to care for the unassigned patients once they are discharged, thereby building their practice. Hospitals can refer the patients according to an equitable schedule approved by the medical staff. By addressing issues related to on-call physician coverage, a hospital can improve medical staff relations.
At Winchester Medical Center in Virginia, family practitioners in the area surrendered their admitting privileges, creating an onerous call schedule for generalist internists. The hospital hired four hospitalists to admit and treat all unassigned patients. Instead of taking call, the internists are part of a primary care roster and rotate responsibility for unassigned patients once they are discharged (6). It has been a win-win solution for the hospital and the medical staff.
Often the unassigned patients have significant discharge planning and placement problems, especially those that are uninsured. While these issues can be daunting to the office-based physicians, hospitalists usually have a more comprehensive knowledge of the resources of the hospital and the community to help solve these placement and post-discharge care issues.
In treating unassigned patients, hospitalists blend their clinical skills with knowledge of their hospital’s objectives, concerns, policies, and procedures. Since they are a relatively small, cohesive group within the institution, hospitalists are often familiar with practice guidelines, medical records documentation requirements, computerized physician order entry (CPOE) systems, quality initiatives, and utilization management requirements.
"The hospitalists’ responsibilities in our program must have a good citizenship component," says Winthrop Whitcomb, MD, Director of the Inpatient Medicine Service at Merry Medical Center in Springfield, MA and co-founder of the Society of Hospital Medicine (SHM). "Each physician must serve on a committee, a project, or a program that serves the hospital. Hospitalists are often the leaders of hospital-wide initiatives directed at quality of care, utilization management, and throughput.”
Stakeholder Analysis
By treating unassigned patients, hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. The benefits to these stakeholders are summarized in Table 1.
Assigning Value to Hospitalists' Work
Hospitalists typically manage unassigned and uninsured patients as part of their regular job duties. It is important that the administrator or leader of the hospital medicine group have a budgetary understanding of how to "score" the services that the hospitalists provide to these patients.
If the hospitalist service is provided by an independent, contracted group, they may be paid for treating the unassigned, uninsured patients. Often the payment is in the form of a case rate, based on the "average" number of services provided in an admission and using a Medicare or other mutually agreed upon fee schedule.
If the hospitalists are employees of the hospital, it is expected that they will assume responsibility for unassigned, uninsured patients. Although the hospital medicine group will not receive direct reimbursement for seeing these patients (unlike a contracted hospitalist group), the value of this service to the hospital must be recognized. In these situations, hospital administrators should acknowledge the critical need to credit the hospitalists for real work that must be performed but that generates little or no revenue. An equivalent case rate can be credited as a paper transaction to the hospitalist group to address the value of these services.
Conclusion
Given the current economic environment, the issue of treating unassigned and uninsured patients will not soon diminish. Demand is likely to increase with the nationwide growth in the number of uninsured patients. Physician resistance to call coverage and the rise of malpractice premiums will continue to create more pressure for hospitals to find solutions to this crisis. "We recognize that hospitalists are only part of the solution," says Ron Angus, MS, Past President of SHM. "Hospitals and government agencies must provide funding to cover the costs of inpatient care for acutely ill, uninsured - and usually unassigned - patients. Hospitals must also find ways to ensure that other specialists are available to hospitalists for acutely ill inpatients who require specialty expertise or procedures. With such cooperation and participation, hospitalists can be an important part of the solution to the problems now reaching crisis proportions in American emergency rooms" (7).
References
- Appleby J. Hospitals plagued by on-call shortage. USA Today June 16. 1999.
- Blaming the docs: patient dumping probes see physicians as culprits in turning away indigent from ERs. Modern Healthcare August 9, 1999.
- Winston K, The Advisory Board Company, Clinical Initiatives Center. Cause for concern: ensuring adequate and timely on-call physician coverage in the emergency department. ED Watch Issue #4, May 2, 2000.
- Foubister V. Is there a dearth of specialists in the ED? American Medical News July 12, 1999.
- Wanted: doctors willing to take ER call. ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, November 2001.
- Aronson M, Beth Israel Deaconess Medical Center. Personal interview. December 2004.
- Angus R, letter to the editor, ACP-ASIM Observer American College of Physicians-American Society of Internal Medicine, December 2001.