User login
Recognizing mimics of depression: The ‘8 Ds’
Discuss this article at www.facebook.com/CurrentPsychiatry
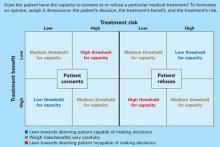
Many psychiatric and medical illnesses—as well as normal reactions to stressors—have symptoms that overlap with those of depressive disorders, including outwardly sad or dysphoric appearance, irritability, apathy or amotivation, fatigue, difficulty making decisions, social withdrawal, and sleep disturbances. This cluster of symptoms forms a readily observable behavioral phenotype that clinicians may label as depression before considering a broader differential diagnosis.
To better understand what other conditions belong in the differential diagnosis, we reviewed a sample of 100 consecutive medical/surgical inpatients referred to our consultation-liaison psychiatry practice for evaluation of “depression.” Ultimately, only 29 of these patients received a depression diagnosis. Many of the other diagnoses given in our sample required attention during inpatient medical or surgical care because they were potentially life-threatening if left unaddressed—such as delirium—or they interfered with managing the primary medical or surgical condition for which the patient was hospitalized.
Hurried or uncertain primary care clinicians frequently use “depression” as a catch-all term when requesting psychiatric consultation for patients who seem depressed. A wide range of conditions can mimic depression, and the art of psychosomatic psychiatry includes considering protean possibilities when assessing a patient. We identified 7 diagnoses that mimic major depression and developed our “8 D” differential to help clinicians properly diagnose “depressed” patients who have something other than a depressive disorder. Although our sample consisted of hospitalized patients, these mimics of depression may be found among patients referred from other clinical settings for evaluation of possible depression.
The perils of misdiagnosis
Depression is common among patients hospitalized with medical or surgical conditions. DSM-IV-TR diagnostic criteria for a major depressive episode (MDE) include the presence of low mood and/or anhedonia, plus ≥4 other depressive symptoms for ≥2 weeks.1 Growing evidence suggests that the relationship between depression and morbidity and mortality in medical illness is bidirectional, and nonpsychiatrists are becoming increasingly aware of major depression’s serious impact on their patients’ physical health.2-5
Although improving nonpsychiatrists’ recognition of depression in medically ill patients is laudable, it comes with a high false-positive rate. In a study of primary care outpatients, Berardi et al found that 45% of patients labeled “depressed” did not meet ICD-10 criteria for major depression, but >25% of those patients were prescribed an antidepressant.6 In a large retrospective study, Boland et al found that approximately 40% of patients referred to an inpatient psychiatric consultation service for depression did not meet criteria for a depressive illness, and primary medical services often confused organic syndromes such as delirium and dementia with depression.7 Similarly, Clarke et al found that 26% of medical and surgical inpatients referred to psychiatry with “depression” had another diagnosis—commonly delirium—that better accounted for their symptoms.8
What is the harm in overdiagnosing depression? Missing a serious or life-threatening diagnosis is a primary concern. For example, unrecognized delirium, which frequently was misdiagnosed as depression in the Berardi,6 Boland,7 and Clarke8 studies, is associated with myriad difficulties, including higher morbidity and mortality.9 Substance use disorders, which also commonly masquerade as depression, frequently are comorbid with medical illness. Delays in appropriate treatment of withdrawal syndromes—particularly of alcohol and sedative/hypnotic medications—are risk factors for increased mortality in these illnesses.10
Inappropriate, potentially harmful interventions are another concern. Many patients diagnosed with depression are prescribed antidepressants, but this is not always a benign intervention. Smith et al found that >10% of adult medical inpatients referred to a psychiatry consultation service who were started on an antidepressant had an adverse drug reaction severe enough to warrant discontinuing the medication.11 Antidepressant side effects relevant to medically ill patients include hyponatremia, serotonin syndrome, and exacerbation of delirium.12
Polypharmacy in medically ill patients increases the risk for serious drug-drug interactions. For example, serotonergic antidepressants can increase the risk for serotonin syndrome when combined with the analgesic tramadol, which has serotonergic activity,13 or the antibiotic linezolid, which is a reversible monoamine oxidase inhibitor.14 Many antidepressants—including paroxetine, fluoxetine, bupropion, sertraline, and duloxetine—are moderate to strong inhibitors of cytochrome P450 2D6 and therefore affect metabolism of many medications, including several beta blockers and antiarrhythmics, as well as the anti-estrogen tamoxifen. In the case of tamoxifen, which is a prodrug converted to active form by 2D6, concomitant use of a 2D6 inhibitor can substantially reduce the medication’s in vivo efficacy and lead to higher morbidity and mortality in breast cancer patients.15 As with any treatment, a decision to prescribe antidepressants needs to carefully be weighed in light of individual risks and benefits. This analysis starts by ensuring that an antidepressant is indicated.
Another concern is failing to recognize immediate human suffering for what it is. Hospitals and doctors’ offices are places of pain and loss as patients encounter morbidity and mortality in themselves and their loved ones. Rushing to pathologize the psychological or social manifestations of this pain can be invalidating to patients and may impair the doctor-patient relationship.
The 8 Ds
To determine what these “depression lookalike” syndromes could be, we identified 100 consecutive consultations to our adult inpatient psychiatry consultation-liaison team with a question of “depression.” We reviewed each patient’s chart, and recorded the diagnosis the psychiatrist gave to explain the patient’s depressed appearance. Data were recorded without patient identifiers, and the Mayo Clinic institutional review board (IRB) determined this study was exempt from IRB review.
Our sample included 45 men and 55 women with an average age of 48 (range: 18 to 91). On evaluation, 3 patients were given no psychiatric diagnosis, 29 were categorized as depressed, and 68 fell into one of 7 other “D” categories we describe below.
Depressed. These patients met criteria for a MDE in the context of major depressive disorder (MDD) or bipolar disorder, dysthymic disorder, mood disorder due to a general medical condition, substance-induced mood disorder, or depressive disorder not otherwise specified.
Demoralized. Patients who had difficulty adjusting to or coping with illness, and received a DSM-IV-TR diagnosis of adjustment disorder with the illness as the inciting stressor were placed in this category. Consistent with adjustment disorder criteria, these patients did not have depressive symptoms of sufficient intensity or duration to meet criteria for MDD or another primary mood disorder.
Difficult. For these patients, the primary issue was a breakdown in the therapeutic alliance with their treatment team. They received DSM-IV-TR diagnoses of personality disorder, noncompliance with treatment, or adult antisocial behavior.
Drugged. Patients in this category appeared depressed as a result of illicit substance use or misuse of alcohol or pharmaceuticals. DSM-IV-TR diagnoses included substance intoxication or withdrawal and substance abuse or dependence.
Delirious. This group consisted of patients with acute disruption in attention and level of consciousness that met DSM-IV-TR criteria for delirium. Patients whose delirious appearance was the result of illicit substance use or pharmaceutical misuse were categorized as “Drugged” rather than “Delirious.”
Disaffiliated. Patients in this category had dysphoria not commensurate with a full-blown mood disorder but attributable to grief from losing a major relationship to death, separation, or divorce. These patients received a DSM-IV-TR diagnosis of bereavement or a partner relational problem.
Delusional. These patients demonstrated amotivation and affective blunting as a result of a primary psychotic disorder such as schizophrenia. In preparation for emergent surgery, these patients had been prevented from taking anything orally, including antipsychotics, and their antipsychotics had not been restarted, which precipitated a gradual return of psychotic symptoms in the days after surgery.
Dulled. Two patients in our sample had irreversible cognitive deficits that explained their withdrawal and blunted affect; 1 had dementia and the other had mental retardation.
Managing the other Ds
In our sample, the most commonly misdiagnosed patients were those having difficulty adjusting to illness (Demoralized) or to other life events (Disaffiliated) (Table 1). In these cases, misdiagnosis has substantial treatment implications because these patients are better served by acute, illness-specific interventions that bolster coping skills, rather than pharmacotherapy or psychotherapy that targets entrenched depressive symptoms. For these patients, psychiatrists may “prescribe” interventions such as visits with a chaplain or other spiritual advisor, telephone calls or visits from family, friends, and other social supports, participation in physical or occupational therapy to improve adaptive functioning, or connecting with other patients in similar situations. Often, the key with these patients is to identify ways they have managed previous stressors and creatively use those resources to adapt to their new situation.
A second large group in our sample consisted of patients actively or passively fighting with their treatment team—the Difficult (Table 2). The treatment team or the patient’s caregivers and loved ones often are more distressed by the “difficult” patient’s symptoms than the patient, who may instead focus on his or her disappointment with caregivers who are unable to meet the patient’s unreasonable expectations. These challenges typically can be addressed by clarifying the salient issues for both the patient and team and establishing a liaison between patient and team to improve communication among all parties. Multidisciplinary care conferences can be an excellent way to ensure that the care team provides the patient with consistent communication and care.
A third group had potentially life-threatening conditions such as substance abuse/withdrawal or delirium as the cause of their “depressive” symptoms—the Drugged and the Delirious (Table 3). Recognizing an organic etiology of mood or behavioral symptoms is important because managing the underlying problem is the primary treatment strategy, not psychopharmacologic or psychotherapeutic intervention. Early identification and appropriate management of these patients could prevent further deterioration, improve medical outcomes, and shorten length of hospital stay.
A final group of patients was those whose chronic psychiatric and cognitive issues may go unrecognized or unappreciated until they interfere with the patient’s medical care—the Delusional and the Dulled (Table 2). In these cases, the correct diagnosis often hinges on obtaining a thorough history through collateral sources. The consulting psychiatrist can be crucial in co-managing these patients by establishing a liaison with outpatient providers, suggesting in-hospital management strategies such as alternate routes of administration of antipsychotics for patients with psychotic disorders, and connecting patients with outpatient supports after hospitalization. Continuity between inpatient and outpatient management is necessary to ensure a successful medical and psychiatric outcome.
Our 8 Ds are limited to the subset of patients referred by their medical teams with a question of depression. These referrals may have been motivated by a variety of patient, family, and team factors above and beyond the categories discussed in this article, and therefore may not accurately represent all patients who present with depressive symptoms in an inpatient setting. However, we hope that providing a mnemonic that suggests an extensive differential for a depressed phenotype may improve identification and management of these issues.
Table 1
Psychological crises that may look like depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Depressed” patients met DSM-IV-TR criteria for a depressive disorder | 29% | Emotional symptoms: Depressed mood, anhedonia Cognitive symptoms: concentration problems, indecisiveness, negative thoughts, irrational guilt Physical symptoms: changes in sleep, appetite, energy | Initiate psychotherapy with or without antidepressants |
| “Demoralized” patients had difficulty coping with a medical illness | 23% | Close temporal association with illness. Few neurovegetative symptoms. Able to maintain future orientation/hope | Provide compassion, recognition, and normalization. Connect patients with illness-specific supports (groups, social work, chaplaincy). Implement interventions to improve functioning (eg, PT/OT). Encourage patients to engage in activities that have helped them cope in the past |
| “Disaffiliated” patients had dysphoria attributable to grief from losing a major relationship | 3% | Few neurovegetative symptoms. Able to maintain future orientation/hope. Improvement typical as time since loss increases | Encourage patients to connect with other supportive relationships. Refer patients to grief resources (eg, hospice, spiritual supports) |
| OT: occupational therapy; PT: physical therapy | |||
Table 2
Differentiating patients with social challenges from those with depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Difficult” patients have a breakdown in the therapeutic alliance with their treatment team | 15% | Mood changes often intense, immediate, and reactive to situation. Frequent breakdowns in communication with care team. Care team more distressed by patient’s symptoms than the patient | Establish frequent communication among care team members. Use multidisciplinary care conferences to clarify salient issues for patients and their team. Provide patients with consistent information and expectations |
| “Delusional” patients had affective blunting as a result of a psychotic disorder | 2% | Suspicious about care team/procedures. Seems frightened or scans the room. On antipsychotics at admission. Slowly developing symptoms over several days after home medications are held | Acquire collateral history (an assigned community case manager or social worker can be an important source). Establish a plan for administering psychotropics in chronically mentally ill patients; consider IM or orally disintegrating formulations |
| “Dulled” patients had irreversible cognitive deficits | 2% | Baseline impairments in memory and/or independent functioning | Acquire collateral history. Perform a safety assessment of home environment with attention to need for additional supports |
| IM: intramuscular | |||
Table 3
Substance abuse and delirium can mimic depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Drugged” patients appeared depressed as a result of substance use/ withdrawal | 12% | Acute presentation closely mimicking mood, anxiety, or psychotic disorders. Emotional symptoms present when intoxicated or withdrawing and resolved during sobriety | Implement safety interventions to prevent self-harm or aggression during acute phase. Support and monitor withdrawal as indicated. Reassess mood state and symptoms once the patient is sober. Refer for chemical dependency evaluation |
| “Delirious” patients met DSM-IV-TR criteria for delirium | 11% | Disoriented and inattentive. Onset over hours to days. Waxing and waning throughout the day. Possible hallucinations (often visual or tactile) | Identify and correct underlying medical cause(s). Restore the patient’s sleep-wake cycle. Provide frequent reorientation and reassurance |
Related Resources
- Stern TA, Fricchione GL, Cassem NH, et al, eds. Massachusetts General Hospital handbook of general hospital psychiatry, 6th ed. Philadelphia, PA: Saunders Elsevier; 2010.
- Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc.; 2011.
- Academy of Psychosomatic Medicine. www.apm.org.
- Caplan JP, Stern TA. Mnemonics in a mnutshell: 32 aids to psychiatric diagnosis. Current Psychiatry. 2008;7(10):27-33.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Linezolid • Zyvox
- Paroxetine • Paxil
- Sertraline • Zoloft
- Tamoxifen • Nolvadex
- Tramadol • Ultracet
Disclosures
Dr. Bostwick reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rackley receives research/grant support from the Maternal and Child Health Bureau, Health Resources and Services Administration, U.S. Department of Health and Human Services, for a Collaborative Office Rounds program with primary care pediatricians.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Hansen MS, Fink P, Frydenberg M, et al. Use of health services, mental illness, and self-rated disability and health in medical inpatients. Psychosom Med. 2002;64(4):668-675.
3. Hosaka T, Aoki T, Watanabe T, et al. Comorbidity of depression among physically ill patients and its effect on the length of hospital stay. Psychiatry Clin Neurosci. 1999;53(4):491-495.
4. McCusker J, Cole M, Ciampi A, et al. Major depression in older medical inpatients predicts poor physical and mental health status over 12 months. Gen Hosp Psychiatry. 2007;29(4):340-348.
5. McCusker J, Cole M, Dufouil C, et al. The prevalence and correlates of major and minor depression in older medical inpatients. J Am Geriatr Soc. 2005;53(8):1344-1353.
6. Berardi D, Menchetti M, Cevenini N, et al. Increased recognition of depression in primary care. Comparison between primary-care physician and ICD-10 diagnosis of depression. Psychother Psychosom. 2005;74(4):225-230.
7. Boland RJ, Diaz S, Lamdan RM, et al. Overdiagnosis of depression in the general hospital. Gen Hosp Psychiatry. 1996;18(1):28-35.
8. Clarke DM, McKenzie DP, Smith GC. The recognition of depression in patients referred to a consultation-liaison service. J Psychosom Res. 1995;39(3):327-334.
9. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364.
10. Franklin JE, Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
11. Smith GC, Clarke DM, Handrinos D, et al. Consultation-liaison psychiatrists’ use of antidepressants in the physically ill. Psychosomatics. 2002;43(3):221-227.
12. Robinson MJ, Owen JA. Psychopharmacology. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
13. Hersh EV, Pinto A, Moore PA. Adverse drug interactions involving common prescription and over-the-counter analgesic agents. Clin Ther. 2007;29(suppl):2477-2497.
14. Sola CL, Bostwick JM, Hart DA, et al. Anticipating potential linezolid-SSRI interactions in the general hospital setting: an MAOI in disguise. Mayo Clin Proc. 2006;81(3):330-334.
15. Stearns V, Johnson MD, Rae JM, et al. Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst. 2003;95(23):1758-1764.
Discuss this article at www.facebook.com/CurrentPsychiatry
Many psychiatric and medical illnesses—as well as normal reactions to stressors—have symptoms that overlap with those of depressive disorders, including outwardly sad or dysphoric appearance, irritability, apathy or amotivation, fatigue, difficulty making decisions, social withdrawal, and sleep disturbances. This cluster of symptoms forms a readily observable behavioral phenotype that clinicians may label as depression before considering a broader differential diagnosis.
To better understand what other conditions belong in the differential diagnosis, we reviewed a sample of 100 consecutive medical/surgical inpatients referred to our consultation-liaison psychiatry practice for evaluation of “depression.” Ultimately, only 29 of these patients received a depression diagnosis. Many of the other diagnoses given in our sample required attention during inpatient medical or surgical care because they were potentially life-threatening if left unaddressed—such as delirium—or they interfered with managing the primary medical or surgical condition for which the patient was hospitalized.
Hurried or uncertain primary care clinicians frequently use “depression” as a catch-all term when requesting psychiatric consultation for patients who seem depressed. A wide range of conditions can mimic depression, and the art of psychosomatic psychiatry includes considering protean possibilities when assessing a patient. We identified 7 diagnoses that mimic major depression and developed our “8 D” differential to help clinicians properly diagnose “depressed” patients who have something other than a depressive disorder. Although our sample consisted of hospitalized patients, these mimics of depression may be found among patients referred from other clinical settings for evaluation of possible depression.
The perils of misdiagnosis
Depression is common among patients hospitalized with medical or surgical conditions. DSM-IV-TR diagnostic criteria for a major depressive episode (MDE) include the presence of low mood and/or anhedonia, plus ≥4 other depressive symptoms for ≥2 weeks.1 Growing evidence suggests that the relationship between depression and morbidity and mortality in medical illness is bidirectional, and nonpsychiatrists are becoming increasingly aware of major depression’s serious impact on their patients’ physical health.2-5
Although improving nonpsychiatrists’ recognition of depression in medically ill patients is laudable, it comes with a high false-positive rate. In a study of primary care outpatients, Berardi et al found that 45% of patients labeled “depressed” did not meet ICD-10 criteria for major depression, but >25% of those patients were prescribed an antidepressant.6 In a large retrospective study, Boland et al found that approximately 40% of patients referred to an inpatient psychiatric consultation service for depression did not meet criteria for a depressive illness, and primary medical services often confused organic syndromes such as delirium and dementia with depression.7 Similarly, Clarke et al found that 26% of medical and surgical inpatients referred to psychiatry with “depression” had another diagnosis—commonly delirium—that better accounted for their symptoms.8
What is the harm in overdiagnosing depression? Missing a serious or life-threatening diagnosis is a primary concern. For example, unrecognized delirium, which frequently was misdiagnosed as depression in the Berardi,6 Boland,7 and Clarke8 studies, is associated with myriad difficulties, including higher morbidity and mortality.9 Substance use disorders, which also commonly masquerade as depression, frequently are comorbid with medical illness. Delays in appropriate treatment of withdrawal syndromes—particularly of alcohol and sedative/hypnotic medications—are risk factors for increased mortality in these illnesses.10
Inappropriate, potentially harmful interventions are another concern. Many patients diagnosed with depression are prescribed antidepressants, but this is not always a benign intervention. Smith et al found that >10% of adult medical inpatients referred to a psychiatry consultation service who were started on an antidepressant had an adverse drug reaction severe enough to warrant discontinuing the medication.11 Antidepressant side effects relevant to medically ill patients include hyponatremia, serotonin syndrome, and exacerbation of delirium.12
Polypharmacy in medically ill patients increases the risk for serious drug-drug interactions. For example, serotonergic antidepressants can increase the risk for serotonin syndrome when combined with the analgesic tramadol, which has serotonergic activity,13 or the antibiotic linezolid, which is a reversible monoamine oxidase inhibitor.14 Many antidepressants—including paroxetine, fluoxetine, bupropion, sertraline, and duloxetine—are moderate to strong inhibitors of cytochrome P450 2D6 and therefore affect metabolism of many medications, including several beta blockers and antiarrhythmics, as well as the anti-estrogen tamoxifen. In the case of tamoxifen, which is a prodrug converted to active form by 2D6, concomitant use of a 2D6 inhibitor can substantially reduce the medication’s in vivo efficacy and lead to higher morbidity and mortality in breast cancer patients.15 As with any treatment, a decision to prescribe antidepressants needs to carefully be weighed in light of individual risks and benefits. This analysis starts by ensuring that an antidepressant is indicated.
Another concern is failing to recognize immediate human suffering for what it is. Hospitals and doctors’ offices are places of pain and loss as patients encounter morbidity and mortality in themselves and their loved ones. Rushing to pathologize the psychological or social manifestations of this pain can be invalidating to patients and may impair the doctor-patient relationship.
The 8 Ds
To determine what these “depression lookalike” syndromes could be, we identified 100 consecutive consultations to our adult inpatient psychiatry consultation-liaison team with a question of “depression.” We reviewed each patient’s chart, and recorded the diagnosis the psychiatrist gave to explain the patient’s depressed appearance. Data were recorded without patient identifiers, and the Mayo Clinic institutional review board (IRB) determined this study was exempt from IRB review.
Our sample included 45 men and 55 women with an average age of 48 (range: 18 to 91). On evaluation, 3 patients were given no psychiatric diagnosis, 29 were categorized as depressed, and 68 fell into one of 7 other “D” categories we describe below.
Depressed. These patients met criteria for a MDE in the context of major depressive disorder (MDD) or bipolar disorder, dysthymic disorder, mood disorder due to a general medical condition, substance-induced mood disorder, or depressive disorder not otherwise specified.
Demoralized. Patients who had difficulty adjusting to or coping with illness, and received a DSM-IV-TR diagnosis of adjustment disorder with the illness as the inciting stressor were placed in this category. Consistent with adjustment disorder criteria, these patients did not have depressive symptoms of sufficient intensity or duration to meet criteria for MDD or another primary mood disorder.
Difficult. For these patients, the primary issue was a breakdown in the therapeutic alliance with their treatment team. They received DSM-IV-TR diagnoses of personality disorder, noncompliance with treatment, or adult antisocial behavior.
Drugged. Patients in this category appeared depressed as a result of illicit substance use or misuse of alcohol or pharmaceuticals. DSM-IV-TR diagnoses included substance intoxication or withdrawal and substance abuse or dependence.
Delirious. This group consisted of patients with acute disruption in attention and level of consciousness that met DSM-IV-TR criteria for delirium. Patients whose delirious appearance was the result of illicit substance use or pharmaceutical misuse were categorized as “Drugged” rather than “Delirious.”
Disaffiliated. Patients in this category had dysphoria not commensurate with a full-blown mood disorder but attributable to grief from losing a major relationship to death, separation, or divorce. These patients received a DSM-IV-TR diagnosis of bereavement or a partner relational problem.
Delusional. These patients demonstrated amotivation and affective blunting as a result of a primary psychotic disorder such as schizophrenia. In preparation for emergent surgery, these patients had been prevented from taking anything orally, including antipsychotics, and their antipsychotics had not been restarted, which precipitated a gradual return of psychotic symptoms in the days after surgery.
Dulled. Two patients in our sample had irreversible cognitive deficits that explained their withdrawal and blunted affect; 1 had dementia and the other had mental retardation.
Managing the other Ds
In our sample, the most commonly misdiagnosed patients were those having difficulty adjusting to illness (Demoralized) or to other life events (Disaffiliated) (Table 1). In these cases, misdiagnosis has substantial treatment implications because these patients are better served by acute, illness-specific interventions that bolster coping skills, rather than pharmacotherapy or psychotherapy that targets entrenched depressive symptoms. For these patients, psychiatrists may “prescribe” interventions such as visits with a chaplain or other spiritual advisor, telephone calls or visits from family, friends, and other social supports, participation in physical or occupational therapy to improve adaptive functioning, or connecting with other patients in similar situations. Often, the key with these patients is to identify ways they have managed previous stressors and creatively use those resources to adapt to their new situation.
A second large group in our sample consisted of patients actively or passively fighting with their treatment team—the Difficult (Table 2). The treatment team or the patient’s caregivers and loved ones often are more distressed by the “difficult” patient’s symptoms than the patient, who may instead focus on his or her disappointment with caregivers who are unable to meet the patient’s unreasonable expectations. These challenges typically can be addressed by clarifying the salient issues for both the patient and team and establishing a liaison between patient and team to improve communication among all parties. Multidisciplinary care conferences can be an excellent way to ensure that the care team provides the patient with consistent communication and care.
A third group had potentially life-threatening conditions such as substance abuse/withdrawal or delirium as the cause of their “depressive” symptoms—the Drugged and the Delirious (Table 3). Recognizing an organic etiology of mood or behavioral symptoms is important because managing the underlying problem is the primary treatment strategy, not psychopharmacologic or psychotherapeutic intervention. Early identification and appropriate management of these patients could prevent further deterioration, improve medical outcomes, and shorten length of hospital stay.
A final group of patients was those whose chronic psychiatric and cognitive issues may go unrecognized or unappreciated until they interfere with the patient’s medical care—the Delusional and the Dulled (Table 2). In these cases, the correct diagnosis often hinges on obtaining a thorough history through collateral sources. The consulting psychiatrist can be crucial in co-managing these patients by establishing a liaison with outpatient providers, suggesting in-hospital management strategies such as alternate routes of administration of antipsychotics for patients with psychotic disorders, and connecting patients with outpatient supports after hospitalization. Continuity between inpatient and outpatient management is necessary to ensure a successful medical and psychiatric outcome.
Our 8 Ds are limited to the subset of patients referred by their medical teams with a question of depression. These referrals may have been motivated by a variety of patient, family, and team factors above and beyond the categories discussed in this article, and therefore may not accurately represent all patients who present with depressive symptoms in an inpatient setting. However, we hope that providing a mnemonic that suggests an extensive differential for a depressed phenotype may improve identification and management of these issues.
Table 1
Psychological crises that may look like depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Depressed” patients met DSM-IV-TR criteria for a depressive disorder | 29% | Emotional symptoms: Depressed mood, anhedonia Cognitive symptoms: concentration problems, indecisiveness, negative thoughts, irrational guilt Physical symptoms: changes in sleep, appetite, energy | Initiate psychotherapy with or without antidepressants |
| “Demoralized” patients had difficulty coping with a medical illness | 23% | Close temporal association with illness. Few neurovegetative symptoms. Able to maintain future orientation/hope | Provide compassion, recognition, and normalization. Connect patients with illness-specific supports (groups, social work, chaplaincy). Implement interventions to improve functioning (eg, PT/OT). Encourage patients to engage in activities that have helped them cope in the past |
| “Disaffiliated” patients had dysphoria attributable to grief from losing a major relationship | 3% | Few neurovegetative symptoms. Able to maintain future orientation/hope. Improvement typical as time since loss increases | Encourage patients to connect with other supportive relationships. Refer patients to grief resources (eg, hospice, spiritual supports) |
| OT: occupational therapy; PT: physical therapy | |||
Table 2
Differentiating patients with social challenges from those with depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Difficult” patients have a breakdown in the therapeutic alliance with their treatment team | 15% | Mood changes often intense, immediate, and reactive to situation. Frequent breakdowns in communication with care team. Care team more distressed by patient’s symptoms than the patient | Establish frequent communication among care team members. Use multidisciplinary care conferences to clarify salient issues for patients and their team. Provide patients with consistent information and expectations |
| “Delusional” patients had affective blunting as a result of a psychotic disorder | 2% | Suspicious about care team/procedures. Seems frightened or scans the room. On antipsychotics at admission. Slowly developing symptoms over several days after home medications are held | Acquire collateral history (an assigned community case manager or social worker can be an important source). Establish a plan for administering psychotropics in chronically mentally ill patients; consider IM or orally disintegrating formulations |
| “Dulled” patients had irreversible cognitive deficits | 2% | Baseline impairments in memory and/or independent functioning | Acquire collateral history. Perform a safety assessment of home environment with attention to need for additional supports |
| IM: intramuscular | |||
Table 3
Substance abuse and delirium can mimic depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Drugged” patients appeared depressed as a result of substance use/ withdrawal | 12% | Acute presentation closely mimicking mood, anxiety, or psychotic disorders. Emotional symptoms present when intoxicated or withdrawing and resolved during sobriety | Implement safety interventions to prevent self-harm or aggression during acute phase. Support and monitor withdrawal as indicated. Reassess mood state and symptoms once the patient is sober. Refer for chemical dependency evaluation |
| “Delirious” patients met DSM-IV-TR criteria for delirium | 11% | Disoriented and inattentive. Onset over hours to days. Waxing and waning throughout the day. Possible hallucinations (often visual or tactile) | Identify and correct underlying medical cause(s). Restore the patient’s sleep-wake cycle. Provide frequent reorientation and reassurance |
Related Resources
- Stern TA, Fricchione GL, Cassem NH, et al, eds. Massachusetts General Hospital handbook of general hospital psychiatry, 6th ed. Philadelphia, PA: Saunders Elsevier; 2010.
- Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc.; 2011.
- Academy of Psychosomatic Medicine. www.apm.org.
- Caplan JP, Stern TA. Mnemonics in a mnutshell: 32 aids to psychiatric diagnosis. Current Psychiatry. 2008;7(10):27-33.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Linezolid • Zyvox
- Paroxetine • Paxil
- Sertraline • Zoloft
- Tamoxifen • Nolvadex
- Tramadol • Ultracet
Disclosures
Dr. Bostwick reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rackley receives research/grant support from the Maternal and Child Health Bureau, Health Resources and Services Administration, U.S. Department of Health and Human Services, for a Collaborative Office Rounds program with primary care pediatricians.
Discuss this article at www.facebook.com/CurrentPsychiatry
Many psychiatric and medical illnesses—as well as normal reactions to stressors—have symptoms that overlap with those of depressive disorders, including outwardly sad or dysphoric appearance, irritability, apathy or amotivation, fatigue, difficulty making decisions, social withdrawal, and sleep disturbances. This cluster of symptoms forms a readily observable behavioral phenotype that clinicians may label as depression before considering a broader differential diagnosis.
To better understand what other conditions belong in the differential diagnosis, we reviewed a sample of 100 consecutive medical/surgical inpatients referred to our consultation-liaison psychiatry practice for evaluation of “depression.” Ultimately, only 29 of these patients received a depression diagnosis. Many of the other diagnoses given in our sample required attention during inpatient medical or surgical care because they were potentially life-threatening if left unaddressed—such as delirium—or they interfered with managing the primary medical or surgical condition for which the patient was hospitalized.
Hurried or uncertain primary care clinicians frequently use “depression” as a catch-all term when requesting psychiatric consultation for patients who seem depressed. A wide range of conditions can mimic depression, and the art of psychosomatic psychiatry includes considering protean possibilities when assessing a patient. We identified 7 diagnoses that mimic major depression and developed our “8 D” differential to help clinicians properly diagnose “depressed” patients who have something other than a depressive disorder. Although our sample consisted of hospitalized patients, these mimics of depression may be found among patients referred from other clinical settings for evaluation of possible depression.
The perils of misdiagnosis
Depression is common among patients hospitalized with medical or surgical conditions. DSM-IV-TR diagnostic criteria for a major depressive episode (MDE) include the presence of low mood and/or anhedonia, plus ≥4 other depressive symptoms for ≥2 weeks.1 Growing evidence suggests that the relationship between depression and morbidity and mortality in medical illness is bidirectional, and nonpsychiatrists are becoming increasingly aware of major depression’s serious impact on their patients’ physical health.2-5
Although improving nonpsychiatrists’ recognition of depression in medically ill patients is laudable, it comes with a high false-positive rate. In a study of primary care outpatients, Berardi et al found that 45% of patients labeled “depressed” did not meet ICD-10 criteria for major depression, but >25% of those patients were prescribed an antidepressant.6 In a large retrospective study, Boland et al found that approximately 40% of patients referred to an inpatient psychiatric consultation service for depression did not meet criteria for a depressive illness, and primary medical services often confused organic syndromes such as delirium and dementia with depression.7 Similarly, Clarke et al found that 26% of medical and surgical inpatients referred to psychiatry with “depression” had another diagnosis—commonly delirium—that better accounted for their symptoms.8
What is the harm in overdiagnosing depression? Missing a serious or life-threatening diagnosis is a primary concern. For example, unrecognized delirium, which frequently was misdiagnosed as depression in the Berardi,6 Boland,7 and Clarke8 studies, is associated with myriad difficulties, including higher morbidity and mortality.9 Substance use disorders, which also commonly masquerade as depression, frequently are comorbid with medical illness. Delays in appropriate treatment of withdrawal syndromes—particularly of alcohol and sedative/hypnotic medications—are risk factors for increased mortality in these illnesses.10
Inappropriate, potentially harmful interventions are another concern. Many patients diagnosed with depression are prescribed antidepressants, but this is not always a benign intervention. Smith et al found that >10% of adult medical inpatients referred to a psychiatry consultation service who were started on an antidepressant had an adverse drug reaction severe enough to warrant discontinuing the medication.11 Antidepressant side effects relevant to medically ill patients include hyponatremia, serotonin syndrome, and exacerbation of delirium.12
Polypharmacy in medically ill patients increases the risk for serious drug-drug interactions. For example, serotonergic antidepressants can increase the risk for serotonin syndrome when combined with the analgesic tramadol, which has serotonergic activity,13 or the antibiotic linezolid, which is a reversible monoamine oxidase inhibitor.14 Many antidepressants—including paroxetine, fluoxetine, bupropion, sertraline, and duloxetine—are moderate to strong inhibitors of cytochrome P450 2D6 and therefore affect metabolism of many medications, including several beta blockers and antiarrhythmics, as well as the anti-estrogen tamoxifen. In the case of tamoxifen, which is a prodrug converted to active form by 2D6, concomitant use of a 2D6 inhibitor can substantially reduce the medication’s in vivo efficacy and lead to higher morbidity and mortality in breast cancer patients.15 As with any treatment, a decision to prescribe antidepressants needs to carefully be weighed in light of individual risks and benefits. This analysis starts by ensuring that an antidepressant is indicated.
Another concern is failing to recognize immediate human suffering for what it is. Hospitals and doctors’ offices are places of pain and loss as patients encounter morbidity and mortality in themselves and their loved ones. Rushing to pathologize the psychological or social manifestations of this pain can be invalidating to patients and may impair the doctor-patient relationship.
The 8 Ds
To determine what these “depression lookalike” syndromes could be, we identified 100 consecutive consultations to our adult inpatient psychiatry consultation-liaison team with a question of “depression.” We reviewed each patient’s chart, and recorded the diagnosis the psychiatrist gave to explain the patient’s depressed appearance. Data were recorded without patient identifiers, and the Mayo Clinic institutional review board (IRB) determined this study was exempt from IRB review.
Our sample included 45 men and 55 women with an average age of 48 (range: 18 to 91). On evaluation, 3 patients were given no psychiatric diagnosis, 29 were categorized as depressed, and 68 fell into one of 7 other “D” categories we describe below.
Depressed. These patients met criteria for a MDE in the context of major depressive disorder (MDD) or bipolar disorder, dysthymic disorder, mood disorder due to a general medical condition, substance-induced mood disorder, or depressive disorder not otherwise specified.
Demoralized. Patients who had difficulty adjusting to or coping with illness, and received a DSM-IV-TR diagnosis of adjustment disorder with the illness as the inciting stressor were placed in this category. Consistent with adjustment disorder criteria, these patients did not have depressive symptoms of sufficient intensity or duration to meet criteria for MDD or another primary mood disorder.
Difficult. For these patients, the primary issue was a breakdown in the therapeutic alliance with their treatment team. They received DSM-IV-TR diagnoses of personality disorder, noncompliance with treatment, or adult antisocial behavior.
Drugged. Patients in this category appeared depressed as a result of illicit substance use or misuse of alcohol or pharmaceuticals. DSM-IV-TR diagnoses included substance intoxication or withdrawal and substance abuse or dependence.
Delirious. This group consisted of patients with acute disruption in attention and level of consciousness that met DSM-IV-TR criteria for delirium. Patients whose delirious appearance was the result of illicit substance use or pharmaceutical misuse were categorized as “Drugged” rather than “Delirious.”
Disaffiliated. Patients in this category had dysphoria not commensurate with a full-blown mood disorder but attributable to grief from losing a major relationship to death, separation, or divorce. These patients received a DSM-IV-TR diagnosis of bereavement or a partner relational problem.
Delusional. These patients demonstrated amotivation and affective blunting as a result of a primary psychotic disorder such as schizophrenia. In preparation for emergent surgery, these patients had been prevented from taking anything orally, including antipsychotics, and their antipsychotics had not been restarted, which precipitated a gradual return of psychotic symptoms in the days after surgery.
Dulled. Two patients in our sample had irreversible cognitive deficits that explained their withdrawal and blunted affect; 1 had dementia and the other had mental retardation.
Managing the other Ds
In our sample, the most commonly misdiagnosed patients were those having difficulty adjusting to illness (Demoralized) or to other life events (Disaffiliated) (Table 1). In these cases, misdiagnosis has substantial treatment implications because these patients are better served by acute, illness-specific interventions that bolster coping skills, rather than pharmacotherapy or psychotherapy that targets entrenched depressive symptoms. For these patients, psychiatrists may “prescribe” interventions such as visits with a chaplain or other spiritual advisor, telephone calls or visits from family, friends, and other social supports, participation in physical or occupational therapy to improve adaptive functioning, or connecting with other patients in similar situations. Often, the key with these patients is to identify ways they have managed previous stressors and creatively use those resources to adapt to their new situation.
A second large group in our sample consisted of patients actively or passively fighting with their treatment team—the Difficult (Table 2). The treatment team or the patient’s caregivers and loved ones often are more distressed by the “difficult” patient’s symptoms than the patient, who may instead focus on his or her disappointment with caregivers who are unable to meet the patient’s unreasonable expectations. These challenges typically can be addressed by clarifying the salient issues for both the patient and team and establishing a liaison between patient and team to improve communication among all parties. Multidisciplinary care conferences can be an excellent way to ensure that the care team provides the patient with consistent communication and care.
A third group had potentially life-threatening conditions such as substance abuse/withdrawal or delirium as the cause of their “depressive” symptoms—the Drugged and the Delirious (Table 3). Recognizing an organic etiology of mood or behavioral symptoms is important because managing the underlying problem is the primary treatment strategy, not psychopharmacologic or psychotherapeutic intervention. Early identification and appropriate management of these patients could prevent further deterioration, improve medical outcomes, and shorten length of hospital stay.
A final group of patients was those whose chronic psychiatric and cognitive issues may go unrecognized or unappreciated until they interfere with the patient’s medical care—the Delusional and the Dulled (Table 2). In these cases, the correct diagnosis often hinges on obtaining a thorough history through collateral sources. The consulting psychiatrist can be crucial in co-managing these patients by establishing a liaison with outpatient providers, suggesting in-hospital management strategies such as alternate routes of administration of antipsychotics for patients with psychotic disorders, and connecting patients with outpatient supports after hospitalization. Continuity between inpatient and outpatient management is necessary to ensure a successful medical and psychiatric outcome.
Our 8 Ds are limited to the subset of patients referred by their medical teams with a question of depression. These referrals may have been motivated by a variety of patient, family, and team factors above and beyond the categories discussed in this article, and therefore may not accurately represent all patients who present with depressive symptoms in an inpatient setting. However, we hope that providing a mnemonic that suggests an extensive differential for a depressed phenotype may improve identification and management of these issues.
Table 1
Psychological crises that may look like depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Depressed” patients met DSM-IV-TR criteria for a depressive disorder | 29% | Emotional symptoms: Depressed mood, anhedonia Cognitive symptoms: concentration problems, indecisiveness, negative thoughts, irrational guilt Physical symptoms: changes in sleep, appetite, energy | Initiate psychotherapy with or without antidepressants |
| “Demoralized” patients had difficulty coping with a medical illness | 23% | Close temporal association with illness. Few neurovegetative symptoms. Able to maintain future orientation/hope | Provide compassion, recognition, and normalization. Connect patients with illness-specific supports (groups, social work, chaplaincy). Implement interventions to improve functioning (eg, PT/OT). Encourage patients to engage in activities that have helped them cope in the past |
| “Disaffiliated” patients had dysphoria attributable to grief from losing a major relationship | 3% | Few neurovegetative symptoms. Able to maintain future orientation/hope. Improvement typical as time since loss increases | Encourage patients to connect with other supportive relationships. Refer patients to grief resources (eg, hospice, spiritual supports) |
| OT: occupational therapy; PT: physical therapy | |||
Table 2
Differentiating patients with social challenges from those with depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Difficult” patients have a breakdown in the therapeutic alliance with their treatment team | 15% | Mood changes often intense, immediate, and reactive to situation. Frequent breakdowns in communication with care team. Care team more distressed by patient’s symptoms than the patient | Establish frequent communication among care team members. Use multidisciplinary care conferences to clarify salient issues for patients and their team. Provide patients with consistent information and expectations |
| “Delusional” patients had affective blunting as a result of a psychotic disorder | 2% | Suspicious about care team/procedures. Seems frightened or scans the room. On antipsychotics at admission. Slowly developing symptoms over several days after home medications are held | Acquire collateral history (an assigned community case manager or social worker can be an important source). Establish a plan for administering psychotropics in chronically mentally ill patients; consider IM or orally disintegrating formulations |
| “Dulled” patients had irreversible cognitive deficits | 2% | Baseline impairments in memory and/or independent functioning | Acquire collateral history. Perform a safety assessment of home environment with attention to need for additional supports |
| IM: intramuscular | |||
Table 3
Substance abuse and delirium can mimic depression
| Category | Percentage of our sample | Distinguishing features | Suggested interventions |
|---|---|---|---|
| “Drugged” patients appeared depressed as a result of substance use/ withdrawal | 12% | Acute presentation closely mimicking mood, anxiety, or psychotic disorders. Emotional symptoms present when intoxicated or withdrawing and resolved during sobriety | Implement safety interventions to prevent self-harm or aggression during acute phase. Support and monitor withdrawal as indicated. Reassess mood state and symptoms once the patient is sober. Refer for chemical dependency evaluation |
| “Delirious” patients met DSM-IV-TR criteria for delirium | 11% | Disoriented and inattentive. Onset over hours to days. Waxing and waning throughout the day. Possible hallucinations (often visual or tactile) | Identify and correct underlying medical cause(s). Restore the patient’s sleep-wake cycle. Provide frequent reorientation and reassurance |
Related Resources
- Stern TA, Fricchione GL, Cassem NH, et al, eds. Massachusetts General Hospital handbook of general hospital psychiatry, 6th ed. Philadelphia, PA: Saunders Elsevier; 2010.
- Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc.; 2011.
- Academy of Psychosomatic Medicine. www.apm.org.
- Caplan JP, Stern TA. Mnemonics in a mnutshell: 32 aids to psychiatric diagnosis. Current Psychiatry. 2008;7(10):27-33.
Drug Brand Names
- Bupropion • Wellbutrin, Zyban
- Duloxetine • Cymbalta
- Fluoxetine • Prozac
- Linezolid • Zyvox
- Paroxetine • Paxil
- Sertraline • Zoloft
- Tamoxifen • Nolvadex
- Tramadol • Ultracet
Disclosures
Dr. Bostwick reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rackley receives research/grant support from the Maternal and Child Health Bureau, Health Resources and Services Administration, U.S. Department of Health and Human Services, for a Collaborative Office Rounds program with primary care pediatricians.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Hansen MS, Fink P, Frydenberg M, et al. Use of health services, mental illness, and self-rated disability and health in medical inpatients. Psychosom Med. 2002;64(4):668-675.
3. Hosaka T, Aoki T, Watanabe T, et al. Comorbidity of depression among physically ill patients and its effect on the length of hospital stay. Psychiatry Clin Neurosci. 1999;53(4):491-495.
4. McCusker J, Cole M, Ciampi A, et al. Major depression in older medical inpatients predicts poor physical and mental health status over 12 months. Gen Hosp Psychiatry. 2007;29(4):340-348.
5. McCusker J, Cole M, Dufouil C, et al. The prevalence and correlates of major and minor depression in older medical inpatients. J Am Geriatr Soc. 2005;53(8):1344-1353.
6. Berardi D, Menchetti M, Cevenini N, et al. Increased recognition of depression in primary care. Comparison between primary-care physician and ICD-10 diagnosis of depression. Psychother Psychosom. 2005;74(4):225-230.
7. Boland RJ, Diaz S, Lamdan RM, et al. Overdiagnosis of depression in the general hospital. Gen Hosp Psychiatry. 1996;18(1):28-35.
8. Clarke DM, McKenzie DP, Smith GC. The recognition of depression in patients referred to a consultation-liaison service. J Psychosom Res. 1995;39(3):327-334.
9. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364.
10. Franklin JE, Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
11. Smith GC, Clarke DM, Handrinos D, et al. Consultation-liaison psychiatrists’ use of antidepressants in the physically ill. Psychosomatics. 2002;43(3):221-227.
12. Robinson MJ, Owen JA. Psychopharmacology. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
13. Hersh EV, Pinto A, Moore PA. Adverse drug interactions involving common prescription and over-the-counter analgesic agents. Clin Ther. 2007;29(suppl):2477-2497.
14. Sola CL, Bostwick JM, Hart DA, et al. Anticipating potential linezolid-SSRI interactions in the general hospital setting: an MAOI in disguise. Mayo Clin Proc. 2006;81(3):330-334.
15. Stearns V, Johnson MD, Rae JM, et al. Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst. 2003;95(23):1758-1764.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
2. Hansen MS, Fink P, Frydenberg M, et al. Use of health services, mental illness, and self-rated disability and health in medical inpatients. Psychosom Med. 2002;64(4):668-675.
3. Hosaka T, Aoki T, Watanabe T, et al. Comorbidity of depression among physically ill patients and its effect on the length of hospital stay. Psychiatry Clin Neurosci. 1999;53(4):491-495.
4. McCusker J, Cole M, Ciampi A, et al. Major depression in older medical inpatients predicts poor physical and mental health status over 12 months. Gen Hosp Psychiatry. 2007;29(4):340-348.
5. McCusker J, Cole M, Dufouil C, et al. The prevalence and correlates of major and minor depression in older medical inpatients. J Am Geriatr Soc. 2005;53(8):1344-1353.
6. Berardi D, Menchetti M, Cevenini N, et al. Increased recognition of depression in primary care. Comparison between primary-care physician and ICD-10 diagnosis of depression. Psychother Psychosom. 2005;74(4):225-230.
7. Boland RJ, Diaz S, Lamdan RM, et al. Overdiagnosis of depression in the general hospital. Gen Hosp Psychiatry. 1996;18(1):28-35.
8. Clarke DM, McKenzie DP, Smith GC. The recognition of depression in patients referred to a consultation-liaison service. J Psychosom Res. 1995;39(3):327-334.
9. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364.
10. Franklin JE, Levenson JL, McCance-Katz EF. Substance-related disorders. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
11. Smith GC, Clarke DM, Handrinos D, et al. Consultation-liaison psychiatrists’ use of antidepressants in the physically ill. Psychosomatics. 2002;43(3):221-227.
12. Robinson MJ, Owen JA. Psychopharmacology. In: Levenson JL, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Washington, DC: American Psychiatric Publishing, Inc.; 2005:387–420.
13. Hersh EV, Pinto A, Moore PA. Adverse drug interactions involving common prescription and over-the-counter analgesic agents. Clin Ther. 2007;29(suppl):2477-2497.
14. Sola CL, Bostwick JM, Hart DA, et al. Anticipating potential linezolid-SSRI interactions in the general hospital setting: an MAOI in disguise. Mayo Clin Proc. 2006;81(3):330-334.
15. Stearns V, Johnson MD, Rae JM, et al. Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst. 2003;95(23):1758-1764.
Life after near death: What interventions work for a suicide survivor?
Completed suicide provokes a multitude of questions: What motivated it? What interventions could have diverted it? Could anyone or anything have prevented it? The question of who dies by suicide often overshadows the question of what lessons suicide attempt (SA) survivors can teach us. Their story does not end with the attempt episode. For these patients, we have ongoing opportunities for interventions to make a difference.
A history of SA strongly predicts eventual completion, so we must try to identify which survivors will reattempt and complete suicide. This article addresses what is known about the psychiatry of suicide survivors—suicide motives and methods, clinical management, and short- and long-term outcomes—from the perspective that suicidality in this population may be a trait, with SA or deliberate self-harm (DSH) as its state-driven manifestations. When viewed in this manner, it is not just a question of who survives a suicide attempt, but who survives suicidality.
CASE REPORT: End of the game
Ms. T, age 39, was admitted to the intensive care unit after an aspirin overdose. She had been living with a man in a southern state for 8 years since the demise of her first marriage, but kept deferring remarriage. She returned to Minnesota with her teenage daughter to visit her family and stayed 6 months. Her partner phoned Ms. T every day, telling her he wanted her to come back. One day he tired of the game and said, “Fine, don’t come back.” She immediately overdosed, then called him to tell him what she’d done. He called her daughter, telling her to go check on her mother and to call 911. When later asked why she did it, Ms. T said, “So he would know how much he loved me.”
Motive for self-harm
Ms. T’s suicide attempt was nonlethal, and she reported it immediately—characteristics of parasuicidal gesturing as a motive. A useful categorization of suicidal behavior divides it into discrete categories or narratives. Gardner and Cowdry describe 4: true suicidal acts, parasuicidal gesturing, self-mutilation, and retributive rage.1 We modify this schema with 4 additional categories: altruism, acute shame, command hallucinations, and panic ( Table 1 ).1-3 Categories are differentiated by affective state, motivation, and goal of behavior, but all involve situations in which the individual feels a lack of other options and resorts to maladaptive strategies.
Although this classification scheme helps clinicians understand a patient’s mindset, the specific motive underpinning DSH or SA is not consistently linked to its lethality. True suicidal acts frequently are marked by careful planning and high-lethality methods that increase the risk of completed suicide, but any motive can lead to a lethal act, whether or not death was intended.2,3
Factors that increase the risk of SA and completed suicide include male gender, age (adolescent or age >60), low socioeconomic status, and alcohol or drug abuse.4 An underlying mood disorder accounts for 73% of attributable risk of suicide or medically serious SA in older adults.5 This connection between mood and suicidality highlights the concept that emotional pain can cause so much suffering that patients seek release from distress by ending their lives.
A useful model by Shneidman6 casts psychological pain as 1 dimension in a 3-dimensional system that includes press and perturbation. In this model:
- Pain refers to psychological pain (from little or no pain to intolerable agony).
- Press means actual or imagined events in the inner or outer world that cause a person to react. It ranges from positive press (good fortune, happy events, protective factors) to negative press (stressors, failures, losses, persecution), which in turn decrease or increase the likelihood of suicide.
- Perturbation refers to the state of being disturbed or upset.
Certain risk factors make SA simultaneously more likely to occur but less likely to be lethal. For example, parental discord, nonheterosexual orientation, and female gender have been found to increase non-fatal attempts among adolescents.7 Borderline personality disorder increases the reattempt rate out of proportion to completion among adults.8 One might interpret a pattern of repeated nonlethal attempts to mean the patient has no real intent to die, but this is not always the case.
8
Table 1
8 categories or narratives of suicidal behavior
| Motive | Characteristics |
|---|---|
| True suicidal act | Release from intense baseline despair/hopelessness; self-nihilism as a permanent end to internal pain (entails highest intent to die and highest risk of completed suicide) |
| Self-mutilation | Relieving dysphoria or dissociation/depersonalization; acts of DSH designed to self-regulate or distract from emotional pain or other overwhelming affects |
| Retributive rage | Revenge; impulsiveness, vengefulness, and reduced capacity to conceive of other immediate options |
| Parasuicidal gesturing | Communication designed to extract a response from a significant other; often repetitive acts of DSH, strong dependency needs |
| Acute shame | Penance designed to escape from or to atone for a shameful act; often occurs within a short time after act is committed |
| Altruism | Relief of real or imagined burden on others; often occurs in setting of medical illness or substantial financial concerns |
| Command hallucinations | Acting in compliance with a command hallucination; often in setting of schizophrenia or depression with psychotic features |
| Panic | Driven by agitation, psychic anxiety, and/or panic attack; action intended as escape from real or imagined factor provoking agitation |
| DSH: deliberate self-harm | |
| Source: References 1-3 | |
CASE REPORT: Caught in the act
Mrs. L, age 35, works at a nail salon and took $12 from the cash register to buy gas so she could visit her husband in the next town. She’d never done anything like that before. She planned to return the money the next day, but her act was captured by a security camera and reported before she had a chance. Her boss said she had to go to the police.
Mrs. L was so ashamed that she decided she wanted to die. She drove her car to a remote hunting area where she tried to shoot herself in the head. The gun bucked, however, and shot her in the shoulder instead. She climbed into the front seat and drove herself to the hospital.
Method of self-harm
Survival of a suicide attempt depends in part on the lethality of the suicide method. Although she survived, Mrs. L’s attempt was intended to be quite lethal and illustrates shame as a motive.
The method’s lethality does not always correlate with the intent to die.9 Attempters with the highest suicidal intent do not reliably choose the most lethal method, either because they overestimate the lethality of methods such as cutting or overdose or because less lethal methods were most accessible.
Firearms, which are both accessible and lethal, remain the most common and deadly method in the United States, with more suicides from gunshot than all other methods combined.13 Cultural factors also are involved, such as in India where poisoning (especially with readily available organophosphates) is more common than gunshot.14 Suicidality screening in psychiatric practice and in the emergency department should always include questioning about convenient access to lethal means, especially those commonly used among the local population.
Clinical management
Treatment goals for patients who have demonstrated suicidal behavior may include decreasing the occurrence of suicidal thoughts, plans, gestures, or attempts. At a population level, accepted management strategies include:
- psychotherapy (cognitive-behavioral therapy [CBT], dialectical behavioral therapy)
- contracts for safety (widely employed but lacking evidence of efficacy)
- medications that target underlying disorders (antidepressants, mood stabilizers, antipsychotics).
Ineffective interventions? A study examining suicide trends since 1990 in the United States18 found disheartening evidence that although treatment dramatically increased, the incidence of suicidal thoughts, plans, gestures, or attempts did not significantly decrease ( Box 1 ).18–26 Based on a systematic review of 15 randomized controlled trials, Arensman et al19 offered 2 explanations for why studies of various psychosocial and pharmacologic interventions showed no significant effect on suicidality compared with usual care:
- the intervention had a negligible effect on patient outcomes
- the sample size was too small to detect clinically important differences in reattempt rates.
Suicide research deploys a single intervention for a diverse group of subjects rather than tailoring the approach to each particular case. A certain intervention may be highly effective for 1 patient because it is well matched to the specific blend of issues driving that patient’s suicidality, yet ineffective for another because it fails to address that individual’s underlying issues. Thus, a single treatment program standardized for research can be simultaneously a success and a failure, depending on which patient is assessed. The overall outcome is statistical insignificance because success is lost in the noise of failure.
Treating the individual. To individualize your treatment approach, it may be useful to recast the case and treatment strategy into Shneidman’s cubic model.6 Identifying the uniquely personal drivers behind a patient’s thoughts and actions helps point toward the most effective management approach. Tailored pharmacologic treatments and psychotherapy can be used to help guide the patient away from maximum suicide risk.
Table 2
Symptom-targeted pharmacologic treatment of suicidal patients
| Drug class | Impulsive-behavioral dyscontrol | Affective dysregulation | Psychotic features |
|---|---|---|---|
| SSRIs | Self-damaging behavior, impulsivity | Mood lability/mood crashes; anger; temper outbursts | |
| Antipsychotics | Anger, temper outbursts | Cognitive symptoms; perceptual symptoms | |
| Mood stabilizers (lithium, carbamazepine, valproic acid) | Self-damaging behavior, impulsivity | Mood lability/mood crashes, anger, temper outbursts | |
| SSRI: selective serotonin reuptake inhibitor | |||
| Source: References 16,17 | |||
Treatment of suicide attempt survivors has dramatically increased in the United States since 1990, but the incidence of suicidal thoughts, plans, gestures, or attempts has not significantly decreased.18 A systematic review of 15 randomized controlled trials using the search methods published by Arensman et al19 reveals very little difference in the suicide reattempt rate, despite extra treatment beyond the “usual standard of care.”
Intervention strategies shown to significantly decrease the rate of self-harm include home visits, behavioral therapy, and a “green card” strategy (patients were issued a card at the time of discharge explaining that a doctor was always available for them and how that doctor could be contacted).20-23
No significant difference in reattempt rate was found with other strategies, although benefits such as lower rates of depression and suicidal ideation or higher outpatient visit attendance were observed in some trials.24-26 Click here for a summary of the studies’ methodologies and results.
Outcomes of self-harm
When considering outcomes of SA, it is important to separate the short-term outcome of a single SA from the long-term outcome of suicidality. Short-term outcome depends on the characteristics and management of the acute episode, whereas long-term encompasses ongoing management of suicidality as a trait.
In the short term, surviving a SA depends heavily on the lethality of method and access to acute treatment. It also depends on medical fitness to withstand injury, which may help account for the higher death rate among elderly suicide attempters. A frail or medically ill person is less likely to survive the bodily insult of a SA.
Long-term outcomes are harder to predict. Some patients’ index attempts result from a transient state—an isolated incident that never will be repeated. In others, suicidality is a trait—a chronic maladaptive pattern that is potentially lethal. After an index attempt, the most reliable predictors for eventual death by suicide are:
- diagnosed mental illness
- high-lethality method on the index SA
- number of reattempts.4
Mood disorders impact long-term outcome, yet only a limited number of studies have found a reduction in suicide rates in response to mood disorder treatment. In a 44-year follow-up study, long-term treatment of depression and bipolar disorder with lithium significantly reduced the suicide rate.30 A meta-analysis of recurrent major affective disorder studies found that subjects on lithium maintenance treatment were 15 times less likely to commit suicidal acts, compared with those not on lithium.31
An important confounding factor in these findings is that effective lithium treatment requires long-term adherence, which implies a long-term doctor-patient relationship. As Cipriani et al32 noted, patients who can maintain an ongoing therapeutic relationship may be “less disturbed” than those who cannot, making them less likely to kill themselves regardless of pharmacologic treatment. Furthermore, patient interviews reveal that the therapeutic alliance created by a continuous relationship can be a protective support against further SA.33
Clinical implications
Suicide survivors often continue to struggle with suicidality well beyond the index attempt. This suicidality is a maladaptive problem-solving method that functions as a chronic morbid illness. As such, it is not enough to analyze the phenomenon of surviving an SA; one must examine the ongoing process of surviving suicidality.
Consider 3 factors. Consider all 3 factors— motive, method, and management—when addressing suicide survivorship.
Method lethality significantly influences survival likelihood. In clinical practice, we have observed that the index attempt is a learning experience for some patients that will inform their choice of method on the next attempt. When interacting with a suicide survivor, carefully assess the reasoning behind their initial choice of method and whether it has evolved toward higher lethality since the index attempt.
Management recommendations after SA continue to evolve. Risk factor management—such as treating underlying mood disorders, home visits to reduce social isolation, and prioritized “green card” contact with psychiatrists—has been shown to decrease reattempt rates, but many other interventions have not shown the expected benefit. Increased intervention rates have not yielded proportional decreases in suicidal ideation, attempts, or completion.
Suicide survivors often continue to struggle with suicidality well beyond the index attempt
Consider the SA motive and method when planning how to manage the survivor
Method lethality significantly influences survival likelihood (firearms are the most common and deadly method in the United States)
In many clinical trials, the incidence of suicidal thoughts, plans, gestures, or attempts has not significantly decreased when SA survivors received extra treatment
Management recommendations after SA continue to evolve; effective techniques appear to be keeping lines of communication open and providing individualized treatment
Individualize pharmacologic treatments and psychotherapy to help guide the patient away from maximum suicide risk
SA: suicide attempt
- American Association of Suicidology. www.suicidology.org.
- American Foundation for Suicide Prevention. www.afsp.org.
- Mayo Clinic Patient/Family Education. Suicide: What to do when someone is suicidal. www.mayoclinic.com/health/suicide/MH00058.
- Carbamazepine • Carbatrol
- Lithium • Eskalith, Lithobid
- Valproic acid • Depakene, Depakote
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Gardner DL, Cowdry RW. Suicidal and parasuicidal behavior in borderline personality disorder. Psychiatr Clin North Am. 1985;8(2):389-403.
2. Bostwick J, Levenson J. Suicidality. In: Levenson J, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Arlington, VA: American Psychiatric Publishing, Inc; 2004:219-234.
3. Bostwick JM, Cohen LM. Differentiating suicide from life-ending acts and end-of-life decisions: a model based on chronic kidney disease and dialysis. Psychosomatics. 2009;50(1):1-7.
4. Jeglic EL. Will my patient attempt suicide again? Current Psychiatry. 2008;7(11):19-28.
5. Beautrais A. A case control study of suicide and attempted suicide. Suicide Life Threat Behav. 2002;32(1):1-9.
6. Shneidman E. Overview: a multidimensional approach to suicide. In: Jacobs D, Brown H, eds. Suicide: understanding and responding. Madison, WI: International Universities Press; 1989:1-20.
7. Beautrais AL. Risk factors for suicide and attempted suicide among young people. Aust N Z J Psychiatry. 2000;34:420-436.
8. Black DW, Blum N, Pfohl B, et al. Suicidal behavior in borderline personality disorder: prevalence, risk factors, prediction, and prevention. J Pers Disord. 2004;18(3):226-239.
9. Plutchik R, van Praag HM, Picard S, et al. Is there a relation between the seriousness of suicidal intent and the lethality of suicide attempt? Psychiatric Res. 1988;27:71-79.
10. Schernhammer ES, Colditz GA. Suicide rates among physicians: a quantitative and gender assessment (meta-analysis). Am J Psychiatry. 2004;161(12):2295-2302.
11. Recupero PR, Harms SE, Noble JM. Googling suicide: surfing for suicide information on the internet. J Clin Psychiatry. 2008;69(6):878-888.
12. Gibb SJ, Beautrais AL, Fergusson DM. Mortality and further suicidal behaviour after an index suicide attempt: a 10-year study. Aust N Z J Psychiatry. 2005;39:95-100.
13. Miller M, Hemenway D. Guns and suicide in the United States. N Engl J Med. 2008;359(10):989-991.
14. Latha KS, Bhat SM, D’Souza P. Suicide attempters in general hospital unit in India: their socio-demographic and clinical profile—emphasis on cross-cultural aspects. Acta Psychiatra Scand. 1996;94(1):26-30.
15. Yildiz A, Sachs GS, Turgay A. Pharmacological management of agitation in emergency settings. Emerg Med J. 2003;20(4):339-346.
16. American Psychiatric Association practice guidelines. Treatment of patients with borderline personality disorder. 2001. Available at: http://www.psychiatryonline.com/pracGuide/pracGuideTopic_13.aspx. Accessed July 8, 2009.
17. Zanarini MC. Update on pharmacotherapy of borderline personality disorder. Curr Psychiatry Rep. 2004;6(1):66-70.
18. Kessler RC, Berglund P, Borges G, et al. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990-1992 to 2001-2003. JAMA. 2005;293(20):2487-2495.
19. Arensman E, Townsend E, Hawton K, et al. Psychosocial and pharmacological treatment of patients following deliberate self-harm: the methodological issues involved in evaluating effectiveness. Suicide Life Threat Behav. 2001;31(2):169-180.
20. Welu TC. A follow-up program for suicide attempters: evaluation of effectiveness. Suicide Life Threat Behav. 1977;7(1):17-20.
21. Linehan MM, Armstrong HE, Suarez A, et al. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48(12):1060-1064.
22. McLeavey B, Daly R, Ludgate J, et al. Interpersonal problem-solving skills training in the treatment of self-poisoning patients. Suicide Life Threat Behav. 1994;24(4):382-394.
23. Morgan HG, Jones EM, Owen JH. Secondary prevention of non-fatal deliberate self-harm. The green card study. Br J Psychiatry. 1993;163:111-112.
24. Salkovskis PM, Atha C, Storer D. Cognitive-behavioural problem solving in the treatment of patients who repeatedly attempt suicide. A controlled trial. Br J Psychiatry. 1990;157:871-876.
25. Hirsch SR, Walsh C, Draper R. Parasuicide. A review of treatment interventions. J Affect Disord. 1982;4(4):299-311.
26. Hawton K, Bancroft J, Catalan J, et al. Domiciliary and outpatient treatment of self-poisoning patients by medical and non-medical staff. Psychol Med. 1981;11(1):169-177.
27. Brown GK, Ten Have T, Henriques GR, et al. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294(5):563-570.
28. Bateman A, Fonagy P. 8-year follow-up of patients treated for borderline personality disorder: mentalization-based treatment versus treatment as usual. Am J Psychiatry. 2008;165(5):631-638.
29. Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. 2003;182:537-542.
30. Angst J, Angst F, Gerber-Werder R, et al. Suicide in 406 mood-disorder patients with and without long-term medication: a 40 to 44 years’ follow-up. Arch Suicide Res. 2005;9(3):279-300.
31. Baldessarini RJ, Tondo L, Hennen J. Lithium treatment and suicide risk in major affective disorders: update and new findings. J Clin Psychiatry. 2003;64(suppl 5):44-52.
32. Cipriani A, Pretty H, Hawton K, et al. Lithium in the prevention of suicidal behavior and all-cause mortality in patients with mood disorders: a systematic review of randomized trials. Am J Psychiatry. 2005;162(10):1805-1819.
33. Sinclair J, Green J. Understanding resolution of deliberate self harm: qualitative interview study of patients’ experiences. BMJ. 2005;330(7500):1112.-
Completed suicide provokes a multitude of questions: What motivated it? What interventions could have diverted it? Could anyone or anything have prevented it? The question of who dies by suicide often overshadows the question of what lessons suicide attempt (SA) survivors can teach us. Their story does not end with the attempt episode. For these patients, we have ongoing opportunities for interventions to make a difference.
A history of SA strongly predicts eventual completion, so we must try to identify which survivors will reattempt and complete suicide. This article addresses what is known about the psychiatry of suicide survivors—suicide motives and methods, clinical management, and short- and long-term outcomes—from the perspective that suicidality in this population may be a trait, with SA or deliberate self-harm (DSH) as its state-driven manifestations. When viewed in this manner, it is not just a question of who survives a suicide attempt, but who survives suicidality.
CASE REPORT: End of the game
Ms. T, age 39, was admitted to the intensive care unit after an aspirin overdose. She had been living with a man in a southern state for 8 years since the demise of her first marriage, but kept deferring remarriage. She returned to Minnesota with her teenage daughter to visit her family and stayed 6 months. Her partner phoned Ms. T every day, telling her he wanted her to come back. One day he tired of the game and said, “Fine, don’t come back.” She immediately overdosed, then called him to tell him what she’d done. He called her daughter, telling her to go check on her mother and to call 911. When later asked why she did it, Ms. T said, “So he would know how much he loved me.”
Motive for self-harm
Ms. T’s suicide attempt was nonlethal, and she reported it immediately—characteristics of parasuicidal gesturing as a motive. A useful categorization of suicidal behavior divides it into discrete categories or narratives. Gardner and Cowdry describe 4: true suicidal acts, parasuicidal gesturing, self-mutilation, and retributive rage.1 We modify this schema with 4 additional categories: altruism, acute shame, command hallucinations, and panic ( Table 1 ).1-3 Categories are differentiated by affective state, motivation, and goal of behavior, but all involve situations in which the individual feels a lack of other options and resorts to maladaptive strategies.
Although this classification scheme helps clinicians understand a patient’s mindset, the specific motive underpinning DSH or SA is not consistently linked to its lethality. True suicidal acts frequently are marked by careful planning and high-lethality methods that increase the risk of completed suicide, but any motive can lead to a lethal act, whether or not death was intended.2,3
Factors that increase the risk of SA and completed suicide include male gender, age (adolescent or age >60), low socioeconomic status, and alcohol or drug abuse.4 An underlying mood disorder accounts for 73% of attributable risk of suicide or medically serious SA in older adults.5 This connection between mood and suicidality highlights the concept that emotional pain can cause so much suffering that patients seek release from distress by ending their lives.
A useful model by Shneidman6 casts psychological pain as 1 dimension in a 3-dimensional system that includes press and perturbation. In this model:
- Pain refers to psychological pain (from little or no pain to intolerable agony).
- Press means actual or imagined events in the inner or outer world that cause a person to react. It ranges from positive press (good fortune, happy events, protective factors) to negative press (stressors, failures, losses, persecution), which in turn decrease or increase the likelihood of suicide.
- Perturbation refers to the state of being disturbed or upset.
Certain risk factors make SA simultaneously more likely to occur but less likely to be lethal. For example, parental discord, nonheterosexual orientation, and female gender have been found to increase non-fatal attempts among adolescents.7 Borderline personality disorder increases the reattempt rate out of proportion to completion among adults.8 One might interpret a pattern of repeated nonlethal attempts to mean the patient has no real intent to die, but this is not always the case.
8
Table 1
8 categories or narratives of suicidal behavior
| Motive | Characteristics |
|---|---|
| True suicidal act | Release from intense baseline despair/hopelessness; self-nihilism as a permanent end to internal pain (entails highest intent to die and highest risk of completed suicide) |
| Self-mutilation | Relieving dysphoria or dissociation/depersonalization; acts of DSH designed to self-regulate or distract from emotional pain or other overwhelming affects |
| Retributive rage | Revenge; impulsiveness, vengefulness, and reduced capacity to conceive of other immediate options |
| Parasuicidal gesturing | Communication designed to extract a response from a significant other; often repetitive acts of DSH, strong dependency needs |
| Acute shame | Penance designed to escape from or to atone for a shameful act; often occurs within a short time after act is committed |
| Altruism | Relief of real or imagined burden on others; often occurs in setting of medical illness or substantial financial concerns |
| Command hallucinations | Acting in compliance with a command hallucination; often in setting of schizophrenia or depression with psychotic features |
| Panic | Driven by agitation, psychic anxiety, and/or panic attack; action intended as escape from real or imagined factor provoking agitation |
| DSH: deliberate self-harm | |
| Source: References 1-3 | |
CASE REPORT: Caught in the act
Mrs. L, age 35, works at a nail salon and took $12 from the cash register to buy gas so she could visit her husband in the next town. She’d never done anything like that before. She planned to return the money the next day, but her act was captured by a security camera and reported before she had a chance. Her boss said she had to go to the police.
Mrs. L was so ashamed that she decided she wanted to die. She drove her car to a remote hunting area where she tried to shoot herself in the head. The gun bucked, however, and shot her in the shoulder instead. She climbed into the front seat and drove herself to the hospital.
Method of self-harm
Survival of a suicide attempt depends in part on the lethality of the suicide method. Although she survived, Mrs. L’s attempt was intended to be quite lethal and illustrates shame as a motive.
The method’s lethality does not always correlate with the intent to die.9 Attempters with the highest suicidal intent do not reliably choose the most lethal method, either because they overestimate the lethality of methods such as cutting or overdose or because less lethal methods were most accessible.
Firearms, which are both accessible and lethal, remain the most common and deadly method in the United States, with more suicides from gunshot than all other methods combined.13 Cultural factors also are involved, such as in India where poisoning (especially with readily available organophosphates) is more common than gunshot.14 Suicidality screening in psychiatric practice and in the emergency department should always include questioning about convenient access to lethal means, especially those commonly used among the local population.
Clinical management
Treatment goals for patients who have demonstrated suicidal behavior may include decreasing the occurrence of suicidal thoughts, plans, gestures, or attempts. At a population level, accepted management strategies include:
- psychotherapy (cognitive-behavioral therapy [CBT], dialectical behavioral therapy)
- contracts for safety (widely employed but lacking evidence of efficacy)
- medications that target underlying disorders (antidepressants, mood stabilizers, antipsychotics).
Ineffective interventions? A study examining suicide trends since 1990 in the United States18 found disheartening evidence that although treatment dramatically increased, the incidence of suicidal thoughts, plans, gestures, or attempts did not significantly decrease ( Box 1 ).18–26 Based on a systematic review of 15 randomized controlled trials, Arensman et al19 offered 2 explanations for why studies of various psychosocial and pharmacologic interventions showed no significant effect on suicidality compared with usual care:
- the intervention had a negligible effect on patient outcomes
- the sample size was too small to detect clinically important differences in reattempt rates.
Suicide research deploys a single intervention for a diverse group of subjects rather than tailoring the approach to each particular case. A certain intervention may be highly effective for 1 patient because it is well matched to the specific blend of issues driving that patient’s suicidality, yet ineffective for another because it fails to address that individual’s underlying issues. Thus, a single treatment program standardized for research can be simultaneously a success and a failure, depending on which patient is assessed. The overall outcome is statistical insignificance because success is lost in the noise of failure.
Treating the individual. To individualize your treatment approach, it may be useful to recast the case and treatment strategy into Shneidman’s cubic model.6 Identifying the uniquely personal drivers behind a patient’s thoughts and actions helps point toward the most effective management approach. Tailored pharmacologic treatments and psychotherapy can be used to help guide the patient away from maximum suicide risk.
Table 2
Symptom-targeted pharmacologic treatment of suicidal patients
| Drug class | Impulsive-behavioral dyscontrol | Affective dysregulation | Psychotic features |
|---|---|---|---|
| SSRIs | Self-damaging behavior, impulsivity | Mood lability/mood crashes; anger; temper outbursts | |
| Antipsychotics | Anger, temper outbursts | Cognitive symptoms; perceptual symptoms | |
| Mood stabilizers (lithium, carbamazepine, valproic acid) | Self-damaging behavior, impulsivity | Mood lability/mood crashes, anger, temper outbursts | |
| SSRI: selective serotonin reuptake inhibitor | |||
| Source: References 16,17 | |||
Treatment of suicide attempt survivors has dramatically increased in the United States since 1990, but the incidence of suicidal thoughts, plans, gestures, or attempts has not significantly decreased.18 A systematic review of 15 randomized controlled trials using the search methods published by Arensman et al19 reveals very little difference in the suicide reattempt rate, despite extra treatment beyond the “usual standard of care.”
Intervention strategies shown to significantly decrease the rate of self-harm include home visits, behavioral therapy, and a “green card” strategy (patients were issued a card at the time of discharge explaining that a doctor was always available for them and how that doctor could be contacted).20-23
No significant difference in reattempt rate was found with other strategies, although benefits such as lower rates of depression and suicidal ideation or higher outpatient visit attendance were observed in some trials.24-26 Click here for a summary of the studies’ methodologies and results.
Outcomes of self-harm
When considering outcomes of SA, it is important to separate the short-term outcome of a single SA from the long-term outcome of suicidality. Short-term outcome depends on the characteristics and management of the acute episode, whereas long-term encompasses ongoing management of suicidality as a trait.
In the short term, surviving a SA depends heavily on the lethality of method and access to acute treatment. It also depends on medical fitness to withstand injury, which may help account for the higher death rate among elderly suicide attempters. A frail or medically ill person is less likely to survive the bodily insult of a SA.
Long-term outcomes are harder to predict. Some patients’ index attempts result from a transient state—an isolated incident that never will be repeated. In others, suicidality is a trait—a chronic maladaptive pattern that is potentially lethal. After an index attempt, the most reliable predictors for eventual death by suicide are:
- diagnosed mental illness
- high-lethality method on the index SA
- number of reattempts.4
Mood disorders impact long-term outcome, yet only a limited number of studies have found a reduction in suicide rates in response to mood disorder treatment. In a 44-year follow-up study, long-term treatment of depression and bipolar disorder with lithium significantly reduced the suicide rate.30 A meta-analysis of recurrent major affective disorder studies found that subjects on lithium maintenance treatment were 15 times less likely to commit suicidal acts, compared with those not on lithium.31
An important confounding factor in these findings is that effective lithium treatment requires long-term adherence, which implies a long-term doctor-patient relationship. As Cipriani et al32 noted, patients who can maintain an ongoing therapeutic relationship may be “less disturbed” than those who cannot, making them less likely to kill themselves regardless of pharmacologic treatment. Furthermore, patient interviews reveal that the therapeutic alliance created by a continuous relationship can be a protective support against further SA.33
Clinical implications
Suicide survivors often continue to struggle with suicidality well beyond the index attempt. This suicidality is a maladaptive problem-solving method that functions as a chronic morbid illness. As such, it is not enough to analyze the phenomenon of surviving an SA; one must examine the ongoing process of surviving suicidality.
Consider 3 factors. Consider all 3 factors— motive, method, and management—when addressing suicide survivorship.
Method lethality significantly influences survival likelihood. In clinical practice, we have observed that the index attempt is a learning experience for some patients that will inform their choice of method on the next attempt. When interacting with a suicide survivor, carefully assess the reasoning behind their initial choice of method and whether it has evolved toward higher lethality since the index attempt.
Management recommendations after SA continue to evolve. Risk factor management—such as treating underlying mood disorders, home visits to reduce social isolation, and prioritized “green card” contact with psychiatrists—has been shown to decrease reattempt rates, but many other interventions have not shown the expected benefit. Increased intervention rates have not yielded proportional decreases in suicidal ideation, attempts, or completion.
Suicide survivors often continue to struggle with suicidality well beyond the index attempt
Consider the SA motive and method when planning how to manage the survivor
Method lethality significantly influences survival likelihood (firearms are the most common and deadly method in the United States)
In many clinical trials, the incidence of suicidal thoughts, plans, gestures, or attempts has not significantly decreased when SA survivors received extra treatment
Management recommendations after SA continue to evolve; effective techniques appear to be keeping lines of communication open and providing individualized treatment
Individualize pharmacologic treatments and psychotherapy to help guide the patient away from maximum suicide risk
SA: suicide attempt
- American Association of Suicidology. www.suicidology.org.
- American Foundation for Suicide Prevention. www.afsp.org.
- Mayo Clinic Patient/Family Education. Suicide: What to do when someone is suicidal. www.mayoclinic.com/health/suicide/MH00058.
- Carbamazepine • Carbatrol
- Lithium • Eskalith, Lithobid
- Valproic acid • Depakene, Depakote
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Completed suicide provokes a multitude of questions: What motivated it? What interventions could have diverted it? Could anyone or anything have prevented it? The question of who dies by suicide often overshadows the question of what lessons suicide attempt (SA) survivors can teach us. Their story does not end with the attempt episode. For these patients, we have ongoing opportunities for interventions to make a difference.
A history of SA strongly predicts eventual completion, so we must try to identify which survivors will reattempt and complete suicide. This article addresses what is known about the psychiatry of suicide survivors—suicide motives and methods, clinical management, and short- and long-term outcomes—from the perspective that suicidality in this population may be a trait, with SA or deliberate self-harm (DSH) as its state-driven manifestations. When viewed in this manner, it is not just a question of who survives a suicide attempt, but who survives suicidality.
CASE REPORT: End of the game
Ms. T, age 39, was admitted to the intensive care unit after an aspirin overdose. She had been living with a man in a southern state for 8 years since the demise of her first marriage, but kept deferring remarriage. She returned to Minnesota with her teenage daughter to visit her family and stayed 6 months. Her partner phoned Ms. T every day, telling her he wanted her to come back. One day he tired of the game and said, “Fine, don’t come back.” She immediately overdosed, then called him to tell him what she’d done. He called her daughter, telling her to go check on her mother and to call 911. When later asked why she did it, Ms. T said, “So he would know how much he loved me.”
Motive for self-harm
Ms. T’s suicide attempt was nonlethal, and she reported it immediately—characteristics of parasuicidal gesturing as a motive. A useful categorization of suicidal behavior divides it into discrete categories or narratives. Gardner and Cowdry describe 4: true suicidal acts, parasuicidal gesturing, self-mutilation, and retributive rage.1 We modify this schema with 4 additional categories: altruism, acute shame, command hallucinations, and panic ( Table 1 ).1-3 Categories are differentiated by affective state, motivation, and goal of behavior, but all involve situations in which the individual feels a lack of other options and resorts to maladaptive strategies.
Although this classification scheme helps clinicians understand a patient’s mindset, the specific motive underpinning DSH or SA is not consistently linked to its lethality. True suicidal acts frequently are marked by careful planning and high-lethality methods that increase the risk of completed suicide, but any motive can lead to a lethal act, whether or not death was intended.2,3
Factors that increase the risk of SA and completed suicide include male gender, age (adolescent or age >60), low socioeconomic status, and alcohol or drug abuse.4 An underlying mood disorder accounts for 73% of attributable risk of suicide or medically serious SA in older adults.5 This connection between mood and suicidality highlights the concept that emotional pain can cause so much suffering that patients seek release from distress by ending their lives.
A useful model by Shneidman6 casts psychological pain as 1 dimension in a 3-dimensional system that includes press and perturbation. In this model:
- Pain refers to psychological pain (from little or no pain to intolerable agony).
- Press means actual or imagined events in the inner or outer world that cause a person to react. It ranges from positive press (good fortune, happy events, protective factors) to negative press (stressors, failures, losses, persecution), which in turn decrease or increase the likelihood of suicide.
- Perturbation refers to the state of being disturbed or upset.
Certain risk factors make SA simultaneously more likely to occur but less likely to be lethal. For example, parental discord, nonheterosexual orientation, and female gender have been found to increase non-fatal attempts among adolescents.7 Borderline personality disorder increases the reattempt rate out of proportion to completion among adults.8 One might interpret a pattern of repeated nonlethal attempts to mean the patient has no real intent to die, but this is not always the case.
8
Table 1
8 categories or narratives of suicidal behavior
| Motive | Characteristics |
|---|---|
| True suicidal act | Release from intense baseline despair/hopelessness; self-nihilism as a permanent end to internal pain (entails highest intent to die and highest risk of completed suicide) |
| Self-mutilation | Relieving dysphoria or dissociation/depersonalization; acts of DSH designed to self-regulate or distract from emotional pain or other overwhelming affects |
| Retributive rage | Revenge; impulsiveness, vengefulness, and reduced capacity to conceive of other immediate options |
| Parasuicidal gesturing | Communication designed to extract a response from a significant other; often repetitive acts of DSH, strong dependency needs |
| Acute shame | Penance designed to escape from or to atone for a shameful act; often occurs within a short time after act is committed |
| Altruism | Relief of real or imagined burden on others; often occurs in setting of medical illness or substantial financial concerns |
| Command hallucinations | Acting in compliance with a command hallucination; often in setting of schizophrenia or depression with psychotic features |
| Panic | Driven by agitation, psychic anxiety, and/or panic attack; action intended as escape from real or imagined factor provoking agitation |
| DSH: deliberate self-harm | |
| Source: References 1-3 | |
CASE REPORT: Caught in the act
Mrs. L, age 35, works at a nail salon and took $12 from the cash register to buy gas so she could visit her husband in the next town. She’d never done anything like that before. She planned to return the money the next day, but her act was captured by a security camera and reported before she had a chance. Her boss said she had to go to the police.
Mrs. L was so ashamed that she decided she wanted to die. She drove her car to a remote hunting area where she tried to shoot herself in the head. The gun bucked, however, and shot her in the shoulder instead. She climbed into the front seat and drove herself to the hospital.
Method of self-harm
Survival of a suicide attempt depends in part on the lethality of the suicide method. Although she survived, Mrs. L’s attempt was intended to be quite lethal and illustrates shame as a motive.
The method’s lethality does not always correlate with the intent to die.9 Attempters with the highest suicidal intent do not reliably choose the most lethal method, either because they overestimate the lethality of methods such as cutting or overdose or because less lethal methods were most accessible.
Firearms, which are both accessible and lethal, remain the most common and deadly method in the United States, with more suicides from gunshot than all other methods combined.13 Cultural factors also are involved, such as in India where poisoning (especially with readily available organophosphates) is more common than gunshot.14 Suicidality screening in psychiatric practice and in the emergency department should always include questioning about convenient access to lethal means, especially those commonly used among the local population.
Clinical management
Treatment goals for patients who have demonstrated suicidal behavior may include decreasing the occurrence of suicidal thoughts, plans, gestures, or attempts. At a population level, accepted management strategies include:
- psychotherapy (cognitive-behavioral therapy [CBT], dialectical behavioral therapy)
- contracts for safety (widely employed but lacking evidence of efficacy)
- medications that target underlying disorders (antidepressants, mood stabilizers, antipsychotics).
Ineffective interventions? A study examining suicide trends since 1990 in the United States18 found disheartening evidence that although treatment dramatically increased, the incidence of suicidal thoughts, plans, gestures, or attempts did not significantly decrease ( Box 1 ).18–26 Based on a systematic review of 15 randomized controlled trials, Arensman et al19 offered 2 explanations for why studies of various psychosocial and pharmacologic interventions showed no significant effect on suicidality compared with usual care:
- the intervention had a negligible effect on patient outcomes
- the sample size was too small to detect clinically important differences in reattempt rates.
Suicide research deploys a single intervention for a diverse group of subjects rather than tailoring the approach to each particular case. A certain intervention may be highly effective for 1 patient because it is well matched to the specific blend of issues driving that patient’s suicidality, yet ineffective for another because it fails to address that individual’s underlying issues. Thus, a single treatment program standardized for research can be simultaneously a success and a failure, depending on which patient is assessed. The overall outcome is statistical insignificance because success is lost in the noise of failure.
Treating the individual. To individualize your treatment approach, it may be useful to recast the case and treatment strategy into Shneidman’s cubic model.6 Identifying the uniquely personal drivers behind a patient’s thoughts and actions helps point toward the most effective management approach. Tailored pharmacologic treatments and psychotherapy can be used to help guide the patient away from maximum suicide risk.
Table 2
Symptom-targeted pharmacologic treatment of suicidal patients
| Drug class | Impulsive-behavioral dyscontrol | Affective dysregulation | Psychotic features |
|---|---|---|---|
| SSRIs | Self-damaging behavior, impulsivity | Mood lability/mood crashes; anger; temper outbursts | |
| Antipsychotics | Anger, temper outbursts | Cognitive symptoms; perceptual symptoms | |
| Mood stabilizers (lithium, carbamazepine, valproic acid) | Self-damaging behavior, impulsivity | Mood lability/mood crashes, anger, temper outbursts | |
| SSRI: selective serotonin reuptake inhibitor | |||
| Source: References 16,17 | |||
Treatment of suicide attempt survivors has dramatically increased in the United States since 1990, but the incidence of suicidal thoughts, plans, gestures, or attempts has not significantly decreased.18 A systematic review of 15 randomized controlled trials using the search methods published by Arensman et al19 reveals very little difference in the suicide reattempt rate, despite extra treatment beyond the “usual standard of care.”
Intervention strategies shown to significantly decrease the rate of self-harm include home visits, behavioral therapy, and a “green card” strategy (patients were issued a card at the time of discharge explaining that a doctor was always available for them and how that doctor could be contacted).20-23
No significant difference in reattempt rate was found with other strategies, although benefits such as lower rates of depression and suicidal ideation or higher outpatient visit attendance were observed in some trials.24-26 Click here for a summary of the studies’ methodologies and results.
Outcomes of self-harm
When considering outcomes of SA, it is important to separate the short-term outcome of a single SA from the long-term outcome of suicidality. Short-term outcome depends on the characteristics and management of the acute episode, whereas long-term encompasses ongoing management of suicidality as a trait.
In the short term, surviving a SA depends heavily on the lethality of method and access to acute treatment. It also depends on medical fitness to withstand injury, which may help account for the higher death rate among elderly suicide attempters. A frail or medically ill person is less likely to survive the bodily insult of a SA.
Long-term outcomes are harder to predict. Some patients’ index attempts result from a transient state—an isolated incident that never will be repeated. In others, suicidality is a trait—a chronic maladaptive pattern that is potentially lethal. After an index attempt, the most reliable predictors for eventual death by suicide are:
- diagnosed mental illness
- high-lethality method on the index SA
- number of reattempts.4
Mood disorders impact long-term outcome, yet only a limited number of studies have found a reduction in suicide rates in response to mood disorder treatment. In a 44-year follow-up study, long-term treatment of depression and bipolar disorder with lithium significantly reduced the suicide rate.30 A meta-analysis of recurrent major affective disorder studies found that subjects on lithium maintenance treatment were 15 times less likely to commit suicidal acts, compared with those not on lithium.31
An important confounding factor in these findings is that effective lithium treatment requires long-term adherence, which implies a long-term doctor-patient relationship. As Cipriani et al32 noted, patients who can maintain an ongoing therapeutic relationship may be “less disturbed” than those who cannot, making them less likely to kill themselves regardless of pharmacologic treatment. Furthermore, patient interviews reveal that the therapeutic alliance created by a continuous relationship can be a protective support against further SA.33
Clinical implications
Suicide survivors often continue to struggle with suicidality well beyond the index attempt. This suicidality is a maladaptive problem-solving method that functions as a chronic morbid illness. As such, it is not enough to analyze the phenomenon of surviving an SA; one must examine the ongoing process of surviving suicidality.
Consider 3 factors. Consider all 3 factors— motive, method, and management—when addressing suicide survivorship.
Method lethality significantly influences survival likelihood. In clinical practice, we have observed that the index attempt is a learning experience for some patients that will inform their choice of method on the next attempt. When interacting with a suicide survivor, carefully assess the reasoning behind their initial choice of method and whether it has evolved toward higher lethality since the index attempt.
Management recommendations after SA continue to evolve. Risk factor management—such as treating underlying mood disorders, home visits to reduce social isolation, and prioritized “green card” contact with psychiatrists—has been shown to decrease reattempt rates, but many other interventions have not shown the expected benefit. Increased intervention rates have not yielded proportional decreases in suicidal ideation, attempts, or completion.
Suicide survivors often continue to struggle with suicidality well beyond the index attempt
Consider the SA motive and method when planning how to manage the survivor
Method lethality significantly influences survival likelihood (firearms are the most common and deadly method in the United States)
In many clinical trials, the incidence of suicidal thoughts, plans, gestures, or attempts has not significantly decreased when SA survivors received extra treatment
Management recommendations after SA continue to evolve; effective techniques appear to be keeping lines of communication open and providing individualized treatment
Individualize pharmacologic treatments and psychotherapy to help guide the patient away from maximum suicide risk
SA: suicide attempt
- American Association of Suicidology. www.suicidology.org.
- American Foundation for Suicide Prevention. www.afsp.org.
- Mayo Clinic Patient/Family Education. Suicide: What to do when someone is suicidal. www.mayoclinic.com/health/suicide/MH00058.
- Carbamazepine • Carbatrol
- Lithium • Eskalith, Lithobid
- Valproic acid • Depakene, Depakote
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Gardner DL, Cowdry RW. Suicidal and parasuicidal behavior in borderline personality disorder. Psychiatr Clin North Am. 1985;8(2):389-403.
2. Bostwick J, Levenson J. Suicidality. In: Levenson J, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Arlington, VA: American Psychiatric Publishing, Inc; 2004:219-234.
3. Bostwick JM, Cohen LM. Differentiating suicide from life-ending acts and end-of-life decisions: a model based on chronic kidney disease and dialysis. Psychosomatics. 2009;50(1):1-7.
4. Jeglic EL. Will my patient attempt suicide again? Current Psychiatry. 2008;7(11):19-28.
5. Beautrais A. A case control study of suicide and attempted suicide. Suicide Life Threat Behav. 2002;32(1):1-9.
6. Shneidman E. Overview: a multidimensional approach to suicide. In: Jacobs D, Brown H, eds. Suicide: understanding and responding. Madison, WI: International Universities Press; 1989:1-20.
7. Beautrais AL. Risk factors for suicide and attempted suicide among young people. Aust N Z J Psychiatry. 2000;34:420-436.
8. Black DW, Blum N, Pfohl B, et al. Suicidal behavior in borderline personality disorder: prevalence, risk factors, prediction, and prevention. J Pers Disord. 2004;18(3):226-239.
9. Plutchik R, van Praag HM, Picard S, et al. Is there a relation between the seriousness of suicidal intent and the lethality of suicide attempt? Psychiatric Res. 1988;27:71-79.
10. Schernhammer ES, Colditz GA. Suicide rates among physicians: a quantitative and gender assessment (meta-analysis). Am J Psychiatry. 2004;161(12):2295-2302.
11. Recupero PR, Harms SE, Noble JM. Googling suicide: surfing for suicide information on the internet. J Clin Psychiatry. 2008;69(6):878-888.
12. Gibb SJ, Beautrais AL, Fergusson DM. Mortality and further suicidal behaviour after an index suicide attempt: a 10-year study. Aust N Z J Psychiatry. 2005;39:95-100.
13. Miller M, Hemenway D. Guns and suicide in the United States. N Engl J Med. 2008;359(10):989-991.
14. Latha KS, Bhat SM, D’Souza P. Suicide attempters in general hospital unit in India: their socio-demographic and clinical profile—emphasis on cross-cultural aspects. Acta Psychiatra Scand. 1996;94(1):26-30.
15. Yildiz A, Sachs GS, Turgay A. Pharmacological management of agitation in emergency settings. Emerg Med J. 2003;20(4):339-346.
16. American Psychiatric Association practice guidelines. Treatment of patients with borderline personality disorder. 2001. Available at: http://www.psychiatryonline.com/pracGuide/pracGuideTopic_13.aspx. Accessed July 8, 2009.
17. Zanarini MC. Update on pharmacotherapy of borderline personality disorder. Curr Psychiatry Rep. 2004;6(1):66-70.
18. Kessler RC, Berglund P, Borges G, et al. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990-1992 to 2001-2003. JAMA. 2005;293(20):2487-2495.
19. Arensman E, Townsend E, Hawton K, et al. Psychosocial and pharmacological treatment of patients following deliberate self-harm: the methodological issues involved in evaluating effectiveness. Suicide Life Threat Behav. 2001;31(2):169-180.
20. Welu TC. A follow-up program for suicide attempters: evaluation of effectiveness. Suicide Life Threat Behav. 1977;7(1):17-20.
21. Linehan MM, Armstrong HE, Suarez A, et al. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48(12):1060-1064.
22. McLeavey B, Daly R, Ludgate J, et al. Interpersonal problem-solving skills training in the treatment of self-poisoning patients. Suicide Life Threat Behav. 1994;24(4):382-394.
23. Morgan HG, Jones EM, Owen JH. Secondary prevention of non-fatal deliberate self-harm. The green card study. Br J Psychiatry. 1993;163:111-112.
24. Salkovskis PM, Atha C, Storer D. Cognitive-behavioural problem solving in the treatment of patients who repeatedly attempt suicide. A controlled trial. Br J Psychiatry. 1990;157:871-876.
25. Hirsch SR, Walsh C, Draper R. Parasuicide. A review of treatment interventions. J Affect Disord. 1982;4(4):299-311.
26. Hawton K, Bancroft J, Catalan J, et al. Domiciliary and outpatient treatment of self-poisoning patients by medical and non-medical staff. Psychol Med. 1981;11(1):169-177.
27. Brown GK, Ten Have T, Henriques GR, et al. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294(5):563-570.
28. Bateman A, Fonagy P. 8-year follow-up of patients treated for borderline personality disorder: mentalization-based treatment versus treatment as usual. Am J Psychiatry. 2008;165(5):631-638.
29. Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. 2003;182:537-542.
30. Angst J, Angst F, Gerber-Werder R, et al. Suicide in 406 mood-disorder patients with and without long-term medication: a 40 to 44 years’ follow-up. Arch Suicide Res. 2005;9(3):279-300.
31. Baldessarini RJ, Tondo L, Hennen J. Lithium treatment and suicide risk in major affective disorders: update and new findings. J Clin Psychiatry. 2003;64(suppl 5):44-52.
32. Cipriani A, Pretty H, Hawton K, et al. Lithium in the prevention of suicidal behavior and all-cause mortality in patients with mood disorders: a systematic review of randomized trials. Am J Psychiatry. 2005;162(10):1805-1819.
33. Sinclair J, Green J. Understanding resolution of deliberate self harm: qualitative interview study of patients’ experiences. BMJ. 2005;330(7500):1112.-
1. Gardner DL, Cowdry RW. Suicidal and parasuicidal behavior in borderline personality disorder. Psychiatr Clin North Am. 1985;8(2):389-403.
2. Bostwick J, Levenson J. Suicidality. In: Levenson J, ed. The American Psychiatric Publishing textbook of psychosomatic medicine. Arlington, VA: American Psychiatric Publishing, Inc; 2004:219-234.
3. Bostwick JM, Cohen LM. Differentiating suicide from life-ending acts and end-of-life decisions: a model based on chronic kidney disease and dialysis. Psychosomatics. 2009;50(1):1-7.
4. Jeglic EL. Will my patient attempt suicide again? Current Psychiatry. 2008;7(11):19-28.
5. Beautrais A. A case control study of suicide and attempted suicide. Suicide Life Threat Behav. 2002;32(1):1-9.
6. Shneidman E. Overview: a multidimensional approach to suicide. In: Jacobs D, Brown H, eds. Suicide: understanding and responding. Madison, WI: International Universities Press; 1989:1-20.
7. Beautrais AL. Risk factors for suicide and attempted suicide among young people. Aust N Z J Psychiatry. 2000;34:420-436.
8. Black DW, Blum N, Pfohl B, et al. Suicidal behavior in borderline personality disorder: prevalence, risk factors, prediction, and prevention. J Pers Disord. 2004;18(3):226-239.
9. Plutchik R, van Praag HM, Picard S, et al. Is there a relation between the seriousness of suicidal intent and the lethality of suicide attempt? Psychiatric Res. 1988;27:71-79.
10. Schernhammer ES, Colditz GA. Suicide rates among physicians: a quantitative and gender assessment (meta-analysis). Am J Psychiatry. 2004;161(12):2295-2302.
11. Recupero PR, Harms SE, Noble JM. Googling suicide: surfing for suicide information on the internet. J Clin Psychiatry. 2008;69(6):878-888.
12. Gibb SJ, Beautrais AL, Fergusson DM. Mortality and further suicidal behaviour after an index suicide attempt: a 10-year study. Aust N Z J Psychiatry. 2005;39:95-100.
13. Miller M, Hemenway D. Guns and suicide in the United States. N Engl J Med. 2008;359(10):989-991.
14. Latha KS, Bhat SM, D’Souza P. Suicide attempters in general hospital unit in India: their socio-demographic and clinical profile—emphasis on cross-cultural aspects. Acta Psychiatra Scand. 1996;94(1):26-30.
15. Yildiz A, Sachs GS, Turgay A. Pharmacological management of agitation in emergency settings. Emerg Med J. 2003;20(4):339-346.
16. American Psychiatric Association practice guidelines. Treatment of patients with borderline personality disorder. 2001. Available at: http://www.psychiatryonline.com/pracGuide/pracGuideTopic_13.aspx. Accessed July 8, 2009.
17. Zanarini MC. Update on pharmacotherapy of borderline personality disorder. Curr Psychiatry Rep. 2004;6(1):66-70.
18. Kessler RC, Berglund P, Borges G, et al. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990-1992 to 2001-2003. JAMA. 2005;293(20):2487-2495.
19. Arensman E, Townsend E, Hawton K, et al. Psychosocial and pharmacological treatment of patients following deliberate self-harm: the methodological issues involved in evaluating effectiveness. Suicide Life Threat Behav. 2001;31(2):169-180.
20. Welu TC. A follow-up program for suicide attempters: evaluation of effectiveness. Suicide Life Threat Behav. 1977;7(1):17-20.
21. Linehan MM, Armstrong HE, Suarez A, et al. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48(12):1060-1064.
22. McLeavey B, Daly R, Ludgate J, et al. Interpersonal problem-solving skills training in the treatment of self-poisoning patients. Suicide Life Threat Behav. 1994;24(4):382-394.
23. Morgan HG, Jones EM, Owen JH. Secondary prevention of non-fatal deliberate self-harm. The green card study. Br J Psychiatry. 1993;163:111-112.
24. Salkovskis PM, Atha C, Storer D. Cognitive-behavioural problem solving in the treatment of patients who repeatedly attempt suicide. A controlled trial. Br J Psychiatry. 1990;157:871-876.
25. Hirsch SR, Walsh C, Draper R. Parasuicide. A review of treatment interventions. J Affect Disord. 1982;4(4):299-311.
26. Hawton K, Bancroft J, Catalan J, et al. Domiciliary and outpatient treatment of self-poisoning patients by medical and non-medical staff. Psychol Med. 1981;11(1):169-177.
27. Brown GK, Ten Have T, Henriques GR, et al. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294(5):563-570.
28. Bateman A, Fonagy P. 8-year follow-up of patients treated for borderline personality disorder: mentalization-based treatment versus treatment as usual. Am J Psychiatry. 2008;165(5):631-638.
29. Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. 2003;182:537-542.
30. Angst J, Angst F, Gerber-Werder R, et al. Suicide in 406 mood-disorder patients with and without long-term medication: a 40 to 44 years’ follow-up. Arch Suicide Res. 2005;9(3):279-300.
31. Baldessarini RJ, Tondo L, Hennen J. Lithium treatment and suicide risk in major affective disorders: update and new findings. J Clin Psychiatry. 2003;64(suppl 5):44-52.
32. Cipriani A, Pretty H, Hawton K, et al. Lithium in the prevention of suicidal behavior and all-cause mortality in patients with mood disorders: a systematic review of randomized trials. Am J Psychiatry. 2005;162(10):1805-1819.
33. Sinclair J, Green J. Understanding resolution of deliberate self harm: qualitative interview study of patients’ experiences. BMJ. 2005;330(7500):1112.-
‘Meth’ recovery: 3 steps to successful chronic management
Clinicians could become discouraged when confronting methamphetamine-dependent patients’ wide-ranging psychiatric symptoms.
These patients often present with:
- overlapping primary psychiatric syndromes and secondary substance abuse
- complex histories fraught with psychological trauma, limited social supports, and court involvement.
Treatment can be successful, however, and patients can change their addictive behaviors with a chronic disease management approach that targets the drug’s cognitive sequelae and psychiatric effects. Medications show limited benefit (Box 1),1-8 but behavioral treatments—including cognitive behavioral therapy (CBT) and motivational incentives—have proven efficacy in treating methamphetamine addiction.
This article discusses how to counteract methamphetamine’s negative cognitive effects and enable patients to engage in psychosocial treatment. Our discussion is informed by an extensive literature search and clinical experience from treating patients in the Midwest—at the geographic heart of the “meth” epidemic.
CASE REPORT: Overwhelmed and suicidal
Ms. D, age 27, presents to the emergency department with anxiety, dysphoria, and a plan to commit suicide by overdose. She feels overwhelmed by her 4-hour-a-day customer service job—a prerequisite for staying at the halfway house where she has lived for 2 months. She has a 13-year history of polysubstance dependence and is under court order to complete chemical dependence treatment or go to jail.
No medications are FDA-approved for treating methamphetamine dependence, and evidence supporting medication use in methamphetamine dependence is extremely limited. Research efforts are aimed at finding medications that might be neuroprotective, decrease craving, block reinforcement mechanisms, or affect other factors behind methamphetamine addiction and relapse.1 Most trials have been conducted in animal models or controlled laboratory evaluations of drug effects on methamphetamine-induced states.
Bupropion has shown slight treatment efficacy, possibly by decreasing neuronal damage and blocking reinforcement.2-4 Modafinil5 and baclofen6 may have potential, but evidence is lacking.
Some results have been unexpectedly negative. Sertraline might be contraindicated in methamphetamine dependence treatment, according to results of a randomized, placebo-controlled trial7 of sertraline and contingency management (Table 1). In a human laboratory study,8 topiramate accentuated—rather than diminished—subjective response to methamphetamine (Table 2).
Ms. D began using drugs at age 14 and has 3 convictions for driving under the influence of alcohol. An average student, she dropped out of high school but obtained a GED certificate. She first had psychiatric contact at age 16 and has been diagnosed at various times with attention deficit/hyperactivity disorder, bipolar disorder, and anxiety disorder. She also has been violently sexually assaulted while engaging in prostitution to support her drug habit.
Ms. D has been hospitalized multiple times—voluntarily and involuntarily—in dual diagnosis treatment centers. Her 5-year-old son no longer lives with her, and she has limited social supports beyond her parents, who live in a neighboring state.
Table 1
Antidepressant trials for treating methamphetamine dependence
| Drug | Investigation | Comments |
|---|---|---|
| Bupropion2-4 | Laboratory | Safety of bupropion with MAP |
| Laboratory | Reduced subjective effects and cue-induced craving | |
| Clinical trial | Trend toward reduced MAP use compared with placebo | |
| Sertraline7 | Clinical trial | Sertraline-treated subjects showed higher use of MAP compared with those receiving placebo and were less likely to complete treatment |
| MAP: methamphetamine | ||
3-step approach
For patients such as Ms. D, clinical evidence supports a 3-step approach to treating methamphetamine dependence:
- step 1: institute acute management and stabilization
- step 2: eliminate or decrease methamphetamine use to “move the frontal lobe back to the front”
- step 3: identify and target psychiatric and psychosocial comorbidities.
- help her eliminate or decrease methamphetamine use to allow neuronal systems to recover
- target maladaptive behaviors that hinder sobriety while providing motivational incentives to help her maintain a methamphetamine-free life.
How ‘meth’ affects cognition
Methamphetamine use has been associated with cognitive dysfunction at initial abstinence and even years later in some patients.10 Ms. D’s cognitive limitations in a fast-paced customer service job—even though hours are limited—lead to anxiety, dysphoria, and loss of self-esteem when she can’t manage patrons’ requests.
Methamphetamine has profound acute and chronic effects on the sympathetic nervous system, and dopaminergic, serotonergic, and noradrenergic neuronal networks. Most evidence of chronic neuronal effects comes from animal research and reflects toxic damage to dopaminergic and serotonergic neuronal systems. Postmortem human studies of direct neurotoxicity from chronic methamphetamine exposure show:
- decreased dopamine and tyrosine hydroxylase levels
- reduced concentrations of dopamine transporters.11
In chronic methamphetamine abusers, functional magnetic resonance imaging, proton magnetic resonance spectroscopy, and positron emission tomography show:
- changes in neurotransmitter, protein, brain metabolism, and transporter levels
- damage in multiple brain areas including the frontal region, basal ganglia, grey matter, corpus callosum, and striatum; smaller hippocampi; and cerebral vasculature changes.14-16
CASE CONTINUED: Does she understand?
After Ms. D is stabilized, her case manager expresses concern about her ability to follow through with treatment planning. He says, “I just don’t think she understands some of the things we discuss.” She then is referred for neuropsychological testing, which shows clear cognitive impairment. Specifically, she has a slowed rate of thinking, general cognitive ineficiency, deficits in learning and memory retention, and mild impulsivity.
Patients with a history of extensive methamphetamine abuse are ruled by the limbic system and may have higher cortical damage that complicates initiating, maintaining, and fully participating in treatment. Patients’ deficits in memory, executive functioning, attention, and cognitive speed may require you to simplify, repeat, and otherwise modify your treatment plan. You will need to provide clear instructions and consistent support—individually and psychosocially—and to recognize and reinforce patients’ treatment gains.
Even before using methamphetamine, patients may have had academic problems or learning disabilities that will compromise their ability to participate in treatment. Infection with HIV, syphilis, or hepatitis C can further hamper cognitive function.18
What treatments are effective?
Medications. Evidence is extremely limited, and no medications are approved to treat methamphetamine-addicted patients. Bupropion has shown some efficacy (Table 1),2-4,7 but other drugs such as sertraline and topiramate may aggravate rather than diminish methamphetamine dependence (Table 2).5,6,8,19
Behavioral treatments supply the evidence basis for methamphetamine dependence treatment. Cognitive behavioral therapy (CBT),20 contingency management (CM),21,22 and a manualized structured treatment—the Matrix Model23—all have proven efficacy.
CBT involves functional analysis and skills training. Patients are guided through analyzing their drug use and associated cognitions, emotions, and expectations and in identifying situations that trigger methamphetamine use or relapse. Skills training involves identifying, reinforcing, and practicing coping skills to help the patient avoid drug use and reinforce the ability to refuse use.
CM is based on operant conditioning—the use of consequences to modify behavior. It involves establishing a “contingent” relationship between a desired behavior/outcome (such as methamphetamine-free urinalysis) and delivering a positive reinforcing event to promote abstinence:
- Vouchers, privileges, or small amounts of money linked to healthy behaviors serve as incentives for negative urine testing.
- Rewards increase as periods of confirmed abstinence lengthen and are reset to smaller rewards if relapse occurs.
CM does not require extensive staff training and has been described as relatively simple to implement. CM also has been used successfully in urban gay and bisexual men with methamphetamine dependence (Box 2).18,25-29
Although CM’s efficacy is well-supported by clinical trials, we have encountered some resistance to the idea of “paying individuals to not use drugs” when training medical students, allied health staff, and residents. The National Institute on Drug Abuse (NIDA) supports the use of motivational incentives in treating substance abuse and offers support materials, resources, and training on this approach (see Related Resources).
Multiple studies show that CBT and CM are equally effective for treating chronic methamphetamine abuse at a 1-year follow-up, although CM may be more effective than CBT for acute treatment.
The Matrix model is a 4-month intensive, manualized treatment program that uses CBT, education on drug effects, positive reinforcement for intended behavioral change, and a 12-step approach.
Methamphetamine dependence outcomes based on the Matrix treatment model were compared with community treatment as usual in a project sponsored by The Center for Substance Abuse Treatment of the Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services.30 End-point outcomes were similar, but the Matrix treatment was more effective in early treatment, including decreased urinalyses positive for methamphetamine and increased abstinence.
Methamphetamine use is estimated to be 5 to 10 times more prevalent in U.S. urban gay and bisexual groups than in the general population25 and likely is contributing to rising human immunodeficiency virus (HIV) infection rates in men having sex with men (MSM).
Used to enhance sexual performance, libido, and mood, methamphetamine is associated with increased rates of unprotected anal sex and multiple partners in MSM.26 An HIV infection rate of 61% was reported in methamphetamine-dependent MSM seeking treatment in a Los Angeles clinical trial.27 Methamphetamine also results in high-risk sexual practices and multiple partners among heterosexual men and women.28
Although seroconverted men report using methamphetamine to alleviate HIV-associated depression, the combination of HIV infection and methamphetamine use may have powerful negative effects. Methamphetamine use is associated with HIV treatment nonadherence and also may suppress immune function.29 Cognitive impairments associated with HIV and methamphetamine use are additive and are further exacerbated by hepatitis C infection.18
Recommendation. Screen for methamphetamine use in MSM populations, and educate these patients about risks associated with methamphetamine use. In all patient groups who report using methamphetamine, provide counseling on high-risk sexual behavior, screen for sexually transmitted diseases, and ensure that patients are vaccinated against hepatitis A and B infection (see Related Resources). Most important, refer for medical treatment when indicated.
In patients such as Ms. D, the structure of court-ordered treatment can provide accountability, enforced abstinence, and mandated treatment resources. This, in turn, may give your patient a better chance to engage a recovering and better functioning frontal lobe to inhibit urges for methamphetamine use and manage stress.
Table 2
Other agents studied in methamphetamine dependence trials
| Drug | Investigation | Comment |
|---|---|---|
| Baclofen6 (GABAergic) | Clinical trial | No statistically significant effect compared with placebo; post hoc analysis showed ‘small’ treatment effects vs placebo |
| Gabapentin6 (GABAergic) | Clinical trial | No statistically signicant effect compared with placebo; post hoc analysis showed no treatment effects vs placebo |
| Topiramate8 (anticonvulsant) | Laboratory | Accentuated (rather than diminished) subjective effects of MAP |
| Aripiprazole19 (SGA) | Laboratory | Decreased subjective effects of amphetamine |
| Modafinil5 (wakefulness agent) | Clinical trial | Successful trial in cocaine dependence; potential option for MAP |
| MAP: methamphetamine; SGA: second-generation antipsychotic | ||
CASE CONTINUED: Racing thoughts and psychosis
Before hospital admission, Ms. D was being treated with gabapentin, 300 mg bid, and sustained-release bupropion, 150 mg/d, for anxiety and dysphoria. Previously, she has received multiple antidepressants and mood stabilizers with reportedly little effect.
Initially guarded, she at first denies psychotic symptoms but acknowledges their extent several days later. She describes periods of 6 months or more when she feels “lost.” The treatment team titrates quetiapine up to 200 mg/d and restarts duloxetine, 30 mg/d, for depressive symptoms, based on her past positive response to this antidepressant.
Methamphetamine abuse can cause and exacerbate psychiatric symptoms. Keep in mind 2 priorities as you approach these symptoms:
Aim for abstinence. Methamphetamine abuse produces a remarkable array of adverse effects. It causes dysphoria, anxiety, and psychosis during active use and in the interval after initial abstinence. Many of methamphetamine’s use and withdrawal symptoms resolve with time, however, and may not require pharmacologic treatment.31 Therefore, achieving abstinence and keeping patients in treatment is high priority.
Use behavioral approaches whenever feasible. Balance the need to use benzodiazepines for ongoing treatment of severe anxiety or agitation with the high risk of addiction or diversion in this group. Anxiety may resolve over time in association with sustained abstinence. Similarly, receiving treatment for methamphetamine dependence and maintaining abstinence appears to ease depressive symptoms, as shown by sustained improvements in Beck Depression Inventory scores at 1 year.32
Manage stress. Stress can worsen psychiatric symptoms, trigger methamphetamine abuse relapse and psychosis, and acutely and chronically augment methamphetamine’s toxic effects.33 You can help patients manage stress by:
- providing case management and CBT training
- advising them about proper sleep, nutrition, and medical care.
Targeting psychiatric symptoms
Step 3 in the chronic disease management approach to methamphetamine dependence is to identify and target psychiatric and psychosocial comorbidities. When approaching psychiatric symptoms, high priorities are to aim for abstinence and manage the patient’s stress (Box 3).31-33
In clinical practice, we find it difficult to diagnostically categorize and treat methamphetamine-abusing patients who show residual post-acute psychotic symptoms. Some appear to have no risk factors for primary psychotic illness, and their symptoms show an association with the severity of their past methamphetamine abuse.
Other patient presentations can be difficult to separate from family histories of psychotic illness. Research suggests that genetic risk factors may be associated with methamphetamine psychosis in some vulnerable patients.35
Unfortunately, no data exist to guide the use of antipsychotics to maintain symptom control. Some patients may need low-dose antipsychotics for maintenance treatment, and second-generation antipsychotics may have a theoretical advantage over first-generation antipsychotics. Use your clinical judgment in determining dosing and treatment duration, and in weighing risks and benefits of continued treatment.
Using imaging, researchers found aggression severity to be directly correlated with past total methamphetamine use and globally decreased serotonin transporter density.36 Serotonin transporter densities were 30% lower in methamphetamine users vs controls after >1 year of abstinence.
CASE CONTINUED: Discharge plans
Because of the severity of her psychiatric symptoms, Ms. D is unable to return to the halfway house after discharge. As her treatment team works to coordinate discharge placement, Ms. D continues to improve. Her psychotic and dysphoria symptoms resolve, and she shows increased spontaneity. These changes—attributed to supports during hospitalization, decreased stressors, and quetiapine treatment—continue until her discharge to a combined mental illness and chemical dependence program.
- Methamphetamine use and sexually transmitted diseases. Centers for Disease Control and Prevention. www.cdc.gov/std/DearColleagueRiskBehaviorMetUse8-18-2006.pdf.
- National Institute on Drug Abuse Blending Initiative. Promoting Awareness of Motivational Incentives (PAMI). www.drugabuse.gov/blending/PAMI.html.
- Aripiprazole • Abilify
- Baclofen • various
- Bupropion • Wellbutrin
- Duloxetine • Cymbalta
- Gabapentin • Neurontin
- Modafinil • Provigil
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Topiramate • Topamax
- Trazodone • Desyrel
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Vocci FJ, Acri J, Elkashef A. Medication development for addictive disorders: the state of the science. Am J Psychiatry 2005;162:1432-4.
2. Newton TF, Roache JD, De La Garza R, 2nd, et al. Safety of intravenous methamphetamine administration during treatment with bupropion. Psychopharmacology (Berl) 2005;182:426-35.
3. Newton TF, Roache JD, De La Garza R, et al. Bupropion reduces methamphetamine-induced subjective effects and cue-induced craving. Neuropsychopharmacology 2006;31:1537-44.
4. Ling W, Rawson R, Shoptaw S. Management of methamphetamine abuse and dependence. Curr Psychiatry Rep 2006;8:345-54.
5. Umanoff DF. Trial of modafinil for cocaine dependence. Neuropsychopharmacology 2005;30:2298; author reply 2299-300.
6. Heinzerling KG, Shoptaw S, Peck JA, et al. Randomized, placebo-controlled trial of baclofen and gabapentin for the treatment of methamphetamine dependence. Drug Alcohol Depend 2006;85:177-84.
7. Shoptaw S, Huber A, Peck J, et al. Randomized, placebo-controlled trial of sertraline and contingency management for the treatment of methamphetamine dependence. Drug Alcohol Depend 2006;85:12-8.
8. Johnson BA, Roache JD, Ait-Daoud N, et al. Effects of acute topiramate dosing on methamphetamine-induced subjective mood. Int J Neuropsychopharmacol 2007;10:85-98.
9. Bostwick J, Lineberry T. The ‘meth’ epidemic: Managing acute psychosis, agitation, and suicide risk. Current Psychiatry 2006;5(11):46-62.
10. Simon SL, Dacey J, Glynn S, et al. The effect of relapse on cognition in abstinent methamphetamine abusers. J Subst Abuse Treat 2004;27:59-66.
11. Wilson JM, Kalasinsky KS, Levey AI, et al. Striatal dopamine nerve terminal markers in human, chronic methamphetamine users. Nat Med 1996;2:699-703.
12. Moszczynska A, Fitzmaurice P, Ang L, et al. Why is parkinsonism not a feature of human methamphetamine users? Brain 2004;127:363-70.
13. Armstrong BD, Noguchi KK. The neurotoxic effects of 3,4-methylenedioxymethamphetamine (MDMA) and methamphetamine on serotonin, dopamine, and GABAergic terminals: an in-vitro autoradiographic study in rats. Neurotoxicology 2004;25:905-14.
14. London ED, Berman SM, Voytek B, et al. Cerebral metabolic dysfunction and impaired vigilance in recently abstinent methamphetamine abusers. Biol Psychiatry 2005;58:770-8.
15. London ED, Simon SL, Berman SM, et al. Mood disturbances and regional cerebral metabolic abnormalities in recently abstinent methamphetamine abusers. Arch Gen Psychiatry 2004;61:73-84.
16. Nordahl TE, Salo R, Leamon M. Neuropsychological effects of chronic methamphetamine use on neurotransmitters and cognition: a review. J Neuropsychiatry Clin Neurosci 2003;15:317-25.
17. Wang GJ, Volkow ND, Chang L, et al. Partial recovery of brain metabolism in methamphetamine abusers after protracted abstinence. Am J Psychiatry 2004;161:242-8.
18. Cherner M, Letendre S, Heaton RK, et al. Hepatitis C augments cognitive deficits associated with HIV infection and methamphetamine. Neurology 2005;64:1343-7.
19. Stoops WW. Aripiprazole as a potential pharmacotherapy for stimulant dependence: human laboratory studies with damphetamine. Exp Clin Psychopharmacol 2006;14:413-21.
20. Yen CF, Wu HY, Yen JY, Ko CH. Effects of brief cognitive-behavioral interventions on confidence to resist the urges to use heroin and methamphetamine in relapse-related situations. J Nerv Ment Dis 2004;192:788-91.
21. Roll JM, Petry NM, Stitzer ML, et al. Contingency management for the treatment of methamphetamine use disorders. Am J Psychiatry 2006;163:1993-9.
22. Shoptaw S, Klausner JD, Reback CJ, et al. A public health response to the methamphetamine epidemic: the implementation of contingency management to treat methamphetamine dependence. BMC Public Health 2006;6:214.-
23. Shoptaw S, Rawson RA, McCann MJ, Obert JL. The Matrix model of outpatient stimulant abuse treatment: evidence of efficacy. J Addict Dis 1994;13:129-41.
24. Sindelar J, Elbel B, Petry NM. What do we get for our money? Cost-effectiveness of adding contingency management. Addiction 2007;102:309-16.
25. Shoptaw S. Methamphetamine use in urban gay and bisexual populations. Top HIV Med 2006;14:84-7.
26. Bolding G, Hart G, Sherr L, Elford J. Use of crystal methamphetamine among gay men in London. Addiction 2006;101:1622-30.
27. Peck JA, Shoptaw S, Rotheram-Fuller E, et al. HIV-associated medical, behavioral, and psychiatric characteristics of treatment-seeking, methamphetamine-dependent men who have sex with men. J Addict Dis 2005;24:115-32.
28. Semple SJ, Patterson TL, Grant I. The context of sexual risk behavior among heterosexual methamphetamine users. Addict Behav 2004;29:807-10.
29. Mahajan SD, Hu Z, Reynolds JL, et al. Methamphetamine modulates gene expression patterns in monocyte derived mature dendritic cells: implications for HIV-1 pathogenesis. Mol Diagn Ther 2006;10:257-69.
30. Rawson RA, Marinelli-Casey P, Anglin MD, et al. A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction 2004;99:708-17.
31. McGregor C, Srisurapanont M, Jittiwutikarn J, et al. The nature, time course and severity of methamphetamine withdrawal. Addiction 2005;100:1320-9.
32. Peck JA, Reback CJ, Yang X, et al. Sustained reductions in drug use and depression symptoms from treatment for drug abuse in methamphetamine-dependent gay and bisexual men. J Urban Health 2005;82:i100-8.
33. Matuszewich L, Yamamoto BK. Chronic stress augments the long-term and acute effects of methamphetamine. Neuroscience 2004;124:637-46.
34. Batki SL, Harris DS. Quantitative drug levels in stimulant psychosis: relationship to symptom severity, catecholamines and hyperkinesia. Am J Addict 2004;13:461-70.
35. Suzuki A, Nakamura K, Sekine Y, et al. An association study between catechol-O-methyl transferase gene polymorphism and methamphetamine psychotic disorder. Psychiatr Genet 2006;16:133-8.
36. Sekine Y, Ouchi Y, Takei N, et al. Brain serotonin transporter density and aggression in abstinent methamphetamine abusers. Arch Gen Psychiatry 2006;63:90-100.
Clinicians could become discouraged when confronting methamphetamine-dependent patients’ wide-ranging psychiatric symptoms.
These patients often present with:
- overlapping primary psychiatric syndromes and secondary substance abuse
- complex histories fraught with psychological trauma, limited social supports, and court involvement.
Treatment can be successful, however, and patients can change their addictive behaviors with a chronic disease management approach that targets the drug’s cognitive sequelae and psychiatric effects. Medications show limited benefit (Box 1),1-8 but behavioral treatments—including cognitive behavioral therapy (CBT) and motivational incentives—have proven efficacy in treating methamphetamine addiction.
This article discusses how to counteract methamphetamine’s negative cognitive effects and enable patients to engage in psychosocial treatment. Our discussion is informed by an extensive literature search and clinical experience from treating patients in the Midwest—at the geographic heart of the “meth” epidemic.
CASE REPORT: Overwhelmed and suicidal
Ms. D, age 27, presents to the emergency department with anxiety, dysphoria, and a plan to commit suicide by overdose. She feels overwhelmed by her 4-hour-a-day customer service job—a prerequisite for staying at the halfway house where she has lived for 2 months. She has a 13-year history of polysubstance dependence and is under court order to complete chemical dependence treatment or go to jail.
No medications are FDA-approved for treating methamphetamine dependence, and evidence supporting medication use in methamphetamine dependence is extremely limited. Research efforts are aimed at finding medications that might be neuroprotective, decrease craving, block reinforcement mechanisms, or affect other factors behind methamphetamine addiction and relapse.1 Most trials have been conducted in animal models or controlled laboratory evaluations of drug effects on methamphetamine-induced states.
Bupropion has shown slight treatment efficacy, possibly by decreasing neuronal damage and blocking reinforcement.2-4 Modafinil5 and baclofen6 may have potential, but evidence is lacking.
Some results have been unexpectedly negative. Sertraline might be contraindicated in methamphetamine dependence treatment, according to results of a randomized, placebo-controlled trial7 of sertraline and contingency management (Table 1). In a human laboratory study,8 topiramate accentuated—rather than diminished—subjective response to methamphetamine (Table 2).
Ms. D began using drugs at age 14 and has 3 convictions for driving under the influence of alcohol. An average student, she dropped out of high school but obtained a GED certificate. She first had psychiatric contact at age 16 and has been diagnosed at various times with attention deficit/hyperactivity disorder, bipolar disorder, and anxiety disorder. She also has been violently sexually assaulted while engaging in prostitution to support her drug habit.
Ms. D has been hospitalized multiple times—voluntarily and involuntarily—in dual diagnosis treatment centers. Her 5-year-old son no longer lives with her, and she has limited social supports beyond her parents, who live in a neighboring state.
Table 1
Antidepressant trials for treating methamphetamine dependence
| Drug | Investigation | Comments |
|---|---|---|
| Bupropion2-4 | Laboratory | Safety of bupropion with MAP |
| Laboratory | Reduced subjective effects and cue-induced craving | |
| Clinical trial | Trend toward reduced MAP use compared with placebo | |
| Sertraline7 | Clinical trial | Sertraline-treated subjects showed higher use of MAP compared with those receiving placebo and were less likely to complete treatment |
| MAP: methamphetamine | ||
3-step approach
For patients such as Ms. D, clinical evidence supports a 3-step approach to treating methamphetamine dependence:
- step 1: institute acute management and stabilization
- step 2: eliminate or decrease methamphetamine use to “move the frontal lobe back to the front”
- step 3: identify and target psychiatric and psychosocial comorbidities.
- help her eliminate or decrease methamphetamine use to allow neuronal systems to recover
- target maladaptive behaviors that hinder sobriety while providing motivational incentives to help her maintain a methamphetamine-free life.
How ‘meth’ affects cognition
Methamphetamine use has been associated with cognitive dysfunction at initial abstinence and even years later in some patients.10 Ms. D’s cognitive limitations in a fast-paced customer service job—even though hours are limited—lead to anxiety, dysphoria, and loss of self-esteem when she can’t manage patrons’ requests.
Methamphetamine has profound acute and chronic effects on the sympathetic nervous system, and dopaminergic, serotonergic, and noradrenergic neuronal networks. Most evidence of chronic neuronal effects comes from animal research and reflects toxic damage to dopaminergic and serotonergic neuronal systems. Postmortem human studies of direct neurotoxicity from chronic methamphetamine exposure show:
- decreased dopamine and tyrosine hydroxylase levels
- reduced concentrations of dopamine transporters.11
In chronic methamphetamine abusers, functional magnetic resonance imaging, proton magnetic resonance spectroscopy, and positron emission tomography show:
- changes in neurotransmitter, protein, brain metabolism, and transporter levels
- damage in multiple brain areas including the frontal region, basal ganglia, grey matter, corpus callosum, and striatum; smaller hippocampi; and cerebral vasculature changes.14-16
CASE CONTINUED: Does she understand?
After Ms. D is stabilized, her case manager expresses concern about her ability to follow through with treatment planning. He says, “I just don’t think she understands some of the things we discuss.” She then is referred for neuropsychological testing, which shows clear cognitive impairment. Specifically, she has a slowed rate of thinking, general cognitive ineficiency, deficits in learning and memory retention, and mild impulsivity.
Patients with a history of extensive methamphetamine abuse are ruled by the limbic system and may have higher cortical damage that complicates initiating, maintaining, and fully participating in treatment. Patients’ deficits in memory, executive functioning, attention, and cognitive speed may require you to simplify, repeat, and otherwise modify your treatment plan. You will need to provide clear instructions and consistent support—individually and psychosocially—and to recognize and reinforce patients’ treatment gains.
Even before using methamphetamine, patients may have had academic problems or learning disabilities that will compromise their ability to participate in treatment. Infection with HIV, syphilis, or hepatitis C can further hamper cognitive function.18
What treatments are effective?
Medications. Evidence is extremely limited, and no medications are approved to treat methamphetamine-addicted patients. Bupropion has shown some efficacy (Table 1),2-4,7 but other drugs such as sertraline and topiramate may aggravate rather than diminish methamphetamine dependence (Table 2).5,6,8,19
Behavioral treatments supply the evidence basis for methamphetamine dependence treatment. Cognitive behavioral therapy (CBT),20 contingency management (CM),21,22 and a manualized structured treatment—the Matrix Model23—all have proven efficacy.
CBT involves functional analysis and skills training. Patients are guided through analyzing their drug use and associated cognitions, emotions, and expectations and in identifying situations that trigger methamphetamine use or relapse. Skills training involves identifying, reinforcing, and practicing coping skills to help the patient avoid drug use and reinforce the ability to refuse use.
CM is based on operant conditioning—the use of consequences to modify behavior. It involves establishing a “contingent” relationship between a desired behavior/outcome (such as methamphetamine-free urinalysis) and delivering a positive reinforcing event to promote abstinence:
- Vouchers, privileges, or small amounts of money linked to healthy behaviors serve as incentives for negative urine testing.
- Rewards increase as periods of confirmed abstinence lengthen and are reset to smaller rewards if relapse occurs.
CM does not require extensive staff training and has been described as relatively simple to implement. CM also has been used successfully in urban gay and bisexual men with methamphetamine dependence (Box 2).18,25-29
Although CM’s efficacy is well-supported by clinical trials, we have encountered some resistance to the idea of “paying individuals to not use drugs” when training medical students, allied health staff, and residents. The National Institute on Drug Abuse (NIDA) supports the use of motivational incentives in treating substance abuse and offers support materials, resources, and training on this approach (see Related Resources).
Multiple studies show that CBT and CM are equally effective for treating chronic methamphetamine abuse at a 1-year follow-up, although CM may be more effective than CBT for acute treatment.
The Matrix model is a 4-month intensive, manualized treatment program that uses CBT, education on drug effects, positive reinforcement for intended behavioral change, and a 12-step approach.
Methamphetamine dependence outcomes based on the Matrix treatment model were compared with community treatment as usual in a project sponsored by The Center for Substance Abuse Treatment of the Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services.30 End-point outcomes were similar, but the Matrix treatment was more effective in early treatment, including decreased urinalyses positive for methamphetamine and increased abstinence.
Methamphetamine use is estimated to be 5 to 10 times more prevalent in U.S. urban gay and bisexual groups than in the general population25 and likely is contributing to rising human immunodeficiency virus (HIV) infection rates in men having sex with men (MSM).
Used to enhance sexual performance, libido, and mood, methamphetamine is associated with increased rates of unprotected anal sex and multiple partners in MSM.26 An HIV infection rate of 61% was reported in methamphetamine-dependent MSM seeking treatment in a Los Angeles clinical trial.27 Methamphetamine also results in high-risk sexual practices and multiple partners among heterosexual men and women.28
Although seroconverted men report using methamphetamine to alleviate HIV-associated depression, the combination of HIV infection and methamphetamine use may have powerful negative effects. Methamphetamine use is associated with HIV treatment nonadherence and also may suppress immune function.29 Cognitive impairments associated with HIV and methamphetamine use are additive and are further exacerbated by hepatitis C infection.18
Recommendation. Screen for methamphetamine use in MSM populations, and educate these patients about risks associated with methamphetamine use. In all patient groups who report using methamphetamine, provide counseling on high-risk sexual behavior, screen for sexually transmitted diseases, and ensure that patients are vaccinated against hepatitis A and B infection (see Related Resources). Most important, refer for medical treatment when indicated.
In patients such as Ms. D, the structure of court-ordered treatment can provide accountability, enforced abstinence, and mandated treatment resources. This, in turn, may give your patient a better chance to engage a recovering and better functioning frontal lobe to inhibit urges for methamphetamine use and manage stress.
Table 2
Other agents studied in methamphetamine dependence trials
| Drug | Investigation | Comment |
|---|---|---|
| Baclofen6 (GABAergic) | Clinical trial | No statistically significant effect compared with placebo; post hoc analysis showed ‘small’ treatment effects vs placebo |
| Gabapentin6 (GABAergic) | Clinical trial | No statistically signicant effect compared with placebo; post hoc analysis showed no treatment effects vs placebo |
| Topiramate8 (anticonvulsant) | Laboratory | Accentuated (rather than diminished) subjective effects of MAP |
| Aripiprazole19 (SGA) | Laboratory | Decreased subjective effects of amphetamine |
| Modafinil5 (wakefulness agent) | Clinical trial | Successful trial in cocaine dependence; potential option for MAP |
| MAP: methamphetamine; SGA: second-generation antipsychotic | ||
CASE CONTINUED: Racing thoughts and psychosis
Before hospital admission, Ms. D was being treated with gabapentin, 300 mg bid, and sustained-release bupropion, 150 mg/d, for anxiety and dysphoria. Previously, she has received multiple antidepressants and mood stabilizers with reportedly little effect.
Initially guarded, she at first denies psychotic symptoms but acknowledges their extent several days later. She describes periods of 6 months or more when she feels “lost.” The treatment team titrates quetiapine up to 200 mg/d and restarts duloxetine, 30 mg/d, for depressive symptoms, based on her past positive response to this antidepressant.
Methamphetamine abuse can cause and exacerbate psychiatric symptoms. Keep in mind 2 priorities as you approach these symptoms:
Aim for abstinence. Methamphetamine abuse produces a remarkable array of adverse effects. It causes dysphoria, anxiety, and psychosis during active use and in the interval after initial abstinence. Many of methamphetamine’s use and withdrawal symptoms resolve with time, however, and may not require pharmacologic treatment.31 Therefore, achieving abstinence and keeping patients in treatment is high priority.
Use behavioral approaches whenever feasible. Balance the need to use benzodiazepines for ongoing treatment of severe anxiety or agitation with the high risk of addiction or diversion in this group. Anxiety may resolve over time in association with sustained abstinence. Similarly, receiving treatment for methamphetamine dependence and maintaining abstinence appears to ease depressive symptoms, as shown by sustained improvements in Beck Depression Inventory scores at 1 year.32
Manage stress. Stress can worsen psychiatric symptoms, trigger methamphetamine abuse relapse and psychosis, and acutely and chronically augment methamphetamine’s toxic effects.33 You can help patients manage stress by:
- providing case management and CBT training
- advising them about proper sleep, nutrition, and medical care.
Targeting psychiatric symptoms
Step 3 in the chronic disease management approach to methamphetamine dependence is to identify and target psychiatric and psychosocial comorbidities. When approaching psychiatric symptoms, high priorities are to aim for abstinence and manage the patient’s stress (Box 3).31-33
In clinical practice, we find it difficult to diagnostically categorize and treat methamphetamine-abusing patients who show residual post-acute psychotic symptoms. Some appear to have no risk factors for primary psychotic illness, and their symptoms show an association with the severity of their past methamphetamine abuse.
Other patient presentations can be difficult to separate from family histories of psychotic illness. Research suggests that genetic risk factors may be associated with methamphetamine psychosis in some vulnerable patients.35
Unfortunately, no data exist to guide the use of antipsychotics to maintain symptom control. Some patients may need low-dose antipsychotics for maintenance treatment, and second-generation antipsychotics may have a theoretical advantage over first-generation antipsychotics. Use your clinical judgment in determining dosing and treatment duration, and in weighing risks and benefits of continued treatment.
Using imaging, researchers found aggression severity to be directly correlated with past total methamphetamine use and globally decreased serotonin transporter density.36 Serotonin transporter densities were 30% lower in methamphetamine users vs controls after >1 year of abstinence.
CASE CONTINUED: Discharge plans
Because of the severity of her psychiatric symptoms, Ms. D is unable to return to the halfway house after discharge. As her treatment team works to coordinate discharge placement, Ms. D continues to improve. Her psychotic and dysphoria symptoms resolve, and she shows increased spontaneity. These changes—attributed to supports during hospitalization, decreased stressors, and quetiapine treatment—continue until her discharge to a combined mental illness and chemical dependence program.
- Methamphetamine use and sexually transmitted diseases. Centers for Disease Control and Prevention. www.cdc.gov/std/DearColleagueRiskBehaviorMetUse8-18-2006.pdf.
- National Institute on Drug Abuse Blending Initiative. Promoting Awareness of Motivational Incentives (PAMI). www.drugabuse.gov/blending/PAMI.html.
- Aripiprazole • Abilify
- Baclofen • various
- Bupropion • Wellbutrin
- Duloxetine • Cymbalta
- Gabapentin • Neurontin
- Modafinil • Provigil
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Topiramate • Topamax
- Trazodone • Desyrel
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Clinicians could become discouraged when confronting methamphetamine-dependent patients’ wide-ranging psychiatric symptoms.
These patients often present with:
- overlapping primary psychiatric syndromes and secondary substance abuse
- complex histories fraught with psychological trauma, limited social supports, and court involvement.
Treatment can be successful, however, and patients can change their addictive behaviors with a chronic disease management approach that targets the drug’s cognitive sequelae and psychiatric effects. Medications show limited benefit (Box 1),1-8 but behavioral treatments—including cognitive behavioral therapy (CBT) and motivational incentives—have proven efficacy in treating methamphetamine addiction.
This article discusses how to counteract methamphetamine’s negative cognitive effects and enable patients to engage in psychosocial treatment. Our discussion is informed by an extensive literature search and clinical experience from treating patients in the Midwest—at the geographic heart of the “meth” epidemic.
CASE REPORT: Overwhelmed and suicidal
Ms. D, age 27, presents to the emergency department with anxiety, dysphoria, and a plan to commit suicide by overdose. She feels overwhelmed by her 4-hour-a-day customer service job—a prerequisite for staying at the halfway house where she has lived for 2 months. She has a 13-year history of polysubstance dependence and is under court order to complete chemical dependence treatment or go to jail.
No medications are FDA-approved for treating methamphetamine dependence, and evidence supporting medication use in methamphetamine dependence is extremely limited. Research efforts are aimed at finding medications that might be neuroprotective, decrease craving, block reinforcement mechanisms, or affect other factors behind methamphetamine addiction and relapse.1 Most trials have been conducted in animal models or controlled laboratory evaluations of drug effects on methamphetamine-induced states.
Bupropion has shown slight treatment efficacy, possibly by decreasing neuronal damage and blocking reinforcement.2-4 Modafinil5 and baclofen6 may have potential, but evidence is lacking.
Some results have been unexpectedly negative. Sertraline might be contraindicated in methamphetamine dependence treatment, according to results of a randomized, placebo-controlled trial7 of sertraline and contingency management (Table 1). In a human laboratory study,8 topiramate accentuated—rather than diminished—subjective response to methamphetamine (Table 2).
Ms. D began using drugs at age 14 and has 3 convictions for driving under the influence of alcohol. An average student, she dropped out of high school but obtained a GED certificate. She first had psychiatric contact at age 16 and has been diagnosed at various times with attention deficit/hyperactivity disorder, bipolar disorder, and anxiety disorder. She also has been violently sexually assaulted while engaging in prostitution to support her drug habit.
Ms. D has been hospitalized multiple times—voluntarily and involuntarily—in dual diagnosis treatment centers. Her 5-year-old son no longer lives with her, and she has limited social supports beyond her parents, who live in a neighboring state.
Table 1
Antidepressant trials for treating methamphetamine dependence
| Drug | Investigation | Comments |
|---|---|---|
| Bupropion2-4 | Laboratory | Safety of bupropion with MAP |
| Laboratory | Reduced subjective effects and cue-induced craving | |
| Clinical trial | Trend toward reduced MAP use compared with placebo | |
| Sertraline7 | Clinical trial | Sertraline-treated subjects showed higher use of MAP compared with those receiving placebo and were less likely to complete treatment |
| MAP: methamphetamine | ||
3-step approach
For patients such as Ms. D, clinical evidence supports a 3-step approach to treating methamphetamine dependence:
- step 1: institute acute management and stabilization
- step 2: eliminate or decrease methamphetamine use to “move the frontal lobe back to the front”
- step 3: identify and target psychiatric and psychosocial comorbidities.
- help her eliminate or decrease methamphetamine use to allow neuronal systems to recover
- target maladaptive behaviors that hinder sobriety while providing motivational incentives to help her maintain a methamphetamine-free life.
How ‘meth’ affects cognition
Methamphetamine use has been associated with cognitive dysfunction at initial abstinence and even years later in some patients.10 Ms. D’s cognitive limitations in a fast-paced customer service job—even though hours are limited—lead to anxiety, dysphoria, and loss of self-esteem when she can’t manage patrons’ requests.
Methamphetamine has profound acute and chronic effects on the sympathetic nervous system, and dopaminergic, serotonergic, and noradrenergic neuronal networks. Most evidence of chronic neuronal effects comes from animal research and reflects toxic damage to dopaminergic and serotonergic neuronal systems. Postmortem human studies of direct neurotoxicity from chronic methamphetamine exposure show:
- decreased dopamine and tyrosine hydroxylase levels
- reduced concentrations of dopamine transporters.11
In chronic methamphetamine abusers, functional magnetic resonance imaging, proton magnetic resonance spectroscopy, and positron emission tomography show:
- changes in neurotransmitter, protein, brain metabolism, and transporter levels
- damage in multiple brain areas including the frontal region, basal ganglia, grey matter, corpus callosum, and striatum; smaller hippocampi; and cerebral vasculature changes.14-16
CASE CONTINUED: Does she understand?
After Ms. D is stabilized, her case manager expresses concern about her ability to follow through with treatment planning. He says, “I just don’t think she understands some of the things we discuss.” She then is referred for neuropsychological testing, which shows clear cognitive impairment. Specifically, she has a slowed rate of thinking, general cognitive ineficiency, deficits in learning and memory retention, and mild impulsivity.
Patients with a history of extensive methamphetamine abuse are ruled by the limbic system and may have higher cortical damage that complicates initiating, maintaining, and fully participating in treatment. Patients’ deficits in memory, executive functioning, attention, and cognitive speed may require you to simplify, repeat, and otherwise modify your treatment plan. You will need to provide clear instructions and consistent support—individually and psychosocially—and to recognize and reinforce patients’ treatment gains.
Even before using methamphetamine, patients may have had academic problems or learning disabilities that will compromise their ability to participate in treatment. Infection with HIV, syphilis, or hepatitis C can further hamper cognitive function.18
What treatments are effective?
Medications. Evidence is extremely limited, and no medications are approved to treat methamphetamine-addicted patients. Bupropion has shown some efficacy (Table 1),2-4,7 but other drugs such as sertraline and topiramate may aggravate rather than diminish methamphetamine dependence (Table 2).5,6,8,19
Behavioral treatments supply the evidence basis for methamphetamine dependence treatment. Cognitive behavioral therapy (CBT),20 contingency management (CM),21,22 and a manualized structured treatment—the Matrix Model23—all have proven efficacy.
CBT involves functional analysis and skills training. Patients are guided through analyzing their drug use and associated cognitions, emotions, and expectations and in identifying situations that trigger methamphetamine use or relapse. Skills training involves identifying, reinforcing, and practicing coping skills to help the patient avoid drug use and reinforce the ability to refuse use.
CM is based on operant conditioning—the use of consequences to modify behavior. It involves establishing a “contingent” relationship between a desired behavior/outcome (such as methamphetamine-free urinalysis) and delivering a positive reinforcing event to promote abstinence:
- Vouchers, privileges, or small amounts of money linked to healthy behaviors serve as incentives for negative urine testing.
- Rewards increase as periods of confirmed abstinence lengthen and are reset to smaller rewards if relapse occurs.
CM does not require extensive staff training and has been described as relatively simple to implement. CM also has been used successfully in urban gay and bisexual men with methamphetamine dependence (Box 2).18,25-29
Although CM’s efficacy is well-supported by clinical trials, we have encountered some resistance to the idea of “paying individuals to not use drugs” when training medical students, allied health staff, and residents. The National Institute on Drug Abuse (NIDA) supports the use of motivational incentives in treating substance abuse and offers support materials, resources, and training on this approach (see Related Resources).
Multiple studies show that CBT and CM are equally effective for treating chronic methamphetamine abuse at a 1-year follow-up, although CM may be more effective than CBT for acute treatment.
The Matrix model is a 4-month intensive, manualized treatment program that uses CBT, education on drug effects, positive reinforcement for intended behavioral change, and a 12-step approach.
Methamphetamine dependence outcomes based on the Matrix treatment model were compared with community treatment as usual in a project sponsored by The Center for Substance Abuse Treatment of the Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services.30 End-point outcomes were similar, but the Matrix treatment was more effective in early treatment, including decreased urinalyses positive for methamphetamine and increased abstinence.
Methamphetamine use is estimated to be 5 to 10 times more prevalent in U.S. urban gay and bisexual groups than in the general population25 and likely is contributing to rising human immunodeficiency virus (HIV) infection rates in men having sex with men (MSM).
Used to enhance sexual performance, libido, and mood, methamphetamine is associated with increased rates of unprotected anal sex and multiple partners in MSM.26 An HIV infection rate of 61% was reported in methamphetamine-dependent MSM seeking treatment in a Los Angeles clinical trial.27 Methamphetamine also results in high-risk sexual practices and multiple partners among heterosexual men and women.28
Although seroconverted men report using methamphetamine to alleviate HIV-associated depression, the combination of HIV infection and methamphetamine use may have powerful negative effects. Methamphetamine use is associated with HIV treatment nonadherence and also may suppress immune function.29 Cognitive impairments associated with HIV and methamphetamine use are additive and are further exacerbated by hepatitis C infection.18
Recommendation. Screen for methamphetamine use in MSM populations, and educate these patients about risks associated with methamphetamine use. In all patient groups who report using methamphetamine, provide counseling on high-risk sexual behavior, screen for sexually transmitted diseases, and ensure that patients are vaccinated against hepatitis A and B infection (see Related Resources). Most important, refer for medical treatment when indicated.
In patients such as Ms. D, the structure of court-ordered treatment can provide accountability, enforced abstinence, and mandated treatment resources. This, in turn, may give your patient a better chance to engage a recovering and better functioning frontal lobe to inhibit urges for methamphetamine use and manage stress.
Table 2
Other agents studied in methamphetamine dependence trials
| Drug | Investigation | Comment |
|---|---|---|
| Baclofen6 (GABAergic) | Clinical trial | No statistically significant effect compared with placebo; post hoc analysis showed ‘small’ treatment effects vs placebo |
| Gabapentin6 (GABAergic) | Clinical trial | No statistically signicant effect compared with placebo; post hoc analysis showed no treatment effects vs placebo |
| Topiramate8 (anticonvulsant) | Laboratory | Accentuated (rather than diminished) subjective effects of MAP |
| Aripiprazole19 (SGA) | Laboratory | Decreased subjective effects of amphetamine |
| Modafinil5 (wakefulness agent) | Clinical trial | Successful trial in cocaine dependence; potential option for MAP |
| MAP: methamphetamine; SGA: second-generation antipsychotic | ||
CASE CONTINUED: Racing thoughts and psychosis
Before hospital admission, Ms. D was being treated with gabapentin, 300 mg bid, and sustained-release bupropion, 150 mg/d, for anxiety and dysphoria. Previously, she has received multiple antidepressants and mood stabilizers with reportedly little effect.
Initially guarded, she at first denies psychotic symptoms but acknowledges their extent several days later. She describes periods of 6 months or more when she feels “lost.” The treatment team titrates quetiapine up to 200 mg/d and restarts duloxetine, 30 mg/d, for depressive symptoms, based on her past positive response to this antidepressant.
Methamphetamine abuse can cause and exacerbate psychiatric symptoms. Keep in mind 2 priorities as you approach these symptoms:
Aim for abstinence. Methamphetamine abuse produces a remarkable array of adverse effects. It causes dysphoria, anxiety, and psychosis during active use and in the interval after initial abstinence. Many of methamphetamine’s use and withdrawal symptoms resolve with time, however, and may not require pharmacologic treatment.31 Therefore, achieving abstinence and keeping patients in treatment is high priority.
Use behavioral approaches whenever feasible. Balance the need to use benzodiazepines for ongoing treatment of severe anxiety or agitation with the high risk of addiction or diversion in this group. Anxiety may resolve over time in association with sustained abstinence. Similarly, receiving treatment for methamphetamine dependence and maintaining abstinence appears to ease depressive symptoms, as shown by sustained improvements in Beck Depression Inventory scores at 1 year.32
Manage stress. Stress can worsen psychiatric symptoms, trigger methamphetamine abuse relapse and psychosis, and acutely and chronically augment methamphetamine’s toxic effects.33 You can help patients manage stress by:
- providing case management and CBT training
- advising them about proper sleep, nutrition, and medical care.
Targeting psychiatric symptoms
Step 3 in the chronic disease management approach to methamphetamine dependence is to identify and target psychiatric and psychosocial comorbidities. When approaching psychiatric symptoms, high priorities are to aim for abstinence and manage the patient’s stress (Box 3).31-33
In clinical practice, we find it difficult to diagnostically categorize and treat methamphetamine-abusing patients who show residual post-acute psychotic symptoms. Some appear to have no risk factors for primary psychotic illness, and their symptoms show an association with the severity of their past methamphetamine abuse.
Other patient presentations can be difficult to separate from family histories of psychotic illness. Research suggests that genetic risk factors may be associated with methamphetamine psychosis in some vulnerable patients.35
Unfortunately, no data exist to guide the use of antipsychotics to maintain symptom control. Some patients may need low-dose antipsychotics for maintenance treatment, and second-generation antipsychotics may have a theoretical advantage over first-generation antipsychotics. Use your clinical judgment in determining dosing and treatment duration, and in weighing risks and benefits of continued treatment.
Using imaging, researchers found aggression severity to be directly correlated with past total methamphetamine use and globally decreased serotonin transporter density.36 Serotonin transporter densities were 30% lower in methamphetamine users vs controls after >1 year of abstinence.
CASE CONTINUED: Discharge plans
Because of the severity of her psychiatric symptoms, Ms. D is unable to return to the halfway house after discharge. As her treatment team works to coordinate discharge placement, Ms. D continues to improve. Her psychotic and dysphoria symptoms resolve, and she shows increased spontaneity. These changes—attributed to supports during hospitalization, decreased stressors, and quetiapine treatment—continue until her discharge to a combined mental illness and chemical dependence program.
- Methamphetamine use and sexually transmitted diseases. Centers for Disease Control and Prevention. www.cdc.gov/std/DearColleagueRiskBehaviorMetUse8-18-2006.pdf.
- National Institute on Drug Abuse Blending Initiative. Promoting Awareness of Motivational Incentives (PAMI). www.drugabuse.gov/blending/PAMI.html.
- Aripiprazole • Abilify
- Baclofen • various
- Bupropion • Wellbutrin
- Duloxetine • Cymbalta
- Gabapentin • Neurontin
- Modafinil • Provigil
- Quetiapine • Seroquel
- Sertraline • Zoloft
- Topiramate • Topamax
- Trazodone • Desyrel
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Vocci FJ, Acri J, Elkashef A. Medication development for addictive disorders: the state of the science. Am J Psychiatry 2005;162:1432-4.
2. Newton TF, Roache JD, De La Garza R, 2nd, et al. Safety of intravenous methamphetamine administration during treatment with bupropion. Psychopharmacology (Berl) 2005;182:426-35.
3. Newton TF, Roache JD, De La Garza R, et al. Bupropion reduces methamphetamine-induced subjective effects and cue-induced craving. Neuropsychopharmacology 2006;31:1537-44.
4. Ling W, Rawson R, Shoptaw S. Management of methamphetamine abuse and dependence. Curr Psychiatry Rep 2006;8:345-54.
5. Umanoff DF. Trial of modafinil for cocaine dependence. Neuropsychopharmacology 2005;30:2298; author reply 2299-300.
6. Heinzerling KG, Shoptaw S, Peck JA, et al. Randomized, placebo-controlled trial of baclofen and gabapentin for the treatment of methamphetamine dependence. Drug Alcohol Depend 2006;85:177-84.
7. Shoptaw S, Huber A, Peck J, et al. Randomized, placebo-controlled trial of sertraline and contingency management for the treatment of methamphetamine dependence. Drug Alcohol Depend 2006;85:12-8.
8. Johnson BA, Roache JD, Ait-Daoud N, et al. Effects of acute topiramate dosing on methamphetamine-induced subjective mood. Int J Neuropsychopharmacol 2007;10:85-98.
9. Bostwick J, Lineberry T. The ‘meth’ epidemic: Managing acute psychosis, agitation, and suicide risk. Current Psychiatry 2006;5(11):46-62.
10. Simon SL, Dacey J, Glynn S, et al. The effect of relapse on cognition in abstinent methamphetamine abusers. J Subst Abuse Treat 2004;27:59-66.
11. Wilson JM, Kalasinsky KS, Levey AI, et al. Striatal dopamine nerve terminal markers in human, chronic methamphetamine users. Nat Med 1996;2:699-703.
12. Moszczynska A, Fitzmaurice P, Ang L, et al. Why is parkinsonism not a feature of human methamphetamine users? Brain 2004;127:363-70.
13. Armstrong BD, Noguchi KK. The neurotoxic effects of 3,4-methylenedioxymethamphetamine (MDMA) and methamphetamine on serotonin, dopamine, and GABAergic terminals: an in-vitro autoradiographic study in rats. Neurotoxicology 2004;25:905-14.
14. London ED, Berman SM, Voytek B, et al. Cerebral metabolic dysfunction and impaired vigilance in recently abstinent methamphetamine abusers. Biol Psychiatry 2005;58:770-8.
15. London ED, Simon SL, Berman SM, et al. Mood disturbances and regional cerebral metabolic abnormalities in recently abstinent methamphetamine abusers. Arch Gen Psychiatry 2004;61:73-84.
16. Nordahl TE, Salo R, Leamon M. Neuropsychological effects of chronic methamphetamine use on neurotransmitters and cognition: a review. J Neuropsychiatry Clin Neurosci 2003;15:317-25.
17. Wang GJ, Volkow ND, Chang L, et al. Partial recovery of brain metabolism in methamphetamine abusers after protracted abstinence. Am J Psychiatry 2004;161:242-8.
18. Cherner M, Letendre S, Heaton RK, et al. Hepatitis C augments cognitive deficits associated with HIV infection and methamphetamine. Neurology 2005;64:1343-7.
19. Stoops WW. Aripiprazole as a potential pharmacotherapy for stimulant dependence: human laboratory studies with damphetamine. Exp Clin Psychopharmacol 2006;14:413-21.
20. Yen CF, Wu HY, Yen JY, Ko CH. Effects of brief cognitive-behavioral interventions on confidence to resist the urges to use heroin and methamphetamine in relapse-related situations. J Nerv Ment Dis 2004;192:788-91.
21. Roll JM, Petry NM, Stitzer ML, et al. Contingency management for the treatment of methamphetamine use disorders. Am J Psychiatry 2006;163:1993-9.
22. Shoptaw S, Klausner JD, Reback CJ, et al. A public health response to the methamphetamine epidemic: the implementation of contingency management to treat methamphetamine dependence. BMC Public Health 2006;6:214.-
23. Shoptaw S, Rawson RA, McCann MJ, Obert JL. The Matrix model of outpatient stimulant abuse treatment: evidence of efficacy. J Addict Dis 1994;13:129-41.
24. Sindelar J, Elbel B, Petry NM. What do we get for our money? Cost-effectiveness of adding contingency management. Addiction 2007;102:309-16.
25. Shoptaw S. Methamphetamine use in urban gay and bisexual populations. Top HIV Med 2006;14:84-7.
26. Bolding G, Hart G, Sherr L, Elford J. Use of crystal methamphetamine among gay men in London. Addiction 2006;101:1622-30.
27. Peck JA, Shoptaw S, Rotheram-Fuller E, et al. HIV-associated medical, behavioral, and psychiatric characteristics of treatment-seeking, methamphetamine-dependent men who have sex with men. J Addict Dis 2005;24:115-32.
28. Semple SJ, Patterson TL, Grant I. The context of sexual risk behavior among heterosexual methamphetamine users. Addict Behav 2004;29:807-10.
29. Mahajan SD, Hu Z, Reynolds JL, et al. Methamphetamine modulates gene expression patterns in monocyte derived mature dendritic cells: implications for HIV-1 pathogenesis. Mol Diagn Ther 2006;10:257-69.
30. Rawson RA, Marinelli-Casey P, Anglin MD, et al. A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction 2004;99:708-17.
31. McGregor C, Srisurapanont M, Jittiwutikarn J, et al. The nature, time course and severity of methamphetamine withdrawal. Addiction 2005;100:1320-9.
32. Peck JA, Reback CJ, Yang X, et al. Sustained reductions in drug use and depression symptoms from treatment for drug abuse in methamphetamine-dependent gay and bisexual men. J Urban Health 2005;82:i100-8.
33. Matuszewich L, Yamamoto BK. Chronic stress augments the long-term and acute effects of methamphetamine. Neuroscience 2004;124:637-46.
34. Batki SL, Harris DS. Quantitative drug levels in stimulant psychosis: relationship to symptom severity, catecholamines and hyperkinesia. Am J Addict 2004;13:461-70.
35. Suzuki A, Nakamura K, Sekine Y, et al. An association study between catechol-O-methyl transferase gene polymorphism and methamphetamine psychotic disorder. Psychiatr Genet 2006;16:133-8.
36. Sekine Y, Ouchi Y, Takei N, et al. Brain serotonin transporter density and aggression in abstinent methamphetamine abusers. Arch Gen Psychiatry 2006;63:90-100.
1. Vocci FJ, Acri J, Elkashef A. Medication development for addictive disorders: the state of the science. Am J Psychiatry 2005;162:1432-4.
2. Newton TF, Roache JD, De La Garza R, 2nd, et al. Safety of intravenous methamphetamine administration during treatment with bupropion. Psychopharmacology (Berl) 2005;182:426-35.
3. Newton TF, Roache JD, De La Garza R, et al. Bupropion reduces methamphetamine-induced subjective effects and cue-induced craving. Neuropsychopharmacology 2006;31:1537-44.
4. Ling W, Rawson R, Shoptaw S. Management of methamphetamine abuse and dependence. Curr Psychiatry Rep 2006;8:345-54.
5. Umanoff DF. Trial of modafinil for cocaine dependence. Neuropsychopharmacology 2005;30:2298; author reply 2299-300.
6. Heinzerling KG, Shoptaw S, Peck JA, et al. Randomized, placebo-controlled trial of baclofen and gabapentin for the treatment of methamphetamine dependence. Drug Alcohol Depend 2006;85:177-84.
7. Shoptaw S, Huber A, Peck J, et al. Randomized, placebo-controlled trial of sertraline and contingency management for the treatment of methamphetamine dependence. Drug Alcohol Depend 2006;85:12-8.
8. Johnson BA, Roache JD, Ait-Daoud N, et al. Effects of acute topiramate dosing on methamphetamine-induced subjective mood. Int J Neuropsychopharmacol 2007;10:85-98.
9. Bostwick J, Lineberry T. The ‘meth’ epidemic: Managing acute psychosis, agitation, and suicide risk. Current Psychiatry 2006;5(11):46-62.
10. Simon SL, Dacey J, Glynn S, et al. The effect of relapse on cognition in abstinent methamphetamine abusers. J Subst Abuse Treat 2004;27:59-66.
11. Wilson JM, Kalasinsky KS, Levey AI, et al. Striatal dopamine nerve terminal markers in human, chronic methamphetamine users. Nat Med 1996;2:699-703.
12. Moszczynska A, Fitzmaurice P, Ang L, et al. Why is parkinsonism not a feature of human methamphetamine users? Brain 2004;127:363-70.
13. Armstrong BD, Noguchi KK. The neurotoxic effects of 3,4-methylenedioxymethamphetamine (MDMA) and methamphetamine on serotonin, dopamine, and GABAergic terminals: an in-vitro autoradiographic study in rats. Neurotoxicology 2004;25:905-14.
14. London ED, Berman SM, Voytek B, et al. Cerebral metabolic dysfunction and impaired vigilance in recently abstinent methamphetamine abusers. Biol Psychiatry 2005;58:770-8.
15. London ED, Simon SL, Berman SM, et al. Mood disturbances and regional cerebral metabolic abnormalities in recently abstinent methamphetamine abusers. Arch Gen Psychiatry 2004;61:73-84.
16. Nordahl TE, Salo R, Leamon M. Neuropsychological effects of chronic methamphetamine use on neurotransmitters and cognition: a review. J Neuropsychiatry Clin Neurosci 2003;15:317-25.
17. Wang GJ, Volkow ND, Chang L, et al. Partial recovery of brain metabolism in methamphetamine abusers after protracted abstinence. Am J Psychiatry 2004;161:242-8.
18. Cherner M, Letendre S, Heaton RK, et al. Hepatitis C augments cognitive deficits associated with HIV infection and methamphetamine. Neurology 2005;64:1343-7.
19. Stoops WW. Aripiprazole as a potential pharmacotherapy for stimulant dependence: human laboratory studies with damphetamine. Exp Clin Psychopharmacol 2006;14:413-21.
20. Yen CF, Wu HY, Yen JY, Ko CH. Effects of brief cognitive-behavioral interventions on confidence to resist the urges to use heroin and methamphetamine in relapse-related situations. J Nerv Ment Dis 2004;192:788-91.
21. Roll JM, Petry NM, Stitzer ML, et al. Contingency management for the treatment of methamphetamine use disorders. Am J Psychiatry 2006;163:1993-9.
22. Shoptaw S, Klausner JD, Reback CJ, et al. A public health response to the methamphetamine epidemic: the implementation of contingency management to treat methamphetamine dependence. BMC Public Health 2006;6:214.-
23. Shoptaw S, Rawson RA, McCann MJ, Obert JL. The Matrix model of outpatient stimulant abuse treatment: evidence of efficacy. J Addict Dis 1994;13:129-41.
24. Sindelar J, Elbel B, Petry NM. What do we get for our money? Cost-effectiveness of adding contingency management. Addiction 2007;102:309-16.
25. Shoptaw S. Methamphetamine use in urban gay and bisexual populations. Top HIV Med 2006;14:84-7.
26. Bolding G, Hart G, Sherr L, Elford J. Use of crystal methamphetamine among gay men in London. Addiction 2006;101:1622-30.
27. Peck JA, Shoptaw S, Rotheram-Fuller E, et al. HIV-associated medical, behavioral, and psychiatric characteristics of treatment-seeking, methamphetamine-dependent men who have sex with men. J Addict Dis 2005;24:115-32.
28. Semple SJ, Patterson TL, Grant I. The context of sexual risk behavior among heterosexual methamphetamine users. Addict Behav 2004;29:807-10.
29. Mahajan SD, Hu Z, Reynolds JL, et al. Methamphetamine modulates gene expression patterns in monocyte derived mature dendritic cells: implications for HIV-1 pathogenesis. Mol Diagn Ther 2006;10:257-69.
30. Rawson RA, Marinelli-Casey P, Anglin MD, et al. A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction 2004;99:708-17.
31. McGregor C, Srisurapanont M, Jittiwutikarn J, et al. The nature, time course and severity of methamphetamine withdrawal. Addiction 2005;100:1320-9.
32. Peck JA, Reback CJ, Yang X, et al. Sustained reductions in drug use and depression symptoms from treatment for drug abuse in methamphetamine-dependent gay and bisexual men. J Urban Health 2005;82:i100-8.
33. Matuszewich L, Yamamoto BK. Chronic stress augments the long-term and acute effects of methamphetamine. Neuroscience 2004;124:637-46.
34. Batki SL, Harris DS. Quantitative drug levels in stimulant psychosis: relationship to symptom severity, catecholamines and hyperkinesia. Am J Addict 2004;13:461-70.
35. Suzuki A, Nakamura K, Sekine Y, et al. An association study between catechol-O-methyl transferase gene polymorphism and methamphetamine psychotic disorder. Psychiatr Genet 2006;16:133-8.
36. Sekine Y, Ouchi Y, Takei N, et al. Brain serotonin transporter density and aggression in abstinent methamphetamine abusers. Arch Gen Psychiatry 2006;63:90-100.
TRAUMATIZED TROOPS How to treat combat-related PTSD
Thousands of U.S. troops are seeking mental health care after being deployed in Iraq. Among 222,000 Army and Marine Iraq veterans, 35% sought treatment in the year after returning home—many for posttraumatic stress disorder (PTSD).In a related article, we discuss the diagnosis and treatment of military sexual trauma, a form of PTSD.
Persistent pathology
The greater the intensity of an Iraq/Afghanistan veteran’s combat experiences (“firefights”), the more likely the soldier is to develop PTSD.Traumatic brain injury: Choosing medications for neurobehavioral symptoms”). Sexual trauma also may cause or exacerbate PTSD.Military sexual trauma: How to identify and treat a unique form of PTSD”).
Table 1
3 domains of posttraumatic stress disorder symptoms
| Domain | Symptoms |
|---|---|
| Re-experiencing |
|
| Avoidance and numbing |
|
| Increased arousal |
|
| Source: DSM-IV-TR | |
FigurePTSD screen for war veterans
Source: U.S. Department of Veterans Affairs. Afghan & Iraq Post-Deployment Screen, Attachment B. Screening for risk factors associated with development of post-traumatic stress disorder (PTSD)
Cognitive therapy
Psychotherapy is the cornerstone of PTSD treatment; skilled therapists may achieve greater efficacy and more-durable results than medications do. Evidence strongly supports cognitive behavioral therapy—including exposure therapy, anxiety management, and cognitive therapy.U.S. troops returning home: Are you prepared? Current Psychiatry 2006;5(1):12-22.
- U.S. Department of Veterans Affairs. Seamless Transition Home. http://www.seamlesstransition.va.gov. Accessed March 13, 2006.
- American Psychiatric Association. Practice guideline for the treatment of acute stress disorder and posttraumatic stress disorder. http://www.psych.org/psych_pract/treatg/pg/PTSD-PG-PartsA-B-C-New.pdf.
Drug brand names
- Carbamazepine • Carbatrol
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Lithium • Lithobid, others
- Mirtazapine • Remeron
- Paroxetine • Paxil
- Prazosin • Minipress
- Sertraline • Zoloft
- Trazodone • Desyrel
- Temazepam • Restoril
- Valproic acid • Divalproex, others
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products. Drs. Lineberry, Bostwick, and Rundell served on active duty in the U.S. Air Force. Dr. Ramaswamy is staff psychiatrist, Omaha Veterans Administration. and Director of Psychopharmacology Research, Creighton University, Omaha, NE.
1. Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA 2006;295(9):1023-32.
2. Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13-22.
3. Schlenger WE, Kulka RA, Fairbank JA, et al. The prevalence of post-traumatic stress disorder in the Vietnam generation: a multimethod, multisource assessment of psychiatric disorder. J Trauma Stress 1992;5:333-63.
4. Prigerson HG, Maciejewski PK, Rosenheck RA. Combat trauma: trauma with highest risk of delayed onset and unresolved posttraumatic stress disorder symptoms, unemployment, and abuse among men. J Nerv Ment Dis 2001;189:99-108.
5. Prigerson HG, Maciejewski PK, Rosenheck RA. Population attributable fractions of psychiatric disorders and behavioral outcomes associated with combat exposures among U.S. men. Am J Public Health 2002;92(1):59-63.
6. Diagnostic and statistical manual of mental disorders (4th ed, text rev). Washington, DC: American Psychiatric Association; 2000.
7. Xydakis MS, Fravell MD, Nasser KE, Casler JD. Analysis of battlefield head and neck injuries in Iraq and Afghanistan. Otolaryngol Head Neck Surg 2005;133:497-504.
8. Okie S. Traumatic brain injury in the war zone. N Engl J Med 2005;352(20):2043-7.
9. Kang H, Dalager N, Mahan C, et al. The role of sexual assault on the risk of PTSD among Gulf War veterans. Ann Epidemiol 2005;15(3):191-5.
10. Bradley R, Greene J, Russ E, et al. A multidimensional metaanalysis of psychotherapy for posttraumatic stress disorder. Am J Psychiatry 2005;162:214-27.
11. Foa EB, Hembree EA, Cahill SP, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: outcome at academic and community clinics. J Consult Clin Psychol 2005;73:953-64.
12. Schnurr PP, Lunney CA, Sengupta A. Risk factors for the development versus maintenance of post-traumatic stress disorder. J Trauma Stress 2004;17:85-95.
13. Friedman MJ, Donnelly CL, Mellman TA. Pharmacotherapy for PTSD. Psychiatric Annals 2003;33(8):57-62.
14. Asnis GM, Kohn SR, Henderson M, Brown NL. SSRIs versus non- SSRIs in posttraumatic stress disorder: an update with recommendations. Drugs 2004;6:383-404.
15. Simon GE, Savarino J, Operskalski B, et al. Suicide risk during antidepressant treatment. Am J Psychiatry 2006;163(1):41-7.
16. Oquendo M, Brent DA, Birmaher B, et al. Posttraumatic stress disorder comorbid with major depression: factors mediating the association with suicidal behavior. Am J Psychiatry 2005;162(3):560-6.
17. Schoenfeld FB, Marmar CR, Neylan TC. Current concepts in pharmacotherapy for posttraumatic stress disorder. Psychiatr Serv 2004;55:519-31.
18. Martenyi F, Brown EB, Zhang H, et al. Fluoxetine versus placebo in posttraumatic stress disorder. J Clin Psychiatry 2002;63:199-206.
19. Brady KT, Sonne SC, Roberts JM. Sertraline treatment of comorbid posttraumatic stress disorder and alcohol dependence J Clin Psychiatry 1995;56(11):502-5.
20. Davidson JR, Rothbaum BO, van der Kolk BA, et al. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry 2001;58(5):485-92.
21. Zohar J, Amital D, Miodownik C, et al. Double-blind placebocontrolled pilot study of sertraline in military veterans with posttraumatic stress disorder J Clin Psychopharmacol 2002;22(2):190-5.
22. Marshall RD, Beebe KL, Oldham M, et al. Efficacy and safety of paroxetine treatment for chronic PTSD: a fixed-dose, placebocontrolled study. Am J Psychiatr 2001;158(12):1982-8.
23. Tucker P, Zaninelli R, Yehuda R, et al. Paroxetine in the treatment of chronic posttraumatic stress disorder: results of a placebocontrolled, flexible-dosage trial. J Clin Psychiatry 2001;62(11):860-8.
24. Raskind MA, Peskind ER, Kanter ED, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry 2003;160(2):371-3.
25. Hamner MB, Deitsch SE, Brodrick PS, et al. Quetiapine treatment in patients with posttraumatic stress disorder: an open trial of adjunctive therapy. J Clin Psychopharmacol 2003;23(1):15-20.
26. Villarreal G, Calais L, Pickard J, et al. Open-label aripiprazole monotherapy in the treatment of posttraumatic stress disorder. Poster presented at: annual meeting of the NIMH New Clinical Drug Evaluation Unit; June 6-9, 2005; Boca Raton FL.
27. Vieweg WVR, Julius DA, Fernandez A, et al. Posttraumatic stress disorder in male military veterans with comorbid overweight and obesity: Psychotropic, antihypertensive, and metabolic medications. Prim Care Companion J Clin Psychiatry 2006;8(1):
28. Stein MB, Kline NA, Matloff JL. Adjunctive olanzapine for SSRI-resistant combat-related PTSD: a double-blind, placebo-controlled study. Am J Psychiatry 2002;159(10):1777-9.
29. Kozaric-Kovacic D, Pivac N, Muck-Seler D, et al. Risperidone in psychotic combat-related posttraumatic stress disorder: an open trial. J Clin Psychiatry 2005;66(7):922-7.
30. Ahearn EP, Mussey M, Johnson C, et al. Quetiapine as an adjunctive treatment for post-traumatic stress disorder: an 8-week open-label study. Int Clin Psychopharmacol 2006;21(1):29-33.
31. Lambert MT. Aripiprazole in the management of post-traumatic stress disorder symptoms in returning Global War on Terrorism veterans. Int Clin Psychopharmacol 2006;21(3):185-7.
32. Warner MD, Dorn MR, Peabody CA. Survey on the usefulness of trazodone in patients with PTSD with insomnia or nightmares. Pharmacopsychiatry 2001;34(4):128-31.
33. Ocasio-Tascon ME, Alicea-Colon E, et al., Torres-Palacios A, et al. The veteran population: one at high risk for sleep-disordered breathing. Sleep Breath 2006 Feb 22;[Epub ahead of print].
34. Krakow B, Lowry C, Germain A, et al. A retrospective study on improvements in nightmares and post-traumatic stress disorder following treatment for co-morbid sleep-disordered breathing. J Psychosom Res 2000;49(5):291-8.
35. Forbes D, Creamer M, Hawthorne G, et al. Co-morbidity as a predictor of symptom changes after treatment in combat-related posttraumatic stress disorder. J Nerv Ment Dis 2003;191:93-9.
Thousands of U.S. troops are seeking mental health care after being deployed in Iraq. Among 222,000 Army and Marine Iraq veterans, 35% sought treatment in the year after returning home—many for posttraumatic stress disorder (PTSD).In a related article, we discuss the diagnosis and treatment of military sexual trauma, a form of PTSD.
Persistent pathology
The greater the intensity of an Iraq/Afghanistan veteran’s combat experiences (“firefights”), the more likely the soldier is to develop PTSD.Traumatic brain injury: Choosing medications for neurobehavioral symptoms”). Sexual trauma also may cause or exacerbate PTSD.Military sexual trauma: How to identify and treat a unique form of PTSD”).
Table 1
3 domains of posttraumatic stress disorder symptoms
| Domain | Symptoms |
|---|---|
| Re-experiencing |
|
| Avoidance and numbing |
|
| Increased arousal |
|
| Source: DSM-IV-TR | |
FigurePTSD screen for war veterans
Source: U.S. Department of Veterans Affairs. Afghan & Iraq Post-Deployment Screen, Attachment B. Screening for risk factors associated with development of post-traumatic stress disorder (PTSD)
Cognitive therapy
Psychotherapy is the cornerstone of PTSD treatment; skilled therapists may achieve greater efficacy and more-durable results than medications do. Evidence strongly supports cognitive behavioral therapy—including exposure therapy, anxiety management, and cognitive therapy.U.S. troops returning home: Are you prepared? Current Psychiatry 2006;5(1):12-22.
- U.S. Department of Veterans Affairs. Seamless Transition Home. http://www.seamlesstransition.va.gov. Accessed March 13, 2006.
- American Psychiatric Association. Practice guideline for the treatment of acute stress disorder and posttraumatic stress disorder. http://www.psych.org/psych_pract/treatg/pg/PTSD-PG-PartsA-B-C-New.pdf.
Drug brand names
- Carbamazepine • Carbatrol
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Lithium • Lithobid, others
- Mirtazapine • Remeron
- Paroxetine • Paxil
- Prazosin • Minipress
- Sertraline • Zoloft
- Trazodone • Desyrel
- Temazepam • Restoril
- Valproic acid • Divalproex, others
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products. Drs. Lineberry, Bostwick, and Rundell served on active duty in the U.S. Air Force. Dr. Ramaswamy is staff psychiatrist, Omaha Veterans Administration. and Director of Psychopharmacology Research, Creighton University, Omaha, NE.
Thousands of U.S. troops are seeking mental health care after being deployed in Iraq. Among 222,000 Army and Marine Iraq veterans, 35% sought treatment in the year after returning home—many for posttraumatic stress disorder (PTSD).In a related article, we discuss the diagnosis and treatment of military sexual trauma, a form of PTSD.
Persistent pathology
The greater the intensity of an Iraq/Afghanistan veteran’s combat experiences (“firefights”), the more likely the soldier is to develop PTSD.Traumatic brain injury: Choosing medications for neurobehavioral symptoms”). Sexual trauma also may cause or exacerbate PTSD.Military sexual trauma: How to identify and treat a unique form of PTSD”).
Table 1
3 domains of posttraumatic stress disorder symptoms
| Domain | Symptoms |
|---|---|
| Re-experiencing |
|
| Avoidance and numbing |
|
| Increased arousal |
|
| Source: DSM-IV-TR | |
FigurePTSD screen for war veterans
Source: U.S. Department of Veterans Affairs. Afghan & Iraq Post-Deployment Screen, Attachment B. Screening for risk factors associated with development of post-traumatic stress disorder (PTSD)
Cognitive therapy
Psychotherapy is the cornerstone of PTSD treatment; skilled therapists may achieve greater efficacy and more-durable results than medications do. Evidence strongly supports cognitive behavioral therapy—including exposure therapy, anxiety management, and cognitive therapy.U.S. troops returning home: Are you prepared? Current Psychiatry 2006;5(1):12-22.
- U.S. Department of Veterans Affairs. Seamless Transition Home. http://www.seamlesstransition.va.gov. Accessed March 13, 2006.
- American Psychiatric Association. Practice guideline for the treatment of acute stress disorder and posttraumatic stress disorder. http://www.psych.org/psych_pract/treatg/pg/PTSD-PG-PartsA-B-C-New.pdf.
Drug brand names
- Carbamazepine • Carbatrol
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Lithium • Lithobid, others
- Mirtazapine • Remeron
- Paroxetine • Paxil
- Prazosin • Minipress
- Sertraline • Zoloft
- Trazodone • Desyrel
- Temazepam • Restoril
- Valproic acid • Divalproex, others
- Venlafaxine • Effexor
- Zolpidem • Ambien
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products. Drs. Lineberry, Bostwick, and Rundell served on active duty in the U.S. Air Force. Dr. Ramaswamy is staff psychiatrist, Omaha Veterans Administration. and Director of Psychopharmacology Research, Creighton University, Omaha, NE.
1. Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA 2006;295(9):1023-32.
2. Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13-22.
3. Schlenger WE, Kulka RA, Fairbank JA, et al. The prevalence of post-traumatic stress disorder in the Vietnam generation: a multimethod, multisource assessment of psychiatric disorder. J Trauma Stress 1992;5:333-63.
4. Prigerson HG, Maciejewski PK, Rosenheck RA. Combat trauma: trauma with highest risk of delayed onset and unresolved posttraumatic stress disorder symptoms, unemployment, and abuse among men. J Nerv Ment Dis 2001;189:99-108.
5. Prigerson HG, Maciejewski PK, Rosenheck RA. Population attributable fractions of psychiatric disorders and behavioral outcomes associated with combat exposures among U.S. men. Am J Public Health 2002;92(1):59-63.
6. Diagnostic and statistical manual of mental disorders (4th ed, text rev). Washington, DC: American Psychiatric Association; 2000.
7. Xydakis MS, Fravell MD, Nasser KE, Casler JD. Analysis of battlefield head and neck injuries in Iraq and Afghanistan. Otolaryngol Head Neck Surg 2005;133:497-504.
8. Okie S. Traumatic brain injury in the war zone. N Engl J Med 2005;352(20):2043-7.
9. Kang H, Dalager N, Mahan C, et al. The role of sexual assault on the risk of PTSD among Gulf War veterans. Ann Epidemiol 2005;15(3):191-5.
10. Bradley R, Greene J, Russ E, et al. A multidimensional metaanalysis of psychotherapy for posttraumatic stress disorder. Am J Psychiatry 2005;162:214-27.
11. Foa EB, Hembree EA, Cahill SP, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: outcome at academic and community clinics. J Consult Clin Psychol 2005;73:953-64.
12. Schnurr PP, Lunney CA, Sengupta A. Risk factors for the development versus maintenance of post-traumatic stress disorder. J Trauma Stress 2004;17:85-95.
13. Friedman MJ, Donnelly CL, Mellman TA. Pharmacotherapy for PTSD. Psychiatric Annals 2003;33(8):57-62.
14. Asnis GM, Kohn SR, Henderson M, Brown NL. SSRIs versus non- SSRIs in posttraumatic stress disorder: an update with recommendations. Drugs 2004;6:383-404.
15. Simon GE, Savarino J, Operskalski B, et al. Suicide risk during antidepressant treatment. Am J Psychiatry 2006;163(1):41-7.
16. Oquendo M, Brent DA, Birmaher B, et al. Posttraumatic stress disorder comorbid with major depression: factors mediating the association with suicidal behavior. Am J Psychiatry 2005;162(3):560-6.
17. Schoenfeld FB, Marmar CR, Neylan TC. Current concepts in pharmacotherapy for posttraumatic stress disorder. Psychiatr Serv 2004;55:519-31.
18. Martenyi F, Brown EB, Zhang H, et al. Fluoxetine versus placebo in posttraumatic stress disorder. J Clin Psychiatry 2002;63:199-206.
19. Brady KT, Sonne SC, Roberts JM. Sertraline treatment of comorbid posttraumatic stress disorder and alcohol dependence J Clin Psychiatry 1995;56(11):502-5.
20. Davidson JR, Rothbaum BO, van der Kolk BA, et al. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry 2001;58(5):485-92.
21. Zohar J, Amital D, Miodownik C, et al. Double-blind placebocontrolled pilot study of sertraline in military veterans with posttraumatic stress disorder J Clin Psychopharmacol 2002;22(2):190-5.
22. Marshall RD, Beebe KL, Oldham M, et al. Efficacy and safety of paroxetine treatment for chronic PTSD: a fixed-dose, placebocontrolled study. Am J Psychiatr 2001;158(12):1982-8.
23. Tucker P, Zaninelli R, Yehuda R, et al. Paroxetine in the treatment of chronic posttraumatic stress disorder: results of a placebocontrolled, flexible-dosage trial. J Clin Psychiatry 2001;62(11):860-8.
24. Raskind MA, Peskind ER, Kanter ED, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry 2003;160(2):371-3.
25. Hamner MB, Deitsch SE, Brodrick PS, et al. Quetiapine treatment in patients with posttraumatic stress disorder: an open trial of adjunctive therapy. J Clin Psychopharmacol 2003;23(1):15-20.
26. Villarreal G, Calais L, Pickard J, et al. Open-label aripiprazole monotherapy in the treatment of posttraumatic stress disorder. Poster presented at: annual meeting of the NIMH New Clinical Drug Evaluation Unit; June 6-9, 2005; Boca Raton FL.
27. Vieweg WVR, Julius DA, Fernandez A, et al. Posttraumatic stress disorder in male military veterans with comorbid overweight and obesity: Psychotropic, antihypertensive, and metabolic medications. Prim Care Companion J Clin Psychiatry 2006;8(1):
28. Stein MB, Kline NA, Matloff JL. Adjunctive olanzapine for SSRI-resistant combat-related PTSD: a double-blind, placebo-controlled study. Am J Psychiatry 2002;159(10):1777-9.
29. Kozaric-Kovacic D, Pivac N, Muck-Seler D, et al. Risperidone in psychotic combat-related posttraumatic stress disorder: an open trial. J Clin Psychiatry 2005;66(7):922-7.
30. Ahearn EP, Mussey M, Johnson C, et al. Quetiapine as an adjunctive treatment for post-traumatic stress disorder: an 8-week open-label study. Int Clin Psychopharmacol 2006;21(1):29-33.
31. Lambert MT. Aripiprazole in the management of post-traumatic stress disorder symptoms in returning Global War on Terrorism veterans. Int Clin Psychopharmacol 2006;21(3):185-7.
32. Warner MD, Dorn MR, Peabody CA. Survey on the usefulness of trazodone in patients with PTSD with insomnia or nightmares. Pharmacopsychiatry 2001;34(4):128-31.
33. Ocasio-Tascon ME, Alicea-Colon E, et al., Torres-Palacios A, et al. The veteran population: one at high risk for sleep-disordered breathing. Sleep Breath 2006 Feb 22;[Epub ahead of print].
34. Krakow B, Lowry C, Germain A, et al. A retrospective study on improvements in nightmares and post-traumatic stress disorder following treatment for co-morbid sleep-disordered breathing. J Psychosom Res 2000;49(5):291-8.
35. Forbes D, Creamer M, Hawthorne G, et al. Co-morbidity as a predictor of symptom changes after treatment in combat-related posttraumatic stress disorder. J Nerv Ment Dis 2003;191:93-9.
1. Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA 2006;295(9):1023-32.
2. Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13-22.
3. Schlenger WE, Kulka RA, Fairbank JA, et al. The prevalence of post-traumatic stress disorder in the Vietnam generation: a multimethod, multisource assessment of psychiatric disorder. J Trauma Stress 1992;5:333-63.
4. Prigerson HG, Maciejewski PK, Rosenheck RA. Combat trauma: trauma with highest risk of delayed onset and unresolved posttraumatic stress disorder symptoms, unemployment, and abuse among men. J Nerv Ment Dis 2001;189:99-108.
5. Prigerson HG, Maciejewski PK, Rosenheck RA. Population attributable fractions of psychiatric disorders and behavioral outcomes associated with combat exposures among U.S. men. Am J Public Health 2002;92(1):59-63.
6. Diagnostic and statistical manual of mental disorders (4th ed, text rev). Washington, DC: American Psychiatric Association; 2000.
7. Xydakis MS, Fravell MD, Nasser KE, Casler JD. Analysis of battlefield head and neck injuries in Iraq and Afghanistan. Otolaryngol Head Neck Surg 2005;133:497-504.
8. Okie S. Traumatic brain injury in the war zone. N Engl J Med 2005;352(20):2043-7.
9. Kang H, Dalager N, Mahan C, et al. The role of sexual assault on the risk of PTSD among Gulf War veterans. Ann Epidemiol 2005;15(3):191-5.
10. Bradley R, Greene J, Russ E, et al. A multidimensional metaanalysis of psychotherapy for posttraumatic stress disorder. Am J Psychiatry 2005;162:214-27.
11. Foa EB, Hembree EA, Cahill SP, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: outcome at academic and community clinics. J Consult Clin Psychol 2005;73:953-64.
12. Schnurr PP, Lunney CA, Sengupta A. Risk factors for the development versus maintenance of post-traumatic stress disorder. J Trauma Stress 2004;17:85-95.
13. Friedman MJ, Donnelly CL, Mellman TA. Pharmacotherapy for PTSD. Psychiatric Annals 2003;33(8):57-62.
14. Asnis GM, Kohn SR, Henderson M, Brown NL. SSRIs versus non- SSRIs in posttraumatic stress disorder: an update with recommendations. Drugs 2004;6:383-404.
15. Simon GE, Savarino J, Operskalski B, et al. Suicide risk during antidepressant treatment. Am J Psychiatry 2006;163(1):41-7.
16. Oquendo M, Brent DA, Birmaher B, et al. Posttraumatic stress disorder comorbid with major depression: factors mediating the association with suicidal behavior. Am J Psychiatry 2005;162(3):560-6.
17. Schoenfeld FB, Marmar CR, Neylan TC. Current concepts in pharmacotherapy for posttraumatic stress disorder. Psychiatr Serv 2004;55:519-31.
18. Martenyi F, Brown EB, Zhang H, et al. Fluoxetine versus placebo in posttraumatic stress disorder. J Clin Psychiatry 2002;63:199-206.
19. Brady KT, Sonne SC, Roberts JM. Sertraline treatment of comorbid posttraumatic stress disorder and alcohol dependence J Clin Psychiatry 1995;56(11):502-5.
20. Davidson JR, Rothbaum BO, van der Kolk BA, et al. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry 2001;58(5):485-92.
21. Zohar J, Amital D, Miodownik C, et al. Double-blind placebocontrolled pilot study of sertraline in military veterans with posttraumatic stress disorder J Clin Psychopharmacol 2002;22(2):190-5.
22. Marshall RD, Beebe KL, Oldham M, et al. Efficacy and safety of paroxetine treatment for chronic PTSD: a fixed-dose, placebocontrolled study. Am J Psychiatr 2001;158(12):1982-8.
23. Tucker P, Zaninelli R, Yehuda R, et al. Paroxetine in the treatment of chronic posttraumatic stress disorder: results of a placebocontrolled, flexible-dosage trial. J Clin Psychiatry 2001;62(11):860-8.
24. Raskind MA, Peskind ER, Kanter ED, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry 2003;160(2):371-3.
25. Hamner MB, Deitsch SE, Brodrick PS, et al. Quetiapine treatment in patients with posttraumatic stress disorder: an open trial of adjunctive therapy. J Clin Psychopharmacol 2003;23(1):15-20.
26. Villarreal G, Calais L, Pickard J, et al. Open-label aripiprazole monotherapy in the treatment of posttraumatic stress disorder. Poster presented at: annual meeting of the NIMH New Clinical Drug Evaluation Unit; June 6-9, 2005; Boca Raton FL.
27. Vieweg WVR, Julius DA, Fernandez A, et al. Posttraumatic stress disorder in male military veterans with comorbid overweight and obesity: Psychotropic, antihypertensive, and metabolic medications. Prim Care Companion J Clin Psychiatry 2006;8(1):
28. Stein MB, Kline NA, Matloff JL. Adjunctive olanzapine for SSRI-resistant combat-related PTSD: a double-blind, placebo-controlled study. Am J Psychiatry 2002;159(10):1777-9.
29. Kozaric-Kovacic D, Pivac N, Muck-Seler D, et al. Risperidone in psychotic combat-related posttraumatic stress disorder: an open trial. J Clin Psychiatry 2005;66(7):922-7.
30. Ahearn EP, Mussey M, Johnson C, et al. Quetiapine as an adjunctive treatment for post-traumatic stress disorder: an 8-week open-label study. Int Clin Psychopharmacol 2006;21(1):29-33.
31. Lambert MT. Aripiprazole in the management of post-traumatic stress disorder symptoms in returning Global War on Terrorism veterans. Int Clin Psychopharmacol 2006;21(3):185-7.
32. Warner MD, Dorn MR, Peabody CA. Survey on the usefulness of trazodone in patients with PTSD with insomnia or nightmares. Pharmacopsychiatry 2001;34(4):128-31.
33. Ocasio-Tascon ME, Alicea-Colon E, et al., Torres-Palacios A, et al. The veteran population: one at high risk for sleep-disordered breathing. Sleep Breath 2006 Feb 22;[Epub ahead of print].
34. Krakow B, Lowry C, Germain A, et al. A retrospective study on improvements in nightmares and post-traumatic stress disorder following treatment for co-morbid sleep-disordered breathing. J Psychosom Res 2000;49(5):291-8.
35. Forbes D, Creamer M, Hawthorne G, et al. Co-morbidity as a predictor of symptom changes after treatment in combat-related posttraumatic stress disorder. J Nerv Ment Dis 2003;191:93-9.
Is your patient making the ‘wrong’ treatment choice?
Consultation/liaison (C/L) psychiatrists assess capacity in 1 of 6 consults,1 and these evaluations must be quick but systematic. Hospital time is precious, and asking for a psychiatry consult inevitably slows down the medical team’s efforts to care for sick or injured patients.
We suggest an approach our C/L service developed to rapidly weigh capacity’s three dimensions—risks, benefits, and patient decisions—to formulate appropriate opinions for the medical team.
A standard for capacity
In most cases, capacity must be assessed and considered adequate before a patient can provide informed consent for a medical intervention. Because a patient might be capable of making some decisions but not others, the standard for determining capacity is not black and white but a sliding scale that depends on the magnitude of the decision being made.
As physicians, psychiatrists understand doctors’ frustrations when they believe a patient is making the wrong treatment choice. When the primary team turns to us, they want us to help determine the most appropriate course of action.
Capacity is determined by weighing whether the patient is competent to exercise his or her autonomy in making a decision about medical treatment. We do not assess global capacity; the goal is to provide an unbiased opinion about specific capacity for a given situation–“Does Mr. X have the ability to accept/refuse this treatment option presented to him?”
Capacity’s three dimensions. The means to achieve this goal are often complex. Roth et al2 proposed that capacity could be measured on a sliding scale. Wise and Rundell3 agreed and developed a two-dimension table to show that capacity can be evaluated at different thresholds, depending on the patient’s clinical situation. We expanded this model (Figure) to include three dimensions to consider when you evaluate capacity:
- risk of the proposed treatment (high vs. low)
- benefit of the treatment (high vs. low)
- the patient’s decision about the treatment (accept vs. refuse).
If a treatment’s benefits far outweigh the risks and the patient accepts that treatment, he is probably capable of making that decision and a lenient (low) threshold to establish capacity applies. If the same patient refuses the high-benefit, low-risk treatment, then he might be incapable of making that decision and a stringent (high) threshold to establish capacity comes into play. Our C/L service often uses this model when discussing capacity evaluations with the primary team. It explains why some capacity evaluations—when a patient agrees to a low-risk, high-benefit procedure—might take minutes, whereas others—those that fall into the medium threshold for capacity—take hours. Consider the following cases.
Figure 3-dimension model for evaluating capacity
Three cases: Is capacity evaluation needed?
Mr. X, age 25, was in a motor vehicle accident that caused trauma to his esophagus. He requires a feeding tube because he will be unable to eat for several weeks. The risk of the procedure (feeding tube placement) is low, and the benefit (getting possibly life-saving nutrition) is high.
If Mr. X refuses the feeding tube, he may be incapable of making this decision and would require a rigorous capacity evaluation (high-threshold capacity). If he consents, he is making a choice with which most reasonable people would agree, and establishing capacity would be less important (low-threshold capacity).
Mr. J, age 95, has congestive heart failure, diabetes, and liver disease. If he consents to a liver transplant—a treatment likely to be low-benefit and high-risk—he would require a rigorous capacity evaluation. If he refuses this surgical intervention, then more-lenient capacity criteria would apply.
Mrs. F, age 59, has breast cancer with metastases. Her oncologist is recommending bilateral mastectomy, radiation, chemotherapy, and an experimental treatment that has shown favorable results. The risk of treatment is high, and the benefit is unknown but most likely high. Since this is a high-risk, high-benefit intervention, the capacity threshold is medium. Whether she consents to or refuses treatment, you must weigh risks and benefits very carefully with her.
The primary team’s role
A common myth holds that only psychiatrists can determine capacity, but any physician can.4 The primary team may feel comfortable deciding a patient’s capacity without seeking consultation after asking the screening questions in Table 1.5,6 A patient who gives consistent and appropriate answers to these screening questions usually also can answer the more detailed questions psychiatrists would ask and thus has sufficient capacity.
When uncertainties remain after screening, we recommend that the primary team ask psychiatry for an opinion. Knowing what the primary team is thinking about a difficult case often helps the psychiatric consultant. So when consulting with psychiatry, we suggest that the primary team:
- clarify the question (such as, “Does Mrs. Z have the capacity to refuse dialysis?”)
- give an opinion about whether the patient does or does not have capacity and why.
When sharing of opinions was studied at institutions trying this idea, C/L teams agreed with the primary teams’ initial impression of patients’ capacity 80% of the time.4 Most consults occurred because the patient was refusing an intervention the primary team felt was “essential,” or the patient and primary team disagreed on code status. At our institution, anecdotal evidence shows that if the primary team spends a few minutes asking screening questions, the C/L service and primary team agree on the patient’s capacity >90% of the time.
Table 1
Primary team capacity evaluation: 5 W’s
Explain to the patient the treatment you recommend. Review risks and benefits of accepting and of refusing the treatment. Describe alternatives. Then ask these screening questions to assess capacity:
|
| Source: References 5,6 |
Tips for the psychiatrist
C/L psychiatrists are usually asked to evaluate capacity in complicated cases, such as when the:
- family disagrees with the patient’s decision
- patient changes his mind several times
- patient has a formidable psychiatric history.
Determining capacity requires that you assess the patient’s ability to communicate choices, understand and retain information about his condition and proposed treatment, appreciate likely consequences, and rationally manipulate information (Table 2).7
You can often gauge a patient’s attitude the moment you walk into his or her room. Those who feel insulted or defensive about being evaluated by a psychiatrist say things like:
- “I’m not crazy; I don’t need to talk to you.”
- “I think you need to evaluate my doctors, not me.”
- “Why is it so hard to believe that I’m ready to die? You can’t change my mind. Get out!”
To put the patient at ease, consider an inoffensive introduction such as: “My name is Dr. Y and I’m one of the psychiatrists who work here. I’m often called by the primary team to help explain the pros and cons of the various treatments we can provide to you. I’m not here to change your mind; I just want to make sure you are aware of all your options.”
Table 2
Psychiatry C/L service capacity evaluation
Ability to communicate choices
|
Ability to understand information about a treatment
|
Appreciation of likely consequences
|
Rational manipulation of information
|
| Source: References 5,6 |
Is it ever ok not to assess capacity?
In rare situations, informed consent does not need to be pursued and neither does capacity. Informed consent occurs when a capable patient receives adequate information to make a decision and voluntarily consents to the proposed intervention.8 Informed consent is not required in emergency, patient waiver, or therapeutic privilege situations.8,9
Emergency exception is permitted if the patient lacks the capacity to consent and the harm of postponing therapy is imminent and outweighs the proposed intervention’s risks. These cases are usually life-threatening situations in the emergency department, such as when a patient suffers severe physical trauma in a motor vehicle accident and is unable to communicate. Although capacity cannot be established, patients are taken immediately to the operating room.
If a patient with capacity refuses emergent treatment, however, the treating physician cannot override the patient’s wishes simply because it is an emergency. For example:
Mrs. L, age 32, lost several liters of blood during a complicated vaginal delivery. Her obstetrician felt she needed an emergent blood transfusion to avoid further medical complications. Mrs. L—a Jehovah’s Witness—refused the transfusion because of her religious beliefs. She was deemed capable of making this decision, and the transfusion was deferred.8-10
Patient waiver applies when a patient does not want to know all the relevant information about a procedure; he or she may wish for the physician (or another person) to make decisions.
Therapeutic privilege, a controversial idea, allows the physician to make decisions for the patient without informed consent when the physician believes the risk of giving pertinent information poses a serious detriment to the patient. In the rare cases when this is invoked, obtain family input if possible. For example:
Mrs. J, age 70, has severe health anxiety. When the primary care physician she has seen for 30 years tries to discuss treatments with her, Mrs. J fixates on potential harms and refuses treatments with even minimal risk. Her doctor tells her that it may be in her best interest to not hear the risks of treatment. Mrs. J agrees and gives her doctor permission to discusses treatment risks and benefits with her daughter, who is intricately involved in her mother’s health care.
Related resources
- Harvard Medical School department of psychiatry. Web site on forensic psychiatry and medicine. www.forensic-psych.com.
- Stern TA, Fricchione GL, Cassem, NH, et al (eds). Massachusetts General Hospital handbook of general hospital psychiatry (5th ed). Philadelphia: CV Mosby; 2004:355-9.
1. Viswanathan R, Schindler B, Brendel RW, et al. Should APM develop practice guidelines for decisional capacity assessments in the medical setting? Presented at: Annual Meeting of the Academy of Psychosomatic Medicine; November 16-20, 2005; Santa Ana Pueblo, NM.
2. Roth LH, Meisel A, Lidz CW. Tests of competency to consent to treatment. Am J Psychiatry 1977;124:279-84.
3. Wise MG, Rundell JR. Medicolegal issues in consultation. In: Clinical manual of psychosomatic medicine: a guide to consultation-liaison psychiatry. Arlington, VA: American Psychiatric Publishing; 2005:254-67.
4. Muskin PR, Kornfeld DS, Aladjem A, Tahil F. Determining capacity: Is it just capacity? Plenary workshop at: Annual Meeting of the Academy of Psychosomatic Medicine; November 16-20, 2005; Santa Ana Pueblo, NM.
5. Malin PJ. Creighton University. Educational handout (adapted with permission).
6. Poole K, Singh M, Murphy J. Law and medicine: the dilemmas of capacity, consultation/liaison psychiatry. Presented at: The Mayo Clinic; February 15, 2001; Rochester, MN.
7. Grisso T, Appelbaum PS. Assessing competence to consent to treatment: A guide for physicians and other health professionals. New York: Oxford University Press; 1998.
8. Nora LM, Benvenuti RJ. Iatrogenic disorders: medicolegal aspects of informed consent. Neurol Clin 1998;16:207-16.
9. Coulson KM, Glasser BL, Liang BA. Informed consent: issues for providers. Hematol Oncol Clin North Am 2002;16:1365-80.
10. Magid M, Reichenberg JS, Philbrick KL. To cut or not to cut: that was the question. Poster presented at: Meeting of the American Academy of Psychiatry and the Law; October 2005; Montreal, Canada.
Consultation/liaison (C/L) psychiatrists assess capacity in 1 of 6 consults,1 and these evaluations must be quick but systematic. Hospital time is precious, and asking for a psychiatry consult inevitably slows down the medical team’s efforts to care for sick or injured patients.
We suggest an approach our C/L service developed to rapidly weigh capacity’s three dimensions—risks, benefits, and patient decisions—to formulate appropriate opinions for the medical team.
A standard for capacity
In most cases, capacity must be assessed and considered adequate before a patient can provide informed consent for a medical intervention. Because a patient might be capable of making some decisions but not others, the standard for determining capacity is not black and white but a sliding scale that depends on the magnitude of the decision being made.
As physicians, psychiatrists understand doctors’ frustrations when they believe a patient is making the wrong treatment choice. When the primary team turns to us, they want us to help determine the most appropriate course of action.
Capacity is determined by weighing whether the patient is competent to exercise his or her autonomy in making a decision about medical treatment. We do not assess global capacity; the goal is to provide an unbiased opinion about specific capacity for a given situation–“Does Mr. X have the ability to accept/refuse this treatment option presented to him?”
Capacity’s three dimensions. The means to achieve this goal are often complex. Roth et al2 proposed that capacity could be measured on a sliding scale. Wise and Rundell3 agreed and developed a two-dimension table to show that capacity can be evaluated at different thresholds, depending on the patient’s clinical situation. We expanded this model (Figure) to include three dimensions to consider when you evaluate capacity:
- risk of the proposed treatment (high vs. low)
- benefit of the treatment (high vs. low)
- the patient’s decision about the treatment (accept vs. refuse).
If a treatment’s benefits far outweigh the risks and the patient accepts that treatment, he is probably capable of making that decision and a lenient (low) threshold to establish capacity applies. If the same patient refuses the high-benefit, low-risk treatment, then he might be incapable of making that decision and a stringent (high) threshold to establish capacity comes into play. Our C/L service often uses this model when discussing capacity evaluations with the primary team. It explains why some capacity evaluations—when a patient agrees to a low-risk, high-benefit procedure—might take minutes, whereas others—those that fall into the medium threshold for capacity—take hours. Consider the following cases.
Figure 3-dimension model for evaluating capacity
Three cases: Is capacity evaluation needed?
Mr. X, age 25, was in a motor vehicle accident that caused trauma to his esophagus. He requires a feeding tube because he will be unable to eat for several weeks. The risk of the procedure (feeding tube placement) is low, and the benefit (getting possibly life-saving nutrition) is high.
If Mr. X refuses the feeding tube, he may be incapable of making this decision and would require a rigorous capacity evaluation (high-threshold capacity). If he consents, he is making a choice with which most reasonable people would agree, and establishing capacity would be less important (low-threshold capacity).
Mr. J, age 95, has congestive heart failure, diabetes, and liver disease. If he consents to a liver transplant—a treatment likely to be low-benefit and high-risk—he would require a rigorous capacity evaluation. If he refuses this surgical intervention, then more-lenient capacity criteria would apply.
Mrs. F, age 59, has breast cancer with metastases. Her oncologist is recommending bilateral mastectomy, radiation, chemotherapy, and an experimental treatment that has shown favorable results. The risk of treatment is high, and the benefit is unknown but most likely high. Since this is a high-risk, high-benefit intervention, the capacity threshold is medium. Whether she consents to or refuses treatment, you must weigh risks and benefits very carefully with her.
The primary team’s role
A common myth holds that only psychiatrists can determine capacity, but any physician can.4 The primary team may feel comfortable deciding a patient’s capacity without seeking consultation after asking the screening questions in Table 1.5,6 A patient who gives consistent and appropriate answers to these screening questions usually also can answer the more detailed questions psychiatrists would ask and thus has sufficient capacity.
When uncertainties remain after screening, we recommend that the primary team ask psychiatry for an opinion. Knowing what the primary team is thinking about a difficult case often helps the psychiatric consultant. So when consulting with psychiatry, we suggest that the primary team:
- clarify the question (such as, “Does Mrs. Z have the capacity to refuse dialysis?”)
- give an opinion about whether the patient does or does not have capacity and why.
When sharing of opinions was studied at institutions trying this idea, C/L teams agreed with the primary teams’ initial impression of patients’ capacity 80% of the time.4 Most consults occurred because the patient was refusing an intervention the primary team felt was “essential,” or the patient and primary team disagreed on code status. At our institution, anecdotal evidence shows that if the primary team spends a few minutes asking screening questions, the C/L service and primary team agree on the patient’s capacity >90% of the time.
Table 1
Primary team capacity evaluation: 5 W’s
Explain to the patient the treatment you recommend. Review risks and benefits of accepting and of refusing the treatment. Describe alternatives. Then ask these screening questions to assess capacity:
|
| Source: References 5,6 |
Tips for the psychiatrist
C/L psychiatrists are usually asked to evaluate capacity in complicated cases, such as when the:
- family disagrees with the patient’s decision
- patient changes his mind several times
- patient has a formidable psychiatric history.
Determining capacity requires that you assess the patient’s ability to communicate choices, understand and retain information about his condition and proposed treatment, appreciate likely consequences, and rationally manipulate information (Table 2).7
You can often gauge a patient’s attitude the moment you walk into his or her room. Those who feel insulted or defensive about being evaluated by a psychiatrist say things like:
- “I’m not crazy; I don’t need to talk to you.”
- “I think you need to evaluate my doctors, not me.”
- “Why is it so hard to believe that I’m ready to die? You can’t change my mind. Get out!”
To put the patient at ease, consider an inoffensive introduction such as: “My name is Dr. Y and I’m one of the psychiatrists who work here. I’m often called by the primary team to help explain the pros and cons of the various treatments we can provide to you. I’m not here to change your mind; I just want to make sure you are aware of all your options.”
Table 2
Psychiatry C/L service capacity evaluation
Ability to communicate choices
|
Ability to understand information about a treatment
|
Appreciation of likely consequences
|
Rational manipulation of information
|
| Source: References 5,6 |
Is it ever ok not to assess capacity?
In rare situations, informed consent does not need to be pursued and neither does capacity. Informed consent occurs when a capable patient receives adequate information to make a decision and voluntarily consents to the proposed intervention.8 Informed consent is not required in emergency, patient waiver, or therapeutic privilege situations.8,9
Emergency exception is permitted if the patient lacks the capacity to consent and the harm of postponing therapy is imminent and outweighs the proposed intervention’s risks. These cases are usually life-threatening situations in the emergency department, such as when a patient suffers severe physical trauma in a motor vehicle accident and is unable to communicate. Although capacity cannot be established, patients are taken immediately to the operating room.
If a patient with capacity refuses emergent treatment, however, the treating physician cannot override the patient’s wishes simply because it is an emergency. For example:
Mrs. L, age 32, lost several liters of blood during a complicated vaginal delivery. Her obstetrician felt she needed an emergent blood transfusion to avoid further medical complications. Mrs. L—a Jehovah’s Witness—refused the transfusion because of her religious beliefs. She was deemed capable of making this decision, and the transfusion was deferred.8-10
Patient waiver applies when a patient does not want to know all the relevant information about a procedure; he or she may wish for the physician (or another person) to make decisions.
Therapeutic privilege, a controversial idea, allows the physician to make decisions for the patient without informed consent when the physician believes the risk of giving pertinent information poses a serious detriment to the patient. In the rare cases when this is invoked, obtain family input if possible. For example:
Mrs. J, age 70, has severe health anxiety. When the primary care physician she has seen for 30 years tries to discuss treatments with her, Mrs. J fixates on potential harms and refuses treatments with even minimal risk. Her doctor tells her that it may be in her best interest to not hear the risks of treatment. Mrs. J agrees and gives her doctor permission to discusses treatment risks and benefits with her daughter, who is intricately involved in her mother’s health care.
Related resources
- Harvard Medical School department of psychiatry. Web site on forensic psychiatry and medicine. www.forensic-psych.com.
- Stern TA, Fricchione GL, Cassem, NH, et al (eds). Massachusetts General Hospital handbook of general hospital psychiatry (5th ed). Philadelphia: CV Mosby; 2004:355-9.
Consultation/liaison (C/L) psychiatrists assess capacity in 1 of 6 consults,1 and these evaluations must be quick but systematic. Hospital time is precious, and asking for a psychiatry consult inevitably slows down the medical team’s efforts to care for sick or injured patients.
We suggest an approach our C/L service developed to rapidly weigh capacity’s three dimensions—risks, benefits, and patient decisions—to formulate appropriate opinions for the medical team.
A standard for capacity
In most cases, capacity must be assessed and considered adequate before a patient can provide informed consent for a medical intervention. Because a patient might be capable of making some decisions but not others, the standard for determining capacity is not black and white but a sliding scale that depends on the magnitude of the decision being made.
As physicians, psychiatrists understand doctors’ frustrations when they believe a patient is making the wrong treatment choice. When the primary team turns to us, they want us to help determine the most appropriate course of action.
Capacity is determined by weighing whether the patient is competent to exercise his or her autonomy in making a decision about medical treatment. We do not assess global capacity; the goal is to provide an unbiased opinion about specific capacity for a given situation–“Does Mr. X have the ability to accept/refuse this treatment option presented to him?”
Capacity’s three dimensions. The means to achieve this goal are often complex. Roth et al2 proposed that capacity could be measured on a sliding scale. Wise and Rundell3 agreed and developed a two-dimension table to show that capacity can be evaluated at different thresholds, depending on the patient’s clinical situation. We expanded this model (Figure) to include three dimensions to consider when you evaluate capacity:
- risk of the proposed treatment (high vs. low)
- benefit of the treatment (high vs. low)
- the patient’s decision about the treatment (accept vs. refuse).
If a treatment’s benefits far outweigh the risks and the patient accepts that treatment, he is probably capable of making that decision and a lenient (low) threshold to establish capacity applies. If the same patient refuses the high-benefit, low-risk treatment, then he might be incapable of making that decision and a stringent (high) threshold to establish capacity comes into play. Our C/L service often uses this model when discussing capacity evaluations with the primary team. It explains why some capacity evaluations—when a patient agrees to a low-risk, high-benefit procedure—might take minutes, whereas others—those that fall into the medium threshold for capacity—take hours. Consider the following cases.
Figure 3-dimension model for evaluating capacity
Three cases: Is capacity evaluation needed?
Mr. X, age 25, was in a motor vehicle accident that caused trauma to his esophagus. He requires a feeding tube because he will be unable to eat for several weeks. The risk of the procedure (feeding tube placement) is low, and the benefit (getting possibly life-saving nutrition) is high.
If Mr. X refuses the feeding tube, he may be incapable of making this decision and would require a rigorous capacity evaluation (high-threshold capacity). If he consents, he is making a choice with which most reasonable people would agree, and establishing capacity would be less important (low-threshold capacity).
Mr. J, age 95, has congestive heart failure, diabetes, and liver disease. If he consents to a liver transplant—a treatment likely to be low-benefit and high-risk—he would require a rigorous capacity evaluation. If he refuses this surgical intervention, then more-lenient capacity criteria would apply.
Mrs. F, age 59, has breast cancer with metastases. Her oncologist is recommending bilateral mastectomy, radiation, chemotherapy, and an experimental treatment that has shown favorable results. The risk of treatment is high, and the benefit is unknown but most likely high. Since this is a high-risk, high-benefit intervention, the capacity threshold is medium. Whether she consents to or refuses treatment, you must weigh risks and benefits very carefully with her.
The primary team’s role
A common myth holds that only psychiatrists can determine capacity, but any physician can.4 The primary team may feel comfortable deciding a patient’s capacity without seeking consultation after asking the screening questions in Table 1.5,6 A patient who gives consistent and appropriate answers to these screening questions usually also can answer the more detailed questions psychiatrists would ask and thus has sufficient capacity.
When uncertainties remain after screening, we recommend that the primary team ask psychiatry for an opinion. Knowing what the primary team is thinking about a difficult case often helps the psychiatric consultant. So when consulting with psychiatry, we suggest that the primary team:
- clarify the question (such as, “Does Mrs. Z have the capacity to refuse dialysis?”)
- give an opinion about whether the patient does or does not have capacity and why.
When sharing of opinions was studied at institutions trying this idea, C/L teams agreed with the primary teams’ initial impression of patients’ capacity 80% of the time.4 Most consults occurred because the patient was refusing an intervention the primary team felt was “essential,” or the patient and primary team disagreed on code status. At our institution, anecdotal evidence shows that if the primary team spends a few minutes asking screening questions, the C/L service and primary team agree on the patient’s capacity >90% of the time.
Table 1
Primary team capacity evaluation: 5 W’s
Explain to the patient the treatment you recommend. Review risks and benefits of accepting and of refusing the treatment. Describe alternatives. Then ask these screening questions to assess capacity:
|
| Source: References 5,6 |
Tips for the psychiatrist
C/L psychiatrists are usually asked to evaluate capacity in complicated cases, such as when the:
- family disagrees with the patient’s decision
- patient changes his mind several times
- patient has a formidable psychiatric history.
Determining capacity requires that you assess the patient’s ability to communicate choices, understand and retain information about his condition and proposed treatment, appreciate likely consequences, and rationally manipulate information (Table 2).7
You can often gauge a patient’s attitude the moment you walk into his or her room. Those who feel insulted or defensive about being evaluated by a psychiatrist say things like:
- “I’m not crazy; I don’t need to talk to you.”
- “I think you need to evaluate my doctors, not me.”
- “Why is it so hard to believe that I’m ready to die? You can’t change my mind. Get out!”
To put the patient at ease, consider an inoffensive introduction such as: “My name is Dr. Y and I’m one of the psychiatrists who work here. I’m often called by the primary team to help explain the pros and cons of the various treatments we can provide to you. I’m not here to change your mind; I just want to make sure you are aware of all your options.”
Table 2
Psychiatry C/L service capacity evaluation
Ability to communicate choices
|
Ability to understand information about a treatment
|
Appreciation of likely consequences
|
Rational manipulation of information
|
| Source: References 5,6 |
Is it ever ok not to assess capacity?
In rare situations, informed consent does not need to be pursued and neither does capacity. Informed consent occurs when a capable patient receives adequate information to make a decision and voluntarily consents to the proposed intervention.8 Informed consent is not required in emergency, patient waiver, or therapeutic privilege situations.8,9
Emergency exception is permitted if the patient lacks the capacity to consent and the harm of postponing therapy is imminent and outweighs the proposed intervention’s risks. These cases are usually life-threatening situations in the emergency department, such as when a patient suffers severe physical trauma in a motor vehicle accident and is unable to communicate. Although capacity cannot be established, patients are taken immediately to the operating room.
If a patient with capacity refuses emergent treatment, however, the treating physician cannot override the patient’s wishes simply because it is an emergency. For example:
Mrs. L, age 32, lost several liters of blood during a complicated vaginal delivery. Her obstetrician felt she needed an emergent blood transfusion to avoid further medical complications. Mrs. L—a Jehovah’s Witness—refused the transfusion because of her religious beliefs. She was deemed capable of making this decision, and the transfusion was deferred.8-10
Patient waiver applies when a patient does not want to know all the relevant information about a procedure; he or she may wish for the physician (or another person) to make decisions.
Therapeutic privilege, a controversial idea, allows the physician to make decisions for the patient without informed consent when the physician believes the risk of giving pertinent information poses a serious detriment to the patient. In the rare cases when this is invoked, obtain family input if possible. For example:
Mrs. J, age 70, has severe health anxiety. When the primary care physician she has seen for 30 years tries to discuss treatments with her, Mrs. J fixates on potential harms and refuses treatments with even minimal risk. Her doctor tells her that it may be in her best interest to not hear the risks of treatment. Mrs. J agrees and gives her doctor permission to discusses treatment risks and benefits with her daughter, who is intricately involved in her mother’s health care.
Related resources
- Harvard Medical School department of psychiatry. Web site on forensic psychiatry and medicine. www.forensic-psych.com.
- Stern TA, Fricchione GL, Cassem, NH, et al (eds). Massachusetts General Hospital handbook of general hospital psychiatry (5th ed). Philadelphia: CV Mosby; 2004:355-9.
1. Viswanathan R, Schindler B, Brendel RW, et al. Should APM develop practice guidelines for decisional capacity assessments in the medical setting? Presented at: Annual Meeting of the Academy of Psychosomatic Medicine; November 16-20, 2005; Santa Ana Pueblo, NM.
2. Roth LH, Meisel A, Lidz CW. Tests of competency to consent to treatment. Am J Psychiatry 1977;124:279-84.
3. Wise MG, Rundell JR. Medicolegal issues in consultation. In: Clinical manual of psychosomatic medicine: a guide to consultation-liaison psychiatry. Arlington, VA: American Psychiatric Publishing; 2005:254-67.
4. Muskin PR, Kornfeld DS, Aladjem A, Tahil F. Determining capacity: Is it just capacity? Plenary workshop at: Annual Meeting of the Academy of Psychosomatic Medicine; November 16-20, 2005; Santa Ana Pueblo, NM.
5. Malin PJ. Creighton University. Educational handout (adapted with permission).
6. Poole K, Singh M, Murphy J. Law and medicine: the dilemmas of capacity, consultation/liaison psychiatry. Presented at: The Mayo Clinic; February 15, 2001; Rochester, MN.
7. Grisso T, Appelbaum PS. Assessing competence to consent to treatment: A guide for physicians and other health professionals. New York: Oxford University Press; 1998.
8. Nora LM, Benvenuti RJ. Iatrogenic disorders: medicolegal aspects of informed consent. Neurol Clin 1998;16:207-16.
9. Coulson KM, Glasser BL, Liang BA. Informed consent: issues for providers. Hematol Oncol Clin North Am 2002;16:1365-80.
10. Magid M, Reichenberg JS, Philbrick KL. To cut or not to cut: that was the question. Poster presented at: Meeting of the American Academy of Psychiatry and the Law; October 2005; Montreal, Canada.
1. Viswanathan R, Schindler B, Brendel RW, et al. Should APM develop practice guidelines for decisional capacity assessments in the medical setting? Presented at: Annual Meeting of the Academy of Psychosomatic Medicine; November 16-20, 2005; Santa Ana Pueblo, NM.
2. Roth LH, Meisel A, Lidz CW. Tests of competency to consent to treatment. Am J Psychiatry 1977;124:279-84.
3. Wise MG, Rundell JR. Medicolegal issues in consultation. In: Clinical manual of psychosomatic medicine: a guide to consultation-liaison psychiatry. Arlington, VA: American Psychiatric Publishing; 2005:254-67.
4. Muskin PR, Kornfeld DS, Aladjem A, Tahil F. Determining capacity: Is it just capacity? Plenary workshop at: Annual Meeting of the Academy of Psychosomatic Medicine; November 16-20, 2005; Santa Ana Pueblo, NM.
5. Malin PJ. Creighton University. Educational handout (adapted with permission).
6. Poole K, Singh M, Murphy J. Law and medicine: the dilemmas of capacity, consultation/liaison psychiatry. Presented at: The Mayo Clinic; February 15, 2001; Rochester, MN.
7. Grisso T, Appelbaum PS. Assessing competence to consent to treatment: A guide for physicians and other health professionals. New York: Oxford University Press; 1998.
8. Nora LM, Benvenuti RJ. Iatrogenic disorders: medicolegal aspects of informed consent. Neurol Clin 1998;16:207-16.
9. Coulson KM, Glasser BL, Liang BA. Informed consent: issues for providers. Hematol Oncol Clin North Am 2002;16:1365-80.
10. Magid M, Reichenberg JS, Philbrick KL. To cut or not to cut: that was the question. Poster presented at: Meeting of the American Academy of Psychiatry and the Law; October 2005; Montreal, Canada.
U.S. troops returning home: Are you prepared?
National Guard and Army Reserve troops constitute an estimated 30% to 40% of the 1 million-plus U.S. military personnel deployed in Iraq and Afghanistan.1-3 Many of these civilian soldiers—once considered “weekend warriors”—are serving a first combat tour, returning home, and being redeployed for additional tours of duty.
Because of these unprecedented deployment policies, civilian psychiatrists will likely play a greater role in treating combat-related mental health problems than in any previous U.S. war. You may need to provide initial and long-term psychiatric care for reservists and Guard members returning to your community during 2006 and beyond.
To help you prepare, we discuss the combat situations these soldiers are experiencing, types of psychiatric problems they are reporting in anonymous surveys, and their attitudes about seeking psychiatric care. We also offer practical resources on combat-related posttraumatic stress disorder (PTSD) for nonmilitary or Veterans Administration clinicians.
A soldier’s story: ‘He’s always jumpy’
Mr. L, age 39, is supervisor for a local construction company and a sergeant first class with 18 years of Army Reserve service who returned from Iraq 7 months ago. He tells you, “My wife made me come see you—I didn’t want to.”
Though he does not think he needs a psychiatrist, his irritability and poor sleep worry his wife. “He isn’t the same anymore,” she says. “He’s always jumpy.”
Reported psychiatric problems
Stress-related symptoms. Within 4 months of returning home from Iraq or Afghanistan, 3 in 10 soldiers have developed “stress-related mental health problems” such as anxiety, depression, nightmares, anger, and concentration difficulties, reports Army Surgeon General Lt. Gen. Kevin Kiley.4 An unknown smaller percentage were reportedly diagnosed with PTSD.
Strained marriages, suicidal thoughts/feelings, nightmares or flashbacks, and fear of losing control or injuring someone else were among problems soldiers acknowledged during post-deployment health assessments between January and August 2005. In these surveys, 28% of 193,000 returnees endorsed mental health problems, according to the Army Center for Health Promotion and Preventive Medicine (Table 1).5
Table 1
Mental health problems reported by troops returning from combat in Iraq*
| Problem | Number among 193,000 U.S. soldiers |
|---|---|
| Nightmares or unwanted war recollections | 20,000 |
| Might “hurt or lose control” with someone else | 3,700 |
| Suicidal thoughts/feeling better off dead | 1,700 |
| * 28% of returnees reported mental health problems in post-deployment surveys between January and August 2005. | |
| Source: Army Center for Health Promotion and Preventive Medicine, reference 5. | |
Unfortunately, this new information may underestimate the number of returnees with psychiatric problems and the severity of those problems. In an anonymous survey of returning Army and Marine soldiers, Hoge et al7 found that those who met criteria for psychiatric diagnoses were less likely to seek assistance because of perceived stigma and concerns about their military careers than those without a psychiatric diagnosis (Table 2).
Table 2
Perceived barriers to seeking mental health services cited by U.S. soldiers after combat duty in Iraq and Afghanistan*
| Perceived barrier | Met screening criteria for a mental disorder? | |
|---|---|---|
| Yes (N=731) | No (N=5,422) | |
| I would be seen as weak | 65% | 31% |
| My unit leadership might treat me differently | 63% | 33% |
| Members of my unit might have less confidence in me | 59% | 31% |
| I would have difficulty getting time off work for treatment | 55% | 22% |
| My leaders would blame me for the problem | 51% | 20% |
| It would harm my career | 50% | 24% |
| It is difficult to schedule an appointment | 45% | 17% |
| It would be too embarrassing | 41% | 18% |
| I don’t trust mental health professionals | 38% | 17% |
| Mental health care costs too much money | 25% | 10% |
| Mental health care doesn’t work | 25% | 9% |
| I don’t know where to get help | 22% | 6% |
| I don’t have adequate transportation | 18% | 6% |
| * Anonymous survey. Those who met criteria for psychiatric diagnoses were less likely to seek assistance because of perceived stigma and concerns about their military careers than those without a psychiatric diagnosis. | ||
| Source: Adapted and reprinted with permission from Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13-22. | ||
Gender per se may not be the most important variable; age, number of years in the military, type of military unit, and ethnic group are also risk factors for developing a war-related psychiatric disorder. Further studies of OIF- and OEF-related psychiatric disorders are needed to determine whether female veterans’ clinical needs differ in important ways from those of male veterans.
PTSD in combat veterans
Every war has seen new names and descriptions for combinations of psychological and somatic symptoms resulting from war experiences (Box).9,11 Compared with persons with PTSD from other types of trauma, combat veterans appear to have the highest rate of delayed-onset PTSD and are less responsive to treatment.9
Initial PTSD rates for soldiers returning from Iraq ranged from 12.2% (Marines) to 12.9% (Army), using diagnostic criteria requiring functional impairment.7 These rates are 2.5 times the rate observed before combat (5%) and 3 to 4 times that of the general population (3.6%), using the same methodology.10
If 12.5% of 1 million combat-exposed service members develop PTSD, 125,000 service members may be affected. This rough estimate—7 times the number of personnel officially reported as “wounded”—does not take into account the wide variability of combat exposure among deployed troops or the effects of combat stress interventions (which might decrease the rate). Nor does it consider the impact of multiple rotations and possible decreased combat simulation training in reserve troops (which might increase the rate).
During the Civil War, soldiers with pathologic reactions to combat were described as having “irritable heart” or “soldier’s heart.”9 Since then, every war has seen new names and descriptions for combinations of psychological and somatic symptoms resulting from war experiences.
Affected troops in World War I were said to have “shell shock,” whereas those in World War II and the Korean War had “combat fatigue.” Those fighting in the jungles of Vietnam had posttraumatic stress disorder (PTSD).
Along with evolving psychiatric nomenclature and diagnostic schema, each war—including those in Iraq and Afghanistan—has had unique symptom constellations.11 These differences relate to the contemporary state of scientific and medical knowledge, sociocultural factors, and popular press concerns. Some differences stem from actual or perceived weapon effects (such as chemical warfare or depleted uranium).
For example, World War I physicians at first considered “shell shock” to result from traumatic effects of high-explosive shells on the brain. This explanation proved inadequate when soldiers without direct concussive exposure expressed trauma-related symptoms.12
To develop, PTSD requires synergy between a severe stressor and a neurobiologic response. Because of genetic endowment or experience, not all persons are susceptible to the high levels of stress and associated hypothalamus-pituitary-adrenal axis activation required for the disorder to occur. Specific individual differences in coping, trauma history, and biology may predispose some individuals to PTSD.11
Mr. L’s story: Detached and irritable
As a combat infantryman, Mr. L was in seven fire fights, in which three of his buddies died. In responding to your questions, he admits feeling disconnected from his children and from his old friends who did not go to Iraq. He describes frequent arguments with his wife, though they had rarely argued previously. He denies psychiatric problems before his 12-month rotation in Iraq.
Being wounded in combat, surviving multiple life-threatening events, and experiencing combat of greater intensity and duration all increase the risk of developing PTSD. Mr. L’s multiple fire fights, loss of three friends, and other combat experiences place him at high risk for developing PTSD.
Typical combat experiences in Iraq and Afghanistan reported by Army and Marine troops are outlined in Table 3.7 Familiarizing yourself with these experiences can help you interview combat-exposed patients after you develop trust and rapport with them.
Table 3
Combat experiences reported by U.S. troops
after deployment in Iraq or Afghanistan
| Experience | Army groups | Marine group | |
|---|---|---|---|
| Afghanistan | Iraq | ||
| Being attacked or ambushed | 58% | 89% | 95% |
| Receiving incoming artillery, rocket or mortar fire | 84% | 86% | 92% |
| Being shot at or receiving small-arms fire | 66% | 93% | 97% |
| Shooting or directing fire at the enemy | 27% | 77% | 87% |
| Being responsible for death of an enemy combatant | 12% | 48% | 65% |
| Being responsible for death of a noncombatant | 1% | 14% | 28% |
| Seeing dead bodies or human remains | 39% | 95% | 94% |
| Seeing dead or seriously injured Americans | 30% | 65% | 75% |
| Knowing someone seriously injured or killed | 43% | 86% | 87% |
| Participating in demining operations | 16% | 38% | 34% |
| Seeing ill or injured women or children whom you were unable to help | 46% | 69% | 83% |
| Being wounded or injured | 5% | 14% | 9% |
| Being shot or hit, but protective gear saved you | * | 8% | 10% |
| Having a buddy who was near you shot or hit | * | 22% | 26% |
| Clearing or searching homes or buildings | 57% | 80% | 86% |
| Engaging in hand-to-hand combat | 3% | 22% | 9% |
| Saved the life of a soldier or civilian | 6% | 21% | 19% |
| * Question not included in this survey | |||
| Source: Adapted and reprinted with permission from Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004; 351:13-22. | |||
Workup of combat veterans
Military psychiatrists provide support and treatment during and immediately after combat, but they do not associate acute reactions with specific psychiatric diagnoses to avoid “pathologizing” brief reactions to combat. To provide appropriate treatment for returning troops, however, you will need to characterize clinically significant psychopathology by using DSM IV-TR criteria for acute stress disorder and PTSD.12
We recommend that you manage a returning service member according to usual clinical practice. This includes a thorough history and appropriate medical and laboratory workup. Because soldiers commonly minimize their symptoms and concerns—particularly if they fear full disclosure could jeopardize their military careers—consider including collateral history from the patient’s family and friends in your assessment.
Differential diagnosis of mental disorders in combat troops is broad. You will need to obtain a thorough substance abuse history, with particular attention to use of alcohol to self-medicate symptoms. It will be important to assess safety issues, including potential for suicide, homicide, and domestic violence.
Many soldiers report difficulties with re-entering family life. Marital and sexual problems may develop because of role changes that occurred during a long separation. Pre-existing marital problems may be exacerbated, and both military members and spouses may express concerns about infidelity. Separation and divorce rates may be high.
Mr. L’s story: Alcohol ‘helps me sleep’
When you ask Mr. L about his use of alcohol, he notes that he was cited for driving while intoxicated at age 28. “I used to have a problem with drinking, but after my ticket I didn’t drink ‘til I came back from Iraq,” he says. “Now it’s the only thing that calms me down and helps me sleep.”
Comorbid diagnoses associated with PTSD are the rule. Mr. L’s drinking to self-medicate his PTSD symptoms puts him at risk of redeveloping alcohol problems. Use current best practices for managing depression, anxiety disorders, and substance abuse (if present) to guide treatment.
Suicidal behavior has also been strongly associated with PTSD.13 Thus, address Mr. L’s access to firearms, and include suicide assessment and regular followup in any treatment plan.
Head injuries in iraq
The use of effective body armor has dramatically changed the types of wounds and injuries sustained in combat. Kevlar body armor has decreased the frequency of mortal chest and abdominal wounds, leading to an unprecedented proportion of head and neck wounds, including eye injuries. In the war in Iraq and Afghanistan, 22% of evacuated casualties have injuries to the head, neck, and face.14
At the same time, rapid treatment of open and closed head injuries—often fatal in past wars—has improved survival. As a result, the prevalence of traumatic brain injury in veteran populations is believed to be substantially higher now than in previous conflicts.15
Mr. L’s story: ‘I forget everything’
Mr. L reports that after he served 8 months in Iraq, his vehicle was destroyed by a roadside bomb. He lost consciousness and was hospitalized briefly before returning to duty and completing his tour.
“I’m having trouble concentrating at work, and it seems like I forget everything,” he says. “My boss has complained about mistakes I make when planning our construction jobs. Could that explosion be causing my problems?”
Mr. L’s loss of consciousness associated with a blast injury and his cognitive complaints suggest possible mild traumatic brain injury. Consider neuropsychological testing and brain imaging studies, along with possible referral to appropriate rehabilitation programs if needed.
Treatment resources
The Iraq War Clinician Guide16 delineates military approaches to prevention, as well as acute intervention and initial treatment after evacuation from a war zone. This guide also:
- outlines rationales for removing affected service members from combat and eventually returning them to duty or medically retiring them if severe symptoms continue to interfere with ability to function.
- describes the biopsychosocial approach used by the Walter Reed Army Medical Center Psychiatric Consultation Service to address the multifactorial needs of the traumatized amputee.
- National Center for PTSD: The War in Iraq. www.ncptsd.va.gov/topics/war.html
Comprehensive Web site designated by Congress to provide information for military veterans with PTSD. Clinician’s guide available, plus fact sheets for family and patients. - National Center for PTSD. Iraq War Clinician Guide (2nd ed). www.ncptsd.va.gov/war/iraq_clinician_guide_v2/iraq_clinician_guide_v2.pdf
Detailed guide for treating the soldier in combat. Includes treatment options for PTSD and the veteran with amputation. - U.S. Army Center for Health Promotion and Preventive Medicine. Supporting Guidelines. www.pdhealth.mil/clinicians/support.asp
Collection of guidelines for PTSD, major depression, and medically unexplained symptoms following combat. - Military One Source. www.militaryonesource.com
Resource for active duty and reserve soldiers and family members. Portal for support services, policies, and education. Brief confidential counseling support for soldiers and family members. - Veterans Administration (VA)/Department of Defense (DOD) Clinical Practice Guideline for Management of PTSD, January 2004. www.oqp.med.va.gov/cpg/PTSD/PTSD_Base.htm
Includes list of clinical trials, medication dosing, and evidence basis for treatment with pharmacotherapy and psychotherapy. - American Psychiatric Association. Practice Guideline for the Treatment of Patients With Acute Stress Disorder and Posttraumatic Stress Disorder. http://www.psych.org/psych_pract/treatg/pg/PTSD-PG-PartsA-B-C-New.pdf
Background and guidelines for managing PTSD, including treatment recommendations, evidence basis, background, and areas for future research.
Disclosure
Drs. Lineberry, Bostwick, and Rundell previously served on active duty in the U.S. Air Force for 12, 5, and 23 years, respectively.
1. Benjamin M. How many have gone to war? Salon.com April 12, 2005. Available at: http://www.salon.com/news/feature/2005/04/12/troops_numbers/index_np.html. Accessed Dec. 13, 2005.
2. United States Government Accountability Office. Testimony before the Committee on Government Reform, House of Representatives. Reserve forces. Army National Guard’s role, organization, and equipment need to be reexamined. Oct. 20, 2005. Available at: http://www.gao.gov/new.items/d06170t.pdf. Accessed Oct. 26, 2005.
3. Wetzel K. Senators told of Guard struggles. Seattle Times Oct. 20, 2005. Available at: http://seattletimes.nwsource.com/html/local-news/2002571967_soldiers20m.html. Accessed Oct. 26, 2005.
4. Associated Press. Survey: 30% of returning Iraq vets suffer mental ills. USA Today July 28, 2005. Available at: http://www.usatoday.com/news/health/2005-07-28-iraq-vets-health_x.htm?csp=34. Accessed Oct. 26, 2005.
5. Zoroya G. One in four Iraq vets ailing on return. USA Today Oct. 18, 2005. Available at: http://www.usatoday.com/news/world/iraq/2005-10-18-troops-side_x.htm. Accessed Oct. 26, 2005.
6. Zoroya G. Troops screened as never before. USA Today Oct. 18, 2005. Available at: http://www.usatoday.com/news/world/iraq/2005-10-18-troops-stress-side_x.htm. Accessed Oct. 26, 2005.
7. Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13-22.
8. Prigerson HG, Maciejewski PK, Rosenheck RA. Combat trauma: trauma with highest risk of delayed onset and unresolved posttraumatic stress disorder symptoms, unemployment, and abuse among men. J Nerv Ment Dis 2001;189:99-108.
9. Narrow WE, Rae DS, Robins LN, Regier DA. Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys’ estimates. Arch Gen Psychiatry 2002;59:115-23.
10. Lieberman HR, Bathalon GP, Falco CN, et al. Severe decrements in cognition, function and mood induced by sleep loss, heat, dehydration, and under-nutrition during simulated combat. Biol Psychiatry 2005;57:422-9.
11. Nemeroff CB, Bremner JD, Foa EB, et al. Posttraumatic stress disorder: a state-of-the-science review. J Psychiatr Res (In press; Oct 2005 epub ahead of publication).
12. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, text rev). Washington, DC: American Psychiatric Association; 2000.
13. Sareen J, Houlahan T, Cox BJ, Asmundson GJ. Anxiety disorders associated with suicidal ideation and suicide attempts in the national comorbidity survey. J Nerv Ment Dis 2005;193:450-4.
14. Xydakis MS, Fravell MD, Nasser KE, Casler JD. Analysis of battlefield head and neck injuries in Iraq and Afghanistan. Otolarnygol Head Neck Surg 2005;133:497-504.
15. Okie S. Traumatic brain injury in the war zone. N Engl J Med 2005;352(20):2043-7.
16. Cozza SJ, Benedek DM, Bradley JC, et al. Topics specific to the psychiatric treatment of military personnel. In: Schnurr PP, Cozza SJ (eds). Iraq War clinician guide (2nd ed). Washington, DC: National Center for PTSD. Walter Reed Army Medical Center; 2004:4-20. Available at: http://www.ncptsd.va.gov/war/iraq_clinician_guide_v2/iraq_clinician_guide_v2.pdf Accessed Oct. 26, 2005.
National Guard and Army Reserve troops constitute an estimated 30% to 40% of the 1 million-plus U.S. military personnel deployed in Iraq and Afghanistan.1-3 Many of these civilian soldiers—once considered “weekend warriors”—are serving a first combat tour, returning home, and being redeployed for additional tours of duty.
Because of these unprecedented deployment policies, civilian psychiatrists will likely play a greater role in treating combat-related mental health problems than in any previous U.S. war. You may need to provide initial and long-term psychiatric care for reservists and Guard members returning to your community during 2006 and beyond.
To help you prepare, we discuss the combat situations these soldiers are experiencing, types of psychiatric problems they are reporting in anonymous surveys, and their attitudes about seeking psychiatric care. We also offer practical resources on combat-related posttraumatic stress disorder (PTSD) for nonmilitary or Veterans Administration clinicians.
A soldier’s story: ‘He’s always jumpy’
Mr. L, age 39, is supervisor for a local construction company and a sergeant first class with 18 years of Army Reserve service who returned from Iraq 7 months ago. He tells you, “My wife made me come see you—I didn’t want to.”
Though he does not think he needs a psychiatrist, his irritability and poor sleep worry his wife. “He isn’t the same anymore,” she says. “He’s always jumpy.”
Reported psychiatric problems
Stress-related symptoms. Within 4 months of returning home from Iraq or Afghanistan, 3 in 10 soldiers have developed “stress-related mental health problems” such as anxiety, depression, nightmares, anger, and concentration difficulties, reports Army Surgeon General Lt. Gen. Kevin Kiley.4 An unknown smaller percentage were reportedly diagnosed with PTSD.
Strained marriages, suicidal thoughts/feelings, nightmares or flashbacks, and fear of losing control or injuring someone else were among problems soldiers acknowledged during post-deployment health assessments between January and August 2005. In these surveys, 28% of 193,000 returnees endorsed mental health problems, according to the Army Center for Health Promotion and Preventive Medicine (Table 1).5
Table 1
Mental health problems reported by troops returning from combat in Iraq*
| Problem | Number among 193,000 U.S. soldiers |
|---|---|
| Nightmares or unwanted war recollections | 20,000 |
| Might “hurt or lose control” with someone else | 3,700 |
| Suicidal thoughts/feeling better off dead | 1,700 |
| * 28% of returnees reported mental health problems in post-deployment surveys between January and August 2005. | |
| Source: Army Center for Health Promotion and Preventive Medicine, reference 5. | |
Unfortunately, this new information may underestimate the number of returnees with psychiatric problems and the severity of those problems. In an anonymous survey of returning Army and Marine soldiers, Hoge et al7 found that those who met criteria for psychiatric diagnoses were less likely to seek assistance because of perceived stigma and concerns about their military careers than those without a psychiatric diagnosis (Table 2).
Table 2
Perceived barriers to seeking mental health services cited by U.S. soldiers after combat duty in Iraq and Afghanistan*
| Perceived barrier | Met screening criteria for a mental disorder? | |
|---|---|---|
| Yes (N=731) | No (N=5,422) | |
| I would be seen as weak | 65% | 31% |
| My unit leadership might treat me differently | 63% | 33% |
| Members of my unit might have less confidence in me | 59% | 31% |
| I would have difficulty getting time off work for treatment | 55% | 22% |
| My leaders would blame me for the problem | 51% | 20% |
| It would harm my career | 50% | 24% |
| It is difficult to schedule an appointment | 45% | 17% |
| It would be too embarrassing | 41% | 18% |
| I don’t trust mental health professionals | 38% | 17% |
| Mental health care costs too much money | 25% | 10% |
| Mental health care doesn’t work | 25% | 9% |
| I don’t know where to get help | 22% | 6% |
| I don’t have adequate transportation | 18% | 6% |
| * Anonymous survey. Those who met criteria for psychiatric diagnoses were less likely to seek assistance because of perceived stigma and concerns about their military careers than those without a psychiatric diagnosis. | ||
| Source: Adapted and reprinted with permission from Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13-22. | ||
Gender per se may not be the most important variable; age, number of years in the military, type of military unit, and ethnic group are also risk factors for developing a war-related psychiatric disorder. Further studies of OIF- and OEF-related psychiatric disorders are needed to determine whether female veterans’ clinical needs differ in important ways from those of male veterans.
PTSD in combat veterans
Every war has seen new names and descriptions for combinations of psychological and somatic symptoms resulting from war experiences (Box).9,11 Compared with persons with PTSD from other types of trauma, combat veterans appear to have the highest rate of delayed-onset PTSD and are less responsive to treatment.9
Initial PTSD rates for soldiers returning from Iraq ranged from 12.2% (Marines) to 12.9% (Army), using diagnostic criteria requiring functional impairment.7 These rates are 2.5 times the rate observed before combat (5%) and 3 to 4 times that of the general population (3.6%), using the same methodology.10
If 12.5% of 1 million combat-exposed service members develop PTSD, 125,000 service members may be affected. This rough estimate—7 times the number of personnel officially reported as “wounded”—does not take into account the wide variability of combat exposure among deployed troops or the effects of combat stress interventions (which might decrease the rate). Nor does it consider the impact of multiple rotations and possible decreased combat simulation training in reserve troops (which might increase the rate).
During the Civil War, soldiers with pathologic reactions to combat were described as having “irritable heart” or “soldier’s heart.”9 Since then, every war has seen new names and descriptions for combinations of psychological and somatic symptoms resulting from war experiences.
Affected troops in World War I were said to have “shell shock,” whereas those in World War II and the Korean War had “combat fatigue.” Those fighting in the jungles of Vietnam had posttraumatic stress disorder (PTSD).
Along with evolving psychiatric nomenclature and diagnostic schema, each war—including those in Iraq and Afghanistan—has had unique symptom constellations.11 These differences relate to the contemporary state of scientific and medical knowledge, sociocultural factors, and popular press concerns. Some differences stem from actual or perceived weapon effects (such as chemical warfare or depleted uranium).
For example, World War I physicians at first considered “shell shock” to result from traumatic effects of high-explosive shells on the brain. This explanation proved inadequate when soldiers without direct concussive exposure expressed trauma-related symptoms.12
To develop, PTSD requires synergy between a severe stressor and a neurobiologic response. Because of genetic endowment or experience, not all persons are susceptible to the high levels of stress and associated hypothalamus-pituitary-adrenal axis activation required for the disorder to occur. Specific individual differences in coping, trauma history, and biology may predispose some individuals to PTSD.11
Mr. L’s story: Detached and irritable
As a combat infantryman, Mr. L was in seven fire fights, in which three of his buddies died. In responding to your questions, he admits feeling disconnected from his children and from his old friends who did not go to Iraq. He describes frequent arguments with his wife, though they had rarely argued previously. He denies psychiatric problems before his 12-month rotation in Iraq.
Being wounded in combat, surviving multiple life-threatening events, and experiencing combat of greater intensity and duration all increase the risk of developing PTSD. Mr. L’s multiple fire fights, loss of three friends, and other combat experiences place him at high risk for developing PTSD.
Typical combat experiences in Iraq and Afghanistan reported by Army and Marine troops are outlined in Table 3.7 Familiarizing yourself with these experiences can help you interview combat-exposed patients after you develop trust and rapport with them.
Table 3
Combat experiences reported by U.S. troops
after deployment in Iraq or Afghanistan
| Experience | Army groups | Marine group | |
|---|---|---|---|
| Afghanistan | Iraq | ||
| Being attacked or ambushed | 58% | 89% | 95% |
| Receiving incoming artillery, rocket or mortar fire | 84% | 86% | 92% |
| Being shot at or receiving small-arms fire | 66% | 93% | 97% |
| Shooting or directing fire at the enemy | 27% | 77% | 87% |
| Being responsible for death of an enemy combatant | 12% | 48% | 65% |
| Being responsible for death of a noncombatant | 1% | 14% | 28% |
| Seeing dead bodies or human remains | 39% | 95% | 94% |
| Seeing dead or seriously injured Americans | 30% | 65% | 75% |
| Knowing someone seriously injured or killed | 43% | 86% | 87% |
| Participating in demining operations | 16% | 38% | 34% |
| Seeing ill or injured women or children whom you were unable to help | 46% | 69% | 83% |
| Being wounded or injured | 5% | 14% | 9% |
| Being shot or hit, but protective gear saved you | * | 8% | 10% |
| Having a buddy who was near you shot or hit | * | 22% | 26% |
| Clearing or searching homes or buildings | 57% | 80% | 86% |
| Engaging in hand-to-hand combat | 3% | 22% | 9% |
| Saved the life of a soldier or civilian | 6% | 21% | 19% |
| * Question not included in this survey | |||
| Source: Adapted and reprinted with permission from Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004; 351:13-22. | |||
Workup of combat veterans
Military psychiatrists provide support and treatment during and immediately after combat, but they do not associate acute reactions with specific psychiatric diagnoses to avoid “pathologizing” brief reactions to combat. To provide appropriate treatment for returning troops, however, you will need to characterize clinically significant psychopathology by using DSM IV-TR criteria for acute stress disorder and PTSD.12
We recommend that you manage a returning service member according to usual clinical practice. This includes a thorough history and appropriate medical and laboratory workup. Because soldiers commonly minimize their symptoms and concerns—particularly if they fear full disclosure could jeopardize their military careers—consider including collateral history from the patient’s family and friends in your assessment.
Differential diagnosis of mental disorders in combat troops is broad. You will need to obtain a thorough substance abuse history, with particular attention to use of alcohol to self-medicate symptoms. It will be important to assess safety issues, including potential for suicide, homicide, and domestic violence.
Many soldiers report difficulties with re-entering family life. Marital and sexual problems may develop because of role changes that occurred during a long separation. Pre-existing marital problems may be exacerbated, and both military members and spouses may express concerns about infidelity. Separation and divorce rates may be high.
Mr. L’s story: Alcohol ‘helps me sleep’
When you ask Mr. L about his use of alcohol, he notes that he was cited for driving while intoxicated at age 28. “I used to have a problem with drinking, but after my ticket I didn’t drink ‘til I came back from Iraq,” he says. “Now it’s the only thing that calms me down and helps me sleep.”
Comorbid diagnoses associated with PTSD are the rule. Mr. L’s drinking to self-medicate his PTSD symptoms puts him at risk of redeveloping alcohol problems. Use current best practices for managing depression, anxiety disorders, and substance abuse (if present) to guide treatment.
Suicidal behavior has also been strongly associated with PTSD.13 Thus, address Mr. L’s access to firearms, and include suicide assessment and regular followup in any treatment plan.
Head injuries in iraq
The use of effective body armor has dramatically changed the types of wounds and injuries sustained in combat. Kevlar body armor has decreased the frequency of mortal chest and abdominal wounds, leading to an unprecedented proportion of head and neck wounds, including eye injuries. In the war in Iraq and Afghanistan, 22% of evacuated casualties have injuries to the head, neck, and face.14
At the same time, rapid treatment of open and closed head injuries—often fatal in past wars—has improved survival. As a result, the prevalence of traumatic brain injury in veteran populations is believed to be substantially higher now than in previous conflicts.15
Mr. L’s story: ‘I forget everything’
Mr. L reports that after he served 8 months in Iraq, his vehicle was destroyed by a roadside bomb. He lost consciousness and was hospitalized briefly before returning to duty and completing his tour.
“I’m having trouble concentrating at work, and it seems like I forget everything,” he says. “My boss has complained about mistakes I make when planning our construction jobs. Could that explosion be causing my problems?”
Mr. L’s loss of consciousness associated with a blast injury and his cognitive complaints suggest possible mild traumatic brain injury. Consider neuropsychological testing and brain imaging studies, along with possible referral to appropriate rehabilitation programs if needed.
Treatment resources
The Iraq War Clinician Guide16 delineates military approaches to prevention, as well as acute intervention and initial treatment after evacuation from a war zone. This guide also:
- outlines rationales for removing affected service members from combat and eventually returning them to duty or medically retiring them if severe symptoms continue to interfere with ability to function.
- describes the biopsychosocial approach used by the Walter Reed Army Medical Center Psychiatric Consultation Service to address the multifactorial needs of the traumatized amputee.
- National Center for PTSD: The War in Iraq. www.ncptsd.va.gov/topics/war.html
Comprehensive Web site designated by Congress to provide information for military veterans with PTSD. Clinician’s guide available, plus fact sheets for family and patients. - National Center for PTSD. Iraq War Clinician Guide (2nd ed). www.ncptsd.va.gov/war/iraq_clinician_guide_v2/iraq_clinician_guide_v2.pdf
Detailed guide for treating the soldier in combat. Includes treatment options for PTSD and the veteran with amputation. - U.S. Army Center for Health Promotion and Preventive Medicine. Supporting Guidelines. www.pdhealth.mil/clinicians/support.asp
Collection of guidelines for PTSD, major depression, and medically unexplained symptoms following combat. - Military One Source. www.militaryonesource.com
Resource for active duty and reserve soldiers and family members. Portal for support services, policies, and education. Brief confidential counseling support for soldiers and family members. - Veterans Administration (VA)/Department of Defense (DOD) Clinical Practice Guideline for Management of PTSD, January 2004. www.oqp.med.va.gov/cpg/PTSD/PTSD_Base.htm
Includes list of clinical trials, medication dosing, and evidence basis for treatment with pharmacotherapy and psychotherapy. - American Psychiatric Association. Practice Guideline for the Treatment of Patients With Acute Stress Disorder and Posttraumatic Stress Disorder. http://www.psych.org/psych_pract/treatg/pg/PTSD-PG-PartsA-B-C-New.pdf
Background and guidelines for managing PTSD, including treatment recommendations, evidence basis, background, and areas for future research.
Disclosure
Drs. Lineberry, Bostwick, and Rundell previously served on active duty in the U.S. Air Force for 12, 5, and 23 years, respectively.
National Guard and Army Reserve troops constitute an estimated 30% to 40% of the 1 million-plus U.S. military personnel deployed in Iraq and Afghanistan.1-3 Many of these civilian soldiers—once considered “weekend warriors”—are serving a first combat tour, returning home, and being redeployed for additional tours of duty.
Because of these unprecedented deployment policies, civilian psychiatrists will likely play a greater role in treating combat-related mental health problems than in any previous U.S. war. You may need to provide initial and long-term psychiatric care for reservists and Guard members returning to your community during 2006 and beyond.
To help you prepare, we discuss the combat situations these soldiers are experiencing, types of psychiatric problems they are reporting in anonymous surveys, and their attitudes about seeking psychiatric care. We also offer practical resources on combat-related posttraumatic stress disorder (PTSD) for nonmilitary or Veterans Administration clinicians.
A soldier’s story: ‘He’s always jumpy’
Mr. L, age 39, is supervisor for a local construction company and a sergeant first class with 18 years of Army Reserve service who returned from Iraq 7 months ago. He tells you, “My wife made me come see you—I didn’t want to.”
Though he does not think he needs a psychiatrist, his irritability and poor sleep worry his wife. “He isn’t the same anymore,” she says. “He’s always jumpy.”
Reported psychiatric problems
Stress-related symptoms. Within 4 months of returning home from Iraq or Afghanistan, 3 in 10 soldiers have developed “stress-related mental health problems” such as anxiety, depression, nightmares, anger, and concentration difficulties, reports Army Surgeon General Lt. Gen. Kevin Kiley.4 An unknown smaller percentage were reportedly diagnosed with PTSD.
Strained marriages, suicidal thoughts/feelings, nightmares or flashbacks, and fear of losing control or injuring someone else were among problems soldiers acknowledged during post-deployment health assessments between January and August 2005. In these surveys, 28% of 193,000 returnees endorsed mental health problems, according to the Army Center for Health Promotion and Preventive Medicine (Table 1).5
Table 1
Mental health problems reported by troops returning from combat in Iraq*
| Problem | Number among 193,000 U.S. soldiers |
|---|---|
| Nightmares or unwanted war recollections | 20,000 |
| Might “hurt or lose control” with someone else | 3,700 |
| Suicidal thoughts/feeling better off dead | 1,700 |
| * 28% of returnees reported mental health problems in post-deployment surveys between January and August 2005. | |
| Source: Army Center for Health Promotion and Preventive Medicine, reference 5. | |
Unfortunately, this new information may underestimate the number of returnees with psychiatric problems and the severity of those problems. In an anonymous survey of returning Army and Marine soldiers, Hoge et al7 found that those who met criteria for psychiatric diagnoses were less likely to seek assistance because of perceived stigma and concerns about their military careers than those without a psychiatric diagnosis (Table 2).
Table 2
Perceived barriers to seeking mental health services cited by U.S. soldiers after combat duty in Iraq and Afghanistan*
| Perceived barrier | Met screening criteria for a mental disorder? | |
|---|---|---|
| Yes (N=731) | No (N=5,422) | |
| I would be seen as weak | 65% | 31% |
| My unit leadership might treat me differently | 63% | 33% |
| Members of my unit might have less confidence in me | 59% | 31% |
| I would have difficulty getting time off work for treatment | 55% | 22% |
| My leaders would blame me for the problem | 51% | 20% |
| It would harm my career | 50% | 24% |
| It is difficult to schedule an appointment | 45% | 17% |
| It would be too embarrassing | 41% | 18% |
| I don’t trust mental health professionals | 38% | 17% |
| Mental health care costs too much money | 25% | 10% |
| Mental health care doesn’t work | 25% | 9% |
| I don’t know where to get help | 22% | 6% |
| I don’t have adequate transportation | 18% | 6% |
| * Anonymous survey. Those who met criteria for psychiatric diagnoses were less likely to seek assistance because of perceived stigma and concerns about their military careers than those without a psychiatric diagnosis. | ||
| Source: Adapted and reprinted with permission from Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13-22. | ||
Gender per se may not be the most important variable; age, number of years in the military, type of military unit, and ethnic group are also risk factors for developing a war-related psychiatric disorder. Further studies of OIF- and OEF-related psychiatric disorders are needed to determine whether female veterans’ clinical needs differ in important ways from those of male veterans.
PTSD in combat veterans
Every war has seen new names and descriptions for combinations of psychological and somatic symptoms resulting from war experiences (Box).9,11 Compared with persons with PTSD from other types of trauma, combat veterans appear to have the highest rate of delayed-onset PTSD and are less responsive to treatment.9
Initial PTSD rates for soldiers returning from Iraq ranged from 12.2% (Marines) to 12.9% (Army), using diagnostic criteria requiring functional impairment.7 These rates are 2.5 times the rate observed before combat (5%) and 3 to 4 times that of the general population (3.6%), using the same methodology.10
If 12.5% of 1 million combat-exposed service members develop PTSD, 125,000 service members may be affected. This rough estimate—7 times the number of personnel officially reported as “wounded”—does not take into account the wide variability of combat exposure among deployed troops or the effects of combat stress interventions (which might decrease the rate). Nor does it consider the impact of multiple rotations and possible decreased combat simulation training in reserve troops (which might increase the rate).
During the Civil War, soldiers with pathologic reactions to combat were described as having “irritable heart” or “soldier’s heart.”9 Since then, every war has seen new names and descriptions for combinations of psychological and somatic symptoms resulting from war experiences.
Affected troops in World War I were said to have “shell shock,” whereas those in World War II and the Korean War had “combat fatigue.” Those fighting in the jungles of Vietnam had posttraumatic stress disorder (PTSD).
Along with evolving psychiatric nomenclature and diagnostic schema, each war—including those in Iraq and Afghanistan—has had unique symptom constellations.11 These differences relate to the contemporary state of scientific and medical knowledge, sociocultural factors, and popular press concerns. Some differences stem from actual or perceived weapon effects (such as chemical warfare or depleted uranium).
For example, World War I physicians at first considered “shell shock” to result from traumatic effects of high-explosive shells on the brain. This explanation proved inadequate when soldiers without direct concussive exposure expressed trauma-related symptoms.12
To develop, PTSD requires synergy between a severe stressor and a neurobiologic response. Because of genetic endowment or experience, not all persons are susceptible to the high levels of stress and associated hypothalamus-pituitary-adrenal axis activation required for the disorder to occur. Specific individual differences in coping, trauma history, and biology may predispose some individuals to PTSD.11
Mr. L’s story: Detached and irritable
As a combat infantryman, Mr. L was in seven fire fights, in which three of his buddies died. In responding to your questions, he admits feeling disconnected from his children and from his old friends who did not go to Iraq. He describes frequent arguments with his wife, though they had rarely argued previously. He denies psychiatric problems before his 12-month rotation in Iraq.
Being wounded in combat, surviving multiple life-threatening events, and experiencing combat of greater intensity and duration all increase the risk of developing PTSD. Mr. L’s multiple fire fights, loss of three friends, and other combat experiences place him at high risk for developing PTSD.
Typical combat experiences in Iraq and Afghanistan reported by Army and Marine troops are outlined in Table 3.7 Familiarizing yourself with these experiences can help you interview combat-exposed patients after you develop trust and rapport with them.
Table 3
Combat experiences reported by U.S. troops
after deployment in Iraq or Afghanistan
| Experience | Army groups | Marine group | |
|---|---|---|---|
| Afghanistan | Iraq | ||
| Being attacked or ambushed | 58% | 89% | 95% |
| Receiving incoming artillery, rocket or mortar fire | 84% | 86% | 92% |
| Being shot at or receiving small-arms fire | 66% | 93% | 97% |
| Shooting or directing fire at the enemy | 27% | 77% | 87% |
| Being responsible for death of an enemy combatant | 12% | 48% | 65% |
| Being responsible for death of a noncombatant | 1% | 14% | 28% |
| Seeing dead bodies or human remains | 39% | 95% | 94% |
| Seeing dead or seriously injured Americans | 30% | 65% | 75% |
| Knowing someone seriously injured or killed | 43% | 86% | 87% |
| Participating in demining operations | 16% | 38% | 34% |
| Seeing ill or injured women or children whom you were unable to help | 46% | 69% | 83% |
| Being wounded or injured | 5% | 14% | 9% |
| Being shot or hit, but protective gear saved you | * | 8% | 10% |
| Having a buddy who was near you shot or hit | * | 22% | 26% |
| Clearing or searching homes or buildings | 57% | 80% | 86% |
| Engaging in hand-to-hand combat | 3% | 22% | 9% |
| Saved the life of a soldier or civilian | 6% | 21% | 19% |
| * Question not included in this survey | |||
| Source: Adapted and reprinted with permission from Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004; 351:13-22. | |||
Workup of combat veterans
Military psychiatrists provide support and treatment during and immediately after combat, but they do not associate acute reactions with specific psychiatric diagnoses to avoid “pathologizing” brief reactions to combat. To provide appropriate treatment for returning troops, however, you will need to characterize clinically significant psychopathology by using DSM IV-TR criteria for acute stress disorder and PTSD.12
We recommend that you manage a returning service member according to usual clinical practice. This includes a thorough history and appropriate medical and laboratory workup. Because soldiers commonly minimize their symptoms and concerns—particularly if they fear full disclosure could jeopardize their military careers—consider including collateral history from the patient’s family and friends in your assessment.
Differential diagnosis of mental disorders in combat troops is broad. You will need to obtain a thorough substance abuse history, with particular attention to use of alcohol to self-medicate symptoms. It will be important to assess safety issues, including potential for suicide, homicide, and domestic violence.
Many soldiers report difficulties with re-entering family life. Marital and sexual problems may develop because of role changes that occurred during a long separation. Pre-existing marital problems may be exacerbated, and both military members and spouses may express concerns about infidelity. Separation and divorce rates may be high.
Mr. L’s story: Alcohol ‘helps me sleep’
When you ask Mr. L about his use of alcohol, he notes that he was cited for driving while intoxicated at age 28. “I used to have a problem with drinking, but after my ticket I didn’t drink ‘til I came back from Iraq,” he says. “Now it’s the only thing that calms me down and helps me sleep.”
Comorbid diagnoses associated with PTSD are the rule. Mr. L’s drinking to self-medicate his PTSD symptoms puts him at risk of redeveloping alcohol problems. Use current best practices for managing depression, anxiety disorders, and substance abuse (if present) to guide treatment.
Suicidal behavior has also been strongly associated with PTSD.13 Thus, address Mr. L’s access to firearms, and include suicide assessment and regular followup in any treatment plan.
Head injuries in iraq
The use of effective body armor has dramatically changed the types of wounds and injuries sustained in combat. Kevlar body armor has decreased the frequency of mortal chest and abdominal wounds, leading to an unprecedented proportion of head and neck wounds, including eye injuries. In the war in Iraq and Afghanistan, 22% of evacuated casualties have injuries to the head, neck, and face.14
At the same time, rapid treatment of open and closed head injuries—often fatal in past wars—has improved survival. As a result, the prevalence of traumatic brain injury in veteran populations is believed to be substantially higher now than in previous conflicts.15
Mr. L’s story: ‘I forget everything’
Mr. L reports that after he served 8 months in Iraq, his vehicle was destroyed by a roadside bomb. He lost consciousness and was hospitalized briefly before returning to duty and completing his tour.
“I’m having trouble concentrating at work, and it seems like I forget everything,” he says. “My boss has complained about mistakes I make when planning our construction jobs. Could that explosion be causing my problems?”
Mr. L’s loss of consciousness associated with a blast injury and his cognitive complaints suggest possible mild traumatic brain injury. Consider neuropsychological testing and brain imaging studies, along with possible referral to appropriate rehabilitation programs if needed.
Treatment resources
The Iraq War Clinician Guide16 delineates military approaches to prevention, as well as acute intervention and initial treatment after evacuation from a war zone. This guide also:
- outlines rationales for removing affected service members from combat and eventually returning them to duty or medically retiring them if severe symptoms continue to interfere with ability to function.
- describes the biopsychosocial approach used by the Walter Reed Army Medical Center Psychiatric Consultation Service to address the multifactorial needs of the traumatized amputee.
- National Center for PTSD: The War in Iraq. www.ncptsd.va.gov/topics/war.html
Comprehensive Web site designated by Congress to provide information for military veterans with PTSD. Clinician’s guide available, plus fact sheets for family and patients. - National Center for PTSD. Iraq War Clinician Guide (2nd ed). www.ncptsd.va.gov/war/iraq_clinician_guide_v2/iraq_clinician_guide_v2.pdf
Detailed guide for treating the soldier in combat. Includes treatment options for PTSD and the veteran with amputation. - U.S. Army Center for Health Promotion and Preventive Medicine. Supporting Guidelines. www.pdhealth.mil/clinicians/support.asp
Collection of guidelines for PTSD, major depression, and medically unexplained symptoms following combat. - Military One Source. www.militaryonesource.com
Resource for active duty and reserve soldiers and family members. Portal for support services, policies, and education. Brief confidential counseling support for soldiers and family members. - Veterans Administration (VA)/Department of Defense (DOD) Clinical Practice Guideline for Management of PTSD, January 2004. www.oqp.med.va.gov/cpg/PTSD/PTSD_Base.htm
Includes list of clinical trials, medication dosing, and evidence basis for treatment with pharmacotherapy and psychotherapy. - American Psychiatric Association. Practice Guideline for the Treatment of Patients With Acute Stress Disorder and Posttraumatic Stress Disorder. http://www.psych.org/psych_pract/treatg/pg/PTSD-PG-PartsA-B-C-New.pdf
Background and guidelines for managing PTSD, including treatment recommendations, evidence basis, background, and areas for future research.
Disclosure
Drs. Lineberry, Bostwick, and Rundell previously served on active duty in the U.S. Air Force for 12, 5, and 23 years, respectively.
1. Benjamin M. How many have gone to war? Salon.com April 12, 2005. Available at: http://www.salon.com/news/feature/2005/04/12/troops_numbers/index_np.html. Accessed Dec. 13, 2005.
2. United States Government Accountability Office. Testimony before the Committee on Government Reform, House of Representatives. Reserve forces. Army National Guard’s role, organization, and equipment need to be reexamined. Oct. 20, 2005. Available at: http://www.gao.gov/new.items/d06170t.pdf. Accessed Oct. 26, 2005.
3. Wetzel K. Senators told of Guard struggles. Seattle Times Oct. 20, 2005. Available at: http://seattletimes.nwsource.com/html/local-news/2002571967_soldiers20m.html. Accessed Oct. 26, 2005.
4. Associated Press. Survey: 30% of returning Iraq vets suffer mental ills. USA Today July 28, 2005. Available at: http://www.usatoday.com/news/health/2005-07-28-iraq-vets-health_x.htm?csp=34. Accessed Oct. 26, 2005.
5. Zoroya G. One in four Iraq vets ailing on return. USA Today Oct. 18, 2005. Available at: http://www.usatoday.com/news/world/iraq/2005-10-18-troops-side_x.htm. Accessed Oct. 26, 2005.
6. Zoroya G. Troops screened as never before. USA Today Oct. 18, 2005. Available at: http://www.usatoday.com/news/world/iraq/2005-10-18-troops-stress-side_x.htm. Accessed Oct. 26, 2005.
7. Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13-22.
8. Prigerson HG, Maciejewski PK, Rosenheck RA. Combat trauma: trauma with highest risk of delayed onset and unresolved posttraumatic stress disorder symptoms, unemployment, and abuse among men. J Nerv Ment Dis 2001;189:99-108.
9. Narrow WE, Rae DS, Robins LN, Regier DA. Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys’ estimates. Arch Gen Psychiatry 2002;59:115-23.
10. Lieberman HR, Bathalon GP, Falco CN, et al. Severe decrements in cognition, function and mood induced by sleep loss, heat, dehydration, and under-nutrition during simulated combat. Biol Psychiatry 2005;57:422-9.
11. Nemeroff CB, Bremner JD, Foa EB, et al. Posttraumatic stress disorder: a state-of-the-science review. J Psychiatr Res (In press; Oct 2005 epub ahead of publication).
12. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, text rev). Washington, DC: American Psychiatric Association; 2000.
13. Sareen J, Houlahan T, Cox BJ, Asmundson GJ. Anxiety disorders associated with suicidal ideation and suicide attempts in the national comorbidity survey. J Nerv Ment Dis 2005;193:450-4.
14. Xydakis MS, Fravell MD, Nasser KE, Casler JD. Analysis of battlefield head and neck injuries in Iraq and Afghanistan. Otolarnygol Head Neck Surg 2005;133:497-504.
15. Okie S. Traumatic brain injury in the war zone. N Engl J Med 2005;352(20):2043-7.
16. Cozza SJ, Benedek DM, Bradley JC, et al. Topics specific to the psychiatric treatment of military personnel. In: Schnurr PP, Cozza SJ (eds). Iraq War clinician guide (2nd ed). Washington, DC: National Center for PTSD. Walter Reed Army Medical Center; 2004:4-20. Available at: http://www.ncptsd.va.gov/war/iraq_clinician_guide_v2/iraq_clinician_guide_v2.pdf Accessed Oct. 26, 2005.
1. Benjamin M. How many have gone to war? Salon.com April 12, 2005. Available at: http://www.salon.com/news/feature/2005/04/12/troops_numbers/index_np.html. Accessed Dec. 13, 2005.
2. United States Government Accountability Office. Testimony before the Committee on Government Reform, House of Representatives. Reserve forces. Army National Guard’s role, organization, and equipment need to be reexamined. Oct. 20, 2005. Available at: http://www.gao.gov/new.items/d06170t.pdf. Accessed Oct. 26, 2005.
3. Wetzel K. Senators told of Guard struggles. Seattle Times Oct. 20, 2005. Available at: http://seattletimes.nwsource.com/html/local-news/2002571967_soldiers20m.html. Accessed Oct. 26, 2005.
4. Associated Press. Survey: 30% of returning Iraq vets suffer mental ills. USA Today July 28, 2005. Available at: http://www.usatoday.com/news/health/2005-07-28-iraq-vets-health_x.htm?csp=34. Accessed Oct. 26, 2005.
5. Zoroya G. One in four Iraq vets ailing on return. USA Today Oct. 18, 2005. Available at: http://www.usatoday.com/news/world/iraq/2005-10-18-troops-side_x.htm. Accessed Oct. 26, 2005.
6. Zoroya G. Troops screened as never before. USA Today Oct. 18, 2005. Available at: http://www.usatoday.com/news/world/iraq/2005-10-18-troops-stress-side_x.htm. Accessed Oct. 26, 2005.
7. Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13-22.
8. Prigerson HG, Maciejewski PK, Rosenheck RA. Combat trauma: trauma with highest risk of delayed onset and unresolved posttraumatic stress disorder symptoms, unemployment, and abuse among men. J Nerv Ment Dis 2001;189:99-108.
9. Narrow WE, Rae DS, Robins LN, Regier DA. Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys’ estimates. Arch Gen Psychiatry 2002;59:115-23.
10. Lieberman HR, Bathalon GP, Falco CN, et al. Severe decrements in cognition, function and mood induced by sleep loss, heat, dehydration, and under-nutrition during simulated combat. Biol Psychiatry 2005;57:422-9.
11. Nemeroff CB, Bremner JD, Foa EB, et al. Posttraumatic stress disorder: a state-of-the-science review. J Psychiatr Res (In press; Oct 2005 epub ahead of publication).
12. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, text rev). Washington, DC: American Psychiatric Association; 2000.
13. Sareen J, Houlahan T, Cox BJ, Asmundson GJ. Anxiety disorders associated with suicidal ideation and suicide attempts in the national comorbidity survey. J Nerv Ment Dis 2005;193:450-4.
14. Xydakis MS, Fravell MD, Nasser KE, Casler JD. Analysis of battlefield head and neck injuries in Iraq and Afghanistan. Otolarnygol Head Neck Surg 2005;133:497-504.
15. Okie S. Traumatic brain injury in the war zone. N Engl J Med 2005;352(20):2043-7.
16. Cozza SJ, Benedek DM, Bradley JC, et al. Topics specific to the psychiatric treatment of military personnel. In: Schnurr PP, Cozza SJ (eds). Iraq War clinician guide (2nd ed). Washington, DC: National Center for PTSD. Walter Reed Army Medical Center; 2004:4-20. Available at: http://www.ncptsd.va.gov/war/iraq_clinician_guide_v2/iraq_clinician_guide_v2.pdf Accessed Oct. 26, 2005.