User login
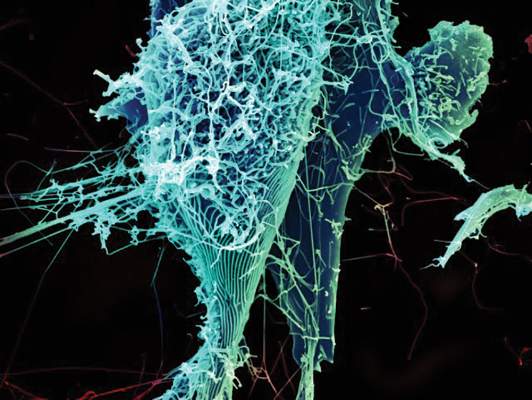
Experimental Ebola and Marburg Vaccines Safe, Well-Tolerated in Ugandan Adults
Experimental vaccines to prevent the Ebola and Marburg viruses were safe, well-tolerated, and produced similar results in Ugandan adults as in U.S. adults, according to findings published Dec. 22 in the Lancet.
In a randomized, phase I trial designed to evaluate the safety and immune response of two investigational vaccines, only one severe adverse event (neutropenia) was reported and was believed to be unrelated to the vaccine.
Dr. Julie E. Ledgerwood and colleagues at the National Institutes of Health studied 108 healthy adults aged 18-50 years in Kampala, Uganda from November 2009 to April 2010. Participants were randomized to receive either the Ebola (EBO) vaccine, the Marburg (MAR) vaccine, both vaccines, or placebo at the start of the study, and again after 4 and 8 weeks (Lancet 2014 [doi:10.1016/S0140-6736(14)62385-0].
Positive T-cell antibody responses were seen for the Ebola Sudan (SUDV) glycoprotein antigen in 43% of patients in the EBO vaccine group (95% confidence interval, 25-63), 3% of patients in the MAR vaccine–only group (95% CI, 0-18), and 33% of those in the group receiving both vaccines (95% CI, 17-53). T-cell responses for the Ebola Zaire (EBOV) glycoprotein were positive in 63% of patients in the EBO vaccine group (95% CI, 44-80), 3% of patients in the MAR vaccine–only group (95% CI, 0-18), and 33% of those in the group receiving both vaccines (95% CI, 17-53). Positive T-cell antibody responses were seen for the MARV glycoprotein antigen in 10% of patients in the EBO vaccine group (95% CI, 2-27), 52% of patients in the MAR vaccine–only group (95% CI, 33-71), and 43% of those in the group receiving both vaccines (95% CI, 25-63).
“This is the first clinical trial to assess an Ebola virus vaccine and a Marburg virus vaccine in an African population,” the authors said in the report.
Additionally, “safety and immunogenicity were similar in U.S. and Ugandan populations, which is important especially for a filovirus vaccine since the people at greatest risk of the disease reside mainly in Africa,” they added.
In an editorial accompanying the study, Dr. Saranya Sridhar of the Oxford University Centre for Clinical Vaccinology and Tropical Medicine comments that this trial could “provide some insight into what might be expected from the ongoing trials of virus-vectored Ebola virus vaccines in Africa.”
The similarity of the safety profile to that of a similar U.S. trial is encouraging in its possible implications for trials currently underway in Mali, he added (Lancet 2014 [doi:10.1016/S0140-6736(14)62445-4]).
“The international response to the present Ebola outbreak is an exemplar of the speed and purpose with which clinical vaccine development can progress and has set the benchmark against which future vaccine development must be judged,” he said.
The study was funded by the U.S. Department of Defense Infectious Disease Clinical Research Program and the U.S. National Institutes of Health Intramural Research Program. The authors did not disclose any conflicts of interest.
Experimental vaccines to prevent the Ebola and Marburg viruses were safe, well-tolerated, and produced similar results in Ugandan adults as in U.S. adults, according to findings published Dec. 22 in the Lancet.
In a randomized, phase I trial designed to evaluate the safety and immune response of two investigational vaccines, only one severe adverse event (neutropenia) was reported and was believed to be unrelated to the vaccine.
Dr. Julie E. Ledgerwood and colleagues at the National Institutes of Health studied 108 healthy adults aged 18-50 years in Kampala, Uganda from November 2009 to April 2010. Participants were randomized to receive either the Ebola (EBO) vaccine, the Marburg (MAR) vaccine, both vaccines, or placebo at the start of the study, and again after 4 and 8 weeks (Lancet 2014 [doi:10.1016/S0140-6736(14)62385-0].
Positive T-cell antibody responses were seen for the Ebola Sudan (SUDV) glycoprotein antigen in 43% of patients in the EBO vaccine group (95% confidence interval, 25-63), 3% of patients in the MAR vaccine–only group (95% CI, 0-18), and 33% of those in the group receiving both vaccines (95% CI, 17-53). T-cell responses for the Ebola Zaire (EBOV) glycoprotein were positive in 63% of patients in the EBO vaccine group (95% CI, 44-80), 3% of patients in the MAR vaccine–only group (95% CI, 0-18), and 33% of those in the group receiving both vaccines (95% CI, 17-53). Positive T-cell antibody responses were seen for the MARV glycoprotein antigen in 10% of patients in the EBO vaccine group (95% CI, 2-27), 52% of patients in the MAR vaccine–only group (95% CI, 33-71), and 43% of those in the group receiving both vaccines (95% CI, 25-63).
“This is the first clinical trial to assess an Ebola virus vaccine and a Marburg virus vaccine in an African population,” the authors said in the report.
Additionally, “safety and immunogenicity were similar in U.S. and Ugandan populations, which is important especially for a filovirus vaccine since the people at greatest risk of the disease reside mainly in Africa,” they added.
In an editorial accompanying the study, Dr. Saranya Sridhar of the Oxford University Centre for Clinical Vaccinology and Tropical Medicine comments that this trial could “provide some insight into what might be expected from the ongoing trials of virus-vectored Ebola virus vaccines in Africa.”
The similarity of the safety profile to that of a similar U.S. trial is encouraging in its possible implications for trials currently underway in Mali, he added (Lancet 2014 [doi:10.1016/S0140-6736(14)62445-4]).
“The international response to the present Ebola outbreak is an exemplar of the speed and purpose with which clinical vaccine development can progress and has set the benchmark against which future vaccine development must be judged,” he said.
The study was funded by the U.S. Department of Defense Infectious Disease Clinical Research Program and the U.S. National Institutes of Health Intramural Research Program. The authors did not disclose any conflicts of interest.
Experimental vaccines to prevent the Ebola and Marburg viruses were safe, well-tolerated, and produced similar results in Ugandan adults as in U.S. adults, according to findings published Dec. 22 in the Lancet.
In a randomized, phase I trial designed to evaluate the safety and immune response of two investigational vaccines, only one severe adverse event (neutropenia) was reported and was believed to be unrelated to the vaccine.
Dr. Julie E. Ledgerwood and colleagues at the National Institutes of Health studied 108 healthy adults aged 18-50 years in Kampala, Uganda from November 2009 to April 2010. Participants were randomized to receive either the Ebola (EBO) vaccine, the Marburg (MAR) vaccine, both vaccines, or placebo at the start of the study, and again after 4 and 8 weeks (Lancet 2014 [doi:10.1016/S0140-6736(14)62385-0].
Positive T-cell antibody responses were seen for the Ebola Sudan (SUDV) glycoprotein antigen in 43% of patients in the EBO vaccine group (95% confidence interval, 25-63), 3% of patients in the MAR vaccine–only group (95% CI, 0-18), and 33% of those in the group receiving both vaccines (95% CI, 17-53). T-cell responses for the Ebola Zaire (EBOV) glycoprotein were positive in 63% of patients in the EBO vaccine group (95% CI, 44-80), 3% of patients in the MAR vaccine–only group (95% CI, 0-18), and 33% of those in the group receiving both vaccines (95% CI, 17-53). Positive T-cell antibody responses were seen for the MARV glycoprotein antigen in 10% of patients in the EBO vaccine group (95% CI, 2-27), 52% of patients in the MAR vaccine–only group (95% CI, 33-71), and 43% of those in the group receiving both vaccines (95% CI, 25-63).
“This is the first clinical trial to assess an Ebola virus vaccine and a Marburg virus vaccine in an African population,” the authors said in the report.
Additionally, “safety and immunogenicity were similar in U.S. and Ugandan populations, which is important especially for a filovirus vaccine since the people at greatest risk of the disease reside mainly in Africa,” they added.
In an editorial accompanying the study, Dr. Saranya Sridhar of the Oxford University Centre for Clinical Vaccinology and Tropical Medicine comments that this trial could “provide some insight into what might be expected from the ongoing trials of virus-vectored Ebola virus vaccines in Africa.”
The similarity of the safety profile to that of a similar U.S. trial is encouraging in its possible implications for trials currently underway in Mali, he added (Lancet 2014 [doi:10.1016/S0140-6736(14)62445-4]).
“The international response to the present Ebola outbreak is an exemplar of the speed and purpose with which clinical vaccine development can progress and has set the benchmark against which future vaccine development must be judged,” he said.
The study was funded by the U.S. Department of Defense Infectious Disease Clinical Research Program and the U.S. National Institutes of Health Intramural Research Program. The authors did not disclose any conflicts of interest.
FROM THE LANCET
FDA Approves Four-Drug Combination for HCV
The Food and Drug Administration has approved the four-drug combination package Viekira Pak for the treatment of hepatitis C virus genotype 1 infection with or without cirrhosis, the agency announced December 19.
Viekira Pak is a combination of three new drugs, ombitasvir, paritaprevir, and dasabuvir; and the previously approved drug ritonavir. It can be taken with or without ribavirin but is not recommended for those with decompensated cirrhosis, the FDA said in a statement.
The FDA studied the drug combination’s efficacy in six clinical trials with 2,308 HCV patients, with or without cirrhosis. Patients were randomized to receive either Viekira Pak or placebo; Viekira Pak with or without ribavirin; or Viekira Pak with ribavirin for 12-24 weeks. Results showed that 91%-100% of participants who received the drug combination achieved sustained virologic response at least 12 weeks after treatment, the FDA said.
The most common side effects in trial participants were tiredness, itching, lack of energy, weakness, nausea, and trouble sleeping.
Viekira Pak is the fourth treatment approved for chronic hepatitis C virus in the past year. Simeprevir (Olysio); sofosbuvir (Sovaldi); and ledipasvir and sofosbuvir (Harvoni) were approved in November 2013, December 2013, and October 2014, respectively.
The recommended dosage for Viekira Pak is two ombitasvir, paritaprevir, and ritonavir tablets once per day at 12.5 mg, 75 mg, and 50 mg, respectively; and one 250-mg dasabuvir tablet twice per day.
The treatment was reviewed via FDA’s priority review program, which allows for expedited review of especially effective treatments for serious conditions.
Viekira Pak is marketed by AbbVie.
The Food and Drug Administration has approved the four-drug combination package Viekira Pak for the treatment of hepatitis C virus genotype 1 infection with or without cirrhosis, the agency announced December 19.
Viekira Pak is a combination of three new drugs, ombitasvir, paritaprevir, and dasabuvir; and the previously approved drug ritonavir. It can be taken with or without ribavirin but is not recommended for those with decompensated cirrhosis, the FDA said in a statement.
The FDA studied the drug combination’s efficacy in six clinical trials with 2,308 HCV patients, with or without cirrhosis. Patients were randomized to receive either Viekira Pak or placebo; Viekira Pak with or without ribavirin; or Viekira Pak with ribavirin for 12-24 weeks. Results showed that 91%-100% of participants who received the drug combination achieved sustained virologic response at least 12 weeks after treatment, the FDA said.
The most common side effects in trial participants were tiredness, itching, lack of energy, weakness, nausea, and trouble sleeping.
Viekira Pak is the fourth treatment approved for chronic hepatitis C virus in the past year. Simeprevir (Olysio); sofosbuvir (Sovaldi); and ledipasvir and sofosbuvir (Harvoni) were approved in November 2013, December 2013, and October 2014, respectively.
The recommended dosage for Viekira Pak is two ombitasvir, paritaprevir, and ritonavir tablets once per day at 12.5 mg, 75 mg, and 50 mg, respectively; and one 250-mg dasabuvir tablet twice per day.
The treatment was reviewed via FDA’s priority review program, which allows for expedited review of especially effective treatments for serious conditions.
Viekira Pak is marketed by AbbVie.
The Food and Drug Administration has approved the four-drug combination package Viekira Pak for the treatment of hepatitis C virus genotype 1 infection with or without cirrhosis, the agency announced December 19.
Viekira Pak is a combination of three new drugs, ombitasvir, paritaprevir, and dasabuvir; and the previously approved drug ritonavir. It can be taken with or without ribavirin but is not recommended for those with decompensated cirrhosis, the FDA said in a statement.
The FDA studied the drug combination’s efficacy in six clinical trials with 2,308 HCV patients, with or without cirrhosis. Patients were randomized to receive either Viekira Pak or placebo; Viekira Pak with or without ribavirin; or Viekira Pak with ribavirin for 12-24 weeks. Results showed that 91%-100% of participants who received the drug combination achieved sustained virologic response at least 12 weeks after treatment, the FDA said.
The most common side effects in trial participants were tiredness, itching, lack of energy, weakness, nausea, and trouble sleeping.
Viekira Pak is the fourth treatment approved for chronic hepatitis C virus in the past year. Simeprevir (Olysio); sofosbuvir (Sovaldi); and ledipasvir and sofosbuvir (Harvoni) were approved in November 2013, December 2013, and October 2014, respectively.
The recommended dosage for Viekira Pak is two ombitasvir, paritaprevir, and ritonavir tablets once per day at 12.5 mg, 75 mg, and 50 mg, respectively; and one 250-mg dasabuvir tablet twice per day.
The treatment was reviewed via FDA’s priority review program, which allows for expedited review of especially effective treatments for serious conditions.
Viekira Pak is marketed by AbbVie.
FDA approves four-drug combination for HCV
The Food and Drug Administration has approved the four-drug combination package Viekira Pak for the treatment of hepatitis C virus genotype 1 infection with or without cirrhosis, the agency announced December 19.
Viekira Pak is a combination of three new drugs, ombitasvir, paritaprevir, and dasabuvir; and the previously approved drug ritonavir. It can be taken with or without ribavirin but is not recommended for those with decompensated cirrhosis, the FDA said in a statement.
The FDA studied the drug combination’s efficacy in six clinical trials with 2,308 HCV patients, with or without cirrhosis. Patients were randomized to receive either Viekira Pak or placebo; Viekira Pak with or without ribavirin; or Viekira Pak with ribavirin for 12-24 weeks. Results showed that 91%-100% of participants who received the drug combination achieved sustained virologic response at least 12 weeks after treatment, the FDA said.
The most common side effects in trial participants were tiredness, itching, lack of energy, weakness, nausea, and trouble sleeping.
Viekira Pak is the fourth treatment approved for chronic hepatitis C virus in the past year. Simeprevir (Olysio); sofosbuvir (Sovaldi); and ledipasvir and sofosbuvir (Harvoni) were approved in November 2013, December 2013, and October 2014, respectively.
The recommended dosage for Viekira Pak is two ombitasvir, paritaprevir, and ritonavir tablets once per day at 12.5 mg, 75 mg, and 50 mg, respectively; and one 250-mg dasabuvir tablet twice per day.
The treatment was reviewed via FDA’s priority review program, which allows for expedited review of especially effective treatments for serious conditions.
Viekira Pak is marketed by AbbVie.
The Food and Drug Administration has approved the four-drug combination package Viekira Pak for the treatment of hepatitis C virus genotype 1 infection with or without cirrhosis, the agency announced December 19.
Viekira Pak is a combination of three new drugs, ombitasvir, paritaprevir, and dasabuvir; and the previously approved drug ritonavir. It can be taken with or without ribavirin but is not recommended for those with decompensated cirrhosis, the FDA said in a statement.
The FDA studied the drug combination’s efficacy in six clinical trials with 2,308 HCV patients, with or without cirrhosis. Patients were randomized to receive either Viekira Pak or placebo; Viekira Pak with or without ribavirin; or Viekira Pak with ribavirin for 12-24 weeks. Results showed that 91%-100% of participants who received the drug combination achieved sustained virologic response at least 12 weeks after treatment, the FDA said.
The most common side effects in trial participants were tiredness, itching, lack of energy, weakness, nausea, and trouble sleeping.
Viekira Pak is the fourth treatment approved for chronic hepatitis C virus in the past year. Simeprevir (Olysio); sofosbuvir (Sovaldi); and ledipasvir and sofosbuvir (Harvoni) were approved in November 2013, December 2013, and October 2014, respectively.
The recommended dosage for Viekira Pak is two ombitasvir, paritaprevir, and ritonavir tablets once per day at 12.5 mg, 75 mg, and 50 mg, respectively; and one 250-mg dasabuvir tablet twice per day.
The treatment was reviewed via FDA’s priority review program, which allows for expedited review of especially effective treatments for serious conditions.
Viekira Pak is marketed by AbbVie.
The Food and Drug Administration has approved the four-drug combination package Viekira Pak for the treatment of hepatitis C virus genotype 1 infection with or without cirrhosis, the agency announced December 19.
Viekira Pak is a combination of three new drugs, ombitasvir, paritaprevir, and dasabuvir; and the previously approved drug ritonavir. It can be taken with or without ribavirin but is not recommended for those with decompensated cirrhosis, the FDA said in a statement.
The FDA studied the drug combination’s efficacy in six clinical trials with 2,308 HCV patients, with or without cirrhosis. Patients were randomized to receive either Viekira Pak or placebo; Viekira Pak with or without ribavirin; or Viekira Pak with ribavirin for 12-24 weeks. Results showed that 91%-100% of participants who received the drug combination achieved sustained virologic response at least 12 weeks after treatment, the FDA said.
The most common side effects in trial participants were tiredness, itching, lack of energy, weakness, nausea, and trouble sleeping.
Viekira Pak is the fourth treatment approved for chronic hepatitis C virus in the past year. Simeprevir (Olysio); sofosbuvir (Sovaldi); and ledipasvir and sofosbuvir (Harvoni) were approved in November 2013, December 2013, and October 2014, respectively.
The recommended dosage for Viekira Pak is two ombitasvir, paritaprevir, and ritonavir tablets once per day at 12.5 mg, 75 mg, and 50 mg, respectively; and one 250-mg dasabuvir tablet twice per day.
The treatment was reviewed via FDA’s priority review program, which allows for expedited review of especially effective treatments for serious conditions.
Viekira Pak is marketed by AbbVie.
Few Receive Evidence-based Counseling About Sex After Myocardial Infarction
Though most men and women are willing to discuss sexual issues with a doctor, very few patients were counseled about sexual activity in the month following acute myocardial infarction, according to results of the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) study, published Dec. 15 in Circulation.
Just 12% of women and 19% of men discussed sex with their physician after AMI, though 84% of women and 91% of men said they were comfortable having such a conversation with their doctor, reported Dr. Stacy Tessler Lindau of the University of Chicago, and her associates.
“Our findings indicate that U.S. and Spanish physicians rarely counsel younger AMI patients, especially women, about resuming sexual activity even though the large majority of these patients were sexually active in the year before their event, valued sexuality as an important part of life before and after AMI, and felt it was appropriate for physicians to initiate discussion of sexual matters in the context of AMI care,” the authors said in the report (Circulation 2014 Dec. 15 [doi:10.1161/circulationaha.114.012709]).
Dr. Lindau and colleagues recruited 2,349 women and 1,152 men in the United States and Spain who were hospitalized for AMI during August 2008–January 2012. Patients were between 18 and 55 years of age. In-person interviews were conducted during hospitalization to collect data on partner status, sexual activity, and sexual attitudes. Follow-up was conducted 1 month later via phone interviews and included questions about sexual activity, attitudes, function, and physician counseling.
Overall, 12% of women and 19% of men had discussed sex with their physician. Sexual activity at baseline significantly increased the likelihood of having the discussion: 15% of sexually active women, compared with 4% of sexually inactive women had the discussion, and 20% and 8% of men, respectively, said they had discussed sex with their physician. In the United States, most discussions were initiated by the patient, whereas in Spain, the doctor more frequently initiated the discussion, a statistically significant difference.
Continue for more on next page >>
Among patients whose doctor issued restrictions on sexual activity, 35% were advised to limit sex, 26% to take a passive role, and 23% to keep heart rate down.
Female sex was significantly associated with no counseling (relative risk, 1.07), as was older age (RR, 1.05) and sexual inactivity at baseline (RR, 1.11). Women in Spain were significantly more likely than women in the United States to be advised to restrict sexual activity (RR, 1.36).
Guidelines from the American College of Cardiology, American Heart Association, and European Society of Cardiology all recommend that physicians counsel patients about sexual activity, and that sex can be resumed as long as the patient is able to tolerate mild to moderate physical activity.
“Physicians could meaningfully narrow the gap between guidelines and practice by adding permission to resume sex to routine counseling about returning to work and exercise,” the authors said. Using patient-centered tools to incorporate this into practice “could help improve outcomes and quality of life for younger women and men with AMI,” they added.
The study was supported by grants from the National Institutes of Health and the Fondo de Investigacion Sanitaria del Salud Carlo III. The authors disclosed relationships with Medtronic, UnitedHealth, AstraZeneca, Bayer, and numerous other pharmaceutical companies.
Though most men and women are willing to discuss sexual issues with a doctor, very few patients were counseled about sexual activity in the month following acute myocardial infarction, according to results of the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) study, published Dec. 15 in Circulation.
Just 12% of women and 19% of men discussed sex with their physician after AMI, though 84% of women and 91% of men said they were comfortable having such a conversation with their doctor, reported Dr. Stacy Tessler Lindau of the University of Chicago, and her associates.
“Our findings indicate that U.S. and Spanish physicians rarely counsel younger AMI patients, especially women, about resuming sexual activity even though the large majority of these patients were sexually active in the year before their event, valued sexuality as an important part of life before and after AMI, and felt it was appropriate for physicians to initiate discussion of sexual matters in the context of AMI care,” the authors said in the report (Circulation 2014 Dec. 15 [doi:10.1161/circulationaha.114.012709]).
Dr. Lindau and colleagues recruited 2,349 women and 1,152 men in the United States and Spain who were hospitalized for AMI during August 2008–January 2012. Patients were between 18 and 55 years of age. In-person interviews were conducted during hospitalization to collect data on partner status, sexual activity, and sexual attitudes. Follow-up was conducted 1 month later via phone interviews and included questions about sexual activity, attitudes, function, and physician counseling.
Overall, 12% of women and 19% of men had discussed sex with their physician. Sexual activity at baseline significantly increased the likelihood of having the discussion: 15% of sexually active women, compared with 4% of sexually inactive women had the discussion, and 20% and 8% of men, respectively, said they had discussed sex with their physician. In the United States, most discussions were initiated by the patient, whereas in Spain, the doctor more frequently initiated the discussion, a statistically significant difference.
Continue for more on next page >>
Among patients whose doctor issued restrictions on sexual activity, 35% were advised to limit sex, 26% to take a passive role, and 23% to keep heart rate down.
Female sex was significantly associated with no counseling (relative risk, 1.07), as was older age (RR, 1.05) and sexual inactivity at baseline (RR, 1.11). Women in Spain were significantly more likely than women in the United States to be advised to restrict sexual activity (RR, 1.36).
Guidelines from the American College of Cardiology, American Heart Association, and European Society of Cardiology all recommend that physicians counsel patients about sexual activity, and that sex can be resumed as long as the patient is able to tolerate mild to moderate physical activity.
“Physicians could meaningfully narrow the gap between guidelines and practice by adding permission to resume sex to routine counseling about returning to work and exercise,” the authors said. Using patient-centered tools to incorporate this into practice “could help improve outcomes and quality of life for younger women and men with AMI,” they added.
The study was supported by grants from the National Institutes of Health and the Fondo de Investigacion Sanitaria del Salud Carlo III. The authors disclosed relationships with Medtronic, UnitedHealth, AstraZeneca, Bayer, and numerous other pharmaceutical companies.
Though most men and women are willing to discuss sexual issues with a doctor, very few patients were counseled about sexual activity in the month following acute myocardial infarction, according to results of the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) study, published Dec. 15 in Circulation.
Just 12% of women and 19% of men discussed sex with their physician after AMI, though 84% of women and 91% of men said they were comfortable having such a conversation with their doctor, reported Dr. Stacy Tessler Lindau of the University of Chicago, and her associates.
“Our findings indicate that U.S. and Spanish physicians rarely counsel younger AMI patients, especially women, about resuming sexual activity even though the large majority of these patients were sexually active in the year before their event, valued sexuality as an important part of life before and after AMI, and felt it was appropriate for physicians to initiate discussion of sexual matters in the context of AMI care,” the authors said in the report (Circulation 2014 Dec. 15 [doi:10.1161/circulationaha.114.012709]).
Dr. Lindau and colleagues recruited 2,349 women and 1,152 men in the United States and Spain who were hospitalized for AMI during August 2008–January 2012. Patients were between 18 and 55 years of age. In-person interviews were conducted during hospitalization to collect data on partner status, sexual activity, and sexual attitudes. Follow-up was conducted 1 month later via phone interviews and included questions about sexual activity, attitudes, function, and physician counseling.
Overall, 12% of women and 19% of men had discussed sex with their physician. Sexual activity at baseline significantly increased the likelihood of having the discussion: 15% of sexually active women, compared with 4% of sexually inactive women had the discussion, and 20% and 8% of men, respectively, said they had discussed sex with their physician. In the United States, most discussions were initiated by the patient, whereas in Spain, the doctor more frequently initiated the discussion, a statistically significant difference.
Continue for more on next page >>
Among patients whose doctor issued restrictions on sexual activity, 35% were advised to limit sex, 26% to take a passive role, and 23% to keep heart rate down.
Female sex was significantly associated with no counseling (relative risk, 1.07), as was older age (RR, 1.05) and sexual inactivity at baseline (RR, 1.11). Women in Spain were significantly more likely than women in the United States to be advised to restrict sexual activity (RR, 1.36).
Guidelines from the American College of Cardiology, American Heart Association, and European Society of Cardiology all recommend that physicians counsel patients about sexual activity, and that sex can be resumed as long as the patient is able to tolerate mild to moderate physical activity.
“Physicians could meaningfully narrow the gap between guidelines and practice by adding permission to resume sex to routine counseling about returning to work and exercise,” the authors said. Using patient-centered tools to incorporate this into practice “could help improve outcomes and quality of life for younger women and men with AMI,” they added.
The study was supported by grants from the National Institutes of Health and the Fondo de Investigacion Sanitaria del Salud Carlo III. The authors disclosed relationships with Medtronic, UnitedHealth, AstraZeneca, Bayer, and numerous other pharmaceutical companies.
FROM CIRCULATION
Few receive evidence-based counseling about sex after myocardial infarction
Though most men and women are willing to discuss sexual issues with a doctor, very few patients were counseled about sexual activity in the month following acute myocardial infarction, according to results of the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) study, published Dec. 15 in Circulation.
Just 12% of women and 19% of men discussed sex with their physician after AMI, though 84% of women and 91% of men said they were comfortable having such a conversation with their doctor, reported Dr. Stacy Tessler Lindau of the University of Chicago, and her associates.
“Our findings indicate that U.S. and Spanish physicians rarely counsel younger AMI patients, especially women, about resuming sexual activity even though the large majority of these patients were sexually active in the year before their event, valued sexuality as an important part of life before and after AMI, and felt it was appropriate for physicians to initiate discussion of sexual matters in the context of AMI care,” the authors said in the report (Circulation 2014 Dec. 15 [doi:10.1161/circulationaha.114.012709]).
Dr. Lindau and colleagues recruited 2,349 women and 1,152 men in the United States and Spain who were hospitalized for AMI during August 2008–January 2012. Patients were between 18 and 55 years of age. In-person interviews were conducted during hospitalization to collect data on partner status, sexual activity, and sexual attitudes. Follow-up was conducted 1 month later via phone interviews and included questions about sexual activity, attitudes, function, and physician counseling.
Overall, 12% of women and 19% of men had discussed sex with their physician. Sexual activity at baseline significantly increased the likelihood of having the discussion: 15% of sexually active women, compared with 4% of sexually inactive women had the discussion, and 20% and 8% of men, respectively, said they had discussed sex with their physician. In the United States, most discussions were initiated by the patient, whereas in Spain, the doctor more frequently initiated the discussion, a statistically significant difference.
Among patients whose doctor issued restrictions on sexual activity, 35% were advised to limit sex, 26% to take a passive role, and 23% to keep heart rate down.
Female sex was significantly associated with no counseling (relative risk, 1.07), as was older age (RR, 1.05) and sexual inactivity at baseline (RR, 1.11). Women in Spain were significantly more likely than women in the United States to be advised to restrict sexual activity (RR, 1.36).
Guidelines from the American College of Cardiology, American Heart Association, and European Society of Cardiology all recommend that physicians counsel patients about sexual activity, and that sex can be resumed as long as the patient is able to tolerate mild to moderate physical activity.
“Physicians could meaningfully narrow the gap between guidelines and practice by adding permission to resume sex to routine counseling about returning to work and exercise,” the authors said. Using patient-centered tools to incorporate this into practice “could help improve outcomes and quality of life for younger women and men with AMI,” they added.
The study was supported by grants from the National Institutes of Health and the Fondo de Investigacion Sanitaria del Salud Carlo III. The authors disclosed relationships with Medtronic, UnitedHealth, AstraZeneca, Bayer, and numerous other pharmaceutical companies.
Though most men and women are willing to discuss sexual issues with a doctor, very few patients were counseled about sexual activity in the month following acute myocardial infarction, according to results of the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) study, published Dec. 15 in Circulation.
Just 12% of women and 19% of men discussed sex with their physician after AMI, though 84% of women and 91% of men said they were comfortable having such a conversation with their doctor, reported Dr. Stacy Tessler Lindau of the University of Chicago, and her associates.
“Our findings indicate that U.S. and Spanish physicians rarely counsel younger AMI patients, especially women, about resuming sexual activity even though the large majority of these patients were sexually active in the year before their event, valued sexuality as an important part of life before and after AMI, and felt it was appropriate for physicians to initiate discussion of sexual matters in the context of AMI care,” the authors said in the report (Circulation 2014 Dec. 15 [doi:10.1161/circulationaha.114.012709]).
Dr. Lindau and colleagues recruited 2,349 women and 1,152 men in the United States and Spain who were hospitalized for AMI during August 2008–January 2012. Patients were between 18 and 55 years of age. In-person interviews were conducted during hospitalization to collect data on partner status, sexual activity, and sexual attitudes. Follow-up was conducted 1 month later via phone interviews and included questions about sexual activity, attitudes, function, and physician counseling.
Overall, 12% of women and 19% of men had discussed sex with their physician. Sexual activity at baseline significantly increased the likelihood of having the discussion: 15% of sexually active women, compared with 4% of sexually inactive women had the discussion, and 20% and 8% of men, respectively, said they had discussed sex with their physician. In the United States, most discussions were initiated by the patient, whereas in Spain, the doctor more frequently initiated the discussion, a statistically significant difference.
Among patients whose doctor issued restrictions on sexual activity, 35% were advised to limit sex, 26% to take a passive role, and 23% to keep heart rate down.
Female sex was significantly associated with no counseling (relative risk, 1.07), as was older age (RR, 1.05) and sexual inactivity at baseline (RR, 1.11). Women in Spain were significantly more likely than women in the United States to be advised to restrict sexual activity (RR, 1.36).
Guidelines from the American College of Cardiology, American Heart Association, and European Society of Cardiology all recommend that physicians counsel patients about sexual activity, and that sex can be resumed as long as the patient is able to tolerate mild to moderate physical activity.
“Physicians could meaningfully narrow the gap between guidelines and practice by adding permission to resume sex to routine counseling about returning to work and exercise,” the authors said. Using patient-centered tools to incorporate this into practice “could help improve outcomes and quality of life for younger women and men with AMI,” they added.
The study was supported by grants from the National Institutes of Health and the Fondo de Investigacion Sanitaria del Salud Carlo III. The authors disclosed relationships with Medtronic, UnitedHealth, AstraZeneca, Bayer, and numerous other pharmaceutical companies.
Though most men and women are willing to discuss sexual issues with a doctor, very few patients were counseled about sexual activity in the month following acute myocardial infarction, according to results of the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) study, published Dec. 15 in Circulation.
Just 12% of women and 19% of men discussed sex with their physician after AMI, though 84% of women and 91% of men said they were comfortable having such a conversation with their doctor, reported Dr. Stacy Tessler Lindau of the University of Chicago, and her associates.
“Our findings indicate that U.S. and Spanish physicians rarely counsel younger AMI patients, especially women, about resuming sexual activity even though the large majority of these patients were sexually active in the year before their event, valued sexuality as an important part of life before and after AMI, and felt it was appropriate for physicians to initiate discussion of sexual matters in the context of AMI care,” the authors said in the report (Circulation 2014 Dec. 15 [doi:10.1161/circulationaha.114.012709]).
Dr. Lindau and colleagues recruited 2,349 women and 1,152 men in the United States and Spain who were hospitalized for AMI during August 2008–January 2012. Patients were between 18 and 55 years of age. In-person interviews were conducted during hospitalization to collect data on partner status, sexual activity, and sexual attitudes. Follow-up was conducted 1 month later via phone interviews and included questions about sexual activity, attitudes, function, and physician counseling.
Overall, 12% of women and 19% of men had discussed sex with their physician. Sexual activity at baseline significantly increased the likelihood of having the discussion: 15% of sexually active women, compared with 4% of sexually inactive women had the discussion, and 20% and 8% of men, respectively, said they had discussed sex with their physician. In the United States, most discussions were initiated by the patient, whereas in Spain, the doctor more frequently initiated the discussion, a statistically significant difference.
Among patients whose doctor issued restrictions on sexual activity, 35% were advised to limit sex, 26% to take a passive role, and 23% to keep heart rate down.
Female sex was significantly associated with no counseling (relative risk, 1.07), as was older age (RR, 1.05) and sexual inactivity at baseline (RR, 1.11). Women in Spain were significantly more likely than women in the United States to be advised to restrict sexual activity (RR, 1.36).
Guidelines from the American College of Cardiology, American Heart Association, and European Society of Cardiology all recommend that physicians counsel patients about sexual activity, and that sex can be resumed as long as the patient is able to tolerate mild to moderate physical activity.
“Physicians could meaningfully narrow the gap between guidelines and practice by adding permission to resume sex to routine counseling about returning to work and exercise,” the authors said. Using patient-centered tools to incorporate this into practice “could help improve outcomes and quality of life for younger women and men with AMI,” they added.
The study was supported by grants from the National Institutes of Health and the Fondo de Investigacion Sanitaria del Salud Carlo III. The authors disclosed relationships with Medtronic, UnitedHealth, AstraZeneca, Bayer, and numerous other pharmaceutical companies.
FROM CIRCULATION
Key clinical point: Most patients, especially women, do not receive guidelines-based counseling about sexual activity following acute myocardial infarction.
Major finding: 12% of women and 19% of men reported having a discussion with their doctor about sex after AMI, with female gender being significantly associated with no counseling.
Data source: A prospective, longitudinal study of 2,349 women and 1,152 men with AMI aged 18-55 years in the United States and Spain.
Disclosures: The study was supported by grants from the National Institutes of Health and the Fondo de Investigacion Sanitaria del Salud Carlo III. The authors disclosed relationships with Medtronic, UnitedHealth, AstraZeneca, Bayer, and numerous other pharmaceutical companies.
Presepsin is an accurate biomarker for late-onset sepsis in preterm newborns
Presepsin is an accurate biomarker for sepsis in premature infants, according to findings published Dec. 15 in the journal Pediatrics.
Investigators from the Careggi University Hospital in Florence, Italy, sampled cultured blood taken from in 40 newborns in the hospital’s neonatal intensive care unit, 19 of whom had late-onset sepsis (LOS). Over the course of the study, presepsin (P-SEP) values were higher in infants with LOS (median = 1,295 ng/L in LOS infants, vs. median = 562 ng/L in controls). Additionally, P-SEP achieved the best accuracy for prediction of sepsis, compared with other biomarkers, at a cutoff value of 885 ng/L with 94% sensitivity (95% confidence interval, 74-100) and 100% specificity (95% CI, 84-100), according to Dr. Chiara Poggi and her associates.
“Our study is the first that investigates the possible role of P-SEP in the diagnosis of LOS in preterm infants,” the investigators wrote. The results confirm findings of previous studies in adult septic patients showing significantly higher P-SEP levels in those with sepsis, they added (Pediatrics 2014 Dec. 15 [doi: 10.1542/peds.2014-1755]).
In the LOS group, blood was sampled for P-SEP, procalcitonin (PCT), and C-reactive protein (CRP) at time of enrollment and again after 1, 3, and 5 days. P-SEP values alone were extracted in the control group. Infants were born at 32 weeks’ gestational age or earlier and were between 4 and 60 days postnatal age at the time of enrollment in the study.
Late-onset sepsis was defined as sepsis occurring after 72 hours of life. Symptoms of infection were rectal temperature instability, pulmonary dysfunction, new-onset crisis of apnea, feeding intolerance, lethargy, bradycardia or tachycardia, hypotension, ashen appearance, and coagulopathy, in addition to abnormal laboratory measures of metabolic acidosis, and hyperglycemia or hypoglycemia.
The study was conducted from May 2013 to April 2014. Over this period, LOS incidence was 11.4%. In the group of LOS infants, 14 infants had severe sepsis, 5 had septic shock, and 2 died. Prophylactic antibiotics were administered upon NICU admission, and were stopped if bacterial cultures came back negative with no symptoms present after 3 or 4 days.
P-SEP values were higher in the LOS group at all four points of blood culture analysis but did not vary in the control group.
The study of P-SEP as a potential predictor of sepsis is important because of the limitations of the CRP and PCT biomarkers, the authors said. Though CRP is commonly used to diagnose sepsis, “its utility is questionable because its peak values are reached only after a 2-3 day delay after the infective stimulus” its value can increase after noninfective inflammatory events, they said. On the other hand, PCT peak values present just 10-12 hours after infection and have not been adequately studied for sepsis diagnosis, they added.
Though the results of the study are “promising,” studies in larger populations are needed to confirm the role of P-SEP as a predictor of sepsis in preterm infants, the investigators said.
“If our results are confirmed, we are confident that P-SEP can be included as a marker that increases the accuracy of sepsis screening for early diagnosis of suspected LOS in preterm infants,” they said.
Dr. Poggi and her colleagues did not report any financial disclosures or conflicts of interest.
Presepsin is an accurate biomarker for sepsis in premature infants, according to findings published Dec. 15 in the journal Pediatrics.
Investigators from the Careggi University Hospital in Florence, Italy, sampled cultured blood taken from in 40 newborns in the hospital’s neonatal intensive care unit, 19 of whom had late-onset sepsis (LOS). Over the course of the study, presepsin (P-SEP) values were higher in infants with LOS (median = 1,295 ng/L in LOS infants, vs. median = 562 ng/L in controls). Additionally, P-SEP achieved the best accuracy for prediction of sepsis, compared with other biomarkers, at a cutoff value of 885 ng/L with 94% sensitivity (95% confidence interval, 74-100) and 100% specificity (95% CI, 84-100), according to Dr. Chiara Poggi and her associates.
“Our study is the first that investigates the possible role of P-SEP in the diagnosis of LOS in preterm infants,” the investigators wrote. The results confirm findings of previous studies in adult septic patients showing significantly higher P-SEP levels in those with sepsis, they added (Pediatrics 2014 Dec. 15 [doi: 10.1542/peds.2014-1755]).
In the LOS group, blood was sampled for P-SEP, procalcitonin (PCT), and C-reactive protein (CRP) at time of enrollment and again after 1, 3, and 5 days. P-SEP values alone were extracted in the control group. Infants were born at 32 weeks’ gestational age or earlier and were between 4 and 60 days postnatal age at the time of enrollment in the study.
Late-onset sepsis was defined as sepsis occurring after 72 hours of life. Symptoms of infection were rectal temperature instability, pulmonary dysfunction, new-onset crisis of apnea, feeding intolerance, lethargy, bradycardia or tachycardia, hypotension, ashen appearance, and coagulopathy, in addition to abnormal laboratory measures of metabolic acidosis, and hyperglycemia or hypoglycemia.
The study was conducted from May 2013 to April 2014. Over this period, LOS incidence was 11.4%. In the group of LOS infants, 14 infants had severe sepsis, 5 had septic shock, and 2 died. Prophylactic antibiotics were administered upon NICU admission, and were stopped if bacterial cultures came back negative with no symptoms present after 3 or 4 days.
P-SEP values were higher in the LOS group at all four points of blood culture analysis but did not vary in the control group.
The study of P-SEP as a potential predictor of sepsis is important because of the limitations of the CRP and PCT biomarkers, the authors said. Though CRP is commonly used to diagnose sepsis, “its utility is questionable because its peak values are reached only after a 2-3 day delay after the infective stimulus” its value can increase after noninfective inflammatory events, they said. On the other hand, PCT peak values present just 10-12 hours after infection and have not been adequately studied for sepsis diagnosis, they added.
Though the results of the study are “promising,” studies in larger populations are needed to confirm the role of P-SEP as a predictor of sepsis in preterm infants, the investigators said.
“If our results are confirmed, we are confident that P-SEP can be included as a marker that increases the accuracy of sepsis screening for early diagnosis of suspected LOS in preterm infants,” they said.
Dr. Poggi and her colleagues did not report any financial disclosures or conflicts of interest.
Presepsin is an accurate biomarker for sepsis in premature infants, according to findings published Dec. 15 in the journal Pediatrics.
Investigators from the Careggi University Hospital in Florence, Italy, sampled cultured blood taken from in 40 newborns in the hospital’s neonatal intensive care unit, 19 of whom had late-onset sepsis (LOS). Over the course of the study, presepsin (P-SEP) values were higher in infants with LOS (median = 1,295 ng/L in LOS infants, vs. median = 562 ng/L in controls). Additionally, P-SEP achieved the best accuracy for prediction of sepsis, compared with other biomarkers, at a cutoff value of 885 ng/L with 94% sensitivity (95% confidence interval, 74-100) and 100% specificity (95% CI, 84-100), according to Dr. Chiara Poggi and her associates.
“Our study is the first that investigates the possible role of P-SEP in the diagnosis of LOS in preterm infants,” the investigators wrote. The results confirm findings of previous studies in adult septic patients showing significantly higher P-SEP levels in those with sepsis, they added (Pediatrics 2014 Dec. 15 [doi: 10.1542/peds.2014-1755]).
In the LOS group, blood was sampled for P-SEP, procalcitonin (PCT), and C-reactive protein (CRP) at time of enrollment and again after 1, 3, and 5 days. P-SEP values alone were extracted in the control group. Infants were born at 32 weeks’ gestational age or earlier and were between 4 and 60 days postnatal age at the time of enrollment in the study.
Late-onset sepsis was defined as sepsis occurring after 72 hours of life. Symptoms of infection were rectal temperature instability, pulmonary dysfunction, new-onset crisis of apnea, feeding intolerance, lethargy, bradycardia or tachycardia, hypotension, ashen appearance, and coagulopathy, in addition to abnormal laboratory measures of metabolic acidosis, and hyperglycemia or hypoglycemia.
The study was conducted from May 2013 to April 2014. Over this period, LOS incidence was 11.4%. In the group of LOS infants, 14 infants had severe sepsis, 5 had septic shock, and 2 died. Prophylactic antibiotics were administered upon NICU admission, and were stopped if bacterial cultures came back negative with no symptoms present after 3 or 4 days.
P-SEP values were higher in the LOS group at all four points of blood culture analysis but did not vary in the control group.
The study of P-SEP as a potential predictor of sepsis is important because of the limitations of the CRP and PCT biomarkers, the authors said. Though CRP is commonly used to diagnose sepsis, “its utility is questionable because its peak values are reached only after a 2-3 day delay after the infective stimulus” its value can increase after noninfective inflammatory events, they said. On the other hand, PCT peak values present just 10-12 hours after infection and have not been adequately studied for sepsis diagnosis, they added.
Though the results of the study are “promising,” studies in larger populations are needed to confirm the role of P-SEP as a predictor of sepsis in preterm infants, the investigators said.
“If our results are confirmed, we are confident that P-SEP can be included as a marker that increases the accuracy of sepsis screening for early diagnosis of suspected LOS in preterm infants,” they said.
Dr. Poggi and her colleagues did not report any financial disclosures or conflicts of interest.
FROM PEDIATRICS
Key clinical point: Presepsin may be a useful biomarker for late-onset sepsis in preterm infants.
Major finding: P-SEP values were higher in infants with LOS over the course of the study (median = 1,295 ng/L in LOS infants vs. median = 562 ng/L in controls), and achieved the best accuracy for prediction of sepsis compared with other biomarkers, at a cutoff value of 885 ng/L with 94% sensitivity (95% CI, 74-100) and 100% specificity (95% CI, 84-100).
Data source: A prospective study of 19 newborns with LOS and 21 uninfected controls, born at 32 weeks gestational age or earlier.
Disclosures: The investigators did not report any financial disclosures or conflicts of interest.
CDC offers pediatric health care providers resources on Ebola in children
Children’s needs differ significantly from the needs of adults, especially when it comes to handling dire situations like the current Ebola outbreak in West Africa that has resulted in a few cases in the United States.
Children may be at increased risk for developing the infection if they have recently traveled to one of the countries experiencing an outbreak. However, since they are very unlikely to be caregivers or participate in funeral activities that raise the risk of exposure, the chances of a child in the United States developing Ebola is very low, according to the Centers for Disease Control and Prevention.
Because information about Ebola can be scary and alarming for children, it is important for healthcare providers to recognize and address their developmental and psychological needs to help them better understand facts about the illness and their risk of exposure. It also helps to be prepared just in case the need arises to address a potential Ebola case.
The CDC recommends the following resources to guide health care providers who work with children:
1. Ebola Virus Disease and Children: What US Pediatricians Need to Know
2. What Obstetrician–Gynecologists Should Know About Ebola
3. Information for Healthcare Workers and Settings
4. Algorithm for Evaluation of the Returned Traveler
5. Checklist for Patients Being Evaluated for Ebola Virus Disease (EVD) in the United States
6. Interim Guidance for Environmental Infection Control in Hospitals for Ebola Virus
7. Ebola Preparedness Considerations for Outpatient/Ambulatory Care Centers
8. Ebola Screening Criteria for Outpatient/Ambulatory Care Centers
Children’s needs differ significantly from the needs of adults, especially when it comes to handling dire situations like the current Ebola outbreak in West Africa that has resulted in a few cases in the United States.
Children may be at increased risk for developing the infection if they have recently traveled to one of the countries experiencing an outbreak. However, since they are very unlikely to be caregivers or participate in funeral activities that raise the risk of exposure, the chances of a child in the United States developing Ebola is very low, according to the Centers for Disease Control and Prevention.
Because information about Ebola can be scary and alarming for children, it is important for healthcare providers to recognize and address their developmental and psychological needs to help them better understand facts about the illness and their risk of exposure. It also helps to be prepared just in case the need arises to address a potential Ebola case.
The CDC recommends the following resources to guide health care providers who work with children:
1. Ebola Virus Disease and Children: What US Pediatricians Need to Know
2. What Obstetrician–Gynecologists Should Know About Ebola
3. Information for Healthcare Workers and Settings
4. Algorithm for Evaluation of the Returned Traveler
5. Checklist for Patients Being Evaluated for Ebola Virus Disease (EVD) in the United States
6. Interim Guidance for Environmental Infection Control in Hospitals for Ebola Virus
7. Ebola Preparedness Considerations for Outpatient/Ambulatory Care Centers
8. Ebola Screening Criteria for Outpatient/Ambulatory Care Centers
Children’s needs differ significantly from the needs of adults, especially when it comes to handling dire situations like the current Ebola outbreak in West Africa that has resulted in a few cases in the United States.
Children may be at increased risk for developing the infection if they have recently traveled to one of the countries experiencing an outbreak. However, since they are very unlikely to be caregivers or participate in funeral activities that raise the risk of exposure, the chances of a child in the United States developing Ebola is very low, according to the Centers for Disease Control and Prevention.
Because information about Ebola can be scary and alarming for children, it is important for healthcare providers to recognize and address their developmental and psychological needs to help them better understand facts about the illness and their risk of exposure. It also helps to be prepared just in case the need arises to address a potential Ebola case.
The CDC recommends the following resources to guide health care providers who work with children:
1. Ebola Virus Disease and Children: What US Pediatricians Need to Know
2. What Obstetrician–Gynecologists Should Know About Ebola
3. Information for Healthcare Workers and Settings
4. Algorithm for Evaluation of the Returned Traveler
5. Checklist for Patients Being Evaluated for Ebola Virus Disease (EVD) in the United States
6. Interim Guidance for Environmental Infection Control in Hospitals for Ebola Virus
7. Ebola Preparedness Considerations for Outpatient/Ambulatory Care Centers
8. Ebola Screening Criteria for Outpatient/Ambulatory Care Centers
Long-term depression prevalent in schizophrenia patients
Persistent depression, or “trait” depression, was significantly higher in patients with schizophrenia than in controls, and was associated with more severe psychosis, a study showed.
Trait depression was not, however, associated with cognitive impairment or decreased white matter integrity, wrote Dr. Joshua J. Chiappelli and his colleagues.
Characterized by “the tendency to experience negative emotions and distressing thoughts” consistently over time, trait depression is distinct from state depression, which includes only current symptoms, said the investigators, who are affiliated with the Maryland Psychiatric Research Center at the University of Maryland in Baltimore.
The study authors examined the association of trait depression with cognitive deficits, functional capacity impairment, and white matter integrity in 126 patients and 151 controls recruited from the Maryland Psychiatric Research Center. Participants completed the Maryland Trait and State Depression (MTSD) questionnaire, which asked 36 questions about the frequency of depressive symptoms over the past week (state questions) and over the course of adult life (trait questions). Cognition was assessed using the Digit Symbol Coding task of the Wechsler Adult Intelligence Scale and the Digital Sequencing task from the Brief Assessment of Cognition in Schizophrenia.
White matter integrity was determined by the measure of fractional anistropy (FA) on a diffusion MRI (Schizophr. Res. 2014;159:243-8).
Severity of both trait and state depression in schizophrenia patients was significantly and positively associated with scores on the Brief Psychiatric Rating Scale (rho = 0.246, P = .005; rho = 0.312, P <.001, respectivley). However, a higher MTSD score was not associated with severe cognitive deficits; in fact, severe trait depression was significantly associated with working memory, processing speed, and functional capacity (rho = 0.186, P = .044; rho=0.206, P = .024; rho = 0.220, P = .017, respectively).
Whole brain FA values were higher in controls than in patients with schizophrenia (FA = 11.86, P = .001). In addition, higher trait depression scores were significantly associated with higher FA values in schizophrenia patients.
“These findings appear paradoxical, especially when examined in comparison to major depressive disorder,” as severity is typically linked to worse cognition, the study authors wrote.
These findings “raise an interesting question on whether trait depression is a relatively separate clinical domain,” compared with major depressive symptoms, or other clinical measures in schizophrenia, the investigators added.
One limitation of the study was possible recall bias in the measure of trait depression, the authors said. In addition, patients who were on antidepressant medication had higher levels of trait depression.
The authors reported no relevant financial disclosures. The study was funded by a grant from the National Institutes of Health.
Persistent depression, or “trait” depression, was significantly higher in patients with schizophrenia than in controls, and was associated with more severe psychosis, a study showed.
Trait depression was not, however, associated with cognitive impairment or decreased white matter integrity, wrote Dr. Joshua J. Chiappelli and his colleagues.
Characterized by “the tendency to experience negative emotions and distressing thoughts” consistently over time, trait depression is distinct from state depression, which includes only current symptoms, said the investigators, who are affiliated with the Maryland Psychiatric Research Center at the University of Maryland in Baltimore.
The study authors examined the association of trait depression with cognitive deficits, functional capacity impairment, and white matter integrity in 126 patients and 151 controls recruited from the Maryland Psychiatric Research Center. Participants completed the Maryland Trait and State Depression (MTSD) questionnaire, which asked 36 questions about the frequency of depressive symptoms over the past week (state questions) and over the course of adult life (trait questions). Cognition was assessed using the Digit Symbol Coding task of the Wechsler Adult Intelligence Scale and the Digital Sequencing task from the Brief Assessment of Cognition in Schizophrenia.
White matter integrity was determined by the measure of fractional anistropy (FA) on a diffusion MRI (Schizophr. Res. 2014;159:243-8).
Severity of both trait and state depression in schizophrenia patients was significantly and positively associated with scores on the Brief Psychiatric Rating Scale (rho = 0.246, P = .005; rho = 0.312, P <.001, respectivley). However, a higher MTSD score was not associated with severe cognitive deficits; in fact, severe trait depression was significantly associated with working memory, processing speed, and functional capacity (rho = 0.186, P = .044; rho=0.206, P = .024; rho = 0.220, P = .017, respectively).
Whole brain FA values were higher in controls than in patients with schizophrenia (FA = 11.86, P = .001). In addition, higher trait depression scores were significantly associated with higher FA values in schizophrenia patients.
“These findings appear paradoxical, especially when examined in comparison to major depressive disorder,” as severity is typically linked to worse cognition, the study authors wrote.
These findings “raise an interesting question on whether trait depression is a relatively separate clinical domain,” compared with major depressive symptoms, or other clinical measures in schizophrenia, the investigators added.
One limitation of the study was possible recall bias in the measure of trait depression, the authors said. In addition, patients who were on antidepressant medication had higher levels of trait depression.
The authors reported no relevant financial disclosures. The study was funded by a grant from the National Institutes of Health.
Persistent depression, or “trait” depression, was significantly higher in patients with schizophrenia than in controls, and was associated with more severe psychosis, a study showed.
Trait depression was not, however, associated with cognitive impairment or decreased white matter integrity, wrote Dr. Joshua J. Chiappelli and his colleagues.
Characterized by “the tendency to experience negative emotions and distressing thoughts” consistently over time, trait depression is distinct from state depression, which includes only current symptoms, said the investigators, who are affiliated with the Maryland Psychiatric Research Center at the University of Maryland in Baltimore.
The study authors examined the association of trait depression with cognitive deficits, functional capacity impairment, and white matter integrity in 126 patients and 151 controls recruited from the Maryland Psychiatric Research Center. Participants completed the Maryland Trait and State Depression (MTSD) questionnaire, which asked 36 questions about the frequency of depressive symptoms over the past week (state questions) and over the course of adult life (trait questions). Cognition was assessed using the Digit Symbol Coding task of the Wechsler Adult Intelligence Scale and the Digital Sequencing task from the Brief Assessment of Cognition in Schizophrenia.
White matter integrity was determined by the measure of fractional anistropy (FA) on a diffusion MRI (Schizophr. Res. 2014;159:243-8).
Severity of both trait and state depression in schizophrenia patients was significantly and positively associated with scores on the Brief Psychiatric Rating Scale (rho = 0.246, P = .005; rho = 0.312, P <.001, respectivley). However, a higher MTSD score was not associated with severe cognitive deficits; in fact, severe trait depression was significantly associated with working memory, processing speed, and functional capacity (rho = 0.186, P = .044; rho=0.206, P = .024; rho = 0.220, P = .017, respectively).
Whole brain FA values were higher in controls than in patients with schizophrenia (FA = 11.86, P = .001). In addition, higher trait depression scores were significantly associated with higher FA values in schizophrenia patients.
“These findings appear paradoxical, especially when examined in comparison to major depressive disorder,” as severity is typically linked to worse cognition, the study authors wrote.
These findings “raise an interesting question on whether trait depression is a relatively separate clinical domain,” compared with major depressive symptoms, or other clinical measures in schizophrenia, the investigators added.
One limitation of the study was possible recall bias in the measure of trait depression, the authors said. In addition, patients who were on antidepressant medication had higher levels of trait depression.
The authors reported no relevant financial disclosures. The study was funded by a grant from the National Institutes of Health.
FROM SCHIZOPHRENIA RESEARCH
Key clinical point: “Trait depression appears to be a highly relevant clinical domain in the care of patients with schizophrenia.”
Major finding: Severity of both trait and state depression in schizophrenia patients was significantly and positively associated with scores on the Brief Psychiatric Rating Scale (rho = 0.246, P = .005; rho = 0.312, P <.001, respectively).
Data source: A study of 126 patients and 151 controls recruited from the Maryland Psychiatric Research Center.
Disclosures:The authors reported no conflicts of interest. The study was funded by a grant from the National Institutes of Health.
CDC Ebola resources for parents and families
Children’s needs differ significantly from the needs of adults, especially when it comes to handling dire situations like the current Ebola outbreak in West Africa that has resulted in a few cases in the United States.
Children may be at increased risk for developing the infection if they have recently traveled to one of the countries experiencing an outbreak. However, since children are very unlikely to be caregivers or participate in funeral activities that raise the risk of exposure, the chances of a child in the United States developing Ebola is very low, according to the Centers for Disease Control and Prevention. It is important to keep in mind that the virus can be transmitted only through direct contact with an Ebola patient when they are symptomatic.
Because information about Ebola can be scary and alarming for children, it is important for parents, schools, and healthcare providers to recognize and address the developmental and psychological needs of children to help them better understand facts about the illness and their risk of exposure. It is also important for health care providers to be prepared just in case the need arises to address a potential Ebola case.
The CDC recommends the following resources to guide families and others who work with children:
1. What You Need to Know About Ebola
2. Ebola: What Parents Need to Know
3. How to Discuss Ebola with Your Children
For schools and child care centers:
Interim U.S. Guidance for Monitoring and Movement of Persons with Potential Ebola Virus Exposure
Children’s needs differ significantly from the needs of adults, especially when it comes to handling dire situations like the current Ebola outbreak in West Africa that has resulted in a few cases in the United States.
Children may be at increased risk for developing the infection if they have recently traveled to one of the countries experiencing an outbreak. However, since children are very unlikely to be caregivers or participate in funeral activities that raise the risk of exposure, the chances of a child in the United States developing Ebola is very low, according to the Centers for Disease Control and Prevention. It is important to keep in mind that the virus can be transmitted only through direct contact with an Ebola patient when they are symptomatic.
Because information about Ebola can be scary and alarming for children, it is important for parents, schools, and healthcare providers to recognize and address the developmental and psychological needs of children to help them better understand facts about the illness and their risk of exposure. It is also important for health care providers to be prepared just in case the need arises to address a potential Ebola case.
The CDC recommends the following resources to guide families and others who work with children:
1. What You Need to Know About Ebola
2. Ebola: What Parents Need to Know
3. How to Discuss Ebola with Your Children
For schools and child care centers:
Interim U.S. Guidance for Monitoring and Movement of Persons with Potential Ebola Virus Exposure
Children’s needs differ significantly from the needs of adults, especially when it comes to handling dire situations like the current Ebola outbreak in West Africa that has resulted in a few cases in the United States.
Children may be at increased risk for developing the infection if they have recently traveled to one of the countries experiencing an outbreak. However, since children are very unlikely to be caregivers or participate in funeral activities that raise the risk of exposure, the chances of a child in the United States developing Ebola is very low, according to the Centers for Disease Control and Prevention. It is important to keep in mind that the virus can be transmitted only through direct contact with an Ebola patient when they are symptomatic.
Because information about Ebola can be scary and alarming for children, it is important for parents, schools, and healthcare providers to recognize and address the developmental and psychological needs of children to help them better understand facts about the illness and their risk of exposure. It is also important for health care providers to be prepared just in case the need arises to address a potential Ebola case.
The CDC recommends the following resources to guide families and others who work with children:
1. What You Need to Know About Ebola
2. Ebola: What Parents Need to Know
3. How to Discuss Ebola with Your Children
For schools and child care centers:
Interim U.S. Guidance for Monitoring and Movement of Persons with Potential Ebola Virus Exposure
FDA: Practice caution when mixing meds and supplements
People often take medications and dietary supplements together without a second thought. But according to the Food and Drug Administration, it may be wise to consider the possible effects of combining the two in order to avoid unintended consequences.
Some dietary supplements affect the potency of prescription and over-the-counter medications by changing the way the drug is absorbed, metabolized, and/or excreted, writes the FDA’s Robert Mozersky. For instance, the herbal supplement St. John’s wort can diminish the effectiveness of several drugs used to treat HIV/AIDS, heart disease, and depression, among others. And warfarin, a blood-thinning drug, may lead to stomach bleeding when combined with other blood thinners such as ginkgo biloba or aspirin.
A Centers for Disease Control and Prevention survey found that 34% of respondents reported taking some kind of dietary supplement with a prescription medicine. It may be fine to take supplements to help with nutrient intake, but dietary supplements should not be used a substitute for healthy foods that contain the same nutrients, the FDA warned.
Additionally, special care should be taken with children, because of variations in metabolism at different ages.
The FDA offers the following tips with regard to medications and dietary supplements:
1. Bring a list of all medications and supplements you are taking along with you to doctor appointments, including details about dosage and frequency.
2. Consult with your doctor before adding a new supplement to your routine.
3. Inform your doctor about any major changes in health status, such as pregnancy, breastfeeding, or surgery.
For more information, visit the FDA website.
People often take medications and dietary supplements together without a second thought. But according to the Food and Drug Administration, it may be wise to consider the possible effects of combining the two in order to avoid unintended consequences.
Some dietary supplements affect the potency of prescription and over-the-counter medications by changing the way the drug is absorbed, metabolized, and/or excreted, writes the FDA’s Robert Mozersky. For instance, the herbal supplement St. John’s wort can diminish the effectiveness of several drugs used to treat HIV/AIDS, heart disease, and depression, among others. And warfarin, a blood-thinning drug, may lead to stomach bleeding when combined with other blood thinners such as ginkgo biloba or aspirin.
A Centers for Disease Control and Prevention survey found that 34% of respondents reported taking some kind of dietary supplement with a prescription medicine. It may be fine to take supplements to help with nutrient intake, but dietary supplements should not be used a substitute for healthy foods that contain the same nutrients, the FDA warned.
Additionally, special care should be taken with children, because of variations in metabolism at different ages.
The FDA offers the following tips with regard to medications and dietary supplements:
1. Bring a list of all medications and supplements you are taking along with you to doctor appointments, including details about dosage and frequency.
2. Consult with your doctor before adding a new supplement to your routine.
3. Inform your doctor about any major changes in health status, such as pregnancy, breastfeeding, or surgery.
For more information, visit the FDA website.
People often take medications and dietary supplements together without a second thought. But according to the Food and Drug Administration, it may be wise to consider the possible effects of combining the two in order to avoid unintended consequences.
Some dietary supplements affect the potency of prescription and over-the-counter medications by changing the way the drug is absorbed, metabolized, and/or excreted, writes the FDA’s Robert Mozersky. For instance, the herbal supplement St. John’s wort can diminish the effectiveness of several drugs used to treat HIV/AIDS, heart disease, and depression, among others. And warfarin, a blood-thinning drug, may lead to stomach bleeding when combined with other blood thinners such as ginkgo biloba or aspirin.
A Centers for Disease Control and Prevention survey found that 34% of respondents reported taking some kind of dietary supplement with a prescription medicine. It may be fine to take supplements to help with nutrient intake, but dietary supplements should not be used a substitute for healthy foods that contain the same nutrients, the FDA warned.
Additionally, special care should be taken with children, because of variations in metabolism at different ages.
The FDA offers the following tips with regard to medications and dietary supplements:
1. Bring a list of all medications and supplements you are taking along with you to doctor appointments, including details about dosage and frequency.
2. Consult with your doctor before adding a new supplement to your routine.
3. Inform your doctor about any major changes in health status, such as pregnancy, breastfeeding, or surgery.
For more information, visit the FDA website.