User login
Asthma Across a Woman’s Lifespan
1. Chowdhury NU et al. Eur Respir Rev. 2021;30(162):210067. doi:10.1183/16000617.0067-2021
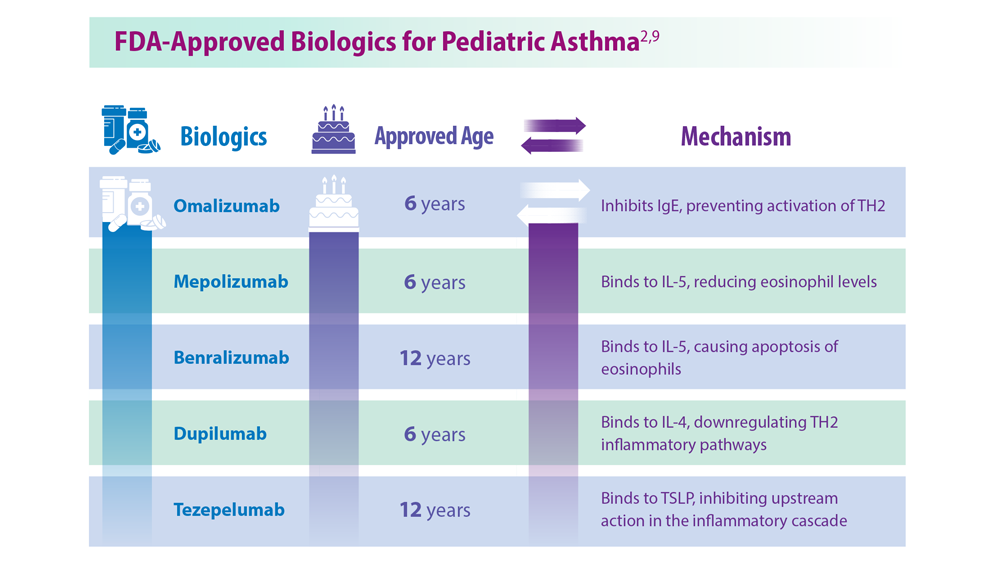
2. Perikleous EP et al. J Pers Med. 2022;12(6):999. doi:10.3390/jpm12060999
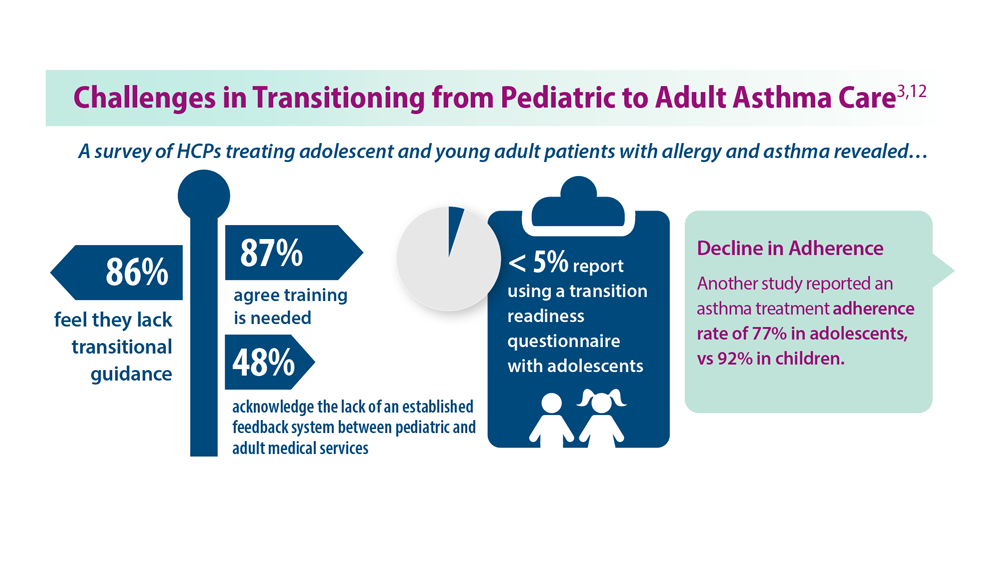
3. Khaleva E et al. Clin Transl Allergy. 2020;10:40. doi:10.1186/s13601-020-00340-z
4. Robijn AL et al. Curr Opin Pulm Med. 2019;25(1):11-17. doi:10.1097/MCP.0000000000000538
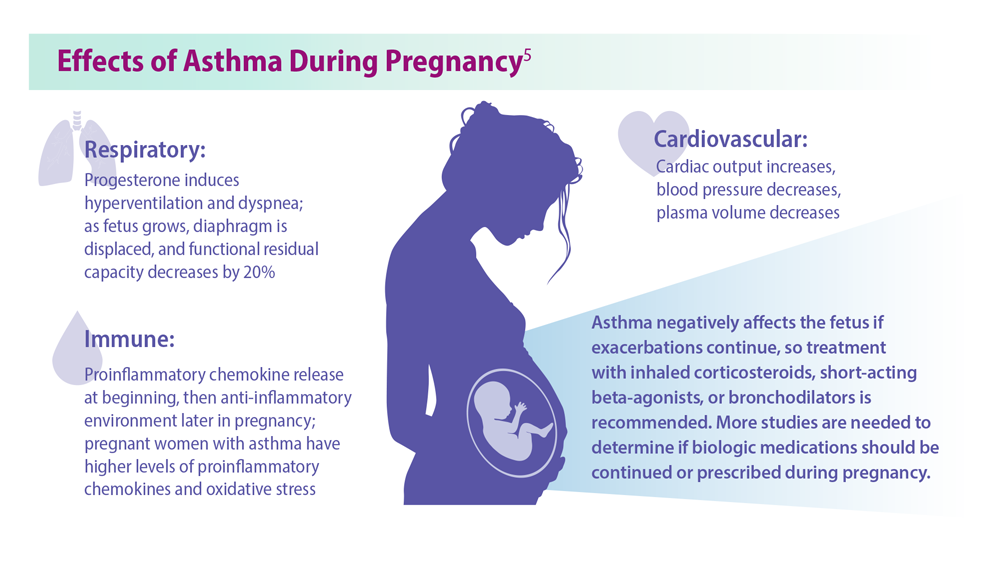
5. Bravo-Solarte DC et al. Allergy Asthma Proc. 2023;44(1):24-34. doi:10.2500/aap.2023.44.220077
6. Wang G et al. J Matern Fetal Neonatal Med. 2014;27(9):934-942. doi:10.3109/14767058.2013.847080
7. Hough KP et al. Front Med (Lausanne). 2020;7:191. doi:10.3389/fmed.2020.00191
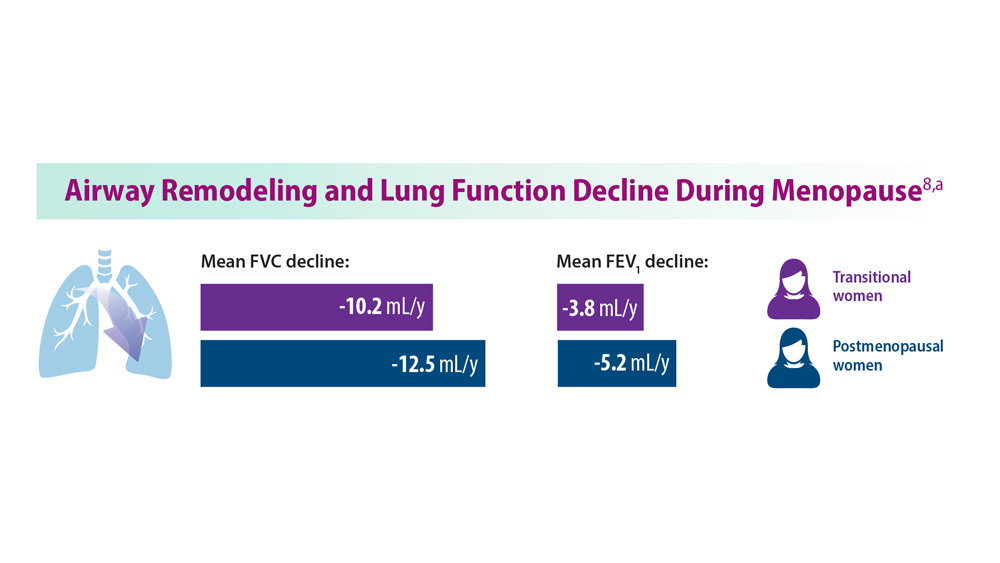
8. Triebner K et al. Am J Respir Crit Care Med. 2017;195(8):1058-1065. doi:10.1164/rccm.201605-0968OC
9. Bacharier LB, Jackson DJ. J Allergy Clin Immunol. 2023;151(3):581-589. doi:10.1016/j.jaci.2023.01.002
10. An amazing journey: how young lungs develop. American Lung Association. Published May 11, 2018. Accessed June 28, 2023. https://www.lung.org/blog/how-young-lungs-develop
11. Strunk RC et al. J Allergy Clin Immunol. 2006;118(5):1040-1047. doi:10.1016/j.jaci.2006.07.053
12. Kaplan A, Price D. J Asthma Allergy. 2020;13:39-49. doi:10.2147/JAA.S233268
1. Chowdhury NU et al. Eur Respir Rev. 2021;30(162):210067. doi:10.1183/16000617.0067-2021
2. Perikleous EP et al. J Pers Med. 2022;12(6):999. doi:10.3390/jpm12060999
3. Khaleva E et al. Clin Transl Allergy. 2020;10:40. doi:10.1186/s13601-020-00340-z
4. Robijn AL et al. Curr Opin Pulm Med. 2019;25(1):11-17. doi:10.1097/MCP.0000000000000538
5. Bravo-Solarte DC et al. Allergy Asthma Proc. 2023;44(1):24-34. doi:10.2500/aap.2023.44.220077
6. Wang G et al. J Matern Fetal Neonatal Med. 2014;27(9):934-942. doi:10.3109/14767058.2013.847080
7. Hough KP et al. Front Med (Lausanne). 2020;7:191. doi:10.3389/fmed.2020.00191
8. Triebner K et al. Am J Respir Crit Care Med. 2017;195(8):1058-1065. doi:10.1164/rccm.201605-0968OC
9. Bacharier LB, Jackson DJ. J Allergy Clin Immunol. 2023;151(3):581-589. doi:10.1016/j.jaci.2023.01.002
10. An amazing journey: how young lungs develop. American Lung Association. Published May 11, 2018. Accessed June 28, 2023. https://www.lung.org/blog/how-young-lungs-develop
11. Strunk RC et al. J Allergy Clin Immunol. 2006;118(5):1040-1047. doi:10.1016/j.jaci.2006.07.053
12. Kaplan A, Price D. J Asthma Allergy. 2020;13:39-49. doi:10.2147/JAA.S233268
1. Chowdhury NU et al. Eur Respir Rev. 2021;30(162):210067. doi:10.1183/16000617.0067-2021
2. Perikleous EP et al. J Pers Med. 2022;12(6):999. doi:10.3390/jpm12060999
3. Khaleva E et al. Clin Transl Allergy. 2020;10:40. doi:10.1186/s13601-020-00340-z
4. Robijn AL et al. Curr Opin Pulm Med. 2019;25(1):11-17. doi:10.1097/MCP.0000000000000538
5. Bravo-Solarte DC et al. Allergy Asthma Proc. 2023;44(1):24-34. doi:10.2500/aap.2023.44.220077
6. Wang G et al. J Matern Fetal Neonatal Med. 2014;27(9):934-942. doi:10.3109/14767058.2013.847080
7. Hough KP et al. Front Med (Lausanne). 2020;7:191. doi:10.3389/fmed.2020.00191
8. Triebner K et al. Am J Respir Crit Care Med. 2017;195(8):1058-1065. doi:10.1164/rccm.201605-0968OC
9. Bacharier LB, Jackson DJ. J Allergy Clin Immunol. 2023;151(3):581-589. doi:10.1016/j.jaci.2023.01.002
10. An amazing journey: how young lungs develop. American Lung Association. Published May 11, 2018. Accessed June 28, 2023. https://www.lung.org/blog/how-young-lungs-develop
11. Strunk RC et al. J Allergy Clin Immunol. 2006;118(5):1040-1047. doi:10.1016/j.jaci.2006.07.053
12. Kaplan A, Price D. J Asthma Allergy. 2020;13:39-49. doi:10.2147/JAA.S233268
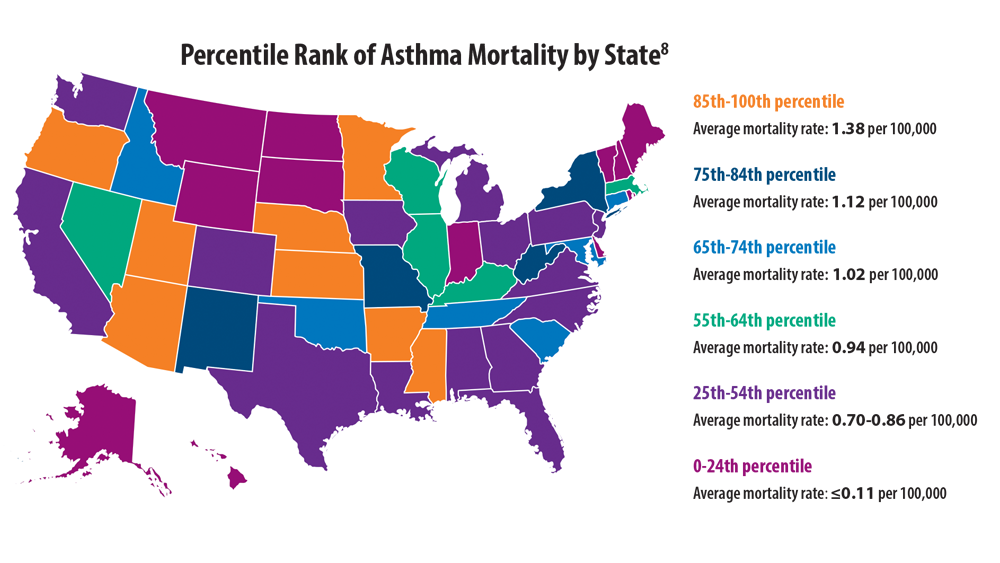
Comorbidities, Racial Disparities, and Geographic Differences in Asthma
- Wenzel M. Gasping for a diagnosis: pediatric vocal cord dysfunction. J Pediatr Health Care. 2019;33(1):5-13. doi:10.1016/j.pedhc.2018.03.002
- Mogensen I, James A, Malinovschi A. Systemic and breath biomarkers for asthma: an update. Curr Opin Allergy Clin Immunol. 2020;20(1):71-79. doi:10.1097/ACI.0000000000000599
- Gibson PG, McDonald VM, Granchelli A, Olin JT. Asthma and comorbid conditions—pulmonary comorbidity. J Allergy Clin Immunol Pract. 2021;9(11):3868-3875. doi:10.1016/j. jaip.2021.08.028
- Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141(4):1169-1179. doi:10.1016/j.jaci.2018.02.004
- Adult obesity facts. Centers for Disease Control and Prevention. Published May 17, 2022. Accessed June 7, 2022. https://www.cdc.gov/obesity/data/adult.html
- Sharma V, Cowan DC. Obesity, inflammation, and severe asthma: an update. Curr Allergy Asthma Rep. 2021;21(12):46. doi:10.1007/s11882-021-01024-9
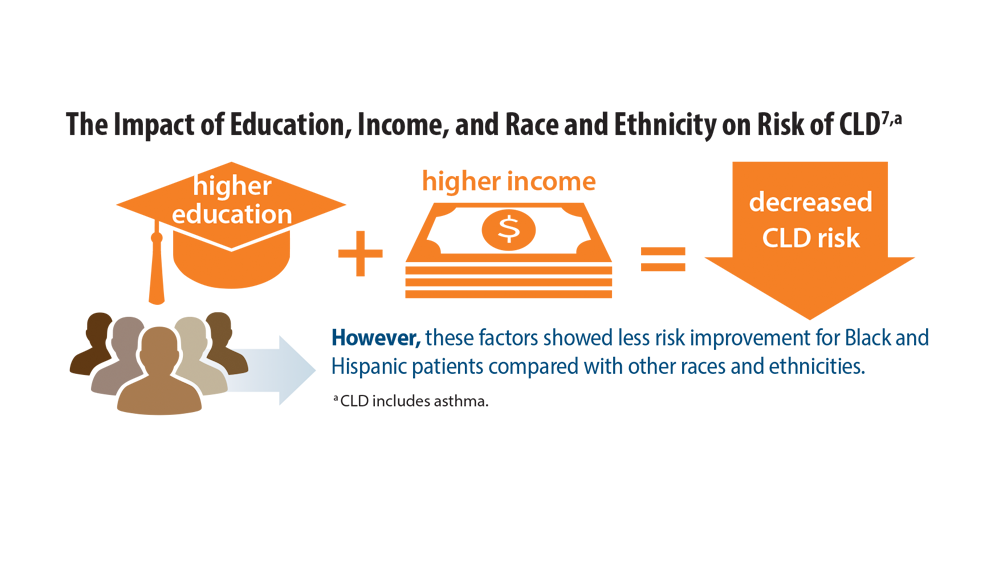
- Assari S, Chalian H, Bazargan M. Race, ethnicity, socioeconomic status, and chronic lung disease in the U.S. Res Health Sci. 2020;5(1):48-63. doi:10.22158/rhs.v5n1p48
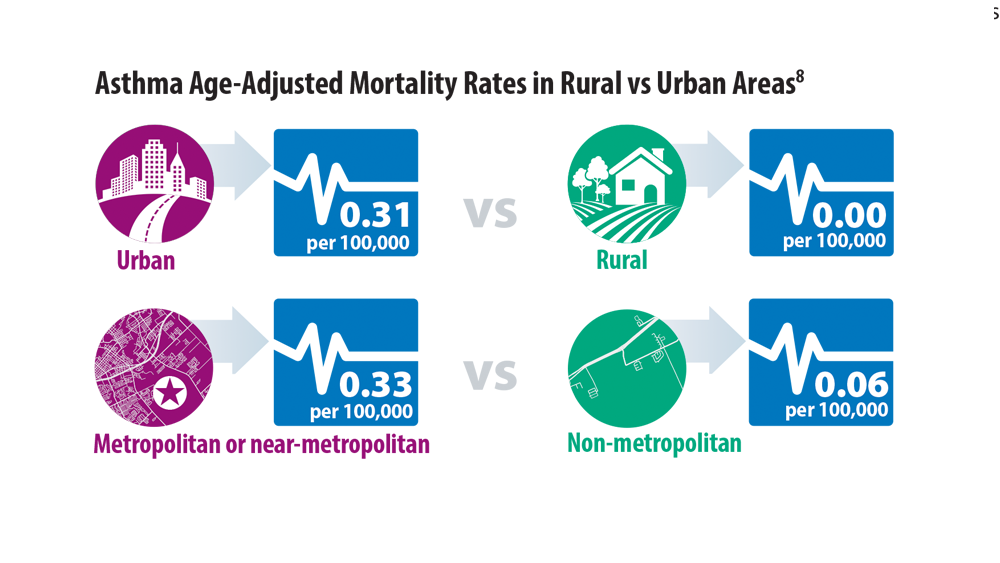
- Bleecker ER, Gandhi H, Gilbert I, Murphy KR, Chupp GL. Mapping geographic variability of severe uncontrolled asthma in the United States: management implications. Ann Allergy Asthma Immunol. 2022;128(1):78-88. doi:10.1016/j.anai.2021.09.025
- Wenzel M. Gasping for a diagnosis: pediatric vocal cord dysfunction. J Pediatr Health Care. 2019;33(1):5-13. doi:10.1016/j.pedhc.2018.03.002
- Mogensen I, James A, Malinovschi A. Systemic and breath biomarkers for asthma: an update. Curr Opin Allergy Clin Immunol. 2020;20(1):71-79. doi:10.1097/ACI.0000000000000599
- Gibson PG, McDonald VM, Granchelli A, Olin JT. Asthma and comorbid conditions—pulmonary comorbidity. J Allergy Clin Immunol Pract. 2021;9(11):3868-3875. doi:10.1016/j. jaip.2021.08.028
- Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141(4):1169-1179. doi:10.1016/j.jaci.2018.02.004
- Adult obesity facts. Centers for Disease Control and Prevention. Published May 17, 2022. Accessed June 7, 2022. https://www.cdc.gov/obesity/data/adult.html
- Sharma V, Cowan DC. Obesity, inflammation, and severe asthma: an update. Curr Allergy Asthma Rep. 2021;21(12):46. doi:10.1007/s11882-021-01024-9
- Assari S, Chalian H, Bazargan M. Race, ethnicity, socioeconomic status, and chronic lung disease in the U.S. Res Health Sci. 2020;5(1):48-63. doi:10.22158/rhs.v5n1p48
- Bleecker ER, Gandhi H, Gilbert I, Murphy KR, Chupp GL. Mapping geographic variability of severe uncontrolled asthma in the United States: management implications. Ann Allergy Asthma Immunol. 2022;128(1):78-88. doi:10.1016/j.anai.2021.09.025
- Wenzel M. Gasping for a diagnosis: pediatric vocal cord dysfunction. J Pediatr Health Care. 2019;33(1):5-13. doi:10.1016/j.pedhc.2018.03.002
- Mogensen I, James A, Malinovschi A. Systemic and breath biomarkers for asthma: an update. Curr Opin Allergy Clin Immunol. 2020;20(1):71-79. doi:10.1097/ACI.0000000000000599
- Gibson PG, McDonald VM, Granchelli A, Olin JT. Asthma and comorbid conditions—pulmonary comorbidity. J Allergy Clin Immunol Pract. 2021;9(11):3868-3875. doi:10.1016/j. jaip.2021.08.028
- Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141(4):1169-1179. doi:10.1016/j.jaci.2018.02.004
- Adult obesity facts. Centers for Disease Control and Prevention. Published May 17, 2022. Accessed June 7, 2022. https://www.cdc.gov/obesity/data/adult.html
- Sharma V, Cowan DC. Obesity, inflammation, and severe asthma: an update. Curr Allergy Asthma Rep. 2021;21(12):46. doi:10.1007/s11882-021-01024-9
- Assari S, Chalian H, Bazargan M. Race, ethnicity, socioeconomic status, and chronic lung disease in the U.S. Res Health Sci. 2020;5(1):48-63. doi:10.22158/rhs.v5n1p48
- Bleecker ER, Gandhi H, Gilbert I, Murphy KR, Chupp GL. Mapping geographic variability of severe uncontrolled asthma in the United States: management implications. Ann Allergy Asthma Immunol. 2022;128(1):78-88. doi:10.1016/j.anai.2021.09.025