User login
Standardized Sign-Outs: An Opportunity to Improve Patient Safety
Emergency physicians routinely perform sign-outs (also referred to as handoffs and handovers) at shift changes and during consultations. Despite their frequency, however, sign-outs continue to be cited as a significant source of medical error in the ED.1
Sign-outs should take place in a quiet area of the hospital, with no distractions, and should allot sufficient time to discuss pertinent aspects of patient care. Unfortunately, this ideal handover process is particularly difficult to achieve in the ED.2-4 Moreover, to date, only a few sign-out studies have evaluated empirical evidence for improved patient care.5
Formal Instruction
Despite multiple studies supporting the implementation of a standardized sign-out process,1,6,7 a 2013 study by Kessler et al4 showed that only 10.9% of US emergency medicine (EM) residents reported receiving hand-off education.4 This number is consistent with the 93.9% of EM program directors who stated that assessments of hand-off proficiencies were not conducted in their US programs.4
In a survey conducted by Sinha et al, 8 only 25.6% of EM residency and pediatric EM fellowship directors reported any formal instruction on sign-outs—even though handoff education is a required component of resident patient safety education in the Clinical Learning Environment Review Program sponsored by the Accreditation Council for Graduate Medical Education in 2011.9
A stronger foundation in quality sign-outs during residency will likely enhance patient care. For example, Horwitz et al10 showed that 29% of house staff had a patient who experienced an adverse event after an ED-to-inpatient transfer. Contributing factors, including inaccurate or incomplete information, can potentially be corrected with a better sign-out process. 10
Sign-Out Tools
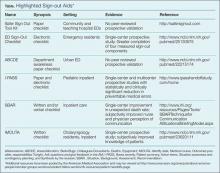
To improve the sign-out process and patient outcomes and experiences, one of the recommendations from the 2012 American College of Emergency Physicians (ACEP) Transitions of Care Task Force Report calls for collaboration with the Society of Hospitalist Medicine to hardwire a process between the EP and hospitalist.11 Since this report, several sign-out materials have become available and are accessible from various organizations. The Table highlights a list of sign-out methods applicable to the ED as well as other hospital departments.
Safer Sign-Out Tool Kit
The most publicized ED tool is Safer Sign Out from the Emergency Medicine Patient Safety Foundation (EMPSF), a third-party nonprofit organization founded in 2003.12 Safer Sign Out focuses on using a physical checklist, dedicated time to sign-out, bidirectional communication, and confirmation of the sign-out with staff. The EMPSF provides all of the necessities to implement their sign-out tool department-wide, including training videos and pre- and postsurveys, in addition to the tool itself. The kit costs $1,695 to implement at a single site.12 Although widely publicized, this toolkit has not yet been externally validated in the peer-reviewed literature.
Sign-Out Checklist
On a smaller scale, Dubosh et al13 recently found success using a sign-out checklist with residents in the ED at a single institution (See Box). The components of their checklist included history of present illness (HPI), ED course, pending studies, likely disposition, possible issues, and algorithms for disposition. In this study, trained research assistants monitored the sign-outs before and after implementation of the checklist. There were statistically significant improvements in the areas of HPI, ED course, possible diagnosis, and team awareness of the treatment plan. Of note, there was no difference in the amount of time required for sign-out with and without the checklist (1.42 vs 1.39 minutes, respectively).13 (See the Box for a convenient pocket-sized reproduction of the sign-out tool.)
ABC of Handover Tool
Developed in the United Kingdom, the ABC of Handover tool was specifically designed for use in the ED. This tool focuses on departmental awareness prior to specific patient sign-outs. The full-sheet paper checklist includes bed allocations in the ED and the hospital; available colleagues and consultants; a list of any deaths or dangerously ill patients; and equipment review. .14 The ABC of Handover tool is essentially a preamble to patient specifics compiled by surveying ED staff and attending physicians at a single urban center. It has not yet been validated in the peer-reviewed literature.14
ACEP Recommendations
Although ACEP does not endorse a particular sign-out tool,11 its Section of Quality Improvement and Patient Safety created a framework of ED sign-outs and recommendations in which EPs should adhere to the following protocol:
- Limit unnecessary patient handoffs;
- Limit interruptions and distractions during sign-out;
- Provide a succinct overview; </lli>
- Highlight remaining tasks, plans, and possible changes for each patient;
- Have laboratory and imaging studies available during sign-out;
- Encourage bidirectional discourse about the assessments and treatment plans;
- Account for all patients; and
- Clearly signal the moment of full-care transfer.
I-PASS Handoff System
The I-PASS Handoff System is a landmark multicenter pediatric intervention largely funded by the US Department of Health and Human Services. The mnemonic I-PASS stands for the following:
- Illness severity;
- Patient summary;
- Action items;
- Situation awareness and contingency planning; and
- Synthesis by the receiver.
This system is part of a complete curriculum for pediatrics residents published in 2014.15 Single-center prospective validation found a 45.9% relative risk reduction in preventable medical errors without an increase in verbal sign-out length (32.3 minutes before the intervention vs 33.3 minutes after the intervention).6 This was confirmed in a multicenter prospective validation that found a 23% relative reduction in preventable medical errors—also without a change in sign-out length with versus without the tool (2.4 minutes vs 2.5 minutes, respectively).16 The bundle and curriculum are available for free and may be accessed online.15
SBAR Tool
The Situation, Background, Assessment, and Recommendation (SBAR) is the time-honored tool most well known in nursing—one that is of benefit to physicians as well.17 In one study, SBAR demonstrated a reduction in unexpected deaths hospital-wide at a single institution when nurses used it to communicate with physicians.18 Additional support, however, is largely based on nurse and physician perception of improved communication and more thorough handoffs.19,20
Format and Outcomes
The format of a sign-out does not appear to influence outcomes, though acronyms and mnemonics appear effective—eg, I-PASS,16 SBAR,17 and IMOUTA21 (an otolaryngology resident tool that stands for identifying data, medical course, outcomes possible tonight, and responsibilities to do tonight). Riesenberg et al5 provide an overview of 24 different mnemonics described in the handoff literature.
In addition to mnemonic tools, paper pocket cards22 and electronic medical record prompts13 also appear effective. Regardless of which tool is employed, the common theme is practice standardization with dedicated time for open commun¬ication.
Practical Challenges
Aside from standardization, there are numerous other factors that can lead to a poor sign-out experience in the ED. These include a loud and disruptive background; the uncertainty of who the charge physician is post-sign-out when both are still physically present; lack of “red flags” that help identify dangerous hand-offs; the goal to be concise; and the economic structure of the physician group.1,5 These systems issues each need to be addressed; however, a standardized hand-off can decrease the margin of error and is relatively easy to implement.
Conclusion
Sign-outs are central to patient care, especially in the ED. Achieving the most effective sign-outs possible is of paramount importance and is deeply supported by respected physician groups.11,12,17,23 Several ED-specific standardized sign-outs exist with varying emphases and empirical support. The method with the most empirical support is the pediatrics initiative, I-PASS, and is one that should be considered by EPs and departments when selecting a standardized method. Even if a department is not adopting a particular method, individual clinicians can implement a standardized sign-out in their own daily practice—beginning with the next shift. A safe and effective sign-out in a reasonable timeframe in a busy ED is not only possible, but imperative.
Dr Phillips is a senior resident in the Stanford/Kaiser Emergency Medicine Residency, Stanford University School of Medicine, California. Mr Malamet is a fourth-year medical student at Philadelphia College of Osteopathic Medicine, Pennsylvania. Dr Williams is the associate program director for the Stanford/Kaiser Emergency Medicine Residency and a clinical associate professor, Surgery - Emergency Medicine at Stanford University School of Medicine, California.
Disclosure Statement: The authors express no conflicts of interest. The views expressed in this article are those of the author and do not represent the official position of the US Air Force, Department of Defense, or US Government.
- Cheung DS, Kelly JJ, Beach C, et al; Section of Quality Improvement and Patient Safety, American College of Emergency Physicians. Improving handoffs in the emergency department. Ann Emerg Med. 2010;55(2):171-802.
- Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Qual Saf Health Care. 2010;19(6):493-497.
- Kessler C, Shakeel F, Hern HG, et al. A survey of handoff practices in emergency medicine. Am J Med Qual. 2014;29(5):408-414.
- Kessler C, Shakeel F, Hern HG, et al. An algorithm for transition of care in the emergency department. Acad Emerg Med. 2013;20(6):605-610.
- Riesenberg LA, Leitzsch J, Massucci JL, et al. Residents’ and attending physicians’ handoffs: a systematic review of the literature. Acad Med. 2009;84(12):1775-1787.
- Starmer AJ, Sectish TC, Simon DW, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262-2270.
- Dhingra KR, Elms A, Hobgood C. Reducing error in the emergency department: a call for standardization of the sign-out process. Ann Emerg Med. 2010;56(6):637-642.
- Sinha M, Shriki J, Salness R, Blackburn PA. Need for standardized sign-out in the emergency department: a survey of emergency medicine residency and pediatric emergency medicine fellowship program directors. Acad Emerg Med. 2007;14(2):192-196.
- Accreditation Council For Graduate Medical Education Web site. Clinical Learning Environment Review (CLER) Program. www.acgme.org/CLER/. Accessed March 3, 2015.
- Horwitz LI, Meredith T, Schuur JD, Shah NR, Kulkarni RG, Jenq GY. Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med. 2009;53(6):701-10.e4.
- Jacquis WP, Kaplan JA, Carpenter C, et al; American College of Emergency Physicians Transitions of Care Task Force. Transitions of Care Task Force Report, 2012. http://www.acep.org/transitionsofcare/. Accessed March 3, 2015.
- Emergency Medicine Patient Safety Foundation. Safer Sign Out Tool Kit. safersignoutcom. Available at: http://safersignout.com/. Accessed March 3, 2015.
- Dubosh NM, Carney D, Fisher J, Tibbles CD. Implementation of an emergency department sign-out checklist improves transfer of information at shift change. J Emerg Med. 2014;47(5):580-585.
- Farhan M, Brown R, Woloshynowych M, Vincent C. The ABC of handover: a qualitative study to develop a new tool for handover in the emergency department. Emerg Med. 2012;29(12):941-946.
- Starmer AJ, O’Toole JK, Rosenbluth G, et al; I-PASS Study Education Executive Committee. Development, implementation, and dissemination of the I-PASS handoff curriculum: A multisite educational intervention to improve patient handoffs. Acad Med. 2014;89(6):876-884.
- Starmer AJ, Spector ND, Srivastava R, et al; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812.
- Institute for Healthcare Improvement. SBAR Technique for Communication: A Situational Briefing Model. http://www.ihi.org/resources/Pages/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.aspx. Accessed March 3, 2015.
- De Meester K, Verspuy M, Monsieurs KG, Van Bogaert P. SBAR improves nurse-physician communication and reduces unexpected death: A pre and post intervention study. Resuscitation. 2013;84(9):1192-1196.
- Randmaa M, Mårtensson G, Leo Swenne C, Engström M. SBAR improves communication and safety climate and decreases incident reports due to communication errors in an anaesthetic clinic: a prospective intervention study. BMJ Open. 2014;4(1):e004268.
- Panesar RS, Albert B, Messina C, Parker M. The effect of an electronic SBAR communication tool on documentation of acute events in the pediatric intensive care unit. Am J Med Qual. 2014. doi:10.1177/1062860614553263.
- Connor MP, Bush AC, Brennan J. IMOUTA: a proposal for patient care handoffs. Laryngoscope. 2013;123(11):2649-2653.
- Bavare AC, Shah PK, Roy KM, Williams EA, Lloyd LE, McPherson ML. Implementation of a Standard Verbal Sign-Out Template Improves Sign-Out Process in a Pediatric Intensive Care Unit. J Healthc Qual. 2013:1-9.
- American Medical Association Web site. Resources for improving patient handoffs. Available at: http://www.ama-assn.org/ama/pub/about-ama/our-people/member-groups-sections/resident-fellow-section/rfs-resources/patient-handoffs.page. Accessed March 3, 2015.
Emergency physicians routinely perform sign-outs (also referred to as handoffs and handovers) at shift changes and during consultations. Despite their frequency, however, sign-outs continue to be cited as a significant source of medical error in the ED.1
Sign-outs should take place in a quiet area of the hospital, with no distractions, and should allot sufficient time to discuss pertinent aspects of patient care. Unfortunately, this ideal handover process is particularly difficult to achieve in the ED.2-4 Moreover, to date, only a few sign-out studies have evaluated empirical evidence for improved patient care.5
Formal Instruction
Despite multiple studies supporting the implementation of a standardized sign-out process,1,6,7 a 2013 study by Kessler et al4 showed that only 10.9% of US emergency medicine (EM) residents reported receiving hand-off education.4 This number is consistent with the 93.9% of EM program directors who stated that assessments of hand-off proficiencies were not conducted in their US programs.4
In a survey conducted by Sinha et al, 8 only 25.6% of EM residency and pediatric EM fellowship directors reported any formal instruction on sign-outs—even though handoff education is a required component of resident patient safety education in the Clinical Learning Environment Review Program sponsored by the Accreditation Council for Graduate Medical Education in 2011.9
A stronger foundation in quality sign-outs during residency will likely enhance patient care. For example, Horwitz et al10 showed that 29% of house staff had a patient who experienced an adverse event after an ED-to-inpatient transfer. Contributing factors, including inaccurate or incomplete information, can potentially be corrected with a better sign-out process. 10
Sign-Out Tools
To improve the sign-out process and patient outcomes and experiences, one of the recommendations from the 2012 American College of Emergency Physicians (ACEP) Transitions of Care Task Force Report calls for collaboration with the Society of Hospitalist Medicine to hardwire a process between the EP and hospitalist.11 Since this report, several sign-out materials have become available and are accessible from various organizations. The Table highlights a list of sign-out methods applicable to the ED as well as other hospital departments.
Safer Sign-Out Tool Kit
The most publicized ED tool is Safer Sign Out from the Emergency Medicine Patient Safety Foundation (EMPSF), a third-party nonprofit organization founded in 2003.12 Safer Sign Out focuses on using a physical checklist, dedicated time to sign-out, bidirectional communication, and confirmation of the sign-out with staff. The EMPSF provides all of the necessities to implement their sign-out tool department-wide, including training videos and pre- and postsurveys, in addition to the tool itself. The kit costs $1,695 to implement at a single site.12 Although widely publicized, this toolkit has not yet been externally validated in the peer-reviewed literature.
Sign-Out Checklist
On a smaller scale, Dubosh et al13 recently found success using a sign-out checklist with residents in the ED at a single institution (See Box). The components of their checklist included history of present illness (HPI), ED course, pending studies, likely disposition, possible issues, and algorithms for disposition. In this study, trained research assistants monitored the sign-outs before and after implementation of the checklist. There were statistically significant improvements in the areas of HPI, ED course, possible diagnosis, and team awareness of the treatment plan. Of note, there was no difference in the amount of time required for sign-out with and without the checklist (1.42 vs 1.39 minutes, respectively).13 (See the Box for a convenient pocket-sized reproduction of the sign-out tool.)
ABC of Handover Tool
Developed in the United Kingdom, the ABC of Handover tool was specifically designed for use in the ED. This tool focuses on departmental awareness prior to specific patient sign-outs. The full-sheet paper checklist includes bed allocations in the ED and the hospital; available colleagues and consultants; a list of any deaths or dangerously ill patients; and equipment review. .14 The ABC of Handover tool is essentially a preamble to patient specifics compiled by surveying ED staff and attending physicians at a single urban center. It has not yet been validated in the peer-reviewed literature.14
ACEP Recommendations
Although ACEP does not endorse a particular sign-out tool,11 its Section of Quality Improvement and Patient Safety created a framework of ED sign-outs and recommendations in which EPs should adhere to the following protocol:
- Limit unnecessary patient handoffs;
- Limit interruptions and distractions during sign-out;
- Provide a succinct overview; </lli>
- Highlight remaining tasks, plans, and possible changes for each patient;
- Have laboratory and imaging studies available during sign-out;
- Encourage bidirectional discourse about the assessments and treatment plans;
- Account for all patients; and
- Clearly signal the moment of full-care transfer.
I-PASS Handoff System
The I-PASS Handoff System is a landmark multicenter pediatric intervention largely funded by the US Department of Health and Human Services. The mnemonic I-PASS stands for the following:
- Illness severity;
- Patient summary;
- Action items;
- Situation awareness and contingency planning; and
- Synthesis by the receiver.
This system is part of a complete curriculum for pediatrics residents published in 2014.15 Single-center prospective validation found a 45.9% relative risk reduction in preventable medical errors without an increase in verbal sign-out length (32.3 minutes before the intervention vs 33.3 minutes after the intervention).6 This was confirmed in a multicenter prospective validation that found a 23% relative reduction in preventable medical errors—also without a change in sign-out length with versus without the tool (2.4 minutes vs 2.5 minutes, respectively).16 The bundle and curriculum are available for free and may be accessed online.15
SBAR Tool
The Situation, Background, Assessment, and Recommendation (SBAR) is the time-honored tool most well known in nursing—one that is of benefit to physicians as well.17 In one study, SBAR demonstrated a reduction in unexpected deaths hospital-wide at a single institution when nurses used it to communicate with physicians.18 Additional support, however, is largely based on nurse and physician perception of improved communication and more thorough handoffs.19,20
Format and Outcomes
The format of a sign-out does not appear to influence outcomes, though acronyms and mnemonics appear effective—eg, I-PASS,16 SBAR,17 and IMOUTA21 (an otolaryngology resident tool that stands for identifying data, medical course, outcomes possible tonight, and responsibilities to do tonight). Riesenberg et al5 provide an overview of 24 different mnemonics described in the handoff literature.
In addition to mnemonic tools, paper pocket cards22 and electronic medical record prompts13 also appear effective. Regardless of which tool is employed, the common theme is practice standardization with dedicated time for open commun¬ication.
Practical Challenges
Aside from standardization, there are numerous other factors that can lead to a poor sign-out experience in the ED. These include a loud and disruptive background; the uncertainty of who the charge physician is post-sign-out when both are still physically present; lack of “red flags” that help identify dangerous hand-offs; the goal to be concise; and the economic structure of the physician group.1,5 These systems issues each need to be addressed; however, a standardized hand-off can decrease the margin of error and is relatively easy to implement.
Conclusion
Sign-outs are central to patient care, especially in the ED. Achieving the most effective sign-outs possible is of paramount importance and is deeply supported by respected physician groups.11,12,17,23 Several ED-specific standardized sign-outs exist with varying emphases and empirical support. The method with the most empirical support is the pediatrics initiative, I-PASS, and is one that should be considered by EPs and departments when selecting a standardized method. Even if a department is not adopting a particular method, individual clinicians can implement a standardized sign-out in their own daily practice—beginning with the next shift. A safe and effective sign-out in a reasonable timeframe in a busy ED is not only possible, but imperative.
Dr Phillips is a senior resident in the Stanford/Kaiser Emergency Medicine Residency, Stanford University School of Medicine, California. Mr Malamet is a fourth-year medical student at Philadelphia College of Osteopathic Medicine, Pennsylvania. Dr Williams is the associate program director for the Stanford/Kaiser Emergency Medicine Residency and a clinical associate professor, Surgery - Emergency Medicine at Stanford University School of Medicine, California.
Disclosure Statement: The authors express no conflicts of interest. The views expressed in this article are those of the author and do not represent the official position of the US Air Force, Department of Defense, or US Government.
Emergency physicians routinely perform sign-outs (also referred to as handoffs and handovers) at shift changes and during consultations. Despite their frequency, however, sign-outs continue to be cited as a significant source of medical error in the ED.1
Sign-outs should take place in a quiet area of the hospital, with no distractions, and should allot sufficient time to discuss pertinent aspects of patient care. Unfortunately, this ideal handover process is particularly difficult to achieve in the ED.2-4 Moreover, to date, only a few sign-out studies have evaluated empirical evidence for improved patient care.5
Formal Instruction
Despite multiple studies supporting the implementation of a standardized sign-out process,1,6,7 a 2013 study by Kessler et al4 showed that only 10.9% of US emergency medicine (EM) residents reported receiving hand-off education.4 This number is consistent with the 93.9% of EM program directors who stated that assessments of hand-off proficiencies were not conducted in their US programs.4
In a survey conducted by Sinha et al, 8 only 25.6% of EM residency and pediatric EM fellowship directors reported any formal instruction on sign-outs—even though handoff education is a required component of resident patient safety education in the Clinical Learning Environment Review Program sponsored by the Accreditation Council for Graduate Medical Education in 2011.9
A stronger foundation in quality sign-outs during residency will likely enhance patient care. For example, Horwitz et al10 showed that 29% of house staff had a patient who experienced an adverse event after an ED-to-inpatient transfer. Contributing factors, including inaccurate or incomplete information, can potentially be corrected with a better sign-out process. 10
Sign-Out Tools
To improve the sign-out process and patient outcomes and experiences, one of the recommendations from the 2012 American College of Emergency Physicians (ACEP) Transitions of Care Task Force Report calls for collaboration with the Society of Hospitalist Medicine to hardwire a process between the EP and hospitalist.11 Since this report, several sign-out materials have become available and are accessible from various organizations. The Table highlights a list of sign-out methods applicable to the ED as well as other hospital departments.
Safer Sign-Out Tool Kit
The most publicized ED tool is Safer Sign Out from the Emergency Medicine Patient Safety Foundation (EMPSF), a third-party nonprofit organization founded in 2003.12 Safer Sign Out focuses on using a physical checklist, dedicated time to sign-out, bidirectional communication, and confirmation of the sign-out with staff. The EMPSF provides all of the necessities to implement their sign-out tool department-wide, including training videos and pre- and postsurveys, in addition to the tool itself. The kit costs $1,695 to implement at a single site.12 Although widely publicized, this toolkit has not yet been externally validated in the peer-reviewed literature.
Sign-Out Checklist
On a smaller scale, Dubosh et al13 recently found success using a sign-out checklist with residents in the ED at a single institution (See Box). The components of their checklist included history of present illness (HPI), ED course, pending studies, likely disposition, possible issues, and algorithms for disposition. In this study, trained research assistants monitored the sign-outs before and after implementation of the checklist. There were statistically significant improvements in the areas of HPI, ED course, possible diagnosis, and team awareness of the treatment plan. Of note, there was no difference in the amount of time required for sign-out with and without the checklist (1.42 vs 1.39 minutes, respectively).13 (See the Box for a convenient pocket-sized reproduction of the sign-out tool.)
ABC of Handover Tool
Developed in the United Kingdom, the ABC of Handover tool was specifically designed for use in the ED. This tool focuses on departmental awareness prior to specific patient sign-outs. The full-sheet paper checklist includes bed allocations in the ED and the hospital; available colleagues and consultants; a list of any deaths or dangerously ill patients; and equipment review. .14 The ABC of Handover tool is essentially a preamble to patient specifics compiled by surveying ED staff and attending physicians at a single urban center. It has not yet been validated in the peer-reviewed literature.14
ACEP Recommendations
Although ACEP does not endorse a particular sign-out tool,11 its Section of Quality Improvement and Patient Safety created a framework of ED sign-outs and recommendations in which EPs should adhere to the following protocol:
- Limit unnecessary patient handoffs;
- Limit interruptions and distractions during sign-out;
- Provide a succinct overview; </lli>
- Highlight remaining tasks, plans, and possible changes for each patient;
- Have laboratory and imaging studies available during sign-out;
- Encourage bidirectional discourse about the assessments and treatment plans;
- Account for all patients; and
- Clearly signal the moment of full-care transfer.
I-PASS Handoff System
The I-PASS Handoff System is a landmark multicenter pediatric intervention largely funded by the US Department of Health and Human Services. The mnemonic I-PASS stands for the following:
- Illness severity;
- Patient summary;
- Action items;
- Situation awareness and contingency planning; and
- Synthesis by the receiver.
This system is part of a complete curriculum for pediatrics residents published in 2014.15 Single-center prospective validation found a 45.9% relative risk reduction in preventable medical errors without an increase in verbal sign-out length (32.3 minutes before the intervention vs 33.3 minutes after the intervention).6 This was confirmed in a multicenter prospective validation that found a 23% relative reduction in preventable medical errors—also without a change in sign-out length with versus without the tool (2.4 minutes vs 2.5 minutes, respectively).16 The bundle and curriculum are available for free and may be accessed online.15
SBAR Tool
The Situation, Background, Assessment, and Recommendation (SBAR) is the time-honored tool most well known in nursing—one that is of benefit to physicians as well.17 In one study, SBAR demonstrated a reduction in unexpected deaths hospital-wide at a single institution when nurses used it to communicate with physicians.18 Additional support, however, is largely based on nurse and physician perception of improved communication and more thorough handoffs.19,20
Format and Outcomes
The format of a sign-out does not appear to influence outcomes, though acronyms and mnemonics appear effective—eg, I-PASS,16 SBAR,17 and IMOUTA21 (an otolaryngology resident tool that stands for identifying data, medical course, outcomes possible tonight, and responsibilities to do tonight). Riesenberg et al5 provide an overview of 24 different mnemonics described in the handoff literature.
In addition to mnemonic tools, paper pocket cards22 and electronic medical record prompts13 also appear effective. Regardless of which tool is employed, the common theme is practice standardization with dedicated time for open commun¬ication.
Practical Challenges
Aside from standardization, there are numerous other factors that can lead to a poor sign-out experience in the ED. These include a loud and disruptive background; the uncertainty of who the charge physician is post-sign-out when both are still physically present; lack of “red flags” that help identify dangerous hand-offs; the goal to be concise; and the economic structure of the physician group.1,5 These systems issues each need to be addressed; however, a standardized hand-off can decrease the margin of error and is relatively easy to implement.
Conclusion
Sign-outs are central to patient care, especially in the ED. Achieving the most effective sign-outs possible is of paramount importance and is deeply supported by respected physician groups.11,12,17,23 Several ED-specific standardized sign-outs exist with varying emphases and empirical support. The method with the most empirical support is the pediatrics initiative, I-PASS, and is one that should be considered by EPs and departments when selecting a standardized method. Even if a department is not adopting a particular method, individual clinicians can implement a standardized sign-out in their own daily practice—beginning with the next shift. A safe and effective sign-out in a reasonable timeframe in a busy ED is not only possible, but imperative.
Dr Phillips is a senior resident in the Stanford/Kaiser Emergency Medicine Residency, Stanford University School of Medicine, California. Mr Malamet is a fourth-year medical student at Philadelphia College of Osteopathic Medicine, Pennsylvania. Dr Williams is the associate program director for the Stanford/Kaiser Emergency Medicine Residency and a clinical associate professor, Surgery - Emergency Medicine at Stanford University School of Medicine, California.
Disclosure Statement: The authors express no conflicts of interest. The views expressed in this article are those of the author and do not represent the official position of the US Air Force, Department of Defense, or US Government.
- Cheung DS, Kelly JJ, Beach C, et al; Section of Quality Improvement and Patient Safety, American College of Emergency Physicians. Improving handoffs in the emergency department. Ann Emerg Med. 2010;55(2):171-802.
- Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Qual Saf Health Care. 2010;19(6):493-497.
- Kessler C, Shakeel F, Hern HG, et al. A survey of handoff practices in emergency medicine. Am J Med Qual. 2014;29(5):408-414.
- Kessler C, Shakeel F, Hern HG, et al. An algorithm for transition of care in the emergency department. Acad Emerg Med. 2013;20(6):605-610.
- Riesenberg LA, Leitzsch J, Massucci JL, et al. Residents’ and attending physicians’ handoffs: a systematic review of the literature. Acad Med. 2009;84(12):1775-1787.
- Starmer AJ, Sectish TC, Simon DW, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262-2270.
- Dhingra KR, Elms A, Hobgood C. Reducing error in the emergency department: a call for standardization of the sign-out process. Ann Emerg Med. 2010;56(6):637-642.
- Sinha M, Shriki J, Salness R, Blackburn PA. Need for standardized sign-out in the emergency department: a survey of emergency medicine residency and pediatric emergency medicine fellowship program directors. Acad Emerg Med. 2007;14(2):192-196.
- Accreditation Council For Graduate Medical Education Web site. Clinical Learning Environment Review (CLER) Program. www.acgme.org/CLER/. Accessed March 3, 2015.
- Horwitz LI, Meredith T, Schuur JD, Shah NR, Kulkarni RG, Jenq GY. Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med. 2009;53(6):701-10.e4.
- Jacquis WP, Kaplan JA, Carpenter C, et al; American College of Emergency Physicians Transitions of Care Task Force. Transitions of Care Task Force Report, 2012. http://www.acep.org/transitionsofcare/. Accessed March 3, 2015.
- Emergency Medicine Patient Safety Foundation. Safer Sign Out Tool Kit. safersignoutcom. Available at: http://safersignout.com/. Accessed March 3, 2015.
- Dubosh NM, Carney D, Fisher J, Tibbles CD. Implementation of an emergency department sign-out checklist improves transfer of information at shift change. J Emerg Med. 2014;47(5):580-585.
- Farhan M, Brown R, Woloshynowych M, Vincent C. The ABC of handover: a qualitative study to develop a new tool for handover in the emergency department. Emerg Med. 2012;29(12):941-946.
- Starmer AJ, O’Toole JK, Rosenbluth G, et al; I-PASS Study Education Executive Committee. Development, implementation, and dissemination of the I-PASS handoff curriculum: A multisite educational intervention to improve patient handoffs. Acad Med. 2014;89(6):876-884.
- Starmer AJ, Spector ND, Srivastava R, et al; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812.
- Institute for Healthcare Improvement. SBAR Technique for Communication: A Situational Briefing Model. http://www.ihi.org/resources/Pages/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.aspx. Accessed March 3, 2015.
- De Meester K, Verspuy M, Monsieurs KG, Van Bogaert P. SBAR improves nurse-physician communication and reduces unexpected death: A pre and post intervention study. Resuscitation. 2013;84(9):1192-1196.
- Randmaa M, Mårtensson G, Leo Swenne C, Engström M. SBAR improves communication and safety climate and decreases incident reports due to communication errors in an anaesthetic clinic: a prospective intervention study. BMJ Open. 2014;4(1):e004268.
- Panesar RS, Albert B, Messina C, Parker M. The effect of an electronic SBAR communication tool on documentation of acute events in the pediatric intensive care unit. Am J Med Qual. 2014. doi:10.1177/1062860614553263.
- Connor MP, Bush AC, Brennan J. IMOUTA: a proposal for patient care handoffs. Laryngoscope. 2013;123(11):2649-2653.
- Bavare AC, Shah PK, Roy KM, Williams EA, Lloyd LE, McPherson ML. Implementation of a Standard Verbal Sign-Out Template Improves Sign-Out Process in a Pediatric Intensive Care Unit. J Healthc Qual. 2013:1-9.
- American Medical Association Web site. Resources for improving patient handoffs. Available at: http://www.ama-assn.org/ama/pub/about-ama/our-people/member-groups-sections/resident-fellow-section/rfs-resources/patient-handoffs.page. Accessed March 3, 2015.
- Cheung DS, Kelly JJ, Beach C, et al; Section of Quality Improvement and Patient Safety, American College of Emergency Physicians. Improving handoffs in the emergency department. Ann Emerg Med. 2010;55(2):171-802.
- Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Qual Saf Health Care. 2010;19(6):493-497.
- Kessler C, Shakeel F, Hern HG, et al. A survey of handoff practices in emergency medicine. Am J Med Qual. 2014;29(5):408-414.
- Kessler C, Shakeel F, Hern HG, et al. An algorithm for transition of care in the emergency department. Acad Emerg Med. 2013;20(6):605-610.
- Riesenberg LA, Leitzsch J, Massucci JL, et al. Residents’ and attending physicians’ handoffs: a systematic review of the literature. Acad Med. 2009;84(12):1775-1787.
- Starmer AJ, Sectish TC, Simon DW, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262-2270.
- Dhingra KR, Elms A, Hobgood C. Reducing error in the emergency department: a call for standardization of the sign-out process. Ann Emerg Med. 2010;56(6):637-642.
- Sinha M, Shriki J, Salness R, Blackburn PA. Need for standardized sign-out in the emergency department: a survey of emergency medicine residency and pediatric emergency medicine fellowship program directors. Acad Emerg Med. 2007;14(2):192-196.
- Accreditation Council For Graduate Medical Education Web site. Clinical Learning Environment Review (CLER) Program. www.acgme.org/CLER/. Accessed March 3, 2015.
- Horwitz LI, Meredith T, Schuur JD, Shah NR, Kulkarni RG, Jenq GY. Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med. 2009;53(6):701-10.e4.
- Jacquis WP, Kaplan JA, Carpenter C, et al; American College of Emergency Physicians Transitions of Care Task Force. Transitions of Care Task Force Report, 2012. http://www.acep.org/transitionsofcare/. Accessed March 3, 2015.
- Emergency Medicine Patient Safety Foundation. Safer Sign Out Tool Kit. safersignoutcom. Available at: http://safersignout.com/. Accessed March 3, 2015.
- Dubosh NM, Carney D, Fisher J, Tibbles CD. Implementation of an emergency department sign-out checklist improves transfer of information at shift change. J Emerg Med. 2014;47(5):580-585.
- Farhan M, Brown R, Woloshynowych M, Vincent C. The ABC of handover: a qualitative study to develop a new tool for handover in the emergency department. Emerg Med. 2012;29(12):941-946.
- Starmer AJ, O’Toole JK, Rosenbluth G, et al; I-PASS Study Education Executive Committee. Development, implementation, and dissemination of the I-PASS handoff curriculum: A multisite educational intervention to improve patient handoffs. Acad Med. 2014;89(6):876-884.
- Starmer AJ, Spector ND, Srivastava R, et al; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-1812.
- Institute for Healthcare Improvement. SBAR Technique for Communication: A Situational Briefing Model. http://www.ihi.org/resources/Pages/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.aspx. Accessed March 3, 2015.
- De Meester K, Verspuy M, Monsieurs KG, Van Bogaert P. SBAR improves nurse-physician communication and reduces unexpected death: A pre and post intervention study. Resuscitation. 2013;84(9):1192-1196.
- Randmaa M, Mårtensson G, Leo Swenne C, Engström M. SBAR improves communication and safety climate and decreases incident reports due to communication errors in an anaesthetic clinic: a prospective intervention study. BMJ Open. 2014;4(1):e004268.
- Panesar RS, Albert B, Messina C, Parker M. The effect of an electronic SBAR communication tool on documentation of acute events in the pediatric intensive care unit. Am J Med Qual. 2014. doi:10.1177/1062860614553263.
- Connor MP, Bush AC, Brennan J. IMOUTA: a proposal for patient care handoffs. Laryngoscope. 2013;123(11):2649-2653.
- Bavare AC, Shah PK, Roy KM, Williams EA, Lloyd LE, McPherson ML. Implementation of a Standard Verbal Sign-Out Template Improves Sign-Out Process in a Pediatric Intensive Care Unit. J Healthc Qual. 2013:1-9.
- American Medical Association Web site. Resources for improving patient handoffs. Available at: http://www.ama-assn.org/ama/pub/about-ama/our-people/member-groups-sections/resident-fellow-section/rfs-resources/patient-handoffs.page. Accessed March 3, 2015.