User login
Richard Pizzi is editor of The Hospitalist. He has been an editor at Frontline Medical Communications since 2015, and previously served as editor of MDedge publications Hospitalist News and ID Practitioner. He has also worked as an editor and in editorial management roles for HIMSS Media, MedTech Media, and the American Association for Clinical Chemistry. Follow him on Twitter @richpizzi
HIV research update: Early July 2016
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Patients who are stable on antiretroviral therapy should be offered a less intensive care package that can lead to improved outcomes while saving resources, including less frequent clinic visits, out-of-clinic drug refills, and reduced laboratory monitoring, according to an analysis by the World Health Organization.
Short-cycle antiretroviral therapy is a viable option for adherent HIV-infected young people who are stable on efavirenz-based ART, according to a study in the Lancet HIV.
In a Thai study of HIV-infected patients treated for GI tract inflammation during acute infection, most restored their immune activation back to baseline levels after 24 weeks of combination antiretroviral therapy, although most acutely infected patients did not restore their CD4+ T cells after 96 weeks of cART.
Second-line antiretroviral therapy treatment failure in a South African clinic was related to adherence, but could be overcome with careful support, investigators found. However, they said controlled interventions are needed to determine what the optimal approach is to improving second-line outcomes and reducing the need for third-line ART.
Only a moderate antibody response to a single H1N1pdm09 AS03-adjuvanted influenza vaccine was detected in a large cohort study of HIV-infected patients with high baseline H1N1 seroprotective titers. The use of booster vaccinations is warranted in order to achieve higher immunogenicity in this population, researchers said.
A longer time with diagnosed HIV infection, rather than age, is the dominating factor contributing to psychological morbidity and lower quality of life in patients, according to a study of HIV-positive adults.
A British study found that, in settings with low tuberculosis prevalence, early start of combined antiretroviral therapy and intensified TB case finding protocols may significantly reduce the incidence of TB in HIV-infected patients.
Despite significant improvements in antiretroviral therapy prescription and viral suppression in recent years in the United States, racial and ethnic disparities persist, particularly for black persons, according to an analysis of Medical Monitoring Project data.
The investigational malaria vaccine RTS, S/AS01 was well tolerated when given to children with WHO clinical stage 1 or 2 HIV disease along with high antiretroviral and co-trimoxazole use. Investigators said children with HIV disease could be included in future RTS,S/AS01 vaccination programs.
A special supplement to the journal AIDS Care, on the psychological and sociomedical aspects of AIDS/HIV in children, is available open access to all interested.
The association of the HIV p24 antigen with blood donation was highly significant and poses a great risk to recipients if screening of blood donors is only carried out by HIV antibody detection, according to a Nigerian study.
Resistance mutations against nucleos(t)ide reverse transcriptase inhibitors antagonized the development of HIV-1 resistance against the integrase strand transfer inhibitor dolutegravir, but not against the INSTIs raltegravir or elvitegravir, a study found.
Resistance to protease inhibitors was detected in 22% of HIV-infected patients with viral loads greater than or equal to 1000 cps/mL, in a study of second-line antiretroviral therapy in Sub-Saharan Africa. Researchers said intensified support for adherence, viral load and drug resistance testing, and third-line drugs would be necessary to ensure long-term ART success in the region.
A study in JAIDS found that adding HIV testing at birth has the potential to improve the number and timing of antiretroviral therapy initiation of HIV-infected infants, leading to a decrease in infant mortality.
The effects of HIV and childhood trauma remained evident at 12-month follow-up in HIV-infected women, despite greater uptake of antiretroviral therapy and improved HIV disease status, according to a study in AIDS Care.
HIV patients with hyperglycemia have severe dyslipidemia and immune activation, a retrospective study revealed, and highly active antiretroviral therapy is an important impact factor of glucose and lipid metabolic disorders.
The prevalence of non-albicans Candida spp. is high among HIV-infected individuals with low CD4 count, placing them at higher risk of invasive infections, according to a study in the International Journal of Infectious Diseases.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Patients who are stable on antiretroviral therapy should be offered a less intensive care package that can lead to improved outcomes while saving resources, including less frequent clinic visits, out-of-clinic drug refills, and reduced laboratory monitoring, according to an analysis by the World Health Organization.
Short-cycle antiretroviral therapy is a viable option for adherent HIV-infected young people who are stable on efavirenz-based ART, according to a study in the Lancet HIV.
In a Thai study of HIV-infected patients treated for GI tract inflammation during acute infection, most restored their immune activation back to baseline levels after 24 weeks of combination antiretroviral therapy, although most acutely infected patients did not restore their CD4+ T cells after 96 weeks of cART.
Second-line antiretroviral therapy treatment failure in a South African clinic was related to adherence, but could be overcome with careful support, investigators found. However, they said controlled interventions are needed to determine what the optimal approach is to improving second-line outcomes and reducing the need for third-line ART.
Only a moderate antibody response to a single H1N1pdm09 AS03-adjuvanted influenza vaccine was detected in a large cohort study of HIV-infected patients with high baseline H1N1 seroprotective titers. The use of booster vaccinations is warranted in order to achieve higher immunogenicity in this population, researchers said.
A longer time with diagnosed HIV infection, rather than age, is the dominating factor contributing to psychological morbidity and lower quality of life in patients, according to a study of HIV-positive adults.
A British study found that, in settings with low tuberculosis prevalence, early start of combined antiretroviral therapy and intensified TB case finding protocols may significantly reduce the incidence of TB in HIV-infected patients.
Despite significant improvements in antiretroviral therapy prescription and viral suppression in recent years in the United States, racial and ethnic disparities persist, particularly for black persons, according to an analysis of Medical Monitoring Project data.
The investigational malaria vaccine RTS, S/AS01 was well tolerated when given to children with WHO clinical stage 1 or 2 HIV disease along with high antiretroviral and co-trimoxazole use. Investigators said children with HIV disease could be included in future RTS,S/AS01 vaccination programs.
A special supplement to the journal AIDS Care, on the psychological and sociomedical aspects of AIDS/HIV in children, is available open access to all interested.
The association of the HIV p24 antigen with blood donation was highly significant and poses a great risk to recipients if screening of blood donors is only carried out by HIV antibody detection, according to a Nigerian study.
Resistance mutations against nucleos(t)ide reverse transcriptase inhibitors antagonized the development of HIV-1 resistance against the integrase strand transfer inhibitor dolutegravir, but not against the INSTIs raltegravir or elvitegravir, a study found.
Resistance to protease inhibitors was detected in 22% of HIV-infected patients with viral loads greater than or equal to 1000 cps/mL, in a study of second-line antiretroviral therapy in Sub-Saharan Africa. Researchers said intensified support for adherence, viral load and drug resistance testing, and third-line drugs would be necessary to ensure long-term ART success in the region.
A study in JAIDS found that adding HIV testing at birth has the potential to improve the number and timing of antiretroviral therapy initiation of HIV-infected infants, leading to a decrease in infant mortality.
The effects of HIV and childhood trauma remained evident at 12-month follow-up in HIV-infected women, despite greater uptake of antiretroviral therapy and improved HIV disease status, according to a study in AIDS Care.
HIV patients with hyperglycemia have severe dyslipidemia and immune activation, a retrospective study revealed, and highly active antiretroviral therapy is an important impact factor of glucose and lipid metabolic disorders.
The prevalence of non-albicans Candida spp. is high among HIV-infected individuals with low CD4 count, placing them at higher risk of invasive infections, according to a study in the International Journal of Infectious Diseases.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Patients who are stable on antiretroviral therapy should be offered a less intensive care package that can lead to improved outcomes while saving resources, including less frequent clinic visits, out-of-clinic drug refills, and reduced laboratory monitoring, according to an analysis by the World Health Organization.
Short-cycle antiretroviral therapy is a viable option for adherent HIV-infected young people who are stable on efavirenz-based ART, according to a study in the Lancet HIV.
In a Thai study of HIV-infected patients treated for GI tract inflammation during acute infection, most restored their immune activation back to baseline levels after 24 weeks of combination antiretroviral therapy, although most acutely infected patients did not restore their CD4+ T cells after 96 weeks of cART.
Second-line antiretroviral therapy treatment failure in a South African clinic was related to adherence, but could be overcome with careful support, investigators found. However, they said controlled interventions are needed to determine what the optimal approach is to improving second-line outcomes and reducing the need for third-line ART.
Only a moderate antibody response to a single H1N1pdm09 AS03-adjuvanted influenza vaccine was detected in a large cohort study of HIV-infected patients with high baseline H1N1 seroprotective titers. The use of booster vaccinations is warranted in order to achieve higher immunogenicity in this population, researchers said.
A longer time with diagnosed HIV infection, rather than age, is the dominating factor contributing to psychological morbidity and lower quality of life in patients, according to a study of HIV-positive adults.
A British study found that, in settings with low tuberculosis prevalence, early start of combined antiretroviral therapy and intensified TB case finding protocols may significantly reduce the incidence of TB in HIV-infected patients.
Despite significant improvements in antiretroviral therapy prescription and viral suppression in recent years in the United States, racial and ethnic disparities persist, particularly for black persons, according to an analysis of Medical Monitoring Project data.
The investigational malaria vaccine RTS, S/AS01 was well tolerated when given to children with WHO clinical stage 1 or 2 HIV disease along with high antiretroviral and co-trimoxazole use. Investigators said children with HIV disease could be included in future RTS,S/AS01 vaccination programs.
A special supplement to the journal AIDS Care, on the psychological and sociomedical aspects of AIDS/HIV in children, is available open access to all interested.
The association of the HIV p24 antigen with blood donation was highly significant and poses a great risk to recipients if screening of blood donors is only carried out by HIV antibody detection, according to a Nigerian study.
Resistance mutations against nucleos(t)ide reverse transcriptase inhibitors antagonized the development of HIV-1 resistance against the integrase strand transfer inhibitor dolutegravir, but not against the INSTIs raltegravir or elvitegravir, a study found.
Resistance to protease inhibitors was detected in 22% of HIV-infected patients with viral loads greater than or equal to 1000 cps/mL, in a study of second-line antiretroviral therapy in Sub-Saharan Africa. Researchers said intensified support for adherence, viral load and drug resistance testing, and third-line drugs would be necessary to ensure long-term ART success in the region.
A study in JAIDS found that adding HIV testing at birth has the potential to improve the number and timing of antiretroviral therapy initiation of HIV-infected infants, leading to a decrease in infant mortality.
The effects of HIV and childhood trauma remained evident at 12-month follow-up in HIV-infected women, despite greater uptake of antiretroviral therapy and improved HIV disease status, according to a study in AIDS Care.
HIV patients with hyperglycemia have severe dyslipidemia and immune activation, a retrospective study revealed, and highly active antiretroviral therapy is an important impact factor of glucose and lipid metabolic disorders.
The prevalence of non-albicans Candida spp. is high among HIV-infected individuals with low CD4 count, placing them at higher risk of invasive infections, according to a study in the International Journal of Infectious Diseases.
On Twitter @richpizzi
Global HIV/AIDS mortality declines, but infection rate is unimproved
HIV/AIDS mortality has been declining at a steady pace since 2005, but the annual rate of new infections has remained relatively constant in that same period, according to a study published July 19 in the Lancet HIV.
The analysis, based on data from the Global Burden of Disease 2015 study, provides national estimates of levels and trends of HIV/AIDS incidence, prevalence, coverage of antiretroviral therapy (ART), and mortality for 195 countries and territories from 1980 to 2015. The authors, led by Haidong Wang, PhD, of the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, used the Estimation and Projection Package and Spectrum software originally developed by the Joint United Nations Programme on HIV/AIDS (UNAIDS) to make their estimates.
Dr. Wang and his coauthors revealed that HIV/AIDS mortality declined from a peak of 1.8 million deaths in 2005, to 1.2 million deaths in 2015. However, they noted that the annual incidence of global HIV/AIDS has stayed relatively constant at about 2.6 million per year (range, 2.5 to 2.8 million) since 2005. The number of people living with HIV/AIDS has been steadily increasing and reached 38.8 million in 2015, thanks in great measure to the scale-up of ART and the prevention of mother-to-child transmission, the coauthors said.
The proportion of people living with HIV on ART increased rapidly between 2005 and 2015, from 6.4% to 38.6% for men, and from 3.3% to 42.4% for women, but Dr. Wang and his colleagues said most countries are still far from achieving the UNAIDS 90-90-90 target of 81% by 2020.
Read the full study in the Lancet HIV (doi:10. 1016/S2352-3018[16]30087-X).
On Twitter @richpizzi
HIV/AIDS mortality has been declining at a steady pace since 2005, but the annual rate of new infections has remained relatively constant in that same period, according to a study published July 19 in the Lancet HIV.
The analysis, based on data from the Global Burden of Disease 2015 study, provides national estimates of levels and trends of HIV/AIDS incidence, prevalence, coverage of antiretroviral therapy (ART), and mortality for 195 countries and territories from 1980 to 2015. The authors, led by Haidong Wang, PhD, of the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, used the Estimation and Projection Package and Spectrum software originally developed by the Joint United Nations Programme on HIV/AIDS (UNAIDS) to make their estimates.
Dr. Wang and his coauthors revealed that HIV/AIDS mortality declined from a peak of 1.8 million deaths in 2005, to 1.2 million deaths in 2015. However, they noted that the annual incidence of global HIV/AIDS has stayed relatively constant at about 2.6 million per year (range, 2.5 to 2.8 million) since 2005. The number of people living with HIV/AIDS has been steadily increasing and reached 38.8 million in 2015, thanks in great measure to the scale-up of ART and the prevention of mother-to-child transmission, the coauthors said.
The proportion of people living with HIV on ART increased rapidly between 2005 and 2015, from 6.4% to 38.6% for men, and from 3.3% to 42.4% for women, but Dr. Wang and his colleagues said most countries are still far from achieving the UNAIDS 90-90-90 target of 81% by 2020.
Read the full study in the Lancet HIV (doi:10. 1016/S2352-3018[16]30087-X).
On Twitter @richpizzi
HIV/AIDS mortality has been declining at a steady pace since 2005, but the annual rate of new infections has remained relatively constant in that same period, according to a study published July 19 in the Lancet HIV.
The analysis, based on data from the Global Burden of Disease 2015 study, provides national estimates of levels and trends of HIV/AIDS incidence, prevalence, coverage of antiretroviral therapy (ART), and mortality for 195 countries and territories from 1980 to 2015. The authors, led by Haidong Wang, PhD, of the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, used the Estimation and Projection Package and Spectrum software originally developed by the Joint United Nations Programme on HIV/AIDS (UNAIDS) to make their estimates.
Dr. Wang and his coauthors revealed that HIV/AIDS mortality declined from a peak of 1.8 million deaths in 2005, to 1.2 million deaths in 2015. However, they noted that the annual incidence of global HIV/AIDS has stayed relatively constant at about 2.6 million per year (range, 2.5 to 2.8 million) since 2005. The number of people living with HIV/AIDS has been steadily increasing and reached 38.8 million in 2015, thanks in great measure to the scale-up of ART and the prevention of mother-to-child transmission, the coauthors said.
The proportion of people living with HIV on ART increased rapidly between 2005 and 2015, from 6.4% to 38.6% for men, and from 3.3% to 42.4% for women, but Dr. Wang and his colleagues said most countries are still far from achieving the UNAIDS 90-90-90 target of 81% by 2020.
Read the full study in the Lancet HIV (doi:10. 1016/S2352-3018[16]30087-X).
On Twitter @richpizzi
FROM THE LANCET HIV
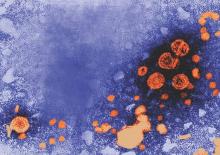
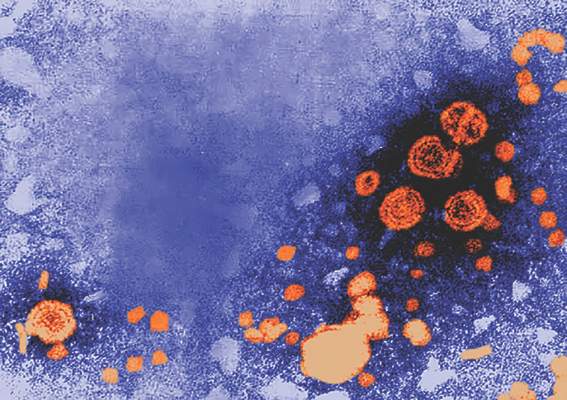
Ebola research update: June 2016
The struggle to defeat Ebola virus disease continues globally, although it may not always make the headlines. To catch up on what you may have missed, here are some notable news items and journal articles published over the past few weeks that are worth a second look.
The World Health Organization declared the end of Ebola virus transmission in the Republic of Guinea on June 1, 2016. The country has entered a 90-day period of heightened surveillance to ensure that any new cases are identified quickly before they can spread to other people.
Ebola virus remained infectious for more than 30 days in human blood spotted onto Sierra Leonean banknotes and in syringe needles under hospital and environmental conditions, according to research published in the Journal of Infectious Diseases. The authors said this indicates that Ebola virus–contaminated items may pose a serious risk to humans.
The Defense Threat Reduction Agency (DTRA) has awarded a 1-year, $3.4 million contract award to Southwest Research Institute and collaborator Texas Biomedical Research Institute to combine two available medications and test the resulting combination drug therapy against the Ebola virus.
The Idylla Ebola Virus Triage Test, distributed by Janssen Pharmaceutica NV, was granted Emergency Use Authorization by the Food and Drug Administration. The test is a diagnostic that detects the presence of the Ebola Zaire virus in patients with signs and symptoms of Ebola virus disease and was jointly developed by Janssen Diagnostics, a division of Janssen Pharmaceutica, Biocartis NV, and the Belgium Institute of Tropical Medicine.
A study by researchers at the University of Texas found lethal models of disease for Bundibugyo, Sudan, and Zaire species of Ebolavirus in the domestic ferret using wild type nonadapted viruses. The authors said this is the only known small animal model developed for Bundibugyo and the only uniformly lethal animal model for Bundibugyo.
Trophoblast infection may be a mechanism of transplacental ebolavirus transmission, according to research published in the Journal of Infectious Diseases.
A majority of participants in a survey conducted after approximately 15 months of an Ebola epidemic in Sierra Leone expressed at least some confidence in the health care system’s ability to treat patients suspected to have Ebola. Respondents from areas with active Ebola transmission had higher confidence in the health care system, as did respondents with higher education levels.
Persons who died of Ebola virus disease at home in rural communities in Liberia and Guinea resulted in more secondary infections than persons admitted to Ebola treatment units, according to a report in Emerging Infectious Diseases. The authors said intensified monitoring of contacts of persons who died of EVD in the community is an evidence-based approach to reduce virus transmission in rural communities.
The World Health Organization declared the end of the most recent outbreak of Ebola virus disease in Liberia on June 9, 2016. The announcement came 42 days after the last confirmed Ebola patient in Liberia tested negative for the disease for the second time. Liberia now enters a 90-day period of heightened surveillance to ensure that any new cases are identified quickly and contained before spreading.
The Ebola virus may be even more widespread than previously suspected, according to a study in Mammal Review. Researchers said the most favorable area for the Ebola virus is significantly associated with the presence of the virus in nonhuman mammals, and their model suggested additional favorable areas are found throughout the coastal areas of West and Central Africa.
Sexual transmission of the Ebola virus can have large effects on epidemic dynamics, according to a study in Biology Letters. The authors say these effects can increase attack ratios from 25% in scenarios without sexual transmission, but with contact-transmission-reducing behavior, up to 80% in equivalent scenarios with sexual transmission.
A retrospective study of Ebola virus disease patients in Sierra Leone found that significant predictors for patient death were shorter time from symptom onset to admission, male sex, high viral load on initial laboratory testing, severe pain, diarrhea, bloody feces, and development of other bleeding manifestations during hospitalization. The authors noted that these risk factors for death could be used to identify patients in need of more intensive medical support.
Parenteral or aerosol routes of Ebola virus exposure in nonhuman primates required higher doses of the virus to produce disease, according to a recent study.
An epidemiological study of 139 laboratory-confirmed Ebola virus disease patients in western Sierra Leone between November 2014 and January 2015 found that mortality of EVD is associated with an older age, fever, and probably hiccups.
A study in the International Journal of Infectious Diseases suggests that the experience of three mass gathering events in Africa during the Ebola epidemic illustrates that such events can be held safely, provided that countries put measures in place for enhanced surveillance and response systems for communicable diseases.
A study in the Journal of Infectious Diseases compared the Ebola virus epidemic in 1976 to the 2013-2016 epidemic, and identified key scientific approaches used in 1976 and their relevance to the 3-country (Guinea, Sierra Leone, and Liberia) West African epidemic.
On Twitter @richpizzi
The struggle to defeat Ebola virus disease continues globally, although it may not always make the headlines. To catch up on what you may have missed, here are some notable news items and journal articles published over the past few weeks that are worth a second look.
The World Health Organization declared the end of Ebola virus transmission in the Republic of Guinea on June 1, 2016. The country has entered a 90-day period of heightened surveillance to ensure that any new cases are identified quickly before they can spread to other people.
Ebola virus remained infectious for more than 30 days in human blood spotted onto Sierra Leonean banknotes and in syringe needles under hospital and environmental conditions, according to research published in the Journal of Infectious Diseases. The authors said this indicates that Ebola virus–contaminated items may pose a serious risk to humans.
The Defense Threat Reduction Agency (DTRA) has awarded a 1-year, $3.4 million contract award to Southwest Research Institute and collaborator Texas Biomedical Research Institute to combine two available medications and test the resulting combination drug therapy against the Ebola virus.
The Idylla Ebola Virus Triage Test, distributed by Janssen Pharmaceutica NV, was granted Emergency Use Authorization by the Food and Drug Administration. The test is a diagnostic that detects the presence of the Ebola Zaire virus in patients with signs and symptoms of Ebola virus disease and was jointly developed by Janssen Diagnostics, a division of Janssen Pharmaceutica, Biocartis NV, and the Belgium Institute of Tropical Medicine.
A study by researchers at the University of Texas found lethal models of disease for Bundibugyo, Sudan, and Zaire species of Ebolavirus in the domestic ferret using wild type nonadapted viruses. The authors said this is the only known small animal model developed for Bundibugyo and the only uniformly lethal animal model for Bundibugyo.
Trophoblast infection may be a mechanism of transplacental ebolavirus transmission, according to research published in the Journal of Infectious Diseases.
A majority of participants in a survey conducted after approximately 15 months of an Ebola epidemic in Sierra Leone expressed at least some confidence in the health care system’s ability to treat patients suspected to have Ebola. Respondents from areas with active Ebola transmission had higher confidence in the health care system, as did respondents with higher education levels.
Persons who died of Ebola virus disease at home in rural communities in Liberia and Guinea resulted in more secondary infections than persons admitted to Ebola treatment units, according to a report in Emerging Infectious Diseases. The authors said intensified monitoring of contacts of persons who died of EVD in the community is an evidence-based approach to reduce virus transmission in rural communities.
The World Health Organization declared the end of the most recent outbreak of Ebola virus disease in Liberia on June 9, 2016. The announcement came 42 days after the last confirmed Ebola patient in Liberia tested negative for the disease for the second time. Liberia now enters a 90-day period of heightened surveillance to ensure that any new cases are identified quickly and contained before spreading.
The Ebola virus may be even more widespread than previously suspected, according to a study in Mammal Review. Researchers said the most favorable area for the Ebola virus is significantly associated with the presence of the virus in nonhuman mammals, and their model suggested additional favorable areas are found throughout the coastal areas of West and Central Africa.
Sexual transmission of the Ebola virus can have large effects on epidemic dynamics, according to a study in Biology Letters. The authors say these effects can increase attack ratios from 25% in scenarios without sexual transmission, but with contact-transmission-reducing behavior, up to 80% in equivalent scenarios with sexual transmission.
A retrospective study of Ebola virus disease patients in Sierra Leone found that significant predictors for patient death were shorter time from symptom onset to admission, male sex, high viral load on initial laboratory testing, severe pain, diarrhea, bloody feces, and development of other bleeding manifestations during hospitalization. The authors noted that these risk factors for death could be used to identify patients in need of more intensive medical support.
Parenteral or aerosol routes of Ebola virus exposure in nonhuman primates required higher doses of the virus to produce disease, according to a recent study.
An epidemiological study of 139 laboratory-confirmed Ebola virus disease patients in western Sierra Leone between November 2014 and January 2015 found that mortality of EVD is associated with an older age, fever, and probably hiccups.
A study in the International Journal of Infectious Diseases suggests that the experience of three mass gathering events in Africa during the Ebola epidemic illustrates that such events can be held safely, provided that countries put measures in place for enhanced surveillance and response systems for communicable diseases.
A study in the Journal of Infectious Diseases compared the Ebola virus epidemic in 1976 to the 2013-2016 epidemic, and identified key scientific approaches used in 1976 and their relevance to the 3-country (Guinea, Sierra Leone, and Liberia) West African epidemic.
On Twitter @richpizzi
The struggle to defeat Ebola virus disease continues globally, although it may not always make the headlines. To catch up on what you may have missed, here are some notable news items and journal articles published over the past few weeks that are worth a second look.
The World Health Organization declared the end of Ebola virus transmission in the Republic of Guinea on June 1, 2016. The country has entered a 90-day period of heightened surveillance to ensure that any new cases are identified quickly before they can spread to other people.
Ebola virus remained infectious for more than 30 days in human blood spotted onto Sierra Leonean banknotes and in syringe needles under hospital and environmental conditions, according to research published in the Journal of Infectious Diseases. The authors said this indicates that Ebola virus–contaminated items may pose a serious risk to humans.
The Defense Threat Reduction Agency (DTRA) has awarded a 1-year, $3.4 million contract award to Southwest Research Institute and collaborator Texas Biomedical Research Institute to combine two available medications and test the resulting combination drug therapy against the Ebola virus.
The Idylla Ebola Virus Triage Test, distributed by Janssen Pharmaceutica NV, was granted Emergency Use Authorization by the Food and Drug Administration. The test is a diagnostic that detects the presence of the Ebola Zaire virus in patients with signs and symptoms of Ebola virus disease and was jointly developed by Janssen Diagnostics, a division of Janssen Pharmaceutica, Biocartis NV, and the Belgium Institute of Tropical Medicine.
A study by researchers at the University of Texas found lethal models of disease for Bundibugyo, Sudan, and Zaire species of Ebolavirus in the domestic ferret using wild type nonadapted viruses. The authors said this is the only known small animal model developed for Bundibugyo and the only uniformly lethal animal model for Bundibugyo.
Trophoblast infection may be a mechanism of transplacental ebolavirus transmission, according to research published in the Journal of Infectious Diseases.
A majority of participants in a survey conducted after approximately 15 months of an Ebola epidemic in Sierra Leone expressed at least some confidence in the health care system’s ability to treat patients suspected to have Ebola. Respondents from areas with active Ebola transmission had higher confidence in the health care system, as did respondents with higher education levels.
Persons who died of Ebola virus disease at home in rural communities in Liberia and Guinea resulted in more secondary infections than persons admitted to Ebola treatment units, according to a report in Emerging Infectious Diseases. The authors said intensified monitoring of contacts of persons who died of EVD in the community is an evidence-based approach to reduce virus transmission in rural communities.
The World Health Organization declared the end of the most recent outbreak of Ebola virus disease in Liberia on June 9, 2016. The announcement came 42 days after the last confirmed Ebola patient in Liberia tested negative for the disease for the second time. Liberia now enters a 90-day period of heightened surveillance to ensure that any new cases are identified quickly and contained before spreading.
The Ebola virus may be even more widespread than previously suspected, according to a study in Mammal Review. Researchers said the most favorable area for the Ebola virus is significantly associated with the presence of the virus in nonhuman mammals, and their model suggested additional favorable areas are found throughout the coastal areas of West and Central Africa.
Sexual transmission of the Ebola virus can have large effects on epidemic dynamics, according to a study in Biology Letters. The authors say these effects can increase attack ratios from 25% in scenarios without sexual transmission, but with contact-transmission-reducing behavior, up to 80% in equivalent scenarios with sexual transmission.
A retrospective study of Ebola virus disease patients in Sierra Leone found that significant predictors for patient death were shorter time from symptom onset to admission, male sex, high viral load on initial laboratory testing, severe pain, diarrhea, bloody feces, and development of other bleeding manifestations during hospitalization. The authors noted that these risk factors for death could be used to identify patients in need of more intensive medical support.
Parenteral or aerosol routes of Ebola virus exposure in nonhuman primates required higher doses of the virus to produce disease, according to a recent study.
An epidemiological study of 139 laboratory-confirmed Ebola virus disease patients in western Sierra Leone between November 2014 and January 2015 found that mortality of EVD is associated with an older age, fever, and probably hiccups.
A study in the International Journal of Infectious Diseases suggests that the experience of three mass gathering events in Africa during the Ebola epidemic illustrates that such events can be held safely, provided that countries put measures in place for enhanced surveillance and response systems for communicable diseases.
A study in the Journal of Infectious Diseases compared the Ebola virus epidemic in 1976 to the 2013-2016 epidemic, and identified key scientific approaches used in 1976 and their relevance to the 3-country (Guinea, Sierra Leone, and Liberia) West African epidemic.
On Twitter @richpizzi
HIV research update: Late June 2016
A great volume of HIV and AIDS research enters the medical literature every month. It can be challenging to monitor everything, so here’s a quick look at some notable news items and journal articles published in recent weeks.
Efforts to increase viral suppression among individuals who inject drugs should focus on increasing antiretroviral therapy initiation and improving adherence to therapy, according to a study in the journal AIDS.
Canadian investigators developed a flexible framework that characterized patient transitions among states of HIV clinical care and demonstrated that multistate models provide a useful approach to supplement “cascade of care” work.
Researchers found that, in the setting of HIV infection, the presence of detectable cardiac troponin was strongly associated with coronary plaque, particularly calcified plaque among an asymptomatic group.
A cohort study found that overall risk of cardiovascular events in HIV-positive patients was twice as high as CVE risk in general population. The authors also found a relative risk for CVE type-1 higher in HIV-positive females, and a higher CVE type-2 risk in male patients.
An Australian study found that HIV-infected people less likely to be using antiretroviral therapy were younger and had a more recent diagnosis of HIV.
A study in AIDS Care underscored the importance of developing culturally appropriate social norm-based HIV interventions among people living with HIV/AIDS (PLWHA) in China, as such interventions have the potential to reduce risk behaviors and to promote condom use among PLWHA.
The frequency of mitochondrial DNA variants (mutations and large-scale deletions) was higher in HIV-infected treatment-experienced patients with or without antiretroviral therapy–induced toxicity than in uninfected controls, according to a study in HIV Medicine.
Immediate antiretroviral therapy was associated with lower mortality and better growth for up to 5 years in children under age 10 years, according to research published in the International Journal of Epidemiology.
A genome-wide association study (GWAS) of liver fibrosis progression in patients coinfected with HCV and HIV identified a new locus associated with fibrosis severity on chromosome 3p25. The authors said the results may help define new targets for drug development or new prognostic tests.
Symptomatic HIV-associated neurocognitive disorders (HAND) warranting neurologic review were highly predicted by a 20-minute, computerized CogState-based screening procedure, according to a study in Clinical Infectious Diseases.
A study undertaken by Nigerian researchers found that the association of the HIV p24 core antigen with blood donation was highly significant and poses a great risk to recipients if screening of blood donor is carried out only by HIV antibody detection.
Fourth-generation immunoassays were the most sensitive at detecting acute HIV infection in patients prior to antiretroviral therapy, according to a recent study, although third-generation immunoassays were the most sensitive during treatment.
Twenty-four weeks of 10-mg daily rosuvastatin decreased coenzyme Q10 concentration and increased CoQ10/LDL ratio in HIV-infected patients on antiretroviral therapy, according to a study in HIV Clinical Trials.
Depression, a higher illness perception score, failure to achieve virologic suppression by week 12, and less-than-perfect adherence could be used to target early interventions in treatment-experienced, high-risk HIV-infected individuals.
High viral suppression rate can hide large gaps between time of HIV infection and time of viral suppression, according to a study in JAIDS. The authors said estimates of the flow-time in between steps of the care continuum should become priority indicators to identify these gaps and monitor whether interventions are successful in closing them.
Researchers at Boston University assessed patient reasons for refusal of HIV testing in the emergency department of a safety net hospital, and found that key themes included the importance of privacy and a respectful approach, ED atmosphere and environment discouraged testing acceptance, the importance of HIV counseling, and the desire to see an medical doctor before testing staff.
Italian researchers found that the use of darunavir/ritonavir (DRV/r), with its flexible dosage in clinical practice, resulted in high rates of virologic response in HIV-infected patients.
With data from the National HIV Surveillance System, CDC investigators found that two-thirds of persons in HIV care had durable viral suppression during 2012-2013, while one-third had high cumulative viral load burden and spent substantial time above viral load levels with increased risk of onward transmission.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It can be challenging to monitor everything, so here’s a quick look at some notable news items and journal articles published in recent weeks.
Efforts to increase viral suppression among individuals who inject drugs should focus on increasing antiretroviral therapy initiation and improving adherence to therapy, according to a study in the journal AIDS.
Canadian investigators developed a flexible framework that characterized patient transitions among states of HIV clinical care and demonstrated that multistate models provide a useful approach to supplement “cascade of care” work.
Researchers found that, in the setting of HIV infection, the presence of detectable cardiac troponin was strongly associated with coronary plaque, particularly calcified plaque among an asymptomatic group.
A cohort study found that overall risk of cardiovascular events in HIV-positive patients was twice as high as CVE risk in general population. The authors also found a relative risk for CVE type-1 higher in HIV-positive females, and a higher CVE type-2 risk in male patients.
An Australian study found that HIV-infected people less likely to be using antiretroviral therapy were younger and had a more recent diagnosis of HIV.
A study in AIDS Care underscored the importance of developing culturally appropriate social norm-based HIV interventions among people living with HIV/AIDS (PLWHA) in China, as such interventions have the potential to reduce risk behaviors and to promote condom use among PLWHA.
The frequency of mitochondrial DNA variants (mutations and large-scale deletions) was higher in HIV-infected treatment-experienced patients with or without antiretroviral therapy–induced toxicity than in uninfected controls, according to a study in HIV Medicine.
Immediate antiretroviral therapy was associated with lower mortality and better growth for up to 5 years in children under age 10 years, according to research published in the International Journal of Epidemiology.
A genome-wide association study (GWAS) of liver fibrosis progression in patients coinfected with HCV and HIV identified a new locus associated with fibrosis severity on chromosome 3p25. The authors said the results may help define new targets for drug development or new prognostic tests.
Symptomatic HIV-associated neurocognitive disorders (HAND) warranting neurologic review were highly predicted by a 20-minute, computerized CogState-based screening procedure, according to a study in Clinical Infectious Diseases.
A study undertaken by Nigerian researchers found that the association of the HIV p24 core antigen with blood donation was highly significant and poses a great risk to recipients if screening of blood donor is carried out only by HIV antibody detection.
Fourth-generation immunoassays were the most sensitive at detecting acute HIV infection in patients prior to antiretroviral therapy, according to a recent study, although third-generation immunoassays were the most sensitive during treatment.
Twenty-four weeks of 10-mg daily rosuvastatin decreased coenzyme Q10 concentration and increased CoQ10/LDL ratio in HIV-infected patients on antiretroviral therapy, according to a study in HIV Clinical Trials.
Depression, a higher illness perception score, failure to achieve virologic suppression by week 12, and less-than-perfect adherence could be used to target early interventions in treatment-experienced, high-risk HIV-infected individuals.
High viral suppression rate can hide large gaps between time of HIV infection and time of viral suppression, according to a study in JAIDS. The authors said estimates of the flow-time in between steps of the care continuum should become priority indicators to identify these gaps and monitor whether interventions are successful in closing them.
Researchers at Boston University assessed patient reasons for refusal of HIV testing in the emergency department of a safety net hospital, and found that key themes included the importance of privacy and a respectful approach, ED atmosphere and environment discouraged testing acceptance, the importance of HIV counseling, and the desire to see an medical doctor before testing staff.
Italian researchers found that the use of darunavir/ritonavir (DRV/r), with its flexible dosage in clinical practice, resulted in high rates of virologic response in HIV-infected patients.
With data from the National HIV Surveillance System, CDC investigators found that two-thirds of persons in HIV care had durable viral suppression during 2012-2013, while one-third had high cumulative viral load burden and spent substantial time above viral load levels with increased risk of onward transmission.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It can be challenging to monitor everything, so here’s a quick look at some notable news items and journal articles published in recent weeks.
Efforts to increase viral suppression among individuals who inject drugs should focus on increasing antiretroviral therapy initiation and improving adherence to therapy, according to a study in the journal AIDS.
Canadian investigators developed a flexible framework that characterized patient transitions among states of HIV clinical care and demonstrated that multistate models provide a useful approach to supplement “cascade of care” work.
Researchers found that, in the setting of HIV infection, the presence of detectable cardiac troponin was strongly associated with coronary plaque, particularly calcified plaque among an asymptomatic group.
A cohort study found that overall risk of cardiovascular events in HIV-positive patients was twice as high as CVE risk in general population. The authors also found a relative risk for CVE type-1 higher in HIV-positive females, and a higher CVE type-2 risk in male patients.
An Australian study found that HIV-infected people less likely to be using antiretroviral therapy were younger and had a more recent diagnosis of HIV.
A study in AIDS Care underscored the importance of developing culturally appropriate social norm-based HIV interventions among people living with HIV/AIDS (PLWHA) in China, as such interventions have the potential to reduce risk behaviors and to promote condom use among PLWHA.
The frequency of mitochondrial DNA variants (mutations and large-scale deletions) was higher in HIV-infected treatment-experienced patients with or without antiretroviral therapy–induced toxicity than in uninfected controls, according to a study in HIV Medicine.
Immediate antiretroviral therapy was associated with lower mortality and better growth for up to 5 years in children under age 10 years, according to research published in the International Journal of Epidemiology.
A genome-wide association study (GWAS) of liver fibrosis progression in patients coinfected with HCV and HIV identified a new locus associated with fibrosis severity on chromosome 3p25. The authors said the results may help define new targets for drug development or new prognostic tests.
Symptomatic HIV-associated neurocognitive disorders (HAND) warranting neurologic review were highly predicted by a 20-minute, computerized CogState-based screening procedure, according to a study in Clinical Infectious Diseases.
A study undertaken by Nigerian researchers found that the association of the HIV p24 core antigen with blood donation was highly significant and poses a great risk to recipients if screening of blood donor is carried out only by HIV antibody detection.
Fourth-generation immunoassays were the most sensitive at detecting acute HIV infection in patients prior to antiretroviral therapy, according to a recent study, although third-generation immunoassays were the most sensitive during treatment.
Twenty-four weeks of 10-mg daily rosuvastatin decreased coenzyme Q10 concentration and increased CoQ10/LDL ratio in HIV-infected patients on antiretroviral therapy, according to a study in HIV Clinical Trials.
Depression, a higher illness perception score, failure to achieve virologic suppression by week 12, and less-than-perfect adherence could be used to target early interventions in treatment-experienced, high-risk HIV-infected individuals.
High viral suppression rate can hide large gaps between time of HIV infection and time of viral suppression, according to a study in JAIDS. The authors said estimates of the flow-time in between steps of the care continuum should become priority indicators to identify these gaps and monitor whether interventions are successful in closing them.
Researchers at Boston University assessed patient reasons for refusal of HIV testing in the emergency department of a safety net hospital, and found that key themes included the importance of privacy and a respectful approach, ED atmosphere and environment discouraged testing acceptance, the importance of HIV counseling, and the desire to see an medical doctor before testing staff.
Italian researchers found that the use of darunavir/ritonavir (DRV/r), with its flexible dosage in clinical practice, resulted in high rates of virologic response in HIV-infected patients.
With data from the National HIV Surveillance System, CDC investigators found that two-thirds of persons in HIV care had durable viral suppression during 2012-2013, while one-third had high cumulative viral load burden and spent substantial time above viral load levels with increased risk of onward transmission.
On Twitter @richpizzi
Hepatitis Outlook: June 2016
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
Identification of a case of acute hepatitis C virus (HCV) infection in a frequent blood donor without other risk factors should be considered a sentinel event and should prompt public health investigation, according to research published in Morbidity and Mortality Weekly Report, because this could indicate a possible health care–associated infection.
Negative media reports about the safety of the hepatitis B vaccine in China harmed perception of the vaccine’s safety among patients, according to a recent study. Although the reports were erroneous, the failure of public health departments to communicate effectively contributed to a rise in the number of parents refusing to vaccinate their children.
An experimental, highly specific and sensitive HCV core antigen enzyme immunoassay (HCV-Ags EIA) was found to have the lowest limit of detection equivalent to serum HCV RNA levels of 150-250 IU/mL. Investigators found that the HCV-Ags EIA reliably differentiated viremic HCV infection from resolved HCV infection, thus accomplishing screening and diagnosis of viremic HCV infection in one step.
Loss of confidence in the hepatitis B vaccine following disproved allegations that the vaccine caused multiple sclerosis persists in France, according to research published in Human Vaccines & Immunotherapeutics.
The approval of the direct-acting antiviral agents (DAAs) grazoprevir and elbasvir with an indication for all levels of kidney function and dialysis has altered the landscape for the treatment of hepatitis C virus in patients with chronic kidney disease, according to a review in Clinical Liver Disease. The authors say this is because other DAAs are either not approved for use in patients with advanced chronic kidney disease or no safety data are available for the dialysis population.
A study in the Journal of Viral Hepatitis found that insulin resistance was associated with an increased risk for loss of vaccine-acquired anti-HBs (hepatitis B surface antigen) in a large sample of a nondiabetic, general population, indicating a possible role of insulin resistance in vaccine-induced immunity.
Grazoprevir, a second-generation HCV NS3/4A protease inhibitor, combined with ribavirin was associated with a rapid and sustained suppression of HCV RNA in a randomized study. The authors said the results support further evaluation of grazoprevir-based treatment regimens.
HIV–HCV coinfected patients treated with a fixed-dose combination of ledipasvir and sofosbuvir (LDV/SOF) showed significant improvement of their health-related quality of life and other patient-reported outcomes during treatment and after treatment cessation, according to a study in the Journal of Viral Hepatitis.
A Swedish study found that diabetes mellitus and cirrhosis are strong risk factors for hepatocellular carcinoma development after sustained virologic response (SVR) following treatment for chronic HCV has been achieved. However, the risk to develop hepatocellular carcinoma diminished significantly 2 years after SVR.
Chinese investigators said serum levels of platelet-derived growth factor (PDGF) decreased remarkably through fibrosis progression and could be used as a noninvasive biomarker for the assessment of fibrosis stage in patients with chronic hepatitis B virus (HBV).
A genome-wide association study of liver fibrosis progression in patients coinfected with HCV and HIV identified a new locus associated with fibrosis severity on chromosome 3p25. The authors said the results may help define new targets for drug development or new prognostic tests.
The RNA helicase DDX5 and E3 ligase Mex3b are important cellular targets for the design of novel, epigenetic therapies to combat HBV infection and poor-prognosis HBV-associated liver cancer, according to a study in Hepatology.
A Japanese study found that daclatasvir (DCV) and asunaprevir (ASV) dual therapy in hemodialysis patients infected with HCV is effective and safe with similar results, compared with patients with normal renal function.
A study evaluating the antiviral effect of ribavirin priming, and its influence on sustained virologic response after combination treatment, found that the lowest response pattern in HCV-infected patients was observed in prior nonresponder patients to pegylated interferon-alfa plus ribavirin combination therapy. The authors said this suggests that not only the individual interferon, but also the ribavirin sensitivity contributes significantly to the nonresponsive state.
A veterinary study provided evidence that hepatitis E virus is able to damage the blood-brain barrier and replicate in the brain and spinal cord.
An all-oral regimen of ledipasvir and sofosbuvir is an effective and safe treatment for a wide range of HCV genotype 4 subtypes in both treatment-naive and -experienced patients, including those with compensated cirrhosis, according to results of a recent study.
AGA Resource
Through the Hepatitis C Clinical Service Line, AGA offers tools to help you become more efficient, understand quality standards and improve the process of care for your patients.
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
Identification of a case of acute hepatitis C virus (HCV) infection in a frequent blood donor without other risk factors should be considered a sentinel event and should prompt public health investigation, according to research published in Morbidity and Mortality Weekly Report, because this could indicate a possible health care–associated infection.
Negative media reports about the safety of the hepatitis B vaccine in China harmed perception of the vaccine’s safety among patients, according to a recent study. Although the reports were erroneous, the failure of public health departments to communicate effectively contributed to a rise in the number of parents refusing to vaccinate their children.
An experimental, highly specific and sensitive HCV core antigen enzyme immunoassay (HCV-Ags EIA) was found to have the lowest limit of detection equivalent to serum HCV RNA levels of 150-250 IU/mL. Investigators found that the HCV-Ags EIA reliably differentiated viremic HCV infection from resolved HCV infection, thus accomplishing screening and diagnosis of viremic HCV infection in one step.
Loss of confidence in the hepatitis B vaccine following disproved allegations that the vaccine caused multiple sclerosis persists in France, according to research published in Human Vaccines & Immunotherapeutics.
The approval of the direct-acting antiviral agents (DAAs) grazoprevir and elbasvir with an indication for all levels of kidney function and dialysis has altered the landscape for the treatment of hepatitis C virus in patients with chronic kidney disease, according to a review in Clinical Liver Disease. The authors say this is because other DAAs are either not approved for use in patients with advanced chronic kidney disease or no safety data are available for the dialysis population.
A study in the Journal of Viral Hepatitis found that insulin resistance was associated with an increased risk for loss of vaccine-acquired anti-HBs (hepatitis B surface antigen) in a large sample of a nondiabetic, general population, indicating a possible role of insulin resistance in vaccine-induced immunity.
Grazoprevir, a second-generation HCV NS3/4A protease inhibitor, combined with ribavirin was associated with a rapid and sustained suppression of HCV RNA in a randomized study. The authors said the results support further evaluation of grazoprevir-based treatment regimens.
HIV–HCV coinfected patients treated with a fixed-dose combination of ledipasvir and sofosbuvir (LDV/SOF) showed significant improvement of their health-related quality of life and other patient-reported outcomes during treatment and after treatment cessation, according to a study in the Journal of Viral Hepatitis.
A Swedish study found that diabetes mellitus and cirrhosis are strong risk factors for hepatocellular carcinoma development after sustained virologic response (SVR) following treatment for chronic HCV has been achieved. However, the risk to develop hepatocellular carcinoma diminished significantly 2 years after SVR.
Chinese investigators said serum levels of platelet-derived growth factor (PDGF) decreased remarkably through fibrosis progression and could be used as a noninvasive biomarker for the assessment of fibrosis stage in patients with chronic hepatitis B virus (HBV).
A genome-wide association study of liver fibrosis progression in patients coinfected with HCV and HIV identified a new locus associated with fibrosis severity on chromosome 3p25. The authors said the results may help define new targets for drug development or new prognostic tests.
The RNA helicase DDX5 and E3 ligase Mex3b are important cellular targets for the design of novel, epigenetic therapies to combat HBV infection and poor-prognosis HBV-associated liver cancer, according to a study in Hepatology.
A Japanese study found that daclatasvir (DCV) and asunaprevir (ASV) dual therapy in hemodialysis patients infected with HCV is effective and safe with similar results, compared with patients with normal renal function.
A study evaluating the antiviral effect of ribavirin priming, and its influence on sustained virologic response after combination treatment, found that the lowest response pattern in HCV-infected patients was observed in prior nonresponder patients to pegylated interferon-alfa plus ribavirin combination therapy. The authors said this suggests that not only the individual interferon, but also the ribavirin sensitivity contributes significantly to the nonresponsive state.
A veterinary study provided evidence that hepatitis E virus is able to damage the blood-brain barrier and replicate in the brain and spinal cord.
An all-oral regimen of ledipasvir and sofosbuvir is an effective and safe treatment for a wide range of HCV genotype 4 subtypes in both treatment-naive and -experienced patients, including those with compensated cirrhosis, according to results of a recent study.
AGA Resource
Through the Hepatitis C Clinical Service Line, AGA offers tools to help you become more efficient, understand quality standards and improve the process of care for your patients.
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
Identification of a case of acute hepatitis C virus (HCV) infection in a frequent blood donor without other risk factors should be considered a sentinel event and should prompt public health investigation, according to research published in Morbidity and Mortality Weekly Report, because this could indicate a possible health care–associated infection.
Negative media reports about the safety of the hepatitis B vaccine in China harmed perception of the vaccine’s safety among patients, according to a recent study. Although the reports were erroneous, the failure of public health departments to communicate effectively contributed to a rise in the number of parents refusing to vaccinate their children.
An experimental, highly specific and sensitive HCV core antigen enzyme immunoassay (HCV-Ags EIA) was found to have the lowest limit of detection equivalent to serum HCV RNA levels of 150-250 IU/mL. Investigators found that the HCV-Ags EIA reliably differentiated viremic HCV infection from resolved HCV infection, thus accomplishing screening and diagnosis of viremic HCV infection in one step.
Loss of confidence in the hepatitis B vaccine following disproved allegations that the vaccine caused multiple sclerosis persists in France, according to research published in Human Vaccines & Immunotherapeutics.
The approval of the direct-acting antiviral agents (DAAs) grazoprevir and elbasvir with an indication for all levels of kidney function and dialysis has altered the landscape for the treatment of hepatitis C virus in patients with chronic kidney disease, according to a review in Clinical Liver Disease. The authors say this is because other DAAs are either not approved for use in patients with advanced chronic kidney disease or no safety data are available for the dialysis population.
A study in the Journal of Viral Hepatitis found that insulin resistance was associated with an increased risk for loss of vaccine-acquired anti-HBs (hepatitis B surface antigen) in a large sample of a nondiabetic, general population, indicating a possible role of insulin resistance in vaccine-induced immunity.
Grazoprevir, a second-generation HCV NS3/4A protease inhibitor, combined with ribavirin was associated with a rapid and sustained suppression of HCV RNA in a randomized study. The authors said the results support further evaluation of grazoprevir-based treatment regimens.
HIV–HCV coinfected patients treated with a fixed-dose combination of ledipasvir and sofosbuvir (LDV/SOF) showed significant improvement of their health-related quality of life and other patient-reported outcomes during treatment and after treatment cessation, according to a study in the Journal of Viral Hepatitis.
A Swedish study found that diabetes mellitus and cirrhosis are strong risk factors for hepatocellular carcinoma development after sustained virologic response (SVR) following treatment for chronic HCV has been achieved. However, the risk to develop hepatocellular carcinoma diminished significantly 2 years after SVR.
Chinese investigators said serum levels of platelet-derived growth factor (PDGF) decreased remarkably through fibrosis progression and could be used as a noninvasive biomarker for the assessment of fibrosis stage in patients with chronic hepatitis B virus (HBV).
A genome-wide association study of liver fibrosis progression in patients coinfected with HCV and HIV identified a new locus associated with fibrosis severity on chromosome 3p25. The authors said the results may help define new targets for drug development or new prognostic tests.
The RNA helicase DDX5 and E3 ligase Mex3b are important cellular targets for the design of novel, epigenetic therapies to combat HBV infection and poor-prognosis HBV-associated liver cancer, according to a study in Hepatology.
A Japanese study found that daclatasvir (DCV) and asunaprevir (ASV) dual therapy in hemodialysis patients infected with HCV is effective and safe with similar results, compared with patients with normal renal function.
A study evaluating the antiviral effect of ribavirin priming, and its influence on sustained virologic response after combination treatment, found that the lowest response pattern in HCV-infected patients was observed in prior nonresponder patients to pegylated interferon-alfa plus ribavirin combination therapy. The authors said this suggests that not only the individual interferon, but also the ribavirin sensitivity contributes significantly to the nonresponsive state.
A veterinary study provided evidence that hepatitis E virus is able to damage the blood-brain barrier and replicate in the brain and spinal cord.
An all-oral regimen of ledipasvir and sofosbuvir is an effective and safe treatment for a wide range of HCV genotype 4 subtypes in both treatment-naive and -experienced patients, including those with compensated cirrhosis, according to results of a recent study.
AGA Resource
Through the Hepatitis C Clinical Service Line, AGA offers tools to help you become more efficient, understand quality standards and improve the process of care for your patients.
On Twitter @richpizzi
Hepatitis Outlook: June 2016
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
Identification of a case of acute hepatitis C virus (HCV) infection in a frequent blood donor without other risk factors should be considered a sentinel event and should prompt public health investigation, according to research published in Morbidity and Mortality Weekly Report, because this could indicate a possible health care–associated infection.
Negative media reports about the safety of the hepatitis B vaccine in China harmed perception of the vaccine’s safety among patients, according to a recent study. Although the reports were erroneous, the failure of public health departments to communicate effectively contributed to a rise in the number of parents refusing to vaccinate their children.
An experimental, highly specific and sensitive HCV core antigen enzyme immunoassay (HCV-Ags EIA) was found to have the lowest limit of detection equivalent to serum HCV RNA levels of 150-250 IU/mL. Investigators found that the HCV-Ags EIA reliably differentiated viremic HCV infection from resolved HCV infection, thus accomplishing screening and diagnosis of viremic HCV infection in one step.
Loss of confidence in the hepatitis B vaccine following disproved allegations that the vaccine caused multiple sclerosis persists in France, according to research published in Human Vaccines & Immunotherapeutics.
The approval of the direct-acting antiviral agents (DAAs) grazoprevir and elbasvir with an indication for all levels of kidney function and dialysis has altered the landscape for the treatment of hepatitis C virus in patients with chronic kidney disease, according to a review in Clinical Liver Disease. The authors say this is because other DAAs are either not approved for use in patients with advanced chronic kidney disease or no safety data are available for the dialysis population.
A study in the Journal of Viral Hepatitis found that insulin resistance was associated with an increased risk for loss of vaccine-acquired anti-HBs (hepatitis B surface antigen) in a large sample of a nondiabetic, general population, indicating a possible role of insulin resistance in vaccine-induced immunity.
Grazoprevir, a second-generation HCV NS3/4A protease inhibitor, combined with ribavirin was associated with a rapid and sustained suppression of HCV RNA in a randomized study. The authors said the results support further evaluation of grazoprevir-based treatment regimens.
HIV–HCV coinfected patients treated with a fixed-dose combination of ledipasvir and sofosbuvir (LDV/SOF) showed significant improvement of their health-related quality of life and other patient-reported outcomes during treatment and after treatment cessation, according to a study in the Journal of Viral Hepatitis.
A Swedish study found that diabetes mellitus and cirrhosis are strong risk factors for hepatocellular carcinoma development after sustained virologic response (SVR) following treatment for chronic HCV has been achieved. However, the risk to develop hepatocellular carcinoma diminished significantly 2 years after SVR.
Chinese investigators said serum levels of platelet-derived growth factor (PDGF) decreased remarkably through fibrosis progression and could be used as a noninvasive biomarker for the assessment of fibrosis stage in patients with chronic hepatitis B virus (HBV).
A genome-wide association study of liver fibrosis progression in patients coinfected with HCV and HIV identified a new locus associated with fibrosis severity on chromosome 3p25. The authors said the results may help define new targets for drug development or new prognostic tests.
The RNA helicase DDX5 and E3 ligase Mex3b are important cellular targets for the design of novel, epigenetic therapies to combat HBV infection and poor-prognosis HBV-associated liver cancer, according to a study in Hepatology.
A Japanese study found that daclatasvir (DCV) and asunaprevir (ASV) dual therapy in hemodialysis patients infected with HCV is effective and safe with similar results, compared with patients with normal renal function.
A study evaluating the antiviral effect of ribavirin priming, and its influence on sustained virologic response after combination treatment, found that the lowest response pattern in HCV-infected patients was observed in prior nonresponder patients to pegylated interferon-alfa plus ribavirin combination therapy. The authors said this suggests that not only the individual interferon, but also the ribavirin sensitivity contributes significantly to the nonresponsive state.
A veterinary study provided evidence that hepatitis E virus is able to damage the blood-brain barrier and replicate in the brain and spinal cord.
An all-oral regimen of ledipasvir and sofosbuvir is an effective and safe treatment for a wide range of HCV genotype 4 subtypes in both treatment-naive and -experienced patients, including those with compensated cirrhosis, according to results of a recent study.
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
Identification of a case of acute hepatitis C virus (HCV) infection in a frequent blood donor without other risk factors should be considered a sentinel event and should prompt public health investigation, according to research published in Morbidity and Mortality Weekly Report, because this could indicate a possible health care–associated infection.
Negative media reports about the safety of the hepatitis B vaccine in China harmed perception of the vaccine’s safety among patients, according to a recent study. Although the reports were erroneous, the failure of public health departments to communicate effectively contributed to a rise in the number of parents refusing to vaccinate their children.
An experimental, highly specific and sensitive HCV core antigen enzyme immunoassay (HCV-Ags EIA) was found to have the lowest limit of detection equivalent to serum HCV RNA levels of 150-250 IU/mL. Investigators found that the HCV-Ags EIA reliably differentiated viremic HCV infection from resolved HCV infection, thus accomplishing screening and diagnosis of viremic HCV infection in one step.
Loss of confidence in the hepatitis B vaccine following disproved allegations that the vaccine caused multiple sclerosis persists in France, according to research published in Human Vaccines & Immunotherapeutics.
The approval of the direct-acting antiviral agents (DAAs) grazoprevir and elbasvir with an indication for all levels of kidney function and dialysis has altered the landscape for the treatment of hepatitis C virus in patients with chronic kidney disease, according to a review in Clinical Liver Disease. The authors say this is because other DAAs are either not approved for use in patients with advanced chronic kidney disease or no safety data are available for the dialysis population.
A study in the Journal of Viral Hepatitis found that insulin resistance was associated with an increased risk for loss of vaccine-acquired anti-HBs (hepatitis B surface antigen) in a large sample of a nondiabetic, general population, indicating a possible role of insulin resistance in vaccine-induced immunity.
Grazoprevir, a second-generation HCV NS3/4A protease inhibitor, combined with ribavirin was associated with a rapid and sustained suppression of HCV RNA in a randomized study. The authors said the results support further evaluation of grazoprevir-based treatment regimens.
HIV–HCV coinfected patients treated with a fixed-dose combination of ledipasvir and sofosbuvir (LDV/SOF) showed significant improvement of their health-related quality of life and other patient-reported outcomes during treatment and after treatment cessation, according to a study in the Journal of Viral Hepatitis.
A Swedish study found that diabetes mellitus and cirrhosis are strong risk factors for hepatocellular carcinoma development after sustained virologic response (SVR) following treatment for chronic HCV has been achieved. However, the risk to develop hepatocellular carcinoma diminished significantly 2 years after SVR.
Chinese investigators said serum levels of platelet-derived growth factor (PDGF) decreased remarkably through fibrosis progression and could be used as a noninvasive biomarker for the assessment of fibrosis stage in patients with chronic hepatitis B virus (HBV).
A genome-wide association study of liver fibrosis progression in patients coinfected with HCV and HIV identified a new locus associated with fibrosis severity on chromosome 3p25. The authors said the results may help define new targets for drug development or new prognostic tests.
The RNA helicase DDX5 and E3 ligase Mex3b are important cellular targets for the design of novel, epigenetic therapies to combat HBV infection and poor-prognosis HBV-associated liver cancer, according to a study in Hepatology.
A Japanese study found that daclatasvir (DCV) and asunaprevir (ASV) dual therapy in hemodialysis patients infected with HCV is effective and safe with similar results, compared with patients with normal renal function.
A study evaluating the antiviral effect of ribavirin priming, and its influence on sustained virologic response after combination treatment, found that the lowest response pattern in HCV-infected patients was observed in prior nonresponder patients to pegylated interferon-alfa plus ribavirin combination therapy. The authors said this suggests that not only the individual interferon, but also the ribavirin sensitivity contributes significantly to the nonresponsive state.
A veterinary study provided evidence that hepatitis E virus is able to damage the blood-brain barrier and replicate in the brain and spinal cord.
An all-oral regimen of ledipasvir and sofosbuvir is an effective and safe treatment for a wide range of HCV genotype 4 subtypes in both treatment-naive and -experienced patients, including those with compensated cirrhosis, according to results of a recent study.
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
Identification of a case of acute hepatitis C virus (HCV) infection in a frequent blood donor without other risk factors should be considered a sentinel event and should prompt public health investigation, according to research published in Morbidity and Mortality Weekly Report, because this could indicate a possible health care–associated infection.
Negative media reports about the safety of the hepatitis B vaccine in China harmed perception of the vaccine’s safety among patients, according to a recent study. Although the reports were erroneous, the failure of public health departments to communicate effectively contributed to a rise in the number of parents refusing to vaccinate their children.
An experimental, highly specific and sensitive HCV core antigen enzyme immunoassay (HCV-Ags EIA) was found to have the lowest limit of detection equivalent to serum HCV RNA levels of 150-250 IU/mL. Investigators found that the HCV-Ags EIA reliably differentiated viremic HCV infection from resolved HCV infection, thus accomplishing screening and diagnosis of viremic HCV infection in one step.
Loss of confidence in the hepatitis B vaccine following disproved allegations that the vaccine caused multiple sclerosis persists in France, according to research published in Human Vaccines & Immunotherapeutics.
The approval of the direct-acting antiviral agents (DAAs) grazoprevir and elbasvir with an indication for all levels of kidney function and dialysis has altered the landscape for the treatment of hepatitis C virus in patients with chronic kidney disease, according to a review in Clinical Liver Disease. The authors say this is because other DAAs are either not approved for use in patients with advanced chronic kidney disease or no safety data are available for the dialysis population.
A study in the Journal of Viral Hepatitis found that insulin resistance was associated with an increased risk for loss of vaccine-acquired anti-HBs (hepatitis B surface antigen) in a large sample of a nondiabetic, general population, indicating a possible role of insulin resistance in vaccine-induced immunity.
Grazoprevir, a second-generation HCV NS3/4A protease inhibitor, combined with ribavirin was associated with a rapid and sustained suppression of HCV RNA in a randomized study. The authors said the results support further evaluation of grazoprevir-based treatment regimens.
HIV–HCV coinfected patients treated with a fixed-dose combination of ledipasvir and sofosbuvir (LDV/SOF) showed significant improvement of their health-related quality of life and other patient-reported outcomes during treatment and after treatment cessation, according to a study in the Journal of Viral Hepatitis.
A Swedish study found that diabetes mellitus and cirrhosis are strong risk factors for hepatocellular carcinoma development after sustained virologic response (SVR) following treatment for chronic HCV has been achieved. However, the risk to develop hepatocellular carcinoma diminished significantly 2 years after SVR.
Chinese investigators said serum levels of platelet-derived growth factor (PDGF) decreased remarkably through fibrosis progression and could be used as a noninvasive biomarker for the assessment of fibrosis stage in patients with chronic hepatitis B virus (HBV).
A genome-wide association study of liver fibrosis progression in patients coinfected with HCV and HIV identified a new locus associated with fibrosis severity on chromosome 3p25. The authors said the results may help define new targets for drug development or new prognostic tests.
The RNA helicase DDX5 and E3 ligase Mex3b are important cellular targets for the design of novel, epigenetic therapies to combat HBV infection and poor-prognosis HBV-associated liver cancer, according to a study in Hepatology.
A Japanese study found that daclatasvir (DCV) and asunaprevir (ASV) dual therapy in hemodialysis patients infected with HCV is effective and safe with similar results, compared with patients with normal renal function.
A study evaluating the antiviral effect of ribavirin priming, and its influence on sustained virologic response after combination treatment, found that the lowest response pattern in HCV-infected patients was observed in prior nonresponder patients to pegylated interferon-alfa plus ribavirin combination therapy. The authors said this suggests that not only the individual interferon, but also the ribavirin sensitivity contributes significantly to the nonresponsive state.
A veterinary study provided evidence that hepatitis E virus is able to damage the blood-brain barrier and replicate in the brain and spinal cord.
An all-oral regimen of ledipasvir and sofosbuvir is an effective and safe treatment for a wide range of HCV genotype 4 subtypes in both treatment-naive and -experienced patients, including those with compensated cirrhosis, according to results of a recent study.
On Twitter @richpizzi
HBV/HIV coinfection a significant risk factor for inpatient mortality
Patients coinfected with hepatitis B virus and HIV are at greater risk for in-hospital mortality, particularly in liver-related admissions, compared with HBV monoinfection, according to a study in the Journal of Viral Hepatitis.
Researchers at Massachusetts General Hospital, Boston, identified patients in the 2011 U.S. Nationwide Inpatient Sample who had been hospitalized with HBV or HIV monoinfection or HBV/HIV coinfection using ICD-9-CM codes. A total of 72,584 discharges with HBV monoinfection, 133,880 discharges with HIV monoinfection and 8,156 discharges with HBV/HIV coinfection were included. The researchers then compared liver-related hospital admissions among the three groups and performed multivariable logistic regression to identify independent predictors of in-hospital mortality, length of stay, and total charges.
According to Raymond T. Chung, MD, director of hepatology at Massachusetts General Hospital, and his coauthors, this study is the first to examine outcomes of HBV/HIV coinfection among hospitalized patients, a “group that represents those with advanced disease and vulnerable to poor outcomes and high health care utilization.” (J Viral Hepat. 2016 Jun 13. doi: 10.1111/jvh.12555)
Patients in the study with HBV monoinfection tended to be older than those with HIV monoinfection or HBV/HIV coinfection. Of those aged 51-65 years, 42% had HBV monoinfection, 34% had HIV monoinfection, and 31% had HBV/HIV coinfection (P less than .001). Males were overrepresented in the HBV/HIV coinfection group (77%), compared with those with HBV monoinfection (57%), and HIV monoinfection (67%). Additionally, the investigators found that patients with HBV monoinfection were more likely to be white (42%) than were those with HIV monoinfection (26%) or HBV/HIV coinfection (27%).
Dr. Chung and his colleagues found that HBV/HIV coinfection was associated with significantly higher adjusted in-hospital mortality, compared with patients with HBV monoinfection (adjusted odds ratio, 1.67; 95% confidence interval, 1.30-2.15), but not compared with HIV monoinfection (aOR, 1.22; 95% CI, 0.96-1.54).
“Interestingly, [the] increase in risk of mortality was primarily observed in liver-related admissions … and not infectious-related hospitalizations,” Dr. Chung and his coauthors said.
The overall adjusted hospital length of stay (LOS;1.53 days; 95% CI, 0.93-2.13; less than .001) and total hospitalization charges ($17,595; 95% CI 11,120-24,069; P less than .0001) were higher in the coinfected group, compared with the HBV monoinfection group – even after adjustment for comorbidity- and disease-related complications, the authors wrote. LOS and total charges also were higher in the coinfected group, compared with the HIV monoinfection group (+0.62 days; P = .034; $8,840; P = .005).
While HBV/HIV coinfection by itself was not associated with higher in-hospital mortality, the presence of HBV along with cirrhosis or complications of portal hypertension was associated with three times greater in-hospital mortality in patients with HIV, compared with those without such complications (odds ratio, 3.00; 95% CI, 1.80-5.02). Researchers also found that LOS (0.62 days; 95% CI, 0.05-1.20; P = .034) and hospitalization cost ($8,840; 95% CI, 2,604-15,077; P = .005) were increased in patients with HBV/HIV coinfection, compared with HIV monoinfection.
“Overall health care utilization from HBV/HIV coinfection is … higher than for either infection alone and higher than the national average for all hospitalizations, emphasizing the health care burden from these illnesses,” the authors concluded.
Three study coauthors were supported in part by grants from the National Institutes of Health, while one coauthor was supported by a career development award from the American Gastroenterological Association and by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Chung reported no financial conflict of interests. One coauthor reported participation on scientific advisory boards of AbbVie and Cubist pharmaceuticals.
On Twitter @richpizzi
Patients coinfected with hepatitis B virus and HIV are at greater risk for in-hospital mortality, particularly in liver-related admissions, compared with HBV monoinfection, according to a study in the Journal of Viral Hepatitis.
Researchers at Massachusetts General Hospital, Boston, identified patients in the 2011 U.S. Nationwide Inpatient Sample who had been hospitalized with HBV or HIV monoinfection or HBV/HIV coinfection using ICD-9-CM codes. A total of 72,584 discharges with HBV monoinfection, 133,880 discharges with HIV monoinfection and 8,156 discharges with HBV/HIV coinfection were included. The researchers then compared liver-related hospital admissions among the three groups and performed multivariable logistic regression to identify independent predictors of in-hospital mortality, length of stay, and total charges.
According to Raymond T. Chung, MD, director of hepatology at Massachusetts General Hospital, and his coauthors, this study is the first to examine outcomes of HBV/HIV coinfection among hospitalized patients, a “group that represents those with advanced disease and vulnerable to poor outcomes and high health care utilization.” (J Viral Hepat. 2016 Jun 13. doi: 10.1111/jvh.12555)
Patients in the study with HBV monoinfection tended to be older than those with HIV monoinfection or HBV/HIV coinfection. Of those aged 51-65 years, 42% had HBV monoinfection, 34% had HIV monoinfection, and 31% had HBV/HIV coinfection (P less than .001). Males were overrepresented in the HBV/HIV coinfection group (77%), compared with those with HBV monoinfection (57%), and HIV monoinfection (67%). Additionally, the investigators found that patients with HBV monoinfection were more likely to be white (42%) than were those with HIV monoinfection (26%) or HBV/HIV coinfection (27%).
Dr. Chung and his colleagues found that HBV/HIV coinfection was associated with significantly higher adjusted in-hospital mortality, compared with patients with HBV monoinfection (adjusted odds ratio, 1.67; 95% confidence interval, 1.30-2.15), but not compared with HIV monoinfection (aOR, 1.22; 95% CI, 0.96-1.54).
“Interestingly, [the] increase in risk of mortality was primarily observed in liver-related admissions … and not infectious-related hospitalizations,” Dr. Chung and his coauthors said.
The overall adjusted hospital length of stay (LOS;1.53 days; 95% CI, 0.93-2.13; less than .001) and total hospitalization charges ($17,595; 95% CI 11,120-24,069; P less than .0001) were higher in the coinfected group, compared with the HBV monoinfection group – even after adjustment for comorbidity- and disease-related complications, the authors wrote. LOS and total charges also were higher in the coinfected group, compared with the HIV monoinfection group (+0.62 days; P = .034; $8,840; P = .005).
While HBV/HIV coinfection by itself was not associated with higher in-hospital mortality, the presence of HBV along with cirrhosis or complications of portal hypertension was associated with three times greater in-hospital mortality in patients with HIV, compared with those without such complications (odds ratio, 3.00; 95% CI, 1.80-5.02). Researchers also found that LOS (0.62 days; 95% CI, 0.05-1.20; P = .034) and hospitalization cost ($8,840; 95% CI, 2,604-15,077; P = .005) were increased in patients with HBV/HIV coinfection, compared with HIV monoinfection.
“Overall health care utilization from HBV/HIV coinfection is … higher than for either infection alone and higher than the national average for all hospitalizations, emphasizing the health care burden from these illnesses,” the authors concluded.
Three study coauthors were supported in part by grants from the National Institutes of Health, while one coauthor was supported by a career development award from the American Gastroenterological Association and by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Chung reported no financial conflict of interests. One coauthor reported participation on scientific advisory boards of AbbVie and Cubist pharmaceuticals.
On Twitter @richpizzi
Patients coinfected with hepatitis B virus and HIV are at greater risk for in-hospital mortality, particularly in liver-related admissions, compared with HBV monoinfection, according to a study in the Journal of Viral Hepatitis.
Researchers at Massachusetts General Hospital, Boston, identified patients in the 2011 U.S. Nationwide Inpatient Sample who had been hospitalized with HBV or HIV monoinfection or HBV/HIV coinfection using ICD-9-CM codes. A total of 72,584 discharges with HBV monoinfection, 133,880 discharges with HIV monoinfection and 8,156 discharges with HBV/HIV coinfection were included. The researchers then compared liver-related hospital admissions among the three groups and performed multivariable logistic regression to identify independent predictors of in-hospital mortality, length of stay, and total charges.
According to Raymond T. Chung, MD, director of hepatology at Massachusetts General Hospital, and his coauthors, this study is the first to examine outcomes of HBV/HIV coinfection among hospitalized patients, a “group that represents those with advanced disease and vulnerable to poor outcomes and high health care utilization.” (J Viral Hepat. 2016 Jun 13. doi: 10.1111/jvh.12555)
Patients in the study with HBV monoinfection tended to be older than those with HIV monoinfection or HBV/HIV coinfection. Of those aged 51-65 years, 42% had HBV monoinfection, 34% had HIV monoinfection, and 31% had HBV/HIV coinfection (P less than .001). Males were overrepresented in the HBV/HIV coinfection group (77%), compared with those with HBV monoinfection (57%), and HIV monoinfection (67%). Additionally, the investigators found that patients with HBV monoinfection were more likely to be white (42%) than were those with HIV monoinfection (26%) or HBV/HIV coinfection (27%).
Dr. Chung and his colleagues found that HBV/HIV coinfection was associated with significantly higher adjusted in-hospital mortality, compared with patients with HBV monoinfection (adjusted odds ratio, 1.67; 95% confidence interval, 1.30-2.15), but not compared with HIV monoinfection (aOR, 1.22; 95% CI, 0.96-1.54).
“Interestingly, [the] increase in risk of mortality was primarily observed in liver-related admissions … and not infectious-related hospitalizations,” Dr. Chung and his coauthors said.
The overall adjusted hospital length of stay (LOS;1.53 days; 95% CI, 0.93-2.13; less than .001) and total hospitalization charges ($17,595; 95% CI 11,120-24,069; P less than .0001) were higher in the coinfected group, compared with the HBV monoinfection group – even after adjustment for comorbidity- and disease-related complications, the authors wrote. LOS and total charges also were higher in the coinfected group, compared with the HIV monoinfection group (+0.62 days; P = .034; $8,840; P = .005).
While HBV/HIV coinfection by itself was not associated with higher in-hospital mortality, the presence of HBV along with cirrhosis or complications of portal hypertension was associated with three times greater in-hospital mortality in patients with HIV, compared with those without such complications (odds ratio, 3.00; 95% CI, 1.80-5.02). Researchers also found that LOS (0.62 days; 95% CI, 0.05-1.20; P = .034) and hospitalization cost ($8,840; 95% CI, 2,604-15,077; P = .005) were increased in patients with HBV/HIV coinfection, compared with HIV monoinfection.
“Overall health care utilization from HBV/HIV coinfection is … higher than for either infection alone and higher than the national average for all hospitalizations, emphasizing the health care burden from these illnesses,” the authors concluded.
Three study coauthors were supported in part by grants from the National Institutes of Health, while one coauthor was supported by a career development award from the American Gastroenterological Association and by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Chung reported no financial conflict of interests. One coauthor reported participation on scientific advisory boards of AbbVie and Cubist pharmaceuticals.
On Twitter @richpizzi
FROM THE JOURNAL OF VIRAL HEPATITIS
Key clinical point: Patients coinfected with HBV and HIV are at greater risk for in-hospital mortality, particularly in liver-related admissions, compared with HBV monoinfection.
Major finding: HBV/HIV coinfection was associated with significantly higher adjusted in-hospital mortality, compared with patients with HBV monoinfection, but not when compared with HIV monoinfection.
Data source: Comparison study of patient discharges from the 2011 U.S. Nationwide Inpatient Sample: 72,584 discharges with HBV monoinfection, 133,880 discharges with HIV monoinfection and 8,156 discharges with HBV/HIV coinfection.
Disclosures: Three study coauthors were supported in part by grants from the National Institutes of Health, while one coauthor was supported by a career development award from the American Gastroenterological Association and by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Chung reported no financial conflict of interests. One coauthor reported participation on scientific advisory boards of AbbVie and Cubist pharmaceuticals.
HIV research update: Early June 2016
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Interventions that seek to promptly house homeless individuals might assist in maximizing the clinical and public health benefits of antiretroviral therapy among people living with HIV/AIDS, according to a study in AIDS Care.
MRSA colonization among HIV-infected youth is more closely related to living in a low-income or slum community than to HIV-related clinical factors, according to a study in the Pediatric Infectious Disease Journal.
Marijuana use was not associated with progression to significant liver fibrosis, in a large cohort study of HIV/hepatitis C virus (HCV) co-infected women. Alcohol use may better predict fibrosis progression in HIV/HCV co-infected women, the authors said.
More than 60% of deaths occurring in a rural South African community between 1992 and 2013 could be attributed directly or indirectly to HIV, according to a recent study. However, the authors noted that there has been an increasing level of non-HIV mortality, which has important implications for local health care provision.
A study in AIDS Care found that providers value same-day, electronic, patient-reported measures for use in clinical HIV care, with the condition that patient-reported outcomes are 1) tailored to be the most clinically relevant to their population; 2) well integrated into clinic flow; and 3) easy to interpret, highlighting chief patient concerns and changes over time.
Investigators found that nasal and salivary samples can be collected from HIV-infected patients in a standardized manner over repeated visits in both low and high resource settings, and these methods may be used in support of future HIV vaccine clinical trials.
A study in the Journal of Infectious Diseases found no intrinsic effect of viral subtype on the efficacy of tenofovir-containing regimens for treating HIV-1 subtype C infections. There were no differences between subtypes C and non-B/C in either univariate or multivariate analysis.
New research provides preliminary evidence that heavy drinking may increase a key inflammatory marker in HIV-infected individuals with suppressed infection.
The phase III Women AntiretroViral Efficacy and Safety study (WAVES) showed that clinical trials of antiretroviral regimens in global and diverse populations of treatment-naive women are possible, investigators concluded. They said their findings support guidelines recommending integrase inhibitor–based regimens in first-line antiretroviral therapy.
A hybrid mobile strategy for HIV testing of adults was leveraged successfully to reach adolescents for HIV treatment and prevention, according to a study in Kenya and Uganda.
With viral suppression induced by combination antiretroviral therapy, women have less reduction in key markers of inflammation and immune activation, compared with men, report the authors of a study in JAIDS.
The transfer of HIV-1-p17-specific T-cell receptors (TCRs) into T-cells is functional both in HIV-1–infected patients and in healthy blood donors, according to a study in the journal AIDS. The authors say TCR-transfer is a promising method to boost the immune system against HIV-1.
HIV-1 subtype C (HIV-1C) exhibits lower in vivo fitness, compared with HIV-1B, which allows successful treatment despite high baseline viral loads, a new study demonstrated. The lower fitness – and potentially lower virulence – together with high viral loads may underlie the heightened transmission potential of HIV-1C and its growing global spread.
Thailand has achieved World Health Organization targets for elimination of mother-to-child-transmission of HIV and can serve as a model for other countries, according to a report in MMWR.
Regular CD4 testing may be unnecessary for virally suppressed children aged 5-15 years with CD4 greater than or equal to 500 cells/mm3, according to a study published in the Journal of the Pediatric Infectious Diseases Society.
Investigators at Case Western Reserve University, Cleveland found that 24 weeks of 10 mg daily rosuvastatin decreases plasma coenzyme Q10 concentration and increases CoQ10/LDL ratio in HIV-infected patients on antiretroviral therapy.
Researchers from the University of California, San Francisco, and Yale University, New Haven, Conn., found that half of people newly infected with HIV experience neurologic issues that are generally not severe and usually resolve after starting antiretroviral therapy.
A study of HIV-infected individuals in metropolitan Washington identified high prevalence of transmitted drug resistance, regardless of gender. The authors said active surveillance for transmitted drug resistance is needed to guide antiretroviral usage and analyses of risk group contributions to HIV transmission and resistance.
Single-nucleotide polymorphisms in genes encoding the Toll-like receptor 4 (TLR4) and CD14 are independently associated with long-term CD4+ T-cell recovery in HIV-infected individuals after antiretroviral therapy, according to a study in the journal AIDS.
In HIV/HCV co-infected individuals, the crude incidence of hepatocellular carcinoma increased from 2001 to 2014, while other liver events declined, according to a recent study.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Interventions that seek to promptly house homeless individuals might assist in maximizing the clinical and public health benefits of antiretroviral therapy among people living with HIV/AIDS, according to a study in AIDS Care.
MRSA colonization among HIV-infected youth is more closely related to living in a low-income or slum community than to HIV-related clinical factors, according to a study in the Pediatric Infectious Disease Journal.
Marijuana use was not associated with progression to significant liver fibrosis, in a large cohort study of HIV/hepatitis C virus (HCV) co-infected women. Alcohol use may better predict fibrosis progression in HIV/HCV co-infected women, the authors said.
More than 60% of deaths occurring in a rural South African community between 1992 and 2013 could be attributed directly or indirectly to HIV, according to a recent study. However, the authors noted that there has been an increasing level of non-HIV mortality, which has important implications for local health care provision.
A study in AIDS Care found that providers value same-day, electronic, patient-reported measures for use in clinical HIV care, with the condition that patient-reported outcomes are 1) tailored to be the most clinically relevant to their population; 2) well integrated into clinic flow; and 3) easy to interpret, highlighting chief patient concerns and changes over time.
Investigators found that nasal and salivary samples can be collected from HIV-infected patients in a standardized manner over repeated visits in both low and high resource settings, and these methods may be used in support of future HIV vaccine clinical trials.
A study in the Journal of Infectious Diseases found no intrinsic effect of viral subtype on the efficacy of tenofovir-containing regimens for treating HIV-1 subtype C infections. There were no differences between subtypes C and non-B/C in either univariate or multivariate analysis.
New research provides preliminary evidence that heavy drinking may increase a key inflammatory marker in HIV-infected individuals with suppressed infection.
The phase III Women AntiretroViral Efficacy and Safety study (WAVES) showed that clinical trials of antiretroviral regimens in global and diverse populations of treatment-naive women are possible, investigators concluded. They said their findings support guidelines recommending integrase inhibitor–based regimens in first-line antiretroviral therapy.
A hybrid mobile strategy for HIV testing of adults was leveraged successfully to reach adolescents for HIV treatment and prevention, according to a study in Kenya and Uganda.
With viral suppression induced by combination antiretroviral therapy, women have less reduction in key markers of inflammation and immune activation, compared with men, report the authors of a study in JAIDS.
The transfer of HIV-1-p17-specific T-cell receptors (TCRs) into T-cells is functional both in HIV-1–infected patients and in healthy blood donors, according to a study in the journal AIDS. The authors say TCR-transfer is a promising method to boost the immune system against HIV-1.
HIV-1 subtype C (HIV-1C) exhibits lower in vivo fitness, compared with HIV-1B, which allows successful treatment despite high baseline viral loads, a new study demonstrated. The lower fitness – and potentially lower virulence – together with high viral loads may underlie the heightened transmission potential of HIV-1C and its growing global spread.
Thailand has achieved World Health Organization targets for elimination of mother-to-child-transmission of HIV and can serve as a model for other countries, according to a report in MMWR.
Regular CD4 testing may be unnecessary for virally suppressed children aged 5-15 years with CD4 greater than or equal to 500 cells/mm3, according to a study published in the Journal of the Pediatric Infectious Diseases Society.
Investigators at Case Western Reserve University, Cleveland found that 24 weeks of 10 mg daily rosuvastatin decreases plasma coenzyme Q10 concentration and increases CoQ10/LDL ratio in HIV-infected patients on antiretroviral therapy.
Researchers from the University of California, San Francisco, and Yale University, New Haven, Conn., found that half of people newly infected with HIV experience neurologic issues that are generally not severe and usually resolve after starting antiretroviral therapy.
A study of HIV-infected individuals in metropolitan Washington identified high prevalence of transmitted drug resistance, regardless of gender. The authors said active surveillance for transmitted drug resistance is needed to guide antiretroviral usage and analyses of risk group contributions to HIV transmission and resistance.
Single-nucleotide polymorphisms in genes encoding the Toll-like receptor 4 (TLR4) and CD14 are independently associated with long-term CD4+ T-cell recovery in HIV-infected individuals after antiretroviral therapy, according to a study in the journal AIDS.
In HIV/HCV co-infected individuals, the crude incidence of hepatocellular carcinoma increased from 2001 to 2014, while other liver events declined, according to a recent study.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Interventions that seek to promptly house homeless individuals might assist in maximizing the clinical and public health benefits of antiretroviral therapy among people living with HIV/AIDS, according to a study in AIDS Care.
MRSA colonization among HIV-infected youth is more closely related to living in a low-income or slum community than to HIV-related clinical factors, according to a study in the Pediatric Infectious Disease Journal.
Marijuana use was not associated with progression to significant liver fibrosis, in a large cohort study of HIV/hepatitis C virus (HCV) co-infected women. Alcohol use may better predict fibrosis progression in HIV/HCV co-infected women, the authors said.
More than 60% of deaths occurring in a rural South African community between 1992 and 2013 could be attributed directly or indirectly to HIV, according to a recent study. However, the authors noted that there has been an increasing level of non-HIV mortality, which has important implications for local health care provision.
A study in AIDS Care found that providers value same-day, electronic, patient-reported measures for use in clinical HIV care, with the condition that patient-reported outcomes are 1) tailored to be the most clinically relevant to their population; 2) well integrated into clinic flow; and 3) easy to interpret, highlighting chief patient concerns and changes over time.
Investigators found that nasal and salivary samples can be collected from HIV-infected patients in a standardized manner over repeated visits in both low and high resource settings, and these methods may be used in support of future HIV vaccine clinical trials.
A study in the Journal of Infectious Diseases found no intrinsic effect of viral subtype on the efficacy of tenofovir-containing regimens for treating HIV-1 subtype C infections. There were no differences between subtypes C and non-B/C in either univariate or multivariate analysis.
New research provides preliminary evidence that heavy drinking may increase a key inflammatory marker in HIV-infected individuals with suppressed infection.
The phase III Women AntiretroViral Efficacy and Safety study (WAVES) showed that clinical trials of antiretroviral regimens in global and diverse populations of treatment-naive women are possible, investigators concluded. They said their findings support guidelines recommending integrase inhibitor–based regimens in first-line antiretroviral therapy.
A hybrid mobile strategy for HIV testing of adults was leveraged successfully to reach adolescents for HIV treatment and prevention, according to a study in Kenya and Uganda.
With viral suppression induced by combination antiretroviral therapy, women have less reduction in key markers of inflammation and immune activation, compared with men, report the authors of a study in JAIDS.
The transfer of HIV-1-p17-specific T-cell receptors (TCRs) into T-cells is functional both in HIV-1–infected patients and in healthy blood donors, according to a study in the journal AIDS. The authors say TCR-transfer is a promising method to boost the immune system against HIV-1.
HIV-1 subtype C (HIV-1C) exhibits lower in vivo fitness, compared with HIV-1B, which allows successful treatment despite high baseline viral loads, a new study demonstrated. The lower fitness – and potentially lower virulence – together with high viral loads may underlie the heightened transmission potential of HIV-1C and its growing global spread.
Thailand has achieved World Health Organization targets for elimination of mother-to-child-transmission of HIV and can serve as a model for other countries, according to a report in MMWR.
Regular CD4 testing may be unnecessary for virally suppressed children aged 5-15 years with CD4 greater than or equal to 500 cells/mm3, according to a study published in the Journal of the Pediatric Infectious Diseases Society.
Investigators at Case Western Reserve University, Cleveland found that 24 weeks of 10 mg daily rosuvastatin decreases plasma coenzyme Q10 concentration and increases CoQ10/LDL ratio in HIV-infected patients on antiretroviral therapy.
Researchers from the University of California, San Francisco, and Yale University, New Haven, Conn., found that half of people newly infected with HIV experience neurologic issues that are generally not severe and usually resolve after starting antiretroviral therapy.
A study of HIV-infected individuals in metropolitan Washington identified high prevalence of transmitted drug resistance, regardless of gender. The authors said active surveillance for transmitted drug resistance is needed to guide antiretroviral usage and analyses of risk group contributions to HIV transmission and resistance.
Single-nucleotide polymorphisms in genes encoding the Toll-like receptor 4 (TLR4) and CD14 are independently associated with long-term CD4+ T-cell recovery in HIV-infected individuals after antiretroviral therapy, according to a study in the journal AIDS.
In HIV/HCV co-infected individuals, the crude incidence of hepatocellular carcinoma increased from 2001 to 2014, while other liver events declined, according to a recent study.
On Twitter @richpizzi
Recurrent C. diff infection much more costly to treat
The costs of treating patients with recurrent Clostridium difficile infection are approximately two to three times the treatment costs for patients with primary CDI, according to a study of hospitalized patients in a large tertiary care center.
Kevin W. Garey, Pharm.D., professor of pharmacy practice at the University of Houston College of Pharmacy, and his coauthors wrote in the Journal of Hospital Infection that the introduction of costly therapies, such as the narrow-spectrum macrocyclic antibiotic fidaxomicin and fecal microbiota transplantation, both of which reduce the risk of recurrent CDI, has increased interest in the economic burden of recurrent CDI (J Hosp Infect. 2016 Jul;93:286-9).
Between 2007-2013, Dr. Garey and his colleagues attempted to assess the additional costs of recurrent CDI by calculating total hospital length of stay (LOS), CDI-attributable LOS, and pharmacologic and hospitalization costs for 540 hospitalized adult patients (42% male) with a diagnosis of primary CDI. Of these patients, 95 (18%) experienced 101 recurrent CDI episodes. CDI-attributable hospital admissions occurred in 307 out of 540 (57%) primary CDI episodes, and 64 out of 101 (63%) recurrent CDI episodes.
The investigators estimated total and CDI-attributable hospitalization costs based on Healthcare Cost and Utilization Project data for average daily health care costs, multiplied by the total and CDI-attributable length of hospital stay. They then compared total hospital LOS, CDI-attributable LOS, and pharmacologic and hospitalization costs between patients with primary CDI only versus patients who experienced recurrent CDI.
Dr. Garey and his colleagues found that CDI-attributable median LOS and costs increased from 7 days and $13,168 for patients with primary CDI only, vs .15 days and $28,218 for patients with recurrent CDI (P less than .0001, each). Total hospital median LOS and costs increased from 11 days and $20,693 for patients with primary CDI only, vs. 24 days and $45,148 for patients with recurrent CDI (P less than .0001, each).
The median cost of pharmacologic treatment while hospitalized was $60 for patients with primary CDI only, and $140 for patients with recurrent CDI (P = .0013).
“Patients with CDI experience a significant health care economic burden that can be directly related to CDI,” the authors concluded.
The study was funded by a research grant from Merck. Dr. Garey reported receiving funding from Cubist, Summit, and Merck, while other coauthors reported research support from Merck, Cubist, and Actelion.
On Twitter @richpizzi
The costs of treating patients with recurrent Clostridium difficile infection are approximately two to three times the treatment costs for patients with primary CDI, according to a study of hospitalized patients in a large tertiary care center.
Kevin W. Garey, Pharm.D., professor of pharmacy practice at the University of Houston College of Pharmacy, and his coauthors wrote in the Journal of Hospital Infection that the introduction of costly therapies, such as the narrow-spectrum macrocyclic antibiotic fidaxomicin and fecal microbiota transplantation, both of which reduce the risk of recurrent CDI, has increased interest in the economic burden of recurrent CDI (J Hosp Infect. 2016 Jul;93:286-9).
Between 2007-2013, Dr. Garey and his colleagues attempted to assess the additional costs of recurrent CDI by calculating total hospital length of stay (LOS), CDI-attributable LOS, and pharmacologic and hospitalization costs for 540 hospitalized adult patients (42% male) with a diagnosis of primary CDI. Of these patients, 95 (18%) experienced 101 recurrent CDI episodes. CDI-attributable hospital admissions occurred in 307 out of 540 (57%) primary CDI episodes, and 64 out of 101 (63%) recurrent CDI episodes.
The investigators estimated total and CDI-attributable hospitalization costs based on Healthcare Cost and Utilization Project data for average daily health care costs, multiplied by the total and CDI-attributable length of hospital stay. They then compared total hospital LOS, CDI-attributable LOS, and pharmacologic and hospitalization costs between patients with primary CDI only versus patients who experienced recurrent CDI.
Dr. Garey and his colleagues found that CDI-attributable median LOS and costs increased from 7 days and $13,168 for patients with primary CDI only, vs .15 days and $28,218 for patients with recurrent CDI (P less than .0001, each). Total hospital median LOS and costs increased from 11 days and $20,693 for patients with primary CDI only, vs. 24 days and $45,148 for patients with recurrent CDI (P less than .0001, each).
The median cost of pharmacologic treatment while hospitalized was $60 for patients with primary CDI only, and $140 for patients with recurrent CDI (P = .0013).
“Patients with CDI experience a significant health care economic burden that can be directly related to CDI,” the authors concluded.
The study was funded by a research grant from Merck. Dr. Garey reported receiving funding from Cubist, Summit, and Merck, while other coauthors reported research support from Merck, Cubist, and Actelion.
On Twitter @richpizzi
The costs of treating patients with recurrent Clostridium difficile infection are approximately two to three times the treatment costs for patients with primary CDI, according to a study of hospitalized patients in a large tertiary care center.
Kevin W. Garey, Pharm.D., professor of pharmacy practice at the University of Houston College of Pharmacy, and his coauthors wrote in the Journal of Hospital Infection that the introduction of costly therapies, such as the narrow-spectrum macrocyclic antibiotic fidaxomicin and fecal microbiota transplantation, both of which reduce the risk of recurrent CDI, has increased interest in the economic burden of recurrent CDI (J Hosp Infect. 2016 Jul;93:286-9).
Between 2007-2013, Dr. Garey and his colleagues attempted to assess the additional costs of recurrent CDI by calculating total hospital length of stay (LOS), CDI-attributable LOS, and pharmacologic and hospitalization costs for 540 hospitalized adult patients (42% male) with a diagnosis of primary CDI. Of these patients, 95 (18%) experienced 101 recurrent CDI episodes. CDI-attributable hospital admissions occurred in 307 out of 540 (57%) primary CDI episodes, and 64 out of 101 (63%) recurrent CDI episodes.
The investigators estimated total and CDI-attributable hospitalization costs based on Healthcare Cost and Utilization Project data for average daily health care costs, multiplied by the total and CDI-attributable length of hospital stay. They then compared total hospital LOS, CDI-attributable LOS, and pharmacologic and hospitalization costs between patients with primary CDI only versus patients who experienced recurrent CDI.
Dr. Garey and his colleagues found that CDI-attributable median LOS and costs increased from 7 days and $13,168 for patients with primary CDI only, vs .15 days and $28,218 for patients with recurrent CDI (P less than .0001, each). Total hospital median LOS and costs increased from 11 days and $20,693 for patients with primary CDI only, vs. 24 days and $45,148 for patients with recurrent CDI (P less than .0001, each).
The median cost of pharmacologic treatment while hospitalized was $60 for patients with primary CDI only, and $140 for patients with recurrent CDI (P = .0013).
“Patients with CDI experience a significant health care economic burden that can be directly related to CDI,” the authors concluded.
The study was funded by a research grant from Merck. Dr. Garey reported receiving funding from Cubist, Summit, and Merck, while other coauthors reported research support from Merck, Cubist, and Actelion.
On Twitter @richpizzi
FROM THE JOURNAL OF HOSPITAL INFECTION
Key clinical point: The economic cost burden increased significantly for patients with recurrent C. difficile infections, compared with patients with primary CDI.
Major finding: Median hospital length of stay and costs attributable to C. difficile infections increased from 7 days and $13,168 for patients with primary CDI only, vs. 15 days and $28,218 for patients with recurrent CDI.
Data source: A prospective, observational cohort study of 540 hospitalized adult patients with primary CDI followed for 3 months to assess for recurrent CDI episodes.
Disclosures: The study was funded by a research grant from Merck. Dr. Garey reported receiving funding from Cubist, Summit, and Merck, while other coauthors reported research support from Merck, Cubist, and Actelion.
FDA approves first cholera vaccine for travelers
The Food and Drug Administration has approved a vaccine for the prevention of cholera caused by serogroup O1 in adults aged 18-64 years traveling to cholera-affected areas.
The vaccine, known as Vaxchora and manufactured by PaxVax, in Hamilton, Bermuda, is the only FDA-approved vaccinefor the prevention of cholera. According to the World Health Organization, serogroup O1 is the predominant cause of cholera globally.
“The approval of Vaxchora represents a significant addition to the cholera-prevention measures currently recommended by the Centers for Disease Control and Prevention for travelers to cholera-affected regions,” said Dr. Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research, in a statement.
According to the FDA announcement, Vaxchora is a live, weakened vaccine that is taken as a single, oral liquid dose of approximately 3 fluid ounces at least 10 days before travel to a cholera-affected area. The FDA stated that the effectiveness of Vaxchora has not been established in persons living in cholera-affected areas.
The FDA said the vaccine’s efficacy was demonstrated in a randomized, placebo-controlled human challenge study of 197 U.S. volunteers from aged 18-45 years. Of the 197 volunteers, 68 Vaxchora recipients and 66 placebo recipients were challenged by oral ingestion of Vibrio cholerae, the bacterium that causes cholera. Vaxchora’s efficacy was 90% among those challenged 10 days after vaccination and 80% among those challenged 3 months after vaccination.
The Vaxchora application was granted fast track designation and priority review status by the FDA. The agency awarded PaxVax a tropical disease priority review voucher, which encourages the development of new drugs and biological products for the prevention and treatment of certain tropical diseases.
In addition to the primary human challenge study, PaxVax conducted two placebo-controlled studies to assess immune system response in the United States and Australia in adults aged 18-64 years. According to the FDA, in the group aged 18-45 years, 93% of Vaxchora recipients produced antibodies indicative of protection against cholera, while in the group aged 46-64 years, 90% produced antibodies indicative of protection against cholera.
The FDA revealed that the safety of Vaxchora was evaluated in adults aged 18-64 years in four randomized, placebo-controlled, multicenter clinical trials; 3,235 study participants received Vaxchora and 562 received a placebo. The most common adverse reactions reported by Vaxchora recipients were tiredness, headache, abdominal pain, nausea/vomiting, lack of appetite, and diarrhea.
On Twitter @richpizzi
The Food and Drug Administration has approved a vaccine for the prevention of cholera caused by serogroup O1 in adults aged 18-64 years traveling to cholera-affected areas.
The vaccine, known as Vaxchora and manufactured by PaxVax, in Hamilton, Bermuda, is the only FDA-approved vaccinefor the prevention of cholera. According to the World Health Organization, serogroup O1 is the predominant cause of cholera globally.
“The approval of Vaxchora represents a significant addition to the cholera-prevention measures currently recommended by the Centers for Disease Control and Prevention for travelers to cholera-affected regions,” said Dr. Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research, in a statement.
According to the FDA announcement, Vaxchora is a live, weakened vaccine that is taken as a single, oral liquid dose of approximately 3 fluid ounces at least 10 days before travel to a cholera-affected area. The FDA stated that the effectiveness of Vaxchora has not been established in persons living in cholera-affected areas.
The FDA said the vaccine’s efficacy was demonstrated in a randomized, placebo-controlled human challenge study of 197 U.S. volunteers from aged 18-45 years. Of the 197 volunteers, 68 Vaxchora recipients and 66 placebo recipients were challenged by oral ingestion of Vibrio cholerae, the bacterium that causes cholera. Vaxchora’s efficacy was 90% among those challenged 10 days after vaccination and 80% among those challenged 3 months after vaccination.
The Vaxchora application was granted fast track designation and priority review status by the FDA. The agency awarded PaxVax a tropical disease priority review voucher, which encourages the development of new drugs and biological products for the prevention and treatment of certain tropical diseases.
In addition to the primary human challenge study, PaxVax conducted two placebo-controlled studies to assess immune system response in the United States and Australia in adults aged 18-64 years. According to the FDA, in the group aged 18-45 years, 93% of Vaxchora recipients produced antibodies indicative of protection against cholera, while in the group aged 46-64 years, 90% produced antibodies indicative of protection against cholera.
The FDA revealed that the safety of Vaxchora was evaluated in adults aged 18-64 years in four randomized, placebo-controlled, multicenter clinical trials; 3,235 study participants received Vaxchora and 562 received a placebo. The most common adverse reactions reported by Vaxchora recipients were tiredness, headache, abdominal pain, nausea/vomiting, lack of appetite, and diarrhea.
On Twitter @richpizzi
The Food and Drug Administration has approved a vaccine for the prevention of cholera caused by serogroup O1 in adults aged 18-64 years traveling to cholera-affected areas.
The vaccine, known as Vaxchora and manufactured by PaxVax, in Hamilton, Bermuda, is the only FDA-approved vaccinefor the prevention of cholera. According to the World Health Organization, serogroup O1 is the predominant cause of cholera globally.
“The approval of Vaxchora represents a significant addition to the cholera-prevention measures currently recommended by the Centers for Disease Control and Prevention for travelers to cholera-affected regions,” said Dr. Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research, in a statement.
According to the FDA announcement, Vaxchora is a live, weakened vaccine that is taken as a single, oral liquid dose of approximately 3 fluid ounces at least 10 days before travel to a cholera-affected area. The FDA stated that the effectiveness of Vaxchora has not been established in persons living in cholera-affected areas.
The FDA said the vaccine’s efficacy was demonstrated in a randomized, placebo-controlled human challenge study of 197 U.S. volunteers from aged 18-45 years. Of the 197 volunteers, 68 Vaxchora recipients and 66 placebo recipients were challenged by oral ingestion of Vibrio cholerae, the bacterium that causes cholera. Vaxchora’s efficacy was 90% among those challenged 10 days after vaccination and 80% among those challenged 3 months after vaccination.
The Vaxchora application was granted fast track designation and priority review status by the FDA. The agency awarded PaxVax a tropical disease priority review voucher, which encourages the development of new drugs and biological products for the prevention and treatment of certain tropical diseases.
In addition to the primary human challenge study, PaxVax conducted two placebo-controlled studies to assess immune system response in the United States and Australia in adults aged 18-64 years. According to the FDA, in the group aged 18-45 years, 93% of Vaxchora recipients produced antibodies indicative of protection against cholera, while in the group aged 46-64 years, 90% produced antibodies indicative of protection against cholera.
The FDA revealed that the safety of Vaxchora was evaluated in adults aged 18-64 years in four randomized, placebo-controlled, multicenter clinical trials; 3,235 study participants received Vaxchora and 562 received a placebo. The most common adverse reactions reported by Vaxchora recipients were tiredness, headache, abdominal pain, nausea/vomiting, lack of appetite, and diarrhea.
On Twitter @richpizzi