User login
Hypothermia in adults: A strategy for detection and Tx
CASE
Patrick S, an 85-year-old man with multiple medical problems, was brought to his primary care provider after being found at home with altered mental status. His caretaker reported that Mr. S had been using extra blankets in bed and sleeping more, but he hadn’t had significant outdoor exposure. Measurement of his vital signs revealed tachycardia, tachypnea, hypotension, and a rectal temperature of 32°C (89.6°F).
How would you proceed with the care of this patient?
What is accidental hypothermia?
Accidental hypothermia is an unintentional drop in core body temperature to <35°C (<95°F). Mild hypothermia is defined as a core body temperature of 32°C to 35°C (90°F - 95°F); moderate hypothermia, 28°C to 32°C (82°F - 90°F); and severe hypothermia, <28°C (<82°F).1
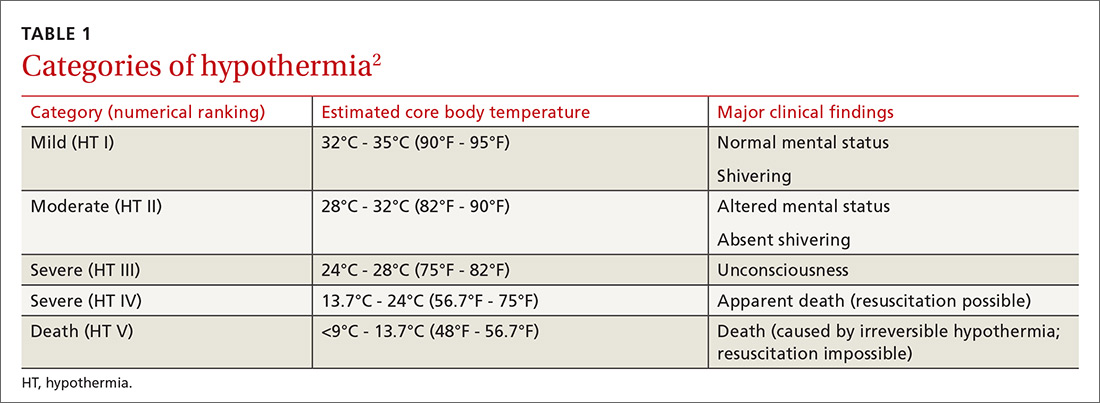
The International Commission for Mountain Emergency Medicine divides hypothermia into 5 categories, emphasizing the clinical features of each stage as a guide to treatment (TABLE 1).2 These categories were adopted to help prehospital rescuers estimate the severity of hypothermia using physical symptoms. For example, most patients stop shivering at approximately 30°C (86°F)—the “moderate (HT II)” category of hypothermia—although this response varies widely from patient to patient. Notably, there are reports in the literature of survival in hypothermia with a temperature as low as 13.7°C (56.7°F) and with cardiac arrest for as long as 8 hours and 40 minutes, although these events are rare.3
Each year, approximately 700 deaths in the United States are the result of hypothermia.4 Between 1995 to 2004 in the United States, it is estimated that 15,574 visits were made to a health care provider or facility for hypothermia and other cold-related concerns.5 Based on reports in the international literature, the incidence of nonlethal hypothermia is much greater than the incidence of lethal hypothermia.5 Almost half of deaths from hypothermia are in people older than age 65 years; the male to female ratio is 2.5:1.1
Variables that predispose the body to temperature dysregulation include extremes of age, comorbid conditions, intoxication, chronic cold exposure, immersion accident, mental illness, impaired shivering, and lack of acclimatization.1 The most common causes of death associated with hypothermia are falls, drownings, and cardiovascular disease.4 In a 2008 study, hypothermia and other cold-related morbidity emergency department (ED) visits required more transfers of patients to a critical care unit than any other reason for visiting an ED (risk ratio, 6.73; 95% confidence interval, 1.8-25).5 Mortality among inpatients whose hypothermia is classified as moderate or severe reaches as high as 40%.3
More than just cold-weather exposure
Accidental hypothermia occurs when heat loss is superseded by the body’s ability to generate heat. It commonly happens in cold environments but can also occur at higher temperatures if the body’s thermoregulatory system malfunctions.
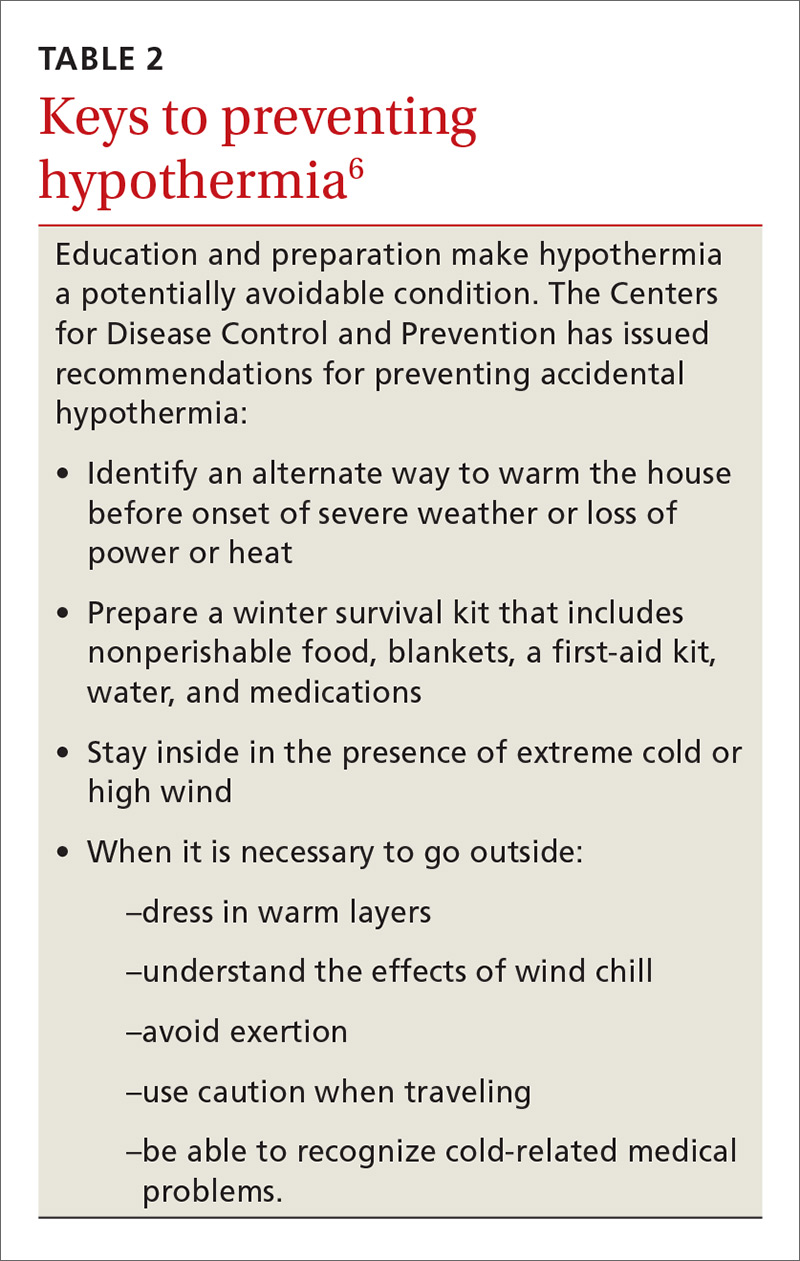
Environmental or iatrogenic factors (ie, primary hypothermia), such as wind, water immersion, wetness, aggressive fluid resuscitation, and heat stroke treatment can make people more susceptible to hypothermia. Medical conditions (ie, secondary hypothermia), such as burns, exfoliative dermatitis, severe psoriasis, hypoadrenalism, hypopituitarism, hypothyroidism, acute spinal cord transection, head trauma, stroke, tumor, pneumonia, Wernicke’s disease (encephalopathy), and sepsis can also predispose to hypothermia.1 Drugs, such as ethanol, phenothiazines, and sedative–hypnotics may decrease the hypothermia threshold.1 (For information on preventing hypothermia, see TABLE 2.6)
Pathophysiology: The role of the hypothalamus
Humans maintain body temperature by balancing heat production and heat loss to the environment. Heat is lost through the skin and lungs by 5 different mechanisms: radiation, conduction, convection, evaporation, and respiration. Convective heat loss to cold air and conductive heat loss to water are the most common mechanisms of accidental hypothermia.7
To maintain temperature homeostasis at 37°C (98.6°F) (±0.5°C [±0.9°F]), the hypothalamus receives input from central and peripheral thermal receptors and stimulates heat production through shivering, increasing the basal metabolic rate 2-fold to 5-fold.1 The hypothalamus also increases thyroid, catecholamine, and adrenal activity to increase the body’s production of heat and raise core temperature.
Heat conservation occurs by activation of sympathetically mediated vasoconstriction, reducing conduction to the skin, where cooling is greatest. After time, temperature regulation in the body becomes overwhelmed and catecholamine levels return to a pre-hypothermic state.
At 35°C (95°F), neurologic function begins to decline; at 32°C (89.6°F), metabolism, ventilation, and cardiac output decrease until shivering ceases. Changes in peripheral blood flow can create a false warming sensation, causing a person to remove clothing, a phenomenon referred to as paradoxical undressing. As hypothermia progresses, the neurologic, respiratory, and cardiac systems continue to slow until there is eventual cardiorespiratory failure.
Assessment and diagnosis
History and physical examination. A high index of suspicion for the diagnosis of hypothermia is essential, especially when caring for the elderly or patients presenting with unexplained illness. Often, symptoms of a primary condition may overshadow those reflecting hypothermia. In a multicenter survey that reviewed 428 cases of accidental hypothermia in the United States, 44% of patients had an underlying illness; 18%, coexisting infection; 19%, trauma; and 6%, overdose.3
There are no strict diagnostic criteria for hypothermia other than a core body temperature <35°C (<95°F). Standard thermometers often do not read below 34.4°C (93.2°F), so it is recommended that a rectal thermometer capable of reading low body temperatures be used for accurate measurement.
Hypothermic patients can exhibit a variety of symptoms, depending on the degree of decrease in core body temperature1:
- A mildly hypothermic patient might present with any combination of tachypnea, tachycardia, ataxia, impaired judgment, shivering, and vasoconstriction.
- Moderate hypothermia typically manifests as a decreased heart rate, decreased blood pressure, decreased level of consciousness, decreased respiratory effort, dilated pupils, extinction of shivering, and hyporeflexia. Cardiac abnormalities, such as atrial fibrillation and junctional bradycardia, may be seen in moderate hypothermia.
- Severe hypothermia presents with apnea, coma, nonreactive pupils, oliguria, areflexia, hypotension, bradycardia, and continued cardiac abnormalities, such as ventricular arrhythmias and asystole.
Laboratory evaluation. No specific laboratory tests are needed to diagnose hypothermia. General lab tests, however, may help determine whether hypothermia is the result, or the cause, of the clinical scenario. Recommended laboratory tests for making that determination include a complete blood count (CBC), chemistry panel, arterial blood gases, fingerstick glucose, and coagulation panel.
Results of lab tests may be abnormal because of the body’s decreased core body temperature. White blood cells and platelets in the CBC, for example, may be decreased due to splenic sequestration; these findings reverse with rewarming. With every 1°C (1.8°F) drop in core body temperature, hematocrit increases 2%.3 Sodium, chloride, and magnesium concentrations do not display consistent abnormalities with any core body temperature >25°C (77°F),3,8 but potassium levels may fluctuate because of acid-base changes that occur during rewarming.1 Creatinine and creatine kinase levels may be increased secondary to rhabdomyolysis or acute tubular necrosis.1
Arterial blood gases typically show metabolic acidosis or respiratory alkalosis, or both.8 Prothrombin time and partial thromboplastin time are typically elevated in vivo, secondary to temperature-dependent enzymes in the coagulation cascade, but are reported normal in a blood specimen that is heated to 37°C (98.6°F) prior to analysis.1,8
Both hyperglycemia and hypoglycemia can be associated with hypothermia. The lactate level can be elevated, due to hypoperfusion. Hepatic impairment may be seen secondary to decreased cardiac output. An increase in the lipase level may also occur.3
When a hypothermic patient fails to respond to rewarming, or there is no clear source of cold exposure, consider testing for other causes of the problem, including hypothyroidism and adrenal insufficiency (see “Differential diagnosis”). Hypothermia may also decrease thyroid function in people with preexisting disease.
Other laboratory studies that can be considered include fibrinogen, blood-alcohol level, urine toxicology screen, and blood and fluid cultures.3
Imaging. Imaging studies are not performed routinely in the setting of hypothermia; however:
- Chest radiography can be considered to assess for aspiration pneumonia, vascular congestion, and pulmonary edema.
- Computed tomography (CT) of the head is helpful in the setting of trauma or if mental status does not clear with rewarming.3
- Bedside ultrasonography can assess for cardiac activity, volume status, pulmonary edema, free fluid, and trauma. (See "Point-of-care ultrasound: Coming soon to primary care?" J Fam Pract. 2018;67:70-80.)
Electrocardiography. An electrocardiogram is essential to evaluate for arrhythmias. Findings associated with hypothermia are prolongation of PR, QRS, and QT intervals; ST-segment elevation, T-wave inversion; and Osborn waves (J waves), which represent a positive deflection at the termination of the QRS complex with associated J-point elevation.8 Osborn waves generally present when the core body temperature is <32°C (89.6°F) and become larger as the core body temperature drops further.3
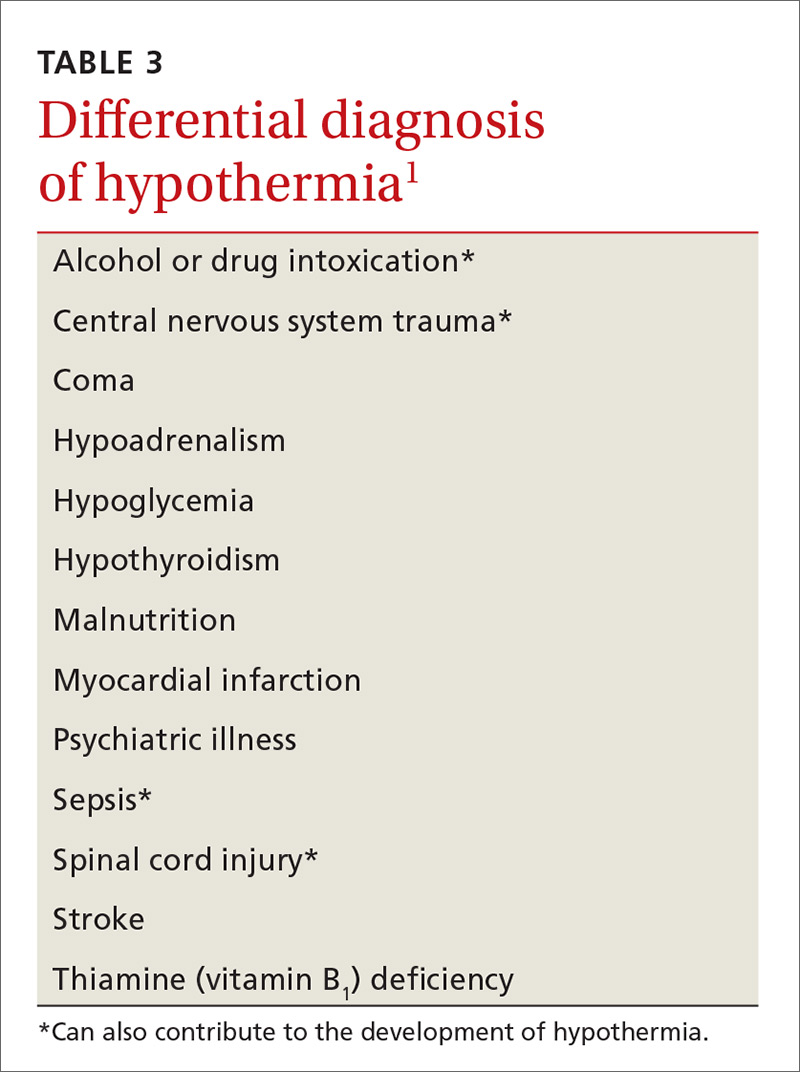
Differential diagnosis. Hypothermia is most commonly caused by environmental exposure, but the differential diagnosis is broad: many medical conditions, as well as drug and alcohol intoxication, can contribute to hypothermia (TABLE 31).
Treatment: Usually unnecessary, sometimes crucial
Most patients with mild hypothermia recover completely with little intervention. These patients should be evaluated for cognitive irregularities and observed in the ED before discharge.9 Moderate and severe hypothermia patients should be assessed using pre-hospital protocols and given cardiopulmonary resuscitation (CPR) for cardiac arrest. Pre-hospital providers should rely more on symptoms in guiding their treatment response because core body temperature measurements can be difficult to obtain, and the response to a drop in core body temperature varies from patient to patient.10
Early considerations: Airway, breathing, circulation (ABC)
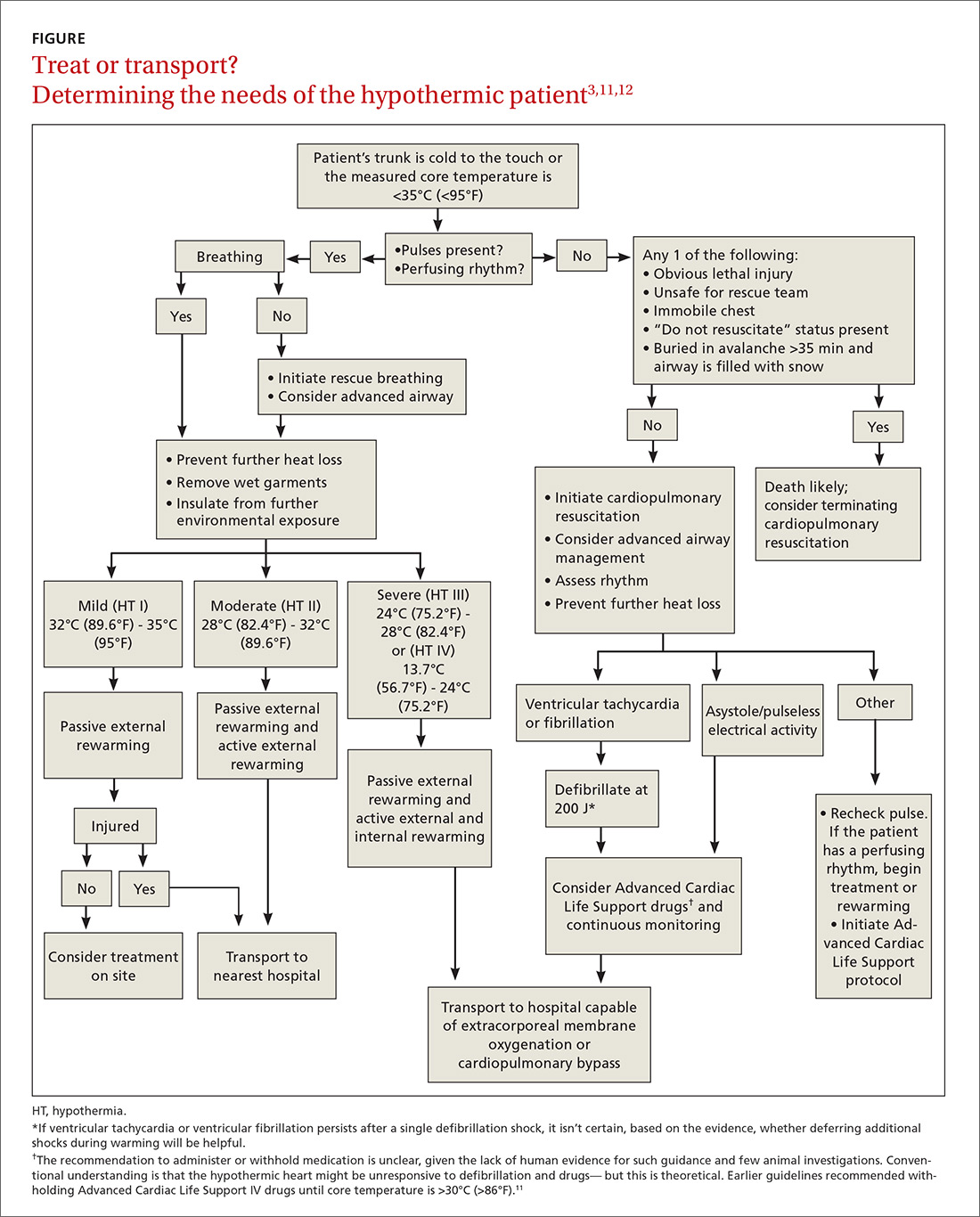
A first responder might have difficulty palpating the pulse of a hypothermic patient if that patient’s cardiopulmonary effort is diminished.9 This inability to palpate a pulse should not delay treatment unless the patient presents with lethal injury; the scene is unsafe; the chest is too stiff for CPR; do-not-resuscitate status is present; or the patient was buried in an avalanche for ≥35 minutes and the airway is filled with snow (FIGURE3,11,12). Pulse should be checked carefully for 60 seconds. If pulses are not present, CPR should be initiated.
Prevention of further heat loss should begin promptly for hypothermic patients who retain a perfusing rhythm.11 Lifesaving interventions, such as airway management, vascular access for volume replenishment, and defibrillation for ventricular tachycardia or ventricular fibrillation should be carried out according to Advanced Cardiac Life Support protocols.11 Patients in respiratory distress or incapable of protecting their airway because of altered mental status should undergo endotracheal intubation. Fluid resuscitation with isotonic crystalloid fluids, warmed to 40°C (104°F) to 42°C (~107°F) and delivered through 2 large-bore, peripheral intravenous (IV) needles, can be considered.
Special care should be taken when moving a hypothermic patient. Excessive movement can lead to stimulation of the irritable hypothermic heart and cause an arrhythmia.
Medical therapy. Caution is advised because the reduced metabolism of a hypothermic patient can lead to potentially toxic accumulation of drugs peripherally. In fact, outcomes have not been positively influenced by routine use of medications, other than treatment of ventricular fibrillation with amiodarone.11 Any intravenous (IV) drug should be held until the patient’s core temperature is >30°C (>86°F).11
Vasopressors can be beneficial during rewarming for a patient in cardiac arrest and are a reasonable consideration.2 Nitroglycerin, in conjunction with active external rewarming, can increase the overall hourly temperature gain in a moderately hypothermic patient.13
Rewarming. The extent of rewarming required can be predicted by the severity of hypothermia (FIGURE3,11,12). Mildly hypothermic patients can generally be rewarmed using passive external measures. Patients with moderate hypothermia benefit from active rewarming in addition to passive measures. Intervention for severe hypothermia requires external rewarming and internal warming, with admission to the intensive care unit.
Treatment plans for severely hypothermic patients differ, depending on whether the person has a perfusing or nonperfusing cardiac rhythm. Patients who maintain a perfusing rhythm can be rewarmed using external methods (although core rewarming is used more often). Patients who do not have a perfusing rhythm require more invasive procedures.11 When using any rewarming method, afterdrop phenomenon can occur: ie, vasodilation, brought on by rewarming, causes a drop in core body temperature, as cooler peripheral blood returns to the central circulation. This effect may be reduced by focused rewarming of the trunk prior to rewarming the extremities.3
Rewarming for mild hypothermia patients begins with passive external techniques. First, the patient is moved away from the environment for protection from further exposure. Next, wet or damaged clothing is removed, blankets or foil insulators are applied, and room temperature is maintained at ≥28°C (82°F).3,11,13,14
If the patient’s temperature does not normalize, or if the patient presented with moderate or severe hypothermia, rewarming is continued with active external and internal measures. Active external rewarming can supplement passive measures using radiant heat from warmed blankets, air rewarming devices, and heating pads.3,13,14 Active internal rewarming techniques rely on invasive measures to raise the core temperature. Heated crystalloid IV fluids do not treat hypothermia, but do help reduce further heat loss and can be helpful in patients in need of volume resuscitation.3,13
Severely hypothermic patients might require more invasive active internal rewarming techniques, such as body-cavity lavage and extracorporeal methods. Body-cavity lavage can be facilitated with large volumes (10-120 L) of warm fluid at 40°C to 42°C, circulated through the thoracic or abdominal cavities to raise core body temperature 3°C to 6°C per hour.3,13
Extracorporeal rewarming can be achieved through hemodialysis, continuous arteriovenous rewarming (CAVR), continuous veno-venous rewarming (CVVR), or cardiopulmonary bypass.3,13 Research has shown cardiopulmonary bypass to be the most effective technique, with as high as a 7°C rise in core body temperature per hour; CVVR and CAVR are less invasive, however, and more readily available in hospitals.3,11,13
Rewarming interventions should continue until return of spontaneous circulation and core body temperature reaches 32°C (89.6°F) to 34°C (93.2°F).11 Overall, resuscitation efforts may take longer than normal due to the need for rewarming and should continue until the patient has achieved a normal temperature of 37°C (97.8°F).
Prognosis varies with severity, the health of the patient
In healthy, mildly hypothermic patients, full recovery is common if heat loss is minimized and the cause is treated. Moderately hypothermic patients who receive proper care can also have a favorable result. Outcomes for severe hypothermia vary with duration, comorbidities, and severity of core body temperature loss.15
Immediate initiation of rewarming by pre-hospital providers improves outcomes, and higher mortality has been demonstrated with hospital admission temperatures <35°C (95°F).15 Almost 100% of primary hypothermia patients with cardiac stability who were treated using active external and minimally invasive rewarming techniques survived with an intact neurologic system.12 Fifty percent of patients who endured cardiac arrest or who were treated with extracorporeal rewarming had an intact neurologic system. In cardiac arrest cases without significant underlying disease or trauma, and in which hypoxia did not precede hypothermia, full recovery is possible (and has been observed).12
CASE
Mr. S was given a diagnosis of mild to moderate hypothermia and transferred to the nearest ED for further treatment. His age had put him at increased risk of hypothermia. The work-up included laboratory testing (CBC, chemistry panel, thyroid-stimulating hormone, urinalysis, and blood cultures), electrocardiography, chest radiography, and CT of the head.
The chest radiograph showed pneumonia. Based on the results of blood culture, bacterial infection (pneumonia) was determined to be the underlying cause of hypothermia. Mr. S was started on antibiotics.
CORRESPONDENCE
Natasha J. Pyzocha, DO, Bldg 1058, 1856 Irwin Dr, Fort Carson, CO 80913; natasha.j.pyzocha.mil@mail.mil.
1. McCullough L, Arora S. Diagnosis and treatment of hypothermia. Am Fam Physician. 2004;70:2325-2332.
2. Durrer B, Brugger H, Syme D; International Commission for Mountain Emergency Medicine. The medical on-site treatment of hypothermia: ICAR-MEDCOM recommendation. High Alt Med Biol. 2003;4.
3. Rischall ML, Rowland-Fisher A. Evidence-based management of accidental hypothermia in the emergency department. Emerg Med Pract. 2016;18:1-18.
4. Study: Hypothermia-related deaths—United States, 2003-2004. Atlanta, GA: Centers for Disease Control and Prevention; 2005. Available at: www.cdc.gov/media/pressrel/fs050224.htm. Accessed March 1, 2018.
5. Baumgartner EA, Belson M, Rubin C, et al. Hypothermia and other cold-related morbidity emergency department visits: United States, 1995-2004. Wilderness Environ Med. 2008;19:233-237.
6. Centers for Disease Control and Prevention. Preventing injuries associated with extreme cold. Int J Trauma Nurs. 2001;7:26-30.
7. Jolly BT, Ghezzi KT. Accidental hypothermia. Emerg Med Clin North Am. 1992;10:311-327.
8. Mechem CC. Hypothermia and hyperthermia. In: Lanken PN, Manaker S, Hanson CW III, eds. The Intensive Care Unit Manual. Philadelphia: WB Saunders; 2000.
9. Weinberg AD. Hypothermia. Ann Emerg Med. 1993;22:370-377.
10. Zafren K, Giesbrecht GG, Danzl DF, et al. Wilderness Medical Society practice guidelines for the out-of-hospital evaluation and treatment of accidental hypothermia. Wilderness Environ Med. 2014;25:425-445.
11. Web-based integrated 2010 & 2015 guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Part 10: Special Circumstances of Resuscitation. Dallas, TX: American Heart Association; 2017. Available at: https://eccguidelines.heart.org/index.php/circulation/cpr-ecc-guidelines-2/part-10-special-circumstances-of-resuscitation. Accessed March 1, 2018.
12. Brown DJ, Brugger H, Boyd J, et al. Accidental hypothermia. N Engl J Med. 2012;367:1930-1938.
13. Petrone P, Asensio JA, Marini CP. Management of accidental hypothermia and cold injury. Curr Probl Surg. 2014;51:417-431.
14. Fudge J. Preventing and managing hypothermia and frostbite injury. Sports Health. 2016;8:133-139.
15. Martin RS, Kilgo PD, Miller PR, et al. Injury-associated hypothermia: an analysis of the 2004 National Trauma Data Bank. Shock. 2005;24:114-118.
CASE
Patrick S, an 85-year-old man with multiple medical problems, was brought to his primary care provider after being found at home with altered mental status. His caretaker reported that Mr. S had been using extra blankets in bed and sleeping more, but he hadn’t had significant outdoor exposure. Measurement of his vital signs revealed tachycardia, tachypnea, hypotension, and a rectal temperature of 32°C (89.6°F).
How would you proceed with the care of this patient?
What is accidental hypothermia?
Accidental hypothermia is an unintentional drop in core body temperature to <35°C (<95°F). Mild hypothermia is defined as a core body temperature of 32°C to 35°C (90°F - 95°F); moderate hypothermia, 28°C to 32°C (82°F - 90°F); and severe hypothermia, <28°C (<82°F).1
The International Commission for Mountain Emergency Medicine divides hypothermia into 5 categories, emphasizing the clinical features of each stage as a guide to treatment (TABLE 1).2 These categories were adopted to help prehospital rescuers estimate the severity of hypothermia using physical symptoms. For example, most patients stop shivering at approximately 30°C (86°F)—the “moderate (HT II)” category of hypothermia—although this response varies widely from patient to patient. Notably, there are reports in the literature of survival in hypothermia with a temperature as low as 13.7°C (56.7°F) and with cardiac arrest for as long as 8 hours and 40 minutes, although these events are rare.3
Each year, approximately 700 deaths in the United States are the result of hypothermia.4 Between 1995 to 2004 in the United States, it is estimated that 15,574 visits were made to a health care provider or facility for hypothermia and other cold-related concerns.5 Based on reports in the international literature, the incidence of nonlethal hypothermia is much greater than the incidence of lethal hypothermia.5 Almost half of deaths from hypothermia are in people older than age 65 years; the male to female ratio is 2.5:1.1
Variables that predispose the body to temperature dysregulation include extremes of age, comorbid conditions, intoxication, chronic cold exposure, immersion accident, mental illness, impaired shivering, and lack of acclimatization.1 The most common causes of death associated with hypothermia are falls, drownings, and cardiovascular disease.4 In a 2008 study, hypothermia and other cold-related morbidity emergency department (ED) visits required more transfers of patients to a critical care unit than any other reason for visiting an ED (risk ratio, 6.73; 95% confidence interval, 1.8-25).5 Mortality among inpatients whose hypothermia is classified as moderate or severe reaches as high as 40%.3
More than just cold-weather exposure
Accidental hypothermia occurs when heat loss is superseded by the body’s ability to generate heat. It commonly happens in cold environments but can also occur at higher temperatures if the body’s thermoregulatory system malfunctions.
Environmental or iatrogenic factors (ie, primary hypothermia), such as wind, water immersion, wetness, aggressive fluid resuscitation, and heat stroke treatment can make people more susceptible to hypothermia. Medical conditions (ie, secondary hypothermia), such as burns, exfoliative dermatitis, severe psoriasis, hypoadrenalism, hypopituitarism, hypothyroidism, acute spinal cord transection, head trauma, stroke, tumor, pneumonia, Wernicke’s disease (encephalopathy), and sepsis can also predispose to hypothermia.1 Drugs, such as ethanol, phenothiazines, and sedative–hypnotics may decrease the hypothermia threshold.1 (For information on preventing hypothermia, see TABLE 2.6)
Pathophysiology: The role of the hypothalamus
Humans maintain body temperature by balancing heat production and heat loss to the environment. Heat is lost through the skin and lungs by 5 different mechanisms: radiation, conduction, convection, evaporation, and respiration. Convective heat loss to cold air and conductive heat loss to water are the most common mechanisms of accidental hypothermia.7
To maintain temperature homeostasis at 37°C (98.6°F) (±0.5°C [±0.9°F]), the hypothalamus receives input from central and peripheral thermal receptors and stimulates heat production through shivering, increasing the basal metabolic rate 2-fold to 5-fold.1 The hypothalamus also increases thyroid, catecholamine, and adrenal activity to increase the body’s production of heat and raise core temperature.
Heat conservation occurs by activation of sympathetically mediated vasoconstriction, reducing conduction to the skin, where cooling is greatest. After time, temperature regulation in the body becomes overwhelmed and catecholamine levels return to a pre-hypothermic state.
At 35°C (95°F), neurologic function begins to decline; at 32°C (89.6°F), metabolism, ventilation, and cardiac output decrease until shivering ceases. Changes in peripheral blood flow can create a false warming sensation, causing a person to remove clothing, a phenomenon referred to as paradoxical undressing. As hypothermia progresses, the neurologic, respiratory, and cardiac systems continue to slow until there is eventual cardiorespiratory failure.
Assessment and diagnosis
History and physical examination. A high index of suspicion for the diagnosis of hypothermia is essential, especially when caring for the elderly or patients presenting with unexplained illness. Often, symptoms of a primary condition may overshadow those reflecting hypothermia. In a multicenter survey that reviewed 428 cases of accidental hypothermia in the United States, 44% of patients had an underlying illness; 18%, coexisting infection; 19%, trauma; and 6%, overdose.3
There are no strict diagnostic criteria for hypothermia other than a core body temperature <35°C (<95°F). Standard thermometers often do not read below 34.4°C (93.2°F), so it is recommended that a rectal thermometer capable of reading low body temperatures be used for accurate measurement.
Hypothermic patients can exhibit a variety of symptoms, depending on the degree of decrease in core body temperature1:
- A mildly hypothermic patient might present with any combination of tachypnea, tachycardia, ataxia, impaired judgment, shivering, and vasoconstriction.
- Moderate hypothermia typically manifests as a decreased heart rate, decreased blood pressure, decreased level of consciousness, decreased respiratory effort, dilated pupils, extinction of shivering, and hyporeflexia. Cardiac abnormalities, such as atrial fibrillation and junctional bradycardia, may be seen in moderate hypothermia.
- Severe hypothermia presents with apnea, coma, nonreactive pupils, oliguria, areflexia, hypotension, bradycardia, and continued cardiac abnormalities, such as ventricular arrhythmias and asystole.
Laboratory evaluation. No specific laboratory tests are needed to diagnose hypothermia. General lab tests, however, may help determine whether hypothermia is the result, or the cause, of the clinical scenario. Recommended laboratory tests for making that determination include a complete blood count (CBC), chemistry panel, arterial blood gases, fingerstick glucose, and coagulation panel.
Results of lab tests may be abnormal because of the body’s decreased core body temperature. White blood cells and platelets in the CBC, for example, may be decreased due to splenic sequestration; these findings reverse with rewarming. With every 1°C (1.8°F) drop in core body temperature, hematocrit increases 2%.3 Sodium, chloride, and magnesium concentrations do not display consistent abnormalities with any core body temperature >25°C (77°F),3,8 but potassium levels may fluctuate because of acid-base changes that occur during rewarming.1 Creatinine and creatine kinase levels may be increased secondary to rhabdomyolysis or acute tubular necrosis.1
Arterial blood gases typically show metabolic acidosis or respiratory alkalosis, or both.8 Prothrombin time and partial thromboplastin time are typically elevated in vivo, secondary to temperature-dependent enzymes in the coagulation cascade, but are reported normal in a blood specimen that is heated to 37°C (98.6°F) prior to analysis.1,8
Both hyperglycemia and hypoglycemia can be associated with hypothermia. The lactate level can be elevated, due to hypoperfusion. Hepatic impairment may be seen secondary to decreased cardiac output. An increase in the lipase level may also occur.3
When a hypothermic patient fails to respond to rewarming, or there is no clear source of cold exposure, consider testing for other causes of the problem, including hypothyroidism and adrenal insufficiency (see “Differential diagnosis”). Hypothermia may also decrease thyroid function in people with preexisting disease.
Other laboratory studies that can be considered include fibrinogen, blood-alcohol level, urine toxicology screen, and blood and fluid cultures.3
Imaging. Imaging studies are not performed routinely in the setting of hypothermia; however:
- Chest radiography can be considered to assess for aspiration pneumonia, vascular congestion, and pulmonary edema.
- Computed tomography (CT) of the head is helpful in the setting of trauma or if mental status does not clear with rewarming.3
- Bedside ultrasonography can assess for cardiac activity, volume status, pulmonary edema, free fluid, and trauma. (See "Point-of-care ultrasound: Coming soon to primary care?" J Fam Pract. 2018;67:70-80.)
Electrocardiography. An electrocardiogram is essential to evaluate for arrhythmias. Findings associated with hypothermia are prolongation of PR, QRS, and QT intervals; ST-segment elevation, T-wave inversion; and Osborn waves (J waves), which represent a positive deflection at the termination of the QRS complex with associated J-point elevation.8 Osborn waves generally present when the core body temperature is <32°C (89.6°F) and become larger as the core body temperature drops further.3
Differential diagnosis. Hypothermia is most commonly caused by environmental exposure, but the differential diagnosis is broad: many medical conditions, as well as drug and alcohol intoxication, can contribute to hypothermia (TABLE 31).
Treatment: Usually unnecessary, sometimes crucial
Most patients with mild hypothermia recover completely with little intervention. These patients should be evaluated for cognitive irregularities and observed in the ED before discharge.9 Moderate and severe hypothermia patients should be assessed using pre-hospital protocols and given cardiopulmonary resuscitation (CPR) for cardiac arrest. Pre-hospital providers should rely more on symptoms in guiding their treatment response because core body temperature measurements can be difficult to obtain, and the response to a drop in core body temperature varies from patient to patient.10
Early considerations: Airway, breathing, circulation (ABC)
A first responder might have difficulty palpating the pulse of a hypothermic patient if that patient’s cardiopulmonary effort is diminished.9 This inability to palpate a pulse should not delay treatment unless the patient presents with lethal injury; the scene is unsafe; the chest is too stiff for CPR; do-not-resuscitate status is present; or the patient was buried in an avalanche for ≥35 minutes and the airway is filled with snow (FIGURE3,11,12). Pulse should be checked carefully for 60 seconds. If pulses are not present, CPR should be initiated.
Prevention of further heat loss should begin promptly for hypothermic patients who retain a perfusing rhythm.11 Lifesaving interventions, such as airway management, vascular access for volume replenishment, and defibrillation for ventricular tachycardia or ventricular fibrillation should be carried out according to Advanced Cardiac Life Support protocols.11 Patients in respiratory distress or incapable of protecting their airway because of altered mental status should undergo endotracheal intubation. Fluid resuscitation with isotonic crystalloid fluids, warmed to 40°C (104°F) to 42°C (~107°F) and delivered through 2 large-bore, peripheral intravenous (IV) needles, can be considered.
Special care should be taken when moving a hypothermic patient. Excessive movement can lead to stimulation of the irritable hypothermic heart and cause an arrhythmia.
Medical therapy. Caution is advised because the reduced metabolism of a hypothermic patient can lead to potentially toxic accumulation of drugs peripherally. In fact, outcomes have not been positively influenced by routine use of medications, other than treatment of ventricular fibrillation with amiodarone.11 Any intravenous (IV) drug should be held until the patient’s core temperature is >30°C (>86°F).11
Vasopressors can be beneficial during rewarming for a patient in cardiac arrest and are a reasonable consideration.2 Nitroglycerin, in conjunction with active external rewarming, can increase the overall hourly temperature gain in a moderately hypothermic patient.13
Rewarming. The extent of rewarming required can be predicted by the severity of hypothermia (FIGURE3,11,12). Mildly hypothermic patients can generally be rewarmed using passive external measures. Patients with moderate hypothermia benefit from active rewarming in addition to passive measures. Intervention for severe hypothermia requires external rewarming and internal warming, with admission to the intensive care unit.
Treatment plans for severely hypothermic patients differ, depending on whether the person has a perfusing or nonperfusing cardiac rhythm. Patients who maintain a perfusing rhythm can be rewarmed using external methods (although core rewarming is used more often). Patients who do not have a perfusing rhythm require more invasive procedures.11 When using any rewarming method, afterdrop phenomenon can occur: ie, vasodilation, brought on by rewarming, causes a drop in core body temperature, as cooler peripheral blood returns to the central circulation. This effect may be reduced by focused rewarming of the trunk prior to rewarming the extremities.3
Rewarming for mild hypothermia patients begins with passive external techniques. First, the patient is moved away from the environment for protection from further exposure. Next, wet or damaged clothing is removed, blankets or foil insulators are applied, and room temperature is maintained at ≥28°C (82°F).3,11,13,14
If the patient’s temperature does not normalize, or if the patient presented with moderate or severe hypothermia, rewarming is continued with active external and internal measures. Active external rewarming can supplement passive measures using radiant heat from warmed blankets, air rewarming devices, and heating pads.3,13,14 Active internal rewarming techniques rely on invasive measures to raise the core temperature. Heated crystalloid IV fluids do not treat hypothermia, but do help reduce further heat loss and can be helpful in patients in need of volume resuscitation.3,13
Severely hypothermic patients might require more invasive active internal rewarming techniques, such as body-cavity lavage and extracorporeal methods. Body-cavity lavage can be facilitated with large volumes (10-120 L) of warm fluid at 40°C to 42°C, circulated through the thoracic or abdominal cavities to raise core body temperature 3°C to 6°C per hour.3,13
Extracorporeal rewarming can be achieved through hemodialysis, continuous arteriovenous rewarming (CAVR), continuous veno-venous rewarming (CVVR), or cardiopulmonary bypass.3,13 Research has shown cardiopulmonary bypass to be the most effective technique, with as high as a 7°C rise in core body temperature per hour; CVVR and CAVR are less invasive, however, and more readily available in hospitals.3,11,13
Rewarming interventions should continue until return of spontaneous circulation and core body temperature reaches 32°C (89.6°F) to 34°C (93.2°F).11 Overall, resuscitation efforts may take longer than normal due to the need for rewarming and should continue until the patient has achieved a normal temperature of 37°C (97.8°F).
Prognosis varies with severity, the health of the patient
In healthy, mildly hypothermic patients, full recovery is common if heat loss is minimized and the cause is treated. Moderately hypothermic patients who receive proper care can also have a favorable result. Outcomes for severe hypothermia vary with duration, comorbidities, and severity of core body temperature loss.15
Immediate initiation of rewarming by pre-hospital providers improves outcomes, and higher mortality has been demonstrated with hospital admission temperatures <35°C (95°F).15 Almost 100% of primary hypothermia patients with cardiac stability who were treated using active external and minimally invasive rewarming techniques survived with an intact neurologic system.12 Fifty percent of patients who endured cardiac arrest or who were treated with extracorporeal rewarming had an intact neurologic system. In cardiac arrest cases without significant underlying disease or trauma, and in which hypoxia did not precede hypothermia, full recovery is possible (and has been observed).12
CASE
Mr. S was given a diagnosis of mild to moderate hypothermia and transferred to the nearest ED for further treatment. His age had put him at increased risk of hypothermia. The work-up included laboratory testing (CBC, chemistry panel, thyroid-stimulating hormone, urinalysis, and blood cultures), electrocardiography, chest radiography, and CT of the head.
The chest radiograph showed pneumonia. Based on the results of blood culture, bacterial infection (pneumonia) was determined to be the underlying cause of hypothermia. Mr. S was started on antibiotics.
CORRESPONDENCE
Natasha J. Pyzocha, DO, Bldg 1058, 1856 Irwin Dr, Fort Carson, CO 80913; natasha.j.pyzocha.mil@mail.mil.
CASE
Patrick S, an 85-year-old man with multiple medical problems, was brought to his primary care provider after being found at home with altered mental status. His caretaker reported that Mr. S had been using extra blankets in bed and sleeping more, but he hadn’t had significant outdoor exposure. Measurement of his vital signs revealed tachycardia, tachypnea, hypotension, and a rectal temperature of 32°C (89.6°F).
How would you proceed with the care of this patient?
What is accidental hypothermia?
Accidental hypothermia is an unintentional drop in core body temperature to <35°C (<95°F). Mild hypothermia is defined as a core body temperature of 32°C to 35°C (90°F - 95°F); moderate hypothermia, 28°C to 32°C (82°F - 90°F); and severe hypothermia, <28°C (<82°F).1
The International Commission for Mountain Emergency Medicine divides hypothermia into 5 categories, emphasizing the clinical features of each stage as a guide to treatment (TABLE 1).2 These categories were adopted to help prehospital rescuers estimate the severity of hypothermia using physical symptoms. For example, most patients stop shivering at approximately 30°C (86°F)—the “moderate (HT II)” category of hypothermia—although this response varies widely from patient to patient. Notably, there are reports in the literature of survival in hypothermia with a temperature as low as 13.7°C (56.7°F) and with cardiac arrest for as long as 8 hours and 40 minutes, although these events are rare.3
Each year, approximately 700 deaths in the United States are the result of hypothermia.4 Between 1995 to 2004 in the United States, it is estimated that 15,574 visits were made to a health care provider or facility for hypothermia and other cold-related concerns.5 Based on reports in the international literature, the incidence of nonlethal hypothermia is much greater than the incidence of lethal hypothermia.5 Almost half of deaths from hypothermia are in people older than age 65 years; the male to female ratio is 2.5:1.1
Variables that predispose the body to temperature dysregulation include extremes of age, comorbid conditions, intoxication, chronic cold exposure, immersion accident, mental illness, impaired shivering, and lack of acclimatization.1 The most common causes of death associated with hypothermia are falls, drownings, and cardiovascular disease.4 In a 2008 study, hypothermia and other cold-related morbidity emergency department (ED) visits required more transfers of patients to a critical care unit than any other reason for visiting an ED (risk ratio, 6.73; 95% confidence interval, 1.8-25).5 Mortality among inpatients whose hypothermia is classified as moderate or severe reaches as high as 40%.3
More than just cold-weather exposure
Accidental hypothermia occurs when heat loss is superseded by the body’s ability to generate heat. It commonly happens in cold environments but can also occur at higher temperatures if the body’s thermoregulatory system malfunctions.
Environmental or iatrogenic factors (ie, primary hypothermia), such as wind, water immersion, wetness, aggressive fluid resuscitation, and heat stroke treatment can make people more susceptible to hypothermia. Medical conditions (ie, secondary hypothermia), such as burns, exfoliative dermatitis, severe psoriasis, hypoadrenalism, hypopituitarism, hypothyroidism, acute spinal cord transection, head trauma, stroke, tumor, pneumonia, Wernicke’s disease (encephalopathy), and sepsis can also predispose to hypothermia.1 Drugs, such as ethanol, phenothiazines, and sedative–hypnotics may decrease the hypothermia threshold.1 (For information on preventing hypothermia, see TABLE 2.6)
Pathophysiology: The role of the hypothalamus
Humans maintain body temperature by balancing heat production and heat loss to the environment. Heat is lost through the skin and lungs by 5 different mechanisms: radiation, conduction, convection, evaporation, and respiration. Convective heat loss to cold air and conductive heat loss to water are the most common mechanisms of accidental hypothermia.7
To maintain temperature homeostasis at 37°C (98.6°F) (±0.5°C [±0.9°F]), the hypothalamus receives input from central and peripheral thermal receptors and stimulates heat production through shivering, increasing the basal metabolic rate 2-fold to 5-fold.1 The hypothalamus also increases thyroid, catecholamine, and adrenal activity to increase the body’s production of heat and raise core temperature.
Heat conservation occurs by activation of sympathetically mediated vasoconstriction, reducing conduction to the skin, where cooling is greatest. After time, temperature regulation in the body becomes overwhelmed and catecholamine levels return to a pre-hypothermic state.
At 35°C (95°F), neurologic function begins to decline; at 32°C (89.6°F), metabolism, ventilation, and cardiac output decrease until shivering ceases. Changes in peripheral blood flow can create a false warming sensation, causing a person to remove clothing, a phenomenon referred to as paradoxical undressing. As hypothermia progresses, the neurologic, respiratory, and cardiac systems continue to slow until there is eventual cardiorespiratory failure.
Assessment and diagnosis
History and physical examination. A high index of suspicion for the diagnosis of hypothermia is essential, especially when caring for the elderly or patients presenting with unexplained illness. Often, symptoms of a primary condition may overshadow those reflecting hypothermia. In a multicenter survey that reviewed 428 cases of accidental hypothermia in the United States, 44% of patients had an underlying illness; 18%, coexisting infection; 19%, trauma; and 6%, overdose.3
There are no strict diagnostic criteria for hypothermia other than a core body temperature <35°C (<95°F). Standard thermometers often do not read below 34.4°C (93.2°F), so it is recommended that a rectal thermometer capable of reading low body temperatures be used for accurate measurement.
Hypothermic patients can exhibit a variety of symptoms, depending on the degree of decrease in core body temperature1:
- A mildly hypothermic patient might present with any combination of tachypnea, tachycardia, ataxia, impaired judgment, shivering, and vasoconstriction.
- Moderate hypothermia typically manifests as a decreased heart rate, decreased blood pressure, decreased level of consciousness, decreased respiratory effort, dilated pupils, extinction of shivering, and hyporeflexia. Cardiac abnormalities, such as atrial fibrillation and junctional bradycardia, may be seen in moderate hypothermia.
- Severe hypothermia presents with apnea, coma, nonreactive pupils, oliguria, areflexia, hypotension, bradycardia, and continued cardiac abnormalities, such as ventricular arrhythmias and asystole.
Laboratory evaluation. No specific laboratory tests are needed to diagnose hypothermia. General lab tests, however, may help determine whether hypothermia is the result, or the cause, of the clinical scenario. Recommended laboratory tests for making that determination include a complete blood count (CBC), chemistry panel, arterial blood gases, fingerstick glucose, and coagulation panel.
Results of lab tests may be abnormal because of the body’s decreased core body temperature. White blood cells and platelets in the CBC, for example, may be decreased due to splenic sequestration; these findings reverse with rewarming. With every 1°C (1.8°F) drop in core body temperature, hematocrit increases 2%.3 Sodium, chloride, and magnesium concentrations do not display consistent abnormalities with any core body temperature >25°C (77°F),3,8 but potassium levels may fluctuate because of acid-base changes that occur during rewarming.1 Creatinine and creatine kinase levels may be increased secondary to rhabdomyolysis or acute tubular necrosis.1
Arterial blood gases typically show metabolic acidosis or respiratory alkalosis, or both.8 Prothrombin time and partial thromboplastin time are typically elevated in vivo, secondary to temperature-dependent enzymes in the coagulation cascade, but are reported normal in a blood specimen that is heated to 37°C (98.6°F) prior to analysis.1,8
Both hyperglycemia and hypoglycemia can be associated with hypothermia. The lactate level can be elevated, due to hypoperfusion. Hepatic impairment may be seen secondary to decreased cardiac output. An increase in the lipase level may also occur.3
When a hypothermic patient fails to respond to rewarming, or there is no clear source of cold exposure, consider testing for other causes of the problem, including hypothyroidism and adrenal insufficiency (see “Differential diagnosis”). Hypothermia may also decrease thyroid function in people with preexisting disease.
Other laboratory studies that can be considered include fibrinogen, blood-alcohol level, urine toxicology screen, and blood and fluid cultures.3
Imaging. Imaging studies are not performed routinely in the setting of hypothermia; however:
- Chest radiography can be considered to assess for aspiration pneumonia, vascular congestion, and pulmonary edema.
- Computed tomography (CT) of the head is helpful in the setting of trauma or if mental status does not clear with rewarming.3
- Bedside ultrasonography can assess for cardiac activity, volume status, pulmonary edema, free fluid, and trauma. (See "Point-of-care ultrasound: Coming soon to primary care?" J Fam Pract. 2018;67:70-80.)
Electrocardiography. An electrocardiogram is essential to evaluate for arrhythmias. Findings associated with hypothermia are prolongation of PR, QRS, and QT intervals; ST-segment elevation, T-wave inversion; and Osborn waves (J waves), which represent a positive deflection at the termination of the QRS complex with associated J-point elevation.8 Osborn waves generally present when the core body temperature is <32°C (89.6°F) and become larger as the core body temperature drops further.3
Differential diagnosis. Hypothermia is most commonly caused by environmental exposure, but the differential diagnosis is broad: many medical conditions, as well as drug and alcohol intoxication, can contribute to hypothermia (TABLE 31).
Treatment: Usually unnecessary, sometimes crucial
Most patients with mild hypothermia recover completely with little intervention. These patients should be evaluated for cognitive irregularities and observed in the ED before discharge.9 Moderate and severe hypothermia patients should be assessed using pre-hospital protocols and given cardiopulmonary resuscitation (CPR) for cardiac arrest. Pre-hospital providers should rely more on symptoms in guiding their treatment response because core body temperature measurements can be difficult to obtain, and the response to a drop in core body temperature varies from patient to patient.10
Early considerations: Airway, breathing, circulation (ABC)
A first responder might have difficulty palpating the pulse of a hypothermic patient if that patient’s cardiopulmonary effort is diminished.9 This inability to palpate a pulse should not delay treatment unless the patient presents with lethal injury; the scene is unsafe; the chest is too stiff for CPR; do-not-resuscitate status is present; or the patient was buried in an avalanche for ≥35 minutes and the airway is filled with snow (FIGURE3,11,12). Pulse should be checked carefully for 60 seconds. If pulses are not present, CPR should be initiated.
Prevention of further heat loss should begin promptly for hypothermic patients who retain a perfusing rhythm.11 Lifesaving interventions, such as airway management, vascular access for volume replenishment, and defibrillation for ventricular tachycardia or ventricular fibrillation should be carried out according to Advanced Cardiac Life Support protocols.11 Patients in respiratory distress or incapable of protecting their airway because of altered mental status should undergo endotracheal intubation. Fluid resuscitation with isotonic crystalloid fluids, warmed to 40°C (104°F) to 42°C (~107°F) and delivered through 2 large-bore, peripheral intravenous (IV) needles, can be considered.
Special care should be taken when moving a hypothermic patient. Excessive movement can lead to stimulation of the irritable hypothermic heart and cause an arrhythmia.
Medical therapy. Caution is advised because the reduced metabolism of a hypothermic patient can lead to potentially toxic accumulation of drugs peripherally. In fact, outcomes have not been positively influenced by routine use of medications, other than treatment of ventricular fibrillation with amiodarone.11 Any intravenous (IV) drug should be held until the patient’s core temperature is >30°C (>86°F).11
Vasopressors can be beneficial during rewarming for a patient in cardiac arrest and are a reasonable consideration.2 Nitroglycerin, in conjunction with active external rewarming, can increase the overall hourly temperature gain in a moderately hypothermic patient.13
Rewarming. The extent of rewarming required can be predicted by the severity of hypothermia (FIGURE3,11,12). Mildly hypothermic patients can generally be rewarmed using passive external measures. Patients with moderate hypothermia benefit from active rewarming in addition to passive measures. Intervention for severe hypothermia requires external rewarming and internal warming, with admission to the intensive care unit.
Treatment plans for severely hypothermic patients differ, depending on whether the person has a perfusing or nonperfusing cardiac rhythm. Patients who maintain a perfusing rhythm can be rewarmed using external methods (although core rewarming is used more often). Patients who do not have a perfusing rhythm require more invasive procedures.11 When using any rewarming method, afterdrop phenomenon can occur: ie, vasodilation, brought on by rewarming, causes a drop in core body temperature, as cooler peripheral blood returns to the central circulation. This effect may be reduced by focused rewarming of the trunk prior to rewarming the extremities.3
Rewarming for mild hypothermia patients begins with passive external techniques. First, the patient is moved away from the environment for protection from further exposure. Next, wet or damaged clothing is removed, blankets or foil insulators are applied, and room temperature is maintained at ≥28°C (82°F).3,11,13,14
If the patient’s temperature does not normalize, or if the patient presented with moderate or severe hypothermia, rewarming is continued with active external and internal measures. Active external rewarming can supplement passive measures using radiant heat from warmed blankets, air rewarming devices, and heating pads.3,13,14 Active internal rewarming techniques rely on invasive measures to raise the core temperature. Heated crystalloid IV fluids do not treat hypothermia, but do help reduce further heat loss and can be helpful in patients in need of volume resuscitation.3,13
Severely hypothermic patients might require more invasive active internal rewarming techniques, such as body-cavity lavage and extracorporeal methods. Body-cavity lavage can be facilitated with large volumes (10-120 L) of warm fluid at 40°C to 42°C, circulated through the thoracic or abdominal cavities to raise core body temperature 3°C to 6°C per hour.3,13
Extracorporeal rewarming can be achieved through hemodialysis, continuous arteriovenous rewarming (CAVR), continuous veno-venous rewarming (CVVR), or cardiopulmonary bypass.3,13 Research has shown cardiopulmonary bypass to be the most effective technique, with as high as a 7°C rise in core body temperature per hour; CVVR and CAVR are less invasive, however, and more readily available in hospitals.3,11,13
Rewarming interventions should continue until return of spontaneous circulation and core body temperature reaches 32°C (89.6°F) to 34°C (93.2°F).11 Overall, resuscitation efforts may take longer than normal due to the need for rewarming and should continue until the patient has achieved a normal temperature of 37°C (97.8°F).
Prognosis varies with severity, the health of the patient
In healthy, mildly hypothermic patients, full recovery is common if heat loss is minimized and the cause is treated. Moderately hypothermic patients who receive proper care can also have a favorable result. Outcomes for severe hypothermia vary with duration, comorbidities, and severity of core body temperature loss.15
Immediate initiation of rewarming by pre-hospital providers improves outcomes, and higher mortality has been demonstrated with hospital admission temperatures <35°C (95°F).15 Almost 100% of primary hypothermia patients with cardiac stability who were treated using active external and minimally invasive rewarming techniques survived with an intact neurologic system.12 Fifty percent of patients who endured cardiac arrest or who were treated with extracorporeal rewarming had an intact neurologic system. In cardiac arrest cases without significant underlying disease or trauma, and in which hypoxia did not precede hypothermia, full recovery is possible (and has been observed).12
CASE
Mr. S was given a diagnosis of mild to moderate hypothermia and transferred to the nearest ED for further treatment. His age had put him at increased risk of hypothermia. The work-up included laboratory testing (CBC, chemistry panel, thyroid-stimulating hormone, urinalysis, and blood cultures), electrocardiography, chest radiography, and CT of the head.
The chest radiograph showed pneumonia. Based on the results of blood culture, bacterial infection (pneumonia) was determined to be the underlying cause of hypothermia. Mr. S was started on antibiotics.
CORRESPONDENCE
Natasha J. Pyzocha, DO, Bldg 1058, 1856 Irwin Dr, Fort Carson, CO 80913; natasha.j.pyzocha.mil@mail.mil.
1. McCullough L, Arora S. Diagnosis and treatment of hypothermia. Am Fam Physician. 2004;70:2325-2332.
2. Durrer B, Brugger H, Syme D; International Commission for Mountain Emergency Medicine. The medical on-site treatment of hypothermia: ICAR-MEDCOM recommendation. High Alt Med Biol. 2003;4.
3. Rischall ML, Rowland-Fisher A. Evidence-based management of accidental hypothermia in the emergency department. Emerg Med Pract. 2016;18:1-18.
4. Study: Hypothermia-related deaths—United States, 2003-2004. Atlanta, GA: Centers for Disease Control and Prevention; 2005. Available at: www.cdc.gov/media/pressrel/fs050224.htm. Accessed March 1, 2018.
5. Baumgartner EA, Belson M, Rubin C, et al. Hypothermia and other cold-related morbidity emergency department visits: United States, 1995-2004. Wilderness Environ Med. 2008;19:233-237.
6. Centers for Disease Control and Prevention. Preventing injuries associated with extreme cold. Int J Trauma Nurs. 2001;7:26-30.
7. Jolly BT, Ghezzi KT. Accidental hypothermia. Emerg Med Clin North Am. 1992;10:311-327.
8. Mechem CC. Hypothermia and hyperthermia. In: Lanken PN, Manaker S, Hanson CW III, eds. The Intensive Care Unit Manual. Philadelphia: WB Saunders; 2000.
9. Weinberg AD. Hypothermia. Ann Emerg Med. 1993;22:370-377.
10. Zafren K, Giesbrecht GG, Danzl DF, et al. Wilderness Medical Society practice guidelines for the out-of-hospital evaluation and treatment of accidental hypothermia. Wilderness Environ Med. 2014;25:425-445.
11. Web-based integrated 2010 & 2015 guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Part 10: Special Circumstances of Resuscitation. Dallas, TX: American Heart Association; 2017. Available at: https://eccguidelines.heart.org/index.php/circulation/cpr-ecc-guidelines-2/part-10-special-circumstances-of-resuscitation. Accessed March 1, 2018.
12. Brown DJ, Brugger H, Boyd J, et al. Accidental hypothermia. N Engl J Med. 2012;367:1930-1938.
13. Petrone P, Asensio JA, Marini CP. Management of accidental hypothermia and cold injury. Curr Probl Surg. 2014;51:417-431.
14. Fudge J. Preventing and managing hypothermia and frostbite injury. Sports Health. 2016;8:133-139.
15. Martin RS, Kilgo PD, Miller PR, et al. Injury-associated hypothermia: an analysis of the 2004 National Trauma Data Bank. Shock. 2005;24:114-118.
1. McCullough L, Arora S. Diagnosis and treatment of hypothermia. Am Fam Physician. 2004;70:2325-2332.
2. Durrer B, Brugger H, Syme D; International Commission for Mountain Emergency Medicine. The medical on-site treatment of hypothermia: ICAR-MEDCOM recommendation. High Alt Med Biol. 2003;4.
3. Rischall ML, Rowland-Fisher A. Evidence-based management of accidental hypothermia in the emergency department. Emerg Med Pract. 2016;18:1-18.
4. Study: Hypothermia-related deaths—United States, 2003-2004. Atlanta, GA: Centers for Disease Control and Prevention; 2005. Available at: www.cdc.gov/media/pressrel/fs050224.htm. Accessed March 1, 2018.
5. Baumgartner EA, Belson M, Rubin C, et al. Hypothermia and other cold-related morbidity emergency department visits: United States, 1995-2004. Wilderness Environ Med. 2008;19:233-237.
6. Centers for Disease Control and Prevention. Preventing injuries associated with extreme cold. Int J Trauma Nurs. 2001;7:26-30.
7. Jolly BT, Ghezzi KT. Accidental hypothermia. Emerg Med Clin North Am. 1992;10:311-327.
8. Mechem CC. Hypothermia and hyperthermia. In: Lanken PN, Manaker S, Hanson CW III, eds. The Intensive Care Unit Manual. Philadelphia: WB Saunders; 2000.
9. Weinberg AD. Hypothermia. Ann Emerg Med. 1993;22:370-377.
10. Zafren K, Giesbrecht GG, Danzl DF, et al. Wilderness Medical Society practice guidelines for the out-of-hospital evaluation and treatment of accidental hypothermia. Wilderness Environ Med. 2014;25:425-445.
11. Web-based integrated 2010 & 2015 guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Part 10: Special Circumstances of Resuscitation. Dallas, TX: American Heart Association; 2017. Available at: https://eccguidelines.heart.org/index.php/circulation/cpr-ecc-guidelines-2/part-10-special-circumstances-of-resuscitation. Accessed March 1, 2018.
12. Brown DJ, Brugger H, Boyd J, et al. Accidental hypothermia. N Engl J Med. 2012;367:1930-1938.
13. Petrone P, Asensio JA, Marini CP. Management of accidental hypothermia and cold injury. Curr Probl Surg. 2014;51:417-431.
14. Fudge J. Preventing and managing hypothermia and frostbite injury. Sports Health. 2016;8:133-139.
15. Martin RS, Kilgo PD, Miller PR, et al. Injury-associated hypothermia: an analysis of the 2004 National Trauma Data Bank. Shock. 2005;24:114-118.
PRACTICE RECOMMENDATIONS
› Measure the patient's temperature with a rectal thermometer capable of reading a temperature <35°C (<95°F) when hypothermia is suspected. C
› Begin prevention of further heat loss promptly for hypothermic patients who retain a perfusing rhythm. C
› Do not consider a patient dead until body temperature has normalized. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series