User login
Bipolar disorder: Making the Dx, selecting the right Rx
THE CASE
A 23-year-old woman seeks medical attention at the request of her boyfriend because she’s been “miserable” for 3 weeks. In the examination room, she slouches in the chair and says her mood is low, her grades have dropped, and she no longer enjoys social gatherings or her other usual activities. She has no thoughts of suicide, no weight loss, and no somatic symptoms.
She says she is generally healthy, does not take any regular medications, and has never been pregnant. When asked about previous similar episodes, she admits to feeling this way about 3 times a year for one to 2 months at a time. She has tried different antidepressants, which haven’t helped much and have made her irritable and interfered with sleep.
When asked about mania or hypomania, she says there are short periods, roughly a couple of weeks 2 or 3 times a year, when she will get a lot of work done and can get by with little sleep. She has never gone on “spending sprees,” though, or indulged in any other unusual or dangerous behavior. And she has never been hospitalized for symptoms.
Bipolar disorders, over time, typically cause fluctuations in mood, activity, and energy level. If disorders go untreated, a patient’s behavior may cause considerable damage to relationships, finances, and reputations. And for some patients, the disorder can take the ultimate toll, resulting in death by suicide or accident.
Subtypes of bipolar disorder differ in the timing and severity of manic (or hypomanic) and depressive symptoms or episodes. Type I is the classic manic-depressive illness; type II is characterized by chronic treatment-resistant depression punctuated by hypomanic episodes; and cyclothymia leads to chronic fluctuations in mood. The diagnostic category “bipolar disorder not otherwise specified” applies to patients who meet some, but not all, of the criteria for other bipolar disorder subtypes.1
Prevalence. As with other mood symptoms or disorders, patients with bipolar disorder are often seen first in primary care due, in part, to barriers to obtaining psychiatric care or to avoidance of the perceived stigma in seeking such care.2 In a systematic review of patients who were interviewed randomly in primary care settings, 0.5% to 4.3% met criteria for bipolar disorder.3 The average age of onset for bipolar disorder is 15 to 19 years.4 In the United States, the prevalence of bipolar disorder type I is 1%; type II is 1.1%.3
The cause of bipolar disorder is unknown, but familial predisposition, biopsychosocial factors, and environment all seem to play a role. Children of parents with bipolar disorder have a 4% to 15% chance of receiving the same diagnosis, compared with children of parents without bipolar disorder, whose risk is only as high as 2%.5,6
Clinical presentation varies
When patients with bipolar disorder are first seen in the office, their state may be depression, mania, hypomania, or even euthymia. Keep in mind that the first 3 aberrations may indicate other disorders, either

Verify a true depressive episode
Symptoms must last for 2 weeks and include anhedonia or depressed mood, as well as some combination of changes in sleep, increased feelings of guilt, poor concentration, changes in appetite, loss of energy, psychomotor agitation or retardation, or suicidal thoughts.1
Know the criteria for mania
True mania is a distinct period of abnormally and persistently elevated, expansive, or irritable mood, accompanied by abnormally and persistently increased activity or energy, and lasting at least one week for most of the day, nearly every day (or any duration if hospitalization is necessary).
During that time, the patient must also exhibit at least 3 or more of the following symptoms (not counting irritability, if present): 1
- distractibility,
- insomnia,
- grandiosity,
- flights of ideas,
- increased goal-directed activity or agitation,
- rapid/pressured speech, or
- reckless behaviors.
How hypomania differs from mania. The symptoms of hypomania are less severe than those of mania—eg, social functioning is less impaired or is even normal, and there is no need for hospitalization. Patients may feel they have been much more productive than usual or have needed less sleep to engage in daily activities. Hypomania may be present but not reported by patients who perceive nothing wrong.1,4
Rule out alternate diagnoses and apply DSM-5 criteria
There are no objective tests to confirm a diagnosis of bipolar disorder. If you suspect bipolar disorder, focus your clinical evaluation on ruling out competing mental health or medical diagnoses, and on determining whether the patient’s history meets criteria for a bipolar disorder as described in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).1
Explore the patient’s psychiatric history (including hospitalizations, medications, and electroconvulsive therapy), general medical history, family history of psychiatric disorders (including suicide), and social history (including substance use and abuse). And carefully observe mental status. Confirming a diagnosis of bipolar disorder may take multiple visits, but strongly suggestive symptoms could warrant empirical treatment.
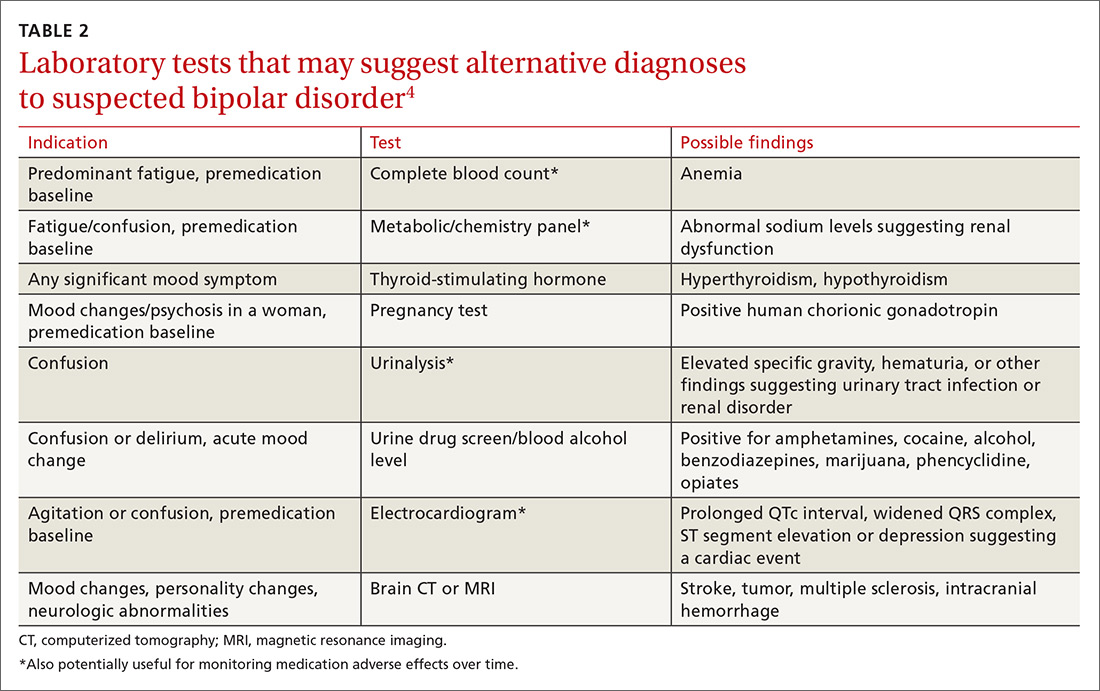
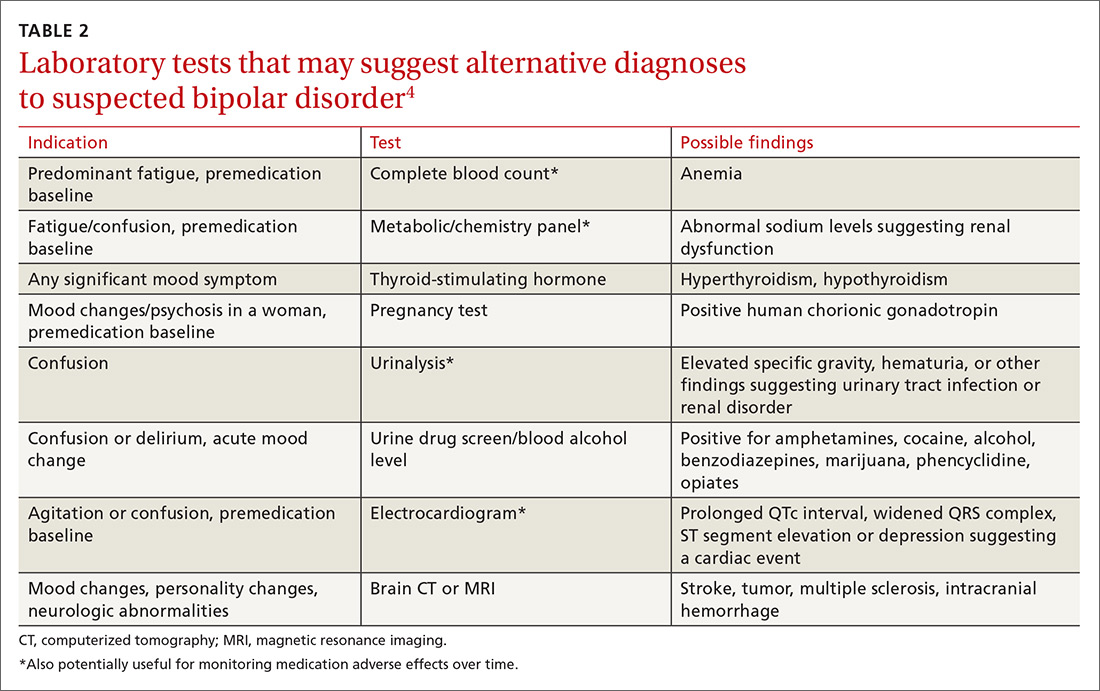
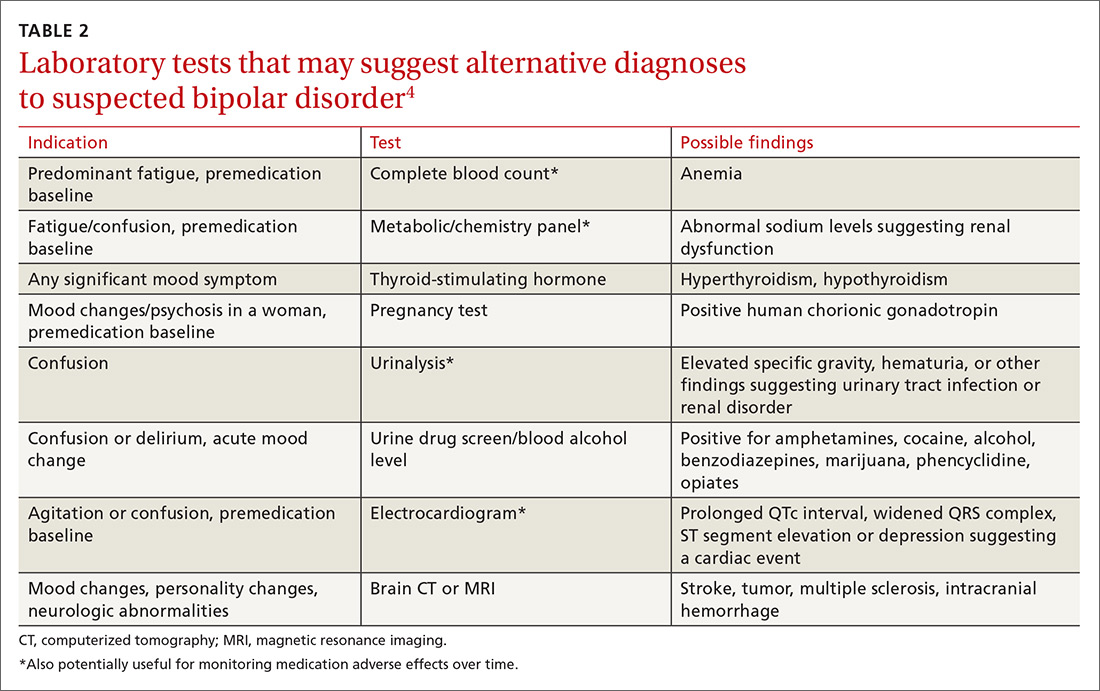
Helpful scales. The Patient Health Questionnaire (PHQ-9; https://www.uspreventiveservicestaskforce.org/Home/GetFileByID/218) and the Beck Depression Inventory (http://www.hr.ucdavis.edu/asap/pdf_files/Beck_Depression_Inventory.pdf) are useful for ruling out depressive disorders. Other scales are available, but they cannot confirm bipolar disorder. Laboratory testing selected according to patient symptoms (TABLE 24) can help rule out alternative diagnoses, but are also useful for establishing a baseline for medications.
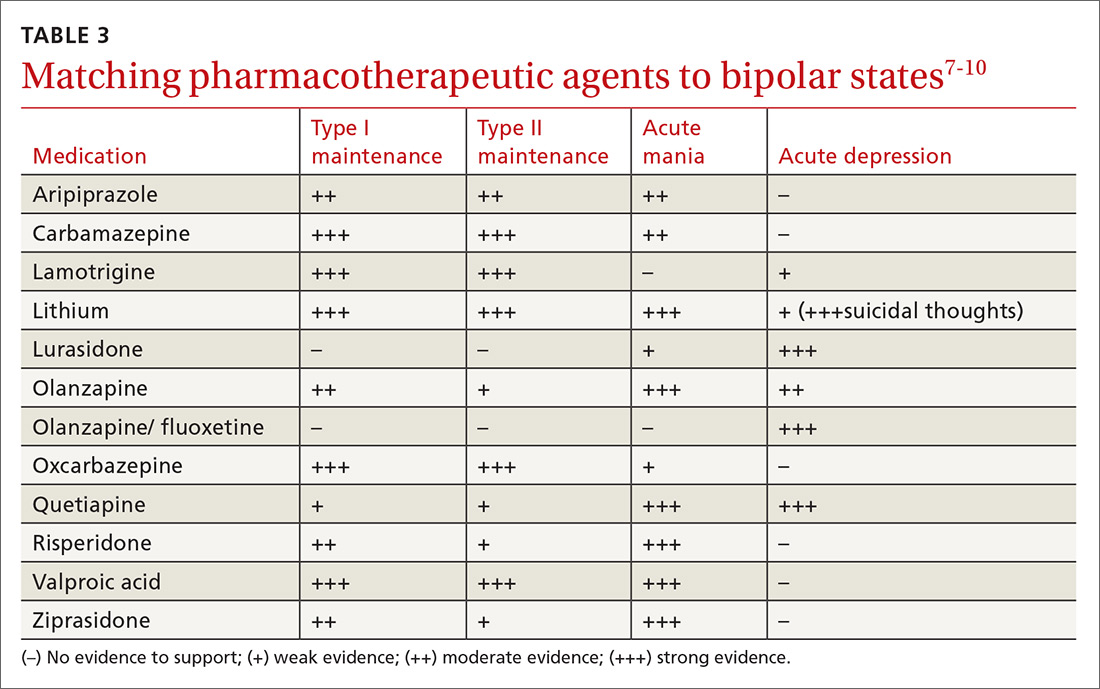
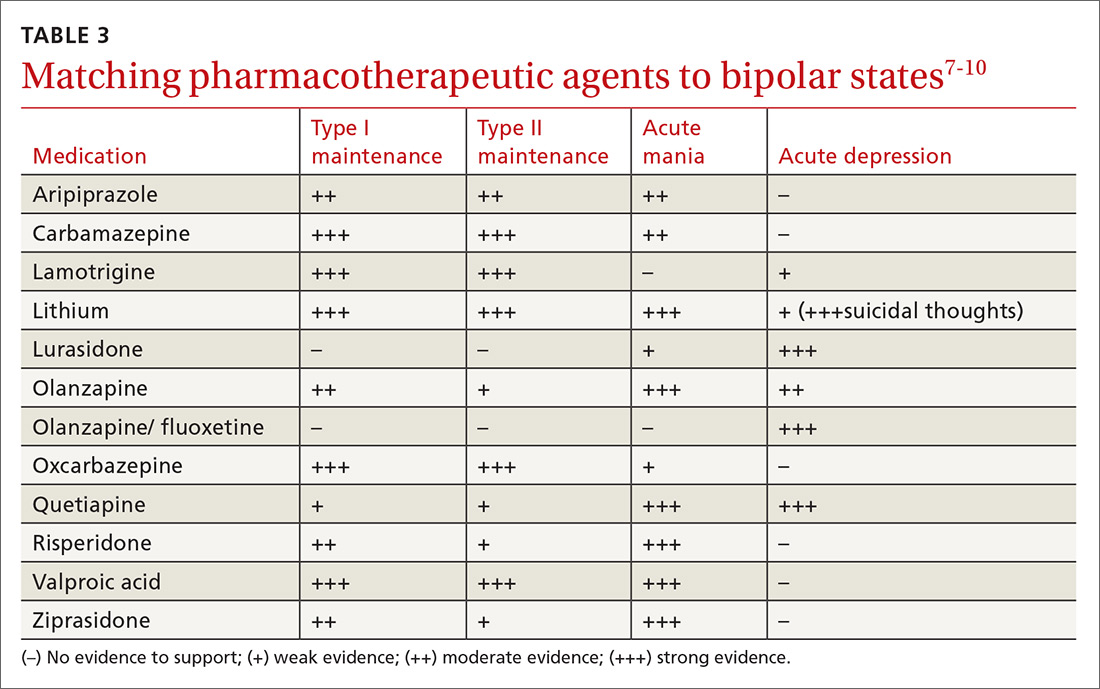
Pharmacologic treatment: Match agents to symptoms
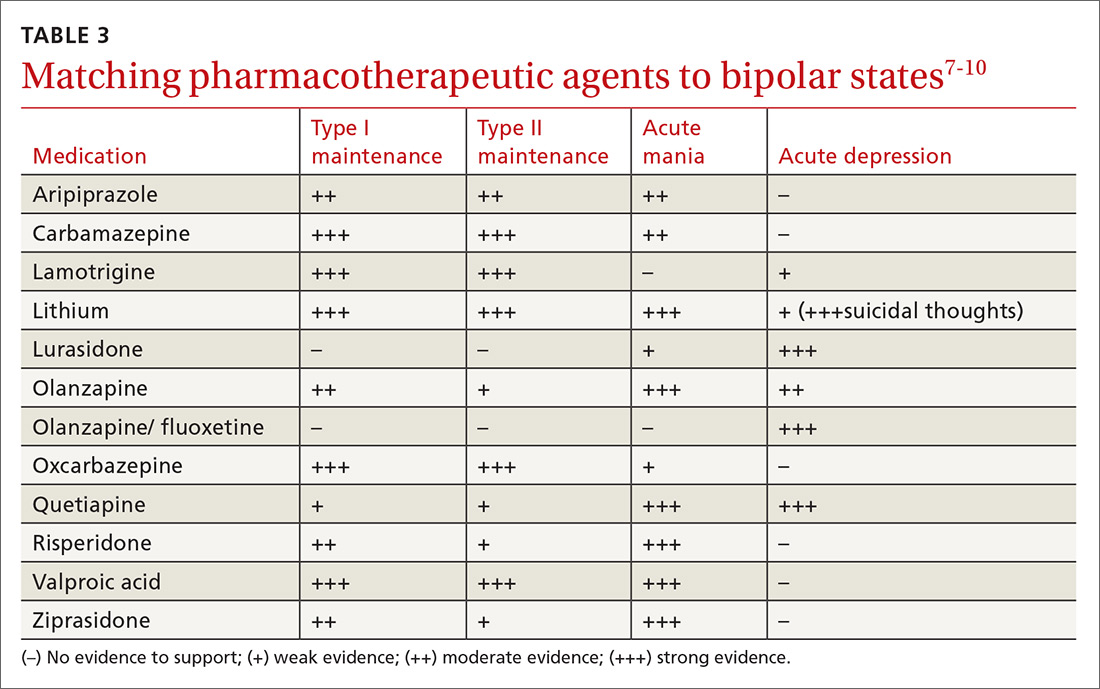
When treating bipolar disorder, choose a drug that targets a patient’s specific symptoms (TABLE 3).7-10 In primary care, the most commonly-used treatments for bipolar disorder type II are lamotrigine, valproic acid, and lithium.11
When to refer
Many cases of bipolar disorder type II can be managed successfully in a primary care practice, as can some cases of stable bipolar disorder type I. Psychiatric consultation may be most beneficial if the patient has recently attempted suicide or has suicidal ideation, has symptoms refractory to treatment, has poor medication adherence, or is misusing medications.
Even when patients are co-managed with psychiatric consultation, family physicians often ensure patients’ medication adherence, help patients understand their illness, manage overall health-related behaviors (including getting sufficient sleep), and make sure patients follow up as needed with their psychiatrist. Often, once patients have achieved equilibrium on mood-stabilizing (or other) medications, you can manage them and monitor medications with further consultation only as needed for clinical deterioration or other issues. Cognitive behavioral therapy may be useful as adjunctive treatment, particularly when patients are in active treatment.12
› CASE
This case is typical for many patients with depressed mood. A few key features in the patient’s history suggest bipolar disorder type II:
- depression that has been refractory to treatment
- multiple failed drug treatments, with mood-related adverse effects
- hypomania perceived as a “productive time,” and not as a problem
- absence of overt manic symptoms.
The patient was given a diagnosis of bipolar disorder type II with current depressed mood and no evidence of acute mania. She was started on valproic acid 250 mg po tid. She reported an initial improvement in mood but stopped the medication after one month because it caused intolerable drowsiness. She was then prescribed lamotrigine progressing gradually in 2-week intervals from 25 mg to 100 mg daily. She tolerated the medication well, and after 3 months of treatment, her mood symptoms improved and she had no further episodes of depressed mood.
CORRESPONDENCE
Michael Jason Wells, MD, Department of Family and Geriatric Medicine, University of Louisville School of Medicine, 201 Abraham Flexner Way, Suite 690, Louisville, KY 40202; mjwell04@louisville.edu.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed (DSM-5). Arlington, VA: American Psychiatric Association; 2013.
2. Kilbourne AM, Goodrich DE, O’Donnell AN, et al. Integrated bipolar disorder management in primary care. Curr Psychiatry Rep. 2012;14:687-695.
3. Cerimele JM, Chwastiak LA, Dodson S, et al. The prevalence of bipolar disorder in primary care samples: a systematic review. Gen Hosp Psychiatry. 2014;36:19-25.
4. Malhi GS, Adams D, Lampe L, et al. Clinical practice recommendations for bipolar disorder. Acta Pscyhiatr Scand. 2009:119(Suppl 439):27-46.
5. Abell S, Ey J. Bipolar Disorder. Clin Pediatr. 2009;48:693-694.
6. Birmaher B, Axelson D, Monk K, et al. Lifetime psychiatric disorders of school-aged offspring of parents with bipolar disorder: the Pittsburgh Bipolar Offspring Study. Arch Gen Psychiatry. 2009;66:287-296.
7. Cipriani A, Hawton K, Stockton S, et al. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ. 2013;346:f3646.
8. De Fruyt J, Deschepper E, Audenaert K, et al. Second generation antipsychotics in the treatment of bipolar depression: a systematic review and meta-analysis. J Psychopharmacol. 2012;26:603-617.
9. Gitlin M, Frye MA. Maintenance therapies in bipolar disorders. Bipolar Disord. 2012:14(Suppl 2):51-65.
10. Labbate LA, Fava M, Rosenbaum JF, et al. Handbook of Psychiatric Drug Therapy. 6th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2010.
11. Ostacher M, Tandon R, Suppes T. Florida Best Practice Psychotherapeutic Medication Guidelines for Adults with Bipolar Disorder: a novel, practical, patient-centered guide for clinicians. J Clin Psychiatry. 2016;77:920-926.
12. Szentagotai A, David D. The efficacy of cognitive behavioral therapy in bipolar disorder: a quantitative meta-analysis. J Clin Psychiatry. 2010;71:66-72.
THE CASE
A 23-year-old woman seeks medical attention at the request of her boyfriend because she’s been “miserable” for 3 weeks. In the examination room, she slouches in the chair and says her mood is low, her grades have dropped, and she no longer enjoys social gatherings or her other usual activities. She has no thoughts of suicide, no weight loss, and no somatic symptoms.
She says she is generally healthy, does not take any regular medications, and has never been pregnant. When asked about previous similar episodes, she admits to feeling this way about 3 times a year for one to 2 months at a time. She has tried different antidepressants, which haven’t helped much and have made her irritable and interfered with sleep.
When asked about mania or hypomania, she says there are short periods, roughly a couple of weeks 2 or 3 times a year, when she will get a lot of work done and can get by with little sleep. She has never gone on “spending sprees,” though, or indulged in any other unusual or dangerous behavior. And she has never been hospitalized for symptoms.
Bipolar disorders, over time, typically cause fluctuations in mood, activity, and energy level. If disorders go untreated, a patient’s behavior may cause considerable damage to relationships, finances, and reputations. And for some patients, the disorder can take the ultimate toll, resulting in death by suicide or accident.
Subtypes of bipolar disorder differ in the timing and severity of manic (or hypomanic) and depressive symptoms or episodes. Type I is the classic manic-depressive illness; type II is characterized by chronic treatment-resistant depression punctuated by hypomanic episodes; and cyclothymia leads to chronic fluctuations in mood. The diagnostic category “bipolar disorder not otherwise specified” applies to patients who meet some, but not all, of the criteria for other bipolar disorder subtypes.1
Prevalence. As with other mood symptoms or disorders, patients with bipolar disorder are often seen first in primary care due, in part, to barriers to obtaining psychiatric care or to avoidance of the perceived stigma in seeking such care.2 In a systematic review of patients who were interviewed randomly in primary care settings, 0.5% to 4.3% met criteria for bipolar disorder.3 The average age of onset for bipolar disorder is 15 to 19 years.4 In the United States, the prevalence of bipolar disorder type I is 1%; type II is 1.1%.3
The cause of bipolar disorder is unknown, but familial predisposition, biopsychosocial factors, and environment all seem to play a role. Children of parents with bipolar disorder have a 4% to 15% chance of receiving the same diagnosis, compared with children of parents without bipolar disorder, whose risk is only as high as 2%.5,6
Clinical presentation varies
When patients with bipolar disorder are first seen in the office, their state may be depression, mania, hypomania, or even euthymia. Keep in mind that the first 3 aberrations may indicate other disorders, either

Verify a true depressive episode
Symptoms must last for 2 weeks and include anhedonia or depressed mood, as well as some combination of changes in sleep, increased feelings of guilt, poor concentration, changes in appetite, loss of energy, psychomotor agitation or retardation, or suicidal thoughts.1
Know the criteria for mania
True mania is a distinct period of abnormally and persistently elevated, expansive, or irritable mood, accompanied by abnormally and persistently increased activity or energy, and lasting at least one week for most of the day, nearly every day (or any duration if hospitalization is necessary).
During that time, the patient must also exhibit at least 3 or more of the following symptoms (not counting irritability, if present): 1
- distractibility,
- insomnia,
- grandiosity,
- flights of ideas,
- increased goal-directed activity or agitation,
- rapid/pressured speech, or
- reckless behaviors.
How hypomania differs from mania. The symptoms of hypomania are less severe than those of mania—eg, social functioning is less impaired or is even normal, and there is no need for hospitalization. Patients may feel they have been much more productive than usual or have needed less sleep to engage in daily activities. Hypomania may be present but not reported by patients who perceive nothing wrong.1,4
Rule out alternate diagnoses and apply DSM-5 criteria
There are no objective tests to confirm a diagnosis of bipolar disorder. If you suspect bipolar disorder, focus your clinical evaluation on ruling out competing mental health or medical diagnoses, and on determining whether the patient’s history meets criteria for a bipolar disorder as described in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).1
Explore the patient’s psychiatric history (including hospitalizations, medications, and electroconvulsive therapy), general medical history, family history of psychiatric disorders (including suicide), and social history (including substance use and abuse). And carefully observe mental status. Confirming a diagnosis of bipolar disorder may take multiple visits, but strongly suggestive symptoms could warrant empirical treatment.
Helpful scales. The Patient Health Questionnaire (PHQ-9; https://www.uspreventiveservicestaskforce.org/Home/GetFileByID/218) and the Beck Depression Inventory (http://www.hr.ucdavis.edu/asap/pdf_files/Beck_Depression_Inventory.pdf) are useful for ruling out depressive disorders. Other scales are available, but they cannot confirm bipolar disorder. Laboratory testing selected according to patient symptoms (TABLE 24) can help rule out alternative diagnoses, but are also useful for establishing a baseline for medications.
Pharmacologic treatment: Match agents to symptoms
When treating bipolar disorder, choose a drug that targets a patient’s specific symptoms (TABLE 3).7-10 In primary care, the most commonly-used treatments for bipolar disorder type II are lamotrigine, valproic acid, and lithium.11
When to refer
Many cases of bipolar disorder type II can be managed successfully in a primary care practice, as can some cases of stable bipolar disorder type I. Psychiatric consultation may be most beneficial if the patient has recently attempted suicide or has suicidal ideation, has symptoms refractory to treatment, has poor medication adherence, or is misusing medications.
Even when patients are co-managed with psychiatric consultation, family physicians often ensure patients’ medication adherence, help patients understand their illness, manage overall health-related behaviors (including getting sufficient sleep), and make sure patients follow up as needed with their psychiatrist. Often, once patients have achieved equilibrium on mood-stabilizing (or other) medications, you can manage them and monitor medications with further consultation only as needed for clinical deterioration or other issues. Cognitive behavioral therapy may be useful as adjunctive treatment, particularly when patients are in active treatment.12
› CASE
This case is typical for many patients with depressed mood. A few key features in the patient’s history suggest bipolar disorder type II:
- depression that has been refractory to treatment
- multiple failed drug treatments, with mood-related adverse effects
- hypomania perceived as a “productive time,” and not as a problem
- absence of overt manic symptoms.
The patient was given a diagnosis of bipolar disorder type II with current depressed mood and no evidence of acute mania. She was started on valproic acid 250 mg po tid. She reported an initial improvement in mood but stopped the medication after one month because it caused intolerable drowsiness. She was then prescribed lamotrigine progressing gradually in 2-week intervals from 25 mg to 100 mg daily. She tolerated the medication well, and after 3 months of treatment, her mood symptoms improved and she had no further episodes of depressed mood.
CORRESPONDENCE
Michael Jason Wells, MD, Department of Family and Geriatric Medicine, University of Louisville School of Medicine, 201 Abraham Flexner Way, Suite 690, Louisville, KY 40202; mjwell04@louisville.edu.
THE CASE
A 23-year-old woman seeks medical attention at the request of her boyfriend because she’s been “miserable” for 3 weeks. In the examination room, she slouches in the chair and says her mood is low, her grades have dropped, and she no longer enjoys social gatherings or her other usual activities. She has no thoughts of suicide, no weight loss, and no somatic symptoms.
She says she is generally healthy, does not take any regular medications, and has never been pregnant. When asked about previous similar episodes, she admits to feeling this way about 3 times a year for one to 2 months at a time. She has tried different antidepressants, which haven’t helped much and have made her irritable and interfered with sleep.
When asked about mania or hypomania, she says there are short periods, roughly a couple of weeks 2 or 3 times a year, when she will get a lot of work done and can get by with little sleep. She has never gone on “spending sprees,” though, or indulged in any other unusual or dangerous behavior. And she has never been hospitalized for symptoms.
Bipolar disorders, over time, typically cause fluctuations in mood, activity, and energy level. If disorders go untreated, a patient’s behavior may cause considerable damage to relationships, finances, and reputations. And for some patients, the disorder can take the ultimate toll, resulting in death by suicide or accident.
Subtypes of bipolar disorder differ in the timing and severity of manic (or hypomanic) and depressive symptoms or episodes. Type I is the classic manic-depressive illness; type II is characterized by chronic treatment-resistant depression punctuated by hypomanic episodes; and cyclothymia leads to chronic fluctuations in mood. The diagnostic category “bipolar disorder not otherwise specified” applies to patients who meet some, but not all, of the criteria for other bipolar disorder subtypes.1
Prevalence. As with other mood symptoms or disorders, patients with bipolar disorder are often seen first in primary care due, in part, to barriers to obtaining psychiatric care or to avoidance of the perceived stigma in seeking such care.2 In a systematic review of patients who were interviewed randomly in primary care settings, 0.5% to 4.3% met criteria for bipolar disorder.3 The average age of onset for bipolar disorder is 15 to 19 years.4 In the United States, the prevalence of bipolar disorder type I is 1%; type II is 1.1%.3
The cause of bipolar disorder is unknown, but familial predisposition, biopsychosocial factors, and environment all seem to play a role. Children of parents with bipolar disorder have a 4% to 15% chance of receiving the same diagnosis, compared with children of parents without bipolar disorder, whose risk is only as high as 2%.5,6
Clinical presentation varies
When patients with bipolar disorder are first seen in the office, their state may be depression, mania, hypomania, or even euthymia. Keep in mind that the first 3 aberrations may indicate other disorders, either

Verify a true depressive episode
Symptoms must last for 2 weeks and include anhedonia or depressed mood, as well as some combination of changes in sleep, increased feelings of guilt, poor concentration, changes in appetite, loss of energy, psychomotor agitation or retardation, or suicidal thoughts.1
Know the criteria for mania
True mania is a distinct period of abnormally and persistently elevated, expansive, or irritable mood, accompanied by abnormally and persistently increased activity or energy, and lasting at least one week for most of the day, nearly every day (or any duration if hospitalization is necessary).
During that time, the patient must also exhibit at least 3 or more of the following symptoms (not counting irritability, if present): 1
- distractibility,
- insomnia,
- grandiosity,
- flights of ideas,
- increased goal-directed activity or agitation,
- rapid/pressured speech, or
- reckless behaviors.
How hypomania differs from mania. The symptoms of hypomania are less severe than those of mania—eg, social functioning is less impaired or is even normal, and there is no need for hospitalization. Patients may feel they have been much more productive than usual or have needed less sleep to engage in daily activities. Hypomania may be present but not reported by patients who perceive nothing wrong.1,4
Rule out alternate diagnoses and apply DSM-5 criteria
There are no objective tests to confirm a diagnosis of bipolar disorder. If you suspect bipolar disorder, focus your clinical evaluation on ruling out competing mental health or medical diagnoses, and on determining whether the patient’s history meets criteria for a bipolar disorder as described in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).1
Explore the patient’s psychiatric history (including hospitalizations, medications, and electroconvulsive therapy), general medical history, family history of psychiatric disorders (including suicide), and social history (including substance use and abuse). And carefully observe mental status. Confirming a diagnosis of bipolar disorder may take multiple visits, but strongly suggestive symptoms could warrant empirical treatment.
Helpful scales. The Patient Health Questionnaire (PHQ-9; https://www.uspreventiveservicestaskforce.org/Home/GetFileByID/218) and the Beck Depression Inventory (http://www.hr.ucdavis.edu/asap/pdf_files/Beck_Depression_Inventory.pdf) are useful for ruling out depressive disorders. Other scales are available, but they cannot confirm bipolar disorder. Laboratory testing selected according to patient symptoms (TABLE 24) can help rule out alternative diagnoses, but are also useful for establishing a baseline for medications.
Pharmacologic treatment: Match agents to symptoms
When treating bipolar disorder, choose a drug that targets a patient’s specific symptoms (TABLE 3).7-10 In primary care, the most commonly-used treatments for bipolar disorder type II are lamotrigine, valproic acid, and lithium.11
When to refer
Many cases of bipolar disorder type II can be managed successfully in a primary care practice, as can some cases of stable bipolar disorder type I. Psychiatric consultation may be most beneficial if the patient has recently attempted suicide or has suicidal ideation, has symptoms refractory to treatment, has poor medication adherence, or is misusing medications.
Even when patients are co-managed with psychiatric consultation, family physicians often ensure patients’ medication adherence, help patients understand their illness, manage overall health-related behaviors (including getting sufficient sleep), and make sure patients follow up as needed with their psychiatrist. Often, once patients have achieved equilibrium on mood-stabilizing (or other) medications, you can manage them and monitor medications with further consultation only as needed for clinical deterioration or other issues. Cognitive behavioral therapy may be useful as adjunctive treatment, particularly when patients are in active treatment.12
› CASE
This case is typical for many patients with depressed mood. A few key features in the patient’s history suggest bipolar disorder type II:
- depression that has been refractory to treatment
- multiple failed drug treatments, with mood-related adverse effects
- hypomania perceived as a “productive time,” and not as a problem
- absence of overt manic symptoms.
The patient was given a diagnosis of bipolar disorder type II with current depressed mood and no evidence of acute mania. She was started on valproic acid 250 mg po tid. She reported an initial improvement in mood but stopped the medication after one month because it caused intolerable drowsiness. She was then prescribed lamotrigine progressing gradually in 2-week intervals from 25 mg to 100 mg daily. She tolerated the medication well, and after 3 months of treatment, her mood symptoms improved and she had no further episodes of depressed mood.
CORRESPONDENCE
Michael Jason Wells, MD, Department of Family and Geriatric Medicine, University of Louisville School of Medicine, 201 Abraham Flexner Way, Suite 690, Louisville, KY 40202; mjwell04@louisville.edu.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed (DSM-5). Arlington, VA: American Psychiatric Association; 2013.
2. Kilbourne AM, Goodrich DE, O’Donnell AN, et al. Integrated bipolar disorder management in primary care. Curr Psychiatry Rep. 2012;14:687-695.
3. Cerimele JM, Chwastiak LA, Dodson S, et al. The prevalence of bipolar disorder in primary care samples: a systematic review. Gen Hosp Psychiatry. 2014;36:19-25.
4. Malhi GS, Adams D, Lampe L, et al. Clinical practice recommendations for bipolar disorder. Acta Pscyhiatr Scand. 2009:119(Suppl 439):27-46.
5. Abell S, Ey J. Bipolar Disorder. Clin Pediatr. 2009;48:693-694.
6. Birmaher B, Axelson D, Monk K, et al. Lifetime psychiatric disorders of school-aged offspring of parents with bipolar disorder: the Pittsburgh Bipolar Offspring Study. Arch Gen Psychiatry. 2009;66:287-296.
7. Cipriani A, Hawton K, Stockton S, et al. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ. 2013;346:f3646.
8. De Fruyt J, Deschepper E, Audenaert K, et al. Second generation antipsychotics in the treatment of bipolar depression: a systematic review and meta-analysis. J Psychopharmacol. 2012;26:603-617.
9. Gitlin M, Frye MA. Maintenance therapies in bipolar disorders. Bipolar Disord. 2012:14(Suppl 2):51-65.
10. Labbate LA, Fava M, Rosenbaum JF, et al. Handbook of Psychiatric Drug Therapy. 6th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2010.
11. Ostacher M, Tandon R, Suppes T. Florida Best Practice Psychotherapeutic Medication Guidelines for Adults with Bipolar Disorder: a novel, practical, patient-centered guide for clinicians. J Clin Psychiatry. 2016;77:920-926.
12. Szentagotai A, David D. The efficacy of cognitive behavioral therapy in bipolar disorder: a quantitative meta-analysis. J Clin Psychiatry. 2010;71:66-72.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed (DSM-5). Arlington, VA: American Psychiatric Association; 2013.
2. Kilbourne AM, Goodrich DE, O’Donnell AN, et al. Integrated bipolar disorder management in primary care. Curr Psychiatry Rep. 2012;14:687-695.
3. Cerimele JM, Chwastiak LA, Dodson S, et al. The prevalence of bipolar disorder in primary care samples: a systematic review. Gen Hosp Psychiatry. 2014;36:19-25.
4. Malhi GS, Adams D, Lampe L, et al. Clinical practice recommendations for bipolar disorder. Acta Pscyhiatr Scand. 2009:119(Suppl 439):27-46.
5. Abell S, Ey J. Bipolar Disorder. Clin Pediatr. 2009;48:693-694.
6. Birmaher B, Axelson D, Monk K, et al. Lifetime psychiatric disorders of school-aged offspring of parents with bipolar disorder: the Pittsburgh Bipolar Offspring Study. Arch Gen Psychiatry. 2009;66:287-296.
7. Cipriani A, Hawton K, Stockton S, et al. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ. 2013;346:f3646.
8. De Fruyt J, Deschepper E, Audenaert K, et al. Second generation antipsychotics in the treatment of bipolar depression: a systematic review and meta-analysis. J Psychopharmacol. 2012;26:603-617.
9. Gitlin M, Frye MA. Maintenance therapies in bipolar disorders. Bipolar Disord. 2012:14(Suppl 2):51-65.
10. Labbate LA, Fava M, Rosenbaum JF, et al. Handbook of Psychiatric Drug Therapy. 6th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2010.
11. Ostacher M, Tandon R, Suppes T. Florida Best Practice Psychotherapeutic Medication Guidelines for Adults with Bipolar Disorder: a novel, practical, patient-centered guide for clinicians. J Clin Psychiatry. 2016;77:920-926.
12. Szentagotai A, David D. The efficacy of cognitive behavioral therapy in bipolar disorder: a quantitative meta-analysis. J Clin Psychiatry. 2010;71:66-72.